Cultural Competency Training and Performance Reports to Improve Diabetes
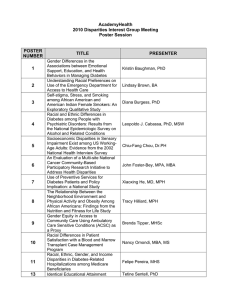
advertisement

Cultural Competency Training and Performance Reports to Improve Diabetes Care for Black Patients Thomas D. Sequist, MD MPH Garret M. Fitzmaurice, ScD Richard Marshall, MD Shimon Shaykevich, MS Amy Marston, BA Dana G. Safran, ScD John Z. Ayanian, MD MPP Harvard Vanguard Medical Associates Division of General Medicine, Brigham and Women’s Hospital Department of Health Care Policy, Harvard Medical School Funding Acknowledgement Finding Answers: Disparities Research for Change A National Program of the Robert Wood Johnson Foundation Background • Racial disparities in diabetes care – Persistence of disparities in outcomes • Role of primary care clinicians – Direct interaction with patient and system – Influence of patient race on clinical decisions – Limited physician awareness of racial disparities Study Question Can cultural competency training and performance feedback significantly impact: 1) Clinician awareness of racial disparities 2) Achievement of clinical control targets for black patients with diabetes Study Setting • Multispecialty group practice • Integrated electronic health record • Team-based primary care – 2 to 3 physicians – Nurse practitioner or physician assistant – NP/PA central role in organizing diabetes care Randomization Scheme 31 primary care teams 91 physicians 33 NP/PA 7,557 patients (≥ 18 years old) Intervention 15 primary care teams 46 physicians 16 NP/PA 3,784 patients Control 16 primary care teams 45 physicians 17 NP/PA 3,773 patients Intervention Components • Cultural competency training – 1 to 2 day course (89% team attendance) – Monthly educational materials • Clinical performance feedback – Monthly distribution – Race-stratified (HbA1c<7%, LDL < 100, BP < 130/80) – Provider level (benchmarked to practice) Patient Survey Feedback Sample Performance Report Study Outcomes • Clinician awareness of racial disparities – “How often do you feel quality of care varies by race?” • Across all health centers • Within local health center • Among patients personally treated • Achieving clinical control among black patients – HbA1c < 7% – LDL cholesterol < 100 mg/dL – BP < 130/80 mmHg • Assessed at baseline and 12 months Analytic Plan • Multivariable logistic regression • Clustering at level of primary care team • Adjusted for baseline clinician awareness or baseline clinical performance Baseline Patient Characteristics Intervention (n = 3,784) Control (n = 3,773) p value 62.5 62.3 0.24 Male, % 50 48 0.41 Insurance Commercial Medicare Medicaid Uninsured 58 35 4 3 57 36 5 3 0.66 Clinical targets, % HbA1c<7% LDL < 100 mg/dL BP < 130/80 mmHg 45 50 26 43 52 31 0.35 0.58 0.04 Mean age, years Baseline Racial Disparities White (n=4,858) Black (n=2,699) p value Process measures, % Annual HbA1c test Annual LDL test 87 83 89 83 0.14 0.99 Outcomes measures, % HbA1c < 7% LDL < 100 mg/dL BP < 130/80 mmHg 46 55 32 40 43 24 <0.001 <0.001 <0.001 Impact on Clinician Awareness % Very or Somewhat Often Do racial disparities in diabetes care exist in…. P=0.04 100 P=0.06 82 80 60 P=0.45 70 59 63 51 43 40 20 0 All health centers Your health center Intervention Your patients Control Clinician Support for Intervention How effective are these strategies to reduce racial disparities? % 'Very Effective' 50 P=0.01 40 P=0.02 34 33 30 20 17 11 10 0 Cultural Competency Training Intervention Performance Feedback Control Diabetes Care Among Black Patients Intervention, % HbA1c < 7% 49 LDL < 100 mg/dL 50 BP < 130/80 mmHg 23 Control, % 47 50 24 P value 0.36 0.68 0.73 Limitations • Advanced care setting – Electronic health record – Team based care • Only 50% of teams had both MD and NP/PA attend cultural competency training – NP/PA central role in diabetes care Conclusions • Intervention increased clinician awareness of disparities • Decreased clinician support for utility of intervention • No impact on clinical outcomes Implications • Increased clinician awareness may be necessary, but not sufficient to improve care for black patients • Additional research needed to understand how to facilitate behavior change for both providers and patients N ov -0 8 8 08 ar - 7 Ju l-0 M N ov -0 7 07 ar - 6 Ju l-0 M N ov -0 % Patients with Race/ Ethnicity Available Race Collection Progress 100 80 60 40 20 0 Clinical Data Feedback The “Not Me” Phenomenon: Primary Care % Very or Somewhat Often Do racial disparities in diabetes care exist in…. 100 90 80 70 60 50 40 30 20 10 0 US Health System HVMA Your health center Your patients Sequist et al; JGIM 2008