Long-Term Care
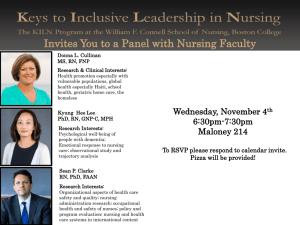
advertisement

Long-Term Care Call for Papers Payers, Recipients & Providers Respond: Behind the Trends in Long-Term Care Utilization Chair: Vincent Mor, Brown University Monday, June 27 • 9:00 am – 10:30 am ●Impact of LTC Insurance on Setting and Use of Formal and Informal Care Christine Bishop, Ph.D., Boryana Dimitrova, Ph.D., Marc Aaron Cohen, Ph.D. Presented By: Christine Bishop, Ph.D., Professor and Director, Ph.D. Program, Schneider Institute for Health Policy, Heller School, Brandeis University, 415 South Street, Mailstop 035, Waltham, MA 02254-9110; Tel: (781)736-3942; Fax: (781)736-3905; Email: bishop@brandeis.edu Research Objective: Using a national sample of elders with disabilities enriched with a study group consisting of elders claiming benefit under private long-term care insurance policies, we investigate 1) the effect of insurance on the relative use of alternative services covered by insurance, namely nursing home care and care at home; and 2) the effect, for persons who remain in the community, of insurance on use of paid care and informal, unpaid care. Study Design: Economic theory suggests that private LTC insurance may affect the service choices of elders with disability needs, because it provides additional resources to insured persons when they need care. Because private LTC insurance has been marketed only relatively recently and is often not used until many years after coverage begins, we use a choice-based sample approach to develop a database with sufficient insured persons to estimate insurance effects on setting of care at the time of observation and the number of hours of paid and informal care for community residents. We account for measured and unmeasured variables that affect selection into insurance using a recursive bivariate probit model, estimated using maximum likelihood for two dichotomous variables: insured status and residence in a nursing home. Insured status is also included as an independent variable in the nursing home probit to assess its effect on choice of setting (Greene 2003). To estimate effects of insurance on formal and informal care for community resident elders, we account for selection effects of insurance and community residence using a Heckman procedure based on the bivariate probit results (Goux and Maurin, 2000). Population Studied: The population studied are elders with disability sufficient to be in benefit under standard LTC insurance policies: disabilities in two or more activities of daily living or cognitive impairment. They are drawn from the 1999 National Long-term Care Survey and from a survey of the elders in benefit under insurance from seven LTC insurance carriers in 2000. Principal Findings: Elders holding private long-term care insurance are more likely to be observed in community residence than are elders without insurance, after accounting for age, marital status, race, income and level of disability. Income has a negative effect on the probability of community residence. Insured elders use about 20 more hours of paid care per week than do noninsured elders. An additional paid hour reduces informal care by about one-half hour, and an additional unpaid hour reduces paid care by about ¾ hour. Conclusions: Even though the additional resources available to insured disabled elders may be used either for nursing home care or care in the community, elders with insurance are more likely to be observed in community residence than are noninsured elders with similar disability and other characteristics. Community-resident insured elders purchase substantially more paid hours of care than similar noninsured elders. Informal care is likely reduced by paid care, but at less than an hour-for-hour rate. Implications for Policy, Delivery, or Practice: Private longterm care insurance appears to allow elders to exercise their preferences, expressed in many surveys, to reside in their communities despite disability. The increasing penetration of private LTC insurance, with 9% of elders insured in 2002, may portend diminishing demand for nursing home services, and affect public planning and investment for future elder care. Tradeoffs suggest that more paid care could be provided without substantially diminishing provision of care by family and friends, enhancing the well-being of the elderly. Primary Funding Source: RWJF ●Moral Hazard in Nursing Home Use David Grabowski, Ph.D., Jonathan Gruber, Ph.D. Presented By: David Grabowski, Ph.D., Assistant Professor, Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115; Tel: (617)432-3369; Fax: (617)-4323435; Email: grabowski@hcp.med.harvard.edu Research Objective: Nursing home expenditures are a rapidly growing share of national health care spending with the government being the dominant payer of services. Yet, we know remarkably little about the effects of government policy on nursing home utilization. Foremost among the unanswered questions: is nursing home utilization elastic with respect to generosity of public programs? Or, is nursing home an option of last resort that does not respond to public policy? We address these questions by using substantial variation in public policy for nursing homes over the past twenty years. Study Design: We estimate transition models to examine how Medicaid income and asset rules affect the odds of community-dwelling elderly entering a nursing home. We also examine whether the adoption of a medically needy program, which allows an individual to count nursing home expenditures against the Medicaid income threshold, influences nursing home use. Finally, we offer some differences-in-differences-in-differences results that compare different spousal protection rules across high and low asset protection states and single and married individuals. Population Studied: All five waves of the National Long-Term Care Survey, a nationally representative sample of Medicare beneficiaries over the period 1982-1999. Principal Findings: We found a negligible effect of medically needy programs on nursing home use. Using the upper limit of the 95% confidence interval, we found that the introduction of a medically needy program increases the probability of nursing home use by 0.44 to 0.9 percentage points (3.4 to 6.9%). Moreover, the income and asset tests employed by different states did not influence utilization. Finally, the adoption of more generous spousal impoverishment protection rules did not affect nursing home use. Conclusions: Results are consistent with inelastic demand for nursing home care – that is, the generosity of Medicaid rules does not influence nursing home utilization. Implications for Policy, Delivery, or Practice: The large increase in nursing home expenditures over the past few decades is not attributable to increased generosity in state Medicaid payment programs. Our results cannot rule out the “crowd-out” of private payers by Medicaid, but generous Medicaid benefits do not attract additional individuals into the nursing home sector. Primary Funding Source: National Bureau of Economic Research variation in the use of SNFs and IRFs across communities, our findings suggest that substitution between PAC modalities is also driven by hospitals’ PAC ownership. Implications for Policy, Delivery, or Practice: While discharging patients to hospitals’ own PAC facilities may improve information sharing during the transitions, it is unknown whether outcomes are comparable or would be better in an alternative PAC setting. Medicare expenditures will be higher if a setting with a higher cost substitutes for similar care provided in a lower cost setting. The implications of outcomes and costs of substitution between PAC modalities warrant further investigation, and future Medicare PAC payment reform needs to take into account of the interchangeability between PAC modalities. Primary Funding Source: AHRQ ●The Effect of Hospitals’ Post-Acute Care Ownership on Medicare Post-Acute Care Use Wen-Chieh Lin, Ph.D., Robert L. Kane, M.D., David R. Mehr, M.D., MS, Richad W. Madsen, Ph.D., Gregory F. Petroski, MS ●Effect of a State Social Insurance Plan on State Medicaid and Family Support Obligations Lawrence Nitz, Ph.D., Lisa Maria B. Alecxih, MPA Presented By: Wen-Chieh Lin, Ph.D., Assistant Professor, Family and Community Medicine, University of MissouriColumbia, M226 Medical Sciences Building, Columbia, MO 65212; Tel: (573)882-1584; Fax: (573)-882-9096; Email: linwe@missouri.edu Research Objective: To examine the influence of hospitals’ post-acute care (PAC) ownership on Medicare PAC use. Study Design: Cross sectional comparison of PAC use and hospitals’ PAC ownership, using multinomial logit regression to control for confounders. Patient, hospital and market area characteristics, including PAC supply, were controlled for in the model. We considered ownership of long-term care units (LTC), swing beds, inpatient rehabilitation facilities (IRFs), and home health agencies (HHAs). Population Studied: Hospitalized elderly Medicare beneficiaries represented in the 5% beneficiary sample of calendar year 2000, with any of three rehabilitative conditions (stroke, hip and knee procedures, and hip fracture) or three medical conditions (chronic obstructive pulmonary disease, pneumonia, and congestive heart failure). Principal Findings: PAC use was strongly associated with PAC ownership; the effect was more prominent for rehabilitative conditions than for medical conditions. Hospitals were more likely to discharge patients to the PAC modality that they owned, while the likelihood of using other PAC modalities decreased. For hospitals owning IRFs, patients discharged with rehabilitative conditions had 2.2 to 3.9 times higher odds of using IRFs over other PAC modalities (SNFs, HHAs, and No PAC) than those discharged from hospitals not owning IRFs. Similarly, the odds of using SNFs over other PAC modalities were 1.2 to 2.2 times higher for patients, either with rehabilitative or medical conditions, discharged from hospitals owning LTC or swing beds than for patients discharged from other hospitals. The effect of hospital ownership of HHAs was less significant. Conclusions: Across all diseases studied, a hospital’s PAC ownership was associated with an increased use in this PAC modality, while the likelihood of using other PAC modalities decreased. This inverse relationship was especially significant between SNFs and IRFs, suggesting a substitution effect between them. While others have previously shown wide Presented By: Lawrence Nitz, Ph.D., Professor, Political Science, University of Hawaii at Manoa, 2424 Maile Way, Room 640, Honolulu, HI 96822; Tel: (808)956-8665; Fax: (808)956-6877; Email: lnitz@hawaii.edu Research Objective: This study offers a prospective examination of the effects on state Medicaid expenditures for institutional and wavered Long Term Care (LTC) services due to the introduction of a social insurance package intended to cover the first year of costs of care. The package was designed to cover an unrestricted of benefits typically delivered in the home or in a community setting, up to a maximum of $70/day (for the first year, 3+% annual increase thereafter). The actuarial model for the package provided for a $10/month flat tax, increasing at an annual anticipated inflation rate of 3%, to be levied on all taxpayers with household incomes above the poverty line. Access to benefits would be graduated over time, so as to present the same opportunity to long term residents and to newly arrived residents Study Design: The study is based on applications the Brookings-Lewin-ICF Long Term Care Financing Model. The base run of the model introduces no new social insurance package, allows retail LTC insurance sales and lapses at typical market rates, and accounts for Medicaid and Medicare expenditures at rates which approximate those paid in the State of Hawaii in 2002. The test runs of the model introduce the proposed social insurance package, stage the gradual acquisition of rights to program benefits, and execute a Monte-Carlo simulation of life stages and LTC-related morbidity events for a 30 year period for the target population. Outcomes are tabulated in terms of numbers of users of LTC services, payments from various sources, age, income and wealth distribution of beneficiaries, and Medicaid and Medicare LTC expenditure totals Population Studied: The original Brookings-Lewin population was renewed in the late 1990s. This population is based on CPS and administrative retirement records, and designed to represent the U.S. population in the aggregate. Each record in the sample database contains information on a person's age, sex, marital status, income, assets, and other characteristics. The model simulates changes for each individual in the sample population from 1986 to 2050, simulating changes in age, economic status, disability status, utilization of long term care, and method of paying for such care. For use in Hawaii, the population was re-weighted to mirror Hawaii’s observed and officially projected age/sex distribution. This was critical because estimates of service utilization and/or cost of services for the elderly in Hawaii would be underestimated by using the Mainland, U.S. population, which has shorter longevity than Hawaii’s. The population size was adjusted to match the values set by the State Department of Business, Economic Development and Tourism for the next decades. Principal Findings: Social insurance programs which offer LTC services at the beginning of frailty have the capacity to provide substantial family relief by making third party care giving possible. The home and community care needs of about 75% of older residents may be met by such a program for a relatively small expenditure, provided that the entire nonpoor population is enrolled. Institutional long term care paid by the social insurance program, though not the focus of its benefit, is typically three to five times the payment made under the conventional private LTC insurance system that exists today. The amount of home and community care paid for by the one year benefit is more than thirty times that paid for in the uninsured base case. Conclusions: A social insurance program for a state's whole population provides an efficient mechanism for financing early and lower-intensity LTC needs of the state's frail edlerly population. Such programs can generate large multiples of home and community service, compared to the quantities funded by common long term care insurance. Savings from the state Medicaid accounts are initially modest, compared to those available from a social insurance program which paid for late-stage care. In such programs, however, the question of how to finance early stage LTC care is unfortunately left open. Implications for Policy, Delivery, or Practice: Partitioning the risk pool for LTC care and paying for part of it by a social insurance pool is an effective mechanism for delivering services, but one which faces substantial opposition from existing providers of financing. Making funded care available through the population, however, increases the opportunity for the mddle-aged caregivers to continue in their labor force positions, securing their own retirement benefits. This opportunity may be critical in states in which larger numbers of married women have traditionally been in the workforce. Primary Funding Source: Research funded in part by the 2002 Executive Office on Aging, of Hawaii's Governor Cayetano Administration. ●Prevention Guidelines and the Risk of Nursing Home Admission Louise Russell, Ph.D., Elmira Valiyeva, Ph.D., Jane E. Miller, Ph.D., Monika M. Safford, M.D. Presented By: Louise Russell, Ph.D., Research Professor, Institute for Health, Health Care Policy and Aging Research, Rutgers University, 30 College Avenue, New Brunswick, NJ 08901; Tel: (732) 932-6507; Fax: (732) 932-6872; Email: lrussell@ihhcpar.rutgers.edu Research Objective: National campaigns are directed toward modifying lifestyle-related factors, such as smoking, elevated blood pressure, and obesity, which contribute to poor health. The U.S. Preventive Services Task Force (USPSTF), the Joint National Committee on Prevention, Detection, Evaluation, and Treatment of High Blood Pressure (JNC), and other groups have published recommendations to help primary care physicians advise their patients. While risks of disease, hospitalization, and death attributable to these factors have been well studied, their effects on the risk of nursing home admission are less well known. This paper examines the risk of nursing home admission attributable to lifestyle-related factors in a nationally representative sample of older adults. Study Design: A multivariable Cox proportional hazards analysis was conducted using data from the NHANES I Epidemiologic Followup Study (NHEFS), a nationally representative sample of U.S. adults whose nursing home use was tracked for 20 years after baseline (1971-1975). Categorical variables were defined to distinguish unhealthy from healthy levels of each baseline risk factor, as defined by the major national guidelines, and to compare the risks of subsequent nursing home admission at those levels. For example, since the USPSTF recommends that physicians counsel patients whose body mass index (BMI) is 30 or higher, BMI 30+ was distinguished from lower BMIs. Smoking, systolic blood pressures 140 mm Hg or higher, lack of regular physical activity, total cholesterol 240 mg/dL or higher (and 200+), diabetes and other chronic conditions diagnosed by baseline, and age, gender, and race were also included in the regressions. Population Studied: A cohort of 6462 community-dwelling adults aged 45-74 at baseline (1971-1975). Persons 45-64 (n=3526) and 65-74 (n=2936) were analyzed separately to explore whether lifestyle choices were equally important in the two age groups. Principal Findings: Persons 45-64 experienced 282 nursing home admissions and those 65-74 experienced 900 admissions over the 20 years of follow up. Except for total cholesterol, all lifestyle-related factors were statistically significant determinants of the risk of nursing home admission in one or both age groups (P<0.05). Diabetes tripled the risk of future nursing home admission for persons 45-64, but increased it only about 50% in persons 65-74. Smoking increased risk by more than 50% among middleaged persons and a third in older persons. Systolic blood pressure 140+ and BMI 30+ increased risk in both groups by about 30%. Lack of regular physical activity increased risk in middle-aged persons, but was not statistically significant in older persons. In the finished paper, attributable fractions will also be presented. Conclusions: Lifestyle-related factors targeted by national prevention guidelines, especially smoking, elevated blood pressure, obesity, and diabetes significantly increase the risk of nursing home admission. Implications for Policy, Delivery, or Practice: If older persons followed the national guidelines for lifestyle choices and management of chronic diseases such as diabetes, nursing home admissions could be substantially reduced. Better choices are effective at older ages as well as in middle age, but the higher rates and numbers of admissions among the oldest make preventive efforts in this age group particularly compelling. Primary Funding Source: AHRQ Call for Papers Improving Nursing Home Outcomes: Measurement & Policy Chair: Christine Bishop, Brandeis University Tuesday, June 28 • 8:30 am – 10:00 am ●Nursing Home Quality as a Public Good David Grabowski, Ph.D., Joseph Angelelli, Ph.D., Jonathan Gruber, Ph.D. Presented By: David Grabowski, Ph.D., Assistant Professor, Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115; Tel: (617) 432-3369; Fax: (617) 4323435; Email: grabowski@hcp.med.harvard.edu Research Objective: Despite differential payment rates across different payer types, policymakers and researchers have generally assumed nursing home quality is common across all residents within a facility. Surprisingly, there has been little work challenging this assumption. Thus, we test whether nursing home quality is in fact a public good. Study Design: We estimate both nursing home and individual fixed-effects models to exploit within-home and within-person (i.e., spend-down) variation in payer type and quality. In the latter model, we also examine the timing of any potential Medicaid effect by examining quality in the periods preceding and following spend-down from private-pay to Medicaid. If there is a Medicaid causal effect, we would expect no effect in the periods preceding spend-down, but negative effects following transition. Population Studied: All Minimum Data Set assessments for seven states over the period 1998-2002. Principal Findings: Using a range of process and outcome based measures of quality, both estimation strategies do not suggest large quality differences across Medicaid and privatepay. In the minority of instances where Medicaid quality appears worse, the timing of the Medicaid effect does not suggest a causal effect, but rather a continuing (unbroken) downward trend. Conclusions: Our results are consistent with the long-held assumption that quality is common within facilities for Medicaid and private-paying residents. Implications for Policy, Delivery, or Practice: State Medicaid programs typically pay below the private-pay price. Thus, there is the potential for free-ridership on the part of state Medicaid programs. Although state Medicaid administrators have historically used certificate-of-need laws to keep private-paying residents in joint care settings, two recent trends potentially undermine the value of private-paying patients to state Medicaid nursing home programs. First, assisted living and other nursing home substitutes have siphoned off some private-paying residents. Second, the nursing home industry has become more segregated by payer type across facilities over the last several years. Primary Funding Source: CMS ●Staffing Levels and Quality of Life Outcomes in Nursing Facilities Jiexin (Jason) Liu, Ph.D., MBA, MS, Robert L. Kane, M.D., Rosalie A. Kane, Ph.D., Boris Bershadsky, Ph.D., Howard H. Degenholtz, Ph.D. Presented By: Jiexin (Jason) Liu, Ph.D., Assistant Director of Research, Institute for Health Policy Research, West Virginia University, 3110 MacCorkle Avenue SE, Charleston, WV 25311; Tel: (304)347-1241; Fax: (304)347-1236; Email: acjliu@hotmail.com Research Objective: Investigates relationships between various staff characteristics (staff levels, pools staff, staff stability) and quality of life (QOL) in nursing facilities while controlling for other factors that may influence quality of life and care. Study Design: QOL is defined as outcomes on 10 psychosocial domains (e.g. security, autonomy, dignity) that were collected through personal interviews for a national Centers for Medicare and Medicaid Services project. QOL is case-mix adjusted for age, gender, cognitive status, baseline activities of daily living, and length of stay in the nursing home. The On-Line Survey and Certification Assessment Review data were obtained for nursing-home staffing levels and administrative questionnaires for turnover/stability and pool use. Latent Variable Structural Equation Modeling method was used to analyze impact of all factors mentioned above on QOL simultaneously. Population Studied: About 2,800 nursing home residents in 100 facilities in 6 states were interviewed. Principal Findings: The results from this study indicate that nursing staff level positively and significantly affects QOL. Among different types of nursing staff, registered nurses play a major role in nursing staff level construction and have the greatest positive impact on residents’ QOL. Pool use negatively affects QOL, but it is not statistically significant. Administrative stability and ownership (non-profit) positively affect nursing staff level that nursing facilities use. Financial constraint negatively affects nursing staff level. Indirect effects from these factors on QOL were also identified. Implications for Policy, Delivery, or Practice: Improving RN, or overall staffing level or offering more medical training to LPN could result higher resident QOL. Primary Funding Source: CMS ●How Have Nursing Homes Responded to the Publication of the CMS “Nursing Home Compare” Quality Report Cards? Dana Mukamel, Ph.D., William Spector, Ph.D., Jacqueline Zinn, Ph.D., Lillian Hsieh, MHS, David Weimer, Ph.D. Presented By: Dana Mukamel, Ph.D., Associate Professor & Senior Fellow, Center for Health Policy Research, University of California, Irvine, 111 Academy Way, Irvine, CA 92697; Tel: (949) 824-8873; Fax: (949) 824-3388; Email: dmukamel@uci.edu Research Objective: In November 2002, the Centers for Medicare & Medicaid Services began publishing clinical quality indicators for all nursing facilities on the Nursing Home Compare web site, as part of the Administration’s strategy for promoting quality. The objective of this study was to determine how nursing facilities have responded and what specific strategies have been adopted following publication. Study Design: Administrators of nursing homes were surveyed regarding their facilities’ responses to the reports. Administrators were queried about 23 specific actions they might have taken, including advertising high quality scores, reforming care protocols, strategies designed to change the organization of the work force, staffing levels, and other actions such as purchase of new technology, development or change in quality improvement programs, interaction with the QIOs, and changes in admission policies. We present the responses and the associations between responses and the ranking of the facility by the published quality indicators. Due to differential response rates by region and profit status, responses were weighted such that the results are representative of the national composition of nursing homes. Population Studied: A random sample of 1,502 nursing homes was drawn from among the 15,212 nursing facilities nationally that had at least one quality indicator reported. Response rate was 48.2%. Principal Findings: A large majority (82%) of facilities reviewed their reported quality indicators. The most important basis for comparison in their view was to their state average scores (32%), followed by comparison to local competitors and to their facilities prior scores. Few (2%) considered a national comparison important. Although they report only minimal interest by residents and their families, over 60% of facilities have taken at least some action. The most common response to the reports (around 30%) was changes in care protocols to improve a low quality score. About 20% reported changes in work structure to empower employees, but less than 10% increased staffing. Those with quality indicators showing poor quality (at the bottom 20% of their state distribution) were more likely to take any action (p<0.01) and were more likely to take more actions (p<0.01). Less than 4% reported change in admission practices as a strategy to improve scores. Conclusions: A majority of nursing homes have acted in response to the reporting of quality measures. Responses included changes in the care protocols used. Implications for Policy, Delivery, or Practice: These findings suggest that the nursing home report card may have a positive effect on the quality of care that nursing homes provide by encouraging changes in care processes. Even though there does not yet appear to be great interest on the part of consumers in these measures, providers use these measures as indicators of care problems and are willing to act upon them. This suggests that report cards may be an important tool to encourage nursing homes to improve quality. Primary Funding Source: NIA ●Diabetes Quality of Care Among Nursing Home New Admission Cohort Charlene Quinn, Ph.D., RN, Conrad May, M.D., Ann GruberBaldini, Ph.D., Jay Magaziner, Ph.D., Bruce Stuart, Ph.D., Van Doren Hsu, Ph.D. Presented By: Charlene Quinn, Ph.D., RN, Assistant Professor, DEPM; Division of Gerontology, University of Maryland, Baltimore, 660 West Redwood Street, Baltimore, MD 21201; Tel: (410)706.2406; Fax: (410)706-4433; Email: cquinn@epi.umaryland.edu Research Objective: To determine diagnostic and secondary prevention procedures provided to a diabetic nursing home (NH) population and adverse utilization outcomes as indicators of poor quality. A secondary aim was to determine differences in care and utilization by dementia status. Study Design: This is a retrospective cohort study of Type 2 diabetes care and utilization among new admissions to NHs. The “Epidemiology of Dementia in Nursing Homes” studied a cohort of 2285 new admissions to 59 nursing homes (NHs). Patients were assessed at admission (1992-1995) and an expert panel determined whether dementia was present. Residents were followed through 2 years after admission (in initial NH) through medical chart abstraction and MDS forms. Recently, Medicare and Medicaid cost records from 1992 to 1997 have been added to this database such that Medicare utilization records are available. Indicators of quality management of diabetes for the period 6 months prior to NH admission and for 1 year post admission were identified by CPT code for 8 primary diagnostic/prevention procedures. Utilization (hospital, emergency room and physician visits) was determined for 4 categories of adverse outcomes by ICD9 codes. Population Studied: Among a cohort of 2285 new admissions, 404 were identified as diabetic by MDS at baseline and were included in this study (n=404). In the parent study, over 50% of new admissions had dementia as determined by an expert panel of psychiatrists, neurologists and a geriatrician. Principal Findings: 1. During an 18-month period, NH diabetics use of diagnostic and secondary prevention services was less than recommended by diabetes clinical practice guidelines (42% had one hemoglobin A1c during the period compared to recommendations for quarterly tests; 35% had an annual eye exam; 45% had annual lipid level tests). 2. Adverse outcomes categorized by dehydration, macro and micro vascular events, metabolic complications and infectious complications identified poor outcomes for this NH population. Nearly 40% had a hospitalization for dehydration, 51% had an emergency room visit for hyperglycemia; 27% received physician visits for diabetic gangrene. 3. Utilization and total costs by service categories are presented and observations of findings by dementia status. Conclusions: 1. Clinical practice guidelines for diagnostic and secondary prevention procedures for diabetics in NHs is not followed by providers. 2. Poor quality management of NH diabetics is related to adverse outcomes in utilization of hospital admissions, emergency room visits, and physician visits. Implications for Policy, Delivery, or Practice: Diabetes is a common and costly chronic illness among nursing home residents. Reported prevalence of known diabetes among NH residents ranges from 7 to 27% of residents. Unlike community-based older adults where the responsibility is selfmanagement of diabetes, residents of nursing homes rely on the NH care plan and providers to manage their diabetes. Although clinical practice guidelines for managing diabetes in the LTC setting exist (AMDA, 2002), this study determined providers may not focus on the diagnostic and secondary prevention evaluation of this chronic disease in a LTC setting. In the current environment of shorter nursing home lengths of stay (27 days), adverse outcomes of diabetes contribute to patient conversion to long stay residents at a cost to all payors. Primary Funding Source: NIA ●Using Propensity Stratification to Compare Patient Outcomes in Hospital-Based versus Freestanding Skilled Nursing Facilities Sally Stearns, Ph.D., Kathleen Dalton, Ph.D., George Mark Holmes, Ph.D., Susanne Seagrave, Ph.D. Presented By: Sally Stearns, Ph.D., Associate Professor, Health Policy and Administration, University of North Carolina at Chapel Hill, CB #7411, Chapel Hill, NC 27599-7411; Tel: (919) 843-2590; Fax: (919) 966-6961; Email: sstearns@unc.edu Research Objective: Hospitalized Medicare patients needing post-acute care are often discharged to either a hospital-based or freestanding skilled nursing facility (SNF). Patterns of care by setting are fairly different, as Medicare patients in hospitalbased skilled nursing units typically have shorter stays but higher costs per day than patients in freestanding skilled nursing facilities. This study assesses the extent to which differences in outcomes by setting may be attributable to patient selection rather than underlying institutional differences. Study Design: The analysis uses a propensity score approach to group observations according to their predicted probability of going to a hospital-based or a freestanding SNF. Stratification by referral probabilities has the potential to provide additional control for selection bias. OLS and probit models estimating outcome differences attributable to hospital-based settings (the HB referral effect) are estimated within propensity groups, and the results are compared to those from unstratified estimates. Three outcomes are selected for illustration: Medicare-covered SNF length of stay; preventable hospital readmissions; and the likelihood of discharge to home or community within 30 days of SNF admission. Population Studied: The analysis uses a 50% sample of Medicare SNF admissions from July 2000 through June 2001, using claims data from qualifying hospital and nursing home stays combined with nursing assessments contained in the Minimum Data Set (MDS) and characteristics of the referring and admitting facilities. The analysis sample is are restricted to patients coming from the 48% of PPS hospitals that operated a SNF during the study period because an explicit choice between type of SNF is most likely for these patients. Principal Findings: The results indicate that patients who are good candidates for faster recovery and discharge to the community are preferentially selected into hospital-based units. In unadjusted comparisons, hospital-based Medicarecovered SNF patients relative to freestanding SNF patients have stays that are 58% shorter (13 versus 31 days), are three times more likely to be discharged to home or community within 30 days (63% versus 21%), and are half as likely to have a preventable readmission (7% versus 13%). The unstratified regression approach reduces the hospital-based differentials by one-third to one-half. The stratified regressions further reduce the differences, especially for patients most likely to be referred to hospital-based units. For these patients, being in a hospital-based SNF is associated with having a Medicarecovered length of stay that is 17% shorter, being 7 percentage points more likely to be discharged to home or community, and being 1.1 percentage points less likely to have a preventable readmission. These remaining differences are, however, statistically significant. Conclusions: While unstratified regressions control for much of the selection, the results suggest that propensity stratification further reduces selection bias for estimating sample average effects of hospital-based settings on the outcomes studied. Implications for Policy, Delivery, or Practice: Much but not all of the difference in outcomes associated with type of SNF are attributable to patient selection that can be accounted for by observed patient characteristics. Remaining differences in outcomes by setting may be due to underlying differences in facility patterns of care or may reflect residual bias due to unobserved factors. Primary Funding Source: Medicare Payment Advisory Commission Related Posters Poster Session A Sunday, June 26 • 2:00 pm – 3:15 pm ●Unmet Service Needs in a Medicaid Population with Physical Disabilities Susan Allen, Ph.D., Susan Wieland, MS, Christine Payne, Ph.D. Presented By: Susan Allen, Ph.D., Associate Professor, Community Health, Brown University, Box G, Providence, RI 02912; Tel: (401) 863-3818; Email: Susan_Allen@brown.edu Research Objective: Persons with chronic disabilities who are covered by Medicaid may need a broad array of supportive services in addition to medical care to manage their conditions. The purpose of this study was to determine the prevalence of unmet service needs in a working age Medicaid population with physical disabilities. Study Design: A randomly selected sample of 550 Medicaid recipients drawn from the Rhode Island Medicaid Management Information System were surveyed by telephone. The prevalence rates of unmet need for 18 specific services were calculated for the full sample as well as for the subset of respondents who reported need for the service in question, and events/trials logistic regression was used to identify factors associated with unmet need, including indicators of program factors that are amenable to change. Population Studied: The target population of this study was the fee-for-service working age Rhode Island Medicaid population with physical disabilities. Principal Findings: Unmet need for medical services was low in this population, i.e., 1% reported inability to get a doctor's appointment when needed, and 8.7% were unable to get needed specialty medical care. Rates of unmet need for ancillary and supportive services were substantially higher. Specifically, 20.2% of the full sample and 31.2% of respondents who reported needing dental care in the previous year were unable to get it, and 15.7% of the full sample and 25% of respondents who reported needing eyeglasses in the past year were not able to get them. Unmet need for other types of ancillary and social services was lower in the full sample but similarly high among respondents who reported needing them. Several program related features were protective against unmet need, including having one's own doctor, having a hospital clinic or health center as a usual source of care, and having help getting services. Conclusions: Although Medicaid is known as the best insurance mechanism for covering long term care, there is inadequate coverage of community-based services hat can help people with disability successfully manage their conditions and maintain community residence. Implications for Policy, Delivery, or Practice: Our findings speak to the need to develop programs that are a better fit with the disabled population covered by Medicaid. These data can be used to target areas of improvement, and speak to the importance of continuity of care and the potential benefits of case management in helping meet the needs of this vulnerable population. Primary Funding Source: No Funding Source ●The Impact of For-Profit Ownership on the Delivery of Hospice Care Melissa D.A. Carlson, MPH, MBA, Elizabeth H. Bradley, Ph.D., Mark J. Schlesinger, Ph.D., Theodore Holford, Ph.D. Presented By: Melissa D.A. Carlson, MPH, MBA, Doctoral student, Health Policy and Administration, Yale University, 60 College Street, New Haven, CT 06520-8034; Tel: (917)4347293; Email: melissa.carlson@yale.edu Research Objective: The decade of the 1990’s witnessed dramatic growth in the number of for-profit hospice providers. Despite this growth, little is known about the relationship between ownership (i.e., for-profit and nonprofit) and the delivery of hospice care and how this relationship may have changed over time as the prevalence of for-profit hospice providers increased. This study estimates differences in hospice care processes for patients of for-profit and nonprofit hospices over the period 1992-2000. Study Design: This paper uses data from the National Home and Hospice Care Survey (NHHCS), a nationally representative dataset of hospice organizations and their patients, over the period 1992 to 2000. Hospice care processes are measured by the range of services received by patients and the predicted probability of receiving individual hospice services. Multivariable ordered logistic regression was used to estimate the association between ownership and service use, adjusting for potentially confounding patient and organizational characteristics. Models were also estimated among subgroups of patients based on hospice certification status, the patient’s referral source, and whether the hospice was horizontally and/or vertically integrated. Population Studied: There were 9,409 discharged hospice patients surveyed over the 5 years of the NHHCS representing a national estimate of approximately 2,000,000 hospice patients after applying the sample weights. Principal Findings: In the subgroup of non-certified hospices, patients of for-profit hospices received a significantly narrower range of services than patients of nonprofit hospices (OR=0.08, 95% CI 0.02,0.31) and this effect was consistent over time. In the full sample, there was a significant interaction between ownership and time (P-value=0.002) on the delivery of hospice services indicating that in earlier years, patients of for-profit hospices received a narrower range of services than patients of nonprofit hospices but this effect was diminished over time and reversed in the final year of the study. This trend over time was particularly evident in services that address the fundamental principles of hospice, including social and family-related services. Differences in the probabilities of receiving these types of services in for-profit compared to nonprofit hospices were substantial, varying up to 20 percentage points in some years. The dynamic effect of ownership over time was evident in the subgroup of standalone hospices but not in vertically and/or horizontally integrated hospices. Conclusions: The relationship between hospice ownership and the delivery of services is complex, depending on the time period, the type of hospice service, and the certification status of the hospice provider. Implications for Policy, Delivery, or Practice: The dramatic and stable effect of ownership in non-certified hospices (and no effect of ownership in certified hospices) lends support for policies that seek to use regulation to address ownership differences in the delivery of healthcare services. Primary Funding Source: No Funding Source ●Rapid Expansion of the Home- and Community-Based Personal Assistance Workforce Susan Chapman, Ph.D., RN, H. Stephen Kaye, Ph.D., Robert Newcomer, Ph.D., Charlene Harrington, Ph.D., RN Presented By: Susan Chapman, Ph.D., RN, Assistant Adjunct Professor, Center for the Health Professions, University of California San Francisco, 3333 California Street, Suite 410, San Francisco, CA 94118; Tel: (415) 502-4419; Fax: (415) 476-4113; Email: susanac@itsa.ucsf.edu Research Objective: People with disabilities often need formal personal assistance or long-term care services in order to live independently in the community. Prior research has shown that lack of availability of such services can lead to adverse health consequences, physical or social isolation, or institutionalization. The objective of this project is to assess whether the size of the personal assistance service (PAS) workforce has kept pace with the needs of people with disabilities for such services, and to study trends in employment conditions for this workforce. Study Design: Multiple time series obtained from secondary analysis of three nationally representative Federal surveys: the basic monthly Current Population Survey (CPS) for 19942004, along with the annual demographic and biennial job tenure supplements to the CPS; the annual National Health Interview Survey (NHIS) for 1994-2003; and the annual American Community Survey (ACS) for 2000-2003. Workforce data are obtained from the CPS and ACS, and data on employment conditions (earnings, job tenure, unemployment, and health insurance) come from the CPS and its supplements. Data on the population needing PAS come from the NHIS. Population Studied: (1) The home health and personal assistance workforce, as defined by stated industry and occupation of employment. (2) Elderly and non-elderly adults and children needing help with one or more Activities of Daily Living (ADL), such as bathing, dressing, or transferring. Principal Findings: There was a rapid expansion in the homeand community-based PAS workforce during the past decade, from 0.5 million workers in 1994 to more than 0.9 million in 2004. Particularly rapid growth occurred during the mid1990s and between 2001 and 2004. With no commensurate decline observed among similar workers employed in nursing homes and residential care facilities, the data suggest that the growth in the PAS workforce is the result of new workers entering this field. The growth rate exceeds that of the community-resident population needing help in ADLs, which also grew substantially during the period, suggesting increasing availability of formal PAS to those needing it. Wage levels for PAS workers remain low, however, and health insurance benefits remain rare. Job tenure data indicate high rates of turnover for these workers. Conclusions: With the expansion in the workforce identified as providing home health or personal assistance services in community settings, exceeding the recent growth in the population needing such services, people with disabilities should be increasingly able to obtain the paid help they need in order to live independently in the community rather than facing institutionalization. High turnover rates, low pay, and lack of benefits suggest, however, that the quality of help received may persist as an important concern. Implications for Policy, Delivery, or Practice: The shift away from institutional care indicates a need to focus a greater share of resources toward training and increased retention of home care workers and personal attendants. Primary Funding Source: National Institute on Disability and Rehabilitation Research ●Hard Choices: The Role of Ethics Committees in Assisted Living Carol Cirka, Ph.D., Carla M. Messikomer, Ph.D. Presented By: Carol Cirka, Ph.D., Assistant Professor, Business and Economics, Ursinus College, 219 Bomberger Hall, Collegeville, PA 19426; Tel: (610)409-3000 x2842; Fax: (610)363-3506; Email: ccirka@ursinus.edu Research Objective: Assess the existence and use of ethics committees (EC) by assisted living facilities (ALFs), licensed in Pennsylvania as “personal care homes” (PCHs), in four suburban Pennsylvania counties adjacent to Philadelphia. This study evolved from a long-term project that examined how everyday ethical issues are identified, managed and resolved in assisted living (AL). Study Design: This study used a three-pronged approach: 1) Ethnographic-type interviews, a portion of which focused on the existence, access to, and use of ethics committees to resolve everyday ethical dilemmas, with staff of five ALFs that vary on a number of dimensions; 2) A case study of the development of an ethics committee in a non-profit CCRC; and 3) A cross-sectional survey (mail/telephone) to Executive Directors and Care Coordinators of licensed PCHs in the study population. Population Studied: 134 Pennsylvania ALFs with 20+ beds in Chester, Bucks, Montgomery and Delaware Counties. Ethnographic-type interviews (averaging two hours each) were conducted with Executive Directors, Care Coordinators and Marketing Directors and caregivers in five Chester County ALFs. Original and current members provided data for the case study of an ethics committee (EC). Executive Directors and Care Coordinators at the 134 ALFs were surveyed with telephone follow up. Questions focused on existence and use of ECs in resolving ethical dilemmas that arose in AL. Principal Findings: ECs are not common in ALFs; however, those that are part of a multi-level system or non-profit are more likely to have access to ECs. When ECs exist, they are not used to resolve issues in AL; further, staff does not view them as a resource for managing everyday problems in AL, nor are they widely understood or publicized. Common responses to ethical dilemmas include: 1) Managing the problem informally and locally; 2) “Calling legal” to determine what to do; or 3) Involving the local Ombudsperson. The response depends on the individual(s) involved, personal values and experiences, and comfort level with the particulars of the problem. Employee training rarely includes formal discussion of ethics, which is often left to the immediate supervisor’s discretion. Staff does not voice significant concern about the legal consequences of action or inaction; confusion exists as to the distinction between legal and ethical dilemmas. Conclusions: ECs represent one organizational mechanism to manage ethical dilemmas that emerge from the everyday operations of ALFs. Evidence indicates that while ECs are institutionalized in acute-care settings, non-acute care settings have been slow to establish and use them. Nursing homes tend to rely on ECs for issues surrounding palliative and endof-life care; however, ALFs, in contrast to both acute care and nursing homes, have little knowledge of or experience with them. Even when ECs exist in a multi-level system, ALFs do not view them as a resource to sort through and manage the complexities of everyday ethical dilemmas. Implications for Policy, Delivery, or Practice: Ethical dilemmas are common in AL; however, resolution often depends only on people involved in the immediate problem. There is a need to develop organizational structures and processes that are not exclusively person-dependent. Doing so should improve quality of care, equity, and staff morale. Primary Funding Source: No Funding Source ●Profit Status and the Relationship Between Medicaid Reimbursement and Quality Carrie Davidson, MA, Ph.D. Presented By: Carrie Davidson, MA, Ph.D., Data Analyst, Ohio KePRO (Medicare QIO), 1495 Woodward Avenue, Lakewood, OH 44107; Tel: (216)221-6998; Email: cxd39@case.edu Research Objective: Determine whether any relationships between Medicaid payments for direct care and efficiency and the facility’s nurse staffing are significantly different depending on the nursing home’s profit status. Study Design: Retrospective cohort design Population Studied: 145 non-profit Ohio Medicaid certified nursing facilities (excluding government-run and hospitalbased facilities) and 391 for-profit facilities with three years of cost reports where costs justified rates paid in subsequent rate years. Principal Findings: Using OLS regression and a stratified sample on the basis of profit status, three distinct ratios of nursing minutes provided (RN, LPN, and Nurse Aide) to nursing minutes needed (using quarterly RUGs-III classifications at the facility level) were regressed on three Ohio Medicaid revenue streams (rate per case mix unit, indirect efficiency payment, and capital efficiency payment) weighted for the percent Medicaid occupancy in the facility. Control variables included the prior year's net operating revenue and non-operating revenue, and current year's percent Medicare days and concentration of private pay inpatient days >= 40%. Both facilities had a positive association between Medicaid-adjusted rates per case mix unit in the first half of the calendar year and all three nurse staffing ratios. However, they differed in their reactions to rate increases that occur in the middle of the calendar year with non-profits demonstrating a positive and significant association between the RPCMU and nurse aide staffing ratios and for-profits a positive and significant association between the RPCMU and LPN staffing ratios. For both facility types, indirect efficiency payments had a significant and negative association with nurse aide staffing and RN staffing ratios. For FP facilities there was also a significant negative association with the indirect efficiency payment and LPN staffing ratios. FP facilities were the only ones that had a significant (and positive) relationship between the capital efficiency payment and nurse staffing, specifically the nurse aide staffing ratio. Conclusions: There were significant differences between forprofit and non-profit nurse staffing ratios. They also differed significantly as to when they changed these ratios and their use of different Medicaid revenue streams for different types of staff. Implications for Policy, Delivery, or Practice: In light of state Medicaid budget crises and impending cuts, it is important to recognize differences in providers' use of different components of the Medicaid rate in order to minimize the effects of budget cuts on quality of care. Primary Funding Source: AHRQ ●Psychometric Properties of A Brief Quality of Life Instrument for Nursing Home Residents Howard Degenholtz, Ph.D., Jules Rosen, M.D., Nicholas Castle, Ph.D., Vikas Mittal, Ph.D., Rosalie A. Kane, Ph.D. Presented By: Howard Degenholtz, Ph.D., Assistant Professor, Health Policy and Management, University of Pittsburgh, 3708 5th Avenue Suite 300, Pittsburgh, PA 15213; Tel: (412)647-5860; Fax: (412)647-5877; Email: degen@pitt.edu Research Objective: The goal of this study was to test a brief (14 item) quality of life (QOL) instrument for use with nursing home residents with varying levels of cognitive impairment. This study specifically examined the impact of different response options. Study Design: In person interviews with nursing home residents. Five interviews, six months apart were conducted with all residents living in the two study facilities at the time of data collection. At each time period the complete version and a brief version of the QOL interview were conducted. The brief QOL scale was developed by selecting items from the longer multidimensional scale that reflected a majority of the dimensions while minimizing length. The response options for the brief version were changed at each wave to test the impact on completion rates. Versions included dichotomous (yes/no) responses, 4-point Likert type scale, and an ‘unfolding’ version of the question that used serial dichotomous responses rather than a 4-point scale (a ‘yes’ response is followed by ‘often/sometimes’ and a ‘no’ response is followed by ‘rarely/never’). This approach provides more information than a simple yes/no response. QOL interview data were merged with the MDS to adjust for cognitive and functional status. Population Studied: All residents of two nursing homes in the Pittsburgh area were eligible to participate. Each facility had approximately 150 residents Interviews were attempted with all residents using an algorithm to discontinue the interview if the resident did not provide coherent responses. Principal Findings: Response rates were approximately 60% at all waves. Residents who are not capable of using the 4point Likert type scale were able to provide a yes/no response. Residents with significant cognitive impairment according to the MDS were capable of using the unfolding version. Conclusions: A brief QOL scale can be used with a wide range of nursing home residents and produces scores that are highly correlated with the original scale. Implications for Policy, Delivery, or Practice: Nursing home operators, clinicians and policy makers are concerned with the QOL of residents. However, the absence of a widely used instrument has hampered efforts to study or improve QOL. This study demonstrates that a brief instrument can produce reliable data that closely parallels the results using a longer multidimensional scale, and provides insight into the response options that maximize participation from residents with relatively low levels of cognitive function. This brief QOL scale can be used as a screener that identifies areas for deeper questioning using the longer scale or it can be used to track quality improvement activities designed to enhance QOL. Primary Funding Source: AHRQ ●Comparison of Undertreatment among Aged Medicare Beneficiaries in Nursing Homes and the Community Setting: A Case Study of Warfarin Use in Atrial Fibrillation Jalpa Doshi, Ph.D. Presented By: Jalpa Doshi, Ph.D., Health Services Research Scientist, Division of General Internal Medicine, University of Pennsylvania, 1214 Blockley Hall, Philadelphia, PA 19104; Tel: (215)898-7989; Fax: (215)898-0611; Email: jdoshi@mail.med.upenn.edu Research Objective: Under the Omnibus Budget Reconciliation Act (OBRA), CMS mandates that the drug regimen of each nursing home (NH) resident be reviewed at least once a month by a licensed pharmacist. As a result, broad oversight of drug therapy is performed by consultant pharmacists for all NH residents. On the other hand, outpatient drug use has not been systematically monitored in the community except for some beneficiaries in Medicare HMOs and Medicaid. Given the differences in the level of monitoring of drug prescribing, one should expect that all else being equal, the prevalence of undertreatment should be higher among aged Medicare beneficiaries residing in the community than those in NHs. Yet no studies till date have directly examined the differences in medication underuse across the two residential settings. This study compares underutilization of warfarin among NH and communitydwelling aged Medicare beneficiaries with atrial fibrillation (AF). Study Design: The study used the Medicare Current Beneficiary Survey (1997-2000) supplemented with data from Medicare claims and a non-publicly available file on institutional drug administrations for NH beneficiaries in the MCBS. The main outcome variable was the prevalence of any warfarin use. A binary variable on the type of residential setting (i.e. NH versus community) was the main independent variable of interest. The control variables included socioeconomic and demographic factors, survey year of observation, and a host of disease-related factors including number of AF-related physician visits and hospitalizations, other CVD risk factors, presence of warfarin contraindications, number of chronic conditions other than CVD, and selfreported health status. Propensity score techniques were used to compare underuse between community and nursing home residents. Population Studied: NH (n=419) and community-dwelling (n=2915) fee-for-service Medicare beneficiaries aged 65 years or older, having Medicare Part B coverage, and one or more hospital or medical service claims with a diagnosis of atrial fibrillation (ICD-9-CM 427.31) in the 1997 through 2000 MCBS files. Principal Findings: Substantial underuse of warfarin was found across both residential settings. In the unadjusted analyses, the warfarin use was substantially higher among community beneficiaries than nursing home beneficiaries (47% vs. 33%, p<0.0001). However, there were substantial differences in the characteristics of the two groups with NH residents more likely to be female, have lower incomes, and be in poorer health. After propensity score adjustment, not only did the warfarin prevalence rates become more similar in the two groups, but the nursing home sample had a slightly higher (32.3%) rate of warfarin use than the communitydwelling sample (29.1%), albeit, the difference was not statistically significant (p=0.395). Conclusions: Warfarin use is similar across the community and nursing home setting and is substantially underutilized in both settings. Implications for Policy, Delivery, or Practice: The study findings have direct implications for the Medicare drug benefit which will provide voluntary prescription drug coverage to all Medicare beneficiaries, regardless of community or institutional residence, starting in 2006. The law requires prescription drug plan sponsors to have a medication therapy management program furnished by a licensed pharmacist that includes elements such as detection of adverse drug events and patterns of overuse and underuse of prescription drugs. This study raises the need for future studies to evaluate the success of such programs in improving the quality of medication use among Medicare beneficiaries once the drug benefit is implemented in 2006. Primary Funding Source: No Funding Source ●Staff Turnover and Quality of Care in Nursing Homes John Engberg, Ph.D., Nicholas Castle, Ph.D. Presented By: John Engberg, Ph.D., Economist, RAND, 201 North Craig Street, Pittsburgh, PA 15213; Email: Engberg@RAND.org Research Objective: The association between nurse aide (NA) plus licensed practical nurse (LPN) and registered nurse (RN) turnover and quality indicators in nursing homes is examined. Study Design: Indicators of care quality used are the rates of physical restraint use, catheter use, contractures, pressure ulcers, psychoactive drug use, and certification survey quality of care deficiencies. In addition, we use a quality index combining these indicators. The turnover rates are grouped into three categories, low, medium, and high, defined as 020%, 21-50%, and greater than 50% turnover, respectively. Population Studied: Turnover information came from primary data collected from 354 facilities in four states, and other information came from the 2003 Online Survey, Certification And Reporting data. Principal Findings: Multivariate analysis shows that decreases in quality are associated with increases in RN turnover, especially increases from low to moderate levels of turnover, and with increases in NA and LPN turnover, especially increases from moderate to high levels of turnover. Conclusions: The one-year turnover rates identified in this study were 98.6%, 66.8%, and 55.4% for NAs, LPNs, and RNs, respectively. This adds to a rather large body of research over the past 20 years also showing high rates of staff turnover. Most importantly, we also show that very low or very high levels of NA+LPN turnover are associated with lower quality of care and that moderate to high levels of RN turnover are associated with lower quality of care. Implications for Policy, Delivery, or Practice: These findings are significant because the belief that staff turnover influences quality is pervasive. The cross-sectional results are only able to show associations, nonetheless, few empirical studies in the literature have shown this relationship. Primary Funding Source: No Funding Source ●Preference-Based Selection Effects in Elders with LongTerm Care Insurance Mary Goldstein, M.D., MS, Jenny Hyun, MPH, Alan Garber, M.D., Ph.D., Tamara Calvillo, MA, Pamela Mahlow, MA, Lorene Nelson, Ph.D. Presented By: Mary Goldstein, M.D., MS, Associate Professor, Primary Care and Outcomes Research, Stanford University and Palo Alto VA Health Care System, 117 Encina Commons, Stanford, CA 94305; Tel: (650) 493-5000 x62105; Fax: (650) 723-1919; Email: Goldstein@stanford.edu Research Objective: The asymmetric information model predicts a positive correlation between insurance and the occurrence of risky events due to moral hazard or adverse selection. Adverse selection occurs because those most likely to purchase insurance are most likely to file a claim; they may be at a higher health risk of a health event or have stronger care preferences. Underwriting practices attempt to correct for selection based on observable risk factors. Insurers, however, are not privy to information about preferences for care and risk aversion. We examined elders in a Medicare managed care program comparing individuals with and without long-term care insurance (LTCI) on health behavior and differences in their preferences for nursing home care. Study Design: The study uses cross-sectional data from a longitudinal study investigating the impact of ADL dependency on health utility ratings. Population Studied: This study used a convenience sample (n=292) of Medicare managed care enrollees 65-years old and older, of whom 82 had LTCI. Those with and without LTCI did not differ significantly in terms of age, number of living children, ADL and IADL limitations, and total household income. Those with LTCI were more likely to be White and had more years of education than those without LTCI. Principal Findings: Elders with LTCI spent less time depressed or sad and were more likely to engage in preventive health behaviors, such as getting a flu shot, within the last 12 months. Ratings of general health, health satisfaction, ADL and IADL limitations, and chronic disease did not differ significantly between LTCI and non-LTCI groups. Elders with LTCI had higher utility ratings for nursing home care than for care in their own homes given hypothetical ADL dependencies, controlling for current health utility scores. On average, those with LTCI rated their preference for nursing home care 0.12 points (on a 0 to 1 scale) higher than those without LTCI. Conclusions: Elders with LTCI spent less time depressed, engaged in more preventive behaviors, and showed a trend toward rating their health better than their peers. This study suggests that individuals with LTCI may have more awareness of future health events--a concern that is manifested in preventive health behaviors. Elders with LTCI are much less averse to nursing home care than those without LTCI, a preference that may increase the likelihood of nursing home utilization. The study design did not allow us to determine whether the preference differences pre-dated the decision to buy LTCI. Implications for Policy, Delivery, or Practice: Findings suggest that those who seek LTCI have risk-aversion characteristics, manifested in health-seeking behaviors, which balance preference-based selection effects for nursing home care. Although these findings are consistent with asymmetric information, they do not suggest an increased probability of a health event. LTCI providers should assess the impact of managed care programs to minimize moral hazard problems post-insurance purchase and should be more attuned to potential advantageous selection characteristics. Primary Funding Source: NIA, Veterans Affairs HSR&D ●Hospice Care in the Nursing Home: Is Diagnosis Associated with Configuration of Care? Andrea Gruneir, MS, Ph.D. Candidate, Kate L. Lapane, Ph.D., Susan Miller, Ph.D. Presented By: Andrea Gruneir, MS, Ph.D. Candidate, Graduate Student, Community Health, Brown Medical School, Box G-Hemisphere, Providence, RI 02912; Tel: (401) 8639260; Fax: (401) 863-3713; Email: Andrea_Gruneir@brown.edu Research Objective: Although initially designed for people with terminal cancer, the increased availability of covered hospice services along with mainstream recognition of its benefits, have lead to efforts to improve the provision of such services to patients with other types of end-stage illnesses. In the nursing home setting, access to and provision of end-oflife care services to patients with Alzheimer’s disease and other dementias is of particular interest. We sought to quantify the effect of a dementia diagnosis on the configuration of hospice services provided in the nursing home. Study Design: We used a cross-sectional study design. All data were obtained from an administrative database maintained by a single large hospice provider. Four diagnostic groups were created based on the primary diagnosis at the time of hospice enrolment: cancer, dementia, debility, and all others. Configuration of care was measured as the percent of patients who received visits, the median total number of minutes spent with patients, and the median visit length. The configuration of care of several types of providers (physicians, RNs, LPNs, aides, social workers, and chaplains) was examined. We focussed on the first 2 days of care. Population Studied: We included residents of US nursing homes who received hospice services from a for-profit hospice provider between January 1, 1998 and September 1, 2000. Principal Findings: Twenty-seven % had a diagnosis of cancer, 23.5% had dementia, 14.9% had a diagnosis of debility, and 34.5% had other diagnoses. Missing information regarding pain assessment was common in all patients: cancer patients (33%), patients with dementia (67%), patients with debility (51%). Fewer than 20% of all patients were seen at least once by an aide, social worker, or chaplain in the initial 2 day period of hospice care and this did not differ by diagnosis group. Patients with dementia and debility were visited by RNs and LPNs but had less overall care time than patients with cancer. Physicians appeared to be the least involved with direct patient care, yet visited patients with dementia and debility less often than those with cancer. Conclusions: Major differences in the configuration of hospice care in the first two days of care were not observed across diagnosis groups. The extent to which this reflects that hospice care is not directly responsive to the varying needs of different groups needs to be explored. Missing information regarding pain assessment in patients with dementia and debility was highly prevalent. These data may reflect the challenges of pain assessment and control, which are mainstays in hospice care, in patients with communication difficulties. Implications for Policy, Delivery, or Practice: The needs of patients with dementia are likely to be vastly different than those with cancer, and further knowledge is needed to determine whether current conceptualizations of hospice appropriately meet these needs. End-of-life care for patients with dementia may require a very different approach than that taken in the same care of patients with other diagnoses, especially cancer. Primary Funding Source: No Funding Source ●Outcomes of the Assisted Living Pilot Program Susan Hedrick, Ph.D., Marylou Guihan, Ph.D., Michael Chapko, Ph.D., Larry Manheim, Ph.D., Jean Sullivan, B.A., Jane Tornatore, Ph.D. Presented By: Susan Hedrick, Ph.D., Research Career Scientist, Health Services Research and Development Center of Excellence, Department of Veterans Affairs, 1100 Olive Way, Suite 1400, Seattle, WA 98108; Tel: (206)764-2085; Fax: (206) 764-2935; Email: susan.hedrick@med.va.gov Research Objective: Assisted living is the fastest growing type of non-institutional long-term care, but is available primarily to those who have sufficient financial resources to obtain such care on the private market. This study evaluated a pilot demonstration of assisted living supported by the Department of Veterans Affairs, the Assisted Living Pilot Program (ALPP), conducted in 7 Medical Centers in 4 Northwest states. ALPP was designed as a transitional benefit where VA paid for care for a limited period with a goal of transitioning to longer term funding through Medicaid or private pay. Study Design: We obtained data on all ALPP residents’ demographics, health status, utilization, and cost of care over a 12-month period from administrative and clinical records. Data were collected for a comparison group of persons who were eligible for but did not enter ALPP. Population Studied: From January 2002 through December 2004, 779 residents were placed in ALPP facilities. The average ALPP resident was a 70 year-old unmarried white male who was referred from an inpatient hospital setting and was living in a private home at referral. Principal Findings: Residents were admitted as planned to all types of community-based residential care programs licensed under state Medicaid-waiver programs: 55% to Assisted Living Facilities, 30% to Residential Care Facilities, and 16% to Adult Family Homes. At referral, 21% percent received assistance with 4 or more Activities of Daily Living and 37% had indicators of cognitive impairment. Adult Family Homes enrolled residents requiring much greater levels of assistance with Activities of Daily Living and with higher indicators of skilled care needs. ALPP residents showed very little change in health status over 12 months post-enrollment. Of the 517 residents who completed the VA payment period, 232 (45%) stayed in ALPP: 55% on private pay and 41% on Medicaid. The mean cost per day for the first 515 residents discharged from ALPP was $74.83, and the mean length of stay in an ALPP facility paid for by the VA was 63.5 days, for a total cost of $5,030 per resident. The total cost per resident of all health care paid for by VA during the 12-month follow-up period was significantly higher than per comparison group member, controlling for baseline differences. Conclusions: ALPP placed residents with significant functional impairment and a wide variety of physical and mental health conditions in settings that varied widely in size and services. The finding that Adult Family Homes enrolled residents with much greater care needs supports the decision to contract with this range of types of settings. As health status typically deteriorates over time in a population in need of residential care, one possible interpretation of our finding of little change in health status is that ALPP may have helped maintain residents’ health over time. Implications for Policy, Delivery, or Practice: ALPP could fill an important niche in the continuum of long-term care services. However, contracting barriers and cost are important issues to address. Primary Funding Source: VA ●Emergency Department Use by the Elderly Living in Nursing Homes Esther Hing, MPH, RobinRemsburg, Ph.D. Presented By: Esther Hing, MPH, Survey statistician, Department of Health and Human Services, National Center for Health Statistics, 3311 Toledo Road, Room 3409, Hyattsville, MD 20782; Tel: (301) 458-4271; Fax: (301) 4584693; Email: ehing@cdc.gov Research Objective: The frail health of nursing home residents poses challenges to emergency department staff. This paper examines ED treatment patterns for nursing home residents in 2001-2002, and compares this care with treatment received by community dwelling elderly. These comparisons were made to investigate whether some emergency care received by nursing home residents could more appropriately have been treated in the nursing home. Study Design: The National Hospital Ambulatory medical Care Survey (NHAMCS) is an annual 4-stage nationally representative sample survey of roughly 35,000 sampled ED medical encounters in about 480 non-Federal, short-stay, and general hospitals. Population Studied: Emergency department visits by the elderly living in nursing homes (n=1,270) and the community (n=9,316) in 2001-2002. Principal Findings: During 2001-2002, ED visits by nursing home residents comprised only 12% of all elderly ED visits, but the nursing home visit rate (123 visits per 100 persons) was significantly higher than the rate for community dwelling elderly (42 per 100 persons). On average, ED patients from nursing homes were older (82 years) than community dwelling elders (77 years). ED diagnoses were similar for community dwellers and nursing home residents with the following exceptions: ED visits by nursing home residents with injuries (20%) and alteration of consciousness (10%) exceeded that of community dwelling elders (16% and 7%, respectively); community dwelling elderly had more diagnoses involving diseases of the musculoskeletal and connective tissue (7% compared with 3% in nursing homes). The percent of elderly ED visits with ambulatory care sensitive conditions (ACSC) was similar among nursing home residents (13%) and the community (14%). On average, nursing home residents received more diagnostic or screening tests (5.9) and surgical procedures (1) per ED visit than community dwelling elderly (4.9 diagnostic tests and 0.7 procedures per ED visit). Almost half (47%) of ED visits by nursing home residents resulted in admission to the hospital compared with 34% from the community. Among the ED visits with ACSC, nursing home residents were more likely to be admitted to the hospital (54%) than community dwelling elders (39%). Nursing home residents spent more time in the ED (4.5 hours on average) than community dwelling elders (4 hours). Conclusions: During 2001-2002, elderly nursing home residents visiting EDs were frailer and sicker than community dwelling elderly. They were older, had more tests and procedures performed during the visit, had longer ED visits, and eventually were admitted to the hospital more often than community dwelling elderly. Although the proportion of ED visits with ACSC was similar among nursing home residents and community dwelling elderly, those living in nursing homes were more likely to be hospitalized than elders living in the community. Implications for Policy, Delivery, or Practice: The acuity level of nursing home residents treated in ED and the subsequent higher percentage of visits resulting in hospital admissions contribute to the strained resources in EDs. Some nursing home resident ED visits presenting with ACSC, however, could have been more appropriately treated in the nursing home. Shifting care for ACSC to other more appropriate care settings could decrease costs, and free resources for emergency care. Primary Funding Source: CDC ●Frontline Workers and Long Term Care Quality Improvement Susan Horn, Ph.D., Julie V. Gassaway, MS, RN, Siobhan S. Sharkey, MBA, Sandra L. Hudak, MS, RN Presented By: Susan Horn, Ph.D., Senior Scientist, Institute for Clinical Outcomes Research, 699 East South Temple, Suite 100, Salt Lake City, UT 84102; Tel: (801)466-5595; Fax: (801)466-6685; Email: shorn@isisicor.com Research Objective: The objective of Real-time Optimal Care Plans for Nursing Home QI Project is to design, support, and facilitate practice change that is associated with improvements in nursing home health care quality. Study Design: The project goal is to develop and implement redesigned clinical care processes using standardized documentation and timely reporting to promote optimal care planning using research-based best practices. The Project Team partnered with frontline clinical staff (RNs and CNAs) and leadership (administrators, DONs, educators, MDS coordinators) at 11 nursing facilities to develop comprehensive CNA documentation that streamlines numerous existing forms into a single form and promotes CNA involvement in the resident care team. Standardized, scannable documentation forms enable implementation of protocoldriven care: thorough documentation, prompts for specific interventions based on resident needs, and timely feedback on resident status and corresponding interventions. Documentation forms are faxed to an electronic project database and are summarized in useful report formats. Reports are used by facilities to promote complete documentation, data-driven resident care planning, and ongoing monitoring of resident status. Evaluation includes staff satisfaction, development of new in-house acquired pressure ulcers, hospitalizations, and emergency department visits. Population Studied: Eleven US long-term care facilities were selected for participation based on pressure ulcer rates and willingness to participate. Each facility selected 1-3 long-stay units to participate. Number of residents per facility ranges from 25 to 100. Principal Findings: Participating facilities have redesigned and standardized CNA documentation practices to reduce redundancy, support timely and complete communication of resident status, and promote use of best practices to prevent pressure ulcers. Practice improvements are integrated efficiently with existing staff workflow and documentation processes. CNA documentation is streamlined and consolidated into a single form used for each resident, reducing number of CNA forms by 3-7 forms per resident. Reports, sent to facilities weekly and monthly, facilitate realtime care decisions based on resident needs, enable timely feedback and monitoring of care delivery, and help to develop individualized optimal care plans that can be updated to address changes in resident status. Facilities report that working as a partnership and sharing experiences increases their ability to implement new care practices and improve quality of care. CNAs report that forms are easier to understand and provide point of care information on resident needs. Next we are focusing on decreasing time to complete documentation. Conclusions: Comprehensive documentation of frontline CNA observations and reporting information back to clinical staff contribute to early intervention and care plan improvements that decrease development of pressure ulcers. Staff report: “I can see trends that were not apparent previously.” “More comprehensive CNA documentation increases accountability.” Frontline workers are empowered when included in care team processes. Implications for Policy, Delivery, or Practice: Implementing standard documentation and reports containing evidencebased best practice information as part of daily work in nursing homes could greatly improve clinical outcomes, particularly pressure ulcers, and decrease overall cost. Sustainability of quality improvement initiative is greatly enhanced by empowering frontline workers. Primary Funding Source: AHRQ ●Use of Post-Acute Care by Nursing Home Residents: How Prevalent and How Appropriate? Carrie Hoverman, BA, Melinda Beeuwkes Buntin, Ph.D., Lisa Shugarman, Ph.D., Debra Saliba, M.D., MPH Presented By: Carrie Hoverman, BA, Research Assistant, Health, RAND, 1200 South Hayes St, Arlington, VA 22202; Tel: (703)413-1100x5192; Email: carrie@rand.org Research Objective: The Medicare program does not cover long-term care, but it does cover post-acute services aimed at restoring patient functioning after a hospital stay. There is concern that long-term nursing home residents, who are already unable to function independently in the community, may be using post-acute services even though they may not be good candidates for rehabilitation. This concern stems from the fact that facilities are reimbursed at much higher rates for post-acute services than for long-term nursing home care – i.e. there is the possibility for payer substitution—patients getting care similar to the level they received, in the same location as prior to the acute stay, but with Medicare paying for it. Whether or not this is a real concern is, however, unknown. The population that resides in nursing homes prior to an acute hospital stay has gone largely unstudied in terms of post-acute care use and outcomes of rehabilitation. Study Design: We examine nursing home residents’ rates of use of Medicare-paid post-acute services provided in Inpatient Rehabilitation Facilities (IRFs), Skilled Nursing Facilities (SNFs), and by Home Health Care (HHC) agencies, patient outcomes at 2 months and 4 months after discharge, and the fraction of patients who return to the same facility after their acute stay. We examine their post-acute care use and outcomes using Medicare standard analytic files. We then use regression models to predict outcomes controlling for observable differences in case-mix. Population Studied: We identify elderly Medicare nursing home residents discharged from acute care facilities between 2001 and 2003 with a diagnosis of hip fracture or stroke who survived 30 days after their hospital discharge using the Minimum Data Set (MDS) for nursing home residents. Principal Findings: Of the nursing home population hospitalized for hip fracture, 78% use the SNF benefit. The nursing home residents who are hospitalized for stroke use the SNF benefit at a slightly lower rate, 59%, while 34% return directly to the nursing home. Those who use the SNF benefit and those who return directly to the nursing home are surprisingly similar in age, complications, and comorbidities; their mortality rates and rates of resuming long-term nursing home care are also similar. Approximately 85 percent of these SNF patients are returning to the same facility they were in prior to the acute stay, with Medicare paying the bill. Conclusions: Nursing home residents use post-acute care at high rates for a population that is not generally considered a good target for rehabilitation. It is surprising that the population who uses the SNF benefit is so similar to those that return directly to the nursing home, and that the rate of SNF use for the hip fracture cohort is higher than that of the stroke cohort, a condition where there is consensus that rehabilitation improves outcomes. Implications for Policy, Delivery, or Practice: There is evidence of payer substitution in nursing home residents returning to the same facility but with Medicare-paid benefits. This issue needs further analysis to determine the benefits of Medicare-paid post-acute care and rehabilitation for the nursing home population. Primary Funding Source: CMS ●Strategic Behaviors Related to Nursing Home Staffing: A Care Orientation Framework Using Financial Ratio Analysis Bita Kash, MBA, FACHE, Charles D. Phillips, Ph.D., MPH, Catherine Hawes, Ph.D. Presented By: Bita Kash, MBA, FACHE, Graduate Research Assistant, Health Policy and Management, School of Rural Public Health, Texas A&M University Health Science Center, 3000 Briarcrest Drive Suite 300, Bryan, TX 77802; Tel: (979)458-0652; Fax: (979)458-0656; Email: bakash@srph.tamhsc.edu Research Objective: To identify nursing home organizational characteristics and strategic behaviors that are associated with higher direct care staffing levels. Our aim was to identify measurable organizational characteristics beyond the traditional for-profit and not-for-profit ownership comparisons using financial ratio analysis. Study Design: We used a financial ratio analysis framework to identify expense ratios that are associated with the construct of a variable representing the facility’s “care orientation.” A Care Orientation Scale (COS) was developed by testing ten expense ratios for significant covariance with ownership status using ANOVA and two Probit models. We then developed the COS using the Cronbach Alpha reliability testing method. The new COS was included as a predictor variable in both OLS and 2SLS regression models with direct care (DC) staff hours per resident day as the dependent variable. The new COS as well as other organizational characteristics and market variables were evaluated for significance in the prediction models. Population Studied: The population of nursing homes was drawn from the 2002 Texas Medicaid Nursing Facility Cost Report, which included 1,016 facilities. This study does not include hospital based facilities. Texas is unique due to the large number of facilities allowing for a large sample size, high percentage of for-profit facilities with large variations of outcomes, and a well established Medicaid cost report process allowing for a thorough examination of expense and growth strategies. Principal Findings: The new COS was developed using three financial expense ratios - Resident Care Cost Ratio, Food Expense Ratio and Basic Earning Power - and demonstrated high reliability measured by alpha at 0.863. For-profit facilities in Texas seem to be operating at higher occupancy rates, higher case mix complexity, with more Medicaid residents, and significantly lower staffing levels than not-for-profits despite offering higher wages. For-profit facilities are also more likely to be both vertically and horizontally integrated. We found that DC staffing is mostly dependent on organizational factors and less on labor market factors. All regression models demonstrated a strong positive and significant relationship between average CMI and DC staffing, a significant negative effect of Medicaid resident percentages on DC staffing, and a positive effect of facility size on staffing levels. As expected, for-profit status had a negative effect on staffing levels. But, effect size and significance of profit status was dramatically reduced by 50% once COS was introduced to the staffing prediction model. Conclusions: We conclude that the proposed COS is a useful method of evaluating strategic behaviors of “care orientation” and a significant predictor of DC staffing levels. We found that only horizontal integration was a positive predictor of DC staffing, while vertical integration had a negative effect on DC staffing levels. Implications for Policy, Delivery, or Practice: From a policy formation standpoint, it is important to know that the new COS can help identify specific strategic behaviors related to profit status. Therefore, it can be a tool for identifying “good for-profit” and “bad not-for-profit” facilities before deficiencies are detected and reported. This allows for the possible use of the new COS as a “red flag” for early detection of problem facilities. Primary Funding Source: No Funding Source ●Personal Care Services: A National Study of Trends in Programs and Policies Martin Kitchener, Ph.D., MBA, Terence Ng, MA, Charlene Harrington, Ph.D. Presented By: Martin Kitchener, Ph.D., MBA, Associate Professor, Social and Behavioral Sciences, University of California, San Francisco, 3333 California Street, Suite 455, San Francisco, CA 94708; Tel: (415)502-7364; Fax: (415)476-6552; Email: martink@itsa.ucsf.edu Research Objective: The expansion of publicly-funded personal care (PC) is a central goal of policies including the President's New Freedom Initiative. For the three main programs that deliver personal care (Medicaid waivers, Medicaid State Plan personal care services (PCS) optional benefit, and Older Americans Act Title III), this paper presents program (participant and expenditure) and policy (eligibility and cost control) trend data for the period 1999-2002. Study Design: This study conducted descriptive analyses on a unique dataset compiled from four sources: (1) CMS Form 372 Medicaid waiver reports for the period 1999-2002, (2) the authors’ national program data survey of Medicaid state plan PCS in 1999-2002, (3) the authors’ national policy survey of waivers and state plan PCS in 2002, and (4) published program data regarding PC provided under OAA Title III (1999-2002). Population Studied: National Medicaid and Older Americans Act participants Principal Findings: In 2002, the two Medicaid programs that deliver personal care (state plan PCS and waivers) combined nationally to pay for almost 99 percent of formal services and 93 percent of participants. Between 1999 and 2002, the total number of waivers delivering PC rose by 27 helping to spur an increase of 82,031 in participants receiving personal care and 46 percent growth in expenditures. Between 1999 and 2002, the adoption of the Medicaid PCS state plan optional benefit by four states (Florida, New Mexico, North Dakota, and Vermont) helped increase national program participation by 164,372 and maintain PCS as the largest single provider of national PC (61 percent of participants and 63 percent of total expenditures). Among findings from the policy survey, 49 waivers providing personal care reported waiting lists in 25 states. The national average number of persons reported on waiver waiting lists is 810 (range 5-47,014) and the average time spent on a wait list is 5 months (range 2-60 months). Conclusions: The findings illustrate trends including the persistance of significant inter-state variations in the provision of publicly-funded personal care and differential national rates of growth in the Medicaid waiver and state plan PCS programs provided that is still only provided in 32 states in 2002. Implications for Policy, Delivery, or Practice: The program and policy trend data presented in this paper are increasingly important in a policy context that includes state buget deficits, litigation against states following the Olmstead decision, and the President’s NFI which includes initiatives to transition Medicaid nursing facility participants to the community. Primary Funding Source: Kaiser Family Foundation ●Determining Problem Perception: Direct Care Worker Turnover and Absenteeism in Long Term Care Thomas Konrad, Ph.D., Jennifer Craft Morgan, MA, Sara Haviland, MA Presented By: Thomas Konrad, Ph.D., Senior Fellow, Cecil G. Sheps Center for Health Services Research, University of North Carolina at Chapel Hill, 725 Airport Road CB 7590, Chapel Hill, NC 27599-7590; Tel: (919) 966-2501; Fax: (919) 966-3811; Email: bob_konrad@unc.edu Research Objective: Direct care worker turnover (DCW) in long-term care (LTC) continues to be a problem in many states despite the recent economic downturn and is expected to worsen as the baby boomers age and their need for LTC services increase. This aim of this paper is to identify environmental, organizational, and structural factors related to long term care managers' perceptions of human resource problems (e.g., direct care worker absenteeism and turnover). Study Design: This paper utilizes data provided by organizational informants from LTC organizations (nursing homes, home health/home care agencies, and adult care homes) across the state of North Carolina (N=602). The full survey response rates were as follows: nursing homes (57%), adult care homes (44%), home health, home care agencies (44%) and hospice agencies (66%). Non-responder analysis was conducted and no significant differences in the structural characteristics of the LTC organizations were detected between non-responding and responding organizations. These data were analyzed using nested ordered logistic regression models. Population Studied: The study population included a subsample of LTC managers of LTC organizations in North Carolina. Principal Findings: Turnover rates and organizational culture measures appear to be important factors in determining managers' human resource problem perception. Community environment and organizational structure variables, excluding type of LTC setting, were relatively unimportant determinants of the dependent variables. Conclusions: The significant impact of our organizational culture measures suggests that managers feel the reasons for turnover are outside their immediate control – poor workforce, competition, high workload and lack of motivation, rather than those things that might be in their control such as wages and benefits. This contrasts with DCWs’ perceptions that, while competition and stress play a part in why aides report they leave, pay and benefits are consistently identified as some of the major reasons for DCW turnover. Implications for Policy, Delivery, or Practice: These findings emphasize the importance of assessing and addressing the cultural context of LTC organizations when developing social and organizational policies/solutions aimed at improving the situation of DCWs. Primary Funding Source: RWJF, The Atlantic Philanthropies ●Update: Using Risk Adjustment to Compare Medicaid Long-term Care Waiver Program Performance Glenn Landers, MBA, MHA, James P. Cooney, Jr., Ph.D, Mei Zhou, MS. MA Presented By: Glenn Landers, MBA, MHA, Senior Research Associate, Georgia Health Policy Center, 14 Marietta Street, Atlanta, GA 30303; Tel: (404)463-9562; Fax: (404)651-3147; Email: glanders@gsu.edu Research Objective: Compare the 2002 costs and outcomes of patients in four Medicaid long-term care waiver programs to 2000 results using risk adjustment methodology. Study Design: Retrospective cohort analysis of Georgia Medicaid claims data for the years 1999-2002 using the DCGHCC risk adjustment system. Population Studied: All 2002 participants of four Georgia Medicaid waiver programs -Community Care Services Program (CCSP): N = 14,968; Service Options Using Resources in Community Environments (SOURCE): N = 1,005; Independent Care Waiver Program (ICWP): N = 428; Shepherd Care: N = 86 Principal Findings: 1.) All waiver programs experienced significant growth between 2000 and 2002. 2.) 2002 DCG HCC scores decreased from 2000 for the CCSP, SOURCE, and ICWP programs (3.2 v. 3.8, 7 v. 4.0, and 5.4 v. 5.7 respectively) and increased for the Shepherd Care program (7.3 v. 5.5). 3.) Most frequently reported primary diagnoses remained unchanged for all programs except CCSP - CCSP: 2000 Essential Hypertension; 2002 - Diabetes; SOURCE: Essential Hypertension; ICWP: Other Paralytic Syndromes; Shepherd Care: Other Paralytic Syndromes; 4.) Lower proportions of patients across programs experienced inpatient admissions and ER visits. 5.) Between 2000 and 2002, adjusted Medicaid costs increased 42% for CCSP, 21% for SOURCE, and 10% for Shepherd Care, while decreasing 38% for ICWP. Conclusions: Medicaid waiver programs, as they grow and mature, are subject to the same inflationary increases as institutional care. One value of waiver programs may be their abilities to reduce hospital admissions and ER visits. Risk adjustment systems allow the comparison of waiver programs designed to serve different populations. Implications for Policy, Delivery, or Practice: The Shepherd Care program, designed to serve severely physically disabled and brain injured patients, continued to control growth in the cost of services while the program itself grew and admitted patients with significantly higher DCG HCC scores than other waiver program patients. Describing the determinants of the Shepherd Care program's success may assist other Medicaid waiver programs in controlling costs and improving outcomes. Primary Funding Source: Georgia Department of Community Health ●Inside the Black Box of Nursing Home Deficiencies Robert Lee, Ph.D., Sarah Forbes-Thompson, Ph.D., RN, Nancy Dunton, Ph.D., Byron Gajewski, Ph.D., Marcia Wrona, BSW Presented By: Robert Lee, Ph.D., Associate Professor, Health Policy and Management, University of Kansas, Mail Stop 3044, 3901 Rainbow Boulevard, Kansas City, KS 66160; Tel: (913)908-8202; Fax: (913)588-8236; Email: rlee2@kumc.edu Research Objective: To estimate the effects on nursing home deficiencies of differences in nursing home staffing (both levels and turnover rates), while controlling for differences in case mix, market structure, and the survey team. Study Design: The study merged five administrative data sets for 2001 and 2002: cost reports, deficiency reports, turnover reports, quality measure reports, and survey agency reports. The study then used a variety of econometric techniques to estimate a path model of nursing home deficiencies. Population Studied: All free-standing nursing homes in a single state during 2001 and 2002. Principal Findings: Higher staff turnover consistently increased deficiencies. Higher staffing levels had variable effects, reducing deficiencies at very low and very high levels of staffing, but having little impact at intermediate levels. Controlling for staffing levels, larger chain facilities in uncompetitive markets consistently had more deficiencies. For-profit firms and firms facing high wage rates systematically had lower staffing levels. Even after controlling for a rich array of facility characteristics, there were meaningful and statistically significant survey agency effects. Conclusions: Staff turnover emerges as a more powerful predictor of deficiencies than staffing levels. At least part of the variation in deficiency levels can be traced to agency characteristics. Implications for Policy, Delivery, or Practice: Improvements in management can sharply reduce turnover and should be a priority. Further standardization of the survey process is needed to enhance its validity. ●Selectivity Between Two Medicare Capitated Benefit Programs Walter Leutz, Ph.D., Nancy Perrin, Ph.D., Kathy Brody, PHN, Lucy Nonnenkamp, MA, Linda Phelps, MA Presented By: Walter Leutz, Ph.D., Associate Professor, Heller School for Social Policy and Management, Brandeis University, MS035, Waltham, MA 02454; Tel: (781) 736-3934; Fax: (781) 736-3965; Email: Leutz@Brandeis.edu Research Objective: To examine selectivity among Medicare beneficiaries who were offered the choice from 1985 to 2002 of enrolling in Kaiser Permanente Northwest (KPNW), an HMO with two benefit programs: a standard HMO and a demonstration Social HMO (SHMO) with a $5 prescription drug co-payment, a community care benefit worth up to $12,000 per year for those dependent on others for daily care, and a higher member premium. Study Design: To assess selectivity we chose four points (expanding the SHMO service area to two new counties, dramatic premium increase, and a stable period) that presented distinct benefit/price conditions, where those offered the choice ("decision makers") could be identified. Comparison groups were drawn from HMO membership year-end files of over 337,000 person-years to identify subjects with continuous enrollment a year before and after the decision. Administrative databases of hospital, pharmacy, and nursing facilities were analyzed after creating person-based variables for each 24-month observation period. Mortality was observed through 2002. Univariate and logistic regression tests of significance were run using SAS and SPSS. Population Studied: 14,927 joined the SHMO over 18 years. The benefit was offered in periods of open enrollment to community beneficiaries and to HMO individual members. Group retirees were not offered the choice. Principal Findings: (1) With premiums at $49/$75 in 1990, 16.9% of 2,094 decision makers in Clackamas County joined the SHMO. Switchers had at least 58% higher hospital and prescription use both prior to and after switching but did not differ in age. Those who picked the SHMO were 1.6 times more likely to die. (2) With the premium difference rising to $66/$125 in 1991, 6,381 had the choice to stay in SHMO, convert from SHMO to HMO, or convert from HMO into SHMO. The 986 who left SHMO used fewer hospital days, prescriptions filled, and days supplied in 1990 than did those who selected SHMO (441) or chose to remain in SHMO (4,954). In 1991 those leaving SHMO continued to have lower utilization than the other two groups. (3) With a premium difference of $81/$156 in 1995, 11.5% of 3,911 Clark County WA decision makers chose SHMO. Pre and post utilization patterns resembled 1990. (4) From 1999-2002 the premium difference was about $100, and 4,580 decision makers could switch between the HMO and SHMO at any time. Those selecting SHMO (either from HMO or community) more often reported poor health (odds ratio 2.7), recent ED visits (OR 4.7), and needing IADL help (OR 2.1) than those choosing HMO. In the post-enrollment year, SHMO choosers had 97% more hospital use and 64% more days of Rx supply. Conclusions: Better prescription drug and community care benefits attracted sicker and more disabled beneficiaries, who were willing to pay more for better benefits at all study points. Implications for Policy, Delivery, or Practice: Supported by a disability-based Medicare payment formula and higher beneficiary premiums, in 1985 KPNW began offering a highoption supplement, including drugs and community care. As its membership aged, KPNW maintained the SHMO option and added geriatric care components for HMO and SHMO members. Primary Funding Source: RWJF ●Creating an Entitlement for Expanded Community Care Walter Leutz, Ph.D., Lucy Nonnenkamp, MA, Kathy Brody, PHN, Linda Phelps, MA Presented By: Walter Leutz, Ph.D., Associate Professor, Heller School for Social Policy and Management, Brandeis University, MS035, Waltham, MA 02454; Tel: (781) 736-3934; Fax: (781) 7363-3965; Email: Leutz@Brandeis.edu Research Objective: To examine the production and consumption from 1985-2002 of the Social HMO (SHMO) demonstration’s expanded care (EC) benefit and services at Kaiser Permanente Northwest (KPNW). The EC benefit provided up to $12,000 per year per eligible person for inhome services and periodic nursing facility care beyond Medicare coverage, to maintain frail elders in the community. We describe the evolution of benefits, eligibility, case mix, participation, utilization, service and care management costs, and revenue sources. Study Design: A longitudinal, in-depth descriptive study using records maintained by KPNW since 1985 which include aggregate data on study variables. EC costs came from records that tracked authorized services (retroactively adjusted by monthly phone calls to the members to determine actual use and satisfaction) rather than expenditures. Descriptive longitudinal data from administrative reports were analyzed using Excel. SAS was used to merge annual service data and membership files to form person-based episodes for descriptive analysis. Population Studied: Aged, non-ESRD Medicare beneficiaries residing in counties served in the greater Portland OR area, and not residing in institutions, were eligible to join SHMO. From 1985-2002, 14,815 beneficiaries joined, and membership averaged 4,531. Principal Findings: Of those enrolled in the demonstration, 80% remained an average of 4.6 years, and 12% remained 10 or more years. Of those who joined, 40% were aged 75 or older, and as they aged in place, the proportion aged 85 or older grew from 12% in 1985 to 25% in 2002. Those eligible for EC rose from 4% to 27%. In recent years, care plans based on patient and family preferences included personal care 40% of the time, accounting for more than 40% of spending. Two services accounted for 39% of spending: homemaking (in 35% of plans) and periodic respite care in nursing facilities (in 20%). Three services added 8% to spending: personal emergency response systems (in 30%); special equipment (in 30%) and medical appointment transportation (in 20%). The remaining services were in 1% to 6% of plans, accounting for 13% of spending: shift care, home nursing, adult day, RCF respite, dentures, and "other." EC costs rose from $21 PMPM in 1985 to $95 PMPM in 2002. Costs were covered by member premiums (rising from $49 to $180 from 1985-2002) and member service plan co-payments (20% since 1992). Rising costs PMPM reflected increasing eligibility for EC and higher wages rather than costs per person served, which fell from a high of $6,164 per year in 1989 to $4,328 in 2002. Expanded care professional staff providing resource coordination accounted for about one-quarter of EC costs since 1992. EC costs were equivalent to 12% to 16% of reimbursement from Medicare, which used a disability adjustment to its standard formula. Conclusions: KPNW served an increasingly disabled membership by reducing costs per EC plan and shifting utilization to a broadened range of community care services. Implications for Policy, Delivery, or Practice: The most comprehensive Medicare supplement in the USA, including community long-term care, has been offered since 1985 by KPNW. Key supports were the demonstration's disabilitybased Medicare payment formula and beneficiaries' willingness to pay additional premiums. Primary Funding Source: RWJF ●The Effect of Disease Management/Health Promotion Information on the Demand for Personal Assistance Hongdao Meng, Ph.D., Bruce Friedman, Ph.D., Andrew Dick, Ph.D., Dana Mukamel, Ph.D. Presented By: Hongdao Meng, Ph.D., Assistant Professor, Preventive Medicine, Graduate Program in Public Health, HSC, Level 3, Room 071, Stony Brook, NY 11794; Tel: (631)444-7281; Fax: (631)444-3480; Email: hongdao.meng@stonybrook.edu Research Objective: To assess the effect of a disease selfmanagement/health promotion nurse intervention on the demand for personal assistance among a sample of elderly Medicare beneficiaries with chronic conditions. Study Design: This study used data collected for the Medicare Primary and Consumer-Directed Care (PCDC) Demonstration. This was a randomized controlled trial in which patients were assigned to one of 4 groups. A two-part model was estimated for annual expenditures on personal assistance services among individuals who participated in the control (n= 287) and the nurse (n=283) groups. We controlled for individual socio-demographic characteristics, health and functional status, prior use of medical care, and state. Population Studied: 570 chronically ill elderly Medicare primary care patients who did not have private long-term care insurance or Medicaid. Individuals had to be impaired in 2 activities of daily living (ADL) or 3 instrumental activities of daily living (IADL); have had a hospital admission, nursing home admission, or Medicare home health use during the prior year, or two emergency department visits during the prior 6 months; and be enrolled in both Medicare Parts A and B. The mean age of the sample was 80 and more than twothirds were female. 57% had less than $20,000 annual household income. The mean number of ADL and IADL dependencies was 2.3 and 3.5, respectively. 72% had 3 or more chronic conditions. Principal Findings: 81% of the sample had positive expenditures on personal assistance goods or services during a 12-month period. Average annual expenditures on personal assistance totaled $3,430 for the full sample. Parameter estimates from the two-part model indicate that the health promotion nurse intervention did not change the likelihood of using personal assistance, but it reduced expenditures on personal assistance conditional on any use. The overall effect of the disease self-management/health promotion intervention was a 14% reduction in personal assistance expenditures. Conclusions: The results suggest that the disease management/health promotion nurse intervention reduced the demand for personal assistance among elderly Medicare beneficiaries with chronic conditions. Further research is needed to identify the mechanisms responsible for the reduction and to evaluate whether this intervention leads to savings for other types of health services. Implications for Policy, Delivery, or Practice: Providing disease self-management/health promotion information through a nurse home visit program can generate cost savings for personal assistance provided to elderly Medicare beneficiaries with chronic conditions. Primary Funding Source: CMS ●Securing the Future: Why Assisted Living Should Focus on Everyday Ethics Carla Messikomer, Ph.D., Carol C. Cirka, Ph.D. Presented By: Carla Messikomer, Ph.D., President, The Acadia Institute, P.O. Box 251, Exton, PA 19341; Tel: (610)3632366; Fax: (610)363-3506; Email: acadiainstitute@comcast.net Research Objective: This study builds on Kane and Kane’s call to focus on “everyday” ethics in long term care by investigating how “everyday” ethical issues are identified and managed in assisted living (AL) settings on both individual and organizational levels. Study Design: This two-year study employed qualitative techniques in five assisted living facilities (ALFs) in Chester County, Pennsylvania. Data were collected through 40 focused interviews (averaging two hours) with AL administrators and staff. Socio-demographic data on participants were also collected. Findings were made available to the ALFs in the Philadelphia area through customized training sessions. Population Studied: As a microcosm of the national AL market, Chester County offered historical, methodological, and practical advantages. The five participating sites represented the range of ALFs in the national market. Principal Findings: Ethical dilemmas arise in every aspect of AL operations. Few formal mechanisms address how to manage them; the preferred method is individual and local. Lack of consensus on the meaning of AL and aging in place leads to inconsistencies in how ethical issues are defined and managed. They arise as a result of: 1) Pressures to achieve profitability compete with pressures to deliver quality care to an increasingly frail population; 2) Untrained personnel deliver higher levels of care to frail residents without medical supervision; 3) Social justice issues arise from limited affordability and varied responses to depletion of resident assets; 4) Care coordinators exercise significant discretion about how and what care is delivered; 5) Recruiting and retaining qualified staff is a problem at all levels; 6) Confusion exists about the appropriate AL business model and whether a social model of care is viable; 7) Staff are unable to define ethical issues conceptually; 8) Tension exists between marketing promises and the lived experience in AL. Conclusions: Multiple industry, philosophical, structural and process factors give rise to a range of ethical dilemmas, which occur frequently, across functions and ALF types, and involve staff, resident and family-centered questions. When organizational mechanisms exist, they are rarely used to resolve ethical dilemmas. Experience is rarely translated to organizational policy and there is an absence of structures that support development of an ethical culture. Localized and individual management of ethical issues increases the chance that decision making around ethical issues will be random and grounded in individual values, rather than organizational values. Formal discussion and development of processes to support effective responses to ethical challenges will positively impact quality of resident care, market position and performance, ability to attract and retain staff, occupancy rates, client satisfaction, and reduce vulnerability to legal action. Implications for Policy, Delivery, or Practice: This project is the first to examine everyday ethical challenges in AL. Understanding them can make “aging in place” a dignified reality for residents and staff, and make care giving more rewarding. Knowledge of the roots of ethical challenges will enable the industry and individual ALFs to be proactive in developing structures and processes to anticipate and effectively manage ethical dilemmas. Primary Funding Source: Private Donations; Ursinus College ●Doing Better to Do Well: Does Innovation Improve Nursing Home Performance? Vincent Mor, Ph.D., Jacqueline Zinn, Ph.D., Zhenlian Feng, Ph.D., Orna Intrator, Ph.D. Presented By: Vincent Mor, Ph.D., Professor, Community Health, Brown University, Box G-H1, Providence, RI 02912; Tel: (401)863-3492; Fax: (401)863-3713; Email: Vincent_Mor@brown.edu Research Objective: The objective of this study is to determine whether and to what extent innovation associated with the provision of sub-acute care impacts nursing home performance and the survival of the nursing facility as a certified provider. Study Design: We used the Online Survey, Certification and Reporting (OSCAR) system data from 1997-2002. Data on 7 different innovations like special care units and specialty nursing services were used to develop a composite innovation score based on "early adoption" relative to other providers in their market. Performance was defined as occupancy rate, having a high proportion of private pay residents and regulatory compliance. Termination was defined as no longer participating in the Medicare/Medicaid program. We used a cross-sectional time series generalized estimating equation (GEE) model with a logit link function to predict each of the four dichotomous outcomes of organizational performance, controlling for market factors. In analyzing termination, the performance measures as well as innovation score were predictors. Population Studied: We conducted these analyses on all free standing (non-hospital based) nursing homes located in standard Metropolitan Statistical areas in the US. Principal Findings: The proportion of facilities adopting innovations increased over time, but 40% still had no innovative features at the end of the study period. Analysis results revealed high innovation was associated with a 10 to 20% increased likelihood of being in the top quartile on all performance measures. Furthermore, high innovation was protective of termination (AoR .632+/-.48-.83) after controlling for the significant effects of occupancy, payer mix and regulatory compliance. Conclusions: The results of our longitudinal analyses indicate that sub-acute care innovation has a positive impact on a number of measures of nursing home performance and is associated with a lower probability of termination. Implications for Policy, Delivery, or Practice: Little research exists on nursing home innovation, in stark contrast to the extensive research on innovation in hospitals. This may be due to the perception that “nursing home innovation” is an oxymoron and rare at best. However, our study demonstrates that innovation is an important contributor to nursing home performance. Given the key role these organizations play in caring for frail and vulnerable populations, innovation needs to be better understood and encouraged. Primary Funding Source: NIA ●Deriving and Validating a Model of the Necessity to Hospitalize Nursing Home Residents Alistair James O'Malley, Ph.D., Edward Marcantonio, M.D., SM, Rachel Murkofsky, M.D., MPH, Daryl J. Caudry, SM, Joan L. Buchanan, Ph.D. Presented By: Alistair James O'Malley, Ph.D., Assistant Professor of Statistics, Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115-5899; Tel: (617) 432-3493; Fax: (617) 432-2563; Email: omalley@hcp.med.harvard.edu Research Objective: To build and evaluate the validity of a model of the necessity of hospitalizing nursing home residents. Study Design: Expert panel methods were used to obtain information on the necessity of hospitalizing nursing home residents presenting with different conditions. Twelve geriatricians with expertise in nursing home practice rated the necessity of hospitalization for 3000 clinical scenarios using a 9-point scale. Scenarios included information on the primary presenting condition, secondary diagnoses, cognitive and functional status, age, gender, and advance directives. The model included a random effect for expert panelist to account for multiple respondents and possible systematic differences in scoring among them. Independent variables included primary diagnoses, physical and cognitive functioning, age, and gender. Secondary diagnoses were incorporated as interactions with the primary diagnoses. Stringent selection criteria based on effect size and face validity were used to limit the number of primary-secondary interactions in the models. To evaluate validity we formulated a theoretical model that assumes facilities act rationally by generally hospitalizing cases with the highest necessity, implying that higher quality homes will hospitalize fewer residents but those that are hospitalized will have greater necessity. The validity of our predictive model was evaluated by regressing the average predicted necessity score (APNS) on the proportion of residents hospitalized per facility-quarter and on a hospitalization-related overall facility-level quality score (FQ) derived from the MDS quality indicators. Population Studied: The data used to develop clinical scenarios and for the modeling come from 1996 Medicare hospital claims linked to the nursing home Minimum Data Set (MDS) from Kansas, Maine, Mississippi and South Dakota. Principal Findings: The primary diagnosis with the highest necessity score was respiratory failure, followed by acute myocardial infarction (AMI), hip fracture, and brain injury. The secondary diagnosis interaction having the greatest impact was respiratory failure on pneumonia. Poor cognitive and physical functioning lowered the risk of hospitalization, as did advance directives. The final model explained 62% of the variation in the expert panelists’ ratings. We found a significant negative association between the facility-level APNS and the proportion of patients hospitalized (p < 0.0001), and a significant positive association between APNS and FQ (p < 0.0001). In a multivariate model both APNS and FQ had negative associations with hospitalization rate, supporting the assumption of the theoretical model that more capable facilities tend to hospitalize the neediest patients. Conclusions: Using expert panel survey data we derived a predictive model of the need for hospitalization. Real data predictions from this model cohere with results predicted from an underlying theoretical model. Implications for Policy, Delivery, or Practice: Although often important to recover from acute medical problems and exacerbations of chronic illness, there is some evidence that hospitalization may be costly and traumatic for nursing home residents. The model we developed can be used to explain the heterogeneity in hospitalization rates across facilities; to help determine if there are non-clinical predictors of hospitalization; and to help construct guidelines of when to hospitalize. Primary Funding Source: AHRQ ●Moving from Nursing Home to Community: Texas’s Rider 37 Initiative in Medicaid Barbara A. Ormond, Ph.D., Anna S. Sommers, Ph.D. Presented By: Barbara A. Ormond, Ph.D., Research Associate, Health Policy Center, The Urban Institute, 2100 M Street NW, Washington, DC 20037; Tel: (202) 261-5782; Fax: (202) 223-1149; Email: bormond@ui.urban.org Research Objective: The Texas Community Based Alternatives program (CBA) is a Medicaid waiver program with a substantial waiting list. The Rider 37 initiative allows Medicaid recipients in nursing facilities to return to the community and receive services under CBA without joining the waiting list or supplanting someone on it. This study examines the role of Rider 37 in meeting the long-term care needs of Texas Medicaid recipients. Specifically, we compare the characteristics of three types of participants—Rider 37 participants, Medicaid nursing facility clients, and CBA clients—to understand how observed differences among participants may contribute to observed differences in service use and outcomes. Study Design: Using Texas Medicaid long-term care administrative data, we compare clients who have moved from a nursing facility to the CBA program (Rider participants) to clients who remain in the nursing facility and clients who entered the CBA program directly from the community rather than from a nursing facility (CBA clients). We examine sociodemographic characteristics, primary diagnosis, prevalence of mental/behavioral conditions, and assigned level of care (TILE score) across samples. Client outcomes at six and twelve months after entering CBA are compared for CBA and Rider samples. Site visits to three counties provide context for the data analysis. Population Studied: Participants in the Rider 37 initiative (n=4,868), non-Rider CBA clients entering CBA after the inception of Rider 37 (n=16,571), and a representative sample of nursing facility residents (n=66,475); all restricted to those age 21 and over. Principal Findings: We find significant differences with respect to age, sex, race/ethnicity, rural/urban residence, diagnosis, and level of care between Rider participants and adult nursing facility residents and also between Rider participants and non-Rider CBA clients. The qualitative findings, particularly those on race/ethnicity, support these quantitative findings. Rider participants are more likely to have had a nursing facility stay during their first six or twelve months on community care than are similar non-Rider CBA clients and are more likely to have died. Rider participants are more unstable medically and more likely to have dementia than non-Rider CBA clients; they are less likely to have family support and so more often rely on assisted living facilities. Conclusions: The Rider initiative provides a mechanism for clients who do not need nursing facility care but who require some support to be able to live independently in the community. The Rider serves a population that differs in important ways from the population served by the CBA program. Service use and outcomes are related to these population differences. Implications for Policy, Delivery, or Practice: How regions across Texas with different community-based delivery systems and client populations responded to the Rider serves as a lesson for other states considering similar initiatives. The differences between Rider participants and non-Rider CBA clients have implications for the supply of community-based care over the long term. Primary Funding Source: Assistant Secretary for Planning and Evaluation ●Organizational Work Environment and Adverse Events in Home Health Care Timothy Peng, Ph.D., Penny Feldman, Ph.D., John Bridges, Ph.D., Lori King, BA, Chris Murtaugh, Ph.D., Robert Rosati, Ph.D. Presented By: Timothy Peng, Ph.D., Research Associate, Center for Home Care Policy and Research, Visiting Nurse Service of New York, 5 Penn Plaza, New York, NY 10001; Tel: (212)609-5765; Email: tpeng@vnsny.org Research Objective: This paper examines the effect of work environment on the rate of (risk-adjusted) adverse events in home health care using an econometric approach to risk adjustment and a two-stage regression analysis. The study aims to provide home health agencies with evidence on which to base management decisions related to how organizational work environment may affect patient outcomes. Study Design: Work environment was measured through a combination of administrative data and staff surveys conducted at a prior point in time from patient outcomes. Staff surveys included a variety of measures, including perceptions of workload, access to resources, equity, teamwork, and supervisor’s safety culture. Patient data were collected over a six-month time frame, resulting in 56,346 episodes of care. The dependent variable was the occurrence of any of the 13 adverse events defined by Center for Medicare and Medicaid Services in its Outcome Based Quality Monitoring Reports. First-stage regression models included risk-adjustment for episode-level case mix, and used a fixedeffects approach to calculate, for each of 87 teams, a quality score based on team-attributable adverse events. Secondstage multivariate regressions modeled the impact of work environment (including volume of episodes, distribution of workload, and staff perceptions of safety culture, workload, teamwork, and equity) on team quality scores obtained from the first regression. The second-stage model also controlled for workforce characteristics such as education and home health experience. Population Studied: Data come from a large urban home health care agency with 87 different teams, staffed by over 2,000 workers. The patient population averages 71 years of age, with 66% female, and is highly diverse; 40% white, 26% black, 24% Hispanic, 4% Asian and 6% other ethnicity. Clinical diagnoses cover a wide spectrum of conditions, with the most common being diabetes (13%), hypertension (8%) and congestive heart failure (5%). Principal Findings: Team-level factors related to fewer adverse events (listed with partial R-squares, followed by pvalues) were: higher volume (.01, p<.01); higher concentration of visits (.02,p<.05); fewer weekend admissions (.13, p<.05); more experienced clinicians (.04, p<.10); higher perceived teamwork (.02, p<.10) and equity (.01, p<.05); and lower perceived supervisor safety culture (.02, p<.01) and manageability of workload (.05, p<.10). Unrelated factors included perceptions of: top-down communication, access to resources, autonomy, and confidence in quality of care. Conclusions: The finding that higher volume and more experience have a protective effect is consistent with prior research. Further, as hypothesized, fewer weekend admissions, more concentrated work distribution, greater perceived equity and stronger teamwork were related to fewer adverse events. Contrary to expectations, greater dissatisfaction with both supervisor safety culture and the manageability of workload was related to fewer adverse events. However, these latter findings are similar to those from other studies demonstrating higher rates of reported adverse events where safety culture is emphasized. Implications for Policy, Delivery, or Practice: Key aspects of organizational climate that influence risk-adjusted adverse events are identified. Home care agencies should consider the importance of staff perceptions of equity and building teamwork into the quality improvement process. The association between better outcomes and less manageable workload raises questions about possible “burnout” among high performing teams or “complacency” among poorer performing teams. Primary Funding Source: AHRQ ●You Get What You Pay For:Using Input Prices To Validate Quality Of Care Measures Steven Pizer, Ph.D., Man Wang, MS, Catherine Comstock, MPH Presented By: Steven Pizer, Ph.D., Economist, Health Care Financing & Economics, Dept. of Veterans Affairs, 150 South Huntington Avevue, Mail Stop 152H, Boston, MA 02130; Tel: (617) 232-9500 x6061; Fax: (617) 278-4511; Email: pizer@bu.edu Research Objective: Economic theory predicts that improvement in quality of care requires commitment of resources in a production function. We use this prediction to validate seven quantitative measures of nursing home quality. Study Design: This is an analysis of secondary data using Veterans Health Administration (VA) data to examine seven quality measures developed for use in both VA and community nursing homes. Two measures rely primarily on data collected externally to the nursing home—either when VA patients receive hospital care or when they die—and the other five measures rely on patient assessment data, collected by VA nursing home staff on a semi-annual schedule. Population Studied: All residents of VA nursing homes between October 1997 and October 2000. Principal Findings: Measures based on data external to the nursing home were positively and significantly associated with input prices (nurses’ wages) in regression models controlling for output volume and case mix, and measures based on facility-reported data were not. These externally reported quality measures were rates of preventable hospitalization and mortality. Among the facility-reported quality measures, case mix effects supported some preference for behavior change and ADL change, although these effects could have been due to weak risk adjustment. Dehydration, pressure ulcer incidence, and urinary tract infection prevalence all failed to exhibit any relationships predicted by theory. Conclusions: Quality measures based on externally reported data appear to be less subject to measurement error than those relying on facility-reported resident assessments (like those chosen by the VA and by Medicare). Implications for Policy, Delivery, or Practice: If the relative strength of externally based measures found in this study is borne out with data from community nursing homes, then the current exclusive reliance on facility-reported quality indicators in the federal Nursing Home Quality Initiative should be reconsidered. Primary Funding Source: VA ●Effects on Quality of Care of a Workforce Development Demonstration Project: The Massachusetts Extended Care Career Ladder Initiative Jones Richard, ScD, Navjeet Singh, MS, William McMullen, MS, John N. Morris, Ph.D., Johan Uvin, Ph.D. Presented By: Jones Richard, Sc.D., Associate Director, Health and Social Policy Research, Hebrew SeniorLife Research and Training Institute, 1200 Centre Street, Boston, MA 02131; Tel: (617)363-8493; Fax: (617)363-8926; Email: jones@mail.hrca.harvard.edu Research Objective: To evaluate the impact of participation in the Massachusetts Extended Care Career Ladder Initiative (ECCLI), a workforce development demonstration project, on nursing home quality of care. Study Design: ECCLI was a demonstration project among Massachusetts nursing homes. Nursing homes, or consortia of nursing homes, applied to participate. An expert panel selected the final list of sites to receive ECCLI support for carrying out workforce development activities targeted at frontline caregivers. This evaluation of the ECCLI program compares the outcomes of nursing home residents living in the 69 facilities that participated in ECCLI to residents living in 189 facilities that did not participate in ECCLI. Comparison facilities were selected using propensity score methods. Population Studied: Older adults living in Massachusetts nursing homes between February 2000 and December 2003. Sixty-nine facilities (representing about 9,000 beds) took part in ECCLI. Of the remaining 465 facilities in Massachusetts, 189 were identified as comparison facilities (representing about 25,000 beds). Information about facilities was obtained from the CMS Provider of Services file and Minimum Data Set (MDS). Hospital-based facilities, government-owned facilities, facilities providing care exclusively to disabled children or head injury patients, and facilities having extremely high average casemix (based on resource utilization groups) were not represented among ECCLI-participating facilities. Among the remaining facilities, a logistic regression procedure was used to model participation. County, bed size, non-profit ownership, average severity of resident’s behavioral problems, average severity of resident’s functional limitations, and staffing (the number of RN FTEs) predicted participation. This model was used to identify up to 4 comparison facilities per participating facility within deciles of the predicted probability of participation. Principal Findings: We compared the rates of change of two clinical indicators of the quality of care across participating and non-participating facilities over 2.5 years: walking performance and behavioral disturbance. We used generalized estimating equation (GEE) procedures to account for the clustering of residents in the same facility. We also examined unadjusted CMS quality indicator scores for mobility decline and behavioral disturbance at the facility level using aggregated resident data, and accounted for clustering within facility over time using GEE methods. Resident-level models suggested no difference between ECCLI-participating and comparison facilities. Facility-level models suggested no difference for mobility decline, but a small difference that was statistically significant (P=.035) and implied an annual decrease in the proportion of residents experiencing worsening behavior in ECCLI-participating facilities relative to comparison facilities (-0.5%). Conclusions: Propensity score methods can be used to identify comparison nursing facilities for evaluation of nonrandomized experiments. A workforce development program may have small but measurable effects on measures of quality of care collected using nursing home MDS data. Implications for Policy, Delivery, or Practice: Policy makers may be reluctant to carry out demonstration projects as randomized trials, however, the confidence in causal inferences based on such designs is stronger than on methods using statistical modeling. To the extent that confidence that the selection of comparison facilities is appropriate, our results suggest that a workforce development program may yield resident quality of care benefits. Primary Funding Source: Commonwealth of Massachusetts ●Volunteer Nursing Homes Achieve Better Quality Improvement Charles Schade, M.D., MPH, Karen A. Hannah, MBA Presented By: Charles Schade, M.D., MPH, Medical Epidemiologist, Scientific Support, West Virginia Medical Institute, 3001 Chesterfield Place, Charleston, WV 25304; Tel: (304) 346-9864; Fax: (304) 346-9863; Email: cschade@wvmi.org Research Objective: To examine whether agreeing to participate in organized nursing home quality improvement efforts was associated with actual improvement in quality measures achieved during the first three years of the Nursing Home Quality Initiative (NHQI). Study Design: Cohort and time series. Population Studied: 114 Medicare and Medicaid certified nursing homes in West Virginia with 10 consecutive quarters of quality information for at least one of the ten original nursing home quality measures reported through the Centers for Medicare & Medicaid Services (CMS) NHQI beginning with the second quarter of CY 2002. We studied a subpopulation consisting of 20 nursing homes volunteering to participate in intensive quality improvement work for four selected measures: prevention of functional decline, pressure ulcer prevalence, and post acute and chronic pain. Nursing homes received training in patient care procedures believed to improve performance in the selected measures, and intensive group members received individualized attention and feedback. Volunteer nursing homes had significantly worse baseline performance in percent of patients with ADL decline at baseline than the entire state (27% vs. 15%). There were no significant differences at baseline in other measures. Principal Findings: Median nursing home performance in West Virginia improved on both pain measures, mirroring national trends. There was no significant difference between the intensive group and others for these measures. Roughly the same proportion of volunteer group nursing homes showed significant improvement as of the entire population. Volunteer group nursing homes reduced the proportion of patients with ADL decline from 26% to 17%, whereas there was no change in the rest of the state’s facilities. Six of eight nursing homes with statistically significant (p<0.05, chi square for trend) negative trends in ADL decline over all 9 quarters were in the intensive group. There were no significant overall changes in either group for pressure ulcer prevalence. Statewide, ten facilities had significant worsening in pressure ulcer performance; none was in the volunteer group. Conclusions: Volunteer nursing home participants performed as well or better than peers who did not volunteer for quality improvement work in this uncontrolled study. Implications for Policy, Delivery, or Practice: These early results suggest organized efforts to improve nursing home quality may be effective. Additional research is needed to determine whether characteristics of nursing homes that led them to volunteer were also associated with improved performance, and the extent to which interventions in the intensive group helped drive the improvement. Primary Funding Source: CMS ●National Estimates in Use of Over-the-Counter Medications in Long-Term Care Linda Simoni-Wastila, BSPharm, Ph.D., Bruce Stuart, Ph.D., Thomas Shaffer, MHS Presented By: Linda Simoni-Wastila, BSPharm, Ph.D., Associate Professor, Pharmaceutical Health Services Research, University of Maryland Baltimore School of Pharmacy, 515 West Lombard Street, Room 162, Baltimore, MD 21201; Tel: (410) 706-4352; Fax: (410) 706-1488; Email: lsimoniw@rx.umaryland.edu Research Objective: Over-the-counter (OTC) medications are often a safe and economical therapeutic alternative for treating many conditions that are treated with prescription drugs that are both more expensive and more likely to cause adverse reactions and other problematic consequences. Little is known, however, about the prevalence of and spending on OTC medication use in nursing homes. The purpose of this study is twofold: 1) to provide national estimates of the use of OTC medications in long-term care facilities, and 2) examine beneficiary characteristics associated with OTC drug use and spending. Study Design: This study is based on the 2001 Medicare Current Beneficiary Study (MCBS). Drug use information is derived from a unique MCBS file (the Institutional Drug Administration file) prepared by the authors for CMS. Our outcome variables are mean monthly OTC drug mentions and OTC drug use mentions as a proportion of all drug mentions. We examine aggregate drug use, as well as use and spending by select therapeutic classes. Ordinary least squares regression is used to model our dependent variables, controlling for gender, age, marital status, educational attainment, geographic region, poverty status, health status, and drug insurance coverage. We adjust for severity-of-illness using CMS-HCC risk adjuster. Population Studied: Nursing home residents (n=789) from a nationally-representative sample of the population of Medicare beneficiaries in 2001. Principal Findings: Examination of OTC utilization patterns demonstrates that 95% of nursing home residents used at least one OTC drug in the study year. OTC use as a proportion of all medication use was high, accounting for 36% of all medication claims. On average, individuals used 3.1 OTC products per month – this varied by type of drug coverage, with Medicaid recipients using 3.2 OTC products, and those with private drug coverage using 2.8 different OTC products. The most frequently used OTC drug classes include analgesics, gastroprotective agents, and vitamin preparations. Multivariate findings revealed that females are more likely to receive OTC medications than males, those living below the poverty level use more OTCs than more affluent individuals, and utilization of OTC medications increases with as individuals become more impaired in their daily activities. Conclusions: OTC use is omnipresent among nursing home residents. Although utilization of OTC medications is not affected by type of drug coverage, gender differences, income differences, and level of disability are statistically significant predictors of OTC use. Implications for Policy, Delivery, or Practice: The new Medicare Part D prescription benefit does not reimburse for OTC medications. This lack of coverage may be particularly problematic for frail beneficiaries residing in nursing homes in whom OTC medication use is a significant component of their therapeutic regimens, especially in several therapeutic categories, such as analgesics and gastroprotective agents, where more expensive prescription products may be substituted. Primary Funding Source: No Funding Source ●Searching for and Selecting an Assisted Living Facility Kristen Sonon, M.H.A., Nicholas Castle, Ph.D. Presented By: Kristen Sonon, M.H.A., Health Policy and Administration, University of Pittsburgh, Pittsburgh, PA 15261; Email: kes31@Pitt.edu Research Objective: Recent research has been performed on the topic of choice in long-term care facilities. To date, most of this research has come from nursing homes. Researchers have not yet addressed the topic of choice in assisted living facilities. In this research, we examine factors associated with the search, selection, and satisfaction of residents in assisted living. Study Design: Face-to-face interviews were conducted with residents residing in assisted living facilities. These interviews were used to determine the principal decision maker, the process of searching for a facility, the factors crucial to facility selection, the time frame from the relocation decision to relocation, and satisfaction with selection. Population Studied: The data was collected from 300 residents of three assisted living facilities surrounding Pittsburgh, Pennsylvania. Principal Findings: We find that most elders are influential in the choice of facility. However, the choices made were seldom based on the quality of the facility. On the one hand search and selection processes were involved. However, on the other hand, in almost all cases, prior knowledge of the chosen facility was limited, and revolved mainly around location. Conclusions: The number of assisted living facilities is around 12,000 nationwide, and they generate about $15 billion per year. Moreover, most facilities are less than 10 years old, reflecting their fast rate of growth. The cost of assisted living care is also high for consumers. However, we show a great deal of uncertainty in the market when it comes to choosing these facilities. Policy implications include the potential need for a report card; delivery implications include more family/resident education initiatives; and, facility practice implications include the potential to improve satisfaction with care. Implications for Policy, Delivery, or Practice: The Assisted Living Federation of America projects that by 2020, as many as 13 million elders will be living in assisted living. The cost of assisted living care is also high. However, we show a great deal of uncertainty in the market when it comes to choosing these facilities. Primary Funding Source: No Funding Source ●What Drives the Selection of Long-Term Care Services: Key Findings of a Qualitative Study in Arkansas Kate Stewart, M.D., MPH, Holly Felix, MPA, Dana M. Perry, MA, Nancy Dockter, Jinger Morgan, Al McCullough, MA Presented By: Kate Stewart, M.D., MPH, Associate Professor, Health Policy and Management, University of Arkansas for Medical Sciences College of Public Health, 4301 West Markham, Slot 820, Little Rock, AR 72205; Tel: (501)526-6625; Fax: (501)526-6620; Email: stewartmaryk@uams.edu Research Objective: This study was undertaken to identify issues and factors that were important to individuals when they were making decisions about which type of long term care services (home and community-based or institutional care) they would utilize. This presentation will report on the qualitative findings of the study. Study Design: The study was comprised of two components. The first component involved analysis of existing quantitative data to profile the long-term care population in Arkansas. The second component involved qualitative data collection and analysis to identify key decision factors. Data was collected through semi-structured interviews with 59 key informants and 4 focus groups of health and social service providers. Population Studied: The study focused on adult users of Medicaid supported long-term care services who had recently made a decision about use of a long-term care service. Specifically, the study targeted the elderly (65 years and older), adults with physical disabilities (18 years and older), and adults with developmental disabilities (21 years and older). Attempts were made to balance this study population based on location (urban and rural), race, gender, and service choice (institutional and home/community-based care). Data collected from actual consumers of services were augmented with data collected from family members/guardians of consumers, health care providers, and social service providers who had been involved in or were knowledgeable of the decision-making process. Principal Findings: Among the key findings to be reported in the presentation are: 1. Access to information played a role in making decisions about long-term care, with many study participants reporting relying on word of mouth and multiple sources of information because of a lack of a central source of information on all long-term care options, 2. The application process and waiting period for home- and community-based (H/CB) services more often were burdensome and long in contrast to that for institutional care, which was relatively simple and short-term, and 3. Workforce and environmental issues often affected decisions about services. Perceptions of quality of care in institutional settings , whether positive or negative, were often mentioned as a determinant in decisions to use various services. A few users of H/CB services mentioned problems finding reliable, dependable home care workers. Conclusions: This study provides insights into the decisionmaking process about long-term care services. Although it is a qualitative study that does not provide generalizable results, it does provide the context under which individuals make decisions about long-tem care services and lays the ground work for further investigations using methods which could produce generalizable results. Implications for Policy, Delivery, or Practice: This study provides implications for policy actions by long-term care services administrators and state policy makers. Specifically, the study authors made multiple recommendations around the three theme areas of: 1. leveling the playing field between institutional and home/community-based options, 2. providing information and counseling, and 3. accessing quality services. Primary Funding Source: Private Fnd and CMS ●Private Finance of Long Term Care: Market Penetration and Potential Eileen Tell, MPH, John A. Cutler, JD Presented By: Eileen Tell, MPH, Senior Vice President, Long Term Care Group Inc., 5 Commonwealth Road, Natick, MA 01760; Tel: (508)651-8800; Fax: (508)651-8804; Email: etell@ltcg.com Research Objective: To compare the current market penetration of private long term care insurance with the market potential, using alternative methodologies to define both market penetration and market potential. Study Design: Analyze existing data sources on policies in force and alternative criteria to use in defining the eligible population for long term care insurance in order to derive a viable measure of market penetration. For market potential, we rely on literature review on affordability as the primary means of analyzing market potential. Population Studied: Focus is on the 50+ population which is the primary target market for private finance of long term care. Principal Findings: Market penetration using policies in force, rather than policies sold, is a more valid estimate of market penetration although this index has not been previously used. Market penetration varies greatly by state and is sensitive to varying definitions for the target population. Market penetration is sensitive to a variety of demographic, policy and provider variables. Market potential is sensitive to key assumptions made about and definitions of affordability. Conclusions: Further analysis of factors driving market penetration should be explored to identify factors that can be influenced to create a more favorable environment for expanded private finance. Examples might include regulatory reform, tax incentives, agent and consumer education and the like. Implications for Policy, Delivery, or Practice: The market penetration for private finance for long term care can be expanded through a variety of initiatives addressing consumer awareness, regulatory reform and other factors. Affordability of private finance for long term care is more subjective and therefore subject to influence than previously believed. Expanding the market for private long term care insurance can help reduce the burden on Medicaid budgets and improve freedom of choice and independence for those who need long term care. Primary Funding Source: No Funding Source ●Improving Nursing Employee Satisfaction in Long-Term Care Facilities: Let Nurses do the Nursing Denise Tyler, MA, Victoria A. Parker, DBA, Ryann L. Engle, MPH, Gary H. Brandeis, M.D., Elaine C. Hickey, RN, MS, Dan R. Berlowitz, M.D., MPH Presented By: Denise Tyler, MA, Ethnographic Interviewer, Health Services, Boston University School of Public Health, 715 Albany Street, Boston, MA 02118; Tel: (781) 687-2000 x6696; Fax: (781) 687-3106; Email: datyler@bu.edu Research Objective: This study examined the causes of job satisfaction and motivation among nursing employees in long-term care (LTC) facilities in relation to the design of nursing care tasks. Study Design: Quantitative and qualitative data were gathered from LTC employees. Job design characteristics, employee satisfaction, and motivation were measured with a modified version of the Job Diagnostic Survey (JDS). To further illuminate details of task design, interviews and observations were conducted. Population Studied: Employees of 20 LTC facilities in eastern Massachusetts. Principal Findings: Certified nursing assistants (CNAs) were found to have significantly higher levels of satisfaction when compared to nurses and nurses were found to have significantly higher levels of motivation. An examination of the causes of satisfaction among LTC employees revealed that although CNA satisfaction was influenced by several factors (task identity, autonomy, intrinsic feedback, and job tenure), satisfaction among nurses was only influenced by intrinsic feedback, or the amount of feedback the employee perceives is provided in the course of performing the job. Among employees in LTC facilities this type of feedback would most likely result from interactions with patients. Most nurses reported dissatisfaction with the amount of time available to interact with patients, while most CNAs reported such interactions as the most satisfying aspect of their jobs. Conclusions: It may be possible to improve job satisfaction among nurses in LTC facilities by increasing the amount of time they have to interact with their patients. Implications for Policy, Delivery, or Practice: This could greatly improve facilities’ ability to retain nurses. Primary Funding Source: AHRQ ●Government Pressure, Structural Issues and Organizational Culture: An Analysis of Their Impact on the Work Environment of Long-Term Care Facilities Denise Tyler, MA, Victoria A. Parker, DBA, Ryann L. Engle, MPH Presented By: Denise Tyler, MA, Ethnographic Interviewer, Health Services, Boston University School of Public Health, 715 Albany Street, Boston, MA 02118; Tel: (781) 687-2000 x6696; Fax: (781) 687-3106; Email: datyler@bu.edu Research Objective: The purpose of the study from which these data were drawn was to understand the causes and consequences of variation among long-term care (LTC) facilities in the design of nursing care jobs. Study Design: Surveys, interviews, and structured observations were utilized in 20 long-term care facilities in eastern Massachusetts. For this analysis the constant comparative method of qualitative data analysis was employed using N’Vivo software. Population Studied: One hundred forty-four LTC employees representing all staffing levels, from nursing directors to frontline certified nursing assistants (CNAs), were interviewed and structured observations of thirty-seven frontline nurses and CNAs were conducted. Principal Findings: Three distinct domains were shown to influence working conditions in long-term care facilities. Governmental pressures were found to be similar across facilities, affecting most in similar ways. Structural issues, such as staffing levels, compensation, and worker to resident ratios, were also surprisingly similar across facilities. It was in the cultural realm of relationships, teamwork, and worker interactions where large differences across facilities were found. Conclusions: Improving working conditions for long-term care employees may not necessarily involve making significant changes to the structural realm, and due to the nature of the care provided and the governmental regulations which control it, this may not be possible. However, working conditions may be greatly impacted by improving the cultural aspects of the work through greater respect, understanding, and teamwork. Implications for Policy, Delivery, or Practice: Improving the organizational culture of LTC facilities could greatly improve facilities’ ability to retain nursing employees. Primary Funding Source: AHRQ ●Beyond Courtesy: Top Satisfaction Scores as a Guide to Service Improvement in Long Term Care Robert Wolosin, Ph.D., Laura Vercler, M.S. Presented By: Robert Wolosin, Ph.D., Research Product Manager, Research & Development, Press Ganey, 404 Columbia Place, South Bend, IN 46601; Tel: (800)232-8032; Fax: (574)232-3485; Email: rwolosin@pressganey.com Research Objective: Many elderly persons make a long-term care (LTC) facility their home. The number of such persons will increase in the future, multiplying the need for LTC facilities and workers. Improving the quality of life for LTC residents will remain a high priority, and front-line workers such as nurses and aides will play a key role. The objectives of this study were: (1) To discover service issues pertaining to LTC front-line workers that are most in need of improvement, across a spectrum of US LTC facilities; (2) To prioritize these issues by their importance for overall service improvement as measured by resident satisfaction. Study Design: A retrospective database analysis of LTC resident satisfaction surveys was undertaken. The analysis used data from a national patient satisfaction measurement/management firm that mails psychometricallyvalidated surveys to residents and/or resident families of client LTC facilities and collects them by return mail. Within each survey, respondents make ratings of care on a balanced 5-point Likert-type scale (1=very poor, 5=very good). All survey items pertaining to front-line workers (nurses, aides, maintenance staff, dining staff, transportation personnel) were selected for further investigation. For each of these items, the overall mean score that reflected the 99th percentile of the national database for each survey type was calculated. Because these scores represent the best the LTC industry currently offers, noting their average values yields data on industry-wide service quality: The lower the mean score, the more improvement is possible within the LTC industry. Population Studied: Surveys were sent to random samples of residents/family members in 96 Independent Living facilities (n=16,105,), 96 Assisted Living facilities (n=4,387), and 484 Nursing Homes (n=27,336) from November 2003-November 2004. Average response rates were approximately 65% (Independent Living), 50% (Assisted Living) and 25% (Nursing Home). Principal Findings: Average 99th percentile scores on items measuring courtesy, friendliness, and respect were typically above 95.3; however, we identified items that measure staff responsiveness, information provided, and perceived technical delivery of care that were at or below an average score 95.5 for the 99th percentile, indicating that there is room for service improvement, even among the industry’s best. When the correlation of each of the latter items with overall resident satisfaction (an index of item importance) is computed and arranged from most to least correlated, the resulting rank order prioritizes industry-level changes that would improve service in LTC facilities. Conclusions: Top performers in the LTC industry show high proficiency in delivering courteous, friendly, respectful care to their residents, but are less adept at responding to residents’ personal issues. Implications for Policy, Delivery, or Practice: Front-line staff’s responses to residents’ complaints and requests, their provision of information to residents, and their attention to resident perception’s of technical ability show the greatest potential for improving service quality in LTC facilities. Primary Funding Source: No Funding Source ●Minimum Nurse Staffing Ratios for Nursing Homes Ning Zhang, M.D., Ph.D., Lynn Unruh, Ph.D., RN, Thomas Wan, Ph.D., MS Presented By: Ning Zhang, M.D., Ph.D., Assistant Professor, Department of Health Administration/College of Health and Public Affairs, University of Central Florida, 3280 Progress Drive, Orlando, FL 32826; Tel: (407)823-3344; Fax: (407)8234895; Email: nizhang@mail.ucf.edu Research Objective: To explore minimum nurse staffing ratios for nursing homes for different quality levels. Study Design: Cross-sectional analyses using multivariate logistic regression and simulation techniques were used to determine the minimum nurse staffing for multiple quality levels. Data were from the On-Line Survey Certification and Reporting System. Quality was measured through an index combining three incidence rates: the presence of indwelling catheters, pressure sores, and physical restraints. Staffing measures included registered nurses (RNs), licensed practical nurses (LPNs), licensed nurses (RNs+LPNs), nurse aides (NAs) and total nurse staffing (including administrators).Using 2002 data, the relationship between nurse staffing and quality was first evaluated by examining the fit of linear and non-linear regressions of these variables. Given a better fit with the non-linear model, minimum staffing levels were assessed using simulations of a non-linear production function to establish the minimum efficient points at which staffing will provide 50, 75 and 90 percent levels of quality. Reliability analysis of the minimum staffing thresholds was completed with 2003 data. Population Studied: All nursing home facilities federally certified for Medicare and Medicaid and their residents in 2002 and 2003. After cleaning, 14,113 nursing homes remained in the study, which represented 85.6% of original number of nursing homes. Principal Findings: Non-linear logistic regressions were a better fit. Minimum levels of registered nurse hours per resident day were 0.31, 1.83, and 3.3 at 50, 75, and 90 percent levels of quality respectively. Licensed nurse and total nursing staff ratios were likewise established. Minimums were similar in 2002 and 2003. The minimum nursing hours associated with a 75 percent level of quality in this study are much higher than the actual average RN hours, or than those suggested by experts. Conclusions: Actual staffing ratios are much too low to support a 75 percent quality level, and that even expert panels are underestimating the staff needed to produce higher quality care. In addition, we estimate the added expense in going from the 50 percent quality level to 75 percent as being: $23.51 per resident per day for RNs, and $71.07 per resident per day for total nursing staff. In an average facility with 95 residents, that would translate to increases in daily expenses of $2,233 for added RNs or $6,751 for added total nursing staff. Implications for Policy, Delivery, or Practice: Our study is the first investigation of minimum nurse staffing levels that are efficient and promote quality. It provides evidence-based information for federal and state governments to adjust their surveillance and reimbursement policy as well as for nursing home administrators to guide their cost containment, personnel management and quality improvement. Primary Funding Source: NIA ●Do Trends in the Reporting of Nursing Home Compare Quality Measures Differ by Nursing Home Characteristics? Jacqueline Zinn, Ph.D., William Spector, Ph.D., Lillian Hsieh, MHS, Dana B. Mukamel, Ph.D. Presented By: Jacqueline Zinn, Ph.D., Professor, Risk, Insurance and Healthcare Management, Temple University, 413 Ritter Annex, Philadelphia, PA 19122; Tel: (215) 204-1684; Fax: (215) 204-4712; Email: Jacqueline.Zinn@temple.edu Research Objective: The Center for Medicare and Medicaid Services (CMS)began publicly reporting scores on quality measures as part of its quality initiative for nursing homes, with the expectation that the information will be useful to consumers when choosing a nursing home and for facilities in their quality improvement efforts. This study examines the relationship between scores on the first set of ten quality measures published by CMS on the Nursing Home Compare web site and five nursing home structural characteristics: ownership, chain affiliation, size, occupancy and hospitalbased vs. free-standing status. Study Design: Using robust linear regressions we examined quality measure scores on first publication and their change over the first five reporting periods, in relation to facility characteristics. Population Studied: The analysis was at the facility level. 14,827 nursing homes nationwide with data on the Nursing Home Compare web site are included in the analysis. Principal Findings: There were significant baseline differences associated with these facility characteristics. In addition, there are clear time trends for five of the ten measures, and all are towards improved outcomes. Pain, physical restraints and delirium exhibit a clear downword trend, with differences between the first reporting period and the fifth ranging from 12.7% to 46%. However, there were only minimal differences in trends associated with facility characteristics. The variation by facility type was larger for the short stay quality measures than for the long stay measures. Furthermore, any differences associated with facility characteristics observed initially narrows over time. Conclusions: Our results suggest that the relative position of facilities on these measures did not change much within this time period. However, the variation by facility type was larger for the short-term quality measures than for the long-term measures. Implications for Policy, Delivery, or Practice: Results suggest that the short-term measures may be more useful to consumers by enabling them to better differentiate performance across facilities. They also suggest that, at least in the short run, publication of these measures did not lead to large changes in them. The finding that several of the quality measures have improved over time suggests that report cards may have an important role to play in promoting high quality nursing home care. However, the impact was limited to only some of the measures. Further research is needed to understand why nursing homes have not been responsive on some measures, and whether other policies, such as reforming the state survey process, are needed in tandem with public quality reporting. Primary Funding Source: NIA