The Heller School for Social Policy and Management, Brandeis University Objective
advertisement

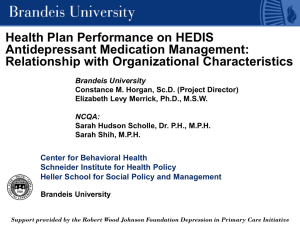
The Heller School for Social Policy and Management, Brandeis University Objective Health Plan Performance on HEDIS Antidepressant Medication Management: Relationship with Organizational Characteristics Brandeis University Constance M. Horgan, Sc.D. (Project Director) Elizabeth Levy Merrick, Ph.D., M.S.W. NCQA: Sarah Hudson Scholle, Dr. P.H., M.P.H. Sarah Shih, M.P.H. Center for Behavioral Health Schneider Institute for Health Policy Heller School for Social Policy and Management Determine whether performance and improvement over time on three antidepressant medication management (AMM) measures in HEDIS differ by how health plans organize, finance, and administer behavioral health care. Brandeis University Support provided by the Robert Wood Johnson Foundation Depression in Primary Care Initiative Context • HEDIS AMM measures overall are low compared to other HEDIS measures • AMM measures are generally not improving over time (unlike other measures) • Most privately insured individuals are in managed care HEDIS Antidepressant Medication Management (AMM) Measures • Effective Acute Phase Treatment • Effective Continuation Phase Treatment • Optional Practitioner Contact • Need to learn what health plan features are associated with better performance Health Plan Domains • Organization • Provider • Consumer Research Design Overview • Linkage of two datasets: Brandeis Health Plan Survey and NCQA’s HEDIS and CAHPS data • Analyzing relationships between key plan characteristics and performance on AMM measures • Both cross-sectional and longitudinal (1999 to 2003) analyses www.heller.brandeis.edu • 781-736-3916 • horgan@brandeis.edu The Heller School for Social Policy and Management, Brandeis University Analytic Approach Data and Sample Brandeis Survey: 2003 health plan survey on alcohol, drug, and mental health services. Nationally representative, linked to 60 Community Tracking Study market areas. N = 368 (812 products). Response rate = 83%. NCQA: 2003 health plan participants in HEDIS. N = 300. Study Sample: All health plans present in both datasets. N = 183 plans, covering 361 HMO and POS products. Effective Acute Phase Treatment Percentage of eligible members who received effective acute phase treatment after a new episode of depression by remaining on antidepressant medication during the first 12 weeks following diagnosis • Mean = 59.5% • 10th percentile = 53.6% • 90th percentile = 66.2% Optimal Practitioner Contact Percentage of eligible members who received at least 3 follow-up office visits with PCP or mental health provider in the 12-week acute treatment phase after diagnosis of depression and prescription of antidepressant medication. • Mean • 10th percentile • 90th percentile = = = 22.1% 12.6% 36.8% • Describe health plans’ 2003 performance on the three HEDIS AMM measures and relationship with key plan characteristics • Conduct multivariate analysis to control for effects of other health plan and market variables. Effective Continuation Phase Treatment Percentage of members who received effective continuation phase treatment by remaining on antidepressant medication continuously in the 6 months after the initial diagnosis and treatment. • Mean = 42.9% • 10th percentile = 37.8% • 90th percentile = 50.5% Organization Domain • Product Type HMO POS 50% 50% • Contracting Arrangement Specialty Comprehensive/Internal 80% 20% • Depression Disease Management Program 47% • Degree of PCP/BH Coordination (0-6 methods) 3.0 www.heller.brandeis.edu • 781-736-3916 • horgan@brandeis.edu The Heller School for Social Policy and Management, Brandeis University Provider Domain Consumer Domain • Provide training on depression guidelines 74% • Provide feedback on individual performance re: guideline adherence 36% • Provide feedback on network performance re: guideline adherence 20% • Degree of support provided for guideline adherence (0 – 3 activities) 1.3 • Plan allows PCP to bill for psychiatric procedure codes 38% • MH screening required by plan 36% • High Cost Sharing for MH Outpatient Visits (> 20% co-insurance or > $20 co-pay) 33% • Pharmacy Tier 2 Cost Sharing (mean) $22 • Access to new SSRIs without restrictions on Tier 2 (0-4 medications) 2.5 • Direct Access – No MH Gatekeeping 39% Rate of Effective Continuation Phase Treatment Rate of Effective Acute Phase Treatment 5.8 Specialty Contract a -1 4.3 -4.9 MH Screening b SSRI Choice b a = P < .01 b = P < .05 -3.5 -3 Adjusted R2 = 0.53 -2.5 -2 -1.5 -1 -0.5 0 0.5 1 1.5 2 2.5 3 3.5 -6 4 4.5 5 5.5 a Degree of PCP/BH Coordination a Feedback Individual Performance a 5.9 MH Screening -4 -3.5 a = P < .01 b = P < .05 -3 -2.5 Adjusted R2 = 0.49 -2 -1.5 -1 b Tier 2 Cost Sharing a -0.9 -0.5 0 0.5 1 1.5 2 2.5 3 3.5 -4.5 -4 -3.5 -3 -2.5 -2 -1.5 -1 -0.5 0 0.5 1 1.5 2 2.5 3 3.5 4 4.5 = P < .01 Regression model included all variables in the three domains, as well as enrollment, tax status and region. Only significant domain variables shown. Conclusions 1.5 -3.6 -5 Adjusted R2 = 0.45 Rate of Optimal Provider Contact -1.8 -5.5 6 Regression model included all variables in the three domains, as well as enrollment, tax status and region. Only significant domain variables shown. Product Type HMO b Direct Specialty Access a -3.7 0.9 Direct Specialty Access b -2.6 -4 High MH Cost Sharing a -5.2 High MH Cost Sharing a -3.6 PCP Psychiatric Billing a -4 PCP Psychiatric Billing a -2.5 -4.5 4.7 Feedback-Individual Performance a Degree of PCP/BH Coordination b Feedback Individual Performance a -5 4.5 Specialty Contract a 4.1 Disease Management a 4 4.5 Regression model included all variables in the three domains, as well as enrollment, tax status and region. Only significant domain variables shown. 5 5.5 6 • Patient cost sharing and choice of SSRIs affect HEDIS AMM performance • Individual feedback to providers helps • Some approaches geared towards improving quality seem to do so (disease management) • Others (e.g., PCP/BH coordination) raise more questions www.heller.brandeis.edu • 781-736-3916 • horgan@brandeis.edu 5