Patient Safety Events IoM estimated that between 44,000 and
advertisement

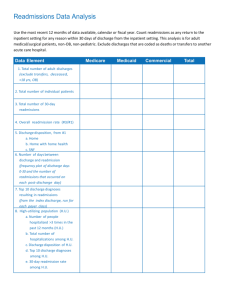
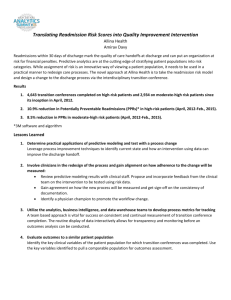
Patient Safety Events IoM estimated that between 44,000 and Adverse Patient Safety Events: Costs of Readmissions and Patient Outcomes Following Discharge 98,000 people die in hospitals each year as a result of medical errors Medical errors is the eighth leading cause of Didem M. Bernard, Ph.D. William E. Encinosa, Ph.D. death in the U.S. IoM recommended at least a 50% reduction in medical errors over 5 years Background Research Questions Medical injuries during hospitalizations lead to Do adverse patient safety events during hospitalizations have an effect on patient outcomes following discharge? Whether adverse patient safety events have a Are there longlong-term costs associated with potentially preventable adverse medical events? excess length of stay, charges and mortality (Zhan and Miller, 2003) significant impact on patient outcomes and costs following discharge is less clear Patient Safety Indicators We use the AHRQ Patient Safety Indicators (PSI) developed by the UCSF - Stanford Evidence - Based Practice Center (EPC) and UC - D avis (2003). EPC selected 14 indicators among 63 complication indicators using – Indicator validity results from the literature – Empirical analyses of the precision and reliability of the candidate PSIs – Review of potential indicators by 11 clinical panels Patient Safety Indicators 1 Anesthesia Complications * 2 Accidental Puncture or Laceration During Procedure 3 Foreign Body Left In During Procedure* 4 Hemorrhage or Hematoma 5 Wound Dehiscence 6 Infection Due to Medical Care 7 Pulmonary Embolism and Deep Vein Thrombosis * Labeled as medical errors 1 Patient Safety Indicators (cont.) 8 Iatrogenic Pneumothorax* 9 Acute Respiratory Failure 10 Sepsis 11 Physiologic and Metabolic Derangements 12 Transfusion Reaction 13 Hip Fracture* 14 Decubitus Ulcer* Data 2002 California Hospital Discharge Data AHRQ Healthcare Cost and Utilization Project (HCUP) State Inpatient Database (SID) Hospital Inpatient Cost to Charge Ratios Area Wage Index (CMS) Number of Hospitals: 349 * Labeled as medical errors Analytic Sample and Methods Major Surgery Discharges (17<age<65) From February 1, 2002 to November 30, 2002 Index admission: A major surgery admission with no hospitalizations in a 30 day window prior to the admission date (N=602,361) Patient Outcomes Probability of readmissions Probability of death during index admission Probability of death during any readmission within 30 days of initial discharge Readmission: Any hospitalization within 30 days of initial discharge Costs of Adverse Patient Safety Events Index admission costs Costs of readmissions Total costs for index admissions and readmissions within 30 days following discharge Basic Model: Hospital Costs yi = β 0 + βPSIPSIi + β xXi + εi i=person y= cost of hospitalization* PSI= (0,1) indicator equals 1 if patient has at least one adverse patient safety event x=control variables * Index admission, readmission or total hospital costs 2 Basic Model: Patient Outcomes yi = β 0 + βPSIPSIi + β xXi + εi i=person y=(0,1) indicator equals 1 if patient is readmitted within 30 days of discharge* PSI= (0,1) indicator equals 1 if patient has at least one adverse patient safety event x=control variables Control Variables Patient: age, sex, race/ethnicity, transfer admission, emergency admission, 30 chronic conditions, MDC, zipcode level median household income Hospital: teaching status, ownership type, bedsize Market: Health Service Area dummies * y=(0,1) indicator equals 1if patient dies during hospitalization hospitalization Patient Outcomes Average Costs PSI=0 PSI=1 Live discharge Death during index admission 84.55% 63.03% 0.86% 5.97% PSI=0 $12,579 $17,927 $15,198 Readmission Death during readmission 14.14% 28.32% PSI=1 $31,096 $33,445 $41,510 0.46% 2.68% Difference 147% N 583,836 18,889 Index Hospitalization Readmission 87% 173% Simulation Results: Outcomes Estimation - link Costs: GLM (Generalized Liner Method) log with Gamma distribution (Manning and Mullahy, 2001) Patient Outcomes: Logit regressions Simulation results: A : Predicted costs/outcomes with PSI=1 B : Predicted costs/outcomes with PSI=0 (A – B) : Predicted costs/outcomes due to adverse patient safety events Total Costs Death during index Death during hospitalization readmission Death within 30 days of discharge PSI=0 0.92% 3.4% 1.4% PSI=1 1.96% 5.2% 2.8% % Difference 1.04%* 1.8%* 1.4%* * Significantly different from zero at the 99% level 3 Simulation Results: Outcomes (cont.) Simulation Results: Costs Probability of readmission Index Hospitalization Readmission Total Costs PSI=0 15.1% PSI=0 $12,801 $18,264 $15,618 PSI=1 20.1% PSI=1 PSI COST $21,190 $8,388* (232) $26,198 $7,933* (529) $26,607 $10,989* (284) % Difference 65.5% 43.4% 70.4% Difference 5.0%* * Significantly different from zero at the 99% level * Significantly different from zero at the 99% level Summary Policy Implications Excess costs and adverse outcomes of adverse patient safety events are not limited to the initial hospitalization Adverse patient safety events during hospitalizations lead to – Higher probability of readmissions – Higher probability of inin-hospital death following discharge – Higher inpatient costs following discharge A reduction in adverse patient safety events will not only improve quality of care but also reduce longlong-term health care costs 4