CER vs CEA – A decision analytic perspective
advertisement

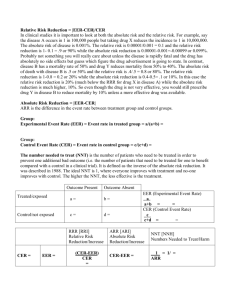
CER vs CEA – A decision analytic perspective How much difference should one letter make? R. Scott Braithwaite, MD, MSc, FACP Before Sept ‘09: Associate Professor of Medicine Yale University School of Medicine After Sept ‘09: Chief; Section of Comparative Effectiveness, Quality, and Value NYU School of Medicine CER vs CEA Some view cost-effectiveness research (CEA) as one type of comparative effectiveness research (CER) Allied tools for getting better performance from our health care system Others view CEA as distinct from CER “Comparative effectiveness” does not have “cost” in it Lighting rod for fears about rationing Argument The whole motivation for CER is to better inform decisions Therefore CER design and questions are informed by decision analytic perspective Decision Analysis: Quantitative, systematic, objective way to put harms and benefits on level playing field Questions: How much information will the study add? Is this information useful for decision making? Decision-analytic perspective: CER Many implications, of which cost is only one: Prioritizing what to study Design decisions Comparators Health outcomes Statistical criteria for hypothesis testing Strength of evidence thresholds for applying results Cost as possible outcome Measure cost? Perform CEA? Roadmap of talk Overview of CER How decision-analytic perspective would impact CER methods in general How decision-analytic perspective would impact CER methods regarding cost Question: Should CER and CEA be completely separate, completely overlapping, or somewhere in the middle? CER-Definition (Institute of Medicine) The generation and synthesis of evidence that compares the effectiveness of alternative methods to prevent, diagnose, treat, monitor, and improve delivery of care for a clinical condition. The purpose of CER is to assist patients, clinicians, purchasers, and policy makers in making informed health decisions. CER – Some Examples For a patient who has severe coronary artery disease and must choose between surgery and a less invasive procedure, what is best? Is the answer the same if patient recently had heart attack? Should men be screened for prostate cancer with the PSA blood test? Is the answer the same if sick from other conditions? How to choose the best high-blood-pressure drug? Is the answer the same for patients who are at high risk for heart attacks and strokes? CER-Study Designs All compatible with cost-estimation or lack thereof RCT Meta-analysis and systematic review Observational analyses Registries Administrative data and EMR Prospectively enrolled cohorts Indirect comparisons Bayesian approaches Mathematical modeling and computer simulations Roadmap of talk Overview of CER How decision-analytic perspective would impact CER methods in general How decision-analytic perspective would impact CER methods regarding cost Question: Should CER and CEA be completely separate, completely overlapping, or somewhere in the middle? What to study first? Preferentially study questions for which additional data or analysis is likely to influence the decision Confers highest value of information (Claxton et al, 1986) Monetarized value of improvements in health outcomes resulting from the better decision-making that is made possible by the study Focus on healthcare services In common practice Large aggregate expenditures Employ rapidly changing technologies for which multiple alternative therapies exist for the same problem Clinical, preventive or treatment areas with substantial uncertainty about what is the best decision Large penalty for making the wrong choice Which comparators to use? One comparator should be the current standard of care or usual care Comparators should include next best alternative e.g. COX-2 inhibitors (marketed for reduced GI side effects) should have been more often compared against dual-therapy with older NSAID + PPI (GI protective drug) Comparators might include systems of care as well as specific interventions e.g. P4P, patient-centered medical home, VBID Which health outcomes to use? Should be able to balance harms against benefits Note: harms may be unanticipated and therefore not reflected in disease- specific outcome measures specified a priori e.g. If you are studying an analgesic and primary outcome measure is pain you may not measure nausea that might offset the benefit of pain improvement Should include quality-of-life measure that is Generic (not disease-specific) Preference-weighted (more reflective of decision making) Gives results on a unidimensional, interval scale Allows explicit weighting of harms and benefits Limited group of instruments satisfy these criteria E.g., EQ-5D, HUI, QWB, SF-6D Disease-specific instruments are sometimes calibrated against these What statistical criterion to use for hypothesis testing? It is customary to mandate greater than a 19-in-20 chance that an improvement is “real” rather than a statistical fluke p-value < 0.05 This might be too strict of a standard when treatments are compared against other treatments rather than placebo May not maximize benefits and minimize harms, particularly if treatment is known to have a favorable toxicity profile from prior study. More research is needed to elucidate if and when less strict statistical criteria are appropriate Should p < 0.10 ever be the criterion? How about others? Vary with budget constraints for gathering additional evidence? What threshold of evidence to require for decision making? It is difficult to specify a priori what threshold of evidence is sufficient to influence a decision Will be based on how certitude of evidence compares with the certitude of the decision maker’s beliefs If decision maker has certitude of belief >> certitude of evidence, then his post-test distr ≈ pre-test distrib Evidence will have little influence on his decision E.g. World-expert reading a single institution case control study If the decision maker has certitude of belief << certitude of evidence, then his post-test distr ≠ pre-test distr Evidence should influence the decision greatly. E.g. world-expert reading 12 RCTs reaching consistent conclusions What threshold of evidence to require for decision making? CER should express strength of evidence using a simple, unidimensional, and transparent scale e.g., United States Preventive Services Task Force Strength of evidence grades: A, B, C, I Separate grades for “this study alone” and “this study added to existing literature” Would facilitate use of CER decision making Uncertain decisions with high evidence thresholds will often have high value of information, and are especially ripe for future study. Roadmap of talk Overview of CER How decision-analytic perspective would impact CER methods in general How decision-analytic perspective would impact CER methods regarding cost Question: Should CER and CEA be completely separate, completely overlapping, or somewhere in the middle? Should CER measure costs? CER is strengthened if it includes measures of costs Essential for estimating value and informing resource allocation Cost measures should Include assessments from societal perspective Not only expenses that accrue to any one party (e.g. the pharmacy, the health plan), but also costs that accrue throughout the system, including to the patient/family Encompass longest feasible time horizon May discount these costs as appropriate (e.g. 3%) Reflect the opportunity cost of resource allocation rather than charges CER more useful if costs measured P4P design Value-based insurance design (VBID) Clinical trial design Informing reimbursement schedules Estimating return on investment (ROI) CER more useful if costs measured Influencing P4P design How large should be the monetary incentives should we give to the highest-quality providers and health systems? Can we pay clinicians and health plans for improving health (e.g., coordinating care), not just for doing procedures and tests? Suppose Plan A has 80% compliance and Plan B has 60% compliance with an evidence-based colorectal cancer screening program. Because colorectal cancer screening confers 0.25 additional high-quality life-years, on average plan A delivers 0.05 more high-quality life-years than Plan B. Therefore, the value of this quality improvement is worth ≥$5,000, assuming a value of health benefits of $100,000 per high-quality life-year. CER more useful if costs measured Value-based insurance design (VBID) When should patients have copayments waived because its value is so favorable? When should patients have copayments increased because its value is so unfavorable? Should patients receive a “health dividend” for healthy behaviors that save money for the healthcare system, such as preventing kidney failure in diabetics? Designing clinical trials Ensuring we can detect improvements sufficiently large to offer favorable value CER more useful if costs measured Influencing reimbursements How much is a particular treatment “worth,” based on the amount of benefit that it gives? How can we make sure that patients and health plans do not pay more than this worth? If a health service is delivers 0.1 high quality lifeyears as a benefit, the maximum reimbursement for that service would be $10,000 assuming a value of health benefits of $100,000 per high-quality life-year CER more useful if costs measured Estimating return-on-investment (ROI) Inappropriate to include only financial consequences in an ROI calculation . Health benefits should be monetarized (e.g., an intervention that delivers 1 high-quality year of additional life delivers at least $100,000 worth of health benefits) and included in ROI calculations. Imperative to consider health benefits when estimating ROI else calculations just reduce to budgetary-impact calculations, which ignore the benefit of investing in health. Roadmap of talk Overview of CER How decision-analytic perspective would impact CER methods in general How decision-analytic perspective would impact CER methods regarding cost Question: Should CER and CEA be completely separate, completely overlapping, or somewhere in the middle? Should CER involve CEA? Not necessarily But it should provide all important inputs for future CEA Outcome measures (quality-of-life, etc) Costs (perspective, etc) CEA using CER data could be funded using alternative mechanisms What to use as a threshold for acceptable value? Value thresholds are subject to intense debate, and vary from time to time and from society to society. That being said, it may be possible to make inferences regarding plausible bounds For example, the appropriate value threshold in the US is likely to be between $100,000 and $300,000 (Braithwaite et al, 2008) Conclusions: CER vs CEA CER will have limited use if costs aren’t measured “Menu without prices” (Garber et al, 2007) It is unclear whether CER should encompass CEA But should measure all important CEA inputs so it can facilitate CEAs CER should measure all outcomes necessary for good decisions Health outcomes Costs