Fundamental Problems with a Class of Quality and Safety Measures The Perils of Exposure‐Time M i c h a e l D. H...
advertisement

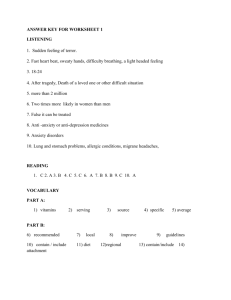
Fundamental Problems with a Class of Quality and Safety Measures The Perils of Exposure‐Time M i c h a e l D. H o we l l , M D M P H D i r e c t o r, C r i t i c a l C a r e Q u a l i t y A s s o c i a t e D i r e c t o r, M e d i c a l C r i t i c a l C a r e D i r e c t o r, R e s e a r c h C o r e f o r I n S I G H T From the Silverman Institute for Health Care Quality & Safety Beth Israel Deaconess Medical Center Harvard Medical School Disclosures E Employment l t Beth Israel Deaconess Medical Center G Grants Robert Wood Johnson Foundation Grant # 65121 (PI): Advancing the Science of Quality Improvement G # 6 (PI) Ad i h S i f Q li I Grant # 66350 (PI): Physician Faculty Scholars Program Center for Integration of Medicine and Innovative Technology (CIMIT) Clinical Systems Innovation Grant 2010 (Co‐investigator) Other (Commercial / Financial / Etc.) None An Important Category of Quality and Safety Measures “EXPOSURE‐TIME” METRICS A Major Category of Measures in QI j g y Q Risk = Risk # of bad events Length of time patients are eligible to have event Ventilator‐Associated Pneumonia (VAP) ( ) VAP risk = 1000 * VAP risk 1000 # of VAPs Ventilator‐days Falls Fall risk = 1000 * Fall risk 1000 # of falls Patient‐days Central Line Infections Central line = 1000 * infections # of line infections Central line days How prevalent are these measures? Recommended, Required, or Being Tested By Metric Falls or falls with injury per 1,000 patient‐days Pneumonias per 1,000 ventilator‐days Bloodstream infections per 1,000 central‐line‐days l d f ll d Infections per 1,000 urinary‐catheter days Institute for Healthcare I Improvement t The Joint C Commission i i 2,3,4,8 10 National National Quality State‐level Healthcare S f t N t Safety Network k F Forum public reporting bli ti 1 9, 10 5,6,7,11,12 Public reporting p g BIDMC rate = 3.44 Conclusion: BIDMC medical floors are 21% safer than Hospital X’s medical floors. Right? g Hospital X’s rate = 4.35 A Research Question Naturally Arises Q y Do these types of metrics provide the “right” right answer to • Researchers? • Quality improvement teams? • Patients P ti t • Payors? • Policymakers? Pragmatic Decision: Focus on Falls Why focus on falls? y Cli Clinical and policy case i l d li Common Lethal L th l Expensive Major national priority Research case High‐quality data available to allow hybrid methods approach High q alit data a ailable to allo h brid methods approach We’re going to talk about three things. three things Three things g Build an existence proof with a thought experiment B ild i t f ith th ght i t 2. Use empirical data to get plausible estimates of 1. How much fall risk varies across the exposure window (LOS)? How much the exposure window (LOS) varies ( ) Among hospitals Within one hospital over time 3. Use simulation studies to determine how much completely artifactural error these variation cause in the exposure‐time metric (falls per 1,000 patient‐ days). ) Step 1: Thought Experiment The Case of Arbitrary Regional General Hospital ARGH QI: 2010 Q ARGH decides to work on improving falls. ARGH d id t k i i g f ll They contract with their insurer to improve falls. If they succeed, insurer agrees to pay for one extra day of LOS. They want to use Teflon©‐coated floors. Management agrees: “It’s not the fall, it’s the friction!” ARGH QI: 2010 Q Admit 100 patients per year. Ad it ti t Risk of falling: HD#1: HD#2: HD#3: HD#4: HD#5: 5% 0% 0% 0% 0% ARGH QI: 2011 Q IImplementation l t ti Takes a whole year It’s hard to install Teflon®! That stuff is slippery. It’ h d t i t ll T fl ®! Th t t ff i li ARGH QI: 2012 (Evaluation Year) Q ( ) Admit 100 patients per year (unchanged) Ad it ti t ( h g d) Median LOS increases to from 2 to 3 days. Risk of falling: Post HD#1: 8% (increased by y 4060%) 35 30 HD#2: 0% 25 20 0 HD#3: 0% 15 10 HD#4: 0% 5 0 HD#5: 0% 1 2 1 2 3 4 5 50 45 40 35 30 25 20 15 10 5 0 Number o of Paitents Number o of Paitents Pre Length of Stay (days) 3 4 Length of Stay (days) 5 What does ARGH conclude? Admissions and Length of Stay Number of admissions Median Length of Stay (days) 2009 (baseline) 2011 (post‐intervention) 100 100 2 3 Truth: Teflon® flooring results in a 45 5 40 10 60% increase in falls. in falls 10 35 g g Patients with a given length of stay One day y Two days Three days Four days y Five days 4 1 30 20 Conclusion: Falls and Fall Risk Teflon® flooring results in a Risk of Falling p y 5% 8% Hospital Day #1 20% reduction in falls in falls. Hospital Day #2 0% 0% Patient‐days Hospital Day #3 Hospital Day #4 176 350 0% 0% 0% 0% How could ARGH have made H ld ARGH h d such a catastrophic error? p Step 2: Empirical data Real‐world variation in fall risk f across the exposure window Results: Inpatient Fall Distribution p Dates evaluated Patients Patient‐days Falls Falls per 1 000 patient days Falls per 1,000 patient days Result 2005 ‐ 2008 121,865 583,786 1,513 26 2.6 Challenge g W We have very few VERY long stay patients. h f VERY l g t ti t Median LOS: 3 days 95% of patients with LOS ≤ 14 days 9 % f ti t ith LOS 1 d Therefore lots of noise as we get to long lengths of stay. Risk of Falling on a Given Hospital Day Dailyy Fall Risk 0.4% 0.3% 0 2% 0.2% 0.1% 0.0% Hospital Day Risk of Falling on a Given Hospital Day Dailyy Fall Risk 0.4% 0.3% 0 2% 0.2% 0.1% y = 0.0006ln(x) + 0.0018 r² = 0.6408 0.0% Hospital Day Real‐world variation in length of stay Methods: Data N National Inpatient Sample 2001 & 2006 ti l I ti t S l & 6 Largest all‐payor database of U.S. discharges Representative, stratified random probability sample R t ti t tifi d d b bilit l n ~ 8,000,000 records ~ 40 million discharges (weighted) n = 1,045 hospitals n = 1 045 hospitals Perce ent of U..S. Hosp pitals LOS variability among hospitals in one year LOS Variability 70% 59.5% 60% 50% 40% 27.0% 30% 20% 6.8% 10% 4.7% 0.9% 0.2% 0.1% 0.1% 0.1% 0.7% 0% 1 2 3 4 5 6 7 8 9 ≥ 10 Median Length of Stay (days) Length of Stay Histogram Among Hospitals with Median LOS of 4 days g y g g p y 50% 45% 40% 35% 30% 25% 20% 15% 10% 5% 0% Length of Stay (Days) Within‐Hospital Variations in Length of Stay Over Time 8 Length of Stay Varies in the Same Hospital g y p Median Length of Stay (Days) 7 6 5 Number of Hospitals Total n = 244 4 1 1 1 1 1 1 2 3 10 11 13 15 16 32 134 3 2 1 NIS 2001 NIS 2006 Conclusions: Empirical data Conclusions from empirical data p Daily fall risk varies by more than two‐fold across the LOS. D il f ll i k i b th t f ld th LOS LOS varies among hospitals in the same year. LOS varies within the same hospital over time. Step 3: Simulation Studies DOES THIS RESULT IN MEANINGFUL VARIATION IN THE “FALLS/1,000 PATIENT‐DAYS” MEASURE? Methods: Hybrid Approach with Real Data y pp Approach: A h Create experimental conditions where: We know the true underlying, time‐varying fall risk. We impose an identical time‐varying fall risk on every hospital. Use real data to provide fall risk distributions and LOS variability measures. Risk of Falling on a Given Hospital Day Daily Fall Risk 0.4% 0.3% 0.2% 0.1% 0.0% Hospital Day Yes Fall 0.0018 Fall Yess 0.9982 0 0022 0.0022 Fall? No Ye es Fall? No Fall 0.0053 0 9978 0.9978 N No Repeat x 800 million. Fall? 0.9947 No Fall HD#1 HD#2 HD#3 HD#365 In this experiment, every patient in every U.S. hospital is exposed to an id i l fall risk distribution. identical f ll i k di ib i Risk of Falling on a Given Hospital Day D Daily Fall Risk 0.4% 0.3% 0.2% 0.1% 0.0% Hospital Day What would these hospitals report? Misleading metric variation among hospitals at one point in time i i i Percen nt of U.S. Hospitaals Artifactual Variation in Falls per 1,000 Patient‐Days Patient Days 30% 25.0% 25% 20.5% 20.5% 20% 15% 9.9% 10% 8.2% 4.5% 5% 2.9% 0.4% 0.2% 0.1% 0.2% 0.4% 1.3% 0.5% 0.7% 1.7% 2.7% 0.4% 0% 1.5 1.7 1.9 2.1 2.3 2.5 2.7 Falls per 1,000 Patient‐Days 2.9 3.1 Is this meaningful? 4 Artifactual Variability ‐‐ California Hospitals How would this affect California? Falls p per 1,000 Patient Days Remember: all of these actually had the SAME fall risk distribution fall risk distribution. 3 2 1 1 3 5 7 9 11 13 15 17 19 21 23 25 27 29 31 33 35 37 39 41 43 45 47 49 51 53 55 57 59 61 63 65 67 69 71 73 75 77 79 81 83 85 Misleading metric variation in individual hospitals over time Within‐Hospital Artifactual Variation Over Time Nu umber off Hospitaals (of 24 44) 60 50 40 30 20 10 0 Percent change in "Falls Per 1,000 Patient Days" Percent change in "Falls Per 1 000 Patient Days" in the same hospital over a 5‐year period Conclusions Conclusions When true fall rates are held constant Wh t f ll t h ld t t… The “falls per 1,000 patient days” metric (exposure‐ time metric) will cause policymakers to mistakenly ) ll l k i k l believe that The “best” and “worst” performers in a single state may have rates that vary by more than 50%. 18% of hospitals in a given year have substantial variation from the average hospital 35% of hospitals 35 p improve or worsen over time by more than 30% p y 3 Next steps p Conduct hybrid empirical / simulation studies on C d t h b id i i l / i l ti t di exposure‐time metrics other than falls Test a potential solution to the errors introduced by the l l h d db h mathematical construction of this metric class Particular thanks to … Robert Wood Johnson Foundation R b t W d J h F d ti Collaborators Meghan Dierks, MD Long Ngo, PhD D. Paul Phillips, PhD (Dept of Mathematics, U. of Dallas) l hilli h ( f h i f ll ) All of the dry erase markers who gave their lives in pursuit of this work i f hi k Thank you. you