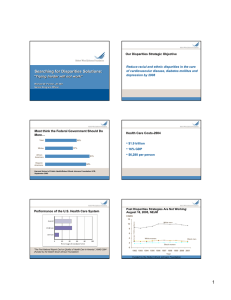
Changes in healthcare disparities following the implementation of a multifaceted quality improvement initiative
advertisement

Changes in healthcare disparities following the implementation of a multifaceted quality improvement initiative Muriel Jean-Jacques, MD, MAPP Stephen D. Persell, MD, MPH Romana Hasnain-Wynia, PhD Jason A. Thompson, BA David W. Baker, MD, MPH Northwestern University Feinberg School of Medicine Division of General Internal Medicine Funding Source: AHRQ Introduction Health information technology (HIT) based interventions have been shown to improve the quality of care. The effects of HIT-based interventions on health equity have been less well studied. Quality and Equity Studies have not found a consistent association between higher quality and greater equity. Most studies of quality and equity have focused on racial and ethnic health disparities; however disparities by gender, health insurance, and socioeconomic status have been similarly pervasive. Study Aim To assess the effects of a multifaceted HIT based quality improvement initiative on disparities in the quality of ambulatory care Examine disparities by race, gender, and socioeconomic status Assess quality through adherence to process of care and intermediate outcome measures Study Setting Academic GIM practice in Chicago 37 attendings: 25,000 patients annually Electronic health record system since 2002 Quarterly feedback to MDs on quality since 2006 Intervention: UPQUAL Study Implemented February 1, 2008 Provider-directed components Point-of-care electronic alerts Standardized reporting of medical or patient exceptions Regular feedback on performance Patient-directed components Outreach to patients who reported financial barriers Educational outreach to patients who declined recommended tests or therapies Quality Measures Coronary Heart Disease • • • • Antiplatelet therapy Lipid lowering therapy Beta-blocker therapy ACE inhibitor or ARB Heart Failure • • • ACE inhibitor or ARB Beta-blocker therapy Anticoagulation for Afib Hypertension • BP control Diabetes Mellitus • • • • • Glycemic control (A1C<8) LDL control (LDL<100) BP control ASA for primary prevention Nephropathy screening or Rx Prevention • • • • • Cervical cancer screening Breast cancer screening Colorectal cancer Screening Pneumococcal vaccination Osteoporosis screening or Rx Data Source and Subjects Data extracted from electronic health record Patient characteristics Quality deficiency: measure not satisfied and no exception documented 10,599 patients Eligible for at least 1 quality measure ≥ 2 visits within 18 months of baseline or follow-up assessments Black or white race Sample size by measure ranged from 102 to 6,322 Statistical Methods Multivariate logistic regression model for each measure: Dependent variable: quality deficiency Main independent variables: Race: recorded by registration staff Gender SES: from geocoding % families below federal poverty level in census block group % high school graduates in census block group Other covariates: age, insurance Statistical Methods Ran logistic regression models using baseline vs. follow-up data Baseline – January 1, 2008 Follow-up – January 1, 2009 Post-model estimation of the adjusted % of patients by group with quality deficiencies for each measure Calculation of adjusted difference in quality by group Results: Racial Disparities There were racial disparities for 4 of 18 measures at baseline Worse QOC for black patients Better QOC for black patients Adjusted Difference (%) 15 11.2 10 7.5 5.5 5 0 0 0 thy HD a C rop -5 let in h ep te N a l tip DM n -7.8 A 0 A M nD i <8 C 1 teo s O -10 Baseline Follow-up 0 ros o p is Results: Racial Disparities At follow-up, disparities were no longer statistically significant for 2 of 4 measures Worse QOC for black patients Better QOC for black patients Adjusted Difference (%) 15 11.2 10 7.5 5.5 5 6.1 * 1.2 0 8 * thy HD DM a C p n -2.7 i -5 let in hro <8 p C e e t N A1 pla M i t D -7.8 An teo s O -10 Baseline Follow-up ros o p is Results: Gender Disparities There were gender disparities for 7 of 15 measures at baseline 9.1 Worse QOC for women Better QOC for women Adjusted Difference (%) 10 8.1 7.4 5.6 5 2 0 0 0 0 0 0 thy HD DM DM DM a C p n n n ro Li 8i Ai h r in < D S p e L A 1C ck Ne A o l DM B-b id Lip -5 0 Rx -5.9 -10 Baseline Follow-up 0 C CR -3.1 Results: Gender Disparities At follow-up, gender disparities were no longer significant for 4 of 7 measures Worse QOC for women Better QOC for women Adjusted Difference (%) 10 9.1 8.1 7.4 5 * 2 2.3 2.9 * 0.7 * 3.7 5.6 * 1.7 0 thy HD RC DM DM DM a C C p n n n i i i o r r in -3.1 3.3 <8 -3.1 DL SA ph -3.3 e L C A e k 1 c N A lo M b -4.9 D B id Lip -5 Rx -5.9 -10 Baseline Follow-up Results: Disparities by SES Worse QOC for patients from poor areas Adjusted Difference (%) There were disparities by neighborhood level poverty for 2 of 18 measures at baseline 14 12.1 12 10 8 6 * 4 2.7 5.2 3.6 2 0 oc -bl ke HF n i r CS R C B Baseline * ing n e cre Follow-up Results: Disparities by SES There were disparities by neighborhood level education for 2 of 18 measures at baseline Better QOC for patients from areas with low education 15 8.9 10 Adjusted Difference (%) Worse QOC for patients from areas with low education 6.1 5 0 -5 -10 -15 -20 oc -bl ke HF n ri B -14.3 teo s O ros po * -25 -30 -35 -40 -33.2 Baseline Follow-up is New Racial Disparities New disparities were apparent by race for 4 measures at follow-up 6 3.3 4 1.7 2 0.8 er ap y -7 n -3.6 oc ca l -5.9 eu m oc th AR B AC E or -8 -3.8 Pn -6 va cc in at io in C Pa p y m og -4 ra ph -2 HD 0 am Better QOC for black patients 7.4 8 M Worse QOC for black patients Adjusted Difference (%) 10 Baseline Follow-up Other New Disparities New disparities were apparent for 1 measure by education and 1 measure by gender at follow-up Education Gender Better QOC for women and patients with lower education Adjusted Difference (%) 0 -1 BP control in DM ACE or ARB therapy in HF -2 -3 -3 -4 -5 -6 -7 -6.6 -8 -9 -8.2 -7.8 Conclusions A generalized HIT-based QI initiative was associated with significant improvements in disparities by race, gender, and SES for some but not all measures with baseline disparities. No clear patterns emerged between the type of measure and changes in disparities. Strengths and Limitations Strengths Assessment of quality of care for several chronic diseases and types of preventive care Disparities assessed by race, gender, SES Models adjusted for important covariates including SES Limitations Single institution study Race data not by selfreport Many patients excluded due to missing race Limited power to detect differences for some measures Implications In evaluating QI efforts, it is important to continuously monitor for health disparities to identify areas where more targeted interventions are needed: Measures with persistent disparities Measures with new disparities