Long-Term Care
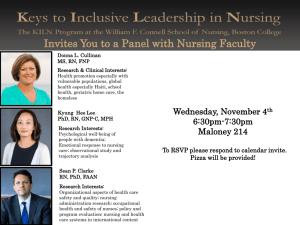
advertisement

Long-Term Care Call for Papers Medical Care Use of Residential Care Patients Chair: Penny Hollander Feldman, Ph.D., M.P.H. Sunday, June 6 • 11:30 a.m.-1:00 p.m. • The Effect of Federal Drug Therapy Guidelines on Patient Safety in Nursing Homes: A Natural Experiment Becky Briesacher, Ph.D., Rhona Limcangco, M.Pharm., Linda Simoni-Wastila, Ph.D., Jalpa Doshi, Ph.D., Jerry Gurwitz, M.D., Edward Mortimore, Ph.D. Presented by: Becky Briesacher, Ph.D., Assistant Professor, School of Pharmacy, University of Maryland, 515 W. Lombard, Baltimore, MD 21201; Tel: 410 706.1490; Fax: 410.706.1488; Email: bbriesac@rx.umaryland.edu Research Objective: To test if federally mandated drug use reviews reduce exposure to potentially inappropriate medications in nursing homes. Study Design: This is a quasi-experimental, longitudinal study using the 1997-2000 Medicare Current Beneficiary Survey (MCBS), a nationally representative dataset on the health status and medical care utilization of the Medicare population. We identified institutionalized beneficiaries and linked their files to a newly available dataset of facility medication administrations. Our analysis calculated quarterly exposures to 38 potentially inappropriate medications in nursing homes (NH) before and after a 1999 policy change to expand the drug use reviews mandated by the Centers for Medicare and Medicaid Services (CMS). CMS requires Medicare- or Medicaid-eligible NHs to submit to surveys of quality indicators, including the use of inappropriate medications, any related adverse drug reactions, and medical record justification for exempted use. Our study compared the prevalence and incidence use of potentially inappropriate drugs in NHs to those in assisted living facilities (ALF), which are not subject to the CMS rules. We used a difference-indifference model and survival regression estimators to calculate the adjusted hazard of post-policy exposures in NHs relative to pre-policy levels and ALF exposures. Our analysis examined criteria drugs restricted for both the entire institutional population and patients with certain diseases. We also stratified inappropriate drug use by three levels of legitimate exceptions: medications always to avoid, rarely appropriate, or have some acceptable indications. Population Studied: Nationally representative population sample of 8 million NH residents [unweighted n=2242], and a comparison group of 2 million ALF residents [unweighted n=664]. Principal Findings: Before the CMS policy change, 28.8% (95% confidence interval [CI], 27.3-30.3) of Medicare beneficiaries in NHs and 22.4% (95% CI, 19.8-25.0) in ALFs received potentially inappropriate medications. Nearly all prepolicy use came from medications with some acceptable indications: 23.4% in NHs (95% CI, 20.4-26.4) and 18.0% in ALFs (95% CI, 15.6-20.4). After the policy change, exposures in NHs declined slightly to 25.6% (95% CI: 24.1-27.1, p<0.05); however a similar decline occurred in ALFs (19.0%; 95% CI, 16.7-21.3, NS). Post-policy use of potentially inappropriate medications with some exempted indications remained high and over half was attributable to incident use: 1 in 5 NH residents (20.6%; 95% CI, 19.0-22.0) and 1 in 6 ALF residents (15.6%; 95% CI, 15.2-15.7). Post-policy use of drugs restricted with certain diseases increased in NH by 33% (13.2%; 95% CI, 12.2-14.2, p<0.05], particularly for seizure disorders or epilepsy. Multivariate results detected no post-policy differences in inappropriate drug use between long-term care facilities with mandatory drug use reviews and those without. Conclusions: Some post-policy declines were noted in the NH use of potentially inappropriate medications but the decrease was uneven and could not be attributed to the federally-mandated drug use reviews. Lower use of the most risky medications occurred also in ALFs suggesting a general prescribing trend rather than policy impact. Prescribing of medications restricted with certain diseases increased in NHs after the policy change. Implications for Policy, Delivery or Practice: Our study is the first evaluation of the CMS policy and it highlights the unclear effectiveness of drug use reviews to improve patient safety in NHs even though this strategy has been widely adopted by state and federal agencies. Primary Funding Source: CMS • Cost-Benefit Analysis of Nursing Home Registered Nurse Staffing Times David Dorr, M.D., Susan Horn, Ph.D., Randall Smout, M.S. Presented by: Susan Horn, Ph.D., Senior Scientist, Institute for Clinical Outcomes Research, 699 East South Temple, Suite 100, Salt Lake City, UT 84102-1282; Tel: 801.466.5595, Ext. 125; Fax: 801.466.6685; E-mail: shorn@isisicor.com Research Objective: Adequate nurse staffing in hospitals, ICUs, ambulatory clinics, and nursing homes has been shown to be critical for quality care. Cost/benefit of better resident outcomes versus additional wages for nurses is largely unknown. Our research objective was to perform a costbenefit analysis of societal benefits of decreased adverse resident outcomes versus additional wages of registered nurses to achieve adequate staffing in nursing homes. Study Design: Retrospective chart review was used to collect data on over 500 resident, treatment, facility, and outcome variables including Comprehensive Severity Index. Multivariate regression analyses evaluated significance of associations between registered nurse staffing times and outcomes, controlling for severity of illness and other confounding variables. Outcomes included development of pressure ulcers (PU), urinary tract infections (UTI), and hospitalizations. Event rates are from National Pressure Ulcer Long-Term Care Study (NPULS). Hospital costs are estimated from Medicare statistics and from charges in the Health Care Cost and Utilization Project. UTI and PU costs are from cost-identification studies. Difference in rates of PU, UTI, and hospitalizations per resident per day were calculated from low staffing and adequate staffing nursing homes. Benefits from reductions in these events are calculated in FY 2001 dollars and compared to costs of increasing nurse staffing. Societal and institutional perspectives are addressed. Population Studied: Cohort of 1,376 residents from 82 longterm care facilities participating in NPULS; inclusion criteria were length of stay > 14 days, at risk of developing pressure ulcers with Braden Scale score < 17, and no pressure ulcer on study entry. Principal Findings: Analysis shows net societal benefit of $319,000 per year for a hundred bed high risk, long stay nursing home unit, which employs sufficient nurses to achieve 30-40 minutes of per resident direct care registered nurse time per day versus those nursing homes who have nursing time of <10 minutes. Sensitivity analyses revealed a robust set of estimates, with no single or paired elements reaching cost/benefit equality threshold. Conclusions: Adequate nurse staffing in nursing homes can have significant societal quality of care and cost benefits, but cost benefits may not accrue to nursing homes under current reimbursement systems. Implications for Policy, Delivery or Practice: A properly functioning market system might lead to appropriate support by consumers of high quality institutions, but existing information asymmetries have been resistant to appropriate discernment of quality. Therefore, incentives for improvement must allow some (or most) of those savings to be returned to nursing homes that voluntarily improve or maintain appropriate staffing ratios. Altering reimbursement to more accurately reflect cost-effectiveness of care has support in the literature, can be implemented relatively quickly, and may improve outcomes; effective nursing care to prevent adverse outcomes must be reflected in these alterations. Primary Funding Source: National Library of Medicine (Training Grant 5T15LM007124-07) • The Effect of Medicaid Rate on Potentially Preventable Hospitalizations from Nursing Home O. Intrator, Ph.D., Vincent Mor, Ph.D., Ning Wu, M.D., M.S., David Gifford, M.D., M.P.H., David Grabowski, Ph.D., Zhanlian Feng, Ph.D. Presented by: O. Intrator, Ph.D., Assistant Professor (Research), Center for Gerontology and Health Care Research, Brown University, Box G-ST2, Providence, RI 02912; Tel: 401.863.3579; Fax: 401.863.9219; E-mail: Orna_Intrator@Brown.Edu Research Objective: Medicaid payment rates are reflected in the availability of the clinical resources (such as availability of physician assistants/nurse practitioners) necessary to manage nursing home residents’ medical conditions. Since over 60% of all nursing home residents are Medicaid recipients, differences in reimbursement rates are likely to contribute to observed inter-state differences in hospitalization rates. This paper tests the hypothesis that nursing home residents in states with higher Medicaid rates experience fewer potentially preventable hospitalizations. Study Design: Data: Minimum Dataset (MDS) clinical assessment data merged with inpatient Medicare claims, Online Survey Certification And Reporting (OSCAR) facility data, Area Resource File county level market data, and a survey of state policies conducted at Brown University. Study Design: Cross sectional study with 6-month hospitalization operationalized as a hierarchical outcome: any potentially preventable hospitalization (measured as ambulatory care sensitive, ACS, diagnoses), any other hospitalization, death versus remaining in the facility. Analyses: Three separate binomial response regressions models for each of the outcomes compared to remaining in the facility were constructed. This allows for Markov Chain Monte Carlo estimation, producing unbiased estimates. Analyses of a fourlevel (resident-facility-market-state) logistic regression model of any ACS hospitalization are reported here. Analyses were conducted using Markov-Chain-Monte-Carlo (MCMC) methods in MLWiN. Population Studied: All continuous nursing home residents in freestanding Medicare/Medicaid certified urban facilities in the 48 contiguous U.S. states during the 2nd quarter of 2000 for 90 days or more were identified from MDS data. Facilities specializing in pediatric, HIV, MS, or brain injury care were excluded, as were residents under the age of 65, and residents who were members of MCOs during any point in 2000. Principal Findings: Among 571,816 long-stay residents of 9,124 facilities, over a six month period, 7.4% experienced a potentially preventable hospitalization, 12.6% experienced other hospitalizations, and 9.2% died. Multilevel, multivariate results revealed that residents in states with a $20 higher reimbursement rate than the median $100 were 9.6% less likely to experience an ACS hospitalization (95% CI of AOR = 0.84-0.97), controlling for many resident, facility and market characteristics. Residents in facilities with nurse practitioners/physician assistants and facilities with the Harrington recommended level of an average of 4.55 nurse hour per patient day were 6.8% and 6.5% less likely to be hospitalized, respectively. Conclusions: States with more generous nursing home reimbursement rates appear to have lower rates of preventable hospitalization of long stay nursing home residents. This direct effect of a higher reimbursement rate is intensified by the indirect effect of higher reimbursement rates on increased availability of more skilled staffing (also associated with reduced hospitalization rates). Implications for Policy, Delivery or Practice: Recent state budgets deficits increase the importance of properly aligning state and Federal policies in the nursing home arena since state investments in higher reimbursement translates into hospital savings which benefit Medicare. Unnecessary hospitalizations for clinical conditions that could be managed in the nursing home are likely to have a negative quality impact on residents’ lives, thereby undermining current state and federal initiatives to improve the quality of nursing home care. Primary Funding Source: NIA • Reduction in Mortality Associated with Influenza and Pneumococcal Vaccination of Elderly in Nursing Homes Sophia Kazakova, M.D., Ph.D., M.P.H., Amy Curtis, Ph.D., Dale Bratzler, DO, Wato Nsa; Linda Steele; Ph.D., Linda McKibben; Richard Chesley, M.D., Abby Shefer, John Jernigan Presented by: Sophia Kazakova, M.D., Ph.D., M.P.H., Epidemic Intelligence Officer, Division of Healthcare Quality Promotion, Centers for Disease Control and Prevention, 57 Executive Park Drive SNE, Atlanta, GA 30329; Tel: 404.498.1128; Fax: 404.498.1101; E-mail: srk7@cdc.gov Research Objective: To examine the impact of influenza and pneumococcal vaccination on mortality among Nursing Home (NH) residents during two recent influenza seasons. Study Design: In this retrospective cohort study, individual vaccination status was assessed for 2000-2001 and 20012002 cohorts of NH residents and linked to the Medicare enrollment database and Minimum Data Set for each resident. We used multilevel multivariate logistic regression analysis, which controls for individual and facility-level factors, to examine the influence of individual influenza and pneumococcal vaccination and facility-level influenza and pneumococcal vaccination coverage on mortality. Population Studied: 36,227 Nursing Home residents randomly selected from 277 NHs in 14 states. Principal Findings: Of the 18,636 residents in the 2000-2001 cohort and 17,591 in the 2001-2002 cohort, 2,935 (15.7%) and 3,020 (17.2%) residents died respectively during the influenza seasons. In both cohorts, about 60% of residents received influenza and 40% received pneumococcal vaccination. For the first cohort, receipt of influenza (RR 0.59; CI 0.53-0.66) and pneumococcal (RR 0.74; CI 0.67-0.82) vaccination and being a resident of a facility with 80% or greater influenza coverage (RR 0.81; CI 0.72-0.91) were independently associated with a reduced mortality. High facility pneumococcal vaccination coverage was not associated with decreased mortality. Similar results were obtained for the second cohort. Conclusions: This is the first study demonstrating the significant protective effect of individual pneumococcal vaccination on mortality among NH residents. This study confirms the important role of individual influenza vaccination in preventing deaths and suggests that residing in a facility with a high influenza vaccination rate independently reduces the risk of death. Implications for Policy, Delivery or Practice: Programs to increase pneumococcal and influenza vaccination among NH residents should be encouraged to decrease mortality. Primary Funding Source: CDC • Medicare Expenditures for Residents in Assisted Living: Data from a National Study Charles Phillips, Ph.D., M.P.H., Scott Holan, M.S., Michael Sherman, Ph.D., William Spector, Ph.D., Catherine Hawes, Ph.D. Presented by: Charles Phillips, Ph.D., M.P.H., Professor, School of Rural Public Health, Texas A&M University System Health Science Center, 3000 Briarcrest Drive, Suite 310, Bryan, TX 77802; Tel: 979.458.0080; Fax: 979.458.0656; E-mail: phillipscd@srph.tamushsc.edu Research Objective: To investigate the level of Medicare expenditures for assisted living facility (ALF) residents and whether an ALF’s characteristics affect residents’ use of Medicare-covered services. Study Design: Cross-sectional analyses using multivariate logistic and ordinary least squares regression techniques were used to determine the effects of individual and facility characteristics on Medicare utilization and expenditures. Population Studied: Primary and secondary data collection. Primary data come from the National Study of Assisted Living for the Frail Elderly conducted in 1998-1999. This study restricted its interest to the approximately 1,200 residents who remained in an ALF from baseline to follow-up data collection. Secondary data are six months of post-baseline Medicare claims acquired for 545 of these residents, who did not differ significantly from the larger sub-sample. Principal Findings: On an annualized basis, assisted living residents incurred Medicare costs of approximately $4,800. Just under 15% of assisted living residents accounted for over 75% of total Medicare costs. Both the likelihood of utilizing Medicare-covered services and the intensity of service use were largely unaffected by the characteristics of the ALF in which residents lived. The only exception to this general finding is that those individuals who utilized services and resided in smaller ALFs had significantly lower expenditures. However, individual characteristics dominated the multivariate models. Conclusions: Both the level of Medicare expenditures and the distribution of Medicare expenditures among ALF residents were similar to those among the general Medicare beneficiary population. Also, assisted living residents had patterns of Medicare payments that resembled those among other community-dwelling in the Medicare Current Beneficiary Survey. Implications for Policy, Delivery or Practice: The lack of impact exhibited by facility characteristics on Medicare expenditures implies that regulatory efforts aimed at developing a specific type of facility will have little effect on affecting Medicare expenditures. Also, the similarity betweeen Medicare payments for those in assisted living and elsewhere in the community may imply that assisted livng, as currently configured, is not a viable alternative to nursing home admission. Primary Funding Source: AHRQ Call for Papers Long-Term Care Community Services & Market Factors Chair: Barbara Gage, Ph.D., M.P.H. Tuesday, June 8 • 9:15 a.m.-10:45 a.m. • Do Children with Developmental Disabilities Benefit from Consumer-Directed Medicaid Supportive Services Programs? Leslie Foster, M.P.A., Stacy Dale, M.P.A., Randall Brown, Ph.D., Barbara Phillips, Ph.D., Jennifer Schore, M.S., M.S.W, Barbara Lepidus Carlson, M.A. Presented by: Leslie Foster, M.P.A., Researcher, Mathematica Policy Research, Inc., P.O. Box 2393, Princeton, NJ 08043; Tel: 609.936.3265; Fax: 609.799.0005; E-mail: lfoster@mathematica-mpr.com Research Objective: To compare the use, quality, and costs of Medicaid supportive services used by children with developmental disabilities under Florida's traditional homeand community-based services waiver program, to that experienced by children under a Cash and Counseling demonstration program, in which parents directed their child's use of supportive services. Study Design: Children who enrolled in the voluntary demonstration were randomly assigned to participate in Consumer Directed Care (the treatment group) or to continue receiving traditional waiver benefits (the control group). Parents of treatment group children had the opportunity to receive a monthly allowance, which they could use to hire their choice of caregivers and to buy other goods and services for their child, with the help of program counselors and bookkeepers. Computer-assisted telephone interviews were conducted at enrollment and nine months later with the parents (or guardians) of 862 children. The nine-month interviews were conducted between April 2001 and July 2002. We used responses to the nine-month follow-up interviews to measure (1) children's use of paid and unpaid personal care services, (2) parents' satisfaction with their child's care and quality of life, (3) children's unmet needs for personal care services and supplies, and (4) children's disability-related health problems, adverse events, and general health status. We used Medicaid claims data to measure the costs of children's goods and services. Program impacts were estimated with regression models that controlled for a comprehensive set of baseline characteristics. Population Studied: Children aged 3 to 17 who were enrolled in Florida's Developmental Services waiver program, and whose parents voluntarily enrolled them in the state's Cash and Counseling demonstration. Principal Findings: Compared with children in Florida's traditional waiver program, children whose parents directed their waiver benefits were more likely to receive personal care from someone who was paid to help them, and their parents were happier with their care and well-being. Treatment group children received more hours of paid personal care, but fewer hours of unpaid personal care, than control group children received. Parents of treatment group children were less likely than their counterparts in the control group to say their child had unmet needs for personal care and supplies, and they were much more satisfied with their child's overall care arrangements and with the way paid caregivers performed their jobs. Moreover, children in the treatment group were less likely than children in the control group to experience certain disability-related health problems, and their parents were more satisfied with the way children were spending their lives. Finally, preliminary claims data suggest that Medicaid waiver costs increased under Consumer Directed Care, but the increases may have been offset by savings on other Medicaid services, especially home health. Conclusions: Children and their parents seemed to benefit from the flexibility afforded by Consumer Directed Care, particularly because they could hire family, friends, or other providers as caregivers. Not only were parents more satisfied with their child's care arrangements under the demonstration program than they would have been under the traditional waiver program, but those arrangements seemed to protect children's health. Medicaid waiver costs increased, perhaps because control group children did not receive all the benefits they were entitled to in the traditional waiver program. Implications for Policy, Delivery or Practice: Our findings should encourage states to consider consumer-directed supportive services program options, as Consumer Directed Care increased parents' satisfaction, and did not jeopardize children's health and safety. Because Consumer Directed Care increased the likelihood that children received paid personal care, it did increase Medicaid waiver costs. Policymakers might find such costs to be warranted, however, since gains in satisfaction were so great and unmet needs were reduced. Furthermore, it appears that the net total costs to Medicaid are small, because of offsetting reductions in children’s use of other Medicaid services. In an earlier evaluation of Cash and Counseling in Arkansas, the demonstration program was found to have similarly positive effects on the satisfaction and well-being of adult Medicaid beneficiaries who were eligible for personal care services. Primary Funding Source: RWJF • Varied Regional Responses to Medicare Post-Acute Care Prospective Payment Systems Wen-Chieh Lin, Ph.D., Robert Kane, Ph.D., David Mehr, M.D., M.S., Richard Madsen, Ph.D., Gregory Petroski, M.S. Presented by: Wen-Chieh Lin, Ph.D., Assistant Professor, Department of Family and Community Medicine, University of Missouri-Columbia, M226 Medical Sciences Building, Columbia, MO 65212; Tel: 573.882.1584; Fax: 573.882.9096; Email: linwe@missouri.edu Research Objective: To examine how regions responded to changes in Medicare post-acute care (PAC) payment systems as enacted by the Balanced Budget Act (BBA) of 1997. Study Design: PAC use variations across census divisions were examined using multinomial logistic regression. The reference category for the dependent variable (PAC settings) was “discharged home without formal care.” We controlled for patient, hospital and market area characteristics. Interaction terms between Year 2000 (the post-BBA indicator) and census divisions were included to examine differential effects of the BBA among regions. Population Studied: Hospitalized elderly Medicare beneficiaries represented in the 5% sample of 1996 and 2000 Medicare claims, with one of either three rehabilitative conditions (stroke, hip procedure, and hip fracture) or three medical conditions (COPD, pneumonia, and CHF). Principal Findings: Hip procedure and CHF are used here as examples. First, data in 1996 and 2000 were analyzed separately. Major differences in the estimated coefficients between these two years of data were observed on variables representing census divisions, while minor differences were noted for patient, hospital, and PAC supply variables. Second, data in 1996 and 2000 were combined and an independent variable indicating the post-BBA period (Year 2000) was added to the model. IRF utilization following hip procedures increased (OR=1.12, 95% CI [1.04, 1.21]) and HHA utilization decreased (OR=0.77, 95% CI [0.71, 0.84]) in 2000; SNF utilization following CHF increased (OR=1.16, 95% CI [1.09, 1.24]) and HHA utilization decreased (OR=0.68, 95% CI [0.65, 0.72]) in 2000. Finally, we analyzed the full model including interaction terms of the post-BBA indicator and variables representing census divisions. Census divisions show substantial differences in response to the BBA changes. For example, using the West South Central as the reference region, SNF use in the New England region increased for both hip procedure and CHF (OR=0.82 in 1996 and OR=2.80 in 2000 for hip procedure; OR=1.71 in 1996 and OR=3.32 in 2000); HHA use following CHF in the New England region increased (OR=1.66 in 1996 and OR=2.68 in 2000). After taking into account for the interaction effects between the post-BBA indicator and census divisions, SNF utilization following hip procedures (OR=0.50, 95% CI [0.40, 0.62]) and HHA utilization following CHF (OR=0.56, 95% CI [0.47, 0.66]) were significant lower in 2000. Conclusions: Responses to the BBA changes differ substantially across census divisions. The BBA changes have minimal differential effects on other patient, hospital, and PAC supply characteristics, as included in our model. Further analyses will explore additional market area characteristics that may explain the area variation. Implications for Policy, Delivery or Practice: The highly varied responses to the BBA changes across regions raise the question of whether patients are discharged to appropriate settings for PAC services. PAC choice not only depends on patient characteristics, but also on patients’ residence and hospital location. Standardized guidelines and optimal outcomes of PAC utilization need to be developed and established to guide the utilization of such highly substitutable and supply-sensitive services. Comparable outcomes assessment information across settings is critical, if we are to monitor adverse outcomes resulting from inappropriate discharge and to address the issue of accountability. Primary Funding Source: AHRQ • Access to Medicare Home Health Care: How Has It Changed Following the Introduction of PPS? Christopher Murtaugh, Ph.D., Nelda McCall, M.A., Timothy Peng, Ph.D., Ann Meadow, Sc.D., Stanley Moore, B.S. Presented by: Christopher Murtaugh, Ph.D., Associate Director, Center for Home Care Policy and Research, Visiting Nurse Service of New York, 5 Penn Plaza, 11th Floor, New York, NY 10001; Tel: 212.609.5777; Fax: 212.290.3756; E-mail: cmurtaug@vnsny.org Research Objective: This paper examines the impact of the Medicare Home Health Prospective Payment System (PPS) on beneficiary access to home health care. A pre-post quasiexperimental design is employed to examine changes in the incidence of use as well as the clinical and sociodemographic characteristics of beneficiaries admitted to care before and after the introduction of PPS in October 2000. The study will provide policymakers with information to evaluate the possible need for adjustments in the payment system. Study Design: The study examines changes in access over a three-year period: federal fiscal year (FFY) 2000 (the last year before PPS) through FFY 2002. The main dependent variable is receipt of home health care during the fiscal year. Sociodemographic measures are from Centers for Medicare and Medicaid Services’ administrative records and include basic demographic and geographic information as well as whether the beneficiary was enrolled in the Medicaid program (i.e., a dual eligible). Clinical data are from inpatient facility and physician (Part-B) claims and include whether the beneficiary had one or more of the diagnoses that lead to a higher score on the clinical dimension of Home Health Resource Groups (HHRGs). Regression models are estimated that control for changes in market conditions and include interaction terms to test for differential effects of PPS on selected groups. Population Studied: The study population is all Medicare beneficiaries living in the 50 states or the District of Columbia, except those in a Medicare HMO or without hospital insurance (Medicare Part-A). The analyses were conducted on a 1% sample of beneficiaries. Home health users are individuals with at least one paid home health visit during the fiscal year. Principal Findings: The incidence of home health use declined after the introduction of PPS from 76.2 users per 1,000 beneficiaries in FFY 2000 to 69.8 in FFY 2001. Preliminary analyses indicate that reductions in use were greatest among dual eligibles, men, those living in rural areas, and beneficiaries residing in states with relatively high historical home health care use. Initial analyses also suggest that PPS generally increased the admission of persons with medical conditions that lead to higher HHRG scores relative to other beneficiaries. Conclusions: The study provides a first look at the impact of the PPS on access to home health care. The decline in the incidence of home health use in the initial year of PPS was not expected since payment levels for the HHRGs are thought to be generous. The shift toward the admission of individuals with orthopedic and other conditions often requiring rehabilitation therapy and decline in the admission of beneficiaries with common medical problems that tend to be clinically difficult to manage (e.g., heart failure) suggest that the latter group should continue to be monitored for unintended access changes and outcome problems. Implications for Policy, Delivery or Practice: Policymakers can address possible access problems by modifying the payment system. The paper discusses alternative approaches including changes in the HHRG scoring system and outlier policy to respond to any evidence of unintended PPS impacts. Primary Funding Source: RWJF • Do Selection or Treatment Effects Explain Differences in Medicare Costs among Hospice and Normal-Care Decedents? Donald Taylor, Jr., Ph.D., M.P.A., Courtney Van Houtven, Ph.D., Jan Ostermann, Ph.D. Presented by: Donald Taylor, Jr., Ph.D., M.P.A., Assistant Professor, Public Policy, Duke University, Box 90253, 122 Old Chemistry Building, Durham, NC 27708; Tel: 919.684.2361; Fax: 919.684.6246; E-mail: dtaylor@hpolicy.duke.edu Research Objective: To determine whether lower end-of-life Medicare costs observed among decedents are due to selection or treatment effects. Study Design: The use of hospice has increased steadily since it became a covered Medicare benefit in 1982, with nearly 20 percent of Medicare decedents using hospice care in 1999. Determining whether the hospice benefit truly reduces total Medicare costs for end-of-life care compared to usual care has been difficult because it requires disentangling treatment effects from selection effects. Selection implies that persons choosing hospice are systematically different utilizers of health care than usual care decedents, while treatment implies that hospice truly reduces Medicare costs of end-of-life care after controlling for selection. We use hazard models to control for the different propensities to use hospice care among all decedents, and create a matched control sample based on daily predicted probabilities of hospice care prior to death between hospice users and non-users. We then compared costs per day from hospice entry to death for those using hospice to costs per day for the same period of time for matched controls (the usual care sample). We also determine whether the results differ by diagnosis (cancer, heart disease, COPD, and neurological degenerative disorders (including Alzheimer’s disease)). Population Studied: We analyzed 9,127 members of a screening sample for the National Long Term Care Survey who died between July 1, 1991 and December 31, 1999. We used Medicare claims records of all types (inpatient, outpatient, home health, physician supplier, SNF, DME, and hospice) to determine total Medicare-financed costs among decedents from January 1, 1991 until death or the censor date. Principal Findings: Bivariate findings show that costs during the last 30 days of life were lower for those using hospice ($4,498) compared to usual care ($6,227, p-value less than 0.001), a pattern that remained when considering the last 60 days of life ($8,320 versus $9,577, p-value equal to 0.02). Costs during the last 90 days of life did not differ by hospice use ($11,421 versus $11,708, p-value equal to 0.19). When comparing costs among hospice users and usual care decedents using our matched approach that controls for selection effects, we found that hospice costs were 6% (pvalue less than 0.01) lower per day compared to controls. Differences were larger for cancer compared to other reasons for using hospice. Conclusions: The results suggest that hospice has a true treatment effect on total Medicare costs after the point of entry into hospice; differences are not only due to selection. Implications for Policy, Delivery or Practice: The results suggest that expansion of hospice care to a larger proportion of Medicare beneficiaries needing end-of-life care may reduce rather than increase the cost to the Medicare program, especially if the benefit can be targeted to persons within 60 days of death. Primary Funding Source: RWJF • Home and Community Based Waivers for Disabled Adults Courtney Van Houtven, Ph.D., Marisa Elena Domino, Ph.D. Presented by: Courtney Harold Van Houtven, Ph.D., Health Economist/Research Assistant Professor, Health Services Research/General Internal Medicine, VA and Duke Medical Centers, 508 Fulton Street, Durham, NC 27514; Tel: 919.286.6936; Fax: 919.416.5839; E-mail: courtney.vanhoutven@duke.edu Research Objective: to examine selection effects and true program effects of a Medicaid Home and Community Based Waiver, controlling for endogenous selection of persons into the program. Study Design: North Carolina Medicaid claims and enrollment data from Fiscal Years 1999-2000 (July 1998-June 2000) were merged together with county-level health care supply, demographic and economic characteristics found in the Area Resource File for North Carolina. We model selection as a function of an array of coded health conditions, using the Chronic Illness and Disability Payment System, developed specifically for the disabled adult population. We then model actual Medicaid expenditures in three areas: total expenditures, nursing home expenditures, and hospital inpatient expenditures, using a two-part model, controlling for the endogeneity in selection through the use of instrumental variables. Population Studied: Adults identified as disabled or blind were identified and selected from Medicaid enrollment data; only persons with more than $10,000 in Medicaid expenditures in the base year were selected in order to focus on those most likely to need facility-based medical care. All claims for these subjects were selected. Principal Findings: We find substantial evidence of selection into the waiver program. Waiver participation leads to a higher likelihood of having any costs, but no difference in total costs for users than for non-participant users. Waiver participants have the same likelihood of any nursing home expenditures as non-participants, but among nursing home users, have a large decrease in expenditures. Waiver participants are no less likely to have any hospital inpatient expenditures than non-participants, but among inpatient users, waiver participants have significantly lower levels of expenditures. Conclusions: Participation in a Medicaid home and community-based waiver leads to substantially different patterns of care. Although no total cost savings are found in this sample, significant decreases are found in the level of nursing home and hospital inpatient expenditures for those on the waiver. Implications for Policy, Delivery or Practice: Although we cannot generalize outside the sample of North Carolina Medicaid waiver participants, the Home and Community Based Waiver program in this state does not seem to hold great promise for decreasing total Medicaid expenditures, especially when those expenditures are not just limited to the targeted nursing home system. This finding may be due in part to the more acutely ill population selected for this analysis, but should also be interpreted as a sign of success. Savings were seen in both the nursing home and inpatient sector for persons who accessed these two service types. Overall costs did not increase, so the combination of results seems to mean that the CAP waiver has met its designed goals of keeping people in the community through the greater use of outpatient or community based services, and not increasing total costs. Related Posters Poster Session A Sunday, June 6 • 6:45 p.m.-8:00 p.m. • Correlates of Long-Term Care Use Among Triply Diagnosed HIV Patients in the HIV/AIDS Treatment Adherence, Health Outcomes and Cost Study Susan Ettner, Ph.D., Alfonso Ang, Ph.D., Marcia Weaver, Ph.D., Chris Conover, Ph.D., Peter Arno, Ph.D. Presented by: Alfonso Ang, Ph.D., Principal Statistician, School of Medicine, University of California, Los Angeles, 911 Broxton Plaza, Suite 201, Los Angeles, CA 90095; Tel: 323.463.8850; E-mail: AAng@mednet.ucla.edu Research Objective: To examine the factors associated with the use of formal and informal long-term care among triply diagnosed patients, who account for 13% of all HIV patients and 27% of their costs. Study Design: Observational cohort study, based on inperson interviews and medical record review. We estimate a multinomial logistic regression for whether the patient received any formal long-term care; informal long-term care only; or no long-term care. Then we estimate a two-part model of the number of home care hours received, separately estimating the probability of any home care use and the conditional level of home care hours and combining the estimates to derive predictive margins for unconditional use. Confidence intervals were derived using bootstrapping methods. Missing data are multiply imputed using Monte Carlo Markov Chain methods. All regressions include fixed effects to adjust for within-site correlation of patients. Population Studied: 1,046 HIV patients meeting clinical criteria for at least one mental health and one substance disorder. Principal Findings: 31% of study patients used long-term care during the 3 months prior to baseline. 2% used nursing homes, 4% used day hospitals, and 27% used home care. Patients with either higher Physical Composite (PCS) or Mental Composite (MCS) Scores were less likely to receive informal care, relative to no long-term care. However, those with higher PCS scores were less likely to receive formal care, while those with higher MCS scores were more likely to receive it. Patients who abused alcohol only were almost twice as likely as those abusing both alcohol and drugs to receive informal care vs. no long-term care. Medicaid beneficiaries were almost three times as likely to receive formal care, relative to receiving no long-term care, and dual MedicareMedicaid beneficiaries were almost fivefold as likely. Dual eligibles were about three times as likely to receive formal long-term care relative to informal care only, and Medicareonly beneficiaries were over four times as likely. Women were 1½ times more likely than men to receive informal care rather than no long-term care, but only half as likely to receive formal care, relative to informal care only. Married persons were only half as likely as never-married persons to receive formal care relative to no long-term care. Women, college-educated patients and patients abusing only a single substance were more likely to receive any home care; patients with higher PCS or MCS scores were less likely. Overall, healthier persons and Latinos received fewer home care hours and women and married and persons received more. Conclusions: Medicare and Medicaid are strongly associated with formal long-term care use among triply diagnosed patients. While health need and availability of caregivers are significant predictors of long-term care patterns, so too are other sociodemographic characteristics that may or may not be related to need. Implications for Policy, Delivery or Practice: Access to longterm care may be a policy concern for HIV patients in certain sociodemographic groups or who lack strong social support systems. Public insurance programs may play a key role in facilitating the use of formal long-term care among vulnerable triply diagnosed patients. Primary Funding Source: Center for Mental Health Services • The Impact of Care Coordination on Use and Expenditures in a Disabled Medicaid Population Sema Aydede, Ph.D., Pamela Coleman, M.B.A., Don Haywood, M.A., Gary Young, JD, Elizabeth Shenkman, Ph.D. Presented by: Sema Aydede, Ph.D., Associate Scholar, University of Florida, Institute for Child Health Policy, 1329 S.W. 16th Street, 5th Floor, Room 5130, Gainesville, FL 32608; Tel: 352.265.7220 Ext. 86335; Fax: 352.265.7221; E-mail: ska@ichp.edu Research Objective: Efficient use of health care resources are becoming more important in an era of state budget deficits and increasing health care expenditures. This study explores how effective integration and coordination of health care services are in achieving efficient use of health care resources. The analysis focuses on STAR+PLUS, a pilot program in Texas for Supplemental Security Income (SSI) beneficiaries. Integration and coordination become especially crucial for disabled and chronically ill populations. The STAR+PLUS program intends to achieve a seamless continuum of care by integrating acute and long-term care in a managed care environment. Study Design: A quasi-experimental design with health status and severity of illness matched intervention and control groups is employed. Enrollment and encounter data on 2315 Medicaid-only SSI adults (aged 21 and above) receiving community-based long-term care services with at least 3 months continuous enrollment in the STAR+PLUS program during September 2001-August 2002 were used in forming the intervention group. Enrollment and encounter data from STAR, the Medicaid managed care organization (MCO) program in Texas, was used in forming a control group with similar characteristics. Both STAR+PLUS and STAR MCO enrollees were grouped into nine mutually exclusive Clinical Risk Group (CRG) categories (such as significant acute, minor chronic, malignancies and catastrophic conditions) using the CRG software. It was found that the voluntary nature of enrollment for SSI beneficiaries in the STAR MCO program results in a self-selection process and a healthier group of SSI is enrolled in STAR MCOs when compared to SSI enrollees in STAR+PLUS. As a result, stratified random sampling at the severity of illness level within each CRG health status category was used in matching the case-mix distribution of the intervention group to that of the control group. Population Studied: Medicaid-only adult SSI beneficiaries receiving community-based long-term care services. Principal Findings: STAR+PLUS enrollees receiving community-based long-term care services are mostly female (63.11%) and almost all live alone (95.98%). Multivariable analyses show that SSI beneficiaries receiving care coordination services in an integrated environment have lower rates of inpatient stays (OR 0.75, 95% CI 0.58-0.94, p=0.0310) and emergency department visits (OR 0.68, 95% CI 0.54-0.86, p=0.0012) when compared to the use rates for SSI beneficiaries in nonintegrated environments without care coordination. Further, PMPM expenditures are lower (coefficient=-0.2556, p=0.0143) for SSI beneficiaries receiving care coordination. Conclusions: Based on findings from this study, integration and care coordination efforts in the STAR+PLUS program are having a positive impact on health care expenditures, inpatient stays and emergency department visits for disabled and chronically ill populations receiving long-term care services. Implications for Policy, Delivery or Practice: The results from this study indicate that state programs would benefit from adopting an integrated approach coupled with care coordination in the provision of health care services to enrollees with complex needs. This approach would not only help states that are experiencing tightened budgets through reductions in health care expenditures, but would also benefit program enrollees through reducing their need for inpatient stays and emergency department visits. Primary Funding Source: Texas Health and Human Services Commission • Long-Term Care Facility Characteristics Predictive of Increased Influenza and Pneumococcal Vaccination Coverage for Residents Barbara Bardenheier, M.P.H., M.A., Abigail Shefer, M.D., Linda McKibben, M.D., M.P.H., Henry Roberts, Ph.D., Dale Bratzler, DO, M.P.H. Presented by: Barbara Bardenheier, M.P.H., M.A., Epidemiologist, National Immunization Program, CDC, 1600 Clifton Road, N.E., MS E-52, Atlanta, GA 30333; Tel: 404.639.8789; Fax: 404.639.8614; E-mail: bfb7@cdc.gov Research Objective: Identify Long-term care facility (LTCF) characteristics associated with increased vaccination coverage. Study Design: Intervention study. Data on LTCF-level characteristics were collected by mailed, self-administered surveys of selected facilities in 14 states and from a Federal administrative database, OSCAR (On-line Survey Certification and Reporting System.) Immunization coverage was abstracted from residents’ medical charts using facility-level samples. Data were collected from a sample of 20 LTCFs in each of 9 intervention states and 5 control states in 2000 for baseline and in 2002 for post-intervention. Population Studied: LTCFs in 9 intervention states (DC, FL, HI, ID, KY, MA, MN, MT, NM) and 5 control states (OH, PA, WI, SC, NV). Principal Findings: 215 (91.9%) facilities participated in the survey both years. Overall, 106(50%) of the facilities’ coverage increased for both vaccines. Influenza vaccination coverage increased an average of 1.4% (range: -35.1%-68.9%) in the intervention facilities and 0.02% (-47.5% - 48.0%) in the control facilities (ns). Pneumococcal vaccination coverage increased an average of 2.4% (range: -95.8% - 87.5%) in the intervention facilities and 1.9% (range: -54.8% - 80.3%) in the control facilities (ns). Only 25 (11.9%) of facilities adopted the ACIP-endorsed standing orders model program (SOP) for influenza, and 22 (10.4%) did for pneumococcal vaccines (baseline: <10% for each). Factors associated with a significant increase in influenza vaccination coverage included: 1) Small facilities (<60 beds): +4.10% vs large facilities (>120 beds): -2.46% ; 2) Change in written immunization protocol to require documentation of refusals by residents or guardians (+5.28% vs -0.14%); and 3) Documentation of influenza vaccinations in a consistent place using a standard form in which the vaccine history could not be removed (+1.17% vs -7.94%). Factors associated with a significant increase in pneumococcal vaccination coverage included: 1) Affiliation with a multi-facility chain (+5.65% vs 1.56%); 2) Adoption of centralized tracking of pneumococcal immunizations (+9.05% vs -0.19%); and 3) Change to record pneumococcal immunizations in a consistent place (+14.55% vs -0.25%). Conclusions: Though very few facilities adopted the SOP, factors that are part of a functioning SOP (i.e., chart documentation and centralized tracking) were associated with significant improvements in vaccination coverage. Implications for Policy, Delivery or Practice: To improve the health of LTCF residents, strategies should be considered that increase immunization coverage including: centralized tracking systems, documenting vaccination status in a consistent place using a standardized form in which the vaccine history cannot be removed to an archived chart, and use of SOPs when possible. Primary Funding Source: CDC • Project Protect: Pneumococcal Vaccination Policies and Coverage in Washington State Nursing Homes M. Patricia DeHart, Sc.D., Leslie Barnette, M.D., Sandra Salinas, RHIT, Leslie Barnette, Jr., M.D., Henry Mustin, M.D., M.P.H., Lewis, Karen, M.P.H., Constance Corbett/ Pamela K. Green, M.P.H./Ph.D. Presented by: Leslie Barnette, M.D., Medical Director, Healthcare Improvement, WA, Medical Affairs, Qualis Health, 10700 Meridian Avenue N., P.O. Box 33400, Seattle, WA 98133; Tel: 206.364.9700 Ext. 7242; Fax: 206.361.5563; E-mail: lesb@qualishealth.org Research Objective: 1) Assess the current prevalence of standing orders or other written guidelines policies and their impact on vaccination rates in nursing homes in Washington State; 2)to increase the number of nursing homes with standing orders or other guidelines for pneumococcal vaccination 3)to estimate the pneumococcal coverage among the nursing home resident population over 65 years of age in Washington, and 4) to increase the percentage of nursing home residents over 65 years if age who receive pneumococcal vaccination. Study Design: In 1999 a baseline survey was developed and sent to every Washington State nursing home to assess current pneumococcal vaccination policies, and explore reasons for not having addressed such a policy. Also tested was the location of documentation of immunization status, and whether a permanent (not thinned from current chart) vaccination record was utilized to facilitate awareness of immunizationstatus of residents. This study was undertaken as a collaboration between Qualis Health, the Quality Improvement Organization for Washington (acting under a contract with the Centers for Medicare and Medicaid Services), the Washington State Department of Health, and the Immunization Action Coalition of Washington. All but one of the surveys were completed and returned (99.6%). In the fall of 2001 all Washington State nursing homes in the OSCAR database were re-surveyed to assess policy changes occurring in the intervening period. All facilities returned the second survey. The project baseline and post-intervention pneumococcal vaccination rates of current residents were derived using the MDS data. Random samples of 1,800 and 1,487 of 17,500 identified residents were selected for chart abstraction. Response rates of 82% and 75% were achieved respectively. Validation samples of 10% of the facilities for inter-rater reliability yielded a concurrence rate (Kappa statistic) of 0.703. An educational and process improvement intervention was undertaked between the surveys. A "toolkit" of materials for use in creating an in-house standing orders program (sample orders, policy and procedures, permanent immunization record for residents, alogrithm for deciding vaccination eligibility, billing information, supporting articles and immunization guidelines from the CDC, OIG, and current immunization medical literature with extensive annotated bibliography) was provided to each nursing home. An interim assessment of standing orders/guidelines use, or facility plans for implementing such a program, was followed by personal telephone contacts. All facilities were offered personal consultative site visits, which were made to 12 facilities requesting them. SAS 8.01 and EpiInfo 6 were used for the statistical analysis. A (p=<0.05) determined significance on all statistical tests. Comparisons were made using chi-squared analyses. Odds ratios were calculated using logistic regression analysis. Population Studied: All (269 in 1999, 257 in 2001)Washington State nursing homes (Long-term care facilities) and a 10% random sample of their 17,500 residents over 65 years of age. Principal Findings: The use of standing orders or other written guidelines policies by nursing homes increased 14 percent from 1999 to 2001. Comparison between pneumococcal vaccination statistics in 2000 (47%) and 2002 (61%) showed a significant increase in the percentage of Washington State nursing home residents over 65 years of age who had received pneumococcal vaccination by 2002 (Chisquared=48.88, p=<0.0001). Residents in facilities having standing orders or other written guidelines were almost three times more likely to have been vaccinated against pneumococcal disease than those in facilities with no policy/guidelines. There were significant increases in the use of standing orders or other written guidelines, and in the percentage of residents vaccinated, between initial and remeasurement periods. Overall, residents were 76% more likely to have received pneumococcal vaccinations in 2002 than in 2000 (OR= 1.76, 95% CI: 1.49, 2.07) and over 95% of the vaccinations were documented in the medical record. Conclusions: In both 2000 and 2002, the odds of a resident receiving a PPV in a Washington State nursing home having standing orders or other written guidelines are estimated to be two and one half times greater than for residents in facilities without any PPV guidelines. (2000: OR=2.59, 95% CI= 1.54, 4.34; 2002: OR=3.19 CI= 1.68, 6.01). The high response rates for both phases of this large statewide survey help insure that the findings can be generalized to the total population of nursing home residents in the state. The strong agreement between vaccination information abstracted by nursing home personnel and project staff, as shown by the kappa statistics, indicates that the findings are reliable. While the educational intervention activities were important parts of this project, the survey was not designed to measure their effect on either the use of standing orders or other vaccination guidelines, nor on pneumococcal vaccination coverage in the nursing home population. Implications for Policy, Delivery or Practice: The effectiveness of having standing orders or written guidelines in effect for the provision of pneumococcal immunizations is clearly shown in this study. At the time of this study there was no specific exemption for the general requirement for physician signature on any order effecting a medical intervention for patients under the CMS regulations. It is believed that this contributed to the "interchangeability" of the terms "standing orders' and "written guidelines" revealed in these surveys, and to concerns which had led to some organizations prohibiting standing orders of any kind in their nursing home facilities. In 2003 CMS has promulgated specific formal legal exception for orders for pneumococcal and influenza immunizations, thus facilitating their use. Further administrative and fiscal policies encouraging installation of standing orders and in otherwise enhancing provision of pneumococcal (and other) immunizations should be helpful in achieving the 2010 healthy people immunization goals of 90% of the over-65 year old population. Primary Funding Source: CMS, Washington State Department of Health • The Perception of Depression in Long Term Care Residents: A Qualitative Study Using Residential Journaling Holly Carroll, MSPH, Ken Watkins, Ph.D., Sandra Evans, Ph.D., Peg Hess, Ph.D. Presented by: Holly Carroll, MSPH, Graduate Assistant, Health Promotion Education and Behavior, University of South Carolina, 550 Harbor Cove Lane, Apartment 1200, Charleston, SC 29412; Tel: 843.364.5696; Fax: 843.876.1104; Email: carrolkh@musc.edu Research Objective: The study addresses the following research questions among residents of LTC: 1. What are the common themes regarding depression and its surrounding issues (i.e., loss, transition, grief, etc.)? 2. What are perceptions of depression as experienced by themselves and others? More specifically, how do they perceive their own emotional well-being, and how do they perceive other residents’ emotional well- being? 3. What resources are utilized as coping strategies? 4. To what extent is journal writing an effective method of gaining qualitative data in the older adult population? 5. What is the relationship between scores of a screening measure for depression (Geriatric Depression Scale, Brink et al., 1982), and the scores of residents’ perceptions of meaning of life (Meaning Survey, Pargament 1999)? 6. What are the relationships of the journal themes to depressive symptoms and perceptions of meaning of life? Study Design: This is a qualitative study that used the grounded theory to identify various domains regarding issues that surround symptoms of depression and long term care residents. The participants responded to statements in a 5-day journal, completed the Geriatric Depression Scale (GDS-15), and the Meaning Survey (MS), and then a follow up interview regarding their feelings about writing in the journal. Population Studied: Twenty-four residents in 6 assisted living facilities and 1 retirement community across three counties in South Carolina participated in a study to gain an understanding of older adults’ perception of depression in long term care (LTC) settings. Principal Findings: The GDS-15 indicated that 33.33% of the participants were depressed. An evaluation of the implications of spiritual meaning regarding the individual’s physical and mental health was measured using the Meaning Survey (MS). The mean score was 3.91 out of a 5 point Likert Scale (SD = .71) Presently there is no interpretation of the scale; however, this score indicates the degree that participants relied upon their spirituality in regards to their physical and mental health. Each participant’s journal consisted of 5- guided questions in relation to emotional, physical, and social health. The participants’ journals yielded six domains reflecting their perceptions of depression: long term care environment, participant emotional well being, overall residential emotional well being, coping resources used, journaling as a coping resource, and enjoyed activities. Follow-up interviews determined that journal writing was appropriate and beneficial for some LTC populations. Conclusions: It was found that for certain populations of older adults in LTC, journaling is an appropriate investigative tool that provides qualitative data for researchers. Implications for Policy, Delivery or Practice: Implications from the findings indicate that LTC facilities’ efforts should be channeled to increase the availability and quality of mental health services to residents. This should include regular residential depression screenings, as well as the standardization of mental health care services within LTC facilities. • Hospice Use among Blacks: Health Beliefs, Spirituality and Social Relationships as Predictive Factors Norma Conner, Ph.D. Presented by: Norma Conner, Ph.D., Visiting Assistant Professor, College of Nursing, University of South Florida, 12901 Bruce B. Downs Boulevard, MDC 22, Tampa, FL 33612; Tel: 813.974.3337; Fax: 813.974.5418; E-mail: nconner@hsc.usf.edu Research Objective: To examine the differential ability of demographic variables, beliefs and values aobut end-of-life, spirituality and social relationships to predict hospice use among Blacks. Study Design: Using a prospective, correlational design, components of The Behavioral Model of Health Services Use were tested to determine their ability to predict Hospice Use Among Blacks. Data were gathered from 104 Black men and women who were determined by their physicians to be appropriate for hospice level of care. Instruments included The Spiritual Involvement and Beliefs Scale (SIBS), Treatment Preferences Scale (TPS), and demographics and follow-up questionnaires. The instruments were completed while patients were at routine clinic appointments or were inpatients. Follow-up for determination of the patient’s hospice services use took place with the physicians four months after the initial data collection. Population Studied: Data were collected and analyzed from 104 Black men and women, recruited between November 2000 and November 2002, from six inpatient and outpatient settings in metropolitan New York and New Jersey hospitals. Principal Findings: Only 34% of the 104 subjects participated in hospice services and even many of those indicated a preference for the most aggressive life-sustaining treatments. Chi-square, sequential and stepwise logistic regressions revealed that the best predictive model consisted of: presence of a caregiver (Wald = 4.46, sig. .035; O.R. 9.67), religious affiliation (Wald = 4.96, sig. .026; O.R. 4.74), and gender (Wald = 3.98, sig. .046; O.R. 2.47). Together these factors predicted 13.7% to 19% of hospice use among Blacks. There was a ceiling effect on the SIBS and TPS. Socioeconomic variables did not vary enough within the sample to be properly tested in this study. Additional factors revealed during the study indicated concerns among potential hospice patients about their family caregiving responsibilities, safe storage of narcotics in a milieu of substance-abusing family members, the non-availability of narcotics at local pharmacies, and terminal prognosis at the time of diagnosis. Conclusions: The Behavioral Model of Health Services Use did not adequately predict hospice use among Blacks. Presence of a caregiver, religious affiliation, and gender together predicted only about 20% of Hospice Use among Blacks. Newer interpretations of the model may be more appropriate. The inclusion of stage of disease at diagnosis, and social role of the patient may impact end-of-life decision making as well. Implications for Policy, Delivery or Practice: The current study findings have ramifications for changing health policy, particularly the Medicare Hospice Benefit. Currently, not all hospices require the presence of an informal caregiver for a patient to participate in hospice. Yet among Blacks, in the absence of an informal caregiver, patients are less likely to choose hospice. The Medicare Hospice Benefit does not allow for a patient’s blood or legal relative to become the paid caregiver. Black caregivers may feel torn between a traditional value of caring for the family member contemplating hospice and their own need to earn a living. National policy that would provide a source of income to the informal caregiver electing to stay with the hospice patient may break down this barrier to hospice use among Blacks. • Policy Implications of Cost and Care Outcome Differences among Dual Eligibles Using Alternative Organizational Models for Long-Term Care James Cooney, Ph.D., Glenn Landers, M.B.A./MHA, Robert Curry, M.D./M.P.H., Jay Bae, Ph.D. Presented by: James Cooney, Ph.D., Professor of Health Administration, Robinson College of Business, Georgia State University, University Plaza, Atlanta, GA 30303; Tel: 404.842.5024; Fax: 404.842.5223; E-mail: jcooney@gsu.edu Research Objective: To assist in improving state Medicaid resource allocation decisions, identify federal and state policy implications of observed cost and care differences between traditional and waivered models of LTC delivery programs Study Design: Retrospective cohort study of long-term and concomitant acute care among Dual Eligible patients of Georgia’s nursing facilities (NF) and waivered home and community-based services (HCBS). Population Studied: The Study cohort encompassed all of the more than 23,000 individuals receiving long-term care in calendar year 1999 in either a Georgia HCBS or NF. All care services and costs for eighty-eight percent of those, verified as Dual Eligibles, were documented for twelve months after their inclusion in the cohort. Principal Findings: The alternative LTC organizational models of NFs and HCBSs do share patient populations with common socio-demographic characteristics (gender, raceethnicity and home of residence), these models also had statistically significant patient population differences affecting care needs and service costs: age; severity of illness as measured by Chronic Illness and Disability Payment and Diagnostic Cost Group systems; and, length of stay and mortality status at discharge. Across the alternative models, it was found that they all shared patterns of frequent and repetitive transfer of patients between LTC programs and hospitals; a large proportion of inter-institutional transfers were for Ambulatory Care Sensitive Conditions; and, all were found to have high cost of care in the last months of life. Over common time periods and across the alternative models, both public insurance programs do make statistically significant contributions to the overall (acute and long-term) care costs of the LTC program clients. Conclusions: The cohort patterns of long-term and concomitant, related care costs appear to be influenced more by parochial payment policies of the public insurers than potential efficiencies of the service delivery alternatives. Viewing only one insurer’s costs (e.g., Medicaid) for only one proportion of a beneficiary’s care (e.g., long-term care) will not provide a sufficiently complete picture of care or cost for resource allocation improvement decisions. Methodologically, an integrated Medicare and Medicaid database provides a more complete perspective on problem detection and system improvement. However, significant problems still exist for integration of the two databases especially when considering the waivered services component of Medicaid long-term care. Implications for Policy, Delivery or Practice: Given the growing aging population and continued separation of Medicare and Medicaid reimbursement policy, there needs to be a greater understanding and use of Inter-institutional planning for patient transfer and care management; For quality improvement and costs control purposes, study of policies facilitating frequent inter-institutional transfers and their outcomes needs greater emphasis and optimistically, greater operational changes; The consequences of HCBS cost-share requirements on care outcomes need more research emphasis and depending on those findings, appropriate adjustment of policy to assured appropriate cost-effective balance; Greater emphasis at both the federal and state(s) levels on more uniform, complete and continuous integration of Medicare and Medicaid long-term care related databases. Such efforts should also be extended to include enhanced options for wavered services research Primary Funding Source: Georgia Department of Community Health • Unmet Need for Help with Daily Activities among Persons 50 and Older with Disabilities Mary Jo Gibson, M.A. Presented by: Mary Jo Gibson, M.A., Senior Policy Advisor, Public Policy Institute, AARP, 601 E. Street, N.W., Washington, DC 20049; Tel: 202.434.3896; Fax: 202.434.6402; E-mail: mjgibson@aarp.org Research Objective: (1) To examine the characteristics of persons age 50 and older with disabilities who do and do not report unmet need for help with daily activities; (2) to determine which socioeconomic and other factors, such as severity or type of disability, are most closely associated with unmet need; (3) to identify adverse consequences associated with unmet need; (4) to identify the changes respondents report would cause a major improvement in their lives; and (5) to draw out the implications for policy and practice. Study Design: This study reports unpublished data from a survey on independent living and disability conducted by Harris Interactive for AARP in Sept. 2002 of 1,100 persons 50 and older with disabilities. The survey probed what respondents perceive as facilitating or impeding their independence and quality of life. We analyze these data by a number of variables, including a measure of unmet need for personal assistance services. The data are supplemented by a review of the literature on unmet need among persons with disabilities. Population Studied: Non-institutionalized adults age 50 and older with disabilities. Principal Findings: Almost one quarter (23%) of the sample reported needing more help than they receive now with daily activities. Persons with unmet needs were more likely to be age 50-64 than 65+; to have severe disabilities, to be black/African American; to have low incomes, to live alone, and to live in an urban area. A substantial majority (63%) of those reporting unmet need were receiving help with activities, predominantly from unpaid family members with whom they lived. Unmet need is associated with greater life dissatisfaction, postponing needed health care, having less control over key decisions, and being completely unable to work because of a disability. However, persons with unmet needs are no more pessimistic about their future than their counterparts who do not report unmet needs. The top three changes persons with unmet need say would cause a major improvement in the quality of their lives are: (1) more control over decisions about services and help needed; (2) someone known and trusted to help with daily activities; and (3) a way to pay for long-term services and equipment. Conclusions: The data paint a picture of both the strengths and vulnerabilities of persons age 50 and older with disabilities who have unmet needs, and help us understand what they need to live with dignity and independence. Findings will be compared with and discussed in the context of other published findings on unmet need among persons with disabilities, such as those from the National Health Interview Survey on Disability. Implications for Policy, Delivery or Practice: Among the many policy implications of the study are the need to: (1) protect and improve the Medicaid safety-net for home and community-based services; (2) encourage consumer-directed services for home and community-based services, including “cash and counseling” type programs; and (3) insure individuals against the high costs of long-term services and supports. Primary Funding Source: AARP Public Policy Institute • Monitoring and Improving the Quality of Long-Term Care: A Comparison of 19 Countries Manfred Huber, Ph.D., Weonjong Kim, Ph.D., Patrick Hennessy, M.Sc.Econ. Presented by: Manfred Huber, Ph.D., Head, Health Indicators, Health and Ageing, Social Policy Division, OECD, 2, rue André-Pascal, Paris, 75775; Tel: 331.4524.7633; Fax: 331.4430.6361; E-mail: manfred.huber@oecd.org Research Objective: To analyse in an international comparison different regulatory approaches to monitor and improve the quality of long-term care in different settings of care (nursing homes and other institutions, home care); to collect available evidence across countries about quality deficits; to examine ways to improve the available evidence base; to consider the implications of better quality for the cost of long-term care. Study Design: Based on a review of the literature, a questionnaire on quality regulation, and widespread concerns about quality deficits was developed and information was collected and analysed in co-operation with a network of national experts. This was done as part of a larger international study on policy trends in long-term care since 1990. Population Studied: Nineteen OECD countries (Australia, Austria, Canada, Germany, Hungary, Ireland, Japan, Korea, Luxembourg, Mexico, the Netherlands, New Zealand, Norway, Poland, Spain, Sweden, Switzerland, the United Kingdom and the United States). Principal Findings: The quality of long-term care services for older persons in many cases does not meet the expectations of the public, the users of services and their families, - more so for institutional care than for home care. Quality regulations for long-term care have been made more comprehensive and complex in recent years with a greater focus on outcomes and continuous quality improvement. Policy concerns from OECD countries link quality deficits to workforce shortages and structural quality. Major investments will be needed to improve quality in dimensions such as the average number of persons sharing rooms in institutions. This will exert cost pressure on long-term care services. Conclusions: The drive to raise quality standards in acute health care has been accompanied in many countries by governments taking a more active role in regulating and inspecting quality of long-term care services. This has two aims: to reduce the risk of receiving poor-quality care (including the risk of harmful care), and to raise average standards of service. Comprehensive publication of quality assessment could become a key to improving consumer protection and in fostering a climate of competition for quality. There is evidence that ad hoc approaches and fragmentation of quality initiatives may result in less-than optimal results with a strong case for co-operation on quality standards and measurement at the national and international levels. Implications for Policy, Delivery or Practice: Concerns about severe quality deficits have been important drivers of long-term care reforms in several countries. The study of quality regulations and outcomes in international comparisons, however, is a relatively new field of study. This study will provide administrations in countries with an overview and best practice examples of quality strategies as well as available evidence about their outcomes, to aid the development of national quality of care strategies. Primary Funding Source: OECD Health Project • The Effect of Medicaid Bed-Hold Policies on Hospital Length of Stay Mark Schleinitz, M.D., M.S., Orna Intrator, Ph.D., Ning Wu, M.D., M.S., Vincent Mor, Ph.D. Presented by: Orna Intrator, Ph.D., Assistant Professor (Research), Community Health, Brown University, Box G-ST2, Providence, RI 02912; Tel: 401.863.3579; Fax: 401.863.9219; E-mail: Orna_Intrator@Brown.edu Research Objective: In some states, Medicaid pays nursing homes a portion of the daily rate when a resident is hospitalized. Such payments reserve a bed in the nursing home, ideally to facilitate hospital discharge. The effect of bedhold policies on hospital length of stay is unknown. We evaluated the hypothesis that such a policy would reduce length of stay compared to no policy, but that a very generous policy may lengthen hospital stays. Study Design: We surveyed bed-hold policies from the 48 contiguous United States and quantified the generosity of these policies by calculating equivalent reimbursement days, or the number of full nursing home days that could be paid for with the maximum, per hospitalization, bed-hold payment in each state. As length of stay depends on whether patients are hospitalized, we used hierarchical modeling to determine the association between bed-hold policy and length of hospitalization. We first used logistic regression to determine the probability of stroke hospitalization for each patient controlling for their state of residence. We used analysis of variance to compare the average probability of stroke hospitalization for each state. We then used a general estimating equation to determine the effect of bed-hold equivalent reimbursement days on length of hospital stay, controlling for the probability of hospitalization. In each analytic stage we clustered at the facility level and controlled for demographic variables, comorbidities, and need for intensive care. Population Studied: Using the nursing home Minimum Data Set and Medicare claims data from 2000, we identified 6,710 non-fatal stroke hospitalizations occurring in long-stay residents of urban, free-standing nursing homes in the 48 contiguous states. After excluding the 12 states with less than 20 such hospitalizations, we further analyzed 6,614 stroke hospitalizations occurring in 490,000 residents from 36 states. Principal Findings: States varied in the generosity of bed-hold policies. Eleven states did not reimburse during hospitalizations, whereas the most generous state had no limit on bed-hold reimbursement. Generosity of bed-hold policy in equivalent reimbursement days did not correlate with the average per diem reimbursement rate. The probability of stroke hospitalization varied by state from a minimum of 0.9% to 2.6% (p<0.0001). Bed-hold policies that provided the average number of equivalent reimbursement days were associated with the shortest mean length of stay. Hospitalizations in states without bed-hold reimbursement were 0.10 days longer, (95% confidence interval 0.03-0.17) and those in states with the most generous policies were 0.33 days longer (0.20-0.45) than the shortest average length of stay. Conclusions: Whereas modest bed hold policies are associated with shorter length of stay than no such policy, our study implies that more generous policies are associated with prolonged hospitalization. Implications for Policy, Delivery or Practice: While the consequences of such policies must be explored further, more generous policies offer no incremental decrease in length of stay over modest policies, and may be associated with increased cost. Primary Funding Source: NIA • Comparing Medicaid Long-Term Care Waiver Programs Glenn M. Landers, M.B.A., M.H.A., James Cooney, Jr., Ph.D. Presented by: Glenn Landers, M.B.A., M.H.A., Senior Research Associate, Georgia Health Policy Center, Andrew Young School of Policy Studies, Georgia State University, 1 Park Place South, Atlanta, GA 30303; Tel: 404.463.9562; Fax: 404.651.3147; E-mail: glanders@gsu.edu Research Objective: Compare the costs and care outcomes of two Georgia Medicaid home and community based waiver programs for older adults. Study Design: Retrospective, cohort analysis using Medicare and Georgia Medicaid administrative claims data. Population Studied: 15,437 Georgians over age 64 who qualified for institutional placement in 1999 but received services from one of two Medicaid waiver programs (CCSP and SOURCE). CCSP is a traditional Medicaid home based waiver program serving as an alternative to institutional placement. SOURCE is a demonstration project that incorporates primary care physician oversight and enhanced case management. Principal Findings: *Patients were similar in age. *Patients were significantly different in race, gender, and residence. *CCSP clients were more dually eligible, and SOURCE clients were more Medicaid-only. *Both CCSP and SOURCE clients used significantly more Medicare home health prior to program admission. *Patients of both programs shared the top four principal diagnoses: essential hypertention, general symptoms, symptoms involving the respiratory system, and diabetes mellitus. *CCSP patients were slightly more likely to experience an inpatient hospital admission. *Patients of both programs used ER, outpatient, and therapy services similarly. *CCSP patients were more likely to experience three or more hospital stays over twelve months. *CCSP had significantly more patients who experienced at least one ambulatory care sensitive condition resulting in a hospital stay over twelve months. *At the end of twelve months, 10 percent of SOURCE patients and 8 percent of CCSP patients resided in nursing facilities. *Illness severity scores of SOURCE patients were slightly higher than CCSP patients. *Total monthly severity adjusted SOURCE costs were slightly higher than CCSP ($2,801 vs. $2,626), with total Medicare costs slightly higher for CCSP and total Medicaid costs slightly higher for SOURCE. Conclusions: *Higher rates of inpatient hospitalization for CCSP clients may be a function of CCSP's higher ratio of patients with dual eligibility. *Medicaid financed home health may substitute for Medicare home health once a patient enters a Medicaid waiver program. *Primary care physician oversight and enhanced case management may reduce ambulatory care sensitive conditions resulting in hospital admission and frequent hospitalizations overall when incorporated in a Medicaid waiver program for elder adults. Implications for Policy, Delivery or Practice: Introduction of primary care physician oversight and enhanced case management to Medicaid waiver programs for older adults may improve patient care at similar cost. The possible incentive to hospitalize based on reimbursement should be investigated further. Primary Funding Source: Georgia Department of Community Health • Do Non-Profit and For-Profit Hospices Behave Differently? Richard Lindrooth, Ph.D., Burton Weisbrod, Ph.D. Presented by: Richard Lindrooth, Ph.D., Assistant Professor, Department of Health Administration and Policy, MUSC, 19 Hagood Avenue, P.O. Box 250807, Charleston, SC 29425; Tel: 843.792.2192; Fax: 843.792.3152; E-mail: lindrorc@musc.edu Research Objective: To test whether non-profit and for-profit hospices respond differently to the financial incentives of Medicare payment policy. Study Design: : A hospice can maximize profit maximizing patient length of stay (LOS), because while daily costs are high several days after admission and several days before impending death, payment is fixed per day and does not vary be diagnosis. Thus by maximizing LOS, the length of interim period of relatively low costs (and higher reimbursement) is also maximized. We posit that a hospice can influence LOS (i.e. patient mix) in the following ways: it can offer attributes that are attractive to patients with a diagnosis associated with a long hospice LOS; market itself to physicians/ discharge planners who treat patients with diagnoses associated with long LOS; and encourage physicians to admit patients earlier in the progression of the disease than they otherwise would. We test these predictions using a dataset of all Medicare hospice admissions in 1993. We examine the shares of each diagnosis in for-profit and non-profit hospices, and test whether there are more ex-ante profitable patients at for-profit hospices. In addition, we test whether there are differences in LOS within each diagnosis. Population Studied: We use a dataset that consists of all Medicare reimbursed hospice admissions in 1993 from the Medicare SAF files. Hospice information was obtained from the MEDPAR files. We have information from a 720 look back window as well as a 2.5 year follow-up. Principal Findings: : Most of the variability in expected LOS is explained by diagnosis, and thus diagnosis is an easily observed patient trait that can be used to cream-skim. Of the diagnoses with relatively high LOS, 12/13 have higher shares at for-profit hospices 10 of these differences are significantly less than zero. Of the diagnoses with relatively low expected LOS, 8/14 have lower shares at for-profit hospices, but 3/14 also had a significantly higher share. The results of the analysis diagnosis are mixed and no significant pattern emerged. Conclusions: The results show that for-profit hospices maximized profit and did attract a higher share of patients with long expected LOS. The results within diagnosis reveal that for-profit hospices were not able to differentially draw relatively profitable patients within each diagnosis; rather they attracted patients with relatively profitable diagnoses. This is probably due to the fact that it is notoriously difficult to predict LOS within a given diagnosis. The results tie directly to the financial incentives inherent in Medicare reimbursement for hospice care. Implications for Policy, Delivery or Practice: Medicare reimbursement for hospices may cause access problems for patients with diagnoses with relatively short lengths of stay because they are unprofitable. We find that if Medicare would reimburse hospices relatively high upon admissions and again relatively high upon death, hospices will not have the incentive to attract certain types of patients. Such a reimbursement schedule would mirror costs more closely and eliminate the incentive to admit only those patients with a long expected LOS. Primary Funding Source: RWJF • The Home as a Site for Long Term Care Patricia McKeever, Ph.D., Mary Chipman, M.A., Helen Scott, M.Sc, Kathy Osterlund, M.A. Presented by: Patricia McKeever, Ph.D., Professor, Faculty of Nursing, University of Toronto, 50 Street George Street, Toronto, On, M5S 3H4; Tel: 416.978.2855; E-mail: p.mckeever@utoronto.ca Research Objective: This study was designed to illuminate the living and working conditions in households receiving long term care services. Study Design: A computer assisted telephone survey (CATI)of a random sample of home care clients who had received at least one publicly funded service at least once a week, for a minimum of eight weeks. Population Studied: Eight hundred and eleven (811) long term home care clients in an urban (n=232), rural (n=267) and remote (n=242) region in Ontario, Canada were interviewed in 2001/2002. Principal Findings: The median age of clients was 77 years and 75% were female. The majority of respondents had not completed high school. Almost half of clients were widowed, had income levels of $20,000 or less, and lived alone. As expected, older females were most likely to live alone. Home care clients who shared dwellings were most likely to live with someone close to their age; more than one third of clients who shared dwellings, lived with someone else with a disability. Clients were able to perform most basic activities of daily living, with the exception of bathing. However, only one quarter of clients were able to prepare meals, perform routine housekeeping and shop without help. Few clients were able to perform heavy housework or yard work, or travel outside of the neighborhood. There were significant differences between males and females in terms of the tasks for which they needed assistance. Family members were most likely to assist home care clients with most activities of daily living, with the exception of bathing, where almost 80% of clients relied on homemakers. Compared to the Canadian population, clients were more likely to live in subsidized housing, and had fewer rooms, bedrooms and bathrooms in their homes. As well, 47% of clients had difficulty meeting their housing costs. Furthermore, 16% and 33% of clients lived in homes that required major and minor repairs, respectively. This study found that clients who rent their homes, live alone or are female, are more likely to be in core housing need than other Canadians. More than 30% of clients required modification to their homes in order to adapt to their physical needs. Only approximately half of homes care clients had completed the required modifications; cost was sited as the main reason for not modifying their homes. Conclusions: These results demonstrate that most home care clients reside in homes that are less than optimal for both domestic life and paid and unpaid long term care provisions. Implications for Policy, Delivery or Practice: Since the homes of home care recipients function simultaneously as domestic dwellings and health care work sites, there needs to be a consideration of the interaction of clients’ needs, workers’ tasks and housing conditions. These results highlight a need to link housing policy to health and social services policies. Primary Funding Source: The Social Sciences and Humanities Research Council of Canada • The Effect of PACE on Use of Hospital and Nursing Home Services in the Long-Term Louise Meret-Hanke, M.A., MOD Presented by: Louise Meret-Hanke, M.A., MOD, Doctoral Candidate, Health Policy and Administration, The Pennsylvania State University, 116 Henderson Building, University Park, PA 16802; Tel: 814.865.1192; Fax: 814.863.2905; E-mail: lam330@psu.edu Research Objective: The purpose of this study is to evaluate the effect of the Program of All-inclusive Care for the Elderly (PACE), a managed long-term care program, on the use of hospital and nursing home services over the long-term. Study Design: The conceptual framework of the study is based on the premise that PACE’s capitated financing of acute and long-term care services and emphasis on preventative care is expected to reduce the use of hospital and nursing home care. The following hypotheses are based on prior research and literature on PACE and the use of hospital and nursing home services. H1: PACE enrollees will have lower use of hospital in-patient services than will members of a comparison group over a three-year follow-up period; H2: PACE enrollees will have lower use of nursing home services than will members of a comparison group over a three-year follow-up period. Use of hospital and nursing home services will be measured by admissions and total days. The study will draw from two secondary data sources, including the PACE public use data set, DataPACE, and the Medicare Current Beneficiaries Survey (MCBS), as well as other relevant data sets. The treatment group will be comprised of PACE enrollees selected from DataPACE. The comparison group will be constructed from a subset of the MCBS sample who have similar characteristics as the treatment group. Propensity score methodology will be used to select the comparison group sample in order to minimize differences between the treatment and comparison group. Two-part model estimation will be used to analyze the study outcomes. Population Studied: The population studied is communitydwelling, frail elderly individuals in the United States. The sample of the proposed study will consist of (1) PACE enrollees who enrolled between 1989 and 1998 and (2) MCBS subjects who were first interviewed between 1991 and 1999. Principal Findings: Currently in progress. Implications for Policy, Delivery or Practice: Providing longterm care to an aging population presents many challenges for policy makers and providers. Costs are rapidly rising and fragmentation and limited coordination jeopardize quality. The findings of this study will provide greater insight into the effect of managed long-term care on the utilization of high-cost services, such as inpatient and nursing home care. The study findings will also identify long-term effects of PACE on use of these services. Future policy and delivery These findings can inform both future policy and service delivery approaches. • Federal Mandates, Interstate Relations, and Other Determinants: Explaining State Policy Change in the Medicaid Nursing Facility Reimbursement Arena, 19801998 Edward Miller, Ph.D., M.P.A. Presented by: Edward Miller, Ph.D., M.P.A., Postdoctoral Fellow, Epidemiology and Public Health, Yale University School of Medicine, 60 College Street, New Haven, CT 065208034; Tel: 734.883.7449; Fax: 203.785.6287; E-mail: edward.a.miller@yale.edu Research Objective: Because nursing home spending consumes a larger portion of state budgets than almost any other category, reimbursement reform is a frequent budget reduction strategy pursued by state officials. As such, this study sought to explain why states choose the Medicaid nursing facility reimbursement policies that they do, and in the process, shed light on a critical policy area that has implications for many, not least of which include state and federal officials and nursing home residents and providers. Study Design: The determinants of state policy adoption arise from factors within each state’s external and internal environment, with external factors consisting of federal policy changes related to the Boren Amendment and prior adoptions by neighboring states, and internal factors consisting of a particular state’s economic and political circumstances. To evaluate the relative influence of the policy making determinants hypothesized I conducted a series of pooled cross-sectional time series analyses using event history, multinomial logit, and mixed modeling techniques. Focusing on state adoption of more cost containing options during 1980-1998, I predicted incremental changes in Medicaid nursing facility per diem rates and payments per recipient, and non-incremental changes in reimbursement methodologies, including adoption of fair rental methods for reimbursing capital, case mix methods for adjusting resident per diems, and general methodologies with stronger incentives for containing costs. Population Studied: The unit of analysis is the state-year. All analyses exclude Arizona, because of missing data and its unique Medicaid system, Hawaii and Alaska, because they do not share borders with neighboring states, and Nebraska, because it has a non-partisan, unicameral legislature. The analysis predicting use of older cost reports also excludes New York and Missouri because they were extreme outliers— neither rebased much during the time period studied. Principal Findings: Results show that the federal government influenced states' reimbursement policy choices, though not always as intended. While court decisions and other federal actions made it more difficult for states to reduce per diem rates, they also spurred the adoption of fair rental methods as states sought alternative ways of meeting their cost containment goals. By providing states with models of reimbursement, the federal government spurred case mix adoption as well. Although results provide evidence of regional diffusion in the context of the incremental outcomes, they provide no such evidence in relation to the nonincremental outcomes, the diffusion of which may have been more national than regional in orientation. Unemployment and medically needy programs were also positive significant predictors of incremental outcomes but not of nonincremental outcomes, while governing capacity was a negative significant predictor of incremental outcomes and a positive significant predictor of non-incremental outcomes. Conclusions: Future research should examine whether the influence of intergovernmental factors, including other states and the federal government, is moderated by internal state characteristics. Implications for Policy, Delivery or Practice: Given the pervasiveness of federal influence in the past, it is likely that states will take advantage of available discretion now that the Boren Amendment has been repealed and they face their worst fiscal conditions since World War II. Primary Funding Source: NIA • Rehabilitation Services Following the Implementation of the Nursing Home Prospective Payment System Patrick Murray, M.D., M.S., Neal Dawson, M.D., Thomas Love, Ph.D., Charles Thomas, BS, Randall Cebul, M.D. Presented by: Patrick Murray, M.D., M.S., Associate Professor, Center for Health Care Research and Policy, Case Western Reserve University, 2500 MetroHealth Drive, Cleveland, OH 44109; Tel: 216.778.3901; Fax: 216-778-3945; Email: pkmurray@metrohealth.org Research Objective: The balanced budget amendment of 1997 (BBA) required that all postacute services supported by Medicare be placed into a prospective payment system. A decline in utilization was the expected result. The purpose of this study was to describe the changes that have occurred in Ohio nursing homes related to the BBA, controlling for changes in patient characteristics. Study Design: Retrospective cohorts from two time periods were compared, controlling for selection bias using a predictive model derived and validated in the pre-BBA cohort. Population Studied: 9246 newly admitted Ohio NH patients from 1994-6 (pre-BBA) and 76,991 from 2000-1 (post-BBA). Principal Findings: More patients were provided therapy in the post BBA period (64.2% pre, 85.6% post, p<0.0001). The amount of therapy per patient was less (7.0 hrs./wk pre, 6.2 post, p<0.01). The greatest increase in rehabiltation service rate was is the two quintiles of patients least likely in the preBBA period to have received it. The greatest decline in the service amount was in the two quintiles most likely to receive rehabilitation. For profit NHs decreased therapy amount in the highest three quintiles. Not for profit NHs cut services only in the highest quintile. Conclusions: The BBA has not caused fewer patients to receive rehabilitation services, but rather decreased the amount of therapy provided. Proprietary status appears to significantly influence the response of NHs to fiscal change. Implications for Policy, Delivery or Practice: The clinical and social outcomes of these changes need to be evaluated. Based on prior work these changes may be shifting services to patients who are more likely to benefit from them. Primary Funding Source: AHRQ • Implementation and Evaluation of a Systems Approach for Quality Improvement in Nursing Homes Sue Nonemaker, R.N., M.S., Katharine Murphy, Ph.D., R.N., John Morris, Ph.D. Presented by: Sue Nonemaker, R.N., M.S., Senior Research Associate, Research and Training Institute, Hebrew Rehabilitation Center for Aged (HRCA), 1200 Centre Street, Boston, MA 02131; Tel: 617.235.5509; Fax: 617-363-8936; Email: nonemaker@mail.hrca.harvard.edu Research Objective: 1. To evaluate the effect of a systems approach for improving nursing home care in the following areas: ADL functional rehabilitation, pain, and depression. 2. To evaluate the feasibility of use and staffs' satisfaction with a Quality Improvement program utilizing "Best Practice" interventions. Study Design: Experimental Population Studied: Nursing home residents Principal Findings: We implemented "best practice" programs in the areas of ADL functional rehabilitation, pain, and depression in test facilities, and evaluated the impact of each program on resident outcomes using standard indicators of quality. Results of the project include the following: a 30-40 percent improvement in residents' capabilities in activities of daily living, such as eating and dressing, and a 22 percent improvement in depression management compared with a 15 percent decline experienced by facilities in a comparison group. Residents of facilities participating in the Pain intervention experienced less pain and exhibited marked declines in behavioral problems. Staff of participating nursing homes reported the programs were relatively easy to use and improved their job satisfaction. Conclusions: Use of systematic "Best Practice" interventions and a nurse educator model as part of a general Quality Improvement program improved resident outcomes in the areas of ADL functional rehabilitation, pain, and depression. Implications for Policy, Delivery or Practice: Quality of care for nursing home residents can be significantly improved through the systematic, consistent implementation of best practice protocols. States and CMS should consider introduction of a "best practice" initiative as a complement to traditional regulatory enforcement programs. Primary Funding Source: Pennsylvania Department of Health • Preventable Hospitalization as a Measure of Quality of Care in Nursing Homes Steven Pizer, Ph.D., Man Wang, M.S., Catherine Comstock, M.P.H. Presented by: Steven Pizer, Ph.D., Health Economist and Assistant Professor, Health Care Financing & Economics, Boston University and Department of Veterans Affairs, 200 Springs Road (Mail Stop 152), Bedford, MA 01730; Tel: 781.687.3088; Fax: 781.687.3106; E-mail: pizer@bu.edu Research Objective: To evaluate the rate of potentially preventable hospitalization as a measure of quality of care in nursing homes relative to established alternatives including those based on facility-reported data and those based on data from external sources. Study Design: We use the preventable hospitalization rate to study a new population (nursing home residents) and develop a new risk-adjustment model. We compare the performance of the preventable hospitalization rate with six established measures of nursing home quality of care. Population Studied: Secondary data were extracted from acute care hospitalization records and nursing home patient assessments for all residents in Veterans Health Administration nursing homes between October of 1997 and October of 2000. Principal Findings: Among seven measures, we find the preventable hospitalization rate to be the second most stable through time and the third most strongly related to staffing. Conclusions: The preventable hospitalization rate compares well with alternative measures of nursing home quality. Furthermore, because preventable hospitalization and mortality rates can be constructed from relatively objective data generated outside the nursing home, they provide valuable alternatives to measures based on facility-reported data. Implications for Policy, Delivery or Practice: Administrators of the federal nursing home quality initiative ought to reassess the list of quality measures currently available to the public and consider adding externally reported measures such as the preventable hospitalization rate. Primary Funding Source: VA • Nursing Homes’ Participation in the Subacute Care Market in the United States: The Role of Environmental and Organizational Factors Amir Qaseem, M.D., Ph.D., M.H.A., Robert WeechMaldonado, Ph.D., M.B.A. Presented by: Amir Qaseem, M.D., Ph.D., M.H.A., Clinical Epidemiologist & Research Manager, Scientific Policy, The American College of Physicians, 1000 Conestoga Road, B123, Bryn Mawr, PA 19010; Tel: 610.527.1718; E-mail: aqaseem@att.net Research Objective: Using resource dependence theory and Porter’s five forces of environmental threats model, this study examines the impact of environmental and organizational factors on nursing homes’ participation in the subacute care market. Study Design: Data sources include the Online Survey Certification of Automated Records (OSCAR), the Area Resource File (ARF), the Medicare managed care market penetration data files, and the Medicaid reimbursement surveys. Subacute care services are defined as nursing homes with specialty beds for hospice, dialysis, head trauma, Huntington disease, AIDS, and special rehabilitation care. A quasi-experimental interrupted time-series analysis using logistic (Glimmix) regression model is employed to test for change in nursing home participation in the subacute care market due to various environmental factors (Medicare prospective payment system [PPS], Medicaid reimbursement rates, Medicare hospital discharges, Medicare managed care market penetration, Herfindahl index, excess capacity, entry barrier, home health agencies, hospital based subacute care beds) and organizational characteristics (size, ownership, chain affiliation, occupancy rate). Population Studied: The sample for this study is all Medicare and Medicaid certified nursing homes in the United States during the period of 1993 to 2000. Principal Findings: Our analysis shows that the nursing homes offering subacute care decreased significantly since the implementation of Medicare PPS. Nursing homes located in markets with a higher Medicaid reimbursement rate were less likely to offer subacute care. Larger nursing homes and forprofit chain affiliated nursing homes were more likely to have subacute care units. In addition, nursing homes with a higher occupancy rate had a lower probability of offering subacute care services. Conclusions: Study findings suggest that the Balanced Budget Act (BBA) of 1997 did not have a significant impact in the number of nursing homes offering subacute care services. However, there has been a declining trend in the participation of nursing homes since the implementation of Medicare PPS for nursing home care. Results also suggest that nursing homes have responded strategically to the environmental demand for subacute care services. Nursing homes located in markets with higher Medicare managed care penetration and higher Medicare hospital discharges were more likely to offer subacute care services. Organizational factors, such as size and for-profit chain affiliation were important enablers in predicting nursing home subacute care participation. Implications for Policy, Delivery or Practice: A reduction in nursing home subacute care services may affect the continuity of care and coordination for patients discharged from hospital. Future research should also examine changes in nursing home subacute care supply on costs and quality of care for Medicare population. • Recruiting and Retaining Nursing Personnel in LongTerm Care Organizations: What are the Role of Financial and Workplace Incentives? Kent Rondeau, Ph.D. Presented by: Kent Rondeau, Ph.D., Associate Professor, Department of Public Health Sciences, University of Alberta, 13-126H Clinical Sciences Building, Edmonton, Alberta, T6M1W7; Tel: 780.492.8608; Fax: 780.492.0364; E-mail: kent.rondeau@ualberta.ca Research Objective: This study reports on the human resource management activities of long-term care organizations directed at attracting and retaining its nurses. Its objective is to assess the predominance and effectiveness of various financial and non-financial (workplace) strategies for recruiting and retaining scarce nursing personnel. Study Design: Strategies aimed at recruiting and retaining human resources are strongly conditioned by the rate of employee turnover, as well as by the relative supply of labor in the marketplace. When RN nursing labor is in short supply, health care organizations may have difficulty in filling their vacancies when employees leave or retire. Attracting and retaining qualified and competent nursing personnel is problematic for many long-term care organizations—some have difficulty in attracting staff, while others have difficulty in retaining them. This study investigates the differential impact of financial and non-financial (human resource) strategies on job vacancy (ostensibly a recruitment problem) and job turnover (primarily a retention issue) for nursing personnel in long-term care organizations. Population Studied: In 2003, a mail survey questionnaire was sent to the directors of nursing care in three hundred (300) long-term care organizations located in four provinces in Western Canada. The study database was randomly selected from all nursing homes. In total, 125 usable questionnaires were returned, and with 10 returned undeliverable or refused, produced a response rate of 43.1 percent. Principal Findings: : Categorical regression analysis was performed with nursing turnover and nursing job vacancy serving as the dependent variable. Four categories of nursing homes were arbitrarily constructed and assessed from our sample set: a) homes with high nursing personnel turnover and high job vacancies, b) homes with high nursing staff turnover but low nursing job vacancies, c) homes with low nursing staff turnover, but experiencing high nurse job vacancies, and d) homes with low turnover and few vacancies (our comparator group of homes). The variety of financial incentives and workplace (human resource) strategies were assessed with respect to their relative contributions in explaining the variation in nursing personnel turnover and nurse job vacancy rates. A number of control variables were also entered into our model, including institutional, workforce, and community characteristics. Conclusions: : Nursing personnel turnover and nursing job vacancies are differential indicators for predicting the effectiveness of recruitment and retention strategies for nursing home personnel. Financial incentives were generally found to have weaker or non-significant associations with nursing staff turnover and nurse job vacancy rates. However, certain workplace and human resource management programs are found to be better predictors of job turnover and job vacancy. Implications for Policy, Delivery or Practice: A national shortage of nursing personnel is affecting the ability of many health care organizations to deliver high quality nursing care. Financial incentives, although touted as critical for attracting and retaining nursing staff, may not be effective at reducing job turnover and job vacancy. Administrators of nursing homes should consider the adoption of more employeecentered programs to assist in attracting and retaining staff. • Risk Factors that Predict an Earlier Onset of Hospitalization in Home Health Care Robert Rosati, Ph.D., Liping Huang, M.A. Presented by: Robert Rosati, Ph.D., Director of Outcomes Analysis and Research, Center for Home Care Policy & Research, Visiting Nurse Service of New York, 5 Penn Plaza, 11th Floor, New York, NY 10001; Tel: 212.609.5776; Fax: 212.290.3756; E-mail: robert.rosati@vnsny.org Research Objective: Hospitalization is a significant quality indicator in home health care. The ability to predict the occurrence of hospitalization can help identify appropriate interventions and improve the management of patient care. The objective of this study was to examine the risk factors associated with hospitalization, especially the factors associated with an earlier onset of hospitalization. Study Design: Two types of analyses were conducted: logistic regression analysis was utilized to examine how sociodemographic, functional and clinical factors from the Outcomes Assessment Information Set (OASIS) at start of care predicted the likelihood of hospitalization, and using Cox’s proportional hazards regression model we assessed the relative risk of these same factors in explaining an earlier onset of hospitalization. In addition, a hazard function that quantifies the adjusted probability of hospitalization over time was developed. Population Studied: Data were selected from patients admitted to the adult (age >=18) acute care program of a home health care agency in a large urban area between January 2002 and August 2003, with length of stay less then 365 days. Among the final number of study observations (N=78,278), there were 18,890 (24.13%) that had one or more events of hospitalization recorded either by the administrative data or OASIS transfer/discharge assessments. Principal Findings: The results from the logistic analysis and hazard model were relatively consistent and both provided similar risk factors of hospitalization. However, there were some differences. The results showed that patients who had private insurance (HR=1.136, p<.0001) and whose caregivers were the spouse (HR=1.061, p<.0001) or other family members (HR=1.073, p<.0001) were more likely to have an earlier onset of hospitalization event, while these factors were not positively associated with the prediction of the overall risk factors of hospitalization (OR=0.754, 0.932 and 0.894, respectively). The result also illustrated that patients who had a medical regimen change 14 days prior to admission (HR=1.077, p=0.0059), lived with family (HR=1.043, p =.011) and whose primary diagnosis was ischemic heart diseases (HR=1.159, p<.0001) were more likely to have an earlier onset of hospitalization, while these factors were not significant in the logistic regression analysis. Nevertheless, patients whose primary diagnosis were CHF, HIV, cancer, pressure or stasis ulcer had approximately 1.5 to 2 times higher risks of an earlier onset hospitalization as well as the overall risk of hospitalization then others (p<.0001). Furthermore, an adjusted hazard function showed that the risk of hospitalization within 7 days of admission was relatively higher than other time periods. Conclusions: The factors of caregiver type, private insurance, certain types of diagnoses, and presence of ulcers are the leading components associated with earlier onset of hospitalizations. Further, the highest probability of the onset of hospitalization is within 7 days of admission. Hospitalizations may not be totally avoidable but there appears to be a clear set of factors on which home health care agencies need to focus when care begins. Implications for Policy, Delivery or Practice: Patient characteristics at start of care for those who receive services from home health care can be linked to the potential for hospitalization. Future research may show that focusing on these factors could reduce hospitalization rates. • Impact of State Quality Improvement Organizations (QIO) on Use of Standing Order Immunization Programs Among Long-Term Care Facilities in the U.S.: Results of the Immunization Standing Orders Project, 1999-2002 Abigail Shefer, M.D., Barbara Bardenheier, M.P.H., Dale Bratzler, DO, M.P.H., Linda McKibben, M.D., M.P.H., ABD, FACPM, Henry Roberts, Ph.D., Paul Stange Presented by: Abigail Shefer, M.D., Medical Epidemiologist, NIP, CDC, MS E-52, 1600 Clifton Road, Atlanta, GA 30333; Tel: 404.639.8233; Fax: 404.639.8615; E-mail: ashefer@cdc.gov Research Objective: Standing order programs (SOPs) are effective immunization-promoting interventions in which nurses or pharmacists are authorized to vaccinate by institution-approved protocol without a physician order or exam. During 1999-2002, a demonstration project was conducted in long-term care facilities (LTCFs) that involved promotion of SOPs for influenza and pneumococcal vaccination by the Centers for Medicaid and Medicare Services Quality Improvement Organizations (QIO). To evaluate impact of QIO promotion on adoption of SOPs in LTCFs and to describe characteristics of LTCFs associated with adoption of SOPs. Study Design: A controlled before-and-after study was conducted in 13 states (8 intervention and 5 control). Population Studied: Information about Medicare or Medicaid-certified LTCFs’ vaccination programs in each state were collected at baseline (June 1999) and post-intervention (March 2001). Intervention strategies employed by QIOs included state-wide conferences, distribution of educational materials, and on-site visits. Data from the completed surveys were linked to the On-line Survey and Certification Reporting System (OSCAR), an administrative database containing information on all Medicare or Medicaid licensed LTCFs in the country. Principal Findings: Of 3,861 LTCFs at baseline, 2,862 (74%) had complete pre and post survey and OSCAR data (n=1353 intervention; n=1509 control). In the intervention and control states at baseline, <10% of facilities used SOPs for influenza or pneumoccocal vaccination. Following the QIO intervention period, 110 (8.1%) additional LTCFs in the intervention states adopted influenza SOPs compared to 102 (6.7%) LTCFs in the control states (ns); for pneumococcal SOPs, the change was 7.8% in the intervention states compared to 5.3% in the control states (p<.05). In a multivariate logistic regression model, the characteristics significantly associated with adopting SOPs for influenza were lack of a consistent place in the medical record to document influenza vaccination and having a greater proportion of Medicaid-payer residents; and for adopting pneumococcal SOPs, the only significant factor was being an LTCF located in an intervention state. Conclusions: Despite few changes overall, state QIOs did appear to positively impact SOP adoption for pneumococcal vaccination. Factors other than the intervention appeared to play a more important role in decisions to adopt SOPs for influenza vaccination in this study. More research is needed to identify other strategies to further promote SOPs for vaccinating resident populations in LTCFs nationally. Implications for Policy, Delivery or Practice: More aggressive strategies such as state regulations may be needed to promote use of evidence-based interventions such as SOPs to improve vaccination of our elderly population. Primary Funding Source: CDC • Skilled Nursing Facility Stroke Rehabilitation and Discharge Home Walter Wodchis, Ph.D., Gary Teare, Ph.D., Gary Naglie, M.D., Susan Bronskill, Ph.D., Sudeep Gill, M.D., Michael Hillmer, B.Sc. Presented by: Walter Wodchis, Ph.D., Research Scientist, Research, Toronto Rehabilitation Institute, 130 Dunn Avenue, Toronto, Ontario, M6K 2R7; Tel: 416.597.3422 Ext. 2242; Fax: 416.530.2470; E-mail: wodchis.walter@torontorehab.on.ca Research Objective: To determine the relationship between Rehabilitation Therapy (RT) intensity and time to resident discharge for stroke residents discharged from hospital to Skilled Nursing Facilities (SNFs). Study Design: Retrospective cohort study. Hazard (time-toevent) regression analyses were stratified by expected outcome. Multivariate analyses and propensity score adjustment techniques were also employed to adjust for nonrandom treatment assignment. Population Studied: All SNF residents admitted to SNFs in Ohio and Michigan, U.S.A. and Ontario, Canada during 1998 and 1999 (N=23,824 admissions). Principal Findings: RT was given to over 95% of residents for whom discharge was expected within 90 days to over 60% of residents for whom discharge was uncertain or not expected. RT increased the relative risk (RR) of discharge for all groups except residents with an expected discharge within 30 days (minimum RR= 1.20, maximum RR=1.78). A dose-response relationship was strongest for residents with either an uncertain discharge prognosis or no discharge expected. The relative risk for discharge home was 1.52 for residents with 'no discharge expected' but who still received the highest levels of RT. Conclusions: RT leads to faster discharges home for stroke patients receiving rehabilitation in SNFs. However, increasingly higher RT intensity does not provide additional benefits to all residents. Implications for Policy, Delivery or Practice: Post-acute residents with an uncertain prognosis are an important target population for intensive RT. • The Influence of Patient, Healthcare Provider, and Organization Characteristics on the Use of Home Hospice Care versus Traditional Home Care Prior to Death Ying Xue, M.S.N., Paula Milone-Nuzzo, Ph.D. Presented by: Ying Xue, M.S.N., Doctoral Student, School of Nursing, Yale University, 100 Church Street South, P.O. Box 9740, New Haven, CT 06536; Tel: 203.624.6470; Fax: 203.624.6470; E-mail: ying.xue@yale.edu Research Objective: Most elders express a preference for receiving terminal care at home. Patients can receive terminal care at home either from traditional home care (THC) or from home hospice care (HHC) in the U.S.. Studies indicated that HHC can provide quality care for dying patient and has the potential to be cost-effective. In response to the increase of the elder population and the escalation of healthcare costs, this study was done to identify strategies to foster appropriate use of HHC and THC prior to death among the elderly population. Study Design: The study employed a cross-sectional research design using SUDAAN software to perform logistic regression with variables hierarchically entered to identify patient, healthcare provider, and organization characteristics on the use of HHC versus THC prior to death. The data are drawn from the revised 2000 National Home and Hospice Care Survey dataset. Discharge data are used because these data represent a complete episode of care. Discharges refer to those patients who were discharged from care by the home health agency or hospice during a designated month between October 1999 and September 2000 that was randomly selected for each agency. Population Studied: A sample of discharged patients who are at least 65 years old and received either HHC or THC before discharge, for whom death was the reason for discharge. Principal Findings: Preliminary analysis revealed that there were 127,361 discharges using THC and 242,366 using HHC prior to death among the elderly population. Analysis of patient, healthcare provider and organization characteristics is not completed as yet. Final results will be completed in March and will be available at the time of the conference. Conclusions: Final results and conclusions will be completed in March and will be available at the time of the conference. Implications for Policy, Delivery or Practice: This study will be important for health care administrators, health care providers, and policy makers who are in the business of managing terminal care in the home. As the key variables associated with the use of HHC versus THC are described, the opportunity to design home care programs that most appropriately target the needs of the community can be developed. From a policy perspective, knowing the factors that are significantly associated with the use of HHC and THC prior to death, policymakers will have the data needed to influence the utilization patterns for improvement in the cost and quality of care. • An Examination of the Nursing Homes Profitability Post the Balance Budget Act (BBA) Mustafa Younis, Dr.PH., M.A., M.B.A. Presented by: Mustafa Younis, Dr.PH., M.A., M.B.A., Assistant Professor, Healthcare Administration, Jackson State University, 350 W. Woodrow Wilson Avenue, Jackson, MS 39213; E-mail: younis68@hotmail.com Research Objective: To describe and examine the variation of profitability between for-profit and non-profit nursing homes. Policy implications due to these variations would be in form of the level of service for the elderly who depend on Medicare and Medicaid program. Study Design: Descriptive statistic and Regression analysis to examine the variables that influence nursing homes profitability. Population Studied: The research used the Nursing Homes Minimum Data Set (MDS)for the year 2000. (over 5000 nursing homes facilities) Principal Findings: Despite the Balance Budget Act, Nursing homes showed a healthy profit margin. For-Profit Nursing Homes had a superior performance in comparison to the Non-Profit counter part. Unlike the hospitals market, nursing homes market is characterized by excess demand and is dominated by For Profit entity. Conclusions: The For-Profit facilities were able to adjust to new regulations faster than Not-For-Profit nursing homes. Another reason for the variations that most nursing homes did not have to comply with the BBA and BBRA immediately. A further study with more recent data when it become available is recommended. Implications for Policy, Delivery or Practice: The importance of the study stems from the debate over the effect of ownership on health care services. If the type of ownership has no effect on the performance and the services provided by the nursing homes, then society might be better off by eliminating charitable donations and the tax-exempt status of N-P nursing homes. The market of skilled nursing facilities due to the aging of the population. The Service providers (SNF) and the insurers (Medicare, Medicaid, and Private insurance) have to come with a payment mechanism that ensures solvency and profitability of the nursing homes without sacrificing quality and access to the services need by the • Institutional Factors Influencing Nursing Home Quality Ning Zhang, Ph.D., M.D., Thomas Wan, Ph.D. Presented by: Ning Zhang, Ph.D., M.D., Assistant Professor, Health Administration, University of Central Florida, Doctoral Program in Public Affairs/College of Health and Public Affairs/UCF/PO Box 162200, Orlando, FL 32816; Tel: 407.823.3344; Fax: 407.823.4895; E-mail: nizhang@mail.ucf.edu Research Objective: The objective of this study is to identify the relative and interaction effects of institutional mechanisms on the isomorphism of the quality of nursing homes in United States and to examine the stability of nursing homes’ quality as measured by deficiencies in 1997 and 2001, using two-level modeling. Study Design: A longitudinal panel design was employed. Data obtained from the On-line Survey Certification and Reporting System (OSCAR) from 1997 and 2001 were the major source for the study. A balance design was formulated with 22 homes randomly selected from each of the states. Population Studied: Using a multi-level design, a sample of 1,056 homes from 48 states was selected. Multi-level analysis examined the predictor variables at both facility and state levels. Principal Findings: There were three major findings in this study. First, nursing home quality is strongly influenced by coercive pressures. Nursing home quality is substantially influenced by the Medicaid reimbursement rate, the demand for nursing home care, the stringency of the Certificate-ofNeed, and the percentage of Medicare patients in nursing homes. The results of this study indicate that regulatory control plays an important role in improving nursing home quality. Higher Medicaid reimbursement rate was found to be positively related to better nursing home quality. Second, the number of hours that registered nurses work per patient per day (RNPRD) is another strong predictor of nursing home quality, with more RNPRD hours leading to better quality. Third, the interaction term between the coercive mechanism and the normative mechanism, as represented by the coercive variable DEMAND and the normative variable RNPRD, was found to be positively associated with nursing home quality. Conclusions: Improvement of nursing home quality depends on governmental, regulatory and societal forces. These external coercive mechanisms shape the change of nursing home practice in a socially desired direction, but not necessarily in a market-desired direction if the two directions are not the same. This analysis shows that, regulation and the government’s role cannot be weakened. On the contrary, federal and state governments should be more active in monitoring and improving nursing home quality. Furthermore, the federal and state governments should increase state Medicaid reimbursement rates, and maintain CON and moratorium programs. A quality-based reimbursement scheme should be developed to provide financial incentives to deliver better quality of nursing home care. Implications for Policy, Delivery or Practice: A quality-based incentive should be devised when the federal and state governments consider designing a new payment system, so that nursing homes will be paid for delivering better quality. Strengthening coercive mechanisms and increasing nurse staffing are imperative. Linking financial rewards with demonstrated quality would reward the best nursing facilities and encourage others to improve. Invited Papers Long-Term Care Financing: Private Sector Solutions & International Comparisons Chair: Vincent Mor, Ph.D. Monday, June 7 • 4:00 p.m.-5:30 p.m. • Panelists: Manfred Huber, Organization for Economics Cooperation and Development (OECD); Jeanne Lambrew, George Washington University; Christopher Murtaugh, Visiting Nurse Service of New York; Judith Feder, Georgetown University (no abstracts provided)