Understanding Changes in Local Public Health Spending
advertisement

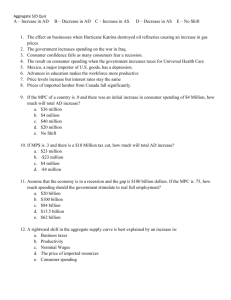
Understanding Changes in Local Public Health Spending Glen Mays, PhD, MPH Department of Health Policy and Management University of Arkansas for Medical Sciences Longitudinal change in spending and mortality •Half of all gains attributable to medical spending •$36,300 per year of life gained •What can we say about public health spending? Cutler et al. NEJM 2006 Geographic variation in spending and mortality Medical spending varies by a factor of more than 2 across local areas Medicare enrollees in highspending regions receive more care but do not experience lower mortality What can we say about public health spending? Fisher et al. Annals 2003 Some research questions of interest… How does public health spending vary across communities and change over time? Are changes in spending associated with changes in population health outcomes? What is the value of public health spending? 15% Variation in Local Public Health Spending 0 Fraction of Agencies 5% 10% Gini = 0.472 $0 $50 $100 $150 Expenditures per capita, 2005 $200 10% 5% 65% 35% 0 Fraction of Agencies 15% Change in Local Public Health Spending, 1993-2005 –$50 –$40 –$30 –$20 –$10 $0 $10 $20 $30 $40 $50 Change in Per Capita Spending (Current Dollars) The problem with public health spending Federal & state funding sources often targeted to communities based in part on disease burden, risk, need Local funding sources often dependent on local economic conditions that may also influence health Public health spending may be correlated with other resources that influence health Sources of Local Public Health Agency Revenue, 2005 Fees 6% Medicare 2% Other 12% Local 28% Medicaid 9% Federal direct 7% Federal pass-thru 13% State direct 23% NACCHO 2005 Example: cross-sectional association between PH spending and mortality 120 205 200 100 195 80 190 60 185 180 40 175 20 170 0 165 Quintile 1 Quintile 2 Quintile 3 Quintile 4 Quintile 5 Quintile of public health spending/capita Deaths per 100,000 Public health spending/capita Public health spending/capita Heart disease mortality Example: cross-sectional association between PH spending and Medicare spending 7200 Public health spending/capita 100 7000 Medicare spending per recipient 6800 80 6600 60 6400 40 6200 20 6000 0 5800 Quintile 1 Quintile 2 Quintile 3 Quintile 4 Quintile 5 Quintiles of public health spending/capita Medical spending/person ($) . Public health spending/capita ($) . 120 Addressing the problem with spending _ Unmeasured economic distress + Mortality PH spending + Approaches Unmeasured disease burden, risk + 1. Cross-sectional regression: control for observable confounders 2. Fixed effects: also control for time-invariant, unmeasured differences between communities 3. IV: use exogenous sources of variation in spending 4. Discriminate between causes of death amenable vs. nonamendable to PH intervention Data used in empirical work Financial and institutional data collected on the national population of local public health agencies (N≈3000) in 1993, 1997, and 2005 Residual state spending estimates from US Census of Governments Residual federal spending estimates from Consolidated Federal Funding Report Community characteristics obtained from Census and Area Resource File (ARF) Analytical approach Dependent variables – Age-adjusted mortality rates, conditions sensitive to public health interventions (infant mortality, heart disease, cancer, diabetes, influenza) – Counterfactual mortality rates (alzheimer’s, unintentional injuries) Independent variables of interest – Local spending per capita, all sources – Residual state spending per capita (funds not passed thru to local agencies) – Direct federal spending per capita Analytical approach: IV estimation Identify exogenous sources of variation in spending, unrelated to outcomes – Governance structures: local boards of health – Centralized state-local PH administration Controls for unmeasured factors that jointly influence spending and outcomes Governance Unmeasured economic distress Mortality PH spending Unmeasured disease burden, risk Analytical approach Other Variables Used in the Models Agency characteristics: type of government jurisdiction, scope of services offered, governance, state-local administration Community characteristics: population size, rural-urban, poverty, education, age distributions, physicians per capita, CHC funding per low income State characteristics: Private insurance coverage, Medicaid coverage, state fixed effects Factors associated with local public health spending Variable Coefficient 95% CI Local board of health (1=Yes) 0.145** (0.099, 0.196) Centralized structure (1=Yes) -0.234** (-0.364, -0.102) Population size (log) -0.136*** (-0.168, -0.103) Income per capita (log) 0.196** (0.001, 0.392) Local tax burden (% of income) 0.234** (0.032, 0.436) **p<0.05 ***p<0.01 Hierarchical logistic regression estimates controlling for community-level and state-level characteristics Multivariate estimates of association between spending and mortality Cross-sectional model Outcome Elasticity St. Err. IV model Elasticity St. Err. Elasticity St. Err. 0.0234 0.0192 -0.6854 0.2668 *** Infant mortality 0.0516 Heart disease -0.0003 0.0051 -0.0103 0.0040 ** -0.3216 0.1600 ** Diabetes 0.0323 0.0187 -0.0487 0.0174 *** -0.1439 0.0605 ** Cancer 0.0048 0.0029 * -0.0075 0.0240 -0.1131 0.0566 ** -0.0400 0.0200 ** -0.0275 0.0107 ** -0.0252 0.0362 Influenza 0.0181 ** Fixed-effects model Alzheimer’s 0.0024 0.0075 0.0032 0.0047 0.0051 0.0472 Injury 0.0007 0.0083 0.0004 0.0031 0.0013 0.0086 *p<0.10 **p<0.05 ***p<0.01 Conclusions Local public health spending varies widely across communities Governance and administrative structures appear influential in spending decisions – Local governing boards – Decentralized administrative structures Growth in spending is associated with reductions in mortality from leading preventable causes of death Limitations Aggregate spending measures – Average effects – Role of allocation decisions? Mortality – distal measures with long incubation periods Confounding—unmeasured factors tightly correlated with public health spending?