Self-reported Effects of Prescription Drug Cost-Sharing: Decreased Adherence and Increased Financial Burden

Self-reported Effects of Prescription Drug
Cost-Sharing: Decreased Adherence and
Increased Financial Burden
Mary Reed, MPH 1
Vicki Fung 1
Richard Brand, PhD 2
Bruce Fireman, MA 1
Joseph P. Newhouse, PhD 3
Joseph V. Selby, MD, MPH 1
John Hsu, MD, MBA, MSCE 1
1 Kaiser Permanente - Division of Research
2 University of California, San Francisco
3 Harvard University
Academy Health Annual Research Meeting June 7, 2004
Introduction
►
Drug expenditures are increasing each year in the US
►
Patients are paying for an increasing share for their prescription drugs: cost-sharing
►
Cost-sharing effects may be influenced by patient knowledge
►
Limited information about:
– Patient knowledge about their prescription drug cost-sharing
– How patients behave when faced with this cost-sharing
Purpose
►
To examine patient knowledge of their prescription drug cost-sharing level:
– Any prescription drug cost-sharing?
– Structure of prescription drug cost-sharing (multi-tier copayments and benefit caps)?
– Amount of drug cost-sharing (copayment amounts and benefit cap amounts)?
►
To examine self-reported patient behavioral responses to prescription drug cost-sharing:
– Do patients report taking less than the prescribed amount of a drug (adherence)?
– Do patients report having to struggle to pay for their prescription drugs (burden)?
Methods
– Design/Population/Sample
►
Cross-sectional Design: Telephone interviews in 2003
►
Population:
– Active members in a large, prepaid integrated delivery system (IDS)
– Age 18 years or more
– English-speaking
– Commercial or Medicare insurance
►
Stratified random sample:
– A: General Population (30%)
– B: Members over age 65 (70%)
►
Population is a subset of a larger study on clinical and economic effects of cost-sharing
Questionnaire Measures
- Adherence
►
“Because of the amount you had to pay, have you”:
– “taken less than the prescribed amount to make it last longer”
– “not filled a prescription for a new medication”
– “stopped refilling a prescription”
Questionnaire Measures
- Burden
►
“Because of the amount you had to pay, have you”:
– “switched to a cheaper medication (e.g. generic)”
– “gotten free medication samples from a doctor”
– “gone to a non-Kaiser pharmacy instead”
– “gotten help paying for medications through an
[assistance] program”
– “borrowed $ to pay for medications”
– “gone without some necessity such as food, rent, heat, or other basics”
– “bought a prescription medication in another country”
– “bought a medication from an internet pharmacy”
Methods
– Analysis
►
Models: Multivariate logistic regression
►
Predictor Measure:
– Perceived/Actual Drug cost-sharing: Generic Copayment ($),
Brand-Generic Copayment ($), Any Benefit Cap
►
Outcome Measures
►
– Decreased Adherence
– Financial Burden
Covariates
– Socio-demographic: age, gender, race/ethnicity, marital status, household income, educational level
– Clinical: self-reported health status, self-reported number of prescription drugs in previous 12 months, comorbidity
(DxCG)
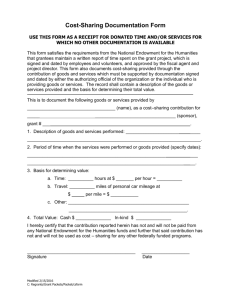
Figure 1. Study Design: Interview Participation n=932 (72%)
KPNC Adult Population: Commercial and Medicare Population
Members Randomly Selected and Contacted for Interview n=1700 [2 Strata]
Overall Population (30%) n=510
Ineligible* n=147 Refused n=109
(30%)
Age 65+ (70%) n=1190
Ineligible* n=261 Refused n=251
(27%)
Interviewed n=254
(70%)
Interviewed n=678
(73%)
*Ineligible = deceased, incapable of phone interview (e.g. hearing difficulties, dementia), non-English speaker, unable to be contacted
Table 1. Participant Characteristics
Characteristic
Age 65+
Female Gender
Non-white Race
Education: less than College Graduate
Married
Household Income: < $35,000
Self Reported Health: Excellent or Very Good
Total
(n=932)
%
77.7
Sample A:
Overall Pop.
(n=254)
%
14.2
55.8
26.2
67.2
63.9
50.5
35.5
59.0
71.6
Sample B:
Age 65+
(n=678)
%
100.0
58.8
22.7
69.7
61.6
43.2
44.4
18.8
53.7
51.3
41.6
Persons with Any Prescription Meds w/in 12 mos. 90.9
Persons with Any ED Visits within 12 mos. 23.8
82.1
21.7
93.5
24.7
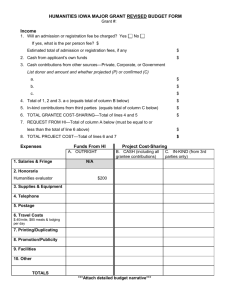
Table 2. Knowledge of Drug Cost-Sharing
Cost Sharing Type Any Cost-Sharing
Self-
Report
%
KP
Actual
%
Correctly
Reported
%
Amount of Cost Sharing
Underestimate
Exactly
Correct
Overestimate
% % %
92.9
82.3
84.9
8.0
70.0
22.0
Generic Copay
Brand Name Tiered Copay 61.2
74.4
73.8
33.3
50.5
16.2
Benefit Cap 31.2
33.4
85.6
5.0
59.4
35.6
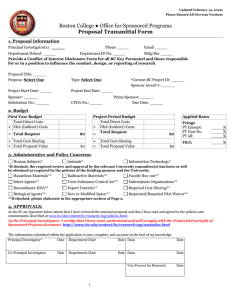
Figure 2. Self-Reported Behavioral Response to Cost-sharing:
Decreased Adherence
Any change in Adherence (N=80)
Taking less than prescribed (N=46) 6.2
10.8
Not filling a new prescription (N=47) 6.4
Not re-filling a prescription (N=45) 6.1
0 2 4 6 8 10 12
Percent of Respondents (%)
Figure 3. Self-Reported Behavioral Responses to Cost-sharing:
Increased Burden
Burden: Any Behavior (N=152)
Sw itched to cheaper medication (N=80)
Received free samples (N=17)
Gone to non-Kaiser pharmacy (N=23)
Bought medications outside of US (N=11)
Bought medications on the internet (N=1)
Used pharmacy assistance program (N=5)
0.1
1.5
2.3
3.1
0.7
Borrow ed $ to pay for medications (N=37)
Gone w ithout a necessity (N=24)
Borrow ed medication from friend/family (N=20)
3.3
2.7
5
0
10.9
20.5
3 6 9 12 15 18 21
Percent of Respondents (%)
Table 3. Behavioral Response to Cost-sharing:
Decreased Adherence Multivariate Logistic Regression
Characteristic Self-Reported
Cost-Sharing
OR
Actual Cost-
Sharing
95% CI OR 95%CI
Drug Cost-Sharing:
Generic Copay ($)
Brand – Generic Copay ($)
Any Benefit Cap
Age 65+
1.04
1.01
†
2.37
‡
0.57
1.73
Female Gender
Non-White Race 1.13
Education: less than College Graduate 0.54*
Married
Household Income < $35,000
1.42
3.08
‡
Health Excellent or Very Good 0.80
Number of RX’s used in 12 mos.: 0,1,2-4,5+ 1.76
†
0.99, 1.10
1.00, 1.03
1.26, 4.47
0.96
1.04
1.76
0.23, 1.40
0.39
0.89, 3.36
0.57, 2.25
0.28, 1.04
0.44
0.75, 2.72
1.50, 6.35
3.03
0.41, 1.56
1.54
1.35
1.43
0.90
1.04, 2.99
1.95
†
‡
‡
‡
0.81, 1.14
0.97, 1.11
0.74, 4.19
0.16, 0.92
0.84, 2.83
0.73, 2.49
0.24, 0.81
0.79, 2.61
1.54, 5.98
0.49, 1.65
1.20, 3.18
Models Adjusted for Comorbidity
*p=<0.10, †p=<0.05, ‡p=<0.01, CI= Confidence Interval
Table 4. Behavioral Response to Cost-sharing:
Increased Burden Multivariate Logistic Regression
Characteristic Self-Reported
Cost-Sharing
Actual Cost-
Sharing
95% CI OR 95% CI OR
Drug Cost-Sharing:
Generic Copay ($)
Brand – Generic Copay ($)
Any Benefit Cap
Age 65+
Female Gender
Non-White Race
1.04* 0.99, 1.09
0.96
1.01
† 1.00, 1.03
1.04
1.94
† 1.16, 3.25
1.76
0.42
1.96
†
†
0.20, 0.86
1.15, 3.35
0.39
1.54
Education: less than College Graduate
Married
1.30 0.76, 2.24
1.35
1.27
0.73, 2.22
0.44
‡
1.59* 0.93, 2.72
1.43
Household Income < $35,000 3.07
‡ 1.73, 5.47
3.03
‡
Health Excellent or Very Good 0.68
0.40, 1.17
0.90
Number of RX’s used in 12 mos.: 0,1,2-4,5+ 1.46*
0.97, 2.19
1.95
‡
†
0.81, 1.14
0.97, 1.11
0.74, 4.19
0.16, 0.92
0.84, 2.83
0.73, 2.49
0.24, 0.81
0.79, 2.61
1.54, 5.98
0.49, 1.65
1.20, 3.18
Models Adjusted for Comorbidity
*p=<0.10, †p=<0.05, ‡p=<0.01, CI= Confidence Interval
Limitations
►
Single IDS with a range of delivery options
►
English-speakers only
►
Modest levels of cost-sharing
►
Self-reports of behavioral responses
►
No measure of clinical impact of behavioral responses
Conclusions
►
Patients appeared to have general knowledge of their prescription drug cost-sharing, but limited knowledge about the amounts
►
Nearly one in four patients changed their behavior in response to their perceived level of prescription drug costsharing
– Over one in ten patients did not take their drugs as prescribed because of their perceived level of drug costsharing
– Nearly one in five patients reported an increased burden in paying for their prescription medications
Implications
►
The impact of drug cost-sharing on behavior may be attenuated due to limited knowledge of actual cost-sharing amounts
►
Persons with more drug use or lower income may be more likely to change their behavior in response to drug costsharing
►
Additional research is needed on the clinical and economic ramifications of prescription drug cost-sharing