Long-Term Care
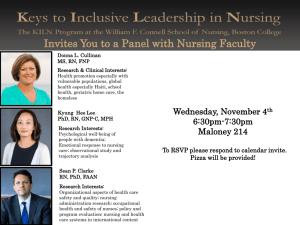
advertisement

Long-Term Care Call for Papers New Evidence on Innovative Approaches to Expanding Community-Based Long-Term Care Chair: Sally Stearns, University of North Carolina, Chapel Hill Sunday, June 25 • 5:45 pm – 7:15 pm ●An Evaluation of the Advanced Illness Management (AIM) Program: Increasing Hospice Utilization in the San Francisco Bay Area Elizabeth Ciemins, Ph.D., M.P.H., Brad Stuart, M.D., Rosemary Gerber, BSN, RN, Jeff Newman, M.D., M.P.H., Marjorie Bauman, BSN, MS, RN Presented By: Elizabeth Ciemins, Ph.D., M.P.H., Health Services Researcher, Institute for Research and Education, Sutter Health, 345 California Street, Suite 2000, San Francisco, CA 94104; Tel: (415) 296-1805; Fax: (415) 296-1844; Email: CieminE@sutterhealth.org Research Objective: In the Medicare population, chronic disease and end-of-life care is fragmented and hospice is underutilized. Evidence suggests that hospice care is associated with increased patient and family satisfaction and reductions in overall health care costs. Advanced Illness Management (AIM) is a home-based program established to ease the transition between curative and comfort care for chronically ill patients who lack coordinated hospital, home health and hospice care. Nursing and social work staff focus on symptom management, advance care planning, disease process education, treatment choices, and helping patients and families identify goals of care. The objective of this study was to measure the impact of the AIM program on the discharge disposition of participating home health patients. Study Design: Utilizing a retrospective cohort study design, univariate and multivariate analyses were conducted comparing intervention and usual care patients on the outcome variable of discharge disposition. Additional variables included in the analyses models were patient demographics, symptom status and length of stay. Population Studied: Patients who received home health services through the Sutter Visiting Nurse Association and Hospice at the Emeryville, California home health site and were discharged between March 2003 and August 2004 were included in this study. Participants were selected based on a prognosis of six months or less as determined by home health staff. Patients who received the AIM intervention were compared to those receiving usual home health care. Principal Findings: A nearly two-fold difference was observed in the number of hospice referrals between patients who received the AIM intervention and usual care patients (49% AIM; 25% UC, p<.0001). Among African American patients, a six-fold increase in hospice referrals was observed among AIM patients (49% AIM, 9% UC, p<.0001). These differences persisted after controlling for symptom status, patient demographics and length of stay. Conclusions: The AIM program was successful at increasing hospice utilization through a targeted intervention focused on palliative and end-of-life care, increased patient education and decision making, and a dynamic treatment approach. The finding of increased utilization by African Americans, a population traditionally reluctant to use hospice, was particularly impressive. Implications for Policy, Delivery, or Practice: The findings from this study provide the necessary preliminary evidence that could eventually affect Medicare reimbursement policy. An improvement in the transition from home health to hospice suggests that fewer patients will rely on costly emergency department and inpatient health care resulting from the lack of a successful care continuum. Because this application of home health services is not currently recognized as valid by Medicare, this demonstrated improvement in the coordination of end-of-life care may affect future Medicare reimbursement policymaking. Primary Funding Source: RWJF ●Community Integration Litigation As a Policy Lever Martin Kitchener, M.B.A., Ph.D., Micky Willmott, MA, Charlene Harrington, Ph.D. Presented By: Martin Kitchener, M.B.A., Ph.D., Associate Professor, Social and Behavioral Sciences, University of California, San Francisco, 3333 California Street, Suite 455, San Francisco, CA 94118; Tel: 415-502-7364; Fax: 415-476-6552; Email: Martin.Kitchener@ucsf.edu Research Objective: To anayze litigation brought to enable the aged and disabled to remain integrated in their communities by expanding Medicaid home and communitybased (HCBS) alternatives to institutional care. Study Design: The conceptual framework for this study differentiates among two forms of community integration litigation: (1) 'Olmstead' cases, brought or decided after the 1999 Olmstead Supreme Court ruling and citing either Olmstead or the 1990 American's with Disabilities Act (ADA). All other community integration cases are termed 'Medicaid HCBS'. A dataset of community-integration cases was assembled from a variety of on-line sources including legal databases (e.g., LexisNexis) and a literature search. Comparative features of the cases were coded and analyzed including: timing, location, status, and target group. Population Studied: Community integration lawsuits in all U.S. states, 1999-2004 Principal Findings: Fifty seven 'Olmstead' suits have been brought in 27 States with a peak of 19 in 2000. There is large inter-state variation in distribution with 5 in Washington, 4 suits in 4 states, 3 cases in 4 states, 2 suits in 6 states and 1 suit in 12 states. The most frequently represented target population in Olmstead suits is persons with MR/DD (44%). The majority of 'Medicaid HCBS' suits concerned waiting lists and again there was large inter-state variation with 14 cases in Pennsylvania alone Conclusions: Although community-integration lawsuits existed for at least a decade before 1999, after the Olmstead ruling they increased nationally but with large interstate variation. Implications for Policy, Delivery, or Practice: Frustrated by limited policy changes following the ADA and Olmstead ruling, consumers have used community integration litigation as a policy lever unevenly throughout the US. Further research is required to examine and compare the outcomes of suits and to explain inter-state variation in litigation patterns. Primary Funding Source: No Funding ●Primary Care Visits Reduce Hospital Utilization of Medicare Beneficiaries at the End Of Life Andrea Kronman, M.D., MSc, Karen M. Freund, M.D., M.P.H., Arlene Ash, Ph.D., Amresh Hanchate, Ph.D., Ezekiel Emanuel, M.D., Ph.D. Presented By: Andrea Kronman, M.D., MSc, fellow; clinical investigator, General Internal Medicine, Boston University Medical Center, 720 Harrison Ave, DOB 1108, Boston, MA 02118; Tel: 617-638-8188; Fax: 617-638-8026; Email: andrea.kronman@bmc.org Research Objective: To examine the relationship between primary care physician visits and subsequent hospital utilization at the end of life. Study Design: Retrospective analysis. Outcome measures were measured during the last 6 months of life: total hospital days, and presence of each of 4 types of potentially preventable hospital admissions (Ambulatory Care Sensitive Conditions, ACSC). Our predictor variable, number of primary care physician visits, and potential confounders were measured during the 12 preceding months. We used bivariate and multivariate analyses to identify and address county-level variations in healthcare utilization, and adjust for nursing home use, Medicaid receipt, comorbidity, and demographics. Population Studied: National sample of Medicare beneficiaries over 65 years of age who died in the second half of 2001; Blacks and Hispanics were over-sampled. Beneficiaries not in the fee-for-service Medicare parts A and B, and those in the End Stage Renal Disease Program were excluded. Principal Findings: Study sample (N=162,992) characteristics: mean age, 81 (range 66 - 98); female, 56%; White, 40%; Black 36%; Hispanic, 10%; Other, 14%. The number of primary care visits in the 6 - 18 months prior to death were inversely associated with total hospital days in the final 6 months of life (15 days for those with no primary care visits vs. 13.8 days for those with 6 - 8 visits vs. 12.8 for those with > 9 visits); the inverse association persisted after adjusting for all covariates (P < .001). Among those with an ACSC diagnosis, those with more preceding primary care visits were also less likely to be hospitalized for the respective ACSC: diabetes mellitus, congestive heart failure, and chronic obstructive pulmonary disease (ORs from .7 - .8, P < .001). Conclusions: More primary care visits in the preceding year are associated with fewer days in the hospital, and admissions for ACSC during the last 6 months of life. Implications for Policy, Delivery, or Practice: Increased primary care access to Medicare beneficiaries may decrease costs and improve quality of care at the end of life. Primary Funding Source: NRSA ●The Demand for Personal Assistance for Medicare Beneficiaries with Chronic Disability: Evidence from a Randomized Experiment Hongdao Meng, Ph.D., Andrew W. Dick, Ph.D. Presented By: Hongdao Meng, Ph.D., Assistant Professor, Preventive Medicine, State University of New York at Stony Brook, HSC, Level 3, Rm071, Stony Brook, NY 11794-8338; Tel: 631-444-7281; Fax: 631-444-3480; Email: hongdao.meng@stonybrook.edu Research Objective: To assess the effect of voucher on the demand for personal assistance among Medicare beneficiaries with chronic illness. To quantify the impact of financial subsidy on out-of-pocket expenditures for personal assistance. Study Design: This study used secondary data collected by a CMS demonstration entitled “A Randomized Controlled Trial of Primary and Consumer-Directed Care for People with Chronic Illnesses”. A reduced-form demand function was estimated to predict the annual expenditures on personal assistance among 609 individuals who participated in the control group and voucher group of the demonstration. I controlled for individual socio-demographic variables, health and functional status variables, prior use of medical care, and supply side variables. I specified a four-part model to account for characteristics of expenditure data and the characteristics of the voucher benefit (capped at $3000 annually). Population Studied: Older Medicare beneficiaries with chronic conditions. Principal Findings: The mean age of the sample was 81 and more than two-thirds were female. 58% participants have less than $20,000 annual household income. The mean ADL impairment score was 5.7 on a 0 to12 scale. 72% participants have 3 or more chronic conditions. 87.5% of the sample had non-zero out-of-pocket expenditure on personal assistance during a 12-month period. The average annual expenditure totaled $3626. The $250 monthly personal assistance voucher benefit increased the probability of using personal assistance and the amount of expenditure conditional on non-zero use. The elasticity of demand for personal assistance is estimated at -0.36. Conclusions: The results confirmed consumer demand theory in the demand for personal assistance. Voucher recipients who faced a lower effective price are more likely to use personal assistance and they also spend more conditional on any use. The price elasticity of demand for personal assistance is similar to the elasticity for dental care reported by the RAND Health Insurance Experiment. Implications for Policy, Delivery, or Practice: Voucher can be an effective mechanism to provide goods and services to chronically ill elderly who need personal assistance. The increased cost associated with voucher benefits can be justified if it is accompanied by better health and functional outcomes and/or satisfaction. Primary Funding Source: CMS ●Selection Bias and Utilization in the Minnesota Senior Health Options Demonstration Hui Zhang, Ph.D., Robert L. Kane, M.D. Presented By: Hui Zhang, Ph.D., Reporting Manager, CA EQRO, APS Healthcare, 560 J Street, Suite 390, Sacramento, CA 95814; Tel: 9162662575; Fax: 9162662542; Email: hzhang@apshealthcare.com Research Objective: Medicare and Medicaid dually eligible beneficiaries (DEBs) are among the frailest, most vulnerable and most costly populations in the United States. DEBs often are disadvantaged by the complicated Medicare and Medicaid programs and the fragmented care systems. The Minnesota Senior Health Options (MSHO) demonstration pools Medicare and Medicaid funding to managed care organizations to provide integrated, coordinated and flexible primary, acute, long term care and social services to DEBs. A prior evaluation of MSHO found the program was more effective in reducing inpatient hospital utilization, emergency room and physician visits for nursing home residents than for community residents compared with control groups during its first three years of operation. However, administrative data limitations, such as missing inpatient diagnosis and functional status, raise concerns about possible selection bias from those unobserved variables and their effects on the findings of the MSHO evaluation study. This study examined the existence and degree of selection bias in the MSHO evaluation study, its impacts on MSHO evaluation results, and the MSHO effects on utilization after adjusting for selection bias on unobservables. Study Design: This study uses a quasi-experimental study design like the MSHO evaluation study, comparing the MSHO nursing home and community enrollees with controls living in the same area, but applies different statistical and econometric models for panel and longitudinal data. Population Studied: The study sample is the dually eligible beneficiaries living in 4 counties of the Minneapolis-Saint Paul Twin Cities metropolitan area, whose eligibility status, frailty status and living arrangements are known between March 1997 and December 2000. The utilization data ran from January 1995 through December 2000. Principal Findings: The panel data models find minor favorable MSHO selection on unobserved chronic health status for the nursing home and community nursing home certifiable groups and minor adverse MSHO selection on unobserved chronic health status for the community nonnursing home certifiable group. The longitudinal data models find little significant selection bias on observed variables, and that the MSHO effects, which lowered some utilization measures, did not significantly increase with longer MSHO enrollment time during the MSHO evaluation period. Conclusions: Overall, the various models applied in this study do not find that selection bias on unobserved variables was important enough to change the general conclusions of the MSHO evaluation study. One possible reason for the lack of greater MSHO effects on utilization may be that the present MSHO care coordination is not sufficiently proactive in providing intensive care to the frail DEBs by incorporating innovative geriatric care models and effectively changing the behavior of the primary care physicians of DEBs. Implications for Policy, Delivery, or Practice: In addition to pooling Medicare and Medicaid payments to manager care organizations, more effective integrated chronic care models are especially needed in MSHO like programs for DEBs to maintain and improve the health status of the frailest dualeligible senior population in the nation. Primary Funding Source: No Funding Call for Papers Taking the Pulse of Nursing Homes in a Changing Policy Environment Chair: Christopher Murtaugh, Visiting Nurse Service of New York Tuesday, June 27 • 8:45 am – 10:15 am ●Trends in Cost and Service Intensity for Medicare Skilled Nursing Care in Freestanding, Hospital-Based and SwingBed Settings, 1997-2003 Kathleen Dalton, Ph.D., Jeongyoung Park Presented By: Kathleen Dalton, Ph.D., Senior Health Services Researcher, Health Care Finance & Payments, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709; Tel: (919) 451-5919; Fax: (919) 541-7384; Email: kdalton@rti.org Research Objective: Inpatient skilled nursing care for Medicare beneficiaries can be provided in skilled nursing facilities (SNFs) that are either freestanding or hospital-based, or in swing beds on acute-care units of small rural hospitals. Intensity of care has historically been highest in hospitalbased units and lowest in swing beds. To reduce incentives for unnecessary ancillary services, Medicare shifted from costbased to prospective (SNF-PPS) payments in certified SNFs beginning 1998. Swing-bed payments to PPS hospitals will come under SNF-PPS after 2003. This study examines per diem costs and intensity of services in each of three skilled nursing settings for the periods surrounding SNF-PPS implementation. It is part of a larger study examining variation in institutions’ strategic responses to Medicare payment incentives. Study Design: Descriptive analyses of retrospective observational data from Medicare nursing facility cost reports from 1997-2003, linked to certification and county data. Outcomes studied include Medicare payments and costs, including routine, rehab therapy, and non-therapy ancillary service per-diems. Median payments and costs are analyzed by type of setting, by ownership and by metropolitan status for all facilities and for the subset that remained open throughout the study period. Population Studied: All skilled nursing facilities filing Medicare cost reports 1996-2003. Principal Findings: In the first SNF-PPS year, freestanding per-diem costs dropped 27% from $283 to $206, declining 37% in therapy, 19% in non-therapy ancillaries and 4% in routine costs/day. Small but steady increases were seen in median costs in all subsequent years. Patterns were similar across ownership type and urban/rural location. In contrast, per-diem costs in hospital-based units were $461 in 1998 yet continued to increase by 3% per year over the following five years, even though payments were much lower. From 1997 to 2003 the number of hospital-based facilities declined by 43% in metropolitan and 20% in non-metropolitan areas. Yet among those that remained open there was no evidence of reduced intensity of care or extension of average stays. Swingbed services were not yet under PPS and costs increased rapidly from 1997 to 2003, with therapy per-diems growing by 10% per year and non-therapy ancillaries by 12% per year. By 2003, median total ancillary cost in swing beds was $211/day, compared to $170 in hospital-based and $104 in freestanding settings. Conclusions: Hospital-based SNFs appear to have responded to lower payments either by closing or absorbing losses, but not by changing care patterns. Freestanding SNFs responded by immediately reducing ancillary cost per/day to levels that assured good payment margins, even while they may have had to absorb more complex patients as a result of hospital-based closures. Median SNF-PPS payment margins remain positive in freestanding settings but negative for hospital-based settings except in very rural areas, where their costs are more similar to those found in freestanding SNFs. Swing-beds have gone from the least to the most intensive skilled nursing setting for ancillary costs/day. Some increased swing-bed costs might reflect changes in case-mix following hospitalbased closures, but by 2003 swing-bed ancillary per-diems were 80% higher than those in remaining rural hospital-based units. Primary Funding Source: HRSA medications considered potentially inappropriate for the elderly and other medications currently excluded from Medicare Part D Drug Benefit reimbursement, such as benzodiazepines and prescription vitamin and mineral products, were also administered to residents. Conclusions: Elderly nursing home residents take numerous medications for various medical conditions. The large number of medications taken per resident, many of whom are potentially very frail and sick, may raise patient safety concerns, such as drug interactions. The data also reveal that some residents took medications currently excluded from Medicare Part D reimbursement. Implications for Policy, Delivery, or Practice: Using the 2004 NNHS medication data, long-term care planners, researchers, and policy makers can gain a better understanding of the medications taken, therapeutic classes, the reasons they were prescribed, the prevalence of polypharmacy and potential interactions and thus implications for patient safety and quality of care. Current medication practices in U.S. nursing homes demonstrate that (1) patient safety initiatives are critical to monitoring the number and types of medications administered to residents and addressing their potential negative consequences and (2) the Medicare Part D Drug Benefit exclusions affect nursing home residents and the long-term care industry Primary Funding Source: CDC ●Medication Practices for the Elderly in U.S. Nursing Homes Lisa Dwyer, M.P.H., Robin E. Remsburg, Ph.D., R.N. ●Quality of Care for Veterans in Community Nursing Homes Christopher Johnson, Ph.D., Robert Weech-Maldonado, Ph.D., Charlie Jia, Ph.D., Dean Reker, Ph.D., Robert Buchanan, Ph.D., Alexandre Laberge, B.S. Presented By: Lisa Dwyer, M.P.H., Health Scientist, Longterm Care Statistics Branch, CDC, National Center for Health Statistics, 3311 Toledo Road, Hyattsville, MD 20782; Tel: 301458-4714; Fax: 301-458-4693; Email: ldwyer@cdc.gov Research Objective: (1) Present preliminary estimates of the use of medications by nursing home residents. (2) Determine the top ten therapeutic classes of medications taken by residents; and (3) Determine if nursing home residents are taking selected medications that are currently excluded from Medicare Part D Drug Benefit reimbursement. Study Design: Cross-sectional analysis of preliminary, unweighted data on medication usage by a sub-sample of nursing homes residents in the 2004 National Nursing Home Survey (NNHS). The specific survey questions were as follows: (1) what medications did the resident receive yesterday, including standing, routine, and as-needed medications; (2) what medications does the resident receive on a regularly scheduled basis but were not administered yesterday; (3) why were the medications prescribed; and (4) did the resident have any type of reaction to a drug or medication since admission or during the past 30 days. Population Studied: 11,885 nursing home residents, 65 or older, who were sampled in the 2004 National Nursing Home Survey (NNHS) and taking at least one medication. Principal Findings: Preliminary un-weighted data reveal the mean number of medications per resident was 9.0. Residents took prescription medications, over-the-counter medications, and vitamin/mineral and herbal supplements. The top ten therapeutic drug classes taken by these nursing home residents included vitamins/minerals, laxatives, analgesics, antidepressants, diuretics, and antipsychotics. Some Presented By: Christopher Johnson, Ph.D., Associate Professor, Health Policy and Management, TAMUS School of Rural Public Health, 3000 Briarcrest Drive, Suite 300, Bryan, TX 77802; Tel: 979-458-4165; Fax: 979-862-8371; Email: cejohnson@srph.tamhsc.edu Research Objective: This study examines the quality of care of nursing homes with Veterans Affairs (VA) per diem residents versus those without VA per diem residents. We hypothesize that because of VA oversight, nursing homes that serve per-diem veterans will maintain higher levels of multidimensional quality. Study Design: Data consist of the Online Survey Certification and Reporting (OSCAR) for 1999-2002. The dependent variables include 1) structural measures of quality (whether a facility met the Center for Medicare and Medicaid Services’ recommended staffing levels for certified nursing assistants (CNAs) and registered nurses (RNs)); 2) process measures of quality (number of residents that required tube feeding, new catheterization, and mobility restraints); and 3) outcome measures of quality (quality of care deficiencies, quality of life deficiencies, total deficiencies, actual harm citations, and number of new pressure sores). The independent variable consists of whether the facility has any veterans (when analyzing all facilities) or whether the facility has a high proportion of veterans (when analyzing VA per-diem facilities only). Control variables include size (beds), for-profit status, proportion of Medicaid and Medicare residents, chain affiliation, and proportion of residents that are bladder incontinent, bowel incontinent, and bedfast. Logistic regression or negative binomial regression is used to model the relationship between presence of VA per-diem residents and quality of nursing home care. Population Studied: Veterans whose care is being paid for by the Department of Veterans Affairs Community Nursing Home Program. Principal Findings: Facilities with any veterans were less likely to meet nurse (CNA/RN) staffing standards; more likely to have patients that require tube feeding, new catheterizations, and mobility restraints; and were more likely to have actual harm citations and new pressure sores, plus quality of care, quality of life, and total deficiencies, than facilities without veterans. However, among VA per diem facilities, those with higher proportions of VA residents were less likely to have patients with restraints or with new pressure sores or to have an actual harm citation. Conclusions: These results raise some initial concerns about the quality of care for veterans within community nursing homes under the VA per-diem program. However, additional VA oversight, as implied by a greater proportion of VA residents, may make a difference in terms of quality of care. Implications for Policy, Delivery, or Practice: Community nursing homes may be using veteran residents as "bed fillers". This implies that certain types of nursing homes may not be interested in participating in the VA community Nursing Home Program. Policymakers and VA management should carefully examine the implications of its nursing home qualification system because veteran care may be compromised. Primary Funding Source: VA ●Area Variation in Rehabilitation Use in Nursing Homes Wen-Chieh Lin, Ph.D., Gregory F. Petroski, Ph.D., David R. Mehr, M.D., MS, Steven C. Zweig, M.D., MSPH, Robert L. Kane, M.D. Presented By: Wen-Chieh Lin, Ph.D., Assistant Professor, Family and Community Medicine, University of MissouriColumbia, M226 Medical Sciences Building, Columbia, MO 65212; Tel: 573-884-2119; Fax: 573-884-6172; Email: linwe@missouri.edu Research Objective: To examine factors associated with the area variation in the proportion of residents using rehabilitation services during Medicare covered skilled nursing facility (SNF) stays. Study Design: Cross sectional comparison of the proportion of SNF stays in each state classified into rehabilitation Resource Utilization Groups (RUGs). Using logit regression on grouped data at the state level, the dependent variable was the log of the odds of the proportion in rehabilitation RUGs and the model produced weighted least square estimates, (STATA Reference manual) which is also known as minimum logit chi-square method. (G.S. Maddala, 1983) We considered the following supply, need, and population factors that are potentially associated with variation across states: the proportion of for-profit SNFs, the numbers of SNF beds and inpatient rehabilitation facility (IRF) beds per 1,000 elderly, the ratio of SNF use to IRF use in patients discharged from hospitals for major rehabilitative conditions, the proportion of people aged 65 and older, and the proportion of Medicare and Medicaid dually eligible elderly. Population Studied: Medicare covered SNF stays in calendar year 2000. RUG-III classification system is based on the federally mandated Minimum Data Set outcomes assessment in nursing homes. Rehabilitation RUGs include five levels of intensity (low, medium, high, very high, and ultra high). Principal Findings: At the national level in year 2000, 64.9% of SNF stays were classified into one of the five rehabilitation RUGs, but the proportions ranged from 40.7% in North Dakota to 73.5% in Michigan. The proportion of rehabilitation RUGs was negatively associated with the number of IRF beds per 1,000 elderly, the ratio of SNF use to IRF use, and the proportion of dually eligible elderly. For example, the odds of rehabilitation use in SNFs decreased 25% when the IRF beds per 1,000 elderly increased one unit. The adjusted R-square for the weighted least square logit estimation was 0.44. However, the predicted proportions of rehabilitation RUGs ranged from 51.4% in Louisiana to 74.3% in Arizona with a median of 64.3%. Conclusions: Evidence strongly suggests the potential substitution between SNF and IRF use: increased IRF bed supply was associated with reduced proportion of rehabilitation RUGs during SNF stays. Nevertheless, substantial state variation in the distribution of rehabilitation RUGs in SNFs remained after we controlled for supply, needs, and population characteristics at the state level in the model. Implications for Policy, Delivery, or Practice: Rehabilitation charges account for a quarter of Medicare SNF charges, and 6.1% of total Medicare program payment was for SNF stays ($11 billion) in 2000. Admitting patients to SNFs under rehabilitation RUGs is potentially financial advantageous for SNFs. However, outcomes from rehabilitation use are not clear, particularly considering that SNF residents consist of heterogeneous groups including residents needing restorative or rehabilitative care for community discharge, transiting through to continue or initiate long-term nursing home stays, and needing palliative care to bridge to Medicare hospice for end-of-life care. The large variation across states warrants further investigation on the appropriateness and outcomes of rehabilitation therapy in SNFs, with controlling for additional patient and facility characteristics. Primary Funding Source: AHRQ ●Nurses as Power Brokers: Changing Roles and Culture Change in Nursing Homes Dana Weinberg, Ph.D., Almas Dossa, M.P.H., MS, Susan Pfefferle, MEd, Ph.D., Rebekah Zincavage, MA Presented By: Dana Weinberg, Ph.D., Assistant Professor, Sociology, Queens College - CUNY, 65-30 Kissena Blvd., Flushing, NY 11367; Tel: (718)997-2915; Fax: (718)997-2820; Email: dana.weinberg@qc.cuny.edu Research Objective: Rather than focusing on long-term care residents’ medical care needs, the culture change model espouses resident-centered care. Integral to this model is empowerment of frontline direct care staff, particularly certified nursing assistants (CNAs). Nurses, who wield significant power under the medical model with its focus on nursing interventions and a hierarchy of nurses supervising CNAs, may resist adoption of culture change. As the bridge between management and frontline workers, nurses play a pivotal role in the success or failure of culture change as an everyday practice. We elucidate nurses’ role in facilitating or impeding greater involvement and power for CNAs in the delivery of care. We also examine the determinants of this role and implications for the CNA workforce and care quality. Study Design: This cross-sectional study, conducted as part of the Better Jobs Better Care Initiative, uses both qualitative and quantitative data from a sample of 36 units from 18 different nursing homes. Population Studied: We draw on 247 interviews with frontline staff, nurse supervisors and charge nurses, and nursing home administrators in high-end nursing homes in Massachusetts. We also use unit-based surveys of 255 certified nursing assistants, 90 nurses, and 148 residents and proxies. Principal Findings: We find considerable variation, both within units and between nursing homes, in nurses’ stance toward CNA empowerment. Nurses broker the culture change process, often independent of management’s position or wishes. Nurses may manipulate the culture change process, making it flourish in facilities where it is not supported by upper management or, alternatively, stifling it even in facilities where management and nurses themselves support culture change efforts. CNAs are more satisfied with their jobs and their ability to provide resident-centered care when their supervising nurses support their involvement and autonomy. Conclusions: Often overlooked, nurses’ buy-in to the culture change model is necessary but not sufficient to ensure successful adoption of culture change. Nurses’ reasons for opposing or supporting culture change extend beyond selfinterested protection of power and control in the nursing home. Additionally, we detect a discordance between nurses’ intentions to implement culture change and their actual practices; this discordance often reflects constraints related to regulations, time, training, and ability. Implications for Policy, Delivery, or Practice: Intentions and practices often do not match, in part due to lack of management savvy on the part of both administrators and nurses. In order to create true culture change in nursing homes, administrators must consider the role of nurses as middle managers. In order to successfully empower the entire nursing home workforce, administrators and supervisory nurses both require training in participatory management. Primary Funding Source: RWJF, Atlantic Philanthropies Related Posters Long-Term Care Poster Session A Sunday, June 25 • 2:00 pm – 3:30 pm ●Prevalence of Medication Problems in High-Risk, DuallyEligible Older Adults: Results from the Community-Based Medication Management Intervention Gretchen Alkema, M.S.W., Kathleen H. Wilber, Ph.D., Dennee Frey, Pharm.D. Presented By: Gretchen Alkema, M.S.W., Doctoral Candidate, Davis School of Gerontology, University of Southern California, 3715 McClintock Avenue, Los Angeles, CA 900890191; Tel: 213-740-9685; Email: alkema@usc.edu Research Objective: To identify the prevalence of medication problems in high-risk, dually-eligible, community-dwelling older adults participating in a Medicaid waiver care management program. Study Design: The Community-Based Medication Management Intervention, part of the Administration on Aging’s Evidence-Based Prevention Initiative, used evidence from a randomized controlled trial in home health (Meredith et al., 2002) to implement an interdisciplinary medication management intervention in a Medicaid waiver care management program. The study employed the Home Health Criteria protocols for four medication problem types: therapeutic duplication, cardiovascular problems, and psychotropic and NSAID use with risk factors. Using these protocols, subjects were screened for problems through consultant pharmacist review of medication lists and relevant clinical data. Population Studied: Sample included 615 older adults aged 65+ who were nursing home certifiable, dually-eligible, and community-dwelling, drawn from three Los Angeles-based sites of a California Medicaid-waiver care management program. Principal Findings: Results showed that those in the Medicaid waiver program had double the prevalence of any medication problem (39.5%) compared to home health (19%). Therapeutic duplication was 4 times greater, and inappropriate psychotropic and NSAID use were more than twice as prevalent. Over 13% of clients had 2+ medication problems; findings were consistent across sites. Conclusions: Consistent with the literature, this study corroborates an emergent concern that medication-related problems are highly prevalent in high-risk, communitydwelling, dually-eligible older adults. Implications for Policy, Delivery, or Practice: High prevalence and potential severity of medication problems among frail, dually-eligible elders demonstrate the need to improve medication management among health and social care providers. Given the implementation of the Medicare Modernization Act of 2003 that includes a drug benefit, effective interventions to improve medication management are imperative. Primary Funding Source: Administration on Aging ●Stability and Change in Community Care Networks Susan Allen, Ph.D., Julie Lima, M.P.H., Frances Goldscheider, Ph.D. Presented By: Susan Allen, Ph.D., Associate Professor, Community Health, Brown University, Box G-ST, Providence, RI 02912; Tel: (401) 863-3818; Fax: (401) 863-3489; Email: Susan_Allen@brown.edu Research Objective: Recognizing the importance of informal caregiving networks to maintaining the health status and community residence of elderly people with disabilities, the objective of this study is to examine stability and change in arrangements for care in a national sample of individuals age 70 and older who require help with activities of daily living, and to identify caregiver characteristics that predict the transfer of care to other caregivers or to an institution over a two year period. Study Design: Data used for this study were collected as part of the Longitudinal Study on Aging II. Three interviews were conducted at two year intervals, for a total of four years of panel data. Wave II data was utilized to enable us to capture prior caregiving history from Wave I data in multivariate analyses. Mulitnomial logistic regression was conducted to identify caregiver characteristics (gender, relationship to care recipient, caregiving history) associated with transitions to no care, to another informal caregiver, to a formal primary caregiver, and to institutionalization vs. stability in primary caregivers from Wave II to Wave III of the LSOA II. Characteristics of the patient are included as controls. Population Studied: The analytic sample consists of 1041 LSOA II respondents who reported difficulty in at least one daily living activity (ADL and/or IADL) at Wave II and who received help from at least one informal caregiver. Principal Findings: Preliminary regression results indicate substantial instability in informal caregiving networks with approximately 45% of sample members reporting transitions in care arrangements over a two year period. Respondents cared for by men at Time 2 were twice as likely as respondents cared for by women to have a new informal caregiver two years later, and three times more likely to be institutionalized. "Other" relatives (not children) and non-relatives were significantly more likely than spousal caregivers to transfer care to other informal relatives, and non-relatives were 10 times more likely to transfer care to a formal caregiver. Time 2 caregivers who had also provided care at Time 1 were less likely to transfer care to other caregivers at Time 3, while caregivers who had "inherited" the role from another Time 1 caregiver were twice as likely as caregivers of people who had no previous caregivers to transfer care to another informal caregiver or to an institution. The strongest predictor of transition to no care was improvement in physical functioning. Conclusions: Caregiving networks are clearly not static, and reflect the difficulty of meeting care needs over extended periods of time. It appears that some elderly people may experience a variety of caregiving arrangements as care needs escalate and/or caregiving resources are depleted. Male caregivers, and caregivers who are not related to the care recipient, represent key indicators of likely network instability. Further research is needed to determine whether network instability is associated with poorer health outcomes for the care receiver. Implications for Policy, Delivery, or Practice: The considerable instability in care arrangements observed in this study indicates the need to expand access to alternative care arrangements (e.g., day care, assisted living) to reduce the risk of nursing home placement. Primary Funding Source: NIA ●Empirical Analysis of Predictors of Falling in Nursing Home Residents Based on the MDS-2.0 Jenya Antonova, M.S., David Zimmerman, Ph.D. Presented By: Jenya Antonova, M.S., Research Assistant, Industrial and Systems Engineering, UW-Madison, CHSRA, 1175 WARF Bldg., 610 Walnut St., Madison, WI 53726; Tel: (608) 263-7455; Fax: (608) 263-4523; Email: jenya@chsra.wisc.edu Research Objective: To build and validate an empirical mixed effect model for identifying nursing home residents’ probability of falling based on non–aggregated items related to multiple health conditions included in the Minimum Data Set (MDS) 2.0. Study Design: Secondary analysis of the MDS 2.0 in II quarter of 2000 was performed. The MDS 2.0 was chosen because it provides mandatory, regular, and comprehensive nursing home residents’ health and care plan assessments. The assessments were voluntary provided by nursing homes in 2000. Hierarchical logistic regression with random slopes and intercepts was performed to model probability of a fall in a resident. Potential predictors were selected based on extensive literature review and ad hoc expert interviews. The model is currently validated based on year 2005 MDS-2.0; the results will be reported. Population Studied: 76429 residents admitted into 588 participating nursing homes in II quarter of year 2000, predominantly women (72%) with average age of 82 years (± 12.5). Principal Findings: Without any predictors included, the probability of falling in a resident was 0.39. After including predictors into the model, the probability of falling for a male resident younger than 70 without any investigated characteristics present, was 0.16. Women were less likely to fall (OR=0.88, CI: 0.84-0.94). Older age increased the odds of falling: for individuals 70-79 y.o. OR=1.64 (CI: 1.48, 1.81), 80-89 y.o. OR=2.01 (CI: 1.82, 2.23), and 90+ y.o. OR=2.36 (CI: 2.11, 2.64). Among other predictors the strongest effect on odds of fall was associated with traumatic brain injury (OR=1.74, CI: 1.15, 2.62), followed by: unstable status (OR=1.59, CI: 1.50, 1.68), medications initiated within past 90 days (OR=1.52, CI: 1.43, 1.62), syncope (fainting) (OR=1.44, CI: 1.02, 2.01), dizziness/vertigo (OR=1.40, CI: 1.20, 1.63), side vision problems (OR=1.35, CI: 1.19, 1.53), Alzheimer's disease (OR=1.34, CI: 1.24, 1.46), Parkinson's disease (OR=1.29, CI: 1.17, 1.42), urinary tract infection(OR=1.28, CI: 1.19, 1.38), balance unsteadiness (OR=1.27, CI: 1.23, 1.31), transient ischemic attack (OR=1.24, CI: 1.10, 1.38), dementia (OR=1.21, CI: 1.15, 1.28), seizure disorder (OR=1.15, CI: 1.04, 1.27), functional limitation in voluntary leg movement (OR=1.10, CI: 1.03, 1.18), and bowel incontinence (OR=1.08, CI: 1.06, 1.11). The number of taken medications did not increase odds of falling, but taking certain type of medications once a week, did: Antidepressants (OR=1.03, CI: 1.02, 1.04), Antipsychotic (OR=1.04, CI: 1.03, 1.05), Antianxiety (OR=1.02, CI: 1.01, 1.03). These odds ratios increased proportionally to the frequency of medication: taking these medications 7 days a week increased the corresponding odds ratios 7-fold. Conclusions: Numerous health conditions reflected in the MDS-2.0 are associated with increased risk of falling in nursing home residents. The MDS-2.0 can be utilized for assessment of probability of falling in nursing home residents. Implications for Policy, Delivery, or Practice: Utilization of the suggested model will help care providers identify nursing home residents with high probability of falling in order to utilize fall prevention strategies, which will improve quality of nursing home care and residents’ quality of life. As the result, it will help save resources that would be otherwise spend on treatment of negative consequences of falls. Primary Funding Source: No Funding ●Factors Influencing Staff Turnover in Long-Term Care Mark Atkin, MMedSci, BSc (Hons.), Pam Enderby, Ph.D., Dr S Davies, Ph.D. Presented By: Mark Atkin, MMedSci, BSc (Hons.), Project Manager, Institute of General Practice, University of Sheffield, Community Sciences, Northern General Hospital, Sheffield, S5 7AU; Tel: 00441142229882; Email: m.atkin@shef.ac.uk Research Objective: Throughout the UK and elsewhere, the high turnover of care staff working within long-term care remains to be an issue that results in implications for both costs and the quality of care provision. This study looks to define and establish interconnectivities between the various factors that contribute to high staff turnover within long-term care in order that new practices may be put in place to limit future staff turnover. Study Design: Initially, qualitative methodology was utilised to construct the key domains that constitute the multi-factorial concept of staff turnover. This information was then used to create an assessment tool that could be administered to a large number of long-term care facilities. To ascertain the effects of various corrective measures that may be taken in response to high staff turnover a randomised control intervention trial has been established within a care provider within the UK. Subsequently, quantitative techniques have been used to evaluate the intervention study. Population Studied: This study has been conducted in partnership with a provider from the UK independent care sector. In total, 106 long-term care facilities have been involved in the program, with the randomised intervention trial containing a total of 60 sites, and inputs from more than 800 care and nursing staff have contributed to the development of the study. Principal Findings: It is clear from our study, based on the opinions of several hundred care and nursing staff, that the importance of non-monetary rewards plays a huge part in determining the success of staff retention within long-term care facilities. Such findings have been incorporated into a conceptual framework that will be described, which proposes how the various factors relate to each in contributing to staff retention. Conclusions: By highlighting potential development gaps that may exist within long-term care facilities through use of a targeted assessment tool, it is possible to prioritise and implement new corrective practices that aim to limit future staff turnover. Implications for Policy, Delivery, or Practice: The assessment tool developed provides targeted information to management and administrators within long-term care on the key contributing factors to staff turnover. This then presents an opportunity to make adjustments to practices in order to optimise staff retention and therefore service delivery. Primary Funding Source: UK Knowledge Transfer Partnerships ●Hospice: From Grassroots Movement to National Industry – Have Services Changed? Melissa Carlson, Ph.D., M.B.A., R. Sean Morrison, M.D., Elizabeth H. Bradley, Ph.D. Presented By: Melissa Carlson, Ph.D., M.B.A., Assistant Professor, Geriatrics and Adult Development, Mount Sinai School of Medicine, One Gustave L. Levy Place, Box 1020, New York, NY 10029; Tel: (212) 241-8994; Fax: (212) 426-9108; Email: Melissa.Carlson@mssm.edu Research Objective: The Medicare Hospice Benefit was designed to meet the needs of patients and families with serious advanced illness. During the past decade, there has been dramatic growth in providers, users, and resources devoted to hospice care. Financial pressure has also increased due to declining hospice lengths of stay and increasing pharmaceutical costs; however, little is known about corresponding changes over time in service delivery within hospice. This study evaluates trends in the range and types of services received by hospice patients during the past decade and examines geographic and urban/rural variation in these trends. Study Design: Observational study. Population Studied: A nationally representative sample of 9,409 patients from 2,066 hospices in the National Home and Hospice Care Survey, 1992-2000. Data regarding patient demographics, clinical characteristics, and service use were obtained via interview with hospice staff and medical record review. Principal Findings: In 2000, only 22% of hospice patients received care across the multiple domains that hospice is intended to address (i.e., nursing care, physician care, medications, counseling, and caregiver support). However, marked variation in service delivery across providers existed. The overall range of services received by patients using hospice, adjusted for patient clinical and demographic characteristics, increased from 1992 to 2000 (Odds Ratio 1.16; 95% Confidence Interval 1.06-1.26). The largest percentage point (pp) increases occurred in medications (21 pp), spiritual care (20 pp), durable medical equipment and supplies (16 pp), and social services (12 pp), although the prevalence of medications (59% in 2000) and respite care (7% in 2000) remain low. Regional variation in the range of services delivered to patients was also observed. Conclusions: Service delivery in hospice has generally increased in scope and frequency over time. Yet the majority of hospice patients do not receive services across the basic domains of palliative care. Implications for Policy, Delivery, or Practice: Whether these findings are the result of inadequate Medicare Hospice per diem reimbursement rates or are related to other factors, is a subject for future research. Primary Funding Source: No Funding ●Skilled Nursing and Swing-Bed use in Rural Areas Following Major Payment Regulatory Changes Kathleen Dalton, Ph.D., Jeongyoung Park, Becky Slifkin, Ph.D. Presented By: Kathleen Dalton, Ph.D., Senior Health Services Researcher, Health Care Finance & Payments, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709; Tel: (919) 451-5919; Fax: (919) 541-7384; Email: kdalton@rti.org Research Objective: The supply and organization of postacute care is sensitive to changes in Medicare payment regulation. Between 1998 and 2003 a number of regulatory changes affected Medicare payments for skilled nursing and acute care, including a change from cost-based to prospective payments for nursing care affecting all skilled nursing facilities (SNFs), and a return from prospective to cost-based payments for acute and swing-bed care affecting nearly half of rural hospitals as they became Critical Access Hospitals (CAHs). Cost-based swing-bed payments can far exceed SNFPPS payments, and CAHs face additional incentives to close SNF units and expand swing-bed care in order to maximize hospital cost-based payments. This project tracks changes in availability and use of inpatient skilled nursing services in rural areas before and after these regulatory changes, and examines CAH participation in post-acute care before and after their conversion from PPS to CAH status. Study Design: : Retrospective, observational study combining data from CMS certification files through September 2004 with hospital and nursing facility cost reports from 1996-2003. Descriptive analyses are conducted by core-based statistical areas (CBSAs), supplemented by multivariate models of the probability of hospital-based SNF closure and of average swing-bed census as functions of size, location, CAH status, SNF case-mix and survey findings. Population Studied: All short-stay hospitals and Medicarecertified SNFs that were open between 1996 and 2003. Principal Findings: Contrary to expectation hospital-based SNFs have not closed more often in CAHs than in other rural hospitals, and swing bed use has grown only slightly faster in CAH settings than elsewhere. In the six years following 1998 implementation of SNF-PPS, 15% of hospital-based facilities in very rural counties closed compared to 26% in micropolitan rural and 43% in metropolitan. Only 8% of CAH converters that operated SNFs in 2000 had closed their units by end of 2004, compared with 19% of other rural hospitals with SNFs. The proportion of Medicare SNF days in swing-bed or hospital-based settings declined steadily in both rural and urban counties; Medicare skilled nursing days increased each year, but the increases occurred in newly certified freestanding SNF beds. Multivariate models found hospital-based unit closure was associated with for-profit ownership, higher Medicare utilization, higher wage-adjusted cost/day and lower average therapy case-mix. Closure was not significantly associated with CAH status, swing-bed participation or a history of survey deficiencies. Although large increases in swing-bed use occurred at a few CAHs, in regressions with multi-year data, average skilled swing census was not associated with CAH conversion. Conclusions: Introduction of SNF-PPS had less effect on supply and use of SNF services in rural than in urban areas. In both, an increasing proportion of Medicare skilled care is being delivered in freestanding facilities. Reintroduction of cost reimbursement to rural hospitals created strong reimbursement incentives to close non-cost-based units, but there is no evidence yet that CAHs are more likely to close their SNF units or substitute swing-bed for SNF care, nor that cost-based swing-bed care is crowding out care from rural SNFs that are under PPS. Primary Funding Source: HRSA ●Nursing Staff and the Outcomes of Nursing Home Stays Frederic Decker, Ph.D. Presented By: Frederic Decker, Ph.D., Social Scientist, LongTerm Care Statistics Branch, National Center for Health Statistics, CDC, 3311 Toledo Road, Room 3435, Hyattsville, MD 20782; Tel: (301) 458-4263; Fax: (301) 458-4693; Email: FDecker@cdc.gov Research Objective: Findings on the relationship between nurse staffing and nursing home outcomes (e.g., dying versus discharges to the community) have been inconsistent. Although some studies show outcomes are related to staffing ratios, many do not show a relationship. Studies showing a staffing effect have been on admission cohorts, and studies showing no effect have been on samples of current residents. Admissions cohorts are primarily short-stay residents and samples of current residents are primarily longer-stay residents. The purpose of this study was to discern if the effect of nursing staffing on discharge status, after controlling for other factors, varies between short and longer stays. Finding different staffing effects across short and longer stays would indicate inconsistent findings in research likely relates to differences in populations studied. Study Design: Models were constructed for short stays (less than 60 days) and longer stays (60 days or greater) applying multinomial logistic regression. Odds ratios were reported in models comparing outcomes such as dying and hospitalizations to the outcome of leaving the nursing home recovered or stabilized, assumed the most favorable outcome. Marginal effects were also calculated to show the change in mean probability of each discharge status occurring with changes in the values of independent variables. Population Studied: Data on discharges came from the 1999 National Nursing Home Survey (n=6,386). Principal Findings: For stays less than 60 days, but not among longer stays, the probability of leaving the nursing home in a recovered or stabilized condition increased, and that of dying decreased, as the staffing ratio of registered nurses (RNs) increased but was unrelated to the staffing ratios of licensed practical nurses and nursing assistants. One outcome, hospitalization, was affected by staffing in longer stays. A greater staffing level may reduce hospitalizations among longer stays but does not impact upon whether a longer-stay resident dies or is discharged recovered/stabilized. Clinical condition was the major risk factor in differentiating discharge status among both short and longer stays. Conclusions: Results indicate a likely reason for past inconsistent findings on staffing. Nurse staffing may affect the disposition at discharge the most for short stays. Research suggests short stays are primarily admissions for recuperative care with recovery the treatment objective. Longer stays more signify impaired function and limited community support where accommodation to impaired functioning is the focus of care. Thus, outcomes sought in and possible from treatment likely varies by duration of stay. One implication of the findings is that in studies on staffing and nursing home outcomes more consideration should be given to the relationship between the sample characteristics and outcomes investigated. Implications for Policy, Delivery, or Practice: The finding that discharge disposition is unrelated to staffing when the sample is long-stay residents does not mean staffing is unimportant. Other outcomes may be more directly related to the processes of care affected by staffing ratios related to caring for longer-stay residents. More research is needed on how, or whether, the sensitivity of outcomes—discharge status as well as other outcomes—to staffing ratios varies across short- and longer-stay residents. Primary Funding Source: No Funding ●Effects of Medicaid Policy on Long-Term Care Decisions and Medical Services Utilization Among the Low Income Elderly Song Gao, M.P.H., Ph.D. Candidate Presented By: Song Gao, M.P.H., Ph.D. Candidate, Economics & Public Health, State University of New York at Stony Brook, 700 Health Sciences Drive, E2072A, Stony Brook, NY 11790; Tel: 631-216-2262; Email: sgao@ic.sunysb.edu Research Objective: This study will provides evidence on long-term care decisions and health services utilization among lowincome senior citizens with respect to the largest meanstested program in the United States: the Medicaid program. Study Design: Nearly all senior citizens have health insurance coverage through Medicare, but those poor seniors with lowincome may also be eligible for the Medicaid program that can fill many gaps in Medicare coverage especially in longterm care coverage. This study is to test the impact of Medicaid coverage on long-term care decisions and medical services utilization. I will also explore the roles of health status, other health insurance plans, family structures using the panel structures of HRS (The Health and Retirement Study) data. My hypotheses are that Medicaid subsidies have positive effects on formal long-term care use and Medicaid take-up is influenced by health care needs and the availability of substitutes for long-term care. The objective is to assess target efficiency of the program. Often, we examine policy effects by comparing the policies before and after expansion. In my study, the data are after 1992 and after Medicaid policies have undergone reform. Given the lack of data to study take-up using structural program change, I will rely on variation in take-up among the homogeneous eligibles. Thus, I narrow my sample to those elderly people with sufficiently low-income to be eligible for the Medicaid program. Population Studied: This paper will use the panel data from HRS (Health and Retirement Study). Population in this study includes everyone aged over 65 in year 1992, 1994, 1996, 1998,2000, and 2002. Principal Findings: The Medicaid take-up rates were around 50%. Sicker people are more likely to participate in Medicaid program. Household memebers are substitutes of formal long-term care givers. Medicaid is the major force for low income people to use formal long-term care. Conclusions: Medicaid program has relatively higher participation rates compared with other welfare programs due to its health care benefits. Medicaid does assist poor elderly with their long-term care utilization. Implications for Policy, Delivery, or Practice: Around 50\% of those people took up Medicaid while the other 50% didn't. I examine the take-up decision in the context of their long-term care decisions and medical services utilization among those two comparison groups under different Medicaid coverage to test the Medicaid effects on their decisions. Therefore, I can evaluate the Medicaid program on the designed beneficiaries-the low-income elderly. This is a policy efficieny examination. Primary Funding Source: Health and Retirement Study ●The Relationship Between Paid Home Care and Informal Home Care among Older Adults with Functional Limitations Ezra Golberstein, B.A., Michael E. Chernew, Ph.D., Mohammed U. Kabeto, M.S., Kenneth M. Langa, M.D., Ph.D. Presented By: Ezra Golberstein, B.A., Doctoral Student, Health Management and Policy, University of Michigan School of Public Health, 109 Observatory, Ann Arbor, MI 48109; Tel: (734)936-5344; Fax: (734)764-4338; Email: egolber@umich.edu Research Objective: The research literature on the relationship between paid and unpaid home care is equivocal. Some studies find that the two forms of home care are substitutes, and some studies find that they are complements. This research takes two approaches to assess the extent to which paid home care substitutes for informal home care. Study Design: The primary approach estimates the relationship between state-level trends in paid home care and informal home care using weighted least squares regression. Separate equations are estimated for the intervals of 19931995, 1995-1998, and 1998-2000. Because of data limitations, our measure of informal home care only includes non-spousal care. Estimates of state level trends in both types of home care are derived from multivariate models that adjust the aggregate trends for changes in demographic variables, functional status, and health states. The secondary approach estimates the effect of exogenous policy-induced changes in paid home care on informal home care using instrumental variables analysis. Population Studied: Data come from the 1993, 1995, 1998, and 2000 waves of the HRS/AHEAD study, a nationally representative longitudinal study of older Americans who were not institutionalized at baseline. Due to the nature of the home care measures, individuals were included in a wave only if they had at least one ADL or IADL limitation in that wave. This yielded a sample of 3,311, 2,789, 2,550, and 2,800 in each respective wave. State-level identifiers were linked to individuals from the HRS/AHEAD limited use dataset. Principal Findings: The state-level analysis indicates a negative association between trends in paid home care and informal home care in all three intervals. In the 1993-1995 and 1998-2000 intervals, for every hour of increased paid home care we estimate a 0.7 hour reduction in informal home care (p<.05). This association is weaker and not statistically significant in the 1995-1998 interval. Preliminary findings from the individual-level instrumental variables analysis are consistent with these results, but less precise. Conclusions: There is some evidence for substitution between paid home care and informal home care. This suggests that increases in paid home care will be partially offset by reductions in informal home care. The benefits of publicly financed home care therefore accrue, in part, to caregivers. Implications for Policy, Delivery, or Practice: Public programs to provide home care to Americans with disabilities are likely to become increasingly controversial as financial pressures to limit care compete with increased demand for care arising from an aging population. Normative opinions about the amount of resources that are devoted to home care will depend, in part, on whether those resources are used to increase the amount of care given to individuals with disabilities versus to allow a respite for unpaid care givers. Both may be valued policy objectives, but it is unlikely they will be viewed as equivalent goals. This work, while unable to determine the optimal policy regarding public provision of paid home care, is relevant to policy makers because it helps illuminate the extent to which greater paid home care leads to more care versus less caregiver burden. Primary Funding Source: No Funding ●Federal and State Civil Money Penalties and Fines for Nursing Homes Charlene Harrington, Ph.D., Theodore Tsoukalas, Ph.D., Cynthia Rudder, Ph.D., Richard Mollot, Ph.D., Helen Carrillo, M.S. Presented By: charlene Harrington, Ph.D., Professor, Social & Behavioral Sciences, University of California, 3333 California Street Suite 455, San Francisco, CA 94118; Tel: 415-476-4030; Fax: 415-476-6552; Email: charlene.harrington@ucsf.edu Research Objective: The purpose of the study was to examine the variations in state nursing home regulatory practices related to issuing and collecting federal and state civil money penalties (CMPs) and fines. Study Design: First, the study described states’ use of federal and state CMPs and fines for nursing homes, whether states have a special fund from CMPs/fines, what funds are available, and how the funds from CMPs/fines have been used by the states, based on primary data from a survey of state officials and freedom of information requests. Second, the study examined factors related to the variation in collection of CMPs/fines by states, using regression analyses of federal and state CMP data. Population Studied: State licensing and certification programs responsible for federal and state CMPs/fines. Principal Findings: The findings showed that 41 states (including the District of Columbia) collected federal CMPs and 21 states collected state CMPs/ fines for a total of 3,057 CMPs/fines worth $21 million in 2004. Forty-six states had a fund account from CMPs/fines with $60 million available in 2005. Of the states with fund accounts from CMPs/fines, 32 states spent $28 million between 1999 and 2005 on a wide range of projects, although 8 states had not used any funds (6 states did not report). Information on the CMPs/fines collected, the fund balances, and the uses of funds are largely unavailable to policy makers and the public. Logistic regressions on whether states collected federal CMPs found that the positive predictors were: the percent of nonwhite population, the SSI/SSP participation rate per 1000 population, the percent of for-profit and chain-owned facilities, and nursing home beds per 1,000 population. Negative predictors of collecting federal CMPs were the number of complaints per nursing home bed, the percent of hospitalbased facilities, the percent of Medicaid nursing home residents, facility occupancy rate, and the certified home health agencies per 1,000 population. Panel regressions for the number of federal CMPs collected per 100 nursing home beds showed a positive relationship with: personal income per capita, facility occupancy rate, and survey and certification budget per nursing home beds in a state. Conclusions: Federal and state CMPs/fines are an important but seldom used intermediate sanction and wide variations in state policies and practices for using CMPs/fines continue to exist. States appear to take facility characteristics and provider supply into account in whether to issue CMPs/fines and in the number of CMPs/fines issued. Implications for Policy, Delivery, or Practice: Funds from federal and state CMPs/fines represent a sizeable resource available to state to use to improve quality of care. Greater attention is needed to develop standard policies and practices for states and to remove barriers to use of CMPs/fines in states. Primary Funding Source: CWF ●Creating Needs-based Tiered Models For Assisted Living Reimbursement Sandra Howell, Ph.D., Dorothy Gaboda, M.S.W., Ph.D., Nancy Scotto Rosato, M.A., Judith A. Lucas, R.N., Ed.D. Presented By: Sandra Howell, Ph.D., Sr. Policy Anyl/ Asst. Res. Prof, Center for State Health Policy, Rutgers University, 55 Commercial Ave, New Brunswick, NJ 08901; Tel: 732-932-4657; Fax: 732-932-0069; Email: showell@ifh.rutgers.edu Research Objective: This research provides state policy makers and others considering developing needs-based reimbursement models for Medicaid-funded assisted living (AL) an evaluation of how different needs-based methodologies (count, rule, and weighted) affect the models’ structures and outcomes. Models were developed with commonly accepted measures to show how using various scoring methods can discriminate cases into appropriate tiers or levels. Study Design: Univariate analyses detailed the sample’s characteristics and variables to be used in the models. Ordinary least squares regression analyses were used to evaluate each model’s ability to predict the time needed to care for individuals with varying types of needs (e.g., Activities of daily living [ADL], Dementia, Special Services.) The Adjusted Coefficient of Multiple Determination (Adjusted-R2) was used to compare the fit of alternative models Population Studied: Assessment data from Medicaidenrolled AL residents and waiver-eligible community individuals (n =726) were used to evaluate count, rule, and weighted methodologies in the design of five needs-based models. Principal Findings: New Jersey’s Medicaid-enrolled AL residents were generally similar demographically and functionally to a national AL resident profile. They required assistance with an average of 2.22 ADLs, were predominately female (72.3%), and widowed (55.6%). Approximately onethird were 76-85 years old, and another one-third was over 85. The test models ranged in fit from .127 to a high of .357 using the adjusted-R2 statistic. Conclusions: Count and weighted models both adequately predict service needs and discriminate individuals into their appropriate tiers. While simple count models are easiest to use and interpret, they neither adjust for severity of need nor provide a broad range of scores. Response options for ADL and IADL scales (independent vs. dependent or by degree of dependency) play a major role in determining whether functional need is captured. Thus, states should use caution in developing tiered reimbursement strategies based on a simple count of physical limitations or dependencies. Broader scaled scoring factors provide wider ranges of cumulative scores, recognize differences in each area of care’s level of need, and can accurately predict the amount of care required. Count models providing for degrees of impairment or performance offer the same ease of use, but are better able to account for impairment or performance variation. Since weighted models have greater score ranges than count models, they offer more flexibility in tier definition, account for severity. Implications for Policy, Delivery, or Practice: Generic tiered models developed with these methods can be tailored to a state’s population. States considering adopting a needs-based tiered model should refine their model based on their state’s resources, AL population characteristics, and the fit of these models their long-term care systems. For the industry, these models can identify levels of care needed in planning for staff time and skill-mix required for AL as well as other long-term care populations. Primary Funding Source: RWJF, CMS ●Hospital and other Palliative Services Used by Nursing Home Residents at End of Life with Cancer and Congestive Heart Failure Grace Johnston, Ph.D., Meaghan O'Brien, M.H.S.A., Dion Mouland, M.H.S.A., Jun Gao, M.Sc., Beverley Lawson, M.Sc., Ron Dewar, M.Sc. Presented By: Grace Johnston, Ph.D., Associate Professor, School of Health Services Administration, Dalhousie University, 5599 Fenwick Street, Halifax, Nova Scotia, B3H 1R2; Tel: (902)494-1309; Fax: (902)494-6849; Email: Grace.Johnston@Dal.Ca Research Objective: To understand services provided to nursing home (NH) residents at end of life with cancer and congestive heart failure (CHF) in Nova Scotia (NS), Canada. Study Design: For cancer studies, an algorithm was developed using death certificate to identify persons NH residents, and for CHF studies, place of family physician visits was used. Linked databases were vital statistics, physician billing and hospital admissions files for CHF. For cancer, vital statistics, Cancer Centre, Palliative Care Program (PCP), and census were linked. There is no province-wide electronic database of NH residents. Multivariate logistic regression analysis was used to identify likelihood and predictors of care. Population Studied: In Nova Scotia, approximately 10,000 adults died of cancer from 2000 to 2003; of these, 648 were NH residents. 2809 individuals died of CHF from 1998 to 2001 and a third were NH residents. Principal Findings: For persons with cancer, residing in a NH appeared to be an enabler of dying out of hospital (Odds Ratio [OR] 24.0, 95% Confidence Interval [CI] 18.6-30.9). Access to other palliative services varied with age and NH status. Of 2809 persons dying of CHF, 618 were longer-term NH residents, ie all physician visits in the last six months of life were in NH. In contrast, 1,886 persons dying of CHF dying had no NH physician visit, ie NH non-residents. 305 had both NH and office or home visits; these recent NH residents include persons admitted to NH in their last six months of life. NH residents were more likely to be female and older than other persons dying of CHF. Both longer-term and recent NH residents were more likely to die out-of-hospital of CHF (Longer-term OR= 2.67, CI: 2.08-3.45; Recent OR=3.85, CI: 2.80-5.29), to have fewer specialist visits and more family physician visits when compared to non-NH residents. Longer term, but not recent NH residents had significantly fewer hospital days in the last six months of life. Recent NH residents were more likely than non-NH residents and longer term NH residents to have spent more than a month in hospital in the last six months of life with CHF. Conclusions: Exploring end of life care the NH residents is viable using non-NH administrative data. In province wide studies, associations between age and end of life care should take NH status into account. There is a need to further explore the role and adequacy of NH care for persons dying of cancer. Implications for Policy, Delivery, or Practice: Since 50% of people diagnosed with cancer die of cancer, palliative care has been developed to a greater extent through the oncology and hospital based palliative care services; however, little is known about palliative cancer care for NH residents. CHF is progressive and eventually fatal with death typically at 80+ years. Palliative care is limited for persons with CHF. Given the aging baby boomers, and consequent needs for increased palliative care, linked administrative data can be used to plan and monitor end of life care provision. Primary Funding Source: Canadian Institutes for Health Research, and Heart and Stroke Foundation ●The Cost of Hospice Care: Are There Differences in Pateint Costs Across Diseases? Brad Killaly, Ph.D., Thomas C. Buchmueller, Ph.D., Paul J. Feldstein, Ph.D. Presented By: Brad Killaly, Ph.D., Assistant Professor, Strategy, Organization and Management, University of California - Irvine, 333 GSM - UC Irvine, Irvine, CA 92697-3125; Tel: 949-824-8782; Email: bkillaly@uci.edu Research Objective: End-of-life hospice care has grown considerably with the number of Medicare beneficiaries using hospice service tripling from 1992 to 2000. Access and quality of hospice care are crucial policy issues as most Americans are Medicare beneficiaries when they die. A cornerstone of the Medicare hospice benefit is that hospices receive a per-diem payment from Medicare for each beneficiary day. While the per-diem varies by location and is updated annually, it does not vary according to patient disease. There is growing qualitative research suggesting that hospice care costs vary by disease. If true, there are potentially adverse effects on access and quality of hospice care as providers seek to constrain costs by searching for lower cost patients. Our paper is the first to systematically measure and test cost differentials in hospice care across different diseases, in this case cancer versus non-cancer patients. Study Design: We use multivariate analysis to estimate a translog cost function of free-standing hospice unit variable costs using cancer and non-cancer patient days as outputs and include the Medicare wage index and local nursing wages as prices. The estimates are then used to construct marginal costs for cancer and non-cancer patients. Population Studied: We estimate our model on two populations. First we model costs within a large, multi-unit, multi-state, Medicare reimbursed for-profit hospice over 25 quarters. This setting is valuable as cost data are detailed and standardized across units, and are available as a complete multiple unit panel. Second we examine costs on a crosssection of free-standing hospices from the Healthcare Cost Report Information System Dataset over 1999-2003 (maximum of 1,396 hospices, 4,832 hospice-years). We combine the HCRIS cost data with aggregate disease volume data calculated from CMS’s Standard Analytical File to estimate the cost function. Principal Findings: We find that cancer patients are more costly than non-cancer. Our results reveal that the mean cancer patient marginal cost is $64/patient day and $54/patient day for non-cancer patients (at mean level of patient days). Further analysis indicates that over 80% of the cost difference is due to direct labor and prescription drug costs. Conclusions: Our results suggest that in the provision of hospice care in free-standing hospices that cancer patients are more costly than non-cancer patients. To our knowledge this study is the first large scale empirical investigation of this important issue. Implications for Policy, Delivery, or Practice: Our findings have important implications for policy and delivery. Systematic cost differences across two broad disease classes imply that adverse incentives may arise in hospice delivery and access under the Medicare system of fixed patient per-diem payments. If cancer patients are relatively more costly, then hospices face incentives that encourage search for lower cost (non-cancer) patients. Additionally, hospices with a greater proportion of cancer patients face relatively stronger incentives to substitute lower cost, possibly less skilled labor, which may adversely and differentially affect patient quality of care across diseases. In general, these findings suggest that the policy of disease agnostic fixed per-diem Medicare hospice payment should be reconsidered in favor of a disease based per-diem payment. Primary Funding Source: No Funding ●Medicaid Home and Community-Based Services: Trends in Programs and Policies Martin Kitchener, M.B.A., Ph.D., Terence Ng, MA, Charlene Harrington, Ph.D. Presented By: Martin Kitchener, MBA, Ph.D., Associate Professor, Social and Behavioral Sciences, University of California, San Francisco, 3333 California Street, Suite 455, San Francisco, CA 94118; Tel: 415-502-7364; Fax: 415-476-6552; Email: Martin.Kitchener@ucsf.edu Research Objective: To anlayse the most recent national trends in participants, expenditures and policies concerning the three main Medicaid home and communitybased(HCBS)programs: 1915(c)waivers,home health, and state plan personal care services(PCS) Study Design: Descriptive anlaysis of CMS Form 372 reports for all waivers (1992-2003)and authors' annual surveys of home health and PCS programs (1999-2003) Population Studied: Medicaid HCBS programs Principal Findings: While the participant and expenditure trend data show annual national increases through 2003 in each program except home health, growth rates are uneven across the states and in some cases slowing. Findings from surveys of cost control policies used on each program illustrate how states are increasing waiver waiting lists and imposing more stringent cost caps. Caps on spending and services provided are also used in almost half the state plan PCS programs and almost a third of all home health programs. Conclusions: Although total Medicaid HCBS spending and particiaption continue to rise, the increased use of cost control policies such as wait lists restrcits access in some states Implications for Policy, Delivery, or Practice: Targeted research is required to examine the outcomes of the inreased use of cost control polices on Medicaid HCBS programs. Primary Funding Source: Kaiser Family Foundation, NIDDR ●Urinary Incontinence: A Neglected Geriatric Syndrome in Nursing Facilities Larry Lawhorne, M.D., CMD, Joseph Ouslander, M.D., CMD, Patricia Parmelee, Ph.D., Barbara Resnick, Ph.D., CRNP, AMDA-F Research Network members Presented By: Larry Lawhorne, M.D., CMD, Assoc Prof of Family mMedicine, College of Human Medicine, MSU, B113 Clinical Center, East Lansing, MI 48824; Tel: (517) 353-0851; Fax: (517) 355-7700; Email: lawhorne@msu.edu Research Objective: The purpose of the present study is to identify resident-level and facility-level factors that foster costeffective, sustainable approaches to the recognition, assessment, and management of UI in the NF setting. Study Design: The resident-level pilot study provides participating Network facilities with a framework to facilitate implementation of the essential steps of the AMDA UI clinical practice guideline, then measures the following outcomes: percent residents with UI classified; percent residents with classification-specific UI care plan in place; number of episodes of incontinence, pressure ulcers and infections; resource utilization; quality of life; and resident, family, and CNA satisfaction. The facility-level study compares Network facilities that perform well on the UI intervention Quality Indicator with those that perform poorly with respect to the following characteristics and outcomes: ownership; residentdays; elements of UI policy and procedures; presence of UI process improvement team; availability of bladder scanner; performance on 9 or more medication Quality Indicators; OSCAR data on: percent dementia, percent foleys, percent dependencies, percent cholinesterase inhibitors, percent “bladder meds;” incontinence product costs; and staff turnover. Population Studied: Physicians, Geriatric Nurse Practitioners, Directors of Nurses, Nursing Assistants Principal Findings: Urinary incontinence (UI) is common but inadequately assessed and treated in nursing facility (NF) residents. Previous work by the American Medical Directors Association (AMDA) Foundation Long Term Care Research Network examined survey responses from 401 physicians (32% response rate), 118 Geriatric Nurse Practitioners (GNP) (23%), 152 Director of Nurses (DONs) (30%), and 277 Nursing Assistants (NAs) (60%) and determined that these 4 groups of health care workers have different views of the importance of UI compared to 5 other geriatric syndromes (behavioral symptoms, falls, unintended weight loss, pain, and delirium) as well as different perceptions about barriers to improving the assessment and management of UI. For example, nursing assistants are more likely to be involved in UI care and more likely to select UI as having an adverse effect on quality of life than physicians, GNPs or DONs. With respect to barriers to improved UI care, physicians see anticholinergic effects, particularly, cognitive function impairment, as the most important while GNPs cite inadequate implementation of behavioral interventions, and DONs and NAs see time constraints as the most important barrier. Conclusions: The Network’s previous work suggests that physicians, GNPs, and DONs are more likely to be involved in evaluating and managing behavioral symptoms, pain, falls, delirium, and unintended weight loss than UI in the NF setting. This leaves NAs as first-line managers for a condition that they (and probably residents) perceive to have an important impact on quality of life. Perceived barriers to improved UI care differ among physicians, GNPs, DONs, and NAs suggesting that approaches to overcoming the barriers should be multi-faceted. Implications for Policy, Delivery, or Practice: Findings from the current study of resident- and facility-level factors should provide guidance in the development of cost-effective, sustainable approaches to the recognition, assessment, and management of UI in the nursing facility setting. Primary Funding Source: Novartis ●Modeling Efficiency at the Process Level Robert Lee, Ph.D., Roma Lee Taunton, Ph.D., Byron Gajewski, Ph.D., Marge Bott, Ph.D. Presented By: Robert Lee, Ph.D., Associate Professor, Health Policy and Management, University of Kansas, 321 Thorn Street, Sewickley, PA 15143; Tel: 913-908-8202; Email: rlee2@kumc.edu Research Objective: This paper examines the efficiency of a single process: how nursing homes complete a standardized, mandatory assessment of residents. This is an important process that drives resource allocation for individual residents and the organization as a whole. One might expect that nursing homes would use similar processes for this assessment, but earlier studies demonstrated that this was not true. Study Design: The data collection process started with construction and validation of a process map for each facility. This identified the steps in the process for each nursing home and drove primary data collection. It is unlikely that data on any significant inputs into the production process are missing. Moreover, these data allow us to identify at which steps production is inefficient, not just which resources appear to be overused. These primary data were merged with survey and MDS data to allow quality and case mix controls. These data were augmented with data from Medicaid cost reports, the Minimum Data Set, and the Online Survey Certification and Reporting System. As a result, we have the data needed to conduct a variety of case mix-adjusted and quality-adjusted Data Envelopment and Stochastic Frontier Analyses. Population Studied: Care planning processes at a stratified random sample of 107 of nursing homes in two states. Principal Findings: Nursing homes varied widely in their efficiency. For example, three facilities with perfect quality scores that averaged 10 care plans per week used 5.6, 8.1, and 16.4 employee hours per plan, meaning that costs varied nearly three-fold. Put differently, the least efficient home wasted the services of more than two FTE employees. In addition, nearly 10% of the homes used more than 16.4 hours per plan and had citations for multiple care planning deficiencies. Preliminary analyses suggest that more efficient homes tended to have an assistant for the MDS nurse and have tightly structured, interdisciplinary care planning meetings. Conclusions: Quality and cost vary widely for the care planning process. Direct analysis of process efficiency is feasible. Implications for Policy, Delivery, or Practice: Inefficient processes result in high costs and low quality throughout health care. By showing that the “business case” for process improvement is compelling, this study extends and confirms earlier findings of widespread inefficiency. Because it controls for quality and validates process structures, this study directly engages Newhouse’s (1994) concerns that earlier studies may have omitted important inputs or ignored important sources of heterogeneity. The techniques developed in this study and its detailed findings are clearly applicable to other areas. The results imply that, whatever their objectives, managers should focus on improving their core processes and policy makers should take steps to facilitate this. Primary Funding Source: National Institute of Nursing Research ●Cost Driver Analysis for Dialysis: Lessons from Renal Clinics in Taiwan Shuen-Zen Liu, Ph.D., Chia-Ching Cho, Ph.D. candidate, James Romeis, Ph.D. Presented By: Shuen-Zen Liu, Ph.D., Professor, Accounting, National Taiwan University, Room 1009, Building II, College of Management, National Taiwan University, No. 1, Sec. 4, Roosevelt Rd. Taipei 106, Taiwan, Taipei, 106; Tel: 886-233661122; Fax: 886-2-23638038; Email: sliu@management.ntu.edu.tw Research Objective: Care for patients with End-Stage Renal Disease (ESRD) is an important issue of medical care. The prevalence and incidence of dialysis patients are rapidly increasing worldwide, so is the size of ESRD budget. The objective of our study is to analyze cost drivers for dialysis using administrative data obtained from a large renal clinic chain in Taiwan. Study Design: We use multiple linear regression analysis to examine factors that influence costs of dialysis in our study. In the analysis, we employ two different measures for dependent variables: total variable costs and total medical variable costs. Concerning the independent variables, we consider potential cost drivers such as patient characteristics (e.g., age, sex, and the existence of hepatitis B, diabetes, and hypertension), medical treatments (e.g., reusing artificial kidney, EPO), and clinic properties (e.g. location, affiliate of hospital, and shares held by the company). Population Studied: The data used in the study comes from internal administrative sources of a large renal clinic chain. The company is the leading provider of dialysis and related services in Asia. It owns or operates about sixty dialysis facilities across Asia, treating nearly four thousand patients. In our analysis, there are 1043 observations of dialysis treatments drawn from 15 dialysis facilities in Taiwan. All of these internal administrative data are from May, 2005; they are the most reliable data source available. Principal Findings: In the multiple linear regression, we find several interesting empirical results. First, male and younger patients consume more dialytic variable costs. Second, clinics located in larger cities use less total medical variable cost per patient. Third, the percentage of shares held by the company is positively associated with dialytic variable costs, indicating that agency problem might exist in renal clinics. Fourth, clinics affiliated with big hospitals are found to incur less variable costs but more total medical variable cost. Finally, we find that quality is positively related with dialytic variable costs. Conclusions: Our analysis indicates that treatment costs of dialysis are influenced by various medical and non-medical factors. The finding is crucial to cost control and performance evaluation for renal clinics. In addition, the positive association between medicare quality and dialytic variable costs indicate that we need to develop some payment scheme for maintaining quality. Implications for Policy, Delivery, or Practice: The Bureau of National Health Insurance (BNHI) in Taiwan has set a stable payment rate for hemodialysis procedures per time. However, we find dialytic variable costs are affected by multiple cost drivers. The results mean that the potential reimbursement distortion from using a single cost driver for allocating treatment costs of dialysis. From a healthcare policy perspective the findings are interesting for the authorities concerned to reconsider the simplistic payment policy. Furthermore, better understanding of the cost drivers can improve future management and potential merger & acquisition strategy for renal clinics. Primary Funding Source: No Funding ●Deteriorating Health Over Time and Its Effects on the Need for Institutional Care Hongji Liu, Ph.D., Hongji Liu, Rick Apodaca, Yuki Jao Presented By: Hongji Liu, Ph.D., Senior Study Director, Survey Operations, WESTAT, 1650 Research Boulevard, Rockville, MD 20850; Tel: 301-294-2055; Email: liuh1@westat.com Research Objective: Data from Medicare Current Beneficiaries Survey (MCBS) indicate that over 9 percent of Medicare beneficiaries (3.7 million) use institutional care. These beneficiaries are the high-cost users of health care services in the Medicare Program. This paper intends to investigate the effects of deteriorating health on the need for institutional care and to estimate subgroups’ rate of change in their institutional needs over 4 years. Specifically, it will: 1) compare the rates of deteriorating health among subgroups; and 2) examine subgroup differences in their rates of institutional care over time. Study Design: The paper uses data from CY1999 – CY 2002 MCBS Access to Care Public Use Files (PUFs). We follow the 1999 panel in MCBS for 4 years. We track the changes in their major health indicators by age subgroups, including prevalence of major diseases, functional limitations, and perceived health status. Then, we evaluate the changes in their need for institutional care with the lapse of time and identify the subpopulation with highest risks. Multivariate analyses are conducted to identify subgroups with most risk factors. Population Studied: Medicare beneficiaries Principal Findings: Preliminary results indicate health status changed at different rates for different age groups. Those aged 85 and over indicated fastest deterioration of health over 4 years. Approximately 10 percent of them reported a change from relatively healthy to poor health; and 14 percent were impacted by some kind of functional limitations. By the end of 4 years, one third of them reported poor health and over three quarters reported functional limitations. Interestingly enough, this subgroup does not show the highest rate of major diseases, including heart diseases, hypertension, cancer, and diabetes. The association between deteriorating health and need for institutional care can be seen from the increasing institutional rate for Medicare beneficiaries as they are aging. Those aged 85 and over group showed the highest rate of new institutional admissions (18 percent) over the 4 years, increasing from the initial 10.8 percent to 28.8 percent; followed by those aged 75-84 (4.4 percent), increasing from 2.9 percent to 7.3 percent. Those aged 65-74 showed the lowest institutional rate (from 1.3 percent in 1999 to 2.9 in 2002) and lowest cumulative rate of new admission (1.5 percent). Multivariate analyses indicate that functional limitation is the primary determinant of the need for institutional care. Conclusions: These findings confirm that health status is the key determinant of institutional care. For certain vulnerable subgroups with significantly higher rate of poor health, such as those aged 85 and over, and those with Medicaid, their need for institutional care is considerably greater. Implications for Policy, Delivery, or Practice: The aging of the population drives up the need for long term care. Institutional care is probably the most resource intensive type of long term care. The understanding of the association between the aging process and the need for institutional care is important in anticipating future health care needs among the Medicare population. Primary Funding Source: CMS ●Consumer Preferences in the Reporting of Long-term Care Satisfaction Data Judith Lucas, Ed.D., Timothy Lowe, Ph.D., Carrie Levin, Ph.D., Stephen Crystal, Ph.D Presented By: Judith Lucas, Ed.D., Rutgers, Division on Aging, 30 College Avenue, New Brunswick, NJ 08540; Tel: 732-932-6940; Email: jlucas@rci.rutgers.edu Research Objective: A few states have initiated reporting programs of Long-term Care (LTC) satisfaction survey results primarily to help consumers make informed choices among LTC providers and to promote quality improvement (QI) efforts. However, there is little information available about how satisfaction survey results should be reported. This study aims to describe family member preferences in reporting LTC satisfaction data and to compare these with the reporting preferences of facility administrators. Study Design: As part of the development and testing of resident and family satisfaction instruments in multiple state projects of nursing home (NH) and assisted living (AL) facilities, we surveyed (mail and telephone) both family members and facility administrators about their preferences in reporting satisfaction data for use in provider selection and QI efforts. We included the same core items about format, scoring, comparisons, and media presentation for all respondents. Population Studied: NH Family members (n= 380) and administrators (n= 142) and AL family members (n= 69) and administrators (n= 7). We defined family member broadly to include: any relative, the listed responsible party, or the legally appointed guardian or conservator. Principal Findings: Both NH and AL family members prefer to: see scores for each area of care and life (domain) and an overall scores vs. item scores; show satisfaction scores over a minimum of three years to see trends; and to be able to compare facilities within a county and by ranking (e.g., symbols or top 20%, mid 70% , bottom 10%); and over half feel confident using results published in booklet form or on a web page, yet they still wanted a toll-free number available for questions. Both NH and AL administrators prefer: to see overall satisfaction scores on the web, and domain scores and item scores (with range and means) on facility reports; facility reports using a percent score, symbols, and graphics; to view the current score and at least one past measure for internal QI efforts; comparisons by county, across peer groups (i.e., by size or ownership) and to the highest score in a domain; and they want to be able to view verbatim comments organized by domain and specific units for internal QI. Conclusions: Less detailed satisfaction reports in printed or web form that allow family members to make comparisons between facilities within a chosen county and over multiple measurement points, would appear to be useful for consumer LTC decisions, especially during time-pressured selection events. LTC administrators prefer more detailed data and comparisons with county scores and with similar facility types for QI. Implications for Policy, Delivery, or Practice: : LTC satisfaction measurement initiatives need to design LTC satisfaction reports for multiple users that provide options that allow comparisons between facilities (for consumers) and that allow users to seek more detailed information for QI efforts (for facilities). Primary Funding Source: Other ●The Same, Only Different: Influenza and Pneumococcal Immunization in Nursing Homes Jill Marsteller, Ph.D., MPP, Ronald Tiggle, Ph.D., Robin Remsburg, Ph.D., Abigail Shefer, M.D., Barbara Bardenheier, M.P.H., MA Presented By: Jill Marsteller, Ph.D., MPP, Assistant Professor, Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, 624 N. Broadway St., Room 433, Baltimore, MD 21205; Tel: 410-614-2602; Fax: 410-955-6959; Email: jmarstel@jhsph.edu Research Objective: Influenza and pneumococcal vaccines are often paired in statistical reporting and in immunization policy making. However, the two vaccines are administered on different schedules and immunization rates achieved thus far for the two vaccines are widely disparate. Thus the two immunizations may merit individual attention. This presentation will compare the determinants of receiving pneumococcal polysaccharide vaccine (PPV) with those of influenza immunization among elderly nursing home residents to inform immunization policy making. Study Design: A comparison of the results of two multinomial logistic regressions. The outcomes are recordbased staff report of whether nursing home residents 1) received influenza vaccination during the past 12 months (yes/no/unknown) or 2) had ever received pneumococcal immunization (yes/no/unknown). Variables tested included resident and facility characteristics and facility practices. Population Studied: A nationally representative sample of 7,350 nursing home residents >65 years old in 1,423 facilities from the 1999 National Nursing Home Survey. Principal Findings: Immunization coverage for influenza was much higher than for pneumococcal vaccine. Twenty-two percent of residents aged 65 and older had never received a pneumococcal immunization (SE=0.81%), and 39% had an unknown status (SE=1.04%). By contrast, only 15% (SE=0.60%) of residents had not received an influenza immunization in the previous 12 months, and 19% had unknown status (SE= 0.77%). Regression results indicated that the facility practices of recording immunizations in the patient’s medical chart and screening for immunizations upon admission had consistent positive effects across both vaccines. Also, for each type of vaccine, immunization with the one increased the likelihood of immunization with the other. Otherwise, the covariates of each type of immunization are different. Younger age and being newly admitted reduce the likelihood of receiving an influenza immunization, but are not related to receipt of PPV. The likelihood of PPV receipt is lower for blacks, residents in southern and western facilities and those in non-governmental homes, but these variables are not related to influenza immunization. Residence in a Medicaidonly certified facility raises the odds of influenza immunization but lowers odds of receiving PPV. Conclusions: Screening for immunizations upon admission and recording immunizations in the resident’s medical chart raise immunization rates for both vaccines. Failure to receive one immunization is associated with failure to receive the other. Implications for Policy, Delivery, or Practice: Facilities may do well to address PPV immunization during annual influenza immunization campaigns. In addition, differences in the covariates of the two immunization types may suggest exploring supplemental strategies tailored to each vaccine type, such as reviewing the records of young and newly admitted residents for influenza immunization but focusing on specific facility types for facility-wide PPV education. Differences between the two immunizations may suggest that reaching the same 90 percent Healthy People 2010 coverage goals within the same timeframe may be difficult. Primary Funding Source: No Funding ●Risk of Nursing Home Admission in Association with Mental Illness Edward Miller, Ph.D., M.P.A., Robert A. Rosenheck, M.D. Presented By: Edward Miller, Ph.D., M.P.A., Assistant Professor, Taubman Center for Public Policy, Brown University, 67 George Street, Box 1977, Providence, RI 029121977; Tel: 401-863-9311; Fax: 401-863-2452; Email: edward_a_miller@brown.edu Research Objective: To determine whether patients with mental health diagnoses in the Department of Veterans Affairs (VA) are more likely to be admitted to nursing homes, and to identify sociodemographic, utilization, and clinical characteristics, especially indicators of mental illness severity, associated with nursing home admission among mentally ill patients. Study Design: Patients receiving treatment in the VA system nationally during FY2000 and having no evidence of nursing home utilization during FY1999 or FY 2000 were followed through FY2003 using administrative claims data. Three-year incidence rates and unadjusted odds ratios were estimated for each diagnosis. Logistic regression was used to examine the correlates of admission among mentally patients, including analyses stratified by age. Population Studied: Patients receiving treatment in the VA system nationally with no previous evidence of nursing home utilization. Principal Findings: Of 3,952,229 VA patients with no prior nursing home use, 15.2% received a mental health diagnosis, of which, 4.6% were eventually admitted to a nursing home. Among mentally ill patients, risk of admission was highest for those with any inpatient medical/surgical days (odds ratio [OR]=2.28), followed by 3+ outpatient medical visits (OR=1.48), inpatient mental health days (OR=1.31), and outpatient mental health visits (OR=1.09). Patients diagnosed with dementia were 58 percent more likely to be admitted. Patients diagnosed schizophrenia (OR=1.26), other psychosis (OR=1.15), and personality disorder (OR=1.14) had the next highest probabilities. Elderly patients with bipolar disorder (OR=1.28) were also more likely to enter. Conclusions: Although factors leading to nursing home entry among the mentally ill are similar to those driving entry in the general population, those with more severe mental health problems are still more likely to be admitted. Implications for Policy, Delivery, or Practice: This study highlights the role of mental health care in preventing future institutionalization among veterans with certain psychiatric conditions. It also highlights the need for continued vigilance in assessing nursing home applicants for mental illness and for ensuring adequate provision of mental health services to those who eventually enter such facilities. Primary Funding Source: No Funding ●Nursing Home Community Discharge Rates are not Affected by Prospective Payment System Patrick Murray, M.D., MS, Randall Cebul, M.D., Charles Thomas, BS, Thomas Love, Ph.D., Neal Dawson, M.D. Presented By: Patrick Murray, M.D., MS, associate professor, Center for Health Care Research and Policy, Case Western Reserve University, 2500 MetroHealth Dr., Cleveland, OH 44118; Tel: 216-778-3901; Fax: 216-778-3945; Email: pkmurray@metrohealth.org Research Objective: Previous studies demonstrate that following the implementation of a prospective payment system for Medicare supported skilled nursing care there was a decline in the intensity of rehabilitation therapy provided, but an increase in the proportion of patients receiving rehabilitation following nursing home admission. The objective of this study is to examine how the changes in rehabilitation service provision affected community discharge rates. Study Design: A retrospective review was conducted of Minimum Data Set and Medicare Current Status Files before and after the implementation of the prospective payment system to ascertain receipt and intensity of rehabilitation services and community discharge within three months of admission. A logistic model of patient characteristics predictive of the likelihood of receiving rehabilitation was developed and validated in the pre-prospective payment sample and applied to the post-prospective payment sample. The two samples were divided into quintiles based on the individual predicted likelihood to receive rehabilitation services and into diagnostic groups. Community discharge rates were compared in the two time periods. Population Studied: First time admissions to free standing Ohio nursing homes during 1994-6 numbered 7006, and during 2000-1, 44,770. Principal Findings: Rehabilitation services were provided to 69 percent and 90 percent of new admissions in the preprospective payment and post-prospective payment period respectively. The intensity of therapy was 7.1 and 6.2 hours per week respectively. The overall community discharge rate was 49.3 percent in the pre-prospective payment period and 50.7 percent in the post-prospective payment period which was significantly different at the p = 0.03 level. Two quintiles, the first or least likely to receive therapy services and third, demonstrated statistically significant but relatively small declines in community discharge rates in the post-prospective payment period. The relative rate of community discharge was 0.79 with 95 percent confidence intervals from 0.72 to 0.88 in quintile 1 and 0.93 with 95 percent confidence intervals from 0.88 to 0.98 in quintile 3. In the fourth and fifth quintiles where the intensity of therapy declined, community discharge rates did not decline. Among patients with diabetes and significant cognitive deficits community discharge rates were higher in the post-prospective payment period. Conclusions: Despite an increased rate of rehabilitation services upon admission to nursing home there has been little change in community discharge rates. There has been no decline in community discharge rates among the groups who received lower intensity services in the post-prospective payment period. The increase in rehabilitation services in patients with medical reasons for admission appears to be associated with a modest increase in community discharge rates. Implications for Policy, Delivery, or Practice: The prospective payment system changes implemented in 1998 does not appear to have changed community discharge rates. While there may be benefits to expanded rehabilitation services if one examined other outcomes, e.g., activities of daily living, the selection of patients to receive rehabilitation in nursing homes deserves further study. Primary Funding Source: AHRQ ●Organizational Characteristics Associated with the Use of Computerized Medical Records in Healthcare Agencies providing Home Health Services in the US William S. Pearson, Ph.D., M.H.A., Anita R. Bercovitz, Ph.D., M.P.H. Presented By: William S. Pearson, Ph.D., M.H.A., Health Scientist, Long-term Care Statistics Branch, Centers for Disease Control and Prevention/National Center for Health Statistics, 3311 Toledo Road, Hyattsville, MD 20782; Tel: 301458-4699; Fax: 301-4584693; Email: wpearson@cdc.gov Research Objective: The objectives of this study are to estimate the extent of computerized medical record use among agencies providing home health services in the US and to determine organizational characteristics associated with their use. Study Design: Secondary analysis of the 2000 National Home Health and Hospice Care Survey. Population estimates were made for the numbers and types of agencies using computerized medical records. Significant associations between agency characteristics and use of a computerized medical record were determined by using chi-square analyses and adjusted logistic regressions. Population Studied: Nationally representative sample of 621 home health agencies and 312 mixed service (providing both home health and hospice services) agencies in the US, derived from the 2000 National Home Health and Hospice Care Survey (NHHCS). This sample represented 7,265 home health agencies and 1,766 mixed service agencies nationally. Principal Findings: Over 2,300 home health agencies reported using a computerized medical record in 2000. This represented 32% of health home agencies in the US at that time. Just over 700, (40%) of all mixed service agencies reported using a computerized medical record. Among all agencies that provided home health services, chi-square analyses suggested that the number of patients being served (p<.01) and the provision of skilled clinical (respiratory therapy, I.V. therapy, eterostomal therapy, dialysis, enteral nutrition) services (p<.01) were found to be significantly associated with CMR use. Among all agencies providing home health services, an adjusted logistic regression showed that number of patients being served and provision of skilled clinical services were significant predictors of using a CMR while controlling for group or chain membership, hospital ownership, number of services offered and geographic location of the agency. Agencies that served more than 100 patients were two and a half times more likely to be using a CMR compared to agencies serving 50 patients or less (2.55 O.R., 1.54-4.21 95% C.I.). Agencies that provided skilled clinical services were nearly three times as likely use a CMR than agencies that did not provide skilled clinical services (2.79 O.R., 1.51-5.19 95% C.I.). Conclusions: Number of patients being served and the ability to offer skilled clinical services are significant predictors of CMR use in agencies that provide home health services. These characteristics may be indicative of the agencies’ level of resources that can be devoted to increasing the quality of care by means of investing in newer technologies. Implications for Policy, Delivery, or Practice: The use of information technology, primarily in the form of electronic medical records, has been proposed as a way to increase the efficiency of delivered services, raise the level of the quality of care provided and decrease the number of medical errors. However in home health care, an area where CMR’s would be especially useful (e.g. coordination of multiple providers), fewer than 40% of agencies were using this technology. Further research should be conducted to determine the organizational characteristics that contribute to the adoption of CMR’s and whether the use of this technology is associated with quality and safety differences in patient outcomes. Primary Funding Source: CDC ●Electronic Information Systems Use for Patient Care in US Nursing Homes: Data from the 2004 National Nursing Home Survey William S. Pearson, Ph.D., M.H.A. Presented By: William S. Pearson, Ph.D., M.H.A., Health Scientist, Long-term Care Statistics Branch, CDC, National Center for Health Statistics, 3311 Toledo Road, Hyattsville, MD 20782; Tel: 301-458-4699; Fax: 301-458-4693; Email: wpearson@cdc.gov Research Objective: To estimate the number of US nursing homes using electronic information systems and to examine how these systems were used. Study Design: Cross-sectional analysis of the 2004 National Nursing Home Survey. National estimates were made for the numbers of homes using an electronic information system and the specific patient care activities they performed. These activities included management of patient records, management of medication orders and drug dispensing, physician order entry, laboratory orders and procedures, management of medication administration records, nursing assistant notes, and dietary notes. Population Studied: Nationally representative sample of 1,174 nursing homes from the 2004 National Nursing Home Survey, which represented 16,079 nursing homes nationally. Principal Findings: Almost one-half (47.2%) of the estimated 16,079 US nursing homes in 2004 were using an electronic information system for the management of patient records. 51.1% of all nursing homes were using an electronic system for medication orders and drug dispensing; 48.4% for physician order entry; 41.4% for laboratory orders and procedures, 38.1% for management of medication administration records, 17.5% for daily nursing assistant notes and 51.2% for dietary notes. Approximately 20% of all US nursing homes were not using an electronic information system for any of seven patient care activities. Seventeen percent were using their information system for at least one activity, and approximately 55% of nursing homes were using their information systems for 2 to 6 patient care activities. Just over seven percent of all homes were using their information system for all seven of the patient care activities. Conclusions: By 2004, many US nursing homes had adopted the use of an electronic information system for some type of patient care activity. However, the use of the information systems for patient care varied among the homes. Implications for Policy, Delivery, or Practice: This study presents data that allow researchers and policy makers to see where nursing homes stand at the beginning of our nation’s move toward a wired health information network. The use of information technology, primarily in the form of an electronic health record, has been proposed as a way to increase the efficiency of delivered services, raise the level of the quality care provided and decrease the number of medical errors. This study suggests that many nursing homes are using the technology for patient care services, although at varied levels. In 2004 Executive Order 1335 set forth a Federal Health IT initiative with the goal of having the majority of the US health care system wired and having most Americans covered by an interoperable health record within the next decade. Nursing homes are a large sector of the overall US healthcare system that provides care to an especially vulnerable population. Therefore, the use of electronic health records may help to ensure quality of care to this population. This survey will allow researchers to conduct studies on outcomes of patients that were treated in homes which utilized electronic information systems for patient care and will help to determine how the use of electronic information systems for patient care affect quality and outcomes. Primary Funding Source: CDC ●The Consistency of Transitions in Residential Living Settings in Medicare Beneficiaries during 1998 - 2001 Thomas Shaffer, M.H.S., Ilene Zuckerman, PharmD, Ph.D. Presented By: Thomas Shaffer, MHS, Research Analyst, The Peter Lamy Center on Drug Therapy and Aging, 515 W. Lombard, Baltimore, MD 21201; Tel: 410-706-2747; Email: tshaffer@rx.umaryland.edu Research Objective: To develop a typology of transitions in residential living and to quantify the degree and types of changes in living situations for the Medicare population both in cross-section and longitudinally. Study Design: Using monthly residence history constructed from survey and administrative data, we analyzed four annual cross-sections (1998-2001) and two longitudinal cohorts each who able to be followed for three years. Transitions were stratified by the number of transitions with a year. Residential settings used to identify and categorize transitions were Community, Skilled Nursing Facility (SNF), and Facility. Within the Facility setting, four specific types of institutional settings (Nursing Home, Assisted Living, Congregate Care Settings, and Miscellaneous –MRDD/Psych/Rehab) were further identified. Acute hospitalizations were not considered a change in residential setting. Population Studied: The study population comprised participants of the Medicare Current Beneficiary Survey (MCBS), a nationally representative sample of the Medicare insured population. Principal Findings: The proportions of individuals making transitions in residential setting were constant across 19982001. Approximately 93% experienced no changes in settings; 4% experienced a single change in residential setting; 2% had two changes, and 1% experienced more than two changes in a year. This was constant across four years despite a 33% infusion of newly sampled persons in each year due to survey sample design with a complete 100% replenishment of entire sample by 2001. Within common strata, changes of specific settings combinations were found across time. For example, within the 2-setting stratum the Community-to-Facility transition decreased from a relative proportion of 30% in 1998 to 15% during 2001. So while the overall proportion experiencing a transition remains constant, the relative proportions of specific combinations of transitions within a stratum changed. Longitudinal stability as measured by the number of transitions encountered across the three years also showed no statistically significant differences in stratified analyses. Conclusions: Transitions of residential living situations are remarkably constant over time and by the types of transitions made. Cross-sectionally, similar proportions of individuals experienced one, two, or more than two transitions per year. Longitudinally, similar progressions of the number of transitions across time were found. This suggests that although different individuals are involved in transitions, the numbers and types of residential transitions are essentially constant by individual year and across time. Implications for Policy, Delivery, or Practice: Transitions in living situations are stressful times for the individual involved and also mark potential sources of discontinuities in care. Understanding the patterns of transitions that can be developed from what appears to be a constant incidence in a large population can create a typology of transitions that can, in turn, be used to identify periods of risk and potentially minimize the consequences of discontinuity of care across residential settings. Primary Funding Source: No Funding ●Variations in “Comfort-Measures-Only” Status Designation Across Acute Care Hospitals and Implications for Assessing the Quality of End-of-Life Care Ying Tabak, Ph.D., Karen Derby, BA, Martha Hays, RHIT, Steve Kurtz, MS, Richard Johannes, M.D., MS Presented By: Ying Tabak, Ph.D., Director, Biostatistics, CTS Clinical Research, Cardinal Health, 500 Nikerson Road, Marlborough, MA 01752; Tel: 508-571-5120; Fax: 508-571-6101; Email: ying.tabak@cardinal.com Research Objective: With an expanding aged population, healthcare professionals face the challenge in providing “endof-life” care to dying patients. The “Comfort-Measures-Only” is designated by physicians to “relieve suffering”. It includes pain management, retaining dignity, and spiritual fulfillment. The clinical decision of “Comfort-Measures-Only” is complicated by patient/family preference, legal, ethical, and cultural factors. To date, little is known on how “ComfortMeasures-Only” is used across hospitals in spite of its importance in quality assessment, especially to end-of-life care. We sought to evaluate whether “Comfort-MeasuresOnly” designation is used uniformly across acute care hospitals. Study Design: We used retrospectively collected clinical data in the Cardinal Health Research Database to examine the distribution of “Comfort-Measures-Only” designated within 24 hours of admission, the in-hospital mortality for those with “Comfort-Measures-Only” status, and discharge destinations by disease groups and hospitals. We focused only on “Comfort-Measures-Only” designated early in the hospitalization because it is more likely related to the admission severity and less confounded with care process. Population Studied: We analyzed 86,100 admissions at 49 Pennsylvania hospitals (23 teaching, 26 non-teaching) in 20032004 with a principal diagnosis of ischemic stroke (n=10,378, 621 deaths), cerebral hemorrhage (n=2,223, 700 deaths), pneumonia (21,852, 806 deaths), respiratory failure (n=4,497, 1,045deaths), acute myocardial infarction (n=10,027, 1,015 deaths) heart failure (n=29,066, 989 deaths), and septicemia (8,057, 1,535 deaths). Principal Findings: Overall the rate of “Comfort-MeasuresOnly” designated within 24 hours was 1.3% for the study population. The “Comfort-Measures-Only” patients were significantly older compared to non-”Comfort-Measures-Only” patients (median age of 83 vs. 76, p < .0001). They were also sicker as indicated by significantly higher admission severity in acute physiologic presentation and severe chronic diseases (median predicted probability of death .29 vs. .03, p < .0001). At the hospital level, there was a wide range in “ComfortMeasures-Only” designation rates (0.23-19.6%), and “Comfort-Measures-Only” in-hospital mortality rates (14.388.9%). There was a general trend that hospitals with higher “Comfort-Measures-Only” rates had lower “ComfortMeasures-Only” in-hospital mortality. Compared to nonteaching hospitals, teaching hospitals had significantly lower “Comfort-Measures-Only” rates (1.0% vs. 1.9%, p <.0001) but higher “Comfort-Measures-Only” mortality rates (65.7% vs. 46.3%, p <.0001). For the 1152 patients with “ComfortMeasures-Only” designated within 24 hours of admission, 56% died in the hospital, 21% were discharged to a skilled nursing facility, 10% to home; 7% to hospice, and 5% to other destinations. For those who died in the hospital, the length of stay was significantly shorter than those discharged alive (average LOS of 2.2 days vs. 5.2 days, p <.0001). Conclusions: There is a wide variation in “Comfort-MeasuresOnly” designation rates and “Comfort-Measures-Only” mortality rates across hospitals. Hospitals with higher “Comfort-Measures-Only” designation rates tended to have lower “Comfort-Measures-Only” mortality. Implications for Policy, Delivery, or Practice: Our findings of large variation in “Comfort-Measures-Only” utilization across hospitals highlight the need for open discussions on whether there should be a uniform definition and application of “Comfort-Measures-Only” status in the acute care settings. Further research on extended mortality (e.g. 30 day mortality) and a survey of patients/families regarding their experience can be potentially beneficial in assessing the quality and appropriateness of “end-of-life care” in general and “ComfortMeasures-Only” designation in particular. Primary Funding Source: No Funding ●Barriers to Medical Care in Community-Dwelling Elderly With Dementia: The Role of Informal Caregiver Life Satisfaction Joshua Thorpe, Ph.D., M.P.H., Courtney Van Houtven, Ph.D., Betsy Sleath, Ph.D., Carolyn Thorpe, M.P.H., Elizabeth Clipp, Ph.D. Presented By: Joshua Thorpe, Ph.D., M.P.H., Assistant Research Professor, Duke University School of Nursing, Trent Drive, DUMC 3322, Durham, NC 27710; Tel: (919) 684-0395; Fax: (919) 681-8899; Email: joshua.thorpe@duke.edu Research Objective: An estimated 50-70% of dementia patients reside in the community, where the majority of care is provided by informal caregivers. Dementia patients often rely on informal caregivers to act as “access to care” agents on their behalf. The negative toll of caregiving on caregiver emotional health and life satisfaction is well-documented, but little is known about how this impacts the caregiver’s ability to facilitate medical care for the care-recipient. The primary aim of this study was to assess whether caregiver life satisfaction influences access to outpatient care in community-dwelling elderly with dementia. Study Design: VA outpatient utilization was linked to data from the 1998 National Longitudinal Caregiver Survey. The sample consisted of 1,264 community-dwelling older male veterans with dementia, and their co-residing female caregivers. Independent variables, collected in early 1998, were used to predict VA outpatient utilization over a 12 month period. The dependent variable, care-recipient outpatient utilization, was classified as (1) primary care, (2) specialty care, and (3) mental health, using clinic stop codes. We dichotomized utilization as any versus none. Our primary independent variable was caregiver satisfaction with life as measured by their response to the question, “Taking all things together, how would you say you find life these days?” The three response categories were: Not Satisfying, Fairly Satisfying, and Very Satisfying. The selection of other independent variables was guided by the Andersen behavioral model of health service use (BMHSU). Predisposing variables included caregiver (CG) age, CG education, care-recipient (CR) race, CG relationship to CR, and CR age. Enabling variables included CG income, CR insurance, CG physical health, assistance from secondary caregivers, distance to nearest VA facility, and region of country. Care-recipient need variables included ADLs and IADLs, behavioral disturbance, duration of symptoms, and comordid conditions. Multivariable logistic regression estimated the association between caregiver life satisfaction and care-recipient outpatient care use, adjusting for BMHSU variables. Population Studied: 1,264 community-dwelling male veterans with dementia and their co-residing informal caregivers. Veterans less than 65 years of age, those with no VA outpatient visits in the previous year, and those who died or entered a nursing home anytime during the 12 month period were excluded. Principal Findings: For primary and specialty care, results support our hypothesis that greater caregiver life satisfaction was associated with increased access. Compared to carerecipients with caregivers who found life “very satisfying,” the odds of care-recipient receipt of primary care were lower when the caregiver was unsatisfied (OR: 0.38; 95% CI: 0.23, 0.65). The adjusted percentage point difference was 10%, (92% for very satisfied, 82% for unsatisfied). A similar pattern was found for specialty care (OR: 0.67; 95% CI: 0.47, 0.96). The adjusted percentage point difference was 9% (66% for very satisfied, 57% for unsatisfied). Conclusions: We found that lower informal caregiver life satisfaction was significantly associated with decreased access to primary and specialty care in community-dwelling elderly with dementia. Implications for Policy, Delivery, or Practice: Interventions to improve caregiver’s quality of life may also improve their ability to facilitate medical care for their care-recipient. Primary Funding Source: AHRQ, VA HSR&D ●Depression and Missed Work among Informal Caregivers of Older Individuals with Dementia Courtney Van Houtven, Ph.D., Michele Wilson, MSPH, Sally C Stearns, Ph.D., Elizabeth C Clipp, Ph.D. RN Presented By: Courtney Van Houtven, Ph.D., Health Economist, Durham VA and Duke, HSR&D, General Internal Medicine, 508 Fulton Street, Durham, NC 27705; Tel: (919)286-6936; Fax: (919)416-5836; Email: courtney.vanhoutven@duke.edu Research Objective: Providing informal care can negatively affect caregiver emotional health and lead to depression, yet the association between caregiver depression and missed work is unknown. Our objective is to examine the relationship between caregiver depression and missed work among working informal caregivers for older veterans with Alzheimer's disease or vascular dementia. Study Design: We use observational data from the National Longitudinal Caregiver Survey to examine the relationship between caregiver depression and missed work among informal caregivers. Two-part models were used to estimate the expected hours of work missed among working caregivers. Depression was estimated using a modified form of the Center for Epidemiologic Studies of Depression score, or CESD score, a validated measure of depression. Modifications were to collapse responses to a yes or no format. Population Studied: The full sample in the National Longitudinal Caregiver Survey consisted of 2,268 communitydwelling older male veterans with dementia and their coresiding female caregivers. Working caregivers, totaling 453, were identified for this study. Most working caregivers were female, 90 percent, 80 percent were white, 17 percent were black, and 3 percent were Latino. Average household income was $36,000. Principal Findings: Over half of working caregivers report missing work in the past 30 days due to their caregiving responsibilities. Mean C-ESD scores were 6 (9 or over indicates depression). Among those who missed any, they missed 7 hours on average. Caregiver depression is significantly associated with both the likelihood of missing work and the amount of time missed at work. A one-unit increase in CES-D score was associated with a 1.84 percentage point increase in probability of missing any work, and a 4.6 percent increase in time missed among those who missed any work. Working caregivers with depression were expected to have an average of an extra half day of work missed per month compared to those without depression. Other important factors, such as having higher income, being a female caregiver, and having relatively intense caregiving responsibilities, also were associated with missed work. Conclusions: The finding on depression supports our hypothesis that depression would be positively associated with missed work. Making assumptions about average hourly wages from the sample’s salary information, our findings represent an average cost to employers of $792 annually for a dementia caregiver without depression who becomes depressed. This calculation does not consider concerns about causality, or the availability of vacation or sick leave to protect against a caregiver’s income losses. Implications for Policy, Delivery, or Practice: From a policy perspective, the relationship between caregiver depression and missed time at work due to caregiving responsibilities is important because missing work results in physical and financial costs to the individual caregivers, to the care recipients in the form of reduced quality of care, to employers in terms of lost productivity, and to overall welfare in society. If the full costs to society were sufficiently high, it would be important for policymakers to consider an intervention strategy targeted at identifying depressed caregivers and providing treatment to minimize depression and consequently the amount of work time missed. First, however, further exploration of this topic is needed, including establishing causality. Primary Funding Source: VA ●Informal Care and Medicare Expenditures Courtney Van Houtven, Ph.D., Edward C Norton, Ph.D. Presented By: Courtney Van Houtven, Ph.D., Health Economist, HSR&D and General Internal Medicine, Durham VAMC and Duke, 508 Fulton Street, Durham, NC 27705; Tel: (919)286-6936; Fax: (919)416-5836; Email: courtney.vanhoutven@duke.edu Research Objective: To measure the effect of informal care provided by adult children on Medicare expenditures of their single elderly parents. Secondarily, to examine whether the effect differs by the source of informal care such as sons versus daughters, children versus others, or whether the effect is smaller for a sample including married parents. Study Design: Two-part expenditures models are used to model Medicare home health care expenditures, skilled nursing expenditures, and inpatient expenditures. We control for endogeneity using instrumental variables probit estimation and two-stage least squares. Characteristics of the children in the family are used as identifying instruments: number of daughters, sons, and children with less than a high school education. We also estimate latent average treatment effects by running simulations on instrument characteristics. Population Studied: The data set consisted of information from the Standard Analytic Files of Medicare Claims and 1994/95 waves of the Asset and Health Dynamics Among the Oldest-Old Panel Survey, AHEAD, a nationally representative sample of non-institutionalized persons over age 70 in the United States. We examine the subset of elderly respondents from the HRS/AHEAD survey who provided their Medicare number to HRS interviewers. The sample consists of 3249 single parent-waves and 8182 married and single parentwaves. Principal Findings: Informal care is a net substitute for Medicare long-term care expenditures, significantly reducing the likelihood of having any home health expenditures, and any skilled nursing home expenditures. Informal care is also a net substitute to inpatient care, reducing amount of Medicare expenditures for inpatient care. Conclusions: Informal care is an effective substitute for Medicare long-term care, even highly skilled care such as skilled nursing. Informal care results in no change in the likelihood of having any inpatient expenditures but reduces the total amount among users, perhaps because patients can be discharged to their homes faster. Number of daughters and number of adult children with less than a high school education significantly increase provision of informal care. Implications for Policy, Delivery, or Practice: The cost to the public purse of policies that support caregivers, such as tax credits, may be offset by the Medicare savings that informal care provides. Given that family structure is an important factor in the provision of informal care for the elderly, policy makers should consider the differential influence of having daughters and low educational attainment when designing policies to support caregivers. Primary Funding Source: NIH, National Institute on Aging ●Cost and Quality: Evidence from Ontario Long Term Care Walter Wodchis, Ph.D., Geoff Anderson, Ph.D., Gary Teare, Ph.D. Presented By: Walter Wodchis, Ph.D., Assistant Professor, Health Policy Management and Evaluation, University of Toronto, 155 College Street - 4th floor, Toronto, ON, M5T 3M6; Tel: 416-946-7387; Fax: 416-978-7350; Email: walter.wodchis@utoronto.ca Research Objective: To examine the relationship between clinical quality and costs of care in Long Term Care Settings. Study Design: Cross-sectional time series analysis. Quality assessed by five prevalence and two incidence measures based on the Minimum Data Set for nursing homes. Population Studied: Data represent all long term care hospitals in Ontario, Canada from 1996 through 2001. Quality measures are individually assessed and aggregated to the facility level where they are compared to facility expenditures. Principal Findings: Cost and quality measures showed a high degree of serial correlation. Reduced costs were associated with lower prevalence of pressure ulcers and incontinent residents without toileting plans. Consistent results with mixed significance values were found in several specifications for 5 other quality measures Conclusions: The results indicate opportunities for facilities to improve both cost and quality performance Implications for Policy, Delivery, or Practice: Facilities with an active prevention strategies for pressure ulcer and incontinence care may also find cost savings. Primary Funding Source: Canadian Institutes for Health Research ●Does Medicare Reimbursement Changes Influence Nursing Home Efficiency of Care? Jackie (Ning) Zhang, M.D., Ph.D., Lynn Unruh, Ph.D., RN, Thomas Wan, Ph.D. Presented By: Jackie (Ning) Zhang, M.D., Ph.D., Assistant Professor, Department of Health Administration, University of Central Florida, 3280 Progress Drive, Orlando, FL 32826; Tel: 407-823-3344; Email: nizhang@mail.ucf.edu Research Objective: Prior studies regarding impacts of the Balanced Budget Act (BBA) in nursing homes have examined the issue of quality, but not efficiency. Furthermore, to our knowledge, studies of efficiency in nursing homes do not consider the possible changes in quality as efficiency changes. It is possible that as efficiency increases, quality decreases. Yet to be able to have a true improvement in efficiency, quality must be held constant. This study assesses the impact of recent Medicare reimbursement changes on efficiency in nursing homes when efficiency is adjusted for quality. Research questions are: 1) Has the implementation of a Medicare prospective payment system (PPS) under the 1997 BBA improved efficiency in U.S. nursing homes when efficiency is adjusted for quality? 2) Has the implementation of the 1999 Balanced Budget Reconciliation Act (BBRA) or the 2000 Benefits Improvement and Protection Act (BIPA) counteracted BBA (reduced efficiency) when efficiency is adjusted for quality? 3) Have other market and facility factors in the years 1997-2003 influenced efficiency? Study Design: Data were from the On-Line Survey Certification and Reporting System (OSCAR) for nursing facilities, Medicare Cost Report, and Area Resource Files for the years 1997-2003. The efficiency variable is a ratio of qualityadjusted total resident days (outputs) to total costs for each facility. Quality was measured by a resident-severity-adjusted deficiency variable derived from OSCAR surveillance system. The deficiency variable was a sum of the number of all deficiency citations. The efficiency score was computed by using input-oriented variable returns to scale method provided by Data Envelopment Analysis software. Trend analysis was conducted to find the changing pattern of efficiencies over time. Finally, the impacts of the policy variables on nursing home efficiency were estimated using generalized repeatedmeasure mixed model with seven-years of longitudinal data. Market and organizational factors were examined as well. Future analyses will include analyzing a model using a nonquality adjusted efficiency variable and comparing results with the quality-adjusted model. Population Studied: We obtained a national random sample of Medicare-certified nursing homes in the U.S. Approximately 7,000 homes were studied each year. Principal Findings: Trend analysis shows that mean values for quality-adjusted efficiency decreased significantly and the standard deviation narrowed over time. The mixed model regression results show that the BBA was significantly negatively related to quality-adjusted efficiency. Subsequent policies (BBRA and BIPA) were not significantly related to efficiency. Licensed nurses per resident days, nursing home size, percent Medicaid patients, and non-profit status were positively related to efficiency. Population income and area competition (Hefindahl Index) were also positively related to efficiency. The fit statistics Chi-square was large and significant. Future analyses will compare these results to those from a model using a non-quality adjusted efficiency variable. Conclusions: The results suggest that the BBA had a significantly negative impact on quality-adjusted efficiency, but the subsequent reimbursement policies had no significant impact on it. Various organizational and market factors also play a significant role. Implications for Policy, Delivery, or Practice: When efficiency is adjusted for quality, efficiency-oriented policy changes, such as the BBA, may have unintended opposite affects on efficiency. Primary Funding Source: NIA ●Clinical Characteristic Associated with Direct Costs in AD: Longitudinal Analysis from the Predictors Study Carolyn Zhu, Ph.D., Nikolaos Scarmeas, M.D., Rebecca Torgan, MA, Mary Sano, Ph.D., Yaakov Stern, Ph.D. Presented By: Carolyn Zhu, Ph.D., Health Science Specialist, GRECC/Geriatrics, Bronx VA Medical Center/Mount Sinai School of Medicine, 130 west kingsbridge road, Bronx, NY 10468; Tel: 718-584-9000x3810; Email: carolyn.zhu@mssm.edu Research Objective: Alzheimer’s disease (AD) is the third most costly disease to society in the US. Most cost studies have been cross-sectional and thus limited in their ability to estimate long-term disease cost trajectories. The goals of this study are 1) to estimate long-term trajectories of the direct costs of caring for patients with AD, and 2) to examine the effects of patients’ clinical and socio-demographic characteristics on direct costs over time. Study Design: Random effect regression models were used to estimate the effects of patients’ characteristics on direct costs of caring for patients with AD. Direct costs included costs associated with medical care (hospitalizations, outpatient treatment and procedures, assistive devices, and medications) and non-medical care (home health aides, respite care, and adult day care). Patients’ clinical characteristics included measures of cognitive status (Folstein Mini-Mental State Examination, MMSE), functional capacity (Blessed Dementia Rating Scale, BDRS), comorbidities, and presence and absence of psychotic symptoms, behavioral problems, depressive symptoms, and extrapyramidal signs. Patients’ demographic characteristics included sex, age at intake, and living arrangements. All clinical variables and patients’ living arrangements were measured at each visit and therefore time variant. Population Studied: The sample (n=198) was drawn from the Predictors Study, a large, multi-center cohort of patients with probable AD, followed annually for up to 7 years in three University-based AD centers in the US. Enrollment required a modified Mini-Mental State Examination (mMMS) score =30, equivalent to a score of approximately =16 on MMSE. Because patients were followed at academic AD centers, they were well characterized with high degrees of certainty in their AD diagnosis. Principal Findings: Total direct cost increased substantially over time, from approximately $9,239 per patient per year at baseline, when all patients were at the early stages of the disease, to $19,925 by year 4 (an average of 13% increase each year). In particular, cost of medications rose steadily from $2,872 to $4,301 (a 50% increase), and costs of non-medical care rose from $1,349 to $9,348 (a 6.9 fold increase). Multivariate results show that after controlling for patients’ clinical and socio-demographic variables, the time effect became insignificant and was only associated with a 1.2% increase in cost each year. A one-point increase in BDRS increased total cost by 7.7%, and one more comorbidity increased total cost by 14.3%. Total costs were 20.8% lower for patients living at home compared to those living in institutional settings. Conclusions: With longitudinal data, this study confirms what has been suggested in cross-sectional studies. Specifically, most of the cost increases were explained by comorbidities, functional capacity, and living arrangement. Moreover, these relationships were consistent over time. Implications for Policy, Delivery, or Practice: Interventions aimed at delaying or preventing institutionalization could reduce direct cost of care for AD patients and may be particularly useful if targeted in the areas of basic and instrumental activities of daily living. However, potential cost savings in direct cost of care need to be balanced with the potential increase in informal caregiving costs. Primary Funding Source: VA, NIH