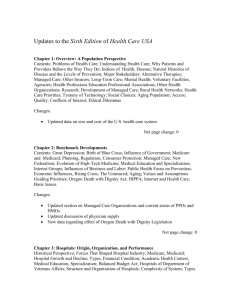
Massachusetts physician groups and an Call for Panels
advertisement

Call for Panels Group Practice, Systems and Quality: Examining the Linkages Chair: L. Gregory Pawlson, M.D., M.P.H. Sunday, June 3 • 11:00 a.m.-12:30 p.m. Panel Overview: Overview: In addition, number of key individuals doing work in related fields will be invited to lead the question/discussion portion of the presentation. Building on findings from current and past research by groups at Harvard, UC Berkeley, NCQA and others, the panel members will examine the growing evidence related to critical relationships between the presence and use of systems in practice, the organization of practice, for example, group structure, and quality as measured by clinical and patient experience of care measures. The work that will be discussed includes data from a national study of large physician organizations, studies of solo and single site small group. The exploration of correlations between characteristics of group practice, the presence and use of practice systems, and higher quality of care can help guide practice improvement work and provide a basis for future research to better understand systems-quality-practice organization linkages. Do integrated medical groups provide higher-quality medical care than individual practice associations? Ateev Mehrotra M.D., M.P.H., Arnold M. Epstein, M.D., M.A., Meredith B. Rosenthal Ph.D. Presented By: Ateev Mehrotra, M.D., M.P.H., Assistant Professor, RAND, 4570 Fifth Street, Suite 600, Pittsburgh, PA 15213, Phone: (412) 683-2300 x4894, Email: mehrotra@rand.org Research Objective: To examine the associations between the organizational structure of physician groups, use of quality improvement strategies, and health care quality. Study Design: Survey of 119 California physician groups who care for approximately 1.7 million enrollees of PacifiCare. Quality of care assessed using six HEDIS quality measures: mammography, Papanicolaou smear screening, Chlamydia screening, diabetic eye examination, use of an asthma controller medication, and beta-blocker after acute myocardial infarction. Supplemented by another survey of 79 Massachusetts physician groups and an examination of factors that are associated with use of quality improvement strategies. Principle Findings: In our California survey, controlling for other factors, Integrated Medical Groups, as compared to IPAs, had a 11% higher mammogram rate, 36% higher Pap smear rate, 10% higher Chlamydia screening rate, and 15% higher diabetic eye screening rate (all p<0.05). Leaders of IMGs were more likely to report using EMRs (37% vs. 2%; P < 0.001) and quality improvement strategies, but these characteristics explained little of the quality differences between IMGs and IPAs. The only other predictor of higher quality was volume of patients seen by the physician group for the quality measure. . In our Massachusetts survey of physician groups we found that pay-forperformance incentives did have an association with the use of quality improvement strategies (OR 1.6 [CI 1.0-2.4]). But several organizational factors had a stronger association including use of employed physicians (OR 3.2 [CI 1.5-7.2]), being part of a larger network (OR 2.3 [CI 1.1.4.8]), and larger size in terms of number of physicians (OR 2.2 [CI 1.0-4.9]). Conclusions: Integrated medical groups in California appear to provide a higher level of clinical quality than independent practice associations. Patients cared for in IMGs generally received higher quality primary care than those cared for in IPAs. Having an EMR and implementation of quality improvement strategies did not explain the differences in quality. Among Massachusetts physician groups larger integrated groups were more likely to use quality improvement strategies. These findings suggest that physician group type influences health care quality. Implications for Policy, Delivery, or Practice: Together the findings of both studies would imply that encouraging more integration in physician groups might result in greater use of quality improvement strategies and higher quality. The second study potentially indicates that this even true in the setting of pay-forperformance incentives Funding: California HealthCare Foundation and the Commonwealth Fund. Development, Testing & Correlation with Selected Quality Measures, of a Survey Instrument to Assess Systemness in Office Practice Sarah Scholle, Greg Pawlson M.D., M.P.H., Leif Solberg, M.D., Sarah Shih, M.P.H., Steve Asche, M.S. Presented By: Sarah Scholle, Dr.P.H., M.P.H., Assistant Vice President, National Committee for Quality Assurance, 2000 L Street NW, Suite 500, Washington, DC 20036, Phone: (412) 624-1825, Fax: (412) 624-2360, Email: scholle@ncqa.org Research Objective: The creation and validation of a tool that assesses the presence and use of systems in office practice. The elements included in the tool are related to the Wagner Chronic Care model. Study design: The development of an assessment tool used an expert panel, literature review and pilot testing to construct a survey related to four domains of Wagner chronic illness model: decision support, delivery system design, clinical information systems and patient self management support. To validate the survey, we obtained 120 respondents of varying job titles, medical director, practicing physicians, nurse coordinators, from 40 sites in 11 medical group practices in Minnesota followed by an onsite audit by trained observer. Correlation studies are based on responses from 41 medical directors representing distinct medical groups completing a revised survey. Data on clinical performance measures using chart review and administrative data was obtained from the Minnesota Measurement Collaborative. Principle Findings: Some of the early findings using the instrument which have been published in the AJMC 2006 11: 789-96, indicate that at least among groups in Minnesota, the presence of practice systems in general was not strongly influenced by whether or not the group had implemented an EMR. Dr. Scholle will also discuss findings from the study that address the validity of the data collection using a survey versus the gold standard of an on site audit, correlations between the use of practice systems in general, and specific areas of the chronic illness model with clinical performance measures and surveys of patient experience of care. Preliminary findings suggest significant correlations between overall systems use and clinical quality of care measures in diabetes. Data from similar concurrent studies being done in California and Massachusetts, comparing systems use to patient perceptions of care, will also be presented. Finally, she will discuss the use of a web enabled version of the survey that is coupled with requirements for documentation of the systems as a basis for payment for physician practice systems in the Bridges to Excellence program and elsewhere. Conclusions: A survey of systems that are related to the elements of the chronic disease model has been developed and validated against the use of an onsite audit. Implications for Policy, Delivery, or Practice: The survey may be useful not only as a research tool, but as a basis of payment for the use of systems in ambulatory care physician practice. Fundering Source: Robert Wood Johnson Foundation The 2nd National Study of Physician Organizations and Management of Chronic Illness Diane R. Rittenhouse, M.D., M.P.H., Stephen Shortell, Ph.D., Lawrence Casalino, M.D., Ph.D., James Robinson, Ph.D., Robin Gillies, Ph.D. Presented By: Diane R. Rittenhouse, M.D., M.P.H., Assistant Professor, Department of Family and Community Medicine, University of California, San Francisco, 500 Parnassus Avenue, BOX 0900, Room MU 308-E, San Francisco, CA 94143-0900, Phone: (415) 5024048, Fax: (415) 476-0705, Email: rittenhouse@fcm.ucsf.edu Research Objective: The National Study of Physician Organizations and Management of Chronic Illness (NSPO) was conducted in 2000/2001 and established an association between the use of organized care management processes (CMPs) and higher levels of external incentives and information technology (IT) capacity. We are currently in the field with the 2nd National Study of Physician Organizations and the Management of Chronic Illness (NSPO II). The goals of this study are (1) to describe the extent to which physician organizations are currently employing CMPs in the routine care of patients; (2) to describe the current practice environment, both internal (eg, adoption of information technology, payer mix, size, structure) and external (eg. external incentives to improve quality, relationships with health plans); and (3) to determine the extent to which these factors, and their interrelationships, have changed over time. In a related study we will be linking these data to outcome measures to better understand the relationship between the structure and processes of physician organizations and improved patient outcomes. Study Design: 25-minute telephone survey. The survey has been in the field since Spring 2006. Targeted response rate: 70% by March 2007. Population Studied: The Medical Director or CEO of all physician organizations (medical groups and independent practice associations) with 20 or more physicians that care for patients with asthma, CHF, depression and/or diabetes. (n=1,216) Principal Findings: Results will be finalized in preparation for the 2007 Annual Meeting. Crosssectional data will be presented, including descriptive statistics for all physician groups across 8 major content domains: organizational background and history (size, specialty, number of sites, etc); information systems (presence of electronic health record, measures of functionality and interoperability); care management and clinical practice (disease registries, reminders, clinical practice guidelines, feedback to physicians, self-management skills, practice re-design, etc); preventive care and health promotion; relationships with health insurance plans; performance incentives (financial and non-financial); revenue sources and compensations methods; and organizational culture. Results of regression models predicting CMP use will also be presented. Comparisons will be made to baseline data from 2000/2001. Conclusions: These new cross-sectional data provide valuable information on the practice environment and quality improvement efforts of large physician organizations nationwide. Implications for Policy, Delivery, or Practice: These data inform the effort by the Institute of Medicine and others to improve the delivery of chronic illness care through delivery system improvements. Funding Source(s): Robert Wood Johnson Foundation; Commonwealth Fund; California HealthCare Foundation. Call for Panels Medicare Advantage Private Plans: Costs & Benefits in 2007 Chair: Stuart Guterman, M.A. Monday, June 4 • 11:00 a.m.-12:30 p.m. Panel Overview: The Medicare Modernization Act (MMA) of 2003 included provisions intended to greatly increase the role of private health plans in Medicare. Consistent with this objective, enrollment in Medicare Advantage (MA) plans increased 24 percent between December 2005 and December 2006. Private plans now manage benefits for over 17 percent of Medicare beneficiaries, the largest share ever. Due to this rapid increase in enrollment as well as recent research findings indicating that MA plans do not contain overall Medicare costs as often claimed but in fact increase costs by 12 percent per plan enrollee, MA private health plans have become a major Medicare issue. Press commentaries report that the future role of MA plans will be a key item on the agenda of the new Congress. Reports from health services researchers on the costs and benefits of MA private plans have played an important role in this debate. The panel would present findings from current research on the status and effects of the MA program. 1. The first presentation summarizes how Medicare Advantage (MA) plan availability, benefits and premiums, and enrollment have changed between 2005 and 2007 by the Medicare Drug, Improvement, and Modernization Act (MMA) of 2003. 2. The second presentation addresses payments to MA plans with a focus on the specific MMA policies that result in MA payments in excess of average fee-for-service costs. Projected amounts and patterns of extra payments in 2006 and beyond would be discussed. 3. The third presentation compares private health plans’ costs of delivering Medicare benefits under the MA program with the costs of delivering those benefits in the fee-for-service program and investigate how private plans’ costs vary across geographic areas and assess the implications for converting Medicare to a premium support system. 4. The fourth presentation addresses the relationship between the legislatively determined payment rates to Medicare managed care plans and MA program enrollment, the availability of particular benefits and plan choices for beneficiaries. Call for Panels Assessing Quality of Care of Medicare Managed Care Health Plans and Frailty Adjustment Using the Medicare Health Outcomes Survey and the Medicare Health Outcomes Survey-Modified Chair: Beth Ellis, Ph.D. Sunday, June 3 • 11:00a.m.-12:30p.m. Panel Overview: With the advent of Medicare Part D Programs, enrollment in Medicare managed care health plans is increasing rapidly. Evaluation of health quality and appropriate frailty adjustment for payment purposes are critical to the success of beneficiary health and continued managed care health plan participation. This panel will discuss uses of the Medicare Health Outcomes Survey (HOS) and the HOS-Modified (HOS-M), which are sponsored by the Centers for Medicare & Medicaid Services. The Medicare HOS assesses a health plan’s ability to maintain or improve the physical and mental health functioning of its beneficiaries over a two-year period of time. The HOS-M instrument, which is a modified version of the Medicare HOS, assesses health functioning of vulnerable program members who are at greatest risk for poor health outcomes to generate information for payment adjustment. We propose five panelists for the 90-minute session. The first panelist will present the background of the Medicare HOS and HOS-M surveys; their history, goals, and purpose. The second speaker will present information on the new quality measures recently added to the HOS, which include questions on falls, height/weight, physical activity, and osteoporosis. The third panelist will present HOS case-mix adjustment, based on the Veteran’s 12-Item Health Survey for the evaluation of managed care health plan performance. The fourth panelist will present information on frailty adjustment, which is used for CMS payment purposes. The final speaker will provide the results of analyses that examine differences in response rates and other outcomes associated with various HOS-M protocols. The Medicare Health Outcomes Survey & the Medicare Health Outcomes SurveyModified: An Introduction Vijit Chinburapa, Ph.D., C.P.H.Q., Beth Hartman Ellis, Ph.D., MaryAnne D. Hope, M.S., Laura Giordano, R.N., M.B.A. Presented by: Vijit Chinburapa, Ph.D., C.P.H.Q., Senior Healthcare Researcher, Surveys, Research & Analysis, Health Services Advisory Group, 1600 Northern Avenue, Phoenix, AZ 85020, Phone: (602) 665-6185, Fax: (601) 241-0757, Email: vchinburapa@azqio.sdps.org Research Objective: The objective of this presentation is to provide an introduction to the national Medicare Health Outcomes Survey (HOS) and the national Medicare Health Outcomes Survey-Modified (HOS-M). Study Design: The Medicare HOS assesses a managed care health plan’s ability to maintain or improve the physical and mental health of its members over time. The Medicare HOS 2.0 instrument incorporates the Veterans 12 Item Health Survey (VR-12), demographics, chronic medical conditions, activities of daily living, the number of unhealthy days, urinary incontinence, depression and other characteristics. The Medicare HOS-M survey is a modified version of the Medicare HOS. Originally entitled the Program of All-Inclusive Care for the Elderly Health Survey (PACE), the HOS-M is administered to vulnerable Medicare beneficiaries at greatest risk for poor health outcomes. The instrument assesses the physical and mental health functioning of Program members to generate information for payment adjustment. Population Studied: The HOS measure is administered at Baseline to a randomly selected sample of beneficiaries from each managed care plan that holds risk and cost contracts. The twoyear follow up sample includes beneficiaries that are identified from the Baseline sample who are alive, enrolled in their original managed care plan, and have sufficient VR-12 data to derive a physical and mental component summary (PCS/MCS) score. Multivariate statistical methods are used for case-mix adjustment so all plans will be as equal as possible in terms of demographic and socioeconomic characteristics, chronic medical conditions, and other covariates. The HOS-M was fielded for the first time in the spring of 2005. Program members are enrolled in specialized Medicare plans-----PACE programs, Minnesota Senior Health Options, Minnesota Disability Health Options, Wisconsin Partnership Program, and Massachusetts MassHealth Senior Care Options. Principal Findings: The PCS and MCS scores derived from the HOS surveys reflect normbased standardized scores with a mean of 50 and a standard deviation of 10, relative to the U.S. general population. The national PCS and MCS scores for the Medicare beneficiaries across the eight cohorts of study from 1998-2005 were relatively stable. The PCS scores ranged from 40.3 to 42.0 with a weighted mean of 41.3. The MCS scores ranged from 51.6 to 52.6 with a weighted mean of 52.0. Conclusions: For all HOS Cohorts, a Baseline Report and a Performance Measurement Report are prepared following data analysis activities. Seniors (age 65 or older) who have a calculatable PCS and MCS score at Baseline are eligible for Performance Measurement. Both Baseline and Performance Measurement Reports are provided to all participating plans as well as all Quality Improvement Organizations. HOS-M reports will be distributed in 2007 and plan data will be available in 2008. Implications for Policy, Delivery or Practice: The Medicare HOS program gathers valid and reliable health status data in the Medicare managed care population for use in quality improvement activities, plan accountability, public reporting, and improving health. Funding Source(s): CMS Impacts of Applying Frailty to Medicare Advantage Plans Thomas Kornfield, M.P.P., Sean Creighton, M.Sc. Presented by: Sean Creighton, M.Sc., Research Analyst, Division of Program Analysis and Performance Measurement, 7500 Security Boulevard, C4-13-01, Baltimore, MD 21244, Phone: (410) 786-9302, Fax: (410) 786-1048, Email: screighton@cms.hhs.gov Research Objective: Evaluate the impact of applying frailty adjustment factors to the entire Medicare Advantage program, based on the Medicare Health Outcomes Survey (HOS) and HOS-Modified (HOS-M) data. Study Design: Cross-sectional analysis of survey data, combined with prospective risk adjustment model. The risk adjustment model was developed by linking data from the 2003 Consumer Assessment of Healthcare Providers and Systems (CAHPS) with Medicare claims data in order to estimate new frailty factors. We included only non-ESRD, non-managed care Medicare enrollees who responded to all six Activities of Daily Living (ADL) questions on the 2003 Fee-for-Service (FFS) CAHPS in the modeling process. For each beneficiary in the sample, we obtained demographic and enrollment information from the Medicare EDB, and used the Data Extract System (DESY) to acquire Medicare claims. We also linked data on long-term institutionalization from the Minimum Data Set, and information on ADL difficulty from the CAHPS. Based on the HOS and HOS-M, data, we calculated contract level frailty factors. We restandardized the ratebook so that the net impact of frailty would be zero. We then adjusted contract bid data from health plans for the 2007 contract year in order to account for the new frailty factors. Finally, we estimated the payment impacts of applying frailty to these contracts. Population Studied: The frailty factor developed from the Medicare FFS CAHPS data was applied to respondents to the HOS and HOS-M data, and a selected group of July 2006 Medicare managed care enrollees. Principal Findings: We used diagnostic information from base year claims for hospital inpatient, outpatient, and physician sources to calculate annualized predicted expenditures based on the CMS-HCC model. We calculated residual expenditures as the annualized actual expenditures minus the annualized predicted expenditures. We then used the residual expenditures in an equation in order to determine the additional costs associated with one of four ADL difficulty groups: no ADLs, 1-2 ADLs, 3-4 ADLs, and 5-6 ADLs. We developed two frailty models: one in which the frailty factors depended on Medicaid status during the payment year, and the other in which the frailty factors were independent of Medicaid status. For both models, we calculated frailty factors for non-ESRD, non-institutionalized individuals aged 55 and over. We evaluated the impacts of applying frailty to the entire Medicare Advantage program to analyze whether or not applying the frailty factor would more accurately pay these contracts for their frail population. Based on bidding data from health plans for the 2007 contract year, we estimated the payment impacts of applying the frailty factor to these plans. We estimated impacts at the contract and contract/plan level. Conclusions: The Medicare HOS and the HOSM measure health status and functional limitations for the entire Medicare managed care population. The availability of the ADL data under HOS and HOS-M provides avenues for exploring new payment options under frailty adjustment. Implications for Policy, Delivery or Practice: The findings have implications for payment policy decisions. Funding Source(s): CMS Comparing Two Approaches to Surveying Frail Enrollees in the 2006 Medicare Health Outcomes Survey - Modified (HOS-M) Edith Walsh, Ph.D., G. Khatutsky, M.S., Ph.D. Candidate Presented by: Edith Walsh, Ph.D., Senior Health Policy Researcher, Aging, Disability and LongTerm Care, RTI International, 1440 Main Street Suite 310, Waltham, MA 02451, Phone: (781) 4341754, Fax: (781) 434-1701, Email: ewalsh@rti.org Research Objective: Due to high frailty and cognitive impairment rates of HOS-M respondents, HOS-M sampling and administration protocols include special efforts to collect detailed contact information for potential proxies in order to increase response rates. However, in 2006 this process was waived for some plans as their enrollments were too large for this process to be feasible. Enrollees in these plans were sampled without making any special provisions to obtain proxy information. This study evaluates these two survey approaches by comparing survey results and discussing future implications for HOS-M administration. Study Design: Examines the differences in response rates, demographic, health, and functional status characteristics between 2006 HOS-M respondents in samples with proxy contact information and those without. Population Studied: Frail dually eligible Medicare beneficiaries aged 55+ residing in the community and enrolled in PACE or Dual Eligible Demonstration Plans in Minnesota, Wisconsin and Massachusetts, and who responded to the 2006 HOS-M. Principal Findings: The overall response rate for plans without proxy contact information was 68.7%, comparing favorably with 74.3% for enrollees in plans surveyed using a protocol including collecting detailed contact information. However, proxy response rates and mean characteristics between the groups were very different. Respondents in the first group reported less functional and cognitive impairment with 33% reporting no limitations in activities of daily living (ADLs), 2 ADL impairments on average and 29% reported cognitive impairment compared to only 19% with no ADL impairments, 3 ADL impairments on average and 45% cognitively impaired in the small plans using the full, extended survey protocol. Conclusions: The overall response rates and lower level of impairment observed in the plans without proxy contact information suggest that implementing burdensome extra efforts to increase response rates may not be warranted for these plans. Nonetheless, it is possible that the HOS-M protocol misses the frailest beneficiaries enrolled in these plans due to nonresponse. In previous HOS-M analyses we found the mean ADLs for self respondents to be substantially lower than for those with proxy respondents (2.5 vs 3.8). Given the greater degree of impairment in the small plans and the high proxy response rates, the extended protocol may be necessary to ensure accurate representation of their enrollment. In addition, any future declines in the response rate could reflect changing enrollment patterns and warrant consideration of using the extended protocol for all plans participating in the HOS-M. Implications for Policy, Delivery or Practice: Creating detailed contact data for the HOS-M sample is burdensome for plans and adds to the overall costs of conducting the HOS-M, yet it does provide enhanced response rates and potentially ensures representation of more impaired beneficiaries. The results of this analysis provide information that policy makers can use to evaluate approaches to data collection for frailty adjustment. Funding Source(s): CMS New Measures in the Medicare Health Outcomes Survey Judy Ng, Ph.D., Lok Wong, M.H.S., Sarah Scholle, Dr.P.H. Presented by: Judy Ng, Ph.D., National Committee for Quality Assurance, 2000 L Street, NW, Washington, DC 20036, Phone: (202) 9553599, Email: ng@ncqa.org Research Objective: The Medicare Health Outcomes Survey assesses health and functional status outcomes of Medicare beneficiaries enrolled in Medicare Advantage. We discuss the background and rationale for the development of a new set of Health Outcomes Survey measures addressing prevalent problems in older populations, including falls, osteoporosis, urinary incontinence, and physical activity. We use descriptive data from the 2006 Medicare Health Outcomes Survey to evaluate the extent of these problems, and to examine whether differences exist by vulnerable populations. Study Design: The Health Outcomes Survey is a mail survey with telephone follow up, administered to a nationally representative sample of Medicare beneficiaries in Medicare Advantage. The survey questionnaire includes the VR12 and other items addressing chronic conditions, physical and functional limitations, and demographics. Importantly, this survey makes it possible to learn whether patients are receiving advice and counseling on important topics related to prevention and functioning for older adults. Population Studied: Community dwelling Medicare beneficiaries, aged 65 and older, enrolled in over two hundred US Medicare Advantage plans. Principal Findings: 2006 Medicare Health Outcomes Survey data will be used to evaluate the overall prevalence of problems with falls, osteoporosis, urinary incontinence and physical activity among elderly beneficiaries, as well as physician counseling and advice for these conditions. The data will also be used to perform subgroup analyses of select populations who are particularly susceptible to health problems, such as non-white racial minorities, and those with lower education or income. Conclusions: The Health Outcomes Survey is the largest scale effort to evaluate health outcomes among the elderly Medicare population, and serves as a platform for evaluating the quality of care and addressing comprehensive health needs of the elderly, particularly vulnerable groups. Implications for Policy, Delivery or Practice: The Health Outcomes Survey is a valuable tool in targeting quality of care in Medicare managed care. The interpretation of Health Outcomes Survey data provides key information in maintaining and improving these efforts. Funding Source(s): CMS Case-Mix Measures for Monitoring System Performance Kazis Lewis, Sc.D, Alfredo Selim, M.D., M.P.H., William Rogers, Ph.D., Shirley Qian, M.S., Xinhua S. Ren, Ph.D. Presented by: Kazis Lewis, Sc.D, Director, Boston University, Center for the Assessment of Pharmaceutical Practices, 715 Albany Street, Boston, MA 02118, Phone: (617) 414-1418, Email: lek@bu.edu Research Objective: This presentation will give methodologies for case mix measures using the Veterans RAND 12 Item Health Survey (VR-12) as the outcome. The VR-12 is modified from the Veterans RAND 36 Item Health Survey and the RAND SF-36. This measure of functional status and wellbeing spans the domains of physical to psychological functioning. The VR-12 has recently been included as one of the performance measures in the HEDIS 2006 Information Data Set. The objectives of this presentation will be to examine measures of health at baseline and at follow-up for purposes of case mix adjustment using the VR-12 PCS (physical function) and MCS (mental function) summary scores for measuring the performance of health plans over two years in the Medicare Advantage Program (MAP). Study Design: The Medicare Health Outcome Survey (HOS) is a cohort design with a baseline sample and a follow-up 2 years later. Cohorts using the VR-12 began in 2006 round 7 at followup. The SF-36 version 1.0 was used in prior cohorts beginning in 1998. The recent addition of the VR-12 for the transition year cohort 7 affords researchers the opportunity to investigate risk adjustments for monitoring changes in health using the 12 item versions including the RAND SF-12 and the VR-12. The case mix methodology for performance measurement (monitoring outcomes of health over 2 years) uses separate case mix models for death, change in PCS and change in MCS. The models for change in PCS or (MCS) are the same or better versus worse. The case mix measures for the change models include demographics (age, gender, race, Medicaid status) and socioeconomic (education, income) status. The mortality models add chronic medical conditions, functional status and design variables (mode of administration). The two models are then combined to calculate the probability of being alive and having PCS (or MCS) the same or better. Scores are reported as the percentage of respondents within a plan who are better, same or worse for a two year period. Population Studied: The Medicare Advantage Program (MAP) cohort 7 is from the HOS that randomly selected 1000 beneficiaries who were continuously enrolled for at least 6 months in each of the MAP plans nationally. Principal Findings: Based upon prior cohorts, the SF-36 PCS and MCS outcome measures have been validated by evaluating the performance of health plans nationally. Recently, parsimonious models using the VR-12 with adjusted PCS and MCS scores are developed capturing fewer case mix adjusters for monitoring performance among the plans. Separate models include the use of adjusted VR-12 PCS and MCS scores cross-sectionally to capture health. Results suggest that cross-sectionally adjusted scores are a function of disease burden with less variability explaining performance. Conclusions: Results of this work provide an important basis for case mix approaches to evaluate plan performance. Implications for Policy, Delivery or Practice: This study has important implications for the monitoring of system performance among the plans. Funding Source(s): CMS Call for Panels Issues in Public Health Finance Chair: Peggy A. Honore', D.H.A., M.H.A. Sunday, June 3 • 3:00 p.m.-4:30 p.m. Panel Overview: Public Health Finance has been described as a field of study that examines the acquisition, utilization, and management of resources for the delivery of public health functions and the impact of those resources on population health and the public health system. This field is both an economic concept and a profession. It is an economic concept, grounded in public finance theories where the focus is on policies to guide resource utilization and financing strategies and also a profession, where financial management concepts should be applied to the utilization of scarce resources. This panel will examine a continuum of issues that lie within the definition of public health finance. Finance topics presented by the panel will include the challenges in public health agencies for financing legislatively mandated state newborn screening programs; assessing two different financing strategies for increasing dental sealant prevalence among Medicaid children; and the development of a comprehensive, evidence-based list of competencies for the public health financial management workforce. Financing Newborn Screenings: Sources, Issues, and Future Considerations Michele Lloyd-Puryear, M.D., Ph.D., Donna Williams, B.S., Kay Johnson, M.P.H., Marie Y. Mann, M.D., M.P.H., Lauren Raskin Ramos, M.P.H. Presented by: Michele Lloyd-Puryear, M.D., Ph.D., Chief, Genetic Services Branch, Division of Services for Children with Special Health Need, MCH Bureaus, HRSA, 5600 FIshers Lane, Rm 18-A-19, Rockville, MD 20857, Phone: (301) 443-8604, Fax: (301) 443-1080, Email: MPuryear@hrsa.gov Research Objective: State Public Health agecnies currently face the challenges of financing state-of-the-art newborn screening systems, which feature tests for more conditions, use of new laboratory technology, staff with skills to use new technology, and more effecetive follow-up with families. The pressures on State public health agencies reflect the coming together of parental concern, private sector marketing, and public opinion. The objective of this resaerch was to document the sources and uses of funding for newborn screening programs. Study Design: Two types of data are reported. The primary data comes from a survey of State public health agencies conducted from Novemebr 2004 - February 2006. These survey data are supplemented with findings from seven case studies: California, Maryland, Minnesota, Mississippi, New York, Oklahoma, and Oregon. The authors particiapted in the design of both the survey and the case studies, as well as analysis of the data reported by the States. Population Studied: The survey population in this research included state public helath agency newborn screenign programs. Principal Findings: Concurrent to the expansion in newborn screening panels has been the increased dependence of newborn screening programs on fees. Findings suggest that the general trend in the amount of funding for newborn screening programs is increasing. Additional laboratory costs for technology, expansion of testing panels, increased follow-up resulting from additional screening tests, and costs for associated public health services accounted for the need for additional funds. Funding increases emanate primarily from fees (22), and to a lesser extent from Medicaid (10), Title V MCH Block Grant (7), and State general revenue funding (3). Twenty States reported no change in the level of Medicaid or Title V fiscal support, and 23 had no increase from State revenues. Conclusions: Regardless of the source of funds, the available evidence indicates that states are committed to maintaining their programs and securing the necessary financing for the initial screening through diagnosis. Use of federal funding is currently limited; however, pressure to provide dedicated federal funding would likely increase if a national recommendation for a uniform newborn screening panel were to be issues. Implications for Policy, Delivery or Practice: With recent increases in costs, fees, and government support, newborn screening has attained greater health care financing visibility. One major misperception is that tax dollars are the primary source of newborn screening funds. When State public health officials request additional funding support from legislatures and governors, they are often confronted with budget constraints. Yet in most States the majority of program funding comes from fees and not from State or Federal sources. A valid funding concern in many States relates to matching funds that are required to support screening for newborns receiving Medicaid assistance. These concerns are of greater concern in the States with larger percentages of Medicaid births. Additional funding concerns for program infrastructure and follow-up arise in States where laboratory services may be contracted to private sources without proper attention to the continuing public health follow-up and service activities that may arise from the testing. Impact of Inceasing Medicaid Dental Reimbursement and Implementing School Sealant Programs on Sealant Prevalence Susan O. Griffin, Ph.D., Kari A. Jones, Ph.D., Stuart Lockwood, D.D.M., M.P.H., Nicholas G. Mosca, D.D.S., Peggy A. Honore, D.H.A. Presented by: Susan O. Griffin, Ph.D., Health Economist, Division of Oral Health, Centers for Disease Control and Prevention, 4770 Buford Highway, Mailstop F-10, Atlanta, GA 30341, Phone: (770) 488.6064, Fax: (770) 488.6080, Email: sig1@cdc.gov Research Objective: Delivering dental sealants to lower-income children has been shown to be cost-saving. Sealant prevalence among these children (25%), however, is well below the HP2010 goal of 50%. This research examined the impact of two financing strategies on dental sealant prevalence among Medicaid children. The two strategies were 1) increasing Medicaid reimbursement for sealant delivery to increase dentists' willingness to supply sealants in clinical settings levels and 2) changing the delivery setting from private dental offices to schools to increase demand for sealants by reducing parental travel and time costs. Study Design: Multivariate time series with comparison group Population Studied: 7- to 9-year-old children enrolled in Medicaid in Alabama (AL) or Mississippi (MS) in 1999 or 2003. Principal Findings: Increasing the sealant reimbursement rate was associated with a 39% and a 102% increase in sealant prevalence in AL and MS, respectively. Implementing school sealant programs more than doubled sealant prevalence - 153% in AL and 200% in MS. Conclusions: Depending upon supply and demand conditions in dental markets, both strategies can be effective in increasing the prevalence of sealants. In areas with dental shortages and where time and travel costs are likely to be especially taxing on parents, and for low income populations at greatest risk for disease, delivery in a school setting becomes increasingly cost-effective. Implications for Policy, Delivery or Practice: Policies for providing sealants in school settings to lower-income children is likely to be the most cost-effective mode of sealant delivery. Developing Competencies for the Public Health Financial Management Workforce Julia F. Costich, J.D., Ph.D. Presented by: Julia F. Costich, J.D., Ph.D., Chair, Dept. of Health Services Management, College of Public Health, University of Kentucky, Lexington, KY 40536-0003, Phone: (859) 2576712, Fax: (859) 257-3909, Email: jfcost0@email.uky.edu Research Objective: The development of a comprehensive, evidence-based roster of competencies for public health financial management. Study Design: Two strategies were used to garner both formal statements of practice standards and the experience of experts in the field. First, a review of competency assessments from cognate disciplines included the work of federal and state finance officers’ professional organizations, health care financial management groups, public health educational and professional associations, and position descriptions in which competency statements were embedded. Second, the principal investigator called on a group of nationally recognized experts in public health finance and related areas to participate in a series of conference calls in which proposed competencies were developed and reviewed. Population Studied: Public health financial managers Principal Findings: Competencies were identified in three broad areas: (a) financial management, analysis and assessment; (b) Policy development and program planning; and (c) general administration. Typical activities were listed in associated with each identified competency. The level of competency required for public health finance staff, management, and senior management was ranked as proficient, knowledgeable, or aware. Conclusions: The work of financial management in public health lies at the intersection of two broad, well-developed disciplines: public sector finance and health care finance. The demand for financial transparency and accountability in taxpayer-funded entities raises the need for more uniformity and accessibility in public health financial data. Meeting these expectations will require high levels of performance and greater investment in financial expertise. Implications for Policy, Delivery or Practice: The next step towards improvement in public health financial management is an assessment of current managers’ training needs from their own perspective as well as that of their supervisors. Once these needs have been identified, existing educational resources should be assessed and where necessary, new materials developed to raise the level of public health financial management performance. Funding Source(s): RWJF Call for Panels Improving Safety Culture in Healthcare Organizations Chair: Sara Singer, M.B.A. Sunday, June 3 • 3:00p.m.-4:30p.m. Panel Overview: Since the Institute of Medicine publicized in 1999 significant lapses in safety in US hospitals, efforts to improve patient safety have received considerable attention from policymakers and practitioners. Based on evidence from organizations that face hazardous conditions akin to healthcare delivery yet achieve strong safety performance, many believe that initiatives that seek to strengthen an organization’s culture of safety are among the most promising for reforming healthcare delivery. In recent years, research has made significant progress in defining and measuring safety culture, understanding how it varies among and within organizations, and using data to direct and evaluate safety performance enhancing improvements. Our panel will review some of the most important research-based initiatives in this field. Four presentations will address this topic. The first presentation will address considerations in choosing the right safety culture survey instrument for one’s own organization or system by presenting a comprehensive review and comparison of safety culture measurement instruments. The second presentation will discuss the importance of comparing safety culture in one’s own hospital to others and will present comparative data from the AHRQ Hospital Survey on Patient Safety benchmarking database. The third presentation will explore internal variations in safety culture for targeting improvement efforts based on findings from an investigation of safety culture survey results from a random sample of 92 US hospitals. The fourth presentation will describe one of the most promising interventions evaluated to date for improving safety culture and performance reliability: the comprehensive unit-based safety program. Safety Climate: Variation by Management Status and Profession Sara Singer, M.B.A., Laurence Baker, Ph.D., David Gaba, M.D., Alyson Falwell, M.P.H., Tobias Rathgeb, B.A., Shoutzu Lin, M.S. Presented by: Sara Singer, M.B.A., Senior Research Scholar, Center for Health Policy/Primary Care and Outcomes Research, Stanford University, 117 Encina Commons, Stanford, CA 94305, Phone: (617) 495-5047, Fax: (617) 325-7451, Email: ssinger@hbs.edu Research Objective: Understanding how safety culture varies within organizations is critical for designing patient safety improvement efforts. Using more aggregated measures of safety culture perceptions and often focusing on narrow groups of hospitals, previous research has identified variations across broad classes of hospital personnel, showing for example that senior managers’ perceptions about safety culture are more optimistic than those of front line employees and that physicians are more optimistic than nurses. To use this information to fashion culture improving strategies, further detail is needed. This paper examines in a nationwide hospital sample whether variations between (1) senior managers and front line personnel and (2) nurses and physicians persist when more detailed measures of safety culture are examined. We also study whether patterns of variation are observed among groups of varying ages, gender, tenure, and work area. Study Design: Individual-level cross sectional comparisons relate survey-based measures of safety culture to individual characteristics. Safety culture measures are derived from the Patient Safety Climate in Healthcare Organizations (PSCHO) survey, administered to personnel at a nationwide sample of hospitals in 2004. Survey results provide an overall measure of each respondent’s perception of the strength of safety culture at their institution, and eight sub-scale measures. Psychometric analysis of response patterns supports data validity. Differences in perceptions are examined using regressions that recognize sample dependence due to the nesting of individuals within work areas within hospitals (e.g. hierarchical and fixed effects modeling). We focus on variations by management status (senior manager, front line worker) and profession (physician, nurse, other staff). Regressions control for hospital, work area, and respondent’s age, gender, and job tenure. Population Studied: All senior managers, all physicians, and a random sample of 10% of other staff at 92 hospitals. The sample includes hospitals of a wide range of sizes and hospitals in all census regions. Principal Findings: While nurses reported more problems than physicians in some areas, physicians reported more problems in other areas. For example, physicians were more likely to experience shame when they needed to ask for help. Also, differences among nurses and doctors depended on additional characteristics of personnel. For example, nurses who were senior managers or near retirement were more optimistic than their younger and more junior counterparts. We also found that while hospital senior managers were more optimistic than nonsenior managers consistently across all dimensions of safety climate, this was not true in all hospitals. In addition, senior managers who were young or who were clinicians were more pessimistic than older, non-clinician senior managers. Conclusions: Physicians do not uniformly perceive safety culture more optimistically than nurses. There are many nuances and interactions that influence safety culture measurement. Implications for Policy, Delivery or Practice: Differences in perceptions of problems between nurses and physicians suggest the need for different interventions for each group. Consistent differences in perceptions between senior managers and front line employees suggest that interventions that engage senior managers and expose them to experiences of front line care could improve safety culture. Funding Source(s): AHRQ Results from the AHRQ Survey on Patient Safety Culture Joann Sorra, Ph.D., Veronica Nieva, Ph.D., Theresa Famolaro, M.P.S., Naomi Dyer, Ph.D. Presented by: Joann Sorra, Ph.D., Westat, 1650 Research Boulevard, Rockville, MD 20850, Phone: (301) 294-3933, Fax: (301) 315-5912, Email: joannsorra@westat.com Research Objective: The AHRQ Survey on Patient Safety Culture Hospital Database represents the largest compilation of data from the AHRQ Hospital Survey on Patient Safety Culture currently available and serves as a useful reference for benchmarking and comparison. This paper presents results from the 2007 database, identifying areas of strength and patient safety culture improvement across the database hospitals. Survey results by hospital characteristics, and respondent staff position and unit are also presented. Study Design: The database consists of survey data from 382 hospitals with 108,621 respondents. Hospitals voluntarily submitted their data to the database. An average of 284 surveys were submitted per hospital, with an average hospital response rate of 56%. Paper surveys had a higher average response rate (62%) than web (43%) or mixed mode (53%). Most hospitals (79%) administered the survey to a census of staff or a sample from all hospital departments. The database hospitals are generally consistent with the national distribution of AHA-registered hospitals (by bed size, teaching status, region). Population Studied: The 2007 database consists of data from 108,621 respondents across 382 U.S. hospitals. Principal Findings: The average percent of positive response on each of the survey’s 42 items and 12 patient safety culture composites was calculated across database hospitals. Teamwork Within Units was the composite with the highest average positive response (78%); Nonpunitive Response to Error had the lowest positive response. On average, the majority of respondents within hospitals (70%) gave their unit a patient safety grade of ‘‘Excellent’’ or ‘‘Very Good.’’ However, the majority of respondents within hospitals (53%) had reported no events over the past year. Smaller hospitals (49 beds or fewer) had the highest average positive response on all 12 patient safety culture composites. Respondents in Administration/Management had the highest average positive response on 11 of the 12 composites. Rehabilitation had the highest percent of respondents who gave their unit a patient safety grade of ‘‘Excellent’’ or ‘‘Very good’’ (81%); Medicine had the lowest percent (58%). ICU (any type) had the highest percent of respondents who had reported one or more events in the past year (69%); the lowest percent reporting was from Anesthesiology (41%). Percentile scores are also presented on the items and composites to show the variability of scores and enable more precise comparisons for hospitals. Conclusions: There is a fair amount of variability on the survey across database hospitals. Averages and percentiles provide useful information to enable hospitals to compare their results. The database also helps identify key areas of strength and patient safety culture improvement for most hospitals. Implications for Policy, Delivery or Practice: It is important for hospitals administering a patient safety culture survey to be able to compare their results against other hospitals. The 2007 database presents statistics across a large number of hospitals and respondents to enable hospitals to compare their results, and provides general conclusions about patient safety culture results across hospitals, and by staff positions and work areas. Considerations for Choosing a Safety Climate Survey Instrument Barry Kitch, M.D., M.P.H., Eric Campbell, Ph.D. Presented by: Barry Kitch, M.D., M.P.H., Institute for Health Policy, Massachusetts General Hospital, 50 Staniford Street, Boston, MA 02114, Phone: (617) 726-4201, Email: bkitch@partners.org Research Objective: Safety culture is important to patient safety and measurable. Yet numerous surveys have been developed in the absence of a clear consensus on required or desirable survey content or a gold standard against which to judge the performance of the instruments. To assist potential users we undertook a review of existing patient safety culture surveys and compared content (e.g. areas or dimensions of safety addressed), survey development, and other features of relevance to their use for quality improvement and research purposes. Study Design: Surveys were identified through a systematic review, which included a MEDLINE and Internet search, expert input, and review of references from relevant articles. We compared the content of surveys by assigning each item in each survey to the area or dimension of safety addressed by that item. For each instrument we also examined target populations, number of questions, reliability and validity testing, and availability of benchmarking. Population Studied: 13 instruments were selected for detailed review. Principal Findings: The instruments varied substantially in content, emphasis, and length. Individual surveys addressed as many as 19 dimensions of safety or as few as 4. While most of the surveys had substantial face validity, limited validation of the instruments by comparison with qualitative measures of patient safety culture, such as in depth interviews or observation, has been done, and little data exists on their ability to predict other existing patient safety outcomes or indicators. Conclusions: Available safety culture instruments vary substantially in content, emphasis, and length. Questions about which dimensions a safety culture survey should include as well as how best to analyze and interpret results remain. Implications for Policy, Delivery or Practice: In choosing an instrument potential users need to be aware of substantial differences between surveys; selection should depend on the intended use, target population, desire for benchmarking, and specific areas of safety that one would like to assess as well as an appreciation for differences across instruments in the rigor and transparency of the development process. An awareness of the differences between the instruments, as well as their collective limitations, should facilitate the process of assessing safety culture and underscores the need for further research. Funding Source(s): AHRQ Safety Culture at Work: Assessing & Improving J. Bryan Sexton, Ph.D., Peter Pronovost, M.D., Ph.D., Eric Thomas, M.D., Martin Makary, M.D. Presented by: J. Bryan Sexton, Ph.D., Assistant Professor, Johns Hopkins Quality and Safety Research Group, Department of Anesthesiology and Critical Care Medicine, The Johns Hopkins University School of Medicine, 1909 Thames, Suite 200, Baltimore, MD 21231, Phone: (443) 287-2274, Fax: (410) 502-3235, Email: sexton@jhmi.edu Research Objective: Here we review 10 years of cross sectional and longitudinal administrations of the Safety Attitudes Questionnaire (SAQ), to elicit frontline caregiver assessments of safety culture. Only recently has research on safety culture in healthcare blossomed, after the Institute of Medicine*s recent suggestion that healthcare organizations improve their safety cultures. Despite the large and growing body of research in other high risk work settings, safety culture research in healthcare is still in the early stages. Early evidence demonstrates that safety culture can be measured, is linked to clinical and operational outcomes, and is improvable with structured interventions. Executives, managers and frontline clinician leaders in quality and safety have widely varying levels of familiarity and comfort with safety culture data, but there is increasing pressure from boards, quality improvement organizations, and the media to do something about the safety culture. Study Design: Using standard psychometric tests such as multi-level confirmatory factor analyses, ICCs, and Rwgs, we demonstrate that consensus assessments of frontline caregivers within a patient care area can be represented by SAQ scale score. Using multi-level structural equation modeling, we demonstrate the relationship between safety culture and clinical outcomes. Using paired samples t-tests, we demonstrate how safety culture at the care area level is responsive to interventions. Population Studied: This review includes 200 USA hospitals between 2004 and 2006, including teaching and non-teaching, urban and rural, and bed sizes ranging from fewer than 50 to over 800. Specific interventions at the care area/nursing unit level that were targeted to test for improvement in safety culture were the Comprehensive Unit-based Safety Program (CUSP), Executive WalkRounds, and Operating Room Briefings. Principal Findings: These three interventions are relatively popular despite a lack of robust evidence in how to implement and monitor them. There is evidence for teamwork and safety climate improving after implementing CUSP. Also, improvements in safety climate were associated with rigorously conducted Executive WalkRounds, while teamwork climate improvements were associated with rigorously conducted OR Briefings. Care areas with fewer than 40 caregivers generally improved more than their medium (40-80) and larger (over 80) counterparts. Many caregivers report that they are not aware of the intervention being implemented in their unit, and there was considerable ambiguity around use of terms like Executive WalkRounds vs., e.g., Safety Rounds. Conclusions: Quality and safety interventions are often implemented without committing to the methodological rigor needed to demonstrate impact. However, when methodological rigor is utilized, the association between interventions and safety culture can be evaluated. Implications for Policy, Delivery or Practice: Given the limited quality and safety resources available to most hospitals and the limited attention afforded to quality by hospital leaders, changes to care delivery processes and structures need to be contingent upon evidence of positive impact, rather than the justification that it needs to be done because it is for quality. There is great promise of safety culture research to inform this evidence and provide actionable information relevant to implementing innovations in healthcare, and tracking the impact of those interventions over time. Call for Panels Lessons from the VA on Patient Safety: From Research to Policy & Practice Implications Chair: Amy Rosen, Ph.D. Sunday, June 3 • 5:00 p.m.-6:30 p.m. Panel Overview: The purpose of this panel is to highlight recent findings on patient safety from the Veterans Administration (VA) that impact both policy and practice. The VA is considered a national leader in patient safety, with numerous initiatives including medication bar coding, computerized physician order entry, and nationwide incident reporting systems. Yet, little is known as to whether these system-wide activities have resulted in improvements in care delivery, patient outcomes, and safety culture. We present results from several current research projects and initiatives in the VA in order to fill this evidence gap. Presentations are focused on: 1) current research priorities and activities of the VA National Center for Patient Safety: assessing their impact on VA policy and practice; 2) the change in resident work hours and its impact on quality and safety in the VA; 3) the variation in safety culture across VA facilities and differences in perceptions between job type and work areas: comparison to the non-VA setting; 4) racial disparities in rates of Patient Safety Indicators (PSIs) across the VA: comparison to the non-VA setting; and 5) processes and structures of care from site visits to low- and high-performing facilities on PSI rates: organizational themes and implications for best safety practices. Efforts to Achieve a Culture of Safety in the Veterans Health Administration Edward Dunn, M.D., M.P.H. Presented by: Edward Dunn, M.D., M.P.H., Director of Policy and Clinical Affairs, VA National Center for Patient Safety, Department of Veterans Affairs, 24 Frank Lloyd Wright Drive, PO Box 486, Ann Arbor, MI 48106-0486, Phone: (734) 930-5872, Fax: (734) 945-0199, Email: Edward.Dunn@va.gov Research Objective: To evaluate the effectiveness of policy changes and national programs designed to enhance patient safety culture across the Veterans Health Administration. Study Design: Before/after analyses of patient safety culture from surveys performed in 2000 and 2005, and descriptive analyses of rationale for pursuing identified interventions in an effort to achieve a culture of safety. Population Studied: Employees of the Veterans Health Administration. Principal Findings: The VA National Center for Patient Safety (NCPS) is guided by a mission of preventing harm to patients. Toward that end, NCPS has established a structure of Patient Safety Managers in 154 VA medical centers and Patient Safety Officers in the 21 VA networks who facilitate program implementation throughout the Veterans Health Administration. NCPS has pursed a multi-pronged strategy to improve the culture of safety within the VA system that includes implementation of patient safety training, patient safety toolkits, medical team training, alerts and advisories, and VA directives. Over the time period examined, measures of patient safety culture have improved in some areas, but have not changed in other areas. Conclusions: The NCPS has made progress in improving a culture of safety within the Veterans Health Administration. Culture is likely to change slowly, so repeat surveys are warranted. Implications for Policy, Delivery or Practice: Future efforts to enhance patient safety culture should target areas where the greatest need for improvement has been identified. Ongoing, regular collection and analysis of patient safety culture can be an effective strategy to identify areas for improvement and monitor progress toward achieving a culture of safety. Funding Source(s): VA Safety Culture in VA Hospitals Priti Shokeen, M.S., Amy Rosen, Ph.D., Shibei Zhao, M.P.H., Mark Meterko, Ph.D., Alyson Falwell, M.P.H., David Gaba, M.D. Presented by: Priti Shokeen, M.S., Health Science Specialist, Center for Health Quality Outcomes and Economic Research, Department of Veterans Affaris - Edith Nourse Rogers Memorial Veterans Hospital, 200 Springs Road (152), Bedford, MA 01730, Phone: (781) 687-3258, Fax: (781) 687-3106, Email: ptrivedi@bu.edu Research Objective: A culture of safety is recognized as a key to reducing adverse events in hospitals. The perceived safety culture may vary within institutions, with potential implications for efforts to improve safety culture. Although the VA (Veterans Administration) is a national leader in patient safety, little is known about the current safety culture in VA hospitals. This study explores the strength and uniformity of safety culture within VA hospitals and compares safety culture between VA and non-VA hospitals. Study Design: We measured safety climate using the Patient Safety Climate in Healthcare Organizations (PSCHO) survey, administered to employees at a nationwide sample of 29 VA hospitals between December 2005 and June 2006. The PSCHO consists of 42 Likert-scale questions and six demographic questions. For each question, a "problematic response" (PR) suggests a weak safety climate. We calculated average percent PR rates and 95% confidence intervals (CIs), accounting for sample proportion and patterns of non-response for each question, job-type, and work area across VA hospitals. A lower percent PR represents a stronger safety climate. T-tests were performed to check for significance between job-types and work areas. We compared results to 105 non-VA hospitals that administered the PSCHO survey during 2004. Population Studied: At each hospital, 100% of hospital-based physicians, 100% senior managers, defined as department heads and above, and 10% random sample of all other personnel were surveyed. At 10 hospitals, we surveyed 100% staff whose primary location of work was a high-hazard unit. Principal Findings: The overall response rate was 49% (4,504 individual responses) and the average overall PR rate across all hospitals was 18.1%; this rate was similar to the private sector (17.3%). Rates of PR varied widely across institutions and by questions. The items eliciting the highest and lowest PR rate were ‘‘My unit recognizes individual safety achievement through rewards and incentives’’ (49.6%) and ‘‘If I make a mistake that has significant consequences and nobody notices, I do not tell anyone about it,’’ respectively (4.4%). Senior managers had a significantly lower PR rate compared to supervisors, frontline staff, and physicians. Nurses had the highest PR rates of any job-type (CI=17.0%-24.7%). Employees in high-hazard units had a higher PR rate (22.6%) than other employees (17.6%). In general, our results are comparable to non-VA hospitals. Conclusions: Both strength and uniformity of safety culture are important in assessing hospitals’ commitment to patient safety. Consistent with the private sector, we found that a) perceptions of safety culture differed among hospitals, job-type, and work area, b) senior managers have a more positive perception of safety culture than frontline staff, and c) employees working in high-hazard areas have a more negative perception of safety culture. Implications for Policy, Delivery or Practice: Despite the positive overall perception of safety culture among VA employees, variation in problematic response warrants further investigation. Efforts to create a uniform safety culture within an institution are necessary to improve patient safety. Activities that reduce differences in perceptions between senior managers and frontline workers, as well as those that focus on high-hazard units, are critical to enhancing efforts to improve safety throughout an organization. Funding Source(s): VA Racial Disparities in Patient Safety Indicator (PSI) Rates in the Veterans Health Administration Stephanie Shimada, Ph.D., Maria Montez-Rath, M.S., Susan Loveland, M.A.T., Shibei Zhao, M.P.H., Nancy Kressin, Ph.D., Amy Rosen, Ph.D. Presented by: Stephanie Shimada, Ph.D., Postdoctoral Health Services Research Fellow, Center for Health Quality Outcomes and Economic Research, Department of Veterans Affaris, 200 Springs Road (152), Bedford, MA 01730, Phone: (781) 687-2000 x6698, Fax: (781) 687-3106, Email: shimada@bu.edu Research Objective: Minorities often experience reduced access to care, poorer quality of care, and worse outcomes. Recent findings from AHRQ using data from the Healthcare Cost and Utilization Project (HCUP), a national sample of inpatient discharges, suggest that there are some disparities in Patient Safety Indicator (PSI) rates between whites and ethnic minorities. However, there is evidence within VA that quality of care does not differ by race and may even be better for minorities because there are fewer financial barriers to access compared with other healthcare systems. We examined whether there are racial/ethnic disparities in the incidence of AHRQ’s Patient Safety Indicators (PSIs) within VA. Study Design: We utilized FY2000 ---- FY2005 inpatient discharge data from 128 acute-care VA hospitals (N=2,281,286 hospitalizations) to calculate PSI events and obtain data on patient characteristics. We then supplemented inpatient race with data from the VA outpatient files to lower the overall rate of missing race to 3.6%. To determine whether race was significantly associated with the likelihood of a PSI event, we ran logistic regression models for fifteen PSIs, controlling for patient age, gender, and comorbidities, adjusting for clustering at the hospital level. Patients were excluded from the analyses if they had missing inpatient race data (3.4 - 4.9% of hospitalizations, depending on the PSI). Population Studied: Veterans who received inpatient care at one of 128 acute-care hospitals in the Veterans Health Administration between FY2000 and FY2005 (N=93,488 ---- 2,281,252 hospitalizations, depending on the PSI). Principal Findings: The odds of decubitus ulcer (OR=1.35, 95%CI [1.20,1.53]) and postoperative pulmonary embolism and deep vein thrombosis (PE/DVT) (OR=1.23, 95%CI [1.13,1.34]) were higher for African-Americans than for whites. In contrast, African-Americans had significantly lower odds than whites for 3 PSIs: complications of anesthesia (OR=0.63, 95%CI [0.44,0.91]), postoperative wound dehiscence (OR=0.71, 95%CI [0.53,0.97]), and accidental puncture/laceration (OR=0.69, 95%CI [0.56,0.84]). Latinos also had significantly higher odds of decubitus ulcer (OR=1.60, 95%CI [1.02,2.50]) but had significantly lower odds of postoperative hemorrhage/hematoma (OR=0.73, 95%CI [0.55,0.97]) compared with whites. No significant racial/ethnic differences were found for the remaining 9 PSIs. Conclusions: The risk of PSI events varied across racial/ethnic subgroups. Many PSIs showed no significant differences across race/ethnicity; the differences found showed that minorities were at higher risk for some patient safety events and at lower risk for others. However, two high-frequency PSI events (decubitus ulcer and postoperative PE/DVT) were more likely to occur in minorities. Implications for Policy, Delivery or Practice: We found fewer differences between ethnic minorities and whites in PSI rates than have been documented in non-VA settings. However, because decubitus ulcer and postoperative PE/DVT are high-frequency adverse events, quality improvement initiatives targeting these conditions, in addition to research exploring the pathways leading to these disparities, should be initiated within the VA. Future research should examine patient- and hospital-level factors that might explain variation in PSI events within the VA and between the VA and non-VA settings. Funding Source(s): VA Moving Patient Safety Improvement Practices to the Next Level: Closing the Organizational Learning Loop Peter Rivard, Ph.D., Victoria Parker, D.B.A., Amy Rosen, Ph.D. Presented by: Peter Rivard, Ph.D., Postdoctoral Fellow, Center for Organization, Leadership and Management Research, Department of Veterans Affairs - VA Boston Healthcare System, 150 South Huntington Avenue (152M), Boston, MA 02130, Phone: (857) 364-5691, Fax: (857) 3544438, Email: rivardp@bu.edu Research Objective: The Veterans Health Administration (VA) is recognized for its initiatives to improve patient safety. Many such initiatives follow the quality-improvement organizational learning model: planning and implementation of safety improvements is driven by collection and analysis of data from within the organization. Examples include adverse event reporting, Root Cause Analyses (RCA) and Healthcare Failure Mode Effects Analyses (HFMEA). The purpose of this study was to identify variation in implementation of patient safety improvement practices between facilities with higher and lower patient safety performance. Study Design: Our research entailed exploratory case studies of four VA acute care hospitals. The sites were selected for their (a) high and low performance on a proxy for patient safety outcomes, and (b) geographic diversity. Safety performance was approximated by the AHRQ Patient Safety Indicators (PSIs), which use administrative data to identify potentially preventable adverse events in acute inpatient care. A subset of PSIs was applied to Fiscal Year 2001-2004 VA discharge data to generate a composite ranking of facilities. At the selected sites, data on safety improvement structures and practices were obtained through face-to-face semi-structured interviews conducted in 2005 with executives, managers, and others involved in patient safety improvement. Interviewers and interviewees were blinded as to facility safety performance on the PSIs. Data analysis explored facility-level variation in implementation of patient safety improvement. Interview transcripts were coded for both a priori constructs and emergent themes. Population Studied: VA facilities that provide acute inpatient care. Principal Findings: The two facilities with patient safety performance that was either better overall or more improved 2001-2004 showed evidence of organizational structures for patient safety learning and improvement that were more comprehensive on two dimensions: (1) Projectlevel evaluation: more follow-up assessment of specific patient safety interventions through monitoring of implementation success and measurement of changes in process and outcomes; (2) Program-level evaluation: more (a) executive-level assessment of the overall effectiveness of the patient safety program and (b) attention to integration across various patient safety initiatives. Our study describes these evaluation practices and presents exemplars. Conclusions: While organizational safety learning practices such as RCAs and HFMEAs help to elevate organizational response to safety problems from first-order ‘‘quick fixes’’ and workarounds to more effective second-order system improvement, this study suggests that higher-performing facilities then progress to a higher order of organizational learning, where they systematically assess the effectiveness and efficiency of their interventions. This is consistent with findings from implementation research: organizations with systems to monitor implementation of innovations and evaluate their impact are more likely to assimilate and sustain the innovation. Implications for Policy, Delivery or Practice: Further research should test the propositions generated by this study, i.e., that a next level of patient safety improvement, after implementation of focused system improvement practices such as event reporting and RCA, consists of systematic assessment of the effectiveness of these interventions, along with steps to prioritize, coordinate and integrate safety improvement initiatives across the facility. Furthermore, our findings suggest that an organization’s progress to this level may not be automatic and may require additional intervention. Funding Source(s): VA The Impact of the ACGME Duty Hour Rules on PSI Rates in VA Hospitals Kevin Volpp, M.D., Ph.D., Amy K Rosen, Ph.D., Paul R. Rosenbaum, Ph.D., Patrick Romano, M.D., Orit Even-Shoshan, M.S., Anne Canamucio, M.S., Susan Loveland, Jeffrey H. Silber, M.D., Ph.D. Presented by: Kevin Volpp, M.D., Ph.D., Staff Physician and Assistant Professor, CHERP Center for Health Equity Research and Promotion, Philadelphia VA Medical Center CHERP, (University of Pennsylvania School of Medicine and the Wharton School), 1232 Blockley Hall, Philadelphia, PA 19104-6021, Phone: (215) 573-0270, Fax: (215) 573-8778, Email: volpp70@mail.med.upenn.edu Research Objective: In response to concern about deaths in American hospitals from medical errors, the Accreditation Council for Graduate Medical Education (ACGME) released rules effective July 1, 2003 that restricted duty hours for all ACGMEaccredited residency programs. The objective of this study was to determine the impact of the duty hour regulations, one of the largest interventions ever undertaken to improve patient safety in teaching hospitals nationwide, on rates of Patient Safety Indicators (PSIs) in VA hospitals. We use one high-frequency wellvalidated PSI, the failure to rescue (FTR) rate (death after surgical complications), to examine this question. As lower (better) FTR rates are generally believed to be associated with early detection of complications, more rested residents may recognize and respond to complications more rapidly, thus reducing FTR. However, more handoffs may also create situations in which residents do not know the patients they cover as well as in the past, thereby lengthening the time before intervention after complications and possibly worsening FTR rates. Study Design: Observational study using interrupted time series analysis with data from July 1, 2000 - June 30, 2005. Logistic regression was used to examine the change in the FTR rate for patients in more versus less teaching-intensive hospitals before and after duty hour reform, adjusting for patient comorbidities, common time trends, and hospital site. Data were obtained from the VA Patient Treatment hospital discharge file, the VA Beneficiary Identification and Record Locator Subsystem file, and the VA Office of Academic Affiliations. Population Studied: All unique patients (n=66,456) admitted to acute-care VA hospitals from July 1, 2000 to June 30, 2005 with complications from general, orthopedic or vascular surgery. Principal Findings: There were no significant relative changes in the FTR rate for patients who suffered complications from general surgery, orthopedic surgery or vascular surgery in either post reform year 1 or 2. Combining the 3 groups of patients to form a ‘combined surgery group’ did not result in significant relative change in the FTR rate in either post-reform year 1 (OR 0.87, 95% CI [0.66, 1.15]) or post-reform year 2 (OR 0.88, 95% CI [0.66, 1.17]). Finally, combining both years of post data also indicated no significant relative change in the FTR rate (OR 0.87, 95% CI [0.70, 1.09]). Conclusions: The ACGME duty hour regulations were not associated with significant changes in the FTR rate for patients in VA hospitals. Implications for Policy, Delivery, or Practice: We found no statistically significant indication that the new duty hour standard harmed or helped surgical patients after developing complications. In contrast, our earlier work indicated that for some medical conditions, there were significant reductions in mortality post-reform. A single duty hour standard may affect trainees in different specialties differently, and further research is needed to better understand why there are differences in the impact of duty hour reform on medical vs. surgical patients. Primary Funding Source: VA Call for Panels Emerging Findings in Public Health Systems Research Chair: Kate Papa, M.P.H. Sunday, June 3 • 5:00 p.m.-6:30 p.m. Panel Overview: The tragedy of 9-11 exposed the long-neglected public health infrastructure in the United States. Bioterrorism threats that followed, along with a series of natural disasters such as the hurricanes of 2004 and 2005 that devastated parts of Florida and the Gulf Coast, have further underscored the inadequacies of public health systems at all levels of government. The emerging field of Public Health Systems Research (PHSR) is responding by growing the evidence base and investigating the public health system at many levels. This field of inquiry examines the organization, financing, performance, and impact of health systems ---defined as the constellation of governmental and non-governmental actors that influence population health, including health care providers, insurers, purchasers, public health agencies, community-based organizations, and entities that operate outside the traditional sphere of health care. This panel will present findings from four projects funded under the Robert Wood Johnson Foundation’s Special Topic Solicitation in PHSR funded through the Changes in Health Care Financing and Organization (HCFO) initiative. The first study explores the definition of measurement of the value of services provided by governmental public health systems and explores alternative methodologies for measuring value. The second study examines local public health service delivery in small jurisdictions. The third study examines regionalization in public health systems, examining differences in development and performance. Finally, the last study examines the relationships between spending and outcomes. Together, these papers will provide a comprehensive snapshot of public health systems, the expectations of these systems, and their effect on preparedness and health outcomes. Causes and Consequences of Change in Local Public Health Spending Glen P. Mays, Ph.D., M.P.H. Presented by: Glen P. Mays, Ph.D., M.P.H., Associate Professor, Chair Pro Tem, Department of Health Policy and Management, Fay W. Boozman College of Public Health, University of Arkansas for Medical Sciences, 4301 W. Markham, #820, Little Rock, AZ 72205, Phone: (501) 526-6647, Email: gpmays@uams.edu Research Objective: A growing body of evidence indicates that the availability and quality of public health services varies widely across communities, but relatively little is known about the factors that give rise to this variation. Public health activities in the U.S. are supported through a patchwork of funding streams that vary considerably across communities and change over time in response to economic and policy shifts. This variability in spending may have important consequences for community health. The objectives of this analysis are to: (1) examine how local public health spending levels and funding sources changed over the past decade; (2) identify the types of communities most likely to experience disparities in public health spending; and (3) determine whether changes in public health spending are associated with changes in community health status and disease burden. Study Design: A longitudinal cohort design is used to analyze changes in spending patterns and population health within service areas of the nation’s 3000 local public health agencies between 1993 and 2005. The National Association of County and City Health Officials (NACCHO) collected data on the organizational and financial characteristics of these agencies through census surveys fielded in 1993, 1997, and 2005. We linked these data with contemporaneous information on community characteristics, federal and state spending, and public health disease burden from other data sources. Multivariate regression models for panel data are estimated to test for changes in spending patterns over time and differences across communities defined by demographic, economic, organizational and geographic characteristics. Instrumental-variables methods are used to identify associations between spending levels and community health while controlling for unmeasured factors that jointly influence spending and health. Population Studied: The study includes all U.S. agencies meeting NACCHO’s definition of a local health department: an administrative or service unit of a local or state government that has responsibility for the health of a jurisdiction smaller than a state. There were 2875 such agencies in 1993 (response rate 77%) and 2864 in 2005 (response rate 80%). Principal Findings: Local public health agency spending increased from a median of $20 per capita in 1993 to $29 in 2005 in nominal dollars, indicating an annual growth rate of less than 4 percent. More than 20% of agencies experienced reductions in per capita spending. Larger increases in spending were observed among agencies serving metropolitan communities, agencies operating as units of local government, and agencies governed by local boards of health (p<0.01), even after adjusting for other agency and community differences. Increases in spending were associated with significant improvements (p<0.05) in several key measures of community health, including infant mortality and case rates for clamydia, gonorrhea, hepatitis, and tuberculosis. Instrumental-variables estimates indicate that even stronger relationships exist after accounting for unmeasured characteristics that jointly influence spending and health. Conclusions: Public health spending varies widely across U.S. communities, and this variability has persisted over time. Differences in spending may contribute to differences in community health outcomes. Implications for Policy, Delivery or Practice: Efforts to improve local public health resources and infrastructure may help to address important differences in health status across communities. Funding Source(s): RWJF Regionalization in Local Public Health Systems: Variation in Rationale, Implementation, and Impact on Public Health Preparedness Michael A. Stoto, Ph.D. Presented by: Michael A. Stoto, Ph.D., Professor of Health Services Administration and Population Health, Georgetown University School of Nursing & Health Studies, 3700 Reservoir Road, NW, Box 571107, Washington, DC 20057-1107, Phone: (202) 687-3292, Email: stotom@georgetown.edu Research Objective: The objective of this study is to provide a better understanding of the regionalization of public health systems in order to inform the many state and local health departments currently developing regional structures. Study Design: In order to learn from areas that have adopted a regional approach we have used comparative case studies to (1) document the variation in the rationale for creating regional public health structures; (2) understand how these structures have been organized, implemented, and governed; and (3) assess the current and likely impact on of regional structures on public health preparedness and public health systems more generally. Population Studied: Massachusetts, Northern Illinois, Nebraska, and the Washington D.C. National Capital Region. Principal Findings: The impetus for forming regions was some combination of the following: a crisis or perceived need for a coordinated response, a need to build local public health capacity, or an effort to use federal preparedness funds more efficiently. The relationship between public health regions and geopolitical jurisdictions in which they sit was complex. Some involve combinations of local health departments, and one set up new health departments for groups of counties. The National Capital Region has multiple definitions, including some that crossed state lines. The regions vary in terms of their congruence with regional structures for partner agencies such as emergency management agencies as well as hospital and health services markets and organizational structure. Some of the regions focus on building formal organizational relationships to coordinate and sometimes standardize preparedness and response activities, and sometimes build regional capacity, while others focused on building informal professional networks. It is not clear which approach will have the largest effect on building social capital. Whatever the approach is chosen, however, it is clear that strong leadership and trust are required for effective planning, emergency response, and sustainability. Conclusions: Does regionalization improve emergency preparedness? Logically, regionalization allows for more efficient use of resources and since disease outbreaks do not respect geopolitical boundaries coordination is needed. The case studies demonstrated progress in terms of planning and coordination; memoranda of understanding; regional capacitybuilding, training, and exercises; and development of professional networks. The case studies also showed effects in terms of the public health response to the flu vaccine shortage in 2004 and anthrax and tularemia alarms in the National Capital Area in 2005. Does regionalization improve public health generally? Logically, the same arguments about sharing resources and coordinated response apply. Also, the case studies identify a number of areas where regional capacities address other needs. It seems likely that preparedness concerns are forcing communities to think about public health structures in a way that has not been done in decades, and that network development may be creating social capital that helps with other concerns. But concerns that preparedness efforts were drawing resources and attention from other areas of public health were also heard. Implications for Policy, Delivery or Practice: Most states have responded to the increased interest in and funding for public health preparedness by setting up regional structures, but the rationale for these structures, the way they are implemented, and presumably the impact of this organizational change vary considerably. As states receive this increase in funding, they will be under increased pressure to demonstrate accountability. These findings will inform states and communities as they develop rationale for such regionalized strictures. Funding Source(s): RWJF Measuring the Value of Public Health Services Peter D. Jacobson, J.D., M.P.H. Presented by: Peter D. Jacobson, J.D., M.P.H., Professor of Health Law and Policy, Director, Center for Law, Ethics, and Health, University of Michigan School of Public Health, 109 Observatory, Ann Arbor, MI 48109-2029, Email: pdj@umich.edu Research Objective: 1) To understand how the value of the services provided by governmental public health systems (GPHSs) can be defined and measured. 2) To determine what methodologies (e.g., contingent valuation, cost-benefit or costeffectiveness analyses) can be used to measure value. 3) To develop an analytical framework for measuring the value of GPHSs. Study Design: First, we conducted a critical synthesis of the literature to: 1) review the methodological literature to examine how various methodologies have been applied to similar efforts (such as disease prevention); 2) examine how other systems (public and private) define and measure the value of their services; and 3) assess general applicability of the literature to the public health system. Second, we interviewed key national, state, and local public health practitioners, policymakers, and elected officials to ascertain participants’ views of how the public health system can define and measure value, as well as the feasibility of doing so. Altogether we conducted more than 40 interviews, including practitioners in three states. Third, we conducted an extensive search for and analysis of economic evaluations of GPHS activities to: identify key gaps in the data; critically evaluate each of the methodologies used to value public health services; and investigate alternative ways for quantitatively measuring the value of GPHS services. Population Studied: The populations studied are national, state, and local public health practitioners. Principal Findings: 1) Despite a large number of articles across different fields, very few focus on the relevant concept of value. Most articles did not explicitly define or outline how value was measured. 2) Limited research on measuring value in related fields. 3) Interview results:Very few current attempts to formally define and measure value; Promising cost accounting-deliberative democracy strategy; Disagreement on the merits of focusing on preventing disease as the measure of value; Limited data available; Criteria emerged to develop a framework for defining and measuring value; Interviews suggest the importance of communication in thinking about value. 4) Methodological results: Several approaches have been used to value public health and prevention strategies, including willingness to pay (contingent valuation), human capital, quality-adjusted life years (QALYs), life-years gained, rate of return on investment, and the use of ‘‘natural’’ health units; None emerged as an optimal method for measuring value; Despite the large number of studies, there are notable variations in the quality and completeness of the literature. Conclusions: We conclude that a framework for analysis can offer ways for GPHSs to define and communicate the value of public health services to various constituencies. Public health practitioners will need to use a combination of methods to measure value. Implications for Policy, Delivery or Practice: It is essential that GPHSs allocate resources to those activities likely to achieve maximum value for improving the public's health. The framework we have developed is the first step toward enabling public health practitioners, policymakers, and elected officials to explain the overall benefits of GPHS to the public. Funding Source(s): RWJF Structural Capacities, Processes, and Performance of Essential Public Health Services by Small Local Public Health Systems Susan Zahner, Dr.P.H., M.P.H., R.N. Presented by: Susan Zahner, Dr.P.H., M.P.H., R.N., Associate Professor, School of Nursing, University of Wisconsin-Madison, H6/246 Clinical Sciences Center, 600 Highland Avenue, Madison, WI 53792-2455, Phone: (608) 263-5282, Email: sjzahner@wisc.edu Research Objective: Contemporary local public health service delivery is conceptualized as being provided by a local public health system that includes, but is not limited to, the local health department. Studies of the performance of local public health systems are limited although research has demonstrated a relationship between local health department size and performance. This study is being conducted to examine the capacities, processes, and performance of local public health systems serving small jurisdictions (under 25,000 population). Study Design: The study is being conducted in two phases. Phase 1 included qualitative, on-site interviews with key informants (n=37) from organizations included in four small, local public health systems. Phase 2 includes survey instrument development and data collection from 34 small local public health systems. Population Studied: Small, local public health agencies in Wisconsin. Principal Findings: Phase 1 results will be summarized and presented. Progress to date in survey instrument development, sample determination, data collection, and analysis plans will be shared. Conclusions: Study methods used may contribute to the development of public health system performance research methodologies particularly in evaluating the organization, financing, and delivery of public health services and in measuring evidence about the effectiveness of public health services and interventions. Implications for Policy, Delivery or Practice: Study findings may be useful to policymakers and administrators in targeting resources and technical assistance in building structural capacities in key areas associated with public health system performance. Funding Source(s): RWJF composite measures of patient experience, in different types of hospitalization, on overall rating of hospital. To ensure that comparisons across hospitals are fair and valid, CMS implemented a randomized experiment to measure and adjust for the effects of survey mode. The third presentation offers new empirical findings from this mode experiment. A full-scale dry run of HCAHPS conducted in 2006 in over 2800 hospitals resulted in key lessons learned in survey implementation and data submission, the topic of the fourth presentation. The fifth presentation examines public reporting of HCAHPS results. Fresh results from consumer testing of the Hospital Compare website are offered, including preferred options for coherently integrating the patient perspective, clinical and mortality elements of the website. Developing and Implementing HCAHPS, the First National, Standardized, Publicly Reported Survey of Patients' Perspectives of Hospital Care William Lehrman, Ph.D., Elizabeth Goldstein, Ph.D. Call for Panels Designing, Collecting, Analyzing and Publicly Reporting Patient Assessments of the Quality of Hospital Care: The HCAHPS Survey Chair: William Lehrman, Ph.D. Presented by: William Lehrman, Ph.D., Health Insurance Specialist, Center for Beneficiary Choices, Centers for Medicare & Medicad Services, S1-13-05, 7500 Security Boulevad, Baltimore, MD 21244-1850, Phone: (410) 7861037, Fax: (410) 786-8004, Email: william.lehrman@cms.hhs.gov Monday, June 4 • 9:00 a.m.-10:30 a.m. Panel Overview: The first national, standardized survey of hospital patients' perspectives of care was launched by Centers for Medicare & Medicaid Services (CMS) in October 2006. The CAHPS® Hospital Survey (HCAHPS) produces hospital-level information on quality of care for public reporting. Beginning in July 2007, HCAHPS will become an ingredient in ‘‘pay-forreporting’’ with the potential to affect billions of dollars of CMS payments to hospitals. HCAHPS will have a direct impact on patient choice, consumer information, public perception, and public policy. This panel describes the development and scope of HCAHPS and presents new empirical findings. The first presentation provides an overview of the purpose, composition, development, and evolving scope of HCAHPS. Drawing on data collected from 50,000 patients in the HCAHPS pilot study, the second presentation examines the differential impact of the survey’s seven Research Objective: This presentation introduces and explores the newly launched CAHPS® Hospital Survey, also known as HCAHPS: the first national, standardized, publicly reported survey of patients' perspectives of their hospital care. HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems) unites patient-centered care with public reporting of hospital quality information. It is intended to augment consumer choice, increase hospital accountability, provide incentives for quality improvement, and add greater transparency, all through the public reporting of meaningful, valid and standardized quality measures. Study Design: After years of development and testing, HCAHPS was launched by CMS in October 2006. HCAHPS was developed to produce comparable hospital-level information for public reporting purposes. Currently, over 2800 acute care hospitals, and hundreds of thousands of patients, are voluntarily participating. However, beginning in July 2007, HCAHPS will become an ingredient in ‘‘pay-forreporting’’ with the potential to affect billions of dollars of CMS payments to hospitals. By mid2007, nearly all eligible hospitals (~4000) are expected to participate. The first public reporting of hospital results should attract wide attention from the healthcare industry and the general public. This presentation will provide the most up to date information on the content, development and scope of HCAHPS. Content and Implementation We present information on HCAHPS’ content (seven areas of vital importance to patients are tapped through 27 items: 18 on experience of care; five demographic; four screeners), participating hospitals (‘‘general,’’ acute-care), eligible patients (adult; alive; overnight stay; discharged; medical, surgical or maternity care), the process and options for implementation (by hospitals or approved survey vendors; four survey modes; standardized protocols; 300 completed surveys per year), how results will be publicly reported (on the Hospital Compare website; integrated with clinical and mortality measures), and how oversight will be conducted. The second part of the presentation discusses the process of developing, testing and refining the survey, from its inception in 2002 to its current form. The purpose of the survey has evolved from the original goal of public reporting, to encompass pay for reporting, and eventually pay for performance. HCAHPS has been developed in a open and participatory manner, which included several opportunities for public scrutiny and comment, independent reviews and endorsements. We will discuss how interests of key stakeholders, particularly hospitals, survey vendors and consumer groups, have been accommodated to the degree possible while maintaining fidelity to original goals. Finally, the impact of HCAHPS on patients, consumers, hospitals, and the healthcare industry will be broached. Because its full impact will not be apparent for some time, we will invite the audience to speculate on possible outcomes, consequences, and avenues for research. Conclusions: By offering new information to consumers and encouraging hospitals to improve the care they provide, HCAHPS will have a significant and direct impact on patient choice, consumer information, public perception, and public policy. This presentation will also provide context and background for other presentations on HCAHPS. Implications for Policy, Delivery or Practice: HCAHPS is the result of a fresh approach to quality improvement, will produce valuable, new publicly reported information, and promises to be a catalyst for change. Funding Source(s): CMS Components of Care Vary in Importance for Overall Patient-Reported Experience by Type of Hospitalization in the HCAHPS Survey Marc Elliot, Ph.D., David Kanouse, Ph.D., Carol Edwards, Lee Hilborne, M.P.H., M.D. Presented by: Marc Elliot, Ph.D., Senior Statistician, RAND Corp., PO Box 2138, 1776 Main Street, Santa Monica, CA 90407-2138, Phone: (310) 393-0411, Email: elliot@rand.org Research Objective: To determine whether the contributions of composite measures of patient experience to overall hospital ratings on the HCAHPS Survey (also known as the CAHPS® Hospital Survey) vary by type of hospitalization. Study Design: We defined 24 hospitalization types using a combination of major diagnostic category and service line (medical, surgical, or obstetrical), pooling across categories when necessary to achieve adequate sample size (n > 180). We examined seven composite measures of patient experience: Doctor Communication with Patients, Nurse Communication with Patients, Staff Responsiveness to Patients’ Needs, Room Clean and Quiet, New Medicines Explained, Pain Control, and Post-Discharge Information. To assess the importance of each composite for each type of hospitalization, we calculated simultaneous partial correlations between composite scores and an overall hospital rating, controlling for patient demographics. Population Studied: 49,812 English- or Spanishspeaking adult patients with non-psychiatric primary diagnoses discharged to home between December 2002 and January 2003 after an inpatient admission lasting at least one day in 132 general acute care hospitals in three states. Principal Findings: Nurse communication was the most important composite overall, with an average partial correlation of 0.34 (range 0.170.49); it was statistically significant (p<0.005) and among the three largest partial correlations for all 24 hospitalization types. Discharge information was the least important overall, with an average partial correlation of 0.05 that was statistically significant for only 10 of 24 types (p<0.05) and among the three most important for only one (r=0.16). Partial F-tests of interactions found significant (p<0.05) variation in partial correlations by hospitalization type for 5 of 7 composites, with the largest variations observed for Nurse Communication, Doctor Communication, and Pain Control (F >2, p<0.005). For example, for Kidney/Urinary Surgery, New Medicines, Pain Control, and Nurse Communication were most important (in that order), whereas for infectious disease hospitalizations, such as tuberculosis, Nurse Communication was much more important than the next two (Pain Control and Discharge). Doctor Communication was most important for non-surgical stays for metabolic disorders; Pain Control was most important for ENT hospitalizations. Conclusions: After controlling for patient demographics and other aspects of care, Nurse Communication is important to overall patient experience for all types of hospitalizations, but especially for some types; Responsiveness and Cleanliness/Quiet are uniformly of moderate importance; Doctor Communication and Pain matter for most types and are especially important for at least six of 24 hospitalization types; Medications and Discharge matter for half of 24 hospitalization types but are important only for a few. Implications for Policy, Delivery or Practice: Results have implications for measurement, reporting, and quality improvement efforts. Because some aspects of patient experience are relevant only for certain types of hospitalization, measuring those aspects for all types adds noise; quality measures might be improved by targeted administration or by restricting administration or scoring to relevant hospitalizations. Web-based reporting could highlight the most important composites for consumers who anticipate a particular hospitalization type. Finally, quality improvement efforts can be targeted to those aspects of patient experience that matter most for each type of hospitalization. Funding Source(s): AHRQ Findings from the HCAHPS Mode Experiment Marc Elliott, Ph.D., Elizabeth Goldstein, Ph.D., William G. Lehrman, Ph.D., Katrin Hambarsoomians, M.S., Laura A. Giordano, R.N., M.B.A., Mary Anne Hope, M.S. Presented by: Marc Elliott, Ph.D., Senior Statistician, RAND Corp., PO Box 2138, 1776 Main Street, Santa Monica, CA 90407-2138, Phone: (310) 393-0411, Email: elliott@rand.org Research Objective: To determine the effects of mode of survey administration on patient responses to the CAHPS® Hospital (HCAHPS) Survey. Study Design: Within each of 45 randomly sampled hospitals, a total of 27,229 patients were randomized in equal proportions to four modes of survey administration: Mail Only, Telephone Only, Mixed Mode (mail with telephone follow-up), or Active IVR (interactive voice response, in which patients respond via telephone keypads). These patients completed the HCAHPS (Hospital Consumer Assessment of Healthcare Plans and Systems) Survey, in which recently discharged patients evaluate aspects of their hospital care. All surveys were administered by a single vendor. Population Studied: English- or Spanishspeaking adult patients with non-psychiatric primary diagnoses discharged alive after at least one overnight stay in a general acute care US hospital with at least 1200 annual discharges. Principal Findings: The 9 HCAHPS outcomes consist of 2 overall ratings and 7 composites constructed from 16 report items. Linear regression was used to model each outcome from fixed effects for mode, hospital identifiers, and patient characteristics. Substantial and statistically significant (p<0.05) mode effects were found for both overall ratings and 4 of 7 composites (Cleanliness & Quiet, Responsiveness of Hospital Staff , Pain Management, and Discharge Information); mode effects were smaller for the 3 composites involving communication (with doctors, nurses, and about medications). Patients provided more positive evaluations in the Telephone Only and Active IVR modes than in the Mail Only and Mixed modes. Differences between Telephone Only and Active IVR responses were small, and there were very few differences in Mail Only and Mixed Mode responses. When measured in terms of hospital-level standard deviations, the Telephone Only and Active IVR scores for the 6 most affected outcomes noted above were at least 0.4-0.5 standard deviations higher and sometimes as much as 1 standard deviation higher than scores from Mail Only and Mixed modes. These mode effects varied little by hospital. Response rates varied strongly by randomized mode (p<0.0001), ranging from 41.2% for Mixed Mode to 20.7% for Active IVR; these patterns were consistent across hospitals. Conclusions: Because a hospital’s choice of vendor or survey mode may be confounded with factors related to underlying quality, an external mode experiment is necessary to estimate mode effects for subsequent fieldings of the survey. We conclude that adjustments for mode effects are necessary to make the reported HCAHPS scores comparable; in the absence of such adjustments a hospital that would have ranked at the 50th percentile in the Mail Only mode would be ranked at the 66th to 84th percentile in the Telephone Only mode for a majority of outcomes. More surveys must be fielded in the Active IVR mode than in the Mixed mode to achieve the target of 300 completed surveys per hospital. Implications for Policy, Delivery or Practice: CMS will employ adjustments derived from this experiment, in conjunction with adjustment for patient-level characteristics, that allow hospitals to administer the HCAHPS Survey in any of four modes without affecting the comparability of their scores with other hospitals, national or regional averages, or their own past performance. Funding Source(s): CMS Lessons Learned from the ‘Dry Run’ of the HCAHPS Survey Laura Giordano, R.N., M.B.A., Mary Anne Hope, M.S., Elizabeth Goldstein, Ph.D., William G. Lehrman, Ph.D. Presented by: Laura Giordano, R.N., M.B.A., Vice President, Surveys, Research & Analysis, Health Services Advisory Group, 1600 East Northern Avenue, Phoenix, AZ 85020-3983, Phone: (602) 665-6162, Email: lgiordano@azqio.sdps.org Research Objective: In preparation for national implementation of the CAHPS® Hospital Survey, also known as HCAHPS, a ‘‘Dry Run’’ for data collection and submission was conducted from April through June 2006. Careful analysis of the processes and procedures was then conducted. The primary purposes of the Dry Run were to provide an opportunity for all participating hospitals ("general," acute care) and approved survey vendors to establish and fully experience the data collection and submission processes. In addition, the Dry Run allowed the Centers for Medicare & Medicaid Services (CMS) to establish the final administrative protocols, in advance of full national implementation, which began on a voluntary basis in October 2006. The data collected for the Dry Run will, however, not be used for public reporting purposes. Study Design: The Dry Run provided an opportunity for hospitals and survey vendors to: select a mode of Survey administration; create a sample frame of eligible patient discharges; administer the Survey to the eligible patients; collect the data; create XML data files or use the online tool for data submission; and utilize the QualityNet system. In addition, the Dry Run provided an opportunity for CMS to: implement and test systems for Survey data storage and retrieval through the QualityNet Exchange system; collect and process Survey data; and develop and implement protocols for providing technical assistance. Population Studied: HCAHPS data were collected for all HCAHPS-eligible patients: English- or Spanish-speaking adults with nonpsychiatric primary diagnoses who were discharged alive after at least one overnight stay in a participating general acute care hospital. Over 2,800 hospitals, and tens of thousands of patients, participated in the Dry Run. Principal Findings: The primary issues encountered in the Dry Run included: the creation of XML format files for data submission; deployment of an HCAHPS on-line tool as an alternative method of data submission for smaller hospitals; unsuccessful data submissions; establishing correct accounts in the QualityNet Exchange data warehouse; and data coding questions. The Dry Run allowed hospitals, survey vendors and CMS to identify and resolve problematic issues before the national implementation, resulting in more efficient data collection and submission processes and improved data integrity. Conclusions: It is essential that a standardized process for data collection and submission be consistently applied by all hospitals and survey vendors participating in HCAHPS. Successful completion of a Dry Run by hospitals and survey vendors greatly improves the standardization of data collection and submission across hospitals, enhances the quality of the data, and provides a critical opportunity for all affected parties to gain valuable experience before HCAHPS results will be publicly reported or play a role in pay for reporting. The lessons learned by participating hospitals, survey vendors, the data warehouse and CMS have resulted in a smoother national implementation of the survey. Implications for Policy, Delivery or Practice: Successful completion of a Dry Run by hospitals and survey vendors will continue to be required prior to participation in HCAHPS. Funding Source(s): CMS Public Reporting HCAHPS in Context David Miranda, Ph.D., Jeanne McGee, Ph.D., Kristin Carman, Ph.D. Presented by: David Miranda, Ph.D., Social Science Research Analyst, Center for Beneficiary Choices, Centers for Medicare & Medicaid Services, S1-13-05, 7500 Security Boulevard, Baltimore, MD 21244-1850, Phone: (410) 7867819, Fax: (410) 786-8004, Email: david.miranda@cms.hhs.gov Research Objective: This presentation examines public reporting of the CAHPS® Hospital Survey, also known as HCAHPS (Hospital Consumer Assessment of Healthcare Providers and Systems), results and integration into a public website with performance information that includes clinical process and outcomes (30day mortality) measures as well. Prior research had indicated the importance of meeting the needs and concerns of both patients and physicians in hospital quality reports. Prior research also had indicated consumer interest in patient survey data. However, preliminary research on integrating HCAHPS into Hospital Compare found considerable difficulties that consumers have understanding the distinction between outcomes, process measures, and patient survey data, let alone combining and weighting the different types of data to fit their needs. The current study involved iterative rounds of qualitative research to design a website with accurate and useful information about hospitals that meets the needs of consumers, physicians, and other audiences including hospitals. Study Design: The research team conducted qualitative research in the form of three rounds of one-on-one interviews and focus groups with patients, their family members, physicians and hospital quality improvement personnel. Interactive web mockups of draft versions of HCAHPS information allows for both structured interviewing and unstructured browsing observed by the research team. Population Studied: People with Medicare, people with a hospitalization experience, consumers who help family members and friends make hospitalization decisions, physicians who refer to or practice in hospitals, hospital quality improvement personnel. Principal Findings: Creative design elements and careful use of drill-down and other navigation features allow for a successful integration of HCAHPS into a website tool with clinical process and outcomes data in a fashion that meets the needs of both physicians and consumers. Careful explanations allow consumers to understand the data well enough to play an active role in making informed hospital care decisions in consultation with their physician. To foster physician buy-in, detailed explanations of composite construction, case mix and mode adjustments, survey fielding and data collection and analysis processes help insure trust and confidence in the data. Conclusions: Creative use of language and design, in conjunction with iterative rounds of qualitative testing, contribute to the successful implementation of HCAHPS public reporting by clarifying and responding to needs of multiple audiences. Implications for Policy, Delivery or Practice: Application of textbook principles of web design cannot substitute for on-going audience testing research to insure that the public reporting meets its goals and objectives. Policy maker and researcher attention to multiple audiences and how they interact around publicly reported measures and the constructs they represent is needed. Funding Source(s): CMS Call for Panels Enhancing Research Through Collaborative Community-Higher Education Partnerships: Models of Community-Based Participatory Research Chair: Michelle Proser, M.P.P. Monday, June 4 • 9:00 a.m.-10:30 a.m. Panel Overview: National organizations, funding agencies, and researchers have called for a renewed focus on an approach to public health research that recognizes the importance of social, political, and economic systems to health behaviors and outcomes. This renewed focus is due to many converging factors, including increased understanding of the complex issues that affect health, the importance of both qualitative and quantitative research methods, and the need to translate the findings of basic, interventional, and applied research into changes in practice and policy. As a result, participatory models of research, in which communities are actively engaged in the research process through partnerships with academic institutions, have become central to the national prevention research agenda as articulated by the Institute of Medicine, the National Institutes of Health, the Centers for Disease Control and Prevention (CDC), Partnership for Prevention, the Public Health Foundation, and the WK Kellogg Foundation. Community-based participatory research (CBPR) can lead to healthier communities through collaborative solutions that bring communities and institutions together as equal partners and build upon the assets, strengths, and capacities of each. Communitycampus partnerships involve communities and higher educational institutions as partners, and may address such areas as health care delivery, research, health professions education, community-wide health improvement, community service, and community/economic development. This panel will describe CBPR, provide models and ‘‘how-tos’’ for establishing effective and sustainable community-academic partnerships, provide examples of CBPR projects, identify helpful resources, and discuss issues related to working with safety-net community-based organizations. A Review of Published Community-Based Participatory Research (CBPR) and Recommendations for Future Scholarly Work Darius Tandon, Ph.D., Eric B. Bass, M.D., M.P.H. Presented by: Darius Tandon, Ph.D., Assistant Professor, The Johns Hopkins University School of Medicine, 1620 McElderry Street, Rm. 203, Baltimore, MD 21205, Phone: (410) 614-5281, Fax: (410) 614-5431, Email: standon@jhmi.edu Research Objective: First, we describe the importance of, and examples of published research in, eight areas of scholarly activity that can promote health partnership research, education, and action: 1. original research, 2. works in progress and lessons learned, 3. policy and practice, 4. theory and methods, 5. education and training, 6. practical tools, 7. systematic reviews, and 8. community perspectives. Second, we provide recommendations on issues, problems, and topics within each area on which CBPR manuscripts submitted to peer-reviewed journals should focus. Study Design: We used a group judgment technique, Delphi Process, to elicit recommendations of expert leaders. During the first stage of the Delphi Process, the idea generation, we sent an open-ended questionnaire to the Associate Editors of a new journal dedicated to the work of community health partnerships, n equals 17, and asked them to provide specific recommendations on the most important issues, problems, or topics on which articles published in Progress in Community Health Partnerships, PCHP, should focus for each of the eight areas above. Recommendations were combined into specific themes in each of the eight areas. During the second stage of the Delphi Process, idea prioritization, we gave the themes and specific recommendations to PCHP’s diverse group of 17 external Editorial Board members, representing academic, governmental, and community perspectives, and asked them to check the topics that are the highest priority for articles in each of the eight areas of scholarly activity. Population Studied: We obtained responses from 17 Associate Editors and 12 Editorial Board members. Principal Findings: Stage 1 generated 318 recommendations across the 8 areas of scholarly activity; these recommendations were collapsed into 62 themes. Based on Stage 2, the most commonly rated priority for Original Research was translation of research into policy and practice. Building community partnerships and challenges in conducting CBPR were most often selected for Work-in-Progress/Lessons Learned. For Policy and Practice, engaging community members in policy/practice was most commonly selected. For Theory and Methods, research methods was most commonly selected. For Education and Training, CBPR curriculum and graduate medical education reform and training new investigators were most commonly selected. The highest priorities for Practical Tools were resources to develop community partners’ skills and to evaluate projects. The highest priorities for Systematic Reviews were reviews on CBPR methods and CBPR effectiveness. For Community Perspectives, the most commonly given priority was community members’ perspectives on research usefulness. Conclusions: The Delphi Process generated many specific recommendations, as well as priority areas, for future CBPR work. Academic and community partners should consider publishing work that can address these issues. Implications for Policy, Delivery or Practice: CBPR is an increasingly used approach for conducting health research. Using Rogers’ diffusion of innovations theory as a framework, future CBPR adoption will occur if CBPR is perceived to have greater relative advantage, compatibility, trialability, and observability, and less complexity than other research approaches. Future peer-reviewed publications, based on our study recommendations, can influence perceptions of CBPR that promote its adoption. Funding Source(s): W. K. Kellogg Foundation Conducting Research Using a CommunityBased Participatory Research Approach Kristine Wong Presented by: Kristine Wong, Program Director, Community-Campus Partnerships for Health, University of Washington, Box 354809, Seattle, WA 98195-4809, Phone: (206) 543-7954, Email: kristine@u.washington.edu Research Objective: This presentation will (1) review the principles of and logic behind community-based participatory research (CBPR), an emerging approach to research that increases rigor in a way that a traditional research approach may not; (2) provide models of CBPR activities in community-based health care settings as well as the continuum of such models; (3) provide tips on how to establish community-academic partnerships and how to develop research designs that will not only serve the community, but also increase the validity of the research through authentic community involvement; (4) discuss funding opportunities and resources available to assist with creating effective partnerships; and (5) demonstrate how studying community-based primary care and prevention at community health centers using a CBPR approach will improve the delivery of care, quality of care, and health outcomes for entire communities. Study Design: Community-Based Participatory Research (CBPR) is a ‘‘collaborative approach to research that equitably involves all partners in the research process and recognizes the unique strengths that each brings. CBPR begins with a research topic of importance to the community and has the aim of combining knowledge with action and achieving social change to improve health outcomes and eliminate health disparities.’’ (W. K. Kellogg Foundation) Population Studied: Community health centers (community-based, safety net ambulatory care providers that are run by patient-majority governing boards) and academics/researchers seeking to develop CBPR partnerships. Community health center governing boards, as well as community institutional review boards established by some health centers, play important roles in vetting researcher proposals. Principal Findings: CBPR benefits both partners. Not only does CBPR increase the rigor of research through authentic community involvement, but it also improves the health of patients and the community. Patient and community health improvement are achieved through improved delivery of care and health outcomes, reductions in health disparities, and enhanced community capacity for future research. Conclusions: Researchers who wish to successfully develop a CBPR study design may need to develop new approaches and perspectives towards working with communities and the providers who serve them. Such approaches are often detailed in community institutional review board procedures. Many foundations and government agencies are increasingly dedicating funding streams to this research approach, which will boost demand for collaborative partnerships with communities. A growing body of resources is available for those interested in learning more about CBPR. Implications for Policy, Delivery or Practice: CBPR provides communities with opportunities to decide what research questions are asked, contribute to research designs that have the best interests of their patients in mind, participate in data collection and analysis, and establish longterm relationships with researchers for future research. Researchers benefit from the inclusion of community expertise and gain opportunities to apply their expertise and skills for the greater good, fulfill personal values and beliefs, and cultivate external funding, as well as build a foundation for new areas of scholarship. Funding Source(s): WKK, NIH, CDC, Robert Wood Johnson, EPA Community-Based Participatory Research: Practical Tips for the Research Community Marshall Chin, M.D., M.P.H., Elbert S. Huang, M.D., M.P.H., MidWest Clinicians’ Network Team Presented by: Marshall Chin, M.D., M.P.H., Associate Professor of Medicine, Section of General Internal Medicine, University of Chicago, 5841 South Maryland Avenue, MC2007, Chicago, IL 60637, Phone: (773) 702-4769, Fax: (773) 8342238, Email: mchin@medicine.bsd.uchicago.edu Research Objective: Given from the ‘‘academic institution perspective,’’ this presentation is intended to provide examples of research strengthened through community-based participatory research (CBPR) and tips for creating effective partnerships with communitybased organizations. The presentation will highlight a major collaborative effort between the University of Chicago and a multi-state community health center network. The collaboration sought to evaluate the impact of a federally-supported chronic care initiative, known as the Health Disparities Collaboratives, on quality of care and outcomes for patients over the seven-year span of the initiative, and to determine ways to enhance the effectiveness, sustainability, and spread of the initiative. With the input of community members and providers, the project will help inform future efforts to improve chronic care management in health centers. Study Design: Between 2004 and 2005, investigators studied approximately 200 community health centers in the Midwest and West Central regions of the country. The study and analysis were done collaboratively with the community health centers involved. Investigators conducted chart review and patient surveys for performance indicators at a subset of 32 health centers. On the universe of 200 health centers, leaders and staff were surveyed to determine incentives and assistance that would be helpful in participating in the Health Disparities Collaboratives, and semi-structured interviews were performed on a sub-sample. Population Studied: This CBPR example studied low income community health center patients with chronic illness who were predominately uninsured or publicly insured. Principal Findings: Community-based providers have better understandings of the needs of the populations they serve, and the barriers to care they face. This presentation will provide recommendations for creating successful CBPR models, such as how to build relationships with the community, when and how to be flexible, working with senior management in community settings, how to create equal partnerships, what the research process should look like, and meeting the interests of various funders. Conclusions: The number of existing CBPR models is small but growing. CBPR opens doors to more research opportunities to study traditionally hard-to-reach populations, but requires the collaboration with the community from start to finish in order to ensure the research is rigorous, comprehensive, meets complex societal problems, and improves patient and community health. Implications for Policy, Delivery or Practice: Seamless partnerships between both academic and community researchers ensures that research is translated into practice or policy. Funding Source(s): AHRQ, Robert Wood Johnson Foundation, NIDDK Community-Based Participatory Research: Working with Community Health Centers Michelle Proser, M.P.P. Presented by: Michelle Proser, M.P.P., Director of Policy Research, National Association of Community Health Centers, 1400 Eye Street, NW, Suite 330, Washington, DC 20005, Phone: (202) 296-1960, Fax: (202) 296-3526, Email: mproser@nachc.com Research Objective: Using community health centers as the example, this presentation will highlight the benefits of working with community-based safety net providers and issues to consider when conducting communitybased participatory research (CBPR). It will also shed light on the research capacity of health centers, including the adoption of health information technology and level of interest in research. Lastly, this presentation will describe a newly established research agenda for community health centers and the medically underserved. Study Design: The community health center research agenda was established through a consensus-driven process bringing together over 100 experts in the field, including those from health centers, health center networks, state primary care associations, researchers/academics, foundations, publishers, government agencies, and national partners. The agenda is being published in the February 2007 issue of Progress in Community Health Partnerships: Research, Education, and Action (Johns Hopkins University Press). Population Studied: Over 5000 community health center delivery sites serve nearly 16 million patients in every state and territory. Health center patients are disproportionately poor, uninsured or publicly insured, and minority: 92% of patients are low income, 40% are uninsured, 36% have Medicaid, and 63% are members of racial and ethnic minorities. The near-elderly make up the fastest growing patient age group. Roughly 25% of encounters are for chronic conditions. Most health centers have been trained in and are employing the Chronic Care Model through the federally-initiated Health Disparities Collaboratives, including the use of electronic patient registries. More and more are adopting electronic health records. Principal Findings: As community-directed providers of care in medically underserved communities, health centers have a history or providing high-quality, patient-centered care to traditionally hard-to-reach populations. Given their expansive knowledge of the communities they serve and the resources they bring to the table, they are ideal partners in health services research. A growing number of health centers are utilizing health information technology, including electronic patient records, making research using patient-level data less complicated and more robust. Health centers are also organizing themselves into networks across large regions, creating forums where patient data are consolidated and case mix even more diverse. In addition, they are actively participating in health professional training opportunities. Conclusions: The number of health centers participating in and interested in CBPR is growing. They are ideal partners for CBPR given their operations and service delivery approaches, in-depth knowledge of their communities, and expertise in delivering high quality care and removing barriers to care. A research agenda for health centers includes research questions on determining their community value, impact on health outcomes, and use of health information technology to improve care. Implications for Policy, Delivery or Practice: Health centers are ideal settings to study community-based primary care and prevention, especially for underserved populations. Such research can improve the delivery and quality of care and health outcomes. Health centers have worked collaboratively with researchers and others to develop a research agenda, and stand ready to engage in more research. Funding Source(s): RWJF, AHRQ, HRSA, The Commonwealth Fund, The Community Clinics Initiative of the Tides Foundation and California Endowment Call for Panels Implementation Issues in Medicare’s Physician Quality Reporting Initiative (PQRI) Chair: Myles Maxfield, Ph.D. related to design and implementation of the voluntary reporting program in the context of recent legislation, and potential adaptation for any future physician pay-for-performance programs in Medicare. Teresa N. Clark, Office of Clinical Standards and Quality, CMS, will moderate. The first study: ‘‘Creating a PQRI Data Validation Strategy that Includes Opportunities for Ongoing Data Collection, Program, and Measure Improvement,’’ provides options for validating data underlying PQRI measures, considering cost, effectiveness, feasibility, scientific soundness, and flexibility, while supporting continuous improvement in program and measurement design. The second study: ‘‘PQRI: Changes in Physician Office Workflows for Quality Reporting: A Perspective from the Trenches,’’ reports qualitative findings on the impact of Medicare quality reporting on physicians’ practice workflows, and the relatively low associated time required for reporting based on site visits to participating practices. The third study: ‘‘PQRI: Performance Reporting and Payfor-Performance Considerations for Providers Treating Vulnerable and Underserved Patients’’ reports interview, survey, and claims analysis findings suggesting specific program design options to limit potential unintended consequences for disadvantaged patients, including reduced access to physician services and hindrance of quality improvement efforts. The fourth study: ‘‘PQRI: Operational Insights and Issues from Early Physician Practice Adopters,’’ reports findings based on discussions with participating physicians, analysis of data from reporting of 2006 PQRI starter set measures, and technical reviews of PQRI performance measure specifications, to examine operational issues related to physician participation in the program. Researchers from Mathematica Policy Research will be joined by discussant Thomas Valuck, Office of Clinical Standards and Quality, CMS. PQRI: Creating a PQRI Data Validation Strategy that Includes Opportunities for Ongoing Data Collection, Program, and Measure Improvement Mary Laschober, Ph.D., Philip Renner, M.B.A., Zakiya Pierre, B.S., Sam Simon, Ph.D., Sarah Davis, M.P.A., Teresa Clark, M.B.A., M.P.H. Monday, June 4 • 11:00a.m.-12:30p.m. Panel Overview: In 2007, CMS will begin to offer physicians payment incentives for reporting standardized quality measures on their Medicare patients. This session explores several issues Presented by: Mary Laschober, Ph.D., Senior Researcher, Health, Mathematica Policy Research, 600 Maryland Avenue, SW, Suite 550, Washington, DC 20024, Phone: (202) 554-7572, Fax: (202) 863-1763, Email: mlaschober@mathematica-mpr.com Research Objective: To provide options to CMS for validating physician quality measurement data for the 2006 Physician Voluntary Reporting Program (PVRP) that take into account cost, feasibility, scientific soundness, flexibility, and applicability to Medicare policy. Options provided should also ensure opportunity for feedback to providers, CMS, and measure developers to support ongoing improvements in program design and measure development. Study Design: Literature review and environmental scan that included discussions with leaders of measurement initiatives using state-of-the-art strategies to validate data for health care quality indicators, plus discussion with a technical expert panel of thought leaders in the field of measurement validation methods. Population Studied: National and regional physician-level and other health care provider quality measurement and reporting programs in the U.S. Principal Findings: We identified 30 providerlevel initiatives with validation for the environmental scan discussions, and the literature review identified 12 reports highly relevant to the study. There is a much deeper literature on scientifically ensuring the validity of quality measures, but few studies address validation of quality measurement and reporting systems. Most physician measurement initiatives use measures based in administrative or medical record data, and are limited to certain payers or regions. Most of the validation methods calculate either an agreement rate between data submitted and re-abstracted chart data, or an estimate of the effect of errors on measure rates. All of the initiatives studied sought to balance accuracy of validation with the burden of validation. Conclusions: An optimal strategy will likely validate PVRP data at the primary nexus of responsibility for ensuring accurate data ---- the individual physician ---- but will employ a twostage sampling strategy to minimize provider and CMS burden. A first-stage broad approach would review a small sample of patients from an approximately 1% random sample of providers and a second-stage narrow approach would review a larger sample of patients from a smaller sample of outliers. Both stages would act to detect systematic unintentional errors and to deter system gaming. Because medical record review (MRR) is the ‘‘gold standard’’ even for electronic medical records, options suggested to CMS will include retrospective MRR, supplemented with Medicare claims analysis, logical built-in edits, and benchmarking and trending of measure results to detect errors at different steps of the reporting system. It may also be desirable to link PVRP validation with Medicare’s existing Part B claims validation and appeals activities. Additionally, CMS is considering patient registries as a supplement to administrative claims for collecting PVRP clinical information, which may require a different auditing operation. Implications for Policy, Delivery or Practice: There is no one perfect solution for validating data underlying physician quality measures. As a result, CMS will likely have to choose among several options, each with their own advantages and disadvantages for ensuring data accuracy, consistency, completeness, reliability, and feasibility. Because the PVRP is a new program, all validation steps should promote learning and improvement among all PVRP stakeholders, including providers, CMS, other health care payers/purchasers, and measure developers. Funding Source(s): CMS PQRI: Changes in Physician Office Workflows for Quality Reporting, A Perspective from the Trenches Angela Merrill, Ph.D., Lorenzo Moreno, Ph.D., Whitney Scott, M.A., Martha Kovak, M.P.H., Jung Kim, M.P.H., M.B.A., Stephanie Peterson, M.P.P. Presented by: Angela Merrill, Ph.D., Senior Researcher, Health, Mathematica Policy Research, Inc., 955 Massachusetts Avenue, 8th Floor, Cambridge, MA 02139, Phone: (617) 3018977, Fax: (617) 491-8044, Email: amerrill@mathematica-mpr.com Research Objective: The 2006 Physician Voluntary Reporting Program (PVRP) was a first step in collecting quality measures from physicians for Medicare fee-for-service patients. Practices participated by reporting specified ‘‘Gcode’’ procedure codes for quality measures on their claims. The objective of this study was to summarize the initial investments, changes to workflows, and time associated with reporting PVRP quality measures. Study Design: Site visits with 15 physician practices reporting PVRP measures in early 2006, conducted October 2006-January 2007. Discussions about start-up investments, workflow changes, time, and challenges to report G-codes on Medicare claims. Population Studied: Physician practices reporting PVRP measures in early 2006. Practice specialties included primary care, cardiology, and surgery. Practice sizes were typically 3 or fewer physicians, with two larger practices. Practices were typically reporting 3 to 6 primary care measures, while surgeons reported one measure. Principal Findings: The common initial steps to participate in PVRP were: (1) learning about PVRP through CMS website or conferences, (2) developing worksheets with G-codes, and (3) adding codes to billing software and resolving issues with billing. These steps typically took less than three hours, although some practices reported many hours of negotiation with billing companies to get them to accept G-codes in claims. The workflow changes typically consisted of three main steps: (1) identifying Medicare patients and attaching a worksheet, (2) physician checking off appropriate G-codes during the visit, and (3) entering the codes to the billing system. For surgeons reporting use of antibiotics, measures were coded after the surgery, through review of the medical record or surgeon dictation. The median time required to report a single G-code on a claim was less than 2 minutes, but ranged from 15 seconds to over 12 minutes for more complicated cases/measures. The most time consuming step was typically time for physician to choose the code. No practices implemented electronic medical records (EMRs) or other clinical management systems to participate; and the two practices with EMR did not use them to generate PVRP reporting. Conclusions: We found that the initial workflow changes and time to report quality measures on claims were relatively modest but did vary across practices, depending on factors such as patient complexity and the number of measures reported. Workflow changes were basic, and did not involve major changes. Addressing billing issues was one of the biggest initial investments. EMRs were not needed to report; however, one practice that stopped reporting thought it would be less time consuming once they had EMR. Implications for Policy, Delivery or Practice: This study provides information on the types of workflow changes physician practices may need to implement to participate in quality reporting programs. Based on the experience of PVRP, practices should be able to report on quality measures with modest workflow changes, but the cost of reporting will be variable, depending on the number and complexity of reported measures, and the mix of staff performing the reporting. Funding Source(s): CMS PQRI: Performance Reporting Considerations for Providers Treating Vulnerable and Underserved Patients Hoangmai Pham, M.D., M.P.H., Erin Fries Taylor, Ph.D., Timothy Lake, Ph.D., Melanie Au, M.P.P., Stephanie Peterson, M.P.P., Myles Maxfield, Ph.D. Presented by: Hoangmai Pham, M.D., M.P.H., Senior Researcher, Center for Studying Health System Change, 600 Maryland Avenue SW, Suite 550, Washington, DC 20024, Phone: (202) 5547571, Fax: (202) 484-9258, Email: mpham@hschange.org Research Objective: We examined barriers to performance reporting among providers treating a disproportionate share of vulnerable and underserved patients and considered strategies to avoid unintended consequences of performance reporting and pay-for-performance for these patients. Study Design: We reviewed literature on prevalence of and barriers to performance reporting among providers treating vulnerable populations, and conducted over 20 semistructured discussions with experts in quality reporting and performance-based incentive programs, providers who treat vulnerable populations, and other stakeholder groups. We convened a meeting of 15 advisors, including quality measurement and case-mix adjustment experts, and representatives from provider organizations, health plans, purchaser organizations, and CMS. We also examined claims data linked to the 2000-2001 Community Tracking Study Physician Survey to compare performance on quality measures (delivery of preventive services) between providers who treat more versus fewer patients of racial/ethnic minorities, and of lower socioeconomic status. Population Studied: This study focused on vulnerable patients and the providers who treat them. The question of what characteristics best define such providers was answered through our discussions. Although some stakeholders preferred a more encompassing definition, most concurred that providers’ status as those who treat vulnerable patients should take into account patients of low socioeconomic status, those who belong to a racial/ethnic minority, and those residing in underserved and/or rural areas. Principal Findings: Stakeholders cited many barriers to participation by providers treating vulnerable populations in performance reporting, although many of these barriers relate to small practice size rather than the types of patients they treat, per se. While financially-strapped providers who treat vulnerable populations may have fewer staff and some types of resources, little evidence exists that providers necessarily face higher reporting costs relative other providers. In pay-for-performance programs, however, providers treating vulnerable populations likely face some distinct disadvantages. The lower cumulative reimbursement rates that some providers receive for treating many Medicaid or uninsured patients mean that such providers likely have fewer practice resources available, which may impair their ability to engage in systematic quality improvement. In addition, some groups of disadvantaged patients treated may be less likely to adhere to recommended treatment, although physicians share responsibility for improving adherence. Finally, fewer support services and resources among these patients, along with lower education and health literacy levels, may require providers who treat vulnerable populations to devote more resources to achieve quality outcomes that are comparable to those of other providers. However, there limited and mixed evidence on the relative quality performance between these provider groups, and more generally on the relationships between patient characteristics, adherence, and quality performance. Conclusions: Providers who treat vulnerable populations likely face some important disadvantages under pay-for-performance programs. If such disadvantages are not taken into account, some providers may be less likely to treat vulnerable and underserved patients-----given their potential effect on performance scores and rewards. Implications for Policy, Delivery or Practice: Differential performance rewards under pay-forperformance may be warranted for providers treating high volumes of patients with low socioeconomic status. More extensive data collection and analysis are needed before similar program design decisions can be made regarding providers treating other vulnerable populations. Funding Source(s): CMS PQRI: Operational Issues and Insights from Early Physician Practice Adopters Timothy Lake, Ph.D., Melissa Neuman, M.S., Mary Laschober, Ph.D., Zakiya Pierre, B.S., Philip Renner, M.B.A., Latousha Leslie, R.N., B.S.N., M.S. Presented by: Timothy Lake, Ph.D., Senior Researcher, Health, Mathematica Policy Research, Inc., 600 Maryland Avenue SW, Suite 550, Washington, DC 20024, Email: tlake@mathematica-mpr.com Research Objective: To examine operational and implementation issues related to physician data collection and reporting of the starter set of 16 PVRP measures in 2006. Study Design: Discussions with clinical and administrative staff at 13 physician practices, technical review of measure specifications, and a descriptive analysis of PVRP reporting data submitted from January 2006 through August 2006. Discussions were conducted in-person or by telephone. Discussions centered on physician decisions to participate in the program and on which measures to report, assistance with understanding the program’s data reporting instructions and process, and ease of program participation. Population Studied: Primary care physicians and specialists operating in solo, single specialty, and multi-specialty group practices that had submitted at least one PVRP measure during the study period. Principal Findings: Early findings suggest that clinical and administrative staff at participating practices had a limited understanding of selected aspects of the 2006 PVRP measurement specifications and were often unsure of how to access additional program information and support. Participants also generally did not review specification updates over time. When uncertainty existed regarding measure instructions, practices generally chose coding and reporting approaches that either appeared most consistent with the specifications or that were most feasible given particular practice circumstances. As a result, reporting processes varied across practice settings. For example, practice staff members were often unsure when and how often to report intermediate outcome measures, such as HbA1C screening test results for diabetes. They also expressed uncertainty about whether a diabetes diagnosis was always required to be on a claim containing diabetes measures. One surgical practice submitted measure information (antibiotic prophylaxis) related to a procedure that was not covered in the existing specifications. Other areas of confusion included when to use exclusion codes, submission of claims with zero-dollar amounts, and interpretation of numerator definitions (such as what constitutes a ‘‘falls assessment’’). Variation and issues arose at several points during the reporting process, including 1) reporting system set-up, 2) patient identification and selection, 3) coding of measures based on clinical service delivery and diagnostic information, and 4) reporting of measures on Medicare claims. Analysis of Medicare claims data indicate that reported measures did not always contain the relevant diagnostic or service delivery information. Conclusions: Limited understanding of measure specifications, and variation in reporting approaches, may affect program participation, the consistency of reported data, and conformity with clinical measure specifications in future quality measurement programs. Implications for Policy, Delivery or Practice: Increased communication and technical assistance resources made available to practices can help ensure the accuracy and consistency of the information collected in quality measurement programs. This could include 1) broader outreach to practices considering participation and 2) increased availability of technical consultation services to participating practices. Existing measurement specifications may also be refined or modified in certain areas to address the varying information needs of practice staff involved in different aspects (for example, clinical coding or billing) of the reporting process. Funding Source(s): CMS Call for Panels Translating Research into Practice: Case Study of Improving Heart Attack Care Chair: Carolyn Clancy, M.D. Monday, June 4 • 2:30 p.m.-4:00 p.m. Panel Overview: The panel, moderated by Carolyn Clancy, MD, Director of the Agency for Healthcare Quality and Research, examines a model of translating research evidence into practices to improve quality and save patients’ lives. As a case study of the proposed model of translation, speakers will describe recent experiences to gather, analyze, publish, and disseminate research on how to reduce door-toballoon time in patients with ST-segment elevation myocardial infarction. Prompt treatment is critical for patient survival after this kind of myocardial infarction, and less than 40% of hospitals meet current guidelines, which recommend a median of 90 minutes or less for door-to-balloon times, i.e., the time between patient presentation at the hospital and balloon inflation to unblock coronary arteries. Panelists represent a range of perspectives central to current efforts to improve hospital performance in door-to-balloon times nationally. Panelists will include leaders from the National Institute of Heart, Lung, and Blood and the Agency for Healthcare Research and Quality; key investigators who produced the research evidence; the central architect from the American College of Cardiology, who oversaw the national campaign to create changes at the level of practicing cardiologists and their hospitals; and the Chief Medical Officer of Blue Cross/Blue Shield who will provide the payer perspective on the importance of research and its diffusion into practice. Taken together, the panelists will illustrate an effective approach for performing and disseminating research to promote evidence-based changes in quality of care. Implications for quality improvement efforts nationally will be discussed. Strategies to Reduce Door-to-Balloon Time in Myocardial Infarction Elizabeth Bradley, Ph.D., Jeph Herrin, Ph.D., Jeptha Curtis, M.D., Brahmajee Nallamothu, M.D., David Magid, M.D., M.P.H., Harlan Krumholz, M.D., S.M. Presented by: Elizabeth Bradley, Ph.D., Professor of Public Health, Epidemiology and Public Health, Yale School of Medicine, 60 College Street, New Haven, CT 06520, Phone: (203) 785-2937, Fax: (203) 785-6287, Email: Elizabeth.Bradley@yale.edu Research Objective: Prompt reperfusion treatment is essential for patients with STsegment elevation myocardial infarction (STEMI); however, the majority of U.S. hospitals fail to meet national guidelines, which recommend median door-to-balloon time of 90 minutes or less for primary percutaneous coronary intervention (PCI). Door-to-balloon time, which is important for patient survival, is the time between the patient’s presentation to the hospital and subsequent balloon inflation for the procedure to unblock the coronary arteries. We sought to identify the hospital strategies that were significantly associated with faster door-toballoon times. Study Design: We surveyed 365 hospitals to identify hospital strategies that were correlated with faster door-to-balloon times. We used hierarchical generalized linear models and patient-level data from the Centers for Medicare & Medicaid Services to determine the association between hospital strategies and door-to-balloon time. Population Studied: Patients with STEMI treated during 2006 in 365 randomly selected U.S. hospitals performing primary PCI. Principal Findings: In multivariable analysis, six strategies were significantly associated with faster door-to-balloon times, including having emergency medicine physicians activate the catheterization laboratory (mean reduction in door-to-balloon time 8.2 minutes), activating with a single call to a central page operator (13.8 minutes), activating based on pre-hospital electrocardiograms while the patient is still en route to the hospital compared with waiting until the patient had arrived (15.4 minutes), expecting interventional cardiologists to arrive within 20 versus within more than 30 minutes of being paged (19.3 minutes), having an attending cardiologist always on site (14.6 minutes), and using real-time data feedback with emergency department and catheterization laboratory staff (8.6 minutes). More strategies resulted in faster times. Despite their effectiveness, these strategies were used by a minority of hospitals. Conclusions: Our findings highlight a discrete set of effective, feasible, and currently underused strategies that hold promise for substantially improving patient care. Implications for Policy, Delivery or Practice: The findings provided a foundation for a national campaign to improve hospital care for patients with STEMI, using evidence-based practices. The work identifies priorities for quality improvement efforts to improve health care delivery and enhance national progress toward meeting the policy recommendation that all hospitals have median door-to-balloon times of 90 minutes or less. Organizational changes needed to accomplish this level of performance may generate benefits for other areas of hospital practice as well. Funding Source(s): National Heart, Lung, and Blood Institute Moving from Research to Practice - D2B: An Alliance for Quality John Brush, M.D., Wayne Bachelor, M.D., Eva Kline-Rodgers, R.N., M.S., Brahmajee Nallamothu, M.D., Elizabeth Bradley, Ph.D., Harlan Krumholz, M.D., S.M. Presented by: John Brush, M.D., Chair, Quality Strategic Directions Committee, President, Virginia Chapter, American College of Cardiology, 844 Kempsville Road, Suite #204, Norfolk, VA 23502, Phone: (757) 466-6100, Fax: (757) 466-1597, Email: jebrush@earthlink.net Research Objective: The American College of Cardiology (ACC), through Guidelines Applied in Practice (GAP) programs, has sought to identify gaps in clinical practice and to develop mechanisms to motivate positive change in cardiology to improve the quality of care. D2B: An Alliance for Quality is a GAP program involving a national campaign launched by the ACC to save time and save lives by reducing the door-to-balloon times in U.S. hospitals performing primary PCI. Currently, only 40% of hospitals achieve median door-to-balloon times of 90 minutes or less. The broad goal of the D2B Alliance is to translate knowledge about how to improve time to treatment into practice. The specific objective of the national campaign is to have all participating hospitals achieve door-toballoon times of 90 minutes or less for at least 75% of their patients treated with primary percutaneous coronary intervention (PCI) for STsegment elevation myocardial infarction (STEMI). Study Design: The ACC assembled the ACC D2B Work Group and 5 subgroups comprised of physician, nurse, and researcher volunteers to summarize the existing evidence on strategies for reducing door-to-balloon time, to develop tools and educational materials to support hospitals’ efforts to adopt effective strategies, and to enroll hospitals into the national campaign to improve times. State chapters of the ACC provided a network of chapter presidents whow were commissioned to recruit physician champions and hospitals across the country. In addition, the ACC effort also partnered with more than 20 additional collaborators and supporters including but not limited to the American Heart Association, Blue Cross/Blue Shield Association, Institute of Healthcare Improvement, the Society for Academic Emergency Medicine, and the National Association for EMS Physicians. Population Studied: Patients with STEMI treated with PCI in hospitals that enroll in the GAP-D2B national campaign. Principal Findings: More than 150 hospitals enrolled in the GAP-D2B campaign within the first 2 months of its launch, and enrollment is continuing. The participants reflect differing geographical regions across the country, and include hospitals of varying size, teaching and non-teaching status, and ownership types. All enrolled hospitals complete a baseline survey to document their current processes to facilitate timely care for patients with STEMI. Hospitals also receive a Tool Kit and Change Package designed by the ACC D2B Work Group based on existing research identifying about effective practices. Hospitals’ door-to-balloon times will be tracked using existing data sources, including publicly report data from Center for Medicare & Medicaid Studies. Conclusions: Practical efforts, based on research-based findings about what works to reduce door-to-balloon time, are being used to translate research into practice and improve quality of care. The role of professional organizations, in collaboration with health services and outcomes researchers, is essential to providing the needed impetus to disseminate best practices and influence the quality of clinical care. Implications for Policy, Delivery or Practice: The D2B national campaign demonstrates a model of moving research findings quickly into improved clinical practice. In this model, the research focused not on ‘‘what’’ to do but "how to do it. Close interaction between research and dissemination teams ensured that the research addressed questions of practical importance while the dissemination efforts remained evidence-based. This approach of translating research into practice with the use of effective networks of leading clinicians, researchers, professional associations, and policy-makers may be helpful in promoting national quality improvement efforts in other clinical areas as well. From Retail to Wholesale in Safety and Quality Improvement Irene Fraser, Ph.D., Irene Fraser, Ph.D., Allen Korn, M.D., F.A.C.P. Presented by: Irene Fraser, Ph.D., Director of the Center for Delivery, Organization, and Markets, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850, Phone: (301) 427-1364, Fax: (301) 427-1542 Research Objective: The door-to-balloon time initiative shows that examination and codification of processes used by top-of-class providers can provide replicable models for substantial leaps in quality and safety. This is tremendous news. But the methods for achieving this breakthrough are slow and somewhat expensive, and require identifying steps specific to each clinical procedure. Moreover, it is not clear whether the combination of procedure-specific safety strategies will add up to success at the hospital level. Is there a way to move from retail to wholesale in identification of winning safety strategies, or must we must continue to make improvements on a ‘‘one-off’’ basis? Our objective is to identify efficient strategies for spreading safety improvements to more sites and more processes. Study Design: This presentation considers the experiences and potential of five potential approaches for moving from retail to wholesale: 1. Create a national campaign to promote takeup of one process redesign. 2. Replicate the approach and methodology in a second study of a second procedure. 3. Spread the methodology itself. 4. Seek system or organizational approaches that will support improvements in multiple clinical outcomes at once 5. Align purchaser (government, employer, plan) incentives to support evidence-based strategies such as this. Population Studied: Patients, providers, and organizations involved with diverse approaches for spreading evidence-based improvements. Principal Findings: Each approach has shown some potential to improve spread of evidencebased improvements, Conclusions: Approaches have varying advantages and disadvantages in design, implementation, and evaluation. Implications for Policy, Delivery or Practice: Using one or more of these strategies will enable funders, payers, and providers to move from retail to wholesale in safety improvement. The Door-to-Balloon (D2B) Project as Part of Translation Research at the National Heart, Lung, and Blood Institute (NHLBI) Lawton Cooper, M.D., M.P.H., Barbara Wells, Ph.D., Lawrence Fine, M..D, Dr.P.H., Denise Simons-Morton, M.D., Ph.D. Presented by: Lawton Cooper, M.D., M.P.H., Medical Officer, Division of Prevention and Population Sciences, National Heart, Lung, and Blood Institute, 6701 Rockledge Drive, Room 10108, Bethesda, MD 20892, Phone: (301) 4350419, Fax: (301) 480-1773, Email: cooperls@nhlbi.nih.gov Research Objective: The NHLBI has invested enormous research resources to identify safe and effective CVD preventive, diagnostic, and therapeutic strategies. However, mechanisms are lacking to ‘‘close the loop’’ from research results to clinical care, i.e., to track actual clinical use of these therapies, to identify factors related to their adoption, and to assess associations of adoption vs. non-adoption with patient outcomes. Study Design: This abstract describes how the D2B project relates to NHLBI research activities in the area of translation of clinical practice knowledge into practice. Principal Findings: The NHLBI supports a number of grants through various funding mechanisms that address the gap between clinical knowledge and practice. The study on door-to-balloon time led by Drs. Krumholz and Bradley that is featured in this panel is an outstanding example. Some features that make it outstanding include the innovative design that merges qualitative and quantitative methods, the focus on concrete actions that could affect the outcome measure, and the dissemination plan that directly engages U.S. hospitals performing PTCI. It thus serves as a model for others studying the translation into practice of other clinical guidelines. NHLBI currently funds translation grants that were initiated by investigators, and others that responded to specific funding announcements, such as RFAs or PAs. One RFA supports grants evaluating interventions in clinical practice to improve implementation of national, evidence-based clinical practice guidelines for the treatment of heart, lung and blood diseases and conditions. Another RFA funds several grants studying clinically feasible interventions related to medical care delivery that increase the proportion of treated hypertensive African American patients whose blood pressure is controlled according to JNC guidelines. Recently the NHLBI released an RFA entitled ‘‘Cardiovascular Research Network (CVRN) in Community-Based Care’’ (RFA-HL-07011), one of whose objectives is to promote research on clinical practice and quality of care. At the NIH level, the new consortium funded by Clinical and Translational Science Awards (CTSAs) is viewed by the NHLBI as an opportunity to reduce the delay between clinical knowledge generation and adoption, by encouraging broader community involvement in research to increase general awareness of ongoing studies and increase interest in research outcomes. Conclusions: The D2B project is a prime example of NHLBI’s history of supporting research activities in the area of translating clinical research into practice. The Institute’s Strategic Plan, currently available for public comment, emphasizes the important role of these activities within the NHLBI’s overall mission, along with traditional basic and clinical research. Implications for Policy, Delivery or Practice: Findings emerging from NHLBI-funded research on the translation of clinical guidelines into practice have significant implications for public health policy and health care delivery. Welldesigned dissemination efforts such as the national D2B campaign promise to take the findings of translational research and translate them into practice. Call for Panels Improving Health and the Use of Medical Services: Analyzing the Contributions of Medicaid and SCHIP Chair: Richard Kronick, Ph.D. Monday, June 4 • 2:30 p.m.-4:00 p.m. Panel Overview: In their role as a ‘‘laboratory for democracy,’’ states have taken a variety of approaches to providing public coverage to low income children and families. States differ significantly in choices made about eligibility, service coverage, and provider payment policies for the Medicaid and State Children’s Health Insurance Program (SCHIP) programs. This panel presents research that explores the impact of some of these different decisions on access to health care and health outcomes, using several datasets from the National Center for Health Statistics. The first paper examines the effect of reductions in state Medicaid physician payment levels on access to care. Understanding these effects is important when considering trade-offs among provider payments, eligibility levels, benefit packages and other demands on state budgets. The second paper questions whether increasing generosity in Medicaid eligibility helps newborns and mothers receive care in the same hospitals as the privately insured in the face of residential segregation, public provision of care, and possibly inadequate public payment of providers. The third paper analyzes the effects of SCHIP implementation on the use of health services among low-income children. The final paper investigates the effect of Medicaid and SCHIP eligibility and other state policies on children’s use of health services and health status, considering the effects of expansions in children’s eligibility on outcomes for both children and families. The implications of these papers for the prospects of further reducing the gap in health between low- and high-income children and families will be discussed during the panel. Medicaid Physician Payment and Ambulatory Care of Medicaid Patients Sandra Decker, Ph.D. Presented by: Sandra Decker, Ph.D., Senior Service Fellow, Division of Health Care Statistics, National Center for Health Statistics, 3311 Toledo Road, HYATTSVILLE, MD 20782, Phone: (301) 458- 4748, Email: sdecker@cdc.gov Research Objective: Although states commonly cut or freeze physician fees in an attempt to control Medicaid spending, little work has assessed the impact of a reduction in physician fees on the care of Medicaid patients. Previous research suggests that reductions in fees may reduce the number of physicians willing to accept Medicaid patients, possibly reducing the quantity of care patients receive and/or leading them to seek care in hospital emergency departments or other sites, but the evidence is not strong. This paper furthers our understanding of the relationship between the level of state Medicaid fees and use of ambulatory care among Medicaid patients. Study Design: I estimate the effect of the generosity of Medicaid physician payment levels on the volume and site of ambulatory care received by Medicaid patients compared to other patients, controlling for age group, gender, race, and state and year effects. The use of state fixed effects and the comparison to treatment of privately-insured patients serves to separate Medicaid's effect on access to care from any correlation between the Medicaid fee and other attributes of the state in which a patient lives. Data on state Medicaid physician payment levels in 1993, 1998 and 2003 were collected by the Urban Institute, and data on the use of health services come from several National Center for Health Statistics (NCHS) surveys in 1993/1994, 1998/99, and 2003/2004. Data on the selfreported total number of physician visits in the past year come from the National Health Interview Survey (NHIS), a nationally representative sample of households in the U.S. Information on site of visits comes from the National Ambulatory Medicare Care Survey (NAMCS) and the National Hospital Ambulatory Care Survey (NHAMCS), nationally representative surveys of visits to office-based physicians and hospital outpatient and emergency departments (OPDs and EDs). Population Studied: Data on the 317,711 individuals in the NHIS and the 462,359 visits in the NAMCS/NHAMCS among those under age 65 and not on Medicare. Principal Findings: Reductions in Medicaid physician fees lead to statistically significant reductions in the number of visits for Medicaid patients compared to privately insured patients. Compared to privately insured patients, Medicaid patients rely much more heavily on OPDs and EDs and less on physician offices, though differences in site of care between Medicaid and privately insured patients are smaller in states with more generous Medicaid physician payment. Reductions in fees lead to a statistically significant shift away from physician offices and toward both EDs and OPDs, though the shift is larger toward OPDs than EDs. Firstlisted diagnoses for which site of care shifts are most pronounced include diabetes, hypertension, asthma, migraine, noninfectious enteritis and colitis, and chest pain. Conclusions: This paper finds a significant link between state policy on Medicaid physician payment levels and both the volume and site of care of Medicaid patients, a link that is significantly stronger and larger than estimated in previous studies using older data. Implications for Policy, Delivery or Practice: Since Medicaid enrollees in states with low Medicaid physician fees receive significantly less care at different sites than patients in other states, future research on the implications of these differences in care for the health status of Medicaid patients is particularly important. Medicaid Eligibility and Hospital Care for Mothers and Newborns Kosali Simon, Ph.D., Robert Kaestner, Ph.D., Sandra Decker, Ph.D., Kosali Simon, Ph.D. Presented by: Kosali Simon, Ph.D., Assistant Professor, Department of Policy Analysis and Management, Cornell University, N227 MVR Hall, Ithaca, NY 14853, Phone: (607) 255-7103, Fax: (607) 255-4071, Email: kis6@cornell.edu Research Objective: When enacted in 1965, the Medicaid program sought to finance medical care for the poor. It was not designed to create a ‘‘two-tiered’’ system of care where publiclyinsured and privately-insured patients receive care from largely different providers. This paper assesses the extent to which Medicaid provides pregnant women with access to the same hospitals and same medical care that is obtained by privately insured mothers. If women with different types of insurance largely receive care at separate facilities, or receive different care within facilities, this could partly explain differences in maternal and infant health by insurance status. Study Design: We compare the characteristics of hospitals and the care received in those hospitals by women with different types of health insurance coverage. To address the nonrandom nature of insurance status, we use the state and time variation in insurance status caused by differences in the timing and magnitude of Medicaid eligibility expansions across states between 1988 and 2003. Specifically, we use a representative sample of women from the Current Population Survey and Medicaid eligibility rules to calculate the fraction eligible for Medicaid in each state and year that is independent of economic and health conditions in the state. We then use this simulated eligibility measure to predict insurance status and identify the effect of insurance status on the type of facility where a pregnant woman receives care. Population Studied: Discharges from short-stay hospitals from the National Hospital Discharge Survey (NHDS), 1988-2003, linked with additional hospital characteristics from the American Hospital Association (AHA) Annual Survey Database, and with simulated Medicaid eligibility by state and year as explained above. Principal Findings: We examine the effect of insurance status on the share of privatelyinsured deliveries in the hospital where a woman gives birth, the probability that the mother gives birth in a hospital with a neo-natal intensive care unit (NICU), the probability that a women gives birth in a proprietary, non-profit or government hospital, the distance between the woman’s home and the hospital she gives birth in, whether or not the child is born by Cesarean section, and mother’s length of hospital stay. Results imply that individuals in low income areas and those on Medicaid largely receive health care at different facilities than others. State expansions in Medicaid eligibility may affect where women give birth and the type of hospital care received. Conclusions: This research points to the need for further investigation of whether or not separate care is equal in quality and in turn whether it is related to differences in health outcome. Implications for Policy, Delivery or Practice: If future research shows that separate care is different in quality, options for eliminating the ‘‘two-tiered’’ system of care should be evaluated. Effects of the State Children’s Health Insurance Program (SCHIP) on Access to Medical Care and Use of Medical Services Hua Wang, Ph.D., Edward Norton, Ph.D., Gary Rozier, Ph.D., Sally Stearns, Ph.D. Presented by: Hua Wang, Ph.D., Research Associate, Department of Policy Analysis and Management, Cornell University, 432A Martha Van Rensselaer Hall, Ithaca, NY 14853, Phone: (607) 255-2505, Fax: (607) 255-4071, Email: hw227@cornell.edu Research Objective: To provide national estimates of implementation effects of the State Children's Health Insurance Program (SCHIP) on medical care access and use for low-income children. Study Design: The study design is based on variation in the timing of SCHIP implementation across states and among children observed prior to and after implementation. Two analyses were conducted. The first estimated the total effect of SCHIP implementation on measures of access to care (dichotomous variables denoting whether a child had a usual place for care and whether a child had experienced in the previous 12 months any delayed medical care, unmet need for medical care, prescription drug and mental care) and medical services utilization (dichotomous variables indicating whether a child had visited a general doctor and specialty doctor in the past year) for low-income children (family income below state SCHIP eligibility thresholds) using county and time fixed effects models. The second analysis estimated differences in medical care access and use among low-income children with SCHIP or Medicaid coverage and their uninsured counterparts, using instrumental variables methods to control for selection bias. Selected instruments for insurance coverage include state SCHIP program features and variables representing whether any family member receives Food Stamps and whether health insurance was offered to a child’s parents through the workplace. Both analyses controlled for child and family characteristics. Population Studied: National representative sample of children in U.S. households from the 1997-2002 National Health Interview Survey. Principal Findings: When SCHIP had been implemented for more than one year, the probability of having visited a general doctor for low-income children increased by 7.4 percentage points. Compared with their uninsured counterparts, those who had SCHIP or Medicaid coverage were more likely to have a usual place for care (23.4%), less likely to report delayed (?12.3%) or unmet medical care need (?7.7%), and more likely to have visited a general (25.7%) and specialty doctor (8.8%) within 12 months. SCHIP program type had no differential effects. Policy simulations suggest further expansion of public insurance may not close the gap between low- and high-income children if the effectiveness of public health programs in improving the use of health services remains the same. Conclusions: Consistent results from two analytical approaches provide evidence that SCHIP implementation significantly increased use of medical services for low-income children in the U.S. Children enrolled in SCHIP or Medicaid had substantially increased access to and use of medical care than the uninsured. Implications for Policy, Delivery or Practice: SCHIP did make a difference in improving medical care access and use for low-income children, though the effectiveness of public health programs in improving the use of health services may need to improve in order to eliminate disparities in medical care access and use between the low- and high-income children. Funding Source(s): National Center for Health Statistics (NCHS)/AcademyHealth Health Policy Fellowship Effect of Recent State Policies (SCHIP/Medicaid Expansions, Welfare Reform and EITC) on Child Health and Health Care Use Maki Ueyama, M.P.A., Rachel Dunifon, Ph.D., Kosali Simon, Ph.D., Maki Ueyama, M.P.A. Presented by: Maki Ueyama, M.P.A., Ph.D. candidate, Department of Policy Analysis and Management, Cornell University, Ithaca, NY 14853, Phone: (607) 255-7978, Fax: (607) 2554071, Email: mu24@cornell.edu Research Objective: To examine the effect of state-level social assistance policies on child health and health care use. Specifically, we use the 1990-2002 National Health Interview Survey accessed through the NCHS Research Data Center to study the impact of SCHIP/Medicaid, welfare reform, and the Earned Income Tax Credit (EITC) on children. Study Design: To examine the impact of Medicaid/SCHIP expansions on children, we use an instrumental variables approach, instrumenting for Medicaid participation and eligibility with an index of state Medicaid/SCHIP generosity created from the Current Population Survey (CPS) at the state/age/year level. We do this both at the child level as well as the family level, since making a larger fraction of the family eligible may have considerable spillovers. We first estimate the effect of any public health insurance eligibility on health insurance status to compare the effect with that reported in other data sets. We then estimate the effect of public health insurance participation (instrumented in the same manner described above) on children’s use of health care and health status (e.g. a parental report of child’s health, whether the child has any limitation of activity, number of doctor visits in past 12 months, number of school days lost to illness in past 2 weeks and 12 months, and a dummy indicating whether the child needed prescription drugs but could not get them in past 12 months). To examine the effects of welfare reform, we use a treatment and control group approach to study the health and health care outcomes for children of single lowskilled mothers before and after welfare reform relative to children of married mothers. In the case of the EITC we take advantage of withinstate changes over time in the generosity of state EITC supplements, as well as the fact that children in different families (married vs. single for example) are differentially affected by these supplements. Population Studied: Low-income children from the 1990-2002 National Health Interview Survey. Principal Findings: Our preliminary analysis shows that public insurance eligibility increased for all children from 1997-2002; eligibility increased especially between 1998 and 1999 with the greatest increase for children ages 6-19. We also find a greater increase in public insurance among children living at 100-200% of the Federal Poverty Line, particularly among older children. Conclusions: This study adds to our understanding of the effects of important social assistance programs on children’s health. In particular, we examine both parents’ and children’s public health insurance eligibility and participation using more recent data, as well as focus on children’s health status and other health-related outcomes. Implications for Policy, Delivery or Practice: The U.S. has seen a slow improvement in child health over the past several decades (Federal Interagency Forum on Child and Family Statistics (FIFCFS) 2004). Although the health gap between low- and high-income children decreased slightly over the years, low-income children remain consistently and considerably less healthy compared to high-income children (FIFCFS 2004). In light of this, it is critical to understand how changes in social welfare policies during the 1990s may have influenced child health. Call for Panels Improving the Quality of Depression Treatment for Ethnic/Racial Minorities Chair: Margarita Alegria, Ph.D. Monday, June 4 • 4:30 p.m.-6:00 p.m. Panel Overview: This panel presents findings from four papers that analyze the provision of quality depression treatment to ethnic/racial minorities and the economic burden of depression in minority populations. All of the papers are based on new data from the combined National Latino and Asian American Study (NLAAS) and the National Comorbidity Survey Replication (NCS-R), one of the most comprehensive data sources available that can be used to study these topics. The objectives of the four papers are: 1) to compare the quality of depression treatment that ethnic/racial minorities receive relative to what non-Latino whites receive; 2) to analyze differences in rates of co-morbidity between chronic physical health conditions and depression across racial/ethnic groups; 3) to compare rates of retention in depression treatment for minorities compared to non-Latino whites; and 4) to estimate and compare the effects of depression on labor market outcomes in minority and majority populations. Findings from the first three papers will supply mental health service providers, researchers, and policy makers with the most recent and best available data related to optimizing assessment, treatment, and retention of ethnic/racial minority patients with depression. Results from the fourth paper will be useful in demonstrating to decision makers that expanding access to high-quality patientcentered depression treatment is not only justified on equity grounds but also on economic grounds. As a whole, findings from this session can be used to target resources, develop public policies, and inform guidelines aimed at making depression prevention and treatment services responsive to the needs of ethnic/racial minorities. Appropriateness and Intensity of Depression Treatment for Ethnic/Racial Minorities Margarita Alegria, Ph.D., Pinka Chatterji, Ph.D., Norah Mulvaney-Day, Ph.D., Lisa Fortuna, M.D., David Takeuchi, Ph.D. Presented by: Margarita Alegria, Ph.D., Director and Professor, Center for Multicultural Mental Health Research, 120 Beacon Street, 4th Floor, Somerville, MA 02143, Phone: (617) 503-8447, Fax: (617) 503-8430, Email: malegria@charesearch.org Research Objective: This paper compares the quality of the depression treatment that ethnic/racial minorities receive to that of nonLatino whites, as well as identifies other individual correlates of receiving quality depression treatment. Study Design: Our analytic sample is limited to NLAAS/NCS-R respondents with last year DSMIV diagnosis of major depression or dysthymia and respondents who are sub-threshold cases of depression. We construct quality measures that capture the appropriateness and the intensity of treatment. Appropriateness of treatment is measured by a dummy variable indicating if either of the following two criteria is met during a 12-month period: 1) four or more visits of at least five minutes of counseling, or 2) antidepressant medication with medical supervision. Intensity of treatment is captured by a continuous index which proxies the average value of treatment services used in the past year. This index is constructed by multiplying the quantity of mental health services reported by the respondent in the 12-month period by the national average prices paid for services, obtained from the 2002 Medical Expenditure Panel Survey (MEPS). We conduct regression analyses to evaluate the effect of ethnicity/race on quality of treatment. Demographic and socioeconomic status (SES) covariates included in the regression model include race/ethnicity (non-Latino white as the baseline, Latino, Asian, African-American, Other), poverty level, age category (18-34 as the baseline, 35-49, 50-64, 65+), gender, marital status, education level, region, nativity, language of interview, insurance (uninsured as the baseline, private insurance, Medicare, Medicaid/other public programs) and a HMO indicator based on whether the respondent belongs to an HMO. Population Studied: The combined National Latino and Asian American Study (NLAAS) and the National Comorbidity Survey Replication (NCS-R) (pooled, N = 14,146) is one of the most comprehensive national data sources available that can be used to study depression treatment for ethnic/racial minorities. Both the NLAAS and NCS-R studies are part of the NIMH Collaborative Psychiatric Epidemiology Surveys (CPES), which focus on collecting epidemiological information on the risk factors for mental disorders as well as extensive information on service usage among the general population with special emphasis on minority groups. Principal Findings: Preliminary findings indicate that after controlling for other factors, AfricanAmericans in need of depression treatment are much less likely to receive appropriate care compared to non-Latino whites in need of depression treatment (OR: 0.33, p-value = 0.03). Respondents classified as ‘‘Other’’ had similarly low odds of receiving appropriate care compared to non-Latino whites (OR: 0.20, p-value=0.03). Medicaid insurance coverage (versus being uninsured) increased the likelihood of receiving appropriate care, as did being in an older age group (compared to the 18 to 34 age group). Models of treatment intensity are in progress. Conclusions: These findings suggest that there are important racial/ethnic disparities in receipt of appropriate depression treatment among depressed individuals. Implications for Policy, Delivery or Practice: This information will help policymakers make multi-tiered recommendations to address gaps in service provision for depression for minorities, and to generate concrete solutions for improving quality of care. Funding Source(s): RWJF Comorbid Chronic Physical Conditions and Depression Across Racial and Ethnic Groups Norah Mulvaney-Day, Ph.D., Margarita Alegria, Ph.D., Pinka Chatterji, Ph.D., Lisa Fortuna, M.D., David Takeuchi, Ph.D. Presented by: Norah Mulvaney-Day, Ph.D., Associate Director, Center for Multicultural Mental Health Research, 120 Beacon Street 4th Floor, Somerville, MA 02143, Phone: 617-5038448, Fax: 617-503-8430, Email: nmulvaneyday@charesearch.org Research Objective: The objective of this paper is to analyze racial/ethnic differences in comorbid depression and other chronic physical health conditions, and test for differences in service patterns across groups. Study Design: This descriptive analysis compares the rates of comorbidity between depressive disorder and seven chronic health/pain conditions across race/ethnicity (non-Latino whites, Latino, Asian, AfricanAmerican, and Other), controlling for age and gender. Health conditions considered were asthma, diabetes, hypertension/cardiovascular disease, any chronic health condition, back/neck pain, headaches and any chronic pain condition. Bivariate tests were conducted to identify significant differences across racial and ethnic groups for all comorbid depression and health conditions. Differences in service patterns for those with comorbid conditions were analyzed, including use of antidepressant medication and whether the individual spoke with a primary care physician about mental health concerns. Population Studied: The combined National Latino and Asian American Study (NLAAS) and the National Comorbidity Survey Replication (NCS-R) (pooled, N = 14,146) is one of the most comprehensive national data sources available that can be used to study depression treatment for ethnic minorities. Both the NLAAS and NCSR studies are part of the NIMH Collaborative Psychiatric Epidemiology Surveys (CPES), which focus on collecting epidemiological information on the risk factors for mental disorders as well as information on service usage among the general population with special emphasis on minority groups. Principal Findings: There were few differences in rates of comorbid depression and any of the three chronic health conditions (diabetes, asthma, or cardiovascular disease) across ethnic and racial groups. Asians and Latinos had lower rates of comorbid depression and any chronic illness while those who where classified as ‘‘Other’’ had higher rates of comorbidity, compared to non-Latino whites. Across chronic pain conditions, Latinos, Asians and African Americans tended to have lower rates of comorbidity with depression, while those classified as ‘‘Other’’ had higher rates than nonLatino whites. Looking at the service patterns, Asians, Latinos and African Americans with comorbid depression and chronic pain were less likely to be asked about their mental health by a primary care physician than non-Latino whites with a similar profile. Although all ethnic/racial minority categories had lower rates of antidepressant use than non-Latino whites for both the chronic illness and chronic pain categories, these differences were not significant in the bivariate models. Multivariate models looking more closely at antidepressant use are currently in progress. Conclusions: This descriptive analysis suggests lower rates of comorbid chronic health/pain problems and depression among racial and ethnic minorities, with the exception of those who are classified as ‘‘Other.’’ However, differences exist in primary care physicians’ assessment of comorbidity in minority patients. Implications for Policy, Delivery or Practice: Quality improvement programs for depression screening in primary care should target multiple chronic health conditions across racial and ethnic groups. Physicians who treat minority patients with chronic pain should inquire about their mental health. Funding Source(s): RWJF Staying in Treatment: Factors Associated with Retention in Depression Care Among Ethnic/Racial Minorities Lisa Fortuna, M.D., Margarita Alegria, Ph.D., Pinka Chatterji, Ph.D., Norah Mulvaney-Day, Ph.D., David Takeuchi, Ph.D. Presented by: Lisa Fortuna, M.D., Psychiatrist, Center for Multicultural Mental Health Research, 120 Beacon Street, 4th Floor, Somerville, MA 02143, Phone: 617-503-8485, Fax: 617-503-8430, Email: lfortuna@charesearch.org Research Objective: The objective of this paper is to identify patient and health system factors associated with retention in depression care among ethnic/racial minorities in the U.S. as compared to non-Latino whites. Study Design: Our analytic sample is limited to NLAAS/NCS-R respondents with sub-threshold depressive disorders or fulfilling full criteria for depressive disorders in the last year and at least one mental health visit during the last year or no visits but stating that they dropped out of care. We conduct a series of regression analyses to evaluate the main effect of ethnicity/race on retention in treatment as well as sequentially adding measures of potential mechanisms related to retention in care. Our dependent variable of interest is a binary outcome of retention in care defined by at least 4 mental health care visits in the last 12 months or fewer visits but currently reporting being in care coded as one; and zero otherwise. Demographic and socioeconomic status (SES) covariates included in the regression model include race/ethnicity (non-Latino white as the baseline, Latino, Asian, African-American, Other), poverty level, age category (18-34 as the baseline, 35-49, 50-64, 65+), gender, marital status, education level, region, nativity, language of interview, insurance (uninsured as the baseline, private insurance, Medicare, Medicaid/other public programs) and a HMO indicator based on whether the respondent belongs to an HMO. We use data from all racial/ethnic categories to fit the best empirical model, reporting differences in retention in care for depression in African Americans, Asians, Latinos, and Other group relative to non-Latino whites. Population Studied: The combined National Latino and Asian American Study (NLAAS) and the National Comorbidity Survey Replication (NCS-R) (pooled, N = 14,146) is one of the most comprehensive nationally representative data sources available that can be used to study depression treatment for diverse groups of ethnic minorities. Both the NLAAS and NCS-R studies are part of the NIMH Collaborative Psychiatric Epidemiology Surveys (CPES). Principal Findings: Preliminary findings indicate that after controlling for other factors, Latinos (OR: 2.22, p-value .06) with depression or dysthymia are more likely to be retained in depression care as compared to their non-Latino white counterparts. Asians, on the other hand, were considerably less likely than non-Latino whites to be retained in care (OR: .40, p-value: .087). These effects are statistically significant at the .10 level. Having Medicaid (OR: 2.7, pvalue=.02) or Medicare (OR: 4.4, p-value=.04) is associated with higher likelihood of retention in treatment. Conclusions: These findings suggest that there are important racial/ethnic differences in retention in depression care with both patient and systems factors, including type of insurance coverage, associated with this outcome. Implications for Policy, Delivery or Practice: Identifying important correlates of retention in treatment is likely to be useful in clinical care and service planning for ethnic/racial minority patients with depression. Funding Source(s): RWJF Estimating the Effects of Depression on Labor Market Outcomes in Diverse Populations Pinka Chatterji, Ph.D., Margarita Alegria, Ph.D., Norah Mulvaney-Day, Ph.D., Lisa Fortuna, M.D., David Takeuchi, Ph.D. Presented by: Pinka Chatterji, Ph.D., Health Economist, Center for Multicultural Mental Health Research, 120 Beacon Street, 4th Floor, Somervile, MA 02143, Phone: 617-503-8449, Fax: 617-503-8430, Email: pchatterji@charesearch.org Research Objective: The objective of this paper is to estimate and to test for racial/ethnic differences in the association between depression and labor market outcomes. Study Design: We use probit models to estimate the association between depression and labor market outcomes. Because of the differences in the labor market pathways of men and women, we run all analyses separately by gender. Our dependent variables are the following dummy indicators: currently employed full-or part-time, absent from work at least once in the past month among those employed, and received any form of public assistance in the last year. Our main covariate of interest is a dummy variable indicating whether or not the respondent meets criteria for depressive disorders in the past year. All models include controls for age, marital status, education, number of household members under age 18, physical health, and psychiatric co-morbidities. Since reverse causality and unobserved heterogeneity are concerns, we test whether main findings are sensitive to these issues by creating gender/race sub-samples for sensitivity analyses. Using these sub-samples, we estimate bivariate probit models, in which the employment/public assistance and depression equations are estimated simultaneously. Population Studied: The combined National Latino and Asian American Study (NLAAS) and National Comorbidity Survey Replication (NCSR) (Pooled, N= 14,146) is one of the most comprehensive national data sources available that can be used to study depression treatment for ethnic minorities. Both the NLAAS and NCSR studies are part of the NIMH Collaborative Psychiatric Epidemiology Surveys (CPES), which focus on collecting epidemiological information on the risk factors for mental disorders as well as extensive information on service usage among the general population with special emphasis on minority groups. Principal Findings: Preliminary findings based on NLAAS indicated that having depression or dysthymia in the past 12 months is associated with statistically significant reductions in the probability of being employed of about 10 percentage points for Latino males and about 23 percentage points for Latino females. There are no statistically significant associations between depressive disorders and employment among Asian models of other outcomes and bivariate probit models based on the combined NLAAS/NCS-R sample are in progress. Conclusions: As a whole, the findings indicate that depression imposes labor market costs on Latinos that are at least as large and as important as those found in studies based on mostly non-Latino white samples. Implications for Policy, Delivery or Practice: Our results suggest that there may be important labor market benefits associated with public health policies targeted at the prevention and effective treatment of depressive disorders in racial/ethnic minority groups. Funding Source(s): RWJF Call for Panels Post Acute Care: Changing with the Times Chair: Marilyn Moon, Ph.D. Monday, June 4 • 4:30 p.m.-6:00 p.m. Panel Overview: Medicare policies and post acute provider responses changed subtly over the past few years. New payment policies went into effect for each of the providers since 1998, attention to IRF certification policies was renewed, and access to services shifted for certain populations as the new PPS underwent incremental adjustments. These changes have taken place in an environment concerned with developing pay for performance initiatives that reward good outcomes and create efficiencies. This panel examines the impact of these policy changes on post-acute payments, utilization, and provider specialization for skilled nursing facilities, inpatient rehabilitation facilities, home health agencies, and long-term care hospitals. The four papers presented here explore the impact of these changes both within and across post-acute care settings. The first paper examines whether differences in severity exist among admissions to different settings. The second paper focuses on the rehabilitation population and their trajectory following discharge. The third paper addresses whether IRFs specialize in certain populations, and discusses alternative measures of specialization that focus on economies of scope and scale. The fourth paper looks at the more medically intensive populations treated in both acute hospitals and Long Term Care Hospitals and examines margins for similar cases treated in these settings. These papers are part of a larger CMS effort to re-examine the incentives in Medicare’s PAC payment policies and how they may affect Medicare program costs and beneficiary outcomes. These issues are important as insurers call for better information on which to develop pay for performance methods. A New Era: Post Acute Use Under PPS Barbara Gage, Ph.D., Melissa Morley, Ph.D., Jeremy Green, B.A. Presented by: Barbara Gage, Ph.D., Deputy Director, Aging, Disability and LTC, RTI International, 1440 Main Street, Suite 310, Waltham, MA 02451, Phone: (781)-434-1717, Email: bgage@rti.org Research Objective: The purpose of this study was to examine how case mix severity affects variations in post-acute utilization. Study Design: Retrospective claims analysis of episodes of post acute care. Episodes of care were created for the first acute hospital discharge of the year and included claims from subsequent inpatient rehabilitation, long term care hospitals, skilled nursing facilities, home health agency, and outpatient therapy services. The All Patient Refined DRG, APR-DRG, software was used to assign a minor, moderate, major, or extreme severity of illness subclass to each hospital admission. Binomial and multinomial logistic regression models were used to test factors predicting the probability of using any PAC following hospital discharge, and to predict the first site of post-acute care. Population Studied: The study population included Medicare beneficiaries with an acute hospital discharge in 2004. The data source was the 2004 Medicare claims and denominator files for a 5-percent sample of beneficiaries. Principal Findings: About one-third of all inpatient hospital discharges in 2004 used some type of PAC. Of those who used PAC, the majority were discharged to a SNF, 41.5 percent. Another 36 percent were discharged to HHA; 13.5 percent to IRFs and 2.2 percent to LTCHs. The average severity of illness level for PAC users was slightly higher than for non-PAC users. Over 36 percent of PAC users were in the two highest APR-DRG severity of illness subclass groups while the non-PAC users had 20.3 percent in the higher severity groups. Analysis of discharges by APR-DRG severity index revealed that those with the highest severity were more likely to be discharged to an institutional setting, particularly a SNF, while those with the lowest severity were more likely to use ambulatory services. After controlling for demographics, severity of illness, medical conditions, and supply of services, the regression results suggested that the most important factors for predicting PAC use and first site of PAC care included specific DRGs, the APR-DRG severity of illness measure, and age. Beneficiaries ages 85 and over were 4.8 times as likely to use PAC services compared to younger beneficiaries. The odds of any PAC use for beneficiaries in the major severity subclass were 57 percent higher than beneficiaries in the minor severity subclass. Beneficiaries classified as extreme severity were 8.3 times more likely to use LTCH than beneficiaries classified as minor severity. Conclusions: These analyses reveal significant differences in the populations using each type of PAC setting. While many of the services in PAC settings are similar, the multinomial model identifies certain factors that clearly distinguish differences in the probability of using each type of setting. The severity measures provide important additional insight into clinical distinctions that may explain differences in PAC level of care needs. Implications for Policy, Delivery or Practice: These findings will be useful as the Medicare program continues to refine its payment systems and the definitions of which populations are appropriate for admission to each of the various PAC settings. Funding Source(s): CMS Changes in IRF Use: Pre and Post PPS Melissa Morley, Ph.D. Presented by: Melissa Morley, Ph.D., Research Associate, RTI International, 1440 Main Street, Suite 310, Waltham, MA 02451, Phone: (781)-4341773, Email: mmorley@rti.org Research Objective: The goal of this study is to investigate whether the populations treated at inpatient rehabilitation facilities, IRFs, have changed in intensity since the implementation of the prospective payment policies in 2002. Study Design: Episodes of care were created for IRF discharges and included claims from subsequent IRF, acute hospital, long term care hospital, skilled nursing facility, home health agency, and outpatient therapy services. The All Patient Refined DRG, APR-DRG, software was used to assign a minor, moderate, major, or extereme severity of illness subclass. Bivariate and multivariate analyses were used to examine differences in diagnoses, severity, length of stay, and payment between 2000 and 2003. Population Studied: The study population included Medicare beneficiaries with an IRF discharge and a prior acute hospitalization in 2000 and 2003. The data source for the analyses was Medicare claims and denominator files for 100% of beneficiaries admitted to IRFs in 2000 and 2003. Principal Findings: The volume of IRF admissions increased by 26 percent from 2000 to 2003, corresponding with a 7 percent increase in the number of IRF providers nationwide. Overall, the severity of beneficiaries admitted to IRFs was slightly higher in 2003 compared to 2000. In 2003, 34 percent of beneficiaries were in the two highest severity of illness groups compared to 32 percent in 2000. Despite the increase in severity, lengths of stay in IRFs were shorter in 2003 compared to 2000, 12.2 days versus 13.8 days. The types of admissions to IRFs also shifted slightly between 2000 and 2003. The three most common types of admissions were DRG 209:Major Joint & Limb Reattachment Procedures of Lower Extremity; DRG 014:Specific Cerebrovascular Disorders except TIA; and DRG 210: Hip & Femur Procedures except Major Joint. The volume and relative ranking of admissions for heart-related conditions including DRG 015: Transient Ischemic Attack & Precerebral Occulsuion and DRG 127: Heart Failure & Shock increased from 2000 to 2003. As expected, length of stay and payments increased with severity of illness. In 2003, 27 percent of IRF admissions for DRG 210 were major or extreme severity compared to 22.8 percent in 2000. The IRF admission lengths of stay for these admissions decreased in 2003. Similar patterns were also observed in other DRGs. Discharge from a short-stay acute hospital was also found to be related to longer IRF length of stay. Conclusions: The number of Medicare IRF admissions and providers continued growing between 2000 and 2003, despite the move from TEFRA-based payments to PPS. After the implementation of prospective payment, the relative mix of diagnoses shifted somewhat, severity of admissions increased, and lengths of stay decreased suggesting that the population treated in IRFs increased in intensity from 2000 to 2003. Other administrative changes in Medicare’s coverage policies may have contributed to these changes. Implications for Policy, Delivery or Practice: The increase in severity of illness in the IRF settings is important for policymakers to understand when considering quality of care in IRF settings and further post-acute care payment reform. Funding Source(s): CMS Medicare Margins Analysis for Long-Term Acute Care Hospitals Kathleen Dalton, Ph.D., Barbara Gage, Ph.D. Presented by: Kathleen Dalton, Ph.D., Senior Research Economist, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709, Phone: (919) 541-5919, Email: kdalton@rti.org Research Objective: 1.To document the impact of prospective payment on long-term acute, LTCH financial performance by analyzing variation in LTCH Medicare margins across facilities and types of cases. 2. To evaluate the new LTCH cost weights by identifying systematic but unintended differences in profitability across DRGs. Study Design: Retrospective analyses of payments, charges and costs from facility cost reports and Medicare LTCH claims. Claims-level costs are estimated using service and facility specific, cost/charge ratios. Claims-level regression models identify adjusted differences in payment-to-cost ratios by DRG after controlling for patient attributes as well as fixed facility effects. Population Studied: Facility-level samples include all LTCHs with cost reports filed from FY 2001 through FY 2004. Claims-level samples include all post-PPS Medicare discharges that could be matched to LTCH cost reports, restricted to facilities that chose to receive payment under 100 percent federal rather than partially phased-in PPS rates. Principal Findings: Medicare and overall facility margins rose dramatically after PPS implementation. Public LTCHs had significantly lower margins both before and after PPS. Median PPS margin was higher among forprofits than others and higher for facilities that were recently certified than for older facilities. At the individual case level, margins varied substantially across DRGs even after stratifying to remove the effects of high-cost outliers, 6 percent of sample, or short-stay outliers, 40 percent of sample. By DRG, average margins were lowest for Rehabilitation, -0.1percent, and highest for Ventilator Support, +21.3 percent. Aggregate margin across all non-outlier cases was +17.4 percent, compared to +13.8 percent for short-stay outliers and -14.3 percent for high-cost outliers. Variation in profitability across DRGs was even greater in the multivariate models than in the descriptive statistics computed across cases. Regression results also confirm high underlying levels of profitability; for a base non- outlier case in 2005 that was admitted as an acute hospital transfer and discharged to home and had a DRG weight equal to 1.00, predicted PPS payment was 23.2 percent above cost. Conclusions: Unusually high average profitability in the first two years of LTCH PPS indicates that the initial PPS base rate was more generous than intended. Variation in profitability across DRGs also suggests substantial bias in the DRG weights, where weights have been systematically overstated for cases using relatively more ancillary services and understated for cases relying more on nursing care. Implications for Policy, Delivery or Practice: Smaller updates in the base rate were implemented for LTCH PPS rules in FY 2006 and 2007, and may have brought underlying LTCH PPS profitability back in line with other Medicare PPS. DRG-level variation suggests additional work is needed for estimating costbased weights, such as those being phased in between 2007 and 2010 for short-stay DRGs. As improved cost-based weights are implemented, the profitability of LTCHs specializing in respiratory care, in particular, may be strongly challenged. Funding Source(s): CMS Inpatient Rehabilitation Facilities: Alternative Definitions of Hospital Specialization Roberta Constantine, Ph.D. Presented by: Roberta Constantine, Ph.D., Research Associate, RTI International, 1440 Main Street, Suite 310, Waltham, MA 02451, Phone: (781) 434-1711, Email: rconstantine@rti.org Research Objective: Inpatient Rehabilitation Facilities, IRFs, must meet the 75 percent rule to qualify for IRF PPS rates in the Medicare program. This study analyzes alternative definitions of IRF specialization that could be used to determine appropriateness of IRF admissions, including measures of volume or intensity rather than types of conditions. Study Design: Retrospective analyses of Medicare claims, Inpatient Rehabilitation Facility Patient Assessment Instrument, IRF-PAI, and Medicare certification data to examine variations in hospital specialization in treating certain types of patients. Twenty-one Rehabilitation Impairment Categories, RICs, were utilized to categorize admissions. Specialization was defined in terms of 3 definitions: proportion of total admissions in RIC groups, volume of admissions in RIC groups, and proportion of all RIC cases nationally per provider. These measures were used to examine the relationship between specialization and functional outcomes at discharge. Population Studied: 100 percent of Medicare IRF admissions with discharge dates between June 2004 and June 2005 that could be matched to an IRF-PAI report. Principal Findings: This study showed that the average FIM score at admission was 65 suggesting patients were fairly impaired at the time of admission. These admission scores ranged but the highest mean and modal scores were between the mid-70s and 80 for populations having Non-Traumatic Spinal Cord Injuries and Replacement of the Lower Extremity Joint. The lower end of impairment scores at admission were in the 50s for Stroke cases and the trauma-related cases. The average length of stay was 14 days but the mean varied by RIC from 10 days for Replacement of the Lower Extremity Joint to 21 days for Traumatic Spinal Cord Injury and Guillain-Barre. Virtually all IRFs had at least one Stroke admission, 99.8 percent, but relatively few, 12.2 percent, had at least one Burn admission. Examining volume of admissions by RIC, admissions ranged from a high of 5 admissions for Guillain-Barre to 1,612 for total admissions. As a percent of total admissions to an IRF, the percent of admissions for a RIC ranged from less than 1 percent for Burns to 22.4 percent for Replacement of Lower Extremity Joint. The third definition of specialization, by the proportion of all RIC cases nationally per provider, ranged from less than 1 percent to as high as 18 percent for Burns. Next, we created four variables for each RIC based on whether the IRF had a proportion of total admissions in certain RIC groups and volume of admissions in RIC group. Finally, we tested whether specialization had an affect on FIM score. Conclusions: This analysis attempts to define specialization for an IRF; an important step in defining what an IRF does and whether this has an affect on patient outcomes. The results showed that outcomes were better for certain populations in facilities specializing in these populations, particularly for those conditions with smaller volume. Implications for Policy, Delivery or Practice: IRFs are the only Medicare hospitals certified on the basis of admitting certain diagnoses. These results will be useful for examining alternative definitions of IRF certification. Funding Source(s): CMS Call for Panels Impact of Florida Legislative and Regulatory Innovations on Nursing Home Turnover, Tenure, Financial Performance and Quality of Care Chair: Kathryn Hyer, Ph.D., M.P.P. Tuesday, June 5 • 9:00 a.m.-10:30 a.m. Panel Overview: Florida is a harbinger of national long-term care issues because of its proportion of residents in the 85+ age group. Florida ranks sixth nationally in nursing home beds, has the nation’s highest mandated nursing home staffing levels and Florida’s bed growth rate is ten times the national average of 2%. Competition from assisted living facilities for residents and staff is keen. From 1999-2007 Florida’s State Legislature implemented several initiatives designed to improve quality in nursing homes. Legislative innovations include financial incentives to increase nurse staffing, mandates to increase paraprofessional staffing over 5-years, improved Medicaid reimbursement, tort reform, enhanced monitoring and new reporting requirements. Current Population survey data is used to explore national nursing turnover and tenure in long term care industry with special attention to Florida. Reconciling data for from three Current Population Survey reports this paper compares turnover rates of LTC workers within the LTC industry and with similarly skilled workers in competing industries. In addition to comparing turnover and tenure by nursing levels, the relative importance of compensation, training, and benefits on turnover are calculated. Nursing home data (Florida State reports, Medicare and Medicaid Cost Reports, Minimum Data Set (MDS), the On-line Survey Certification of Automated Records (OSCAR) file, and the Area Resource File (ARF)) is matched at the facility level to provide comprehensive understanding of how quality innovations and legislative mandates impact administrative tenure and turnover, staffing and financial performance, stability of workforce and quality outcomes in Florida’s long-term care facilities. Mandates Matter: Florida Nursing Home Provider Response to Financial Incentives to Increase Nurse Staffing Kathryn Hyer, Christopher E. Johnson, Ph.D., Jeffery Harman, Ph.D., Mishu Popa, M.S.G., Robert Weech-Maldonado, Ph.D., M.B.A. Presented by: Kathryn Hyer, 13301 Bruce B. Downs Boulevard MHC 1323, Tampa, FL 33612, Phone: 813-974-3232, Email: khyer@cas.usf.edu Research Objective: Florida’s State Legislature provided $40 million (annualized) in the Medicaid Direct Care Staffing Adjustment (DCSA) as an add-on to the patient care component of the Medicaid per diem rate in nursing homes. The financial incentives allowed providers freedom in spending money as long as total resources for direct care staffing increased over baseline. This pre- post- study assesses how the nurse staffing incentives beginning in April 2000 (compared to 1999) were used by nursing homes to increase hours per resident day, increase wages of current staff or to change use of agency staff. We examine impact for the RN, LPN and CNA staffing levels, and analyze if the incentive resulted in sustained higher staffing levels. The impact of nurse staffing change on quality is measured by deficiencies and quality measures. Study Design: The data comes from Florida State reports, Medicare and Medicaid Cost Reports, Minimum Data Set (MDS), the On-line Survey Certification of Automated Records (OSCAR) file, and the Area Resource File (ARF) for the period of 1999-2001. Facilities were categorized into quartiles (N=145) receiving most incentive money and least incentive money. The dependent variable, quality of care is measured by deficiencies, chronic (ADL improvement, fractures, pain, pressure sores), and post-acute outcomes (pain, walk improvement, pressure sores). Independent variables consist of structure (staffing ratios), process (restraints and catheters), and control variables (ownership/chain affiliation, Herfindahl index, payer mix, case mix, and size). Quality indicators were calculated for the six month period immediately preceding implementation and for six months following the incentive. A loglinear multivariate regression model assessed the impact of incentive payments on quality indicators. Population Studied: Medicaid and medicare nursing homes in Florida from 1999-2002. The analysis of 595 Florida homes certified as Medicaid homes that participated in the financial incentive programs Principal Findings: When offered incentives, providers in top quartile of incentives responded differentially from providers in lowest quartile. Quartile receiving the most money ($68,117) increased total nurse staffing from 1.77 hours per resident day to 2.08 hours per resident day, wages stayed stable and use of agency increased. Facilities receiving least money ($34,163) decreased from 2.54 to 2.33 hours per resident day, increased wages for paraprofessionals and decreased use of agency. The lowest staffed highest Medicaid facilities increased RN, LPN and CNA staffing but higher staffed homes decreased highest skill nurses and substituted lower cost nurses. Difference in difference results indicate pressure sore quality measures were significant. Conclusions: Providing incentives results in absolute dollar increases allocated to direct care staff but skill mix decreases and total hours per resident day may not increase. Difference in differences shows mixed quality outcomes and suggests threshold needs to be reached before quality differences can be seen. Implications for Policy, Delivery or Practice: Legislatures wanting increased direct care staffing per resident need mandates. Providers, when given choice respond differentially but substitute lower skilled workers for higher skilled workers and increase wages for current workers. The implications of skill mix on quality outcomes are uncertain, especially since staffing per resident day remain below CMS preferred levels Funding Source(s): CWF, Administration on Aging Employee Turnover in the Long-Term Care Industry David Macpherson, Ph.D., William Even, Ph.D. Presented by: David Macpherson, Ph.D., Rod and Hope Brim Eminent Scholar in Economics, Director of the Pepper Institute on Aging and Public Policy, Florida State University, Mail Code: 2180, Florida State University, Tallahassee, FL 32306, Phone: (850) 644-3586, Email: dmacpher@mailer.fsu.edu Research Objective: The presentation will discuss several potential causes of understaffing in the long-term care (LTC) industry. First, we present measures of the extent of turnover in several key occupations within the LTC industry and discuss the importance of compensation, training, worker characteristics and working conditions on the extent of turnover. We compare the turnover rates of LTC workers with similarly skilled workers in competing industries and explain the source of differentials in the turnover rate. Second, the presentation will provide evidence on the source of workers moving into the LTC industry and the destination of workers moving out of the industry. Study Design: Current Population survey data is used to explore national nursing turnover and tenure in long term care industry with special attention to Florida. Registered nurses, licensed nurse, health, personal and home care aides and nursing aides, orderlies and attendants------are tracked from 1989-2002. Employee turnover can be reduced with a variety of incentives that are not equally effective. Direct comparison of cost effectiveness of approaches to reducing turnover to policies increasing wages or fringe benefits is not possible. Reconciling data from three Current Population Survey reports, this paper compares turnover rates of LTC workers within the LTC industry with similarly skilled workers in competing industries. In addition to comparing turnover and tenure by nursing levels, the relative importance of compensation, training, and benefits on turnover are calculated. Population Studied: Detailed examination of worker turnover in nursing and personal care industry for four key occupations: RN, LPH, nurse aides and health aides. Three different data sets were employed and several measures of turnover are examined. Principal Findings: Different measures of turnover can lead to different conclusions regarding whether workers have higher turnover than other groups. A single measure does not address all concerns. Regression analysis used to determine the influence of worker and job characteristics on turnover reveal improved pension and health insurance reduces turnover in all nursing levels. Unionism and job training reduce turnover but environmental disamenities or physical demand increase turnover. In a comparison of increased wages, pension coverage or health insurance, pension coverage is the lowest cost approach to reducing turnover. Conclusions: Employee turnover can be reduced with a variety of incentives that are not equally effective. Direct comparison of cost effectiveness of approaches to reducing turnover to policies increasing wages or fringe benefits is not possible Implications for Policy, Delivery or Practice: This information is important to understanding how future changes in the U.S. economy are likely to influence the supply and demand for long-term care workers. While this study provides evidence on how to reduce employee turnover questions remain about how turnover is affected by working conditions and staffing levels and how low-cost facilities may impact turnover. Funding Source(s): Administration on Aging Impact of Top Management Tenure on Nursing Home Turnover and Quality Christopher Johnson, Ph.D., Kathryn Hyer, Ph.D., Jeffery Harman, Ph.D., Robert WeechMaldonado, Ph.D., M.B.A., Mishu Popa, M.S.G. Presented by: Christopher Johnson, Ph.D., Associate Professor, Department of Health Policy and Management, School of Rural Public Health, Room 311 SRPH Building, College Station, TX 77843-1266, Phone: (979) 458-4165, Email: cejohnson@srph.tamhsc.edu Research Objective: The objective of the is research is to examine the impact of nursing home top management (administrator and director of nursing) tenure on nursing staff turnover and quality of care in Florida nursing homes. We hypothesize that organizations with higher administration turnover rates have higher nursing staff turnover and poorer quality of care outcomes Study Design: We analyzed the impact of nursing home administrator and director of nursing (DoN) tenure from 2002-2004 using Florida Medicaid Nursing Home Staffing Reports for 580 Medicaid nursing homes, CMS’ Online Survey Certification and Reporting (OSCAR), Medicare Cost reports, State of Florida Medicaid Cost reports, CMS Minimum Data Set (MDS) and Area Resource File (ARF). Tenure was defined as the administrator or DoN being the same for the 12-month period of the Nursing Home Staffing Reports for that year. The dependent variables include 1) turnover (certified nursing assistant and licensed nurses) and 2) change in quality of care from previous year (MDS activities of daily living, fractures, and pressure sore chronic care indicators). The independent variables include 1) administrator and DON salary, 2) administration tenure, 3) facility resources, 4) facility characteristics, 5) county demographic variables, and 6) county market factors. These variables were analyzed using a two-staged least squares regression to adjust for potential endogeniety between staffing and administration tenure, and to analyze the impact of the adjusted variables on nurse staff tenure and quality of care. Population Studied: All Medicaid certified nursing homes in Florida. Principal Findings: Tenure trends in nursing home administrator and DoNs in Florida followed similar patterns of sharp decline in 2003 (from roughly 22% being present for one year to 18%) and modest increases during 2004 (to roughly 20%), but not to the higher 2002 levels. Higher certified nursing assistant and licensed nurse turnover rates and poorer quality of care were associated with higher tenure rates among top management Conclusions: These results raise questions about the impact that top management stability has on nursing home performance in Florida’s facilities. While some top management turnover may be required (in order to remove ‘‘bad apples’’), there may be a threshold above which facilities will experience decreasing negative results across nursing home performance measures Implications for Policy, Delivery or Practice: Much attention has been spent on turnover within nursing staffs within policymaker efforts to improve quality of care. Approximately 80% of the nursing homes in Florida did not have the same administrator and/or DoN for the entire year during the time period of this study. States and organizations may need to think of ways of increasing tenure in nursing home administrations as part of an overall nursing staff and facility quality Funding Source(s): CWF, Administration on Aging The Relationship between Staffing, Quality, and Financial Performance: For-Profit versus Not-for-Profit Nursing Homes Robert Weech-Maldonado, Ph.D., M.B.A., Christopher Johnson, Ph.D., Zhou Yang, Ph.D., Alex Laberge, M.B.A., Kathryn Hyer, Ph.D. Presented by: Robert Weech-Maldonado, Ph.D., M.B.A., Associate Professor, Department of Health Services Research, University of Florida, College of Public Health and Health Professions, 101 S. Newell Drive, Gainesville, FL 32610-0195, Phone: (352) 273-6080, Fax: (352) 273-6075, Email: rweech@phhp.ufl.edu Research Objective: Nursing homes are experiencing increased revenue constraints as a result of changing reimbursement policies and declining demand for nursing home care. At the same time, nursing homes are facing increasing costs pressures as a result of higher nurse staffing and liability insurance costs. As the financial performance of nursing homes deteriorates, there are concerns that quality of care will also decline. Using Donabedian’s structure, process, and outcomes framework of quality assessment, this study examines the relationship between staffing, quality, and financial performance, and whether this relationship varies by ownership (for-profit versus not-for-profit status). Study Design: The data for this study comes from the Medicare and Medicaid Cost Reports, Minimum Data Set (MDS), the On-line Survey Certification of Automated Records (OSCAR) file, and the Area Resource File (ARF) for the period of 2000-2004. The dependent variable consists of financial performance tier: low (bottom quartile), medium (2nd and 3rd quartiles), and high (upper quartile), based on the operating margin. The independent variables consist of structure (RN, LPN, and CNA staffing ratios), process (use of restraints and catheters), chronic care outcomes (ADL improvement, fractures, pain, pressure sores), and post-acute outcomes (pain, walk improvement, pressure sores). Control variables consist of ownership/chain affiliation, payer mix, case mix, and size. Ordered probit regression is used to model the relationship between financial performance tier and the quality measures, with year as a fixed effect. Standards errors are adjusted for clustering due to repeated observations for facilities over time using Huber/White correction. The models are run for the overall sample, and separately for the for-profit and notfor-profit samples. Population Studied: All Medicare and Medicaid certified nursing homes in Florida for the period of 2000-2004, approximately 575 facilities per year Principal Findings: For the overall sample, better financial performance was characterized by lower RN/LPN ratios but higher CNA ratios, but there were no significant differences in process and outcomes of care by financial performance tier. Among not-for-profit nursing homes, better financial performance was characterized by lower RN staffing, higher CNA staffing, lower fractures, and lower pressure sores (chronic care). While among for-profit homes, those with better financial performance were characterized by lower RN staffing, lower restraints, lower catheters, and higher ADL improvement. Conclusions: The relationship between quality and financial performance varies by type of quality measure. Both for-profit and not-profit nursing homes that have better financial performance have better resident outcomes in some areas, yet have lower RN staffing ratios than those with worse financial performance. However, there are some differences by ownership type. Not-profit homes with better financial performance have higher CNA staffing ratios than not-for-profit nursing homes with worse financial performance, and for-profit homes with better financial performance have better processes of care than for-profit nursing homes with worse financial performance. Implications for Policy, Delivery or Practice: Further research is needed to examine the management strategies of the higher performing nursing homes by which they are able to achieve better processes and outcomes of care with lower RN staffing ratios Funding Source(s): Administration on Aging Call for Panels Medication Use by Aged and Disabled Medicare Beneficiaries across the Spectrum of Morbidity Chair: Stuart Guterman, M.A. Tuesday, June 5 • 10:45 a.m.-12:15 p.m. Panel Overview: The multiplicity of Part D plans and benefit designs available to Medicare beneficiaries raises serious issues regarding the quality of medication use under the new prescription drug benefit. One important and under-studied aspect of medication quality is how overall disease burden affects physician prescribing and patient utilization behavior. This issue is the subject of a Commonwealth Fund sponsored monograph to be published in April 2007 entitled, Chartbook of Medication Use by Aged and Disabled Medicare Beneficiaries across the Spectrum of Morbidity. The Chartbook provides descriptive benchmarks showing how drug utilization varies with overall disease burden for 8 common chronic diseases: diabetes, depression, dementia, COPD, arthritis, hypertension, ischemic heart disease, and heart failure. A major aim of the project collaboration is to generate hypotheses for future research on the relationship between polymorbidity and polypharmacy. This proposed ARM panel includes 5 related papers that follow up on hypotheses generated during the Chartbook collaboration. The first paper describes the project and presents major descriptive findings. The second paper addresses geriatricians’ concerns about overly aggressive treatment at end of life by examining medication profiles for survivors and decedents with diabetes, COPD and CHF. The next two papers examine disparities in medication use for therapies recommended for dementia and depression. They find both racial and age-related disparities that grow wider with increasing disease burden. The final paper addresses a common problem at the nexus of polypharmacy and polymorbidity; namely, growing side effects of use of analgesics and anti-inflammatory agents to treat arthritis. Charting Medication Patterns of Medicare Beneficiaries with Rising Disease Burden: Summary of Findings Research Objective: This paper summarizes findings from the Commonwealth Fund Chartbook of Medication Use by Aged and Disabled Medicare Beneficiaries across the Spectrum of Morbidity scheduled for publication in April 2007. The Chartbook provides nationally-representative benchmarks of drug utilization by Medicare beneficiaries with 8 common chronic diseases: diabetes, depression, dementia, COPD, arthritis, hypertension, ischemic heart disease, and heart failure. It is a reference work designed to help policy makers and health services researchers better understand the complex relationship between medication use and disease burden and to develop a research agenda for addressing suboptimal medication utilization patterns in the Medicare population. A key feature of the Chartbook is that all major classes of pharmaceuticals are profiled for each disease cohort, thereby demonstrating how medication regimens evolve with accumulating morbidity. Study Design: Data come from the 2002 Medicare Current Beneficiary Survey. The study sample comprises fee-for-service communitydwelling beneficiaries divided into 8 diseasespecific cohorts using ICD-9 codes from Medicare claims and self/proxy reports (for selected conditions). Each cohort is divided into deciles or quintiles (depending on sample size) based on beneficiaries’ cumulative annual spending on all medical care services. Medical spending is a useful proxy for overall disease burden and has the further advantage that the study methods that can be readily applied in any payor setting. Variables include: drugs classified by UPS pharmacological and therapeutic category, counts of medication-sensitive conditions from the CMS RxHCC risk adjustment model, drug spending, total medical spending, demographic and socioeconomic characteristics, health status measures, and health system contact variables. Charts for each disease state show how medication intensity changes with quintile/decile of medical spending. Medication intensity measures include: drug spending as a fraction of total medical spending, prescription fills per RxHCC, prevalence and level of drug use by USP category, and prevalence and utilization rates for drugs specifically recommended to treat each of the 8 conditions. The Charts are augmented by extensive appendix tables. All results are weighted to be representative of the Medicare population. Population Studied: Aged and disabled Medicare beneficiaries in 2002 (N = 8,455), with disease-specific cohorts ranging in size from 521 (dementia) to 4,617 (hypertension). Principal Findings: Selected charts from among the 82 contained in the Chartbook will be presented. A consistent finding across the 8 diseases is that medication intensity increases with spending to a plateau and then declines. This inverted U shape pattern is observed in each of the medication intensity measures, albeit the steepness of the rise and fall as well as the peak threshold points varies by disease and drug measure. Suboptimal use of recommended agents is found at both ends of the spectrum. Conclusions: The Chartbook presents only unadjusted cross-tabulations and further research is necessary to identify the reasons behind the unusual inverted U shape patterns in medication use observed among Medicare beneficiaries with the 8 diseases. Implications for Policy, Delivery, or Practice: The Chartbook provides an overview of the ‘‘medication landscape’’ pre-MMA that will help policy makers design and target quality initiatives under Part D. Medication Use by Community Dwelling Medicare Beneficiaries at the End of Life: Is it Too Much Too Late? Research Objective: Geriatricians argue that aggressive medication regimens appropriate for healthy seniors should be tempered late in life, particularly when time-to-benefit exceeds life expectancy. Geriatric guidelines for diabetes and certain other chronic diseases recognize this issue, but it is unclear how these recommendations are implemented in practice. The objective of this study is to empirically determine the extent to which Medicare beneficiaries in their last year of life receive less intense medication regimens than survivors, all else being equal. Study Design: The study uses data from the 2002 Medicare Current Beneficiary Survey (MCBS) compiled as part of the Commonwealth Fund Chartbook project. Annualized differences in medication use between survivors and those who died in 2002 are analyzed for the community-dwelling Medicare population and for 3 nonexclusive disease cohorts with diabetes, COPD, and congestive heart failure. Aggregate medication intensity is measured as prescription fills per medication-sensitive condition using the CMS RxHCC risk adjustment model. Medication intensity is also compared for drugs specifically recommended for each of the three conditions. All estimates are weighted to be nationallyrepresentative and adjusted for the complex MCBS survey design. Population Studied: A nationally representative sample of fee-for-service community-dwelling Medicare beneficiaries (n=8,455) and three subgroups of beneficiaries with diabetes (N=1,956), COPD (N=1,016), and CHF (N=1,140) in 2002. Principal Findings: 3.6% of the overall sample died during 2002. Mortality rates in the diabetes, COPD, and CHF cohorts were 4.6%, 11.4%, and 13.2%, respectively. Annualized rates of prescription fills per RxHCC were consistently higher for decedents compared to survivors: 5.5 versus 4.4 for the whole population; 5.6 versus 5.5 for the diabetes cohort; 5.2 versus 4.2 for those with COPD; and 5.0 versus 4.2 for the CHF cohort. Unadjusted rates for recommended medications were lower in patients at end of life but the differences disappear in multivariate analyses adjusting for mean survival time, sociodemographic characteristics, health status, and health system contact variables. For example, diabetes patients at the end of life had insignificantly higher odds of receiving any antidiabetic medication [OR 1.61 95% CI (0.69 3.77)], and among users, the number of fills was insignificantly higher among decedents [0.30 fills 95% CI (-2.86, 3.47)]. Multivariate analyses for the COPD and CHF groups are ongoing. Conclusions: We find no evidence that medication utilization rates are lower among Medicare beneficiaries in their last year of life and some evidence that they may be higher. Implications for Policy, Delivery, or Practice: The study findings have important clinical and policy relevance given the recent implementation of the Medicare drug benefit. Part D improves access to medications in general and may potentially increase polypharmacy in patients late in life. There is an urgent need to develop explicit guidelines to facilitate joint decision making among physicians, patients, and families on when it is appropriate to consider withholding or discontinuing medications in patients late in life. Racial and Ethnic Disparities in Treatment of Dementia among Medicare Beneficiaries Research Objective: To determine whether there are systematic racial and ethnic differences in the treatment of dementia among communitydwelling Medicare beneficiaries. Specifically, we examine the prevalence and intensity of use of antidementia drugs across racial/ethnic groups and by level of disease burden. Study Design: Cross-sectional study building on data files constructed for the forthcoming Commonwealth Fund Chartbook. Antidementia drugs include cholinesterase inhibitors available for use in 2002 (tacrine, donepezil, galantamine, rivastigmine). Antidementia drug prevalence is defined as the presence of one or more prescriptions for an antidementia drug during 2002. Antidementia drug intensity among users is based on number of prescription fills for an antidementia drug during the year. Beneficiaries’ overall disease burden is categorized by quintile of cumulative annual medical spending from all payor sources (including out-of-pocket) with quintile #1 representing the lowest disease burden, and quintile #5 the highest. As of this writing, descriptive analyses are complete and multivariate analyses are underway. Projected time for completion of the paper is the end of March, 2007. Population Studied: Data were obtained from the 2002 Medicare Current Beneficiary Survey (MCBS), a nationally-representative database on Medicare beneficiaries’ use and cost of health services. Community-dwelling persons were selected based on either a self/proxy report of dementia or the presence of a claim with an ICD9 code indicating dementia. The final MCBS sample with dementia comprised 521 individuals, representing approximately 1.5 million beneficiaries nationally in 2002. Principal Findings: Over one-fourth of community-dwelling beneficiaries with dementia had a prescription fill for an antidementia drug in 2002. Antidementia drug prevalence was highest among those in quintile #2 (38%) and lowest (18%) in the group with the least disease burden (quintile #1), suggesting that use of these agents rises with low to moderate disease burden, then drops off with increasing disease burden to just 23% in quintile #5. White, non-Hispanics had higher prevalence of antidementia drug use overall (28.8%) and in every spending quintile compared to nonwhite Medicare beneficiaries (18.8%). The difference was nearly two-fold in quintile #2, with prevalence among whites at 43% compared to other races at 21%. However, among beneficiaries who used antidementia drugs during the year, medication intensity did not vary among the race/ethnicity categories, with the mean number of antidementia prescriptions similar overall (whites=5.7, nonwhites=5.5) and across spending quintiles. Conclusions: These descriptive results suggest important racial differences in who receives treatment with antidementia drugs, but no evidence that the intensity of use varies by race/ethnicity. Logistic models are being estimated to determine if the racial/ethnic disparities remain in adjusted analyses controlling for a rich array of demographic, socioeconomic, and health status variables available in the Chartbook analytic data files. Implications for Policy, Delivery or Practice: Understanding the etiology and implications of these observed racial differences will enable policy makers to assess the human and economic impact of racial differences in dementia treatment. Differentials in Medication Treatment of Aged and Disabled Medicare Beneficiaries with Depression Research Objective: Depression is common among both aged and SSDI disabled Medicare beneficiaries, but as demonstrated in the Commonwealth Fund Chartbook of Medication Use by Aged and Disabled Medicare Beneficiaries across the Spectrum of Morbidity, medication treatment patterns are far different for the two groups. Specifically, utilization rates for antidepressants, anxiolytics, opioid analgesics, and sedative hypnotics are all much greater among disabled beneficiaries with depression, and the difference increase with rising comorbidity. The purpose of this study is to further investigate the source and clinical significance of these differences. Study Design: Data are from the 2002 Medicare Current Beneficiary Survey (MCBS). Descriptive univariate and bivariate analyses of drug utilization patterns for study subjects focus on the following medication classes: antidepressants (SSRI and other), anxiolytics, sedative-hypnotics, and opioid analgesics. Prevalence of use and counts of prescription fills for each type of medication are computed for the population with depression as a whole and stratified by aged (65+) and SSDI disabled (<65) eligibility status. Overall disease burden is proxied by quintile of cumulative total medical spending. Negative inflated binomial models are used to test for significant aged/disabled differences in utilization of these agents with interaction terms for overall disease burden (quintile of spending), controlling for sociodemographics, health status measures, and other comorbidities. Population Studied: The sample comprises of 910 community-dwelling beneficiaries categorized through ICD-9 codes and/or selfreport as having major depression. More than one-quarter of the sample (27.5%) are under age 65 SSDI beneficiaries. Principal Findings: Utilization rates for all drug classes studied were much higher for SSDI disabled beneficiaries compared to aged beneficiaries with depression, and the differences mount with growing disease burden. For example, antidepressant use by the SSDI subset varies from 7 fills in quintile 1 to 13.3 in quintile 5. By contrast, antidepressant use for the aged subset is 6.2 fills in quintile 1 and 6.4 in quintile 5. Prescription fills for anxiolytics vary from 6.5 to 7.5 for both subsets of beneficiaries between quintiles 1 and 3, but then diverge sharply, with disabled beneficiaries filling 3.8 more anxiolytic prescriptions than aged beneficiaries by quintile 5. Similar patterns are noted for the other drug groups. Multivariate analysis is in progress. Conclusions: Preliminary findings identify stark differences in the use of prescription medications known to ease the emotional and physical suffering associated with depression among aged and disabled Medicare beneficiaries. Additional analysis is necessary to determine whether these differences remain after controlling for sociodemographics and health status measures. Implications for Policy, Delivery or Practice: Most of the policy attention given to understanding patterns of medication use by Medicare beneficiaries has focused on those aged 65 and older. The results from this paper suggest that more attention should be given to the under age 65 population. Arthritis, Disease Burden, and the Impact of Medication Complications Research Objective: This paper examines medication use and complication rates for Medicare beneficiaries with osteoarthritis (OA) and rheumatoid arthritis (RA) as a function of rising overall disease burden. Previous research demonstrates patients and clinicians must carefully balance the benefits from arthritis drugs with potential complications. This balancing becomes increasingly problematic as overall disease burden increases. Little prior research has looked specifically at these issues for a national sample of Medicare beneficiaries with arthritis. Study Design: Data come from the 2002 Medicare Current Beneficiary Survey. The study sample comprises fee-for-service communitydwelling beneficiaries with OA or RA divided into deciles based on beneficiaries’ cumulative annual medical spending as a proxy for overall disease burden. The principal independent variables are drugs used to treat arthritis pain and inflammation (nonsteroidal antiinflammatory drugs, corticosteroids, opioid analgesics). The dependent variables are inpatient admissions, drugs, and other health services that are markers for potential medication complications. Control variables include counts of medication-sensitive conditions from the CMS RxHCC risk adjustment model, demographic and socioeconomic characteristics, health status measures, and health system contact variables. Regression models test both the independent effect of drug use and the mediating effect of drug use and decile assignment on complication rates. All results are weighted to be representative of the Medicare population. Population Studied: Aged and disabled fee-forservice community-dwelling Medicare beneficiaries in 2002 who had two or more Medicare claims for OA or RA or had one claim and a self-report of arthritis (N = 2,066). Principal Findings: In 2002 more than 24 percent of community-dwelling Medicare beneficiaries were diagnosed with arthritis. The comorbidity profile of this population shows a strong positive association with annual medical spending. In the lowest spending decile 1, the most prevalent comorbidities were hypertension (47%) diabetes (15%), and ischemic heart disease (11%). By decile 10, 83% had hypertension, 61% had IHD, 41% CHF, and 39% COPD. Approximately 55% of Medicare beneficiaries with arthritis use NSAIDs. Opioid use is very high (36% in the OA subset and 44% in the RA subset). Corticosteroid use is also surprisingly high with 13% of persons with OA and almost 25% of persons with RA using these drugs. Rising disease burden is associated with increased markers for antiarthritic medication complications, particularly gastrointestinal drugs. Conclusions: Initial analyses raise several questions about appropriate protection from medication complications associated with arthritis treatment for Medicare beneficiaries with OA or RA. Ongoing multivariate analysis is designed to address the prevalence of arthritis medication complications on Medicare beneficiaries with rising morbidity. Implications for Policy, Delivery, or Practice: The paper suggests opportunities for Medicare to improve prescribing and reduce costs associated with arthritis treatment through appropriate management of pharmacotherapy for the pain and inflammation associated with the disease. Call for Panels Advancing Diabetes Self-Management Chair: Joseph Burton, M.S. Tuesday, June 5 • 10:45a.m.-12:15p.m. Panel Overview: Chronic diseases, including diabetes, place a significant burden on the patient and family, the community, and the health care system. Over the past 30 years, patients have been increasingly encouraged to take a more active role in their health care, including managing chronic illness. Providers increasingly need to reorient their care strategies and systems from a focus on acute care model to chronic illness care. With the goal of demonstrating the feasibility of self-management interventions in real-world settings, the Diabetes Initiative of the Robert Wood Johnson Foundation funded six grantees to develop and implement self-management programs in primary care settings and another eight grantees to demonstrate partnerships between clinical and community organizations to improve resources and supports for self-management. The programs take one or more different approaches to promoting self-management: improving nutrition, increasing physical activity, use of lay health workers/promotoras, group medical visits and support groups, and expanded use diabetes registers. The evaluation of the initiative includes case studies, the collection of clinical data, and a three-wave participant survey. Grantees conducted internal evaluations, participated in work groups, and hosted site visits. We surveyed participants about their level of physical activity and diet and nutrition behaviors and the extent to which they participated in program related activities. We also collected clinical data over time from the medical registers of the grantees that maintained and used them as part their care processes. This series of papers discuss lessons learned from the diabetes initiative and implications for improving chronic illness care. Managing Depression to Improve Diabetes Self-Management Daren Anderson, M.D., Carla Bann, Ph.D., Daren Anderson, M.D., Claire Horton, M.D. Presented by: Daren Anderson, M.D., Medical Director, Community Health Center, Inc., 635 Main Street, Middletown, CT 06457, Phone: (860) 347-6971, Email: andersdr@chc1.com Research Objective: Improving diabetes selfmanagement includes both lifestyle changes and, often, adherence to regimes for taking prescription medications. Both the lifestyle and medical management of diabetes can be challenging for persons with diabetes mellitus and can be particularly challenging for individuals with depression. We examine the differences in outcomes between persons who exhibit depressive symptoms compared to those who do not and review the successes of interventions in improving the self-management behaviors among both groups. Study Design: As part of a three-wave, comprehensive telephone survey, we assessed the key self-management behaviors of diet, exercise, smoking, and self-monitoring. We also assessed mental health status through eight of the nine questions composing the patient health questionnaire (PHQ-9). The PHQ-9 is typically used in practice settings to screen for depressive symptoms; in this study we used it to gauge overall mental health status among the participants in the various diabetes programs. We collected glycated hemoglobin levels and blood pressure values over time from medical registers and linked these to the survey responses. We analyzed mental health status, behaviors, and clinical outcomes through a series of multivariate regression and survival analyses. Population Studied: The Robert Wood Johnson Foundation funded 14 programs designed to advance diabetes self-management and improve community supports for diabetes care. The programs varied in terms of the clinical settings, populations served, age ranges, and racial/ethnic backgrounds. Participants from 11 of the programs were surveyed up to three times. Principal Findings: Controlling for several personal and program characteristics, we found persons who reported poorer mental health (more depressive symptoms) were less confident in being able to solve problems related to diabetes, had a family history of diabetes and were more likely to smoke; persons reporting better mental health tended to be married, younger, and reported greater access to resources and support for managing their illness. Persons in better mental health exercised more and ate better compared to those with poorer mental health, but both groups reported similar levels of self-monitoring. Eating behaviors------perhaps the most challenging dimension of change------were better among those in good mental health even when controlling for marriage, reported supports, and confidence. Clinical indicators and depressive symptoms improved slightly over time among those followed longitudinally Conclusions: The relationship between mental health and behavior change is complex and challenging to measure and particularly so among persons with diabetes because of the bidirectional nature of depression and diabetes. Addressing depression is an important part of diabetes care and, when treated, can lead to improved self-management behaviors and, ultimately, improved clinical outcomes. Implications for Policy, Delivery or Practice: Persons with diabetes from underserved, disadvantaged or minority populations have high rates of depressive symptoms, which might affect their ability to self-manage their disease. Mental health status appears to moderate behavior change, suggesting that strategies for improving mental health be a core component of self-management programs. Understanding the role of mental health in diabetes care and more generally, chronic illness care, can lead to improved programs for improving selfmanagement, lifestyle behaviors, and well-being. Funding Source(s): RWJF Enhancing Chronic Care Delivery in Primary Care Settings Through Planned and MiniGroup Visits Devin Sawyer, M.D. Presented by: Devin Sawyer, M.D., Family Physician, Providence St. Peter Family Practice Residency, 525 Lilly Rd. NE, Olympia, WA 98506, Phone: (360) 493-7230, Email: devin.sawyer@providence.org Research Objective: Planned visits are performed by medical assistants prior to routine visits and include blood pressure, weight and foot checks, routine laboratory tests, immunizations, referrals and patient goal setting. Mini-group visits occur when a physician meets with three patients at a time with the same chronic illness (i.e., diabetes mellitus) for approximately one hour. This research describes the preparatory steps needed to implement planned and mini-group visits including use of a disease registry and staff training. We review the purpose and benefits of planned and mini-group visits, as well as the time commitment, billing codes, and staff support needed to make these visits efficient. In addition, we discuss the characteristics of good visits, facilitation challenges, group dynamics, and techniques for intervention. Lastly, teaching the skills required for effective mini-group visits within a residency program are identified. Study Design: The study synthesizes results from case study of the residency program, internal observations documented from the program’s quality assurance efforts, a three-wave patient survey, and a review of clinical indicators collected over time. We tracked blood pressure, glysocated hemoglobin, weight, and cholesterol levels of patients participating in the visits. We also summarize provider reports related to medications, histories, challenges, and successes. Population Studied: Programs funded under the Robert Wood Johnson Foundations Diabetes Initiative were designed to advance diabetes self management and promote community supports for diabetes. This study investigates the care processes and related outcomes of patients who received one or both of interventions offered by the Providence St. Peter Family Practice Residency Program. A portion of the patients also participated in a multi-wave survey questionnaire administered as part of the national Diabetes Initiative. Principal Findings: Planned visits provide physicians with current health measures and patient goals, hence allowing more time for dialogue during individual and mini-group appointments. This improves the patient provider dynamics and patient satisfaction with the care process. We observed improvements in several clinical indicators among the participating patients. In addition, while the primary purpose of mini-group visits is medical care, patients also experience peer support and increased confidence to manage their disease. Conclusions: Medical assistants are an integral part of a diabetes care team in a practice setting. With appropriate training and provider buy-in, medical assistants and other non-physician professionals can lead patients in goal setting, skill building, and problem solving. They also can improve a practice’s efforts to provide monitoring and ongoing support for patients with chronic illnesses. Both planned and minigroup visits provide a structure to better integrate a chronic disease care team within billing guidelines. Implications for Policy, Delivery or Practice: With the number of people living with chronic disease on the rise, primary care physicians are ill-equipped to manage patients under the traditional acute care system of medicine. As a result, primary care organizations continue to experience poor health outcomes, missed opportunities to maximize care, and greater medical costs. To answer these challenges, the medical community has needed new models and approaches to chronic care. Planned and minigroup visits are two potential solutions to chronic care that may improve patient outcomes, as well as promoting a patients ability to selfmanage their chronic illnesses. Funding Source(s): RWJF Measuring Diabetes Self-management: Findings from the RWJF Diabetes Initiative Lauren McCormack, Ph.D., Carla Bann, Ph.D., Pam Williams-Piehota, Ph.D., Joseph Burton, M.S., Claudia Squire, M.S., Doug Kamerow, M.D., M.P.H. Presented by: Lauren McCormack, Ph.D., SSSHSER-PHE-HC, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709-2194, Phone: (919) 541-6277, Fax: (919) 990-8454, Email: lmac@rti.org Research Objective: Assessing lifestyle changes and support? for chronic illness care requires the use of standardized indicators, and the complexity of self-management in diabetes poses special challenges for such assessment. Measures must have content validity, empirical support, be feasible to implement in a variety of settings, and be understood by those with various levels of health literacy. Here we describe a new measure: ‘‘Resources and Supports for Self Management’’ (RSSM), developed as part of the Robert Wood Johnson Foundation’s Diabetes Initiative. We describe the measures developed and their association with the behavioral and clinical outcomes that the fourteen interventions sought to improve. Study Design: We administered three waves of a cross-site, telephone survey of participants that sought to measure whether and how the interventions funded contributed to participants’ perceived access to resources and supports for self-management (RSSM). We also measured key lifestyle behaviors including diet, exercise, smoking, and medical management regimens. RSSM indicators included (1) individualized assessment, (2) collaborative goal setting, (3) communication, (4) skills, and (5) provider follow-up. These reflect a combination of items from existing survey instruments and newly developed items that fill important gaps and ensure a patient-centered focus. We conducted both cross-sectional and longitudinal analyses. Population Studied: Programs funded under the Robert Wood Johnson Foundations diabetes initiative were designed to advance diabetes self management and promote community supports for diabetes. They focused on one of more of the following: improving nutrition, increasing physical activity, use of lay health workers or promotoras, group medical visits, and support groups. Over 700 [check] participants with diabetes who participated in one of 12 interventions different interventions completed at least two waves of the survey. Principal Findings: The scale and its 18 items demonstrated good psychometric properties. Confirmatory factor analysis supported creation of five subscales, representing the five components of RSSM. The overall scale and 5 subscales were internally consistent Participants reporting higher levels of RSSM checked their blood sugar and feet more frequently, had better diet and nutrition behaviors, and were more likely to be physically active. Conclusions: The RSSM scales developed are shown to predict self-management behaviors related to diet, exercise, and medical regimens. In addition, the findings suggest that programs to promote self-management skills may lead to improved health behaviors which, in turn, can lead to improved clinical outcomes. Messages for improving self-management can be targeted at patients who are less likely to engage in a healthier lifestyle. Implications for Policy, Delivery or Practice: The RSSM is a promising new instrument. Its ecological orientation and link to the Chronic Care framework confer potential for broader application including the potential to serve as a benchmark for national performance measurement. In addition, the RSSM constructs offer guidance and lessons learned for designing and improving care processes for chronic illness. Funding Source(s): RWJF Synthesizing Lesson Learned from Fourteen Diabetes Initiatives Joe Burton, M.S. Presented by: Joe Burton, M.S., Researcher, RTI International, 1440 Main Street, Waltham, MA 02451, Phone: (781) 434-1710, Fax: (781) 4341701, Email: joeburton@rti.org Research Objective: The Diabetes Initiative of the Robert Wood Johnson Foundation includes 14 projects in primary care settings and in community-clinical partnerships. The primary purpose of the Initiative was to demonstrate feasible and sustainable approaches to promoting diabetes self management in primary care and community settings. Projects serve predominantly indigent populations from varied cultural and linguistic backgrounds in urban, rural, and frontier settings. This paper describes the Initiative, its ecological perspective on self management, and implications for program development and sustainability in primary care and community settings. It also discusses methodological challenges in assessing multisite interventions. Study Design: The evaluation of the initiative includes case studies, the collection of clinical data, and a three-wave participant survey. Grantees conducted internal evaluations, participated in work groups, and hosted site visits from both the National Program Office and an external evaluator. Population Studied: Participants in 14 different interventions designed to advance diabetes self management and promote community supports for diabetes. Principal Findings: Several of the Initiative’s grantees observed improvements in key selfmanagement behaviors and clinical indicators among engaged patients over time. Overall, reported rates of physical activity were higher than national levels. Greater community resources for physical activity were associated with higher levels of physical activity. Individuals who were older, more confident, less depressed, ate most of their meals at home, or had greater program participation tended to eat healthier. Participants reported very high levels of perceived support from their diabetes care teams. Programs were able to adapt and evolve based on sharing ideas through a learning network and active workgroups. Conclusions: Ecological perspectives stress varied levels of influence ranging from individuals to communities and policies. The Initiative identified key components of Resources and Supports for Self Management (Individualized Assessment, Collaborative Goal Setting, Enhancing Skills, Follow Up and Support, Community Resources, and Continuity of Quality Clinical Care). These constructs are predictive of self-management. Lessons learned include the central roles of Community Health Workers, integration of healthy coping and attention to negative emotion and depression in self management, community partnerships, approaches to ongoing follow up and support, organizational factors in sustaining programs, and the utility of a "Collaborative Learning Network" for program development. Sustainability stresses organizational and policy supports for program. Implications for Policy, Delivery or Practice: The Diabetes Initiative demonstrates that effective self management programs and supports can be implemented in real-world clinical and community settings, providing models of worthwhile, sustainable programs. Funding Source(s): RWJF Ongoing Follow Up and Support in Diabetes Management and the Critical Role of the Community Health Worker Edwin Fisher, Ph.D., Carol Brownson, Ph.D., Mary O'Tolle, Ph.D., Victoria Anwuri, M.A., Gowri Shetty, Ph.D., Kia Davis, Ph.D. Presented by: Edwin Fisher, Ph.D., Professor and Chair, Department of Health Behavior and Health Education, University of North Carolina at Chapel Hill, Campus Box 7440, Chapel Hill, NC 27599-7440, Phone: (919) 966-6693, Email: fishere@email.unc.edu Research Objective: Ongoing follow up and support is a critical determinant of sustained behavior change across many areas of health and health behavior, including chronic disease and diabetes management. Study Design: The study included collaboration with grantees to identify key features of ongoing follow up and support, key approaches to providing these, and the contributions of Community Health Workers to this. Population Studied: Grantees, programs, and program participants of the Diabetes Initiative of the Robert Wood Johnson Foundation. Principal Findings: From discussions with grantees of key features of ongoing follow up and support, key characteristics include: (a) being centered on a personal relationship with a member of the diabetes care team, (b) availability and accessibility as needed or desired by the participant, as opposed to according to limited schedules or venues, (c) including opportunities for engagement that do not require high levels of investment to behavior change by participants, (d) proactive maintenance of contact with participants (at least every 3 ---- 4 mos) to identify changes in status or needs for further care and to provide sense of continuity of contact and concern by the care team, (e) unrestricted in time and topics discussed and responsive to the needs and interests of the participant as opposed to being limited by protocol. Across these features emerges the importance of choices for participants in the ways in which they maintain contact with the care team and are monitored by them. Grantees have provided these key features, including participant choice, through a wide variety of approaches, ranging from open events and activities such as ‘‘breakfast clubs,’’ culturally specific activities such as inclusion of diabetes issues in ‘‘Talking Circles’’ in American Indian settings, to contact of patients not seen for over several months by teams of Community Health Workers and nurses. Community Health Workers make major contributions to ongoing follow up and support by being available to participants, having time to talk about diverse topics, coaching participants on adapting management plans to their individual living circumstances, providing emotional support, and facilitating ongoing linkage between the individual and the rest of the diabetes care team. Conclusions: Ongoing follow up and support for diabetes management entails a range of key features and the importance of participant choice and, correspondingly, requires diverse programmatic approaches. Community Health Workers can make substantial contributions to these types of services. Implications for Policy, Delivery or Practice: Practice settings can arrange a variety of activities and types of services to provide ongoing follow up and support for diabetes management. The range and inclusion of choices among diverse approaches may be as important as any single program component. Including Community Health Workers in the care team can facilitate implementation of this range of types of service and contact. Funding Source(s): RWJF Call for Panels Monitoring the Healthcare Safety Net at the State and Local Levels Chair: John Billings, J.D. Tuesday, June 5 • 10:45 a.m.-12:15 p.m. Panel Overview: The healthcare safety net in the United States is crucial to the health of underserved populations and the financial stability of the health sector. The nation’s large and growing uninsured population combined with the lack of consensus on how to reduce the number of uninsured highlights the importance of maintaining a strong and sustainable safety net. The proposed research panel will present a broad range of perspectives on surveillance and improvement of safety net services at the state and local levels. Presentations representing four diverse regions of the United States will describe recent efforts to collect and standardize data, quantify the supply and demand for safety net services, define the boundaries of safety net care, and use data to improve service delivery. The following overlapping themes will be addressed: coordination of multiple health and social services, definition of safety net concepts, determination of service areas, data assembly and dissemination, qualitative versus quantitative information, and partnerships with consumers of research. In addition to presenting findings from their research, presenters will address challenges that were encountered and what actions are needed to better meet these challenges in the future. Use of Charity Care Records to Optimize Care for the Uninsured Derek DeLia, Ph.D. Presented by: Derek DeLia, Ph.D., Assistant Professor/Senior Policy Analyst, Rutgers Center for State Health Policy, 55 Commercial Ave, New Brunswick, NJ 08901-1340, Phone: (732)9324671, Fax: (732)932-0069, Email: ddelia@ifh.rutgers.edu Research Objective: Use hospital administrative records in New Jersey (NJ) to document the healthcare needs of the low-income uninsured and highlight areas where cost management strategies may be successfully employed. Study Design: Charity care claim records are used to determine the most prevalent and costly services provided to charity care patients. Concentration of costs and potentially avoidable utilization are analyzed. Population Studied: Users of hospital-based charity care in NJ in 2003. Principal Findings: Prenatal care and delivery are the most common services provided to NJ’s charity care population. Mental health and substance abuse services are also heavily used by this population. A wide variety of other charity care services are provided including treatment for circulatory disorders, hypertension, and diabetes. Charity care costs are highly concentrated among a small number of patients with 50% of costs attributable to 5% of patient encounters (i.e., outpatient visits plus inpatient admissions). Since high-cost patients are expected to have multiple encounters, the costs are likely to be even more concentrated among individuals. Finally, 10% of charity care costs are attributable to emergency department visits and inpatient admissions for conditions that may have been avoided with more timely access to primary care (e.g. episodes of asthma, congestive heart failure). Conclusions: The scope of services used by NJ’s charity care population reveals a wide safety net held by hospitals across the state. Nevertheless, a number of charity care services provided by hospitals might be redirected or better managed to improve patient care or reduce costs. For example, many pregnant women currently relying on charity care may be eligible for Medicaid or the state’s Family Care Program. In addition, the prevalence of utilization for mental health, substance abuse, and primary care sensitive services suggests that many of these medical episodes could be prevented with earlier intervention. The concentration of costs within a small number of users points to an area where targeted management of high-cost cases may generate substantial savings. Implications for Policy, Delivery or Practice: Study findings are especially timely as state officials in NJ are currently considering ways to restructure the hospital sector and reduce the costs of charity care subsidies. The findings highlight the need to thoroughly screen individuals who may be eligible for coverage before funding their services through charity care. A great deal of potential exists for reducing costs through focused management of high-cost uninsured patients. Better coordination of services for the uninsured outside of the hospital such as mental health, substance abuse, and primary care may improve outcomes and efficiency as well. This coordination may be challenging as charity care users include a complicated mix of individuals who are employed, unemployed, homeless, transient, undocumented, and moving in and out of the criminal justice system. An important barrier to using the charity care claims database as a care management tool is its lack of identifiers for patient race/ethnicity, immigration status, area of residence, and repeat utilization. However, these identifiers, or reasonable proxies, may be added to charity care records with little incremental cost. Funding Source(s): Johnson & Johnson Challenges of Urban Safety Net Evaluation Glenn Landers, M.B.A., M.H.A. Presented by: Glenn Landers, M.B.A., M.H.A., Senior Research Associate, Georgia Health Policy Center, 14 Marietta Street, Suite 221, Atlanta, GA 30303, Phone: (404) 463-9562, Email: glanders@gsu.edu Research Objective: Evaluate the supply of and demand for safety net health care services in seven metropolitan Atlanta counties and identify challenges and opportunities in data collection. Study Design: Secondary analysis of individual characteristics, community level variables, and health care access and outcomes for seven counties. Primary data collection and analysis using survey, administrative, and interview data from 35 safety net organizations representing 101 service delivery sites. Population Studied: Safety net health care delivery sites in seven metropolitan Atlanta counties, defined as: o Public hospitals that participate in the Disproportionate Share Hospital program (DSH) o Hospital-based clinics o Federally Qualified Health Centers (FQHC) o Community Health Centers (CHC) o Independent clinics or Freestanding Primary Care Clinic, including faith-based clinics o County health departments o Community Service Boards and affiliated mental health providers o Non-traditional providers, including those that focus on specific diseases, conditions, or populations o Individuals not covered by public or private insurance. Principal Findings: The determination of the supply of and demand for health care safety net services at the community or regional level is challenged by: 1. Lack of common data definitions and reporting across service providers. 2. The potential shortcomings of self-reported data. 3. The lack of reliable estimates of the uninsured at the county or community level. 4. Administrative idiosyncrasies across service sites. 5. The time and effort involved in primary data collection. A qualitative study of community safety net providers can surface potential partnerships, collaborations, and joint ventures that might not otherwise be evident. Analysis across communities can also point to common needs (root causes) such as stable housing and employment opportunities not apparent in publicly available data sets. Conclusions: In spite of the challenges encountered in measuring the supply of and demand for health care safety net services, the information gained from such an effort can contribute to a greater understanding of community-specific needs and opportunities. Implications for Policy, Delivery or Practice: Safety net providers are focused on their core business of health care delivery, not the accurate and reliable collection of administrative data that might be used to create system-wide efficiencies and promote collaborative partnerships. There are, however, important opportunities that might be exploited for safety net populations through the coordination and alignment of safety net services across providers within communities or regions. Such opportunities might include economies of scale or more efficient referral patterns. Toward the better coordination of safety net services, states have an interest in encouraging partnerships and promoting efficiencies. Such partnerships and efficiencies can be supported through the establishment of standardized data collection and reporting requirements that enable reliable measurement of safety net service supply and demand. States might consider supporting sustainable safety net monitoring systems that enhance the capacity and efficiency of individual providers and that promote partnership and collaboration across communities. Funding Source(s): Community Foundation of Greater Atlanta Community Data Needs Assessment for Monitoring Portland’s Health Care Safety Net Jennifer Lin, M.D. Presented by: Jennifer Lin, M.D., General Internal Medicine Fellow, P3-Health Services Research Division, Portland VA Medical Center, P.O. Box 1034, Portland, OR 97207, Phone: 503220-8262, Fax: 503-273-5367, Email: linje@ohsu.edu Research Objective: This study was designed to assess the information and data needs from organizations comprising the infrastructure of Portland’s health care safety net (HCSN). Our objectives were to understand the current use of available information and data to support decision-making; to understand perceived information and data needs as identified by decision makers within the HCSN; and to identify recent initiatives to address these needs. Study Design: We purposively sampled organizations from a Portland-based HCSN umbrella organization. We conducted semistructured interviews to elicit information in three domains which paralleled our objectives. Interview findings were hand scribed and analyzed for thematic content. Population Studied: We interviewed 22 executive-level decision makers in clinic and hospital systems, associations of primary care and hospitals, funding agencies, advocacy and support organizations, health plan organizations, state planning agencies, and a state advisory council; three directors of IT within these organizations; and we reviewed 11 supporting documents. Principal Findings: Everyone acknowledged our deficit in understanding the health needs of patients receiving care through the safety net and the viability of the HCSN at the community level. Those in decision-making roles who routinely used external data sources did not find them very useful (e.g. not available at the local level, not current, not in a useful format, and no support staff to conduct secondary data analysis). Those who routinely used internal data had well-staffed IT departments, but infrequently shared their data to non-clients, primarily due to lack of requests for their data. Most people felt that there is wealth of potential information and data, and an emerging regional health information infrastructure. Many expressed skepticism about using this data in decision making because of current limitations, including lack of: (1) transparency of existing measures; (2) coordination and integration of data (i.e. across health systems, state/county borders, and sectors of health care); (3) policies to address political, legal, and technical challenges of sharing data; and (4) skilled staff and monies to support data management and analysis. Other limitations include: (1) data gaps in specific health care sectors (i.e. dental, mental health, social services, pharmacy and prescription drug use), (2) data gaps in specific populations (i.e. uninsured, migrant workers, homeless), and (3) gaps and concerns in measurement development (e.g. valid costbased measures, quality of care measures, meaningful outcome-based measures, and the importance of tracking qualitative measures like local politics and leadership capabilities and community dialogue within the HCSN). We identified several routine and ad hoc survey mechanisms for future data collection and community and state-based initiatives to support data sharing and integration, and measurement development. Conclusions: There appears to be a wealth of information and data that could better inform decision making, and potential leadership and mechanisms in our community to foster data collection, data coordination, and measurement development. Implications for Policy, Delivery or Practice: This study highlights many priority concerns for policy making and targeting solutions within our HCSN and identifies underutilized existing resources that should shape ongoing or future initiatives. Bridging State and Local Safety Net Data Gaps: Strategies and Initial Results Jeff Bontrager, M.S.P.H., Reid Reynolds, Ph.D., Pamela Hanes, Ph.D. Presented by: Jeff Bontrager, M.S.P.H., Research Analyst, Colorado Health Institute, 1576 Sherman Street, Suite 300, Denver, CO 80203, Phone: (303) 831-4200, Fax: (303) 831-4237, Email: bontragerj@coloradohealthinstitute.org Research Objective: To assess the capacity of Colorado’s health care safety net system to meet the basic medical, dental and mental health care needs of Colorado’s most vulnerable populations and to provide relevant, reliable and timely information on which sound policy decisions can be based. Study Design: This project employs both quantitative and qualitative methods over a multi-year timeframe. Initial steps included establishing operational definitions of the safety net and vulnerable populations who use safety net services. With the guidance of an advisory committee of influential stakeholders, data gaps were identified and criteria for selection of an initial set of indicators were established. Data sharing agreements were secured with various safety net providers (e.g., federally qualified health centers, rural health clinics, non-profit and faith-based clinics, community mental health centers and hospitals). A set of interactive Webbased tools is currently under development to uniformly collect, analyze, and report safety net indicators. Whenever possible, county and subcounty data were identified, although state-level data were utilized when sub-state data were not available. Concurrently, agreements were secured within select Colorado communities to participate in community case studies. Population Studied: For this project, vulnerable populations were defined as Medicaid and SCHIP enrollees, as well as uninsured Coloradans with family incomes below 250 percent of the federal poverty level. Principal Findings: The first year of data collection has revealed a complex array of safety net providers distributed unevenly across the state. Although these providers recognize the importance of uniformly collected data about safety net services and the populations that use them, their ability to collect, analyze and report patient-level data varies widely. Development of a user-friendly Web-based data portal holds great promise for this data collection effort. Building a uniform database comprising patient demographic information, access variables and health status indicators is a critical starting point for a safety net monitoring system. Preliminary estimates indicate that increases in safety net capacity have been roughly matched by growth in the size of vulnerable populations. Other early analysis that will be presented is the relationship between regional variations in the incidence of ambulatory care sensitive conditions and safety net capacity. Conclusions: Striking a balance between qualitative and quantitative approaches, state and local data and short-term and long-term reporting strategies is essential to building Colorado’s safety net monitoring system. Establishing collaborative and mutually beneficial data sharing agreements with safety net providers has also assisted in addressing development and implementation challenges. Sub-state safety net data are most in demand by policymakers and stakeholders but continues to be the least available on a uniform basis. Implications for Policy, Delivery or Practice: With increasing interest among Colorado policymakers for shoring up the state’s safety net, the necessity of collecting, analyzing and translating reliable data into policy-relevant information is key among the project’s objectives. Data on the characteristics of the uninsured and those enrolled in state coverage programs have already assisted policymakers to better target policy options. The project will continue to build a portfolio of communications strategies for the dissemination of information that can be utilized for informed policy decisionmaking. Funding Source(s): Other Foundation, Colorado Health Foundation Monitoring the Safety Net at the Local Level: Oregon’s Health Indicators Project (HIP) Heidi Allan, M.S.W. Presented by: Heidi Allan, M.S.W., OHREC Project Director, Office for Oregon Health Policy & Research, State of Oregon, 255 Capitol Street NE, 5th floor, Salem, OR 97310, Phone: (503) 378-2422, Fax: (503) 378-5511, Email: heidi.allen@state.or.us Research Objective: In Oregon, there is no single source where safety net data is collected or analyzed. Information on the safety net is difficult to assemble and incomplete. Local safety net initiatives struggle to describe gaps in services, to measure the success or failure of community interventions, and to compare themselves with other communities or state averages on measures of access. The Health Indicators Project was developed to provide local safety-net collaboratives with a common unit of analysis for purposes of comparison and monitoring, and to identify shared indicators of access that communities could use utilizing existing sources of data. Study Design: Safety-net collaborations in Oregon’s urban areas were contacted to participate in focus group discussions with the goal of achieving agreement on defining common-sense geographic units of analysis and a set of indicators measuring health care access. A series of focus groups were held in five urban areas. Population Studied: Participants were individuals who had participated in 100% safetynet access collaborations and represented a variety of public and private stakeholder organizations. Principal Findings: Defining the geographic unit of analysis required several meetings in each community to problem-solve issues related to changing demographics. Ultimately, the participants developed Primary Care Service Areas (PCSA) that represented the five urban areas and aligned with the rural PCSAs to create a state-wide unit of analysis representing contemporary and common-sense boundaries for local safety-net systems. Multiple shared indicators measuring access were identified from existing data sources and agreed upon by participants. Utilizing existing data sources presented several challenges: 1) it is difficult to define access within the limitations of the indicators available for analyses, there is rarely a denominator including individuals who are not utilizing services; 2) there is little data granular enough for analysis at the PCSA level; 3) there were no good proxies of access to outpatient mental health and preventative dental services; and 4) race data is not widely available. Conclusions: The Health Indicators Project has provided safety-net communities with a common unit of analysis for comparisons and a set of shared indicators of health care access. Ongoing monitoring of the indicators could assist safety-net collaboratives in using limited financial and data capacity resources in an efficient progression towards identified objectives by: o Accurately defining and quantifying the problem at the level of concern (PCSA, local, regional, or state). o Utilizing baseline measures to evaluate the relative success of interventions. o Applying for funding to address unmet needs. Implications for Policy, Delivery or Practice: In order to truly maximize the benefits of the Health Indicator Project, limitations in the available data sources to measure health access should be addressed, particularly related to identifying demand (including foregone health care) and disparities. Developing a coordinated and targeted approach to understanding health care access at the local, regional, and state level will require continued collaboration between state and safety-net community collaboratives. Funding Source(s): HRSA Call for Panels Patient Outcomes and Costs Related to Nurse Staffing Chair: Chuan-Fen Liu, Ph.D., M.P.H. Tuesday, June 5 • 1:00 p.m.-2:30 p.m. Panel Overview: In this panel, we present results of recent, large-scale studies of nurse staffing, patient outcomes and costs of care at 124 medical centers in the Veterans Health Administration, Department of Veterans Affairs (VA). Previous studies of nurse staffing and patient outcomes have focused primarily on facility-level analyses, in part due to lack of data at the unit level. Using detailed data from VA administrative databases, we were able to examine associations between nurse staffing, nursing skill mix and patient mortality at the unit level as well as the facility level. Using survey data on reorganization of VA hospitals during the past decade, we examined the effect of nursing service organization (nurse executive line authority for nurse staffing) on patient care costs. Our results suggest that nurse staffing and skill mix have different effects on patient mortality for patients with ICU stays versus those without any ICU stay. While nurse staffing levels and market variables affect patient care costs, nursing service organization measured as line authority for nurse staffing does not appear to be associated with patient care costs. We interpret these results in the context of a wide range of studies on the relationships between nurse staffing, skill mix, nursing work environment, and patient outcomes such as length of stay and hospital-acquired complications, with attention to data and methods used in previous research. The Association Between Nursing Factors & Patient Morality in the Veterans Health Administration: The View from the Nursing Unit Level Presented By: Anne Sales, Ph.D., M.S.N., Associate Professor, University of Alberta, 3-114 Clinical Sciences Building, Edmonton, Alberta T6G 2G3, Canada, Phone: (780) 492-8432, Fax: (780) 492-2551, Email: anne.sales@ualberta.ca Abstract: Nurse staffing is not constant across an entire hospital. Most previous studies of the association of nurse staffing with in-hospital patient mortality have used data aggregated to the facility level, due to limitations of the available data. In this study, we present findings from the first large-scale study of in-hospital patient mortality and its association with registered nurse staffing and skill mix at the unit level. We included patient-level data from all inpatient admissions to acute care (intensive care and non-intensive care) units in 124 Veterans Health Administration Medical Centers within the United States Department of Veterans Affairs (VA). Staffing and skill mix variables at the unit level came from VA national accounting and payroll databases. We obtained patient inhospital mortality outcomes and other characteristics for risk adjustment from VA’s National Patient Care Databases. We used hierarchical multi-level multiple regression models to adjust for patient, unit, and hospital characteristics. Estimating results at the facility level, even with adjustment for facility level clustering, yielded more highly significant results for both RN hours per patient day and RN skill mix than when results were estimated at the unit level, with clustering accounted for at both unit and facility level. Splitting the sample among patients with any and no ICU stay during their hospitalization resulted in differing effects of RN staffing and skill mix across these two patient populations. Our findings suggest that the association between RN staffing and skill mix and in-hospital patient mortality is not as clear as it appears when facility-level data are used. Nurse Staffing & Patient Outcomes in Hospitals: Current Findings & Future Directions Presented By: Jack Needleman, Ph.D., Associate Professor, University of California, Los Angeles, 650 Charles Young Drive S., Room 31-236B CHS, Los Angeles, CA 90095-1772, Phone: (310) 2672706, Email: needlema@ucla.edu Abstract: The Department of Veterans Affairs (VA), a federal agency of the United States government, has implemented extensive organizational changes to improve efficiency of inpatient care since the mid-1990s. One reorganization strategy, implemented during the period 1996-2000, was the use of interdisciplinary patient care teams within service line structures, which in turn affected nursing supervision and reporting structures. Although Service Lines were intended to provide more efficient and economical patient care, shifting control of nurse staffing decisions to an interdisciplinary service line also had the potential to decrease efficiency by creating new barriers to cross-service planning for staffing and to reassignment of nursing staff from low to high census areas. This study examines the relationship between nurse executive line authority for nursing staff and patient care costs between 02/2003 and 06/2003 at 124 acute care VA hospitals. The unit of analysis is the hospital. We assessed nurse executive line authority for nurse staffing based on information from the VA Office of Nursing Services and a survey of nurse executives. Other data sources were VA Decision Support System inpatient extracts (patient care costs and nurse staffing), administrative databases (patient characteristics and health outcomes); and national databases (market/health service area characteristics). The dependent variable was the total patient care cost per bed day of care for each hospital. Among 125 hospitals, 87 had Nurse Executive line authority for nurse staffing in 2003. Compared to hospitals without Nurse Executive line authority for nurse staffing, these 87 hospitals had lower patient care costs per bed day of care ($258 versus $283, p=0.058), fewer registered nurse hours per patient day (4.2 hours versus 4.7 hours, p=0.083), and fewer total nursing hours per patient day (7.2 hours versus 7.9 hours, p=0.033). After controlling for nurse staffing and patient, facility, and market area characteristics, the relationship between patient care cost and line authority for nurse staffing was not statistically significant. The factors significantly associated with high patient care costs were higher nurse staffing levels (RN and non-RN hours) and the RN wage index, comparing costs of nursing wages across different markets. Our study results provide no evidence that moving to a service line organizational structure offers cost efficiency, nor evidence that there are inefficiencies associated with this organizational change. The Relationship Between Line Authority for Nurse Staffing & Patient Care Cost Presented By: Chuan-Fen Liu, Ph.D., M.P.H., Research Health Scientist, VA Puget Sound Health Care System, 1100 Olive Way, Seattle, WA 98101, Phone: (206) 764-2587, Fax: (206) 7685343, Email: fliu@u.washington.edu Abstract: Current research on nurse staffing and patient outcomes in hospitals, using a wide range of data sets and methods, finds strong evidence that nurse staffing levels and skill mix influence a variety of outcomes: length of stay, hospital-acquired infections and other complications, pain management, and patient satisfaction. There is strong but less conclusive evidence for the association of nurse staffing and mortality. Other studies examine the association of other dimensions of the nurse work environment, such as use of overtime and professional autonomy, on patient outcomes. Estimates of the costs of increasing nurse staffing levels to those of the best staffed hospitals fall within a range of 1-3% of hospital costs, but estimates of the offsetting cost savings from reduced length of stay and avoided complications, reduced staffing turnover, and other impacts vary more widely. We review the literature on nurse staffing and patient outcomes, with particular attention to the data and methods used and the limitations and challenges these impose on the ability to study these associations; identify issues of estimating the costs and cost offsets of increasing nurse staffing; and discuss directions for future research to resolve current conflicts.