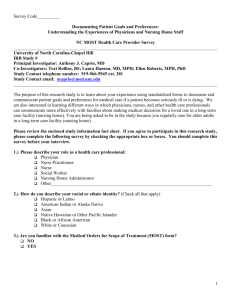
Workforce
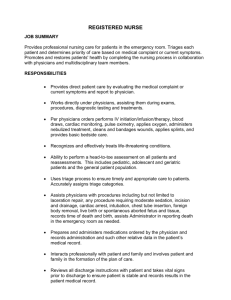
advertisement

Workforce Call for Papers Meeting the Workforce Needs in Rural America Chair: Julie Sochalski, University of Pennsylvania Sunday, June 25 • 8:30 am – 10:00 am ●US Rural Physician Workforce and Medical Education Frederick Chen, M.D., M.P.H., L. Gary Hart, Ph.D., Meredith Fordyce, Ph.D. Presented By: Frederick Chen, M.D., M.P.H., Deputy Director, Family Medicine, WWAMI Rural Health Research Center, 4311 11th Avenue NE, Ste. 210, Seattle, WA 98195; Tel: (206) 5437813; Fax: (206) 616-4768; Email: fchen@u.washington.edu Research Objective: Among the most enduring problems within rural America is the shortage and maldistribution of rural health care providers. In addition, the dramatic decline in U.S. medical graduates choosing generalist residency positions, high malpractice costs, tight reimbursement policies, and a shift within generalist disciplines to greater proportions of women are creating an impending crisis in access to physicians for rural populations, especially in the smallest and most isolated rural communities. At the same time, medical education policies have been unable to ensure a continued commitment to the supply of rural physicians. We sought to describe the training pathway of rural physicians in the US. Research Objectives: 1. To describe the composition, specialty distribution, and medical training of the rural physician workforce. 2. To show that medical schools and residencies vary dramatically in the number and proportion of their graduates who practice in rural areas. Study Design: We performed a national cross-sectional analysis of the 2005 AMA and AOA Masterfile physician data. The Masterfiles were linked with Rural-Urban Commuting Area (RUCA) codes, Claritas demographic data, the Area Resource File, HPSA designations, and ERS persistent poverty counties. We identified physicians’ rural locations based on ZIP codes and geocoded these to RUCA categories. Rural physicans were aggregated to each medical school and compared across the medical schools to show the percentage of the rural physicians who are produced by the largest producers and the lowest producers. Population Studied: We examined a ten-year cohort of allopathic and osteopathic physicians who graduated from medical school 1988 through 1997. Principal Findings: There were 175,649 physician graduates between 1988 and 1997. 20,037 (11%) were currently practicing in a rural RUCA location. 18% of osteopathic physicians practice in a rural location but only 11% of allopathic physicians were in a rural location. The specialty of rural physicians varied widely. 23% of rural physicians are family physicians, 16% are general surgeons, 11% are internists, and 9% are pediatricians. The proportion of each specialty that practices in a rural area remained fairly consistent over the ten year period. The top 10 medical schools placed between 21-36% of their graduates in rural areas. Conclusions: This national analysis shows that the proportion and number of rural physicians has been stable, compared to earlier analyses. Osteopathic physicians and primary care physicians are much more likely to practice in rural areas. As we expected, a small number of medical schools and residency programs are responsible for training the majority of rural physicians in this country. Recent trends that are not yet reflected in these data, however, may adversely affect rural physician supply and distribution. Implications for Policy, Delivery, or Practice: This project provides needed information on the specifics of the production of physicians for the nation's rural communities. Many federal and state programs are aimed at increasing the supply of physicians within rural areas (e.g., the Medicare Incentive Program and the National Health Service Corps). The findings provide decision-makers with critically needed information upon which to tailor federal and state programs (e.g., GME funding alternatives, and NHSC scholarship and loan repayment acceptance criteria). In addition, the project provides comparative data that demonstrate how well medical schools and states meet the rural needs of their respective populations in comparison to other states and the nation at large. At the state and local rural level, the results provide the information needed as an impetus for change in medical school and residency rural training activities. Primary Funding Source: HRSA ●Health Care Employees’ Contributions to the Economy of a Rural State: A study based on the Nebraska Rural Health Works Project Roslyn Fraser, M.A., Li-Wu Chen, Ph.D., Keith Mueller, Ph.D. Presented By: Roslyn Fraser, M.A., data analyst, Preventive and Societal Medicine, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198-4350; Tel: 402-559-5260; Email: rfraser@unmc.edu Research Objective: To examine the contribution of employees of the health care sector to the state economy. Study Design: Using an economic input-output analysis model and IMPLAN software, we estimated the direct and indirect impact of the health care sector on jobs, income, and output on the state economy. Type SAM (Social Account Matrix) multipliers were used because they adjust effects based on spending patterns amongst different income groups. This level of analysis is most accurate and allows us to compare health care employees to employees of other sectors. An aggregate model was built to compare the health care sector to eight other economic sectors in Nebraska. Sectors were ranked by overall impact on job creation, income creation, total output, and contribution to gross state product. We examined the direct effects (initial business spending), indirect effects (businesses buying and selling to each other), and induced effects (household spending based on income earned) of the aggregated sectors. Particular attention was paid to induced effects as a measure of employees’ spending activity; this allowed us to examine their contribution to the economy. Population Studied: We used industry input-output data from the 2002 Nebraska IMPLAN data supplemented with employee and payroll data from the Nebraska Hospital Association. Principal Findings: The heath care sector ranks fourth in overall (i.e., direct and indirect) impact on job creation in Nebraska (161,140 jobs), third in overall impact on income creation ($6.308 billion), fifth in overall impact on output produced ($13.310 billion), and third in overall contribution to gross state product ($8.024 billion) based on our statewide analysis. When the specific spending activity of health care employees is examined, the induced effects consistently rank in second place. Within the healthcare sector, offices of physicians, dentists, and other health professionals had the highest induced effect, followed by employees of home health care services. Conclusions: Based on our findings, we see that the health care industry provides high quality jobs with high incomes. Health care employees have the second highest household spending based on income earned and are more likely than employees in any other sector, except one, to spend labor income locally. Nebraska benefits from health care employees not only because of the services they provide, but because their income is relatively high and is spent locally. Implications for Policy, Delivery, or Practice: The population of 70 of Nebraska’s 93 counties is in decline. Given out-migration trends, rural Nebraska is experiencing a rise in its elderly population and a loss of well-educated people of working age. Apprehension about the changing demographics in rural areas places rural economic development at the top of many policy agendas. As one of the strongest contributors to overall economic activity, healthcare is a vital sector in Nebraska. Rural Nebraska benefits from the draw of health care professionals who provide necessary services, hold professional degrees, earn higher incomes, and spend locally. Because health care has the potential to increase jobs, income, output, and attract educated professionals to an area, investing in health sector development is one way to stimulate rural economic development. Primary Funding Source: State Office Of Rural Health ●Uses of Rural-Urban Commuting Areas (RUCAs) Version 2.0 in Health Workforce Research Gary Hart, Ph.D. Presented By: Gary Hart, Ph.D., Director and Professor, Rural Health Research Center & Center for Health Workforce Studies, Family Medicine, University of Washington, Box 354982, University of Washington, Seattle, WA 98195-4982; Tel: 206-685-0402; Fax: 206-616-4768; Email: garyhart@u.washington.edu Research Objective: A key to performing quality research regarding the health workforce is how the geography of studies is measured. Generally, differences along the ruralurban continuum have been measured using county definitions, with the Office of Management and Budget (OMB) Metropolitan/Non Metro definition taking precedence. Refinements to the OMB definition, such as the Economic Research Service's Urban Influence Codes UICs) are often used in studies. These county-based measures suffer from lack of spatial specificity-they often grossly over and under bound cities. The Census Bureau's Urban definition is based on census tracts, which are not typically available in health care data sets. This definition has only three categories and often does not meet workforce analysis needs. The objective of this study is to describe a new methodological geographic tool upon which to base many health workforce and other health services research studies: the ZIP code-based RUCAs. In addition, it introduces the updated Version 2.0 of the geographic taxonomy and demonstrates its use with national physician workforce data. An additional tool (remoteness) developed for use with the RUCAs is also introduced. The remoteness tool provides the travel distance and time between each ZIP code and the nearest edge of an Urbanized Areas of 50,000 or more and/or the nearest edge of an Urban Cluster of 10,000 to 49,999. This allows researchers to use remoteness in combination with the RUCA geographic taxonomy. The remoteness tool can be employed per researcher specification to identify “frontier” areas. Study Design: The new Version 2.0 of the RUCAs and the new remoteness tool were utilized in combination with the 2005 American Medical Association (AMA) Masterfile and the 2005 American Osteopathic Association (AOA). Additional environmental population data such as poverty were linked to the ZIP code areas. Patient care physician supply by specialty was examined by RUCA code aggregations (e.g., remote and isolated small rural ZIP code areas) by state and Census Bureau Division and poverty, for example. In addition, findings were compared to results using the UIC county-based taxonomy. Population Studied: Population Studied: All the nation's patient care allopathic and osteopathic physicians were studied for the 50 states and the District of Columbia. Principal Findings: The nation's remote isolated small rural communities have extremely limited supplies of physicians, especially in combination with poverty. The findings show this to be much more true than previously reported using less precise geographic measures. Conclusions: The study results indicate that the RUCAs and the remote tool provide much more meaningful results in a basic workforce analysis than county-based alternatives. The findings show that there are dramatic variations in physician supply across the nation, even more so than previously reported. The description of the study results and of the RUCA taxonomy will help the audience understand the importance of better methodological specification of study geographic units and categories. Implications for Policy, Delivery, or Practice: Better geographic measurement of workforce supply is essential to effective policy development in implementation. Defining rural and urban must be a methodological priority for healthrelated workforce and other studies. Systematically dealing with geographic problems can enhance the validity and usefulness of health-related studies. Primary Funding Source: HRSA ●Is Physician Supply in Rural Ohio Associated With Unmet Need for Physician Visits? Lars Peterson, David Litaker, M.D., Ph.D. Presented By: Lars Peterson, Ph.D. candidate, Epidemiology and Biostatistics, Case Western Reserve University School of Medicine, 10900 Euclid Avenue, Cleveland, OH 44122; Tel: 216-407-0313; Email: lars.peterson@case.edu Research Objective: Rural areas have fewer physicians per capita compared to urban areas and rural residents receive fewer health care visits than urban residents. Federal rural health policy tends to focus on increasing availability of health care but evidence from previous research is contradictory about the effects of the local supply of physicians on utilization of physician visits. The purpose of this study, therefore, is to examine this issue further by assessing the association between physician supply in rural Ohio counties with a resident’s self-reported unmet need for physician visits. Study Design: The current study is a cross sectional multilevel analysis of individual level data from the Ohio Family Health Survey (OFHS) linked at the county level to the Area Resource File, which supplied the data on per capita physician supply. Our dependent variable is whether or not respondents reported an unmet need for a physician visit. We created random intercept models to examine the independent association of contextual physician supply characteristics with an individual’s report of an unmet need for physician visits. Effects of increasing rurality were measured using rural urban continuum codes (RUCC). Survey weights are incorporated in our analysis to yield results that are representative of the county population. Population Studied: 11,255 residents residing in all 48 rural Ohio counties in 2003-2004 obtained from the OFHS. Principal Findings: After controlling for individual factors often associated with unmet needs (female gender, minority status, lower educational attainment, intermittent or continuous absence of insurance coverage, having lower income, lack of a usual source of care, unemployment, not married, lower rating of physical health status) the weighted multi-level model revealed that the primary care physician to total physician (PCP/MD) ratio is associated with a lower probability that an individual reports an unmet need for a physician visit (OR = 0.25 (95% CI 0.07, 0.95)). Total MD’s per capita (OR = 0.95 (0.89, 1.03)), PCP’s per capita (OR = 1.11 (0.98, 1.27)) and RUCC (OR = 1.05 (0.83, 1.32)) are all not significantly associated with report of an unmet need for a physician visit. Models restricted solely to contextual factors demonstrated only the PCP/MD ratio is significantly associated with an unmet need for a physician visit (OR = 0.28 (0.08, 0.93)). Conclusions: Rural health policy has traditionally focused on increasing the supply of physicians as a means of maintaining the health of rural populations. Our results indicate, however, that it is not the number of physicians but rather the composition of the physician population in rural counties that is associated with an unmet need for physician visits. These results are consistent with other reports demonstrating the population health benefits of health care systems with an emphasis on primary care. Implications for Policy, Delivery, or Practice: To meet health care needs in rural areas, policy analysts should consider workforce composition (the PCP supply relative to overall supply) and not just the absolute number of physicians. Primary Funding Source: No Funding Call for Papers Does Structure Matter? Exploring the Impact of Physician & Nursing Models of Care Chair: Barbara Mark, University of North Carolina, Chapel Hill Sunday, June 25 • 10:30 am – 12:00 pm ●Team Structure and Patient Outcomes: Predictors of Adverse Events in Home Health Care Penny Hollander Feldman, Ph.D. Presented By: Penny Hollander Feldman, Ph.D., Vice President, Research and Evaluation, Director, Center for Home Care Policy and Research, Visiting Nurse Service of New York, 107 East 70th Street, New York, NY 10021; Tel: 212609-1530; Email: PFeldman@VNSNY.org Research Objective: To examine relationships between team “structure” and adverse events in home healthcare. Structural characteristics include variations in work volume, work distribution, staff education and experience. The research contributes to the empirical literature on predicting and reducing adverse events, and to the theoretical literature on how organizational characteristics such as staffing affect patient outcomes. Study Design: The study was conducted in a large home healthcare agency with 86 structurally varied nursing teams. Using clinical data for 56,346 patient care episodes delivered over six months, we created an index of adverse events based on 13 home care-specific measures classified by CMS as potential adverse events. Then we used a comprehensive risk adjustment technique to derive severity-adjusted quality scores (Z-Score and FE-Score) for each team. Using detailed administrative data, we captured information on staff age, education and job tenure, and also constructed objective measures of team structure – e.g., volume of episodes, volume of weekend admissions, volume of weekend visits and relative concentration of visits among nurses (HerfindahlHirschman index). Then we used multi-variate techniques to examine the relationship between the team quality scores (i.e., team-attributable adverse event rates) and the selected structural variables. Population Studied: The 86 teams, which varied widely in episode and visit volume, were staffed by group of core nurses (8-24) plus assorted therapists, social workers and “float nurses.” Average staff age was 44; average job tenure was 7.5 years. The patient population, averaging 71 years of age, was two-thirds female and ethnically diverse (40% white, 26% black, 24% Hispanic, 4% Asian, 6% other). Clinical diagnoses varied widely, with the most common being diabetes (13%), hypertension (8%) and congestive heart failure (5%). Principal Findings: Controlling for patient case-mix severity, the multivariate FE-score regressions found that adverse event rates were significantly lower for teams with higher patient volume (number of episodes) (P=0.01), greater workload concentration (Herfindahl) (P=0.06) and more weekend visits (p=0.02). Rates were significantly higher for teams with more weekend admissions (p=0.01). Nurses’ age, education and tenure at the agency were not significant (although tenure reached a significance level of p=0.22, with fewer years associated with higher adverse event rates). Conclusions: The protective effect of patient volume suggests that home healthcare teams may function more like hospital surgical teams who can adjust their procedure load and schedule to the available personnel, than like nurses on a general hospital or nursing home unit, who have less control over their workload or the resources to manage it. The protective effect of concentrated workload may be due to the narrower span of clinical managers’ control and/or to greater expertise gained by nurses among whom care delivery is concentrated. Implications for Policy, Delivery, or Practice: The findings underscore the riskiness of patient transitions, especially on weekends when organizations are understaffed. Further, the protective effect of weekend visits suggests that mobilizing personnel for frequent “off-hours” visits may be a critical safety factor in home care agencies, where weekend coverage is often spotty. However, if busy, productive teams produce better outcomes, care must be exercised to protect staff health and safety and to guard against nurse burnout. Primary Funding Source: AHRQ ●Does Increasing Hospital Nurse Staffing Lead to Better Patient Outcomes? R. Tamara Konetzka, Ph.D., R. Tamara Konetzka, Ph.D., Jingsan Zhu, M.B.A., Kevin G. Volpp, M.D., Ph.D. Presented By: R. Tamara Konetzka, Ph.D., Assistant Professor, Department of Health Studies, University of Chicago; Tel: (773) 834-2202; Fax: (773) 702-1979; Email: konetzka@uchicago.edu Research Objective: Proposals to mandate minimum nurse staffing levels are being debated in state legislatures across the country, motivated by findings from cross-sectional studies that link better outcomes with higher staffing levels. This longitudinal study informs those debates by (1) investigating the degree to which changes in hospital nurse staffing influence patient outcomes; 2) determining the shape of the staffing-outcomes relationship; and 3) identifying subgroups of hospitals that benefit the most from increasing staffing levels. Study Design: Annual hospital financial data and patient discharge data linked to death certificates for 1991 through 2001 from California’s Office of Statewide Health Planning and Development were used in multivariate regression models to determine whether changes hospital nurse staffing levels (RN, LVN, and nurse aides) well as RN skill mix (i.e., the percent of nursing personnel that are RNs) influenced mortality. Four AHRQ inpatient quality indicators—30-day mortality among acute myocardial infarction, stroke, hip fracture, and gastro-intestinal hemorrhage patients—serve as the outcome measures. We control for differences in the mix of patients across hospitals and for secular changes over time that could influence overall staffing levels. We use hospital fixed effects to control for time-invariant differences between hospitals and correct standard errors to account for clustering of patients within hospitals. We characterize the shape of the staffing-outcomes relationship by examining whether returns to quality diminish as staffing levels increase and whether thresholds exist in the relationship between staffing and outcomes. Population Studied: Patients with a primary diagnosis of AMI (529,914), stroke (728,194), hip fracture (326,905) and GI hemorrhage (464,919) in 450 short-term acute California hospitals. Principal Findings: Mortality declined significantly among AMI and stroke patients as RN staffing levels rose, though the effects were small: increasing RN staffing by one hour per patient day resulted in a 1.4% reduction in mortality. Increasing RN skill mix was associated with lower mortality among AMI patients, but these effects were likewise small. Changes in RN staffing levels and RN skill mix did not contribute independently to mortality among hip fracture and GI hemorrhage patients. Baseline staffing levels have an inconsistent effect on the staffing-mortality relationship across conditions. Conclusions: Longitudinal analyses of the relationship between nurse staffing levels and patient outcomes produce a much more tempered portrait than the findings from crosssectional studies. They suggest that a more nuanced analysis that investigates potential threshold effects in these relationships may be more informative. Implications for Policy, Delivery, or Practice: Determining whether and how changes in nurse staffing affects patient outcomes is critical to the current legislative debates over mandatory minimum nurse staffing levels. Without this information, staffing decisions based on cross-sectional associations could result in significantly overestimating or underestimating how much improvement in outcomes would be realized by changing staffing levels, both of which could have costly consequences. Primary Funding Source: Doris Duke Charitable Foundation ●Resident Physician Team Workload and Organization Effects on Patient Outcomes in an Academic General Internal Medicine Inpatient Service Michael Ong, M.D. Ph.D., Alan Bostrom, Ph.D., Arpana Vidyarthi, M.D., Charles McCulloch, Ph.D., Andrew Auerbach, M.D., M.P.H. Presented By: Michael Ong, M.D. Ph.D., Assistant Professor of Medicine, Medicine, UCLA, 911 Broxton Avenue, 1st Floor, Los Angeles, CA 90024; Tel: 310-794-0154; Fax: 310-794-0766; Email: michael.ong@ucla.edu Research Objective: Resident physician work-hour requirements have required residency programs to re-engineer inpatient services. However, there is little research on how resident physician workload or organization influences patient outcomes. This study examined the effects of internal medicine team workload and organization on patient mortality, readmission, and resource utilization. Study Design: Two-level mixed model analyses of patient inpatient mortality, 30-day readmission, lengths of stay, and total costs. Team structure and personnel information were merged with patient-level data to create variables of interest. Key adjusters included patient sociodemographic factors, severity adjustment by DRG weights and ICU stays, hospitalist supervision, discontinuities in care due to team personnel switches. Additional controls included service census effects, the academic quarter, year of admission, and if the admission occurred on a weekend. Population Studied: 5742 adults initially admitted to an academic medical center general medical service between July 1998 and June 2001. Principal Findings: Each increase in the admitting team’s admissions on a patient’s admission day increased length of stay (3.09%, 95% CI 2.22-3.96), total costs (2.31%, 95% CI 1.29-3.33), and risk of inpatient mortality (OR: 1.09, 95% CI 1.02-1.15). This mortality risk increase rises substantially when admitting over 9 patients. However, each increase in the admitting team’s average patient census during a patient’s hospitalization reduced length of stay (5.30%, 95% CI 4.546.07) and total costs (5.11%, 95% CI 4.20-6.00). This increase is concentrated in average censuses over 15 patients. Each increase in teams working on the day of admission also reduced length of stay (4.03%, 95% CI 0.96-7.01) and total costs (4.68%, 95% CI 1.09-8.15). In addition, admission to a team with two interns instead of one intern increased risk of 30-day readmission (OR: 1.41, 95% CI 1.05-1.89). Conclusions: Our findings suggest that higher internal medicine resident physician workload on admitting days increases resource utilization and potentially inpatient mortality risk. Higher team patient censuses are associated with reduced resource utilization, which may reflect teams’ responses to higher workloads. Increasing the overall number of GMS teams reduces resource utilization independent of team admission and census counts, and may be related to other benefits of workload reduction such as more time for teaching and learning. Two-intern teams may experience less supervision than one-intern teams, resulting in increased readmission rates. Implications for Policy, Delivery, or Practice: Programs seeking to minimize total costs and lengths of stay may want to find ways to reduce team admission loads. While teams appear able to reduce total costs and lengths of stay through internal mechanisms, these mechanisms may no longer be available in an era of strict adherence to work hours regulation. Primary Funding Source: No Funding Call for Papers Beyond the Numbers: Innovations in National & International Health Workforce Research Chair: Chapin White, Congressional Budget Office Monday, June 26 • 2:00 pm – 3:30 pm ●Physician Migration to the United States, Canada, United Kingdom and Australia: Profiling the Source Countries Onyebuchi A. Arah, M.D., M.P.H., Ph.D., Uzor C. Ogbu, M.D. Presented By: Onyebuchi A. Arah, M.D., M.P.H., Ph.D., Assistant Professor, Department of Social Medicine, Academic Medical Center of the University of Amsterdam, Meibergdreef 9, PO Box 22700, Amsterdam, 1100 DE; Tel: +31205665049; Fax: +31206972316; Email: o.a.arah@amc.uva.nl Research Objective: The World Health Organization has earmarked its 2006 world health report, appropriately titled “Working for Health”, for health workforce issues facing health systems. Developed and developing countries both have pressing shortages in nursing and physician workforces. Unfortunately, such staffing shortages, lack of specialist training positions in poorer countries, and the financial lure of the rich west have resulted in the so-called ‘fatal flows’ of physicians and nurses from the developing to the developed countries. Between 23 and 28 percent of physicians in the four large English-speaking countries, namely the United States, Canada, the United Kingdom, and Australia, are international medical graduates, 40 to 75 percent of whom come from lowto-middle income countries. It is not clear, however, whether the poorest and most disadvantaged source countries suffer more brain drain than other relatively poor countries. Therefore, our study is aimed at profiling the low-to-middle income countries that supply the most international medical graduates to the United States, Canada, United Kingdom and Australia. Study Design: We used the most recent data from the World Health Organization, World Bank and peer-reviewed articles to relate country characteristics to the magnitude of physician migration from source (low-to-middle income) countries to the United States, Canada, United Kingdom, and Australia. We examined the contemporaneous correlations between the per capita number of source countries’ physicians working in the four host countries and source countries’ characteristics including gross domestic product, physician density, health expenditure, percentage of population on less than one dollar per day, urban population annual growth, density of nurses, immunization rates, life expectancy at birth, under-five mortality and infant mortality rates. Population Studied: Thirty-six low-to-middle income countries from eight regions of the world that supplied the most international medical graduates to the United States, Canada, United Kingdom, and Australia, between 1999 and 2002. Principal Findings: We found that, among low-to-middle income countries, those that supplied more physicians to the United States, Canada, United Kingdom, and Australia were relatively richer, healthier, with higher immunization rates, and had higher physician density and health expenditure than their fellow source countries. Higher physician migration was not associated with unemployment rates, rural population density, and receipt of workers’ remittances in source countries. Conclusions: Even among poorer source countries, the poorest may not be the ones losing the most physicians to the wealthy countries. It is quite possible that as low-income countries get marginally less poor, their meager facilities allow them to train, but not retain or even sustain, quality physicians who then migrate to take up residency positions in the United States, Canada, United Kingdom, and Australia. Implications for Policy, Delivery, or Practice: As international medical graduates, we will like to see a more sophisticated analysis of the current issues surrounding physician brain drain, rather than the prevailing winners-andlosers and normative discussions that obscure the complexity of the causes, consequences and solutions of the global workforce problems. We hope our analysis will encourage developing countries to contribute actively to the ongoing debates and help craft intelligent solutions. Primary Funding Source: No Funding ●Determinants of First Practice Location Choice by New Physicians Chiu-Fang Chou, MPA, Anthony T. LoSasso, Ph.D. ensure that new physicians are prepared to meet the needs of the neediest populations. Primary Funding Source: HRSA Presented By: Chiu-Fang Chou, MPA, Doctoral Candidate/Research Assistant, The Division of Health Policy and Administration, School of Public Health, Midwest Center for Health Workforce Studies, University of Illinois at Chicago, 1747 W. Roosevelt Road, Room 558, M/C 275, Chicago, IL 60608-1264; Tel: (312)996-1792; Fax: (312)996-0065; Email: cchou4@uic.edu Research Objective: This study is aimed at understanding how new physicians choose their initial practice locations. The objectives of this study are to assess whether malpractice premiums have an effect on new physicians' choice of practice location and to examine how other local characteristics affect where new physicians choose to practice. Study Design: Statistical analysis involved conditional logit models to examine the factors affecting the choice of initial practice location by new physicians. Data are from a unique survey of exiting medical residents acquired by the HRSAfunded New York Workforce Center at SUNY Albany. These data are matched to data on malpractice premiums from Medical Liability Monitor. Additional location information is from the Area Resource File (ARF). The dependent variable is the choice of location among the 357 metropolitan statistical areas (MSAs) and non-metropolitan areas within each state in the United States. Where appropriate, independent variables have been weighted by area population. Other local market characteristics include hospital beds, per capital income, and the local unemployment rate. Population Studied: The sample consists of 9,133 physicians who just finished their residency training in New York and California in 1998-2003 and who are beginning their careers in patient care. Principal Findings: Preliminary conditional logit results indicate that malpractice premiums do not appear to be a deterrent to locating in a particular area, even for high malpractice specialties such as obstetrics and surgery. Conclusions: Given that malpractice premiums do not appear to be an important factor affecting new physician location choices, our results suggest that other factors outweigh anticipated malpractice concerns. These other factors might include lifestyle variables that are difficult to measure. Our results could also suggest that salaries for new physicians might already compensate for high malpractice costs. Implications for Policy, Delivery, or Practice: Newly graduated physicians represent a highly dynamic segment of the supply of physicians, and their practice location decisions can have a lasting impact on the future healthcare workforce. Therefore, it is critical to have a better understanding of how new physicians establish their careers, provide medical care, and meet their own expectations in the 21st Century healthcare market. Given the concerns about the distribution of physicians relative to need, finding the most salient characteristics associated with new physicians’ practice location would help state and national healthcare policymakers understand the needs of young physicians for strategic workforce planning. This study can also help medical education policymakers make future improvements in recruitment and in the overall medical education system to ●An Economic Analysis of the Labor Market for Dental Hygienists and Dental Assistants in California: 1997-2005 Tracy Finlayson, Ph.D., Timothy Brown, Ph.D., Richard M. Scheffler, Ph.D. Presented By: Tracy Finlayson, Ph.D., AHRQ Postdoctoral Scholar, School of Public Health, UC Berkeley, 140 E Warren MC7360, Berkeley, CA 94720-7360; Tel: 510-642-5652; Fax: 510643-4281; Email: tracyf@berkeley.edu Research Objective: A perceived shortage of both registered dental hygienists (RDHs) and dental assistants (DAs) was documented among dentists in 1999 by an American Dental Association Workforce Needs Assessment survey. This study used an economic framework to examine whether or not there was a labor market shortage for RDHs or DAs in California anytime between 1997 and 2005. Study Design: Labor shortages occur in a market economy when demand for workers is greater than the supply of workers who are qualified, available, and willing to do that job, at a given market wage. We used rising average inflationadjusted wages as a measure of labor shortage. Data on the demand for dental services, supply of RDHs and DAs, and market-determined wages for each profession were examined over time. The estimated numbers of and average hourly wages for RDHs and DAs in each metropolitan statistical area (MSA) in California were obtained from the U.S. Bureau of Labor Statistics’ Occupational Employment Statistics Survey. Trends in the number of candidates passing the California Hygienist Licensing Exam were also explored. Demand for dental services was assessed by the percent of adults with a dental visit last year, percent with dental insurance, and state dental expenditures. The numbers of RDHs and DAs were adjusted for the California population using California Department of Finance data, and wages were adjusted for inflation using the Consumer Price Index. Population Studied: This study focused on RDHs and DAs in California. Principal Findings: A clear rise in average inflation-adjusted wages for RDHs started in 1999. Wages appear to have peaked in 2002 and leveled off, at approximately 48% above their 1999 levels. This indicates that a fairly severe shortage of RDHs did occur during this period. There was no significant supply response in the population-adjusted number of RDHs to this increase in average inflation-adjusted wages. The average inflation-adjusted wages of DAs increased by 13.9% between 1997 and 2001. There was a large supply response in the population-adjusted number of DAs to the increase in average inflation-adjusted wages for DAs, and their numbers rose by 28% from 1997 until their peak in 2003. This resulted in the average inflation-adjusted wages for DAs returning to 1997 levels by 2005. Demand for dental services increased by 11.2% from 1997 to 2004. State dental expenditures rose 18.6% from 1995 to 2000. Between 1995 and 2003, the percentage of Californians with dental insurance increased 18.1%. Conclusions: Between 1997 and 2005, the demand for dental services appeared to increase in California. Inflation-adjusted wages increased for both RDHs and DAs, suggesting there were labor shortages during this time period. Labor markets for these professions behaved differently. Wages for RDHs increased substantially then stabilized at a higher level, and there was little supply response. DA’s wages increased slightly before returning to the previous level, and the shortage was corrected by an increase in DAs. Implications for Policy, Delivery, or Practice: This study provides information for understanding and responding to changes in the labor market of RDHs and DAs. Results have implications for future training, distribution and supply of the dental auxiliary workforce in California. Primary Funding Source: California Dental Association Foundation and UC Berkeley Petris Center ●The Evidence Base for Diversity in the Health Professions Somnath Saha, M.D., M.P.H., Scott Shipman, M.D., M.P.H. Presented By: Somnath Saha, M.D., M.P.H., Associate Professor, Medicine, Oregon Health & Science University and Portland VAMC, Portland VAMC (P3MED)/3710 SW U.S. Veterans Hospital Rd., Portland, OR 97239; Tel: 503-220-8262 x55418; Fax: 503-721-7807; Email: sahas@ohsu.edu Research Objective: Increasing the racial and ethnic diversity of the health professions workforce is commonly cited as essential to reducing racial/ethnic disparities in the quality of health care. Programs promoting diversity, however, including affirmative action policies, have become vulnerable in the last decade. Sustaining such programs will increasingly require documented evidence of the benefits of health professions diversity. The most compelling argument for a more diverse health professions workforce is that it will lead to improvements in public health. We therefore examined the evidence addressing the contention that health professions diversity will lead to improved population health outcomes. Study Design: Based on a conceptual model describing the potential impact of health professions diversity on health care access, quality, and outcomes, we conducted a systematic review to identify studies addressing four hypotheses: 1) that minority and non-minority health care providers serve different populations; 2) that racial/ethnic and language concordance between patients and health care providers is associated with minority patients´ use of services and adherence, quality of care, and health outcomes; 3) that institutional workforce diversity is associated with minority patients´ trust in health care institutions and use of services; and 4) that minority and non-minority health care providers, leaders, and researchers advocate for and implement different programs, policies, and research agendas. We searched the MEDLINE, HealthSTAR, CINAHL, and PsycINFO databases using strategies tailored to each hypothesis. We also reviewed the reference lists of included studies and relevant review articles. One reviewer read and qualitatively summarized each original study in terms of quality, characteristics (e.g., population, health profession category), and principal findings. Population Studied: Literature review. Principal Findings: Our search retrieved 586 abstracts, and we identified 55 original studies for inclusion. Seventeen studies addressed the service patterns of physicians (16) and dentists (1). These studies, many of them rated as highquality, uniformly found that minority providers disproportionately served minority, poor, Medicaid, and uninsured populations. Thirty-six studies addressed race and language concordance between patients and physicians (20), mental health providers (11), substance abuse counselors (4) and medical students (1). These studies were mixed in their results but generally found that both race and language concordance were associated with higher interpersonal quality of care (usually assessed with patient satisfaction surveys), and to a lesser extent, utilization and adherence. No studies directly addressed our hypotheses about institutional diversity and patient trust, or about differential program, policy, and research priorities between minority and non-minority health professionals. Conclusions: Current studies related to the impact of healthcare workforce diversity on access, quality, and outcomes are generally limited to those demonstrating that minority physicians disproportionately serve underserved populations, and that patient-provider race and language concordance are associated with higher interpersonal quality of care. Implications for Policy, Delivery, or Practice: Further research is needed to examine the service patterns of minority and non-minority health professionals other than physicians; the impact of race and language concordance on quality and outcomes of care; the association between institutional diversity and patient trust and use of services; and the programmatic and policy priorities of minority and nonminority health professional leaders. Such studies may play an important role in determining the fate of programs and policies aimed at increasing the diversity of the health professions workforce. Primary Funding Source: HRSA Related Posters Workforce Poster Session A Sunday, June 25 • 2:00 pm – 3:30 pm ●Mental Illness, Employment, and Labor Force Participation Pierre Alexandre, Ph.D.; M.S.; M.P.H. Presented By: Pierre Alexandre, Ph.D.; M.S.; M.P.H., Assistant Professor of Health Economics, Mental Health, Johns Hopkins University - Bloomberg School of Public Health, 624 n broadway, Ste 833, Baltimore, MD 21205; Tel: 410-502-2588; Fax: 410-955-9088; Email: pialexan@jhsph.edu Research Objective: Previous studies based on labor market effects of mental disorders using national representative surveys did not distinguish the employed from those who were in the labor force. This study investigates the differential effects of mental illness on employment and labor force participation. Study Design: We merged survey years 2002 and 2003 of the National Survey on Drug Use and Health (NSDUH), used Kwallis-ranksum tests to test differences in outcomes and control variables by mentally ill (SMIs) and non-mentally ill (NSMIs)individuals. Multivariable stantard probits as well as bivariate probit models that control for the potential endogeneity of mental illness in the labor market specifications were use to estimate the likelihood of employment and labor force participation. Population Studied: The study is based on individuals aged 25 to 64 from the 2002 and 2003 National Survey on Drug Use and Health (NSDUH),formerly the National Household Survey on Drug Abuse (NHSDA). Principal Findings: The main findings of our analysis were that mentally ill men and women were less likely to be employed or in the labor market relative to their non-mentally ill counterparts in both the univariate probit models and the bivariate probit models. Test of endogeneity suggest that the maximum likelihood estimates from the standard probit models were consistent. Conclusions: The findings of the present study are consistent with other labor market studies in that mental disorders have negative impacts on both men and women. Implications for Policy, Delivery, or Practice: The main policy implication of the study is that expansion of mental health services as a means to improve quality-of-life may promote economic benefits. Programs that prevent mental illness or improve mental health may sustain or even enhance work force productivity through avoiding the negative consequences of mental illness on labor market outcomes. Previous studies suggest that such programs were generally cost-effective and increased employment and job retention. Although these public health interventions may not lead to overall increases in labor supply, they may be justified on social welfare grounds. Primary Funding Source: NIAAA ●Mentoring Function as a Workforce Retention Strategy: Do mentoring needs change over time? Mary K. Anthony, Ph.D., John M. Clochesy, Ph.D. Presented By: Mary K. Anthony, Ph.D., Associate Professor, College of Nursing, 113 Henderson Hall, Kent State University, P. B. Box 5190, Kent, OH 44242; Tel: (330) 672-8824; Fax: (330) 672-1564; Email: manthony@kent.edu Research Objective: Hospitals struggle with the high turnover in critical care. Mentored orientation programs have been introduced as one way to improve retention and help new nurses transition into ICU. Mentoring has been found to be one of the most important relationships a novice can have, enhancing satisfaction and effectiveness. As part of the larger demonstration project to retain ICU nurses, the purpose of this study is to compare and assess the change in nurses’ actual and perceived importance of key mentoring functions over two time points during a 25 week ICU orientation program. Study Design: A descriptive comparative design using survey methodology is used. Two cohorts of RN novice nurses were hired into a 25 week mentored ICU orientation program into one of four critical care units at a major university hospital. Each novice nurse was assigned a mentor who met the criteria for assuming a mentoring role and attended a workshop on the responsibilities associated with mentoring. The 39-item 8dimension Fowler mentoring survey was distributed to novice nurses at approximately 3 and 6 months after hire. For each item, respondents were asked to rate both the importance and the extent that the mentoring function actually occurred. Of the 37 RNs hired into the program, 8 dropped out prior to completing the first 3-4 months of orientation and one nurse was on maternity leave, leaving a sample size of 26. Data is reported on a sample of 22 nurses who returned their surveys. Population Studied: The average age of nurses was 27.0 years, 86.4% had other healthcare experience, and 9.1% had worked with a mentor in a job outside of nursing, while 13.6% worked with a mentor in nursing. Principal Findings: Data collection for Cohort 2 at 6 month will be completed in February, 2006 and a new cohort (cohort 3) of nurses will be hired in March, 2006 and will be included in future analyses. For the 8 mentoring functions: personal and emotional guidance, coaching, advocacy, career development, role modeling, advice on strategies for working in a system, learning facilitation, and friendship, preliminary data suggest that in general nurses place higher importance on mentoring functions than they actually experience in the mentoring relationships, creating gaps between what is valued and what is received. Role facilitation, coaching and role modeling were rated the highest in both importance and actual occurrence. Conclusions: Twenty–two percent of nurses who were hired into ICU jobs left approximately 3-4 months after hire. At 3 months, novice nurses counted most on their mentor for learning the role, role modeling and coaching. In our final analysis, we will 1. compare whether the ordering of importance changes and 2. whether the extent to which nurses experience each mentoring function also changes. Implications for Policy, Delivery, or Practice: Shortages in the nursing workforce, particularly in critical care units, are projected to worsen. Gaps in what nurses perceive to be important and what they actually experience may be an important predictor of job retention. Primary Funding Source: HRSA ●Hospital Decision Making About Nurse Overtime Barbara Berney, Ph.D., M.P.H. Presented By: Barbara Berney, Ph.D., M.P.H., Assistant Professor, Department of Urban Public Health, Hunter College, 425 E. 25th Street Box 606, New York, NY 10010; Tel: (212)481-5165; Fax: (212)481-5260; Email: bberney@hunter.cuny.edu Research Objective: Nurse overtime in hospitals has become a contentious issue. Prior work done has found great variation in the use of overtime across hospitals, but no prior studies investigate management decision making in relation to use of overtime versus alternative staffing strategies. This study compares the use of overtime, agency, per diem, internal swing staff and other staffing strategies for handling peak staffing demand in hospitals. Study Design: Structured interviews with hospital nurse executives. Population Studied: Ten New York State hospitals, five with high overtime, five with low overtime. Principal Findings: Preferences for overtime versus agency staff depends on cost differentials and contract requirements. Most nurse executives interviewed indicated they would prefer to hire additional staff than use overtime or other alternative staffing, but are unable to do so because of constrained supply. Most overtime is worked as additional shifts, not following a completed shift. Most nurse executives also feel constrained to use twelve hour shifts because preferences of nurses for such shifts make this an important recruiting tool. They experess concern that nurses working fewer shifts per week due to twelve hour shifts results in less continuity of care for patients. Conclusions: The level of overtime use by hospitals is a management decision, with use of overtime influenced by relative cost and contract requirements. Implications for Policy, Delivery, or Practice: Results are directly applicable for hospital managers, regulators, and policy makers developing policy for controlling and regulating nurse overtime. Further work is needed to study the impact of twelve hour shifts on continuity of care. Primary Funding Source: PSC-CUNY ●Satisfaction of Frontline Nursing Home Workers: Effect of Organizational and Individual Factors and Impact on Resident Well-being Christine Bishop, Ph.D., Dana Beth Weinberg, Ph.D., Jody Hoffer Gittell, Ph.D., Lisa Dodson, Ph.D., Walter Leutz, Ph.D. Presented By: Christine Bishop, Ph.D., Professor and Director, Ph.D. Program, Heller School for Social Policy & Management, Brandeis University, 415 South Street Mailstop 035, Waltham, MA 02454-9110; Tel: 781-736-3942; Email: bishop@brandeis.edu Research Objective: To examine how workplace relationships and the organization of work affect turnover of front-line nursing home workers; and whether worker satisfaction is related to resident satisfaction. Study Design: Administrators and front-line supervisors were interviewed in fifteen Massachusetts nursing homes to gather information on human resources management and work practices. Surveys concerning work-place relationships, job satisfaction, and resident care were designed and administered to all nurse supervisors (Response Rate: 89%) and Certified Nurse Assistants (CNAs) (RR: 94%) on two units in each nursing home. A resident satisfaction survey was administered to a sample of five residents on each unit (RR: 87%). The impact of organizational, relational, and individual characteristics on intent to stay in current job was estimated using statistical techniques that account for clustering of the sample. Differences between general attitudes of supervisory nurses toward CNAs and CNA perception of own supervisor’s attitudes and practices were explored for impact on satisfaction. The relationship between CNA job satisfaction and resident satisfaction was investigated. Population Studied: 252 Certified Nurse Assistants (CNAs) in 15 Massachusetts nursing homes Principal Findings: The quality of a CNA's relationship with her/his own nursing supervisor is highly associated with intent to stay in a job; staffing levels and sense of teamwork with other CNAs also affect intent to stay, as do individual age and education. Empowerment of CNAs to participate in care planning does not appear to improve job satisfaction. Statistical analysis suggests some linkage between CNA satisfaction and resident well-being. Conclusions: As has been found in other industries, quality of supervision is critically important to job satisfaction of nursing home workers. Task interdependency of the CNA-nurse supervisor dyad may decrease the relevance of relationships with other CNAs to job satisfaction. Difficulties in measuring resident satisfaction can impede attempts to identify organizational practices that support resident well-being. Implications for Policy, Delivery, or Practice: Results suggest that the supervisory skills, attitudes, and practices of licensed nursing personnel are a key to reducing CNA turnover and improving resident well-being, and are highly relevant for transition to resident-centered care (“culture change”). Primary Funding Source: RWJF, Atlantic Philanthropies ●The Centers for Medicare and Medicaid Services (CMS) Direct Service Workforce Demonstration Grants: Lessons Learned and Preliminary Findings of 10 Grantees Working to Improve Recruitment and Retention of Direct Service Professionals Carrie Blakeway, M.P.A., Karen Linkins, Ph.D., Lisa Alecxih, M.P.A. Presented By: Carrie Blakeway, Master of Public Affairs (MPAff), Senior Associate, Applied Economics, The Lewin Group, 3130 Fairview Park Drive, Suite 800, Falls Church, VA 22042; Tel: 703-269-5711; Fax: 703-269-5501; Email: carrie.blakeway@lewin.com Research Objective: To assess the preliminary outcomes of the Centers for Medicare and Medicaid Services (CMS) Demonstration to Improve the Direct Service Workforce grants that were awarded in 2003 and 2004. Our purpose is to inform policy makers and other stakeholders about the progress that has been made by these grantees, and in what areas, and the impact they have had on recruitment and retention of direct service professionals after after almost three years for the 2003 grantees and two years for the 2004 grantees. Study Design: We reviewed data from the following sources for this analysis: grantees’ work plans and evaluation plans, grantees’ quarterly reports submitted to CMS, granteereported turnover and retention data at participating agencies, grantees' requests for technical assistance and other grantee communications with TA providers, and other grantee materials. We present process findings and workforce outcomes across all grantees and broken down by types of interventions and year of grant award. Population Studied: The ten CMS DSW grantees (state agencies and private employers) working to improve recruitment and retention of direct service professionals. Six grantees are implementing interventions that provide or promote health care coverage for direct service workers. The North Carolina, New Mexico, and Virginia grantees pay for all or part of workers’ health insurance in multiple participating agencies. Maine and Washington are marketing and assisting workers to enroll in state sponsored health insurance programs, and the Indiana offers workers in one agency a monthly cafeteria-style benefit that they can use to cover health care expenses. Five of these six states are implementing other interventions such as offering workers peer mentorship programs, certificate programs, professional networking opportunities, and participation in worker registries. Four grant projects (in Delaware, Louisiana, Arkansas and Kentucky) offer these kinds of expanded training opportunities and workplace enhancements for workers without a health insurance intervention. Principal Findings: Overall, five of the ten grantees have made some or significant progress toward their goals in all major areas of grant activity. Some have demonstrated reduced turnover and improved retention in participating agencies. Grantees have reported the most challenges in the area of intervention design, such as working out the details of interventions or redesigning interventions when problems were discovered upon implementation. Grantees have reported successful strategies in many areas, including designing workplace enhancements that are attractive to agencies and workers - an area where significant challenges had also been reported Implications for Policy, Delivery, or Practice: As the demand for long term support services increases, the Centers for Medicare and Medicaid Services (CMS) recognizes the importance of making informed decisions and building policy in this area based on a strong groundwork of evidence. These demonstrations will serve to better inform federal and state policy makers, private employers, direct service workers, consumers and other stakeholders about what kinds of employee benefits, training, job structure, management, recognition and rewards have a positive impact on recruitment and retention in this field. In addition, the experience of these grantees in implementing their grant projects should help to inform others interested in undertaking similar types of workplace interventions and recruitment strategies. Primary Funding Source: CMS ●Physician Stress and Life Satisfaction Richard Bogue, BA, MA, Ph.D., Herdley Paolini, Psy.D., Brian Fisak, Ph.D. Presented By: Richard Bogue, BA, MA, Ph.D., Senior Research Fellow and Director, Center for Health Futures, Florida Hospital, 200 N. Lakemont Av., Winter Park, FL 32792; Tel: 407-646-7119; Fax: 407-646-7146; Email: richard.bogue@flhosp.org Research Objective: Physician stress and satisfaction are associated with quality, cost, job burnout and longevity. Physician supply may be inadequate to future demand. Helping "doctoring" be more satisfying may increase both the supply and productivity of physicians. This research (1) examines stress and satisfaction in physicians' professional lives, and (2) learns why some physicians are more highly satisfied. Study Design: The study used survey and interview methods. The survey gathered demographics, practice characteristics, self-rated stress, and 17 self ratings on satisfaction. The single stress item had reasonable reliability (r for matched subsamples = .245, p < .001). The satisfaction scale had good reliability (Cronbach's Alpha = .87). Quantitative analyses of factors associated with stress were conducted with ANOVA and hierarchical regression. Twenty-four semi-structured interviews were conducted with physicians who (a) scored very highly satisfied and (b) represented a variety of specialties, career stages, and both genders. The interviews identified and detailed "life practices" that the highly satisfied physicians believe explain their higher satisfaction. Qualitiative analyses included transcription and Q-Sorting. Population Studied: 705 physicians participated from the 1,800 member staff of a southeastern US regional health system. Principal Findings: Age, hours worked per week, and an index based on a subset of satisfaction items associated with Personal and Family Issues were most strongly associated with stress. Gender, number of children, and several workspecific issues were less strongly associated. Hierarchical regression revealed that Personal and Family issues accounted for 2.6 times more of the variation explaining stress than hours worked per week, and three times more than age. Q-Sorts of interviews with highly satisfied physicians revealed 10 types of Life Practices explaining higher satisfaction. The three most common explanations were (a) Implementing choices about how to organize the practice of medicine, (b) Taking steps to create positive sentiments with patients, (c) Observing one's own momentary stress responses and intervening promptly. Conclusions: Physician stress is most strongly associated with satisfaction with Personal and Family Issues, rather than work-specifc items. Results suggest that satisfaction around Personal and Family Issues buffers doctors from stressful work-related effects. Health systems, hospitals and physicians themselves can take concrete steps improve physician satisfaction. Implications for Policy, Delivery, or Practice: More productive business and personal relationships with physicians could result from an appreciation of this study's findings. Health system and physican leaders might consider a more comprehensive approach to physician relations to find ways to improve physicians' satisfaction beyond the business and clinical relationship. Personal counseling services, children's day care, free access to fitness centers, and other concrete steps may contribute to stronger bonds with more satisfied and productive physicians. Primary Funding Source: Winter Park Health Foundation ●The Allied Health Workforce: Occupational Change in International Context - A Comparative Study of Australia and the UK Rosalie A. Boyce, B.Sc., M.Bus., Ph.D., Susan Nancarrow, Ph.D. Presented By: Rosalie A. Boyce, B.Sc., M. Bus., Ph.D., Research Fellow, School of Health & Rehabilitation Sciences, University of Queensland, University of Queensland, School of Health & Rehabilitation Sciences, Brisbane, 4072; Tel: 61 7 3365 1048; Fax: +61 7 3365 4754; Email: r.boyce@uq.edu.au Research Objective: International analyses of workforce planning techniques advocate moving away from singleprofession models towards integrated inter-professional or service-focused approaches. Lack of knowledge about the allied health professions has been identified consistently as an impediment to progressing new inter-professional workforce planning and development models. As the health workforce is increasingly perceived in global terms and trans-national migration of workers is expected to expand, it is important that we increase our understanding of the workforce in a range of national contexts. The objective of this research is to add to the limited body of international knowledge about the allied health professions (non-physician, non-nursing). This objective is achieved by focusing on Australia and the United Kingdom and presenting results from a comparative study that examines (a) trends in workforce supply, (b) key issues in the national policy contexts of each country that underpin workforce outcomes and (c) how senior profession managers and clinicians perceive the relative importance of workforce dilemmas in each national context. Study Design: Data was gathered from official national statistical agencies to chart trends in workforce change. National policy documents were analyzed to identify key issues in each national context and the organisational and professional context were examined by reference to secondary research sources. NVIVO qualitative thematic analysis software was utilized on survey data (n=261) to identify issues and barriers to workforce change in each country. Population Studied: Senior profession managers and clinicians in the allied health professions in Australia and the United Kingdom. In these national contexts allied health does not include nursing, medicine or dentistry. Professions designated as core members of allied health in Australia and /or the United Kingdom include physiotherapy, occupational therapy, speech pathology, audiology, dietetics, social work (Australia), pharmacy, podiatry, clinical psychology, medical imaging, orthoptics and prosthetics and orthoptics. Principal Findings: In Australia growth in allied health significantly has exceeded that of medicine, nursing, all health occupations and national population growth since the 1990s. Strong growth patterns have also been observed in the UK particularly since growth targets have been set as part of recent policy positions. Australian’s rated ‘professional tribes’ and status and hierarchy highly as key issues in achieving workforce change. UK respondents rated explicit Department of Health policy initiatives and funding issues highly. Respondents from both countries highlighted several issues as shared concerns: recruitment and retention issues, changing roles, lack of involvement in policy development and a lack of research capacity. Conclusions: Workforce change in allied health in the UK has largely progressed as a result of top down policy initiatives. Conversely, in Australia, the lack of an overarching federal policy framework for achieving workforce change has resulted in more diversity of approaches and more bottom-up initiatives from the organisational level of health service agencies and segments of the professions themselves. Implications for Policy, Delivery, or Practice: The study confirmed that the nature of allied health professions is specific to the national context. As a result, making assumptions about the homogeneity of allied health at the level of international analysis is fraught with difficulty. Development of Allied Health Workforce Investment Strategies are recommended. Primary Funding Source: Australian Research Council; Univerisity of Queensland Research Fellowship Scheme ●Effect of RN Staffing on RN Workgroup Satisfaction Diane K. Boyle, RN, Ph.D., Peggy A. Miller, RN, MS, Byron J. Gajewski, Ph.D., Susan F. Klaus, RN, MSN, Nancy Dunton, Ph.D. Presented By: Diane K. Boyle, RN, Ph.D., Associate Professor, School of Nursing, Univerisity of Kansas Medical Center, MS 4043, 3901 Rainbow Blvd., Kansas City, KS 66160; Tel: (913) 588-1686; Fax: (913) 588-1660; Email: dboyle@kumc.edu Research Objective: To examine the effect of patient-to-RN ratio on RN workgroup satisfaction in a national sample of four adult, acute care unit types: step-down, medical, surgical, and combined medical-surgical. Study Design: We used cross-sectional analyses of linked data from the 2004 National Database of Nursing Quality Indicators’ (NDNQI) RN Satisfaction Survey and unit staffing data. For each unit type, logistic regression models estimated the effect of patient-to-RN staffing ratio on three RN workgroup outcomes: low general job enjoyment, low organizational satisfaction (including satisfaction with nurse manager, nursing administration, professional development), and low practice satisfaction (including satisfaction with nurse-nurse interaction, nurse-physician interaction, task, autonomy). Analyses controlled for hospital structural (e.g., Magnet status, size, ownership) and RN workgroup characteristics (e.g., mean years on unit, mean years in practice, percent full-time). To calculate staffing ratio, unit RN care hours per patient day (RNHPPD) were divided by 24. RNHPPD were collected according to National Quality Forum specifications (limited to RNs with direct patient care responsibilities). The NDNQI RN Satisfaction Survey subscales exhibit individual and workgroup (unit) level reliability and validity. NDNQI satisfaction scores are calculated as T-Scores, with T-scores less than 40 (more than one standard deviation below mean) considered low satisfaction. Population Studied: The sample included 206 NDNQI hospitals in 44 states. A total of 801 patient care units met the criteria of (a) participation in the RN Satisfaction Survey, and (b) submission of RNHPPD for 3-months prior to the RN Satisfaction Survey: 160 step-down (3,454 RNs), 234 medical (4,621 RNs), 188 surgical (4049 RNs), and 219 combined medical-surgical (4,278 RNs). Principal Findings: Mean patient-to-RN ratios for the unit types were: step-down 3.63:1, medical 5.14:1, surgical 4.89:1, and combined medical-surgical 5.00:1. For medical units, an increase of 1 patient per RN was significantly associated with the likelihood of low RN workgroup satisfaction (T score < 40) on all three outcomes: job enjoyment (OR 1.35), organizational satisfaction (OR 1.39), and practice satisfaction (OR 1.58). For step-down units, an increase of 1 patient per RN was significantly associated with the likelihood of low RN workgroup satisfaction on two outcomes: organizational satisfaction (OR 1.40) and practice satisfaction (OR 1.61). For combined medical-surgical units, only low practice satisfaction was associated with an increase in 1 patient per RN (OR 1.30). Patient-to-RN ratio was not associated with RN workgroup satisfaction on surgical units. Conclusions: Previous research on RN staffing and satisfaction used state or regional samples and conducted analyses at the hospital or total sample level. Using a sample from 44 states, we were able to document staffing effects on RN workgroup satisfaction when unit types were examined separately. Our data indicate that RN workgroups with higher patient workloads in step-down, medical, and combined medical-surgical units are significantly more likely to experience low satisfaction. For example, RN workgroups in medical units with a patient-to-nurse ratio of 8:1 would be 3.94 times more likely (i.e., 1.58 taken to the 3rd power) to express low practice satisfaction than medical unit RN workgroups with a 5:1 ratio. Implications for Policy, Delivery, or Practice: There is a documented link between job satisfaction, burnout, and turnover of RNs. Improvements in RN staffing may be accompanied by improved RN satisfaction, and thereby decreased burnout, turnover, and reduced replacement costs. Primary Funding Source: American Nurses Association ●An Examination of RN Workforce Participation Over Time Carol S Brewer, Ph.D., RN, Christine T Kovner, Ph.D., RN, William Greene, Ph.D., Yow-Wu-Wu, Ph.D., Ying Cheng, MA Presented By: Carol S Brewer, Ph.D., RN, Assocaite Professor, School of Nursing, University at Buffalo, 918 Kimball Tower, Buffalo, NY 14214; Tel: 716-829-3241; Fax: 716-829-2021; Email: csbrewer@buffalo.edu Research Objective: We examine the time 1 factors that influence Registered Nurses’ workforce participation (full-time or part-time), conditional on choice to work or not work, at time 2. Study Design: Two wave panel survey design (one year apart). The year 1 survey included demographic questions, work setting variables, and movement constraints. Year two included actual work status. We added county characteristic as controls from Metropolitan Statistical Area data from Interstudy, the Bureau of Labor Statistics, and the Area Resource File. Population Studied: A random sample of 4000 RNs from 40 MSAs in 29 states was randomly selected; we achieved a 48% response rate in year one. In year 2, 1348 RNs responded to both surveys (70.7% response rate). We selected female RNs (N=1172). Principal Findings: The data were analyzed using bivariate probit regression with selection bias correction. The WK/NW probit excluded work setting variables. The NW/Work and PT/FT relationship (rho) is not significant unless intent to work in the next 12 months is in the model. RNs with children both under and over 6 reduced the probability of working in year 2. Higher predicted wages, foreign graduate RNs or RN intention to work increased the probability of working in year 2. In the FT/PT regression, RNs who were an APN, resided in a small MSA or an MSA with higher inpatient per day ratios, had a higher quantitative workload, paid time off or health insurance increased the probability of working FT. If RNs were a minority, had any children under 6, wanted to work more hours, thought benefits were not important or worked in an MSA with a higher RN ratio, the probability of working parttime (PT) in year 2 was increased. Conclusions: As predicted by organizational theory, intent to work was a major predictor of actual work status. Different factors influence deciding to work or not versus working FT or PT. Variables such as satisfaction and organizational commitment, typically important in organizational turnover, did not affect work status in year 2 although intent and quantitative workload inventory did. MSA market level variables influence RN work participation, and need to be included in more RN work participation studies. Implications for Policy, Delivery, or Practice: Wages predicted whether or not nurses chose to work at all, but did not impact FT/PT status, indicating that non-wage factors, such as benefits that are under the control of employers, were more important in predicting FT work status. There were no differences between hospitals and non-hospitals, suggesting that all employers need to work to attract nurses. The consistent importance of children under 6 in reducing work participation of RNs suggests this is an important target for employers. Except for workload, traditional organizational factors used in turnover models did not explain FT/PT participation of the workforce. It is possible that variables used in turnover studies to predict turnover may predict leaving a particular organization, but not actual participation in the workforce. Most measures of market forces have been ignored in studies of RN workforce participation, but indicate that RNs make work decisions in the context of opportunities in their MSAs. Primary Funding Source: AHRQ, R01 HS11320 ●The Labor Supply of Advanced Practice Nurses Timothy Brown, Ph.D. Presented By: Timothy Brown, Ph.D., Associate Director of Research, Petris Center - School of Public Health, University of California at Berkeley, 140 Earl Warren Hall, MC7360, Berkeley, CA 94720-7360; Tel: 510-643-4103; Fax: 510-643-4281; Email: tbpetris@berkeley.edu Research Objective: To determine the sensitivity of the supply of labor of Advanced Practive Nurses (APNs) to changes in earnings per hour. The labor supply behavior of APNs has not been studied previously according to my knowledge. Study Design: The supply of labor is estimated as a function of earnings per hour and unearned income. The model is estimated as both a three-part supply model (labor participation, hours per week, weeks per year) and a two-part model (labor participation, annual hours). Control variables include sex, age, the square of age, education, race/ethnicity, children at home, and year dummies. Work setting is also included in the sensitivity analysis. Selection corrections are included as appropriate. Earnings per hour is adjusted to include only after-tax earnings (estimated federal and state income taxes are excluded). Separate models are run for single and married APNs. A squared term for earnings per hour is also included to pick up the effect of any backward bend in the labor supply curve. Three waves of the National Sample Survey of Registered Nurses (1992, 1996, 2000) are combined with data from the Bureau of Labor Statistics, the Area Resource File, and the National Bureau of Economic Research. Labor participation equations are estimated using two-stage probit models. Hours per week, weeks per year, annual hours equations are estimated using two-stage generalized least square models. Since earnings per hour are endogenous, they are instrumented by the wages of non-APN registered nurses, the lagged wages of registered nurses, physicians per capita, hospital beds per capita, and unemployment (all measured at the level of the Metropolitan Statistical Area to proxy labor markets). The strength of the instruments in the first stage are tested using the StaigerStock test. The exogeneity of the instruments is tested using an overidentification test. The endogeneity of the earningsper-hour predictions is tested using a Hausman-type test. All estimates also account for the complex survey design of the data. Population Studied: Advanced Practice Nurses in the U.S. for the years 1992, 1996, and 2000 as sampled by the National Sample Survey of Registered Nurses. Principal Findings: The labor market for APNs is functioning Conclusions: APNs do respond to economic incentives. Implications for Policy, Delivery, or Practice: Economic incentives should be the first line of response to perceived labor shortages or labor surpluses of APNs. Primary Funding Source: AHRQ ●Physical Therapy Education Programs in California: Trends and Policy Implications Susan Chapman, Ph.D., RN, Timothy Bates, M.P.P. Presented By: Susan Chapman, Ph.D., RN, Assistant Professor and Director of Allied Health Workforce Studies, Center for Health Professions, University of California, San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: (415) 502-4419; Fax: (415) 476-4113; Email: schapman@thecenter.ucsf.edu Research Objective: Although the decision was controversial, the physical therapy profession is moving toward doctoral level preparation for practice. The rationale is that clinical scope, consumer recognition, interaction with medical colleagues, and management skills will be enhanced. This additional education is not required for licensure; graduates from accredited BS, MPT, or DPT programs are all eligible to sit for the licensure exam. The purpose of this project was to assess how the move toward doctoral education shifted the number and type of education programs available, the number of degrees awarded at each educational level, and thus the supply of licensed PTs in California. An additional objective was to assess the impact on PT assistant (PTA) programs and supply. Study Design: The research was conducted in California as part of a larger health workforce tracking project. The data source used is a series of “Completions” surveys administered through the Integrated Postsecondary Education Data System (IPEDS), through the Department of Education. Population Studied: Education/training programs for Physical Therapists and Physical Therapy Assistants in the state of California. Principal Findings: Since 1998, there have been shifts in the level and number of degree awards for professional programs in both PT and PTA. Within Physical Therapy, the shift is away from the Master of Physical Therapy (MPT) toward the Doctor of Physical Therapy (DPT). In 1998, DPT awards were only 17% of the total number of awards; in 2004, their share was 31%. Additionally, whereas in 1998 only two schools offered the DPT, in 2004 this number had grown to six in California. In 2004, in California, 14 programs reported PT awards at the Master’s or Doctoral level. Of these 14, 4 offered both the DPT and the MPT, 8 offered only the MPT, 2 offered only the DPT. Although the number of institutions offering PTA Associate Degree programs has remained stable, there has been a significant decline in the number of awards. In 1998, there were 271 Associate Degrees awarded; in 2004, there were only 95. In contrast to the declining numbers of Associate Degree awards for the PTA, opportunities for training as a Physical Therapy Aide (unlicensed) appear to be on the rise. The Bureau of Private Postsecondary & Vocational Education in the California Department of Consumer Affairs lists approximately 35 different institutions offering training as a Physical Therapy Aide. Conclusions: The shift in program offerings in physical therapy education is quickly moving to favor the doctoral degree for entry level practice despite the lack of consensus that it is clinically warranted. We expected to see an increase in PTA awards yet data indicates a decrease in PTA degrees as well. Further study is needed to determine whether a shortage is practicing clinicians is perceived. Implications for Policy, Delivery, or Practice: Will “degree creep” happen in similar professions? Education costs will increase for students and educational institutions. Potential decrease in supply of practicing PTs as time in pipeline increases. Will more unlicensed staff be used in practice? Consumer confusion as to who is a PT. Primary Funding Source: The California Endowment ●Estimates of Multiple Jobholding and Wages of Registered Nurses in Metropolitan Statistical Areas Ying Cheng, MA, Ph.D. Candidate, Carol S. Brewer, RN, Ph.D., Christine K. Kovner, RN, Ph.D., FAAN Presented By: Ying Cheng, MA, Ph.D. Candidate, Research Assistant, Economics, State University of New York at Buffalo, 924 Kimball Tower, Buffalo, NY 14214; Tel: 716-829-3611; Fax: 716-829-2021; Email: ycheng5@buffalo.edu Research Objective: The effects on wages of demographic characteristics, working conditions and geographic variation have been studied. However, the relationships between multiple jobholding (holding one or more secondary jobs), wages and work hours have not been explicitly examined in an endogenous framework. Our objective was to examine the determinants of multiple jobholding and test whether endogeneity exists in moonlighting behavior of registered nurses (RNs) in metropolitan statistical areas (MSA). Study Design: In spite of economic theory that suggests endogeneity exists between wages and work hours, researchers have not considered multiple jobholding as an endogenous variable in this model. We address the explicit relationship between multiple jobholding, wages and work hours through endogenous equation models. The models include demographic variables (age, education, gender, race, marital status), MSA level variables, work variables (working settings, positions, schedule, work benefits) and work attitude measures (work family conflicts, work load, work motivation). Two-step estimation and 2-stage conditional maximum likelihood regression models are used to test the existence of endogeneity. Population Studied: The survey design had a randomly selected sample of RNs from 40 MSAs in 29 states and 1907 RNs responded (48%). Of this sample, a subsample of working RNs (n=1645) was used in the analysis. This survey data was merged with the BLS (Bureau of Labor Statistics) unemployment rate data, Interstudy Competitive Edge Part III Regional Market Analysis data and the Area Resource File. The final dataset includes RN demographic variables, RN work setting variables and MSA market variables. Principal Findings: Endogeneity exists in multiple jobholding behavior (the chi-square test is significant at 5% level). Education (Diploma), small MSA size and work hours are negatively related to the probability of holding secondary job. Race, partner’s income and marital status have no significant effect. RNs with Master's or Doctoral degree, male, higher work family conflicts and wages are more likely to hold secondary jobs. Conclusions: This study demonstrated the effects of wages on RNs’ multiple jobholding behavior, as well as showed that MSA level variables and demographic factors as well as work attitudes were influential on RNs’ jobholding behavior. These results indicated that RNs moonlight in a secondary job because of market demand for more human capital, but not for the need to meet regular household expenses, as workers in other occupations reported in Current Population Survey. Implications for Policy, Delivery, or Practice: The differential pattern in the acquisition of secondary job by gender, MSA size and education is consistent with the persistent income gap in household between males and females and across regions. RNs with more educational human capital can respond to the demand for RNs by accepting a secondary position. Primary Funding Source: AHRQ ●Do Physicians and their Relatives have a Decreased Rate of Caesarean Section? A 4-year Population-based Study in Taiwan Yiing-Jenq Chou, M.D, Ph.D., Cheng-Hua Lee, M.D, DrPH, Nicole Huang, Ph.D., I-Feng Lin, Chung-Yeh Deng, Yi-Wen Tsai, Long-Shen Chen, Presented By: Yiing-Jenq Chou, M.D, Ph.D., Associate Professor, Department of Social Medicine, National Yang Ming University, 155, Li-Nong Street, Section 2, Taipei, 112; Tel: 886-2-28201458; Fax: 886-2-28261002; Email: yjchou@ym.edu.tw Research Objective: The increase in the rate of cesarean deliveries may be due partly to a lack of consumer knowledge. Assuming that physicians and their relatives are well informed of the risks and benefits associated with the different methods of delivery, our goal was to compare caesarean rates between female physicians, female relatives of physicians, and women with high socioeconomic status in Taiwan. Study Design: A pooled cross-section time-series design. Population Studied: Two subgroups of 588 female physicians and 5,021 relatives of physicians aged 20-50 years were compared with 96,104 with monthly wage?40,000 New Taiwan (NT) dollars included from a nation-wide representative sample of the general population of Taiwan from 2000 to 2003. Principal Findings: Female physicians (adjusted odds ratio 0.66; 95% CI 0.47, 0.93) and female relatives of physicians (adjusted odds ratio 0.84; 95% CI 0.74, 0.95) were significantly less likely to undergo a caesarean section than other high socioeconomic status women, adjusted for clinical and non-clinical factors. Conclusions: In the study, the cesarean rate was lower among women who may have greater access to medical knowledge. However, the lower rates observed among female physicians and physician relatives in Taiwan are still considerably higher than the national averages of many countries. This suggests that other than information, practice pattern, social and cultural milieu, may play a role. Implications for Policy, Delivery, or Practice: Debates about the appropriate use, rates, and relative safety of caesarean section are likely to continue. Using physicians and family members of physicians as a reference may be reasonable in the short term, but is perhaps not good enough. In the long run, efforts must continue to contain the rising trend of caesarean sections, and minimize the potentially inappropriate use of this procedure. Sufficient and reliable information must be made available to pregnant women, so that they can make informed decisions. Also, in developing countries, strategies to further reduce cesarean rates to an acceptable global standard should take diverse social and cultural factors into consideration. Primary Funding Source: Taiwan's National Science Council ●The Professional Scope of Practice of Dental Hygienists and Favorable Oral Health Outcomes for Children and Adults: A Multi-level Model Analysis Tracey Continelli, BA, Margaret Langelier, MS, Paul Wing, D Engin Presented By: Tracey Continelli, BA, Research Assistant, Center for Health Workforce Studies, 7 University Place / Room 334, Rensselaer, NY 12144-3458; Tel: (518) 402-0250; Email: tac02@health.state.ny.us Research Objective: Concern for the oral health status of Americans was heightened with the 2000 publication of "Oral Health in America: A Report of the Surgeon General." The impact of poor oral health was a fundamental theme of the report which presents the major economic and social issues surrounding the effects on individuals and society of poor oral health, and most importantly, the need to extend oral health services to a variety of Americans with inadequate access to fundamental dental services. One important way to improve access is the expansion of the legally mandated scope of practice for dental hygienists. Levels of legally prescribed professional status differ widely from state to state, such as requirements for differing levels of supervision, continuing education, and actual services that can be provided. The tasks permitted to dental hygienists in statute and regulation affect the ability of the profession to provide preventive oral health services to patients, particularly vulnerable population or rural populations, which often encounter difficulty with access to care. The goal of this analysis is to investigate whether or not the professional scope of practice for dental hygienists can exert an impact upon oral health outcomes in children and adults within the United States. Study Design: An index was created to quantify the professional practice environment of dental hygienists. This index summarizes the legal practice environment prescribed by State law for the profession in each of the 50 States and the District of Columbia for the year 2001. Four aspects of the design emerged: a legal / regulatory environment, levels of supervision, tasks permitted under varying levels of supervision, and reimbursement. This index was factor analyzed and found to be a single factor called the Dental Hygiene Professional Index (DHPI). Higher scores on the DHPI are associated with broader sets of tasks, more autonomous practice environments, and greater opportunities for direct reimbursement for services. Multi-level modeling is employed estimating the effect of state level variables, including the DHPI, upon oral health outcomes for individuals nested within each state. Population Studied: In addition to the DHPI, the supply of dentists, dental hygienists, and dental assistants per capita are utilized at the state level as well as the percentage of the population on a fluoridated public water supply. Individual level data are drawn from the Behavioral Risk Factor Surveillance System (BRFSS) for adults, and the National Survey of Children’s Health (NSCH) for children. The BRFSS is a cross-sectional telephone survey conducted by state health departments with technical and methodological assistance provided by the CDC for all 50 States and the District of Columbia. The dataset contains oral health variables as well as a number of pertinent socio-demographic factors. The National Survey of Children’s Health (NSCH), also a telephone survey, was developed by the National Center for Health Statistics of the CDC, and contains a number of oral health as well as socio-demographic variables for children. Both datasets contain large samples within each state and are designed to be representative of the state population. Principal Findings: Both dental hygienists and the DHPI exerted a positive and statistically significant effect upon favorable oral health outcomes for both children and adults. The final model suggests that it is the DHPI which is the most important factor. The supply of dentists and dental assistants per capita had no impact upon oral health outcomes. Conclusions: The areas of health promotion, risk assessment, and disease prevention are considered core competencies for dental hygienists who function as preventive oral health specialists. The findings of this analysis indicate that dental hygienists play an important role in the prevention of dental decay and disease. Implications for Policy, Delivery, or Practice: The scope of practice for dental hygienists has important implications for the oral health of both children and adults within the United States. Both children and adults living within States with less restrictive legally prescribed practice environments for dental hygienists have better oral health. The professionalization of dental hygienists has important health implications for the U.S. population. Primary Funding Source: No Funding ●Physician Workforce: Rural vs. Urban Pamela Dinkfelt, Ph.D., John M Westfall, M.D, M.P.H., Richard G May, M.D, Kristina Wenzel, RN, MBA, Robin A Harvan, EdD Presented By: Pamela Dinkfelt, Ph.D., Manager, Health Workforce Analysis, Colorado Health Institute, 1576 Sherman St, Denver, CO 80203; Tel: (303) 831-4200 x218; Fax: (303) 8314247; Email: dinkfeltp@coloradohealthinstitute.org Research Objective: Of Colorado’s 64 counties, 47 (73%) are considered rural. Many of these rural communities face a shortage of physicians. This research compares demographic and practice characteristics of physicians working in rural and urban counties in Colorado in 2005. Study Design: A one-page workforce-related questionnaire was sent by the Colorado Board of Medical Examiners to all physicians licensed to practice in the state. The survey form was enclosed with materials required for license renewal in 2005, and respondents were asked to return the completed survey form with their licensure documents. Of the 16,183 physicians who renewed their license, 7,694 (48%) completed the questionnaire. Population Studied: Survey respondents who indicated they were currently practicing medicine, and also provided a Colorado zipcode for the location of their primary practice were included in the analysis. County designation of the practice location zipcode was determined using a geomapping software, and county designation of urban or rural was determined using 2003 US Bureau of the Census classifications. Of the 4,759 physicians practicing in Colorado with identifiable counties, 4,245 (89%) practiced in urban counties and 514 (11%) in rural counties. Principal Findings: Findings from the 2005 physician survey indicate rural physicians were significantly more likely to have grown up in a rural location than urban physicians (Rural = 34%, Urban = 20%; p<0.001). Rural physicians did not, however, differ from urban physicians in gender distribution (R Females = 26%, U Females = 29%), nor in mean age (R = 50.4 years, U = 50.2 years). Rural physicians were significantly more likely to designate their primary medical specialty as family medicine, general medicine, internal medicine or pediatrics than urban physicians (R = 49%, U = 41%; p<0.001), and more likely to accept new Medicaid patients (R = 66%, U = 55%, p<0.001) and new Medicare patients (R = 73%, U = 63%, p<0.001). In comparison to a similar 2001 survey, the 2005 findings show the mean age of physicians increased, and the percentage of physicians accepting new Medicaid and Medicare patients decreased. Conclusions: The analysis showed differing demographic and practice characteristics between physicians working in rural counties and those working in urban counties. Given the shortage of physicians in rural communities and the aging of the physician workforce, further examination of rural physician characteristics is imperative. The need for study is amplified by a general population that is aging and will have increased need for healthcare, and compounded by the decreased acceptance of new Medicaid and Medicare patients. Implications for Policy, Delivery, or Practice: According to 2003 US Census Bureau estimates, in year 2000, nonmetro America comprised 2,052 counties and was the home to 17 percent (49 million) of the US population. A key, persistent characteristic of the rural health landscape in Colorado and in the nation is the uneven distribution and shortage of healthcare providers. By better understanding the demographic and practice characteristics of physicians who choose to work in rural areas, recruitment and retention strategies could be enhanced and more directed. Primary Funding Source: The Colorado Trust ●Antecedents to Physician Retirement Gaetano Forte, BA, David Armstrong, BA, Gaetano Forte, BA, Jean Moore, MS considered in future forecasts of physician supply and assessments of the relationship between supply and demand. Primary Funding Source: HRSA Presented By: Gaetano Forte, BA, Director of Information Management, Center for Health Workforce Studies, 7 University Place / Room 334, Rensselaer, NY 12144-3458; Tel: (518) 402-0250; Fax: (518) 402-0250; Email: gjf01@health.state.ny.us Research Objective: After many years of concern about an oversupply of physicians, there is a growing consensus that the supply of physicians will soon be inadequate to provide health care services to the population. To date, most efforts to assess the adequacy of the supply of physicians in the U.S. and forecast future requirements have focused on the pipeline of new physicians, including medical school capacity and graduate medical training. Surprisingly, very little attention has been given to studying physician retirement rates, trends, and the factors that may have influence on them. In order to contribute to efforts to assess the adequacy of the physician supply, the present study examines the antecedents of physician retirement and plans to reduce patient care hours. Study Design: The primary data source for the paper is the 2004 – 2006 New York State Physician Re-registration Survey. Other data sources include 2000 – 2003 New York State Resident Exit Survey and the Medical Liability Mutual Insurance Company. The New York State Physician Reregistration Survey is conducted in cooperation with the New York State Education Department. In 2004, over 77,000 physicians held licenses to practice medicine in New York. All physicians are required to register with the State Education Department every two years. The present registration cycle began in January 2004 and will last until January 2006. Included in each registration packet is a questionnaire that requests responding physicians to provide information on a number of personal, professional, and practice characteristics. A logistic regression analysis was used to access the antecedents of physician retirement. Apart from considering demographic variables, indicators of practice setting, specialty demand, and malpractice insurance premiums were also included in the model. Population Studied: Active, patient care physicians practicing in New York between the years 2004 and 2006. Principal Findings: There was substantial variation in retirement rates across specialties. Further, several demographic variables, including age, as well as solo practice setting and high insurance premiums were significant predictors of retirement. Conclusions: Given the aging, baby-boom population, physician retirement and plans to reduce work effort are increasingly important pieces of the physician supply and demand puzzle. Not only does the present study confirm that retirement rates vary greatly by specialty, but it also highlights a number of critical factors that affect retirement. Among these factors are practice setting and insurance premiums. Implications for Policy, Delivery, or Practice: We are just beginning to understand the importance of physician retirement patterns to the future supply of physicians. As a result, additional research is needed in order to clarify their implications. The findings of this present study suggests, however, that the antecedents of retirement (such as: age, race/ethnicity, practice setting, and premium rates) should be ●Nursing Compensation Policy and Health Care Outcomes: The Relationship between Pay Level and Coronary Survival Rates in California Jonathon Halbesleben, Ph.D., Mark P. Brown, Ph.D., Anthony R. Wheeler, Ph.D. Presented By: Jonathon Halbesleben, Ph.D., Research Assistant Professor, Department of Health Management & Informatics, University of Missouri, Columbia, 324 Clark Hall, Columbia, MO 65211; Tel: (573) 884-1723; Fax: (573) 882-6158; Email: halbeslebenj@health.missouri.edu Research Objective: In recruiting and managing nurses, a key concern is the appropriate level of pay, relative to competitors, to adequately attract and retain nurses to provide high quality health care for patients. Efficiency wage theory predicts that for some job categories (e.g., RNs) a lead pay policy (where nurses are paid higher wages than average) will lead to better outcomes for hospitals while a lag policy (where nurses are paid lower wages than average) for other job categories (e.g., nursing aides and orderlies) will lead to better outcomes. The objective of this study was to examine this predicted relationship using a sample of hospitals from California. Study Design: Data from state-mandated disclosure reports to the state of California from 354 hospitals across nine years were used to test the predictions. The reports included pay data for nurses by job category (RN, LPN, and aides/orderlies); pay level variables were calculated by standardizing the average pay by job category for each hospital; the resulting variables were scaled such that positive scores indicated a lead policy, a zero score indicated a match policy, and negative scores indicated a lag policy. The pay level data were then compared to coronary survival rates for each hospital after adjusting for common control variables. Adjusted coronary survival rates were calculated by subtracting the reported heart attack death rate from the riskadjusted expected heart rate (as estimated for each hospital by the state of California) for each hospital. Population Studied: Short-term-stay, acute care, general hospitals in the state of California from 1991-1999. Principal Findings: After controlling for profit status, ownership status, hospital size, cost of living in the area where the hospital was located, case mix, and unionization status, we found that a lead pay policy among RNs was associated with a higher adjusted coronary survival rate. On the other hand, pay policy was not associated with higher adjusted coronary survival rate for LPNs or aides and orderlies. Conclusions: This study found a relationship between pay policies of hospitals and patient outcomes. It suggests that by paying employees in higher skill level job categories at a rate that exceeds the market, patients benefit. This benefit may be the result of attracting higher quality job candidates to these jobs, which translates to better outcomes for patients. Future research that replicates these findings with other patient outcomes would provide greater credence to the conclusions. Implications for Policy, Delivery, or Practice: This research supports the notion of differentiating pay level strategy by job category; specifically, the findings suggest utilizing a lead pay policy for high skill jobs in order to recruit better qualified candidates who can provide better care to patients. For lower skill jobs, pay level is not related to patient outcomes; as such, a lead policy is unlikely to lead to benefits in terms of patient outcomes. As health care organizations struggle with attraction and retention of nursing staff in light of contemporary workforce shortages, understanding the implications of pay level may be valuable in determining compensation policy. Primary Funding Source: No Funding ●Predictors of Home Healthcare Nurse Job Retention Carol Hall Ellenbecker, RN, Ph.D., Frank Porell, Ph.D., Linda W. Samia, RN, Ph.D.c Presented By: Carol Hall Ellenbecker, RN, Ph.D., Associate Professor, College of Nursing and Health Sciences, University of Massachusetts Boston, 100 Morrissey Blvd, Boston, MA 02125; Tel: 617-287-7515; Email: carol.ellenbecker@umb.edu Research Objective: The purpose of this study was to test a theoretical model of the direct and indirect effects of job satisfaction, individual nurse characteristics, and intent to stay on job retention for home healthcare nurses. Study Design: This was a descriptive correlation study. A second wave of self-report data was collected from nurses using the Home Healthcare Nurses Job Retention Questionnaire. The 14 item instrument measures home healthcare nurse retention. This data was linked to nurse level job satisfaction data collected one year earlier with the 30 item HHNJS and Intent to Stay Instrument, nurse demographic and descriptive agency level data. Population Studied: A representative sample of 2,500 home healthcare nurses was recruited from Certified Home Healthcare Agencies throughout the New England region from a probability proportionate to size random sample of 123 agencies. The 2,300 (96%) of nurses who agreed to future contact during the first wave of data collection were recruited to Phase II of the Retention Study using Dillman’s Tailored Design Method. There was an 83% response rate to the mailed self-report survey (N= 1900) and another 34% of nonrespondents (N=238) provided information via follow-up phone call. Principal Findings: The strongest predictor of job retention was nurse job satisfaction. Fourteen percent of home healthcare nurses left their jobs one year following the initial wave of data collection and over 50% gave as their primary reason for leaving “dissatisfaction.” Nurses describe reason for dissatisfaction due to “overwhelming and stressful demands,” and secondly because of relationships with administration. Conclusions: Nurses’ job retention is affected most by the organizational environment and other extrinsic factors over which administrators and policy makers have control. The theoretical model developed from an integration of the findings of empirical research related to job satisfaction and retention, in institutional settings, may not be a good fit for home healthcare settings. The results of this research suggest that characteristics viewed as extrinsic, i.e. Autonomy and Independence of hours and work activities for the home healthcare nurse may actually be perceived by home healthcare nurses to be intrinsic to job of the home health care nurse. Likewise, the previously hypothesized intrinsic characteristics of Relationship with Administration while intrinsic to the job for nurses in institutional settings may be extrinsic to the role of the home healthcare. Implications for Policy, Delivery, or Practice: Predicted severe nursing shortages and an increasing demand for home healthcare services have made the retention of experienced, qualified nursing staff a priority for healthcare organizations. Knowledge of variables that contribute to job retention in home healthcare provides the information necessary to maintain nursing staff and assure access to quality home healthcare services. Job satisfaction and retention for home healthcare nurses is dependent on factors over which agencies have control. This suggests avenues for intervention that will improve job satisfaction with implications for higher retention, greater access, and improved patient care. Primary Funding Source: AHRQ, R01 # HS013477-02 ●Evidence of Wage Discrimination Between Internationally and US Educated Nurses Sat Hayde, MSN, RN (HSA) Presented By: Sat Hayde, MSN, RN (HSA), Doctoral Student; UNCC Ph.D. Program, Public Policy, Email: sahayden@uncc.edu Research Objective: Is there evidence of wage discrimination among nurses? Do wages paid to internationally educated nurses (IENs) differ from wages paid to nurses educated in the United States (USRNs) and can those differences can be explained by productivity factors or do they provide evidence of wage discrimination? A number of studies and reports have been done on the phenomenon of nurse shortages and importation of nurses to alleviate projected supply and demand imbalances. These studies have been done using a variety of perspectives. The purpose of this study is to use an economic perspective to explore differences in salaries between these two groups of nurses as an explanation of the growing use of IENs to alleviate domestic nursing labor shortfalls. Study Design: Wage differences will be investigated using an Oaxaca wage decomposition formula along with a CottonNeumark extension. The current study builds on earlier work by Kalist (2002) and Jones and Gates (2004) in which evidence of gender related wage discrimination in nurses responding to the year 2000 National Sample Survey of Registered Nurses (NSSRN) was investigated. Once the data from the 2004 National Sample Survey of Registered Nurses is released, the current study will incorporate this latest data for comparison purposes. To elucidate the relationships between lifestyle and productivity factors, marital status, children at home, work setting, primary job role, experience and highest level of education attained were included in the analysis. Population Studied: The 2000 National Nurses Sample Survey (NSSRN) contains information about 1291 foreign educated nurses as well as information about 29000 domestically educated nurses. This study looks only at those nurses who work full time in urban areas who responded to the survey. Due to the limitations of the dataset, this study was unable to further compare gender based differences between IENs and USENs; with the release of the 2004 NSSRN dataset, it may be possible to expand the study to include this important dimension. Principal Findings: Analysis suggests that wage differences between IENs and USENs exist in the US health care market. These differences cannot be explained by differences in experience, level of education, job role, job settings or job function nor can they be explained by family status. Implications for Policy, Delivery, or Practice: The development this research can help health service researchers and policy makers to identify a way to better understanding the impact of international nurse migration on the United States health care industry. For researchers the study provides a platform for additional investigation of the impact of nurse migration on health care market in general and nursing labor shortages in particular. For policy makers the study provides an economic lens through which to view international nurse migration as a foreign policy issue or to develop policy solutions to nurse shortages in their jurisdictions locally. For health services administrators the framework can assist in nurse recruitment and retention decision making within their organizations and in particular managing the impact of increasing diversity in their nurse work forces due to international nurses. Primary Funding Source: No Funding ●International Migration of Physicians to the United States: Implications for US Workforce Policy Peter Hussey, Ph.D. Presented By: Peter Hussey, Ph.D., Associate Policy Researcher, RAND, 1200 S. Hayes St. w6340, Arlington, VA 22202; Tel: (703) 413-1100 x5460; Email: hussey@rand.org Research Objective: This study examines the characteristics of visas obtained by physicians immigrating to the United States. The objective is to determine how immigration rates could potentially be changed and the implications of physician immigration for the countries of origin. Study Design: Descriptive analysis of Immigration and Naturalization Service data on U.S. permanent resident visas granted to physicians between 1994 and 2000. Data on countries of origin were compiled from the World Bank, the International Monetary Fund, and other sources. Population Studied: All physicians receiving U.S. permanent resident visas between 1994 and 2000. Principal Findings: Two-thirds of physicians received permanent resident visas on the basis of their family ties, not through employment. Emigration rates were highest from upper-middle-income countries: 11.2 emigrants per 1000 physicians in the country of origin per year, compared to 7.3 emigrants per 1000 physicians from low-income countries and 4.4 per 1000 from lower-middle-income countries. The absolute number of physicians migrating to the US from poorer countries was substantial: 66%, or 19,761, physician immigrants were from low-income or lower-middle income countries. Emigration rates were also highest from countries with the lowest average life expectancy: 9.8 per 1000 from countries with average life expectancy <50 years, compared to 4.0 per 1000 for countries with life expectancy >70 years. Conclusions: The brain drain of physicians was substantial from both low- and middle-income countries and was most common from countries with the lowest life expectancy. Most physicians migrated based on their family ties to the US, not based on agreements with employers. This is in contrast with other professions such as scientists and nurses. Implications for Policy, Delivery, or Practice: Efforts to reduce physician immigration through immigration policy would be most effective if focused on the one-third of immigrants receiving employment-preference visas. The most effective target for this type of policy would be temporary work visas, particularly the H-1B visa, which could be replaced with J-1 visas. Preventing family-based immigration would be more to justify and difficult to target to physicians. There may be large numbers of physicians living in the US who have immigrated on family preference visas and are not practicing as physicians. These individuals represent a potential recruitment pool, assuming they are appropriately skilled; efforts could be made to identify them and reduce the barriers to licensure. Primary Funding Source: AHRQ ●Medical Staff Availability and Nursing Home Quality Orna Intrator, Ph.D. Presented By: Orna Intrator, Ph.D., Assistant Professor (Research), Center for Gerontology and Health Care Research, Brown University, 2 Stimson Avenue, Providence, RI 02912; Tel: 401-863-3579; Fax: 401-863-9219; Email: Orna_Intrator@brown.edu Research Objective: As the severity of illness of nursing home residents continues to increase, the physician’s role in their care will grow in importance. However, the scant existing literature paints a picture of physicians as a shadowy presence in most nursing homes1 suggesting that for many staff and residents, the MD’s seem to be “missing in action”. The limited involvement of physicians in nursing homes impedes interdisciplinary communication and effective treatment, often leading to deleterious resident outcomes, such as avoidable hospitalizations, and inadequate pain management and inadequate pressure ulcer care.2-6 This picture is complicated by substantial variation among and within states in their efforts to increase MD involvement and to utilize nurse practitioners (NP) and physician assistants (PA). Study Design: Proposed model of organizational behavior to be tested using a survey of New York nursing homes in 1997 which captured organizational behavior, along with resident performance as measured on the Minimum Data Set, and nursing home characteristics as measured in the Online Survey Certification And Reporting (OSCAR). Population Studied: Long stay nursing home residents in urban freestanding facilities. Principal Findings: Multilevel models examining the relationship between the availability of physicians and separately the availability of nurse practitioners or physician assistants (NP/PAs), controlling for many facility and resident characteristics, reported that facilities with medical staff were less likely to restrain residents, and were more likely to have residents’ pain controlled. Moreover, using a novel method to determine level of delirium, these facilities were also more likely to diagnose sub-syndromal delirium. Conclusions: The availability of medical staff enhances quality of care for residents, yet it is not clear whether there is a threshold effect, and whether there are other organizational factors controlling medical staff that lead to the observed effects. Implications for Policy, Delivery, or Practice: More attention needs to be given to considerations of the organization of medical staff as evidence of its effectiveness on resident quality is made apparent in the literature. Study of medical staff is the next frontier of studies of the relationships of staffing and quality in nursing homes. Primary Funding Source: No Funding ●Preliminary Evaluation of a Unique K-12 Program Designed to Prepare Underrepresented Minorities for Scientific Careers Micheala Jones, Ph.D., Marian Johnson-Thompson, Ph.D. Presented By: Micheala Jones, Ph.D., Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, 4101 Five Oaks Drive Unit 33, Durham, NC 27707; Tel: 615289-9251; Email: mjones@schsr.unc.edu Research Objective: The Bridging Education and Science Technology K-12 Program (BEST), was established at Hillside High School (HHS), in Durham, North Carolina as a partnership between the National Institute of Environmental Health Sciences (NIEHS), National Institutes of Health, and Durham Public Schools. Its goals were to increase students’ enthusiasm for science, to increase opportunities for motivated students to pursue science careers, and to assure the availability of a well-trained scientific workforce. BEST students received mentoring by NIEHS scientists and participated in a molecular biology course taught at HHS. Students also gained summer research experiences at local and state institutions and participated in after-school enrichment activities. BEST students have completed summer research internships at UNC-Chapel Hill, Duke University, NC State University, NIEHS, the US Environmental Protection Agency and the Centers for Disease Control. After completing research internships, students prepared research posters and presented their research findings at various meetings (e.g. the American Association for the Advancement of Science and the NC Academy of Sciences Research Meeting). An AcademyHealth Committee reported that minorities represented 15.3% of public health students in 1990 and 19.5% in 1999. Currently, the percentage of minorities is 25% and this number is expected to double within the next 50 years. Health experts suggest that if more minorities were involved public health careers, the gap in health disparities could be decreased. The objective of this study was to determine the effectiveness of the BEST program in encouraging minorities to pursue math/science disciplines that might prepare them for public health related degrees. Study Design: Data were collected via collegiate and internet searches, personal references, and the project director. Data were confirmed by phoning colleges and performing collegiate and internet searches. Participants who have graduated college were interviewed via phone and were asked to provide their race, college attended and major, and post-college plans, while, for those participants who were currently pursuing undergraduate degrees, data were obtained from the program director. Population Studied: Sixty-two high school students who participated in the BEST program from 1998-2005 that were accepted into college. Principal Findings: The percent of BEST students who were minorities: Cohort 1998-2000 (100%), 2001 (90%), and 2002-2005 (97%). The percent of BEST students who majored in a math/science discipline: Cohort 1998-2000 (100%), 2001 (88%), and 2002-2005 (90%). Of those, the percent who received/are pursuing graduate degrees: Cohort 1998-2000 (60%), 2001 (30%), and 2002-2005 (N/A). Of those, the percent of graduate degrees that are math/science disciplines: Cohort 1998-2000 (95%), 2001 (67%), and 20022005 (N/A). Conclusions: These findings demonstrate that 100% of the BEST participants were accepted into college and more than 88% majored/are majoring in a math/science discipline. The BEST program is partially responsible for preparing students for math and science based disciplines. Implications for Policy, Delivery, or Practice: The BEST program could be implemented in school systems as a viable mechanism for increasing the number of minorities who pursue public health related careers. Potentially, these students represent future health professionals who will play significant roles in decreasing the health disparities gap. Primary Funding Source: AHRQ ●Not on the Radar: Public Policy in Canada and Health Human Resource Migration from Sub-Saharan Africa Arminee Kazanjian, Dr. Soc., Lars Apland, MA Presented By: Arminee Kazanjian, Dr. Soc., Professor, Health Care & Epidemiology, University of British Columbia, 5804 Fairview Crescent, Vancouver, British Columbia, V6T 1Z3; Tel: (604) 822-4618; Fax: (604) 822-4994; Email: a.kazanjian@ubc.ca Research Objective: Despite common acknowledgement that the migration of health professionals from Sub-Saharan Africa (SSA) and the resultant loss of capacity to deliver health services are devastating for countries in that region, Canadian public policy interest in, and consideration of, the “brain drain” of health human resources (HHR) from SSA seems cursory, at best. While memorandums of understanding and other non-binding types of international agreements pay lip service to ethical principals of recruitment, these seem to be largely ignored or by-passed in the context of relations among federal, provincial, and territorial levels of government in Canada. The objectives of this research were to explore the incongruity between public policy principles and objectives, and to highlight a path whereby these may converge with most effective overall results. Study Design: This research was part of a larger study that examined the scope, implications, and effects of the “brain drain” of health professionals from SSA to Canada. Using mixed methodology, it explored the conditions, primarily in Canada but also in source countries of the developing world, which allow, promote, and facilitate HHR migration and the subsequent “brain drain” from countries that can least afford to lose trained personnel. Telephone and face-to-face interviews were the data collection methods for this paper. Population Studied: A select sample of key Canadian governmental and professional informants responsible for, or involved in, HHR policy and recruitment in a number of provinces were interviewed. They were asked to share their views and understanding of issues, as well as their knowledge of respective governmental or organizational policies, surrounding the recruitment and migration of trained health professionals from developing countries, particularly those of SSA, to Canada. Principal Findings: Canadian federal and provincial public policy may be well-intentioned, but a number of factors contribute to the incongruity between principle and policy and, perhaps inadvertently and to an unnecessary extent, undermine policy objectives and efficacy. These factors include the nature of the division of constitutional powers among federal and other levels governments in Canada, the local conditions that variously force provincial and territorial policy-makers to address pressing needs in their own jurisdictions, as well as facilitative migration policies and the often harsh realities of life in source countries that drive citizens to seek opportunities internationally. Conclusions: Broadly based domestic HHR and international policy objectives invariably conflict, with inconsistent, counterproductive and unsatisfactory results that continue to work to the detriment of source countries of the developing world. Implications for Policy, Delivery, or Practice: A key challenge for public policymakers, at all levels of government in federal systems, is to co-ordinate and find common ground whereby specific domestic HHR needs and “brain drain” issues, as they affect source countries, can be simultaneously and effectively addressed. Primary Funding Source: No Funding ●Radiation Oncologists in the United States Rebecca Lewis, Jonathan Sunshine Presented By: Rebecca Lewis, American College of Radiology, Email: rebeccal@acr.org Research Objective: Given the increasing use of radiation therapy in treatment of cancer, to provide an extensive and detailed portrait of radiation oncologists, their professional activities, the practices in which they work, and to assess trends in the number of radiation oncologists over the past decade. Study Design: We analyzed data from the American College of Radiology’s 2003 Survey of Radiation Oncologists, a nationally-representative, confidential, stratified random sample mail survey of radiation oncologists in the United States, with a total of 479 useable responses. Data were weighted to make them representative of all radiation oncologists in the United States. Comparisons were made to the results of the previous 2000 Survey. Population Studied: Some analyses were performed on all radiation oncologists, including those in-training and retired (temporarily or permanently). Most of the analyses were performed on post-training, professionally active radiation oncologists. Principal Findings: Approximately 39% of post-training professionally active radiation oncologists were <45 years old and 23% were women. Twenty-six percent of radiation oncologists in training were women. The largest percentage (33%) of radiation oncologists were located in the South. The largest percentage (48%) of radiation oncologists are in nonacademic private radiation oncology practices. Of those report a primary specialty, the largest percentages specialize in prostate (23%), breast (18%), and brachytherapy (13%). Of those who are involved in clinical practice in hospitals, the mean percent of work time spent at it is approximately 83% (compared to about 77% for diagnostic radiologists). Of those involved in clinical practice in non-hospital sites, the mean percent of work time spent at it is approximately 39%. About one-third of radiation oncologists spend some time teaching and about one-quarter spend some time in research. Sixty-two percent of post-training, professionally active radiation oncologists reported that their workload was about right. Full-time radiation oncologists work on average 51 hours/week, about the same as the mean weekly hours worked by diagnostic radiologists. Conclusions: Most demographic, professional, and practice characteristics remained relatively constant between 2000 and 2003. We do not have yet specific conclusions regarding trends in the population of radiation oncologists, but expect to have this data, along although with a comparison of U.S. radiation oncologists to the number of patients who are undergoing radiation oncology. Implications for Policy, Delivery, or Practice: With radiation therapy increasing as a treatment of cancer, and a potential rise in overall incidence of cancer, sufficient numbers of trained radiation oncologists are critical. Primary Funding Source: No Funding ●Association Between Nurse Staffing and Length of Stay in VHA Chuan-Fen Liu, Ph.D., Ann E. Sales, Ph.D., Yu-Fang Li, Ph.D., Gwendolyn T. Greiner, M.P.H., Nancy D. Sharp, Ph.D., Elliot Lowy, Ph.D. Presented By: Chuan-Fen Liu, Ph.D., Investigator, VA Puget Sound Health Care System (152), VHA, 1100 Olive, Suite 1400, Seattle, WA 98101; Tel: (206)764-2587; Fax: (206)764-2935; Email: Chuan-Fen.Liu@va.gov Research Objective: Several large scale studies have found associations between nurse staffing and length of stay for hospitalized patients, aggregated to the facility level. However, nurse staffing levels vary greatly across inpatient units within a facility. In this study we provide the first largescale analysis using nursing unit-level data to examine the association between staffing levels, skill mix, and patient length of stay (LOS). Study Design: Data came from several sources: VA nursing labor files; VA National Patient Care Databases for data on all patients admitted to VHA inpatient acute care between 2/036/03; and a national data file linking inpatients to nursing units. We defined the nurse staffing level as nursing hours per patient day by type of nurse provider (registered nurseRN, licensed practical nurse- LPN, nurse aide- NA). The skill mix was defined as the proportion of RN hours to total nursing hours. The dependent variable was natural log(LOS) due to skewness and kurtosis. We developed a 2-step multilevel regression model with patient, nursing unit and hospital level data corrected for clustering at the unit and facility levels. The first step predicted patient probability of developing a serious complication using patient-level predictors. The second step estimated log(LOS) on predicted patient complications, nursing unit and facility-level predictors. We stratified the analysis by whether or not the patient received any intensive care (compared to those with no intensive care). All analyses were conducted using the xtmixed procedures in STATA with two levels of clustering (unit and facility). Population Studied: The study included 126,382 patients from 463 nursing units in 119 VAMCs. 184 were intensive care, and 279 non-intensive acute care units. Principal Findings: The mean RN hours per patient day (RNHPPD) was 8.4 (SD=6.6) and the proportion of RN hours averaged 0.69 (SD=0.19). The average LOS was 11.5 days (SD=37.1), with a median of 4 days. In all cases, patient risk was the most significant factor associated with log(LOS). The nurse staffing level measured by RNHPPD was positively associated with log(LOS) for patients receiving any intensive care (n=34,638) (coefficient=0.019, p<0.0001), while it was adversely associated with log(LOS) for those receiving no intensive care (n=91,744) (coefficient=0.061, p<0.0001). There was no was no significant relationship between the proportion of RN-hours and log(LOS) in both patient groups, which may be due to the high collinearity between RNHPPD and the proportion of RN hours (r=0.84). Conclusions: This study shows that the relationship between nurse staffing (RNHPPD) and LOS varies by patient group in unit level analyses. Aggregating both patients and nurse staffing to the facility level may result in biased estimates through mixing very heterogeneous groups. Implications for Policy, Delivery, or Practice: When considering a change in nurse staffing to reduce patient LOS, hospital managers need to examine the impacts separately for patients with different risk profiles. Primary Funding Source: No Funding ●Factors Affecting Physician Productivity in a Proceduralist Specialty, Radiology Cristian Meghea, Ph.D., Jonathan Sunshine, Ph.D. Presented By: Cristian Meghea, Ph.D., Senior Researcher, Research, American College of Radiology, 1891 Preston White Drive, Reston, VA 20191; Tel: 703-648-8983; Email: cmeghea@acr.org Research Objective: There is only a small literature on the production function of physicians. We seek to add to this literature, making a number of new contributions, methodological and substantive, such as: • We measure the productivity of the physician group, the production unit of medical services, while the focus of the previous literature was the individual physician. • This study examines the effect of technology, unlike previous work. • We account for the measurement error generally present in inputs data. • This is the first study of a procedure-centered medical specialty. Previous literature focused on physician visits. • We control for case mix in more detail than previous studies. Restraining the growth of health expenses is a recurrent concern in almost all developed nations, and identifying methods to improve productivity may help ease the problem. Study Design: We empirically investigate the determinants of productivity of radiology practices, exploring the effect of physician labor input, physician characteristics, purportedly productivity-enhancing technologies and operational practices, and other practice characteristics. Data are from the American College of Radiology’s (ACR’s) 2003 Survey of Radiologists, a nationally representative stratified random sample survey of radiologists in the United States. We estimate the production function via OLS with the outcome being the logarithm of practice’s procedures per year. The physician labor inputs -- full-time equivalent (FTE) radiologists, weekly hours, weeks worked annually -- enter in both linear and logarithmic forms allowing for the possibility of non-constant input elasticities. To address the downward bias introduced by measurement error in labor inputs, we made various plausible estimates of the error size and then used Monte Carlo methods to find what true elasticity combined with each plausible estimate of measurement error yields the elasticity observed in the regression. Population Studied: Radiology practices in the US Principal Findings: The FTE-radiologists elasticity of output directly implied by the OLS is 0.8 (true elasticity between 0.850.90 if accounting for bias), the weekly hours elasticity is 0.4 (0.5-0.7, bias accounted) and the annual weeks elasticity is 0.4 (0.5-0.7, bias accounted). Three of eight techniques/practices used in radiology practices have a positive independent impact on productivity. Surprisingly, practices where individual radiologists work in more locations have higher productivity. Government owned practices are 18 percent less productive than practices owned solely by members. Practices in the Northeast and West census regions are more productive than practices in the South. Conclusions: Due to unaccounted measurement error, previous studies probably underestimated the input elasticities in the production function of medical services. To increase output it is more efficient to add radiologists to the practice than to increase the hours or weeks worked. Some techniques used to improve radiologist productivity have less than the generally believed effect. Implications for Policy, Delivery, or Practice: There is a growing consensus that U.S. faces (or will shortly face) a shortage of specialist physicians. In that context, it is critical to identify ways to increase productivity. We show which technologies and operational practices increase productivity and which do not. If one accepts the view that physicians have an income goal, then enhancing productivity may facilitate lower per-service prices than otherwise feasible, thereby helping contain health costs. Primary Funding Source: No Funding ●A Survey of Registered Dental Hygienists in California Elizabeth Mertz, MA, Public Affairs, Dennis Keane, M.P.H., Kevin Grumbach, M.D. Presented By: Elizabeth Mertz, MA, Public Affairs, Program Director, Center for the Health Professions, University of California, San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: 415-502-7934; Fax: 415-476-4113; Email: bmertz@thecenter.ucsf.edu Research Objective: To evaluate the current demographics, practice settings, educational backgrounds, scope of work, and opinions regarding professional issues of the registered dental hygiene (RDH) workforce in California. The survey was inspired by the need for data to inform policy debates regarding an expanded role for RDHs within the context increasing access to dental care and reducing the prevalence of dental disease. Study Design: The study was conducted in two phases, development and implementation. Development consisted of a relevant literature search, policy analyses, and over 25 expert interviews, which were followed by a field test involving a six person focus group of urban RDHS and five individual phone interviews with rural RDHs. It was then revised for clarity in order to focus around the key policy issues of adequacy of size of the workforce, scope of practice, supervision requirements, and alternative practice settings. The implementation phase involved sending the survey to a random sample of 3802 licensed dental hygienists in California. RDHs with rural addresses were over sampled, as were RDHs with certification in alternative practice (RDHAP) or extended function (RDHEF). Population Studied: The dental hygienist workforce in California with active licenses, both practicing and not practicing. Principal Findings: While there has been much written about the potential of the RDH workforce to fill an important need in delivering oral health care to those who have limited access to a dentist, there is little research on the capacity and interest of the existing workforce to expand into these new areas. In addition, there have been few efforts to collect comprehensive data on the RDH workforce - and particularly few focused on practices in alternative or public health settings. The field testing revealed a complex set of practice patterns of respondents, varying career path expectations, and a mixed interest of RDHs in practicing outside a dental office, primarily due to concerns around quality of care. Preliminary survey response is expected in May 2006. Conclusions: The final survey results will inform policy makers about the pipeline and attrition, practice realities, patient populations, and professional ambitions of the RDH workforce. In particular, the data will address the issues which have a direct relationship to the profession’s ability to affect access to care: scope of practice, supervision requirements, and practice in alternative and public health settings. Implications for Policy, Delivery, or Practice: Current dental workforce policy discussions commonly focus on disputes about the role of RDHs in meeting broader oral health system goals. Dental hygienists are central to the discussion of the capacity of the dental workforce to increase access to dental care through alternative practice models and expansion of the workforce in general. Yet these disputes and discussions are rarely supported by good data. This study will reveal the current demographics and practice patterns of dental hygienists as well as examine the opinions and aspirations of this workforce, all of which will directly impact educational, regulatory and finance policy. Primary Funding Source: UCSF/NIDCR(prime)/HRSABHPr/California Dental Association ●Supply of CRNA Faculty Elizabeth Merwin, Ph.D., RN, FAAN, Steven Stern, Ph.D., Lorraine M. Jordan, Ph.D., CRNA Presented By: Elizabeth Merwin, Ph.D., RN, FAAN, Madge M. Jones Professor of Nursing, School of Nursing, University of Virginia, McLeod Hall, Charlottesville, VA 22908; Tel: 434-9823286; Fax: 434-982-1809; Email: merwin@virginia.edu Research Objective: Identify current issues regarding supply and demand for faculty members in the nation’s academic programs preparing Certified Registered Nurse Anesthetists. Study Design: A mixed-methods quantitative and qualitative study was conducted. A secondary analysis of a survey of over 16,000 CRNAs was used to compare and contrast supply characteristics of CRNAs employed in colleges and universities with other CRNAs including salary and retirement plans. A random sampling of the nation’s CRNA program directors were invited to participate in a qualitative interview regarding faculty shortages. Twelve program directors were interviewed. The results of the quantitative and qualitative analyses were used to design an online survey to be administered to 100% of faculty in the nation’s CRNA programs during the Winter of 2006. Population Studied: The nation’s population of CRNAs. Program Directors and Faculty of Nurse Anesthetist programs. Principal Findings: Only 2.2% of CRNA’s are employed by colleges or universities. CRNA educators are significantly older (53.0 yrs) than other CRNAs (51.5 yrs) although in 2001 they earned $10,000 a year less than other CRNAs on average (t 5.41, <.0001). Thirty-nine percent of this small group of CRNA educators plan to retire by 2012. There is no difference in the rate of planned retirement for educators versus other CRNAs (36%). A logistic regression model reveals that men are less likely to plan to retire by 2012 (odds ratio of 0.7), while older individuals, part-timers an (odds ratio of 1.8) are more likely to plan to retire and being an CRNA educator was not significant in explaining plans for retirement. The qualitative interviews reveal that the earnings differential is a major barrier to recruitment to educator positions and makes retention difficult as many faculty return to clinical positions. The higher and more stressful workloads of faculty without reimbursement for additional hours worked was a related challenge in the retention of faculty. Many programs find it difficult to fill faculty positions and some are unsuccessful in recruiting efforts. Future challenges include planned retirements, the lack of doctorally prepared faculty and responding to policy changes and recommendations such as the recent call by professional nursing for doctorate of nursing practice programs for entry into specialty practice. Conclusions: The high rate of planned retirements among all CRNAs, the disparity in income with CRNAs in other employment settings, and a small educator group will continue to challenge the adequacy of educator workforce. This study launches the beginning of a more detailed report and analysis of the nurse anesthesia faculty workforce. Implications for Policy, Delivery, or Practice: If many schools choose to implement a doctorate of nursing practice program there will be a need to increase the availability of doctorally prepared CRNAs to teach in these programs. At the same time the profession will be faced with a high number of retirements, as well as disparities in income with other settings, posing more serious workforce challenges than seen in the past. Primary Funding Source: American Association of Nurse Anesthetists ●Determinants of Maternal Outcomes: The Impact of Anesthesia, Nursing and Medical Care Ann Minnick, Ph.D., RN, FAAN Presented By: Ann Minnick, Ph.D., RN, FAAN, Chenault Professor, School of Nursing, Vanderbilt Unviersity, 21st Avenue, 424 Godchaux Hall, Nashville, TN 37240; Tel: 615 343 2998; Email: Ann.Minnick@vanderbilt.edu Research Objective: (1) describe the relationship of anesthesia, nursing, and medical provider models and staffing practices in obstetrical settings in US hospitals and (2) determine the extent to which anesthesia provider models and other administrative variables predict maternal outcomes. Health care policy makers and anesthesia providers have a continuing interest in how privileges, supervisory laws, and service accreditation policies should be crafted to improve outcomes and if the interaction of provider models of nursing, anesthesia and medicine explains outcomes. Obstetrical care, the leading cause of US anesthesia administration, produces enough cases to allow for a statistically sound study of these knowledge gaps. This project is the first to include labor and capital variables from more than one discipline. Study Design: Using a conceptual framework which specified that maternal outcomes are the product of patient characteristics, comorbidities, problem severity and treatment (defined as what was done, timing, setting, provider training and experience), a data base was developed that included (1) information regarding patient characteristics, outcomes and some institutional characteristics from the American Hospital Association, state and federal agencies during 1999-2001 and (2) data concerning anesthesia, nursing, and medical practices acquired through a 2003-4 survey of all hospitals (n= 1124) that reported at least one live birth in 2002 in California, Florida, Kentucky, New York, Texas, Washington and Wisconsin. The states were chosen based on (1) data availability (2) the combinations ability to represent US demographic and population disbursement patterns and (3) attainment of a data pool sufficient to meet statistical requirements. Hospital survey development efforts included content expert panels (anesthesia providers, registered nurses and physicians) and two pilot tests to ascertain validity, data availability, response burden and regional terminology differences. Complication rates for each maternal outcome (defined as all patients and as only those who had Caesarean section) were estimated for each of the five anesthesia provider models that emerged from the hospital survey. The equality of the rate to the physician anesthesiologist only model were tested using logistic regression with standard errors adjusted for clustering. Population Studied: 995 hospital years and 1,141,641 obstetrical events The survey response (rate=49%) reflects national distributions by hospital type and size. Principal Findings: Death, anesthesia complications, other complications and obstetrical trauma rates were basically unaffected by anesthesia provider model.. There was no consistent pattern of other hospital, provider or patient characteristics associated with the complications studied. Conclusions: Unlike single state studies of specific adult surgical conditions, the results provide no support for the adoption of any one anesthesia provider model or changes in other policies concerning delivery location or staffing based on outcome differences. Implications for Policy, Delivery, or Practice: Given anesthesia providers serve many types of patients, a repetition of this methodology with other outcomes is warranted before any changes or additional rules are made in anesthesia delivery. Policies which support this type of research as a part of any rule change activity would provide a scientific basis for future decisions. Primary Funding Source: American Association of Nurse Anesthetists ●Defining US Anesthesia Models in Labor and Delivery Settings Ann Minnick, Ph.D., RN, FAAN, Jack Needleman, Ph.D. Presented By: Ann Minnick, Ph.D., RN, FAAN, Chenault Professor, School of Nursing, Vanderbilt University, 21st Avenue, 424 Godchaux Hall, Nashville, TN 37240; Tel: 615 343 2998; Email: Ann.Minnick@vanderbilt.edu Research Objective: To describe the personnel models used by US hospitals to provide obstetric anesthesia. Debates over attempts to restrict or enlarge the conditions under which anesthesiologists, nurse anesthetists, physicians and nurses may provide anesthesia are continuing policy agenda points. The traditional approach to defining provider models has been to classify models in individual cases as “anesthesiologists (ANES) only”, “certified registered nurse anesthetists (CRNA) only” and “both types of providers used”. The resulting variable is then used to study outcomes. The limitations of this approach have been (1) its failure to account for differences in models within an institution (e.g.. CRNA only in obstetrics and ANES only in the operating room) outcomes (2) reliance on billing codes to attribute individual provider behaviors and (3) the inability to determine what duties are required of and what support mechanisms are available to the provider. Study Design: Data concerning anesthesia, nursing, and medical practices were acquired through a 2003-4 survey of all hospitals (n= 1124) that reported at least one live birth in 2002 in California, Florida, Kentucky, New York, Texas, Washington and Wisconsin. The states were chosen based on (1) data availability (2) the combination’s ability to represent US demographic and population disbursement patterns and (3) attainment of a data pool sufficient to meet statistical requirements. Hospital survey development efforts included content expert panels (anesthesia providers, registered nurses and physicians) and two pilot tests to ascertain validity, data availability, response burden and regional terminology differences. Population Studied: The survey response (rate=49%) reflects national distributions by hospital type and size. Principal Findings: Five models emerged from the data: (1) ANES only (33%) (2) CRNA only (24%) (3) both types of providers with the ANES required to be present at the beginning of every Caesarian section (C-section) regardless of anesthesia type (ANES-CRNA I) (16%) (4) ANES not required at the beginning of every C-section (25%) and (5 ) one model used in the operating room and another in the obstetric area (3%). In ANES-CRNAI institutions, 58% allowed the CRNA to insert epidurals versus 85% at ANES-CRNAII. with similar large differences for spinal privileges: 65% versus 93%. Models were associated with hospital characteristics such as location. Key obstetric resources (OR open for obstetric cases at all times, anesthesia provider present at all times, availability of C-section in labor and delivery, board certified obstetricians, number of professionals at planned and emergency C-sections) were least likely to be found in CRNA institutions. Conclusions: Although anesthesia models were largely similar in the operating room and the obstetric area, differences in actual ANES and CRNA roles indicate that the use of the traditional three model typology is not warranted. The CRNA only model may be a proxy for key resource availability. Implications for Policy, Delivery, or Practice: Studies proposing to link outcomes to anesthesia models should be evaluated in part on the precision of model delineation and measures taken to determine the roles of obstetric resources. Primary Funding Source: American Association of Nurse Anesthetists ●Workplace Civility, Aggressive Behavior and Employee Outcomes David Mohr, Ph.D., Nicholas Warren, ScD, MAT, Michael Hodgson, M.D, M.P.H. Presented By: David Mohr, Ph.D., Investigator, Center for Organization, Leadership and Management Research, Department of Veterans Affairs, VA Boston Healthcare System (152M) 150 S. Huntington Ave, Boston, MA 02130; Tel: 857364-5679; Email: david.mohr2@med.va.gov Research Objective: To assess whether individual perceptions of workplace civility are dependent on the source of aggressive behavior in the workplace and how civility and aggression perceptions influence employee outcomes. Workplace aggression has been found to negatively relate negatively to performance, satisfaction and retention. Workplace civility may offer a way to reduce some of negative effects. These are key issues in retaining a health care workforce. Study Design: Data were obtained from a census survey of employees in a national health care organization. A total of 74,622 responses were obtained (36.5%). Workplace civility was a factor constructed for this study, which consisted of items relating to cooperation, diversity acceptance, cooperation and coworker support. The survey also asked respondents to report on frequency of active (as opposed to passive) verbal aggressive behavior in the workplace. A dichotomous measure of workplace aggressive behavior was developed for each of six statements asking about the frequency of behaviors employees experienced in the past twelve months. These items included such behaviors as name calling, provoking arguments, shouting, and intimidating gestures. Individuals who had experienced 4 or more events were categorized as working in an aggressive environment. This variable was then regressed in a generalized linear mixed model that included a measure of workplace civility and these covariates: gender, race, age, tenure, job category (administrative, clerical, professional, technical, wage grade), level of supervisory status, pay grade, hours worked per pay period, regular day shift status and field facility or office location. Analyses were performed at the individual level with individuals nested within facility. All models are crosssectional. Population Studied: A census survey conducted in 2001 of employees of a large national health care system. Principal Findings: The strongest predictor (for all values p <.001) was workplace civility (parameter estimate = -0.92). Thus individuals who had higher perceptions of workplace civility reported lower frequency of aggressive events as might be expected. Also significant in the model were: hourly worker status (est = .42), administrative employees (est = .32) being male (est = .24), minority status (est =.32) and several of the dummy coded variables were significant as well. In additional models where civility and experience of aggressive behavior was entered into a model, we found civility and experiences of aggressive behavior significantly predicted individuals workgroup performance assessment (civility est = .50, aggression est = -.04), overall job satisfaction (civility est = .64, aggression est = -.19) and intention to leave (civility est = .43, aggression est = .23). We found a very high rate of reported aggressive behavior incidents of four or more times (49%). Conclusions: The strongest predictor of the frequency of aggressive incidents in a health care setting is perceived workplace civility rather than individual or job characteristics. The influence of workplace civility was found to be a better predictor than experiences of aggressive incidents for job satisfaction, performance ratings, and intention to leave. Implications for Policy, Delivery, or Practice: Workplace civility was a strong predictor for key attitudinal outcomes that may impact the satisfaction and retention rates of health care employees as well as quality of work provided within the team. Incidents of aggressive behavior in the workplace, given the high reported frequency, should not be overlooked. Primary Funding Source: VA ●Workplace Civility and Sick Leave Rate Usage over Time David Mohr, Ph.D., Nicholas Warren, ScD, MAT, Michael Hodgson, M.D, M.P.H., Mark Meterko, Ph.D., Richard Lin, M.D. Presented By: David Mohr, Ph.D., Investigator, Center for Organization, Leadership and Management Research, Department of Veterans Affairs, VA Boston Healthcare System (152M), 150 South Huntington Ave, Boston, MA 02130; Tel: 857-364-5679; Email: david.mohr2@med.va.gov Research Objective: The purpose of this study was to examine the influence that increases in workplace civility have on sick leave usage among administrative employees in a health care setting. One way to get increased efficiency from employees is to reduce sick leave rates. Study Design: We sought to test the hypothesis that increased civility would decrease sick leave usage rates. We used data collected from a national health care system at two different time points; 2001 and 2004. A census survey designed to assess employee perceptions of their organizations was conducted during both years which obtained a response rate of 37% and 52% respectively. We selected employees who were classified under “General Service” as opposed to clinical staff. We examined an independent data set for the facility-level sick leave usage for employees for those two years as well. In the intervening years, the system undertook systematic, though locally varied, interventions to improve behavior among individuals. A factor, “workplace civility” was constructed for this study from items relating to conflict resolution, cooperation, respect, diversity acceptance, and coworker support. We conducted analyses using a mixed model with repeated measures for group effects. We controlled for facility-level factors in the model: number of hospital beds, teaching affiliation, urban/rural location and geographical region). Population Studied: Administrative data from a census survey conducted in 2001 and 2004 with general service employees of the Veterans Healthcare Administration. Principal Findings: Workplace civility did predict sick leave rate usage over time. System wide average sick leave usage rates for 2004 (Mean = 68 hours, SD = 6.6) were statistically higher by 1.75 days than 2001 (Mean = 54 hours SD = 6.4). Workplace civility was significantly higher in 2004 (Mean = 3.60, SD = .13) than in 2001 (Mean = 3.39, SD = .16). We tested ordinary least square regression models first to ascertain if civility was a predictor of sick leave rates in 2001 and 2004 separately. Civility was a significant predictor in both models. Next, in a mixed effects repeated measures model, workplace civility was a significant predictor (estimate = -16.78, p <.001) of sick leave rate usage. A one point change in civility was associated with about two fewer sick leave days per general service employee, if all other factors are held equal. The variable of urban status also had a significant entry in this model; individuals who work in rural locations were less likely to use sick leave (est = -2.11, p <.001). There were also small differences based on geographic region. If the average cost per employee time included fringe benefits was approximately $20 an hour, then improving the civility score by 1 standard deviation (0.15) would lead to 2.5 fewer hours or $50 in savings per employee or approximately $50,000 in a typical facility with 1,000 employees. Adding in lost productivity would also increase savings as well. Conclusions: The study found that sick leave rates were prospectively related to workplace civility. Covariates had a much smaller influence on sick leave rates. The increase in both sick leave usage and civility scores might be explained by facility change efforts during the time period, but a closer inspection at site specific strategies is warranted. Implications for Policy, Delivery, or Practice: Over time, some medical centers were able to improve civility which led to substantial improvements going against the general trend. These finding highlight the possible effects that workplace civility may have among general service employees in terms of reducing sick leave rate usage. Sick leave hours can be converted to dollar amounts for lost time and lost productivity. Primary Funding Source: VA ●Nursing Representation and the Nursing Shortage in a Rural State Patricia Moulton, Ph.D., Karen Speaker, B.A. Presented By: Patricia Moulton, Ph.D., Assistant Professor, Rural Health, University of North Dakota, 501 N. Columbia Road, Grand Forks, ND 58202-9037; Tel: (701)777-6781; Fax: (701)777-6779; Email: pmoulton@medicine.nodak.edu Research Objective: With the current and worsening shortage of nurses throughout the United States, addressing the workplace environment will be critical in retaining an adequate workforce. The existence of formal nursing representation structures has been advocated to help improve the workplace environment. The Robert Wood Johnson Foundation Chief Nursing Officer Study (Kimball & O’Neil, 2002) found that 76% of the hospital chief nursing officers reported some sort of nursing representation structure in place. Study Design: The North Dakota Nursing Needs Study, a legislative-mandated study is designed to examine issues of supply, demand, recruitment and retention. This study is funded by the North Dakota Board of Nursing. Of the several possible measurements for nursing shortages, vacancy and turnover rates are the most common. Vacancy rates indicate the number of vacant positions relevant to the number of budgeted positions and a consistent vacancy rate above 6% is thought to indicate a shortage (Prescott, 2000). Turnover rates reflect fluctuation in staffing levels and can be another indicator of the stability of a work environment. Between 2002 and 2004, turnover and vacancy rates have increased throughout North Dakota. This study was designed to determine whether there is a relationship between the increase in turnover and vacancy rate, rurality and nursing representation. Population Studied: Surveys were sent to all hospitals and long-term care facilities in North Dakota in the fall of 2002 and 2004. A total of 65 facilities (hospitals and long-term care) completed the survey in both years which allows for a comparison across the two years. Principal Findings: In 2002, study results indicated that only 45% of hospitals and 38% of long-term care facilities reported having a formal nurse representation structure with most of these facilities located in urban areas. In 2004, 36% of hospitals and 49% of long-term care facilities reported having nurse representation. Despite the overall reduction in representation, an increase was found in rural facilities with 55% of hospitals and 40% long-term care facilities indicating nursing representation in 2004. This presentation will explore possible relationships using regression between indicators of shortage (vacancy and turnover) and the existence of nursing representation structures in rural and urban hospital and longterm care facilities. Conclusions: This presentation will explore possible relationships using multiple regression between indicators of shortage (vacancy and turnover) and the existence of nursing representation structures in rural and urban hospital and longterm care facilities. Implications for Policy, Delivery, or Practice: This information will be useful for healthcare facilities as they look at the many possible retention strategies including nurse representation to prioritize those strategies which have the largest possible impact on maintaining an adequate workforce. Primary Funding Source: North Dakota Board of Nursing ●Comparison of Young Adults' Perceptions of an Ideal and a Healthcare Career Mary Val Palumbo, DNP, APRN, Betty Rambur, DNSc Presented By: Mary Val Palumbo, DNP, APRN, Director, Office of Nursing Workforce, Department of Nursing, University of Vermont, 106 Carrigan Drive, Burlington, VT 05405-0068; Tel: (802) 656-0023; Fax: (802) 656-8306; Email: mpalumbo@uvm.edu Research Objective: The purpose of this study was to compare and contrast young adults’ (age 18-24 years of age) perceptions of an ideal career versus their perceptions of six health professions: nursing, medical laboratory science, pharmacy, respiratory therapy, radiation technology, and physical therapy. Study Design: Design: Survey. Measures: Developed by May et al 1991, the instrument measures 17 parallel items on a 5 point Likert scale and has been assessed for reliability (coefficient alpha .81-.84) and content validity through a panel of experts. Analysis: Descriptive statistics and paired t-tests, with Bonferoni adjusted alpha significance at p < 0.0028. Population Studied: Sample: A convenience sample of 720 18-24 year olds recruited from job fairs and community events between Jan 2005 and Sept 2005. Setting: One metropolitan statistical area within a rural, northeastern state and two less urbanized adjacent communities. Principal Findings: All six health professions were perceived as significantly less desirable (p< 0.001) than the ideal career in the area of “being respected”. All six health careers were perceived as “working with high technology” more than was desired in an ideal career. “Care for people” was the third highest attribute of an ideal career and only pharmacy and radiation technology were found to be statistically significantly lower in this area (p<0.001). Only nurses were significantly perceived (p<0.001 )as having job security that matched the ideal. Additional similarities and differences are detailed. Conclusions: Inaccurate perceptions of healthcare careers may hamper the development of an adequate pipeline of new recruits to these professions, which has the potential to impact all health disciplines. Respect for the work of healthcare professionals was not recognized by this sample. Working with “high technology” was not seen as important in an ideal career. Strategies to address these conclusions and areas for further research are outlined. Implications for Policy, Delivery, or Practice: A shrinking pool of young adults will be tapped for careers in many disciplines in the decade ahead. Quality healthcare in the future will depend on a workforce of these young adults who are adequately prepared for and interested in healthcare careers. Healthcare is increasingly dependent on highly collaborative multidisciplinary teams. Lessons learned from the renewed interest in nursing careers (as evidenced by the increased numbers of nursing students and applicants), may need to be applied across the disciplines in order to prevent future shortages. Primary Funding Source: HRSA ●American Indians and Alaska Natives on the Path to Physician Careers: Supports and Challenges Davis Patterson, Ph.D., Walter Hollow, M.D, Apanakhi Buckley, Ph.D., Polly Olsen, Laura-Mae Baldwin, M.D, M.P.H. Presented By: Davis Patterson, Ph.D., Research Associate, University of Washington Dept. of Family Medicine, WWAMI Center for Health Workforce Studies, 4311 11th Ave NE, Suite 210, Seattle, WA 98105; Tel: (206) 616-6256; Fax: (206) 6164768; Email: dpatterson@fammed.washington.edu Research Objective: American Indians and Alaska Natives (AI/ANs) have persistent health status disparities compared with the rest of the U.S. population. Addressing this problem will require training more AI/AN physicians, who are more likely to choose primary care, locate in underserved communities, and deliver culturally appropriate care. Yet AI/ANs have not achieved parity with whites in medical school enrollment. The purpose of this study is to understand the path to physician careers among matriculated American Indian and Alaska Natives (AI/ANs), focusing on the significant people and experiences that motivated or supported students as well as challenges and barriers along the way. Study Design: This study used qualitative semi-structured, one-on-one, confidential interviews. The research team used grounded theory to content-analyze the interviews and arrive at a consensus on salient support and barrier themes. Study subjects were also invited to give feedback on the themes identified in their own interviews. Population Studied: The study is based on a sample of 10 AI/AN students at the University of Washington School of Medicine. Principal Findings: This research documented six major supports and eight major barriers to AI/AN students’ paths to medical school. The themes included students’ educational experiences, competing career options and priorities, health care experiences, financial factors, cultural connections, family and friends, spirituality, and discrimination. Ties to Native communities both supported students and created conflict between Native culture and the culture of modern Western medicine. Students also reported financial barriers severe enough to constrain participation in the medical school application process, a finding that has not been reported elsewhere. Another unique finding of this study was that spirituality played an important role in the lives of these students as they pursued a medical career. Conclusions: The AI/ANs in this study gained entry to medical school by relying on important supports while facing significant challenges. Their experiences suggest that promoting greater AI/AN participation in medical careers can be facilitated with strategies appropriate to the academic, financial, and cultural needs of AI/AN students. Implications for Policy, Delivery, or Practice: Several strategies based on this study’s findings, and on the authors’ experience conducting programs to support AI/ANs pursuing health professions, might improve recruitment and retention of AI/AN medical students: (1) providing role models, advisors, and mentors; (2) providing early research opportunities by involving AI/AN communities in research on Native health issues; (3) anticipating students’ traditional Native spiritual practices; (4) providing professional socialization opportunities for faculty and AI/AN medical students; (5) creating and implementing rigorous curricula that include indigenous perspectives; and (6) developing a pro-diversity institutional mission statement to inform admissions policies. Collaboration with AI/AN individuals, organizations, and communities is critical to this effort but not a familiar role for most academic medical centers; suggestions for cross-cultural outreach and collaboration are provided. The authors also identify organizations in a position to fund and implement these strategies, along with a list of resources. Increasing the numbers of AI/AN physicians is a matter of social equity and basic fairness, but successful collaborations will also enrich the medical community. Primary Funding Source: HRSA ●Family Physicians in the Child Healthcare Workforce Robert Phillips, M.D, M.S.P.H., Martey Dodoo, Ph.D., Andrew Bazemore, M.D. Presented By: Robert Phillips, M.D., M.S.P.H., Director, The Robert Graham Center, 1350 Connecticut Ave NW, Suite 201, Washington, DC 20036; Tel: 202-331-3360; Fax: 202-331-3374; Email: bphillips@aafp.org Research Objective: Studies of the child healthcare workforce tend to focus exclusively on pediatricians. We sought to understand the evolving role of the family physician (FP) workforce in caring for children, and the potential causes of this change. This included study of specific populations of children and whether family medicine's role remains important. Study Design: We did a comprehensive literature review of recent and past child health workforce analyses for trends and potential explanations of an observed decline in visits to family physicians by children. This review helped shape a secondary analysis of data from the AMA Masterfile data from 1981 through 2004, Area Resource File, US Census (1980 – 2000), Medical Expenditure Panel Survey (1996, 2002), and National Ambulatory Medical Care Survey (1992-2002). Population Studied: We studied the care of children from birth to age 18, and the US physician workforce that cares for them. Principal Findings: In 2004, there was one pediatrician who spends the majority of their time in direct patient care for about every 1,570 children in the US, and about one FP for every 3,200 people. Given the current contribution of family physicians to children’s healthcare, there is one full time equivalent physician for every 1000-1200 children. Visits by children to family physicians have fallen by nearly 25% relative to a 20% rise in visits to pediatricians over the last decade, and a one-third reduction in average annual children’s visits per FP. Erosion of family medicine’s role is due in large part to a doubling of the general pediatrician workforce and a decline in the crude birth rate since 1981. The decline in care provided by family physicians to children has occurred largely in more affluent urban and suburban areas as pediatricians are less likely to locate in rural and low income areas. Both specialties play an important role in caring for children reliant on safety net programs; however community health centers and the National Health Service Corps are more dependent on FPs. Uninsured children and those on Medicaid are less likely (than privately insured children) to have a pediatrician as their usual source of care. FPs’ role in caring for adolescents is more stable than for younger children (26% of visits vs 24% of visits for pediatricians); however, half of adolescents are now seen by other specialties. Conclusions: The role of FPs remains important, particularly to rural and underserved populations, despite a significant erosion of their role in providing care to children. The growth of the child healthcare physician workforce has outpaced the birth rate in the US, producing a robust workforce for children’s health that meets or exceeds sufficiency by measures offered by the American Academy of Pediatrics. Implications for Policy, Delivery, or Practice: Despite there being one child healthcare physician for every 1200 children, eight million children lack insurance and more than seven million children lack a medical home. There are real opportunities for pediatricians and FPs to turn from a period of growth and competition to collaborate on resolving access problems and tackling the family and community sources of childhood morbidity and mortality. Primary Funding Source: The American Academy of Family Physicians ●Who Are the Dentists Who Provide Care to Publicly Covered Patients? Nadereh Pourat, Ph.D., Dylan Roby, Ph.D., Roberta Wyn, Ph.D., Marvin Marcus, DDS Presented By: Nadereh Pourat, Ph.D., Senior Research Scientist, Health Services, UCLA Center for Health Policy Research, 10911 Weyburn Ave, Suite 300, Los Angeles, CA 90024; Tel: 310/794-2201; Fax: 310/794-2686; Email: pourat@ucla.edu Research Objective: Public coverage of dental care is the solution of choice to provide access to care for the low income, yet, delivery of care may be negatively influenced by parsimonious payment policies and program restrictions. Such policies can impact providers’ decisions on the scope of public patients in their practice, staffing, practice structure, and patient care delivered. We examined the independent association of demographic, business structure, and patient care characteristics of dentists with the presence of publicly covered patients in their practice to gain insights into potential differences in delivery of dental care to these patients. Study Design: A cross-section of dentists in private practices in California was surveyed. Survey topics included demographics, practice characteristics, and patient care. Characteristics of dentists by presence of publicly covered patients in their practice were examined in bivariate and multiple logistic regression analysis. Analyses were weighted to account for disproportionate sampling of dentists in rural and less populated counties and adjusted for the clustering of dentists by county. Population Studied: A cross-section of dentists in private practice in all California counties with licensed dentists. About 4,300 eligible dentists participated in the mail survey with telephone follow up, with an adjusted response rate of 51%. The sample consisted of approximately 3,800 respondents who were generalists or specialists who provided general care. Principal Findings: Preliminary analyses show that about half of dentists had publicly covered patients in their practices, had been in practice between 6-20 years, and accepted sliding scale fees. The majority were generalists, in solo practice, and spoke a language other than English or had staff that could do so. Regression analysis revealed that dentists with publicly covered patients were more likely to have a second language capacity, accept sliding scale fees, or have multiple practice locations than those who did not have any such patients. Also, dentists with publicly covered patients were more likely to practice in rural and less populated counties rather than Los Angeles County. Dentists with publicly covered patients were more likely to have fewer hygienists, spend less time in preventive care, and had shorter appointment times than dentists without any publicly covered patients. Dentists with more than 5% publicly covered patients in their practice were more likely to accept sliding scale fees and have multiple practice locations than dentists with fewer publicly covered patients. They also had fewer dentists and hygienists in their practice. Conclusions: Results suggest that dentists who provide care to publicly covered patients work in different types of practices such as multiple locations, have a possibly larger volume of low income patients (as evidenced by accepting sliding scale fees), employ fewer hygienists; and differ in some aspects of their patient care, such as shorter appointment times and less preventive care. Implications for Policy, Delivery, or Practice: The delivery of dental care to publicly covered patients may differ in content and quality. Understanding the differences in care provided to such patients is essential in examining the success of public programs in improving delivery of care to low income populations. Primary Funding Source: California Dental Association Foundation ●Supply and Demand Across Four Health Professions in a Rural State Betty Rambur, DNSc, Mary Val Palumbo, DNP, Robert Ross, Ph.D., Burton Wilcke Jr., Ph.D., Barbara McIntosh, Ph.D. Presented By: Betty Rambur, DNSc, Professor of Nursing and Dean, College of Nursing and Health Sciences, University of Vermont, 105 Rowell Building, Burlington, VT 05405-0068; Tel: (802) 656-2216; Fax: (802) 656-2191; Email: betty.rambur@uvm.edu Research Objective: To explore rural healthcare workforce demographics from the perspective of the individual and the employer as a basis for evidence-based health workforce planning. Study Design: This two-part, survey design study utilized the State of Vermont as a health workforce laboratory. In Part One, the workforce minimum data set recommended by Colleagues in Caring was used to analyze demographics, job satisfaction, intention to leave current position and profession, and reasons for such intention. These data were gathered in spring 2005 from four healthcare professions: medical laboratorians, radiographers, respiratory therapists, and registered nurses. Part Two explored hospital vacancy and turnover rates for these same professions at two points in time, 2003 and 2005. This instrument was developed following an extensive literature review, tested for content validity through panel of experts, and pilot tested in the field (detailed in Reinier, K., Palumbo, M, McIntosh, B., Rambur, B., Kolodinsky, J., Hurowitz, L., & Ashikaga, T. (2005). Measuring the nursing workforce: clarifying the definitions. Medical Research and Review, 62(6), 741-755.) Population Studied: The entire populations of registered nurses, medical laboratorians, radiographers, and respiratory therapists and all hospitals in the State of Vermont were surveyed. Response rates for Part One were: respiratory therapists 65% (n=100); medical laboratorians 51%, (n=241); radiographers 58% (n=315); registered nurses, 65%, (n=5805). Response rates for the employer-based surveys range were 94% (15 of 16 hospitals) in 2003 and 75% (12 of 16 hospitals) in 2005. Principal Findings: Radiographers were the youngest profession (x= 43.8) and had the broadest age distribution. RNs were the oldest (x= 48), followed by laboratorians (x= 45). Seventy-six percent of laboratorians were over the age of forty, and laboratorians also held the greatest proportion of bachelor and higher degree (58%). Income, however, did not parallel education. Radiographers and registered nurses reported the highest albeit modest satisfaction, with 55% and 54% indicating they were “very satisfied” with their current position, respectively. Nevertheless, 22% percent of the radiographers and 23% of the registered nurses were “somewhat likely” or “very likely” to leave their position within the next year, as were a substantial number of the respiratory therapists (28%) and medical laboratorians (23%). Of those intending to leave their position, 21% of respiratory therapists, 16% of the radiographers, 13% of the RNs and 9% of the laboratorians plan to leave their profession. The most common reason given by medical laboratorians was “job stress” at 45%. Vacancy and turnover rates for registered nurses and laboratorians showed substantial but less dramatic change than for respiratory therapists, who had a hospital vacancy rate of 18% in 2003 and 5% in 2005, for example, perhaps reflecting the 23% turnover rate in 2003 and 6% in 2005. Conclusions: While the nursing shortage has received growing attention, these data suggest that ongoing workforce assessment across all health professions is necessary to assess trends and develop appropriate strategies to ensure adequate supply of these essential healthcare capacities. Implications for Policy, Delivery, or Practice: Ongoing, reliable, valid, and easily accessible health workforce data across professions is essential to health planning and offers a strategic use of state funds. This is particularly important in rural states, where relatively small changes in absolute numbers can mean dramatic changes in availability of providers and essential services. Primary Funding Source: HRSA ●Older Nurse Recruitment and Retention Initiatives across Four Settings in a Rural State Betty Rambur, DNSc, Mary Val Palumbo, DNSc, Barbara McIntosh, Ph.D. Presented By: Betty Rambur, DNSc, Professor of Nursing and Dean, College of Nursing and Health Sciences, University of Vermont, 105 Rowell Building, Burlington, VT 05405; Tel: (802) 656-2216; Fax: (802) 656-2191; Email: betty.rambur@uvm.edu Research Objective: The aim of this study was to describe, compare, and contrast recruitment and retention policies directed toward older (age 50+) registered nurses (RNs) across four settings: hospitals, home health agencies, long term care facilities, and office practices in a rural state, as a first step toward evidence-based nurse resource management. Study Design: This study was part of a larger statewide survey designed for the analysis of workforce patterns in hospitals, home health agencies, long term care facilities, and office settings. The instrument was developed following an extensive literature review, tested for content validity through a panel of experts, and pilot tested, as detailed elsewhere (Reinier, K., Palumbo, M, McIntosh, B., Rambur, B., Kolodinsky, J., Hurowitz, L., & Ashikaga, T. (2005). Measuring the nursing workforce: clarifying the definitions. Medical Research and Review, 62(6), 741-755.) The survey was mailed to the facility’s chief nursing officer, regardless of position title. Population Studied: The entire state population of hospitals, home health agencies, long term care facilities and primary care offices listed by the State Department of Health and/or Area Health Education Center were surveyed, with the following response rates: hospital, 75% (n = 12); home health agencies, 83% (n = 10); long term care facilities, 42%; (n=18); primary care offices, 40% (n=85). Principal Findings: Only 10% of hospitals reported have initiatives directed toward recruitment of the older RN, compared to 40% of home health agencies, 35% of long term care facilities, and 14% of primary care offices. Retention initiatives directed toward older RNs were more commonly reported by respondents, with 60% of hospitals, 70% of home health agencies, 59% of long term care facilities, and 35% of primary care offices reporting such strategies. The qualitative data, however, suggests that existing practices vary in depth and complexity. Moreover, comments reflected a varied understanding of the purpose and value of such initiatives. Conclusions: Facilities and agencies are not consistently implementing meaningful strategies to recruit and retain the older RN. Implications for Policy, Delivery, or Practice: Older nurses provide a pool of experience that the health system is ill prepared to forego. In the study setting, for example, 39% of working RNs are over age 50, and there are more working RNs over the age of 60 than under the age of 30. Nurses who are currently 50 -55 years old will likely be necessary to augment the emerging nursing pipeline, thus recruitment and retention is extremely important. Best practices for recruitment and retention of older RNs should be developed and disseminated. Primary Funding Source: HRSA ●Changes in Physician Productivity 1993 – 2003 Mary Rimsza, M.D, Mark Speicher, MHA, Mary Ellen Rimsza, M.D, William G. Johnson, Ph.D., Michael Grossman, M.D. Presented By: Mary Rimsza, M.D, Professor, School of Health Management and Policy, Center for Health Information and Research Seidman Research Institute, Arizona State University, PO Box 874506, Tempe, AZ 85287-4506; Tel: (480) 965 1622; Fax: (480) 965 6654; Email: mary.rimsza@asu.edu Research Objective: Conventional wisdom holds that physician workloads have changed, and not for the better. Both patients and physicians believe that doctors have less time for patients, and that physicians are seeing more patients that ever. There has been recognition of a number of workload issues as a cause for physician dissatisfaction, active doctors leaving medicine and an inability to recruit new physicians to certain areas or specialties. Reasons for this change in workload may include population demographics, the continuing increase in managed care, changes in access to care caused by economic swings or levels of insurance coverage, and physician lifestyle issues such as gender, worklife balance, choice of specialty and practice location (rural vs. urban), etc. Study Design: The Arizona Medical Board and the Arizona Board of Osteopathic Examiners collect information on physicians as a part of the license renewal process. This data includes specialty, office location, education, age and other information. Between 1992 and 1997, an Arizona State University project added survey questions to the license renewal packet. In 2003, the project was resumed as a joint effort of Arizona State University and the University of Arizona. The survey of practicing physicians from 2003 was used to compare data on licensed allopathic and osteopathic physicians practicing in Arizona in 1993, 1994, 1996, 1997, and 1998 and 2003 to determine the change in time spent in practice as well as number of patients seen during the survey periods. (Results for 1998 were self-reported by survey respondents in 2003.) The direction and magnitude of changes are reviewed by age group, specialty and geographic location in Arizona. Population Studied: All licensed allopathic and osteopathic physicians were surveyed during the survey years. The survey of practicing physicians is distributed and collected as a part of the annual or biennial license renewal process for all allopathic and osteopathic physicians through a cooperative agreement with the physician licensing boards. Principal Findings: As estimated by the survey respondents, the number of patients seen for all practicing physicians increased from 69 per week in 1994 (n=11,794) to 88 in 1997 (n=8,451) to 84 in 1998 and 84 in 2003 (both reported on the 2003 survey; n=7,675). Productivity (patients seen per week and hours worked per week) increased across all specialty and practice settings in roughly the same pattern; while patients seen per week varied greatly between specialties. In 2004, for example, anesthesiologists reported seeing an average of 37 patients per week, cardiologists 106, family practitioners 95, internists 85, obstetricians 90, and surgeons 52. Conclusions: The number of patients seen per week in rural areas is significantly higher than in urban areas (though the gap is narrowing over time) but hours worked per week do not differ as greatly between urban and rural areas. Implications for Policy, Delivery, or Practice: Models of the need for health care providers are important for health planning and policy decisions. The productivity of physicians is an important but generally unknown component of workforce planning models. Primary Funding Source: Other Foundation, Flinn Foundation, St. Luke's Health Initiatives, BHHS Legacy Foundation ●Human and Social Capital of Nursing Personnel in Magnet Hopitals and Long Term Care Organizations Kent Rondeau, Ph.D., Terry Wagar, Ph.D., LLB Presented By: Kent Rondeau, Ph.D., Associate Professor, Public Health Sciences, University of Alberta, 13-103 Clinical Sciences Building, Edmonton, Alberta, T6G 2G3; Tel: (780) 492-8608; Fax: (780) 492-0364; Email: kent.rondeau@ualberta.ca Research Objective: This reseach seeks to explore the contribution of intellectual (human and social) capital of nursing personnel towards magnet status in hospitals and long-term care organizations. Study Design: A mail survey questionnaire was sent to the directors of nursing care in 2250 Canadian hospitals and longterm care organizations in late 2005. Approximately 600 hospitals and nursing homes constitute our study database. Population Studied: Directors of nursing care in Canadian hospitals and long-term care establishments are asked to about their existing practices with respect to how they organize and manage their nursing human resources. Nursing unit goals and strategies, human resource management practices, nursing recruitment/retention approaches, magnet strength, nursing intellectual capital, decision making culture, employee training and development practices, labor-management relations, nursing workforce and establishment characteristics are assessed in each organization. Principal Findings: Hospitals and nursing homes which have strong magnet characteristics are more likely to have adopted certain human resource practices, to have inculcated in their nursing workforce highly progressive and participatory decision making approaches, and to characterize their nursing workforce as possessing higher levels of human and social capital. Conclusions: Health care organizations which want to develop stronger magnet capacity with respect to recruiting and retaining their nursing personnel will be more effective if they develop nurse workforce human and social capital. Implications for Policy, Delivery, or Practice: Investments in increasing intellectual capital of nurses can have a significant impact in improving the capacity of health care organizations to recruit and retain nursing personnel. Primary Funding Source: Private funding ●Residency Choice Among Women Medical Students-Effect of Economic and Time-Constraint Factors Shuolun Ruan, B.S., Mythreyi Bhargavan, Ph.D., Victoria K. Potterton, B.S., Kimberly E. Applegate, M.D., M.S., Jonathan H. Sunshine, Ph.D., Howard P. Forman, M.D., M.B.A. Presented By: Shuolun Ruan, B.S., M.D./Ph.D.-Health Services Research & Policy, University of Rochester, 1323 Genesee St., Rochester, NY 14611-4201; Tel: 913-558-3547; Email: shuolun.ruan@aya.yale.edu Research Objective: To determine the extent to which quantifiable measures of residency and in-practice lifestyle, and also practice income, can explain differences and trends in the percent of women in the entering residency class for 24 specialties over the 12 years 1993-2004. Study Design: Annual data on the number of women and men entering residency, by specialty, during the period 19932004 was collected from the American Medical Association (AMA) and the Association of American Medical Colleges. Data on residency lifestyle characteristics were obtained from the Fellowship and Residency Electronic Interactive Database, and median annual income was obtained from the Medical Group Management Association. Data on in-practice hours and hours worked per year were obtained from AMA publications. Using the percentage of women among entrants to each residency as the dependent variable, we applied multivariate linear regression analysis to measure the effect of number of years in residency, weekly duty hours in the first year of residency, in-practice weekly hours, income per hour in practice, and a time trend from 1993 to 2004 on the percentage of women entering a specialty. In addition, we regressed separate models for residency characteristics and practice characteristics. All models included interaction terms. Population Studied: Women entering the first year of specialty-specific residency training. Principal Findings: Longer years of residency, longer weekly hours in practice, and higher in-practice income per hour were inversely associated with percent women entering a specialty. Conversely, longer hours per week in the first year of residency was associated with more women. These factors explained fully 61 percent of the variance across specialties and over time in the proportion of residency program entrants who are women. Dermatology and OB/GYN, however, have had consistently much higher percentages of women entrants than can be explained by these factors, and orthopaedic surgery has consistently had a lower percentage. Including a control for concordance between the gender of most patients and the physician explained an additional 12 percent of the variance in percentage of women in residency programs. Conclusions: Residency and in-practice lifestyle characteristics and income are important factors for women's specialty choices. There remains, however, substantial variation not explained by these factors including career satisfaction of women in various specialties, presence of mentors and role models, competitiveness of residencies, discrimination, training program and practice flexibility. We do not have data to address these in this study. Implications for Policy, Delivery, or Practice: We find that residency and in-practice lifestyle and in-practice income offer much explanation for the percentages of women found entering many specialties such as pediatrics, diagnostic radiology, or general surgery. For specialties such as dermatology and orthopaedic surgery, however, there are other advantages and disadvantages, respectively, being considered by women. These additional considerations provide valuable interventional opportunities, including providing mentors and greater practice flexibility, to attract women into areas that have historically had few female physicians. With documented incidences of some patients preferring women providers, a lack of women in any specialty undermines the goal of equal access to quality healthcare. Primary Funding Source: No Funding ●How Do Physicians Perceive the Effect of Evidence-Based Guidelines on Their Practice? Christine Sammer, R.N., M.P.H., Kristine Lykens, MPA, Ph.D., Karan Singh, M.S., Ph.D. Presented By: Christine Sammer, R.N., M.P.H., Doctoral Candidate, Health Management and Policy, Unversity of North Texas Health Science Center, 3500 Camp Bowie Blvd., Fort Worth, TX 76107; Tel: 817-568-5306; Fax: 817-735-2446; Email: christine.sammer@ahss.org Research Objective: The study explores physician and practice characteristics that may contribute to the effect practice guidelines have on their practice of medicine. Study Design: Intercooled Stata 8.1® software survey commands for binomial logistic and ordinal logistic regression models were used for assessing the associations of various factors on the perceived impact practice guidelines have on a physician’s practice. For this analysis the restricted data set of the Community Tracking Study (CTS) Physician Survey was obtained from the Center for Studying Health Systems Change. This data set included the sample design variables necessary to make statistical adjustments for the study design. Independent variables included demographics such as gender; race; year of graduation from medical school; specialty areas; practice types; and computer usage. Population Studied: The study analyzes data from the third round of the CTS Physician Survey, 2000-2001, a large-scale investigation of changes in the health care system and their effects on people. The survey was administered to physicians in the 60 CTS sites and to a supplemental national sample of physicians. Principal Findings: Responses from 12,126 physicians were included in the regression models. In the binomial logistic regression, twelve of the 34 variables were significant at alpha .05. The analysis showed that more recent (since 1996) graduates from medical school were significantly more likely to state practice guidelines had an effect on their practice. Physicians who use computers to access information in their practices were also strongly correlated with a perceived impact of guidelines on practice. Other factors that positively influenced the dependent variable and were significant at alpha .05 were female gender, the specialty of Ob-Gyn, and all non-solo practice types. An ordinal logistic regression was also estimated to capture the full range of responses regarding the perceived impact of practice guidelines from no effect to a very strong effect. The results of this model were consistent with the binomial logistic model. Conclusions: Whereas the goal of EB guidelines has been to provide a strong scientific framework and to improve outcomes, many barriers have prevented wide acceptance and impact among the medical community. We found year of medical school graduation and practice setting correlates with the perceived impact of evidence-based guidelines. In addition, our findings indicate the importance of information technology concepts in the effects of evidence-based guidelines in medical education. Implications for Policy, Delivery, or Practice: Our findings regarding year of graduation from medical school and use of technology would suggest that current medical school practices, such as addressing guidelines during clinical training and requirements that students purchase laptop computers as an information resource, will have positive effects on physician practice. The findings further suggest research to identify other factors affecting the effect of practice guidelines on physician practice. More research related to behavior, attitudes, and perceptions related to loss of autonomy would be a valuable addition to the body of knowledge. Primary Funding Source: No Funding ●Money, Planning and Outcomes: Three Critical Issues in Continuing Medical Education Sandra Schwanberg, Ph.D., RN Presented By: Sandra Schwanberg, Ph.D., RN, Senior Clinical Researcher, Medical Education, Lovelace Clinic Foundation, 2309 Renard Pl SE, Albuquerque, NM 87106; Tel: 505-2627568; Fax: 505-262-7598; Email: Sandra.schwanberg@lcfresearch.org Research Objective: The purpose of the paper is to discuss three primary issues that influence the quality of continuing medical education programs and to provide remedies for program improvement. The issues include a lack of stable funding for continuing education programs, a lack of formal planning processes and structures in creating programs and a dearth of ongoing effectiveness evaluation. Study Design: Descriptive Principal Findings: Funding- Approximately 62% of continuing medical education activities is funded through the pharmaceutical industry or other healthcare related companies. Independence from industry influence on continuing education content is an ongoing concern. Continuing education programs may be informally planned to secure funding rather than meet ongoing educational needs. Funding sources for continuing education need to be expanded and address programmatic issues rather than the current piecemeal approach. Planning- Much of the planning for continuing medical education is informal focusing on limited interviews with practitioners, small group meetings, surveys with low response rates and previous conference or event evaluations. This process contributes to a “hodgepodge” of subjects for continuing education programs rather than a needed formal curriculum that extends graduate medical education to help clinicians maintain and improve standards of care. A formal curriculum for continuing medical education would require standardized data based needs assessments, program planning and a formal evaluation process. Health care professionals involved in graduate medical education would be the best prepared to plan and evaluate activities. Evaluation- Few continuing education programs implement an actual evaluation plan. Most “effectiveness” evaluation focuses on attendee reactions to events, rather than ability to use the information, apply standards of care or changes in patient health status indicators. In addition, the evaluation of conference faculty expertise and teaching ability also requires attention, development and evaluation. Conclusions: Continuing medical education is required for relicensure. Education is essential as medical information changes rapidly. In addition, ongoing concerns about healthcare quality and patient safety have focused on provider education yet surprisingly little attention has been focused on funding, planning and evaluation. Implications for Policy, Delivery, or Practice: Continuing medical education programs should be planned, evaluated and funded through new approaches connected with academic health sciences centers. Primary Funding Source: No Funding ●The Role of Physician Supply in Determining Health Care Services Utilization in Rural Canada Lyn Sibley, BSc, M.H.A. Presented By: Lyn Sibley, BSc, M.H.A., Student, Health Policy & Management, Johns Hopkins Bloomberg School of Public Health, 1418 West 37th Street, Baltimore, MD 21211; Tel: 443320-3239; Fax: 410-995-3781; Email: lsibley@jhsph.edu Research Objective: The goal of this research is to gain an understanding of the degree to which the supply of general and specialist physicians determines health care services utilization among rural populations of Canada. Study Design: This is a cross-sectional study of the population of Canada using data from the 2003 Canadian Community Health Survey (CCHS). Multilevel regression models were constructed to identify the individual, community and health system variables that are independent predictors of health care services utilization. The models also indicate the independent effect of level of community ruralness on utilization of services. Population Studied: The CCHS is a national survey designed to gather health-related data at the health region level. The study sample includes all survey respondents aged 18 and older who resided in one of the ten provinces (N=119,104). Using Statistic Canada’s Statistical Area Classification the population is divided in to six cohorts based on the level of rurality of their community. Principal Findings: The main dependant variable, health care services utilization, is indicated by four measures: had an influenza immunization in the last two years, consulted a family physician in the previous 12 months, consulted a specialist in the previous 12 months, and had a mammogram in the last two years (for woman aged 50 and above). The independent variables are divided into three categories: individual characteristics, community level social factors, and health system characteristics. The community level social factors were derived from the 2001 Census and aggregated at the municipality level. Similarly health system characteristics were derived from data collected by the Canadian Institute for Health Information and aggregated at the health region level. Conclusions: Universal health insurance coverage has eliminated many barriers to receiving appropriate, high quality health care in Canada, however, geography remains as a obstacle to access. Rural populations, when compared to those that are urban, have lower health care services utilization rates even after adjusting for age, sex, and other social factors. Implications for Policy, Delivery, or Practice: This paper presents the findings of the multilevel models described above, with particular attention given to mutable health system variables such has physician supply and distribution. This research will help to inform policy makers on whether an increase or change in physician supply will address the reduced access to care in rural populations or if policies aimed at social factors would be more appropriate. Primary Funding Source: Canadian Institutes of Health Research ●Does the Specialty of the Chemotherapy Provider Inflence Outcome? Jeffrey H Silber, M.D, Ph.D., Paul R. Rosenbaum, Ph.D., Daniel Polsky, Ph.D., Richard N. Ross, Ph.D., Katrina Armstrong, M.D, Thomas C. Randall, M.D Presented By: Jeffrey H Silber, M.D, Ph.D., Professor of Pediatrics and Director, The Center for Outcomes Research, The University of Pennsylvania/The Children's Hospital of Philadelphia, 3535 Market Street, Suite 1029, Philadelphia, PA 19104; Tel: 215-590-5635; Fax: 215-590-2378; Email: Silberj@Wharton.UPENN.edu Research Objective: Medical Oncologists (MOs) specialize in administering chemotherapy while Gynecologic Oncologists (GOs) specialize in the surgical management of gynecologic cancers as well as providing chemotherapy. We asked whether survival differed according to the type of specialist providing the chemotherapy after ovarian cancer surgery. It is always difficult to compare specialists due to selection bias. In this case, it was especially difficult since the type of surgeon influenced the stage of the patient, the stage of the patient influenced outcome, and the chemotherapy provider was associated with the type of surgeon. Study Design: We identified patients who were diagnosed with ovarian cancer after the age of 65 and who received chemotherapy from a GO after surgery performed by any type of surgeon. Using optimal matching and a propensity score based on 35 prognostic characteristics, we identified similar patients who were operated on, and staged, by nearly identical types of surgeons but who received chemotherapy from an MO. Population Studied: Merged SEER-Medicare clinical and administrative data from the years 1991 through 2001. Principal Findings: We identified 344 patients who were given chemotherapy for ovarian cancer by GOs after having undergone surgery by either GOs (76%), Gynecologists (16%), or general surgeons or other surgical specialties (8%). Patients given chemotherapy by MOs were matched to these patients. Both groups had nearly identical surgical specialists, age, year of treatment, stage, tumor grade, race and 32 other prognostic factors. There was no difference in overall survival between the GO or MO groups (P = 0.45, paired PrenticeWilcoxon test). The 5 year survival was 35% (sd=2.6%) for the GO group and 34% (sd=2.6%) for the MO group. However, MOs administered chemotherapy over more weeks than did the GOs (patient mean = 16.5 Vs 12.1 weeks, P < 0.0023, Wilcoxon rank sum test) and MO patients had more weeks that included at least one of the following chemotherapy associated adverse events (neutropenia, anemia, thrombocytopenia, diarrhea, dehydration or mucositis) than did the GO group (patient mean = 16.2 Vs 8.9 weeks, P < 0.0001, Wilcoxon rank sum test). Conclusions: Despite differences in training, specialty emphasis, and practice style concerning the use of chemotherapy (MO patients had more weeks of chemotherapy and more weeks with chemotherapy associated adverse events than GO patients), we found no difference in survival between patients who received chemotherapy administered by gynecologic oncologists and medical oncologists. Implications for Policy, Delivery, or Practice: From a policy perspective, it would appear that specialists tend to use the tools they were trained to use. The natural bias of the medical oncologist was to treat more intensely with chemotherapy, not realizing that less chemotherapy yielded identical outcomes. From a research perspective, Health Services Researchers are often asked to evaluate and compare specialty performance. Multivariate matching can be a powerful tool in helping to make these comparisons by more transparently addressing potential confounders than the standard regression approach. Primary Funding Source: NCI ●Where Have the Nurses Gone? An Exploratory Study of RNs with Expired Licenses in Washington State Susan Skillman, MS, Lorella Palazzo, PhC, L. Gary Hart, Ph.D., David Keepnews, Ph.D., J.D., RN, FAAN ●Measuring the Marginal Productivity of Financial Support for Nursing Students Joanne Spetz, Ph.D., Susan Chapman, Ph.D., RN, Jean Ann Seago, Ph.D., RN Presented By: Susan Skillman, MS, Deputy Director, University of Washington, Family Medicine, Center for Health Workforce Studies, 4311 11th Ave. NE, Suite 210, Seattle, WA 98105; Tel: (206)543-3557; Fax: (206)616-4768; Email: skillman@u.washington.edu Research Objective: To describe the characteristics of Washington RNs who are no longer in nursing, the reasons for leaving, and the circumstances under which they might return to practice. Study Design: We surveyed a 50% sample of Washington RNs in 2002 and 2003 who did not renew their licenses and conducted extensive followup on a sample of nonrespondents. Population Studied: RNs in Washington state with expired licenses. Principal Findings: Our expectations that many of these RNs with expired licenses had moved out of state was confirmed by the low (20%) survey response rate, and subsequent followup of a sample of nonrespondents. Of the survey respondents, 70.1% were not working as nurses, citing retirement, followed by health problems, domestic or family reasons, and job stress as reasons for leaving the field. Nonworking RNs were almost evenly split between those reporting being satisfied or dissatisfied with their last nursing position. A minority of former RNs was employed in another occupation, and even fewer were searching for RN work. Change in personal situation was most often cited by workingage former RNs as an inducement to reenter nursing, but over 50% said that they would never practice nursing again. Reflecting on their nursing careers, most respondents reported changes in nursing practice: some conditions improved (e.g. RN pay, variety of career opportunities in available in nursing), others worsened (e.g. dangers and physical demands of the job). Yet, a majority of non-practicing RNs said they still considered themselves to be nurses and would advise a young person to enter the profession. Conclusions: This study suggests that most RNs who leave active practice do so for personal reasons and while they may still view themselves as nurses, they show little propensity for rejoining the nursing workforce in the foreseeable future. Implications for Policy, Delivery, or Practice: This study adds to our understanding of why RNs leave nursing, and contributes to formulating proposals to increase retention of currently-practicing RNs. Primary Funding Source: HRSA Presented By: Joanne Spetz, Ph.D., Associate Professor, Community Health Systems, University of California, San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: 415-502-4443; Fax: 415-476-4113; Email: jojo@alum.mit.edu Research Objective: In response to the national shortage of registered nurses, federal and state governments have provided funding to nursing education programs to expand the supply of RNs. Most of these programs either provide financial support to currently-enrolled students, with the goal of improving the productivity of education programs, or expand the number of education slots available for students. There has been no research of the relative effectiveness of these strategies. This study compares the costs and results of programs to provide financial support to nursing students and expand nursing education slots, using new data from California. Study Design: Twenty-two regional groups were awarded a total of $28 million to expand RN supply, with projects ending in 2005. Some of these groups used the funds to provide financial support to students, some expanded education slots, and some did both. In addition, some programs received private funds from hospitals and other local agencies to support their regional efforts. We are using data provided by the California Board of Registered Nursing, California Community Colleges Chancellors Office, the funded groups, and other state government agencies. To estimate the effectiveness of the financial support programs, we estimate a multivariate equation in which the graduation rate is the dependent variable, and the key explanatory variable is the percent of students receiving financial support. The coefficients from this equation are then used to estimate the net increase in graduating RNs resulting from the financial support programs. To estimate the effect of the slotexpansion programs, we multiply the number of new slots by the share of students expected to graduate. These two numbers of “net new nurses” are compared with the costs of each strategy. Population Studied: All registered nursing education programs in California. Principal Findings: Over 1500 RN students received financial support to improve program productivity, and over 1800 new education spaces were created. Preliminary data suggest that the programs providing financial support to students had a substantial effect on student attrition. However, the programs that used funds to expand slots have allowed for the education of many additional nurses. It appears that the slot expansion programs provide more nurses per dollar. Final data are now being received by the research team and a final report will be written by March 31, 2006. Conclusions: Preliminary results indicate that slot expansion programs provide more nurses per dollar. Implications for Policy, Delivery, or Practice: Policymakers should focus resources on expanding space in nursing programs rather than financial support for current students. Primary Funding Source: California Employment Development Dept. ●The Impact of Obesity on Employment and Work Limitations among U.S. Adults, 1986-1999 Kaan Tunceli, Ph.D., Kemeng Li, M.A., L. Keoki Williams, M.D, M.P.H. measured weight and height, the implications of obesity on labor market outcomes are enormous for patients, families, employers, and policy makers. Primary Funding Source: No Funding Presented By: Kaan Tunceli, Ph.D., Health Economist, Center for Health Services Research, Henry Ford Health System, One Ford Place, Suite 3A, Detroit, MI 48202; Tel: 313-874-5485; Fax: 313-874-7137; Email: ktuncel1@hfhs.org Research Objective: To determine the relationship between body mass index (BMI) and workforce participation and work limitations in a U.S. working-age population. Study Design: Individuals were classified into the following weight categories: underweight (BMI <18.5), normal weight (BMI >=18.5 but <25), overweight (BMI >=25 but <30) and obese (BMI >=30). Using multivariable probit models, we estimated the effect of obesity on the probability of employment and work limitations. Analyses with work limitation as the outcome were limited to respondents working in 1999. In models, we controlled for smoking, selfreported health, age, race, marital status, level of education, wealth, the number of children, and baseline employment status. All analyses were stratified by sex. Because a number of individuals (n = 1,991) did not respond to the survey in 1999 but were otherwise eligible, we assessed for potential participation biases that could have affected our results. Population Studied: The empirical analysis uses data from the 1986 and 1999 panels of the Panel Study of Income Dynamics (PSID), a nationwide prospective cohort. The selfreported height and weight information was collected for the first time in 1986 and again in 1999. We restricted our study population to those who participated in both interviews in 1986 (baseline) and 1999 (follow-up) and who were of working age (i.e., age 18 years and older in 1986 and less than age 65 years in 1999). This resulted in a final study sample of 4,290 respondents (1,895 men and 2,395 women). Principal Findings: After adjusting for baseline sociodemographic characteristics, smoking status, exercise, and self-reported health, obesity was associated with reduced employment at follow-up (men: marginal effect [ME] -4.8 percentage points [pp]; p < 0.05; women: ME -5.8 pp ; p < 0.10). Among employed women, being either overweight or obese was associated with an increase in self-reported work limitations when compared with normal weight individuals (overweight: ME +7.7 pp; p < 0.01; obese: ME +20.1 pp; p < 0.01). Among men, the relationship between obesity and work limitations was of borderline significance (ME +4.9 pp ; p < 0.10). Adjusting for the propensity to participate in followup did not alter the previously described relationships between obesity and either employment or work limitations. Conclusions: Our findings suggest that obesity leads to reductions in employment for both men and women after thirteen years of follow-up. We also show that being overweight or obese may contribute to work limitations at follow-up, especially in women. Implications for Policy, Delivery, or Practice: As the prevalence of obesity in the U.S. has increased, so too have associated economic burdens. The prevalence of obesity is likely to escalate further. This implies that the number (and proportion) of obese individuals among working age population will be even greater in the future. Indeed, with as many as 1 in 3 people already obese based on objectively ●Measuring the Potential Financial Impact of Mandatory Nurse-Staffing Ratios on Hospitals in Massachusetts: Initial Estimates and Methodological Challenges Michael Tutty, M.H.A., Debra Hurwitz, M.B.A., BSN Presented By: Michael Tutty, M.H.A., Senior Project Director, Center for Health Policy and Research, University of Massachusetts Medical School, 222 Maple Avenue, Higgins Building, Shrewsbury, MA 01545; Tel: (508) 856-4350; Fax: (508) 856-4456; Email: michael.tutty@umassmed.edu Research Objective: To estimate the financial impact on hospitals of proposed legislation requiring mandatory minimum nurse-to-patient ratios in Massachusetts hospitals. Study Design: Data from 2004 on registered nurse (RN) staffing and inpatient utilization, broken out by hospital unit, was collected from a convenience sample of Massachusetts hospitals. Nurse-to-patient ratios were calculated for units with usable data. The actual ratios were then compared with the proposed minimum ratios, to determine whether hospital units would have had to increase staffing, had the ratios been in effect. For units with nursing shortfalls, the cost of compliance with the staffing ratios was calculated. Nontransferability of nurses between hospital units was assumed. Population Studied: Analysis was limited to a convenience sample of nine hospitals. While not statistically representative, the sample group included hospitals of different types (community, teaching, state-owned, rehabilitation, and psychiatric) and from different regions within the state. Principal Findings: Analysis of unit staffing and utilization data suggested that the proposed mandatory ratios’ potential cost impact varied greatly by hospital type, and, to a lesser extent, by region. Boston-area community and teaching hospitals would have felt the least impact, while general hospitals outside of the Boston area would have been more strongly affected. Within the sample group, the one stateowned hospital and the two specialty hospitals (psychiatric and rehabilitation) would have incurred the highest costs. Serious deficiencies in currently available data limited our ability to estimate the overall impact of mandatory nursestaffing ratios on hospitals in Massachusetts. No centralized, statewide data repository on nurse staffing by unit is currently available, and the hospitals in our sample group could not provide unit-specific data for all units. Conclusions: Among the sample group of hospitals examined here, variation in actual staffing as compared with the proposed mandates suggests several points. First, because of the distinct models of care in rehabilitation and psychiatric hospitals, which rely heavily on other health care disciplines (such as physical therapists, mental health workers, or social workers) rather than nurses, these specialty hospitals are likely to encounter more serious financial impacts from mandatory ratio proposals than are general acute care hospitals. Psychiatric and rehabilitation units within general hospitals in the sample group faced similar effects. Second, public (stateowned) hospitals, which often have fewer resources than other sectors, may also face very high costs in meeting mandatory staffing ratios. Third, regional variations are important; urban and suburban general hospitals tend to be the most richly staffed. Finally, the lack of systematic, statewide nurse staffing data is a serious barrier to policy analysis of mandatory nursestaffing ratios. Implications for Policy, Delivery, or Practice: Proposals for regulating hospital nurse-staffing ratios should account for different models of care in certain facility types, such as specialty rehabilitation and psychiatric hospitals, and for other relevant hospital characteristics. Mandated nurse-staffing levels could disproportionately impact public hospitals as well. Policymakers and researchers should collaborate to improve data collection and analysis of hospital nurse staffing, as recent trends suggest this will be an area of intense scrutiny in the coming years. Primary Funding Source: Commonwealth Medicine/UMass Medical School ●State Level Changes in the Pharmacist Labor Market between 1990 and 2000 Surrey Walton, Ph.D., Glen Schumock, MBA, Pharm D, Katherine Knapp, Ph.D., Laura Miller, Ph.D. Presented By: Surrey Walton, Ph.D., Associate Professor, Pharmacy Adminstration, UIC, 833 S. Wood St (M/C 871) rm. 241, Chicago, IL 60612; Tel: (312) 413-2775; Fax: (312) 9960868; Email: Walton@uic.edu Research Objective: The purpose of this study was to examine long term changes in the US pharmacist labor market across states. There were four specific objectives: 1) to analyze in-state graduates, state level migration of pharmacists between 1995 and 2000, and changes in the number of pharmacists by state between 1990 and 2000; 2) to examine pharmacist migration patterns by age; 3) to measure long term changes in the wages of pharmacists, and variation in wages across states; and 4) to examine state level relationships between wages, migration, graduates, and changes in the number of pharmacists across states. Study Design: The majority of the analyses in this study were based on the 5% Public Use Microdata Samples (PUMS) from the 1990 US Census and the 2000 US Census. The 2000 PUMS data also contain information on where the individual lived in 1995 which was used to define migration. Various descriptive analyses were conducted to characterize state level differences in the number of pharmacists and sources of change in the number of pharmacists across states. Rates of migration across age for all pharmacists were examined. Descriptive statistics were also calculated for inflation adjusted wages of pharmacists relative to inflation adjusted wages of college educated workers in general. Population Studied: The PUMS data were used to examine pharmacists based on self reported occupation and also in some instances to examine the number of pharmacists or the level of pharmacist wages relative to the general population. To complement the census data, information on the number of graduates per state was also used. For wages, working pharmacists between the ages of 21 and 65 with at least a bachelor degree were used. Principal Findings: Consistent with past findings, there is substantial variance in the number of pharmacists and the number of pharmacists per 100,000 population across states according to the Census. Migration also varies significantly across states. New graduates and net in migration were negatively correlated after controlling for population. However, neither the number of graduates, nor net in migration were correlated significantly with the percent change in the resident number of pharmacists. Pharmacists are more likely to migrate at younger ages than the general population, but less likely at older ages. In addition, there were substantial increases in the wages of pharmacists relative to similarly educated workers between 1990 and 2000. Conclusions: As the country moves towards greater reliance on the use of medications to manage medical conditions, understanding of the market for pharmacists will continue to be important. The general variance seen across states in broad measures of supply remains unexplained, and detailed consistent data at the state level remains scarce. Further, changes in the number of pharmacists can come from a variety of sources. Hence, there needs to be increased efforts to measure and evaluate the labor market for pharmacists. Implications for Policy, Delivery, or Practice: The shortage has had a significant impact in terms of increased wages which suggests value in policies geared towards promoting increased supply. However, there remains wide variation in the number of pharmacists across states and wide variation in the patterns of migration and new graduates, the implications of which has yet to be evaluated. Clearly there is ample room for future research to better understand the underpinnings of the market and to examine policy decisions surrounding the pharmacist labor market. Primary Funding Source: HRSA, ●Relationship Between State Nurse Aide Training Requirements and Quality of Care Alan White, Ph.D., Donna Hurd, R.N. Presented By: Alan White, Ph.D., Senior Associate, Abt Associates, 55 Wheeler Street, Cambridge, MA 02138; Tel: (617) 349-2489; Email: alan_white@abtassoc.com Research Objective: Federal regulations require that training programs for nurse aides must be a minimum of 75 hours, including 16 hours of supervised clinical training. There is concern that this amount of training is insufficient for adequately training nurse aides and that clinical training should account for a higher proportion of total training time. More than half of the states have additional training requirements beyond the minimum federal training requirement. This research has two primary objectives: 1) To examine the relationship between state nurse aide training requirements and resident quality of care; 2) To examine how actual nurse aide training program length is related to state requirements. Study Design: A series of multivariate regression models were estimated to explore the relationship between state nurse aide training requirements and a subset of nursing home quality measures that are most directly related to the care provided by nurse aides. Independent variables also included information on facility staffing, payor mix, and other characteristics. Information on actual training program length is based on interviews with state officials and the limited amount of available data. Population Studied: The study included most nursing homes in the United States, excluding those with missing data. We used data from 2003. Principal Findings: We find a significant relationship between higher state training requirements and better performance on several resident outcome measures, including ADL decline, urinary tract infection, mobility decline, pressure ulcers, and indwelling catheter use. We found mixed evidence of a relationship between clinical training requirements and resident outcomes. Our review of nurse aide training programs in several states suggests that a substantial portion of training programs exceed the state minimum requirement, even for states that require more than the federal minimum number of hours. Conclusions: While state requirements are not necessarily reflective of the actual length of training programs in states, our findings are consistent with the hypothesis that increasing federal nurse aide training requirements can lead to improvements in resident outcomes. Our results provide empirical support for increasing nurse aide training requirements, although it is not possible to know whether the differences observed across states with different training requirements are actually due to differences in training requirements or other factors that may be correlated with these requirements. Implications for Policy, Delivery, or Practice: Since passage of the 1987 Nursing Home Reform Act, the average acuity level of nursing home residents has increased, but there have been no changes in the federal training requirements for nurse aides. Improving nurse aide training time may lead to improvements in the quality of care furnished by nurse aides, leading to better resident outcomes. The fact that, even in states that have only the 75-hour minimum, there are many programs that are longer reflects a belief among program coordinators that it is not possible to cover all of the required material in 75 hours. Primary Funding Source: CMS ●Factorial Validity of the Transformational, Transactional and Laissez-faire Leadership Constructs among Physician Executives Sudha Xirasagar, MBBS, Ph.D. Presented By: Sudha Xirasagar, MBBS, Ph.D., Research Assistant Professor, Health Services Policy and Management, University of South Carolina, Arnold School of Public Health, 800 Sumter St., Columbia, SC 29208; Tel: (803) 576-6093; Fax: (803) 777-1836; Email: sxirasagar@sc.edu Research Objective: To verify the factor structure and validity of transformational, transactional and laissez-faire leadership, and their sub-constructs, among physician executives Study Design: Exploratory factor analysis of cross-sectional data on leadership behaviors of physician executives as rated by their supervisors, using principal factor method to extract the factors, followed by promax rotation. An adapted version of Bass and Avolio’s Multifactor Leadership Questionnaire Form 5X-Short was used, with items measuring leadership behaviors (34 items) and effectiveness (9 items). Executive directors of community health centers judged how frequently each statement fit their medical director, on a 0-4 Likert scale (0=Not at all, 4=Frequently, if not always). Population Studied: A nation-wide anonymous mail survey of executive directors of all 663 community health centers (CHC) of the contiguous United States was conducted in fall 2002, yielding 269 respondents (response rate=40.9%). Executive directors responding to questions about their medical director’s leadership style formed the study sample. Their responses to the 34 leader behavior items were subjected to exploratory factor analysis. Principal Findings: The data support a 3-factor structure, with 21, 6, and 7 items, respectively, loading on the factors (=0.40), with simple structure. Based on the content of items, the factors were conceptually identified as transformational, transactional and laissez-faire leadership, closely similar to Bass and Avolio’s constructs. The data did not support the factorial independence of Bass and Avolio’s subscales of transformational leadership, (idealized influence, inspirational motivation, individualized consideration, and intellectual stimulation), and of transactional leadership, (contingent reward, management-by-exception active, and managementby-exception passive). Reliability coefficients for all subscales except management by exception passive ranged between 0.77 and 0.92. Anomalous loadings relative to Bass and Avolio’s three leadership factors included the following: a) two contingent reward items loaded on transformational leadership, b) one item of contingent reward showed suboptimal factor loadings (<0.40) but highest loading on transformational leadership, c) one item of idealized influence loaded on transactional leadership, and d) all items of management-by-exception passive loaded on laissez-faire (the latter being well documented in the literature). Likely reasons for the anomalous loadings are: a) Exclusion of two of Bass’s original survey items from this survey, b) Measurement error due to the (anomalously loading) items requesting supervisors’ perceptions about the leader’s interactions with subordinates, and c) Lack of construct distinction between management-by-exception passive and laissez faire among physicians, due to their (essentially) autonomous role functioning. Conclusions: This study empirically validates among physician executives, a 3-factor leadership model that closely approximates Bass and Avolio’s constructs of transformational, transactional and laissez-faire leadership. Implications for Policy, Delivery, or Practice: Factorial validity of the transformational-transactional leadership model, together with its predictive validity vis-a-vis objective measures of clinical leadership effectiveness (impacting the center’s clinical performance goals), documented in an earlier paper, strengthen the case for refining this leadership development model. New research studies should explore physician provider perceptions and responses to the subconstructs of transformational and transactional leadership, and variations in the salience of each sub-construct of transformational and transactional leadership among a) private versus public and non-profits, b) institutionallyemployed versus independent physicians, c) physicians versus non-physician subordinates, and d) physician executives versus non-physician managers and executives. Primary Funding Source: No Funding ●Evaluation of Nursing Responses to Technology Adoption in Home Health Agencies Brye Yant, Ph.D., M.P.H., Kathryn Dansky, Ph.D. Presented By: Brye Yant, Ph.D., M.P.H., Researcher, Philadelphia VA Medical Center, 3615 Chestnut St, Philadelphia, PA 19104; Tel: (215)573-9747; Email: byant@mail.med.upenn.edu Research Objective: The home health industry has been exploring its potential to monitor patients in an environment of shrinking financial and human resources by using telehealth. Using the Technology Acceptance Model, this study examines the relationship between technology adoption and the use of telehealth technology with home health agency nurse job satisfaction. Study Design: Primary data was collected in June 2003 and June 2004 by means of a questionnaire. Nurses were asked about their previous experience with computer systems, use of telehealth, length and intensity of use of the technology, perceived value and ease of use associated with telehealth, organizational support for telehealth, and job satisfaction. Nurses were divided into four telehealth adoption groups according to the existence and duration of telehealth adoption within their organization. Analysis of Variance tests were employed to examine differences in scores across time and between adoption groups at one point in time. Factor analysis was performed to examine ways in which telehealth was perceived by nurses. Separate regression analyses were then utilized to determine predictors of job satisfaction of nurses. Population Studied: A sample of 580 nurses in June 2003 and 629 nurses in June 2004 from 36 participating home health agencies in Pennsylvania. Principal Findings: Results indicated that job satisfaction levels were statistically similar among the adopters and non adopters of telehealth and most of the nurses surveyed were satisfied with their jobs. The results from this study provided some evidence to support the Technology Acceptance Model in forecasting the predictors of job satisfaction of nurses. Positive significant predictors of job satisfaction included previous nursing job satisfaction levels, user perception of organizational support for telehealth, and to a lesser extent the perception of telehealth as being useful. Telehealth intensity was found to be a negative predictor of job satisfaction. Computer experience, average hourly pay, patient case mix, and the ease of use for telehealth were shown to not significantly predict job satisfaction among nurses. Conclusions: As the nursing shortage continues, home health agencies must determine the optimal balance between maintaining a nursing workforce while producing the most sufficient level of nursing visits to uphold patient care and health. The findings of this study indicate that nurses were generally satisfied with their current job regardless of whether or not their organization adopted telehealth. However, results suggest that agencies choosing to adopt telehealth should pay careful attention to the implementation stages following adoption. Home health agencies must monitor not only how nurses perceive the technology and the extent to which the technology is being used as part of a nurse’s weekly activity, but it is important to also encourage managers to offer organizational support for the use of telehealth. Implications for Policy, Delivery, or Practice: Understanding the sources of nurses’ job satisfaction may help to solve recruitment and retention issues faced in the current and future nursing shortage. If telehealth becomes an accepted way of handling workforce and reimbursement issues, changes are likely to be needed regarding management training and expressed support for telehealth, nursing education, and monitoring the degree of its use in home health practices. Primary Funding Source: HRSA ●Satisfaction of US Radiologists: Findings from 2003 and comparison to 1995 Hanna Zafar, Jonathan H. Sunshine, Mythreyi Bhargavan, Rebecca S. Lewis Presented By: Hanna Zafar, University of Pennsylvania, Email: Hanna.Zafar@uphs.upenn.edu Research Objective: Professional satisfaction can affect not only work motivation but also career decisions, personal health, and relationships with others. The dynamic and sometimes unpredictable health care environment renders physicians, including radiologists, particularly susceptible to feelings of uncertainty and lowered professional satisfaction. Specifically, increasing concern over self referral, malpractice, and reimbursement have generated pressures within the field of radiology. This paper ascertains what characteristics of radiologists, their practices, and their work environment affect their professional satisfaction and explains changes in satisfaction since 1995. Study Design: Data comes from the American College of Radiology’s 2003 Survey of Radiologists, a nationallyrepresentative mail survey of radiologists in the United States with a 63% response rate. The five answer options to questions about level of current satisfaction with the radiology profession were scored +2 (very satisfied), +1 (somewhat satisfied), 0 (neither satisfied nor satisfied), -1 (somewhat dissatisfied), and -2 (very dissatisfied). A similar question was asked regarding the satisfaction compared to five years before the Survey. Univariate analysis and multiple regression analysis were performed examine the associations between the level of professional satisfaction and characteristics of the radiologists and the main practice they work in. Comparisons were made to the results of the 1995 Survey. Population Studied: Professionally active radiologists in the US. Principal Findings: Although over 90% of radiologists enjoy radiology “very much” or “somewhat,” there was a decrease in mean satisfaction of post-training, professionally-active radiologists from 1995 (1.62) to 2003 (1.47). Thirty two percent of radiologists reported enjoying radiology more than five years ago; 41% said they enjoyed it less. Excessive workload reduced current satisfaction and satisfaction relative to five years ago; working in the Midwest was associated with both. Subspecialty and practice type had more varied effects. In 2003, medico-legal climate, workload, and reimbursement / financial pressures were the three most common reasons for decreased satisfaction; in 1995, interference from managed care, government regulations / control / red tape, and increased administrative burden were most prominent. Lifestyle/workhours and income were the most prominent causes of increased satisfaction in 2003, but were also often mentioned as causes of decreased satisfaction. Conclusions: Other studies show that radiologists have higher levels of professional satisfaction than other physicians. However, as with physicians overall, their satisfaction has decreased over time. The decrease in current satisfaction between 1995 and 2003 continues a trend already seen for 1992-1995. The medico-legal environment, specifically the increasing cost of medical malpractice insurance and associated practice of defensive medicine have superseded concerns of a decade ago regarding managed care as the most prominent cause of decreased satisfaction. Implications for Policy, Delivery, or Practice: Further policy changes and reductions in radiology reimbursement seem to be coming. Given increasing concern over self referral, malpractice, and reimbursement and persistent levels of dissatisfaction, the percent of radiologists reporting dissatisfaction may continue to rise in the next few years. Mammography is by far the leading source of malpractice lawsuits against radiologists (a main source of dissatisfaction), and a relatively low-revenue activity within radiology. If fewer radiologists specialize in or interpret mammograms, this may affect breast imaging and/or exacerbate access problems. Primary Funding Source: No Funding ●Hospital Staffing Decisions: Does Financial Performance Matter? Mei Zhao, Ph.D., Gloria J. Bazzoli, Ph.D., Jan P. Clement, Ph.D., Richard C. Lindrooth, Ph.D., Askar Chukmaitov, Ph.D., Presented By: Mei Zhao, Ph.D., Assistant Professor, Public Health, University of North Florida, 4567 St. Johns Bluff Road, South, Jacksonville, FL 32224-2673; Tel: (904)620-1444; Fax: (904)620-1035; Email: mzhao@unf.edu Research Objective: Hospitals during the late 1990s experienced many pressures, which led to declining financial performance and efforts to shore up declining margins by reducing hospital workforces and associated labor costs. Given existing evidence on the relationship between quality of care and the level of hospital staffing, the objective of this paper is to assess how changes in hospital financial performance affected the size and composition of a hospital’s workforce. Study Design: A panel study design is applied to data from 1995-2000 to examine the effect of incremental change in hospital financial condition on staffing changes. Hospital total FTE intensity, RN FTE intensity, LPN FTE intensity, and RN/LPN skill mix were chosen as the staffing measures. The dynamic panel econometric model of Arellano and Bond (ReStud 1991) was used to examine these effects. Population Studied: All nonfederal short term general medical-surgical hospitals in operation between 1995 and 2000 were included in this study. Principal Findings: We found that there is a significant positive relationship between incremental change in financial condition (cash flow and operating margin) and incremental change in LPN FTE staffing intensity, after controlling for hospital and market characteristics, and unobserved hospitalspecific effects. However, the effects of financial change on total FTE and RN FTE staffing are inconclusive. Although the cash flow models suggest a significant positive relationship between cash flow changes and total FTE staffing intensity (marginally significant for RN FTE staffing intensity), the operating margin models do not find such an association. No significant relationship was detected between financial performance and RN still mix. Conclusions: The findings of this panel study are consistent with empirical studies and anecdotal reports about reductions in hospital staffing due to hospital financial deterioration. These findings also correspond to the previous study that the least profitable hospitals limited the growth of their staffs significantly below those of the most profitable group to constrain their growth in total costs. However, the findings suggest that hospitals do try to retain their core patient care workforce, namely RNs, even when confronted with financial difficulties. Implications for Policy, Delivery, or Practice: The major finding in this study—hospital financial performance is positively related to LPN staffing decisions -- has significant implications for hospital management. The reductions in LPN staffing means that RNs and other professionals are likely picking up the work that these lower skilled people previously did, which likely leads to nursing burn out and dissatisfaction. Therefore, a short-term financial fix for hospitals through LPN staffing reduction could lead to staff morale and nurse retention problems down the road. Thus, although reducing the number of nurses may cut costs in the short term, such a myopic approach may increase hospital costs in the long run. Primary Funding Source: AHRQ