Outline Issues in Cost-Effectiveness Analysis
advertisement
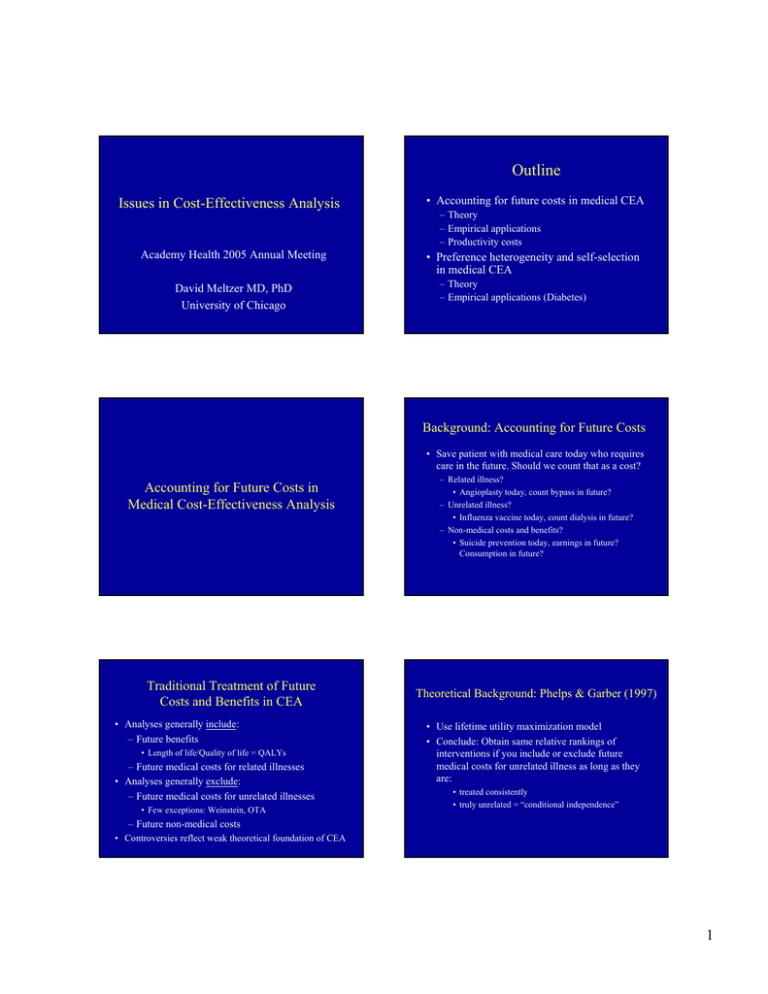
Outline Issues in Cost-Effectiveness Analysis Academy Health 2005 Annual Meeting David Meltzer MD, PhD University of Chicago • Accounting for future costs in medical CEA – Theory – Empirical applications – Productivity costs • Preference heterogeneity and self-selection in medical CEA – Theory – Empirical applications (Diabetes) Background: Accounting for Future Costs • Save patient with medical care today who requires care in the future. Should we count that as a cost? Accounting for Future Costs in Medical Cost-Effectiveness Analysis Traditional Treatment of Future Costs and Benefits in CEA • Analyses generally include: – Future benefits • Length of life/Quality of life = QALYs – Future medical costs for related illnesses • Analyses generally exclude: – Future medical costs for unrelated illnesses • Few exceptions: Weinstein, OTA – Related illness? • Angioplasty today, count bypass in future? – Unrelated illness? • Influenza vaccine today, count dialysis in future? – Non-medical costs and benefits? • Suicide prevention today, earnings in future? Consumption in future? Theoretical Background: Phelps & Garber (1997) • Use lifetime utility maximization model • Conclude: Obtain same relative rankings of interventions if you include or exclude future medical costs for unrelated illness as long as they are: • treated consistently • truly unrelated = “conditional independence” – Future non-medical costs • Controversies reflect weak theoretical foundation of CEA 1 Intuition Theoretical Background: Meltzer (1997) • Consider two interventions with equal current cost that both produce one QALY • Use lifetime utility maximization model • Conclude: • A increases life expectancy by one year at QOL=1 • B increases life expectancy by two years at QOL=0.5 – Must include all future net resource use • Medical costs - both related and unrelated - and future non-medical costs net of earnings • “Net resource use”= consumption + medical expenditures - earnings • From -$10,000/ year @ age 25 to +$20,000/year @ age 85 • Which is preferred? – From utility side: Indifferent – From cost side: A preferred since it saves the costs of supporting an extra year of life – Hence, A preferred overall – Relative rankings of interventions not independent of future costs • Analyses that omit future costs favor interventions that extend life over those that improve quality of life – Phelps/Garber inadvertently assume net annual resource use is zero • Omitting future costs favors interventions that extend life (B) versus those that increase QOL (A) Consumption, Medical Expenditure, Earnings and Net Resource Use by Age Accounting for Future Costs Present Value of Future Net Resource Use Per Year of Life Saved by Averting Death (by Age) 30 20 Dollars (in thousands) Δcost Δpresent cost Δfuture cost = + ΔQALY ΔQALY ΔQALY Δpresent cost C * ΔLY = + ΔQALY ΔQALY Δpresent cost ΔLY = + C* ΔQALY ΔQALY 10 Consumption Medical Expenditure Earnings Net Resource Use 0 -10 -20 25 45 55 65 75 85 Age Approximate Effects of Future Costs Intervention 30 Dollars (thousands) 35 Cost/QALY without future costs C ΔLE/ΔQALY C∗(ΔLE/ΔQALY) Cost/QALY with future costs 20 Treatment Severe Hypertension Men Age 40 $18,000 -$5,000 1.03 -$5,200 $12,800 10 Treatment Severe Hypertension Men Age 60 $60,000 $8,000 1.07 $8,500 $68,500 Adjuvant Chemo Duke’s C Colon CA Men Age 60 $67,000 $8,000 18 $144,000 $211,000 Hemodialysis for ESRD Men Age 60 $117,000 $8,000 1.5 $12,000 $129,000 0 -10 25 35 45 55 Age 65 75 85 2 So why not include future costs? • Believe they belong, but don’t know how to include them • But methods are available: • Believe they belong in theory, think it’s “mean spirited” • Meltzer JHE ‘97, Johannesson et al. MDM ‘97 • Can be as simple as including an age-specific average net resource use • Imprecise estimates better than zero Effects of Future Costs for Interventions among the Elderly INTERVENTION Hip Replacement Women age 60 Hip Replacement Men age 85 Treatment Mild HTN Men age >70 Radiation Tx. MDPC Age 65 ΔLY ΔQALY ΔLY/ΔQALY So why not include future costs? Δcost/ΔQALY w/o future costs Δcost/ΔQALY w/ future costs -0.03 6.9 -0.005 Cost-saving Cost-saving -0.02 2.0 -0.01 $9,177 $9,042 0.06 0.05 1.25 $5,000 $32,000 0.8 0.4 2 CECRC CECRC+$32,000 Prostatectomy MDPC 0.7 0.2 3.5 CECRC CECRC+$56,000 Age 65 HTN = Hypertension, MDPC = Moderately Differentiated Prostate Cancer CECRC = Cost-effectiveness based on Current and Related Costs – “Won’t this make it look like nothing is costeffective, don’t you believe in medicine?” – “I have an 80 year-old father, the way I understand your argument, you’re saying I should kill him” Effects of Future Costs for Interventions among the Young and Elderly Without Future Costs With Future Costs Cost-saving Cost-saving Treatment Mild HTN Men Age>70 $5,000/QALY $30,000/QALY Hip Replacement Men Age 85 $9,177/QALY $9,042/QALY Intensive Therapy IDDM Starting Age 13-39 $30,000/QALY $15,000/QALY Hip Replacement Women Age 60 So why not include future costs? • Don’t believe they belong; think future costs implicit in people’s answers to quality of life questions • However, Do People Consider Financial Factors in Answering Quality of Life Questions? – Costs due to increased life expectancy largely not borne by individuals – Empirical evidence that people do not consider these costs when answering QALY questions 3 Background (continued) Background • Economic analysis of medical technology requires accurate measurement of benefits and costs – All relevant factors measured once and only once – In accounting for future costs, this implies that lost income should be counted as a cost • Report of the Panel on Cost-effectiveness in Health and Medicine argues that lost income should not be counted as a cost in cost-effectiveness analysis – Based on assumption that individuals consider income changes when answering quality of life questions – This has been used as an argument for excluding lost income in accounting for future costs • Active debate whether productivity costs are fully reflected in QOL Measures (Brouwer et al. 1997, Meltzer and Johnanesson 1999) – Discrepancies between personal and social costs • public and private insurance • payroll and income taxes – Ambiguities about whether respondents consider personal economic costs in answering QOL questions • Health Utilities Index explicitly excludes lost income • All other utility elicitation techniques silent on lost income Effect of Economic Concerns on QOL Ratings Objective • To determine whether people consider financial factors in answering quality of life questions – Randomized subjects to versions of time trade-off (TTO) questions that differ in guidance about incorporating financial consequences of illness – Asked patients whether they considered economic factors when answering these questions – Performed analyses for TTO questions concerning blindness and back pain Sample question: Which of the following would you prefer? Live with blindness for 10 years. Live in perfect health for 7 years. No preference because these seem about the same. QOL (TTO) No Guidance (NG) 4.95 - Receive Disability (D) 4.83 P(D vs. NG) < N.S. Not Receive Disability (ND) 4.84 P(ND vs. NG) < N.S. Effect of Economic Concerns on QOL Ratings Were People Thinking about Economic Concerns? Sample question: Which of the following would you prefer? Live with severe back pain for 10 years. Live in perfect health for 7 years. No preference because these seem about the same. Question: When you answered this last set of questions, were the possible financial effects of this back pain a factor in your answer? % Yes QOL (TTO) No Guidance (NG) 5.09 - Receive Disability (D) 5.78 P(D vs. NG) < 0.1 Not Receive Disability (ND) 4.24 P(ND vs. NG) < 0.03 No Guidance (NG) 13 - Receive Disability (D) 20 P(D vs. NG) < 0.01 Not Receive Disability (ND) 21 P(ND vs. NG) < 0.01 4 Were People Thinking about Economic Concerns? Question: When you answered these questions, were you thinking about whether you would work? Did Thinking about Financial Effects Change TTO Values in the Absence of Guidance? % Yes No Guidance (NG) 24 - Receive Disability (D) 31 P(D vs. NG) < 0.01 Not Receive Disability (ND) 40 P(ND vs. NG) < 0.01 QOL (TTO) Not Thinking about Financial Effects 5.32 Thinking about Financial Effects 4.15 P-value for difference < 0.02 Conclusions • Financial considerations may alter answers to TTO questions – Average TTO values change with guidance about financial factors – Standard TTO questions without guidance generate heterogeneous assumptions across respondents • Most people do not consider financial effects • Respondents who consider financial effects give lower average TTO values Effects of Self-Selection on Cost-Effectiveness • Even with guidance about financial factors, most respondents say they were not a factor or that they were not thinking about effects of illness on work • Probably best to instruct people to ignore economic consequences of illness and count those costs separately Background • Traditional CEA uses preferences (utilities) that average across individuals • However, utilities may vary across individuals or populations and influence expected benefits of treatment Standard CEA with Heterogeneous Individuals CE Δ costs m – Implies cost-effectiveness can vary for individuals or populations that differ in preferences • Preferences can also affect treatment choice Δ effectiveness – Specifically, patients whose preferences favor an option may be more likely to choose it • How might “self-selection” affect cost-effectiveness? Blue Dots = Treated Patients 5 Perfect Self-Selection Effect of Perfect Self-Selection on CEA CE Δ costs m CE Δ costs m Δ effectiveness Blue Dots=Pts gain from Tx; Orange Dots=Pts lose from Tx Empirical Self-Selection CE Δ costs m Δ effectiveness Blue Dots=Pts choose Tx; Orange Dots=Pts reject Tx Methods: Interviews • Interviewed 515 diabetes patients over age 65 attending University of Chicago clinics from 1/1/01 to 1/1/2003 • Preferences (utilities) obtained by time trade-off questions • Utilities obtained for – Conventional and intensive glucose lowering (using insulin or oral medications) – Blindness, end-stage renal disease, lower extremity amputation • Data on treatment choices and patient characteristics collected by medical records review m’ Δ effectiveness Blue Dots=Pts gain from Tx; Orange Dots=Pts lose from Tx (reject) Background: Diabetes in the Elderly • Diabetes care guidelines call for intensive lowering of glucose among younger patients • However, unclear if this should apply to older patients – Gains in life expectancy smaller – Side effects of treatment may dominate – CE models of intensive therapy in older patients: • Minimal or even negative effects on QALYs • Not cost-effective – Know many patients refuse intensive therapy • Suggests self-selection may have important effects on CEA in diabetes Methods: Modeling • NIH simulation model of intensive therapy for type 2 diabetes (HbA1c 7% vs. 10%) – Incorporated patient-specific data • Age, sex, race, duration of diabetes • Ran model using each individual’s utilities – Intensive/conventional therapy, diabetic complications • Analyses of cost-effectiveness of: – Intensive vs. conventional therapy with insulin – Intensive vs. conventional therapy with oral medications • Contrast – All patients vs. Perfect self-selection vs. Empirical selfselection 6 Results: Intensive Insulin Therapy vs. Conventional Therapy N CE Approach Group Standard Full Population Results: Intensive Insulin Therapy vs. Conventional Therapy Change in Change in CE Ratio Costs ($) QALYs ($/QALY) 515 4826 -0.46 -- Perfect Self-Selection Effect for Intensive Insulin Therapy N CE Approach Group Change in Change in CE Ratio Costs ($) QALYs ($/QALY) Standard Full Population 515 4826 -0.46 -- Perfect SelfSelection ΔQALY>0 309 4255 0.32 13K ΔQALY<0 206 5682 -1.63 -- Empirical Self-Selection Effect for Intensive Insulin Therapy 20000 20000 CE 15000 15000 10000 10000 5000 5000 m m’ 0 0 -8 -6 -4 -2 0 2 4 -8 -6 -4 -2 0 2 4 -5000 -5000 Blue dots--the cost-effectiveness values of individuals with an expected benefit from intensive therapy. Orange dots-- the cost-effectiveness values of individuals with a decrement in expected benefits with intensive therapy. M-- CE ratio for whole population. M’—CE ratio after self-selection. Results: Intensive Insulin Therapy vs. Conventional Therapy N CE Approach Group Standard Full Population 515 4826 Perfect SelfSelection ΔQALY>0 309 ΔQALY<0 206 Self-identified intensive insulin therapy All others Empirical Self-Selection Blue dots-- cost-effectiveness values for individuals who identify their care as intensive therapy with insulin. Orange dots-- cost-effectiveness values for all other individuals. M-- CE ratio for orange dot individuals. M’-- CE ratio for blue dot individuals. Results: Intensive vs. Conventional Oral Therapy CE Approach Group N Change in Change in CE Ratio Costs ($) QALYs ($/QALY) -0.46 -- 4255 0.32 13K 5682 -1.63 -- 97 2386 -0.03 -- 418 5421 -0.56 -- Standard Full Population 515 Change Change in CE Ratio in Costs QALYs ($/QALY) ($) 4826 0.17 28K 7 Results: Intensive vs. Conventional Oral Therapy N CE Approach Group Change Change in CE Ratio in Costs QALYs ($/QALY) ($) Results: Intensive vs. Conventional Oral Therapy N CE Approach Group Change Change in CE Ratio in Costs QALYs ($/QALY) ($) Standard Full Population 515 4826 0.17 28K Standard Full Population 515 4826 0.17 28K Perfect Self-Selection ΔQALY>0 427 4791 0.42 11K Perfect Self-Selection ΔQALY>0 427 4791 0.42 11K ΔQALY<0 88 4996 -1.04 -- ΔQALY<0 88 4996 -1.04 -- All Oral Therapy 219 5892 0.06 104K On Intensive Oral Therapy 11 3294 0.29 11K On Non-intensive 208 Oral Therapy 6029 0.04 136K Empirical Self-Selection CDC-AAMC PEP Initial Results: Intensive vs. Conventional Therapy Limitations • Modest sample size • Limitations of the diabetes simulation model N CE Approach Group – Model only compares HbA1c of 10% and 7% – Does not model other diabetes-related treatments Standard Full Population 394 Change Change in CE Ratio in Costs QALYs ($/QALY) ($) 8007 -0.35 - • Other definitions of intensive therapy – E.g., actual treatments used, HbA1c – Results stable with alternative definitions • Unclear if utilities are valid or stable over time – Might undermine predictive validity / welfare interpretation CDC-AAMC PEP Initial Results: Intensive vs. Conventional Therapy CE Approach Group N Implications Change Change in CE Ratio in Costs QALYs ($/QALY) ($) Standard Full Population 394 8007 -0.35 - Empirical Self-Selection On Intensive Therapy 122 7777 0.18 43K • Results of standard CEA may be misleading – CEAs should consider the importance of selfselection • Provides framework to value guidelines, decisionaids, or improved patient-doctor communication to make care more consistent with patient preferences • Suggests framework to design co-payment systems to enhance cost-effectiveness of therapies • Provides insight into policy making for voluntary vs. involuntary interventions 8 Funding • Centers for Disease Control and Prevention – AAMC PEP (Meltzer, Huang) – Center of Excellence in Health Promotion Economics (Meltzer) • National Institutes of Health – NIDDK (Meltzer, Huang) – NCI (R01 Meltzer) • Robert Wood Johnson Foundation – Generalist Physician Faculty Scholar Award (Meltzer) Implications - I Implications - II • Results of standard CEA may be misleading – In contrast to the suggestion of standard CEA, offering intensive glucose lowering to all older people likely cost-effective – CEAs should consider the importance of selfselection • Accounting for self-selection provides a framework to value guidelines, decisionaids, or improved patient-doctor communication that can make care more consistent with patient preferences • Distinction between perfect and empirical selfselection is potentially important – Data on who will use a treatment if it is offered is important Motivation for Decision Aids CE Δ costs m Aim of Decision Aids CE Δ costs m Δ effectiveness Blue Dots=Pts getting Tx; Orange Dots=Pts not getting Tx Δ effectiveness Blue Dots=Pts getting Tx; Orange Dots=Pts not getting Tx 9 Value of Decision Aids CE Δ costs m Δc Δ effectiveness Δe Value of Decision Aid • Effectiveness = ΣPts Δ Δe • Costs = ΣPts Δ Δc • Total Benefit ΣPts Δ Δc Cost-Benefit = (1/λ) ΣPts Δ Δe + Net Health Benefit = ΣPts Δ Δe + λ ΣPts Δ Δc Blue Dots=Pts getting Tx; Orange Dots=Pts not getting Tx Implications - III Motivation for Copayment • Self-selection suggests a framework to design copayment systems to enhance the cost-effectiveness of therapies Δ costs CE m Δ effectiveness Blue Dots=Pts getting Tx; Orange Dots=Pts not getting Tx Motivation for Copayment (πc) πc Δ costs CE Implications - IV • Self-selection provides insight into policy making for voluntary vs. involuntary interventions – Voluntary: most medical interventions • Self-selection improves value vs. population estimates m – Involuntary: environmental policy / safety regulation • Population estimates more likely to be appropriate Δ effectiveness – Harms of pollution / safety risk non-selectively distributed – Harms of regulation also non-selectively distributed – Different standards for environmental regulation? • • • • Traditionally high value of life -> low threshold for regulation Reasonable if environmental harms not selectively avoidable Not reasonable if harms of regulation also not selectively avoidable Better approach: model selection and use common threshold Blue Dots=Pts getting Tx; Orange Dots=Pts not getting Tx 10 Funding • Centers for Disease Control and Prevention – AAMC PEP (Meltzer, Huang) – Center of Excellence in Health Promotion Economics (Meltzer) • National Institutes of Health – NIDDK (Meltzer, Huang) – NCI (R01 Meltzer) • Robert Wood Johnson Foundation – Generalist Physician Faculty Scholar Award (Meltzer) Specific Aims Effects of Quality of Life on the Cost-Effectiveness of Prostate Cancer Treatment David O. Meltzer, MD, PhD Anirban Basu, MS Brian L. Egleston, MPP Qi Zhang, PhD Background on Prostate Cancer • Most commonly diagnosed non-cutaneous cancer, among US men • Second most common cause of cancer-related death among US men • To develop a sophisticated decision-analytic model to evaluate cost, effects, and costeffectiveness alternative treatments for clinically localized prostate cancer by age and tumor grade • To assess how the cost-effectiveness of prostate cancer treatments will be affected by including possible effects of anxiety on QOL • To assess how patient self-selection might affect the cost-effectiveness of treatment Challenges • PC screening and treatment remains controversial • Effects on mortality unclear – Little clear evidence from randomized trials – Mortality trends post screening not established • Presence of significant morbidities associated with treatment • 198,100 new cases diagnosed and 31,500 deaths in 2001 • Significant variation in outcomes by tumor grade, patient age • ~80% of clinically diagnosed PC in men 65+ • Significant costs of screening and treatment of localized PC • Because older persons have high competing risks of death, many men die with prostate cancer rather than of it. • Cost-effectiveness studies of treatment differ in findings • <10% men with PC die of it within 5 years of diagnosis • Cost-effectiveness studies of screening differ even more greatly – Increase QALYs (Kattan) – Increase survival but not QALYs (Fleming) 11 Flaws in Published Models • Failure to model PC incidence as a dynamic process affected by previous screening through effects on prevalence of latent disease • Failure to distinguish between cancers of differing stage and grades (heterogeneity) • Model progression based on clinical rather than pathological stage, or without any empirical basis • Many models are of one-time screen (exception: Etzioni et. al. 1999) • Other problems: – Confuse PPV/NPV of screening tests vs. sensitivity/specificity, – Failure to model QOL and/or cost, – Other technical and data related issues. Key Features of Our Model vs. Published Models Prostate Cancer Model: Overview • Development of Model Structure – Natural history model – Detection model • Parameter Estimation – – – – – Literature review Secondary data analysis Mathematical modeling Fitting to aggregate incidence, prevalence, & mortality by age Maximum likelihood estimation • Cancer stage and grade transitions • Mortality rates from metastatic disease • Estimation of Cost-Effectiveness of: • Screening policies • Treatment policies The Model • Markov model of screening and treatment – Annual cycles from age 50 to 99 • Tumor heterogeneity and progression rates by grade • Misclassification of tumor stage due to the discrepancy between clinical and pathologic stage • The ability of screening and treatment to affect the prevalence of prostate cancer in the undetected population • The effect of benign prostatic hypertrophy and its management on the detection of prostate cancer • The potential effects of screening and treatment on quality of life, as measured by quality-adjusted life expectancy Model Structure: Overview • Natural history model including stage and grade – Possibility of early metastases • Repeat screening requires treating many factors as state variables – Even small rates lead to 100% intervention rates over time – We created a state vector with 1,440 states BPH symptoms PSA/Rectal detectable History of screening Presence of metastases Metastatic detectable History of TURP Local cancer stage Local grade Model Structure: Natural History N A B C D Initial Stage Distribution Well Moderate Poor No Cancer N A B C D Detection Non-Detected Population Transition Probabilities N A B C D Incidence Rate Cured N A B C D Death from Other Causes Not Cured N A B C D Death from Prostate Cancer or Other Causes N A B C D Local Stage A Local Stage B Local Stage C Transition Probabilities Death from Prostate Cancer or Other Causes Non-metastatic disease Metastatic disease 12 Model Structure: Detection Symp = Symptoms Mot = Motivated Pos = Positive Neg = Negative TURP = Transurethral Resection of the Prostate MWU = Metastatic Work-up Palp Ext = Palpable Extension Clin = Clinical Stage Comp = Complications Model Structure: State Variables – Pathologic Stage • Local stage (no cancer, A, B, C) • Presence of metastases (D) – Grade • Well, moderate, poor – Presence of BPH symptoms – Presence of cancer symptoms – History of TURP for BPH symptoms – Cancer detectability • Digital rectal exam and/or PSA detectability – History of regular prostate cancer screening Parameter Estimation: Direct Approaches Parameter Derivation Technique Primary References P(Symptom Motivated Exam) Literature Review Meigs et al., 1998 P(Biopsy | Positive Exam) Secondary Data Analysis Richie et al., 1993 P(Biopsy Positive | Pathologic Stage) Geometric Prostate Model McNeal et al., 1986 Catalona et al., 1996 Lu-Yao et al., 1996 Parameter Estimation: Direct Approaches Parameter Derivation Technique P(Prostate Cancer | Age) Meta-Analysis Multiple sources P(DRE or PSA Detectable Prostate Cancer) Maximum Likelihood Estimation and Secondary Data Analysis Literature Review Richie et al., 1993 P(Metastatic Work-Up Positive) Mathematical Modeling P(Clinical Stage | Pathologic Stage) Secondary Data Analysis SEER data P(Symptomatic BPH) P(Treatment | Clinical Stage) Secondary Data Analysis SEER data P(Symptoms | Prostate Cancer) P(Complications | Treatment) Literature Review Wasson et al., 1993 P(Cure Rates | Treatment and Pathologic Stage) Literature Review and Model Assumptions D’Amico et al., 1998 P(Transurethral Resection of the Prostate [TURP]) Secondary Data Analysis P(Postive Pathologic Findings | TURP) Literature Review and Mathematical Analysis National Hospital Discharge Survey National Survey of Ambulatory Data Coffield et al., 1992 Babaian et al., 1991 P(Routine Screening Exam for Prostate Cancer) Literature Review Meigs et al., 1998 P(History of Prostate Cancer Screening) Literature Review Meigs et al. 1998 Model Validation and Indirect Parameter Estimation Relationship between grade and stage Mathematical Modeling Literature Review Literature Review Primary References Meigs et al., 1998 Multiple Sources Middleton et al., 1988 Prostate Cancer Related Mortality Data Analysis SEER Data Age-Specific All-Cause Mortality Literature Review Quality of Life Literature Review Social Security Administration Multiple Sources Model Fit • Curve fitting – Aggregate SEER incidence and mortality data • Maximum likelihood estimation – Individual level SEER-Medicare data • Stage-treatment-age • Outcomes (mortality, metastatic disease) • e.g. P(die PC age 76| T1a, RPx, 68) 13 Cost-Effectiveness of Treatment Baseline Analysis (Age 55 yrs) Individual Fitting: SEER vs. Life Table Data Age (years), and Well Differentiated Outcome WW Age SEER PC Mort 3.58% 2.07% 1.38% 1.71% 1.25% 55 65 75 85 95 SEER Non-PC Mort 0.36% 2.03% 2.72% 3.72% 2.92% Life Table Non-PC Mort 0.89% 2.23% 4.86% 11.82% 26.15% RP RT Moderately Differentiated WW RP RT Poorly Differentiated WW RP RT 55 + Expected Costs Non-Discounted LYs + Discounted LYs + Discounted QALYs 5483 34515 35125 6463 27630 28106 8047 23435 23815 21.82 22.53 22.64 19.88 21.61 21.71 16.48 19.21 19.3 13.39 13.63 13.69 12.49 13.18 13.24 10.75 11.93 11.98 13.32 9.84 11.45 12.28 9.48 11.02 10.38 8.52 9.89 + Discount Rate of 3% is used, Costs is 1993 $. QOL weight for Impotence, Incontinence, Bowel Dysfunction, Urethral Stricture and Metastasis are added. Cost-Effectiveness of Treatment Cost-Effectiveness of Treatment Baseline Analysis (Age 65 yrs) Baseline Analysis (Age 75 yrs) Age (years), and Well Differentiated Outcome WW RP RT Moderately Differentiated WW RP RT Age (years), and Poorly Differentiated Well Differentiated Outcome WW RP RT Moderately Differentiated Poorly Differentiated WW RP RT WW RP RT WW RP RT 75 65 + + Expected Costs 5993 39044 39733 4784 20181 20527 5646 12613 12795 Expected Costs 4612 31935 32502 3320 17389 17689 2466 6255 6315 Non-Discounted LYs 14.83 15.17 15.25 13.53 14.46 14.53 10.85 11.78 11.84 Non-Discounted LYs 9.24 9.26 9.32 8.71 8.85 8.9 7.15 7.24 7.28 7.41 7.52 7.56 6.91 7.23 7.27 5.73 6.08 6.11 Discounted LYs 3.73 3.73 3.75 2.39 2.39 2.4 2.99 3.01 3.03 3.71 2.69 3.13 3.48 2.57 2.99 2.80 2.09 2.41 + Discounted LYs + Discounted QALYs 7.37 5.43 6.32 6.76 5.19 6.04 5.43 4.28 + Discount Rate of 3% is used, Costs is 1993 $. QOL weight for Impotence, Incontinence, Bowel Dysfunction, Urethral Stricture and Metastasis are added. Two-way Sensitivity Analysis of Cost-Effectiveness with Impotence & Incontinence QOL (Age 55 yrs) 4.95 + + Discounted QALYs + Discount Rate of 3% is used, Costs is 1993 $. QOL weight for Impotence, Incontinence, Bowel Dysfunction, Urethral Stricture and Metastasis are added. Psychological Anxiety • Patients with known prostate cancer may have anxiety that affects QOL. QOL of Patients detected with prostate cancer = Anxiety QOL (if no other side effects) • Anxiety may be reduced with treatment With Surgery: If Cured: Patient’s QOL =1.0 (i.e. Confirmed Elimination of PC related Anxiety) If not cured: Patient's QOL = Anxiety QOL With Radiation: If Cured: Patient’s QOL = (1+ Anxiety QOL)/2 (i.e. Unconfirmed Elimination of PC related Anxiety) If not cured: Patient's QOL = Anxiety QOL 14 Moderately Differentiated Poorly Differentiated Age 55 Age 55 W QALYs QALYs W R R 6 4 2 0 0.6 0.7 0.8 0.9 1 W 12 W R R R 10 R R R 8 7 6 5 4 3 2 1 0 R W 8 6 4 2 0 0.6 0.7 0.8 0.9 0.6 0.7 1 0.8 0.9 W R R W 0.7 0.8 0.9 Anxiety QOL * Letter above bar indicates most beneficial treatment that is cost-effective (<$100K/QALY) Poorly Differentiated Age 65 Age 65 W 0.6 1 Anxiety QOL Anxiety QOL Anxiety QOL Moderately Differentiated Age 65 14 QALYs 14 12 10 8 14 12 10 8 6 4 2 0 W Well Differentiated QALYs Age 55 QALYs Well Differentiated One-way Sensitivity Analysis of Anxiety QOL on Baseline Estimates (Age 65 yrs) 1 8 7 6 5 4 3 2 1 0 W R R R W 0.6 0.7 0.8 0.9 Anxiety QOL QALYs One-way Sensitivity Analysis of Anxiety QOL on Baseline Estimates (Age 55 yrs) 1 8 7 6 5 4 3 2 1 0 R R R 0.6 0.7 0.8 W 0.9 W 1 Anxie ty QOL * Letter above bar indicates most beneficial treatment that is cost-effective (<$100K/QALY) CEA Phase Diagrams with Anxiety, Impotence and Incontinence QOL for Age = 55 yrs One-way Sensitivity Analysis of Anxiety QOL on Benefits and Cost-Effectiveness (Age 75 yrs) Well Differentiated Moderately Differentiated W W R W Age 75 W 0.6 0.7 0.8 0.9 Anxiety QOL 1 4 3.5 3 2.5 2 1.5 1 0.5 0 W R R W W QALYs 4 3.5 3 2.5 2 1.5 1 0.5 0 1.0 Poorly Differentiated Age 75 QALYs QALYs Age 75 Anxiety QOL 0.6 0.7 0.8 0.9 1 4 3.5 3 2.5 2 1.5 1 0.5 0 W R R W W 0.8 0.6 0.7 Anxiety QOL 0.8 0.9 1 Anxiety QOL 0.6 * Letter above bar indicates most beneficial treatment that is cost-effective (<$100K/QALY) CEA Phase Diagrams with Anxiety, Impotence and Incontinence QOL for Age = 65 yrs CEA Phase Diagrams with Anxiety, Impotence and Incontinence QOL for Age = 75 yrs Anxiety QOL Anxiety QOL 1.0 1.0 0.8 0.8 0.6 0.6 15 RESULTS • Treatments cost-effective vs. watchful-waiting only at high QOL of impotence and incontinence and younger ages. • Radiation tends to be cost-effective than surgery • Results not sensitive to bowel dysfunction and metastasis QOL • Results very sensitive to anxiety QOL. – Anxiety QOL=0.8 makes radiation cost-effective even at low QOL of other complication. • Patient preferences important determinant of optimal care • Self-selection may be a critical determinant of costeffectiveness Panel’s Position on Morbidity Costs • Effects on income and leisure should be excluded from costs since included in QALY weights – Assume people take private economic effects into account in answering QOL questions – Exception: effects of lost productivity borne by others (e.g. “friction costs” borne by employees and coworkers) Problems with Panel’s Position on Morbidity Costs • Inappropriate exclusion of lost earnings not reflected in private costs • Disability insurance (public or private) • Taxes (employee and employer) • Inappropriate inclusion of costs already reflected in private costs • Out-of-pocket health care costs • Time costs in chronic illness (e.g. ESRD) Conclusions • Financial considerations may alter answers to TTO questions – Average TTO values change with guidance about financial factors – Standard TTO questions without guidance generate heterogeneous assumptions across respondents • Most people do not consider financial effects • Respondents who consider financial effects give lower average TTO values • Even with guidance about financial factors, most respondents say they were not a factor or that they were not thinking about effects of illness on work • Probably best to instruct people to ignore economic consequences of illness and count those costs separately – But further study is needed 16 Cost-Effectiveness of Pap Smears Increase in LE vs. no screening Cost vs. no screening Average Cost per Life-Yr Saved Marginal increase in Cost Marginal Increase in Cost Marginal Cost per Life-Yr Saved 3 years 70 days $100 $521/LY 70 days $100 $521/LY 2 years 71 days $150 $771/LY 1 day $50 $18,250 /LY 1 year 71 days 8 hours $300 $1,535/LY 8 hours $150 $165,909 /LY Frequency Why the difference versus Phelps and Garber? • In some models, they assume consumption = production in every period – This sets future costs = 0 • In others, they incorrectly apply an equilibrium condition from a model without future costs to a model that includes future costs – This holds in the future costs model only if future costs = 0 Limitations • Estimates of future costs may be imprecise – Prostate cancer estimates based on ΔLY/ΔQALY • Ideally, costs should be included directly in the decision model – Future consumption, medical expenditures and earnings may be hard to predict. However: • Imprecise estimates are presumably better than implicit estimate of zero • Sensitivity analyses can and should be performed • This should include estimates that exclude future costs – Reflection of resource costs in QALYs not clear • Especially non-market consumption and production • This is an issue for current costs as well QALYs • Total years lived with each year weighted between 0 and 1 – Death: 0 – Perfect health: 1 • QALYs = Σ tStQt – St survival probability – Qt quality of life adjustment – < 1 time preference discount factor Limitations • Estimates of future costs may be imprecise – Prostate cancer estimates based on ΔLY/ΔQALY • Ideally, costs should be included directly in the decision model – Future consumption, medical expenditures and earnings may be hard to predict. However: • Imprecise estimates are presumably better than implicit estimate of zero • Sensitivity analyses can and should be performed • This should include estimates that exclude future costs – Reflection of resource costs in QALYs not clear • Especially non-market consumption and production • This is an issue for current costs as well Methods • Study Population – 831 adults interviewed while waiting for scheduled physician visits in an academic primary care practice – Separate surveys for blindness (N=429) and back pain (N=402) – Ages 18-65 • Survey Design – Description of health states • “permanent blindness” • “severe chronic back pain that occurs every day for at least half the day” • No explicit mention of effects on work in health state description – Subjects then asked time trade-off question in one of three randomly assigned forms: 17 TTO Versions Version 0: “Imagine you have developed severe chronic back pain and have 10 years to live.” Version 1: Version 0 + “Depending on your occupation and personal choice, this might or might not prevent you from working. If you were unable to work, I would like you to assume that you would receive disability payments equal to 60% of your current income” Version 2: Version 0 + “Depending on your occupation and personal choice, this might or might not prevent you from working. If you were unable to work, I would like you to assume that you would receive no disability payments.” Methods: Follow-up Questions • “When you answered this last set of questions, were the possible financial effects of this illness a factor in your answer?” • “Were you thinking about whether you would work?” • Beliefs about effects of the illness on employment status and income • Demographic information, current employment status, and income Results: Population Characteristics Age (years) Mean (SD) Race Black White Other Job Status Working Retired Student Homemaker Disabled Unemployed Other Household Income < $25,000 $25,000 - $50,000 >$50,000 Overview 39 (14) 52% 34% 14% 63% 14% 10% 3% 3% 3% 5% • Theory of self-selection • Initial results on self-selection in diabetes treatment • Prostate cancer model and likely importance of self-selection 28% 34% 38% Overall Aim and Hypotheses • Overall Aim: To evaluate the impact of self-selection on the cost-effectiveness of intensive glucose lowering therapy among older patients with diabetes Results: Patient Characteristics (N=515) Mean Age, years (Std. Deviation (SD)) Female, % 74 (5.9) 63 Ethnicity • H1: Perfect self-selection will make intensive therapy more cost-effective compared to its cost-effectiveness in the full population of older patients with diabetes African American, % Caucasian, % Hispanic, % • H2: Empirical self-selection will make intensive therapy more cost-effective compared to its cost-effectiveness in the full population of older patients with diabetes Asian, % Mean duration of Diabetes, years (SD) 79 16 2.5 0.4 13 (10) 18 Results: Complication Health State Utilities Results: Treatment Health State Utilities Health State Mean (95% CI) Health State Mean (95% CI) Blindness 0.39 (0.36-0.42) Conventional glucose lowering 0.76 (0.73-0.78) End-stage renal disease 0.36 (0.34-0.39) 0.77 (0.75-0.80) Lower extremity amputation 0.45 (0.42-0.48) Intensive glucose lowering with oral medications Intensive glucose lowering with insulin 0.64 (0.61-0.67) Results: Effects of Future Costs for Interventions among the Young Without Future Costs With Future Costs Intensive Therapy IDDM (Meltzer et al. 1999) $48,000/LY $23,000/LY Intensive Therapy IDDM (Meltzer et al. 1999) $30,000/QALY $15,000/QALY HAART – base case (Sendi et al., 1999) $22,000/LY Cost-saving HAART – pessimistic case (Sendi et al., 1999) $30,000/LY $4,000/LY 19