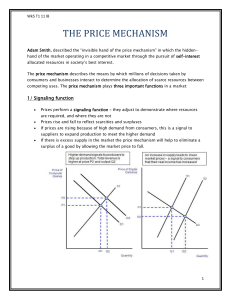
Cli i l E id I Clinical Evidence, Insurance Coverage and “Rationing”
advertisement

Clinical Evidence, Insurance Cli i l E id I Coverage and “Rationing” Coverage and Rationing Bryan Dowd and Kirk Allison Division of Health Policy and Management School of Public Health University of Minnesota AcademyHealth A d H lth June 2010 1 Who cares about evidence? H.R. 3590: Patient Protection and Affordable Care Act Affordable Care Act Abolished: Ab li h d Federal Coordinating Council for Comparative Effectiveness Research Created: Patient Centered Outcomes Research Institute Patient Centered Outcomes Research Institute (“neither an agency nor an establishment of the (“neither an agency nor an establishment of the United States Government”) 2 HR 3590 now allows … • “The Secretary may only use evidence and findings … to make a determination regarding coverage under Title XIII if such use is through an iterative, transparent process which includes public hi h i l d bli comment and considers effect on subpopulations.” • But “not … in a manner that treats extending the life of an elderly, disabled or terminally ill individual as of lower value than extending the life of an i di id l h i individual who is younger, nondisabled, or not di bl d terminally ill.” 3 Patient Centered Outcome Research Institute Funding Patient Centered Outcomes Trust Fund • 2010‐2012 ‐ $210M (total) • 2013 2013‐2019 2019 ‐ $150M per year $150M per year ((=$1.05B) $1.05B) plus 2013 $1 2013: $1 per health plan enrollee * h lh l ll * 2014‐2019: $2 per health plan enrollee •Medicare A or B; Insured or Self‐insured •Medicare A or B; Insured or Self‐insured 4 But before we get too giddy … g g y • Most Americans never have heard of health services research (HSR). CER may be the way they will hear of us • CER may be the way they will hear of us. • What will they hear? – We are the technical assistance arm for the “death panels” – We are helping health plans (which we now know to be evil) ration care – We are independent producers of objective data on the efficacy of medical treatments and delivery y y systems. 5 Crashing the party Crashing the party • Martin Feldstein writing in the Wall Street J Journal (April 12, 2009) says “ObamaCare Is l (A il 12 2009) “Ob C I All About Rationing: Overspending is far preferable to artificially limiting the availability preferable to artificially limiting the availability of new procedures and technologies.” • Senator Orrin Hatch (September, 2009): "We We don don'tt want to turn health care over to a want to turn health care over to a bunch of bureaucrats in Washington, who then will determine what kind of health care we have … (a)nd you know that rationing is going to happen." 6 What rationing isn’tt What rationing isn • Peter Singer (NY Times, 2009): Peter Singer (NY Times 2009): “(h)ealth care is a scarce resource, and all scarce resources are rationed in one way or another.” • So all consumption decisions are rationing? So all consumption decisions are rationing? • An example of “linguistic larceny.” • Are all armed conflicts war? (Duels, skirmishes battles?) skirmishes, battles?) 7 What rationing is: A A necessary but not sufficient condition b t t ffi i t diti • Rationing is a binding g g constraint imposed on p consumption quantities by an entity that is not the consumer, but is external to the consumer. the consumer, but is external to the consumer. • Rationing is the opposite of “self‐rationing.” • Rationing can be a ceiling (supply) quantity or a floor (demand) quantity floor (demand) quantity. • Rationing care on the basis of age is a ceiling g g g constraint on supply. Mandatory health insurance (H R 3590) is a floor constraint on insurance (H.R. 3590) is a floor constraint on demand. 8 The purposes of health plans p p p The purposes of health insurance: 1 Spread random risk among a group of individuals. 1. S d d ik f i di id l 2. Provide a Nyman‐esque financing mechanism in the absence of capital markets (e.g., to finance a dangerous, but potentially life‐saving operation) to pay for efficient moral hazard for efficient moral hazard. Additional services health plans can provide 1. Negotiate discounts from providers. y (p q y) 2. Overcome information asymmetries (price and quality) between consumers and providers. Not to redistribute income between the rich and poor. to redistribute income between the rich and poor. That’s the job of government and private charities. 9 How do health plans accomplish the first two purposes? By putting some portion By putting some portion of the cost of some of the cost of some services into the health insurance premium. • The question is what portion of what services? • All health plans, public and private, face this same question. • Private health plans’ decisions are disciplined by the market by the market. • Public health plans’ decisions are disciplined b by politicians. li i i 10 What can go wrong? What can go wrong? • Market failure: • Price Price distortion (e.g., inadequate risk distortion (e g inadequate risk adjustment) • Poor information (e.g., inability to target services precisely) p y) • Public choice problems: • Group purchase, state‐dependent preferences inappropriate government preferences, inappropriate government intervention 11 Four types of health care services Four types of health care services 1. Riskless services (e.g., preventive care) – not i insurable, no financing function required, but bl fi i f i i d b some might represent services with a positive return on investment for the health f h h lh plan 2. Cost‐saving services – no coverage issues 3 Services with (a) no medical benefit; or (b) 3. Services with (a) no medical benefit; or (b) risks that exceed benefits 4. Costly services with medical benefits that y exceed the risks and (a) less costly therapeutically equivalent; or (b) not. 12 1. Riskless services • Not insurable, but consumers often demand coverage anyway why? coverage anyway, why? • If everyone consumed the service, consumers would be indifferent between having the cost in the premium or paying it out of pocket. • The “risk” involves other people’s consumption If you consume the services consumption. If you consume the services and others don’t, you get a “second discount.” • When the cost of riskless services is put into the premium, who subsidizes whom? the premium, who subsidizes whom? 13 Examples • The cost of mammography ranges between $80 and h f h b $ $200. Is financing a rationale? • Coverage of mammograms transfers income from: Non‐using using women to using women women to using women • Non • From men and children to women • Who are the eligible non‐users? Older women and minorities subsidize younger white women (Ra l et al 2000) (Rawl, et al., 2000) • Reducing the point‐of‐purchase price for everyone is an extraordinarily inefficient di il i ffi i way to make a service more k i affordable for the poor (Manning, et al., 1987). It’s also likely to be regressive likely to be regressive. • Symmetric results for PSA screening. 14 2. Cost‐saving services • If the health plan saves more than a dollar for y p g every dollar spent on coverage for a service, the health plan will go to the bank, take money out of p p y its profits account and pay consumers to consume the service. • Neither coverage nor rationing should be an issue. Neither coverage nor rationing should be an issue • Examples (Cohen, et al., 2008): – One‐time colonoscopy screening for colorectal cancer y in men 60–64 years old – Cochlear implants in profoundly deaf children. – Paying people to take Paying people to take their meds (Belluck, 2010) or use th i d (B ll k 2010) health clubs. 15 3: Medically ineffective services or risks exceed benefits a. Medically ineffective services y – Virtual colonoscopies on 49 year old asymptomatic Presidents of the United States – Arthroscopic knee surgery for osteoarthritis (2 randomized trials). Medicare suspended payment but we still do 1 million a year at $7,000 each. still do 1 million a year at $7,000 each. b. Medically effective services with risks that exceed b Medically effective services with risks that exceed benefits – Angiograms on patients with shortness of breath g g p – Lung volume reduction surgery (some benefit but 10 percent mortality risk) – CT scan for coronary calcium in 49 year old asymptomatic Presidents of the United States 16 4 Medically effective services but 4. Medically effective services, but … aa. There is a less expensive, therapeutically There is a less expensive therapeutically equivalent alternative – Proper sequence of care – Pharmaceutical regimens Pharmaceutical regimens – Back pain b. So the interesting case is costly, medically b So the interesting case is costly medically effective care with benefits that exceed the risks and no therapeutically equivalent lower risks, and no therapeutically equivalent lower cost alternative. 17 What rationing isn’tt, revisited What rationing isn revisited Rationing is not failure to cover: Rationing is not failure to cover: • Riskless care, unless there are missing capital markets • Medically ineffective care Medically ineffective care • Care for which the risks exceed the costs • Treatment A when therapeutically equivalent Treatment B costs less … and that’s the health plan I want to join. 18 The role of CER and HSR 1. Identify effective and ineffective medical t t treatments (either universally or specific to t ( ith i ll ifi t particular patients); 2. Identify risks and benefits of treatments; and 3 Identify therapeutically equivalent treatments. 3. Identify therapeutically equivalent treatments HSR has additional roles, such as policy analysis, organizational, sociological, legal and organizational, sociological, legal and management issues; pricing issues; identification of and proposed solutions for identification of, and proposed solutions for, sources of market failures. 19 Effective communication Effective communication 1 Information 1. Information that educates consumers and that educates consumers and providers about the risks and benefits of medical treatments is likely to be effective di l t t t i lik l t b ff ti (lung volume reduction surgery). 2. Information that pits consumers against “society” society (e.g., (e g “the the treatment is medically treatment is medically effective but costs too much” or “produces t f QUALY too few QUALYs per dollar”) is likely to be d ll ”) i lik l t b ineffective, especially if the consumers are part of a well‐organized interest group. 20 What can go wrong with CER? 1. Public and private health plans could use the results to limit payment for medically effective care. Policy question: Why exactly would that happen? 2 2. H R 3590 language on research methods (p. 614‐616): H.R. 3590 language on research methods (p 614‐616): “The Institute shall establish a standing methodology committee (which), shall adopt … the methodological standards developed p and updated p byy the methodology gy committee…” aa. Industry could attempt to make the methodological Industry could attempt to make the methodological requirements so strict that little research can be done. b. Methodologists could insist that only RCTs produce valid b Methodologists could insist that only RCTs produce valid causal knowledge, accomplishing the same effect as (a).