Acknowledgements The Relationship Between CMS Quality Indicators and Long -
advertisement

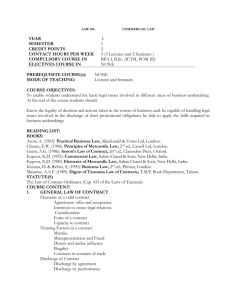
Acknowledgements Q Duke Clinical Research Institute (DCRI) O Lesley Curtis, Ph.D. O Adrian Hernandez, M.D. O Bradley Hammill, Hammill, M.S. O Kevin Schulman, M.D. O Eric Peterson, M.D. Q UCLA Medical Center O Gregg Fonarow, M.D. Q Funding Sources O Contract with GlaxoSmithKline O Duke CERTs grant (AHRQ grant #U18HS10548) The Relationship Between CMS Quality Indicators and LongLong-term Outcomes Among Hospitalized Heart Failure Patients Mark Patterson, Ph.D., M.P.H. PostPost-doctoral Fellow Duke Clinical Research Institute (DCRI) PayPay-forfor-Performance and Process Measures Q Q Q CMS Heart Failure Process Measures Goal of PayPay-forfor-Performance: Encourage providers to follow recommended clinical care by providing financial incentives Improving heart failure care remains a priority for CMS O Prevalence = 5 million; Cost = $30 billion Q 4 Core Process Measures O Providing discharge instructions O Conducting left ventricular ejection fraction (LVEF) assessment O Prescribing ACE inhibitors or angiotensin receptor blockers at discharge O Providing smoking cessation counseling Theory: Financial incentives Æ improve providers’ providers’ adherence Æ improve clinical outcomes Process Measures: Estimate providerprovider-level adherence to this recommended clinical care Associations between process measures (PM) and mortality Q Q Objective Mixed evidence in regards to the associations between process measures and mortality O Acute coronary syndrome1 O AMI2 O Heart failure3 Q Measure associations between the 4 current CMS heartheart-failure process measures and 11-year mortality O Q No evidence in regards to associations between PM and longlong-term mortality 1: Peterson et al., JAMA, 2006 2. Bradley et al., JAMA, 2006 3. Fonarow et al., JAMA, 2007 1 H1: HospitalHospital-level process measures will be associated with patientpatient-level mortality Data Sources Q Retrospective cohort study Q Matched HF patients within the OPTIMIZE registry with their Medicare Part A claims (2003 – 2004 O OPTIMIZEOPTIMIZE-HF O Medicare Part A O CMS denominator files Q Participants Q Medicare feefee-forfor-service HF patients matched to the OPTIMIZEOPTIMIZE-HF registry (N=22,483) Q Excluding patients who died before discharge Q Excluding hospitals with O missing process measures O with less than 25 patients Q Final analytic dataset (N=22,451) Matched on age, gender, discharge date, and hospital HospitalHospital-level single process measures (PM) HospitalHospital-level combined process measures Q Q Discharge instructions N=15,142 (67%) Q LVEF assessment N=20,061 (89%) Q ACEI or ARBs at discharge N=5,457 (24%) Q Smoking cessation at discharge N=902 (4%) Total number of processes documented -----------------------------------------------------------Total number of opportunities to perform Q Outcome and Control Variables PatientPatient-level Mortality O CMS denominator file Q PatientPatient-level controls O Demographics O Comorbities O Clinical measures Creatinine, Creatinine, weight, blood pressure Q DefectDefect-free N=22,451 Proportion of patients within the hospital having documentation for ALL the PM that they were eligible to receive Frequency of PM documentation ------------------------------------------------------------Number of patients eligible to receive PM Q Composite N=22,451 Statistical Analysis HospitalHospital-level volume O Total HF discharges O % HF discharges of total 2 Q Cox multivariate regressions O Controlling for demographics, clinical measures, selected coco-morbidities, and hospital volume indicators O Accounting for clustering of patients within hospitals Q 6 final models O 4 Models for each single PM O 2 Models for each combined PM Hospital PM Adherence Rates (N=178) Selected Baseline Characteristics (N=22,451) Variable Mean age (s.d (s.d)) Male White Black Other Prior AMI Prior PVD Prior Hyperlipidemia Mean Serum Creatinine (mg/dL (mg/dL)) (s.d (s.d)) Mean Systolic BP (mmHg) (s.d (s.d)) Mean Weight (kg) (s.d (s.d)) % 79 (7.8) 44% 84% 10% 6% 23% 15% 33% 1.6 (1.2) 142 (32) 77.4 (20.8) Process Measure (PM) Single Discharge Instructions LVEF Assessment ACEI / ARBs at Discharge Smoking Cessation Combined Composite DefectDefect-free Associations between hospitalhospital-level process measures and patient mortality LVEF Assessment ACEI / ARBs at Discharge Smoking Cessation Combined Composite DefectDefect-free N Unadjusted Adjusted 15,142 20,061 5,457 902 1.0 (0.99 – 1.02) 1.0 (0.96 – 1.04) 0.94 (0.89 – 0.99) 0.99 (0.96 – 1.03) 0.99 (0.98 – 1.01) 1.0 (0.96 – 1.03) 0.97 (0.93 – 1.02) 0.98 (0.93 – 1.04) 22,451 22,451 1.0 (0.99 – 1.03) 1.0 (0.99 – 1.03) 1.0 (0.98 – 1.01) 1.0 (0.99 – 1.01) Limitations Q CrossCross-sectional design Q Unobserved factors confounding associations O PatientPatient-level O HospitalHospital-level Q S.D. Range 0.52 0.87 0.75 0.57 0.30 0.12 0.16 0.35 (0 – 1.0) (0.29 – 1.0) (0.25 – 1.0) (0 – 1.0) 0.72 0.54 0.15 0.22 (0.32 – 1.0) (0 – 1.0) Discussion HR (95 % CI) Process Measure (PM) Single Discharge Instructions Mean Score Q Current CMS heart failure process measures (PM) are not associated with 11-year mortality in Medicare beneficiaries diagnosed with HF Q Explanation for null findings O Care given at discharge may not affect 11-year mortality O Documentation of care does not capture the intensity or accuracy of care O High variation for PM may prevent ability to detect small changes if they exist Strengths Documentation of process measure at discharge may not reflect the care given over 1 year Q First known study to link clinical registry data with CMS data to examine associations between process measures and longlong-term outcomes Q Generalizeable to Medicare feefee-forfor-service heart failure patients1 Q Models O Include both patient and hospital-level covariates O Account for clustering 1: Curtis et al., Abstract Proceedings at AHA, 2007 3 Conclusions & Recommendations Q Null findings do not undermine the need to continue providing care that is good clinical practice Q Need to more firmly establish link between PM and outcomes before broadly implementing P4P Q Improve the accuracy of the measures Q Continue evaluating the effects of PM O Within the context of longitudinal data O Using PM with known clinical efficacy 4