Mental Health and Substance Abuse Under Parity and Health Reform:
advertisement
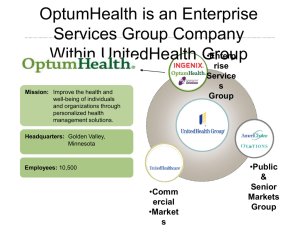
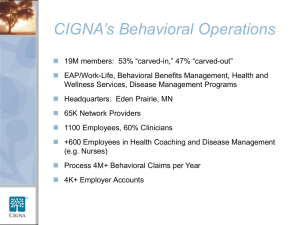
Mental Health and Substance Abuse Under Parity and Health Reform: Marriage Made in Heaven? Kavita Patel, MD, MSHS Ken Wells MD, MD MPH Moderators A d AcademyHealth H l h 2010 Background to Panel Coverage for MHSA care has expanded and contracted over the last 40 years For past 10-15 years, MHSA care has been more intensively managed than medical care in private sector. Arguments for and against parity and level of coverage overall and for vulnerable MHSA groups are based on principles/biases, market experience, and some data; But over the last 15-20 years, has typically been less generous than for medical care. Opinions are often strong and findings are somewhat mixed and lag behind the evolving market and new policies. Complex p policy p y changes g and their rationale are often not transparent p in the community. Can we understand together what may happen and what we need to know to make health reform & parity work for MHSA? Panel Members Kavita Patel – Policy staff perspective Haiden Huskamp (Harvard) – MHSA parity and reform/federal employees Dominic Hodgkin (Brandeis) – MHSA reform and parity; substance abuse F li Jones Felica J (Healthy (H l h African Af i American A i FFamilies) ili ) – community i perspective Benjamin Miller (University (Uni ersit off C Colorado) l rad ) – medical homes h mes and mental health Francisca Azocar (Optum Health Behavioral Solutions) – behavioral health management perspective Ken Wells (UCLA/RAND) – old guy (historical) perspective 10 Key Questions 1. What are opportunities for parity & reform to improve public MHSA? Who will gain and how? 2. What will happen to access, costs, and quality of behavioral health care? 3. How will the market for behavioral health services change? 4. What will happen to the public sector and persons left out of coverage (such as undocumented immigrants)? 5. What are the challenges -- what might go wrong? 6. How can community members become informed of choices and options for behavioral health care? Can there be community accountability? 7. What about Wh b prevention? i ? Can C it i bbe d defined, fi d implemented, i l d and d covered d for f behavioral health under reform? 8. Medical homes: what do we know and for whom, in terms of behavioral health care and outcomes? 9. What can be achieved in health information technology for MHSA? 10. What are key research questions? How can they be addressed to inform policy in real time? Applicability Financial Coverage Mental Health Parity and Addiction Equity Act (2008) Patient Protection and Affordable Care Act (2010) Comments Group plans subject to: • Employee Retirement I Income SSecurity i A Act • Public Health Services Act • Internal Revenue Code Added to previous Group plans: + “Q “Qualified lifi d Health H l h Plans” Pl ” + Medicaid The major expansion comes from the intro. of the rules to the exchanges =Annual/Lifetime limits =Deductibles, Co-pays and out-of-pocket expenses across Mental, Surgical, and Medical coverage. No Change (non-managed care benchmark and benchmark-equivalent) benchmark eq i alent) + Individual plans. The financial parity i established by the MHPAEA continue under the PPACA MHPAEA PPACA Comments Treatment Coverage Equivalent limits on the freq. of: • treatments • # of visits • # days of coverage • other limits on scope or duration of treatment. treatment Creates the Essential Health Benefits Package • Must be offered byy all plans in the exchanges. EHBs will include both mental health treatments as well as addiction and substance abuse assistance. Small S ll Business Exemption Companies averaging C 1 to 100 employees/year. ??? PPACA doesn’t d ’ clarify if the exchange’s rules will apply to the previously exempted small businesses. Parity Law: Access and Cost MHPAEA improves benefits for some who already had MH/SA coverage Based on previous parity experience: Expect reduced out-of-pocket burden, but little effect on utilization or total spending (on average) But new restrictions on managed care tools could mean different impacts this time (the final regulations are crucial) MHPAEA could lead some employers to drop MH/SA coverage Little sign of this so far Federal Health Reform: Access and Cost Under U d PPACA, PPACA many uninsured i d people l will ill get coverage – improving access: Low-income uninsured can jjoin Medicaid Others will get private insurance (some through exchanges) But, issues: Will state MH/SA budgets be shifted to Medicaid? Implications for safety-net providers? Insurance models mayy not cover wraparound p services currentlyy provided through state systems Key Issues for Research Impact of parity for non-quantitative treatment limits, diagnoses covered, covered out of network benefit Impact on public system – will vary based on state/local response Can provider capacity handle increased demand? Differingg impacts p for subgroups g p depending p g on prior p situation (e.g. newly insured vs. other) Complications for research include: Multi-layered implementation of parity and health reform laws Difficulty identifying comparison groups for many segments of population Lack of information on MH/SA management practices Felica Jones: HAAF Parity and health reform are first of all about improving social justice in healthcare Can underserved communities and those with behavioral h l h conditions health di i understand d d and d benefit? b fi ? Community engagement skills are needed to realize the goals l off parity/reform i / f for f MHSA: MHSA Advocacy: Bring people to the table, support their voice, and exercise their options for themselves themselves, their family family, and their community under parity/reform Knowledge Exchange: 2 2-way way sharing of information across people affected, to build capacity for all, to use and respond to opportunities & challenges of reform How We Build Capacity Build relationships and trust, & invite people to the table Knowledge exchange activities: conferences, Knowledge-exchange conferences webinars webinars, websites websites, discussion groups, newsletters, radio Develop a common, simple language S Support working ki groups off many stakeholder k h ld levels, l l to workk together as equals on key parity/reform issues Develop action plans & programs to support understanding and implementation Disseminate information & products to community Witness 4 Wellness & Community Partners in Care 37% of underserved community agency clients are depressed Many agencies are stressed and short-staffed Limited Li it d kknowledge l d off evidence-based id b d services i delivery d li models d l High cultural competency and knowledge of local populations Little understanding of parity/reform and what it means for them CPIC (Community Partners in Care) Fragmentation Physical Health y Mental Health Care Delivery Systems Payment Systems Training and Education Systems P bli P Public Perception i Primary Care Mental Health Never Sits Alone Psychosocial Determinants of Health Medical Presentations Which Need Behavioral Treatment Mental Health Presentations Comorbid Medical and Psychological Presentations Severe Mental Health/ Substance Abuse Presentations Annual Cost – those without MH condition Annual Cost – those with MH condition Heart Condition $4,697 $6,919 High Blood Pressure $3,481 $5,492 Asthma , $2,908 $4,028 , Diabetes $4,172 $5,559 Number of Physical Symptoms and Likelihood of Mental Diagnosis 90% 80% 70% 60% 50% 40% 30% 20% 10% 0% 0-1 01 2-3 23 4-5 45 6-8 68 >8 Original source data is the U.S. Dept of HHS the 2002 and 2003 MEPS. AHRQ as Spitzer, R. L., J. B. W. Williams, et al. (1994). "Utility of a New Procedure for Diagnosing Mental cited in Petterson et al. “Why there must be room for mental health in the Disorders in Primary Care: The PRIME‐MD 1000 Study." JAMA 272(22): 1749‐1756. medical home (Graham Center One‐Pager) Opportunities within the Patient‐Centered Medical Home? Joint Principles of PCMH Personal Physician Physician Directed Practice y Whole Person Orientation Care is Coordinated Care is Coordinated and/or Integrated Quality and Safety Enhanced Access to Care Enhanced Access to Care Payment to Support PCMH Federal Mental Health Parity: A Managed Behavioral Health Perspective Brief overview of the Federal Mental Health Parity (FMHP) regulations What are the tools and processes that MBHO’s are following to become parity compliant What are the challenges faced by health plans, MBHO’s employers, patients and providers What are some unforeseen consequences What are opportunities for improving access and quality of care Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. General Rule and Categories Group health plans offering both medical/surgical benefits and mental health or substance use disorder benefits must ensure that the financial requirements q and treatment limitations are no more restrictive than those predominately applied to substantially all medical/surgical benefits under the plan No coverage mandate – plans (or state law for insured plans) drive what is covered, but if you cover it, you must do so in parity 1. Financial Requirements: Copayments Coinsurance C i Deductibles Out-of-pocket maximums Annual dollar limits on benefits* Lifetime dollar limits on benefits* *Exceptions to Interim Final Rule per 1996 MHP Act requirements. Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. General Rule and Categories 2. Quantitative Limits (illustrative list, not exhaustive): Examples: Day limits Visit limits Limits on number of episodes of treatment 3. Non-Quantitative Limits (illustrative list, not exhaustive): M Medical di l managementt standards t d d lilimiting iti or excluding l di b benefits fit b based d on medical di l necessity or medical appropriateness, or based on whether the treatment is experimental or investigative Formulary design for prescription drugs Standards for provider admission to participate in a network, including reimbursement rates Plan methods for determining usual, customary and reasonable charges Refusal to pay for higher-cost therapies until it can be shown that a lower-cost therapy is not effective (also known as fail-first or step therapy protocols) – Example: EAP gatekeeper t k models d l Exclusions based on failure to complete a course of treatment Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. Benefit Category Classification The Interim Final Rule organizes benefits by y Classification You must align the Type, Level and Coverage g Unit for each classification Classification Type The Rule establishes six benefit classifications: Refers to a requirement or limitation of the same nature t (e.g., ( copayments, t coinsurance i and d deductibles are different types of financial requirements) 1 Inpatient, In-Network 2 Inpatient, Out-of-Network Compare p type yp to type yp 3 Outpatient, In-Network Level 4 Outpatient, Out-of-Network Refers to varied magnitudes of a single type that may exist (e.g., copayments of $10, $20 or $30 based on service, each of those is a Level of the copayment Type) 5 Pharmacy 6 Emergency Apply the predominant level Coverage Unit Parity is to be assessed classification by classification Refers to groupings of individuals used to determine benefits, premiums or contributions (e.g., individual, individual + spouse, family, etc.) Assess parity for coverage unit Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. Quantitative Treatment Limitations Quantitative treatment limitations (e.g., day and visit limits): Apply the same test as financial requirements C Cumulative l ti quantitative tit ti ttreatment t t li limitations it ti may not be separate! IInpatient, i in-network i k limit li i off 60 d days ffor medical di l and d 60 d days for MH/SUD does not comply, must have a single combined day limit Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. Non-Quantitative Treatment Limitations General parity rule is applied differently to non-quantitative treatment limits than for financial requirements q and q quantitative treatment limits No “substantially all” or “predominant” test applies to non-quantitative treatment limits The rule for non-quantitative treatment limits is stated as: The processes, strategies, evidentiary standards or other factors used in applying non-quantitative treatment limits must be “comparable”, and applied no more stringently” stringently for mental health and substance use “applied disorder benefits, to the processes, strategies, etc. applied to medical/surgical benefits in the same Classification Processes for applying medical management standards specifically include: pre-authorization, concurrent review, retrospective review, case management and d utilization ili i review i Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. Next Steps: Compliance Assessment Tool Developed an assessment guide to assist our clients in applying pp y g the formula and tests articulated by y the Interim Final Rule Sections include: q Financial Requirements Quantitative Treatment Limitations Non-Quantitative Treatment Limitations Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. Next Steps: Benefit Data Assessment Profile This toolcollects the required medical and behavioral plan data needed to assess both p parity y compliance p ((in conjunction j with the Compliance p Assessment Tool)) and the cost impact of parity changes necessary for compliance with the Interim Final Rule This tool works to align key medical and behavioral plan data for the purposes of: Identifying non-compliant elements of the existing plan designs Providing information regarding potential plan changes so that a cost estimate can be established for new designs Confidential property of OptumHealth. Do not distribute or reproduce without express permission from OptumHealth. Touch of History: H lth IInsurance E Health Experiment i t (HIE) Randomized trial of variations in familyy health insurance plans p on use/costs/outcomes (1976-1981) -- individual deductible, free care, or coinsurance (25,50,95) plans up to cap on out-of-pocket expenses. Annual MH outpatient costs/enrollee modest in free care; costs less in less generous plans; MH costs more price responsive than medical but less than expected. No significant average difference by plan in mental health outcome (MHI) but significant interaction: Low income & good MH less distress in cost-sharing than free care plans Low income & poor MH tend to have greater well-being in free care than h cost sharing h plans l Keeler, Manning, Wells (1988); Manning et al., (1986); Wells et al (1987;89;90) ( ; ; ) What are roles of MH professionals in realizing parity goals? (KW) Adopt p a public p health perspective p p Implement a range of EBPs, more rigorously Monitor outcomes, improve p data systems y Expand prevention/early intervention programs and outcomes Develop practice quality and efficiency standards Work with diverse stakeholders toward implementation Develop new models of services delivery in partnership to achieve reach/quality Evaluate cost-effectiveness/comparative effectiveness Ad Advocate for f iinclusion l i off consumers and d community i members b with ih MHSA conditions as co-leaders 10 Key Questions 1. What are opportunities for parity & reform to improve public MHSA? Who will gain and how? 2. What will happen to access, costs, and quality of behavioral health care? 3. How will the market for behavioral health services change? 4. What will happen to the public sector and persons left out of coverage (such as undocumented immigrants)? 5. What are the challenges -- what might go wrong? 6. How can community members become informed of choices and options for behavioral health care? Can there be community accountability? 7. What about Wh b prevention? i ? Can C it i bbe d defined, fi d implemented, i l d and d covered d for f behavioral health under reform? 8. Medical homes: what do we know and for whom, in terms of behavioral health care and outcomes? 9. What can be achieved in health information technology for MHSA? 10. What are key research questions? How can they be addressed to inform policy in real time?