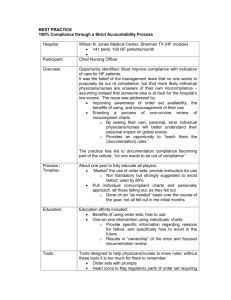
Workforce
advertisement

Workforce Call For Papers Health Workforce Studies - A Profession-Specific Perspective Chair: Jean Moore, State University of New York, Albany Sunday, June 26 • 8:30 am – 10:00 am ●Physician Gender, Physician Marriage and the Supply and Distribution of Medical Services Ann Boulis, Ph.D. Presented By: Ann Boulis, Ph.D., Postdoctoral Fellow, Department of Sociology, University of Pennsylvania, 3718 Locust Walk, Philadelphia, PA 19104; Tel: (215)898-7665; Fax: (215)573-2081; Email: aboulis@pop.upenn.edu Research Objective: To understand how changes in the personal lives and demographic characteristics of US physicians have affected the supply and distribution of medical services. Study Design: Data from the 1980, 1990 and 2000 Census 5 percent samples were used to assess how changes in the representation of women, and changes in the characteristics of physicians’ spouses has affected both overall work effort and the tendency to locate outside of metropolitan areas. First, we track trends in the overall population of physicians in the study years. Then, we create a file of married physicians and their spouses to assess the influence of spousal characteristics on physicians’ work effort and general location. Population Studied: This study focuses on individuals who identify themselves as physicians in the Census and who indicate that they have at least three years of graduate level education. Principal Findings: Although female physicians are less likely than their male colleagues to work for pay, the gender difference in employment is negligible. Between 1980 and 2000, the labor force participation rates of female physicians are consistently over 90 percent and never less than 95 percent of comparable rates for male physicians. Further, while employed women physicians continue to work less per week than their employed male colleagues, the gap in average work effort is closing over time. Between 1980 and 2000, employed female physicians went from working 85 to 90 percent of the average male physicians’ work week. Similarly, over time, the disproportionate tendency for male physicians to locate outside of metropolitan areas is declining. Between 1980 and 2000, male physicians went from being 59 to 35 percent more likely than their female colleagues to locate in rural areas. While the influence of gender per se on the supply and distribution of medical manpower is declining, the effect of marital characteristics on physician work effort is increasing. I find that the total work effort of married physicians is constrained by the labor force participation of their spouses and that, over time, the effect of spousal employment on physician work effort is increasing. In 1980, male physicians with employed spouses worked 0.9 hours less per week and female physicians worked 4.8 hours less per week. By 2000, these differences had grown to 2.3 hours less work for married men and 8.1 hours less work for married women. Similarly, I find a significant and increasingly negative association between spousal education and the tendency to locate outside of a metropolitan area for married male physicians. In 1980, married male physicians whose wives had graduate level education were 81 percent as likely as men whose spouses did not have a bachelor’s degree to locate outside of a metropolitan area. By 2000, men with highly educated wives were only 58 percent as likely as their peers with less educated wives to live in a rural area. Comparable figures for married women physicians were 29 percent in 1980 and 33 percent in 2000. Finally, the frequency with which the spouses of male physicians work for pay increased from 44 percent in 1980 to 58 percent in 2000. The frequency with which male physicians' spouses reported graduate level education also increased significantly during the study period from 24 percent in 1980 to 42 percent in 2000. Conclusions: Increases in the representation of women in the US medical workforce are associated with a decline in the overall supply of medical labor and with a more skewed distribution of medical professionals but over time the extent of these associations is declining. One potential explanation for the declining significance of gender may be the increasing salience of marriage to the work effort and location decisions of male physicians. Implications for Policy, Delivery, or Practice: Although family life issues continue to affect the work related decisions of female physicians more than the decisions of their male colleagues, the spouses of male physicians are having an increasing influence on the location and work effort of male doctors. Greater effort needs to be made to understand the effects of family life on the work effort and location of physicians, and ultimately to incorporate this knowledge into health workforce planning and policy. Primary Funding Source: Macy Foundation ●Applying a Public Policy Approach to Issues of Global Nurse Migration Sat Ananda Hayden, MSN, RN, HSA, Lutchmie Narine, Ph.D. Presented By: Sat Ananda Hayden, MSN, RN, HSA, Doctoral Student in Health Policy, Ph.D. Program in Public Policy, University of North Carolina, Charlotte, 9201 University City Boulevard, Charlotte, NC 28223; Tel: (704)687-6272; Fax: (704)583-4467; Email: sahayden@uncc.edu Research Objective: To identify implicit or explicit policy models that may have shaped current discourse, policies, and practices related to the importation of nurses into the US health care system. Using a variety of perspectives, a number of studies and reports have been done on the phenomenon of nurse shortages and importation of nurses to alleviate projected supply and demand imbalances. In this study we describe these approaches, identify common themes and elements, and develop a comprehensive research model that incorporates the various perspectives. The model can be used to apply and evidenced-based approach to policy decisions. Study Design: This research is a meta-synthesis of existing studies. Studies were identified using major key search terms on Medline, CINHAL, social science citation index, and other health care databases. Published and unpublished papers addressing ethical recruitment of nurses by national and international professional nursing organizations and major institutions were also reviewed. Population Studied: Previous studies on the phenomenon of global nurse migration. Principal Findings: Few studies on global nurse migration have indicated a policy perspective or theoretical approach. However, a number of approaches or views of nurse migration were implicitly apparent in these studies. These included looking at nurse migration as a supply of labor issue, as a moral and ethical dilemma, as perpetuating north versus south human and social capital inequities, as a feminist issue, as a function of migratory push and pull factors, as a free trade issue, as an organizational issue involving work design and work force diversity challenges, as a threat to established professional standards and norms, and as a basic human right issues. The key variables associated with each perspective were identified along with their relevant measures. These were then organized according to context, population, themes and put into a broad model that elucidated their interrelationships. Conclusions: The plethora of existing studies on international nurse migration while being influenced by particular perspectives are not informed by theory and lack a common theoretical research framework. Studies are predominately descriptive rather than analytical. This has in turn limited the usability and applicability of study findings. Implications for Policy, Delivery, or Practice: The development of our comprehensive research can help researchers and policy makers identify a way to better understanding the phenomenon of international nurse migration. For researchers the model provides a common platform from which they can study the impact of nurse migration on health care delivery in general and nursing practice in particular. For policy makers the existence of a common framework or lens through which they can look at international nurse migration can help them to make better sense of the findings from the research literature and so develop policy solutions to nurse shortages in their jurisdictions. For health services administrators the framework can assist in nurse recruitment and retention decision making within their organizations and in particular managing the impact of increasing diversity in their nurse work forces due to international nurses. Primary Funding Source: No Funding ●Who’s Overworked and Who’s Underworked Among Radiologists? Cristian Meghea, Ph.D., Jonathan Sunshine, Ph.D. Presented By: Cristian Meghea, Ph.D., Senior Researcher, Research, American College of Radiology, Email: cristianm@acr.org Research Objective: Concerns about physician shortage or surplus are recurrent in developed nations and we seek to empirically investigate the situation. Typically the “market” for physician services does not clear. For radiology in the United States reasons include: prices are set administratively by insurers; the number of entrants to any given specialty is relatively rigid because all physician training programs tend to guard their trainee slots even when the demand for their graduates is low; and the demand for radiology work is relatively inflexible in the short term because it is not ethical for radiologists to postpone requested work. Similar situations characterize other physician fields and other countries. Also, the usual measure of labor market imbalance, the unemployment rate, is often of little relevance because it is essentially zero. We analyze the radiology labor market using a new measure of shortage/surplus, namely the desire for more or less work if accompanied by a proportional change in income. The desire for less work is an indicator of a shortage, while the desire for more work suggests a surplus. Study Design: Data are from the American College of Radiology’s (ACR) 2003 Survey of Radiologists, a nationally representative stratified random sample survey of all radiologists in the United States. Responses were weighted to make the data representative of all radiologists in the United States. We present overall descriptive statistics and also use multiple OLS regression analysis. Population Studied: All radiologists in the United States. Principal Findings: The net average workload change sought was approximately 0.1 percent of the current workload and not significantly different from zero, indicating that the overall total workload is what is desired. However, radiologists working in academic or government practices were seeking, respectively, 4% and 12% more work while those in private practices sought 2% less work, although radiologists in government practices worked similar hours to radiologists in private groups and those in academic practices worked more hours. In addition, radiologists working in non-metropolitan practices were seeking 3% less work relative to those in large metropolitan areas. Regression results showed that an additional hour worked was associated with a desire for only 0.1 hour greater reduction in workload. Conclusions: There was an overall balance between the demand and the supply of radiologists in 2003. We found some imbalances, including surpluses in academic and government-owned practices, a shortage of radiologists in private radiology groups, and a shortage of radiologists in non-metropolitan areas. There were differences in radiologists’ desired workload by gender, age, and type and location of practice. Implications for Policy, Delivery, or Practice: Concern about whether the supply of physicians in the U.S. is excessive or inadequate is again becoming prominent, with the concern now focusing on a shortage of physicians. Thus it becomes important to have good measures of the surplus or shortage situation, but there are no agreed-upon measures. We introduce what should be a sound and particularly realistic measure, namely, physicians’ desire for change in workload if accompanied by a proportional change in income. We also show that it is a useful and illuminating measure. Primary Funding Source: No Funding ● Title: Supply and Demand in the LPN Workforce: Effects of Scope of Practice, Demographics, and Local Markets Joanne Spetz, Ph.D., Wendy Dyer, MS, Susan Chapman, Ph.D., RN, Jean Ann Seago, Ph.D., RN LPNs in the United States would remedy the national nursing shortage, unless substantial expansions of the scope of practice of LPNs were implemented. Primary Funding Source: HRSA Presented By: Joanne Spetz, Ph.D., Associate Professor, Community Health Systems, University of California, San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: (415)502-4443; Fax: (415)502-4992; Email: jojo@alum.mit.edu Research Objective: Registered Nurse (RN) licenses are conferred after 2-4 years of study and passage of an examination, and Licensed Practical Nurse (LPN) licenses are conferred after 1-2 years of study and passage of an examination. The scope of practice for LPNs varies state-tostate, and this scope of practice affects demand for LPNs. The demographic characteristics of LPNs are different from RNs. This study examines how scope of practice, demographics, and local market characteristics affect demand for and supply of LPNs. Study Design: Scope of practice information was collected from every U.S. state nursing board and was categorized scope of practice according to the breadth of scope of practice, and the specificity with which scope of practice rules are written. Data on employment levels of LPNs and other nursing personnel were obtained from the 2000 American Hospital Association’s Annual Survey of Hospitals. Demand for LPNs was estimated using multivariate regression equations, using instrumental variables to address the potential endogeneity of scope of practice and wages. Multivariate models of the supply of LPNs were estimated using data from the Current Population survey, with supply being a function of individual and family demographics, employment setting, and market factors. The labor supply equations were estimated using two-stage least squares regression to address the potential endogeneity of wages. Population Studied: All hospitals in the United States, and LPNs who responded to the US Current Population Survey. Principal Findings: Demand for LPNs is lower when scope of practice regulations are more restrictive, and to a lesser degree when scope of practice regulations are specific. LPN wages have a negative effect on demand for LPNs, but this effect is not significant when instrumental variables are used to control for the endogeneity of LPN wages. Hospitals with a higher share of Medicaid inpatient days have greater demand for LPNs, as do district and government hospitals. Employed licensed nurses who are male, non-white, or foreign-born work more hours per week and are more likely to work full-time. The presence of children in the household has a negative effect on labor supply. The effect of age is convex. Employed LPNs respond to changes in their own wage by working additional hours per week until a certain wage, after which further increases induce LPNs to work less. Conclusions: Because the education and practice of LPNs is limited, hospitals have relatively little latitude to substitute LPNs for RNs. Many of the same demographic, family and market factors influence LPNs’ and RNs’ decisions of how much to work once working. Implications for Policy, Delivery, or Practice: Employers have limited ability to use LPNs as substitutes for RNs, and LPN decisions on how much labor to supply are similar to those of RNs. Thus, it is unlikely that increasing the supply of ●Can Wage Increases End Nursing Shortages? A Reexamination of the Supply Curve of Registered Nurses Lynn Unruh, Ph.D., RN, Joanne Spetz, Ph.D. Presented By: Lynn Unruh, Ph.D., RN, Health Services Administration Program, University of Central Florida, University of Central Florida, Orlando, FL 32816; Tel: (407)8234237; Fax: (407)823-6138; Email: lunruh@mail.ucf.edu Research Objective: The United States and many other nations are experiencing a severe shortage of registered nurses (RNs), and the shortage is predicted to persist for the foreseeable future. Economic theory indicates that a labor shortage should be accompanied by wage increases, and these wage increases will reduce demand and increase supply, thus bringing the labor market into balance. However, a variety of factors might prevent this neoclassical prediction from occurring: demand may not adjust due to regulations, long-term supply may not increase due to barriers to entry, and short-term supply might not rise if the labor supply curve is backward-bending. This study examines the relationship between the supply of RNs and wages using standard labor supply models and data from the 2000s. The question of whether and to what extent nurses’ labor supply is backwardbending is examined. Study Design: We estimate the supply of registered nurses using the National Sample Survey of Registered Nurses (NSSRN) and the United States Census Bureau – Bureau of Labor Statistics Current Population Survey (CPS). We estimate the equations for all years of the NSSRN (19772000) and ten years of the CPS. We estimate simple supply equations using ordinary least squares regression, controlling for RN and market characteristics. This analysis suffers from two problems. First, the supply of RNs is endogenous with wages, and thus instrumental variables regression must used to correct this problem. Second, the number of hours worked by a RN is predicated on the RN’s decision to work, and thus a correction for this selection should be considered in the analysis. We estimate regression equations using instrumental variables and Heckman selection corrections to address these problems. We pay particular attention to changes in the labor supply function that have occurred over time and the importance of family characteristics. Population Studied: RNs in the United States. Principal Findings: Preliminary equations estimated using the Current Population Survey demonstrates that there is some backward bend in the labor supply of RNs. Conclusions: If the labor supply of RNs is backward-bending, wage increases may not increase the short-term supply of nurses. The extent to which this might be true depends on the exact relationship between wages and supply. However, the long-term supply of RNs might be positively affected by wage increases. Thus, although the short-term effect of wage increases might not be an abatement of the shortage of RNs, the long-term effect could be resolution of the disequilibrium in this labor market. Implications for Policy, Delivery, or Practice: In the short term, policymakers and employers should not expect wage increases to improve the national shortage of RNs. However, in the long term these wage increases will induce more people to enter the nursing profession, thus remedying the shortage. Primary Funding Source: California Employment Development Department Call for Papers Health Workforce Studies: An Organizational Perspective Chair: Bob Konrad, University of North Carolina, Chapel Hill Sunday, June 26 • 3:30 pm – 5:00 pm ●Clinical Staffing on Labor and Delivery Units in California Ida R. Shihady, MPH, Linda Burnes Bolton, DrPh, RN, FAAN, Moshe Fridman, Ph.D., Lisa M. Korst, Ph.D., Paula Broussard, RN, RDMS, Kimberly D. Gregory, M.D., MPH Presented By: Kimberly D. Gregory, M.D., MPH, Director, Maternal Fetal Medicine, Obstetrics and Gynecology, CedarsSinai Medical Center, 8700 Beverly Boulevard, Suite 160W, Los Angeles, CA 90048; Tel: (310) 423-5420; Fax: (310) 4230140; Email: gregory@cshs.org Research Objective: Mandated nurse-to-patient ratios have been put forth as key ingredients for improving the quality and safety of care. The majority of these directives are based on data obtained from medical/surgical, and critical care units. While obstetrical admissions are the most common cause of hospital admissions in the United States, literature on the application of staffing standards and the organization of care on L&D is limited. The current study describes the clinical staffing and organizational structure employed by L&D units in California, and utilizes a measure of unit activity to describe variation in nurse staffing among hospitals. Study Design: We interviewed L&D nurse managers at hospitals reporting more than 50 deliveries during 2002 in a structured telephone interview. Information collected included daily patient flow, number of nurses and hours per shift, staffing models, clinical management of low and high-risk patients, and type of health care personal available. We measured unit activity by combining same day patients, admissions, discharges/transfers, and midnight census. Nurse-to-patient ratios were calculated by comparing the unit activity measure to a self-reported average number of RNs per 12-hour shift. We classified hospitals into low (first quartile), average (middle quartiles), and high (fourth quartile) staffing levels. We present summaries of staffing patterns, organizational factors, and clinical policies by delivery volume, stratified into quartiles (Q1 = <750, Q2 =750-1699, Q3 = 17002759, and Q4 = >2760 deliveries per year). Staffing level association to hospital characteristics (region, delivery volume, ownership, and teaching status) are examined. Population Studied: California hospital L&D nurse managers Principal Findings: We surveyed 225 (84%) out of 268 eligible hospitals. Most hospitals use 12-hour nursing shifts, and budget staffing based on acuity; however high volume hospitals are more likely to use both 8- and 12-hour shifts. Almost all hospitals use a call system or rely on supplemental staff to meet staffing ratios. About 50% of hospitals were staffed with a 1:2 nurse-to-patient ratio or better; 18% had a ratio of 1:3 or worse. Northern CA hospitals and low volume hospitals were significantly higher staffed compared with Southern CA and Los Angeles area hospitals (p=0.003) and high volume hospitals (p<.0001), respectively. Ownership and teaching status were not associated with nurse staffing ratios. High-risk patients are more likely to be managed on L&D, except in high volume hospitals where a “special” unit is common. High volume hospitals are more likely to have >10 MD’s and access to a Maternal Fetal Medicine specialist. Availability and use of unit secretaries, scrub techs, doulas, midwives, residents, and anesthesiologists varies widely. Conclusions: L&D units in California approach nurse staffing in a consistent manner. Other structural variables such as use of ancillary personnel and clinical setting for different levels of patient acuity vary and are associated with hospital volume, as is nurse staffing by unit activity. Implications for Policy, Delivery, or Practice: Staffing patterns and organization of care on L&D units vary. Additional research is needed to understand whether this variation is associated with birth outcomes, and to determine best practices for ideal outcomes. Primary Funding Source: AHRQ ●The Impact of Organizational Changes on Supply and Demand for Intensivist Services Atul Grover, M.D., Ph.D., Tim Dall, MS, Jim Cultice, MS Presented By: Atul Grover, M.D., Ph.D., Senior Consultant, The Lewin Group, 3130 Fairview Park Drive, Suite 800, Falls Church, VA 22042; Tel: (301)526-3883; Fax: (301)897-5810; Email: HealthPolicy@jhu.edu Research Objective: The aging and expansion of the population will increase demand for health care in the US, including demand for critical care (intensivist) physicians. A growing body of literature supports the use of intensivists as a way to improve patient outcomes in intensive care units. This model of care has been encouraged by public and private organizations whose goal is to improve quality of care. Subsequent changes to the delivery and organization of care in the ICU will significantly alter the current and future demand for physicians trained in critical care. Our study assesses the adequacy of the supply of practicing intensivists through 2020. Study Design: The Physician Supply and Demand Models of the National Center for Health Workforce Analysis were adapted to project the supply of, and demand for, adult intensivists. The number of practicing intensivists is projected based upon new entrants and losses from the critical care workforce. Demand projections are modeled using information about population growth and aging, insurance status, and changes in science and technology. In addition, changes in the organization and delivery of critical care services are modeled based upon the literature linking intensivist staffing patterns to quality of care. Population Studied: Practicing US intensivists from 20002020, including domestic and international medical graduates. Practice data obtained from AMA Masterfile and physician surveys. Principal Findings: Based on evidence supporting intensivistdirected care for ICU patients, two thirds of patients may be receiving less than optimal care today. Even if only half of ICU patients are cared for by full time intensivists, it implies a current shortage of 1,200 intensivists, about 25% of current supply. This is projected to exceed 2,000 by 2020 if current trends continue. Conclusions: The evolving standard of care for ICU patients indicates that utilization patterns are changing towards greater use of intensivists, moving the US closer to an optimal standard of care, and suggesting that applying current utilization patterns to future populations underestimates the growth in demand for intensivists. After taking this into account, the projections suggest an inadequate supply of physicians trained in critical care at the present time with a growing shortage over the coming decade. Implications for Policy, Delivery, or Practice: While the proportion of hospitals whose critical care is directed by intensivists has doubled over the last several years in response to studies linking staffing to quality of care, many hospitals and communities will not be able to achieve this standard of organization of care because of an inadequate supply of intensivists. This shortage is likely to be severe by 2020, when the aging population will consume a far greater volume of critical care services. Moreover, the lack of practicing intensivists will disproportionately affect patients who are already underserved. Major changes will need to occur to ensure an adequate supply of intensivists and their ability to deliver the highest quality of care in the ICU. Primary Funding Source: HRSA ●Staffing Patterns and Vacancy Rates of the Nation’s Federally Funded Rural Health Centers Gary Hart, Holly Andrilla, Roger Rosenblatt Presented By: Gary Hart, Director and Professor, Department of Family Medicine, Rural Health Research Center & Center for Health Workforce Studies, University of Washington, University of Washington, Box 354982, Seattle, WA 981954982; Tel: (206)685-0402; Fax: (206)616-4768; Email: ghart@fammed.washington.edu Research Objective: Federally funded health centers (HCs) have been at the core of the U.S. federal government’s safety net system. The current administration has made a commitment to expand the size and number of HCs. The level of success of this expansion will depend on the ability of these centers to recruit and retain qualified health care providers. The objective of this study is to describe the staffing patterns of federally funded HCs and to determine which types of rural clinics have the highest vacancy rates. Study Design: A 2004 survey of HC grantees yielded an overall response rate of 79%, with a rural center response rate of 98%. Survey data were linked to BPHC Uniform Data System and other demographic and provider data. Weights were created to make the respondents nationally representative. SUDDAN was applied to adjust standard errors. Population Studied: All the 846 federally funded 330 health clinic grantees (e.g., community health clinics and migrant health clinics) that were clinically operational during 2003 constitute the study population (over 4,800 sites). Principal Findings: HCs vary greatly in their size and the complexity of their workforces. Family physicians (FPs) (3,072) represent half of all HC physicians. There are 3,286 NPs and PAs; 1,491 dentists; and 3,389 RNs employed by HCs. HC vacancy rates vary greatly by their location and characteristics. Rural rates are higher for most professions than for their urban counterparts, with RNs being an exception. Vacancy rates are highest for physicians, dentists and RNs. Vacancy rates for FPs are 12% for urban, 12% for large rural, 19% for small rural, and 18% for isolated small rural locations while the comparative rates for NPs are 9%, 7%, 8%. Rural HCs located in persistent poverty counties had dentist vacancy rates that were about 10 percentage points higher than those who were not so located. Over a quarter of the physician staffing of HCs (over a third in rural HCs) is made up of NHSC scholarship, NHSC loan, state loan, and J-1 physicians who are currently working off their program obligations. Rural high vacancy rate HC directors indicate that expansion of programs that increase NHSC slots, residency slots, visibility of HCs during training, and minorities graduating will help them recruit and retain providers better. Conclusions: This study shows that many of the nation’s HCs, especially rural HCs, face substantial challenges in recruitment of provider staff. High vacancy rates are strongly associated with their locations and characteristics. HC staffing is heavily dependent on federal programs such as the NHSC and J-1 visa waivers. Implications for Policy, Delivery, or Practice: This study is important to help identify the barriers to recruitment and retention of HC workforce. The study results can be used to identify and target appropriately tailored therapeutic interventions to those HCs where they are needed most. The results are not only relevant to federal policy makers and program managers but to those at the federal and state level who are responsible for planning and provider training. Primary Funding Source: No Funding ●The Influence of Organizational Culture on Physician and Nurse Resignation Rates David Mohr, Ph.D., Mark Meterko, Ph.D., Gary Young, JD, Ph.D., Martin Charns, DBA Presented By: David Mohr, Ph.D., Health Services Researcher, VA Boston Healthcare System (152M), Department of Veterans Affairs, 150 South Huntington Avenue, Boston, MA 02116; Tel: (617)232-9500-5679; Email: david.mohr2@med.va.gov Research Objective: The influence of organizational culture was examined as it related to facility-level resignation rates for physicians and registered nurses. Numerous studies have used employee attitudes to explain individual turnover intention and behavior, however, few studies have examined the influence of group-level factors such as organizational culture on actual facility-level resignation rates in health care organizations. Study Design: A job satisfaction survey was administered to a census of employees of the Veterans Health Administration (VHA) during the spring of 2004, this included a battery of 14 items based on the Zammuto and Krakower model of organization culture. This measure yields culture dimension scores for: group, entrepreneurial, bureaucratic and rational. Following common practice, we combined the scores for the group and entrepreneurial dimensions. Nation-wide 5,485 (38%) physicians and 18,954 (49%) registered nurses responded to the survey. Culture scores for these respondents were aggregated to the facility-level for both the physician (n=112) and nurse (n=127) cohorts. These scores were then matched to a database containing facility-level resignation rates for the fiscal year the survey was conducted. Separate doctor and nurse hierarchical regression analyses were then conducted to examine the ability of group/entrepreneurial and bureaucratic culture to explain the resignation rates for the two professional groups. Because resignation data was proportional with a restricted range, an arcsine transformation was applied for regression models. In each analysis, four dichotomous control variables were entered into the model first: large hospital staff size, small hospital staff size, teaching status, and urban location. Population Studied: Physician and registered nurses in a cross-national sample from The Veterans Health Administration. Principal Findings: The median facility-level resignation rate was 7% for physicians and 5% for registered nurses. Group/entrepreneurial culture significantly improved the percent of variance accounted in facility-level resignation rates in a stepwise regression models for both professional groups. For physicians, the combined group/ entrepreneurial culture scale explained an additional 3% of the variance (p<.05) in turnover rates above the organizational covariates (model adjusted r2 = .10). In the model with nurses, group/entrepreneurial culture explained an additional 4% of the variance (p<.05) beyond that accounted for by the organizational covariates (model adjusted r2 = .06). Bureaucratic culture did not explain incremental variance in resignation rates for either professional group. For covariates, teaching affiliation was positively related to resignation rates for physicians and a large hospital characteristic was negatively associated with nurse resignation. The difference in resignation rates at facilities with the highest 25% and lowest 25% combined group/entrepreneurial culture was 1% (p =.18) for nurses and 3% (p<.01) for physicians. Conclusions: Group/entrepreneurial culture was negatively related to facility-level resignation rates after controlling for size, teaching affiliation and urban status. Organizations with higher scores on this culture dimension experienced lower resignation. A difference in turnover rates of 3% for physicians and 1% for nurses between facilities at the highest and lowest quartiles for group/entrepreneurial culture can be a source of significant costs in recruitment for highly skilled professions. Implications for Policy, Delivery, or Practice: Physicians and nurses are less likely to resign at facilities with higher levels of group/entrepreneurial culture. Efforts to increase group/entrepreneurial-oriented organizational culture may yield benefits to skilled workforce retention. Primary Funding Source: VA ●Increasing the Supply of Certified Nursing Assistants Holly Rodin, Doctoral Candidate, M.P.A. Presented By: Holly Rodin, Doctoral Candidate, M.P.A., 2997 Chatsworth St N, Roseville, MN 55113; Tel: (651)490-5035; Email: rodi0016@umn.edu Research Objective: To estimate the effect of wages increases and availability of Employer Sponsored Insurance on the probability of working age adults choosing work as Certified Nursing Assistants and on the number of hours worked as a Certified Nursing Assistant in healthcare. Study Design: A maximum likelihood probit estimation with selection is used to estimate the probability of working as a Certified Nursing Assistant as annual wages and offers of Employer Sponsored Insurance change. A Heckman selection model is used to estimate how hours worked as a Certified Nursing Assistant change based on changes in annual wages and availability of Employer Sponsored Insurance. Recycled probability methods are used to estimate adjusted rates of change as wages and offers of Employer Sponsored Insurance increase. Selection corrected wages are predicted for all observations. A two-sample estimation method is used to predict the probability of being offered Employer Sponsored Insurance, using the Medical Expenditure Panel SurveyHousehold Component for the years 1996-2001. Population Studied: Current Population Survey-Annual Demographic Survey respondents, age 15 to 64, who are employed as well as those respondents not working for reasons other than disability or retirement. A pooled dataset (1996 to 2002 of the Current Population Survey-Annual Demographic Survey) with a sample size of 628,290 is used for this analysis. Principal Findings: Findings indicate that Certified Nursing Assistants have a positive, inelastic response to wage increases, increasing the probability of working as a Certified Nursing Assistant between .3% and 1.1. Hours worked would decrease as wages increase, ranging from –1.6% to -4.8%. Increasing offers of Employer Sponsored Insurance would increase the probability of working as a Certified Nursing Assistant by 2.3% as well as increasing hours worked by 6.4%. Conclusions: Increasing the offer of Employer Sponsored Insurance would have the largest positive impact on increasing the probability that workers will work as Certified Nursing Assistants in healthcare, as well as increasing the number of hours worked. Wage increases would increase the probability that workers will become Certified Nursing Assistants, but hours worked would decrease, resulting in a net decrease of Certified Nursing Assistants working in healthcare. A combination of wages and offers of Employer Sponsored Insurance would result in the largest net gain in the number of Certified Nursing Assistants, although the estimates of the percentage increase in workers is still far below the number projected to meet the increased demand for these services. Implications for Policy, Delivery, or Practice: State Medicaid agencies and the federal Centers for Medicare and Medicaid Services are devoting resources to address the current shortage of Certified Nursing Assistants, especially in long term care. This analysis provides policy makers with a set of estimates that indicate that a combination approach of wage increases and offers of Employer Sponsored Insurance could out perform policies that only consider wage increases. As the demand for these health services increases in the future, and the potential pool of workers decreases, additional resources will need to be devoted to ensure adequate staffing in order to provide quality care for the elderly. Primary Funding Source: AHRQ Related Posters Poster Session A Sunday, June 26 • 2:00 pm – 3:15 pm ●Public Perception of Adequacy of Physician Supply Holly Biola, M.D., Donald E. Pathman, M.D., MPH Presented By: Holly Biola, M.D., NRSA Primary Care Research Fellow, Family Medicine, UNC- Chapel Hill, 2507 West Woodrow Street, Durham, NC 27705; Tel: (919)843-4818; Fax: (919)966-0536; Email: hollyrose@unc.edu Research Objective: Increasing physician supply may not enhance people’s sense of their access to health care if perception of physician supply is based on factors other than number of physicians in their area. Our aim is to assess how closely people’s perceptions about the adequacy of the local physician supply relate to actual numbers of physicians in their county, and to identify which other factors are associated with perception of an adequate physician supply. Study Design: A telephone survey consisting of 89 questions about demographic, attitudinal, care utilization, and access-tocare measures was fielded from November 2002 to July 2003 in 150 rural counties of 9 states in the U.S. Southeast as part of the evaluation of the Robert Wood Johnson Foundation’s Southern Rural Access Program. These analyses focus on the question, How much do you agree with the statement:“I feel that there are enough doctors in my community.” and its association with demographic, attitudinal and county variables. Bivariate logistic regression and multivariable logistic regression analyses were used. All analyses were weighted to adjust for demographic group response likelihood. Population Studied: Participants were English- or Spanishspeaking adults 18 years and older who had lived for at least a year at their current residence. They were reached via random-digit dialing to exchanges within study counties. The overall response rate to the survey was 51.0%, with 4,879 participants and 4,682 refusals. Principal Findings: About half (54.4%) of respondents felt there were enough doctors in their communities. Respondents in areas with lower physician densities (1 physician per > 3,999 people) were significantly less likely to feel that there were enough doctors in their community than people in areas with high physician densities (1 physician per < 1,000 people) (49.2% vs. 59.4%; p= .006). Although physician-to-population ratios were significant correlate of perceived physician supply adequacy, other characteristics had stronger associations. People significantly more likely to feel there were enough physicians in their communities were those over 65 years old, male, white, in good health, had more confidence and satisfaction in their physicians, did not find cost of care a problem, typically traveled less than 30 minutes to care, and lived in counties with lower proportions of racialethnic minorities and poverty. The strongest correlate of believing that there are enough doctors in one’s community was the attitude that people should not go to doctors except as a last resort (p <.001; O.R.=2.03; CI95=1.63-2.53). Conclusions: People who live in areas with lower physician densities are more likely to perceive that there are too few physicians; however people’s attitudes about and experiences with health care are also strongly correlated with perceived doctor shortages. Implications for Policy, Delivery, or Practice: Current efforts to increase physician supplies in rural areas might succeed in increasing physician numbers but still not eliminate the perception that there are too few physicians. If the goal is for people to feel that there are enough physicians locally, interventions will also need to address people’s satisfaction with and confidence in their physicians, cost, and other barriers to care. Primary Funding Source: HRSA ●RN Satisfaction: Evidence from the National Database of Nursing Quality Indicators Diane K. Boyle, Ph.D., Peggy A. Miller, MS, Byron Gajewski, Ph.D., Nancy Dunton, Ph.D. Presented By: Diane K. Boyle, Ph.D., Associate Professor, School of Nursing, University of Kansas, 3901 Rainbow Boulevard, MS 4043, Kansas City, KS 66160; Tel: (913)5881686; Fax: (913)588-8737; Email: DBOYLE@kumc.edu Research Objective: Job satisfaction is crucial to retention of RNs and therefore provision of quality patient care. Given the growing shortage of RNs, hospital executives, policy makers, and regulatory bodies are challenged to improve the work environment for nurses. We examined the differences among types of patient care units in acute care hospitals on Registered Nurse (RN) job satisfaction, satisfaction with work environment, perceived quality of care, and intent to stay on the job. Study Design: Data for this descriptive correlational study were collected in a 2004 RN survey, which was primarily webbased. Hierarchical linear models were used to assess differences across unit types. A random effect for hospital was included, which allowed units within the same hospital to be correlated. Population Studied: The population studied was RNs working as direct care providers in acute care hospitals in the United States. The sample included >75,000 RNs in >5,000 nursing care units in 206 hospitals across the country. Member hospitals of the American Nurses Association’s National Database of Nursing Quality Indicators choose to participate in the annual survey. Eligibility criteria included full or part-time RNs, regardless of job title, who spend a minimum of 50% of their time in direct patient care and have been employed a minimum of 3 months on the current unit. RNs working on all types of patient care units were eligible, including critical care, step-down, medical-surgical, maternalnewborn, neonatal, pediatric, psychiatric, rehabilitation, surgical services, ambulatory care, and the emergency department. The hospitals represented 44 states, 90% are general hospitals, 43% have achieved Magnet designation by the American Nurses Credentialing Center. Principal Findings: Significant differences existed among types of patient care units on RN satisfaction with specific job aspects, including task, RN-RN interaction, RN-MD interaction, decision-making, autonomy, professional status, and pay; on RN satisfaction with aspects of the work environment, including professional development, nursing management, and nursing administration; and on general job enjoyment. Significant differences were also found among types of patient care units on perceived quality of care delivered and intention to stay on the job. Conclusions: Unit environment significantly impacted RN job satisfaction. It is important to go beyond the hospital level to a unit level analysis to understand RN job satisfaction, quality of care, and intention to remain on the job. Implications for Policy, Delivery, or Practice: These results will assist policymakers and hospital administrators design targeted, effective interventions to improve RN work environments of different types of units. Primary Funding Source: No Funding Source ●Does the Market Value Racial and Ethnic Concordance in Timothy Brown, Ph.D., Richard M. Scheffler, Ph.D., Sarah Tom, MS, MPH, Kevin Schulman, M.D., MBA Presented By: Timothy Brown, Ph.D., Associate Director of Research, Petris Center - School of Public Health, University of California at Berkeley, 2150 Shattuck Avenue, Suite 525, Berkeley, CA 94720-7380; Tel: (510)643-4103; Fax: (510)6434281; Email: tbpetris@berkeley.edu Research Objective: To determine if the market places an economic value on racial/ethnic concordance in potential physician-patient relationships. Study Design: Using SUDAAN, population-averaged regression models with area fixed effects were used to estimate the determinants of earnings per hour for physicians in a two-period panel (12,886 observations). Controls for physician characteristics and area population characteristics were included. Various interactions between the race/ethnicity of the physician and the race/ethnicity of the local population were performed. Population Studied: Physicians from the 1998-1999 and 2000-2001 Community Tracking Study Physician Surveys Principal Findings: Black physicians are paid approximately 5.6% more in earnings per hour than non-Black physicians for every percentage point increase in the percentage of the population that is Black and insured by Medicaid or other public insurance. Hispanic physicians are paid 1.2% more in earnings per hour than non-Hispanic physicians for every percentage point increase in the difference between the percentage of the population that is Hispanic and the percentage of physicians who are Hispanic. Conclusions: While neither Black nor Hispanic physicians earn more than non-Black or non-Hispanic physicians when comparing simple means, both Black and Hispanic physicians earn more when practicing in areas where the degree of potential racial/ethnic concordance between physicians and patients is lower than the potential demand for such relationships. This suggests that there are shortages of Black and Hispanic physicians in such areas. Implications for Policy, Delivery, or Practice: Additional Black and Hispanic physicians should be trained in order to reduce current shortages. Primary Funding Source: WKK ●A Geographic Analysis of Dental Schools, Dental Graduates, and Residential Status of Dental School Enrollees Gayle Byck, Ph.D., Linda M. Kaste, DDS, Ph.D. Presented By: Gayle Byck, Ph.D., Deputy Director, Midwest Center for Health Workforce Studies, University of Illinois at Chicago, 1747 West Roosevelt Road, Room 558, Chicago, IL 60608; Tel: (312)355-4761; Fax: (312)355-2801; Email: gbyck1@uic.edu Research Objective: The purpose of this study is to provide descriptive data on the presence of dental schools, dental school graduates, in-state enrollment and interstate dental education agreements for states in the United States. This information about the dental education pipeline may be helpful to states deciding to open or maintain a dental school., as well as to policy makers addressing dentist workforce, supply and education. Study Design: Using data from the American Dental Association, American Dental Education Association, and US Census Bureau, cross-sectional comparisons were made for dental schools (presence of, public versus private), graduates (1990-2000), and residential status of dental school enrollees (1998-2000) for the following geographic levels: state, Census division, and Census region. Population Studied: Dental school enrollees (1998-2000), and dental graduates (1990-2000) by state and Census division and region. Principal Findings: In 2000, there were 54 dental schools, in 35 states. There were 43,289 dental school graduates during 1990-2000, with little fluctuation by year. Over half (56%) of the graduates were from public schools. The distribution of schools and graduates differed by geographic region. The South had the largest unadjusted number of graduates; however, the Northeast graduated the largest number of dentists per capita. Over 80% of residents in most Census divisions stayed in their division for dental school, while residents in the Mountain division/West region needed to look outside their geographic area for dental school opportunities. The Mid-Atlantic schools were the most “national” in terms of student enrollment, while the West South Central and Pacific schools attracted enrollees mainly from their geographic areas. Schools and states without dental schools varied considerably in their reliance on interstate agreements. There appeared to be an inverse relationship between dentist supply and in-state enrollment. Conclusions: US states vary widely on the number of dental schools, dentists, dental school graduates, and residential status of first year dental school enrollees. Further assessment on additional factors such as dental health provider shortage areas and state oral health status is needed to more fully view the impact of these factors. Implications for Policy, Delivery, or Practice: With many states facing dentist shortages in many counties and an aging dentist workforce, the importance of having an in-state dental school and/or interstate agreements on the future supply of dentists for a state is an area of interest. The state and regional-level data presented here on dental school enrollees and graduates, and dentist supply, contribute to current ongoing discussions about the dental workforce, the future of dental education, and access to oral health care. Primary Funding Source: HRSA ●The Allied Health Workforce: Out of the Shadows and into the Spotlight Susan Chapman, Ph.D., RN, Edward H. O'Neil, Ph.D., MPA, Wendy Dyer, MS, Vanessa Lindler, MA Presented By: Susan Chapman, Ph.D., RN, Assistant Adjunct Profesor, Social & Behavioral Sciences and Center for Health Professions, University of California, San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: (415) 502-4419; Fax: (415) 476-4113; Email: susanac@itsa.ucsf.edu Research Objective: The health care industry’s focus on the nursing shortage has overshadowed a growing and significant shortage of allied health workers. These workers provide the bulk of diagnostic, therapeutic and direct care in hospitals, nursing homes and in the home. Position vacancy rates range between 8% -15% although there is inconsistent measurement and variability in demand by geographic and health care setting. Previous studies have documented the supply of and demand for allied health professionals but they have been largely regionally or profession-specific. The objective of this project was to use secondary data to identify supply and demand trends nationally and to assess state and regional variations in the production of and need for greater numbers of workers now and in the next decade. Study Design: Data were collected, summarized, and trended using a variety of secondary sources. The Current Population Survey (CPS) 1998-2003 was used to assess demographic characteristics; the BLS (OES) and Census for the number of workers per population in each state and the U.S., the AMA Health Professions Education Directory (1997-2003) for the number of program graduates, the BLS for quarterly job openings, and a review of literature, previous HRSA workforce reports, and key informant interviews. Population Studied: (1) Allied health occupations ranging from entry level nurse aides to masters prepared physical and occupational therapists (2) Accredited allied health educational programs in the U.S. Principal Findings: The U.S. average number of allied health workers to population is 21.4/1000, with state averages ranging from 16.7 to 30/1000. Graduation rates have been flat for 8 years. Many states produce too few graduates to meet demand for open positions e.g., California graduates 500 radiologic technologists for over 700 new positions per year. Key informants indicate that recruitment suffers due to relatively low wages and lack of career advancement opportunities. Conclusions: An aging population and the pending retirement of current allied workers will create a greater demand for increased production of allied health workers. The technical fields continue to grow and specialize as new technology in imaging and the clinical lab have created the need for new technicians. A new infusion of support for community colleges and baccalaureate programs is critical to maintain access for entry level and career ladder students. Implications for Policy, Delivery, or Practice: Increased funding support is needed at the community college and baccalaureate level to increase the capacity of allied health educational programs. Labor-management partnerships to promote career development for incumbent workers may be a successful approach to reduce turnover and encourage new entrants to the allied health field. Primary Funding Source: The California Endowment and the CaliforniaHealthcare Foundation ●Advanced Practice Nurses in Genetics: A Workforce That Can Increase Access to Genetics Services Judith Cooksey, M.D., MPH, Dale H. Lea, RN, MPH, CGC, APNG, FAAN, Gaetano Forte, BA, Patricia A. Flanagan, MA, Janet Williams, RN, CGC, NP, Ph.D., Miriam Blitzer, Ph.D. Presented By: Judith Cooksey, M.D., MPH, Faculty, Department of Epidemiology and Preventive Medicine, University of Maryland School of Medicine, 660 West Redwood Street, Baltimore, MD 21201; Tel: (410) 706-1277; Email: jcookseyumuic@aol.com Research Objective: Despite new genomics advances each year, the US has few genetics specialists, and limited capacity to produce new professional entrants. Advanced practice nurses (APNs) in genetics are one of only three recognized genetics specialty groups; the others are medical geneticists (1,600 MDs and PhD geneticists) and genetic counselors (about 2,000). Nurses in genetics are the least studied and smallest group. An ongoing problem is limited genetics content in general nursing educational curricula; and the paucity of master’s or doctoral level nurse education programs in genetics. The major organization for APNs in genetics is the International Society of Nurses in Genetics (ISONG); membership is open to all nurses. ISONG has advanced the profession and recently developed a new credential for nurses with demonstrated competency in genetics. This study describes the professional roles of ISONG members in an effort to better inform overall genetics workforce planning. Study Design: Confidential written survey of all US members of ISONG, conducted in July 2004. The survey included 49 questions on demographics, education and credentials, professional activities, patient care, and perspectives. The study had IRB approval by UMB and NYSDOH. Population Studied: All US nurses who were ISONG members in July 2004. Response rate was 72% (211 of 293 ISONG members); results reported for 201 professionally active nurses. Principal Findings: Respondents are predominantly women (98%), white (94%) with a median age of 51 years. There is high educational attainment, almost 40% have a doctoral degree and 95% have a master’s degree. Primary work settings are diverse: colleges of nursing 32%, hospitals/associated clinics 18%, government 17%, academic health centers 16%, clinics/physician offices 7%, and other settings 12%. In aggregate, professional time is distributed among teaching 26% of time, direct patent care 24%, research 23%, administration 17%, public health/community health 10%, and other activities 2%. About 67% of respondents have direct patient care in clinical areas of genetics 26%, oncology 22%, pediatrics/neonatal 13%, family/adult 13%, womens health 8%, and other areas 18%. Genetics-related services include family history & analysis, genetic counseling, physical exam, psychosocial counseling, and care coordination. Average genetic-related patient care volume is 180 new and 220 follow-up patient visits per year. About 20% of respondents list their primary position as a researcher or research coordinator, with varied research fields. A majority of respondents had no formal genetics courses or clinical rotations during their graduate studies; often undertaken in the 1970s and 1980s. A majority rate current genetics educational opportunities for advanced nurse education as fair or poor. Conclusions: APNs in genetics have divers roles and responsibilities, with almost equal time distributed among teaching, research, and patient care. There are and have been insufficient genetics-specific advanced educational opportunities for nurses, possibly contributing to small numbers of younger APNs in genetics. Implications for Policy, Delivery, or Practice: APNs in genetics provide complementary professional roles and patient care services to those provided by physicians, medical geneticists, and genetic counselors. Expansion of this nurse specialty workforce could help impprove access to genetic services. However, there is a serious need to expand geneticsspecific training and educational programs for nurses. Primary Funding Source: HRSA, NHGRI - ELSI Program ●Evaluating Variations in Individual Nurse Workload Perceptions in Relationship to Regulatory Mandates Karen Cox, Ph.D, Shelly C. Anderson, MSN MBA, Susan L. Teasley, BSN, Cathryn A. Carroll, Ph.D. Presented By: Karen Cox, Ph.D., Senior Vice President, Patient Care Services, Children's Mercy Hospitals and Clinics, 2401 Gillham Road, Kansas City, MO 64108; Tel: (816)2343933; Fax: (816)346-1333; Email: kcox@cmh.edu Research Objective: To evaluate (1) state specific variations in individual nurse workload perceptions and (2)compare workload perceptions for nurses employed in states with and without regulatory mandates. Study Design: A cross-sectional evaluation of individual nurse workload perceptions. Data specific to demographic and institutional information was obtained in addition to nurse workload perceptions through the completion of the validated Individual Workload Perception Scale. Univariate statistics were used to compare mean values of workload perceptions. Population Studied: A convenience sample of over 4,000 nursing professional located throughout the United States. Principal Findings: State variations were observed in individual nurse workload perceptions with nurses employed in some states having worse perceptions of workload than nurses employed in other states. The adoption of regulatory strategies to improve nurse workload appear to have been effective with statistically significant differences in workload perceptions being observed in states with and without mandatory ratios, mandatory staffing plans, mandatory overtime and right to work states. Conclusions: State specific variations in nurse workload perceptions do occur and regulatory tools used to improve nurse workload do appear to have some effect. Nurse managers must be aware of regional variations in workload perceptions. Implications for Policy, Delivery, or Practice: As nurse professionals advocate for the adoption of regulatory interventions to improve nurse workload, specific consideration should be given to the adoption of mandatory staffing plans prior to the adoption of alternative regulatory interventions such as mandatory ratios, right to work legislations, etc. Primary Funding Source: No Funding Source ●All Physicians are not Created Equal: Supply and Demand Projections for 19 Physician Specialties Tim Dall, MS, Atul Grover, M.D., Ph.D., Jim Cultice, MS Presented By: Tim Dall, MS, Vice President, Applied Economics, The Lewin Group, 3130 Fairview Park Drive, Falls Church, VA 22042; Tel: (703) 269-5743; Fax: (703) 269-5503; Email: tim.dall@lewin.com Research Objective: Recent reports have reflected a growing concern over the potential shortage of physicians in the US. However, analyses and commentaries have focused on the adequacy of the aggregate number of physicians; more specific studies usually examine total numbers of specialists or generalists, but not particular specialties. This study attempts to assess the adequacy of the physician workforce for nineteen individual physician specialties through 2020. Study Design: The Physician Supply and Demand Models of the National Center for Health Workforce Analysis were used to project the supply of, and demand for, 19 physician specialties. The number of practicing physicians is projected based upon new entrants and losses from the workforce while demand projections are modeled using information about population growth and aging, insurance status, and changes in science and technology. Specialty-specific physician-topopulation ratios are also examined which reflect trends in provider availability. Population Studied: Practicing US physicians from 20002020, including domestic and international medical graduates. Physician practice and utilization data were obtained from the AMA’s Physician Masterfile, their Socioeconomic Characteristics series, and the National center for Health Statistics. Population projections came from the US Census Bureau. Other supply and demand determinants were incorporated based upon findings from the physician workforce literature. Principal Findings: Aggregate physician supply is likely to meet the demands of a growing and aging population until close to 2017, when the number of exits from the physician workforce will begin to exceed the number of new physicians under current conditions. However, the number of physicians in some specialties, particularly those serving the elderly, will be inadequate to meet demand for physician services given current utilization patterns. Physician-to-population ratios adjusted by primary population served (e.g., OB/Gyn to female ratio) reveal widely varied results. The ratio of OB/Gyns to target population will grow by 21% and for general pediatricians will increase by 15%, which may indicate a future surplus of these specialists. However, the ratio of cardiologists to target population will fall by 28%; the provider to population ratio for other internal medicine subspecialties will also decline by 23%, which point to a shortage of these providers in the next 15 years. Conclusions: While some authors have suggested that there will be national shortage of physicians or of all physician specialists, this is not likely to occur given current practice and utilization patterns. However, those specialties which care primarily for elderly patients may not be able to meet demand for their services given current conditions. Other specialties, particularly those caring mostly for younger patients, are unlikely to experience significant shortages in the next 15 years. Implications for Policy, Delivery, or Practice: Aggregate physician workforce projections do not reflect potential specialty imbalances between supply and demand. The calls for increasing the total numbers of physicians in the US do not account for specialty-specific practice patterns and may ignore the ability of the physician workforce to meet future demands by changes in specialization rates and practice patterns by new physicians. More specialty-specific research on the physician workforce is necessary to ensure that physician workforce policy is well-informed on future trends in specialty requirements. Primary Funding Source: HRSA ●Nurse Staffing and Quality of Care: Findings from the Economic Value of Nursing Model Tim Dall, MS, Peggy J. Maddox, RN, Ph.D., Juliette Chen, MPH, Paul F. Hogan, Ph.D. (abd) Presented By: Tim Dall, MS, Vice President, Applied Economics, The Lewin Group, 3130 Fairview Park Drive, Falls Church, VA 22042; Tel: (703) 269-7543; Fax: (703) 269-5503; Email: tim.dall@lewin.com Research Objective: This study models the implications of alternative nursing systems of care on patient risk of nosocomial complications, and the implications in terms of premature mortality, excess length of stay, and excess medical costs. Study Design: By combining findings from the literature with original empirical analysis, we developed the Economic Value of Nursing Model (EVNM) that can be used to quantify changes in patient risk of nosocomial complication under alternative nursing systems of care. Population Studied: RNs providing tertiary care in general, acute care hospitals, as well as the patients for whom they provide care. Principal Findings: Over 7 million cases of nosocomial complication occur each year in general, acute care hospitals. These complications are directly responsible for 450,000 premature deaths, 20 million additional inpatient days, and $53 billion in excess medical costs. Improved nurse staffing— whether defined in terms of higher staffing levels or higher skill mix—has the potential to reduce (but not eliminate) the incidence of nosocomial complications and the mortality, additional length of stay, and additional medical costs attributed to these complications. Conclusions: A growing body of research documents the impact of improved nurse staffing on patient outcomes, but more research is needed. Moreover, future research will prove more valuable if the findings are estimated and presented in such a way that they can be combined with the findings of other researchers into a systematic model of the economic and quality of care implications of nurse staffing decisions. Implications for Policy, Delivery, or Practice: It is in the interest of all parties—employers, patients, insurers, policy makers and nurses—to gain a better understanding of the contribution of professional nursing care as this knowledge will contribute to the improved efficacy and efficiency of healthcare services. Such information will help inform operational decisions regarding appropriate systems of nursing care. Primary Funding Source: Nursing's Agenda for the Future and its sponsoring associations ●A Comprehensive Model to Project the Primary Care Physician Workforce Martey Dodoo, Ph.D., Robert L. Phillips, M.D., MSPH, Jessica L. McCann, MA, Ginger Ruddy, M.D., Larry A. Green, M.D., Lisa S. Klein Presented By: Martey Dodoo, Ph.D., Senior Economist, The Robert Graham Center, 1350 Connecticut Avenue N W, Suite 201, Washington, DC 20036; Tel: (202)331-3360; Fax: (202)3313374; Email: mdodoo@aafp.org Research Objective: To assess prior models to forecast the adequacy of the Primary Care Physician Workforce, develop a comprehensive model with both demand and supply segments, and use the model to project the primary care physician workforce to 2020. Study Design: We critically reviewed recent models to forecast the adequacy of the Primary Care Physician Workforce. We developed a comprehensive physician workforce model with demand and supply segments. Demand was based on need and supply was simulated from production components and training cohorts. Key variables were identified using regression techniques. We estimated the model using 20 months of data. Tested the model with 20 additional months of data. Used the model to project the primary care physician workforce to 2020. Population Studied: The US primary care physician population Principal Findings: The medical training pipeline is relatively supply inelastic. The results of the best-fit regression analysis identified three out of six variables that were strongly related to the size of the primary care physician workforce. These were the real GDP three years prior, the civilian resident population and the percentage of the population that is insured. In evaluations the model accounted for more than 95 percent of the historical primary care physician workforce. In a status quo projection the physician workforce of general internists grows at a higher rate than that of family physicians. The projection results were 97,000 family physicians, 90,000 general internal medicine physicians, and 48,000 general pediatricians in 2010; and 151,000 family physicians, 173,000 general internists, and 89,000 general pediatricians in 2020. Conclusions: This analysis identified significant relationships between key variables in both the supply and demand segments of the primary care physician workforce market. The primary care physician workforce is sensitive to growth in the GDP, population and proportion of the population insured. These relationships and variables appear to determine the level of the primary care physician workforce within the shortrun 5-year period. Implications for Policy, Delivery, or Practice: There should be concerns about the relative inelasticity of the medical training pipeline, and whether a physician workforce driven mainly by economic factors will sufficiently provide the needed health care. This analysis illustrates that analytical rigor could be effectively employed in projecting the physician workforce. Primary Funding Source: No Funding Source ●Home Healthcare Nurse Job Satisfaction and Intent to Stay Carol Ellenbecker, RN, Ph.D., Carol Ellenbecker, RN Ph.D., James Byleckie, Ph.D., Linda Samia, RN, MS Presented By: Carol Ellenbecker, RN, Ph.D., Associate Professor, Nursing, University of Massachusetts Boston, 100 Morrissy Boulevard, Boston, MA 02125; Tel: 617-287-7515; Email: carol.ellenbecker@umb.edu Research Objective: The purpose of this study was to examine the relationship of job satisfaction and individual nurse characteristics to intent to stay in home healthcare nurses and to test a theoretical model of nurse job satisfaction and intent to stay. Study Design: This was a descriptive correlation study. Selfreport data were collected from home healthcare nurses using the Home Healthcare Nurses Job Satisfaction (HHNJS) scale. The 30 item HHNJS measures job satisfaction of home healthcare nurses and has demonstrated validity and reliability. Population Studied: A representative sample of 2,500 home healthcare nurses was recruited from Certified Home Healthcare Agencies throughout the New England region. First, a probability proportional to size sample of 150 agencies was generated from the Medicare provider file. Second, the selected agencies were contacted and asked to participate in the study by allowing researchers access to nurses employed at their agency. All nurses at participating agencies meet the criteria for inclusion and were asked to participate in the study Principal Findings: Global job satisfaction mean scores varied from 2.42 to 4.97 and were highly correlated with intent to stay. Demographic variables were not related to job satisfaction. Factors most strongly correlated with intent to stay were Professional Pride and Relationship with Administration, Autonomy and Independence; follow by Salary and Benefits, Stress and Workload, Relationship with Peers, Relationship with Patients, and Relationship with Physician in that order. There was a greater variability among the factors hypothesized as intrinsic and extrinsic than in global job satisfaction. Nurses’ relationship with Administration had the greatest amount of variability, while nurses’ relationship with patients the least. Conclusions: Nurses’ job satisfaction and their desire to stay at their jobs may be effected most by the organizational environment and other extrinsic factors over which administrators and policy makers have control. The theoretical model developed from an integration of the findings of empirical research related to job satisfaction and retention, in institutional settings, may not be a good fit for home healthcare settings. The results of this research suggest that characteristics viewed as extrinsic, i.e. Autonomy and Independence of hours and work activities for the home healthcare nurse may actually be perceived by home healthcare nurses to be intrinsic to job of the home health care nurse. Likewise, the previously hypothesized intrinsic characteristics of Relationship with Administration while intrinsic to the job for nurses in institutional settings may be extrinsic to the role of the home healthcare Implications for Policy, Delivery, or Practice: Predicted severe nursing shortages and an increasing demand for home healthcare services have made the retention of experienced, qualified nursing staff a priority for healthcare organizations. Knowledge of variables that contribute to job retention in home healthcare will provide the information necessary to maintain nursing staff and assure access to quality home healthcare services. Job satisfaction for home healthcare nurses is dependent on factors over which agencies have control. This suggests avenues for intervention that will improve job satisfaction with implications for higher retention, greater access, and improved patient care. Primary Funding Source: AHRQ ●Determining User Satisfaction with Online Public Health Preparedness Training Jennifer Horney, MA, MPH, Erin Rothney, MPH, Lorraine Alexander, DrPH, Pia MacDonald, Ph.D., MPH Presented By: Jennifer Horney, MA, MPH, Assistant Project Director, Director of Training and Education, North Carolina Center for Public Health Preparedness, University of North Carolina, Campus Box 8165, Chapel Hill, NC 25799-8165; Tel: (919) 843-5566; Fax: (919) 843-5563; Email: jen.horney@unc.edu Research Objective: The North Carolina Center for Public Health Preparedness, in the North Carolina Institute for Public Health at the University of North Carolina at Chapel Hill School of Public Health, works to improve the capacity of the public health workforce to prepare for and respond to terrorism and other emerging public health threats. NCCPHP’s Training Website offers more than 100 free Internet-based training modules on surveillance, bioterrorist agents, emerging/re-emerging diseases, and other topics. Each 30- to 60-minute module offers free continuing education units. For continuous improvement of training services and marketing, NCCPHP surveyed the Training Website’s registered users to determine module effectiveness, suggest topics for new modules, and gather demographic data. Study Design: A survey was designed to assess use of and satisfaction with the training modules. Registered users of the training website were sent an e-mail asking them to participate and providing a link to the online survey. Responses were anonymous. Population Studied: The survey was distributed to all 2752 registered users of the NCCPHP Training Website. Principal Findings: Four hundred sixteen registered users participated in the survey, a 15 percent response rate. The two largest occupational groups of respondents were epidemiologists: 68, and public health nurses: 61. Twentyseven percent of respondents discovered the website through an Internet search; a colleague referred 22 percent to the site. Most public health nurses learned about the training site through the North Carolina Public Health Workforce Development System, a learning management system available from NCCPHP. Fifty-four percent completed at least one training module in the last year. Of those who did, 98 percent said the module provided them with the information they were seeking, 92 percent said the module made them feel better equipped to do their jobs, 62 percent recommended the website to colleagues, and 61 percent bookmarked the website on their computers. Fifty-four percent said the website is one of the first three places they look online for training related to terrorism and other emerging health threats. Sixty-four percent of epidemiologists and 54 percent of public health nurses completed a training module in the last year; 96 percent of epidemiologists and 100 percent of nurses said the module provided the information they needed. More than half of all respondents desired more training in emerging/reemerging diseases, outbreak investigation, epidemiology methods, and surveillance. Epidemiologists requested additional training in epidemiology methods, surveillance, geographic information systems, and biostatistics. Public health nurses desire additional training in outbreak investigation, emerging/reemerging diseases, and public health law. Conclusions: Online training modules from NCCPHP provide most users with needed information and help equip them to do their jobs. This website is one of the first places that users look for preparedness training; many bookmark this site and have recommended it to others. A limited population completed this survey, so results cannot be generalized to a larger population without additional research. Implications for Policy, Delivery, or Practice: Short, online modules are a highly effective way to provide necessary information to public health workers for public health preparedness topics. Distance learning is useful for bioterrorism preparedness because it allows quick access to just-in-time training. Primary Funding Source: CDC ●Direct Care (DC) Staffing and Turnover in Nursing Homes: An Attempt to Identify Instrumental Variables Bita A. Kash, MBA, FACHE, Charles D. Phillips, Ph.D., MPH, Catherine Hawes, Ph.D. Presented By: Bita A. Kash, MBA, FACHE, Graduate Research Assistant, Health Policy and Management, School of Rural Public Health, Texas A&M University Health Science Center, 3000 Briarcrest Drive, Suite 300, Bryan, TX 77802; Tel: (979)458-0652; Fax: (979)458-0656; Email: bakash@srph.tamhsc Research Objective: 1) To identify firm-specific variables related to DC staff turnover, and 2) to test the usefulness of identified instrumental variables in the construction of 2SLS models of DC staffing, where staff turnover has been identified as endogenous. Study Design: We used an economic framework of human capital and on-the-job training (OJT) to test potential predictors of staff turnover. We also tested other potential variables related to staff mix, benefits, and management capacity which could affect turnover, and therefore may be useful in the development of a 2SLS model of DC staffing. These potential instrumental variables (IVs) were tested for significant covariation with staffing versus turnover using Pearson correlation methodology. Next, staffing regression models were developed to predict direct care (DC) staff hours per resident day. We then analyzed the usefulness of the identified IVs for 2SLS regression modeling. Population Studied: The population of nursing homes originated from the 2002 Texas Medicaid Nursing Facility Cost Report (1,016 facilities). This study did not include hospital based facilities. Texas is unique due to the large number of facilities allowing for a large sample size, and a well-established Medicaid cost report process allowing for a thorough examination of expense categories. Principal Findings: We tested five potential IVs and identified only one - expense ratio - as a unique indicator of staff turnover. This IV was DC Staff Training Expense Ratio, as proposed in the human capital framework. All other proposed IVs were either significantly correlated with both staff levels and staff turnover, or only related to staffing. The direction of the relationship between staff turnover and staff training expense was negative as expected. The results from the OLS and 2SLS regressions were expected and consistent: percent Medicaid had a significant negative effect on staffing, while average case mix complexity (CMI) demonstrated a significant positive effect. The size of the facility proved to be a significant positive predictor of staffing levels. Although staff training expense ratio was identified as an IV for staff turnover rates, and the hypothesized relationship of specific training and turnover was accepted, we did not see enough support for the use of 2SLS models in DC staffing prediction models. Conclusions: Both OLS and 2SLS models are consistent in identifying the significant predictors of nursing home DC staffing levels. Most predictors of staffing are organizational characteristics, making DC staffing supply less dependent on market factors and more sensitive to ownership status and facility resources. OTJ training does matter when looking at staff turnover. Our process of IV identification assumed that all resident care staff training expenses were strictly for longterm care “specific training.” In order to improve this approach to analyzing DC staff turnover, one would need more detailed information on the type of training received (e.g., general versus specific OJT). Implications for Policy, Delivery, or Practice: As we are able to explain turnover rates with a growing number of unique predictor variables, opportunities for developing effective retention practices and supportive public policies will emerge. Primary Funding Source: No Funding Source ●Physician-Patient Race Concordance May Reduce Risks of Potentially Avoidable Maternity Complications for African American Medicaid Beneficiaries Sarah Laditka, Ph.D., James Laditka, DA, Ph.D. Presented By: Sarah Laditka, Ph.D., Associate Professor, Dept. Health Services Policy and Management, University of South Carolina, HESC Building, 800 Sumter Street, Columbia, SC 29208; Tel: (803)777-1496; Fax: (803)777-1836; Email: sladitka@gwm.sc.edu Research Objective: There is evidence that minority patients prefer treatment by minority physicians, and that minority physicians are more likely to treat minority patients and those whose insurance status limits access to health services. Communication, understanding, and trust may be enhanced with greater physician cultural competence. Patients who understand and trust their physicians may be more likely to adhere to recommended behaviors and health care regimens. We examined associations between physician-patient race concordance and pregnancy outcomes associated with the accessibility and success of prenatal care, for African American Medicaid beneficiaries. We used an indicator of prenatal care access and quality, Potentially Avoidable Maternity Complications (PAMCs). This indicator uses hospital discharge data to identify pregnancy complications that may often be prevented through successful prenatal care. We defined PAMCs with an expert panel including obstetricians, with external physician review. PAMCs are defined by combinations of primary and secondary diagnoses, such as a delivery hospitalization with both a urinary tract infection and a complication known to be associated with such infections. Study Design: Data were obtained from the South Carolina Budget and Control Board. The data included de-identified records of all deliveries covered by Medicaid in year 2000, all health care encounters for the mothers in the 12 months preceding delivery, and provider information that included patient-physician race concordance. PAMC risk was estimated using multilevel logistic regression. Individual-level controls included age, education, marital status, income, and comorbidities. Area-level controls included rurality, median income, physician supply, and the availability of either a community or rural health center. Population Studied: 10,687 year 2000 delivery hospital discharges for African American women whose pregnancy care was provided by Medicaid in South Carolina. Principal Findings: Women in the study received treatment from a total of 3,776 physicians who were not African American, and 136 physicians who were African American. Of all deliveries, 3.2% included PAMCs; 23% of African Americans had at least one race concordant prenatal care visit, whereas only 3.7% had race concordance in more than one-third of their visits. In adjusted results, each 1% increase in the proportion of prenatal care visits that were race concordant was associated with a 3.2% decrease in PAMC risk (p=.001). The odds of having a PAMC for those with any race concordant prenatal care visit were only 45% of the odds for those having no race concordant visits (p=.002). The odds of having a PAMC for women with at least two-thirds of visits being race concordant were only 28% of those for others (p=0.013). Race concordance had a larger effect on model fit than any other predictor. Conclusions: Pregnant African American Medicaid beneficiaries have notably improved pregnancy outcomes when they obtain prenatal care from African American physicians. Implications for Policy, Delivery, or Practice: United States policies encourage physician training for African Americans and other minorities. Although our results could be influenced by selection effects, they suggest these policies should be supported and expanded. Results also suggest the need for additional cultural competence for majority physicians who treat vulnerable minority Medicaid beneficiaries. Primary Funding Source: HRSA, Office of Rural Health Policy ●Breast Imagers Rebecca Lewis, MPH, Mythreyi Bhargavan, Ph.D. Presented By: Rebecca Lewis, MPH, Researcher, American College of Radiology, 1891 Preston White Drive, Reston, VA 20191; Tel: (703)295-6771; Fax: (703)264-2443; Email: rebeccal@acr.org Research Objective: Much has been discussed recently in popular media and in academic literature about breast imaging, specifically mammography and its effectiveness, effect of low reimbursement and lawsuits on potential access to mammography, and the quality of mammography in the country, particularly in the context of the Mammography Quality Standards Act (MQSA) which was reauthorized in 2004. Little is written about those radiologists who interpret mammograms, such as measures of their training and experience, practice patterns, and the volume of work. This study seeks to fill that gap. Study Design: This paper uses data from the American College of Radiology’s 2003 Survey of Radiologists. We quantify the pool of available breast imagers using a variety of definitions of breast imagers: based on training, volume of mammograms, percentage of time spent in breast imaging, and self-identification. We document the average level of training and experience that they have relative to other radiologists. We measure if there are any differences in access to mammographers across geographic locations (census regions) and types (e.g., urban versus rural). We use the age distribution across physicians and other practice characteristics to estimate the available supply of mammographers in the future. Population Studied: All analyses were performed on posttraining, professionally active radiologists, and were weighted to be representative of all radiologists in U.S. Principal Findings: Roughly 58% of those radiologists who perform any mammograms, interpret >=480 mammograms per year, which is an approximation of the current MQSA requirement of 960 mammograms across two years. 55% of radiologists interpret fewer than 1000 mammograms per year. Of those who perform any mammograms, 98% are boardcertified, and 4% have a fellowship in breast imaging, while 57% have a fellowship of any type. Most mammographers are located in the Midwest and South, work in private radiology (50%) or multi-speciality private practices (32%), and practice in the main city of smaller metropolitan areas. Statistically significantly more women than men report having a specialty in breast imaging, and report breast imaging or women’s imaging as their primary specialty. Significantly more women than men report spending 30% or more of their clinical time in breast imaging and women perform significantly more mammograms than men. Conclusions: The large majority of mammographers are welltrained in that they are board-certified, and/or have a fellowship in breast imaging. There is no obvious evidence that women in rural areas or in certain census regions have lower access to mammography than others. Implications for Policy, Delivery, or Practice: Women predominately undergo training in and exhibit a preference for breast imaging subspecialties, and the number of women going into radiology is not increasing; the combination of these factors could affect the access to breast imaging in the future. A large number of radiologists perform low volumes of mammograms per year. As a result, any changes in regulations related to volume requirements must take into account the effect on patient access to qualified mammographers. Primary Funding Source: No Funding Source ●Survey of Nursing Work Environment: a Confirmatory Factor Analysis of the Nursing Work Index-Revised Yu-Fang Li, Ph.D., RN, Anne Sales, MSN, Ph.D., RN, Nancy Sharp, Ph.D., Gwen Greiner, MS, MPH, Elliott Lowy, Ph.D. Presented By: Yu-Fang Li, Ph.D., RN, Research Health Science Specialist, HSR&D, VA Puget Sound Health Care System, 1100 Olive Way, Suite 1400, Seattle, WA 98101; Tel: (206) 768-5383; Fax: (206) 764-2935; Email: yufang.li@med.va.gov Research Objective: Associations between perception of work environment, nurse retention and recruitment, and patient outcomes have been supported by previous studies, although their properties are not fully assessed. The objective of this study was to assess properties of three different factor solutions for the Nursing Work Index-Revised (NWI-R). Study Design: Data came from 6650 staff registered nurses who participated in the Nurse Staffing and Patient Outcomes in VA project nursing staff survey conducted by mail in 2003. Reliabilities of the NWI-R and its subscales were evaluated using Cronbach’s alpha. We conducted confirmatory factor analyses (CFA) using 50% of the sample to examine the goodness-of-fit of one-, three-, and five-factor models of the NWI-R. Unidimensionality of individual factors was examined if a model revealed a poor fit to the data. The modified models were cross-validated using the other half of the sample. Population Studied: Registered Nurses working at VHA Medical Centers with acute inpatient units. Principal Findings: Cronbach’s alphas ranged from .90 to .95 for the three solutions of the NWI-R and .80 to .88 for the subscales. None of the original models tested provided good overall fit to the data. Items underlying nurse-physician relations and adequacy of support appeared to be consistent across models. Large standardized residuals between items suggested that these items may reflect constructs other than those previously described. Five new models were created by including additional factors, dropping ambiguous items, or allowing correlated error covariance and items to cross-load on multiple factors. Results from cross-validations suggested that an alternative five-factor model representing the areas of career advancement, adequate support, nurse-physician relationships, supportive management, and foundations for quality care might be most stable in repeated samples. Conclusions: Effective measurement of nurses’ perceptions of their work environment requires that researchers are assured of the reliability and validity of the instrument used in their studies. Results suggested that the three forms of the NWI-R examined in this study required adjustments to strengthen their psychometric properties. Implications for Policy, Delivery, or Practice: Despite the increased interest in job satisfaction of nursing staff, VHA has not standardized an instrument to investigate this construct systematically. This study presented a form of the NWI-R, a commonly used nursing job satisfaction instrument, to serve as a starting point toward this effort. Primary Funding Source: VA Health Services Research and Development ●America's Health Workforce: Larger and More Complex Than We Thought Ana Maria T. Lomperis, MA, Ph.D. Presented By: Ana Maria T. Lomperis, MA, Ph.D., Associate Professor of Health Management and Policy, Department of Health Management and Policy, Saint Louis University, 3545 Lafayette Avenue, Salus Center, Suite 300, St. Louis, MO 63104-1314; Tel: (314)977-3236; Fax: (314)977-1674; Email: lomperat@slu.edu Research Objective: Today two-thirds of health care costs are generated by labor. Yet, as many have argued, the health workforce continues to be largely neglected as a focus of health policy research (e.g., McLaughlin 1994; Iglehart). Reliable, systematic data on the health workforce are rare. Moreover, there is no agreement in the literature on how to define America's health workforce, and by extension, how large it really is. Estimates range from the 10 million "conventional" health care workers, such as physicians and nurses, to the roughly 12 million jobs in "conventional" health delivery industries, such hospitals and physician offices. But these approaches overlook millions in other settings from mental and public health workers to those employed by pharmaceutical firms, health insurance companies and in the health policy research field. The main objective of this study is to identify the range of occupations and industries that should be included in a definition of the health workforce and provide an estimate of the total number of individuals employed in them that reflects their full contribution to the health sector in the United States today Study Design: Michael Grossman's seminal work in 1972 on the production of health provides the theoretical basis for this study. According to Grossman, consumers produce "good health" by combining their own time with a wide variety of health care and other goods and services. Thus, the health workforce should include everyone whose livelihood contributes to the production of health - from the conventional health care occupations typically studied to the "other health" occupations typically overlooked. The study develops a matrix that identifies both such "conventional" and "other health" occupations and industries based on the federal government's classification systems. Detailed unpublished data from the U.S. Bureau of Labor Statistics' 2000-10 National Industry-Occupation Employment Matrix are then used to fill the matrix to produce estimates of the total number of jobs in these health occupations and industries in 2000, as well as those projected for 2010. Population Studied: The population studied includes members of the U.S. labor force, whatever their occupation and wherever they work. Principal Findings: This study finds that America's health workforce is much more complex and far larger than commonly understood. Specifically, it identifies 343 more occupations and 17 additional industries that are overlooked in previous works. It also estimates that the U.S. health workforce, broadly defined, represented nearly 16 million jobs and 11 percent of the overall U.S. labor force in 2000 -considerably more than the 9.6 million jobs and 6.6 percent of the overall workforce in the conventional health care occupations and the 11 million jobs and 7.6 percent of the total in the conventional health services industries typically counted. Conclusions: The health workforce is more complex and far larger than most previous studies have suggested. This study provides a first step in reaching this understanding and suggests avenues for future research. Implications for Policy, Delivery, or Practice: The findings of this study should be of broad interest to health policy researchers and practitioners seeking ways to more effectively utilize the skills and talents of the millions of individuals employed in the health sector. Primary Funding Source: University funding ●The Impact of Nosocomial Complications on Patient Mortality: Findings from the Economic Value of Nursing Model Peggy Maddox, RN, Ph.D., Tim Dall, MS, Juliette Chen, MPH, Paul F. Hogan, Ph.D. (abd) Presented By: Peggy Maddox, RN, Ph.D., Director, School of Nursing, Center for Health Policy and Research, Fairfax, VA ; Tel: (703) 993-1982; Email: pmaddox@mason.gmu.edu Research Objective: This study quantifies the additional mortality risk attributed to each of 10 nosocomial complications acquired in general, acute care hospitals. These nosocomial complications are recognized as nursing sensitive outcomes—i.e., patient outcomes that are sensitive to the quality of nursing care received. This research is part of a larger effort sponsored by the Nurses’ Agenda for the Future (NAF) to quantify the patient care and economic implications of alternative nursing systems of care. Study Design: Using patient-level discharge data from the 2002 National Inpatient Sample (NIS), we use regression analysis to isolate the contribution of each nosocomial complication on patient mortality controlling for patient acuity and other risk factors. The 10 nosocomial complications modeled are urinary tract infection (UTI), decubitus ulcer, pneumonia, deep vein thrombosis/pulmonary embolism (DVT/PE), upper gastrointestinal tract infection (UGI), central nervous system (CNS) complications, sepsis, shock/cardiac failure, postoperative infection, and pulmonary failure. Using the Economic Value of Nursing Model (EVNM), we quantify the relationship between RN staffing and patient risk of complications, and the relationship between complications and mortality risk to estimate the relationship between nursing systems of care and patient mortality. Population Studied: Patients admitted to general, acute care hospitals. Separate analyses are conducted for patients admitted for major surgery (i.e., the surgical pool), and all other patients (i.e., the medical pool). Principal Findings: In 2002, an estimated 450,000 premature deaths are directly attributed to nosocomial complications. The increase in mortality risk attributed to patient complications differs by type of complication and differs among patients in the medical and surgical pools. The three leading complications in terms of the attributed (i.e., after controlling for patient acuity) number of deaths are shock/cardiac failure (167,600 deaths), pulmonary failure (69,600 deaths), and hospital-acquired pneumonia (60,500 deaths). When these mortality risk estimates are incorporated into the EVNM, the estimated relationship between nurse staffing and patient risk of in-hospital mortality is similar to estimates in the literature of the relationship between nurse staffing and failure to rescue. Conclusions: Patients who experience complications are at increased risk of mortality. This fact highlights the importance of providing adequate nurse staffing levels and skill mix that can help prevent the occurrence of nosocomial complications. Implications for Policy, Delivery, or Practice: These findings on the mortality risk attributed to nosocomial complications are useful to hospitals, clinicians and researchers developing new methods and practices to improve patient care. Clinicians tracking the incidence of nosocomial complications as part of initiatives to improve patient care can apply these attributed mortality risks to quantify the effects of their initiatives on patient mortality. Primary Funding Source: Nurses' Agenda for the Future and contributing associations ●Are We There Yet? Distance to Pediatric Subspecialty Providers in the United States Michelle Mayer, Ph.D., MPH, RN Presented By: Michelle Mayer, Ph.D., MPH, RN, Rsearch Fellow, Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, CB #7590, Chapel Hill, NC 27599-7590; Tel: (919)966-7666; Fax: (919)966-3811; Email: michelle_mayer@unc.edu Research Objective: There is currently widespread concern that the supply of pediatric subspecialists is not adequate to meet the needs of children. To date, no one has estimated the distances that children must travel to obtain pediatric subspecialty services in the United States. Our objective was to estimate the distance between pediatric populations in the United States and identify county characteristics that are associated with greater distances to pediatric subspeciality care. Study Design: Using physician data from the American Board of Pediatrics and county level data from the Bureau of Health Professions Area Resource File (ARF), we calculated the straight line distance between each county in the United States and the nearest pediatric subspecialty provider. For each county and pediatric medical subspecialty, we calculated the shortest straight-line distance to the nearest physician. We merged 2003 estimates of the under-18 population from the United States Bureau of the Census. Using distance and population data, we calculated the percentage of the pediatric population living within 10, 11-50, 51-100, 101-200, and 200 or more miles of a provider for each specialty. Using county level observations for all pediatric subspecialties simultaneously, we performed random effects logit to identify county characteristics associated with living more than 50 miles from a pediatric subspecialty provider. Population Studied: United States Counties (n=3141). Principal Findings: Across all counties in the United States, the population-weighted average distance to a board-certified pediatric subspecialist ranged from 12.6 miles for neonatology to 76.7 miles for pediatric sports medicine. For most pediatric subspecialties, more than 75% of the pediatric population lives within 50 miles of a certified physician. Adolescent medicine, developmental and behavioral pediatrics, pediatric rheumatology, and pediatric sports medicine are exceptions. Non-metropolitan counties and those in the Pacific and Mountain regions of the United States were significantly more likely to be located more than 50 miles from a pediatric subspecialist. Conclusions: For most pediatric subspecialties, more than 75% of the under-18 population lives within 50 miles of a provider. Pediatric subspecialists in adolescent medicine, developmental pediatrics, rheumatology, and sports medicine are less widely available. These results suggest that the practice locations of pediatric subspecialists parallel the geographic distribution of children in the United States. Nonetheless, children from non-metropolitan counties and those in selected regions of the United States face significant geographic barriers to receipt of pediatric subspecialty care. Implications for Policy, Delivery, or Practice: Future studies should identify ways to improve access for those children living in areas without a nearby provider and should evaluate the extent to pediatric subspecialist supply is adequate to meet patient demand in the areas that currently have providers. Primary Funding Source: AHRQ ●Progress and Potential of Women and Minorities in Health Care Management: Results of Two Nationwide Studies Ann Scheck McAlearney, Sc.D., MS Presented By: Ann Scheck McAlearney, Sc.D., MS, Assistant Professor, Health Services Management and Policy, The Ohio State University, 1583 Perry Street, Atwell 246, Columbus, OH 43210; Tel: (614)292-0662; Fax: (614)438-6859; Email: mcalearney.1@osu.edu Research Objective: Despite a sense that women are making effective strides in achieving higher ranks in health care management, objective evidence shows considerable disparities still existent, slow growth of numbers over time, and appallingly few numbers of minorities of either gender in health care leadership roles. This research was designed to explore these issues in greater depth, combining results of both quantitative and qualitative studies to improve our understanding of how health care is or is not supporting and promoting women and minorities, and how far we have to go. Study Design: Results of two nationwide studies were analyzed to assess issues of inclusion and development for women and minorities in health care management. First, a nationwide survey of all U.S. hospital chief executives, conducted between August and December 2004, asked about leadership experiences, perspectives about leadership impact, and plans for the future. Analyses included descriptive statistics, chi-squared analyses, linear regression, and logistic regression. Second, an extensive qualitative study, consisting of expert interviews and organizational case studies, was completed between September 2003 and December 2004. Hour-long in-person and telephonic interviews included topics such as inclusion, opportunities for mentoring, and perspectives about the challenges faced by women and minorities in health care management. All interviews were transcribed and analyzed using both deductive and inductive methods. Population Studied: Our nationwide survey had 844 chief executive respondents (response rate =17.2 percent). Consistent with other studies, our respondents were overwhelmingly white (96 percent), making analysis by race infeasible. The qualitative study included 60 organizational case studies and 35 expert interviews. A total of 160 informants were interviewed across the country, including organizational representatives with titles such as Chief Executive Officer (CEO), Director of Human Resources, and Director of Organizational Development. Informants from expert interviews included consultants, recruiters, association leaders, and academic researchers. Principal Findings: Our survey showed that female and male chief executives do not share the same experiences, nor the same perspectives. Controlling for age, women respondents were statistically significantly less likely to have previously been CEOs (41 percent vs. 61 percent, p<.005), had shorter tenures in their current chief executive positions (9.2 years vs. 13.5 years, p<.005), and were less likely to lead health systems percent vs. 19 percent, p<.005) than men. Further, women respondents rated themselves lower than men on several measures of leadership effectiveness, including meeting their goals with respect to management team functioning and financial performance. Women were also significantly more likely than men to strongly agree that offering internal leadership programs, permitting flexibility in job assignments, and targeting women and minorities for leadership development should be an organizational priority. From the qualitative study, three major themes emerged around these issues: 1) barriers hindering progress; 2) strategies to overcome barriers; and 3) opportunities and concerns about targeting women and minorities as special cases in health care leadership development. Conclusions: Organizations aiming to increase the representation and visibility of women and minorities in health care leadership must acknowledge the disparities that exist, and take active steps toward greater inclusion. Incorporating suggested strategies such as establishing participation metrics for senior leadership and board roles, consciously broadening women’s and minorities’ experiences and promoting their successes, and supporting formal mentoring can help health care organizations by promoting greater diversity in management so that senior leadership can become more reflective of both the employee population and communities that health care organizations typically serve. Implications for Policy, Delivery, or Practice: By understanding differences between women’s and men’s experiences and perspectives and by considering potential opportunities to help women and minorities advance, organizations can make informed decisions about investments in leadership development strategies and successfully maximize the potential for these underrepresented groups to attain higher ranks in health care leadership. Primary Funding Source: Center for Health Management Research ●Evaluation of the introduction of US-trained Physician Assistants to the UK NHS Hugh McLeod, BSc, MSc, Ph.D., Juliet Woodin, Ph.D., Richard McManus, MBChB, Ph.D., Kim Jelphs, MSc Presented By: Hugh McLeod, BSc, MSc, Ph.D., Research Fellow, Health Services Management Centre, University of Birmingham, Park House, 40 Edgbaston Park Road, Birmingham, B15 2RT; Tel: 0044 21 414 7620; Fax: 0044 21 414 7620; Email: h.s.t.mcleod@bham.ac.uk Research Objective: US physician assistants (PAs) are professionals licensed to practice medicine with physician supervision. In 2003 and 2004, US-trained PAs were recruited to the UK NHS, in family practice and emergency department settings. The initiative was a local response to a shortage of medical staff in a deprived area. This study assessed the impact of the PAs in terms of: their clinical workload compared to physician and nurse colleagues; the views of staff and patients; and lessons for development of new UK-trained practitioner roles. Study Design: The clinical workload of the PAs was compared with their physician and nurse colleagues using consultation data recorded by the clinicians both for the study and routinely. Data on consultations’ presenting problem(s) were coded using the International Classification of Primary Care (ICPC). Data on emergency department attendees were coded using International Classification of Diseases (ICD10) codes. Data from PAs, supervising physicians and a range of nursing and support staff were collected using semistructured interviews. Data from patients were collected using focus groups. Our analysis used Pawson and Tilley’s (1997) ‘context, mechanism, outcome’ conceptual framework. Population Studied: The study included all 15 PAs employed in the NHS in the West Midlands. Seven PAs worked in family practices, four in two emergency departments, two in both settings. Three PAs returned to the US. Five of the remaining 12 PAs had more than 10 years’ PA experience. Principal Findings: The PAs in family practices increased medical capacity by seeing a range of undifferentiated acutely presenting patients similar to their supervising physicians. The PAs’ contributions were influenced by factors including consultation duration (10 to 20 minutes), practices’ clinic arrangements, and supervising physicians’ and PAs’ preferences. The PAs were positively regarded by clinical colleagues, and noted for strong interpersonal and communication skills, and a team-working ethos. The contribution made by the PAs working in the emergency departments varied with the extent of their previous experience and perceptions of the available supervisory support. Patients were overwhelmingly positive in their response to the PAs. The inability of the PAs to prescribe medicines without a physician’s signature was the key limitation to the PAs’ practice. Conclusions: The PA profession has made a successful transition from the US and has effectively increased medical capacity in an under-doctored area. However, like physicians, PAs contribute in a range of ways and fulfilment of a PA’s potential requires that their skills are well matched to a specific local need. Implications for Policy, Delivery, or Practice: Interest in UStrained PAs is increasing in the NHS, and recruitment is expanding. The experience of the PAs included in this study is informing the Department of Health’s current development of a Medical Care Practitioner (MCP) role, which is likely to be similar to the PA role in certain respects. In the future, registration of PAs as MCPs may resolve the key prescribing issue. However, the PAs’ supervisory relationship with physicians explicitly facilitates patient-centred care, an attribute which may be lost if the MCP role is granted independent status. Primary Funding Source: UK Department of Health ●Physician Assistant Workforce Research Using Existing National Health Surveys: Trials and Tribulations Perri Morgan, MS, PA-C, Justine Strand, MPH, PA-C, Truls Ostbye, M.D., MPH, MBA, Ph.D., FFPH Presented By: Perri Morgan, MS, PA-C, Physician Assistant Research Fellow, Physician Assistant Division, Duke University, DUMC 3848, Durham, NC 27710; Tel: (919) 681 3161; Fax: (919)-681-9666; Email: perri.morgan@duke.edu Research Objective: Given the expanding role of nonphysician clinicians (NPCs) in the health workforce, high health care costs, and predicted physician shortages, there is a pressing need for research detailing the current and potential activities, quality of care, and costs of NPCs such as physician assistants (PAs). Although this research is inherently interdisciplinary, research resources are often disciplinespecific. This study details strengths and weaknesses of existing national healthcare surveys for research on physician assistants and proposes remedies for existing barriers Study Design: This paper is based on a critical literature review and an analysis of existing large nationally representative health surveys. The methodologies of several of these surveys (Medical Expenditure Panel Survey, National Health Interview Survey, National Ambulatory Medical Care Survey, and Community Tracking Study) are scrutinized for appropriateness for research on PAs. As an example, we compare national estimates of NPC patient encounters from each survey Population Studied: Health workforce of the United States and the population that uses health services. Principal Findings: Although research has generally found that PAs provide high quality, cost-effective care, PA workforce analysts face several unique problems. First, since PAs are by definition dependent providers who work under the supervision of a physician, studies would ideally focus on care provided by the team. National surveys, however, do not support analysis at the team level. Second, PA practice is extremely heterogeneous, with scope of practice carved out at the individual level between a PA and a physician, subject to constraints of varying state regulations. This variation complicates any analysis of PA practice, but especially limits the generalizability of local studies in which practice patterns may be expected to be more homogeneous. National surveys, however, have frequently under-represented PA practice and have often phrased survey questions to apply to physicians only. Third, research comparing PA to physician performance is frequently criticized for failing to account for potential differences in complexity of patients. Analyses that take these issues of case mix into account require data that can be evaluated both at the individual and at the team level. Again, existing national surveys lack this level of detail. Conclusions: With the looming need to expand the health workforce, there is a critical need for information about the viability of alternative types of healthcare providers. Existing evidence documenting the high quality and cost-saving care provided by NPCs has prompted workforce analysts to advocate development and evaluation of team models of care. Modifications in data collection and analysis techniques are required to support conduct of high-quality, generalizable research at the team level. For example, health care provider data could be collected at both the individual provider and team levels, with variables linking team members added to the national survey datafiles. Implications for Policy, Delivery, or Practice: Funding agencies and researchers should pursue analyses of team approaches to healthcare provision. Toward this end, national workforce data collection and research methodology should 1)integrate physician and nonphysician surveys and analyses, 2)promote evaluation of team practice, and 3)support examination of both separate and joint contributions of physicians and nonphysicians. Primary Funding Source: Duke University Physician Assistant Research Fellowship ●Measuring Change in Obstetrical Provider Supply at the Hospital Level: MA 2002-2004 Angela Nannini, FNP, Ph.D., Emily Lu, MPH, Wanda Barfield, M.D., MPH, Donna Johnson, MSW Presented By: Angela Nannini, FNP, Ph.D., Assistant Professor, School of Nursing, Northeastern University, 106D Robinson Hall, Huntington Avenue, Boston, MA 02115; Tel: (617) 373-3112; Fax: (617) 373-8675; Email: a.nannini@neu.edu Research Objective: 1. Measure change in supply of obstetrical providers by perinatal hospital level and geography in Massachusetts from 2002 to 2004. 2. Report reasons for loss of providers. 3. Compare change in supply of providers among Level I, II and III perinatal hospitals with trends in numbers of deliveries at each level of perinatal care. Study Design: A survey adapted from MA ACOG was sent to Obstetrical Chiefs in all MA maternity hospitals (n=50) with a 88% response rate overall and 88% by each level of hospital. The survey assessed obstetrical providers from 2002 to 2004; the number and type of obstetrical providers [OB, family practitioner (FP), and certified nurse midwife (CNM)], number of recruited providers, and number who stopped obstetrical practice and why. Percent change in obstetrical providers by type and overall were reported by perinatal hospital level (I,II,III) and geographic area. Trends in numbers of births at each hospital and level of perinatal care from 2001 to 2003 were calculated and compared to losses or gains of providers. Population Studied: Obstetricians, certified nurse midwives and family practitioners who perform deliveries at perinatal hospitals in Massachusetts. Principal Findings: Overall, 7.6% of all OB providers and 10.7% of OBs were loss in MA between 2002 to 2004. Level I, II and III lost 14.6%, 5.8 % and 9.4% of OBs respectively. Western MA lost 1 in 4 OBs but other areas lost only 1 in 18. 50% of Level I hospitals had <= 4 OBs and 18% had <= 4 OB providers. Cost of liability insurance accounted for nearly 40% of loss of OBs. Other major issues related to provider loss were recruitment, retention, retirement and change of practice patterns. Conclusions: Loss of obstetricians was greater than loss of other providers. Hospitals designated as Level I perinatal facilities or located in western MA suffered the greatest losses. OB services in hospitals with <=4 providers may be in jeopardy of closing. This survey at the hospital level yielded better response rates than previous surveys to individual providers. Implications for Policy, Delivery, or Practice: Overall statewide estimates of obstetrical provider loss may obscure geographic and hospital level losses. The disproportionate loss of providers at Level I hospitals and in Western MA may encourage women to seek care at more costly facilities and travel longer distances to get care. The relationship of these losses to the ability of women to access prenatal care needs to be monitored. Primary Funding Source: No Funding Source ●The Canadian Contribution to the US Physician Workforce Robert Phillips, M.D., MSPH, Georger Fryer, Jr., Ph.D., Walter Rosser, M.D., Jessica McCann, MS, Martey Dodoo, Ph.D. Presented By: Robert Phillips, M.D., MSPH, Director, The Robert Graham Center, American Academy of Family Physicians, 1350 Connecticut Avenue NW, Suite 201, Washington, DC 20036; Tel: (202)331-3360; Fax: (202) 3313374; Email: bphillips@aafp.org Research Objective: To understand the net emigration of Canadian physicians to the United States in the context of a physician shortage in Canada. We measure the size of effect of this emigration and consider its repercussions for the physician workforce in other developing countries. Study Design: We performed a cross-sectional analysis of the 2004 AMA Masterfile, the 2002 Area Resource File, and reported data from the Canadian Institute for Health Information, the Canadian Medical Association, and the Association of Canadian Medical Colleges to produce a count of Canadian graduates who have ever come to the US, those in the US as of 2004, those in active practice, those in rural or underserved areas, and their net, annual contribution to the US physician workforce. We also examine the immigration of other foreign-trained physicians to Canada compared to physician emigration to test whether retention of émigrés could achieve physician workforce self-sufficiency for Canada. Population Studied: US physician workforce, Canadian physician workforce Principal Findings: Two-thirds of the 11,912 Canadianeducated physicians living in the US spend the majority of their time in direct patient care and are more likely than US graduates to practice in rural areas (p<0.001). From 19601997, an average of 184 Canadian-educated physicians from each graduating class joined the US physician workforce and spend the majority of their time in direct patient care. This migration appears to be slowing; however Canada still realized a net loss of 80 physicians in 2003. There are 13,286 foreigntrained, licensed physicians in Canada excluding those in training. This contrasts with 8,665 to 9,852 (depending on status of non-classified physicians) similarly active Canadiantrained physicians in the United States. Conclusions: In the midst of a physician shortage, Canada has been a net supplier of physicians to the United States. This physician export is equivalent to having nearly two, average-sized Canadian medical schools dedicated to producing physicians for the US. This trend may be waning but requires more longitudinal observation. There are just 402 US-trained physicians practicing in Canada. The net migration of Canadian-trained physicians working in the United States represents 65%-75% of the current foreigntrained physician workforce in Canada. The foreign-trained physicians in Canada come predominantly from lessdeveloped countries, with South Africa as the leading donor. Implications for Policy, Delivery, or Practice: Workforce policies that promote physician supply self-sufficiency in the United States could reduce the draw for Canadian-trained physicians and support workforce needs there. Likewise, polices that promote retention of Canadian-trained physicians within Canada could reduce reliance on foreign physicians. Policies in both countries that support self-sufficiency would further benefit the, largely, less-developed countries, which fill the gaps to the detriment of their own health workforce needs. Primary Funding Source: American Academy of Family Physicians ●Shortage of Dental Hygienists in Private Practices of General Dentists Nadereh Pourat, Ph.D., Roberta Wyn, Ph.D., Dylan Roby, MPhil, Marvin Marcus, DDS, MPH Presented By: Nadereh Pourat, Ph.D., Senior Research Scientist, UCLA Center for Health Policy Research, 10911 Weyburn Avenue, # 300, Los Angeles, CA 90024; Tel: (310)794-2201; Fax: (310)794-2686; Email: pourat@ucla.edu Research Objective: Data on capacity for dental care is scant and less is known on the adequacy of supply of dental personnel such as hygienists in dental practices. Nevertheless, a perception of shortage of such personnel has been documented. We examine the perceptions of shortage of dental hygienists, the concordance between perceived shortage and delays in hiring of dental hygienists, and predictors of perceptions and delay in hiring of these personnel. Study Design: A cross-section of dentists in private practices in California was surveyed. Survey topics included demographics, practice setting, and specialty of dentists; practice location; dental assistant and hygienist questions including size, salary, benefits, work status and dentists’ perceptions of availability of dental personnel. Concordance of dentists’ perception of shortage and experienced delays in hiring of dental hygienists were evaluated in bivariate and multivariate analysis. Analyses were weighted to account for disproportionate sampling of dentists in rural and less populated counties and adjusted for the clustering of dentists by county. Population Studied: A cross-section of dentists in private practice in all California counties with licensed dentists. About 4,300 eligible dentists participated in the mail survey with telephone follow up, with an adjusted response rate of 52%. Principal Findings: Preliminary analysis shows that 52% of dentists reported having an opening for hygienists currently or in the past year. Of these dentists, 47% experienced delays in hiring hygienists defined as more than 1.5 months time to hire hygienists. Dentists who experienced delays more frequently offered dental care and vacation benefits to their full time hygienists and offered higher salaries to the hygienists currently employed in their practices. Those experiencing delays were more frequently clustered in larger urban areas in northern and southern California and had a lower average ratio of full-time equivalent (FTE) hygienists to FTE dentists in their county of practice. Ninety-seven percent of dentists who had experienced delays in hiring believed that there was a shortage of hygienists in their area. Examining the predictors of delays in hiring in a logistic regression model only revealed geographic region of practice and gender to be significant predictors of delays. Examining predictors of having an opening for hygienists revealed that dentists with more hygienist turnover, those owning their practice, and those reporting being too busy or overworked were more likely to have openings for hygienists. Geographic region was also a significant predictor of having an opening. Examining predictors of perceived shortage of hygienists revealed that dentists who offered more benefits, paid higher salaries, and had higher turn over of hygienists were more likely to perceive a shortage of hygienists. In contrast, those not experienced delays or not having hired hygienists in the past year, younger dentists and those within five years of graduation from dental school, and those of Latino or African American decent were less likely to perceive a shortage of hygienists. Conclusions: Results suggest that delays in hiring of hygienists are tied to geographic location of the practice and so are openings for these personnel. Both factors suggest a possibility of differential supply of hygienists by geographic region in California counties. Dentists’ perception of hygienist shortage are seemingly dependent on experienced delays in hiring these personnel but not exclusively so. Other experiences of dentists also play a role in this perception, suggesting additional differential in experiences of dentists in relation to their employment of hygienists. Implications for Policy, Delivery, or Practice: Access to dental care is partly determined by capacity of dentists to provide care and this capacity is dependent on adequate supply of essential personnel such as hygienists. Examining the issues in hiring and retention of dental hygienists in dental practices would illuminate the pathways to insuring a sufficient supply of allied dental personnel. Primary Funding Source: California Dental Association Foundation ●Comparing Characteristics of Dentists and their Practices in California and the U.S. Dylan Roby, M.Phil, Nadereh Pourat, Ph.D., Roberta Wyn, Ph.D., Marvin Marcus, DDS Presented By: Dylan Roby, M.Phil, Senior Research Associate, Center for Health Policy Research, UCLA, 10911 Weyburn Avenue, Suite 300, Los Angeles, CA 90024; Tel: (310)794-3953; Email: droby@ucla.edu Research Objective: To examine the characteristics of dentists and dental practices in California and how they compare to national data. Study Design: A cross-section of general dentists in private practice in California was surveyed by mail in 2003. Survey topics included demographics, practice setting, and specialty of dentists; practice location; staffing questions on size of the practice, salary for assistants, hygienists, and front office personnel, benefits, work status and dentists’ perceptions of availability of dental personnel. The information generated from this survey is the first of its kind in the state, and allows us to compare the California dentists’ and their practices to nationwide data using 1998 and 2001 reports of American Dental Association (ADA) data, the latest data available Population Studied: A cross-section of general dentists in private practice in all California counties with licensed dentists. About 4,300 dentists participated in the mail survey with telephone follow up, with an adjusted response rate of 52%. Principal Findings: Preliminary analysis shows that dentists in private practice in California have different characteristics when compared to the entire nation. More tend to practice general dentistry (90% vs. 84%), work in larger practices (48% vs. 32% have two or more dentists), less frequently employ hygienists (88% vs. 73% have no full-time hygienists) but they employ more dental assistants (7% vs. 32% have no full-time dental assistants), pay higher hourly salaries to hygienists ($42 vs. $29) and dental assistants ($16 vs. $13) than dentists nationally. California dentist less often own the practice that they work in (82% vs. 90%), and spend less time in patient treatment activities (92% vs. 88%) than dentists nationwide. In their demographic characteristics, California’s dentists are more often women (27% vs. 10%) than in the rest of the country and tend to be slightly older (86% vs. 80% are between 30-59 years old). More than half (53%) of California dentists are white, 34% are Asian, 6% are Latino, other races make up 6% of the dentists, and only 1% are AfricanAmerican. Over half (53%) of dentists practice in Southern California, with 27% concentrated in the Bay Area. Lastly, 60% of dentists in the state speak a language other than English, while 68% of the dental practices have staff members that speak another language as well. There are no comparative national data for these demographic characteristics. Conclusions: Findings suggest that California’s dentists differ from the rest of the nation in a number of demographic and practice characteristics. Due to these differences, national policies on dental personnel and access to care may influence California dentists differently or in unexpected directions. Implications for Policy, Delivery, or Practice: A true understanding of the dental care personnel and delivery of dental care in California is more likely to be achieved using California specific data. Policies to improve access to care or to insure adequate supply of dental personnel may not otherwise achieve their intended effects. Primary Funding Source: California Dental Association Foundation ●Advancement of Minorities in Nursing: Is There Discrimination? Jean Ann Seago, Ph.D., RN, Joanne Spetz, Ph.D. Presented By: Jean Ann Seago, Ph.D., RN, Associate Professor, Community Health Systems, University of California, San Francisco, Box 0608, San Francisco, CA 94143; Tel: (515)402-6340; Email: jean.ann.seago@nursing.ucsf.edu Research Objective: America’s diverse population is not reflected in its nursing workforce, especially at senior and executive levels. The purpose of this study was to provide baseline data on the experiences of registered nurses who selfidentify as members of ethnic minority groups. We examine how the experiences of ethnic minority nurses are similar or different from majority nurses as they seek such positions or work to resolve issues in the workplace. Study Design: A survey of 6000 registered nurses across California was conducted. Ethnic minority groups were oversampled. The survey focused on (1) the career paths of nurses of different ethnic backgrounds and (2) the barriers which minority nurses may face. The survey data were analyzed both univariate and multivariate methods. Multivariate regression equations were used to examine the independent contributions of race, ethnicity, and age. Population Studied: 6000 Registered Nurses in California in 2004. Principal Findings: Two-thirds of the Filipino nurses in the survey believe they have the opportunity to advance in their workplace. White nurses were the least likely to believe that they have the opportunity to advance in their workplace. However, only 18.3% of white nurses reported that there were barriers to the advancement of their careers in the workplace in contrast to about 40% of Filipino nurses who perceived barriers to the advancement of their career. While African American nurses applied for promotions more often than nurses from other ethnic groups, 42.8% of them feel that they have been denied a promotion that they were qualified for. Most of these nurses felt that favoritism and race were the primary factors responsible for the denial of their promotion. Only 29.6% of white nurses felt that they have been denied a promotion that they felt they were qualified for. Most white nurses (57%) believed that they do not have a good working relationship with other nurses in their workplaces. However, when asked about feelings of isolation, African American and Other Asian nurses, more than nurses of other ethnicities, expressed that they felt isolated by other nurses in their workplaces. Filipino and African American nurses reported that nurses of their ethnicities were not treated equally in their workplaces. Eighty-four Filipino nurses, the highest number among all groups, have been criticized by coworkers or their supervisors for speaking a language other than English at work. Multivariate analyses indicate that age is a factor affecting satisfaction and promotion opportunities. Since white nurses are older, on average, than minority nurses, they are particularly dissatisfied. Once age has been controlled in multivariate analyses, the differences between ethnic groups are smaller. Conclusions: The most surprising finding was the profound dissatisfaction of the majority nurses in our sample compared to the minority nurses. That they were dissatisfied was not a surprise, but the large percent differences toward the negative for most items was startling. Implications for Policy, Delivery, or Practice: The encouragement of larger numbers of minority persons to enter and remain in nursing can be supported because the minority nurses are more satisfied with their work. Primary Funding Source: Impact Fund ●Nurses in VHA Hospitals: Results from the Nurse Staffing and Patient Outcomes in VA Nursing Staff Survey Nancy Sharp, Ph.D., Anne E. Sales, Ph.D., RN, Gwendolyn T. Greiner, MPH, MSW, Yu-Fang Li, Ph.D., RN, Pamela Mitchell, Ph.D., RN, Julie Sochalski, Ph.D., RN Presented By: Nancy Sharp, Ph.D., Health Sciences Research Specialist, Health Services Research & Development, VA Puget Sound Health Care System, 1100 Olive Way, Suite 1400, Seattle, WA 98101; Tel: (206) 277-3584; Fax: (206) 768-5343; Email: nancy.sharp@med.va.gov Research Objective: The nursing workforce, including registered nurses (RNs), licensed practical or vocational nurses (LPNs or LVNs), nurse aides (NAs), and health technicians (HTs), makes up the largest group of health care providers in the VHA. We report on demographic characteristics of nursing staff working in VHA hospitals and their self-report of perceptions of work environment and quality of care, and compare VHA RNs to RN responses reported by a recent study of nurses in five countries. Study Design: The nursing staff survey was part of an observational, cross-sectional study examing associations between nurse staffing, nursing outcomes, and patient outcomes in VHA. The survey instrument, adapted from a survey developed by the International Hospital Outcomes Consortium (IHOC), included questions about workload, working environment, job satisfaction and quality of care in addition to demographic data. Population Studied: We administered a survey to 46,277 nursing staff in 125 VHA facilities with acute inpatient services. Principal Findings: We received responses from 11,378 VHA nurses for a response rate of 24.6% overall. RNs, LPN/LVNs and combined NA/HTs showed significant differences in demographic characteristics, with a higher proportion of men and racial and ethnic minorities among NAs/HTs than in other nursing categories. Perceptions of the nursing work environment also differed. RNs reported more positive perceptions of salaries, while NA/HTs reported more positive perceptions of management response to nurses’ concerns, participation by nurses in policy decisions, opportunities for advancement, and adequacy of support staff. LPNs were more likely than other nurses to report an increase in the number of patients assigned to them in the past year. Compared to RNs described by the IHOC study, a higher proportion of VHA RNs perceived that there were enough staff to get the work done and enough staff to provide high quality care, and fewer VHA RNs reported a decrease in the number of nurse managers over the past year than the IGIC groups. Overall, VHA RNs looked more like respondents in countries other than the US, represented in the IHOC study by RNs in Pennsylvania, and painted a relatively positive picture by comparison with RNs in other countries and health care systems. Conclusions: VHA nurses report different levels of job satisfaction and different perceptions of their working environment and quality of care depending on their job type. In general, RNs appear least satisfied, and to have the lowest perceptions of the quality of the work environment of the three types of personnel. However, VHA RNs compare favorably on many measures to RNs from non-VHA hospitals in the U.S. and other countries. Implications for Policy, Delivery, or Practice: VHA facilities compete for personnel in all categories with other health care organizations and providers in local, regional, and national markets. Understanding how nurses’ perceptions of their working environment and quality of care differ across job type and health care system is important for developing successful recruitment and retention initiatives in VHA. Primary Funding Source: VA ●Professional Liability Issues and Practice Patterns of Obstetrical Providers in Washington State Susan Skillman, MS, Thomas Benedetti, M.D., MHA, LauraMae Baldwin, M.D., MPH, Elise Bowditch Presented By: Susan Skillman, MS, Deputy Director, Center for Health Workforce Studies, University of Washington, Box 354982, Seattle, WA 98195; Tel: (206) 543-3557; Fax: (206) 6164768; Email: sskillman@fammed.washington.edu Research Objective: To describe Washington State obstetrical providers’ (obstetrician/gynecologists (OBs), family practice physicians (FPs), certified nurse midwives (CNMs) and licensed midwives (LMs)) clinical practice organization, recent changes in their obstetrical practice patterns, and the potential relationship between practice changes and liability insurance factors. Study Design: Mailed four-page questionnaire to obstetrical providers asking about demographic and practice characteristics, type and amount of liability insurance, practice changes and limitations due to liability insurance issues, extent of obstetrical services provided, and future plans for providing obstetrical care. Population Studied: All OBs (n=828), rural FPs (n=579), CNMs (n=255), LMs (n=92), and a 45% random sample of urban FPs (n=1,157), identified from Washington state professional associations and licensing files. Principal Findings: Response rates were 55% (OBs), 41% (urban FPs), 55% (rural FPs), 68% (CNMs), and 71% (LMs). Significantly fewer FPs (28% of urban FPs and 46% of rural FPs) provide obstetrical services than OBs (79%) , CNMs (85%), and LMs (100%). The median age of OBs (47) and CNMs (48) is greater than FPs (43) and LMs (43). Median annual number of deliveries among obstetrical providers is 120 (OBs), 20 (FPs), 70 (CNMs) and 25 (LMs). Liability insurance premiums for obstetrics providers have increased by 58% (OBs), 108% (FPs), 153% (CNMs), and 31% (LMs) from 2002 to 2004. Tail coverage costs affected practice for more OBs (45%) than FPs (27%), CNMs (17%) or LMs (13%). Practitioners reported reducing compensation; reducing liability coverage; and raising cash through loans, liquidating assets or using savings as the most common monetary responses to liability insurance issues. The most common practice changes in the past two years were increasing the number of deliveries (reported by 57% of LMs and 42% of CNMs), increasing the number of C-sections (53% of OBs and 46% of CNMs), increasing OB consults (50% of FPs and 43% of CNMs), and decreasing high-risk OB procedures (49% of FPs). The majority (90-100%) of obstetrical practices accept new obstetrical patients, and plan to increase or maintain the number of obstetrical patients in the coming year (73-98%). Conclusions: Liability insurance premiums have risen dramatically in the past three years for providers practicing obstetrics in Washington state. The cost of tail coverage has affected practice decisions for many providers. Among these practitioners there have been numerous recent practice changes that may represent “defensive medicine”. The effects of liability insurance on obstetrical access for patients in Washington is not clear, but the aging of the OB workforce is a risk for the near future. Implications for Policy, Delivery, or Practice: Many providers have needed to make difficult adjustments to rising liability insurance premiums, leading to the policy question “can further increases be tolerated?” The mean age of Washington’s OB workforce, the highest volume provider group, is nearing the mean age for providers leaving obstetrical practice. If providers leave obstetrical practice, whether because of aging or liability insurance costs, rural areas are most vulnerable because FPs, who are less likely to do obstetrical care and can most easily drop that component of their practices, provide much of the obstetrical care in rural areas. Primary Funding Source: HRSA ●Access in Oregon: An Initial Analysis of Primary Care Physicians from the 2004 Oregon Physician Workforce Survey Jeanene Smith, M.D., MPH, Janne Boone, MPH, Charles Gallia, MS, Tina Edlund, MS Presented By: Jeanene Smith, M.D., MPH, Deputy Director, Office for Oregon Health Policy and Research, 255 Capitol Street NE, 5th floor, Salem, OR 97310; Tel: (503) 378-2422 x420; Email: jeanene.smith@state.or.us Research Objective: Physician workforce adequacy and acceptance of public payers are critical to access to care for low-income, vulnerable populations. The initial analysis of a subset of statewide survey results assesses Oregon’s current capacity to deliver primary care and identifies the barriers to physician participation in public programs. Study Design: A mail-return survey of all licensed physicians in the state. Information was gathered regarding demographics, career satisfaction, anticipation of changes in physician’s practices, acceptance and perceptions of payers and issues regarding the Oregon Health Plan, Oregon’s Medicaid program. Population Studied: The study population of 10,354 physicians, from a database updated quarterly by the Oregon Medical Association (OMA) and the Board of Medical Examiners, were mailed a unique survey instrument designed collaboratively by the OMA with the state’s Medicaid and health policy offices. The response rate was 24% representing 2,419 physicians. Physicians not involved in direct patient care or from hospital-based specialties were excluded from this analysis. Principal Findings: The focus of this analysis includes those in primary care (44% of the respondents) and those in medical and surgical subspecialties (32% of the respondents). Differences between subgroups were tested using chi-square tests of independence. Primary care and specialist satisfaction was similar (86% and 87% somewhat or very satisfied); older providers were more likely to be “very satisfied”, with urban providers more satisfied. Less satisfied physicians were less likely to accept public payers. Patient relationships are the greatest source of satisfaction (59%) while income was a much less important satisfier (4.7%). Cost of doing business emerged as the most important practice issue and public payers’ (Medicaid and Medicare) reimbursement and cost of liability insurance followed. Increased referral of complex cases was the most often noted anticipated change in their practices (37%) in the next two years. Reducing patient care hours, increasing diagnostic procedures performed, and retiring from practice were major changes under consideration. Nineteen percent of primary care providers and 27% of specialists plan to retire in the next five years; this retirement rate is greater than the influx of new physicians into the state. Physicians balance acceptance of public payers with commercial payers, and practices limiting Medicare were more likely to limit Medicaid. Increasing referral of more complex cases (26%) was the most commonly reported reaction to rising liability premiums. Conclusions: Physician response to rising cost pressures and medical liability include increasing referral of complex cases and decreasing hours. These actions further reduce access to primary care. Physicians balance payer types to counter rising costs, and the decision to accept or limit Medicare directly impacts the decision to accept or limit Medicaid. Implications for Policy, Delivery, or Practice: National Medicare reimbursement policy influences physicians’ acceptance of Medicaid as a payer. State Medicaid policy options to stabilize physician participation are limited by this interaction between public payers. Opportunities open to state policymakers to increase physician participation in Medicaid include reduction of administrative costs and support of patient-physician relationships. Primary Funding Source: Oregon Medical Association ●Employment-Based Benefits of Nurses Joanne Spetz, Ph.D. Presented By: Joanne Spetz, Ph.D., Associate Professor, Community Health Systems, University of California, San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: (415)502-4443; Fax: (415)502-4992; Email: jojo@alum.mit.edu Research Objective: A large share of the workforce of the United States receives non-wage benefits in addition to a wage or salary. The principal objective of this study is to provide an overview of what benefits are available to nurses as compared with the general workforce, how health care leaders are approaching the provision of employment-based benefits for nurses, and what nurses have to say about the employmentbased benefits they receive and do not receive. Study Design: The research team analyzed the US Current Population Survey, reviewed the literature, conducted interviews with health care leaders, and conducted focus groups with RNs in two states. Population Studied: Registered Nurses and Licensed Practical Nurses in the United States, and their employers. Principal Findings: RNs are more likely to be enrolled in health and retirement benefits than are U.S. workers in general and those with some college education. LPN enrollments in employer-provided benefits are similar to those of other workers with some college education, but higher than the general workforce. The demographic patterns of enrollment in benefits among LPNs are similar to those of other collegeeducated workers. All the key informants representing employers said their organizations provide a wide range of benefits to their nursing staff. The underlying reasons for offering these benefits included a desire to invest in staff, the need to competitively recruit and retain qualified employees, and the consideration of benefits as part of a total compensation package. Most interviewees who represented employers said their firm offers benefits to nurses working 20 or more hours per week. Focus group participants agreed that the most important benefit is health insurance. Most RNs who do not have benefits work per diem and part-time, and value the flexibility associated with these employment arrangements. These RNs generally received health insurance through their spouses’ employers. Attitudes toward the benefits received at work varied greatly, with some RNs believing that they are very important to overall job satisfaction and others viewing them as less important. Conclusions: Nurses value the benefits they receive as part of their employment. Relatively high shares of RNs receive benefits from their employers, as compared both to the general workforce and those workers who have some college education. LPNs are enrolled in health and retirement benefits at rates similar to those of other college-educated employees. Health care leaders must tread carefully when considering changes to the benefits offered to nurses. It is essential that nurses be consulted about the benefits they want and need, through surveys and focus groups. Implications for Policy, Delivery, or Practice: Improved benefits packages, and higher wages, will not magically solve the problem of recruiting and retaining qualified nurses. Employers must recognize that the financial wages and benefits received by staff must match the market, but that the overall satisfaction of nurses, and their ability to provide highquality care, depends on developing holistic approaches to improving the workplace. While fringe benefits play a role in this holistic approach, they should not be the sole focus of human resource managers. Primary Funding Source: RWJF ●Working Conditions and Organizational Climate in ICUs Patricia Stone, Ph.D., Cathy Mooney-Kane, MS, Elaine Larson, Ph.D., Teresa Horan, MPH, Jack Zwanziger, Ph.D., Andrew Dick, Ph.D. Presented By: Patricia Stone, Ph.D., Assistant Professor of Nursing, School of Nursing, Columbia University, 617 West 168th Street, New York, NY 10032; Tel: (212 )305 1738; Fax: (212) 305 6937; Email: ps2024@columbia.edu Research Objective: The purpose was to identify factors related to working conditions that influence the organizational climate (OC) perceived by intensive care unit (ICU) nurses. Study Design: A cross-sectional design was used. Nurses employed in ICUs were surveyed using the Perceptions of Nurse Work Environment Scale to measure OC. Market- and hospital-level characteristics were identified using American Hospital Association, hospital zip code and Bureau of Labor statistics data. A random effects GLS regression model was developed and respondents were grouped by ICU. We controlled for hospital neighborhood characteristics (i.e., proportion of population in hospital zip code living in poverty and median income). Independent main effects of nurses’ income (actual mean wages adjusted by region and ratio of nurses’ wages to teachers’ wages by region), nurses’ workload (staffing ratios, Nursing Intensity Weights [NIW] and proportion of overtime), setting characteristics (teaching status, Magnet accreditation, National Nosocomial Infections Surveillance [NNIS] affiliation, bedsize and ICU type) and nurses’ characteristics (gender, education, full versus parttime, and ICU experience) were entered into the model. Population Studied: The sample consisted of 647 nurses (response rate 47%) employed in 27 ICUs from 17 hospitals across the nation. The majority of hospitals (n=10) were large (>=400 beds), affiliated with NNIS (n=13) and located in either the Central (n=7) or Pacific (n=7) region. The average respondent was 38.5 years old (SD =9.41), had 9.8 years (SD=9.40) ICU experience, and had worked in their current position for 7.5 years (SD= 7.21). Principal Findings: Approximately 20% of the variance in OC (p <0.05) was explained. Both measures of nurses’ income had significant independent positive effects (RN wages relative to teachers wages [ß = 0.69, 95% CI 0.03, 1.35] and nurses’ mean actual wages [ß = 0.73, 95% CI 0.17, 1.35]) as did NIW (ß = 0.63, 95% CI 0.16, 1.10). Significant setting characteristics included NNIS affiliation (ß = 0.20, 95% CI 0.001, 0.40) and hospital teaching status (ß = -0.28, 95% CI 0.41, -0.14). Nurses with ICU experience less than 1 year perceived the OC more positively than those with more than 12 years experience (ß = 0.19, 95% CI 0.05, 0.33). Conclusions: Controlling for use of overtime and staffing, nurses working in ICUs with more complex patients as measured by the NIWs perceive a more positive OC. The positive relationship between OC and complexity of patients may be related to nurses’ finding rewards in challenging tasks given enough staff. Hospitals active in the NNIS system and paying nurses higher wages have ICU nursing staff who perceive a more positive OC. Implications for Policy, Delivery, or Practice: Many of the factors we found to be independently related to OC are amenable to change. Market solutions (e.g., wage increases) may help, but they are not the only solutions. Designing wellstaffed but challenging workloads may improve the OC. While the model presented is not causal, results may help hospitals to develop and implement strategies aimed at improving the OC in their setting, which may ultimately result in improved patient and institutional outcomes. These findings are important in context of the reports of nurse dissatisfaction and workforce shortages. Primary Funding Source: AHRQ ●Service Requiring Scholarship and Loan Repayment Programs for Nurses in the Southeastern U.S. Samir Thaker, Barbara A. Mark, RN, Ph.D., FAAN, Donald E. Pathman, M.D., MPH, Dennis Zaenger, MPH Presented By: Samir Thaker, Graduate Research Assistant, Cecil G. Sheps Center for Health Services Research, 725 Airport Road, Chapel Hill, NC 27516; Tel: (919) 966-7445; Fax: (919) 966-5764; Email: thaker@unc.edu Research Objective: States and the federal government use service-requiring scholarships and loan repayment incentives to entice nurses into rural and underserved areas. These programs have grown rapidly since the early 1990s when states created many new support-for-service programs for licensed practical nurses, registered nurses, advanced-practice nurses, nurse practitioners and nurse midwives. Relatively little, however, is known about the combined size and operations of these programs, the ways state and federal programs interact, and the optimal design of such programs. In this study, we: (1) identify all programs in the southeastern U.S. that provide financial support for training costs to entice nurses to underserved areas and describe the basic operations of these programs; (2) identify and characterize federal programs operating in this region; (3) describe the region’s nursing support-for-service programs, their combined workforce composition, new program directions, and challenges; and (4) clarify how federal and state programs augment and/or duplicate one another. Study Design: We identify eligible programs through an iterative approach. An initial list of potentially eligible organizations is generated by searching available compendia of nursing and state health professions support programs and by contacting personnel at state nursing boards and schools of nursing. We then conduct semi-structured telephone interviews with program directors to verify program eligibility, obtain program information, and learn of other potentially qualifying programs. Program directors will next be asked to complete surveys about their programs, participants, key challenges, and new directions. Population Studied: Data are being collected from all state and federal scholarship, loan repayment and similar supportfor-service programs intended to entice RNs, LPNs, NPs, CRNAs, CNMs, or CNSs to work in rural and/or underserved regions of eight southeastern states: Alabama, Florida, Georgia, Kentucky, Mississippi, North Carolina, South Carolina, and Texas. We exclude initiatives whose primary purpose is to attract nurses to specific hospitals and communities as well as those that do not make financial support contingent on practice in underserved areas. Principal Findings: We have found that states and intra-state entities employ a wide variety of strategies to entice nurses into needy areas through subsidization of nursing education costs. We will describe this group of programs, their operations and workforces, and greatest strength and weakness. We expect to find that the combined workforce of these state and federal programs is substantial, representing a major thrust in public efforts to maintain an adequate nursing workforce in underserved communities. Implications for Policy, Delivery, or Practice: The findings of this study will help clarify the nature and contributions of these programs and help states and the federal government improve current and future support-for-service programs. Enhancing the effectiveness of nuring support-for-service programs will be an important step toward remedying the geographic maldistribution of health care workers in the southeastern U.S. and other regions. Primary Funding Source: HRSA, ●Dental Hygiene Professional Practice Index Paul Wing, DEngin, Ann Battrell, MA, Margaret Langelier, MS Presented By: Paul Wing, DEngin, Deputy Director, Center for Health Workforce Studies, 1 Discovery Way, B334, Rensselaer, NY 12144; Tel: (518)402-0250; Fax: (518)402-0252; Email: pow01@health.state.ny.us Research Objective: To create a numerical index that rates the legal practice environment of DHs in the 50 states and DC, and to explore the relationship of this index to access to dental services and oral health outcomes. Study Design: A Dental Hygiene Professional Practice Index (DHPPI) is described that defines the professional status, supervision, tasks permitted, and reimbursement options for DHs in each of the 50 states and DC as of December 31, 2001. Spearman rank order correlations between the DHPPI and numbers of oral health professionals, utilization of oral health services, and oral health outcomes in the 50 states are also presented. Population Studied: This study involves cross-sectional analyses of statistics for the 50 states and DC. Principal Findings: 1) There are significant differences in the legal practice environment (as reflected in the DHPPI) across the 50 states and DC. 2) Between 1990 and 2001 the numbers of DHs per capita increased by 46% in the US, while the number of dentists per 100,000 population increased by only 10%. 3) The DHPPI was not significantly correlated with the numbers of DHs or dentists in the 50 states in 2001. 4) The DHPPI was significantly positively correlated with the salaries of DHs in 2001. 5) The DHPPI was also significantly and positively correlated with a number of indicators of utilization of oral health services and oral health outcomes. Implications for Policy, Delivery, or Practice: Both access to oral health services and oral health outcomes are positively correlated with the DHPPI. This suggests that states with low DHPPI scores would be logical candidates for revised DH practice statutes and regulations to accomplish these objectives. Primary Funding Source: HRSA ●Characteristics of Internationally Educated Nurses in the U.S. Yu Xu, Ph.D., Chanyeong Kwak, Ph.D. Presented By: Yu Xu, Ph.D., Associate Professor, School of Nursing, University of Connecticut, 231 Glenbrook Road, U2026, Storrs, CT 06269; Tel: (860)486-0593; Fax: (860)4860001; Email: Yu.Xu@uconn.edu Research Objective: To profile and analyze characteristcs of internationally educated nurses in the U.S. nurse workforce. Study Design: Secondary analysis of the 2000 National Sample Survey of Registered Nurses (the latest available survey) Population Studied: internationally educated nurses in the U.S. in 2000. Principal Findings: Out of an estimated 2.7 million U.S. registered nurse workforce in March 2000, 3.7% were internationally educated nurses from other countries. Internationally educated nurses tended to be younger, unmarried females from the Philippines, Canada, India, or the United Kingdom in their 40s and 30s living or working in urban areas; they had more years of experience as registered nurses, and were more likely to have completed diploma or baccalaureate nursing programs as their basic nursing preparation; they tended to work in hospitals as staff nurses in direct patient care on medical/surgical units and intensive care units; a disproportionately higher rate were employed in long-term care facilities; they were more likely to work full time in nursing, worked more hours, and earned more. Conclusions: 1. Internationally educated nurses have distinctive demographical, educational, and employment characteristics when compared to U.S.-trained nurses. 2. Internationally ucated nurses as a group were not only more likely to be in the labor workforce, but also participated to a greater extent. Based on these findings, it can be inferred that, given the same number of nurses, internationally educated nurses appear to have a greater effect on relieving the current nurse shortage because they had a longer and more productive working career. Implications for Policy, Delivery, or Practice: Although U.S. healthcare industry has traditionally recruited foreign nurses to relieve periodic nurse shortages, it is unrealistic and impossible to depend solely on foreign nurses to resolve the issue. Policy-makers need to develop a long-term socially responsible workforce policy in order to eliminate the cyclic nurse shortage. However, until then, recruiting foreign nurses to relieve U.S. domestic nurse shortage remains a pragmatic alternative, at least for now and the foreseeable future. Primary Funding Source: No Funding Source