Developing a Business Case Model for Integrated Child Health Information Systems Academy Health
advertisement

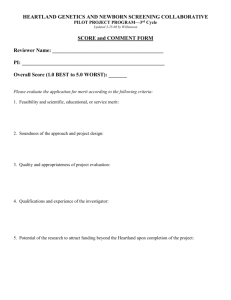
Developing a Business Case Model for Integrated Child Health Information Systems Academy Health June 27, 2006 The Lewin Group ● Tim Dall ● Yaozhu Chen PHII ● Kris Saarlas ● Jim Mootrey ● Dave Ross ● Alan Hinman Why is integration of child health information systems important? • Provide comprehensive, timely and accurate child health information to support the provision of service through medical home, public health program needs, and decision-making at the point of service • Ensure children receive necessary preventive, screening, therapeutic and follow-up services • Coordinate medical care and public health activities • Coordinate public health program services • Eliminate duplicative services 2 Integrated Child Health Information Systems (ICHIS) • What is integration? • Which child health information systems are states integrating? – – – – – – – Immunizations (immunization registries) Newborn dried blood spot screening systems (NDBS) Early Hearing, Detection and Intervention program (EHDI) Lead EPSDT WIC Others (birth defects and disease registries, Early Intervention, Children with Special Health Care Needs) 3 What is a business case and why is it necessary? • What is a business case? – A tool that supports planning and decisionmaking – Assessment of the benefits and costs of various alternatives • Why is it necessary? – States/communities need to justify return on their investment—increased focus on accountability – Need for sustainable funding for child health information systems – Increase participation in ICHIS 4 What is the Business Case Model? • An Excel-based tool to quantify benefits and costs of integrating various child health systems • Provides information important to different perspectives: society, providers, parents, and public health programs • Answers the question, “what benefits can I expect to see if I integrate this system(s) with that system(s)?” • Flexible tool that is responsive to various state and local models and future growth of ICHIS 5 Integration Benefits Modeled • Focus on improved effectiveness of services, efficiency, quality of care, coordination of care, health outcomes • Areas of Benefits: – Benefits to Families – Benefits to Physicians/providers – Public Health Decisions – Data Quality – Case Management 6 Examples of Data and Sources • Government-collected statistics – – – – Newborn/child demographics Newborn screening and follow-up rates Disease prevalence rates Child health program participation rates • Medical and economics literature – Health care utilization/sequelae/costs per disease case – Special education, productivity, and long term care costs • Expert opinion (pending additional research) – Changes in screening, follow-up, and program participation rates from ICHIS 7 Process for Business Case Model development and deployment • Funding provided by HRSA/MCHB/GSB and RWJF • Formed workgroup of stakeholders from PH, private physicians, family advocates, health plans • Solicited input from expert health economists and program specialists • Researched literature • Beta testing of tool with 4 states January 2006 • Development of training materials spring 2006 • Model being provided free* to public health departments and researchers • Formation of a User Group and possibly limited technical support** 8 9 Business Case Model Overview 10 12 14 Challenges to developing a business case on ICHIS • Added/marginal value of integration vs. value of programs and independent systems • Lack of data on costs and benefits on individual programs and information systems • Change in behavior that integration of data brings—i.e., data not available now to physicians, who’s responsible for follow up • ROI not always basis for decision making 15 Thank You! Contact Information: Tim Dall tim.dall@lewin.com www.lewin.com Kristin Saarlas ksaarlas@phii.org www.phii.org 16 Extra Slides 17 Benefits to Families • Parents have access to CHIS information in consolidated format • Reminders/recalls • Convenience when moving/changing providers • Time saved (scheduling appointments, missing records, reduced data entry) • Reduced visits/efficiency and coordination of care • Improved health outcomes (reduced lifetime care costs, increased earnings of family/child) 18 Benefits to Providers • Providers have access to data they didn’t have before • Reduce chart pulls if electronic access is available • Quality of care—reduction in duplicative services, timeliness of care, pay for performance • Increased number of visits? Increased revenues? 19 Benefits to Public Health • Assess risk factors to completeness of care • ID medical home and health care utilization rates • Linkage to other data—hospital discharge, education, social services • Long term surveillance—population trends • Quality assurance—public health role • Changes in policies? 20