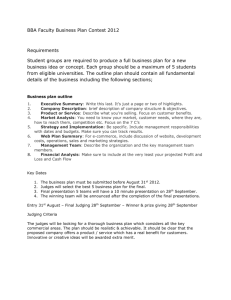
Hospital Ownership Form and Quality Changes: Changes in Nurse Staffing
advertisement

Hospital Ownership Form and Quality Changes: Changes in Nurse Staffing and Failure-to-Rescue following the BBA of 1997 David K. Song, M.D., Ph.D. Kevin G. Volpp, M.D., Ph.D. We thank VA HSR&D, the Doris Duke Foundation, and The National Bureau of Economic Research for financial support. Purpose of the Research Agenda Do hospitals decrease quality in response to fiscal pressure? Do NP and FP hospitals respond differently to changes in government reimbursement of medical services? In this presentation, we examine whether FP hospitals differed from NP hospitals in the adjustment of nurse staffing and failure-to-rescue following the passage of the Balanced Budget Act of 1997. Caveat: Since quality is multi-dimensional and hard to define, we put our study within the context of other attempts to examine multiple outcome measures in various provider settings. FP vs. NP: Nurse Staffing RN per adjusted day 7.5 7 6.5 6 5.5 5 4.5 4 3.5 3 FP 1 FP 4 1996 1997 1998 1999 2000 2001 RN per adjusted day 7.5 7 6.5 6 5.5 5 4.5 4 3.5 3 NP 1 NP 4 1996 1997 1998 1999 2000 2001 The Balanced Budget Act (97) and Hospital Operating Income By decreasing the growth rate in Medicare reimbursement, the BBA enforced fiscal discipline on hospitals. The passage of the law coincided with a nationwide decline in operating income. We find that hospitals, particularly for-profits, decreased their operating expenses in proportion to their Medicare exposure, but not enough to offset the Medicare revenue shortfall. Changes in quality may be part of the story. Operating Income Operating Income in U.S. Hospitals 200 100 2000 1999 1998 1997 1996 1995 1994 1993 1992 (100) 1991 $/admission 0 California Florida (200) Illinois New York (300) Texas National (400) (500) (600) Hypotheses Hypothesis 1: Hospitals with greater exposures to the BBA tend to decrease RN staffing and increase FTR to a greater degree. – Hospitals under financial stress may trade off profits and quality above profit-maximizing level. – Evidence from previous studies that 30-day AMI mortality worsened in hospitals more affected by BBA. Hypothesis 2: NP and FP hospitals in California do not differ in degree of change in RN staffing or FTR for a similar degree of BBA impact. – According to utility-based models of hospital behavior, NP firms are more responsive to changes in regulated prices under many conditions, but this result does not hold for some profit functions. – Previous work demonstrated no differential impact by FP/NFP hospitals on 30-day AMI mortality. Primary Sources of Data California hospital characteristics from the Office of Statewide Health Planning and Development (OSHPD) from 1995-2001. California patient discharge data to examine deaths from surgical complications. Construction of the BBA Variable Prior to BBA’s implementation, the AHA provided a forecast for every hospital’s Medicare revenues from 1998-2000 under two scenarios: (1) BBA implementation; (2) reimbursement without BBA The difference in revenue under these two scenarios provides us with a plausibly exogenous source of variation in the change in hospital revenue Forecast focuses on changes in reimbursement per admission, not “secondary” effects such as firm’s strategic responses To assess the impact of BBA on patient outcomes, we scale to level of institution, i.e. 1% expected decrease in total firm revenue, rather than $1 expected decrease in Medicare revenue. Hence, our leading measure is: | Forecasted revenues from 1998 to 2000 under BBA - Forecasted revenues from 1998 to 2000 under non - BBA | , [Forecaste d revenues from 1998 to 2000 under non - BBA] scaled by the proportion of Medicare revenues for the hospital in 1997 (pre - BBA). Empirical Strategy 1999-1997 Change Regression of the following form: If c = 1 for revenue change regressions, the impact on actual revenues is very strong. If c is less than 0.5, one major explanation is that firms responded with top-line measures. If c = 1 for operating expense regressions, firms responded with aggressive cost-cutting measures. Figure 5: BBA and Hospital Revenue Response Dependent Variable---------------> Explanatory Variable log[BBA/non-BBA]a Log [Revenue] (1) 0.587362 (0.22324) FP*log[BBA/non-BBA] Log % [Revenue] [Revenue] (2) ** (3) % [Revenue] Revenue / Admission97 Revenue / Admission97 (4) (5) (6) 0.428141 (0.44169) 0.140814 (0.35490) [BBA change]/[non-BBA]b 0.613107 (0.30363) FP*[BBA change]/[non-BBA] ** 0.5036518 (0.53629) 0.092948 (0.40947) [BBA change]/[Admissions1997]c 0.254696 (0.13002) ** FP*[BBA change]/[Admissions1997] R-squared: N: 329 a b c * ** 0.02 0.02 0.01 0.01 0.05 Difference in the natural logarithm of the forecasted revenue under the BBA policy and the log of the forecasted revenue under the non-BBA policy Difference in the forecasted revenue under the BBA policy and the forecasted revenue under the non-BBA policy, divided by the forecasted revenue under the non-BBA policy Difference in the forecasted revenue under the BBA policy and the forecasted revenue under the non-BBA policy, divided by baseline admissions (year 1997) Significant at the 10% level or lower Significant at the 5% level or lower 0.1623242 (0.12299) 1.421067 (1.11632) 0.10 BBA and Hospital Operating Expenses Dependent Variable---------------> Column # Explanatory Variable log[BBA/non-BBA]a Log [Operating Expenses] 1 Log [Operating Expenses] 2 0.2397437 * (0.14336) -0.333348 (0.29203) 0.5325457 ** (0.23585) FP*log[BBA/non-BBA] [BBA change]/[non-BBA]b % [Operating Expenses] 3 0.4970544 ** (0.19824) FP*[BBA change]/[non-BBA] % [Operating Expenses] 4 Operating Expenses / Admission97 5 0.0160219 (0.32526) 0.4877474 ** (0.24436) [BBA change]/[Admissions1997]c -0.0040325 (0.57416) FP*[BBA change]/[Admissions1997] R-squared: N: 329 0.01 0.03 0.02 Operating Expenses / Admission97 6 0.04 0.01 -0.6890022 (0.67179) 1.467882 ** (0.67462) 0.02 Empirical Strategy For patient outcomes, we estimate linear probability models of the following form (the form is similar for hospital-level nurse staffing): Yi β'X i 1 * BBAi 2 * POSTi 3 * ( BBAi * POSTi ) 4 * (OWNERi ) 5 * (OWNERi * POSTi ) 6*(OWNERi * BBAi * POSTi ) i We use dummy variables that proxy for the degree of BBA impact. This is based on division of the magnitude of BBA impact into three groups, low (excluded), middle, and high impact. Results are qualitatively similar to the results involving the continuous variable. Robust errors for clustering. Results Failure-to-rescue Variable Year99 Year00 BBA_MID BBA_MID * Year99 BBA_MID * Year00 BBA_HI BBA_HI * Year99 BBA_HI * Year00 FP FP * BBA_HI FP * BBA_MID FP * BBA_HI * Year99 FP * BBA_MID * Year99 FP * BBA_HI * Year00 FP * BBA_MID * Year00 FP * Year99 FP * Year00 Constant R-squared N Coefficient -0.0064 -0.00034 -0.00213 -0.00416 -0.0152 -0.00225 0.0048 -0.01329 0.00649 -0.01822 -0.01559 0.020114 0.036133 0.039951 0.055005 -0.02353 -0.03322 0.078946 0.1948 130889 Nurse Staffing * * * * ** Variable Year99 Year00 BBA_MID BBA_MID*Year99 BBA_MID*Year00 BBA_HI BBA_HI*Year99 BBA_HI*Year00 FP FP*BBA_MID FP*BBA_HI FP*BBA_MID*Year99 FP*BBA_HI*Year99 FP*BBA_MID*Year00 FP*BBA_HI*Year00 FP*Year99 FP*Year00 Constant R-squared N Coefficient -0.46723 0.02446 -0.46211 0.441297 -0.27738 -0.82616 * 0.623277 -0.03178 -1.31556 1.413058 0.892203 -2.24392 * -2.4639 * -1.33034 -1.84781 1.873551 1.540503 6.59583 ** 0.2001 879 Results (2) FR Year99 Year00 BBA_MID BBA_MID*Year99 BBA_MID*Year00 BBA_HI BBA_HI*Year99 BBA_HI*Year00 FP FP*BBA_HI FP*BBA_MID FP*Year99 FP*Year00 Constant N R-squared RN -0.0093 -0.01401 ** 0.001415 0.005527 0.005784 -0.00356 -0.00792 -0.00793 0.012831 -0.00655 -0.0222 0.000646 0.003902 0.076642 ** 130889 0.19 Year99 Year00 BBA_MID BBA_MID*Year99 BBA_MID*Year00 BBA_HI BBA_HI*Year99 BBA_HI*Year00 FP FP*BBA_MID FP*BBA_HI FP*Year99 FP*Year00 Constant N R-sq 0.178249 0.486571 -0.02614 -0.24126 -0.67702 ** -0.25372 -0.20321 -0.6347 * -0.12838 0.238267 -0.75254 -0.16496 0.122821 6.119017 ** 879 0.2 Discussion We find a relationship between the expected revenue change under BBA and changes in revenue, operating expenses, and operating income. – FP’s more aggressively cut operating expenses relative to NP’s. FP hospitals, relative to NP hospitals, have associated increases in the probability of failure to rescue for a given expected decrease in patient revenue. Nurse staffing in FP hospitals with higher BBA revenue impact decreased to a greater degree than nurse staffing in NP hospitals for similar changes in revenue from the BBA implementation. Some evidence that nurse staffing changes were related to revenue changes for the California hospital sample. In spite of FP-NP differences, not much evidence that failure rate changes were related to revenue changes overall. Future Work Future work will examine NP-FP differences across multiple states and different outcomes, further testing the robustness of our conclusions. Examination of the impact of the BBA on charity care. Examination of NP-FP differences in firm strategies following the BBA. More work on financial distress: e.g. BSM pricing models in publicly traded hospital chains, and Ohlson’s for NP and FP’s. Recent work by others on distress in non-profit firms in general has clarified the direction of research in financially distressed hospitals. Market-level analysis to assess further the welfare implications of the BBA. For example, patients may have been able to identify hospitals least affected by the BBA, and so the law could have had a minimally detrimental effect on quality within the market.