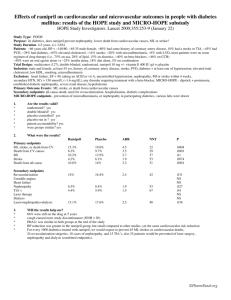
Motivation Gold Standard = RCT but…
advertisement

Using Observational Data to Extend the Results of a Randomized Controlled Trial: an Application to the HOPE Trial Motivation Gold Standard = RCT but… Randomized Controlled Trials (RCT) can never address all research questions Paul L. Hebert, PhD Mary Ann McLaughlin, MD, MPH Jodi Casabianca, MS Anu Lala, MD Jason Wang, PhD Certain patient groups under-represented Head-to-head drug trials are rare Observational studies subject to selection bias Causal statistical models rely on untestable assumptions Instrumental variables: Uncorrelated with unobserved factors Propensity score modeling, Inverse Probability of Treatment Weighting: “Ignorability” assumption Funding provided by NIDDK R21DK64322 (Hebert) Concept Find an RCT that was widely accepted, but left some questions unanswered Use statistical models on observational data to “recreate” the results of the RCT If models worked, then apply the same models to patients who were excluded from original RCT, or treatments that were not considered in the RCT Unanswered questions from HOPE Application: The Heart Outcomes PrEvention (HOPE) Trial (2000) Does ramipril work just as effectively in non-white patients? Are other ACEIs as effective as ramipril (i.e., is there a class effect for ACEIs)? Ramipril $53.03/ 30 day supply Benazepril $23.99 Captopril $12.99 Enalapril $8.19 22% lower rate of death/stroke/AMI in ramipril group Important: similar benefit found in subset of patients with hypertension Limitations of HOPE findings 95% of patients in HOPE were white HOPE used ramipril--a newer, more expensive ACEI Data 9297 patients with risk factors for heart disease randomized to ramipril vs placebo Results: Ramipril is effective in patients at high risk of cardiovascular events Dually-eligible Medicare+Medicaid beneficiaries from CA, 19961999. During time when HOPE was conducted. Medicaid SMRF/MAX files (inpat, outpat, and rx) + Medicare MedPAR (inpatient) and Physician/Supplier (outpatient) claims Inclusion criteria Filled an Rx for antihypertensive in 1996 and 1997 Eligible for Medicare because of age, surviving spouse, or disability Exclusion criteria HOPE-specific Other reasonable exclusions Age 55+, No CHF, stroke/MI in last 4 weeks, overt nephropathy Charlson score>5, age>=85, ESRD, taking antihypertensive for < 9 months Ever in an HMO, 1996-99 1 Sensitivity Estimation Strategy Recreate HOPE: Logit model for White patients Instrumental variable estimates of ramipril vs. other antihypertensives Outcome: combined outcome of death or hospitalization for stroke or MI from 1997 to 1999 Key Independent Variable: filled RXs for ramipril in 1997 Control variables: Age-squared, gender, Long-term care, disabled, indicators of conditions in Charlson, log(per capita income in ZIP), other medications in 1996 (diuretics, calcium channel blockers, beta blockers, statins, NSAIDs, antiarythmias) Repeat on non-white patients Repeat using other ACEIs ACE Inibitors Non-ACEI Ramipril Captopril Enalapril Benazepril Total 100,508 4,436 3,656 16,329 9,504 134,433 71.6 69% 52% 12% 6% 20% 24% 8% 11% 12% 70.4 66% 55% 12% 10% 17% 26% 4% 17% 9% Are patients dieing of things that ramipril could prevent? 71.6 69% 59% 13% 8% 14% 31% 12% 23% 11% 71.5 68% 56% 13% 7% 17% 26% 9% 19% 11% 70.8 70% 54% 14% 7% 18% 27% 6% 18% 10% 71.5 69% 53% 13% 6% 19% 25% 8% 13% 11% Estimate time to stroke/MI, COPD by ACEI used Stroke/MI should be preventable by better ACEI No evidence that better ACEI should prevent COPD Rare event so use Propensity Score Matching Could compliance with medications explain improved outcomes for ramipril vs other ACEIs? Results: Table 1 N Demographics Age Female White Black Hispanic Other/Unk race Disabled Long-term Care Diabetes COPD Medications Number Medications Beta Blocker Calcium Channel Blocker Diuretics Instruments= % ramipril use in ZIP code, county HMO market penetration Generate compliance-adjusted estimates using stratified Cox models with time-varying indicator for filled ACEI prescriptions on propensity score matched samples Yit=b0+b1ACEIi+b2Compliantit+uit Results: Can we match HOPE in NH white patients (n= 54,970)? Is ramipril just as effective in non-white patients (n= 39,476)? White Black, Hispanic or Unknown Lipid Lo we ring Ag ent Di uretic Ca lcium Ch ann el Blocker Beta Blocker Nu mber of Med s Ho sp ita lized 19 96 Tu mor Di abetes CO PD De mentia CV D Prior MI Di sa bled Fe male 7.6 23% 54% 36% 10.3 13% 37% 32% 13.9 18% 48% 49% 12.6 19% 52% 42% 11.1 21% 54% 43% 8.7 22% 53% 38% Age- Squa red RA MIPRIL .5 1 1.5 2 2.5 .5 1 1 .5 2 2.5 Odds Ratio Graphs by racegrp Other control variables: liver disease, rheumatic disease, ulcers, long-term care residence, log(per capita income in ZIP code), NSAIDs, anti-arythmias Results: Are other ACEIs as effective as ramipril? White Sensitivity Analysis: Instrumental Variables Correlation with instruments Black, Hispanic or Unknown % Ramipril use by ZIP code, Los Angeles Lipid Lo we ring Ag ent Di uretic Ca lcium Ch ann el Blocker Beta Blocker LPM of ramipril use. F(2,54970)=596 Coef (s.e.) P-value Constant 0.021 (0.003) <0.001 % Ramipril in 1 mile radius of ZIP code 0.8718 (0.0274) <0.001 HMO market Penetration in County -0.0246 (0.0054) <0.001 Nu mber of Med s Ho sp ita lized 19 96 Tu mor Di abetes CO PD De mentia CV D Prior MI Di sa bled Fe male Age- Squa red BENA ZE PRIL ENALA PRIL CA PTOPRIL RA MIPRIL .5 1 1.5 2 .5 1 1.5 2 Odds Ratio Other control variables: liver disease, rheumatic disease, ulcers, long-term care residence, log(per capita income in ZIP code), NSAIDs, anti-arythmias 2 Instruments uncorrelated with unobserved risk factors? IV results: Effect of ramipril on death/stroke MI Coefficient on ramipril use Ramipril users versus users of other Antihypetensives Other HTNs Age Female COPD Diabetes Hospitalizations prior year Medications Number of Medications Beta Blockers Calcium Channel Blockers Diuretics Lipid Lowering Agents Long term Care High ramipril ZIP codes versus low ramipril ZIP codes High Low Ramipril Ramipril ZIP Ramipril Difference ZIP codes Codes Difference 71.8 72% 13% 11% 0.2 70.7 70% 10% 17% 0.1 -1.2 -2% -3% 6% -0.1 71.9 73% 13% 12% 0.2 71.5 72% 13% 11% 0.2 -0.4 -1% -1% 0% 0.0 8.0 24% 49% 41% 18% 11% 11.0 14% 36% 33% 24% 5% 3.0 -10% -13% -8% 5% -6% 8.1 24% 48% 41% 18% 12% 8.3 23% 48% 40% 19% 9% 0.1 -1% 0% -1% 1% -3% White (n= 54,973) Black, Hispanic Unknown (n=39,476) Linear Probability Model -0.0596 (p<0.001) -0.014 (p=0.084) Instruments: % Ramipril use within own ZIP code, county HMO penetration -0.1076 (p=0.056) 0.011 (p=0.843) Instruments: % Ramipril use within 1 mile of ZIP code , county HMO penetration -0.1134 (p=0.041) 0.0171 (p=0.760) Instruments: % Ramipril within 3 miles of ZIP code, county HMO penetration -0.0784 (p=0.162) 0.0261 (p=0.653) * NOTE: Estimates are not stable. Sensitive to alternative specifications. Sensitivity: Effects of noncompliance Summary Effectiveness of other ACEIs compared to ramipril at preventing death, stroke/MI, and COPD in propensity score matched samples; unadjusted and compliance adjusted Cox proportional hazard models with time-varying indicators of compliance with ACEI. Estimated on propensity-score matched samples. Death/stroke/MI Stroke/MI Attempts to match results of HOPE had mixed success COPD B ena ze pril Same statistical procedures applied to Non-white patients suggest no benefit of ramipril Same procedure applied to ramipril versus other ACEI suggests ramipril is better than enalapril and captopril, similar to benazepril With better data, this could be a good strategy for using observational data to extend the results of randomized trials E nala pril Benazapril vs. ramipril 1006 matched pairs Ca pto pril Enalapril vs. ramipril 1136 matched pairs .5 1 1.5 2 .5 1 1.5 2 .5 1 1.5 Logistic worked IV Unstable 2 Hazard Ratio Captopril vs. ramipril 859 matched pairs Unadjusted Compliance Adjusted Note: Ramipril is the reference drug Are other ACEI’s as effective as ramipril? Odds ratios from logistic regression of death, stroke or MI for ACEI users versus Patients taking other antihypertensives White Only (n=43,572) Antihypertensive in 1997 Non-ACEI Ramipril Captopril Enalapril Benazepril Reference 0.80 [0.64,1.00] 1.06 [0.90,1.26] 1.03 [0.93,1.14] 0.81 [0.71,0.92] Black, Hispanic, Oth/Unk Race (n=31,211) Reference 1.03 [0.78,1.35] 1.25 [1.00,1.57] 1.15 [1.01,1.32] 1.09 [0.92,1.28] All Races (n=83,474) Reference 0.87 [0.73,1.03] 1.13 [0.99,1.29] 1.09 [1.01,1.18] 0.93 [0.84,1.03] Control variables: age-squared, demographics, other drug use, comorbidities, Long term care residence, log(per capita income) 3