Cognitive Impairment and End-of-Life Treatment Intensity Lauren Nicholas Jack Iwashyna
advertisement

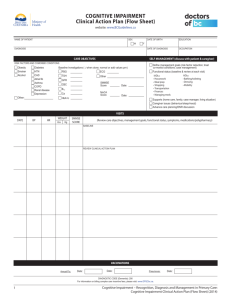
Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Lauren Nicholas Jack Iwashyna Ken Langa David Weir University of Michigan June 29, 2010 Lauren Nicholas Jack Iwashyna Ken Langa David Weir Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Motivation Motivation End-of-life care is a controversial policy topic: Should Medicare pay for discussions about end-of-life treatment preferences? Help to ensure patients life-sustaining treatment requests honored, but raises concern about treatment denials Care for beneficiaries with chronic illnesses during the last two years of their lives accounts for about one-third of all Medicare spending (Dartmouth Atlas Project) It is unknown whether high-intensity, lifesaving efforts reflect patient preferences Many patients reach end-of-life without advance directives Cognitive impairment likely to inhibit patients’ abilities to provide informed consent Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Motivation Cognitive Impairment is Common Near the End-of-Life Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Motivation End-of-Life Preferences Not Well Documented Prior to End of Life Advance Directive AD- All Possible Care AD- limit EOL Care AD- refuse certain Treatments AD- Palliative Care Only R consulted others about EOL R has Power of Attorney R talk about EOL EOL decisions needed R Participate in EOL decisions EOL decision all care possible Normal Cog 0.47 0.03 0.91 0.83 0.93 0.28 0.54 0.61 0.41 0.45 0.18 Nicholas et al. CIND 0.43 0.06 0.90 0.82 0.95 0.28 0.53 0.56 0.41 0.32 0.18 Dementia 0.40 0.03 0.93 0.82 0.95 0.26 0.56 0.48 0.42 0.18 0.18 Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Empirical Approach Research Questions 1 Does end-of-life treatment intensity vary for cognitively impaired and unimpaired older adults? Intensive Care Unit Life-Sustaining Medical Treatment Hospice Care 2 Are advance directives related to differential use of end-of-life treatment options? Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Empirical Approach Data Health and Retirement Study Longitudinal, nationally representative survey of older Americans Collect demographic, health characteristics of respondents including cognitive functioning assessment Conduct exit interviews with next-of-kin after death of a respondent including end-of-life treatments and preferences 86% of eligible respondents consent to Medicare claims linkage, providing administrative records of health care utilization for those aged 65 and above or disabled Study population includes 4,339 decedents with assessed cognitive functioning and linked Medicare data 4,245 also have exit interviews Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Empirical Approach Data Cognitive Functioning in the End-of-Life Period Cognitive functioning was determined by using a 35-point cognitive scale for self-respondents, assessments of memory and judgment for respondents represented by a proxy Sample limited to decedents with a completed interview in the wave prior to death Cognitive functioning data used to classify respondents as normal cognition, cognitively impaired non-demented (CIND), or cognitively impaired based on an algorithm mapping HRS question responses to clinical dementia screenings conducted in the Aging, Demographics, and Memory Study Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Empirical Approach Data Medicare Claims: End-of-Life Treatment Intensity Limit sample to beneficiaries enrolled in Fee-for-Service Medicare for all of the 6 months prior to death Use MEDPAR inpatient hospitalization records to capture measures of end-of-life treatment intensity following Barnarto (2009): Life-Sustaining treatments: intubation/mechanical ventilation, tracheostomy, gastrostomy tubes, hemodialysis, enteral or parenteral nutrition, CPR Intensive Care Unit Hospice claims provide information about whether and how long decedent received palliative hospice care Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Empirical Approach Methods Analytic Methods Multivariate logistic regression models of end-of-life treatments on respondent cognitive functioning and demographic characteristics All-decedent models examine odds of any hospitalization and hospice use in the last six months of life ICU usage and life-sustaining treatments conditional on hospitalization CIND and dementia pooled in cognitively impaired category, results are similar for demented-only vs. normal or with 3 categories Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Descriptive Statistics HRS Decedents, 1998 - 2007 Any EOL Hospitalizations EOL Hospice Age at Death Female Non-White Years Education Household Wealth ($) Household Income ($) Married Divorced Widowed or Single Observations Normal Cog 0.60 0.33 78.2 0.46 0.10 12.19 303,705 35,488 0.53 0.09 0.37 1,816 Nicholas et al. CIND 0.62 0.31 82.6 0.51 0.19 10.73 209,757 28,078 0.44 0.07 0.49 1,199 Dementia 0.56 0.32 85.7 0.59 0.21 9.68 149,104 21,558 0.36 0.06 0.58 1,324 Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Descriptive Statistics Utilization at the End of Life .4 .2 0 0 .2 .4 .6 Life-Sustaining Treatment Cognitively Impaired and Unimpaired Decedents .6 End of Life Hospitalization Cognitively Impaired and Unimpaired Decedents no CI CI or CIND no CI CI or CIND .4 .2 0 0 .2 .4 .6 Any Hospice Cognitively Impaired and Unimpaired Decedents .6 Any ICU Stay Cognitively Impaired and Unimpaired Decedents no CI CI or CIND Nicholas et al. no CI CI or CIND Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Descriptive Statistics Advance Directives and Treatment Intensity Life-Sustaining Treatment 0 .1 .2 .3 .4 Cognitively Impaired and Unimpaired Decedents no CI CI or CIND No AD Nicholas et al. no CI CI or CIND AD Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Multivariate Results Risk-Adjusted End-of-Life Treatment Intensity: 1998 - 2007 Any Hospitalization Hospice Cog. Impaired 0.95 [0.83,1.08] 0.94 [0.81,1.08] Female 1.08 [0.95,1.22] 1.14 [0.99,1.30] Non-White 1.12 [0.94,1.33] 0.60** [0.49,0.73] Age < 70 1.35* [1.05,1.75] 0.71* [0.54,0.94] Age 75-80 1.25 [0.98,1.58] 0.94 [0.73,1.21] Age 80-85 1.21 [0.96,1.52] 0.93 [0.73,1.18] Age 85-90 1.33* [1.05,1.67] 0.95 [0.74,1.21] Age 90+ 1.06 [0.84,1.33] 1.15 [0.90,1.46] Odds ratios and 95% confidence intervals * (p<0.05), ** (p<0.01) 4,339 decedents enrolled in FFS Medicare. Models include controls for year of death. Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Multivariate Results Risk-Adjusted End-of-Life Treatment Intensity: Hospitalized Decedents 1998 - 2007 Intensive Care Unit Inpatient Death Life-sustaining Cog Impair 0.68** [0.57,0.81] 0.98 [0.82,1.16] 0.82* [0.67,0.99] Female 1.14 [0.97,1.34] 1.03 [0.88,1.21] 0.99 [0.82,1.19] Non-White 1.52** [1.22,1.89] 1.45** [1.15,1.81] 2.53** [2.01,3.19] Age < 70 1.23 [0.89,1.71] 0.96 [0.69,1.34] 2.07** [1.46,2.94] Age 75-80 1.15 [0.85,1.57] 1.09 [0.80,1.49] 1.24 [0.88,1.75] Age 80-85 0.96 [0.71,1.28] 1 [0.74,1.34] 1.02 [0.73,1.42] Age 85-90 0.77 [0.57,1.04] 0.98 [0.73,1.33] 0.88 [0.62,1.24] Age 90+ 0.58** [0.42,0.79] 0.82 [0.60,1.11] 0.63* [0.44,0.90] Odds ratios and 95% confidence intervals, * (p<0.05), ** (p<0.01) 2,579 decedents enrolled in FFS Medicare. Models include controls for year of death. Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Multivariate Results Life-Sustaining Treatments in the Last Six Months of Life: Hospitalized Decedents 1998 - 2007 Cognitively Impaired Non-White Intubation/Ventilation 0.8 [0.63,1.01] 2.15** [1.64,2.82] Tracheostomy 0.72 [0.39,1.31] 1.24 [0.60,2.59] CPR 0.85 [0.54,1.33] 1.87* [1.12,3.10] Hemodialysis 1.09 [0.72,1.64] 3.06** [2.02,4.64] Gastrostomy 1.11 [0.76,1.62] 2.45** [1.66,3.62] Any Feeding Tubes 1.02 [0.76,1.37] 2.19** [1.59,3.00] Odds ratios and 95% confidence intervals, * (p<0.05), ** (p<0.01) 2,579 decedents enrolled in FFS Medicare. Models include controls for year of death, age and sex. Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Multivariate Results Decedent Preferences and End-of-Life Treatment Intensity: 1998 - 2007 Any Hospitalization Hospice Cog. Impaired 0.91 [0.79,1.05] 1.06 [0.91,1.24] <HS EDU 1.21* [1.02,1.44] 0.99 [0.83,1.19] HS grad 1.17 [0.98,1.38] 1.03 [0.86,1.23] Advance Directive 0.71** [0.58,0.86] 1.19 [0.97,1.46] R consult others EOL 1.46** [1.20,1.77] 1.48** [1.21,1.81] Power of Attorney 1.01 [0.87,1.18] 1.32** [1.12,1.55] R talk about EOL wishes 1.21** [1.05,1.39] 1.18* [1.02,1.37] Odds ratios and 95% confidence intervals * (p<0.05), ** (p<0.01) 4,245 decedents enrolled in FFS Medicare with exit interviews. Models control for age, race, sex, wealth, year of death. Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Results Multivariate Results Decedent Preferences and End-of-Life Treatment Intensity: Hospitalized Decedents 1998 - 2007 Cog. Impaired < HS EDU HS grad Advance Directive Power of Attorney R talk EOL wishes Intensive Care 0.63** [0.53,0.76] 1.29* [1.03,1.62] 1.1 [0.87,1.37] 0.71* [0.54,0.94] 0.9 [0.74,1.09] 0.91 [0.76,1.08] Inpatient Death 0.92 [0.76,1.11] 0.99 [0.79,1.23] 0.96 [0.77,1.20] 0.76* [0.58,0.98] 0.81* [0.66,0.98] 0.85 [0.71,1.01] Life-Sustaining 0.75** [0.61,0.93] 0.98 [0.76,1.27] 0.87 [0.67,1.12] 0.66** [0.48,0.90] 0.98 [0.78,1.22] 0.9 [0.74,1.10] Odds ratios and 95% confidence intervals, * (p<0.05), ** (p<0.01) 2,535 decedents enrolled in FFS Medicare with exit interviews. Models control for age, race, sex, wealth, year of death. Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Conclusions and Policy Implications Summary of Findings 58% of older adults hospitalized in the last 6 months of life are moderately or severely cognitively impaired Only 40% of this group has an advance directive More than 41 of this group receive life-sustaining treatment and 40% treated in ICU Odds of aggressive treatment receipt are much higher for minority seniors Cognitively impaired and unimpaired face same odds of any admission and in-hospital death Power of attorney and associated with higher odds of hospice use, less inpatient treatment intensity Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity Cognitive Impairment and End-of-Life Treatment Intensity Conclusions and Policy Implications Policy Implications Large proportion of decedents reach EOL without documented treatment preferences and possible incapacity for informed consent Physician discussions earlier in life potentially helpful to create awareness, decisions while unimpaired, emphasize advance directives Increased distribution of advance directives in outpatient setting Change default treatment options, less care rather all care possible as automatic Recognition of cognitive impairment as a terminal illness Nicholas et al. Cognitive Impairment and End-of-Life Treatment Intensity