Primary Care
advertisement
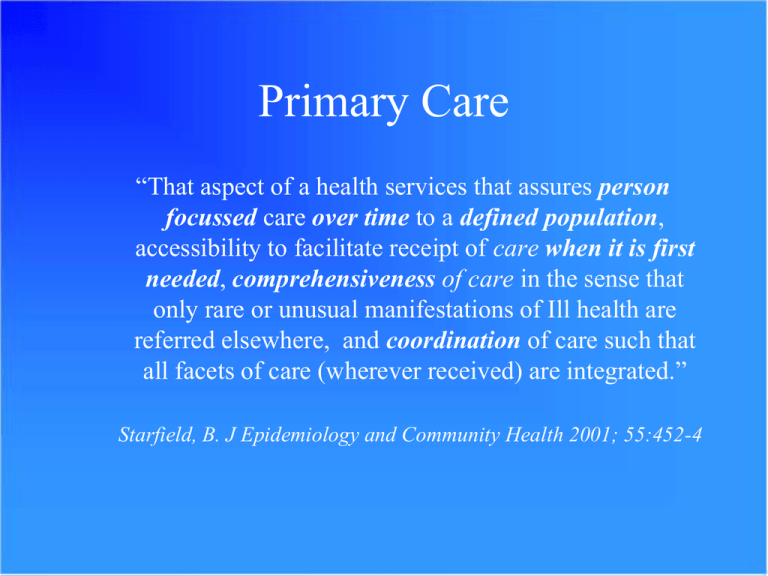
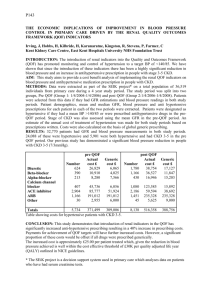
Primary Care “That aspect of a health services that assures person focussed care over time to a defined population, accessibility to facilitate receipt of care when it is first needed, comprehensiveness of care in the sense that only rare or unusual manifestations of Ill health are referred elsewhere, and coordination of care such that all facets of care (wherever received) are integrated.” Starfield, B. J Epidemiology and Community Health 2001; 55:452-4 General Practice in England • In 2002 the Audit Commission published A Focus on General Practice in England. They reported; “General practice is an important service, accounting for eight out of ten patient contacts with the NHS, but only one-fifth of NHS spending (£8.3 billion). Most people see the GP as the first port of call when they are feeling unwell and 99 per cent of the population are registered with a GP, usually close to where they live. General practice is highly rated by the public and evidence shows some overall improvement in quality.” • The c.8,500 practices in England deliver 314m consultations each year (Healthcare Commission “State of the Nation” Report 2006). This represents an average 6 per year for each person or 720 weekly by each practice. • There were 30,358 GPs in September 2003, and 33,091 in September 2006. QOF The Quality and Outcomes Framework was the first example of its kind in the world, introducing a dramatically more systematic focus on evidence-based care. 95 100 75 79 72 58 50 41 43 30 25 0 AUS CAN GER NETH NZ GPs are ahead of family doctors in comparator countries in uptake of financial incentives for quality, IT use and chronic disease management UK US Percent receive financial incentive: AUS CAN GER NETH NZ UK US Achieving certain clinical care targets 33 10 9 6 43 92 23 High ratings for patient satisfaction 5 — 5 1 2 52 20 Managing patients with chronic disease/ complex needs 62 37 24 47 68 79 8 Enhanced preventive care activities 53 13 28 18 42 72 12 Participating in quality improvement activities 35 7 21 28 47 82 19 Source: 2006 Commonwealth Fund International Health Policy Survey of Primary Care Physicians. Recent research has shown that care for some chronic conditions improved more rapidly when QOF was introduced, although subsequent gains have been more difficult •The rate at which quality was improving increased for asthma and diabetes immediately following the introduction of the scheme •The rate of improvement continued for coronary heart disease at the same rate as before the scheme •In subsequent years, the rate of quality improvement appears to have slowed down •QOF needs to be continually reviewed in order to support optimum health outcomes for patients Source: Campbell SM et al; National Primary Care Research and Development Centre However, there have been criticisms of early QOF that its clinical indicator set didn’t correlate well with possible population health gains • QOF indicators are not optimally aligned with interventions and activities that will have the maximum impact on population health • Cookson et al* correlated evidence on the population health gains from cardiac prescribing interventions with the relevant QOF payments • Plotted points associated with these interventions against likely lives saved p.a. per 100,000, with a relatively poor fit. Source: Fleetcroft, R. and Cookson,, R. (2005) Do the incentive payments in the new NHS contract for primary care reflect likely population health gains? Journal of Health Care Research and Policy The incentives in the Quality and Outcomes Framework for evidence based quality care are predominantly focused on diagnosis, management and secondary prevention of long term conditions. Everyday activity Some primary prevention activity clearly takes place in GP practices, but there is no systematic framework for ensuring that people who need it have access to it or for measuring quality. Preventio n points Only 7.5% of the QOF is dedicated to health promotion/illness prevention, covering: • registers for obesity and learning disability • recording blood pressure and smoking status • having a stop smoking strategy. • for 2009/10: CVD primary prevention and sexual health QOF 2009/10 Mostly disease manageme nt Primary prevention Disease management Organisational Patient Experience 8 Proposed scope and frequency of review ‘flu indicators Advice from JCVI Indicators out of scope Indicators within scope Organisational indicators RCGP practice accreditation Patient experience indicators Disease management and secondary prevention (excluding flu indicators) GP patient survey Primary prevention and health inequalities Frequency of output for indicators managed by NICE: •to review all 88 indicators in 3-4 years (20-30 per year) •cost effectiveness evidence for an additional 10 indicators per year Local flexibility Rationale for local indicators There may be a high prevalence of certain diseases within a PCT that is not representative of the general population - eg HIV in Southwark, London Current barriers to uptake •need for technical expertise in the development of evidence based indicators; •IM&T support required to extract data from clinical systems and to link this with payment calculations. •no national decisions to set aside part of the £1 billion national investment in QOF for local investment. Menu of QOF indicators Solution QOF indicators ______ ______ ______ ______ ______ ______ % for national use % for local use NHS Employers consult GPC The NHS and Social Care Long Term Conditions Model Better outcomes Community Resources Case Management Empowered and informed patients Decision support tools and clinical information system (NPfIT) Health and social system environment Disease Management Supported Self care Promoting Better Health Creating Delivery System Supporting Infrastructure Prepared and proactive health and social care teams CQUIN • The Commissioning for Quality & Innovation (CQUIN) scheme has been introduced to ensure organisations pay a higher regard to quality by making a proportion of a provider’s income conditional on quality and innovation. Commissioners will agree with their providers, the areas of service to be subject to a CQUIN scheme. • For the current year 2009/10, commissioners have the option of implementing a full CQUIN scheme with their community providers or a more limited scheme linking payment to an agreed quality improvement plan. The latter recognised the importance of establishing a good baseline for monitoring quality. • A full CQUIN scheme will be mandatory for all community providers from April 2011. NHS Next Stage Review (Darzi) Final Report Personal Health Budgets • The pilots will test a range of models of personal health budgets: this is not necessarily about a direct cash payment (although we are bringing forward primary legislation so we can test that), but could include people simply being aware of the choices available to them within a notional budget or through a budget held by a third party. • Personal health budgets will not be suitable for all types of care or for all patients, but they have the potential to be one of the levers that drives the much wider cultural change we are aiming for.