Hospital Financial Distress and Patient Outcome: A Panel Study
advertisement

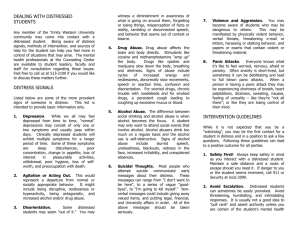
Hospital Financial Distress and Patient Outcome: A Panel Study Rationale for the Study z Mei Zhao, MHA z Virginia Commonwealth University Gloria J. Bazzoli, Ph.D. z Virginia Commonwealth University Henry J. Carretta, MPH Virginia Commonwealth University About 1/3 US hospitals have negative total margins Medical mistakes result in the deaths of 44,000 to 98,000 hospitalized Americans a year (IOM, 1999) Some Patient safety indicators are deteriorating – Respiratory failure ↑ 31% – Infection due to medical care ↑ 14% – Decubitus ulcer ↑ 19% – Septicemia ↑ 41% (Romano et al., 2003) Agency for Healthcare Research and Quality,Grant # R01 HS13094 Research Questions z What differences exist in the quality of care and patient safety between financially distressed and non-distressed hospitals? z What differences exist in the structural and organizational characteristics between these two groups? Method z z Key Variables z z Financial Distress – Average negative operating margin 93-95 Patient Outcome – IQIs (5): AMI, CHF, Stroke, GI hemorrhage, and Pneumonia – PSIs (9): Complications of anesthesia, Death in low mortality DRGs, Decubitus ulcer, Failure to rescue, infections due to medical care, post-op hemorrhage, post-op PE, sepsis, and accidental puncture Agency for Healthcare Research and Quality, Grant number R01 HS13094 z Design – A panel study design is applied to data from 1995-2000 Sampling – Nonfederal short term general hosps from 11 states (AZ, CA, CO, FL, IA, MD, MA, NJ, NY,WA, and WI), about 1,300 per year Data collection – AHA, MCR, HCUP (SID) 1995-2000 Analytic Strategies z Descriptive statistics and cross-tabulations – Adjusted Least Square Means (ALSM) – Patient age, gender, acuity, and case-mix 1 Results: Comparison of Hospital Structure and Organizational Characteristics Distressed Bed Size Non-distressed Mean SD Mean SD t-statistics Results z No significant difference between distressed and nondistressed hospitals 201.7 212.1 184.78 148.2 4.93 *** Publicly Owned (%) 0.29 0.45 0.10 0.30 7.40 *** Major Teaching (%) 0.11 0.31 0.03 0.18 7.71 *** Medicaid Payer (%) 0.22 0.19 0.16 0.15 4.69 *** FTEs/1000 Case-Mix APDs 9.44 4.36 9.54 3.26 -. 94 RN FTEs/1000 Case-Mix APDs 2.24 1.08 2.43 0.92 -3.22 ** z LPN FTEs/1000 Case-Mix APDs 0.41 0.4 0.39 0.37 -. 34 z – IQIs – PSIs z z z z AMI Complications of anesthesia infections due to medical care post-op PE sepsis accidental puncture Note: * Significant at the .05 level; ** significant at the .01 level; *** significant at the .001 level. Results Results Comparison between Distressed and Non-distressed Hosps for IQIs: 1995-2000 Comparison between Distressed and Non-distressed Hosps for IQIs: 1995-2000 0.1 0.08 CHF-nondis CHF-distress Pneumonia-nondis Pneumonia-distress 0.06 0.04 IQI R ate (A LS M) IQI Rates (Adjusted Least Square Means) 0.12 0.02 0.16 0.14 0.12 0.1 0.08 0.06 0.04 0.02 0 0 1995 1996 1997 1998 1999 Stroke-nondis Stroke-distress GI hemo-nondis GI hemo-distress 1995 2000 1996 1997 Results 1999 2000 Results PSI Comparison:1995-2000 PSI Comparison:1995-2000 0.18 0.025 0.16 Decubitus-nondis 0.02 0.015 Decubitus-distress 0.01 0.005 0 1995 1996 1997 1998 1999 2000 Post hemorrhagenondis Post hemorrhagedistress Ye a r 0.14 P S I Rate (ALS M ) P S I R a te (A L S M ) 1998 Y ear Year 0.12 0.1 Failure to rescue-nondis 0.08 Failure to rescue-distress 0.06 0.04 0.02 0 1995 1996 1997 1998 1999 2000 Y ear Agency for Healthcare Research and Quality, Grant number R01 HS13094 2 Summary z Distressed hospitals are more likely to be – z z z Publicly owned, major teaching, and larger proportion Medicaid patients Distressed hospitals have smaller RN ratio Better financial performance, better patient outcomes: CHF, Pneumonia, and Decubitus The gap narrowed for the mortality indicators beginning in 1998: Stroke and Pneumonia Significance to Policy and Future Research z z z z Agency for Healthcare Research and Quality, Grant number R01 HS13094 Cost control policies may have had unintended negative effects on patient outcomes Hospitals experiencing financial distress may have fewer resources to invest in the quality of their services BBA may have had an immediate adverse effect on patient outcomes for both distressed and nondistressed hospitals Examine how financial condition influences process and resource investments related to quality of care 3