A multifaceted analysis of HIV-1 protease multidrug resistance phenotypes Please share
advertisement

A multifaceted analysis of HIV-1 protease multidrug
resistance phenotypes
The MIT Faculty has made this article openly available. Please share
how this access benefits you. Your story matters.
Citation
Doherty, Kathleen M. et al. “A Multifaceted Analysis of HIV-1
Protease Multidrug Resistance Phenotypes.” BMC Bioinformatics
12.1 (2011): 477. Web.
As Published
http://dx.doi.org/10.1186/1471-2105-12-477
Publisher
BioMed Central Ltd.
Version
Final published version
Accessed
Wed May 25 18:32:06 EDT 2016
Citable Link
http://hdl.handle.net/1721.1/70131
Terms of Use
Creative Commons Attribution
Detailed Terms
http://creativecommons.org/licenses/by/2.0
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
RESEARCH ARTICLE
Open Access
A multifaceted analysis of HIV-1 protease
multidrug resistance phenotypes
Kathleen M Doherty1, Priyanka Nakka1, Bracken M King2, Soo-Yon Rhee3, Susan P Holmes4, Robert W Shafer3 and
Mala L Radhakrishnan1*
Abstract
Background: Great strides have been made in the effective treatment of HIV-1 with the development of secondgeneration protease inhibitors (PIs) that are effective against historically multi-PI-resistant HIV-1 variants.
Nevertheless, mutation patterns that confer decreasing susceptibility to available PIs continue to arise within the
population. Understanding the phenotypic and genotypic patterns responsible for multi-PI resistance is necessary
for developing PIs that are active against clinically-relevant PI-resistant HIV-1 variants.
Results: In this work, we use globally optimal integer programming-based clustering techniques to elucidate multiPI phenotypic resistance patterns using a data set of 398 HIV-1 protease sequences that have each been
phenotyped for susceptibility toward the nine clinically-approved HIV-1 PIs. We validate the information content of
the clusters by evaluating their ability to predict the level of decreased susceptibility to each of the available PIs
using a cross validation procedure. We demonstrate the finding that as a result of phenotypic cross resistance, the
considered clinical HIV-1 protease isolates are confined to ~6% or less of the clinically-relevant phenotypic space.
Clustering and feature selection methods are used to find representative sequences and mutations for major
resistance phenotypes to elucidate their genotypic signatures. We show that phenotypic similarity does not imply
genotypic similarity, that different PI-resistance mutation patterns can give rise to HIV-1 isolates with similar
phenotypic profiles.
Conclusion: Rather than characterizing HIV-1 susceptibility toward each PI individually, our study offers a unique
perspective on the phenomenon of PI class resistance by uncovering major multidrug-resistant phenotypic
patterns and their often diverse genotypic determinants, providing a methodology that can be applied to
understand clinically-relevant phenotypic patterns to aid in the design of novel inhibitors that target other rapidly
evolving molecular targets as well.
Background
For over fifteen years, drug resistance has been a primary challenge in the effective treatment of HIV, and
our understanding of resistance mechanisms has evolved
along with the virus itself as new therapies have
emerged[1-6]. Thanks to worldwide efforts to tackle
HIV drug resistance, many successful treatment regimens have been developed, including combination
therapies[7,8] such as the Highly Active Anti-Retroviral
Therapy (HAART) regimens[9,10], but treatment
options have been uncertain for patients who fail these
* Correspondence: mradhakr@wellesley.edu
1
Department of Chemistry, Wellesley College, 106 Central Street, Wellesley,
MA 02481, USA
Full list of author information is available at the end of the article
regimens due to the accumulation of drug-resistant
mutations[11]. More recently, in addition to targeting
molecules other than HIV-1 reverse transcriptase (RT)
and protease, second-generation RT and protease inhibitors (PIs) have been developed such that they remain
potent against variants resistant to first-generation inhibitors. Specifically, tipranavir[12] and darunavir[13], the
two PIs most recently approved for clinical use, have
been shown to be potent against viruses harboring multidrug resistance mutations such as V82A and L90M, in
the cases of both tipranavir and darunavir[13-16], and
V82T or I84V in the case of darunavir[13,16]. However,
even these drugs have been shown to lose potency in
the presence of certain mutations or mutation patterns
[14,17-20]. In fact, the existence of HIV-1 variants
© 2011 Doherty et al; licensee BioMed Central Ltd. This is an Open Access article distributed under the terms of the Creative Commons
Attribution License (http://creativecommons.org/licenses/by/2.0), which permits unrestricted use, distribution, and reproduction in
any medium, provided the original work is properly cited.
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
showing resistance to all clinically-approved inhibitors
highlights the issue of cross resistance, or the existence
of mutation patterns arising from a certain therapeutic
regimen that simultaneously cause resistance to other
drugs as well. Cross resistance among HIV-1 PIs has
been studied[21-26] and reviewed[1,4,27-29] extensively
for over a decade, with several key mutation patterns
thought to confer cross resistance to the vast majority
of PIs. Consequently, one strategy is to take advantage
of the lack of cross resistance when a mutation confers
resistance to one PI but maintains susceptibility to other
PIs. For example, D30N and I50L are associated with
resistance specifically to either nelfinavir and atazanavir,
respectively, but such mutations do not greatly reduce
susceptibility (and I50L actually increases susceptibility)
to other PIs[30-33]. Sequential or simultaneous administration of regimens that are each potent against variants
toward which the other fails may be a potential strategy
to prevent drug resistance and treatment failure[34]. In
light of the combinatorial number of both potential
treatment regimens and potential mutation patterns, it
is becoming increasingly important to understand both
the major mutation patterns conferring resistance on
the genotypic level as well as the major phenotypic patterns of cross resistance - or lack thereof - of these
mutation patterns toward the nine clinically-approved
PIs.
Computational analyses have played a key role in
increasing our understanding of the genotypic and phenotypic patterns of HIV drug resistance and our ability
to predict drug response phenotype from genotype
[35-37]. The large amount of publicly available data has
greatly facilitated these analyses[35,38]. Several computational studies have analyzed new or existing data to
identify mutations associated with one or more PI or
RT drugs[39-48]. Some studies have presented longitudinal mutagenetic tree or mutation pathway models for
the temporal appearances and contingencies of such
mutations[49-52]. Others have uncovered pairs or clusters of correlated mutations associated with PI or RT
therapy through direct enumeration, statistical or information-theory based methods, clustering, or a combination of techniques[39,43-46,51,53-63]. One particularly
successful application of computational analysis is the
accurate prediction of drug resistance (phenotype) often measured as a fold-change in IC 50 of a drug
toward the mutant vs. wild-type - of a target variant
given its amino acid sequence (genotype). Many
approaches have been used to create prediction models,
including regression-based methods[26,64-69], decision
trees[70], and other machine learning methods, including artificial neural networks, support vector machines,
and others[67,71-74]. Several studies have also comparatively evaluated or combined methods to improve
Page 2 of 19
accuracy[67,72,73,75]. Models have also been created for
predicting drug resistance phenotype[76] and virological
success or failure[77-80] resulting from combination
therapies. In addition to these data-driven approaches,
structure-based approaches for predicting drug response
have also been developed, often in conjunction with the
bioinformatics-based approaches[66,81,82]. Taken
together, the large collection of available predictive
methods still require interpretation and comparison
when making patient treatment decisions[83,84], but
overall they have been valuable tools both for practical
decision-making and for increasing scientific
understanding.
The many computational studies of HIV genotypephenotype data therefore demonstrate the power of
uncovering patterns in data, with each study providing a
valuable perspective on important features of HIV drug
resistance. However, the vast majority of studies have
offered a perspective at the genotypic level first - that is,
they look for patterns on the genotypic level that correlate with phenotypic responses, usually to one drug or
drug regimen at a time, in turn. To our knowledge, a
rigorous cluster-based analysis of genotype-phenotype
data that first uncovers patterns within the complete
phenotypic space and then determines representative
genotypes giving rise to the multidrug response phenotypes has yet to be done. The goal of this study is therefore to provide this unique, simultaneous view into the
existing phenotypic patterns amongst all the HIV-1 PIs,
as such a perspective can provide novel insights into the
major combinations of PIs for which cross resistance
can occur.
In this work, we analyze phenotypic drug resistance
patterns by considering experimental resistance data of
398 clinical isolates of HIV-1 protease measured against
the nine clinically-approved HIV-1 protease inhibitors.
To determine phenotypic drug resistance patterns
toward all nine drugs, a constrained k-medoids clustering method implemented via integer programming was
employed. Clusters were validated by quantifying their
ability to predict a sequence’s level of resistance toward
one drug knowing the sequence’s level of resistance
toward other drugs. The selection of representative genotypic sequences from each cluster indicated mutations
associated with common patterns of phenotypic resistance and can serve as a “panel” of mutants that collectively represent clinically important variants.
Furthermore, our direct analysis of phenotypic space
allowed us to determine that the virus often utilizes
multiple genotypes to achieve similar phenotypic patterns of multidrug resistance. We also show that certain
drugs show highly correlated antiviral activities, while
other drugs - especially tipranavir - have unique
responses. Finally, information theoretic approaches
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 3 of 19
were employed to determine amino acid positions and
identities within HIV-1 protease that are most informative for selection into a phenotypic cluster. Taken
together, this work provides a simplified framework for
understanding major drug resistance patterns toward
clinically-approved HIV protease inhibitors and the
mutation patterns that best characterize them.
Table 1 Scaling and capping of raw fold-change values.
Drug
Base
Max
Min
RTV
2.5
7.30
-1.76
NFV
3.6
4.99
-0.94
ATV
5.2**
3.97
-0.73
APV
6.6*
3.17
-0.85
IDV
10**
2.70
-0.52
Methods
LPV
22.3*
2.00
-0.52
Data set
SQV
5.3*
4.16
-0.97
We analyzed 398 HIV-1 isolates in the HIV Drug Resistance Database[38] (HIVDB) for which cell-based in
vitro PI susceptibility testing had been performed by the
PhenoSense (Monogram, South San Francisco, CA)
assay[85]. Susceptibility was quantified by the Monogram-measured fold-change[85], defined as the ratio of
the 50% inhibitory concentration (IC50) of the isolate to
the IC50 of a wild-type control. Only those isolates for
which susceptibility had been tested against all nine
clinically-approved inhibitors were included. The nine
inhibitors considered were amprenavir (APV), atazanavir
(ATV), indinavir (IDV), lopinavir (LPV), nelfinavir
(NFV), ritonavir (RTV), saquinavir (SQV), tipranavir
(TPV), and darunavir (DRV). The data set size was limited by the availability of isolates tested for DRV susceptibility. Many clinical isolates contained mixtures at
one or more amino acid positions. Due to the limited
data, mixtures were not excluded from the data set. In
this work, we will refer to clinical isolates as
“sequences,” though we recognize that some contain
mixtures at certain positions.
To estimate the degree to which mutation frequencies
in the genotype/phenotype (n = 398) data set are representative of true population frequencies, the frequencies
of non-polymorphic treatment-selected mutations within
non-WT sequences were compared between a larger
genotype-only data set of 12,290 sequences[38] and the
data set used here. Reasonable correlation (Spearman’s r
= 0.88) was found between the data sets (Fig. S1, Additional File 1).
Fold-change values were log-scaled such that for a
given drug, a constant factor of fold-change is represented by a constant numerical difference. Because the
relationship between fold-change and clinical response
is different for each drug, scaled values were standardized so that they represent predicted clinical responses,
the phenotype of interest in this work. To do this, the
logarithm base used for the log scaling of each drug was
set to either the Monogram biological cutoff, the geometric mean of the Monogram lower and upper clinical
cutoffs, or the single clinical cutoff provided, depending
on which type of cutoff was available for a particular
drug (Table 1). Monogram biological cutoffs are defined
as the fold-change values below which 99% of the WT
TPV
4.0*
4.82
-1.16
DRV
30.0*
1.83*
-0.47*
The bases used for log scaling each drug were informed by Monogram
biological and clinical cutoffs as described in the text. Unstarred bases are
equal to the available Monogram biological cutoffs; singly-starred bases were
calculated as the geometric mean of lower and upper clinical cutoffs. Doublestarred bases are equal to the single available Monogram clinical cutoff. For
all drugs, scaled values were capped to the least extreme minima and
maxima (those of DRV, shown in bold and starred). Maxima in the table were
generally used when assay upper limits had been reached, representing that
the actual fold resistance was higher than the assay could accurately
determine. The maximum measurable fold-change can vary for a given drug
between isolates, but due to the cap being well below their ranges of
maximum fold-change values, our results are entirely unaffected by variation
for most drugs; the upper fold-change limits for DRV and LPV may have at
times been slightly lower than the upper cap used here, but as a check for
robustness, preliminary results were generated with varying upper caps and
were qualitatively similar to those shown here.
sequences reside, and therefore fold-changes above this
value likely have decreased susceptibility. Monogram
lower and upper clinical cutoffs are fold-change values
at which reduced clinical response and unlikely clinical
response occur for a given drug, respectively. Ritonavirboosted cutoff values were used when available. After
log-scaling, scaled resistance values of 1 and 0 qualitatively signify decreased susceptibility and susceptibility
equal to WT, respectively, for all drugs. To equalize the
range of variation in the scaled resistances for each drug
and to confine variation to a clinically meaningful range,
we capped the maximal and minimal scaled resistances
of all drugs to the least extreme value of these among
the nine inhibitors – those of DRV (Table 1). The upper
cap of the scaled values (1.83) corresponded to a raw
fold-change value for DRV of 500, the upper-limit value
used when the fold-change toward DRV was greater
than the upper limit of the assay. Sequences with scaled
resistances equal to the capped values are therefore considered either highly resistant (upper cap) or potentially
hypersusceptible (lower cap). An interpretation of scaled
resistance values is in Table 2.
Clustering
Sequences were clustered based on their drug-resistance
phenotypes, quantified by scaled resistance values. A
globally-optimal constrained k-medoids clustering
approach was implemented via a linear integer program
similar to other variations of integer and mixed-
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 4 of 19
Table 2 Interpretation of the scaled resistance values
used throughout this work.
Scaled
resistance
Interpretation
Resistance
Score
>1.5
Highly resistant
4
1 to 1.5
Decreased susceptibility
3
0.5 to 1
Slightly decreased susceptibility
2
0 to 0.5
No resistance
1
<= 0
No resistance or
hypersusceptibility
0
programming-based k-means and k-medoids clustering
formulations[86-89]. The k-medoids approach was chosen after exploration of multiple clustering methods (kmeans, hierarchical, and a method based on a tight clustering approach[90]), as it was deterministic, provably
optimal, and allowed for the easy implementation of
hard constraints, which we felt were crucial here for
generating clusters that were phenotypically similar
across all drugs.
The clustering method was as follows: First, each
sequence was assigned a point in a 9-dimensional space
whose coordinates are the scaled resistances toward the
nine inhibitors. From these points, a distance matrix
was generated, in which element dij is the Euclidean 2norm distance between the ith and jth sequences. The
goal was to select k cluster centers (medoids) from
within the data set and assign each point in the data set
to one of these k medoids such that the sum of the distances from points to their assigned medoids was
minimized.
Constraints were placed on this optimization to guarantee phenotypic similarity within a cluster, as the goal
of this work is for the clusters to represent major phenotypic patterns. First, a hard constraint was set to
bound the distance between any cluster member and its
medoid to be less than or equal to a specified value, C.
Secondly, a hard constraint was set to cap the maximum
infinity norm of the distance between any cluster member and its medoid to a specified value, C∞. Such a constraint prohibits grouping together two sequences that
are highly similar toward 8 drugs but differ qualitatively
in their level of resistance toward only one drug - an
undesirable outcome if we wish for our clusters to highlight major cross resistance patterns.
k, the number of clusters, is determined by feasibility;
it is the minimum value of clusters for which the constraints are satisfied. In this work we use C = 0.95 and
C∞ = 0.58; the value of C = 0.95 occurs roughly at the
“elbow”[91] or “kink”[92] of a plot of the minimum k
needed as a function of tightness (C and C∞) (Fig. S2,
Additional File 1), suggesting that it allows a reasonable
balance between maintaining both a low number of
clusters and adequately tight clusters. A C ∞ of 0.58
guarantees that a given cluster members’ scaled resistances toward any given drug cannot vary by more than
2 C∞ = 1.16; there will not be a pair of cluster members
in which one sequence shows no resistance to a given
drug while another shows high levels of resistance (see
Table 2). Higher values of C∞ would make clusters too
diffuse along individual dimensions, preventing their
interpretation as clinically-relevant phenotypic patterns.
Lower values were found to be too restrictive and generated additional clusters with redundant patterns (data
not shown). To check for robustness of clustering as a
function of these parameters, C and C∞ were each varied in turn up to +/-0.05 units in increments of 0.025.
Qualitative phenotypic patterns remained very similar,
and pairs of sequences that were clustered together in
the original clustering remained together an average of
71% as these parameters were varied.
Figure S3 (Additional File 1) is a plot of the number
of clusters (k) vs. data set size, using random subsets of
the data. As our data set is currently not large enough
to show robust convergence (k increases with increasing
data set size), the quantitative results that are affected
by data set size are to be considered preliminary; more
data could allow for more robust convergence in future
studies and would increase confidence in the quantitative conclusions.
The integer programming formulation used is shown
in Supplementary Methods (Additional File 1). All integer programs in this work were implemented using the
GAMS interface (GAMS Development Corporation,
Washington, D.C.) and were solved using CPLEX 11.0.0
(IBM ILOG, Armonk, NY).
Validation
The clustering was validated by its effectiveness (relative
to controls) in predicting the level of drug resistance of
a sequence to one drug based on the sequence’s levels
of drug resistance toward other drugs, using the following n-fold cross-validation procedure[92]:
remove each sequence (in turn) from the data set label it sequence “A.”
cluster the remaining sequences using the above
method.
choose one of the nine drugs and eliminate its phenotypic data for sequence “A”.
Assign sequence “A” to the cluster to whose centroid
it is closest, based on 8-dimensional distance (i.e.
removing the eliminated drug’s dimension)
Predict the level of drug resistance of sequence A
toward the eliminated drug to equal the cluster centroid’s scaled resistance value for the eliminated drug.
Based on this value, classify sequence A with a resistance score from 0-4 (Table 2).
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
For each drug, the total RMS error and the percent
correctly classified after leaving out each sequence in
turn was compared to two controls:
Control 1 ("Random Control”): To predict the resistance of a sequence toward a drug, randomly choose a
value from the distribution of scaled resistances in the
data set toward the particular drug, and classify it using
the corresponding resistance score. This control
assumes that the level of resistances between drugs is
not correlated.
Control 2 ("Average Control”): To predict the resistance of a sequence toward a given drug, simply use the
mean of the levels of sequence “A’s” scaled resistances
to the other eight drugs, and classify with the corresponding resistance score. This control assumes that
resistances toward the nine drugs are highly correlated.
Genotypic Analyses
In the absence of amino acid mixtures at positions
within isolates, the genotypic distance between any two
sequences was defined simply as the number of positions at which their amino acid sequence differed. For
some analyses, all 99 protease positions were considered.
To reduce noise due to polymorphic positions in certain
analyses, only 21 positions that have been associated
with resistance or drug treatment by previous statistical
learning or analysis methods [26,39,48] were considered,
unless otherwise noted: 10, 24, 30, 32, 33, 43, 46, 47, 48,
50, 53, 54, 71, 73, 74, 76, 82, 83, 84, 88, and 90. We
note that there may be unavoidable arbitrariness in the
selection of such a set without considerable initial genotypic-phenotypic analysis (which was exactly what we
sought to avoid in this study), and in the course of our
research we tried multiple sets, allowing us to check for
robustness.
To account for mixtures in isolates, the contribution
toward the genotypic difference between two sequences
due to a position, dm, was defined in the general case as
follows:
dm = 1 − (c/max(s))
where “c” is the number of amino acids that the isolates have in common at that position, and max(s) is the
number of amino acids in the mixture with the greater
number of amino acids at that position. As an example,
if one isolate contained a mixture of leucine and
methionine at a position and another contained only
leucine, then dm for this position would be (1-(1/2)) =
1/2.
Intracluster genotypic or phenotypic variability was
estimated as the average of all the pairwise genotypic or
phenotypic distances. A bootstrapping procedure was
used to generate p-values to assess statistical significance
Page 5 of 19
of either distance for selected clusters. Random clusters
of a size equal to the considered cluster were selected
with replacement from the unclustered data, and the
distance metrics were calculated. This procedure was
repeated 10,000 times to generate distributions for both
genotype and phenotype distances, from which p-values
were calculated. Bootstrap studentized statistics were
obtained by dividing the difference between a value and
the bootstrapped distribution mean by the standard
deviation of the distribution.
From each cluster, representative sequences were
selected. For genotypically diverse clusters, we wished to
select multiple representative sequences from each cluster to highlight genotypic diversity. To that end, constrained k-medoids optimizations were run on each
cluster using integer programming; the resulting
medoids became the representative sequences. For each
phenotypic cluster, the minimum value of k was determined such that all sequences within the cluster would
be within a genotypic distance of t i of at least one
medoid. We used a value of ti = 9 when possible, as it
produced one representative sequence for all but the
most diverse clusters (except for other exceptions noted
below), allowing for easy interpretability. Additionally, at
this k, the sum of the distances between each sequence
and its assigned medoid was minimized. Sequences containing mixtures at any of the 21 positions listed above
were excluded from being representative, as were
sequences with any of the 99 amino acid positions
undefined (only 2 within the data set). With this constraint, it becomes possible for phenotypic clusters
(other than single-membered ones containing mixtures
at relevant positions) not to generate any representative
sequences with t i = 9. To account for this, t i was
increased to 10 for clusters 3 and 19 and 10.5 for cluster
10. The integer-programming formulation used here is
shown in Supplementary Methods (Additional File 1).
Sets of sequence positions or amino acid residue identities most informative of overall cluster assignment or
membership in an individual cluster were identified
according to an incremental mutual information (MI)based method described previously (MIST)[93]. Briefly,
the method approximates high-order joint entropies to
determine an optimal small subset of features (e.g., residue positions) that collectively have the highest mutual
information (MI) with a given output (e.g., phenotypic
cluster). These approximated MI values have also been
shown to correlate with classification error and with
exact MI values in analytically solvable systems. First,
the MI between variables of interest was computed,
using the frequencies to estimate probabilities. For each
MI, the bias in the value was estimated by computing
the MI of the pair after randomizing the ordering of the
sequence data for each variable 100 times. Variables
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
whose MI with the outputs exceeded their maximum
shuffled MI were considered statistically significant and
included in subsequent steps; remaining positions were
omitted. Sequence positions or binary mutation variables were then selected incrementally to maximize the
joint-MI (as estimated by MIST) between the set of all
chosen variables and either the cluster assignment or
membership in a specific cluster. Mixtures were not
included in the distributions. Features were added incrementally until all positions or mutations were included,
yielding a full ranking.
Miscellaneous
Data scaling and other matrix manipulations, including
principal component analysis, were done using Matlab
2010a and 2011a (The Mathworks, Natick, MA). Matlab
and Microsoft Excel (Microsoft, Inc., Bellevue, WA)
using VBA were used for figure generation.
Results
Cluster Analysis Reveals Specific Phenotypic Resistance
Patterns Among Clinical Isolates
Globally-optimal k-medoids clustering was used to find
groups of sequences with similar multidrug phenotypes,
using the tightness constraints C and C∞ mentioned in
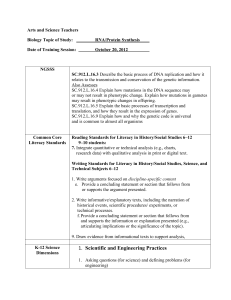
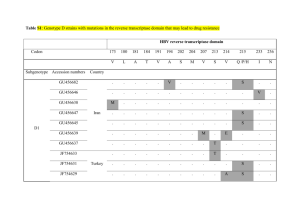
the Methods to enforce thresholds of phenotypic similarity. The clustering yielded 36 multi-membered clusters, along with 14 outliers. Figure 1 shows the resulting
clusters; each cluster is represented as a row, with each
of the colored boxes within the row representing the
resistance score (Table 2) toward the corresponding
drug of the cluster’s centroid (i.e., average phenotype),
according to the legend. At right, representative
sequences are shown for each cluster, with non-WT
amino acid identities shown at selected positions. A listing of mutations at all positions for each representative
sequence is provided as Supplementary Information
(Table S1, Additional File 1). For two clusters (5 and 9),
more than one representative sequence was needed due
to the genotypic diversity.
Generally, the largest clusters were those in which (a)
there was no resistance (or very mild resistance) to any
drug, (b) there was high resistance to all drugs, (c) there
was high resistance toward all drugs except DRV, to
which there was moderate resistance, (d) there was high
resistance toward all drugs except DRV and TPV, (e)
there was resistance toward only NFV and RTV, and (f)
there was high resistance to APV, ATV, NFV, RTV, and
SQV.
The clusters demonstrate that there is often cross
resistance of sequences toward many drugs. Generally,
sequences are most commonly resistant to RTV and
NFV, followed by ATV and SQV, then APV, IND, and
LPV, and finally TPV, and DRV. In general, resistance
Page 6 of 19
to DRV implies resistance to nearly all other drugs, with
a few exceptions: Three clusters showed moderate to
high levels of resistance against all drugs except TPV
(clusters 5, 8, and 12), and two clusters showed moderate to high levels of resistance against all drugs except
SQV (clusters 11 and 15). In both cases, the representative sequences of the clusters each had at least one
mutation that has been associated with hypersusceptibility toward the particular drug in a previous study in
which mutations were the independent variables and
fold-change was the dependent variable[26]. These
mutations include L10F, G48V, I50V, I54L, and L76V in
the case of the clusters with unique susceptibility to
TPV and I47A in the case of the clusters with unique
susceptibility to SQV.
One may ask if grouping 398 sequences into 36 phenotypic clusters and 14 outliers shows that HIV is
exploring a large or small part of the available phenotypic space. To address this question, we repeatedly generated sets of 398 random points within the same ninedimensional scaled space of our data set and clustered
them using the same constraints applied to the true
data set. The average minimum number of clusters
needed over 300 trials was 375, with the smallest number of clusters needed being 357. Clearly, the fact that
only 50 clusters (including outliers) were needed to partition the actual data within the constraints demonstrates that HIV protease is exploring a very small
portion of possible phenotypic space. In fact, due to the
constraints used in the clustering, the volume of 9dimensional phenotypic space occupied by each cluster
must be less than the smaller of either the volume of a
hypersphere of radius C or a hypercube of length 2C∞.
Using our constraint values, the smaller of these is the
former, with a value of ~2.1 volume units. The volume
of clinically-relevant phenotypic space can be calculated
from the maximum and minimum scaled values in
Table 1 to be 1800 volume units. Therefore, only
(2.1*50)/1800 = ~6% of phenotypic space, at best, has
been explored by the considered isolates, compared to
(2.1*375)/1800 = ~44% for a random data set of equal
size.
If a drug is removed from the data set, the minimal
number of clusters needed to represent the phenotypic
diversity must be less than or equal to the minimal
number needed with that drug included. One way to
measure the additional phenotypic diversity provided by
each drug is to remove each drug in turn and re-cluster
using the k-medoids approach under the same distance
constraints. Drugs that, upon removal, greatly reduce
the number of required clusters have phenotypes that
vary somewhat independently from the other drugs.
Drugs that, upon removal, do not greatly reduce the
number of required clusters have phenotypes that vary
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 7 of 19
&
&*
)
)
)
)
)
)
)
)
)
"
"
"
"
"
"
"
"
"
"
'
'-
)
)
)
)
)
)
)
)
'
"
"
"
"
"
"
"
"
"
"
"
(
)
)
)
)
)
)
)
)
'
'
"
"
"
"
)
&%
)
)
)
)
(
(
)
(
(
"
"
"
"
"
"
!
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
*
+
)
)
)
)
)
)
)
&
(
"
"
"
"
"
"
"
"
"
"
+
+
)
)
)
)
(
(
(
)
'
"
"
"
"
"
"
"
"
"
"
"
"
"
"
,
(&
)
)
)
)
)
(
)
'
'
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
-
(
)
)
)
)
)
)
)
%
'
"
"
"
"
.
,
)
)
)
)
(
(
)
'
'
&%
)
)
)
)
'
)
(
)
)
&&
'
)
)
)
)
)
)
%
&'
+
)
)
)
)
'
(
&(
*
)
)
(
(
(
'
&)
&%
)
)
)
'
(
&*
(
)
)
(
)
&+
-
)
)
)
'
&,
(
)
)
)
(
&-
)
)
)
)
&.
)
)
)
'%
-
)
)
'&
*
)
''
'
)
'(
'
)
')
*
'*
(
'+
&(
',
*
'-
)
'.
.
(%
'
(&
('
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
&
"
"
"
"
"
"
"
"
"
"
"
(
'
"
"
"
"
"
"
"
"
"
"
"
"
"
)
%
'
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
'
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
'
)
'
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
(
)
%
'
'
"
"
"
"
"
"
(
(
)
%
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
(
(
'
%
&
"
"
"
"
"
"
"
"
"
"
"
"
"
&
(
(
)
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
(
(
'
'
&
(
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
'
'
'
'
'
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
(
'
(
'
'
&
&
"
"
"
"
"
"
"
"
"
"
"
)
)
'
'
'
'
&
&
"
"
"
"
"
"
"
"
"
"
)
(
(
'
(
&
%
&
"
"
"
"
"
"
"
"
"
"
"
"
"
)
)
)
&
(
&
)
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
(
&
'
(
(
&
%
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
)
'
&
'
&
'
&
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
(
'
'
&
&
'
%
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
)
'
&
'
&
'
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
(
'
&
&
&
&
&
&
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
'
)
'
&
&
&
&
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
)
'
&
&
&
&
&
&
'
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
*
)
(
&
%
&
&
&
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
((
)
'
'
&
%
&
%
&
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
()
,&
&
&
&
%
&
%
&
&
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
(*
+
(
%
&
%
%
%
%
&
&
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
(+
,,
%
%
%
%
%
%
%
%
%
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
!
(,
&
)
)
)
)
)
)
'
(
(
"
"
"
"
"
"
"
"
"
"
"
"
(-
&
)
)
'
'
(
(
)
%
&
"
"
"
"
"
"
"
"
"
"
"
(.
&
)
)
&
)
(
(
'
%
'
)%
&
)
)
)
(
&
&
)
%
&
"
"
"
"
"
"
"
)&
&
)
)
(
(
&
'
%
)
&
"
"
"
"
)'
&
)
(
%
'
(
(
'
%
&
"
"
"
"
)(
&
)
(
'
&
&
&
%
)
&
"
"
"
"
))
&
(
'
&
(
'
(
%
&
&
"
"
"
"
"
)*
&
)
'
&
(
&
&
&
&
&
)+
&
'
&
)
&
%
&
%
%
%
),
&
%
'
%
'
&
&
%
&
&
)-
&
%
)
&
&
%
%
%
&
%
).
&
%
)
&
&
&
%
%
%
%
*%
&
%
%
)
%
%
%
%
%
%
" "
"
"
!
&% )+ *)
,& ,+ -)
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
"
!
&%
(' )+
), ,&
"
"
"
"
"
"
"
!
&% ((
)+ *%
-'
"
"
"
"
"
"
"
"
"
"
"
!(% (( ,& --
"
"
"
"
"
"
"
"
"
"
"
!*%
,& ,( -'
!! !!
!! !
Figure 1 Optimal phenotypic clustering of clinical data set. The optimal set of clusters obtained by using constrained k-medoids clustering
with integer programming. 36 multi-membered clusters and 14 single-member “clusters”, or outliers, were obtained. Each row represents one
cluster. The second column indicates the cluster size. The next 9 columns represent the cluster centroids’ phenotypic drug resistance scores,
colored according to the legend. The columns at right indicate mutations in the sequence selected to represent the cluster at selected positions.
Because isolates with mixtures at any of the specified positions were not allowed to represent a cluster, certain single-membered clusters do not
have a representative “sequence.” The representative sequences chosen for clusters 29, 31, 34, and 36 show no mutations at the positions listed
here, but they have substitutions at other positions (Table S1, Additional File 1).
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 8 of 19
predictably with (though not necessarily in a correlated
manner with) the remaining drugs. When this analysis
was carried out, it was found that removal of TPV
reduced the number of needed clusters by the most
(from 50 to 31), suggesting that TPV’s response toward
sequences varies somewhat independently from other
drugs. In other words, TPV might show varied, graded
responses toward certain groups of sequences toward
which other drugs show relatively constant responses.
Removal of ATV, SQV, or APV also reduced the number of needed clusters by over 10 (from 50 to 37, 38,
and 38, respectively). Removal of LPV, DRV, NFV, RTV,
or IDV reduced the number of required clusters the
least (to 44, 44, 43, 43, and 41, respectively) suggesting
that their scaled resistances either vary predictably with
those of the other drugs or do not vary appreciably in
general.
Phenotypic clustering allows for potentially improved
prediction of unknown drug phenotypes given
phenotypic information for other drugs
Our results indicate that a small portion of the full
phenotypic space has been explored by the virus,
assuming a representative data set; consequently, one
may be able to successfully predict resistance to a
given inhibitor given resistance data toward other inhibitors, without knowing any genotypic information. To
test this hypothesis, we used a cross-validation procedure in which each sequence from the data set was
removed in turn and the sequence’s resistance toward
each drug was estimated based on a clustering assignment using the other eight resistance phenotypes (see
Methods). Pairs of sequences that were clustered
together in the original clustering remained together
an average of 99.3% of the time across all n runs of
the validation, not counting runs in which a member
of the pair was excluded in turn, demonstrating the
stability of the clustering during the cross-validation
procedure. The results of the cluster-based prediction
are summarized in Table 3.
Two controls were used for comparison and are
described in the Methods. Control 1 ("Random”), which
randomly reported a value from the distribution of
scaled resistances in the data set toward the particular
drug, was able to correctly categorize resistance 21%36% of the time, depending on the drug. The RMSE’s of
the actual scaled resistance values were often over a
whole unit away, meaning that it would often predict no
resistance when there was in fact resistance, and vice
versa. NFV and RTV were classified correctly most
often; the clustering suggests that this may be because
they were more likely to exhibit either no resistance or
complete resistance, providing a less graded distribution
overall from which to sample.
Control 2 ("Average”), which guessed the “unknown”
phenotype to be the average of the other 8 known phenotypes for the isolate, performed much better overall
than Control 1, categorizing resistance correctly for
more than half of the sequences for ATV, APV, IND,
LPV, and SQV. Its strong performance is additional evidence for the high level of both correlation between
drug responses and cross resistance. Performance was
worse for (1) NFV and RTV, which are often inactive to
viruses toward which other drugs are effective, as Figure
1 indicates, (2) DRV, which, according to Figure 1, often
remains effective toward viruses resistant to other drugs,
Table 3 Cluster-based prediction of phenotypic resistance relative to controls.
With all data
RTV
NFV
ATV
APV
IDV
LPV
SQV
TPV
DRV
29
CTL1 (Random)
% correct
35
36
29
21
22
26
29
31
CTL1 (Random)
RMSE
1.34
1.13
1.21
1.2
1.05
1.01
1.26
0.98
0.76
CTL2 (Average)
% correct
46
43
62
60
62
56
57
47
34
CTL2 (Average)
RMSE
0.60
0.54
0.36
0.34
0.26
0.28
0.41
0.67
0.67
Cluster-based
% correct
81
75
74
70
63
67
65
50
67
Cluster-based
RMSE
0.35
0.34
0.38
0.33
0.29
0.25
0.50
0.71
0.29
RTV
NFV
ATV
APV
IDV
LPV
SQV
TPV
DRV
29
Without nonresistant clusters
CTL1 (Random)
% correct
78
66
45
27
22
29
34
18
CTL1 (Random)
RMSE
0.54
0.68
0.84
0.97
0.86
0.83
1.06
1.00
0.74
CTL2 (Average)
% correct
28
32
49
51
52
43
46
28
11
CTL2 (Average)
RMSE
0.74
0.64
0.45
0.41
0.32
0.34
0.51
0.84
0.84
Cluster-based
% correct
89
82
73
62
55
58
60
34
56
Cluster-based
RMSE
0.26
0.23
0.38
0.40
0.36
0.31
0.62
0.89
0.36
Percent of viruses whose resistance score toward each drug was correctly classified ("% correct”), as well as the RMS error (in scaled resistance units) over all
sequences of the phenotypic difference between predicted and actual phenotype ("RMSE”) using the two controls described in the text ("CTL1 (Random)” and
“CTL2 (Average)” and the cluster-based prediction. The top panel presents results using all 398 sequences, and the bottom panel shows results after removing
the two clusters showing little or no phenotypic resistance to any drug.
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
and (3) TPV, which, as shown above, has less phenotypic similarity to other drugs.
Compared to either control, the cluster-based prediction correctly classified a higher percentage of viruses
for every drug, although the improvement over Control
2 was modest in some cases, with the RMSE’s being
marginally higher in some cases as well, suggesting that
when the cluster-based classification was incorrect, it
was quite different. The improvement in classification
was largest for NFV, RTV, and DRV. Classification rates
overall were well over 50% correct with RMS errors
being fairly small (generally <= 0.5 units away). The
notable exception is TPV, again supporting TPV’s
uniqueness.
The relatively large number of sequences susceptible
to all drugs in our data set might bias the prediction
accuracy of certain methods to be higher than what
would be expected from a data set that contained a
more even distribution of all multidrug phenotypes. To
control for this, we redid the above analysis after having
left out the sequences corresponding to the two clusters
shown in Figure 1 that show no or very little resistance
to all nine drugs (clusters 36 and 34, with 77 and 71
members, respectively). Not surprisingly, Control 1 performs much better with RTV and NFV, as now, nearly
all sequences in the data set are resistant to either drug.
Also unsurprisingly, Control 2 performs worse because
the two clusters that were removed contained sequences
whose responses to all drugs were highly correlated.
Page 9 of 19
The cluster-based classifier still has the highest classification accuracy, but again, the RMSE values were sometimes greater than those for Control 2. Nevertheless,
these results show that an understanding of major phenotypic resistance patterns can allow for reasonable prediction of a sequence’s resistance toward one drug given
resistance information toward other drugs, and the
strong performance of the controls under certain circumstances further highlights the underlying structure
in the resistance patterns.
The accumulation of HIV protease mutations results in a
“path” in phenotypic space
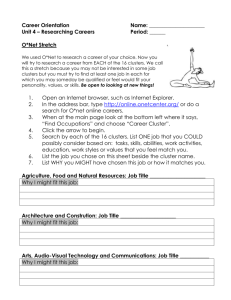
Principal component analysis (PCA) was used to project
the nine-dimensional, columnwise-centered drug-resistance phenotypes of all sequences onto the two dimensions along which there is most variation. Figure 2 is a
plot of the sequences in this two-dimensional space,
colored by the total number of amino acid differences
from consensus-B wild type protease (considering all 99
amino acid positions). The first two principal components are able to capture approximately 90% of the variation in the data, again suggesting that there are large
correlations between drug responses toward the
sequences. As indicated in Table 4, the first principal
component indicates resistance toward all drugs (i.e.,
complete cross resistance), with slightly less resistance
toward TPV and DRV, relative to their means. The second principal component indicates resistance toward
Figure 2 Projection of the phenotypic data onto its first and second principal components. Points are colored by the total number of
amino acid substitutions relative to the consensus B WT sequence, according to the scale at right; a mixture at a position (including those
containing the WT amino acid) is counted as one substitution. The phenotypes and genotypes of selected sequences are indicated. The 9-digit
shorthand phenotypic code used to describe the sequences indicates the resistance score (Table 2) to each of the 9 PIs in the order shown in
Fig. 1: RTV, NFV, ATV, APV, IDV, LPV, SQV, TPV, DRV. All “outlying” sequences are fully listed in Supplementary Information (Fig. S4, Additional File
1).
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 10 of 19
Table 4 The nine principal components in scaled
phenotypic space.
Principal
Component
1
2
Ritonavir 0.39
0.35
0.60 -0.16
Nelfinavir 0.36
0.33
0.22 -0.05 -0.10
Atazanavir 0.39
3
5
6
7
8
9
0.30 -0.37 -0.32 -0.05 -0.07
0.31
0.75 -0.11
0.17
0.23
0.01
0.72 -0.49 -0.12 -0.04
Amprenavir 0.36 -0.29 -0.17 -0.49
0.29
0.13
Indinavir 0.33
0.12 -0.10
4
0.04 -0.14 -0.02 -0.62 -0.23
0.07
0.63 -0.12
0.02 -0.02 -0.65
Lopinavir 0.31 -0.12 -0.18 -0.33 -0.43 -0.19 -0.21 -0.15
Saquinavir 0.38
0.15 -0.48
Tipranavir 0.23 -0.71
0.48
0.58
0.11
0.14
0.14
0.43 -0.12 -0.02
0.07
0.07
0.07
Darunavir 0.19 -0.37 -0.21 -0.23
Percent 83.7
Variance (%)
6.0
3.1
0.67
0.29 -0.38
2.7
0.39 -0.04
1.6
1.0
0.12 -0.72 -0.21
1.0
0.6
0.3
The first two principal components together capture approximately 90% of
the variance in the data and represent development of high resistance toward
all drugs and development of high resistance to NFV and RTV with increasing
resistance toward ATV, SQV and IDV, respectively.
NFV and RTV, less resistance to ATV, SQV, and IDV,
and low resistance or even increased susceptibility
toward APV, LPV, DRV, and especially TPV, relative to
each drug’s mean resistance value.
Interestingly, the points in Figure 2 form a “path”
through phenotypic space. Such “horseshoe"-shaped
paths are often indicative of a non-linear ordering or
underlying gradient in the data[94]. Here, the path
clearly tracks the genotypic mutations accrued by the
sequences. Sequences with few mutations appear to
have resistance toward NFV, RTV, ATV, SQV, and IDV,
but little resistance to APV, LPV, DRV, or TPV (i.e., the
phenotypic path “veers upward” in the principal component space), while sequences with many mutations are
resistant to all drugs (far right in the principal component space). Three sequences along the path are selected
in Figure 2 and their corresponding scaled phenotypes
and genotypes are listed to the right of the plot. The
point selected on the intermediate portion of the path
represents a sequence that includes the mutations M46I
and L90M, which have been shown to be highly correlated[59] and to be associated with resistance to NFV,
IDV, and RTV, and other drugs to a lesser extent[56].
The point selected at the right end of the path represents a sequence that shows at least moderate resistance
to all drugs, and includes the mutations V82T, I84V
associated with resistance to TPV[18], and L33F, I47V,
and I54M, associated with resistance to both TPV[18]
and DRV[20], in addition to containing mutations that
harbor resistance toward first-generation drugs.
As a whole, Figure 2 supports the historical “path” of
drug development, in that it is relatively easy to become
resistant to first-generation drugs with relatively few
mutations (RTV, NFV, SQV, etc.), but many
accumulated mutations appear to be necessary to confer
resistance to the newer drugs, such as darunavir[16,19].
Whether or not this pathway is due to history and treatment regimens or whether it is a fundamental consequence of the structural features of the drugs and the
viable evolutionary space of HIV-1 protease requires
further study.
A handful of sequences lie “off” the pathway. Three
such sequences are indicated in Figure 2, and several
more are listed in Fig. S4 (Additional file 1). The top
and bottom sequences indicated in Figure 2 are both
uniquely susceptible to SQV and have the mutation
V82L which has been associated with increased SQV
susceptibility[26]. The middle sequence shows low levels
of resistance across all nine drugs. All three of these
sequences fall off the pathway because of their non-negligible levels of resistance toward one or more secondgeneration drugs while maintaining susceptibility to one
or more first-generation drugs. Additional outliers are
shown in the Supplementary Information (Additional
File 1).
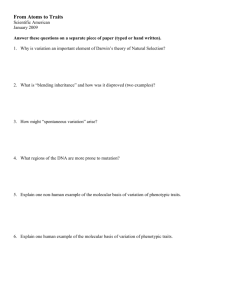
Phenotypic Similarity Does Not Imply Genotypic Similarity
Figure 3a is a plot of scaled phenotypic distance vs. genotypic distance for all (398*397)/2 = 79003 sequence
pairs, using all amino acid positions to compute genotypic distances. Not surprisingly, sequences that are genotypically similar are phenotypically similar; there are no
points in the upper-left corner of the plot. However,
there are many sequences that are very different genotypically and yet have similar scaled resistance phenotypes
(there are many points in the lower-right corner), suggesting that HIV-1 may arrive at the same multidrug
resistance phenotype via rather varied genotypes. Figure
3b is again a plot of all pairwise phenotypic distances vs.
their genotypic distances, except now, only the resistance-associated positions specified in the Methods have
been included in calculating genotypic distance. While
the upper left corner of this plot is still sparse, this plot
indicates that polymorphic or accessory positions not
considered in genotypic distance may still affect resistance profiles in the absence of mutations commonly
associated with drug resistance (i.e. there are pairs of
sequences with a genotypic distance of zero in Figure 3b
but a moderate phenotypic distance). Again, there are
still sequences that are genotypically very different yet
show similar resistance phenotypes.
Mutations from two sample pairs of sequences from
the lower-right quadrant of each figure are shown. In
Figure 3b only the mutations contributing to the genotypic distance are shown. As can be seen, very different
genotypes can generate similar resistance patterns. For
example, the sequences shown in the lower box at the
right of Figure 3a show high levels of resistance toward
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 11 of 19
Figure 3 Pairwise phenotypic distance vs. pairwise genotypic distance for all pairs of sequences. (a) Scaled phenotypic distance vs.
genotypic distance with all positions considered in calculating genotypic distance and (b) with only resistance-associated positions used in
calculating genotypic distance. The density of points is colored according to the scale at right. The sequence pairs corresponding to two points
are indicated. The 9-digit shorthand used to describe the two pairs of sequences indicates the resistance score (Table 2) to the PIs in the order
used in Fig. 1: RTV, NFV, ATV, APV, IDV, LPV, SQV, TPV, DRV.
all drugs; each sequence has a subset of documented
drug resistance mutations, such as V32I, L33F, M46I,
I47V, F53L, G73S, V82A, and L90M in the case of the
first sequence and M46L, I54V, V82F, and I84V in the
case of the second sequence, but the sequences have
few mutations in common (K20R, E35D, M36I, L63P,
A71V, and I93L), most of which are considered highly
polymorphic accessory mutations[95]. The variety of
mutations through which the protease is able to achieve
similar multidrug clinical phenotypes demonstrates that
phenotypic similarity does not imply genotypic
similarity. Recall here that two sequences that are both
sufficiently above the clinical fold-change cutoff for
resistance for a given drug are both considered phenotypically identical toward that drug, due to the capping of
scaled resistance values above a threshold. Therefore,
while they are phenotypically similar from a clinical perspective, they may possess quite different (but both
large enough to be considered resistant) raw fold-change
values toward a given drug.
Another way to understand the genotypic variation for
a given phenotypic pattern is to analyze the genotypic
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 12 of 19
diversity within each phenotypic cluster. For each individual phenotypic cluster obtained in the above analysis,
we used a k-medoids approach to identify representative
genotypes for that cluster. Through constraints, a more
genotypically diverse phenotypic cluster would require
more sequences to represent it. Figure 1 shows the
representative sequences chosen for all phenotypic clusters. As can be seen, two clusters (5 and 9), even though
they are of similar sizes to others, require multiple
representative genotypic sequences. Multiple representative sequences for a cluster suggest multiple genotypic
paths to the phenotype.
To quantify phenotypic and genotypic diversity within
clusters, resampling was carried within each cluster as
described in the Methods. Table 5 summarizes the
results for all clusters with more than 6 members. The
p-values for intracluster phenotypic distance ("P Pheno”)
show significantly low variation, but hard constraints in
the clustering enforced phenotypic similarity so this low
variation is by design. It is also not surprising that the
genotypes of non-resistant clusters are also statistically
similar (bootstrap studentized statistics for clusters 34
and 36 are -11.3 and -13.3), as none of these sequences
would be expected to bear a resistance-associated mutation, so they should all effectively be “wild-type”. However, among multidrug resistant phenotypes, there is
either no more or no less genotypic variation between
members within a cluster than there is between any two
random sequences in the data set (insignificant
“P_Geno” values), or there is more genotypic variation
than would be expected by random sampling in the
cases of clusters 5 and 7 (P_Geno < 0.01; bootstrap studentized statistics are 2.26 and 2.16). Furthermore, on
average, pairs of sequences from the same cluster generally share less than 50% of their mutations (using resistance-associated positions listed in the Methods); the
one exception is the cluster containing sequences resistant to all drugs (cluster 1), whose members share 54%
of their mutations on average; indeed the average intracluster genotypic distance for this cluster is in some
cases less than that for clusters containing fewer mutations on average, suggesting that a higher number of
mutations may not mean greater genotypic variation,
and also indicating that the most highly resistant
sequences might need to have some “key” mutations in
common. When removing from the data set one from
each pair of 28 sequences from the same patient at two
different time points and reclustering, the most highly
resistant cluster still had >50% shared mutations on
average and a lower intra-cluster genotypic distance
than some other resistant clusters, although it now
required two representative sequences, suggesting that
some - but not all - of this similarity may be due to
including data at different time points from the same
patient. This idea is further addressed in the Discussion.
Nevertheless, while a larger data set would allow for a
Table 5 Statistical analysis of phenotypic and genotypic variability within each cluster containing 6 or more members.
NUM
Phenotype
#Seqs
Intra_Pheno
P_Pheno
Intra_Geno
P_Geno
Avg_Muts
Shared_Muts
Shan._Ent.
1
444444444
15
0.69
0
6.15
0.47
9.1
4.95
14.52
2
444444442
28
0.56
0
7.31
0.02
8.3
3.4
18.78
4
444433433
10
0.64
0
7.83
0.05
8.7
3.84
18.33
5
444444413
6
0.63
2E-04
9.63
0.001
9.8
3.9
18.33
6
444433342
6
0.81
7E-04
7.07
0.27
7.7
3.33
13.74
7
444443422
31
0.8
0
7.5
0.008
7
2.43
19
9
444433422
7
0.63
0
8.31
0.04
8.6
3.79
16.91
12
444423402
6
0.65
2E-04
7.82
0.12
7.8
3.04
15.73
14
444232421
10
0.91
1E-04
6.61
0.34
5.9
2.19
14.14
16
444233401
8
0.82
1E-04
6.54
0.38
6.4
2.36
13.84
20
444222221
8
1.01
2E-04
6.18
0.49
5.2
1.41
13.84
26
442121211
13
0.85
0
4.11
0.05
3
0.71
9.88
29
321111111
9
0.8
0
2.38
7E-03
1.3
0.07
5.64
34
111010110
71
0.65
0
0.94
0
0.5
0.03
2.95
35
301000011
6
0.64
2E-04
0.67
3E-03
1
0.67
1.48
36
000000000
77
0.6
0
0.24
0
0.1
0
0.89
“Phenotype” is the nine-digit shorthand describing the binned level of resistance of the cluster centroid toward each of the nine drugs (see Fig. 1 for drug order).
“Intra Pheno” is the average intra-cluster phenotypic distance (in scaled resistance unites). “P pheno” are p-values for intra-cluster phenotypic distance. A p-value
of 0 indicates that a more extreme distance was not sampled in 10,000 trials. Analogous headings are shown for genotypic distance as well; genotypic distance
was defined using the list of non-polymorphic positions in the Methods. “Avg Muts” is the average number of mutations at non-polymorphic positions for
sequences within the cluster. “Shared Muts” is the average number of shared mutations between all pairs within a cluster. Shan. Ent. is the computed Shannon
Entopy (in bits) for the cluster, adding up the entropies at each non-polymorphic position.
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
more rigorous control for the number of mutations
within a cluster when computing p-values and for the
exclusion of data from the same patients at multiple
time points, thus allowing for fairer comparisons, this
simple analysis suggests again that in general, phenotypic similarity does not imply genotypic similarity, and
certain multidrug phenotypes may be achieved by more
varied genotypes than others.
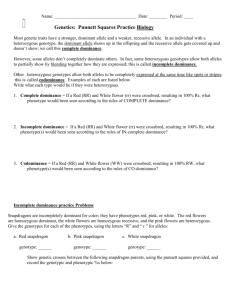
Feature selection uncovers important positions and
mutations for cluster assignment
Finally, we sought to rigorously determine sets of amino
acid positions and mutations that were most informative
of membership in the phenotypic clusters. Figure 4a
shows the results of greedily selecting one position at a
time such that at each step (going left to right), the
(approximate) mutual information (MI) between the
chosen set of features and the cluster assignment is
maximized. Only those positions that had significant MI
with the output are included. The red bars indicate the
MI between an individual position and the cluster
assignment, with the yellow star indicating the threshold
for statistical significance (p = 0.01). The blue bars indicate the joint MI between the subset selected thus far
and the cluster assignment. Note that positions are not
strictly selected in decreasing order of individual MI.
Because mutations at certain positions may be highly
coupled with positions already in the feature set, less
individually informative positions may contribute to a
more informative set of positions. This technique therefore chooses highly non-redundant features that are still
informative of the output. Finally, the black bar shows
the total information content of the output, the cluster
assignments.
Figure 4a indicates that several positions have significant MI with the final cluster assignment, especially
positions 54, 90, 84, 46, 33, 20, 82, 32, 88, and 71. This
is consistent with findings that these positions are
known to mutate in the presence of drug resistance,
either as primary or accessory mutations[4,47,48]. Collectively, these positions are computed to be nearly as
informative of ultimate cluster assignments as the entire
set of positions considered. The fact that position 54 is
chosen as the most informative feature is not surprising,
given the large range of drug-resistant mutations commonly found at this position and their varied effects
toward certain drugs as either primary or secondary
mutations; I54L, I54M, I54V, etc., can have different
consequences toward drugs such as TPV, DRV, and
APV[4,95] Also interesting is the redundancy of position
10 and, to a lesser extent, position 71; although position
10 has a high mutual information with the cluster output, it does not provide additional information once the
identities at the ten positions listed above are known.
Page 13 of 19
Position 71 provides some additional information but is
also quite redundant. These results are consistent with
the amino acids at positions 10 and 71 both being
highly correlated with those at other positions such as
54, 90, 82, 84, and others[54,55,59], as it is believed that
mutations at these positions can be compensatory in
nature[54,55,96]. Finally, one should note that the
approximate joint MI calculated between all of the positions and the output is still quite less than the true
information content of the output, suggesting that
amino acids considered at all positions still may not
result in perfect prediction of these output data. This is
likely due to the true importance of higher-order information (i.e. patterns of three or more amino acids
occurring together) in contributing to ultimate phenotypes - the importance of which has been noted previously[61] - as well as noise in the measurement and
clustering of the phenotypic data, thus highlighting the
inherent difficulty of accurately predicting phenotype
from genotype in these complex systems. The limitations of the second-order approximation also result in
the approximated total joint mutual information
between the features and the output (blue bars) failing
to be monotonically increasing as they would be were
an exact calculation feasible, again highlighting the complex relationship between various protease positions and
phenotype.
Figure 4b shows the specific amino acid identities calculated to be most informative of ultimate cluster
assignment. Here, key resistance mutations are chosen
that cause broad resistance to many of the older drugs,
such as L90M and I84V. At positions that can bear several identities, such as 54, 46, and 82, the selection of
the wild type amino acid suggests the importance of the
lack of any mutation at these positions in determining
cluster assignment.
Figures 4c and 4d show sample results for mutations
that are informative of assignment into specific clusters
- cluster 1 (c), the most resistant cluster, and cluster 36
(d), the completely nonresistant cluster. All other results
for clusters with 8+ members are shown in Figure S5
(Additional File 1). Figure 4c indicates that the amino
acid identities most informative of membership into the
“most” resistant cluster include several mutations that
have been associated with resistance to DRV[97] including V11I, L33F, V32I, L89V, and G73S, as well as mutations such as I84V and L90M that are associated with
broad cross resistance toward other PIs.
Finally, many of the informative residues in the nonresistant cluster (Figure 4d) are actually wild type amino
acids. This suggests that the lack of mutations at these
positions correlates with low levels of resistance. Additionally, several mutations listed are at accessory positions such as 10, 63 and 36, suggesting that mutations
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
Page 14 of 19
A
3.5
3
MI (nats)
2.5
2
1.5
1
0
B
54
90
84
46
33
20
82
32
88
71
76
70
62
58
50
24
85
74
13
10
53
11
89
72
93
35
47
43
48
73
30
36
full
0.5
position
3.5
3
MI (nats)
2.5
2
1.5
1
0
54I
90M
84V
46M
33F
82V
32I
20K
71V
13I
88N
76V
62I
10F
70K
47A
50I
53L
24L
92Q
48G
74T
58E
63P
73G
85V
54L
4P
72I
34Q
20R
93I
24I
50L
30D
76L
54V
20T
53F
11I
46L
43T
30N
54M
35E
43K
91T
32V
10H
36I
58Q
63L
66I
71T
82L
82A
73S
93L
82T
88D
84I
90L
71I
62V
20I
89L
35G
48V
13V
85I
46I
35D
47V
88G
74S
34E
70R
70E
50V
36M
11V
89V
33L
10I
47I
71A
10L
full
0.5
amino acid identity
C
0.18
0.16
0.14
MI (nats)
0.12
0.1
0.08
0.06
0.04
0
11V
33F
73A
70T
60D
11L
24M
36I
51A
51G
92Q
20V
35E
12P
33L
55N
79P
20K
79A
11I
35G
20T
36M
32V
47V
54L
89L
32I
10F
16A
34E
34Q
54M
73S
89V
71I
73G
13I
90L
10L
13V
54I
71A
84I
84V
90M
clust 1
0.02
amino acid identity
D
0.5
0.45
0.4
0.35
MI (nats)
0.3
0.25
0.2
0.15
0.1
0
10L
63P
36M
53F
55K
35D
62I
54M
10F
10I
20I
24L
36I
35E
93I
85V
74T
71T
20R
62V
10V
71I
88N
63A
63S
63Q
82T
82A
93L
48G
63L
58Q
73G
11V
11I
33F
33L
46L
58E
60D
60E
73S
73T
84I
84V
54V
54L
32I
32V
43T
43K
47I
47V
46I
46M
20K
54I
82V
71V
90L
90M
71A
clust 36
0.05
amino acid identity
Figure 4 Stepwise selection of HIV-1 protease positions and mutations that are important for cluster assignment. (a) Stepwise selection
of HIV-1 protease positions (from left to right) such that at each step, the mutual information between amino acids at positions selected so far
and the cluster assignment is maximized. Red bars indicate (bias-adjusted) MI between each individual position and cluster assignment. ‘x’s’ are
the standard deviation of MI estimation for two independent variables, and asterisks indicate the threshold for statistical significance (p=0.01).
Blue bars are the estimated joint MI between the subset chosen and the cluster assignment. The black bar indicates the total information
content of the cluster assignments. (b) Stepwise selection of the most informative amino acid identities at specific positions for assignment into
phenotypic clusters. (c) and (d): Stepwise selection of particular amino acid identities whose collective presence or absence are maximally
informative of membership specifically into cluster 1 (c) and cluster 36 (d).
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
at these positions are reasonable markers for “any” resistance in general. It is important to note that while this
method highlights which mutations are most informative of cluster assignment, it does not identify whether it
is the presence or the absence of the mutation that is
associated with cluster membership.
Discussion
This study highlighted major patterns of phenotypic
resistance across all nine clinically-approved HIV-1 PIs.
Cluster analysis yielded several phenotypic patterns,
including clusters showing resistance to all drugs, all but
one specific drug (such as TPV, SQV, or DRV), a large
subset of drugs, a small subset of drugs, and only one
drug (such as NFV or ATV). Through choosing representative sequences for each phenotypic pattern, we
have corroborated previously reviewed observations
[4,27,29] that mutations such as L33F, V82A, I84V, and
L90M are associated with broad cross resistance, while
others, such as D30N and I50L are associated with resistance to only one drug and still others such as I47A and
I54L are linked with hypersusceptibility toward a given
drug. While we have uncovered a variety of phenotypic
patterns, not every possible resistance pattern was
sampled, suggesting that cross resistance and other factors cause highly correlated drug responses, assuming
our data set is representative. Indeed, our considered
isolates occupy only a small portion (~6%) of the available, clinically-relevant phenotypic space. For example,
no cluster shows a moderate or high level of resistance
toward DRV without resistance to several other drugs,
including APV and LPV. Whether this result is due to
patient treatment histories or the intrinsic properties of
the drug–protease interactions requires further study. If
the latter is at least partly the case, it corroborates the
observation that DRV may have a higher genetic barrier
to resistance[16,19].
TPV’s response toward sequences often shows little
relationship to other drugs’ responses. The relative lack
of cross resistance to TPV may make it particularly useful[14] in conjunction with other inhibitors to “cover”
the mutation space of the virus. TPV’s differing
response profile may follow from its unique structural
characteristics. It is the only clinically-approved inhibitor
that does not use a water molecule to mediate hydrogen
bonds with the flap regions of the protease, suggesting
the importance of developing structurally diverse drug
molecules toward a target as a strategy to combat resistance[98].
The representative sequences of four clusters (29, 31,
34, and 36) had no mutations at the 21 positions considered in computing genotypic distance for this purpose, and yet their phenotypes were not identical on
average. This suggests a potential role for mutations at
Page 15 of 19
other positions that may not be associated with primary
drug resistance. A rigorous study that analyzes the differences in mutation frequencies in such clusters and
considers their impacts on the susceptibilities of individual cluster members, while beyond the scope of the
current work, would be interesting potential future
work, especially when more data are available.
We demonstrated that phenotypic clustering may
allow for prediction of resistance to a particular drug
based only on resistance information toward other drugs
and no genotypic information. While our goal was not
to develop a prediction method that is superior to the
available genotypic-based methods specific to each drug,
especially as it may be rare to have multidrug phenotypic data available, it is interesting to assess how well our
“genotype-blind” method performs when compared to
genotype-based methods. Rigorous comparisons to
mean standard error values in other studies are difficult
due to different scaling and capping procedures used
here for phenotypic standardization. Nevertheless, some
studies used a Pearson correlation coefficient (R)
between predicted and actual log-fold-change as a measure of accuracy. R values for PIs available at the time
of selected studies ranged from 0.85-0.97[69], 0.65-0.93
(across multiple methods)[67], and 0.78-0.89[64]. From
the cross-validation procedure used to generate Table 3,
our “genotype-blind” method gave R-values ranging
from 0.84-0.94 using all 398 data set members, with the
exception of TPV, although these numbers may be artificially high due to our capping of extreme values. Predictions of resistance to TPV had an R value of only
0.45, consistent with the observed difficulty in predicting
TPV resistance based on the phenotypes shown toward
other drugs. Finally, our reported classification accuracies are lower than those reported for genotype-based
predictions, but this is partly because we use five categories as opposed to the binary or 3-way classifications
commonly used. If we adopt a naive binary classification
scheme (scaled resistance < 1.0 is not resistant; scaled
resistance >= 1.0 is resistant), our cluster-based classification accuracies using the n-fold cross validation procedure for the entire data set range from 85%-95%
excluding TPV(79%), compared with 85%-95% for binary
classification schemes reported in the literature
[65,72,74] (TPV and DRV were not part of these studies). It is interesting to note that while not the major
goal of our paper, we have shown that with the exception of TPV, it may be possible to approach comparable
drug resistance prediction accuracy without any genotypic information; this level of accuracy demonstrates the
restricted phenotypic space occupied by the virus.
Our analysis was limited by the number of accessible
isolates that have each undergone phenotypic resistance
testing against all nine inhibitors. A large priority for
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
future work is acquiring enough data such that the
number of clusters is robust to the data set size such
that one could be confident that all or nearly all phenotypic patterns have been sampled. One strategy is to
pool isolates phenotyped by different assays to bolster
the amount of data; indeed, a preliminary clustering was
carried out in which the data analyzed here were combined with 196 isolates phenotyped using the Antivirogram (Virco, Mechelin, Belgium)[99] assay, but
differences between the assays may have subtle but
important effects on the interpretation of scaled resistance values, even when using cutoffs specific to each
assay, creating potential artifacts in the clustering (we
obtained 67 clusters with the combined data set, a larger
number than expected given the pattern shown in Fig.
S3). More data would allow for larger cluster sizes in
general, and therefore a higher confidence in associating
certain genotypic features with cluster assignments; one
could also look for differences in phenotypes between
virus subtypes if such data were concurrently available.
Additionally, more data may allow for cluster sizes to
accurately represent the relative frequencies of phenotypes within the population and would allow us to
exclude isolates containing mixtures at key positions;
such an exclusion would have been too restrictive with
the amount of data currently accessible.
Finally, larger clusters would also allow us to account
for and potentially exclude sequences that may be from
the same patient at different times, allowing for more
robust conclusions to be made about the genotypic
variability within a cluster. Preliminary analyses were
conducted in which one sequence each from 28
sequences pairs from the same patient in our data set
was arbitrarily excluded (even if the pair differed significantly in genotype), yielding a 370-member set. Qualitative results of genotypic variability remained similar, in
that several resistant clusters showed as much or more
genotypic diversity than randomly chosen data set members, although again, the most resistant cluster showed a
higher percentage of shared mutations between cluster
members on average even though it now required two
representative sequences. 48 clusters were needed to
cluster the “unique-patient” data set as opposed to 50
for the original data set, suggesting that data from the
same patient taken at different time points can provide
additional phenotypic diversity. 98% of sequence pairs
grouped together in the smaller data set were grouped
together in the original data set, showing that the overall
clustering remained very similar.
Since the time the manuscript had been originally
drafted, we obtained approximately 50 more isolates,
and we have carried out very preliminary analyses of a
larger (n = 453) data set including these new sequences.
52 clusters were needed to group the data using the
Page 16 of 19
same constraints with the original data set, and the phenotypic patterns of most clusters were identical or
highly similar; 86% of sequences pairs that had been
grouped together originally remained together in the
clustering of the larger data set. We also used our original (n = 398) clusters to predict resistance to each drug
for each of the new isolates, using the other drugs’ resistance values to select the closest centroid (i.e., the same
procedure used in the n-fold cross validation). Scaled
resistance scores (0-4) were predicted correctly from
66%-82% of the time, depending on the drug; interestingly, predictions for TPV (67%) and DRV (82%) were
better than seen in the n-fold cross validation, while
those for NFV (66%) and RTV (76%) were worse. Prediction accuracy may be affected by the points in time
at which the data were obtained, as resistance patterns
may change over time.
Treatment histories were not entirely available for the
current data set; acquiring such information and analyzing future data in their context can provide additional
insights. For example, one could determine the extent to
which treatment histories affect the “path” seen in Figure 2 and the dependence on individual multidrug resistance phenotypes on past treatment; such analyses could
highlight the extent to which treatment histories affect
the genotypic variation within a phenotypic cluster.
While the methodology and analyses were applied
here to the HIV-1 protease system, the framework is
generally applicable to any system for which there are
phenotypic data across multiple drugs. In addition to
continuing to analyze HIV-1 protease as the available
data grow, another natural next step is to apply these
methods to the HIV-1 nucleoside or non-nucleoside
reverse transcriptase inhibitor systems and to compare
the patterns of cross resistance within those systems
with the ones obtained in the present study. By rigorously studying phenotypic resistance patterns of multiple
systems, one may begin to address more general ideas,
including whether cross resistance has equally affected
all target systems and whether potential genotypic diversity within phenotypic clusters is a general feature of
target systems.
Conclusions
To our knowledge, this study provided the first clusterbased analysis of the clinically-explored multidrug phenotypic space of HIV-1 protease, uncovering major multidrug patterns of resistance, cross resistance, and
potential hypersusceptibility. We showed that while genotypic similarity implies clinical phenotypic similarity,
the converse is not necessarily the case. We also provided genotypic determinants of phenotypic patterns.
Rather than consider each drug in turn, as others have
done, we have accounted for their relationships and
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
collapsed the vast nine dimensional space into a smaller
one through clustering, allowing us to consider genotypic features that are associated with a simultaneous
nine-drug response. We have therefore provided a new
perspective on existing drug resistance patterns and
their associated genotypic features. Such a framework
will be useful as new therapies emerge and will require
evaluation in the context of existing drug resistance.
Page 17 of 19
7.
8.
9.
10.
Additional material
Additional file 1: Contains the formal integer-programming
formulations used within the work, five supplementary figures
(Figures S1-S5) and one supplementary table (Table S1). This file also
contains a link to a website containing the n = 398 data set used in this
work. (http://www.wellesley.edu/Chemistry/Radhakrishnan/projects.html).
Acknowledgements
The authors acknowledge Morgan Carr-Markell, Patrick Flaherty, Kevin Gold,
Tim McMurry, and Bruce Tidor for helpful discussions. KMD was partially
supported by the National Science Foundation (NSF-REU). PN was partially
supported by the Wellesley College Brachman-Hoffman fund and the
Howard Hughes Medical Institute. BMK was partially supported by the
National Institutes of Health (GM82209). SYR and RWS were supported by
the NIH grants P01GM066524-06 and AI068581. SPH was supported by NIHR01GM086884. MLR was supported by Wellesley College.
Author details
1
Department of Chemistry, Wellesley College, 106 Central Street, Wellesley,
MA 02481, USA. 2Department of Biological Engineering, Massachusetts
Institute of Technology, 77 Massachusetts Avenue, Cambridge, MA 02139,
USA. 3Division of Infectious Diseases, Department of Medicine, Stanford
University, 300 Pasteur Drive, Stanford, CA, 94305, USA. 4Department of
Statistics, Stanford University, Sequoia Hall, Stanford, CA 94305, USA.
Authors’ contributions
RWS and MLR conceptualized the research. KMD, PN, BMK, SYR, and MLR
implemented methods and performed analyses. SYR and RWS acquired data.
SPH provided critical support for certain analyses. RWS, BMK, PN, and MLR
drafted the manuscript. All authors have read and approved the final
manuscript.
Received: 27 August 2011 Accepted: 15 December 2011
Published: 15 December 2011
References
1. Shafer RW: Genotypic testing for human immunodeficiency virus type 1
drug resistance. Clinical Microbiology Reviews 2002, 15:247-277.
2. Burlet S, Pietrancosta N, Laras Y, Garino C, Quelever G, Kraus JL: Prospects
for the resistance to HIV protease inhibitors: Current drug design
approaches and perspectives. Current Pharmaceutical Design 2005,
11:3077-3090.
3. Yin PD, Das D, Mitsuya H: Overcoming HIV drug resistance through
rational drug design based on molecular, biochemical, and structural
profiles of HIV resistance. Cellular and Molecular Life Sciences 2006,
63:1706-1724.
4. Kim R, Baxter JD: Protease inhibitor resistance update: Where are we
now? AIDS Patient Care and Stds 2008, 22:267-277.
5. Shafer RW, Schapiro JM: HIV-1 drug resistance mutations: an updated
framework for the second decade of HAART. AIDS Reviews 2008, 10:67-84.
6. Ali A, Bandaranayake RM, Cai YF, King NM, Kolli M, Mittal S, Murzycki JF,
Nalam MNL, Nalivaika EA, Ozen A, Prabu-Jeyabalan MM, Thayer K,
Schiffer CA: Molecular Basis for Drug Resistance in HIV-1 Protease.
Viruses-Basel 2010, 2:2509-2535.
11.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
Palella FJ, Delaney KM, Moorman AC, Loveless MO, Fuhrer J, Satten GA,
Aschman DJ, Holmberg SD: Declining morbidity and mortality among
patients with advanced human immunodeficiency virus infection. New
England Journal of Medicine 1998, 338:853-860.
Staszewski S, Morales-Ramirez J, Tashima KT, Rachlis A, Skiest D, Stanford J,
Stryker R, Johnson P, Labriola DF, Farina D, Manion DJ, Ruiz NM: Efavirenz
plus zidovudine and lamivudine, efavirenz plus indinavir, and indinavir
plus zidovudine and lamivudine in the treatment of HIV-1 infection in
adults. New England Journal of Medicine 1999, 341:1865-1873.
Bonfanti P, Capetti A, Rizzardini G: HIV disease treatment in the era of
HAART. Biomedicine & Pharmacotherapy 1999, 53:93-105.
Murphy EL, Collier AC, Kalish LA, Assmann SF, Para MF, Flanigan TP,
Kumar PN, Mintz L, Wallach FR, Nemo GJ: Highly active antiretroviral
therapy decreases mortality and morbidity in patients with advanced
HIV disease. Annals of Internal Medicine 2001, 135:17-26.
Deeks SG: Treatment of anti retroviral-drug-resistant HIV-1 infection.
Lancet 2003, 362:2002-2011.
Turner SR, Strohbach JW, Tommasi RA, Aristoff PA, Johnson PD, Skulnick HI,
Dolak LA, Seest EP, Tomich PK, Bohanan MJ, Horng MM, Lynn JC,
Chong KT, Hinshaw RR, Watenpaugh KD, Janakiraman MN, Thaisrivongs S:
Tipranavir (PNU-140690): A potent, orally bioavailable nonpeptidic HIV
protease inhibitor of the 5,6-dihydro-4-hydroxy-2-pyrone sulfonamide
class. Journal of Medicinal Chemistry 1998, 41:3467-3476.
Koh Y, Nakata H, Maeda K, Ogata H, Bilcer G, Devasamudram T, Kincaid JF,
Boross P, Wang YF, Ties YF, Volarath P, Gaddis L, Harrison RW, Weber IT,
Ghosh AK, Mitsuya H: Novel bis-tetrahydrofuranylurethane-containin
nonpeptidic protease inhibitor (PI) UIC-94017 (TMC114) with potent
activity against multi-PI-resistant human immunodeficiency virus in
vitro. Antimicrob Agents Chemother 2003, 47:3123-3129.
Larder BA, Hertogs K, Bloor S, van den Eynde C, DeCian W, Wang YY,
Freimuth WW, Tarpley G: Tipranavir inhibits broadly protease inhibitorresistant HIV-1 clinical samples. AIDS 2000, 14:1943-1948.
Rusconi S, Catamancio SLA, Citterio P, Kurtagic S, Violin M, Balotta C,
Moroni M, Galli M, D’Arminio-Monforte A: Susceptibility to PNU-140690
(Tipranavir) of human immunodeficiency virus type 1 isolates derived
from patients with multidrug resistance to other protease inhibitors.
Antimicrob Agents Chemother 2000, 44:1328-1332.
Lefebvre E, Schiffer CA: Resilience to resistance of HIV-1 protease
inhibitors: Profile of darunavir. AIDS Reviews 2008, 10:131-142.
Doyon L, Tremblay S, Bourgon L, Wardrop E, Cordingley MG: Selection and
characterization of HIV-1 showing reduced susceptibility to the nonpeptidic protease inhibitor tipranavir. Antiviral Research 2005, 68:27-35.
Baxter JD, Schapiro JM, Boucher CAB, Kohlbrenner VM, Hall DB, Scherer JR,
Mayers DL: Genotypic changes in human immunodeficiency virus type 1
protease associated with reduced susceptibility and virologic response
to the protease inhibitor tipranavir. J Virol 2006, 80:10794-10801.
De Meyer S, Vangeneugden T, Lefebvre E, Azijn H, De Baere I, Van Baelen B,
de Bethune MP: Phenotypic and genotypic determinants of resistance to
TMC114: Pooled analysis of POWER 1, 2 and 3. Antiviral Therapy 2006, 11:
S83-S83.
Mitsuya Y, Liu TF, Rhee SY, Fessel WJ, Shafer RW: Prevalence of darunavir
resistance-associated mutations: Patterns of occurrence and association
with past treatment. Journal of Infectious Diseases 2007, 196:1177-1179.
Tisdale M, Myers RE, Maschera B, Parry NR, Oliver NM, Blair ED: Crossresistance analysis of human-immunodeficiency-virus type-1 variants
individually selected for resistance to 5 different protease inhibitors.
Antimicrob Agents Chemother 1995, 39:1704-1710.
Hertogs K, Bloor S, Kemp SD, Van den Eynde C, Alcorn TM, Pauwels R, Van
Houtte M, Staszewski S, Miller V, Larder BA: Phenotypic and genotypic
analysis of clinical HIV-1 isolates reveals extensive protease inhibitor
cross-resistance: a survey of over 6000 samples. AIDS 2000, 14:1203-1210.
Parkin NT, Chappey C, Maranta M, Whitehurst N, Petropoulos CJ: Genotypic
and Phenotypic Analysis of a Large Database of Patient Samples Reveals
Distinct Patterns of Protease Inhibitor Cross-Resistance[abstract]. Antiviral
Therapy 2001, 6(Suppl 1):49.
Harrigan PR, Larder BA: Extent of cross-resistance between agents used
to treat human immunodeficiency virus type 1 infection in clinically
derived isolates. Antimicrob Agents Chemother 2002, 46:909-912.
Watkins T, Resch W, Irlbeck D, Swanstrom R: Selection of high-level
resistance to human immunodeficiency virus type 1 protease inhibitors.
Antimicrob Agents Chemother 2003, 47:759-769.
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
26. Rhee SY, Taylor J, Fessel WJ, Kaufman D, Towner W, Troia P, Ruane P,
Hellinger J, Shirvani V, Zolopa A, Shafer RW: HIV-1 Protease Mutations and
Protease Inhibitor Cross-Resistance. Antimicrob Agents Chemother 2010,
54:4253-4261.
27. Race E: Cross-resistance within the protease inhibitor class. Antiviral
Therapy 2001, 6:29-36.
28. Yusa K, Harada S: Acquisition of multi-PI (protease inhibitor) resistance in
HIV-1 in vivo and in vitro. Current Pharmaceutical Design 2004,
10:4055-4064.
29. Kozal M: Cross-resistance patterns among HIV protease inhibitors. AIDS
Patient Care and Stds 2004, 18:199-208.
30. Patick AK, Duran M, Cao Y, Shugarts D, Keller MR, Mazabel E, Knowles M,
Chapman S, Kuritzkes DR, Markowitz M: Genotypic and phenotypic
characterization of human immunodeficiency virus type 1 variants
isolated from patients treated with the protease inhibitor nelfinavir.
Antimicrob Agents Chemother 1998, 42:2637-2644.
31. Colonno R, Rose R, McLaren C, Thiry A, Parkin N, Friborg J: Identification of
I50L as the signature atazanavir (ATV)-resistance mutation in treatmentnaive HIV-1-infected patients receiving ATV-containing regimens. Journal
of Infectious Diseases 2004, 189:1802-1810.
32. Yanchunas J, Langley DR, Tao L, Rose RE, Friborg J, Colonno RJ, Doyle ML:
Molecular basis for increased susceptibility of isolates with atazanavir
resistance-conferring substitution I50L to other protease inhibitors.
Antimicrob Agents Chemother 2005, 49:3825-3832.
33. Weinheimer S, Discotto L, Friborg J, Yang H, Colonno R: Atazanavir
signature I50L resistance substitution accounts for unique phenotype of
increased susceptibility to other protease inhibitors in a variety of
human immunodeficiency virus type 1 genetic backbones. Antimicrob
Agents Chemother 2005, 49:3816-3824.
34. Kemper CA, Witt MD, Keiser PH, Dube MP, Forthal DN, Leibowitz M,
Smith DS, Rigby A, Hellmann NS, Lie YS, Leedom J, Richman D,
McCutchan JA, Haubrich R: Sequencing of protease inhibitor therapy:
insights from an analysis of HIV phenotypic resistance in patients failing
protease inhibitors. AIDS 2001, 15:609-615.
35. Beerenwinkel N, Sing T, Lengauer T, Rahnenfuhrer J, Roomp K, Savenkov I,
Fischer R, Hoffmann D, Selbig J, Korn K, Walter H, Berg T, Braun P,
Fatkenheuer G, Oette M, Rockstroh J, Kupfer B, Kaiser R, Daumer M:
Computational methods for the design of effective therapies against
drug resistant HIV strains. Bioinformatics 2005, 21:3943-3950.
36. Lengauer T, Sing T: Innovation - Bioinformatics-assisted anti-HIV therapy.
Nature Reviews Microbiology 2006, 4:790-U799.
37. Cordes F, Kaiser R, Selbig J: Bioinformatics approach to predicting HIV
drug resistance. Expert Review of Molecular Diagnostics 2006, 6:207-215.
38. Rhee SY, Gonzales MJ, Kantor R, Betts BJ, Ravela J, Shafer RW: Human
immunodeficiency virus reverse transcriptase and protease sequence
database. Nucleic Acids Research 2003, 31:298-303.
39. Wu TD, Schiffer CA, Gonzales MJ, Taylor J, Kantor R, Chou SW, Israelski D,
Zolopa AR, Fessel WJ, Shafer RW: Mutation patterns and structural
correlates in human immunodeficiency virus type 1 protease following
different protease inhibitor treatments. J Virol 2003, 77:4836-4847.
40. Chen LM, Perlina A, Lee CJ: Positive selection detection in 40,000 human
immunodeficiency virus (HIV) type 1 sequences automatically identifies
drug resistance and positive fitness mutations in HIV protease and
reverse transcriptase. J Virol 2004, 78:3722-3732.
41. Kantor R, Katzenstein DA, Efron B, Carvalho AP, Wynhoven B, Cane P,
Clarke J, Sirivichayakul S, Soares MA, Snoeck J, Pillay C, Rudich H,
Rodrigues R, Holguin A, Ariyoshi K, Bouzas MB, Cahn P, Sugiura W,
Soriano V, Brigido LF, Grossman Z, Morris L, Vandamme AM, Tanuri A,
Phanuphak P, Weber JN, Pillay D, Harrigan PR, Camacho R, Schapiro JM,
Shafer RW: Impact of HIV-1 subtype and antiretroviral therapy on
protease and reverse transcriptase genotype: Results of a global
collaboration. PLoS Medicine 2005, 2:325-337.
42. Rhee SY, Fessel WJ, Zolopa AR, Hurley L, Liu T, Taylor J, Nguyen DP,
Slome S, Klein D, Horberg M, Flamm J, Follansbee S, Schapiro JM,
Shafer RW: HIV-1 protease and reverse-transcriptase mutations:
Correlations with antiretroviral therapy in subtype B isolates and
implications for drug-resistance surveillance. Journal of Infectious Diseases
2005, 192:456-465.
43. Sing T, Svicher V, Beerenwinkel N, Ceecherini-Silberstein F, Daumer M,
Kaiser R, Walter H, Korn K, Hoffmann D, Oette M, Rockstroh JK,
Fatkenheuer G, Perno CF, Lengauer T: Characterization of novel HIV drug
Page 18 of 19
44.
45.
46.
47.
48.
49.
50.
51.
52.
53.
54.
55.
56.
57.
58.
59.
60.
61.
62.
resistance mutations using clustering, multidimensional scaling and
SVM-based feature ranking. In Knowledge Discovery in Databases: Pkdd
2005 Edited by: Jorge A, Torgo L, Brazdil P, Camacho R, Gama J 2005,
3721:285-296.
Svicher V, Ceccherini-Silberstein F, Erba F, Santoro M, Gori C, Bellocchi MC,
Giannella S, Trotta MP, Monforte AD, Antinori A, Pern CF: Novel human
immunodeficiency virus type 1 protease mutations potentially involved
in resistance to protease inhibitors. Antimicrob Agents Chemother 2005,
49:2015-2025.
Kagan RM, Cheung PK, Huard TK, Lewinski MA: Increasing prevalence of
HIV-1 protease inhibitor-associated mutations correlates with long-term
non-suppressive protease inhibitor treatment. Antiviral Research 2006,
71:42-52.
Garriga C, Perez-Elias MJ, Delgado R, Ruiz L, Najera R, Pumarola T, AlonsoSocas MD, Garcia-Bujalance S, Menendez-Arias L: Mutational patterns and
correlated amino acid substitutions in the HIV-1 protease after
virological failure to nelfinavir- and lopinavir/ritonavir-based treatments.
Journal of Medical Virology 2007, 79:1617-1628.
Shafer RW, Rhee SY, Pillay D, Miller V, Sandstrom P, Schapiro JM,
Kuritzkes DR, Bennett D: HIV-1 protease and reverse transcriptase
mutations for drug resistance surveillance. AIDS 2007, 21:215-223.
Bennett DE, Camacho RJ, Otelea D, Kuritzkes DR, Fleury H, Kiuchi M,
Heneine W, Kantor R, Jordan MR, Schapiro JM, Vandamme AM,
Sandstrom P, Boucher CAB, van de Vijver D, Rhee SY, Liu TF, Pillay D,
Shafer RW: Drug Resistance Mutations for Surveillance of Transmitted
HIV-1 Drug-Resistance: 2009 Update. PLoS One 2009, 4:e4724.
Beerenwinkel N, Daumer M, Sing T, Rahnenfuhrer J, Lengauer T, Selbig J,
Hoffmann D, Kaiser R: Estimating HIV evolutionary pathways and the
genetic barrier to drug resistance. Journal of Infectious Diseases 2005,
191:1953-1960.
Beerenwinkel N, Drton M: A mutagenetic tree hidden Markov model for
longitudinal clonal HIV sequence data. Biostatistics 2007, 8:53-71.
Deforche K, Camacho R, Grossman Z, Silander T, Soares MA, Moreau Y,
Shafer RW, Van Laethem K, Carvalho AP, Wynhoven B, Cane P, Snoeck J,
Clarke J, Sirivichayakul S, Ariyoshi K, Holguin A, Rudich H, Rodrigues R,
Bouzas MB, Cahn P, Brigido LF, Soriano V, Sugiura W, Phanuphak P,
Morris L, Weber J, Pillay D, Tanuri A, Harrigan PR, Shapiro JM,
Katzenstein DA, Kantor R, Vandamme AM: Bayesian network analysis of
resistance pathways against HIV-1 protease inhibitors. Infection Genetics
and Evolution 2007, 7:382-390.
Beerenwinkel N, Sullivant S: Markov models for accumulating mutations.
Biometrika 2009, 96:645-661.
Gonzales MJ, Belitskaya I, Dupnik KM, Rhee SY, Shafer RW: Protease and
reverse transcriptase mutation patterns in HIV type 1 isolates from
heavily treated persons: Comparison of isolates from Northern California
with isolates from other regions. Aids Res Hum Retrovir 2003, 19:909-915.
Hoffman NG, Schiffer CA, Swanstrom R: Covariation of amino acid
positions in HIV-1 protease. Virology 2003, 314:536-548.
Hoffman NG, Schiffer CA, Swanstrom R: Covariation of amino acid
positions in HIV-1 protease (vol 314, pg 536, 2003). Virology 2005,
331:206-207.
Rhee SY, Liu T, Ravela J, Gonzales MJ, Shafer RW: Distribution of human
immunodeficiency virus type 1 protease and reverse transcriptase
mutation patterns in 4,183 persons undergoing genotypic resistance
testing. Antimicrob Agents Chemother 2004, 48:3122-3126.
Chen L, Lee C: Distinguishing HIV-1 drug resistance, accessory, and viral
fitness mutations using conditional selection pressure analysis of treated
versus untreated patient samples. Biology Direct 2006, 1:14.
Liu Y, Eyal E, Bahar I: Analysis of correlated mutations in HIV-1 protease
using spectral clustering. Bioinformatics 2008, 24:1243-1250.
Rhee SY, Liu TF, Holmes SP, Shafer RW: HIV-1 subtype B protease and
reverse transcriptase amino acid covariation. PLoS Computational Biology
2007, 3:836-843.
Wang Q, Lee C: Distinguishing Functional Amino Acid Covariation from
Background Linkage Disequilibrium in HIV Protease and Reverse
Transcriptase. PLoS One 2007, 2:e814.
Haq O, Levy RM, Morozov AV, Andrec M: Pairwise and higher-order
correlations among drug-resistance mutations in HIV-1 subtype B
protease. BMC Bioinformatics 2009, 10(Suppl 8):S10.
Reuman EC, Rhee SY, Holmes SP, Shafer RW: Constrained patterns of
covariation and clustering of HIV-1 non-nucleoside reverse transcriptase
Doherty et al. BMC Bioinformatics 2011, 12:477
http://www.biomedcentral.com/1471-2105/12/477
63.
64.
65.
66.
67.
68.
69.
70.
71.
72.
73.
74.
75.
76.
77.
78.
79.
80.
inhibitor resistance mutations. Journal of Antimicrobial Chemotherapy 2010,
65:1477-1485.
Zhang J, Hou TJ, Wang W, Liu JS: Detecting and understanding
combinatorial mutation patterns responsible for HIV drug resistance.
Proceedings of the National Academy of Sciences of the United States of
America 2010, 107:1321-1326.
Beerenwinkel N, Daumer M, Oette M, Korn K, Hoffmann D, Kaiser R,
Lengauer T, Selbig J, Walter H: Geno2pheno: estimating phenotypic drug
resistance from HIV-1 genotypes. Nucleic Acids Research 2003,
31:3850-3855.
Wang K, Jenwitheesuk E, Samudrala R, Mittler JE: Simple linear model
provides highly accurate genotypic predictions of HIV-1 drug resistance.
Antiviral Therapy 2004, 9:343-352.
Jenwitheesuk E, Wang K, Mittler JE, Samudrala R: PIRSpred: a web server
for reliable HIV-1 protein-inhibitor resistance/susceptibility prediction.
Trends in Microbiology 2005, 13:150-151.
Rabinowitz M, Myers L, Banjevic M, Chan A, Sweetkind-Singer J, Haberer J,
McCann K, Wolkowicz R: Accurate prediction of HIV-1 drug response from
the reverse transcriptase and protease amino acid sequences using
sparse models created by convex optimization. Bioinformatics 2006,
22:541-549.
Saigo H, Uno T, Tsuda K: Mining complex genotypic features for
predicting HIV-1 drug resistance. Bioinformatics 2007, 23:2455-2462.
Vermeiren H, Van Craenenbroeck E, Alen P, Bacheler L, Picchio G, Lecocq P:
Prediction of HIV-1 drug susceptibility phenotype from the viral
genotype using linear regression modeling. Journal of Virological Methods
2007, 145:47-55.
Beerenwinkel N, Schmidt B, Walter H, Kaiser R, Lengauer T, Hoffmann D,
Korn K, Selbig J: Diversity and complexity of HIV-1 drug resistance: A
bioinformatics approach to predicting phenotype from genotype.
Proceedings of the National Academy of Sciences of the United States of
America 2002, 99:8271-8276.
Sevin AD, DeGruttola V, Nijhuis M, Schapiro JM, Foulkes AS, Para MF,
Boucher CAB: Methods for investigation of the relationship between
drug-susceptibility phenotype and human immunodeficiency virus type
1 genotype with applications to AIDS Clinical Trials Group 333. Journal of
Infectious Diseases 2000, 182:59-67.
Srisawat A, Kijsirikul B: Combining classifiers for HIV-1 drug resistance
prediction. Protein and Peptide Letters 2008, 15:435-442.
Wang D, Larder B, Revell A, Montaner J, Harrigan R, De Wolf F, Lange J,
Wegner S, Ruiz L, Perez-Elias MJ, Emery S, Gatell J, Monforte AD, Torti C,
Zazzi M, Lane C: A comparison of three computational modelling
methods for the prediction of virological response to combination HIV
therapy. Artificial Intelligence in Medicine 2009, 47:63-74.
Heider D, Verheyen J, Hoffmann D: Machine learning on normalized
protein sequences. BMC Research Notes 2011, 4:94.
Rhee SY, Taylor J, Wadhera G, Ben-Hur A, Brutlag DL, Shafer RW: Genotypic
predictors of human immunodeficiency virus type 1 drug resistance.
Proceedings of the National Academy of Sciences of the United States of
America 2006, 103:17355-17360.
Beerenwinkel N, Lengauer T, Daumer M, Kaiser R, Walter H, Korn K,
Hoffmann D, Selbig J: Methods for optimizing antiviral combination
therapies. Bioinformatics 2003, 19:I16-i25.
Altmann A, Beerenwinkel N, Sing T, Savenkov I, Daumer M, Kaiser R,
Rhee SY, Fessel WJ, Shafer RW, Lengauer T: Improved prediction of
response to antiretroviral combination therapy using the genetic barrier
to drug resistance. Antiviral Therapy 2007, 12:169-178.
Larder B, Wang DC, Revell A, Montaner J, Harrigan R, De Wolf F, Lange J,
Wegner S, Ruiz L, Perez-Elias MJ, Emery S, Gatell J, Monforte AD, Torti C,
Zazzi M, Lane C: The development of artificial neural networks to predict
virological response to combination HIV therapy. Antiviral Therapy 2007,
12:15-24.
Wittkop L, Commenges D, Pellegrin I, Breilh D, Neau D, Lacoste D,
Pellegrin JL, Chene G, Dabis F, Thiebaut R: Alternative methods to analyse
the impact of HIV mutations on virological response to antiviral therapy.
BMC Medical Research Methodology 2008, 8:68.
Altmann A, Daumer M, Beerenwinkel N, Peres Y, Schulter E, Buch J,
Rhee SY, Sonnerborg A, Fessel WJ, Shafer RW, Zazzi M, Kaiser R, Lengauer T:
Predicting the Response to Combination Antiretroviral Therapy:
Retrospective Validation of geno2pheno-THEO on a Large Clinical
Database. Journal of Infectious Diseases 2009, 199:999-1006.
Page 19 of 19
81. Draghici S, Potter RB: Predicting HIV drug resistance with neural
networks. Bioinformatics 2003, 19:98-107.
82. Hou TJ, Zhang W, Wang J, Wang W: Predicting drug resistance of the
HIV-1 protease using molecular interaction energy components. ProteinsStructure Function and Bioinformatics 2009, 74:837-846.
83. Liu TF, Shafer RW: Web resources for HIV type 1 genotypic-resistance test
interpretation. Clinical Infectious Diseases 2006, 42:1608-1618.
84. Rhee SY, Fessel WJ, Liu TF, Marlowe NM, Rowland CM, Rode RA,
Vandamme AM, Van Laethem K, Brun-Vezinet F, Calvez V, Taylor J, Hurley L,
Horberg M, Shafer RW: Predictive Value of HIV-1 Genotypic Resistance
Test Interpretation Algorithms. Journal of Infectious Diseases 2009,
200:453-463.
85. Petropoulos CJ, Parkin NT, Limoli KL, Lie YS, Wrin T, Huang W, Tian H,
Smith D, Winslow GA, Capon DJ, Whitcomb JM: A novel phenotypic drug
susceptibility assay for human immunodeficiency virus type 1.
Antimicrob Agents Chemother 2000, 44:920-928.
86. Vinod HD: Integer programming and theory of grouping. Journal of the
American Statistical Association 1969, 64:506-519.
87. Rao MR: Cluster analysis and mathematical programming. Journal of the
American Statistical Association 1971, 66:622-626.
88. Bradley PS, Fayyad UM, Mangasarian OL: Mathematical programming for
data mining: Formulations and challenges. Informs Journal on Computing
1999, 11:217-238.
89. Saglam B, Salman FS, Sayin S, Turkay M: A mixed-integer programming
approach to the clustering problem with an application in customer
segmentation. European Journal of Operational Research 2006, 173:866-879.
90. Tseng GC, Wong WH: Tight clustering: A resampling-based approach for
identifying stable and tight patterns in data. Biometrics 2005, 61:10-16.
91. Tibshirani R, Walther G, Hastie T: Estimating the number of clusters in a
data set via the gap statistic. Journal of the Royal Statistical Society Series BStatistical Methodology 2001, 63:411-423.
92. Hastie T, Tibshirani R, Friedman J: The Elements of Statistical Learning.
New York, NY: Springer;, 2 2009.
93. King BM, Tidor B: MIST: Maximum Information Spanning Trees for
dimension reduction of biological data sets. Bioinformatics 2009,
25:1165-1172.
94. Diaconis P, Goel S, Holmes S: Horseshoes in multidimensional scaling and
local kernel methods. Annals of Applied Statistics 2008, 2:777-807.
95. HIV Drug Resistance Database. [http://hivdb.stanford.edu/cgi-bin/
PIResiNote.cgi].
96. Mammano F, Trouplin V, Zennou V, Clavel F: Retracing the evolutionary
pathways of human immunodeficiency virus type 1 resistance to
protease inhibitors: Virus fitness in the absence and in the presence of
drug. J Virol 2000, 74:8524-8531.
97. de Meyer S, Vangeneugden T, van Baelen B, de Paepe E, van Marck H,
Picchio G, Lefebvre E, de Bethune MP: Resistance profile of darunavir:
Combined 24-week results from the POWER trials. Aids Res Hum Retrovir
2008, 24:379-388.
98. Nalam MNL, Peeters A, Jonckers THM, Dierynck I, Schiffer CA: Crystal
structure of lysine sulfonamide inhibitor reveals the displacement of the
conserved flap water molecule in human immunodeficiency virus type 1
protease. J Virol 2007, 81:9512-9518.
99. Hertogs K, de Bethune MP, Miller V, Ivens T, Schel P, Van Cauwenberge A,
Van den Eynde C, Van Gerwen V, Azijn H, Van Houtte M, Peeters F,
Staszewski S, Conant M, Bloor S, Kemp S, Larder B, Pauwels R: A rapid
method for simultaneous detection of phenotypic resistance to
inhibitors of protease and reverse transcriptase in recombinant human
immunodeficiency virus type 1 isolates from patients treated with
antiretroviral drugs. Antimicrob Agents Chemother 1998, 42:269-276.
doi:10.1186/1471-2105-12-477
Cite this article as: Doherty et al.: A multifaceted analysis of HIV-1
protease multidrug resistance phenotypes. BMC Bioinformatics 2011
12:477.