Regionalization in Local Public Health: Variation in Rationale, Implementation, and Impact
advertisement
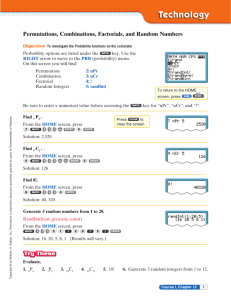
Regionalization in Local Public Health: Variation in Rationale, Implementation, and Impact on Public Health Preparedness Michael A. Stoto PHSR CyberSeminar, May 2007 Washington Metropolitan Area Definitions • National Capital Region (NCR) • Metropolitan Washington Council of Governments (COG) • Media market • Healthcare markets • Federal government Stoto PHSRCyberSeminar 2 5/07 NCR organization and governance • Who’s in charge? – “Let me speak to the health officer for the National Capital Region” • MWCOG Health Officers Committee (HOC) – Forum to communicate on a regular basis, but no legal authority • Senior Policy Group (SPG) and COG Chief Administrative Officers (CAO) committee – Receive and distribute federal funds Stoto PHSRCyberSeminar 3 5/07 Regional capacity in the NCR • ESSENCE II regional surveillance system • MWCOG – Conference call facility – Regional Incident Communication and Coordination System (RICCS) • DC Hospital Association emergency radio network (H-MARS) • VDH Northern Virginia Regional Team Stoto PHSRCyberSeminar 4 5/07 NCR conclusions • Regional capacity created • Numerous regional entities and relationships among public health and partners • Relationships tend to be informal – More formality may not be possible – May be optimal: personal relationships more important than formal arrangements in an emergency • “Who’s in charge” will remain an issue • Biggest challenge is role of the federal government Stoto PHSRCyberSeminar 5 5/07 Cross-cutting issues: Impetus for regionalization • Efficient use of preparedness funds – MA, others to lesser degree • Crisis or perceived need for a coordinated response – MA 4b, NCR, others to lesser degree • Building local public health capacity – Strengthening existing local public health structures (No. IL) – Building local public health itself (NE) Stoto PHSRCyberSeminar 6 5/07 Formal organizational relationships vs. informal professional networks • NACCHO Public Health Ready typology – Coordination Standardization – Centralization Networking • Describes collaboration of existing LHDs – Not as effective for building local public health capacity (e.g. MA, NE) • Does organization build social capital? • Or, are the professional networks built through regionalization the most important effect? Stoto PHSRCyberSeminar 7 5/07 Relationship between public health regions and geopolitical jurisdictions • Variety of combinations – Combinations of local LHDs (No. IL, MA) – Combinations of counties (NE) – NCR: multiple definitions, cross-state, sub-regions • Congruence with – Regional structures for partner agencies (e.g. EMA) – Hospital markets, HRSA funding regions, etc. – Need to preserve existing relationships if possible • Impact on political support and social capital? – Authority and resources for public health follow jurisdictional lines, but outbreaks don’t Stoto PHSRCyberSeminar 8 5/07 Leadership, trust and sustainability • MA 4b started with a small group formed in a crisis and grew from 15 to 27 communities with state funding – Cambridge (fiscal agent) had to ensure it was not perceived as “driving” • Competition for UASI funds in NCR • Can the perceived need for regional response overcome home rule barriers? – Need perception that at the end of the day it will be worth it • Do regions build social capital? – Does this help with sustainability? Stoto PHSRCyberSeminar 9 5/07 Does regionalization improve preparedness? • May depend on setting, existing resources, and variety of regionalization • Logically, yes – More efficient use of resources – Outbreaks don’t respect geopolitical boundaries, so need coordination • Demonstrated progress in – Planning and coordination – Memoranda of Understanding, etc. – Development of local and regional capacity, training, exercises – Professional network development • Response to – Flu vaccine shortage (MA) – Anthrax and tularemia alarms (NCR) Stoto PHSRCyberSeminar 10 5/07 Does regionalization improve public health generally? • Same efficiency, communication needs • Regional capacities address other needs – Regional epidemiology in NCR • Preparedness concerns are forcing us to think about public health structures in a way not done in decades – Communities think about preparedness in terms of day-to-day activities • Network development may be creating social capital that helps with other concerns • But, do preparedness demands draw resources and attention from other areas? Stoto PHSRCyberSeminar 11 5/07 Acknowledgements RWJ HCFO Public Health Systems Initiative MA: Howard Koh, Christine Judge MA 4b: John Grieb, Mary Clark No. IL: Patrick Lenihan NE: Dave Palm, Colleen Svoboda NCR: Lindsey Morse Contact Information stotom@georgetown.edu (202) 687-3292