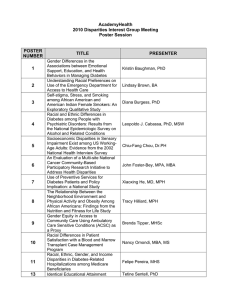
Disparities
advertisement

Disparities Call for Papers Disparities & the Care of Children Chair: Anne Beal, M.D., M.P.H. Monday, June 7 • 8:30 a.m.-10:00 a.m. • Disparities for Latino Children in Receipt of Timely Medical Care David Brousseau, M.D., M.S., Jennifer Yauck, M.S., Raymond Hoffmann, Ph.D., Ann Nattinger, M.D., M.P.H., Glenn Flores, M.D. Presented by: David Brousseau, M.D., M.S., Assistant Professor, Pediatrics, Medical College of Wisconsin, 9000 W Wisconsin Avenue, Milwaukee, WI 53226; Tel: 414.266.2625; Fax: 414.266.2635; E-mail: dbrousse@mail.mcw.edu Research Objective: Latinos (Ls) are now the largest minority population in the US, but little is known about whether L children experience disparities in their ability to access healthcare in a timely fashion. Our objective was to compare the parent-reported ability of children to get timely care among L, White (W) and African-American (AA) children. Study Design: Cross-sectional analysis of the 2000 Medical Expenditure Panel Survey Population Studied: We analyzed data from the 2000 Medical Expenditure Panel Survey for children 0-17 years old with a usual source of care. Data were weighted to provide national population based estimates. Parental survey responses were used to evaluate the timeliness of care children receive in four areas: 1) timely routine care from a provider, 2) timely illness or injury care from an office, clinic or ED, 3) phone help from a provider, and 4) brief wait time with appointment. The percent of children always receiving timely care was compared between L and W and AA children. Multiple logistic regression, with Ls as the referent group to allow comparisons to both Ws and AAs, was done to determine the odds of always receiving timely care, adjusting for known confounders. The regression was then repeated adding the effect of interview language. Principal Findings: 4,120 children, weighted to represent 47 million children, were included in the analysis. The average age was 8 years, 51% were male, 24% were covered by Medicaid. 30% were Ls, 53% Ws and 17% AAs. In univariate analysis, L children were significantly (p<0.005) less likely to always receive timely care compared to Ws and AAs respectively in 3 areas: routine care 44% vs. 54% and 54%; phone help 40% vs. 49% and 47%; and brief wait time 36% vs. 55% and 44%, but not illness care 61% vs. 66% and 64%. Multivariate regression revealed increased odds (OR, 95% CI), compared to Ls, for Ws and AAs, in the same 3 areas: routine care: W (1.28,1.04-1.56), AA (1.48, 1.15-1.98); phone help: W (1.37, 1.16-1.62), AA (1.29, 1.05-1.58); brief wait time: W (1.96, 1.66-2.32), AA (1.43, 1.16-1.76). Adding interview language to the regression decreased the differences between groups: routine care: W (1.19, 0.95-1.50), AA (1.38, 1.04-1.82); phone help: W (1.28, 1.07-1.54), AA (1.20, 0.96-1.50); brief wait times: W (1.65, 1.38-1.99), AA (1.19, 0.95-1.49). Conclusions: Latino children experience marked disparities in obtaining timely medical care. These differences are only partially explained by language differences. Implications for Policy, Delivery or Practice: Improvements are needed in the delivery and efficiency of medical care for Latino children. Primary Funding Source: Ambulatory Pediatric Association • Children at Risk of Receiving Sub-standard Asthma Care Findings from a Nationally Representative Sample Alex Chen, M.D., MSHS, Jose Escarce, M.D., Ph.D., Ronald Ferdman, M.D., M.Ed. Presented by: Alex Chen, M.D., MSHS, Assistant Professor, Pediatrics, Childrens Hospital Los Angeles, 4650 Sunset Boulevard, MS# 30, Los Angeles, CA 90027; Tel: 323.671.7620; E-mail: alexchen_y@yahoo.com Research Objective: To examine socioeconomic and demographic factors associated with sub-standard quality of care in children with asthma. Study Design: This is a secondary data analysis of the Medical Expenditure Panel Survey (MEPS) using the Household Full Year File and the Prescribed Medicines Event File from 1996-2000. All children 5-17 years of age with asthma were identified using ICD-9 codes. The Event File for those children was linked to the Household File. The name, formulation, and quantity of prescribed medicine filled during the year for those children were counted and categorized as inhaled short-acting beta2 agonists (SAB), inhaled corticosteroids, inhaled cromolyn, oral corticosteroids, longacting beta2 agonists, leukotriene modifiers, and theophylline. Guidelines for the Diagnosis and Management of Asthma (NHLBI expert panel reports) were used to establish four criteria, based on medication usage, for sub-standard asthma care: 1) >= 4 months supply of SAB filled per year without any primary controller (defined as inhaled corticosteroids, inhaled cromolyn, leukotriene modifiers) in the same year; 2) >= 2 Emergency Department visits per year without a primary controller prescription; 3) >= 1 hospital admissions per year without a primary controller prescription; and 4) >= 2 courses of oral corticosteroids per year without a primary controller prescription. Univariate and multivariate logistic regression analyses were conducted using person-year as the unit of analysis. All analyses were weighted to account for sample design and survey nonresponse. Standard errors were adjusted for clustering at the person level. Population Studied: A nationally representative sample of children 5-17 years of age with asthma who are also eligible for any one of the four sub-standard care criteria (for example, a child is eligible for criteria 1 if he/she had >= 4 months supply of SAB during the year; a child fulfills criteria 1 if he/she also did not have a prescription for any primary controller). Principal Findings: Among U.S. children 5-17 years of age with asthma, 21.4 % received >= 4 months supply of SAB during the year. Among those that received >= 4 months supply of SAB, 52.8 % did not receive a prescription for any primary controller that year. Among children eligible for any one of the four criteria, children of mothers with high school diploma or higher were less likely to have sub-standard care compared to children of mothers with lower education (O.R.=0.32, p=0.02), adjusted for race, age, family income, health status, and insurance status. Having Medicaid or SCHIP was also protective against sub-standard asthma care (O.R.=0.23, p=0.06). Conclusions: A substantial percentage of children in the U.S. received sub-standard quality of care for asthma as assessed by medication usage and visit patterns. Children of mothers who have not completed high school were at significantly increased risk for sub-standard care, Medicaid and SCHIP reduced the risk of sub-standard care. Implications for Policy, Delivery or Practice: Efforts should continue to enroll children in SCHIP or Medicaid. Additional resources may need to be directed toward children of mothers with low educational backgrounds. Health Plans can adopt standards from practice guidelines to identify patients receiving sub-standard care using pharmacy and/or claims data. Primary Funding Source: Intramural • Does Disadvantage Start at Home? Racial and Ethnic Disparities in Early Childhood Home Routines, Safety, and Educational Practices/Resources Glenn Flores, M.D., Lynn Olson, Ph.D, Sandra Tomany, M.S. Presented by: Glenn Flores, M.D., Director, Community Outcomes; Associate Director, Center for the Advancement of Urban Children, Pediatrics, Medical College of Wisconsin/Children's Hospital of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226; Tel: 414.456.4454; Fax: 414.456.6385; E-mail: gflores@mail.mcw.edu Research Objective: Little is known about whether racial/ethnic differences exist in the home environment in family activities, safety, and educational opportunities known to impact healthy development, behavior, and future school success in young children. The study goal was to examine whether there are racial/ethnic disparities in early childhood home routines, safety, and educational practices/resources. Study Design: The 2000 National Survey of Early Childhood Health is a telephone survey of a national random sample of responsible parents/guardians of 2,608 children aged 4 to 35 months. Differences in selected shared family activities, safety practices, and educational practices and resources were examined for non-Latino white (W), non-Latino AfricanAmerican (AA), and Latino (L) children (sample sizes were inadequate to analyze other racial/ethnic groups). STATA was used for statistical analyses, national estimates, and to obtain odds ratios (ORs) and 95% confidence intervals (CIs) by multivariate analyses adjusting for insurance coverage, health status, family income, age, parental education, and language of interview. Population Studied: A national random sample from all 50 states of parents/guardians of 2,608 children aged 4 to 35 months. Principal Findings: W children are significantly more likely than minority children to have their meals at the same time each day (80% vs. 70% for Ls and 65% for AAs; P<0.001) and go to bed at the same time each day (76% vs. 69% for Ls and 65% for AAs; P<0.001). Minority children are significantly more likely to never eat lunch or dinner together with their family or to do so only 1-2 days/week (AAs, 26%; Ls, 26%; Ws, 10%; P<0.001). Minority parents are significantly more likely to want to spend a lot more time with their child (AAs, 29%; Ls, 29%; Ws, 20%; P<0.001). Minority parents are significantly less likely to install baby gates (AAs, 62%; Ls, 67%; Ws, 82%; P<0.001) and put safety latches/locks on cabinets (AAs, 73%; Ls, 78%; Ws, 85%), and AA parents are less likely to turn down hot water settings (45% vs. 56% in Ws and 60% in Ls; P<0.001). There are high rates (> 90%) of putting plugs in electrical outlets that do not differ by race/ethnicity, and minorities are more likely to put padding on hard/sharp surfaces (AAs, 58%; Ls, 58%; Ws, 46%; P<0.001). Minority parents are significantly less likely to read every day to their child (Ls, 29%; AAs, 46%; Ws, 61%; P<0.001), Latino parents are more likely to never read to their child (15% vs. 5% for AAs and 3% in Ws; P<0.001) and minority households have a lower mean number of children’s books (Ls, 33; AAs, 41; Ws, 83; P<0.001). AA children average a significantly greater number of hours watching TV daily (2.4 vs. 1.6 in Ws and 1.6 in Ls), but AA parents are most likely to play music and sing with their child (84% vs. 76% in Ws and 65% in Ls; P<0.001). Disparities persisting in multivariate analyses included: AA children not having regular meal times (OR, 1.8; 95% CI, 1.2-2.6), eating lunch or dinner together less than every day (OR, 2.0; 95% CI, 1.4-2.8), and watching an average of about 1 more hour of TV daily; AA parents wanting to spend a lot more time with their children (OR, 1.6; 95% CI, 1.1-2.4), not turning down hot water settings (OR, 1.5; 95% CI, 1.1-2.1), and not installing cabinet safety locks (OR, 1.8; 95% CI, 1.2-2.7); minority parents having about twice the odds of not reading to their child daily (Ls: OR, 1.9; 95% CI, 1.3-2.6; AAs: OR, 1.7; 95% CI, 1.2-2.4) and of not putting up baby gates (AAs: OR, 2.4; 95% CI, 1.6-3.5; Ls: OR, 1.8; 95% CI, 1.2-2.7); and minority homes having significantly fewer children’s books (adjusted mean number of books per household: AAs: 32 [95% CI, -42, -22]; Ls: -23 [95% CI, -36, -12]). Language of interview adjustment eliminated L disparities for never reading to children and mitigated the number of children’s books at home. In multivariate analyses, children whose parents completed surveys in Spanish also experienced multiple disparities (compared with children completing English surveys), including quadruple the odds of never being read to by their parents, almost triple the odds of the parents not putting stoppers or plugs in electrical outlets, an average of 33 fewer children’s books in the household, and increased odds of irregular meal times. Conclusions: Young minority children experience multiple disparities in home routines, safety, and educational practices and resources that have the potential to impede their healthy development, behavior, personal safety, and future school success. The greatest number and severity of disparities generally occur in African-American children, and daily reading and children’s books in the home are alarmingly uncommon for Latino children. Children of parents completing surveys in Spanish also experience multiple disparities. Implications for Policy, Delivery or Practice: The study findings suggest that disparities in early childhood home routines, safety, and educational practices and resources for minority children and those whose parents complete surveys in Spanish might be reduced or eliminated through targeted family education and interventions by pediatric providers. Primary Funding Source: RWJF, Agency for Healthcare Research and Quality • Unequal Treatment for Young Children? Racial and Ethnic Disparities in Early Childhood Health and Healthcare Glenn Flores, M.D., Lynn Olson, Ph.D., Sandra Tomany, M.S. Presented by: Glenn Flores, M.D., Director, Community Outcomes; Associate Director, Center for the Advancement of Urban Children, Pediatrics, Medical College of Wisconsin/Children's Hospital of Wisconsin, 8701 Watertown Plank Road, Milwaukee, WI 53226; Tel: 414.456.4454; Fax: 414.456.6385; E-mail: gflores@mail.mcw.edu Research Objective: Racial/ethnic disparities in healthcare recently have received much national attention, but few studies have focused on disparities in children, especially in the youngest age groups. The study aim was to examine racial/ethnic disparities in early childhood health and healthcare using a nationally representative sample. Study Design: The 2000 National Survey of Early Childhood Health is a telephone survey of a national random sample of parents/guardians of 2,608 children aged 4 to 35 months. Differences in selected health and healthcare measures were examined for non-Latino white (W), non-Latino AfricanAmerican (AA), and Latino (L) children (sample sizes were inadequate to analyze other racial/ethnic groups). STATA was used for statistical analyses, national estimates, and to obtain odds ratios (ORs) and 95% confidence intervals (CIs) by multivariate analyses adjusting for insurance coverage, health status, family income, age, parental education, and language of interview. Population Studied: A national random sample from all 50 states of parents/guardians of 2,608 children aged 4 to 35 months. Principal Findings: L and AA children are significantly less likely than W children to be in excellent or very good health (72% vs. 79% vs. 90%, respectively; P<.001), but more likely to have been uninsured at some time in the past year (31% vs. 18% vs. 9%; P<.001), to have no regular healthcare provider, and to have been assigned their provider when they have one. L parents are significantly more likely than AA and W parents to report their child’s provider did not spend enough time with the child during the visit. Only 60% of L parents and 77% of AA parents are very likely to recommend their child’s provider to others, compared to 84% of W parents (P<.001). Compared with W parents, minority parents are more likely to report their child’s regular provider never or only sometimes understands how the parent prefers to raise the child (W: 35%; AA: 45%; L: 46%; P<.001) and never/only sometimes respects that the parent is the expert on the child. L parents were more likely than others to report that the provider never/only sometimes understands the specific needs of their child (L: 30%; AA: 15%; W: 10%; P<.001). Providers significantly more often asked minority parents about community violence, difficulty paying for children’s needs, and household members smoking, drinking or using drugs, but also significantly more often asked minority parents about car seat use, childcare arrangements, and reading to children. Minority parents averaged fewer phone calls to their child’s doctor in the past year (L: 2.0; AA: 3.1; W: 4.3; P<.001), and minority children were more likely to have made an emergency department (ED) visit. Pediatric providers significantly less often referred minority children to specialists, at 22% for Ws, 17% for AAs, and 11% for Ls (P<.001). In multivariate analyses, some disparities disappeared for minority children, including having an assigned provider, and for L children, having no regular provider, providers not spending enough time with the child, and a lower likelihood of excellent/very good health. Disparities persisting in multivariate analysis included L parents being more likely to not recommend their child’s provider (OR, 1.9; 95% CI, 1.1-3.3) and to report providers never/only sometimes understand the child’s needs (OR, 2.3; 95% CI, 1.4-3.6); AA children not being in excellent/very good health (OR, 2.1; 95% CI, 1.3-3.3), being more likely to have made ED visits in the past year (OR, 1.5; 95% CI, 1.1-2.2) and having providers who more often asked about household smoking, trouble paying for the child’s needs, spouse/partner support of parenting, childcare arrangements, and the importance of reading to children; minority children being more likely to be uninsured (L: OR, 2.3; 95% CI, 1.4-3.8; AA: OR, 1.7, 95% CI 1.02–2.9), minority parents reporting providers never/only sometimes understand parents’ childrearing preferences, minorities being asked about community violence and household drinking and drug use, minority parents making fewer calls to their child’s doctor, and minority children being least likely to be referred to specialists (AA: OR, 1.8; 95% CI, 1.1-2.9; L: OR, 1.7; 95% CI, 1.1-2.8). In multivariate analyses, children whose parents completed surveys in Spanish also experience multiple disparities, including increased odds of being uninsured, poorer health status, not receiving care in a private/group practice, providers never/only sometimes understanding the child’s specific needs, discussion of community violence and household alcohol and drug use, fewer calls to the child’s doctor, and not being referred to specialists. Conclusions: Certain health disparities for minority children can be accounted for by prevalence differences in income, insurance coverage, and language of interview. But compared to white children, minority children experience multiple disparities in health status, lack of insurance coverage, the content of pediatric visits, parents feeling understood by pediatric providers, parental satisfaction with care, phone calls to providers, and referrals to specialty care. Children whose parents complete surveys in Spanish also experienced multiple disparities in health and healthcare. Implications for Policy, Delivery or Practice: The U.S. is experiencing a demographic surge in minority children, particularly among the youngest age groups; by 2030, minorities will outnumber non-Hispanic whites by 1.1 million among children 0-5 years old. As the number and proportion of minority U.S. children grow, racial/ethnic disparities in early childhood health will take on even greater importance as pediatric providers care for increasingly diverse populations. Elimination of such inequities may require more research on possible root causes of disparities, additional education for healthcare providers, and ongoing monitoring for disparities by health plans, the State Children’s Health Insurance Program, Medicaid, and other healthcare systems. Primary Funding Source: RWJF, Agency for Healthcare Research and Quality • Mortality Among Very Low Birthweight Infants in Hospitals Serving Minority Populations Leo Morales, M.D., Ph.D., Douglas Staiger, Ph.D., Jeffery Horbar, M.D., Joseph Carpenter, M.A., Michael Kenny, M.A., Jeannette Rogowski, Ph.D. Presented by: Leo Morales, M.D., Ph.D., Assistant Professor, Medicine, UCLA, 911 Broxton Avenue, Los Angeles, CA 90024; Tel: 310.794.2296; E-mail: morales@rand.org Research Objective: It is not known whether very low birth weight (VLBW) infants treated in minority-serving hospitals receive the same quality of care as those treated in other hospitals. The purpose of this study is to investigate whether neonatal mortality is higher for infants treated in minorityserving hospitals compared to other hospitals. Study Design: This study was set in three hundred thirty two neonatal intensive care units in the United States participating in the Vermont Oxford Network. Medical records were reviewed and linked to secondary data sources including the American Hospital Association’s survey of hospitals, the area resource file and the 1990 US Census. The main outcome investigated was neonatal mortality, defined as death prior to discharge home during the first 28 days after live birth. Detailed risk-adjustment was performed using patient characteristics available immediately after birth. Population Studied: The study sample consisted of 74, 050 black and white VLBW infants (501 grams to 1500 grams) treated in participating hospitals from 1995 to 2000. Principal Findings: Overall, 57% of VLBW black infants and 17% of VLBW white infants were treated in minority-serving hospitals (defined as hospitals where more than 35% of VLBW infants treated in the NICU were black). Risk-adjusted neonatal mortality was higher for both black and white infants in minority-serving hospitals relative to hospitals where less than 15% of the VLBW infants were black (whites: OR=1.30, 95% CI 1.09-1.56; blacks: OR=1.29, 95% CI 1.01=1.64; pooled: OR=1.28, 95% CI 1.10-1.50). Higher mortality in minorityserving hospitals could not be explained by other factors including financial factors, urban versus rural location, patient volume, level of care in the NICU, or the use of surfactants and antenatal steroids. Black neonatal mortality among VLBW infants would have been reduced by 8.5% if black infants had been treated in minority-serving hospitals in the same proportions as white infants. Conclusions: VLBW infants treated in minority-serving hospitals have higher mortality than infants treated in other hospitals. Because VLBW black infants are disproportionately treated in minority-serving hospitals, higher neonatal mortality rates at minority-serving hospitals may contribute to racial disparities in infant mortality in the United States. Implications for Policy, Delivery or Practice: Our results suggest that neonatal morality was similarly elevated for VLBW black and white infants treated by minority-serving hospitals compared with other hospitals. These results suggest that, at least among VLBW infants, system level factors may be more important than infant level factors, such as race per se, in understanding racial disparities in care. Interventions to reduce neonatal infant mortality at minorityserving hospitals are needed. Primary Funding Source: AHRQ Call for Papers Disparities in Primary Care Chair: Kevin Fiscella, M.D., M.P.H. Monday, June 7 • 2:00 p.m.-3:30 p.m. • Characteristics of primary care physicians who treat whites and blacks in the United States Peter Bach, M.D., MAPP, Hoangmai Pham, M.D., M.P.H., Deborah Schrag, M.D., M.P.H., J. Lee Hargraves, Ph.D. Presented by: Peter Bach, M.D., MAPP, Assistant Attending, Epidemiology and Biostatistics, Memorial Sloan-Kettering Cancer Center, 1275 York Avenue, Box 221, New York, NY 10021; Tel: 646.735.8100; Fax: 646.735.0011; E-mail: bachp@mskcc.org Research Objective: To examine whether black patients receive their care from a subset of US primary care physicians who have inferior qualifications or resources Study Design: Cross sectional analysis of black and white Medicare beneficiaries who were treated by physicians participating in the Community Tracking Study survey. Population Studied: 4,355 primary care physicians in visits with 43,032 patients. Principal Findings: Black Medicare beneficiaries received primary care from a small group of physicians (80% of visits provided by 25% of physicians). Compared to white patients, black patients were more likely to have visits with physicians who were black (22.4% vs. 0.7%, p< 0.001), not board certified (22.6% vs. 13.9%, p = 0.02), and who derived a greater percentage of their practice revenue from Medicaid (13.4% vs. 9.3%, p< 0.001). Blacks also had a higher proportion of visits with physicians who reported that they were not able to consistently provide high quality care (27.8% vs. 19.3%, p= 0.005), or secure access for their patients to high quality ancillary services (37.7% vs. 27.8%, p = 0.02), high quality diagnostic imaging (25.2% vs. 17.0%, p= 0.01), or elective admission to the hospital (47.8% vs. 36.1%, p < 0.001). Conclusions: A small subset of primary care physicians is responsible for most of the care received by black Medicare patients. These physicians appear to have poorer qualifications and fewer resources than those who treat whites. Implications for Policy, Delivery or Practice: Interventions to reduce racial disparities should target providers who assume most responsibility for treating blacks, and address gaps in their training and access to resources. Primary Funding Source: RWJF, National Cancer Institute • The Role of Race in Physician Participation in Medicaid: What Happens When Poverty and Race are Conflated? Jessica Greene, Ph.D., Beth Weitzman, Ph.D., Jan Blustein, M.D., Ph.D., Dahlia Remler, Ph.D. Presented by: Jessica Greene, Ph.D., Assistant Professor, Planning, Public Policy and Management, University of Oregon, 1209 University of Oregon, Eugene, OR 97403; Tel: 541.346.0138; Fax: 541.346.2040; E-mail: jessicag@uoregon.edu Research Objective: Getting physicians to participate in Medicaid has been a challenge since the program’s inception. While low reimbursement rates have been a barrier, other factors matter. In surveys, physicians have expressed concern about mixing Medicaid patients with their existing patient base. Studies have shown that physicians are less likely to participate in Medicaid if they practice in areas with greater racial segregation, leading some to hypothesize that racial dissimilarity between Medicaid and non-Medicaid patients may be a barrier to participation. This study examines the degree to which racial dissimilarity between poor and nonpoor populations affects the likelihood that a physician will participate in Medicaid. Study Design: This was a cross sectional study of the association between physician participation in Medicaid and the racial/economic environment of the county in which they practice. County-level data from Census 2000 were used to construct a race/poverty dissimilarity ratio (RPDR) that compares the percent of poor county residents that are white to the percent of non-poor residents that are white. Analyses of the association between physician participation in Medicaid and RPDR controlled for physician and practice characteristics (gender, age, race, type of primary care provider, board certification status, US or foreign medical school graduate, and private or institution-based practice) as well as characteristics of the county of practice (county per capita income and urban/rural practice) and Medicaid policy variables (Medicaid/Medicare reimbursement ratio, standalone or Medicaid expansion SCHIP program, and Medicaid managed care penetration rates). Population Studied: A nationally representative sample of over 6,500 primary care physicians who provide at least 20 hours a week of patient care, and who participated in the 1998/1999 Community Tracking Survey. Principal Findings: Primary care physicians were substantially less likely to participate in Medicaid if the poor population in their county was racially dissimilar from the non-poor population, after adjusting for individual and county-level factors that are known to influence participation. Conclusions: Physician reluctance to participate in Medicaid may be partly driven by the racial dissimilarity between their traditional (non-poor) patient base and the race of poor Medicaid patients. Implications for Policy, Delivery or Practice: Policies aimed at improving physician participation in Medicaid, such as increasing Medicaid reimbursement rates and Medicaid managed care implementation, may not be sufficient to eliminate disparities in access for poor people of color, particularly in communities where poverty and race are highly correlated. Primary Funding Source: CWF • The Effects of Survey Methodology on Race, Ethnicity and Health Status Reporting Verna Lamar-Welch, Ph.D., M.P.H., Natalia Oster, R.N., M.P.H., Junling Ren, M.Ed., Claire Spettell, Ph.D., Elizabeth Lowry, R.N., B.S.N., Joette Majerus, B.S. Presented by: Verna Lamar-Welch, Ph.D., M.P.H., Researcher, Health Policy and Management, Emory University, Rollins School of Public Health, Emory Center on Health Outcomes and Quality, 1518 Clifton Road, Atlanta, GA 30322; Tel: 404.712.8531; Fax: 404.727.9198; E-mail: vlamar@sph.emory.edu Research Objective: To explore whether collection methodology impacts racial and ethnic self-reporting among those enrolled in a managed care organization’s (MCO) DDMP. Study Design: Approximately 19,000 MCO members were enrolled into the diabetes disease management program (DDMP) over the phone, and were asked to self-identify their race/ethnicity. Identification of race/ethnicity was optional, and participants could move to the next question if desired. Within 1 to 3 months of enrollment, participants were mailed a self-administered health assessment survey, and were asked again to self-identify race/ethnicity. In both collection methods, identifying information was separated from health related responses to protect the respondents’ anonymity and privacy. Cross-sectional analyses of data from those who returned the health assessment surveys were conducted. Population Studied: Enrollees in a MCO's diabetes disease management program (n=19,078). Principal Findings: Of the 19,078 health assessment surveys mailed, 6,433 were returned for a response rate of 34%. Nineteen percent (1214) of enrollees provided race/ethnicity data during enrollment on the phone. Of those, 209 (17%) were African American, 99 (8%) were Hispanic and 871 (72%) were Caucasian; the remaining 35 (3%) were from other races/ethnicities. Via the mailed health assessment survey, 5147 (81%) self-identified racial and ethnic data, and of those 15% were African American, 7% were Hispanic and 72% were Caucasian; the remaining 6% were from other races/ethnicities. Of the 1198 (19%) participants that reported racial and ethnic data over both the phone and in the mailed health assessment survey, 92% reported the same race/ethnicity regardless of data collection method (96% African Americans, 91% Hispanics, and 98% Caucasians). An additional 16 participants (<1%) self-identified racial and ethnic data via the phone, but not in the mailed health assessment survey. Differences were observed in health status reporting by data collection method. Excellent or very good overall health status was reported by 23% of mail only respondents, 7% of phone only respondents, and 20% of those responding to both (p=0.03). Self-management behaviors such as annual cholesterol screening (p=0.01), annual eye exam (p=0.001), regular exercise (p=0.005), and pneumococcal and influenza vaccinations (p<0.001) also differed by data collection method. No differences were observed in receiving dental exam, foot screening, urinalysis, and glycosolated hemoglobin screening by data collection method. Conclusions: In our study, the type of collection methodology used did affect rates of racial, ethnic and health status selfreporting. Implications for Policy, Delivery or Practice: Clearly more research is needed to explore why participants may be more or less willing to self-report demographic and health status data depending on collection methodology. Primary Funding Source: Academic Medicine and Managed Care Forum • Ethnic Disparities in the Impact of Copayment on Adherence to Anti-Hypertensive Medications among Asian Pacific Americans Deborah Taira, Sc.D., M.P.A., James Davis, Ph.D., Todd Seto, M.D., M.P.H. Presented by: Deborah Taira, Sc.D., M.P.A., Research Manager, Care Management, HMSA (BCBS of Hawaii), 818 Keeaumoku Street, P.O. Box 860, Honolulu, HI 96808-0860; Tel: 808.948.5337; Fax: 808.948.6043; E-mail: deb_taira@hmsa.com Research Objective: To determine whether there are ethnic differences in the impact of copayment on adherence to antihypertensive medications among Asian Pacific Americans. Study Design: This retrospective observational study examined adherence based on possession ratios, using administrative data from a large health plan in Hawaii. Loglinear regression models were used to determine the percent change in days of adherence to anti-hypertensive medications resulting from a 1 percent increase in copayment level. Interaction terms were used to examine whether this “price elasticity of adherence” differed by patient ethnicity after controlling for age, gender, type of coverage (HMO vs. PPO), specific therapeutic class of anti-hypertensive medication, education level, morbidity level, geographic location, diabetes, congestive heart failure, and coronary artery disease. All analyses were conducted in STATA 8.0 and adjusted for member clustering. Population Studied: Adult health plan members with a diagnosis of hypertension who filled at least one prescription for an anti-hypertensive medication between July 1999 and June 2003 (n=74,740). Members were followed for up to three years after their first prescription. Principal Findings: Ethnic differences in cost sensitivity were significant, with elasticities ranging from –0.29 for Japanese to -0.37 for Koreans, p<0.001. Based on these estimates, we found that a $1 increase in copayment per month was associated with annual decreased adherence of 7.4 days for Japanese, 7.8 days for Hawaiians, 8.3 days for Chinese, 8.7 days for whites, 8.9 days for Filipinos, and 9.1 days for Koreans. Other key variables were type of coverage and isle of residence. For HMO members, a $1 increase in copayment was associated with a 10-day decrease in adherence, while living on the rural islands of Molokai or Lanai was associated with 10- and 15-day decreases, respectively. Conclusions: While increases in copayment were associated with decreased adherence to anti-hypertensive medications for all groups, the level of response differs by ethnicity, even after adjustment for patient characteristics. The significant variation found among Asian Pacific Islander groups highlights the need to examine sub-groups separately. Implications for Policy, Delivery or Practice: Programs, including generic drug promotion and mail order substitution, may lower copayments and improve adherence for all groups. Certain sub-groups, who are the most cost sensitive, such as Koreans, Filipinos, or rural residents, may need targeted interventions, such as educational material on generic drug usage in appropriate languages, to maintain adherence when copayment increases are anticipated. Alternatively, health plans, through their disease management programs, may find it cost-effective to provide discounted pharmaceutical coverage for members most at risk of dropping essential medications. Primary Funding Source: AHRQ • Perceived Racism and Delay of Pharmacy Prescriptions Courtney Van Houtven, Ph.D., Corrine Voils, Ph.D., Eugene Oddone, M.D., MHSc., Kevin Weinfurt, Ph.D., Joelle Friedman, M.P.A., Hayden Bosworth, Ph.D. Presented by: Courtney Van Houtven, Ph.D., Health Economist/Research Assistant Professor, Health Services Research/General Internal Medicine, VA and Duke Medical Centers, 508 Fulton Street, Durham, NC 27705; Tel: 919.286.6936; Fax: 919.416.5839; E-mail: courtney.vanhoutven@duke.edu Research Objective: Delaying filling pharmacy prescriptions can lead to poor medication adherence and poor health outcomes. In this study, we investigated whether perceptions of unfair treatment in the health care system due to race or ethnicity are associated with pharmacy prescription delays, controlling for resource constraints and demographic factors. Study Design: Telephone interviews elicited people’s care seeking behavior for pharmacy prescriptions, as well as demographic information, insurance status, economic resources, and self-reported health and depression. Logistic regression was used to model the effect of perceived racism on the likelihood of delaying filling a pharmacy prescription. Robust standard errors are estimated. Population Studied: A community sample of 181 Blacks, 148 Latinos, and 224 Whites in Durham County, North Carolina. A sample of Whites and Blacks was obtained using standard list-assisted random-digit dialing methodology. Census tracks that had 10% or more Black households were identified to ensure oversampling of Blacks; these census tracks were then matched to phone exchanges. Because Durham has few Latino households in general, and the Latino population is not clustered, Latinos were recruited from a Durham County list of Latino surname households. Principal Findings: Nearly 17 percent of the sample had delayed or not filled a prescribed medication. Fifty-two percent of the sample felt that race or ethnicity caused unfair treatment in healthcare. After controlling for insurance, resource availability, and self-reported health, the odds of delaying a pharmacy prescription was 2.11 higher for persons who perceived unfair treatment. The odds of Blacks delaying pharmacy treatment were not significantly different from the odds of Whites doing so. The odds of Latinos delaying treatment was significantly lower than Whites; the odds-ratio was 0.46. People with self-reported depression were also significantly more likely to delay pharmacy tests; the odds-ratio was 2.44. Significant results reported had p-values less than .05. Conclusions: Perceptions of racism and self-reported depression were important factors in explaining delays in filling pharmacy prescriptions. Economic resource and health insurance constraints did not explain delays in pharmacy prescriptions. Implications for Policy, Delivery or Practice: Our findings echo what other disparities researchers have found: Economic and insurance constraints do not fully explain disparate utilization patterns by race and ethnicity. In fact, in our study, perceived general racism in health care was more important than economic constraints in explaining prescription delays. Being Latino and being depressed also were associated with a higher odds of delaying filling prescriptions. Ameliorating perceived racism in the health care system may reduce prescription delays and improve prescription adherence and health outcomes. Call for Papers Strategies to Address Health Disparities Chair: Kaytura Felix-Aaron, M.D. Monday, June 7 • 4:00 p.m.-5:30 p.m. • Racial/Ethnic Disparities in the Appropriate Use of HighVolume Hospitals Bradford Gray, Ph.D., Shannon Mitchell, Ph.D., Emily Horowitz, Ph.D., Mark Schlesinger, Ph.D. Presented by: Bradford Gray, Ph.D., Director, Health & Science Policy, The New York Academy of Medicine, 1216 Fifth Avenue, New York, NY 10029; Tel: 212.822.7287; Fax: 212.822.7369; E-mail: bgray@nyam.org Research Objective: This project addresses a largely unexamined source of racial/ethnic disparities in health services and outcomes--the use of providers of different quality. Specifically the study examines racial/ethnic disparities in the use of high-volume hospitals (HVHs) for 22 procedures and conditions for which a positive volumeoutcome relationship has been documented in prior research. We examine patient characteristics (insurance status, education, proximity) that may explain such disparities and whether the disparities are mitigated by managed care and public policies that concentrate care in fewer institutions. Study Design: The study examines racial/ethnic disparities in the use of high-volume hospitals among residents of New York City and adjacent counties. “High volume” is defined by available threshold standards published by AHRQ and the LeapFrog Group or by alternative measures such as top decile or quartile. Logistic regression analysis is used to determine the amount of disparities between Whites, Blacks, and Hispanics in the use of HVHs, controlling for patient characteristics including insurance status, co-morbidities, proximity to a HVH, and education (measured at census tract). Separate models are estimated for each procedure and condition. Population Studied: Data come from NY’s Statewide Planning and Research Cooperative System (SPARCS) inpatient discharge records. The patients included in the study will consist of residents of NYC and adjacent NY counties who were treated in a NY hospitals 2001 or 2002 for the procedures and conditions included in the study. Principal Findings: In preliminary analyses, we found that Whites were about twice as likely as African-Americans to have their carotid endarterectomy done at a HVH. Patients of other racial/ethnic groups were also substantially less likely than Whites to use a HVH. Whites were also twice as likely as African-Americans to use a HVH for cancer surgery. Differences with the other ethnic groups were smaller. These effects remain stable even after uninsured persons were excluded. For the presentation at AcademyHealth, we will have results for the full analysis of results for 22 procedures/conditions, with appropriate statistical controls as mentioned earlier. We will also examine whether disparities are smaller for HMO enrollees and for procedures concentrated in fewer institutions. Conclusions: Our analyses are still underway, so we do not offer conclusions at this time. However, there are striking differences in the racial/ethnic composition of the patient population of hospitals in NYC. The volume-outcome literature suggests that the hospital used affects outcomes for many procedures and conditions. Racial/ethnic differences in the use of high-volume hospitals have not been previously identified as a source of disparities in services and outcomes. Implications for Policy, Delivery or Practice: Our findings will contribute to the goal of reducing racial/ethnic disparities in quality. First, the findings will provide empirical evidence of a heretofore unrecognized source of disparities in care. Documenting its dimensions is a first step toward a solution. Second, our data analysis strategy is defined in policy-relevant terms. That is, we are planning our data analysis to shed light on (a) causes of the problem and (b) the feasibility of different approaches to solution. Primary Funding Source: AHRQ, The Commonwealth Fund • Providing Health Care Services to the Formerly Homeless: A Quasi-Experimental Evaluation of Outcomes Andrea Ciaranello, M.D., Richard Kravitz, M.D., Fred Molitor, Ph.D., Martin Leamon, M.D., Daniel Tancredi, Ph.D., Christina Kuenneth, M.S., Alison Diamant, M.D. Presented by: Richard Kravitz, M.D., Professor; Director, Center for Health Services Research in Primary Care, Internal Medicine, UC Davis Medical Center, 4150 V. Street, Suite 2400, Sacramento, CA 95822; Tel: 916.734.2818; E-mail: rlkravitz@ucdavis.edu Research Objective: Transitional housing programs are designed to re-integrate homeless individuals into the community, but housing alone is unlikely to alleviate chronic health problems acquired during homelessness. Using a quasi-experimental design, we evaluated the effects of a focused health care intervention (the HEALTH Project) on access to needed care, delivery of preventive services, and health status for residents of transitional housing facilities (THFs) in one northern California city. Study Design: Beginning in Fall, 1999, a multidisciplinary team provided direct services (comprehensive physical examinations, diagnostic studies, referrals, social services, and counseling) to residents at 4 intervention THF sites. Survey and physical examination data were collected from residents of the 4 intervention sites and 2 control sites at baseline and 6 and 18 months later. Outcomes were evaluated using mixed effects models that accounted for missing observations and clustering by site and estimated the effects of the program (intervention vs. control) over time while adjusting for residents´ baseline sociodemographic characteristics. Population Studied: The HEALTH Project's target population was single adult THF residents. At any given time, there were approximately 450 members of the target population living at the intervention sites. Approximately 50 residents lived at the control sites. Principal Findings: Survey and physical examination participation rates exceeded 70% at all sites. HEALTH Project staff delivered services to 511 THF residents in more than 2400 clinical encounters. The Project significantly reduced the odds of "not receiving medical care when needed" (adjusted OR 0.42, 95%CI 0.26-0.69, p < 0.05). There was also a significant improvement in the receipt of gynecologic preventive services: Papanicolaou tests within the past year among female residents 18 years of age or older (AOR 7.52; 95%CI 2.37-23.86) and mammograms within the preceding two years among women aged 40 years or older (AOR 9.54, 95%CI 1.36-67.02). The intervention had no effect on access to specialists, dentists, or optometrists; on frequency of emergency department visits or hospital admissions; on timeliness of care; on self-reported health status; or on blood pressure or vision (p>.05 in all cases). Conclusions: The HEALTH Project reflected successful community collaboration and met several clinically relevant goals in improving access to care. The intervention had robust effects on proximal outcomes (those directly provided or easily arranged by the on-site health care team) but failed to impact more distal outcomes. Implications for Policy, Delivery or Practice: These results highlight the challenges of implementing health care outreach for residents of transitional housing programs and may inform the design of future interventions. Specifically, improved outcomes may result from prioritization of project goals, assessment of community needs, and efficient use of community and medical resources. Primary Funding Source: California Healthcare Foundation • Examination and Evaluation of Initial State Implementation of the Breast and Cervical Cancer Prevention and Treatment Act Kathleen Maloy, J.D., Ph.D., Chaya Merrill, M.P.H., Dr.PH Candidate, Sarah Blake, M.A., Kyle Kenney, M.P.H. Presented by: Chaya Merrill, M.P.H., Dr.PH (candidate), Senior Research Associate, Department of Health Policy, The George Washington University, 2021 K Street, NW, Suite 800, Washington, DC 20006; Tel: 202.530.2337; Fax: 202.296.0025; E-mail: cmerrill@gwu.edu Research Objective: The BCCPTA established a new coverage option under Medicaid that permits states to extend Medicaid to uninsured women under 65 who are diagnosed with breast and/or cervical cancer through a national screening program. This coverage option is groundbreaking in its use of population-wide public health screening program as pathway for publicly funded health insurance. As states did not begin to implement BCCPTA until 2001, little is known about states’ implementation experiences and how women’s access to breast and cervical cancer treatment might be affected. The research objectives are to (1) describe and evaluate initial BCCPTA implementation, and (2) design research to measure and assess the effect of BCCPTA on health outcomes for women with breast and cervical cancer. Study Design: Case study methods were used to examine sixteen states that were among the first to implement BCCPTA. Data collection, conducted during July through December 2002, included structured interviews with key stakeholders, including state Medicaid officials, Title XV (i.e., NBCCEDP) grantees, community/advocacy organizations, and document review. Data collection and analysis focused on (1) designs of states’ Medicaid expansions, (2) collaboration between Medicaid and Title XV officials; (3) development of BCCPTA Medicaid enrollment procedures; (4) effect of BCCTPA implementation on Title XV agencies; and (6) states’ experiences in implementing BCCPTA. Population Studied: State Medicaid and Title XV officials Principal Findings: (1) Relatively smooth implementation with states using existing provider screening networks; (2) Wide range across states of enrollment procedures and redetermination practices. (2) Substantial variation across states in their experiences with Medicaid enrollment and expenditures versus prior estimations/expectations; (3) Notable and variable impact on the activities of Title XV agencies; and (4) Uncertainty about long-term costs associated with BCCPTA coverage due to early stage of implementation. Conclusions: Study findings suggest that screening programs can be an effective pathway to publicly-funded insurance coverage (i.e., Medicaid). Uncertainty about costs may present longer-term challenges to ongoing implementation. A summary of the findings includes: (1) Early success in enrolling women in BCCPTA Medicaid, (2) Effective collaboration between Medicaid and Title XV to implement this unique coverage expansion, and (3) Substantial state support for BCCPTA. Implications for Policy, Delivery or Practice: Study findings provide the essential first step toward conducting impact evaluation research that will (1) evaluate the effectiveness of BCCPTA in improving the ability of uninsured women with breast and/or cervical cancer to secure earlier and better treatment and, thereby, to experience improved outcomes, and (2) assess whether using prevention programs as a pathway for publicly-funded insurance coverage promotes access to quality care and improves health outcomes. Primary Funding Source: CDC • Reducing Racial and Ethnic Health Disparities: Estimating the Impact of High Health Center Penetration in Low-Income Communities Peter Shin, Ph.D., M.P.H., Karen Jones, M.S., Sara Rosenbaum, J.D. Presented by: Peter Shin, Ph.D., M.P.H., Assistant Research Professor, Health Policy, George Washington University, 2021 K Street, NW, Suite 800, Washington, DC 20006; Tel: 202.530.2313; Fax: 202.296.6922; E-mail: pshin@gwu.edu Research Objective: The health disparities literature suggests that although the lack of health insurance is the most basic barrier to health care, improved access to clinically appropriate care is key, particularly in the case of minority and low-income populations where the health risks are greatest. This study examines the relationship between health center penetration into medically underserved communities and the reduction of statelevel health disparities. Study Design: We designed this study to permit a comparison between the magnitude of state-level racial and ethnic disparities for certain key health indicators and the proportion of low-income persons served by health centers for each state. We first compiled measures of health status available by state and race, as well as state and income level. Data collection was restricted primarily to those data sources for which data already were compiled for all states and the District of Columbia. Our specific focus was on health measures that have been shown in the literature to reveal significant disparities between white and minority populations. We also were interested in measures that have been shown to be ambulatory care sensitive, that is, that are amenable to control through comprehensive primary health care aimed at both preventing the onset of health conditions and treating and managing conditions at early stages. Six point-in-time indicators with sufficient reliable state-level data were selected to permit disparities calculations between white persons and black persons, and white persons and Hispanic persons. Because of limitations in the data, state-level comparisons could not be drawn for other health measures. Furthermore, data limitations prevented comparisons for other racial and ethnic subgroups. Thus, this analysis is limited to black/white and Hispanic/white health disparities. The measures that ultimately were chosen for this analysis were: infant mortality (2000); total death rate (1999), heart disease death rate (1999); diabetes death rate (1999); tuberculosis case rate (2000) and level of prenatal care (2000). We conducted multiple regression models which included health center penetration (i.e., percent of the state’s lowincome population served by health centers) and controlled for age, education, population density, per capita income, and percent of the state population without health insurance. A measure of the generosity of the state Medicaid program was also examined in the health disparities models, in view of the well established association between health insurance and access to health care. The purpose of this measure was to determine whether health center penetration still mattered as an independent consideration even in those states with relatively generous Medicaid eligibility levels. In addition, we supplemented our quantitative estimates with interviews conducted during the first half of 2003 with the staff of five health centers. These health centers are located in five communities selected on the basis of geography, urban/rural location, and a is proportionately high volume of minority and low income patients relative to the already high average rate for health centers nationally. Population Studied: Community health center presence (as measured by the proportion of low-income resident served by health centers); black, Hispanic, and white populations. Principal Findings: The results of our analysis showed that greater levels of health center penetration (i.e., proportion of low-income individuals served) were associated with significant and positive reductions in minority health disparities. In the case of black/white health disparities, we found that penetration was significantly associated with a narrowing of the health disparities gap in the case of total death rate and prenatal care. The infant mortality gap also narrowed as penetration increased, although the reduction was not as great. In the case of Hispanic/white disparities, health center penetration was significantly associated with health disparity reductions in the case of the tuberculosis case rate and prenatal care. Our interviews with individual health centers confirm that clinics actively pursue the overall program mission of bringing affordable and clinically appropriate health care to low-income communities. By themselves, state Medicaid eligibility levels were determined to have no significant association with state level measures of health disparities. However, because one third of health center operating revenue is derived from Medicaid, state Medicaid coverage and payment policies are integral to the ability of health centers to achieve high penetration. Therefore, if health centers are shown to have a significant relationship with reduced health disparities, state Medicaid policy remains a critical component of health center efforts to reduce health disparity. Conclusions: The results of our regression analysis showed a significant association between health center penetration and reduced racial and ethnic health disparities for certain key outcomes measures. Specifically, greater penetration levels were associated with larger reductions in disparities. Implications for Policy, Delivery or Practice: Although the goal of reducing health disparities is national, in the end it is the underserved communities themselves -- and the states in which these communities are located -- that shoulder much of the practical burden of achieving the types of health systems changes (such as better insurance coverage and greater health care access) that have been associated with a reduction in minority health disparities. In this regard, health centers are a principal strategy for anchoring accessible, high quality primary health care in pervasively poor and uninsured communities that, without such an investment, could not hope to independently attract and support sufficient private medical care practices. This study suggests that a national policy that aims for increased health center penetration, coupled with adequate operational support via strengthened insurance coverage of lower income persons, can be expected to make a significant difference in minority health status at the local community level. Primary Funding Source: National Association of Community Health Centers • Developing an Intervention to Improve Quality of Care and Reduce Health Disparities in Minority Communities Jane Sisk, Ph.D., Paul Hebert, Ph.D., Mary Ann McLaughlin, M.D., M.P.H., Carol Horowitz, M.D., M.P.H., Cheryl Goldstein, M.D., Leah Tuzzio, M.P.H. Presented by: Jane Sisk, Ph.D., Professor, Health Policy, Mount Sinai School of Medicine, One Gustave L. Levy Place, New York, NY 10029-6574; Tel: 212.659.9567; Fax: 212.423.2998; E-mail: jane.sisk@mssm.edu Research Objective: Hypertension exacts a greater burden on Black than White populations, with earlier and more severe onset and higher rates of sequelae, including coronary-heart disease, stroke, and renal failure. Despite proven-effective therapies, only 28% of hypertensive Black people nationally have controlled blood pressures. We sought to identify problems underlying uncontrolled hypertension among treated African-Americans and Latinos in Harlem, and design an intervention to address them. Study Design: To identify underlying problems, we used the following qualitative and quantitative methods: interviews with key informants, focus groups with patients, and a survey of clinicians. The clinician survey included hypothetical clinical vignettes in which patients’ demographic characteristics were randomly assigned. This allowed us to estimate whether patient demographics affected care. We also performed retrospective chart review to assess whether clinical care manifested the problems suggested by key informants, focus-group participants, and surveyed clinicians. Population Studied: Key informants consisted of administrators and clinicians at the four hospitals, Harlem, New York City. Nine focus groups in English and Spanish included African-American and Latino hypertensive patients from hospital clinics managing hypertension. We surveyed the 469 clinicians in those clinics. We reviewed charts of 99 consecutive uncontrolled hypertensives with scheduled appointments who had been treated at least six months and whose blood pressures exceeded guidelines by 10mmHg systolic or 5mmHg diastolic. Principal Findings: Key informants noted access problems; patients’ profound life problems; and patient mistrust of the health system. Focus-group patients were well aware of the importance of medications and lifestyle, but sometimes skeptical about their medication regimens. Some reported lack of respect at certain medical centers, access problems, and interest in home blood-pressure monitors. From the 79% of surveys completed, clinicians were knowledgeable about evidence-based blood-pressure targets (86% or more), except for renal disease (9%). Clinicians’ blood-pressure targets were not significantly associated with patient demographic characteristics in the hypothetical vignettes. But clinicians’ expectations about achieving control had significant negative associations with patients’ being unemployed, employed as cashiers, African-American, or Hispanic. According to chart review, in the year before the scheduled appointment, patients averaged 5.1 clinic visits after the first uncontrolled blood pressure. For visits with uncontrolled pressures, physicians incorrectly noted control for 11%, entered no comments for 28%, noted patients’ non-adherence for 24%, and recorded no action for 51%. Conclusions: Problems underlying uncontrolled hypertension among treated Harlem patients relate to patient selfmanagement, lack of clinical adjustments despite frequent contacts, and system and cultural barriers. Implications for Policy, Delivery or Practice: Based on these exploratory studies, we designed and implemented a nursemanagement intervention to target the problems underlying hypertension control in this community, and are evaluating its effectiveness and cost-effectiveness in a randomized controlled trial. Bilingual nurses counsel patients; train them to use home blood-pressure monitors; follow-up regularly by telephone and provide social support; interact with clinicians to adjust medications until control is attained; and facilitate access to social work and insurance coverage. The program has strong clinical and administrative support. Primary Funding Source: AHRQ Call for Papers Health Literacy, Cultural Competence & Perceived Racism Chair: Joseph Betancourt, M.D., M.P.H. Tuesday, June 8 • 9:15 a.m.-10:45 a.m. • Cultural Competence: A Systematic Review of Health Care Provider Educational Interventions Mary Catherine Beach, M.D., M.P.H., Eboni Price, M.D., Tiffany Gary, Ph.D., Karen Robinson, M.Sc., Aysegul Gozu, M.D., Ana Palacio, M.D., M.P.H., Carole Smarth, M.D., Mollie Jenckes, M.H.S., R.N., Carolyn Feuerstein, B.A., Eric Bass, M.D., M.P.H., Neil Powe, M.D., M.P.H., M.B.A., Lisa Cooper, M.D., M.P.H. Presented by: Mary Catherine Beach, M.D., M.P.H., Assistant Professor, Medicine, and Health Policy and Management, Johns Hopkins University, 2024 East Monument Street, Suite 2-500, Baltimore, MD 21287; Tel: 410.614.1134; Fax: 410.614.0588; E-mail: mcbeach@jhmi.edu Research Objective: To reduce racial and ethnic disparities in care, efforts have been made to improve the cultural competence of health professionals. We synthesized the findings of studies evaluating interventions to improve cultural competence. Study Design: We performed a systematic review of literature from 1980 through June 2003 using electronic and hand searches to identify studies that evaluated interventions designed to improve the cultural competence of health professionals. Population Studied: Eligible studies were in English, with original data, and described an intervention evaluated with a pre- and a post- test or by comparison to a control arm. Two reviewers abstracted data on the effectiveness and cost of cultural competence training, and graded the strength of the evidence as excellent, good, fair or poor using predetermined criteria. Principal Findings: Thirty-four studies were included in our review. Four studies were published between 1980-1989, 14 between 1990-1999, and 18 between 2000-2003. Targeted learners were most often nurses (n=17) and physicians (n=18). Most curricula focused on specific cultural content (n=26), general concepts of culture (n=19), language (n=10), and patient-provider interaction (n=8); fewer focused on health care access (n=3), racism (n=2), and socio-economic status (n=2). Most curricular interventions used more than one training method. The most common training methods were group discussion (n=17), lectures (n=17), case scenarios (n=12), clinical experiences (n=10), presentations by members of another culture (n=9), small group work (n=9), and cultural immersion (n=8). Evidence is excellent that training improves the knowledge of health professionals (17 of 19 studies demonstrated a beneficial effect). Evidence is good that training improves the attitudes and skills of health professionals (21 of 25 studies demonstrated a beneficial effect and 14 of 14 studies demonstrated a beneficial effect, respectively). Evidence is good that training impacts patient satisfaction (3 of 3 studies demonstrated a beneficial effect) and poor that training impacts patient adherence (although the one study designed to do this demonstrated a beneficial effect). No studies have evaluated patient health status outcomes. There is insufficient evidence to determine the costs of cultural competence training. Conclusions: Cultural competence training shows promise as a strategy for improving the knowledge, attitudes and skills of health professionals. However, evidence is lacking that it improves patient adherence, health outcomes and equity of services across racial and ethnic groups. Implications for Policy, Delivery or Practice: Future cultural competence research should include an assessment of the impact of training on patient adherence, health outcomes and equity of services across racial and ethnic groups, determine which teaching methods and content are most effective, and use evaluation strategies that adhere to basic principles of study design and performance. This work will help health care managers and educators determine whether cultural competence training for health professionals is an effective strategy to eliminate minority healthcare disparities. Primary Funding Source: AHRQ • Serving Diverse Communities in Hospitals and Health Systems Edward Martinez, M.S., Linda Cummings, Ph.D., Linda Cummings, Ph.D., Lindsay Davison, B.A., Ingrid Singer, M.H.S., Arsenio DeGuzman, M.P.A., Marsha Regenstein, Ph.D. Presented by: Linda Cummings, Ph.D., Director of Research, National Public Health and Hospital Institute, 1301 Pennsylvania Avenue, N.W., Suite 950, Washington, DC 20004; Tel: 202.585.0130; Fax: 202.585.0101; E-mail: lcummings@naph.org Research Objective: The patient population served by large, urban safety net health systems is highly diverse, both culturally and linguistically. Quality health care in this setting reflects strategies that address the disparities in health services and health outcomes experienced by minority and low-income patients. NPHHI undertook a study to identify promising and innovative practices designed to improve care for cultural and linguistic minorities and to address health disparities. Study Design: The study team reviewed federal standards for culturally and linguistically appropriate services and conducted a literature review of research on health disparities and care for diverse populations. Structured interviews were conducted with senior executives at 35 public hospitals and health systems, and a focus group was held with the chief executive officers of major safety net institutions. Case studies of selected practices at safety net health systems were developed to identify promising and innovative approaches. The practices were organized under six headings: leadership, interpreter services, community relations and outreach, infrastructure, staff training, and clinical services. Population Studied: Large safety net hospitals and health systems geographically dispersed across the country were selected for the case studies. The participating institutions have highly diverse patient populations in terms of race, ethnicity, language and insurance status. Principal Findings: Public hospitals and health systems have undertaken the provision of culturally and linguistically appropriate services because these practices are a fundamental component of their mission. The most highly developed practices to serve diverse communities are in the area of interpreter services. Leadership is crucial to initiating and sustaining practices that focus on disparities and serving diverse communities. Technological applications are highly promising in the development of practices to serve diverse populations. The need for comprehensive, timely data is crucial to the development of metrics that will enable hospitals and health systems to measure performance in providing culturally and linguistically appropriate care and to measure impact on disparities. Conclusions: For major safety net systems across the country, providing health care in a culturally competent manner is crucial to quality of care, patient satisfaction, successful staff training and recruitment and the financial viability of safety net institutions. Although these practices are central to efforts to reduce disparities, they are generally the result of entrepreneurial activity by senior executives and undertaken without supplemental resources, burdening already constrained safety net institutions. Implications for Policy, Delivery or Practice: At the federal level more effective coordination is needed among agencies issuing standards, guidelines, and directives in the area of cultural and linguistically appropriate services. Additional resources should be directed at supporting those safety net institutions that are providing care to diverse populations, many of whom are uninsured, on Medicaid, and do not speak English. Resources are also needed to develop data systems to provide timely, accurate metrics to monitor performance in providing this care and to measure efforts to reduce health disparities for diverse populations. • Development of an Easy-to-Use Spanish Health Literacy Assessment Tool Shoou-Yih Lee, Ph.D., Rafael Ruiz, Sc.M., Debra Bender, Ph.D., M.P.H., Young Cho, Ph.D. Presented by: Shoou-Yih Lee, Ph.D., Assistant Professor, Health Policy and Administration, University of North Carolina at Chapel Hill, 1101 McGavran-Greenberg Hall, Chapel Hill, NC 27599-7411; Tel: 919.966.7770; Fax: 919.966.6961; E-mail: sylee@email.unc.edu Research Objective: The study was intended to develop and validate a health literacy assessment tool, termed the Short Assessment of Health Literacy for Spanish Adults (SAHLSA), for the Spanish-speaking population. Health literacy means the degree to which individuals have the capacity to obtain, process, and understand basic health information and services needed to make appropriate health decisions. Research has shown that low health literacy may be associated with low health status, and increased rates of emergency room use and hospitalization. Healthy People 2010 Objectives: Draft for the Public Comment notes that health literacy is "increasingly vital to help people critically evaluate health information." The 2000 census showed that America’s Latino population increased 58 percent during the 1990s. In 2003, Latinos surpassed African Americans as the nation’s largest minority group. Given the rapid growth of the Latino population, development of a reliable and easy-to-use health literacy assessment tool in Spanish cannot be overemphasized. Study Design: The design of SAHLSA was based on the Rapid Estimates of Adult Literacy in Medicine (REALM), known as the most easily administered tool for assessing health literacy in English. In addition to the word-recognition test in REALM, SAHLSA incorporates a comprehension test using multiplechoice questions designed by an expert panel. Validation of SAHLSA involved testing and comparing the tool with other health literacy assessment instruments in a sample of 201 Spanish-speaking and 202 English-speaking subjects recruited from the Ambulatory Care Center at the University of North Carolina Hospitals. Population Studied: Spanish- and English-speaking populations. Principal Findings: With only the word recognition test, REALM could not differentiate the level of health literacy in Spanish. Incorporation of the comprehension test in SAHLSA significantly improved the differentiation among Spanishspeaking subjects. The correlation between SAHLSA and the Test of Functional Health Literacy in Adults (TOFHLA), another health literacy assessment instrument, was 0.66 in the Spanish-speaking subjects, comparable with the correlation (r=0.74) in the English-speaking sample. SAHLSA was also significantly correlated with educational attainment (years of schooling) and health status in both the Spanishand English-speaking samples. Finally, we tested and found SAHLSA to have high test-retest reliability (r=0.90). Conclusions: The new instrument, SAHLSA, was satisfactory based on reliability and validity tests. Implications for Policy, Delivery or Practice: With further improvement and validation, SAHLSA could be used in clinics and public health settings to assess the health literacy level of Spanish-speaking patients. This would enhance health professionals’ ability to communicate with and, thus, deliver better medical services, to their Spanish-speaking patients. SAHLSA, used as a health literacy screening tool in local Latino communities, could improve our understanding of the specific health and personal needs of Latino residents and help policy-makers, researchers and community groups design intervention and educational programs that suit the health literacy level of this under-served population. Primary Funding Source: AHRQ • Language Barriers and Seniors: Implications for Medicare Policies Ninez Ponce, M.P.P., Ph.D., Leighton Ku, Ph.D., William Cunningham, M.D., M.P.H. Presented by: Ninez Ponce, M.P.P., Ph.D., Assistant Professor, Health Services, UCLA School of Public Health, 31254B CHS, Los Angeles, CA 90095-1772; Tel: 310.206.4021; Fax: 310.455.9475; E-mail: nponce@ucla.edu Research Objective: Most research concerning health disparities related to limited English proficiency (LEP) or immigration status has focused on low-income children and families and, therefore, on Medicaid policies. This study investigates whether such disparities also occur among seniors covered by Medicare. Study Design: We assessed language barriers as a 3-level measure of English language proficiency: 1) LEP, in which the individual speaks English well or not well; 2) bilingual, in which the individual speaks English well or very well and speaks another language; and 3) speaks English only. We measure whether and to what extent there are disparate patterns by English language proficiency in self-reported physical and mental health, having a usual source of care, seeing a doctor over the past year, and utilization of recent breast and colorectal cancer screening tests. We employed simple logit regressions, weighted to the California 2000 population, adjusting for relevant demographic and socioeconomic covariates. Population Studied: We studied the 2001 California population, age 65 and older, covered by Medicare. Our data source was the population-based 2001 California Health Interview Survey (n =10, 509), conducted in English, Spanish, Mandarin, Cantonese, Vietnamese, Korean and Khmer. Principal Findings: We compared health status, access and utilization measures of LEP and bilingual seniors to the referent: seniors who speak English only. LEP was associated with higher rates of reporting fair or poor health; both LEP and bilingual seniors were more likely to report sadness most or all of the time; and LEP seniors were also more likely to not have a usual source of care. We found no differences by language ability in having seen a doctor over the past year. Although LEP was not associated with lower use of mammograms and colorectal cancer tests, seniors who lived in the U.S. less than ten years were less likely to receive these screening tests. Conclusions: LEP played a significant role in a senior’s assessment of their physical and emotional health and in their lack of a usual source of care. The language effect diminished for utilization and cancer screening tests. The effect on utilization may have been attenuated because of high visit rates among the insured elderly (95% ) across all language groups. For cancer screening tests, years lived in the U.S., had a significant effect suggesting that US tenure confers increasing social support and familiarity with the health care system in a way that promotes adherence to cancer screening guidelines. Thus, though language had no effect, the immigrant dimension in utilization of preventive tests was still important. Implications for Policy, Delivery or Practice: Federal civil rights policy, based on Title VI of the Civil Rights Act, requires that health care providers and other organizations that receive federal funds offer language assistance to those with limited English proficiency. Our study demonstrates that language and immigrant-related barriers exist for seniors in Medicare, so that federal policy-makers, such as the Congress or the Department of Health and Human Services, may become more broadly interested in language assistance policies. Primary Funding Source: NIA, Commonwealth Fund • Impact of Perceived Discrimination on Use of Preventive Services Amal Trivedi, M.D., M.P.H., John Ayanian, M.D., M.P.P. Presented by: Amal Trivedi, M.D., M.P.H., Fellow, Department of Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115; Tel: 617.432.3138; E-mail: trivedi@hcp.med.harvard.edu Research Objective: Prior research has documented disparities in the use of health services based on race, gender, and insurance status. We examined the frequency of perceived discrimination in the health care system, and the relation between perceived discrimination and the receipt of preventive services. Study Design: We conducted a cross-sectional study of the 2001 California Health Interview Survey, a random–digit telephone survey, to assess the relation between the perception of having been discriminated against in a health care setting over the past 12 months and receipt of the following preventive health services over this time period: aspirin use and cholesterol testing among people with heart disease or hypertension, foot examination and HbA1C testing among people with diabetes, colon cancer screening for adults >age 50, PSA testing among men >age 50 , flu vaccination among adults >age 65, mammography among women age 5079, and Pap testing among women age 18-65. We used multivariate logistic regression to control for multiple demographic and clinical characteristics with SUDAAN software. Population Studied: 54,968 Californian adults aged 18 and older. Principal Findings: Of the 54,968 subjects, 2830 (4.7%) reported experiencing discrimination in a health care setting over the past 12 months; among these individuals, the most frequent types of perceived discrimination was related to insurance type (27.4%), race (13.7%), and income (6.6%). Female gender, non-white race, lack of insurance, rural residence, low income, lack of high school education, limited English proficiency, presence of comorbid medical conditions, more frequent physician visits, fair or poor health status, current tobacco use, unmarried status, and obesity were significantly associated with reporting discrimination (all p<0.05). Persons who reported discrimination were less likely than those not reporting discrimination to have had HbAIC testing (78.5% vs. 86.1% p=0.04), cholesterol testing (71.0% vs. 79.2% p<0.01), mammography (78.4% vs. 83.6% p=0.03) and PSA testing (37.1% vs. 45.7% p=0.03.) There was no significant difference in aspirin use (33.4 vs. 35.2% p=0.38), foot examination (60.8% vs. 67.6% p=0.12), colon cancer screening (41.8% vs. 44.0% p=0.26), flu vaccination (62.5% vs. 67.5% p=0.10) and Pap testing (87.7% vs. 87.1% p=0.61). After adjustment, there was no significant relation between perceived discrimination and use of preventive services except for cholesterol testing (OR 0.69, 95% CI: 0.55-0.88, p<0.01). Conclusions: The adjusted association between perceived discrimination and decreased use of preventive health services was relatively small in magnitude and significant only for cholesterol testing. Given these limited associations and the small percentage of adults who reported discrimination, perceived discrimination is unlikely to account for a large portion of observed disparities in use of preventive health services. Implications for Policy, Delivery or Practice: Future studies should validate the results of this study using longitudinal data, focus on specific experiences related to perceived discrimination in the health care system, and examine whether discrimination has other impacts on use of health services. Primary Funding Source: NIH NRSA Research Training Grant Call for Papers Disparities in Hospital Care Chair: Edward Guadagnoli, Ph.D. Tuesday, June 8 • 11:15 a.m.-12:45 p.m. • Racial and Ethnic Differences in the Time to Acute Reperfusion Therapy for Patients Hospitalized with Myocardial Infarction Elizabeth Bradley, Ph.D., Yongfei Wang, M.S., Jeph Herrin, Ph.D., Tashonna Webster, M.P.H., Martha Blaney, D.Pharm., Harlan Krumholz, M.D. Presented by: Elizabeth Bradley, Ph.D., Associate Professor, Health Policy and Administration, Yale School of Public Health, 60 College Street, New Haven, CT 06520; Tel: 203.785.2937; Fax: 203.785.6287; E-mail: elizabeth.bradley@yale.edu Research Objective: Racial and ethnic disparities in cardiovascular care are well documented. Recent reports indicate that patients with acute myocardial infarction identified as non-white experience significantly longer door-todrug and door-to-balloon times than patients identified as white, raising concerns of health care disparities. However, we know little about the reasons for these differences. We sought to examine the extent to which sociodemographic factors, insurance, clinical characteristics, and hospital-level factors mediate, and thus potentially explain, racial and ethnic differences in time to acute reperfusion. Door-to-drug and door-to-balloon times are critical quality indicators for cardiovascular care because prompt reperfusion substantially reduces subsequent morbidity and mortality. Study Design: This is a retrospective, observation study using patient level data from the National Registry of Mypcardial Infarction (NRMI) and hospital-level data from the American Hospital Association Hospital Survey from 2000. We use sequential, hierarchical modeling to examine crude and adjusted racial/ethnic differences in time to treatment patients receiving primary reperfusion therapy after acute myocardial infarction. Population Studied: Patients admitted to hospitals participating in NRMI, the largest longitudinal registry for myocardial infarctions in the U.S., from January 1, 1999 through December 31, 2002, with a diagnosis of ST-elevation myocardial infarction or left bundle branch block and who underwent primary reperfusion therapy (fibrinolytic therapy: n=73,278 patients; percutaneous coronary intervention (PCI): n = 37,214 patients). Principal Findings: We found marked differences in time to reperfusion by race/ethnicity, with patients identified as African American/black on average having about 20% longer door-to-drug and door-to-balloon times than patients identified as white. This difference translates into times that are 7 minutes longer for door-to-drug time and 19 minutes longer for door-to-balloon time. We also found significant differences in times to acute reperfusion therapy for patients identified as Hispanic although the magnitude of these differences were modest (P-values < 0.01). A substantial portion of the differences were mediated by hospital-level factors. Even after additional adjustment for sociodemographic, insurance type, clinical, and admission data, patients identified as African American/black or Hispanic had significantly longer times to treatment after hospital arrival (P-values < 0.01) Conclusions: Differences by race and ethnicity persist in key quality indicators for cardiovascular care. Much of the differences are reduced after accounting for hospital-specific effects, suggesting that a substantial portion of the racial/ethnic disparities may be due to differences in the hospitals where minority patients are more likely to be treated, rather than differential treatment inside the hospital. Implications for Policy, Delivery or Practice: Our study has important implications for efforts to eliminate disparities in time to acute reperfusion. Although efforts to raise awareness of racial/ethnic disparities are important, our finding suggests the need for parallel efforts directed toward improving the care at hospitals around the country that are lagging in their quality, as measured by prompt treatment for patients with acute myocardial infarction. Interventions to eliminate racial/ethnic disparities are likely to fall short of their goals unless they are accompanied by systemic changes that can ensure all patients have access to high quality hospitals. Primary Funding Source: National Heart, Lung, Blood Institute • Veteran Status Is not an Independent Risk Factor for CABG Mortality William Weeks, M.D., M.B.A., Dorothy Bazos, Ph.D., David Bott, Ph.D., Edward Hannan, Ph.D., Michael Racz, M.A., Steven Wright, Ph.D., Elliott Fisher, M.D. Presented by: Dorothy Bazos, Ph.D., Associate Director, Rural Health Initiative, VA Medical & Regional Office Center-White River Junction, VT, VAMC(11Q), White River Junction, VT 05009; E-mail: Dorothy.Bazos@med.va.gov Research Objective: Recent studies demonstrating poorer cardiac care outcomes in VHA compared to the private sector raise the question of whether veteran status is an independent risk factor that explains these differences. Study Design: From New York’s Cardiac Surgery Reporting System (CSRS), we identified 3,032 enrolled veterans and 54,118 non-veterans who obtained isolated CABG between 1997-1999. Using the CSRS logistic regression model that adjusts mortality rates for patient and surgical characteristics, we compared risk-adjusted mortality rates for veterans to those for non-veterans undergoing surgery in private sector hospitals in New York. Using veteran status as a dummy variable in the regression model, we also calculated odds ratios for veteran compared to non-veteran mortality for each year and for the three-year period. Population Studied: 57,150 male residents of New York who obtained isolated Coronary Artery Bypass Grafting (CABG) from 1997-1999. Principal Findings: Although the expected mortality rate was somewhat higher for veterans (2.42 (95% CI:1.92-2.95)) vs. 2.19 (95%CI:2.07-2.31), veterans had slightly lower riskadjusted mortality rates compared to non-veterans undergoing CABG in private sector hospitals (2.05:95% CI:1.59-2.59 vs. 2.21:95%CI:2.09-2.34). We found no statistical difference in risk-adjusted mortality rates when comparing mortality rates in each year. Conclusions: In New York, although veterans have more severe disease than non-veterans, veteran status is not an independent risk factor for CABG mortality in the private sector, after adjustment for the case-mix measures available in the CSRS. Implications for Policy, Delivery or Practice: Additional studies are needed to assess whether factors other than illness burden account for the higher mortality seen within VHA. In areas where access is challenging and monitoring systems are in place, VHA should consider contracting for CABG services. Primary Funding Source: VA • Separate and Unequal: Hospital Racial Segregation and Disparity in Pressure Ulcers in New York State Kevin Fiscella, M.D., M.P.H., Sean Meldrum, M.S., Steve Barnett, M.D., Peter Franks, M.D. Presented by: Kevin Fiscella, M.D., M.P.H., Associate Professor, Family Medicine, University of Rochester School of Medicine & Dentistry, 1381 South Avenue, Rochester, NY 14620; Tel: 585.506.9484 Ext. 106; Fax: 585.473.2245; E-mail: Kevin_Fiscella@urmc.rochester.edu Research Objective: To examine the extent to which patient racial composition of hospitals explains racial disparity in pressure ulcers in New York State. Study Design: Cross-sectional, marginal effects models of hospital discharge data for adult acute care patients (New York State Inpatient Data 1998-2000). Initial model included patient characteristics (type of admission and length of stay, age, gender, ethnicity, income and insurance, and comorbidity) and hospital characteristics (bed size, ownership, teaching status, nursing and resident to bed ratios and total number of annual discharges). Final model included proportion of hospital discharges of black patients. Population Studied: 2.1 million patient discharges from acute care facilities in New York State 1998-2000. Principal Findings: African Americans (3.4%) had higher adjusted rates (0.9%; 95% CI 0.4 - 1.4%) of pressure ulcers than whites (2.5%) after controlling patient and hospital characteristics. This disparity was eliminated when proportion of black discharges by hospital was included in the model (0.01 %; 95% CI -0.1 - 0.3). Hospitals with larger percentage of black discharges showed significantly higher rates of pressure ulcers. Percentage of black discharges was strongly associated with percentage of hospital discharges that were insured through Medicaid and MSA size of the hospital location. Nonetheless, the relationship between percent black and pressure ulcer rate remained after adjusting for these factors. Conclusions: Racial disparity in pressure ulcers is largely explained by a single hospital characteristic: percentage of black patient discharges suggesting that hospital segregation is associated with adverse effects. Implications for Policy, Delivery or Practice: Further research is needed to confirm these findings for other quality measures and to determine whether they reflect the financial stress of heavily black hospitals. Primary Funding Source: AHRQ • Technology Diffusion, Geographic Variation, and Racial Disparities among Elderly Medicare Beneficiaries: 19892000 Peter Groeneveld, M.D., M.S., Sara Laufer, M.A., Alan Garber, M.D., Ph.D. Presented by: Peter Groeneveld, M.D., M.S., Assistant Professor of Medicine, University of Pennsylvania School of Medicine, 1122 Blockley Hall, 423 Guardian Drive, Philadelphia, PA 19104-6021; Tel: 215.898.2569; Fax: 215.573.8779; E-mail: petergro@mail.med.upenn.edu Research Objective: To determine if geographic differences in utilization of emerging medical technologies contributed to racial disparity in healthcare, and if reductions over 12 years in geographic variation in the use of selected procedures were accompanied by decreases in national rates of racial disparity for these technologies. Study Design: This was a retrospective cohort study. The outcome of interest was receipt of a selected emerging technology within 90 days of a hospital admission for a diagnosis that indicated eligibility. Multivariate logistic regression models were constructed to assess the effect of race, year of admission, and residence in a health service area with >30% black population on the primary outcome. Covariates included age, sex, clinical comorbidity, urban residence, race-specific, community levels of education and income, and admission to an academic hospital. For each technology, the interaction between year of admission and race was examined to assess for time trends in racial disparity. Similarly, interactions between year of admission and living in an health service area with >30% black population were examined to assess geographic diffusion into areas with larger black populations. Population Studied: 3,630,819 hospitalized, elderly Medicare beneficiaries potentially eligible, as determined by prespecified International Classification of Diseases-Ninth Revision diagnosis codes, for one of eight emerging medical technologies between 1989-2000. Principal Findings: Racial disparities were identified in seven of the eight selected technologies. Dual-chamber pacemaker implants, lumbar/lumbosacral spinal fusion, and cardiac electrophysiologic study rates, which showed no significant temporal changes in racial disparity from 1989-2000, demonstrated less variation (trend p<0.001 for all) between white and black geographic areas with time. Endoscopic biliary procedures were performed with progressively greater geographic variation (trend p=0.03), yet there was no concurrent exacerbation in national rates of racial disparity. Internal mammary artery coronary bypass grafting demonstrated decreased racial disparity with time (p=0.03 for trend), but with no observed change in geographic variation. The remaining 3 procedures (aortic valve replacement with tissue, interruption of the vena cava, and vaginal suspension/fixation) had no temporal change in either racial disparity or geographic variation. Conclusions: Reduction in the geographic variation of technology utilization in black and white areas was not associated with decreasing racial disparity. Conversely, the sole emerging technology for which racial disparity diminished had no change in geographic variation. We find little evidence to support the role of reduction in geographic heterogeneity as a driver of racial equity in healthcare. Implications for Policy, Delivery or Practice: Policies designed to reduce racial disparities by increasing procedure use in localities with large minority populations may not be effective. Local factors, rather than geographic variation among localities, may be the predominant cause of persistent racial disparity in health care. Primary Funding Source: NIA • The Effect of Cuts in Medicare Reimbursement on Quality of Hospital Care Meena Seshamani, Ph.D., Kevin Volpp, M.D., Ph.D. Presented by: Meena Seshamani, Ph.D., Medical Student, , University of Pennsylvania School of Medicine, Box 265, 3450 Hamilton Walk, Philadelphia, PA 19104; Tel: 215.901.6419; Fax: 215.573.8778; E-mail: meena.seshamani@marshallscholarship.org Research Objective: The Balanced Budget Act (BBA) of 1997 was introduced as a cost-saving measure that was designed to reduce Medicare reimbursements to health care providers by $116.4 billion from 1998 to 2002. There is concern that the financial strain induced by these revenue reductions could adversely affect the quality of patient care in hospitals. This study seeks to determine if hospitals under different levels of financial strain from the BBA had differential changes in 30day mortality for a variety of conditions, and to see if vulnerable patient populations such as the uninsured or minorities were disproportionately affected. Study Design: Pennsylvania hospital discharge data was obtained for fiscal years 1997 to 2001 for six conditions identified by the Agency for Health Care Research and Quality as Inpatient Quality Indicators. The hospital impact of the BBA was estimated using an American Hospital Association simulator that projected Medicare reimbursements with and without the BBA effects. A patient-level logistic regression analysis (n=807,723) examined the likelihood of dying within 30 days of admission in relation to fiscal year and hospital BBA impact (measured as top quartile, bottom quartile, and middle 50%), controlling for other hospital and patient characteristics. Differential effects of the BBA on uninsured patients and blacks were assessed using interaction terms with the BBA impact variable. To illustrate the effects of the BBA on health outcomes, the likelihood of death was estimated for the different hospital impact groups for insured and uninsured patients and for whites and blacks, holding all other patient and hospital characteristics constant. Population Studied: All patients in Pennsylvania hospitalized with one of six conditions, divided into conditions for which admission is non-discretionary (hip fracture, stroke, acute myocardial infarction, stroke) and for which admission may be discretionary (congestive heart failure, pneumonia). Principal Findings: The average magnitude of Medicare payment reduction on overall hospital net revenues was estimated at 2.0% for the low impact group and 4.1% in the high impact group in 1998, worsening to 2.9% and 5.2%, respectively, by 2000. Insured patients treated in high impact hospitals were found to have an increased likelihood of dying from conditions with non-discretionary admission (from 18.1% in 1997-98 to 19.4% in 2001) while patients from low impact hospitals had a decreased likelihood of dying (19.1% to in 1997-98 to 18.5% in 2001). These differences in the rate of change were significant (p<0.01). Uninsured patients were found to have a significantly larger increase in the likelihood of dying than insured patients in the high impact hospitals (22.8% in 1997-98 to 30.2% in 2001, p<.05) but the difference in the rate of change in mortality risk between the insured and uninsured patients in middle and low impact hospitals was insignificant (p=0.14). There was no differential effect between whites and blacks, nor were there any significant effects of the BBA on 30-day mortality rates for conditions with discretionary admission criteria. Conclusions: Increased financial strain in hospitals may adversely affect quality of patient care, particularly within vulnerable patient groups such as the uninsured. Implications for Policy, Delivery or Practice: Hospital reimbursement cuts may exacerbate existing disparities in care and should be considered in the evaluation of cost-saving policy reforms. Primary Funding Source: Doris Duke Foundation Related Posters Poster Session B Tuesday, June 8 • 7:30 a.m.-8:45 a.m. • Racial Differences in Diabetes Therapy Intensification and Glycemic Control Alyce Adams, Ph.D., Connie Mah, M.S., Fang Zhang, M.S., Stephen Soumerai, Sc.D., Ken Kleinman, Ph.D., James Meigs, M.D., M.P.H., Richard Grant, M.D., M.P.H., Steven Simon, M.D., M.P.H., Dennis Ross-Degnan, Sc.D. Presented by: Alyce Adams, Ph.D., Assistant Professor, Ambulatory Care and Prevention, Harvard Medical School, 133 Brookline Avenue, 6th Floor, Boston, MA 02215; Tel: 617.509.9863; Fax: 617.859.8112; E-mail: aadams@hms.harvard.edu Research Objective: Previous studies have identified failure to intensify therapy (“clinical inertia”) as one potential barrier to glycemic control among diabetes patients. To test this hypothesis, we assessed therapy intensification (from diet-only to oral drug therapy to insulin use) and glycemic control in black vs. white diabetes patients. Study Design: We used generalized estimating equations to estimate the odds of therapy intensification and of very poor glycemic control (HbA1c=10.0) among blacks vs. whites, controlling for patient characteristics (e.g., age, BMI, baseline HbA1c). Population Studied: We analyzed 2,303 patients from a large multispecialty care group in MA serving mostly privately insured patients. We included patients with a diagnosis of diabetes (diagnosis of diabetes on 1 inpatient claim or 2 outpatient encounters or = 1 diabetes drug dispensing; not gestational diabetes) in 1992 or 1993, who were 18 or older at diagnosis, and continuously enrolled from 1994 to 1999. Principal Findings: In multivariate models, blacks had significantly higher odds of very poor glycemic control (OR: 1.5; 95%CI: 1.2,1.8) but no greater likelihood of therapy intensification (OR: 0.97; 95%CI: 0.63,1.5) vs. white patients. Significant predictors (p<0.01) of therapy intensification included: number of physician visits, diet-only regimen at baseline, current HbA1c level, higher BMI, and higher baseline HbA1c. Conclusions: Black race was an independent predictor of very poor glycemic control but not of intensification of hypoglycemic therapy. Implications for Policy, Delivery or Practice: These findings suggest that observed racial differences in diabetes outcomes may be due more to system and patient level factors contributing to differences in control than to differences in treatment by race. Primary Funding Source: NIDDK • Predictors of Patient Compliance with Endoscopic Colorectal Cancer Screening Recommendations Nasar Ahmed, Ph.D., Tabassum Insaf, M.P.H., Ashar Ata, M.P.H., Steven Stain, M.D. Presented by: Nasar Ahmed, Ph.D., Director, Epi-Stat Division, Internal Medicine, Meharry Medical College, 1005 D.B. Todd Boulevard, Nashville, TN 37208; Tel: 615.327.5800; Fax: 615.327.5847; E-mail: nahmed@mmc.edu Research Objective: Colorectal Cancer (CRC) is the third leading cause of cancer death in the United States. Regular screening can greatly reduce the CRC mortality rates and the disease burden. Endoscopic screening has been shown to be effective in early diagnosis of CRC yet screening rates remain low. Physician recommendation is the determining factor for the screening. Among those who receive a physician’s recommendation a considerable portion is still not compliant. Not much is known about the correlates of their noncompliance. Our study examined predictors of patient compliance with endoscopic screening recommendation in US population. Study Design: We used the NHIS 2000 data. Bivariate and multivariate logistic regression analyses were used to evaluate the predictors of compliance with screening recommendation. Population Studied: There were 5733 adults over the age of 50 who were eligible for screening, did not have past history of colorectal cancer and visited a physician in the past year. Among these 1488 (27%) received a recommendation for endoscopic screening. 76% of those who received a recommendation were compliant. Principal Findings: Bivariate analysis shows that the elderly, males and retired personnel were more likely to be compliant. Insurance coverage and frequency of doctor visits were positively associated with compliance. Multivariate analyses showed increasing compliance with increasing age with the elderly (>74 years) being more than 3 times as likely to be compliant as 50-54 year old. Females were 53% less likely to be compliant. Blacks were 68% more likely to be compliant than Whites. Compliance increased with increasing level of education. College graduates were twice as likely to comply as compared to subjects who had not completed high school. The underweight were 77% less likely and the obese were 32% less likely to comply as compared to those with normal BMI. Current alcohol drinkers were 39% less likely to be compliant than lifetime abstainers of alcohol. Conclusions: Level of education, age and gender of patients, frequency of doctor visit, body mass index, alcohol use and being African American play a significant role in compliance with physician recommendation. Implications for Policy, Delivery or Practice: Physicians could educate the identified non-compliant groups to increase the effectiveness of screening recommendations. Interventions targeted to increase awareness of the risk of CRC among non-compliant groups should be developed. Primary Funding Source: NCI • Disadvantaged at Discharge: The Influence of Race and Education on Post-Acute Placement in Low Quality Nursing Homes Joseph Angelelli, Ph.D., David Grabowski, Ph.D., Vincent Mor, Ph.D. Presented by: Joseph Angelelli, Ph.D., Assistant Professor, Health Policy & Administration, Pennsylvania State, 116 Henderson, University Park, PA 16802; Tel: 814.865.5177; Fax: 814.863.2905; E-mail: jangel@psu.edu Research Objective: To determine whether African-American and other minority patients over age 65 are at greater risk of being discharged to the lowest quality nursing homes within a given Hospital Service Area (HSA). Study Design: The 2002 national Minimum Data Set (MDS) is used to examine patient and market factors predictive of admission into nursing homes. Population Studied: The sample is restricted to 150 HSAs with at least four freestanding nursing homes and at least 50 African-American patients age 65 and over admitted to those nursing homes in the calendar year, yielding a nationwide sample of 121,443 unique admissions to nursing homes. Principal Findings: Controlling for education, other demographic factors and clinical severity measures, AfricanAmericans are 32% (95% CI, 14-54) more likely than whites to be admitted to the lowest quality nursing homes in areas with multiple hospitals and 70% (95% CI, 4-279) more likely to be admitted to low quality nursing homes in markets with just one hospital. Individuals with no college education are 20% (95% CI, 7-34) more likely to be admitted to the lowest quartile of nursing homes in a given HSA. Conclusions: Our findings offer evidence that existing racial disparities in nursing home care are attributable in part to hospital discharge practices that direct minorities to lower quality nursing homes. Implications for Policy, Delivery or Practice: Education is also negatively related to placement in lower quality post-acute settings, suggesting the need for a new emphasis in the training of hospital discharge planners to better translate publicly available information about nursing home quality to prospective nursing home admissions and their families. Primary Funding Source: NIA • Racial and Socioeconomic Disparities in Mortality after Injury Melanie Arthur, Ph.D., Richard Mullins, M.D., Jerris Hedges, M.D., M.S. Presented by: Melanie Arthur, Ph.D., assistant professor, Sociology, Portland State University, P.O. Box 751, Portland, OR 97207-0751; Tel: 503.725.3615; Fax: 503.725.3957; E-mail: arthurm@pdx.edu Research Objective: Injury is a major cause of death in adults. Though racial disparities in access to medical care and health outcomes are well documented, trauma care is generally assumed to represent an exception to this pattern. We sought, using a nationally representative sample, to determine whether race was associated with risk of in-hospital death after injury. Study Design: We performed a risk-adjusted analysis of inhospital mortality after injury, controlling for age, gender, preexisting conditions, injury severity, primary payer, median income of zip code of residence, region and hospitalization at an urban teaching hospital, urban non-teaching hospital or rural hospital. Multivariate models were estimated using generalized estimating equations to control for clustering of patients within hospitals. Population Studied: From the Healthcare Cost and Utilization Project, years 1998-2000, we selected for analysis all patients age 18-64 with a primary diagnosis consistent with injury (ICD-9-CM codes 800-959, excluding late effects of injury). Excluded were all patients with discharge disposition indicating transfer to another acute care facility, and patients hospitalized in any of five states which do not release patient race data. Principal Findings: Relative to injured white patients, black patients had a higher likelihood of in-hospital mortality (2.1% versus 1.5%, multivariate odds ratio=1.15, p<.05). Other race/ethnicity groups showed no significant difference from white patients. There were significant differences in cause of injury between black and white patients, with 25% versus 32% injured in motor vehicle crashes and 26% versus 5% injured in an assault or attempted homicide. In stratified analyses, we found the largest racial disparities among mild to moderately injured patients (multivariate odds ratio=1.52, p<.001). Socioeconomic variables also showed an association with mortality, but did not eliminate the observed black/white disparity. Residence in a zip code with a median income of <$45000 was associated with higher odds of death for black patients but not for white patients, and lack of insurance was associated with increased mortality for patients of all ethnic groups (OR=1.72 relative to private insurance, p<.001). Conclusions: These data show that black patients have a higher risk of death after injury, even in models which control for health status, injury characteristics, and limited socioeconomic indicators. This association is strongest among hospitalized patients with mild to moderate injuries, where there is likely to be more discretion in treatment decisions. Further, we found evidence of socioeconomic disparities in mortality after injury, especially for black patients. It is unclear whether the observed disparities in mortality after injury are related to access to care or other unmeasured differences in injury characteristics and preexisting health status. Implications for Policy, Delivery or Practice: While these data do not offer the depth of information necessary to draw firm conclusions as to the cause of the observed disparities, they raise important questions about access to quality trauma care for black patients, residents of poor neighborhoods and the uninsured. Primary Funding Source: CDC • A Comparison of Title III Agencies Funded by the Minority AIDS Initiative Vs. All Other Title III Agencies Jill Ashman, Ph.D. Presented by: Jill Ashman, Ph.D., Health Statistician, HIV/AIDS Bureau Office of Science and Epidemiology, DHHS/HRSA, 5600 Fishers Lane, Room 7-90, Parklawn Building, Rockville, MD 20857; Tel: 301.443.4364; Fax: 301.594.2511; E-mail: JAshman@hrsa.gov Research Objective: To examine whether the characteristics of and clients served by Ryan White Title III agencies that were funded by the Minority AIDS Initiative were different from other Title III agencies. Study Design: The Means procedure in SPSS as well as Standard chi-square tests, when appropriate, were used to test for statistically significant differences (p<0.05) between the characteristics of and clients served by organizations receiving MAI funding with those agencies that did not receive MAI funding. Population Studied: Data are from the 2002 CARE Act Data Report, a required annual report for agencies receiving funding through the Ryan White Comprehensive AIDS Resources Emergency (CARE) Act. The 415 Title III agencies, all of which provide comprehensive primary health care services for individuals living with HIV disease, were divided into two groups, those that received funding through the Minority AIDS Initiative (MAI) (n=109) and those that did not (n=306). Congress established the MAI in 1999 in response to both the disproportionate impact of the HIV epidemic in minority communities and the disparities in documented morbidity and mortality data for African American persons with HIV/AIDS. The MAI was implemented as part of the existing Title III program and used to expand Title III funding to organizations serving communities of color in order to increase access to HIV primary care for highly impacted and/or underserved communities. Principal Findings: MAI-funded agencies were 1.5 times more likely to be located in the Southeast (34% vs. 20%) and Midwest (12% and 8%) and half as likely to be located in the Northeast, Northwest, Rocky Mountain, and Plains states (8% and 22%). They were equally likely to be located in CA, NJ, NY, and the Mid-Atlantic States. They were more likely to be publicly-funded community health centers (47% vs. 29%) and less likely to be hospitals (18% vs. 32%). Twice as many of the MAI funded agencies (56% vs. 27%) had over 50% of their staff and board members who were members of minority groups. The size of the agency, as measured by the number of HIV positive clients served, was the same for both groups. However, a larger percentage of patients at MAI-funded agencies were new HIV positive patients (an average of 33% of patients vs. 27%) and African American patients (an average of 56% of patients vs. 39%), and a smaller percentage of patients were White (on average 29% of patients vs. 45%) and male (on average 65% of patients vs. 69%). Conclusions: The Minority AIDS Initiative is a success. On average, they are reaching a larger percentage of new HIV patients as well as a larger percentage of African American patients than other Title III agencies, suggesting that they may be better equipped to outreach to these groups. Implications for Policy, Delivery or Practice: The MAI is reaching and providing quality care to African American patients living in areas that are disproportionately impacted by the HIV epidemic, and Congress should continue to earmark part of the Ryan White CARE Act Title III appropriation to this worthwhile program. • Are the Characteristics and Service Utilization Patterns of HIV-infected Individuals Who Were Reported as Deceased by the End of the Calendar Year Different from Those Patients Who Were Not Reported as Deceased? Jill Ashman, Ph.D. Presented by: Jill Ashman, Ph.D., Health Statistician, HIV/AIDS Bureau Office of Science and Epidemiology, Health Resources and Services Administration, 5600 Fishers Lane, Room 7-90, Parklawn Building, Rockville, MD 20857; Tel: 301.443.4364; Fax: 301.594.2511; E-mail: jashman@hrsa.gov Research Objective: To examine whether the characteristics and service utilization patterns of HIV-infected individuals who were reported as deceased at the end of the calendar year were different from those who were not reported as deceased. Study Design: Standard chi-square tests were used to test for statistically significant differences (p<0.05) between the demographic characteristics and service utilization patterns of HIV-positive patients who died by the end of the calendar year with HIV positive individuals who did not die. Data examined include client characteristics, health indicators, and service utilization including primary care as well as services that support individuals’ entry and retention in primary care. Population Studied: 2002 Year End Data from the Health Resources and Services Administration’s (HRSA) Client Demonstration Project (CDP) are used. Principal Findings: There were no statistically significant differences between the two groups for gender, race, being homeless and their likelihood to receive the following services: mental health and substance abuse treatment/counseling, dental care, housing assistance and emergency financial assistance. Individuals who died were more likely to be older, and they were less likely to be Hispanic. In addition, those who died were more likely to have either injecting drug use (IDU) or men having sex with men and injecting drug use (MSM&IDU) as their HIV exposure category (26% vs. 15%). Conclusions: Not surprisingly, HIV-infected patients who died in 2002 tended to be sicker than HIV-infected patients who did not die. The patients who died were more likely to receive hospice services as well as home health services, services that are designed for patients who are too sick to go to the doctor’s office. Individuals who died were also more likely to be IDUs. Implications for Policy, Delivery or Practice: More emphasis needs to be placed on getting IDUs into care early in their disease and finding effective ways to manage both their HIV and drug abuse so that IDUs stay healthy. • Diabetes Risk: Obesity and Physical Inactivity among Latino Ethnic Groups in California Susan Babey, Ph.D., Allison Diamant, M.D., MSHS, Neetu Chawla, M.P.H., E. Richard Brown, Ph.D. Presented by: Susan Babey, Ph.D., Research Scientist, School of Public Health, UCLA Center for Health Policy Research, 10911 Weyburn Avenue, Suite 300, Los Angeles, CA 90024; Tel: 310.794.6961; Fax: 310.794.2686; E-mail: sbabey@ucla.edu Research Objective: To estimate the prevalence of obesity and physical inactivity among Latino ethnic groups in California, and to identify the factors related to obesity and physical inactivity among Latino adults as indicators of diabetes risk. Study Design: We used data from the 2001 California Health Interview Survey (CHIS). CHIS 2001, a random-digit dial (RDD) telephone survey of more than 55,000 households drawn from every county in California, is the largest statewide health survey in the United States. The sample was designed to provide estimates for California's overall population, its major racial and ethnic groups, and a number of smaller ethnic groups. Logistic regression analyses were used to determine factors associated with obesity and physical inactivity among Latino adults. Factors examined included age, gender, and Latino ethnic group, as well as measures of access to health care, indicators of acculturation, physical activity and eating five or more servings of fruits and vegetables per day. Population Studied: We focused on adults, age 18 and older, who reported being of Latino or Hispanic origin and who reported they had not been diagnosed with diabetes. Principal Findings: Among Latino adults not diagnosed with diabetes, 22.7% were obese and 18.1% did not participate in physical activity. Obesity varied by Latino ethnic group with Latinos of Mexican heritage having the highest rate and South Americans the lowest rate of obesity (24.0% vs. 13.2%, p < 0.0001). After controlling for age, gender, education, income, and measures of access to care – Mexicans, those living in rural areas, those who do not participate in physical activity, and those who eat fewer than five servings of fruits and vegetables a day were more likely to be obese. Latino adults who lived in the US less than half of their lives were less likely to be obese than those born in the US. Lack of physical activity also varied by Latino ethnic group ranging from 11.3% among South Americans to 22.4% among Central Americans (p < 0.05). After controlling for age, gender, education, income, and measures of access to care – Latinos who eat fewer than five servings of fruits and vegetables a day and those who speak Spanish at home were more likely not to participate in physical activity. Conclusions: These findings suggest that the prevalence of obesity and physical activity level, both risk factors for diabetes, vary among Latino/Hispanic ethnic groups in California. In addition, mutable risk factors for obesity and participation in physical activity are present among Latinos. Implications for Policy, Delivery or Practice: Diabetes is a growing problem in California and the rest of the United States and Latinos are at particularly high risk for type 2 diabetes. Obesity and lack of physical activity are factors that increase the risk of developing type 2 diabetes. Identification of factors associated with obesity and lack of physical activity among Latinos can aid in the development of targeted interventions to reduce the risk factors for and thereby minimize the risk of developing diabetes among individuals in this population. Primary Funding Source: The California Endowment • Access to Specialty Care for Rural American Indians in Two States Laura-Mae Baldwin, M.D., M.P.H., Walter Hollow, M.D., Susan Casey, Ph.D., L. Gary Hart, Ph.D., Eric Larson, Ph.D., David Grossman, M.D., M.P.H. Presented by: Laura-Mae Baldwin, M.D., M.P.H., Associate Professor, Family Medicine, University of Washington, Box 354982, Seattle, WA 98195; Tel: 206.685.4799; Fax: 206.616.4768; E-mail: lmb@u.washington.edu Research Objective: The Indian Health Service (IHS) per capita expenditure for American Indian and Alaska Native (AI/AN) health services is less than half that spent per year on the U.S. civilian population. Many AI/ANs, especially in rural areas, depend on the IHS as their only source of funding for health care. Concerns have been raised that specialty services, which are largely funded through contracts with outside practitioners, are limited by this insufficient IHS funding. In this study, we explore medical providers’ perceptions of the level of access to specialty consultation services among rural AIs compared to their non-AI counterparts. Study Design: Cross-sectional study design in which three mailings of a 31-item questionnaire addressing access to specialty physicians, perceived barriers to access, and access to nonphysician clinical services were sent to primary care providers working in rural Indian and non-Indian health clinics in two Western states. Population Studied: 115 physicians, nurse practitioners, and physician assistants working in rural Indian health clinics in Montana and New Mexico and 96 physicians, nurse practitioners, and physician assistants working in rural nonIndian clinics within 25 miles of the Indian clinics. Principal Findings: Montana’s rural Indian clinic providers reported poorer patient access to specialty care than providers in rural non-Indian clinics, while New Mexico’s providers reported comparable access. Rural Indian clinic providers in both states most frequently cited financial barrier to specialty care. Rural Indian clinics providers in both states reported better access to several nonphysician services than rural nonIndian clinic providers. Conclusions: Rural primary care providers report restricted specialist access for Indian patients compared to non-Indian patients in Montana, where they are dependent on private, community-based specialists, but not New Mexico, where a contractual agreement with a tertiary-care university hospital exists. In both states, financial factors serve as significant barriers to rural Indian and non-Indian patients’ access to specialists. The multidisciplinary approach to care taken in many IHS and tribal-administered clinics is associated with greater perceived access to nonphysician services among rural Indian compared to non-Indian clinic providers. Implications for Policy, Delivery or Practice: Ensuring specialty care access for rural Indian patients nationwide will require equitable and adequate funding for the Indian Health Service as well as well developed specialty referral relationships and systems. Primary Funding Source: Federal Office of Rural Health Policy • Improving Health Care Quality For Racial/Ethnic Minorities: A Systematic Review of Interventions Mary Catherine Beach, M.D., M.P.H., Tiffany Gary, Ph.D., Eboni Price, M.D., Karen Robinson, M.Sc., Aysegul Gozu, M.D., Ana Palacio, M.D., M.P.H., Carole Smarth, M.D., Mollie Jenckes, M.H.S., R.N., Carolyn Feuerstein, B.A., Eric Bass, M.D., M.P.H., Neil Powe, M.D., M.P.H., M.B.A., Lisa Cooper, M.D., M.P.H. Presented by: Mary Catherine Beach, M.D., M.P.H., Assistant Professor, Medicine, and Health Policy & Management, Johns Hopkins University, 2024 East Monument Street, Suite 2-500, Baltimore, MD 21287; Tel: 410.614.1134; Fax: 410.614.0588; Email: mcbeach@jhmi.edu Research Objective: Racial and ethnic disparities in health care quality have been extensively documented, but little is known about the effectiveness and cost of strategies to improve the quality of care for racial/ethnic minorities. We synthesized findings of studies evaluating interventions targeted at health care providers to improve health care quality and/or reduce disparities in care for racial/ethnic minorities. Study Design: We performed a systematic review of literature from 1980 through June 2003 using electronic and hand searches to identify studies that evaluated interventions designed to improve health care quality and/or reduce disparities in care for racial/ethnic minorities. Population Studied: Eligible studies were in English, had original data, were conducted in the United States, focused on providers or organizations and were either randomized controlled trials or concurrent controlled trials. Two reviewers abstracted data on the effectiveness and cost of these interventions. We synthesized and graded the strength of the evidence as excellent, good, fair or poor using predetermined criteria. Principal Findings: There were 27 studies that met criteria for review. Almost all (n=26) took place in the primary care setting, and most (n=19) focused on improving the provision of preventive services. Only two studies were designed specifically to meet the needs of racial/ethnic minority patients. All 10 studies that used a provider reminder system for the provision of standardized services (mostly preventive)reported favorable outcomes (excellent evidence). The following quality improvement strategies demonstrated favorable results but were used in a small number of studies: bypassing the physician using a nurse or medical assistant to offer preventive services directly to patients (2 of 2 studies favorable), provider education alone (2 of 2 studies favorable), use of a structured questionnaire to assess adolescent health behaviors (1 of 1 study favorable), and use of remote simultaneous translation (1 of 1 study favorable). Interventions that used more than one main strategy (multifaceted) were used in 9 studies with inconsistent results (fair evidence). There are limited data on the costs of these strategies because only one study reported data on costs. Conclusions: There are several promising strategies that may improve health care quality for racial/ ethnic minorities, but a lack of studies specifically targeting the disease areas and the processes of care for which disparities have been documented. Implications for Policy, Delivery or Practice: Further research is needed to evaluate strategies designed to reduce disparities in health care quality for racial/ ethnic minorities. These studies will determine whether generic quality improvement strategies are adequate to eliminate minority health care disparities or whether interventions need to be specifically targeted to reduce disparities. This work will also guide decision-making regarding health resource allocation and organization and delivery of health services to ethnic minorities. Primary Funding Source: AHRQ • Beyond Race & Ethnicity: A Statewide Strategic Approach to Reducing Asthma in California Lisa Benton, M.D., M.P.H., Barbara Cowan, M.P.H, Rick Kreutzer, M.D. Presented by: Lisa Benton, M.D., M.P.H., Public Health Medical Officer/ Health Disparities Specialist, California Department of Health Services, California Breathing, 1515 Clay Street, Suite 1700, Oakland, CA 94612; Tel: 510.622.4453; Fax: 510.622-4902; E-mail: lbenton@dhs.ca.gov Research Objective: Interventions targeting inequity in asthma morbidity and mortality focus on eliminating health disparity primarily through introducing culturally-appropriate training and education to patients and providers, and by targeting unequal access to health care services. Strategies and interventions addressing other indicators of health disparity and poorer health outcomes are less widely implemented. Alternative strategies that highlight improving intermediate outcomes in environmental asthma triggers and promote “asthma friendly” homes, communities, schools, and work places, will redistribute the economic and social burden of asthma and mobilize stakeholders for advocacy and sustainable change. Through introduction of participatory action research models focused on the objectives of the Strategic Plan for Asthma in California, the California Department of Health Services intends to promote formation of broad-based coalitions for education, advocacy, and treatment of asthma. Study Design: The five (5) goals and twenty-eight (28) objectives of the Strategic Plan for Asthma in California were examined. Strategies targeting each objective were identified within the five-year California Breathing initiative beginning in 2003. Key informant interviews, case studies, and focus groups were conductive and combined with available descriptive epidemiology studies of asthma prevalence within California. Follow-up stakeholder meetings and expanded epidemiology studies were convened in response to stakeholder needs for information, technical assistance, intervention formulation, and outcome analyses. Population Studied: Key informant interviews, case studies, and focus groups composed of individuals having distinct roles for actualizing the CA Strategic Plan for Asthma: patients, parents, caretakers, health care providers, educators, community based organizations and stakeholder advocacy organizations, scientists, and researches with interests in reducing gaps in asthma morbidity and mortality within CA. Principal Findings: The literature is replete with data supporting disparities of health outcomes attributable to race and/or ethnicity. A much smaller body of literature posits sustainable strategies to eliminate these disparities or expands the examination of health disparities to alternate inequities. Key informants and focus group participants express wide awareness of disparities related to race/ethnicity, and also significant recognition of disparities associated with access, quality of life, and other social and economic determinants of health such as housing, food, transportation, and work. Participants wanted solutions rather than further descriptions of the problem from researchers and health care agencies, provided local knowledge, and focused study questions. Participants readily conceptualized solutions that addressed their immediate needs and involved their larger communities. Conclusions: In the case of asthma disparities in California, the frame of racial and/ethnic disparities is emphasized. While racial and/ethnic differences probably contribute to the unequal burden of asthma, dynamic disparities such as those pertaining to quality of life, work, and play seem to hold distinct roles in the California asthma morbidity and mortality patterns. Key informants, focus groups, and other stakeholders implicitly recognize this and believe that building partnerships for education, research, and advocacy to address asthma triggers and wider societal disparities will lead to sustainable declines in asthma morbidity and mortality. Implications for Policy, Delivery or Practice: In an environment of decreasing resources and increasing gaps in health care services, interventions targeting racial and ethnic disparities would become more effective when integrated into a global health disparities framework that will shift the economic and social burden to improve asthma outcomes to a wider circle of stakeholders. Primary Funding Source: CDC • Variation in Expectations and Satisfaction of Health Care Services among Disabled Minorities in the Medicare Feefor-Service Program Shulamit Bernard, Ph.D., R.N., Nathan West, MPA, Elvessa Aragon-Logan, M.S. Presented by: Shulamit Bernard, Ph.D., R.N., Director, Program on Health Care Quality and Outcomes, Division of Health Economics Research, RTI International, 3040 Cornwallis Road, Research Triangle Park, NC 27709; Tel: 919.967.9393; Fax: 919.990.8454; E-mail: sbernard@rti.org Research Objective: To examine patterns of reported experiences and satisfaction with health care services among a population of disabled Medicare Fee-for-Service beneficiaries. We give particular attention to disabled minorities since preliminary findings indicate greater differences in reported health care experiences and satisfaction levels among racial minority groups. Study Design: Data from the 2000-2002 Medicare CAHPS® Fee-for-Service surveys were combined to create an analysis file with 344,342 survey respondents. In order to identify the original reason for Medicare eligibility, we created a variable that determines whether a sample member has ever been entitled to Medicare benefits due to disability (prior to turning 65 years of age) from the CMS Enrollment Database (EDB). We determined that 16.1 % of the respondents had ever been entitled due to disability alone or disability and End Stage Renal Disease (ESRD). Survey data were weighted, then casemix adjusted using the CAHPS® 3.4 Survey and Reporting Kit macros Population Studied: Beneficiaries enrolled in the Medicare Fee-for-Service program between 2000-2002. Principal Findings: We found that disabled Medicare beneficiaries consistently report more problems in all composites and ratings as compared with the non-disabled, and these differences are even greater among disabled minorities. For instance, approximately 14 percent of disabled Native Americans reported having a big problem getting necessary care compared to only 6 percent of non-disabled Native Americans during 2000 - 2002. Similarly, about twice the proportion of disabled African-Americans reported having a big problem getting necessary care compared to nondisabled African Americans during the same period (9 percent vs. 4 percent). With regards to satisfaction levels of health care services, disabled and non-disabled beneficiaries gave similarly high ratings for their personal doctor and specialists. However, disabled beneficiaries gave lower ratings for their overall health care and the Medicare plan. This is particularly true among disabled African Americans and Native Americans, who gave fewer most positive (“10”) ratings than their non-disabled counterparts. Conclusions: Our findings suggest that disabled minorities in the Medicare program experience greater problems obtaining needed care, getting care quickly, and communicating with their physicians as compared with non-disabled minorities as well as lower satisfaction with the Medicare program and their overall health care. This pattern persists for the over 65 disabled population as well as for the younger disabled beneficiaries. Implications for Policy, Delivery or Practice: The findings suggest that despite the insurance coverage offered by the Medicare program, the disabled experience more barriers and delays to obtaining health care services. This is particularly true for certain racial minorities, among them African Americans and Native Americans. Further studies are needed to examine the impact of these differences in perceived access and satisfaction on the quality of health care and outcomes for the disabled. Primary Funding Source: CMS • Hispanic vs. non-Hispanic White Disparities in Access among Rural Elders Tyrone Borders, Ph.D. Presented by: Tyrone Borders, Ph.D., Assistant Professor and Chief, Health Services Research, Texas Tech University Health Sciences Center, 3601 4th Street, MS 8161, Lubbock, TX 79430; Tel: 806.743.6984; Fax: 806.743.1292; E-mail: tyrone.borders@ttuhsc.edu Research Objective: The purpose of this study was to examine whether there were Hispanic versus non-Hispanic disparities in reports of eight dimensions of health care access among community-dwelling elders residing in a rural region of the southwestern United States. Study Design: A cross-sectional, population-based telephone survey of approximately 2,100 Hispanic and non-Hispanic whites age 65 and older. Reports of several dimensions of access were adapted from the CAHPS. These included reports of the ability to obtain care (see personal doctor/nurse, see specialist, obtain help over phone, and obtain transportation to the clinic) and reports of the ability to obtain care without a long wait (get help over the phone without a long wait, see provider for illness/injury when wanted, see provider for routine care when wanted, and have short office waiting times). Independent variables included predisposing, enabling, and need factors. Univariate and multivariate logistic regression analyses were conducted. Population Studied: The study data were collected among community-dwelling elderly persons (age 65 years and older) residing in the 46 rural (counties with fewer than 50,000 persons) and 50 frontier counties (counties with fewer than 50,000 persons and fewer than 7 persons per square mile) of West Texas. Principal Findings: In unadjusted analyses, Hispanic elders had worse reports of their ability to always/usually see their personal doctor, see a specialist, obtain transportation to the clinic, see a doctor for illness/injury when wanted, and see a doctor for routine care when wanted. In adjusted analyses, only two reports (always/usually able to see a doctor/nurse for illness or injury when wanted and always/usually able to see a doctor/nurse for routine care when wanted) differed significantly by ethnicity. Conclusions: The results indicate that rural, older Hispanics experience greater problems with several dimensions of access, but many of their problems are attributable to enabling factors, rather than ethnicity itself. Implications for Policy, Delivery or Practice: Rural medical care providers and managers should consider directly targeting Hispanics to improve their timely access to acute and routine care. Strategies may include expanding office hours or transportation services. Moreover, health policy makers should consider expanding health insurance benefits to improve the accessibilty of personal doctors and specialists among Hispanic and non-Hispanic white elders alike. Primary Funding Source: AHRQ • The Meaning of Self Rated Health in Different Populations Ann Boulis, Ph.D., Judith Long, M.D. Presented by: Ann Boulis, Ph.D., Post Doctoral Fellow, Sociology, University of Pennsylvania, 3718 Locust Walk, Philadelphia, PA 19104-6299; Tel: 215.8986722; Fax: 215.573.2081; E-mail: aboulis@pop.upenn.edu Research Objective: To better understand how social characteristics affect the determinants of self-rated health, and to ultimately examine whether persistent race, class and sex based differences in self-rated health stem, in part from differences in how these groups define health. Study Design: Data from the 1995-96 National Survey of Midlife Development were used to assess how the correlates of self-rated health differ for more and less educated individuals, men and women, and whites and non-whites. The survey’s measure of self-rated health was dichotomized to equal 1 if respondents indicated they had very good or excellent health and 0 otherwise. This variable was then regressed on a series of covariates measuring respondents’ physical and emotional health as well as key aspects of their current and past life conditions. Population Studied: The National Survey of Midlife Development in the U.S. (MIDUS) is a nationally representative random-digit-dial sample of 4,242 noninstitutionalized, English-speaking adults, aged 25 to 74. Principal Findings: hese analyses suggest a striking similarity in the correlates of self rated health for those with a bachelor’s degree or more and those with less than a bachelor’s degree. The one exception is effort put into work. Regardless of educational level, self reported work effort is positively associated with self-rated health. However, the strength of this relationship is significantly more pronounced for those with less than a college degree. In contrast to our assessment of education, we find that gender interacts with several correlates of self-rated health. Most notably, health problems or chronic conditions are a stronger correlate of self-rated health for women than for men, while work effort is a stronger determinant of self-rated health for men than for women. Finally, we find two key differences between the correlates of self rated health for whites and non-whites. First, BMI is a significant correlate for whites and not for non-whites. Second, perceived neighborhood quality is a significant correlate for whites, but not for non-whites. Conclusions: These results suggest that social characteristics such as education, gender and race influence a person’s definition of their overall health. They also imply that social conditions such as job characteristics and neighborhood quality can contribute to individuals’ understanding of the overall health. Implications for Policy, Delivery or Practice: Public health professionals may enhance their ability to promote minority health by developing a better understanding of how such communities define health. • What Modifies the Negative Effect of Poverty on Functional and General Health Status Measures? Janet Bronstein, Ph.D., Shailender Swaminathan, Ph.D., Joshua Klapow, Ph.D. Presented by: Janet Bronstein, Ph.D., Professor, Health Care Organization and Policy, University Alabama at Birmingham, 1350 Third Avenue South, Birmingham, AL 35294-0022; Tel: 205.975.8962; Fax: 205-934-3347; E-mail: jbronste@uab.edu Research Objective: Most studies show a clear gradient in health status measures related to individual poverty levels, with the steepest gradient occurring at the lowest income levels. This study compares the relationship between poverty levels and the physical component of the SF12 and a global rating of health status and assesses the extent to which other demographic factors modify the impact of poverty for the two measures. Study Design: We group individuals surveyed in the household survey component of the Community Tracking Study (a study of 60 representative communities in the U.S.) into four poverty level categories, (1) below 125% FPL, (2) 125200% FPL, (3) 200%-300% FPL and (4) above 300% FPL. We successively add measures of race, education, region, rurality and a measure of income inequality in the county and assess the relationship between these factors and the PCS12 (reported physical health status) and global health status (reports of health status ranging from excellent through poor). Standard errors are corrected for the stratified nature of sampling design. Population Studied: We include all adults over age 17 responding to Round 3 of the household survey component of the Community Tracking Study and those adults responding in Rounds 1 and 2 who were not represented in Round 3, for a total sample size of 90,276. Fifty seven percent of the sample was above 300% of the FPL; the remaining respondents were almost equally distributed across the other three income categories. Principal Findings: Controlling for age and sex, poverty level is highly correlated to both health status measures, with the lowest income groups most likely to have both lower PCS12 scores and more respondents reporting poor overall health. All non-white individuals report worse health status than white individuals, with African Americans reporting lowest scores for both health measures. When poverty level is controlled , all non-white individuals report lower health status than white individuals, but Hispanics are not different from whites on the PCS12. When education is controlled, Hispanics score significantly higher than whites on the PCS12, but still report worse overall health. Education is positively correlated to both health measures, and reduces the negative effect of poverty on the health status measures by about 25%. Controlling for individual factors, residents of very rural areas and Southern states have lower PCS12 scores. Residents of Southern and Midwestern states also report worse global health on the general health status measure. Our measure of income inequality in the county of residence was not significantly associated with health status measures. Conclusions: Poverty is a persistent risk factor for poor perceived health status, measured either as level of physical functioning or report of overallperceived health quality. African American and Native/Asian ethnicities are additional but much less influential risk factors. Education is protective for the health risks of poverty. Some geographic areas have residents of poorer health across all income, ethnicity and education categories. Implications for Policy, Delivery or Practice: Income differences are the major source of disparities in health status for the U.S. population. Primary Funding Source: University of Kentucky Center for Poverty Research • Disparities in Diabetes Management: Self-Monitoring of Blood Glucose and Medication Use in a Population-Based Sample Neetu Chawla, M.P.H., Susan Babey, Ph.D., Allison Diamant, M.D., M.S.HS, E. Richard Brown, Ph.D. Presented by: Neetu Chawla, M.P.H., Research Associate, UCLA Center for Health Policy Research, 10911 Weyburn Avenue, Suite #300, Los Angeles, CA 90024; Tel: 310.794.8362; Fax: 310.794.2686; E-mail: nchawla@ucla.edu Research Objective: To identify disparities in glucose monitoring and medication use as indicators of diabetes management in a population-based sample of California adults. Study Design: This study used data from the 2001 California Health Interview Survey (CHIS). CHIS 2001 is a random-digit dial (RDD) telephone survey of 55,428 households drawn from every county in California and is the largest statewide health survey conducted in the United States. The sample was designed to provide estimates for California's overall population, its major racial and ethnic groups, and a number of ethnic subgroups. Logistic regression analyses were used to determine factors associated with glucose monitoring practices and medication use among adults with diabetes. Factors studied include age, gender, race/ethnicity, income level, education, level of acculturation, insurance status, having a usual source of care, and duration of diabetes. Population Studied: The population studied was California adults, age 18 and older, who reported that they had been diagnosed with diabetes. Principal Findings: Latinos and Asian/Pacific Islanders had higher rates of inadequate glucose monitoring compared to whites (p<0.01). After controlling for factors such as gender, race/ethnicity, income, and education, multivariate regression analysis showed that Latinos, recent immigrants, adults 65 and older, the uninsured, those without a usual source of care, and those who had a shorter duration of diabetes (3 years or less) were significantly more likely to inadequately monitor their blood glucose compared to other groups. Similar analyses were conducted for medication use, examining the outcome of not taking any medications for diabetes. Latinos had higher rates of not using medication compared to Asian/Pacific Islanders (p<0.01), American Indian/Alaska Natives (p<0.05), African Americans (p<0.001), and whites (p<0.001). In a multivariate model, our results showed that the following groups were more likely to not use medications: younger adults, females, those with no usual source of care, and adults who have shorter diabetes duration. Conclusions: These findings suggest that Latinos, recent immigrants, those with shorter diabetes duration, and those lacking access to health care are more likely to inadequately monitor their glucose. In addition, young adults, women, those without a usual source of care, and those having shorter diabetes duration may not be taking needed medications. Therefore, these groups may be at increased risk for inappropriate management of diabetes. Implications for Policy, Delivery or Practice: Inadequate glucose monitoring and lack of medication use are indicators of poorly managed diabetes, which can result in increased risk of complications, poorer health, and increased healthcare costs. Programs promoting self-monitoring of blood glucose should be implemented, particularly targeting Latinos, recent immigrants, adults with diabetes who are 65 and older, those who have shorter diabetes duration, and those lacking health insurance or a usual source of care. In addition, interventions that help ensure continuity of diabetes care and target adults with no usual source of care, younger adults, women, and those who have shorter diabetes duration could improve rates of medication use among California’s adults with diabetes. Primary Funding Source: The California Endowment • Cost of Hospital Admissions Attributable to Minority Health Disparities in South Carolina Kit Simpson, Dr.P.H., Elinor Chumney, Ph.D., Patrick Mauldin, Ph.D., Helen Gary, M.P.H., Jennifer Mazyck-Brown, Pharm.D. Presented by: Elinor Chumney, Ph.D., Assistant Professor, Pharmacy Practice, Medical University of South Carolina, 280 Calhoun Street, Charleston, SC 29425; Tel: 843.876.1242; Fax: 843.792.1712; E-mail: Chumneye@musc.edu Research Objective: To measure the cost of racial health disparities resulting in hospital admissions over a five year period. Study Design: Retrospective analysis of archival data to measure expected versus observed admission rates, charges, and estimated costs for black and white patients stratified by major diagnostic category (MDC) and age. Population Studied: All patients admitted to SC hospitals during the 1998-2002 time period with a code of black or white on the race variable. Principal Findings: The admission rate for black patients was higher than the observed rate for white patients in all but the 2 MDCs containing joint replacement and mental health admissions. Annual charges for hospital admissions attributable to disparities in health status between white and black patients of similar age range from $253 to $423 million. The largest contributers to the cost of admissions due to minority health disparities were admissions for stroke, seizures, headache, pneumonia, bronchitis, amputations, heart failure, diabetes, nutritional/metabolic problems, renal failure, kidney and UTI infection, medically complicated deliveries, sickle cell disease, septicemia, and HIV/AIDS. Conclusions: Large disparities in the health of black and white patients of similar age result in much higher age-adjusted hospital admission rates for black patients in SC when compared to whites. These disparities resulted in more than 1.6 billion in hospital charges over 5 years. Many admissions were for conditions that could be avoided with preventive interventions, or which would be managed in a community setting if patients had access to primary care. While some of these differences in hospital admission rates could be due to patient or provider preferences, we expect that most of the differences observed in this study are due to true differences in health status and medical care needs. Implications for Policy, Delivery or Practice: The existence of minority health disparities is enormously costly to the health care system and should be actively addressed by improving minority access to primary and preventive care. Primary Funding Source: AHRQ, National Institute of Ageing • Obstetric and Sociodemographic Factors Associated with Epidural Anesthesia During Labor and Vaginal Delivery Emily Belmont Conn, Ron Keren, M.D., M.P.H. Presented by: Emily Belmont Conn, Student, Pediatrics, University of Pennsylvania/Children's Hospital of Philadelphia, 166 Gramercy Road, Bala Cynwyd, PA 19004; Tel: 267.679.4017; Fax: 215.590.0426; E-mail: ebconn@sas.upenn.edu Research Objective: The decision to use epidural anesthesia during childbirth is a complex one, involving considerations of patient preferences, obstetric history, and provider practice style. The objective of this study was to explore the relationship of obstetric and sociodemographic factors to receipt of epidural anesthesia during labor and vaginal delivery. Study Design: This was a retrospective cohort study. The outcome variable was receipt of epidural anesthesia during labor and vaginal delivery. The predictor variables were obstetric and sociodemographic factors. Population Studied: The population studied was 2568 women who delivered vaginally between 1993 and 1997 at an urban community teaching hospital in Pennsylvania and took part in the hospital supervised early discharge follow-up program. Principal Findings: 1753 (68.26%) women received epidural anesthesia during labor. In a multivariable logistic regression model, the following factors were associated with receipt of epidural anesthesia: race/ethnicity (as compared to white): African American (odds ratio [OR] = 0.75; 95% confidence interval [95 % CI], 0.57-0.97), Hispanic (OR = 0.70; 95% CI, 0.42-1.19), Asian (OR = 0.47; 95% CI, 0.30-0.72), and other (OR = 0.42; 95% CI, 0.19-0.93); infant birth weight (/kg) (OR = 1.37; 95% CI, 1.07-1.75); forceps delivery (OR = 11.79; 95% CI, 4.59-30.25); vacuum delivery (OR = 2.53; 95% CI 1.75-3.67); oxytocin induction or augmentation (OR = 6.01; 95% CI, 4.917.36); and parity (OR = 0.75; 95% CI, 0.69-0.82). The model controlled for median household income, maternal age, driving time to the hospital, gestational age, prolonged rupture of membranes, and the gender of the infant. Conclusions: Controlling for known predictors of epidural anesthesia, women of Asian, African American, and other racial background received epidural anesthesia during labor and vaginal delivery less often than white women. Implications for Policy, Delivery or Practice: Additional research is needed to understand whether healthcare system factors, educational and cultural differences, patient preference, and/or provider bias are responsible for these disparities. • Gender, Race, and Age Differences in the Receipt of Preventive Services for Cardiovascular Risk Factors Rosaly Correa-de-Araujo, M.D., M.Sc., Ph.D., Sari Siegel, MA, Ernest Moy, M.D., Denise Remus, Ph.D., R.N., Francis Chesley, M.D. Presented by: Rosaly Correa-de-Araujo, M.D., M.Sc., Ph.D., Senior Advisor on Women's Health, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850; Tel: 301.427.1550; Fax: 301.427.1562; E-mail: rcorrea@ahrq.gov Research Objective: Coronary heart disease accounts for the majority of cardiovascular disease deaths in women, disproportionately affecting minorities. Because the condition is often fatal and nearly 2/3 of women who die suddenly have no prior recognized symptoms, it is critical that this priority population be targeted with adequate delivery of preventive services. This study compares the effectiveness of primary care for cardiovascular disease risk factors in both women and men in age groups below and above 65 years old. Study Design: Evaluation of 5 quality measures used in the National Health Care Quality and National Health Care Disparities Reports. These measures were derived from a variety of national data sources reflecting health care information for year 2000 (National health Interview Survey [NHIS] and Medical Expenditure Panel Survey [MEPS]). Population Studied: Both women and men age 18 and over,from a variety of national data sources reflecting health care information for year 2000 (National health Interview Survey [NHIS] and Medical Expenditure Panel Survey [MEPS]). Principal Findings: Elderly individuals (65 and up) are more likely to receive preventive services (blood cholesterol measurement, blood pressure measurement, and smoking cessation counseling) compared to younger adults. Gender and race differences among younger adults indicate that: women of lower socioeconomic status are less likely to have their blood cholesterol checked; both black women and men have higher rates of blood pressure measurement, while women and men with low income status are less likely to have their blood pressure measured and to receive counseling to quit smoking; Hispanic women are less likely than nonHispanic white women and men to receive advice to quit smoking; data are limited or show no significant differences in the percentage of young adults with diabetes who had their HbA1c measured at least once in the past year. Conclusions: Elderly individuals seem to receive adequate preventive services, while among younger adults opportunities for prevention are frequently missed particularly among minorities. Black women and men are doing well as relates to blood pressure measurement, but due to the seriousness of risk factors in the development of fatal cardiovascular outcomes in these populations improvements in preventive care are recommended. Implications for Policy, Delivery or Practice: These results are useful for health care professionals, policymakers, and health system leaders working to reduce disparities by improving access, receipt, and quality of care. Primary Funding Source: AHRQ • A Qualitative Assessment of Charlotte REACH: An Ecological Perspective for Decreasing CVD and Diabetes among African Americans Rita DeBate, Ph.D., M.P.H., CHES, Marcus Plescia, M.D., M.P.H., Denis Joyner, M.P.H., LaPronda Spann, BS Presented by: Rita DeBate, Ph.D., M.P.H., CHES, Assistant Professor, Health Behavior and Administration, University of North Carolina at Charlotte, 9201 University City Boulevard, Charlotte, NC 29201; Tel: 704.687.2866; Fax: 704.687.6122; E-mail: rdigioac@email.uncc.edu Research Objective: The Charlotte REACH 2010 project is part of a national collaborative effort of the Centers for Disease Control and Prevention to eliminate health disparities among identified population groups through community driven interventions. The Charlotte initiative focuses on the reduction and control of cardiovascular disease and diabetes in the Northwest Corridor of Charlotte. An ecological perspective of health promotion was utilized as the framework for a Charlotte community-based intervention to eliminate health disparities in cardiovascular disease and diabetes. This ecological approach involves interventions targeted on five levels of influence with interaction between levels creating a supportive system for sustained change. In order to create sustained change, all levels of influence must be addressed and designed to work together to create a strong, supportive environment for change. Due to the complexity of multileveled ecological interventions, feedback on the process and impacts of the activities is crucial for ensuring success.The purpose of this qualitative assessment was to explore changes that have occurred among and between the following levels of influence: intrapersonal, interpersonal, organizational, community, and policy. Study Design: An exploratory assessment of the Charlotte REACH initiative was conducted using focus group methodology. A qualitative approach was chosen for this assessment as it enabled the researchers to facilitate an exploration of the process and initial impacts of the ecologically framed health promotion program. Qualitative methodology included 10 focus groups. Three independent coders hand-coded all focus groups utilizing modified coding methods developed by Spradley. Coding was then compared and an agreement of final codes was reached. Final codes were entered into NVivo qualitative analysis software. Once entered, codes were compared and contrasted into overarching themes and sub-themes. Population Studied: The geographic area of this initiative is bordered by three connected thoroughfares and contains a population of 19,670 of which approximately 95% are African American. Local health disparities in cardiovascular disease and diabetes have been documented in community health surveys and assessments. This qualitative assessment consisted of 10 focus groups. The focus groups were conducted with the Charlotte REACH Lay Health Advisors (1) Charlotte REACH program staff (1), residents of the target population who have participated in Charlotte REACH program activities (4), and residents of the target area who had not participated in Charlotte REACH activities (4). Principal Findings: A total of 84 participants were involved in the focus groups; 12 Lay Health Advisors, 6 program staff, and 66 community residents (29 who participated in REACH activities and 37 who have not participated in REACH activities). The focus group methodology implemented in this exploratory assessment yielded rich descriptive data regarding the status of the development of supportive system for sustained change. Overall, the findings from this study support positive changes within and between levels of change. Intrapersonal level changes were identified among target area residents who have participated in REACH activities. Changes in knowledge, attitudes, and behavior regarding cardiovascular disease and diabetes prevention strategies were voiced among participants in various REACH activities including nutrition groups, diabetes support groups, and exercise interventions. Participants also noted improvements in health status. In addition, LHAs changed their perception of health from a diseased focus definition to a prevention oriented one. Interpersonal mediators include support and role definition from peers, family, and friends. LHAs have been established as peer role models and provide individual support for residents in the target community. These findings demonstrate interpersonal support among program participants through camaraderie that has been developed within the various program activities. Participants expressed that this fellowship is a motivating factor for continuation of health promoting activities. Evidence of interaction between intrapersonal and interpersonal levels is supported by the diffusion of knowledge, skills, and behaviors from REACH participants to various family members. Organizational level changes include institutional/organizational rules, policies or informal structures that promote targeted behavior change. The majority of REACH program participants stated their primary care physician referred them to REACH activities. The informal structure of utilizing the prescription pads when referring patients who are in need of nutritional changes, exercise or smoking cessation provided a cue to action for their patients. Additionally, a formal communication structure was developed with the LHA as the liaison between the community residents and the REACH program staff. The results of this evaluation suggest that both program staff and LHAs note existence and importance of this collaboration, but agree that improvements can be made to increase the level and process of the two-way communication flow. Community and public policy level changes include social norms in addition to local, state and federal policies and laws that promote preventative health behaviors. It is evident from this assessment that all levels identify the establishment of the neighborhood farmer’s market as a positive community change. Interaction between interpersonal and community levels is supported by the LHAs’ work in overcoming cultural barriers. Conclusions: This initiative was designed to stimulate community based prevention research and support community-based demonstration projects that promote health and eliminate racial and ethnic disparities. In establishing a community-based intervention in which the mission is to eliminate health disparities in cardiovascular disease and diabetes, the Charlotte REACH 2010 initiative was developed within an ecological framework. This ecological approach to eliminating health disparities involves interventions targeted on five levels of influence with interaction between levels creating a supportive system for sustained change. Due to nature of this multi-leveled approach an assessment of program processes and initial impacts is necessary. The qualitative nature of this evaluation enabled researchers to assess program progress by exploring changes that have occurred within levels in addition to assessing interaction between levels. Findings from the assessment are encouraging in that they reveal positive steps toward mobilizing community efforts to influence healthy behavior change and risk reduction for cardiovascular disease and diabetes. The findings also demonstrate the challenge of implementing multifaceted, connected interventions from an ecological perspective. A primary concern is the need for ongoing, effective communication between community representatives, project staff and service providers in order to maximize understanding of local needs and strengths and to identify further opportunities for planning or modifying community sensitive intervention strategies for sustained change. Implications for Policy, Delivery or Practice: Effective health promotion programs are grounded in theories suitable for reaching the anticipated outcome. The projected outcome of the REACH 2010 demonstration project includes eliminating disparities in six health priority areas. This initiative was designed to stimulate community based prevention research and support community-based demonstration projects that promote health and eliminate racial and ethnic disparities. In establishing a community-based intervention in which the mission is to eliminate health disparities in cardiovascular disease and diabetes, the Charlotte REACH 2010 initiative was developed within an ecological framework. This ecological approach to eliminating health disparities involves interventions targeted on five levels of influence with interaction between levels creating a supportive system for sustained change. Implications from this study suggest the need for ecologically based programs which establish a supportive social sytem for program institutinalization and sustained program change. Primary Funding Source: CDC • The Characteristics Associated with Adequate Adjuvant Chemotherapy for Stage III Colon Cancer Sharon Dobie, M.D., MCP, Barbara Matthews, M.S., Jason Dominitz, M.D., MHS, Kevin Billingsly, George Wright, Ph.D., Laura-Mae Baldwin, M.D., M.P.H. Presented by: Sharon Dobie, M.D., MCP, Associate Professor, Family Medicine, University of Washington, Box 356390, Seattle, WA 98125; Tel: 206.543.9425; Fax: 206.543.3821; E-mail: dob@u.washington.edu Research Objective: To explore whether the disparity found in initiation of chemotherapy for stage III colon cancer between blacks and whites persists throughout colon cancer treatment, resulting in less adequate adjuvant chemotherapy for African Americans compared to Caucasians. Study Design: Using the 1991-1998 Surveillance, Epidemiology, and End Results (SEER)-Medicare claims database with physician data from the American Medical Association (AMA) Masterfile, we defined adequacy of chemotherapy for stage III colon cancer as five months of chemotherapy during the treatment period. Using multiple logistic regression, we examined the relationship between race and receipt of adequate chemotherapy, then added patient (e.g. age, marital status, socio-economic status, location of residence, comorbidity, and rehospitalization) and physician ( e.g. age, gender, race and ethnicity, specialty, years in practice, practice volume) characteristics to the model to determine any influence on this relationship. Population Studied: 3888 African American and Caucasian Medicare beneficiaries 66 and older reported to one of the 12 SEER cancer registries with a diagnosis of stage III colon cancer between January 1, 1992 and December 31, 1996, and alive for two years after their cancer diagnosis Principal Findings: Of the 2308 who received adjuvant chemotherapy, the adequacy rates were similar for African Americans (87%) and Caucasians (82%). Increasing age was associated with decreased adequacy: 65-70 years as reference; 71-75 years OR=1.02 (P=.9); 76-80 years OR=.46 (P<.01); 81-85 OR=.35 (P<.01); =86 OR=.32 (P<.01). Widowed persons were less likely (OR .59; P=.01) than married and those living in remote rural areas were more likely than urban dwellers (OR=2.3; P=.01) to receive adequate therapy. Co-morbidity, measured using the Romano-Charlson index, was not associated with differences in adequate chemotherapy, while hospital re-admissions were (no readmission as reference; readmission in weeks 7-16 OR=.39; P=.01; weeks 17-30 OR=.52; P=.01). Volume of chemotherapy patients was the only physician characteristic associated with adequate chemotherapy (physicians < 4 patients per year as reference; 8-12 patients annually OR= 1.4; P=.05; 13+ patients annually OR=1.5; P=.05). Conclusions: African Americans are equally likely to complete their chemotherapy course once begun, making initiation of care crucial to his group. An alternate explanation is that the African Americans most likely to complete therapy are those who initiate it, whereas a more diverse group of Caucasians initiates therapy. The negative association of increasing age and rehospitalizations with adequate chemotherapy suggests that these variables represent more powerful measures of case severity than the Romano-Charlson index. Of interest are the lower adequacy rates for widowed individuals and higher rates for those living in remote areas. The former suggests lack of social support, while the latter may relate to relocation for the duration of therapy. Implications for Policy, Delivery or Practice: This study demonstrates the utility of administrative claims in examining the quality of chemotherapy. These findings can be used to develop programs that identify and facilitate receipt of adequate chemotherapy by vulnerable groups. In the case of African Americans, our findings underscore the need for policies that ameliorate their barriers to initiating adjuvant therapy. Primary Funding Source: NCI • ER Utilization Among Washington State's Medicaid Recipients Jean Du, Ph.D. Presented by: Jean Du, Ph.D., Program Evaluation Manager, Medical Assistance Administration, State of Washington, 1011 Plum Street, Olympia, WA 98504-5562; Tel: 360.725.1033; Fax: 360.586.9548; E-mail: dujj@dshs.wa.gov Research Objective: Using a standard and consistent measure of ER visit, track Washington State Medicaid ER utilization overtime to 1) describe system characteristics and patterns of ER utilization by Medicaid recipients; 2) identify possible disparities in ER utilization by ethnicity, age groups, and geographic location; 3) inform policy and programs where to target limited resources for better program benefits. Study Design: For the first time in Washington State’s Medicaid program, this study distinguishes ER visits that result in hospital admissions and those that do not. The distinction is believed to be important in addressing issues like access-to-care (where more providers may be recruited) or inappropriate use of ER (where education and/or utilization management may be needed). Using Medicaid claims data maintained by the State, the study tracks the same measures for five years, from 1999 through 2003. Population Studied: This is a study of the entire Fee for Service (those not served by a managed care plan) Medicaid population in Washington State. Principal Findings: ER visits that do not end up in hospital admission make up the overwhelming majority of total ER visits and are growing from 86% of total ER in 1999 to 89% in 2003. During the last five years, this type of ER saw a much faster growth than ER visits that result in admissions (82.8% v. 33.7%). While much of the increase in ER utilization was driven by caseload expansion (up 48% during the same time period), total ER visits per 1,000 recipients climbed 19%, from 789 per 1,000 in 1999 to 941 per 1,000 in 2003, with 2003 seeing the biggest one-year increase (7.1%). On a per-cap basis, ER visits that result in hospital admissions dropped 9% over the five-year period while those that do not result in admissions increased 24%. Native Americans, African Americans, and Caucasian recipients have disproportionately higher ER utilization. Adults between ages 30 and 44 have disproportionately higher ER utilization than any other age group under consideration (new-born, 1-3, 4-12, 13-17, 18-29, 30-44, 45-64, 65 and over). Of all FFS recipients, 44% used ER in 2003. Most ER users (80%) had between one to two ER visits per year while a small portion (less than 2% ER users) had twelve or more ER visits per year and incurred 14% of total ER visits among the FFS population. Conclusions: Consistent with many studies of ER utilization across the nation, Washington state experienced rapid growth in ER visits. While much of the increase is attributable to caseload expansion, the findings also point a lack of access to care for some recipients and possibly inappropriate use of ER among others. Implications for Policy, Delivery or Practice: The findings suggest that Washington Medicaid program should consider two policy/program directions: 1) expand efforts in recruiting FFS providers to keep up with the client caseload increase; 2) develop programs with its partners (providers, client advocates, and the community) in ER utilization education and case management, including closer monitoring of frequent ER users. Primary Funding Source: State Funds • Utilization of Pediatric Care by Latino Children: The Effects of Limited English Proficiency among Parents O. Kenrik Duru, M.D., MSHS, Leo Morales, M.D., M.P.H. Presented by: O. Kenrik Duru, M.D., MSHS, NRSA Research Fellow, Division of General Internal Medicine, University of California, Los Angeles, 911 Broxton Plaza, 3rd Floor, Los Angeles, CA 90024; Tel: 310.794.8138; E-mail: kduru@mednet.ucla.edu Research Objective: Studies in adult populations have documented that limited English proficiency (LEP) is associated with decreased access to care, and may explain a significant component of racial/ethnic health disparities in utilization. Children depend on parents to access health care on their behalf, and minority children of LEP parents may be less likely to receive appropriate care. Latino children are less likely than white children to receive care, but few analyses have examined the possible unmeasured effect of primary language on children´s utilization of care. Study Design: Race/language pairings were used as the primary independent variable (white, Latino/English, Latino/Spanish), for three probit regressions predicting the likelihood of a clinic visit in different settings. In the first, we assessed whether the child had a clinic visit in the setting of an acute or chronic illness. In the second, we assessed whether the child had a clinic visit if an appointment had been made. In the third, we assessed whether children under two had any lifetime well child visit or immunization visit. To ease interpretation of our results, we estimated predicted probabilities and standard errors of a clinic visit for children from each race/language pairing. Errors were adjusted to control for clustering by health plans. Population Studied: We used 2000/2001 CAHPS survey data on 29,564 children enrolled in 27 health plans participating in the State of California Children´s Health Insurance Program. Principal Findings: For each analysis, predicted clinic visit rates for white children were significantly higher than for Latino/Spanish children. With an illness, the probability of a visit for white children within six months was 92%, but only 79% for Latino/Spanish children. If an appointment was successfully made, the probability of a visit within six months was 94% for white children as compared to 82% for Latino/Spanish children. The predicted probability of a lifetime well child or immunization visit for children under two years of age was 93% for white children, whereas it was only 79% for Latino/Spanish children. In each case, there was no statistical difference between predicted probabilities for visits by white children and Latino/English children. All reported results were significant at the p<0.05 level. Conclusions: Within the insured population of children we studied, differences in utilization of care by primary language exist in different situations measuring a perceived or evaluated need for care. These findings suggest that racial/ethnic disparities in utilization of pediatric care between Latinos and whites may in fact reflect issues related to LEP. Implications for Policy, Delivery or Practice: Strategies to reduce racial/ethnic disparities in utilization of pediatric care should target parents with limited English proficiency. Primary Funding Source: HRSA training grant • Blood Pressure Treatment and Control among African American and Caucasian Hypertensive Patients in South Carolina Brent Egan, M.D., Katharine Hendrix, Ph.D., Jan Basile, M.D., Shakaib Rehman, M.D., Daniel Lackland, Dr.PH Presented by: Brent Egan, M.D., Professor of Medicine and Pharmacology, General Internal Medicine, Medical University of South Carolina, 96 Jonathan Lucas Street, 826 CSB, Charleston, SC 29425; Tel: 843.792.1715; Fax: 843.792.0816; Email: eganbm@musc.edu Research Objective: Although evidence now more than 20 years old indicates that better BP control is attainable and will reduce disparities, the promise of this research has not been realized. The purpose of this research was to better quantify the current disparity in BP control. Study Design: We compared data on treatment patterns and control rates among African Americans and Caucasians in our database. Population Studied: ~75,000 hypertensive patients in South Carolina. Principal Findings: Mean BP values are ~3/4 mmHg higher and control rates to <140/90 mmHg ~8% lower in African American than Caucasian hypertensives. The disparities in BP control do not appear to reflect a less intensive therapeutic effort, since providers are prescribing an equal or greater amount of all major classes of antihypertensive mediations with the exception of b- and a,b-blockers to African American than Caucasian hypertensives. Conclusions: These data suggest that hypertension is more difficult to control in African Americans than Caucasians with traditional medical care and could reflect biological, socioeconomic, and/or cultural differences that impact response to treatment. It is also likely that access, affordability of care, and compliance with medication and lifestyle recommendations contribute to these differences. Implications for Policy, Delivery or Practice: Interventions to ensure more effective implementation of the hypertension guidelines have significant potential for improving cardiovascular and renal health, especially in the African American community. Primary Funding Source: AHRQ • Substance Abuse and Not Race Determines Outpatient Mental Health Service Use: The BASIS-R Study A. Rani Elwy, Ph.D., Susan Eisen, Ph.D. Presented by: A. Rani Elwy, Ph.D., Postdoctoral Fellow, Center for Health Quality, Outcomes and Economic Research, Department of Veterans Affairs, 200 Springs Road (152), Bedford, MA 01730; Tel: 781.687.2000 Ext. 6707; Fax: 781.687.3106; E-mail: relwy@bu.edu Research Objective: Substance use disorders are a frequent comorbid illness for individuals with serious psychiatric illness. Patients with comorbidities are more likely to have higher rates of healthcare utilization. African Americans have a greater number of dual diagnoses of schizophrenia and substance abuse than similar white patients, yet African Americans have previously been found to receive less specialty mental healthcare than whites. Our objective was to examine whether race, substance abuse (SA) disorders, or dual diagnoses of psychiatric and substance abuse, determines outpatient mental health (MH) service use. Study Design: Self-reported symptom and problem difficulty, including problems due to alcohol and/or drug use was assessed at patients’ first outpatient visit and two months later using the revised Behavior and Symptom Identification Scale (BASIS-R). Demographic and clinical data including up to five DSM-IV diagnoses were retrieved from chart review. Using analysis of covariance we examined the main effects of patient race (African American, Native American, Asian, Native Hawaiian/Pacific Islander, multiracial, or white), diagnoses, and program type (MH, or SA including dual diagnoses) on MH outpatient use. We controlled for patient age, sex, marital status, education and comorbidities. We also examined interactions between patient race, diagnoses and program type on MH outpatient use in the two months following intake. Population Studied: 1843 clients from outpatient MH or MH/SA delivery sites in each of the four US census regions. 12 percent of patients were African American, 79 percent were white and 9 percent were from other racial groups. 56 percent of patients were female. 58 percent had an MH diagnosis only, 20 percent had a SA diagnosis only and 22 percent had both mental health and substance abuse diagnoses. Principal Findings: A main effect of having a SA diagnosis was found, in that patients with a SA diagnosis only had a greater number of outpatient visits during the two month study period than patients without a diagnosis of SA (F=4.6, p=.03). There was no main effect for patient race on number of outpatient visits. However, there was a significant interaction between patient race and program type, such that African Americans received more services from SA programs than from MH only programs (F=2.7, p=.01). Conclusions: A diagnosis of SA and not patient race determined greater MH outpatient service use. Implications for Policy, Delivery or Practice: Patients with SA disorders may require more intensive outpatient treatment than patients with MH disorders only. Increasing healthcare providers’ ability to treat SA disorders is necessary for effectively serving this population. An awareness of SA disorders occurring in all races is important for accurately diagnosing and treating patients who require this intensive treatment. Primary Funding Source: NIMH • Variation in Quality of Care Received by American Men Kaytura Felix Aaron, M.D., Ernest Moy, M.D., M.P.H., Minsun Kang, M.P.H., Mona Patel, Francis Chesley, M.D., Carolyn Clancy, M.D. Presented by: Kaytura Felix Aaron, M.D., Senior Advisor on Minority Health, HHS, AHRQ, 540 Gaither Road, Rockville, MD 20850; Tel: 301.427.1395; Fax: 301.427.1562; E-mail: kfaaron@ahrq.gov Research Objective: Men have been characterized as “an invisible population,” overlooked by public and private efforts to improve health status of women, children and the elderly. However, policy makers; researchers and advocates are increasingly addressing men’s health care needs. This study compares the quality of care received by racial and ethnic minority men with that of non-Hispanic white men. Study Design: Several aspects of quality of care issues, i.e., preventative services, chronic disease management, avoidable hospitalizations, surgical safety and post-operative safety are evaluated. Measures are derived from the National Health Interview Survey, the Medical Expenditure Panel Survey, the CMS End Stage Renal Disease Clinical Performance Measures Project, the U.S. Renal Data System and the Healthcare Cost and Utilization Project State Inpatient Database 16-state database. The relative difference between each racial/ethnic group and a fixed reference group is used to assess differences in use of services. Statistical significance is assessed using z-tests. Principal Findings: : Hispanic men were much less likely to receive colorectal cancer screening (relative risk [RR] range: 0.61-0.69), cardiovascular risk factor screening and management (RR: 0.84-0.88) and vaccinations (RR: 0.470.94). African American and Asian men were significantly less likely to have received selected preventive services (adult immunization and colorectal cancer screening). The differences in end-stage renal disease care that African American and white men received were statistically significant (RR: 0.39-0.97); with African American men consistently receiving worse care. For some measures of management of end-stage renal disease, Asian men received care that was similar to, or better than, that received by non-Hispanic whites. For example, they were more likely to be placed on a kidney transplant waiting list. However, despite being placed on the waiting list at higher rates, Asian men received kidney transplants at about half as often as non-Hispanic whites. With respect to avoidable hospitalizations, African American; Hispanic and Asian men, respectively, almost always; sometimes and almost never had higher rates than nonHispanic whites. In contrast, patient safety problems were experienced more often by all three groups relative to nonHispanic whites. Conclusions: Racial/ethnic minority men are at a markedly elevated risk for the receipt of poor health care quality in multiple, diverse domains of clinical care. However, there is considerable variation in the magnitude, direction and significance of these risks for different minority groups. Implications for Policy, Delivery or Practice: Generalizations about “minority” men are likely to be misleading and incomplete. Further exploration of the differences between racial/ethnic minority groups can enhance our understanding of which factors are most important in generating significant differences – an understanding likely to help improve quality for all men. • Aligning Public Health Insurance Recertification with the Process of Graduating from Elementary, Junior and Senior High Schools in Order to Provide Children with Continuous Health Care Coverage Bertha Fertil, MGA, M.P.H., Tracy Grant, B.S., M.S.W., DelRoy Williams Presented by: Bertha Fertil, MGA, M.P.H., Director, NYC HRA Medical Insurance and Community Services Administration, 15934 Riverside Drive, #2B, New York, NY 10032; Tel: 212.928.9264; E-mail: BFertil@aol.com Research Objective: No child in the United States should be without health insurance. The number of uninsured children (18 and under) in the United States is approximately 10 million. Of this group half a million reside in New York State. Further complicating their lives, many of these children live in poverty or in households with little income security where financial resources do not enter the home in a consistent manner. In addition, because of numerous social, health and economic issues (employment with inflexible work hours, substance abuse, mental health issues, food and housing insecurity) the parents of these children do not recertify their children’s public health insurance on a regular basis even when the face-to-face recertification interview is eliminated and a mail-in recertification application process is put in place. After having their Medicaid case closed, these individuals are returning an average of 1.62 years later to reapply. This is usually after the child is in need of medical care or is reengaged by a health plan. As a result, many of these children during the most critical years of their lives go without health insurance for more than a year and half. The objective of this study is to find a means by which children can retain their health care coverage in a manner that enables for continous coverage without overwhelming their parents. Study Design: In a case review of 4,000 new applications for public health insurance, we analyzed the following: the number of times the individual had Medicaid coverage and the case was closed, the number of children on the case record, family income over five year, case type and whether the case was submitted by a plan. Population Studied: During a three month period we studied the case records of 4,000 New York City residents who submitted a new application for public health insurance. The study was completed using a confidence level of 99% and a margin of error of +/-2. Principal Findings: In our study of 4,000 New York City individuals who submitted a new application for public health insurance during the months of June to August 2003 it was found that 80% of the children only cases where already known to Medicaid. However, their cases were closed because the parents fail to mail-in the recertification application even after the face-to-face interview process was eliminated. More interestingly the parents did return to apply for public health insurance more than a year and a half (1.62 years) after the case closed. In addition, it was found that the parent’s income did not significantly change over a five-year period. Conclusions: By extending the annual recertification to four years for these children only cases, the states would be aligning the recertification period with the graduation from different schools levels (elementary/primary, intermediate/junior and senior high). By aligning the recertifying with school, the state can partner with the school systems in getting children enrolled in public health insurance. In homes with more than one child, the graduation date of the youngest child could be used to provide the longest possible continuous coverage period for the children. Implications for Policy, Delivery or Practice: The current annual recertification works as an access barrier to health care for many of New York City’s most vulnerable populations. The extended recertification period would provide children with a continuum of care. This process would enable children to be able to meet their preventative health care milestones without overwhelming parents, individuals who are already stressed by negotiating the public welfare system. If the incomes of the parents of the children only cases are looked over a five-year period, especially parents of children under five years old, the income either remains the same or is reduced. In addition for children with chronic health care issues the annual recertification process potentially puts their lives at risk. Lastly, this process would save the state monies by reducing the cost of processing the applications on an annual basis. Presently, it cost the state approximately $220 - $280 per application per year to complete a new application. Therefore, each time a parent fails to renew a child’s public health insurance, the state (the taxpayers) pays the cost. • The Effect of Gender on Treatment of Acute Myocardial Infarction Patients Janet Young, M.D., M.H.S.A., David Foster, Ph.D., M.P.H., David Foster, Ph.D., M.P.H., Sivana Heller, M.D., M.P.H. Presented by: David Foster, Ph.D., M.P.H., Vice President, Clinical Informatics, Solucient, LLC, 5400 Data Court, Ann Arbor, MI 48108; Tel: 734.930.7982; Fax: 734.930.7611; E-mail: dfoster@solucient.com Research Objective: To compare treatment of male and female inpatients diagnosed with acute myocardial infarction (AMI). Study Design: Retrospective cohort study. Population Studied: Data for 23,017 patients with a principal diagnosis of AMI discharged between October 1, 2002 and September 30, 2003 was extracted from ACTracker, Solucient’s proprietary database with detailed inpatient diagnostic, demographic, and drug information. Principal Findings: Women with a principal diagnosis of AMI admitted to hospitals with a catheterization lab are significantly less likely than men to undergo surgical intervention – either percutaneous coronary intervention (PCI) or coronary artery bypass graft (CABG), adjusting for age, race, payer, hospital characteristics and subendocardial infarction (OR .698, 95% CI .657, .742). However, there was no statistical difference in the likelihood of receiving a stent by gender among AMI patients who underwent PCI (OR .987, 95 % CI .844, 1.155). Although women undergoing PCI were somewhat less likely than men to receive a glycoprotein IIb/IIIa inhibitor, this finding was not statistically significant (OR .907 ,95% CI .812, 1.011). Women treated medically for a transmural infarction are significantly less likely than men to receive a thrombolytic agent (OR .754, 95% CI .629, .904). Conclusions: Recent data shows that women with a principal diagnosis of AMI remain less likely than men to receive treatments that have been reported to improve outcomes (i.e. survival, reinfarction), including surgical intervention and thrombolytic agents. However, women who undergo PCI are as likely as men to receive a stent, a device which has been reported to decrease restenosis. Implications for Policy, Delivery or Practice: Cardiovascular disease remains the most common cause of death in women. Additional studies are required to determine why women are less likely than men to receive treatments that have been reported to improve outcomes. Primary Funding Source: Solucient, LLC • "They Don't Hear What I am Saying at All." Language Access Disparities among Haitian, Latino and Russian Immigrant Parents Seeking Health Care for Their Children in New York City Jennifer Fuld, M.A., Ph.D. Candidate, Linda Weiss, Ph.D., Tamar Bauer, J.D. Presented by: Jennifer Fuld, M.A., Ph.D. Candidate, Research Associate, New York Forum for Child Health, The New York Academy of Medicine, 1216 Fifth Avenue, New York, NY 10029; Tel: 212.822.7390; Fax: 212.822.7369; E-mail: jfuld@nyam.org Research Objective: Immigrant families and particularly children face many obstacles to accessing health services in New York City. Research demonstrates that children in immigrant families are more likely to be uninsured, have no regular source of care and face other barriers than children in native citizen families, but little is known qualitatively about these issues. This research examines the experiences immigrant parents have navigating the health insurance and health care system in NYC. In this current analysis, we compared Haitian, Latino and Russian parents' experiences with language access issues during children's health care visits over the past two years. Study Design: We conducted 75 semi-structured interviews of immigrant parents living in New York City, from August 2003 December 2003 (25 Haitian, 25 Latino, 25 Russian). Interviews were conducted in Haitian-Creole, Spanish and Russian and audio-taped. Respondents were recruited using purposive sampling through collaboration with communitybased organizations. All eligible respondents had to be an immigrant parent caring for a child (under age 18). The child had to be uninsured at the time of the parent's interview, or insured with CHP A (Medicaid) or CHP B but to also have also had a period of uninsurance within the past two years. Coding and analysis of qualitative data was conducted with the aid of Atlas.ti. Population Studied: The population studied was Haitian, Latino, and Russian immigrant parents and children living in New York City. We limited our sample to children in immigrant families who are uninsured but eligible for CHP A (Medicaid) or CHP B and children who are insured with CHP A or CHP B. Children in immigrant families with private insurance were excluded. Principal Findings: Most parents were limited English proficient (LEP) and were caring for young children. Parents described being continually frustrated and feeling that they were getting only a partial picture of their children's health during many health care visits. Parents who had taken their children to the emergency room described experiences where they were not provided any type of language assistance, they were not properly informed about their child's health, they were told to sign forms in English that they could not read and they felt dismissed by the doctors because they were LEP and doctors were not bilingual. In contrast, parents described experiences at community-based health centers as more positive and as visits with doctors and staff who were bilingual. Parents believed that as these visits, in relation to hospital visits, they left with a better understanding of their child's health and healthcare needs. Differences among the three groups included: Haitian parents often bring along a Haitian friend or family member who speaks English to children's health care visits since they expect to be provided with no language assistance in Haitian-Creole; Latino parents often resign themselves to a stranger or staff person with very poor Spanish to provide language assistance during a child's visit since they feel that it is likely someone at the location will speak some Spanish, even if it is extremely limited; and Russian parents seek out Russian doctors in their community. Conclusions: Immigrant parents in all three immigrant groups, face many barriers during children's health care visits when there is limited language assistance available. Parents negotiate a health care system that provides limited language assistance at many places by relying on culturally-based norms that reflect factors such as the size of the immigrant group, geographic settlement patterns, social support and coping strategies. Overall, parents report that their knowledge of their children's health is comprised by limited language assistance and that each negative health care visit cumulatively impacts their ability to care for their child's development. Implications for Policy, Delivery or Practice: It is critical that immigrant parents are able to communicate with and understand the health care providers who care for their children. These findings add to the growing evidence that New York City health care providers, especially hospitals, need to improve language access services and that ad-hoc interpreters such as strangers, friends and other family members are not a substitute for medical interpretation. Primary Funding Source: Foundation for Child Development • Racial Differences in Consumer Empowerment and Health Care Experiences in the US Health System Lisa Gary, M.S., M.P.H., Mark Schlesinger, Ph.D. Presented by: Lisa Gary, M.S., M.P.H., Ph.D. Candidate, Health Policy and Administration, Yale University School of Public Health, 60 College Street, P.O. Box 208034, New Haven, CT 06520; Tel: 203.787.9943; Fax: 203.785.6287; E-mail: lisa.gary@yale.edu Research Objective: Objective: To investigate racial differences in consumer empowerment behavior and health care experiences in the American health system and to investigate the role of consumer trust in that process. This study also explores whether these racial differences vary significantly across 3 domains of health care experiences: interactions with physicians, health plans and hospitals. Background: Studies show that racial minorities have worse health outcomes than whites across a large array of health indicators. Recent studies suggest that the racial differences in health outcomes are in part due to racial minorities receiving lower quality health care than their white counterparts. Controlling for socioeconomic status, minority patients have less adequate communication with their physicians and are less likely to receive appropriate preventive care. To understand the origins of racial disparities in care, it is important to assess whether minority patients are experiencing a higher rate of problematic treatment in the first instance; and secondly are they less able to effectively address the inadequacies that occur in the course of their medical care. Essentially, are minority consumers empowered enough to voice when they experience problems with their health care? What are the consumer characteristics and health system characteristics that are associated with consumer empowerment behavior? Study Design: Data are from the Yale/New York Academy of Medicine Survey of Consumer Experiences in Health Care conducted from June 2002 to early September 2002, a telephone survey of approximately 5000 individuals representing the US non-institutionalized population. The conceptual model for this research builds on two models of health behavior and health care utilization to examine the phenomenon of consumer self-advocacy. Data have been analyzed to assess the prevalence of problematic experiences in the health care system for African Americans compared to whites. Further analysis focuses on their responses to those perceived problems i.e. - their level of consumer empowerment/self-advocacy. In addition to describing the nature and distribution of the health care problems experienced by consumers, data on satisfaction with the problem resolution within the health care system will be analyzed. Additional multiple logistic regression and Poisson regression models will focus on the role of self-efficacy and consumer trust as well as health plan characteristics in promoting empowerment behavior. Population Studied: There are 485 black/African American and 3825 white insured adults in the study. Principal Findings: Initial analyses show that minority consumers experience more problems with their health care. The possible problems with their health care range from delays in care to being treated unfairly due to their race. Preliminary analysis also shows that minority consumers often feel mislead by their health plans when trying to address a health care problem. Conclusions: Although the study is in progress, the implications for this research are far-reaching. This research will be beneficial for developing interventions within health plans that encourage a sense of agency and empowerment for minority health care consumers and non-minority consumers as well. Additionally, consumer empowerment may have significant effects on medical care practice. For instance, empowered consumers Primary Funding Source: NIMH and Atlantic Philanthropies • Examining Racial and Ethnic Disparities in Site of Usual Source of Care Darrell Gaskin, Ph.D., Joses Arbelaez, M.D., Fernando Wagner, ScD, Jorielle Brown, Ph.D, Hanno Petras, Ph.D. Presented by: Darrell Gaskin, Ph.D., Associate Professor, Health Policy and Management, Johns Hopkins Bloomberg School of Public Health, 624 N. Broadway, Room 441, Baltimore, MD 21205; Tel: 443.287.5297; Fax: 410.614.8964; E-mail: dgaskin@jhsph.edu Research Objective: To examine the disparities in site of usual source of care by race and ethnicity. Minority subgroups have a lower propensity to use private doctors’ offices for their usual source of care than Whites. We attempt to explain this observed difference. In particular, we determine whether observed differences persist after controlling for other factors, such as demographic, socioeconomic and individuals’ values and beliefs about health care. We also identify which factors were most important for each race/ethnic subgroup. Study Design: We estimated a multinomial logistic regression model where the dependent variable is the site of the respondents’ usual source of care using those who use a doctor’s office as the reference group. Using this model, we computed the relative risk ratios for each minority group compared to Whites of using a community health center relative a doctor’s office and hospital outpatient department relative to a doctor’ office, and hospital emergency room/ no regular source of care relative to a doctor’s office. We also estimated model separately for each subgroup to ascertain whether the relative importance of factors differ across groups. Population Studied: This study used the Commonwealth Fund’s Health Care Quality Survey of adults conducted between April and November 2001. African Americans, Hispanics and Asians were over-sampled to enable researchers to examine differences by race and ethnicity. The survey covered several domains including usual source of care, health care utilization, unmet medical needs, satisfaction, health status, socioeconomic status, attitudes about value of medical care and perceptions about the presence of racial/ethnic bias in medical treatment. Principal Findings: While insurance and income play a major role in determining whether minorities obtain their care at the private doctor’s office, other factors such as demographic, education, health status and attitudes towards health care matter too. The relative importance of these factors differs across subgroups. Whites who felt there was racial/ethnic bias in the delivery of health care were less likely to use community health centers while minorities who felt this way were more likely to use community health centers. African Americans and Hispanics perceptions of racial and ethnic bias in the delivery of health care did not explain the within subgroup variation in site of care. Only income and the lack of health insurance were statistically significant factors for all four subgroups as a determinant of hospital emergency room use or reporting no usual source of care. Conclusions: To encourage minorities the rely more care in private doctors’ office, policy makers will have to use more than financial mechanisms (i.e. insurance coverage and income subsidies) to achieve this goal. Outreach and education programs targeted to particular segments within each minority community may be required to change care seeking patterns. In addition, improving the viability of private physician practices in urban and rural areas is an important consideration. Primary Funding Source: National Institute of Minority Health and Health Disparities • Racial Disparities in the Enjoyment of Cancer Survival Advances over the Past 30 Years in the United States: Evidence of Institutionalized Racism Kevin Gorey, Ph.D., M.S.W., Isaac Luginaah, Ph.D., Emma Bartfay, Ph.D. Presented by: Kevin Gorey, Ph.D., M.S.W., Professor, School of Social Work, University of Windsor, 401 Sunset Avenue, Windsor, N9B 3P4; Tel: 519.253.3000; Fax: (519) 973-7036; Email: gorey@uwindsor.ca Primary Funding Source: Canadian Institutes of Health Research • Urgent Need for Specialist Care among Homeless Pediatric Patients Roy Grant, M.A., Peter Sherman, M.D., Irwin Redlener, M.D. Presented by: Roy Grant, M.A., Director of Research, Research, The Children's Health Fund, 317 East 64th Street, New York, NY 10021; Tel: 212.535.9400; Fax: 212.535.7699; E-mail: rgrant@chfund.org Research Objective: 1. To determine the specialist referral needs of homeless children when they begin a primary care medical home program. 2. To replicate findings of an initial study completed in 2000, which found a very high level of need in the population. Study Design: Retrospective review of electronic and paper charts of all patients of the New York Children’s Health Project referred to a specialist based on initial pediatric assessment in 1998 (2,205 patients). Virtually all were domiciled in a homeless or domestic violence shelter. To test whether the initial findings were representative, this was repeated for patients seen during 2001 (2,425) to allow for virtually 100% patient turnover. Population Studied: Homeless children experience more acute and chronic conditions, and worse health status, than housed low-income children (Weinreb et al, 1998; Parker et al., 1991; Wood et al., 1990). Prior to becoming homeless, they may have had inadequate access to health care services, reflected by, among other indicators, under-immunization (Fierman et al., 1993; Orenstein et al., 1992; Miller and Lamm, 1988). Principal Findings: In the 1998 cohort, 509 patients (23.1%) required at least one specialist referral. Two ore more specialist referrals were required by 183 patients (8.3% of patients; 35.9% of referred patients). Conditions identified suggest that serious medical conditions were not identified or, if identified, not adequately treated in this predominantly Medicaid eligible population. Conditions include club foot, hearing loss, visual impairment, seizure disorder, and hydrocephaly. In 2000, for a new cohort of patients who, based on improved immunization status were likely to have had better prior access to care, 544 patients were referred (22.2%), of whom 150 (6.1% of patients; 27.6% of referred patients) required two or more specialist referrals. Similar conditions were identified. Conclusions: Medically underserved pediatric patients may present with serious needs when they begin a medical home progam. Based on the nature of conditions identified, EPSDT standards may not be consistently met for these high-risk Medicaid eligible patients. Implications for Policy, Delivery or Practice: Because of prior access or quality of care issues, high-risk pediatric patients may require longer primary care visits than typical. They may present urgent need for specialist referral, requiring enhanced access to specialist care. These findings may have an impact on cost of care whether by capitation or fee for service. Primary Funding Source: BPHC • Race/Ethnicity, Socioeconomic Experience and Adult Health Lisa Green, Ph.D. Candidate Presented by: Lisa Green, Ph.D. Candidate, Student, Health Policy & Management, Johns Hopkins Bloomberg School of Public Health, 3601 Greenway #601, Baltimore, MD 21218; Tel: 410.889.5916; E-mail: ligreen@jhsph.edu Research Objective: To better elucidate the role of socioeconomic experience in the race/ethnicity and health relationship among working-age adults, this study examines multiple domains of socioeconomic experience within a lifecourse paradigm. The aims of this study are to identify the racial/ethnic differences in global health outcomes among working age adults, and to determine what role individual-level socioeconomic experience has in explaining these differences. Study Design: Sex and sex-race stratified multivariate linear regression models were used to examine the impact of education, occupational prestige and 19 year income on five health outcomes (SF-12 Physical and Mental Health Summary Scores, depression, major morbidities and minor morbidities) measured at age 40. Data were drawn from the National Longitudinal Survey of Youth 1979 for the years 1979-2000. Population Studied: The NLSY79 cohort is a nationally representative sample of the non-institutionalized, civilian population aged 14-21 in 1979 with an over-sample of civilian Hispanic and Black respondents. Respondents were surveyed annually from 1979 to 1994 and then biennially through the present. Those who have reached age 40 and answered the age 40 health module were included (n=3,154) in this study. Principal Findings: In sex stratified models, socioeconomic factors alone fully accounted for observed disparities, and provided a protective effect for major and minor morbidities among black and Mexican respondents, compared to white counterparts. Income in particular played a strong role in explaining racial/ethnic differences. The sex and race stratified models revealed that socioeconomic factors impact different population groups in different ways. Income appeared to have a lagged effect among black men and women, and no effect on Mexican men and women. Education exhibited a gradient effect for most sex-race categories and occupational prestige had minimal to no effect on health outcomes.respondents, compared to white counterparts. Income in particular played a strong role in explaining racial/ethnic differences. In sex and race stratified models, income appeared to have a lagged effect among black men and women, and no effect on Mexican men and women. Education exhibited a gradient effect for most sex-race categories and occupational prestige had minimal to no effect on health outcomes. Conclusions: This study addresses gaps in the literature on whether more complex and perhaps more robust definitions of socioeconomic experience attenuate observed racial/ethnic disparities in health, and on how such socioeconomic patterns over the life course predict health in adulthood. Health status is also key to understanding the health of working adults, where morbidity is relatively low and mortality is disproportionately dominated by HIV, injury and homicide. The working age population represents the most productive segment of the U.S. population, both economically and socially, and represents a much overlooked subgroup ripe for preventive health intervention. Understanding the health differentials and needs during this productive time period, prior to more significant and rapid health declines in later life, are critical. Prior reviews have examined mortality or disease endpoints (e.g. cardiovascular, cancer, other morbidity) with substantially less attention paid to more global concepts of health. Additional research capturing both the longitudinal and contextual dimensions of socioeconomic experience in a broader population is still needed. Implications for Policy, Delivery or Practice: Results suggest that policies addressing socioeconomic inequities may reap significant health benefits. Programs aimed at improving education, income distribution and earnings should be considered in the health disparities discussion. However, additional research on the pathways between socioeconomic factors and health are needed to better guide such program endeavors. Primary Funding Source: NIH NRSA Training Grant • Racial and Ethnic Differences in Need and Unmet Need for Mental Health Care Katherine Harris, Ph.D., Sharon Larson, Ph.D. Presented by: Katherine Harris, Ph.D., Research Fellow, Office of Applied Studies, Substance Abuse and Mental Health Services Administration, 5600 Fishers Lane, 16-105, Rockville, MD 20856; Tel: 301.443.0747; E-mail: kharris@samhsa.gov Research Objective: To compare need for and use of mental health care across a wide range of racial and ethnic subgroups and to measure the robustness of observed differences to clinical and socio-demographic covariates. Study Design: We analyze data from combined rounds of the 2001 National Household Survey on Drug Abuse (NHSDA) and the renamed 2002 National Survey on Drug Use and Health (NSDUH, formally called NHSDA). We present rates of mental health need (one or more mental health symptoms and probable serious mental illness), use of mental health care, and self-reported unmet need for mental health care by racial and ethnic group. We use multivariate logistic regression to assess the sensitivity of observed differences to covariates and report odds ratios from adjusted and unadjusted models. Population Studied: Our sample is large enough to permit us to examine a wider array of racial and ethnic subgroups compared those compared in the existing literature on racial disparities in mental health care: (1) white (n=62,072), (2) African American (n=10,188), (3) American Indian/Native Alaskan(n=1,105), (4) Asian (n=2,793), (5) multiple racial categories (n=1,428), (6) Mexican (n=6,885), (7) Puerto Rican (n=1,375), (8)Central and South American (n=1,888), and (9) other Hispanic-Latinos (1,190). Principal Findings: We found substantial variation in mental health need and use across racial groups. The highest rates of serious mental illness were observed among American Indian/Native Alaskan (12%) and multiple racial category (11%) groups. The lowest rates of serious mental illness were observed among Asian (4%) and Central and South American (4%) groups. However, the two groups with the highest rates of mental health need used mental health services at rates statistically comprable to whites. At the same time, groups with low need used mental health care at substantially lower rates compared to whites (p<.05). The American Indian/Native Alaskan group reported the highest rates of unmet need for mental health care (35% vs. 17% for whites and 6% for Asians). The ability of covariates to explain group differences was not uniform across groups or measures. In general, covariates explained differences in rates of mental health care use among those with mental health need and mental health care need and use between whites and Asians. We find substantial variation in need and use among Hispanic-Latino subgroups with highest rates of need and use among Puerto Rican groups and the lowest rates of need and use among Mexican and Central and South Americans. The use of covariates increased differences in the rates of mental health need between whites and African Americans. Conclusions: Our results reveal wide differences in need, use, and unmet need both between and whites and racial minorities and among minority groups that have been either observed elsewhere in the literature or hypothesized based on indirect comparisons using single group studies. The impact of controls on inferences about racial and ethnic differences varied across groups and across dependent variables in ways that are complex and not anticipated by the disparities literature. Implications for Policy, Delivery or Practice: The sensitivity of group differences in rates of mental health care use to clinical and socio-demograhpic covariates suggests that policies aimed at reducing economic barriers to access may reduce disparities in treatment rates. Primary Funding Source: Substance Abuse and Mental Health Services Administration/Office of Applied Studies. • Collection of Race, Ethnicity, and Primary Language Data in Hospitals: Barriers and Facilitators Romana Hasnain-Wynia, Ph.D., Romana Hasnain-Wynia, Ph.D., David Nerenz, Ph.D., Connie Currier, DrPH, Debra Pierce, BA Presented by: Romana Hasnain-Wynia, Ph.D., Director, Research and Evaluation, Health Research and Educational Trust/AHA, One North Franklin, 30th Floor, Chicagto, IL 60606; Tel: 312.422.4568; Fax: 312.422.4568; E-mail: rhasnain@aha.org Research Objective: As attention shifts from the documentation of disparities to the testing of initiatives to reduce disparities, the role of hospitals is crucial. Yet little is known about the collection of data on race, ethnicity and primary language in hospitals. The research objectives are to: 1 assess whether hospitals collect information on patient race, ethnicity, and primary language;2 assess who provides the information; 3 assess when and where the information is collection 4 understand what the information is used for; 5 understand the barriers and facilitators to collecting this information. Study Design: The study design incorporated the development and implementation of a survey to hospitals and site visits to select hospitals to conduct key informant interviews. Population Studied: The survey was sent to a nationally representative sample of 1000 hospitals stratified along four dimensions: whether hospital was in a state where there was a mandate to collect race and ethnicity data; urban and rural hospitals; teaching hospital status; and whether the hospital was part of a system or a stand alone. We conducted site visits to six hospitals including Northwestern Memorial Hospital, Henry Ford Health System, University of Pittsburgh Medical Center Health System, Massachusetts General Hospital, Parkland Memorial Hospital, and Kaiser Permanente (Northern California) to conduct key informant interviews about each organizations' data collection policy and to understand the barriers and facilitators to collecting race and ethnicity data in hospitals. Principal Findings: Survey findings indicate that the majority of hospitals (78)percent indicate that they collect data on patient race,ethnicity, and lanuage. Hospitals located in states where there is a state mandate to collect race and ethnicity data, urban hospitals, and teaching hospitals are more likely to say they collect these data. There was not a significant difference between hospitals that are part of a system versus stand alone in regard to race ethnicity data collection. In addition, the findings highlight who provides the information in the hospital setting, when the data are collected in the hospital, reasons for collecting the data, race and ethnicity categories used by hospitals, who has access to race and ethnicity data. Those hospitals that stated that they do not collect race and ethnicity data, the findings highlight reasons for not collecting the data. The key informant interviews conducted during the site visits provide contextual information regarding the barriers and facilitators to data collection. Conclusions: Seventy-eight percent of hospitals that responded to the survey state that they collect data on patient race and ethnicity. Given the effort being made to collect this information several general conclusions can be made about collecting race, ethnicity and primary language information in hospitals. Barriers and facilitators to data collection are defined coupled with recommendations to hospitals, other health care organizations,practitioners, and policy makers. Implications for Policy, Delivery or Practice: Collection of data on patients' race and ethnicity should be standardized with regard to: Who provides the information When it is collected in a hospital setting What racial and ethnic categories are used Where data are stored Ensuring that data are collected in a meaningful context e.g.,efficiently and respectfully Primary Funding Source: CWF, National Academies of Science • Racial Differences in Pharmacotherapy and Healthcare Expenditures for the Treatment of Asthma in a Medicaid Population Kevin Hawkins, Ph.D., Richard Stanford, PharmD, M.S., Lucinda Orsini, DPM, M.P.H., Ron Ozminkowski, Ph.D., Chang Jiang, Ph.D. Presented by: Kevin Hawkins, Ph.D., Senior Economist, Outcomes Research & Econometrics, The Medstat Group, 777 E. Eisenhower, Ann Arbor, MI 49230; Tel: 734.913.3145; Fax: 734.913.3200; E-mail: kevin.hawkins@medstat.com Research Objective: To compare pharmacotherapy and healthcare expenditures by race for asthma patients in a Medicaid population. Study Design: This analysis used the MarketScan® claims and eligibility data for a multistate Medicaid population between 1999 - 2000. Because Medicaid eligibility is updated monthly, 24 monthly files were constructed to capture all Medicaid asthmatic patients in 1999 and 2000. Patients were included in the study if they had an asthma diagnosis or prescription for an asthma-related drug in any given month. Patients were grouped by race, a variable often not found in healthcare claims data sets. Type of pharmacotherapy, demographics, health status, healthcare utilization, and expenditures were measured to assess differences between the racial groups. Descriptive analysis was used to determine medication use and healthcare costs across racial cohorts. Population Studied: 2,724,008 subjects were eligible for evaluation over the 2 year observational period. Principal Findings: Overall, patients used 1.8 times as many rescue medications compared to long term controller medications per month. Hispanics used 2.5 times more rescue medications. African-Americans (AA) used 2 times more rescue medications, and Caucasians used 1.6 times more rescue medications. Compared to Caucasians, asthmarelated drug expenditures were 20% and 69% lower for AA and Hispanics respectively. However, asthma-related inpatient costs were 94% higher for AA and 58% higher for Hispanics compared to Caucasians. Similarly, asthma-related emergency room (ER) costs were 48% higher for AA and 13% higher for Hispanics compared to Caucasians. Overall, the largest component of the asthma care among all groups was pharmacotherapy, at 50% of total asthma expenditures ($64 per month). Conclusions: term controller asthma medications were underused by all, but more so among minorities. This difference in use was reflected in the cost of inpatient and ER asthma care across the racial cohorts. Implications for Policy, Delivery or Practice: Further research is needed to understand why minorities are receiving sub-optimal pharmacotherapy for asthma. Once this problem is better understood, interventions can be designed to help correct it. Primary Funding Source: GlaxoSmithKline • Racial and Gender Differences in Access to Substance Abuse Services among Medicaid Adolescents Craig Anne Heflinger, Ph.D., Jamie Chatman, B.S., Robert Saunders, M.P.P. Presented by: Craig Anne Heflinger, Ph.D., Associate Professor, Human and Organizational Development, Vanderbilt University, 230 Appleton Way, Box 90 Peabody College, Nashville, TN 37203; Tel: 615.322.8275; Fax: (615) 3432661; E-mail: c.heflinger@vanderbilt.edu Research Objective: This study examined the disparities in access to substance abuse treatment among minority and female Medicaid adolescents in one state. Study Design: Data were extracted from Medicaid claims/encounter and enrollment data sets for July 1995 through June 2001. Access to substance abuse services for the population of Medicaid-enrolled adolescents was examined in two ways. The first considered annual access rates (proportion of the population who used a service) and probability of substance use. The second subset the data to consider the pool of adolescents who used their first substance abuse service within the time period by studying the age at which their first substance abuse service was received. Each of these approaches addressed a slightly different aspect of the disparity question: the annual analysis considered whether race or gender differences in access existed in this population; the “first use” analysis considered whether there were system-wide differences in the detection of substance abuse problems for black and female adolescents, as compared to whites and males. Descriptive and regression analyses were used to examine racial and gender disparities in annual access rate, probability of service use, and age at first substance abuse service. Youth age, Medicaid eligibility category, and previous use of mental health services were included as covariates. Population Studied: Statewide Medicaid-enrolled 12-17 year olds. Principal Findings: The study demonstrated significant differences by race and gender in all access measures. Whites were nearly two times as likely as blacks (OR 1.96) to access substance abuse services, while males accessed services at a 75% greater rate(OR 1.78) than females. Gender and race were also both significant predictors of age at first substance abuse service, controlling for other covariates, with female and white adolescents being significantly younger as they entered treatment. Conclusions: This study’s findings that white adolescents are gaining access to substance abuse treatment at significantly higher rates and an earlier age than black adolescents may be explained by previous research findings that the use of alcohol and drugs is higher among whites than blacks. However, the disparities found in this study are greater than differences in prevalence rates explain. Each comparison between these groups shows white males being treated at a higher rate than any of the other groups, almost twice the rate of white females and black males, and more than six times that of black females. These proportions clearly are discrepant with the information available on differing prevalence rates for these groups. By far the most underserved group according to this and other measures in this study is black females. Implications for Policy, Delivery or Practice: The low access rates, in general, and the differential access rates by race and gender raise questions regarding the identification of substance abuse problems at the system level. The implementation of guidelines for screening by primary care physicians and psychiatrists is discussed, along with barriers to implementation and accurately reporting substance abuse diagnoses.These findings indicate the importance of appropriate monitoring of and research about access, not only broadly but for key population groups, such as adolescents and minority groups. Primary Funding Source: NIDA • Ethnic, Gender, and Age Related Differences in Treatment and Control of Dyslipidemia among Hypertensive Patients Katharine Hendrix, Ph.D., Jessica Riehle, R.N., Brent Egan, M.D. Presented by: Katharine Hendrix, Ph.D., Executive Administrator, Hypertension Initiative, General Internal Medicine, Medical University of South Carolina, 96 Jonathan Lucas Street, 826 CSB, Charleston, SC 29425; Tel: 843.792.6340; Fax: 843.792.0816; E-mail: hendrikh@musc.edu Research Objective: Assess demographic differences in lipid control rates and treatment patterns among dyslipidemic, hypertensive patients in primary care. Study Design: Demographic information, blood pressure, LDL-cholesterol, and medications were obtained on 72,351 hypertensive patients from 262 primary care providers at 69 sites in the Southeast. Population Studied: 72,351 hypertensive patients from the Hypertension Initiative database. 38,116 of these patients were also diagnosed with concomittant dyslipidemia. Principal Findings: Fifty-two percent of patients did not have a cholesterol measurement documented in the past year. Women and patients <40 years old were less likely to have an annual cholesterol measurement than men and older, samerace counterparts (p<0.001). Thirty-five percent of all hypertensive dyslipidemic patients had not been prescribed any anti-lipidemic medication, whereas 15% were on a statin and another anti-lipidemic. Women received fewer statin prescriptions than men (48.8% vs. 63.7%, p<0.0001). Fewer African Americans (AA) than Caucasians (C) reached LDL levels of <100 or <130 mg/dL (p<0.0001). Among C and AA patients, those <40 years old were less likely than older, samerace counterparts to have reached LDL <100 or <130 mg/dL (p<0.001). Younger patients had fewer annual cholesterol measurements and were less likely to receive anti-lipidemic medication and to have LDL controlled than older, same-race counter-parts in each ethnic group(p<0.0001) Conclusions: Demographic characteristics of hypertensive patients, especially younger age group, are associated with significant differences in diagnostic testing, treatment and control of hyperlipidemia in primary care. This primary care information can be used to guide education and policy interventions to improve outcomes and reduce disparities. Implications for Policy, Delivery or Practice: This primary care information can be used to guide education and policy interventions to improve outcomes and reduce disparities. Primary Funding Source: Duke Endowment greater probability of choosing a plan, rather than being assigned. Sample members who learned about plans from their doctors were more likely to report the information was very useful, but these sample members were less likely to choose their plans. People with mental retardation were more likely to rely on friends and family for information, but these sources were not associated with choosing plans and providers. Less than half of SSI enrollees rated providers’ information about tests and procedures very good or excellent, and a fifth rated it poor or fair. Adults with communications impairments were the least satisfied with information about tests and procedures. Conclusions: Although SSI enrollees faced barriers to informed participation, most were able to overcome the barriers. Others, especially people with cognitive and communication impairments, were less able to receive information or make informed decisions. Implications for Policy, Delivery or Practice: Information dissemination should be tailored to the diverse needs of people with disabilities. While most people with disabilities appear to be able to overcome barriers to receiving and using information to make health care decisions about plans and providers, greater efforts may be needed to assist people with communications and cognitive impairments. Information resources targeted to the family and friends of people with mental retardation may improve their ability to make informed decisions. Additional assistance is needed to facilitate information sharing between providers and people with communication impairments. Primary Funding Source: DHHS Assistant Secretary for Planning and Evaluation • Barriers to and Enablers of People with Disabilities’ Informed Participation in Health Care: Evidence from SSI Enrollees in TennCare Steven Hill, Ph.D., Judith Wooldridge, MA • Predictors of Early Prenatal Care Use, Preterm Birth and Low Birthweight Among Rural and Urban Women Marianne Hillemeier, Ph.D., M.P.H., Carol Weisman, Ph.D., Gary Chase, Ph.D., Megan Darnell, M.S. Presented by: Steven Hill, Ph.D., Service Fellow Economist, CFACT, AHRQ, 540 Gaither Road, Rockville, MD 20850; Tel: 301.427.1672; Fax: 301.427.1276; E-mail: shill@ahrq.gov Research Objective: Describe people with disabilities’ barriers to informed participation in health care for people with disabilities, and assess which information sources are more useful and associated with choosing plans and providers, rather than being assigned. Study Design: Telephone survey of Supplemental Security Income (SSI) enrollees in TennCare, Tennessee’s Medicaid managed care program. Population Studied: SSI enrollees in TennCare in Shelby County, Tennessee, 1998-1999. Principal Findings: Some SSI enrollees have cognitive impairments, difficulty using a telephone, and difficulty communicating, which can hinder informed participation in health care. In TennCare, most SSI enrollees chose their plan and providers, but a minority did not know they could choose and were assigned to them. Most SSI enrollees received information to help them choose plans, and most were confident they could find out how to change providers. On the other hand, a minority did not know they could choose plans and were dissatisfied with the choice of providers. Information from the state and plans was associated with a Presented by: Marianne Hillemeier, Ph.D., M.P.H., Assistant Professor, Health Policy & Administration, Pennsylvania State University, 116 Henderson Building, University Park, PA 16802; Tel: 814.863.0873; Fax: 814.863.2905; E-mail: mmh18@psu.edu Research Objective: To examine predictors of prenatal care use, preterm birth, and low birthweight at the individual and community levels and to examine the impact of urban-rural maternal residence using measures that capture the differences among types of rural communities. Study Design: Birth certificate records were analyzed for the 28-county central Pennsylvania region, which contains urban areas as well as a sizable rural population. Birth record data were merged with county-level indicators of socioeconomic status and health care resources from the Area Resource File and U.S. Census data. Multiple logistic regression analyses were conducted to model the determinants of 1) receipt of early (first trimester) prenatal care; 2) preterm birth (<37 weeks gestation); and 3) low birthweight (<2500 grams). Independent variables included measures of maternal sociodemographics (age, education, race/ethnicity), maternal health (smoking, chronic high blood pressure, diabetes), and county-level socioeconomic and health care resources (percent high school graduates, percent nonwhite, percent of persons below poverty level, primary care physicians/100,000 population), and urban-rural maternal residence. Rurality was measured in two ways: 1) using RUCA codes aggregated into four categories; and 2) using 9-category Urban Influence Codes for counties. Each regression model was estimated for all births, all singleton births (using previous preterm birth as a covariate), and for all first births in 2002. Population Studied: All births, all singleton births, and all first births in the 28-county central Pennsylvania region in 2002. Principal Findings: Maternal education was a strong predictor of early prenatal care (adjusted odds ratio=5.91, 95% CI 5.49 to 6.36, p<.0001). Maternal health was also a significant predictor of early prenatal care, as well as preterm birth and low birthweight. For example, the adjusted odds ratio for chronic hypertension as a predictor of early prenatal care was 1.57 (95% CI 1.06 to 2.34, p=.0258), and the corresponding odds ratio for low birthweight was 3.50 (95% CI 2.64 to 4.63, p=<.0001). County-level characteristics were not uniformly informative, but the percent of persons in poverty predicted preterm birth, low birthweight, and reduced likelihood of early prenatal care. Results for the two measures of rurality were similar. Urban focused areas had the highest levels of early prenatal care, while isolated smaller rural areas had the lowest levels. Isolated rural towns had significantly lower rates of early prenatal care than all other areas, but the pattern of increase was not monotonic with decreasing rurality. Conclusions: Women’s health status is an important predictor of early prenatal care use, and has implications for adverse infant outcomes. Women in isolated small rural areas have the least optimal prenatal care patterns, however the association between decreasing rurality and greater likelihood of early prenatal care use is not linear. Implications for Policy, Delivery or Practice: Access and appropriate utilization of prenatal care among women in isolated small rural areas is of particular concern. Detailed study of the relationships between degree of rurality and medical care use is needed to optimally target intervention activities. • Racial and Ethnic Disparities and Perceptions of Health Care: Does Health Plan Type Matter? Kelly Hunt, M.P.P., Ayorkor Gaba, B.A., Risa Lavizzo-Mourey, M.D., M.B.A. Presented by: Kelly Hunt, M.P.P., Research Officer, Research and Evaluation, The Robert Wood Johnson Foundation, Route 1 and College Road East, Princeton, NJ 08543; Tel: 609.627.5994; E-mail: khunt@rwjf.org Research Objective: To examine whether differences in the distribution of health plans by race and ethnicity explain differences in satisfaction and trust with health care providers across racial/ethnic groups. Study Design: Multivariate analyses used regression methods to detect independent effects of patient/respondent race and ethnicity on satisfaction and trust with health care provider, while controlling for demographics, geography, and enrollment in different types of health plans. Population Studied: Data were derived from the 1998-99 Community Tracking Household and Followback Studies (CTS) and consisted of a nationwide sample of adults (18 and over). Principal Findings: Racial and ethnic minorities are more likely than whites to have lower levels of trust and satisfaction with their health care provider. Plan type does not mitigate the relationship between race/ethnicity and trust and satisfaction. Conclusions: Disparate levels of trust and satisfaction exist within ethnic and minority populations, even when controlling for the distribution of individuals across types of health plans. The results demonstrate a need to consider the issue of disparate trust and satisfaction as fundamentally about race and ethnicity and not plan type. Implications for Policy, Delivery or Practice: Our findings suggest that trust and satisfaction should be carefully considered as interventions are designed to address racial and ethnic disparities in health care. In evaluating programs designed to reduce disparities in trust and satisfaction, we need the ability to measure patient assessments of care as well as other health outcomes to be sure we address the issue on all levels because they have been linked to patient assessments of health care, service utilization, the decision to switch health plans, and treatment compliance. • Racial/Ethnic Disparities in Hospital Readmissions for Diabetes-Related Conditions H. Joanna Jiang, Ph.D., Roxanne Andrews, Ph.D., Daniel Stryer, M.D., Bernard Friedman, Ph.D. Presented by: H. Joanna Jiang, Ph.D., Social Scientist, Center for Delivery, Organization, and Markets, Agency for Healthcare Research and Quality, 540 Gaither Road, Rockville, MD 20850; Tel: 301.427.1436; Fax: 301-427-1430; E-mail: jjiang@ahrq.gov Research Objective: Considerable differences in prevalence of diabetes and management of the disease exist among racial/ethnic groups. More needs to be known about the relationship of race/ethnicity, health care treatment, and health outcomes for diabetes. The purpose of this study is to examine racial/ethnic differences in hospital readmissions for diabetes-related conditions. Effective outpatient follow-up care can help reduce readmission rates. Study Design: Logistic regressions were employed to estimate racial/ethnic differences in the likelihood of sixmonth readmission by payer adjusting for patient demographic, clinical, and socioeconomic characteristics and hospital attributes. Population Studied: Nonmaternal adult insured patients hospitalized for diabetes-related conditions in five states (CA, MO, NY, TN, VA) identified from the 1999 hospital discharge data of the Healthcare Cost and Utilization Project (HCUP). Principal Findings: The risk-adjusted likelihood of readmission was significantly (p<.05) higher for Hispanics (odds=1.12, 1.14, 1.29 among private, Medicaid, and Medicare patients, respectively) and nonHispanic blacks (odds=1.12 among Medicare patients) compared with nonHispanic whites. In the Medicare subpopulation, nonHispanic blacks and Hispanics had higher percents of readmissions for acute complications and microvascular disease while nonHispanic whites had higher percents of readmissions for macrovascular conditions. Conclusions: Racial/ethnic minorities have higher hospital readmission rates for diabetes-related conditions even controlling for demographic, clinical, and socioeconomic characteristics. The racial/ethnic differences are greater among Medicare patients than among patients with private insurance or Medicaid coverage. Readmission diagnoses also vary by race/ethnicity with some of the complications that are potentially preventable with effective postdischarge care. Implications for Policy, Delivery or Practice: The finding that disparities are strongest among the Medicare population underscores the importance of the new national initiatives that the Centers for Medicare & Medicaid Services (CMS) is undertaking through the Quality Improvement Organizations (QIOs) for improving outpatient diabetes care among the underserved populations. Among the three largest racial/ethnic groups, Hispanics have the highest likelihood of poor outcomes across the entire adult population. Considering that the Hispanic population is growing faster than the nation as a whole and Hispanics have a substantially high risk of developing diabetes, policy makers and clinicians need to devote more attention to address the special needs of this population. Primary Funding Source: AHRQ • A Model of Health Determinants and Health Status Among Midlife Low-Income Women Teresa Barry, M.S.N, RNC, Katherine Kaiser, Ph.D., APRN, BC, Katherine Laux Kaiser, Ph.D., APRN, BC Presented by: Katherine Kaiser, Ph.D., APRN, BC, Associate Professor, College of Nursing, University of Nebraska Medical Center, 985330 Nebraska Medical Center, Omaha, NE 681985330; Tel: 402.559.6576; Fax: 402.559.6379; E-mail: kkaiser@unmc.edu Research Objective: The primary objective was to pilot the Population Health Determinants and Health Status Model (Barry, 2003) with a midlife low-income population of women. The secondary objective was to describe the perceived health status of midlife low-income women. Study Design: This research study used a descriptive correlational design to pilot test the model and describe the relationship of health determinants and health status. The study was conducted using a secondary analysis of selected cross-sectional extant enrollment data from the Nebraska Medicaid Managed Care program. Population Studied: The study population included 1,100 low-income women in Nebraska aged 40-64 who enrolled in Medicaid Managed Care from July 2000 through June 2002. Principal Findings: The results of the pilot study indicate that the model is predictive of the influence of multiple health determinant indicators on perceived health status in midlife low-income women. Results demonstrate that health determinant indicators accounted for 31.3% to 43.6% of the variance in perceived health status. Preliminary results from this study provide a foundation for further research with the Population Health Determinants and Health Status Model. Descriptive results indicate the illness burden of this population is great, with only 16% reporting no medical conditions, and nearly half of the sample reporting their overall perceived health status as fair/poor. Health Status Questionnaire-12 (HSQ-12) mean scores overall were lower for this population than other studies have found. Conclusions: Poverty is a systemic and ongoing source of vulnerability and poor health for women. The cumulative burden of social, economic, and political disparities as well as individual conditions and life events negatively impacts perceived health status for women, especially as they reach midlife. In addition, poverty and illness burden of midlife women has a profound impact on society, particularly their potential influence on the health status of the next generation, their children. 25% or more of the children in the US are reared in female-headed households, and almost 50% of these children are in poverty. Policy, practice, and service delivery are all influenced by the long-term consequences of vulnerability and poor health. Implications for Policy, Delivery or Practice: Reducing disparities for midlife low-income women will take improvement in three arenas of policy, practice and delivery. Related to policy, preventive health policies for women of all ages are critically important, but crucial to those populations with increased illness burden. Understanding and shaping the interaction of determinants, perceived health, and interventions to reduce illness burden, promote health management, and increase quality of life is needed to meet the needs of this vulnerable population. In practice, we need to raise awareness of vulnerability of this age group, and their influence on the health of their children. Increasing focus should be placed on primary prevention strategies such as promoting healthy lifestyles, health management, early detection, and disability limitations. Service delivery implications include understanding patterns of health service use, the influence of women on their children’s health, and interventions to increase the use of primary prevention services. Primary Funding Source: , Lincoln/Lancaster County Health Department/Nebraska Health and Human Services System • Neighborhood and Individual Determinants of Low Birth Weight in Los Angeles County Judith Katzburg, Ph.D, M.P.H., R.N., Ronald Andersen, Ph.D. Presented by: Judith Katzburg, Ph.D, M.P.H., R.N., AHRQ Post doctoral Fellow, Health Services, UCLA, 801 Sassafras Way, Oak Park, CA; Tel: 818.889.8739; E-mail: jkatzbur@ucla.edu Research Objective: Significant low birth weight disparities exist by race/ethnicity as well as by geographic region in Los Angeles County. Current public health planning considers geographic as well as racial and ethnic disparities in funding allocations. This research intends to inform policy by identifying individuals and areas of the County wherein exists the greatest need to reduce low birth weight infants and improve pregnancy outcomes. This study intends to examine both individual and neighborhood determinants of low birth weight. The appropriateness of targeting geographic regions will be considered. Study Design: This is a retrospective study using logistic regression and multilevel modeling to analyze the outcome of low birth weight in Los Angeles County. A unique data set was created by linking the year 2000 birth certificate data with the year 2000 U.S. census data. Selected individual characteristics of the mothers as well as selected neighborhood effects of their respective census tracts were evaluated. In particular, racial and ethnic effects at both the individual and census tract level are evaluated. In addition, outcomes at the level of the eight service planning areas of Los Angeles County is currently being evaluated. Population Studied: The population studied includes over 150,000 infants born in the year 2000 to mothers who are residents of Los Angeles County. Selected individual characteristics of the mothers as well as selected neighborhood effects of their respective census tracts were evaluated. Principal Findings: Only certain groups appear to be at risk. In multivariate analyses, Latina women do not appear to be at increased risk for low birth weight in comparison to White women. However, both Asian and African American women have increased odds for having a low birth weight infant in comparison to Latinas. Other significant determinants at the individual level include infant's birth order and gender, mother's place of birth (with women born in Mexico appearing to have a protective effect), mother's marital status and age, and early and adequate access to prenatal care. The neighborhood effects were particularly informative. Race/ethnicity had no significant effect at the neighbor level. However, the socio-economic status of the neighborhood did make a difference. In neighborhoods with higher levels of education, the odds of having a low birth weight infant were significantly reduced. Conclusions: Disparities at the individual level do exist with African American and Asian women at greatest risk. Socioeconomic disparities at the neighborhood level appear to play a role in outcomes as well. However, racial and ethnic differences in neighborhoods do not appear to be determinants in low birth weight outcomes. Implications for Policy, Delivery or Practice: Racial and ethnic disparities in birth outcomes continue to be of concern in Los Angeles County. However, policies that target interventions to geographic regions based on racial and ethnic differences may be misguided. Rather, neighborhoods might better be targeted according to their economic risk, with lower SES neighborhoods receiving more intensive interventions. Within these neighborhoods, programs interventions developed to target specific racial and ethnic groups at risk may be appropriate. Nonetheless, given that Latina births account for the highest number of births in the County, it would be misguided to ignore the issue of low birth weight among this population, given that many of the county’s LBW babies come from this population. Primary Funding Source: AHRQ • Impact of Medical Mistrust and Perceptions of Racism on Breast Cancer Screening Amal Khoury, Ph.D., M.P.H., Nedra Lisovicz, Ph.D., M.P.H., Amanda Avis, M.P.H., Deonna Allen, M.P.H. Presented by: Amal Khoury, Ph.D., M.P.H., Assistant Professor, Center for Community Health, University of Southern Mississippi, 118 College Drive #5122, Hattiesburg, MS 39406; Tel: 601.266.5435; Fax: 601.266.5043; E-mail: amal.khoury@usm.edu Research Objective: Breast cancer is a major cause of morbidity and mortality in American women. Disparities in breast cancer screening rates and mortality rates among subgroups of women are well-documented. Researchers have examined the association between women's adherence to screening guidelines and such factors as knowledge and attitudes about breast cancer and sociodemographic characteristics. This study examines the association between utilization of screening services among women in the deep south and medical mistrust and perceptions of racism. We hypothesize that mistrust and perceptions of racism are independent predictors of screening utilization after controlling for other variables. Study Design: A cross-sectional survey of women 40 years of age and older was conducted in summer 2003. Computerassisted telephone interviewing, CATI, was used. A survey questionnaire was developed, pilot tested with 30 women, revised, and finalized. An extensive literature review established face validity of the questionnaire. The questionnaire took 15 minutes to complete and collected data about 1) general healthcare utilization; 2) knowledge, attitudes, and practices regarding breast cancer screening; 3) medical trust and perceptions of racism within the healthcare system; and 4) sociodemographic data. Population Studied: The target population was all women 40 years of age and older residing in the state of Mississippi. A representative sample of 1052 was surveyed. Principal Findings: Two-thirds of surveyed women reported having a mammogram wihin the year preceding survey, and 72% reported having a clinical breast exam within the past year. Screening rates were lower among minorities and lowincome groups. Three items assessed women's trust of the healthcare system. Approximately 2 of 3 women agreed that rich people received better medical care than poor people, and 3 of 4 women agreed that health insurance affected the kind of care that a person received. Almost half of the respondents indicated that hospitals sometimes did not tell patients the truth. Three other items assessed women's perceptions of racism. A majority of women believed that doctors took the medical complaints of people of their race seriously. However, 31% reported that doctors hid information from patients of their race, and 42% believed that hospitals did not provide the same kind of care to people of different racial groups. Analysis of the association between screening utilization and medical mistrust and perceptions of racism is underway Conclusions: Significant proportions of women in Mississippi do not adhere to breast cancer screening guidelines. Disadvantaged women are less likely to adhere to screening guidelines and report higher levels of medical mistrust and perceptions of racism than other groups. Implications for Policy, Delivery or Practice: Medical mistrust and perceptions of racism appear to be barriers to screening. Research is needed to better understand the reasons behind the relatively high levels of medical mistrust. Interventions are needed to address those barriers, particularly among disadvantaged groups. Such interventions should complement the efforts to eliminate healthcare disparities. Primary Funding Source: The Susan G. Komen Breast Cancer Foundation • Socioeconomic Disparities in Children's Out-of-Pocket Health Care Expenditures Sabrina Wong, Ph.D., Sue Kim, Ph.D., M.P.H., Alison Galbraith, M.D., Paul Newacheck, Dr.PH Presented by: Sue Kim, Ph.D., M.P.H., Postdoctoral Scholar, Department of Medicine, University of California, San Francisco, 3333 California Street, Suite 335, San Francisco, CA 94143-0856; Tel: 415.502.4078; Fax: 415.502.8291; E-mail: sekim@medicine.ucsf.edu Research Objective: Attention has focused on identifying and ameliorating disparities in health and health care, including economic disparities. While Medicaid expansions in the 198090s were designed to improve financial access to health services for low-income children, little is known about economic disparities in the financial burden of children's outof-pocket (OOP) health care expenditures. This study’s objective is to examine whether poor children experience similar financial burden of OOP health care expenditures compared to children in other income groups, and to examine the effect of insurance on financial burden. Study Design: The primary outcome, financial burden, was measured as the amount of money spent OOP for each child per $1000 of family income. All OOP health care expenditures for each child were aggregated for the year. Each child's family income was categorized by Federal Poverty Level (FPL). Multivariate linear regression was used to model the degree of financial burden for different income groups, controlling for insurance status, age, sex, race/ethnicity, family size, and region. Due to the existence of skewed data in the outcome, analyses were done using log-transformed data, then backtransformed. Stata was used in the analyses to account for the complex survey design. Population Studied: We selected children 0-18 years of age from the 2000 Medical Expenditure Panel Survey (MEPS) (n=7,714) with household income>0. Principal Findings: Children in families in the poorest income groups had significantly increased financial burden of OOP medical expenditures. Compared to children in families with incomes greater or equal to 400% FPL, children in families with incomes less than 100% FPL had about 3 times greater financial burden (P<.01), 100-199% FPL had 1.3 times greater financial burden (P<.01), and 200-300% FPL had about 0.5 times greater financial burden (P<.01). Uninsured children had financial burden that was about 65% greater than that of insured children (P<.01). Conclusions: Economic disparities exist in the financial burden of children’s OOP health care expenditures, with the poorest children having three times the financial burden as children in the highest income group. However, having insurance has a salutary effect in reducing financial burden. Implications for Policy, Delivery or Practice: Despite the large scale expansions of Medicaid coverage and implementation of the State Children’s Health Insurance Program (SCHIP), families in the lowest income groups experience higher financial burden. It would be important to examine provisions that limit cost-sharing and consider policies that will alleviate the regressive pattern of financial burden. Primary Funding Source: AHRQ • Understanding Rural-Urban Differences in Access to Care: Is It Who You Are or Where You Live? Sharon Long, Ph.D., Jennifer King, B.A., Terri Coughlin, M.P.H. Presented by: Sharon Long, Ph.D., Principal Research Associate, Health Policy Center, The Urban Institute, 2100 M Street, N.W., Washington, DC 20036; Tel: 202.261.5656; Fax: 202-223-1149; E-mail: slong@ui.urban.org Research Objective: To examine rural-urban differences in access to health care for the overall adult population and for low-income adults. To describe the share of observed disparities in access to care due to individual and community characteristics and the share which cannot be explained by differences in observed characteristics. Study Design: We compare the characteristics of urban and rural adults and examine differences in their access to health care using three broad measures: having a usual source of care, doctor visits, and unmet need for medical care. Through regression-based decomposition methods, we determine the share of the observed differences in these access measures that can be explained by differences in individual and family characteristics, health and disability status, the local health care market, and community characteristics. In addition to conducting this analysis for the overall population, we examine access disparities between low-income urban and rural adults, an especially vulnerable subgroup. Population Studied: A nationally representative sample of adults from the 1997, 1999, and 2002 National Survey of America’s Families. County-level community characteristics and local health care market data are from a variety of sources including the Area Resource File and the U.S. Census. Principal Findings: Preliminary findings indicate that adults in rural areas have less access to health care than those in urban areas, both in the overall population and the lowincome population. Some, but not all, of this disparity can be attributed to differences in the characteristics of the individuals in rural areas and the communities in which they reside. Conclusions: Given our preliminary findings, it appears that adults in rural areas face additional access barriers compared to adults with similar characteristics in urban areas. Implications for Policy, Delivery or Practice: Public efforts to reduce disparities in access to health care for rural residents should take into account the unique circumstances of those individuals and their communities. These include the greater share of elderly persons (and their long term care needs) and the more dispersed and small scale of providers that are available in rural areas. Primary Funding Source: CMS • Socioeconomic and Cultural Factors: African Americans and Tuberculosis Ana Lopez - De Fede, Ph.D, Muriel Harris, M.P.H.,Ph.D. Presented by: Ana Lopez - De Fede, Ph.D, Research Associate Professor, Institute for Families in Society, University of South Carolina, 937 Assembly Street - Carolina Plaza, Columbia, SC 29208; Tel: 803.777.5789; Fax: 803.777.1793; E-mail: adefede@sc.edu Research Objective: African Americans have a disproportianate share of TB cases in the United States - 48% of all US -born cases. The disparity remains as a legacy of poverty. racism, and poor access to care. The primary objective of this study was to identify and examine the impact of knowledge, beliefs and values of African Americans on health seeking and adherence behaviors. Study Design: Data were collected through in-depth interviewing using a semi-structure interview guide. Snowball and purposive sampling techniques were used with community advocates as gatekeepers. Standard qualitative analytic methods were used to interpret the data, including taxonomic and content analysis and code mapping. Population Studied: Fifty-two African Americans were interviewed with a diagnosis of TB residing in one of nine rural communities in South Carolina. Principal Findings: Results suggest a strong association between socioeconomic factors (poverty, rural residence, educational attainment,unemployment and accessto health care) and adherence to treatment. Cultural factors identified suggest the need for careful attention to trainig nurses and related personnel with increased emphasis on culturally appropriate outreach methods. TB carries a stigma within the community with an association with HIV/AIDS preventing effective case identification and treatment. Conclusions: Stigma and the legacy of racial relationships in the South cannot be ignored - TB is a disease that has traditionally been associated with issues of disparity and poverty. The ability of health care professionals to provide effective treatment will require careful attention to socioeconomic and cultural factors. Implications for Policy, Delivery or Practice: The research in the United States on TB has been limited to urban and foreign-born populations. This study provides insight into a growing problem among US-born African Americans residing in rural communities. Primary Funding Source: CDC • Gender Differences in the Diagnosis and Treatment of Schizophrenia and Other Serious Mental Illnesses in the VHA: Special Issues for Women Veterans Kristen Barry, Ph.D., John McCarthy, Ph.D., John McCarthy, Ph.D., Frederic Blow, Ph.D., Deborah Welsh, M.S., Laurie Brockmann, M.P.H., M.S.W. Presented by: John McCarthy, Ph.D., Research Investigator, HSR&D Field Program, Department of Veterans Affairs, P.O. Box 130170, Ann Arbor, MI 48113-0170; Tel: 734.769.7100 Ext. 6253; Fax: 734-761.2617; E-mail: John.McCarthy2@med.va.gov Research Objective: Women veterans constitute a small but growing minority of all patients receiving care in the Veteran Affairs (VA) health care system. In general, women appear to use disproportionately more mental health services than men, with particular concerns raised for patients with schizophrenia and other serious mental illnesses. The purpose of this study was to evaluate gender differences in utilization of physical and psychiatric health services among veterans with schizophrenia and other serious mental illnesses in the VA health care system. Study Design: This was a two-year cohort study. Study variables included demographics, diagnoses, cumulative days of hospitalization, outpatient visits, prescription drugs by diagnosis and age, and comorbidities. Changes in care and status for these veterans between Fiscal Year (FY) 1999 and FY 2000 were analyzed with specific analyses on veterans with schizophrenia. Population Studied: The sample in this study was drawn from the VA’s National Psychosis Registry, a data base used to monitor and provide feedback to the VA on all veterans with psychosis treated in the system, and consisted of 12,166 women (7%) and 161,576 men (93%) treated in the VA in FY 1999. Principal Findings: Women and men differed along two important dimensions: diagnosis and age. Women were younger and more likely to have a bipolar diagnosis. Women also had more outpatient visits in FY 1999 than men. However, significantly more men (47%) than women (43%) with schizophrenia were prescribed any atypical antipsychotic medications. Conclusions: Women suffering from schizophrenia and other serious mental illnesses present unique treatment issues and challenges in the VA health care system and their care will require focused research and policy attention. Implications for Policy, Delivery or Practice: While a substantial gender minority in the VA health care system, there has been little research to examine gender differences among VA patients with serious mental illness. This is the first national study on one of the largest populations of women with serious mental illnesses to determine differences in diagnoses and care of women with schizophrenia compared to men. Best practices recommendations are given to address concerns for this vulnerable population of female veterans with schizophrenia and other serious mental illnesses. Primary Funding Source: VA • Functional Limitation and Chronic Disease in American Indian and Alaska Native Elders Leander McDonald, Ph.D., Patricia Moulton, Ph.D., Kyle Muus, Ph.D., Alana Knudson, Ph.D. Presented by: Leander McDonald, Ph.D., Assistant Professor, Center for Rural Health, University of North Dakota, 501 N. Columbia Road, Grand Forks, ND 58202-9037; Tel: 701.777.3848; Fax: 701-777-6779; E-mail: rmcdonal@medicine.nodak.edu Research Objective: There is a paucity of information about the prevalence of chronic disease and functional limitations among American Indian and Alaska Native elderly populations, and there is no information available about rural/urban differences among the tribes. The objective of this study is to determine if there are differences in prevalence of chronic disease among Native elders across age groups (5564, 65-74, 75-84 and 85+) in urban vs. rural vs. frontier counties. In addition, the relationship between functional limitation and chronic disease rates will be determined. Study Design: The data for this study were derived from a nationwide assessment survey of rural Native American elders’ health and social needs conducted in 2000 by researchers at the University of North Dakota Center for Rural Health’s National Resource Center on Native American Aging (NRCNAA). The survey included self-reported chronic disease measures (arthritis, congestive heart failure, stroke, asthma, cataracts, breast cancer, colon/rectal cancer, lung cancer, other cancer, high blood pressure and diabetes). Activities of daily living (ADLS) and instrumental activities of daily living (IADLs) were also included. Regression analysis was used to assess the influence of functional limitation on prevalence of chronic disease. Population Studied: The Native elder data set (N=9,403) is comprised of American Indian and Alaska Native elders (age 55+) from throughout the United States. The data set represents over 133 tribes from 89 different sites with 11 of 12 Indian Health Service regions represented. Principal Findings: It is generally hypothesized that higher rates of self-reported rates of chronic disease will be associated with areas of low population density and individuals with greater functional limitation. Preliminary results indicate that differences in disease prevalence exist across severity of functional limitation. Conclusions: Findings illustrate, rural America’s American Indian and Alaskan Native elders experience significant health problems in regard to chronic disease that lead to a loss of the quality of life. Implications for Policy, Delivery or Practice: Policy implications for improving access to needed health and social services among this swiftly expanding age/ethnic cohort will be provided. These implications will be of interest to health care facilities which serve Native elders. Information about functional limitation and chronic disease in older individuals may also be relevant to the general population when considering quality of life issues. Primary Funding Source: HRSA • How Do Homeless Veterans Fare in Usual VA Primary Care? Jim McGuire, Ph.D. Presented by: Jim McGuire, Ph.D., Program Evaluation Director, Homeless Services, Community Care, VA Greater Los Angeles Healthcare System, 11301 Wilshire Boulevard, Bldg 500, Room 6651 (Mail: 10H-5), Los Angeles, CA 90073; Tel: 301.478.3711 Ext. 41450; Fax: (310) 268-4946; E-mail: James.McGuire@med.va.gov Research Objective: To determine predictors among homeless veterans referred to standard VA primary care providers for a. use of primary care services and b. receipt of preventive care interventions. Study Design: This study uses interview and medical record data from the comparison group (N=130) in a quasiexperimental longitudinal program evaluation. Population Studied: Homeless veterans with serious mental illness who had no primary care during the year prior to study enrollment and were assigned at study entry to usual VA primary care. Principal Findings: Fifty eight per cent of the sample were assigned and met with a primary care provider. Regression analyses based on Gelberg’s access to care for vulnerable populations model identified the following significant predictors: a. for primary care service use (adjusted model R square = .30, p<.001), social support for medical care (.393), SF-36 physical functioning score (.057), and having an assigned primary care provider (2.486); b. for appropriate prevention interventions received (adjusted model R square = .25, p<.001), years of education (.049), having an assigned primary care provider (.243), and number of primary care visits (.043). Conclusions: Homeless veterans in this sample have a much lower rate of access to usual VA primary care than other veterans. Once connected with a primary care provider, health care need and social support are related to use of services, and use of services and education are related to receipt of primary care prevention. Implications for Policy, Delivery or Practice: Alternative models of connecting homeless people to primary care and encouraging and ensuring their return for care could improve care for this vulnerable patient population. Primary Funding Source: VA • Community-Based Innovative Approaches to Meeting Rural Health Care Demands Heather McIlvaine-Newsad, Ph.D., Heather McIlvaineNewsad, Mary Jane Clark, R.N., M.S., CHES Presented by: Heather McIlvaine-Newsad, Assistant Professor, Illinois Institute for Rural Affairs and Sociology & Anthropology, Western Illinois University, Stipes Hall 525, 1 University Circle, Macomb, IL 61455; Tel: 309.298.1613; E-mail: h-mcilvaine-newsad@wiu.edu Research Objective: Rural residents of Illinois are disproportionately more likely to encounter barriers to health care than their urban counterparts. First the health care needs of rural residents exceed those of their urban counterparts, and second the resources to address those needs are usually inadequate. This study identifies innovative strategies rural communities in Illinois and Ohio have implemented to provide their residents with improved health care. Study Design: This study applied a three-prong approach. First data were collected through a questionnaire administered to non-metro municipalities, critical access hospitals, and economic development organizations in Illinois. Second, a qualitative case study approach was applied using key informant interviews with community leaders, health care providers, and social services, public and school health providers, and focus groups of health care leaders. Finally, a secondary analysis of 2003 Census Data, and state and county data on health care resources and demographics was performed. Population Studied: In-depth case studies of six innovative strategies were conducted in Illinois and Ohio. Principal Findings: Findings indicate twenty of the twentyseven counties in Illinois designated as having under-served populations are rural counties. Despite the dire state of health care services in rural Illinois and Ohio, communities and agencies have been implementing creative strategies to help meet the needs of those individuals who are under-served. These approaches include volunteer rural emergency medical services departments, mobile mammography clinics, inschool wellness centers, telemedicine clinics, community based health care clinics for the uninsured, urgent care centers for patients with non-emergency needs, and innovative group insurance policies for self-employed individuals. Conclusions: Regardless of the focus or scope of the project, three main variables were present in all of the projects surveyed including: (1) Collaboration with a plethora of federal, state, and private agencies. Evidence of a collaborative approach to problem solving and resource sharing was present in all successful projects. (2) Community involvement and support. Those projects that were most sustainable reported community involvement and support as one of the key reasons why the project succeeded. (3)Funding continues to be the most significant barrier for attaining long-term success of a project. Agency directors, community leaders, and project managers spoke in depth about the importance of finding, attaining, and maintaining funding to support projects. Implications for Policy, Delivery or Practice: Additional follow-up work is needed to make this general information more useful and available for health care providers and others involved in meeting the health care needs of Illinois’ rural population. Collaboration, networking, and sharing of resources are effective ways for those working on innovative health care projects to attain funding and develop effective community-based models. Demographic, economic, and cultural barriers influence rural health care decisions made by consumers’ about when and where to seek health care. Primary care providers should be encouraged to work in rural areas, or to provide services on a routine basis to rural clients. Many successful and innovative projects are providing valuable services to rural health care consumers. Primary Funding Source: Illinois Governor’s Rural Affairs Council & Illinois Department of Public Health-Center for Rural Health Gender also had an effect on utilization of various health services: women were more likely than men to use a service or report a doctor visit. Specialist visits were the only service that females were less likely to use than males. In terms of race and ethnicity, two nonwhite groups had greater utilization than whites did for certain services: blacks for ER visits, taking prescription medicines, using medical equipment and home health care; and American Indians for hospitalizations and ER visits. Otherwise, utilization by nonwhite groups tended to be the same as or less than that of whites. Conclusions: Although all health condition variables were found to be statistically significant predictors of every health utilization measure, it does not necessarily mean that whether or not a person has a particular health condition makes a great deal of difference in the propensity to use health care services. For many types of services, demographic factors were as important--if not more important--in explaining variations in use. Implications for Policy, Delivery or Practice: Even if chronic conditions were ameliorated, it would have only a small impact on use of such health care services as emergency rooms, special therapy, and home care. Primary Funding Source: CMS • Health Services Utilization among M+C Enrollees with Chronic Health Conditions James Moser, Ph.D., Ioana Montel • Relationship between Unmet Health Needs, Age, Gender and Rurality in American Indian and Alaskan Native Elders Patricia Moulton, Ph.D., Brent King, M.A., Alana Knudson, Ph.D., Russ McDonald, Ph.D., Kyle Muus, Ph.D. Presented by: James Moser, Ph.D., Manager, BearingPoint, 1676 International Drive, McLean, VA 22102; Tel: 703.747.6962; Fax: 703.747.8750; E-mail: jwmoser@bearingpoint.net Research Objective: The focus of this study is on how the utilization of health services by Medicare+Choice enrollees is affected by having or not having at least one of five chronic health conditions. Study Design: Using data from the MMC-CAHPS Enrollee surveys, estimate models of health services utilization while controlling for characteristics of enrollees and other exogenous factors. Population Studied: Persons enrolled in Medicare+Choice (M+C) plans in 1997, 1998, or 1999. Principal Findings: For all five chronic conditions, persons with the condition were more likely to utilize health services than those without the condition. Health conditions were an important predictor of utilization for inpatient hospitalization, prescription drugs use and emergency room visits. Aged (65 and over) enrollees were less likely than non-aged enrollees to use all services. Aged beneficiaries were less likely to report a doctor’s office visit compared with respondents under age 65. Among the aged, the tendency to utilize services rose with age, in contrast to the finding for doctor’s office visits. Doctor visits were positively associated with years of schooling. College graduates were more likely to have had a doctor’s office visit than were those in the least educated group. Level of education was also positively associated with use of specialist visits, medical equipment and special therapy; for other services, however, level of education did not matter. Presented by: Patricia Moulton, Ph.D., Assistant Professor, Center for Rural Health, University of North Dakota, 501 N. Columbia Road, Grand Forks, ND 58202-9037; Tel: 701.777.6781; Fax: (701) 777-6779; E-mail: pmoulton@medicine.nodak.edu Research Objective: Little information exists regarding the health needs of Native elders. The objective of this study was to asess the qualitative nature of American Indian and Alaskan Native elders unmet health needs and examine response differences by rurality of gender and age categories. Study Design: The data for this study were derived from a nationwide assessment survey of rural Native American elders’ health and social needs conducted in 2000 by researchers at the University of North Dakota Center for Rural Health’s National Resource Center on Native American Aging (NRCNAA). The survey included an open-ended question "Do you have any unmet health needs that haven't been addressed?" Responses were analyzed for overlying themes and the number of responses for each theme. In addition, data were delinated and analyzed by rurality of respondents' residential location, gender and age category. Population Studied: The Native elder data set (N=9,403) is comprised of American Indian and Alaska Native elders (age 55+) from throughout the United States. The data set represents over 133 tribes from 89 different sites with 11 of 12 Indian Health Service regions represented. Principal Findings: Findings suggest differences between elders living in urban vs. rural vs. frontier areas in self-reported unmet health needs. These needs included dental, vision and hearing services/equipment, transportation to health care services and medical equipment, including new wheel chairs and other items. Conclusions: The need for increased access to health care services and medical equipment was indicated by American Indian and Alaskan Native elders and attitudinal differences were found depending on the population of the area the elder resided. Implications for Policy, Delivery or Practice: Policy implications for improving access to needed health and social services among this swiftly expanding age/ethnic cohort will be provided. These implications will be of interest to health care providers and facilities which serve American Indian and Alaskan Native elders. Information about health needs of older individuals may also be relevant to the general population. Primary Funding Source: HRSA • Relationship between Access to Health Care and Prevalence of Chronic Disease in American Indian and Alaska Native Elders Kyle Muus, Ph.D., Leander McDonald, Ph.D., Patricia Moulton, Ph.D., Alana Knudson, Ph.D. Presented by: Kyle Muus, Ph.D., Assistant Professor, Center for Rural Health, University of North Dakota, 501 N. Columbia Road, Grand Forks, ND 58202-9037; Tel: 701.777.3848; Fax: 701-777-6779; E-mail: klmuus@medicine.nodak.edu Research Objective: There is a paucity of information about prevalence of chronic disease among American Indian and Alaskan Native populations and there is no information about rural/urban differences in older Native elders. Furthermore, limited research is available on the association between chronic disease and availability of health services among Native elders. The objective of this study is determine if there are differences in prevalence of chronic disease in American Indian and Alaskan Native elders across age groups (55-64, 65-74, 75-84 and 85+) in urban vs. rural vs. frontier counties. In addition the relationships between measures of health care access and rates of chronic disease among Native Elders will be determined. Study Design: The data for this study were derived from a nationwide assessment survey of rural Native American elders’ health and social needs conducted in 2000 by researchers at the University of North Dakota Center for Rural Health’s National Resource Center on Native American Aging (NRCNAA). The survey included self-reported chronic disease measures (arthritis, congestive heart failure, stroke, asthma, cataracts, breast cancer, colon/rectal cancer, lung cancer, other cancer, high blood pressure and diabetes). Native elder data records were linked via state/county FIPS code with a subset of the 2003 Area Resource File (ARF). ARF is a health resource information system that contains more than 6,000 variables for each county in the U.S., including geographic codes and classifications; health personnel demographics; health facility numbers and types; hospital utilization; population characteristics and economic data; environment; and health professions training resources. Regression analysis was used to assess the influence of health care access on prevalence of chronic disease. Population Studied: The Native elder data set (N=9,403) is comprised of American Indian and Alaska Native elders (age 55+) from throughout the United States. The data set represents over 133 tribes from 89 different sites with 11 of 12 Indian Health Service regions represented. Principal Findings: It is generally hypothesized that higher self-reported rates of chronic disease will be associated with areas of low population density and poor access to hospital and physician care. Preliminary results indicate that differences in disease prevalence exist across categories of health care access. Conclusions: Findings illustrate specific, significant problems regarding the health status of rural Native elders and gaps in care access. Implications for Policy, Delivery or Practice: Policy implications for improving access to needed health and social services among this swiftly expanding age/ethnic cohort will be provided. These implications will be of interest to health care facilities which serve American Indian and Alaskan Native elders. Information about health care access and chronic disease in older individuals may also be relevant to the general population. Primary Funding Source: HRSA • Socioeconomic Determinants of Farmers' Health in the Lower Mississippi Delta Ari Mwachofi, Ph.D. Presented by: Ari Mwachofi, Ph.D., Post-Doctoral Research Fellow, Institute for Health Services Research and Policy Studies, Northwestern University, 339 E Chicago Avenue, 7th Floor, Chicago, IL 60611; Tel: 312.503.0448; Fax: 312.503.2936; E-mail: a-mwachofi@northwestern.edu Research Objective: What are the significant socioeconomic determinants of health of minority and majority farmers in the Mississippi Delta? Study Design: The study interviewed a stratified random sample of 649 farm households in Arkansas, Louisiana and Mississippi. The study over-sampled minority farm households in order to learn more about this population. Socioeconomic and self-assessed health data were collected through structured interviews. The study estimated the following six equations by logistic regression: 1. Self-assessed health = f(wealth, age, gender, marital status, years of schooling, and ethnicity) 2. Self-assessed health = f(household money income, age, gender, marital status, years of schooling, and ethnicity). 3. Self-assessed health = f(relative household income, age, gender, marital status, years of schooling, and ethnicity) 4. Changes in self-assessed health = f(wealth, age, gender, marital status, years of schooling, and ethnicity) 5. Changes in self-assessed health = f(household money income, age, gender, marital status, years of schooling, and ethnicity) 6. Changes in self-assessed health = f(relative household income, age, gender, marital status, years of schooling, and ethnicity) Population Studied: Minority and majority farmers in Arkansas, Louisiana and Mississippi. Principal Findings: The significant determinants of health are: wealth, age, race, schooling. Money income, relative income are statistically insignificant in explaining variations in health. Minority farmers have a higher probability of having poor health than majority farmers. Conclusions: 1.There is a significant and positive relationship between socioeconomic status and health. 2.Minority farmers have a higher probability of poor health than majority farmers 3. Wealth is a better measure of socioeconomic status than money income. Implications for Policy, Delivery or Practice: To be effective in improving health policies have to be wholistic to include improvement of socioeconomic status of farm households. Primary Funding Source: NIDRR • The Influence of Informal Care on Home Health Care Characteristics and Disparities Maryam Navaie-Waliser, Dr.P.H., Aubrey Spriggs, M.A., Shiela Neder, R.N., M.S.N., M.P.H. Presented by: Maryam Navaie-Waliser, Dr.P.H., Senior Research Associate, Center for Home Care Policy and Research, Visiting Nurse Service of New York, 5 Penn Plaza, 11th Floor, New York, NY 10001; Tel: 212.609.5762; Fax: 212.290.3756; E-mail: maryam.navaie@vnsny.org Research Objective: Although the literature has identified environmental, provider, and consumer characteristics as contributors to disparities in health care delivery, little is known about support factors that impact care processes, especially in a home health setting. This study examined whether informal (i.e., unpaid family/friends) care influenced the content and intensity of formal (i.e., paid professionals) home health services. Study Design: A prospective cohort study was conducted during 2001-2002 with home health recipients, their primary informal caregivers, and their formal home healthcare coordinators (nurses or therapists). In-person and telephone interviews were performed to gather primary data that were linked to secondary clinical and administrative data. Descriptive and multivariate analyses were performed. Population Studied: Formal home healthcare coordinators (n=186) and informal (n= 121) caregivers of cognitively-intact adults, 50 years of age or older, receiving post-acute home health services following orthopedic or cardiac surgery (n=313). Principal Findings: Most home care recipients were women, racial/ethnic minorities, of low income and limited education. Roughly 1 in 5 care recipients had no informal caregiver. Care recipients with no informal care received a broader and more intensive array of formal home health services than care recipients with informal care, including more social work (30% vs. 15%) and home health aide services (76% vs. 45%), and a greater average volume of nursing visits (22 vs. 13). As compared to care recipients with informal care, in the absence of informal care, care recipients’ length of stay was longer (average 77 days vs. 47 days), the total number of home care visits was greater (36 vs. 23), and hours of home health aide provided were greater (315 vs. 242). In addition, care recipients without informal care were significantly more likely than those with informal care to receive assistance with ADL (82% vs. 68%), entitlements counseling (49% vs. 36%), health behavior management (74% vs. 58%), and care instruction and coordination. Reduced formal services to care recipients with informal care appeared to be offset by family/friends who despite health problems and little/no formal training, provided an average of 37 hours/week of intensive care. Case-mix adjusted regression models revealed significant associations between informal and formal caregiving intensity, where care recipients with no/low informal care were more likely to receive moderate/high formal care in disease management (AOR=2.68, CI=1.10, 6.63), health promotion (AOR=2.31, CI=1.12, 3.61), and functional care (AOR=2.31, CI=1.67, 4.29). Conclusions: Disparities exist in the type, quantity, and content of formal home health services based on informal care support. The appropriateness and comparability of this “substitution effect” between informal and formal home health care warrants further exploration. Implications for Policy, Delivery or Practice: The influence of informal care on home health delivery has both positive and negative implications. On one hand, care recipients with little/no informal support are more vulnerable, thus formal caregivers are addressing an important gap. On the other hand, most informal caregivers lack training in caregiving tasks and experience high caregiving burden, therefore disparities in health care delivery could adversely affect their well-being and presents equity concerns for care recipients. Primary Funding Source: The Langeloth Foundation • Racial and Ethnic Differences in Obtaining Lung Resection for Lung Cancer at Higher Operative Volume Hospitals Charles Neighbors, Ph.D., M.B.A., Michelle Rogers, Ph.D., Scott Novak, Ph.D., Christopher Sciamanna, M.D., Edmund Shenassa, Sc.D., Melissa Clark, Ph.D. Presented by: Charles Neighbors, Ph.D., M.B.A., Assistant Professor (Research), Centers for Behavioral and Preventative Medicine, Brown Medical School, Coro Building, Suite 500, One Hoppin Street, Providence, RI 02903; Tel: 401.793.8130; Fax: (401)793-8059; E-mail: Charles_Neighbors@brown.edu Research Objective: This study examined ethnic and racial differences among lung cancer patients undergoing lung resection at hospitals with varying levels of experience with the procedure. The hypothesis was that African Americans, Latinos, and Other Non-European ethnicities (e.g. Asians, Native Americans) would undergo lung resection in hospitals that performed these procedures infrequently. Study Design: Four years of data (1998-2001) were combined from the National Inpatient Survey (NIS), a nationally representative sample of all US hospitalizations. These data were also merged with hospital level data from the Area Resource File, allowing the computation of both individual and hospital level variables. Total volume of lung resection procedures over four years was computed for each hospital. Two sets of analyses examined whether the above ethnic groups were associated with resections at lower volume hospitals, controlling for demographic and hospital level covariates, including medical comorbidities, secondary malignancies, number of hospitals and ethnic density in the hospitals’ demographic area. Regression analysis on logtransformed hospital volume examined whether there were overall trends in hospitalization of above ethnic groups in lower volume hospitals. Additionally, potential non-linear effects across the distribution of procedure volume were tested by grouping hospitals into quintiles (1st = lowest, 5th = highest) and computing an adjacent category logistic model. Population Studied: A subset of all NIS cases with both lung resection and lung cancer diagnosis were examined, producing a sample size of 22,231. The sample was 87.5% non-Latino White, 6.9% African American, 2.7% Latino, 2.9% other non-European ethnicity, and balanced between males and females. Principal Findings: Regression analysis found that that each of the ethnicities under study was associated with hospitalization in a lower volume hospital as compared to non-Latino Whites. Standardized parameter estimates (betas) were -.09, -.06, and -.06 for African Americans, Latinos, and other non-European ethnicities respectively (all p < .0001). Quintile comparisons in the adjacent category logit model generally supported the finding that ethnicity was associated as hypothesized with procedures conducted in lower volume hospitals. Exceptions to the general finding included nonsignificant differences for Latinos compared to non-Latino Whites in undergoing resection in a 2nd quintile versus 1st quintile hospital or in a 5th versus 4th quintile hospital. Additionally, comparisons between the 4th and 3rd quintiles indicated no significant differences in procedures undergone in lower volume hospitals between non-Latino Whites and African Americans or non-European ethnicities. Conclusions: Despite prior research indicating that greater experience with lung resection leads to more favorable lung cancer treatment outcomes, this study found that African Americans, Latinos, and individuals of non-European ethnicity have this procedure performed in lower volume hospitals compared to non-Latino Whites. Controlling for the number of hospitals in the hospital’s region (a proxy for limited choice) and the ethnic density of the hospital region (a proxy for hospital proximity) did not account for these relationships. Implications for Policy, Delivery or Practice: The study supports the need for more research on the causes of this phenomena as well as targeted policies that increase the likelihood of lung resection procedures in larger volume hospitals for African Americans, Latinos, and individuals of non-European ethnicity. Primary Funding Source: NCI • Perceived Efficacy and its Influence on Follow-up to Abnormal Mammography Debora Paterniti, Ph.D., Linda Stelljes, MA, Sharon Eason, M.P.H., Julianne Souchek, Ph.D., Tracie Collins, M.D., M.P.H., Carol Ashton, M.D., M.P.H. Presented by: Debora Paterniti, Ph.D., Assistant Adjunct Professor, Internal Medicine, University of California, Davis, 2103 Stockton Boulevard, Suite 2224, Sacramento, CA 95817; Tel: 916.734.2367; Fax: 916.734.2349; E-mail: dapaterniti@ucdavis.edu Research Objective: We seek to understand barriers to follow-up (FU) to abnormal mammography for diverse women over 50 years of age. Study Design: Research assistants, trained to use a record abstraction form and to take notes on the process of follow-up and care, reviewed clinic records from January 2000 through December 2001. A nonprobability sample of 37 women matching the population characteristics was invited to participate in a total of four focus group interviews. Guiding questions for focus groups were developed based on conceptual models of self-efficacy (Bandura) and adherence to medical recommendations (Becker & Rosenstock). Data gathered during record review and chart abstraction were analyzed using descriptive statistics. Women’s race/ethnicity and likelihood of follow-up to inconclusive or abnormal mammograms were compared. A multidisciplinary team of investigators inductively developed categories for qualitative interview data that reflected prominent themes related to efficacy and barriers to follow-up on abnormal mammography. Coding categories were developed through an iterative process; a code book was developed, and transcripts were uploaded to the qualitative software program and coding categories assigned to all focus group data. Population Studied: We studied women receiving mammograms at a nonprofit breast clinic in the Houston area. Inclusion criteria were women 50 years of age and over who received an inconclusive or abnormal mammogram requiring follow-up. Principal Findings: Data from patient medical records show white women to be twice as likely to follow-up on abnormal mammography than non-white women (p=.003). Patient reports of family history of breast cancer were not significantly related to FU. Qualitative analysis suggests women’s perspectives on insurance are inversely related to their perceived self-efficacy and intent to FU. Those who reported having no insurance or having problems with insurance were more likely to describe greater self-efficacy and social network support related to FU than those with no perceived financial or insurance barriers. Faith played an important role in the perceptions of efficacy related to FU in African American women and in those women with late FU. Conclusions: Perceived efficacy not only impacted women's reports of intent to follow-up but was influenced by other factors, such as insurance status, social network support, and faith. Women's descriptions of the impact of other factors on perceived efficacy and FU were linked to patient self-reported ethnicity. Perceived efficacy is an important aspect of intention for action and may encode barriers to health-related behaviors, such as FU on inconclusive or abnormal clinical results. Implications for Policy, Delivery or Practice: Untimely follow-up to abnormal mammograms, that which extends three months or longer past identification of an abnormal mammogram, may have serious implications for potential cancer cure and survival rates. Attention to differential rates of follow-up among diverse women might include communication-based interventions that address self-reported barriers to perceived efficacy in FU to clinically inconclusive or abnormal results. Primary Funding Source: AHRQ • Health Care Market Structure & Colorectal Cancer Screening Among High-Risk Asians & Pacific Islanders Ninez Ponce, M.P.P., Ph.D., Soonim Huh, M.P.H., Roshan Bastani, Ph.D. Presented by: Ninez Ponce, M.P.P., Ph.D., Assistant Professor, Health Services, UCLA School of Public Health, 31254 CHS, Los Angeles, CA 90029-1774; Tel: 310.206.4021; Fax: 310.455.9475; E-mail: nponce@ucla.edu Research Objective: To examine the effects of salient health care market characteristics (HMO penetration, competition; percent group/staff model HMOs) on colorectal cancer screening behaviors among Asians and Pacific Islander (AAPI) compared to white adults, ages 40+, with a family history of cancer. Study Design: Random intercept multilevel logit analysis of individuals nested in health care markets defined by metropolitan-statistical area (MSA). Population Studied: First-degree relatives, ages 40-80 recruited through a random sample of colorectal cancer cases from the population-based California Cancer Registry; HMO data from InterStudy Principal Findings: Controlling for individual characterisitcs including income, insurance coverage and percent lifetime in the U.S., even among this high-risk group, a higher percent of staff group model HMOs within an MSA-bound market area lowers the likelihood of AAPIs receipt of a sigmoidoscopy/colonoscopy in the past 5 years. A higher degree of HMO competition was also associated with lower FOBT receipt among AAPIs. Conclusions: Our results are counter to the general intuition that staff and group model HMOs and competition --which leads to more choices, are market factors that promote cancer screening. Thus market conditions that are "favorable" to increasing cancer screening among the general population appear to penalize high-risk AAPIs. Implications for Policy, Delivery or Practice: Policies that promote competition and types of HMO market structure should consider their differential impact on vulnerable groups such as AAPIs, who have lower cancer screening rates than most other groups. Primary Funding Source: NCI • The Link between Socio-Economic Status and Hospitalization Gary Pickens, Ph.D., Paul Presken, M.P.P., Adam Sales, B.A., Paul Presken, BA, MPP Presented by: Paul Presken, M.P.P., VP, Content Development, Solucient, 1800 Sherman Avenue, Evanston, IL 60201; Tel: 847.440.9735; Fax: 847.475.7830; E-mail: ppresken@solucient.com Research Objective: Primary Goal: To design a method of assigning a socio-economic status (SES) score to every community in Arizona, California, and Nevada in order to compare relative community need between hospitals in that region. Secondary Goal: To link the SES scores to the health status and healthcare utilization of communities. Study Design: The following 5 measures and 9 indicators were used to score each and every ZIP code in CA, AZ and NV: INCOME BARRIERS – Percentage of elderly, children and single parent poverty CULTURAL BARRIERS – Percentage non-White/non-Hispanic and percentage with poor English-speaking skills EDUCATIONAL BARRIERS – Percentage without high school diploma INSURANCE BARRIERS - Percentage uninsured and percentage unemployed HOUSING BARRIERS – Percentage renting houses For each of the five indicators, every ZIP code for the entire region was rank ordered (1 to 2089) For each of the five indicators, every ZIP code was assigned a score on a 5-point scale based on the quintile of their rank order (e.g. 1,2,3,4 or 5) For every ZIP code, all five indicators were averaged together for a final score. All five indicators were given equal weight (20% each) in the average. Population Studied: 3 States: California, Arizona, Nevada 2043 Populated ZIP Codes 43,000,000 Population in 2003 4,300,000 Admissions in 2002 Principal Findings: There is a strong correlation (95.5%) between the SES score of a community and the hospitalization rate of a community. Conclusions: In these three states, various demographic variables can be combined to predict socio-economic status of a community. In addition, these variables can also be used as a very good predictor of variation in health status, access and utilization of hospital services. Implications for Policy, Delivery or Practice: Such analysis can be used to identify communities particularly vulnerable to access to care issues so that funding can be properly allocated from the government or providers. Primary Funding Source: Solucient, LLC • Validity of Using Surnames to Define Chinese Ethnicity: A Cross Sectional Survey Hude Quan, M.D. Ph.D., William Ghali, M.D. M.P.H., Stafford Dean, M.A., Peter Faris, Ph.D., Diane Galbraith, B.N., Michelle Graham, M.D. and Merril Knudtson M.D. Presented by: Hude Quan, M.D. Ph.D., assistant professor, Community Health Sciences, University of Calgary, 3330 Hospital Dr., N.W., Calgary, T2N 4N1; Tel: 403.944.8912; Fax: 403.944.8950; E-mail: hquan@ucalgary.ca Research Objective: Ethnic and racial diversity in population health and health care delivery has been increasingly studied. To overcome lack information on the ethnicity of individual patients in secondary databases, researchers have commonly used surnames as an alternative source of information for defining ethnicity. Although surname methodologies are promising, little is know about their validity. In this study we assessed the agreement between self-perceived Chinese ethnicity and ethnicity defined using Chinese surnames. Study Design: We conducted a telephone survey in a randomly selected sample in Calgary, Alberta, Canada in 2003 to collect information on self-reported ethnicity and surname. Chinese ethnicity was assigned using the Chinese surname list developed by Tjam following Cantonese and Mandarin phonological rules. (Can J Public Health 2001;2:138-42). The list included 226 distinctive possible Chinese surnames. We subsequently revised the list by removing surnames that were common in both Chinese and other ethnic groups and adding some Chinese surnames. Chinese ethnicity was then reassigned using the revised surname list. Principal Findings: Of the 2808 people surveyed, 5.4% were self reported as Chinese. This was higher than the 4.8% of people identified as Chinese using Tjam's original surname list and was the same as the 5.4% identified by our revised surname list. Compared with self-reported Chinese ethnicity (reference standard), the original surname list had a sensitivity of 73.0%, positive predictive value (PPV) of 82.2%, specificity of 99.1% and negative predictive value (NPV) of 98.5%. The revised surname list had 92.8% sensitivity, 93.4% PPV, 99.6% specificity and 99.6% NPV. The senstivity of the revised surname list varied by age (89.8% for 18-34 years, 95.1% for 35-64 and 91.7% for 65 or over), by sex (96.8% for male and 90.0% for female) and by marital status (93.3% for married/common law/separated/widowed and 91.5% for never married/divorced). When stratifing by sex and marital status, the sensitivity was 100% for married men, 95.0% for never married men, 89.8% for married women and 90.5% for never married women. Conclusions: The validity of defining Chinese ethnicity using Tjam's surname list is moderate. The revised Chinese surname list has excellent agreement with self-reported ethnicity. Primary Funding Source: Calgary Health Region and Institute of Health Economics, Alberta, Canada • Prehospital Delay in African Americans Presenting with Acute Myocardial Infarction Mark Callahan, M.D., Debra Quinn, M.D. M.P.H., Kawai Oneida, M.P.H., Maryelena Vargas, RN, Rachel Skeete, M.D., Eliot Lazar, M.D., Alvin Mushlin, M.D., Sc.M. Presented by: Debra Quinn, M.D., M.P.H., Assistant Professor, Public Health, Weill Medical College of Cornell University, 411 East 69th Street, New York, NY 10021; Tel: 212.746.3087; Fax: 212.746.8544; E-mail: daq2002@med.cornell.edu Research Objective: This study is designed to evaluate quality of care and predictors of outcomes for patients with acute myocardial infarction, with the goal of understanding predictors of R/E disparities. Study Design: Retrospective cohort of patients admitted to 12 hospitals in the New York metropolitan region. A random sample of patients from each institution was abstracted and multivariate logistic regression was used to analyze predictors of mortality. Population Studied: 673 patients from the 12 study institution were selected based on DRG assignment for acute myocardial infarction. Principal Findings: 36 % of African American (AA) patients presented within 24 hours of onset of chest pain, as compared to 54% of Hispanic-Latino (H-L), 50% of Caucasian (C)(P = 0.02). Once admitted to the hospital, patients from all ethnic groups had similar quality of care, including similar door-toneedle times for thrombolytic therapy, equivalent use of aspirin, beta-blockers, ACE-inhibitors, anti-cholesterol therapy and diagnostic services. However, mortality rates for AA patients were significantly higher (30% AA, 14% H, 18% C)(P <0.001), which persisted after multivariate adjustment for patient demographics, payer status, and co-morbidities. Conclusions: Once admitted to hospitals, AA patients receive similar quality of care for acute myocardial infarction. However, AA patients are more likely to delay presenting to the hospital after onset of symptoms, and suffer a higher mortality rate in-hospital despite similar patterns of treatment. Implications for Policy, Delivery or Practice: Significant delays in presenting to the hospital exist for all ethnic/racial groups, but these delays are worse for AA patients. Delays in presentation may lead to worse outcomes, as many of the cardiovascular treatment options for patients with an AMI are less effective the longer the intervention is delayed. Further research is warranted to understand the causes of the delays, and to identify effective strategies for reducing the excess cardiovascular mortality suffered by AA patients. Primary Funding Source: Institutional • Racial Disparities in the Use of Assistive Devices for Mobility Linda Resnik, Ph.D., PT, Susan Allen, Ph.D. Presented by: Linda Resnik, Ph.D., PT, Postdoctoral Fellow, Center for Gerontology and Health Care Research, Brown University, 2 Stimson Avenue, Providence, RI 02906; Tel: 501.863.9214; E-mail: Linda_Resnik@Brown.edu Research Objective: Use of mobility devices, such as canes, walkers or wheelchairs, are an important strategy for providing assistance with mobility that can supplement or substitute for personal assistance, and enhance safety. Although mobility device use can be an effective resource for managing mobility impairments, little is known about patterns of use in minority populations. Thus, the purpose of this study was to quantify the association between race/ ethnicity and mobility device use in a national sample of adults reporting difficulty walking. Study Design: The study is a secondary analysis of the Adult Disability Follow-Back Survey (NHIS-D Phase II). Race was grouped into three categories; black, Hispanic non-black, and white non-Hispanic. The dependent variable was use of any assistive device for mobility in the past two weeks. Factors hypothesized to be related to assistive device use were examined using chi-square analyses. Logistic regression models were developed adjusting for these predictors of device use. Interactions between race/ethnicity and age were examined using relative excess risk attributable to interaction as advocated by Rothman. Population Studied: The analytic sample consisted of 7336 adults with reported difficulty walking. This figure represents an estimated population of 41,003,809 US residents. Principal Findings: Bivariate analyses revealed a disparity in mobility device use with Hispanics less likely to use any device (OR.79, CI .65-.96 P=.02), and blacks more likely to use any device (OR 1.2, CI 1.0-1.4 P<.000) Controlling for age of respondents eliminated the decreased likelihood of device use for Hispanics, but did not eliminate the increased likelihood of device use among blacks. Logistic regressions controlling for predictors found a positive association between black race and mobility device use (OR 1.6 CI, 1.4-2.0 P=<000), however, the relative excess risk attributable to the interaction of being over 75 years of age and black was a 50% decrease in likelihood of using a device. In addition, the relative excess risk attributable to the interaction of over 75 years of age and Hispanic was an 84% increase in likelihood of using an assistive device. Conclusions: The reduced likelihood of mobility device use among Hispanics was explained by adjusting for the population’s younger age. Overall, blacks were more likely to use devices, but the effect of race varied across categories of age. An interaction between race/ethnicity and oldest age was observed, with the oldest blacks being less likely to use devices than expected and the oldest Hispanics being more likely to use devices than expected. Implications for Policy, Delivery or Practice: Assistive devices for mobility are an important strategy for preventing injury and promoting independence, yet are often underutilized. Underutilization of assistive devices for mobility is a growing problem given the aging of the population. This is a particular concern for the growing population of minority elders who have greater prevalence of disability. More research is needed to understand the reasons for differential rates of assistive device use among minority groups to guide the design of culturally appropriate interventions aimed at promoting device use for people with mobility impairments. • Patterns of Utilization for Asthma Patients in a Rural Hispanic Border Community Mary Rimsza, M.D., William Johnson, Ph.D., Tricia Johnson, Ph.D., Amy Bartels, M.P.H. Presented by: Mary Rimsza, M.D., Adjunct Professor, School of Health Administration & Policy, Arizona State University, Box 2104, Tempe, AZ 85287-2104; Tel: 480.965.1145; Fax: 480.965.4605; E-mail: Mary.Rimsza@asu.edu Research Objective: This study uses micro-data from a unique community health data system to identify patters of health care utilization for Hispanic and non-Hispanic asthma patients in a rural border community. Study Design: We use data from health care providers and health-related organizations in Yuma County, Arizona to create the Yuma County Community Health Data System (CHDS). The Yuma County CHDS merges data from the hospital system, federally qualified community health centers, private pediatric practices, state Medicaid and immunization data, employer-based health insurance and a survey of primarily Hispanic neighborhoods. More than 60% of children ages 0-19 are Hispanic. After identifying patients with asthma we study the treatment received and use a logistic regression model to measure the influence of predictor variables including age, sex, race, geographic distribution and insurance type. Population Studied: Participants include Hispanic and nonHispanic asthmatic children 0 to 19 years of age, living in a semi-rural border county in Arizona in 1999. Principal Findings: 981 children were diagnosed with asthma in 1999 and utilized care in 1999, 2000 and 2001. Seventythree percent of the children are Hispanic. We evaluate and describe the pediatric asthma medical utilization patterns of Hispanic and non-Hispanic children in this border community. Conclusions: Proximity to health care services is an important predictor of service utilization. Furthermore, while lack of insurance coverage increases the likelihood of using the emergency department and inpatient hospital care, it has no effect on the likelihood of using physician services. Implications for Policy, Delivery or Practice: Asthma is a significant cause of morbidity and mortality in children and has been associated with high rates of emergency department utilization. The use of longitudinal data from a community data system provides detailed information for several years on the care provided to children. The CHDS model offers the advantage of following individuals over time and providing extensive information on the type and quantity of health care utilized by the persons included in the data. The results can be used to identify disparities and create strategies for eliminating them. Primary Funding Source: The Flinn Foundation & Arizona State University • Spatial Variations in Access to AIDS Services in Los Angeles County: Implications for Service Availability and Health Outcomes Paul Robinson, Ph.D., Keisha Paxton, Ph.D., Arleen Leibowitz, Ph.D. Presented by: Paul Robinson, Ph.D., Assistant Professor, RCMI, Charles R. Drew University, 5266 Eageldale Avenue, Los Angeles, CA 90041; Tel: 313.868.8069; Fax: 313.631.1495; E-mail: parobins@cdrewu.edu Research Objective: This project explores the relationship between persons living with HIV/AIDS, the geographic distribution of primary and ancillary services in Los Angeles County, California, and post antiretroviral treatment mortality rates(1996-2002). The principal research objectives were 1) to determine how HIV/AIDS service providers are stratified geographically and by type within the study area, 2)how the locations of these services correspond with the residence areas of HIV/AIDS patients. 3) To determine the relationship between distance to HIV/AIDS services and AIDS longevity in Los Angeles County. Study Design: The AIDS Project Los Angeles comprehensive HIV/AIDS services database was geo-coded. Estimated number of Persons Living with AIDS in each Zip Code was calculated. Service availability by type of service was analyzed by Service Planning Area. Distances between each zip codes weighted population centers and primary and ancillary services were calculated. Estimated annual AIDS mortality rates (1988-2002) were calculated for zip codes. Population Studied: Persons living with HIV/AIDS Principal Findings: The location of AIDS service intake points is an important influence upon the longevity and quality of life of PLWA. The Antelope Valley has a shortage of services of all types. South Los Angeles has a shortage of targeted youth services. Geographic distance from a AIDS medical service provider is an important factor in the longevity of PLWA. This relationship is moderated by distance to ancillary service providers. Conclusions: Although the importance of physical distance on utilization of health services is well established, it is often not considered with respect to the relationship it has with health outcomes. Particularly for Persons living with HIV/AIDS, physical distance alone can stand as a barrier to a sound treatment regimen. The strategic placement of ancillary services can serve as a forward linkage to good primary care. Implications for Policy, Delivery or Practice: As HIV/AIDS moves into new population groups, the placement of AIDS services both primary and ancillary, should consider the distance decay relationship. Strategically placed ancillary services, such as transportation services, can counteract the distance decay relationship. Primary Funding Source: NIH/NCRR • Disparity in Use of Highly Active Anti-Retroviral Therapy (HAART) for Medicaid Patients with HIV/AIDS in South Carolina. Kit Simpson, Dr.P.H, Rajesh Sarang, M.D., M.P.H, Rajesh Sarang, M.D., M.P.H, Shayna Padgett, M.S, Jennifer MazyckBrown, Pharm.D., Pamela Mazyck, Pharm.D. Presented by: Rajesh Sarang, M.D., M.P.H, Statistical Data Analyst III, Pharmacy Practice, Medical University of South Carolina, 280 Calhoun Street, Charleston, SC 29425; Tel: 843.792.5535; Fax: 843.792.1712; E-mail: sarangry@musc.edu Research Objective: To assess the disparity of drug prescription and usage of HAART among HIV/AIDS patients of South Carolina using Medicaid Data. Study Design: Retrospective analysis of archival data to determine the factors influencing the prescription and use of Highly Active Anti-Retroviral Therapy(HAART)in the state of South Carolina (SC). A retrospective analysis using multiple logistic regression with HAART as the dependent variable and gender, location, race, school, age, marriage, total cost, total paid, eligible days, total patients per physician, whether a person visits a physician in an outpatient hospital or office, and Miles traveled by the patient to visit his physician as independent variables. Population Studied: All Medicaid patients with a diagnosis code of HIV/AIDS during the years 2000-2001. Principal Findings: People who see their physician in the office have a higher probability of getting HAART as compared to those who visit their doctor at a hospital clinic (p<0.02)CI= 1.061-2.052). Females are less likely to get HAART as compared to males (p=0.01) (CI= 0.463-0.901). Patient age is not significantly associated with HAART use (p=0.07)(CI=0.953-2.440). Patients who receive care from hysicians with many AIDS patients a physician have higher likelyhood getting HAART (p<0.0001) (CI =1.010-1.019). Patients who travel a greater distance as compared to those who visit physician close by have a greater chance of receiving HAART. (p=0.02) (CI=1.062-2.738). The weighted mean rate of HAART use was 40-45% in most of the ACSA’s for the year 2000, this number increased by approximately 5% in the year 2001. Even though the weighted mean use of HAART was around 45% in most of the ACSA’s, 3 out of the 11 areas had mean rates of 30-35%, which was far less as compared to other areas. These areas will be the target areas for programs to increase the usage of HAART. Conclusions: Disparities in the use of HAART were found which are associated with patient gender, the number of AIDS patient in a practice, and whether a patient visits a doctor in an outpatient clinic or in a private office. HAART use is also significantly associated with the place of residence of a patient and the amount of distance he/she travels to see his/her physician. Implications for Policy, Delivery or Practice: Programs must make special efforts to target African American and Female HIV/AIDS patients to assure that these patients understand the potential life saving benefits of HAART. Once a patient is in care, physicians must develop culturally sensitive methods for regular assessment of patients' readiness to initiate HAART. Geographic areas with low use of HAART should be targeted for programs to help support local medical practitioners in HIV-disease management, and referral networks should be strenghtened where needed. Primary Funding Source: AHRQ • Literacy as a Socioeconomic Determinant of Health: Clarifying the Nature of the Relationship in a Nationally Representative Sample Tetine Sentell, Ph.D. Presented by: Tetine Sentell, Ph.D., Postdoctoral Fellow, Psychiatry, USCF, 2727 Mariposa, Suite 100, San Francisco, CA 94110; Tel: 415.437.3075; Fax: 415.437.3020; E-mail: tsentell@itsa.ucsf.edu Research Objective: Existing studies finding a positive relationship between adult literacy and health have typically operationalized literacy as a dichotomous variable, comparing those with inadequate vs. adequate skills. This ignores three important research questions with key implications for disparities research: 1) Is higher literacy associated with better health among those with inadequate skills?; 2) Does the health/literacy relationship end at the threshold of basic skill attainment or continue across a gradient?; and 3) Does the strength of the health/literacy relationship vary between those who have inadequate and adequate literacy? These questions were tested in a nationally representative sample. Study Design: Using 1992 National Adult Literacy Survey, a nationally representative sample of US residents, continuous literacy was measured by a score of 0 (lowest) to 500 on an extensive functional literacy test. Using this score, literacy was also coded dichotomously as inadequate (<225) or adequate (225+) based on published guidelines. Health status was measured by 2 yes-or-no questions: 1) Do you have a condition that keeps you from work? 2) Do you have a longterm health condition? Logistic models using continuous literacy to predict health status were run using separate samples for adults with inadequate and adequate literacy skills. Sociodemographic variables were controlled. Odds ratios (OR) are reported for 50-point literacy score intervals and were used to compare the strength of the health literacy relationship between the two proficiency groups. Population Studied: Blind (243), mentally retarded (54), and respondents under 18 (776) were excluded from analyses, leaving 23,889 individuals. Nineteen percent of the sample (4,537) had inadequate literacy. Principal Findings: For adults with inadequate literacy, continuous literacy was significantly negatively associated with having a work-impairing condition (OR: 0.92; p<.01), but not with a long-term illness (p=.36). For adults with adequate literacy, continuous literacy was significantly negatively associated with having a work-impairing condition (OR: 0.89; p<.01) and a long-term illness (OR: 0.95; p<.01). Conclusions: In a nationally representative sample, literacy did not have a threshold effect, as previous health literacy research has implicitly assumed. Even slightly better literacy has health benefits for adults with both inadequate and adequate reading skills. However, at least for some measures of health status, the marginal benefit for the same increase in literacy skills actually confers greater health advantages for those with adequate skills compared to those with inadequate skills. A fifty point increase in literacy is associated with a 11% less likelihood of having a work-impairing condition among those with adequate literacy and an 8% less likelihood among those with inadequate literacy. The relationship between literacy and health appears to vary by health status measure, with literacy having a stronger association with work-impairing conditions than with long-term illness. Implications for Policy, Delivery or Practice: Low adult literacy has been recently recognized as a key contributor to health disparities. Even a little bit more literacy skill may improve health at all reading proficiency levels indicating that collaborations between adult literacy and health care may reap multiple benefits. Literacy is associated more strongly with certain health conditions suggesting that interventions targeting those areas may be most effective. Primary Funding Source: National Institute of Mental Health • Trends In Health Insurance Coverage among Latinos, 1993-2002 N. Sarita Shah, M.D., Andrea Guerra, B.A., Olveen Carrasquillo, M.D., M.P.H. Presented by: N. Sarita Shah, M.D., Post-doctoral Research Fellow, Medicine, Columbia University College of Physicians & Surgeons, 200 E. 72nd Street, Apartment 30-H, New York, NY 10021; Tel: 212.706.2668; Fax: 212.305.9349; E-mail: ns597@columbia.edu Research Objective: One third of Latinos are uninsured and during the last decade the number of uninsured Latinos has increased by 60%. In contrast, the number of uninsured nonHispanic whites and blacks has either decreased or remained stable, respectively. Given the diversity of the Latino population, we examine trends in the number of uninsured Hispanics by sub-group and immigration status. Study Design: We analyzed data from the Census Bureau’s Current Population Survey (CPS) from 1993 to 2002. All estimates were derived using weights that account for the sample design and non-response (16.2% in 2002). Consistent with conventions for demographic data, differences were significant if the 90 percent confidence interval (CI) for point estimates did not overlap. Population Studied: Prior to 1999 the CPS sample consisted of approximately 160,000 persons. Subsequently the sample was expanded to about 210,000 persons. Other changes in CPS methodology during this 10-year period have included a revision of insurance questions and use of updated population controls based on the 2000 Census data. Based on the four largest sub-groups, Latinos were categorized as Mexican, Puerto Rican, Cuban, Dominican, or other (primarily Central and South Americans). By immigration status, Hispanics were categorized as US-born (born in the United States or foreign-born with at least one American parent), immigrant citizens (foreign-born naturalized citizens) or noncitizen immigrants (foreign-born persons residing in the US who are not US citizens, including undocumented persons). Principal Findings: From 1993-2002, the number of uninsured Dominicans and Cubans did not increase. However, there was a significant increase in the number of uninsured Mexicans 5.7 (CI,5.5-5.9) to 9.5 million (CI,9.2-9.8), Puerto Ricans 480,000 (CI,390-580,000) to 720,000 (CI,640810,000), and other 1.6 (CI,1.4-1.7) to 2.3 million (CI,2.2-2.5). Similarly, the number of uninsured US-born Latinos and immigrant citizen Latinos also increased 3.7 (CI,3.5-3.9) to 5.5 million (CI,5.2-5.7) and 0.50 (CI, 0.40-0.59) to 1.1 million (CI, .096-1.2), respectively. However, these increases were primarily due to population growth as for most groups the percent uninsured did not change e.g. the percent of US-born Hispanics without insurance fluctuated between 22 to 23%. In contrast, both the number and percent of uninsured noncitizen immigrants increased 4.2 (CI, 4.0-4.4) to 6.7 million (CI, 6.6-6.9) and 50.0% (CI,47.6-52.3) to 56.5% (CI,55.0-57.9), respectively. The percentage change was primarily due to reductions in employer-provided coverage. Conclusions: The rise in the number of uninsured Hispanics from 1993 to 2002 was primarily due to population growth and occurred among various Latino sub-groups as well as both US born and immigrant Latinos. However the most dramatic increase was among non-citizen immigrants. Implications for Policy, Delivery or Practice: These findings support the need for additional targeted outreach as well as specific policy initiatives. Primary Funding Source: HRSA • The Role of GIS in Establishing Boundaries for Vulnerable Health Services Areas in Rural America Keith Mueller, Ph.D., Michael Shambaugh-Miller, Ph.D., M.A., B.A., Louis Pol, Ph.D., Julie Stoner, Ph.D., Woodrow Lucas, B.A. Presented by: Michael Shambaugh-Miller, Ph.D., M.A., B.A., Faculty Medical Geographer, Preventive and Societal Medicine, University of Nebraska Medical Center, 984350 Nebraska Medical Center, Omaha, NE 68198-4350; Tel: 402.559.7858; Fax: 402.559.7259; E-mail: mdmiller@unmc.edu Research Objective: Through the use of Geographic Information Systems and Principal Components Analysis, to define those rural communities in which providers are very unlikely to generate sufficient revenue from patient care to sustain their business. That is, we would expect their operating margins to be consistently negative. Study Design: Three conceptual criteria were used to determine vulnerable areas: 1) Population characteristics associated with patient revenue: too few people to support providers, too few users of the service (e.g., racial and ethnic minorities that are less frequent users of health care services); 2) Insufficient payment from clients due to high percentages of low income uninsured households, Medicaid clients, and Medicare beneficiaries; 3) Lower percentage of paying clients who pay above costs: high income households, patients with full coverage through private insurance. A community is vulnerable if its population size and/or composition make it unlikely that a health service provider (e.g., a clinic or a hospital) can operate and realize financial success in that community without public sector support. Moreover, a vulnerable community is one that is not within a reasonable travel time/distance from another community where adequate health services are offered. Vulnerable communities were determined through a two step process. First through population and spatial considerations using a GIS, communities were formed by merging census block groups based around core census places of 3500 to 50,000 persons. These new communities were then limited to total populations of no more than 100,000 persons. The remaining communities were then classified using a technique (principle components analysis) that clustered them according to proportions of the study variables; those communities in the most dissimilar clusters (high positive scores based on proportions low income, unemployed, and minority households) are considered vulnerable. Population Studied: Selected demographic data collected at the Census block group level for 20 U.S. states of the Great Plains region (11 study states along with 9 bordering states). Principal Findings: In delineating vulnerable rural communities in 11 sample states, an initial determination is that those rural areas falling outside of 25 mile buffers around towns/cities of 3,500 or more persons are vulnerable areas. That criterion defines areas in 20 study area states as vulnerable, with sizeable proportions of the region vulnerable by population density. The definition of community as a core town of 3,500 or more and the surrounding 25 miles defined 447 communities in the 20 state region. However, several of those communities contained 100,000 or more persons, which would argue there is sufficient population to sustain health care delivery systems, even with above average proportions of populations deemed to generate less revenue than the cost of care. In addition, it was determined that vulnerability of a community is positively associated with the four community characteristics under investigation, the minority proportion, the below poverty proportion, the proportion 25 and over with less than a high school education, the unemployment proportion, and the proportion of the population aged 65 and older. The vulnerable communities are likely to be those with high principal component scores, or very low principal component scores. It is clear that the increased scores are being driven primarily by the minority proportion and the proportion below poverty. In total, 138 communities were designated as vulnerable places, where health care providers cannot be expected to generate sufficient revenue from paying patients to sustain viable operations. Those communities are in addition to those places where low populations would indicate extreme difficulties in sustaining local health care systems. Conclusions: The approach developed in this project can be used as a guide for public policy by replacing the current myriad of policies by exception: hospitals are paid through prospective except for those; physicians are paid by a fee schedule, except those in shortage areas can earn a bonus; etc. However, replacing one system (albeit a conglomeration of policies) with another would create winners and losers. Recognizing this reality, two adjustments could be made. First, if this or another new approach is adopted, it could be done in phases to permit early testing of its impacts. Second, if a single approach is used, exceptions could be permitted that are consistent with the framework that created the approach. For example, if the geography of an area is such that the 25 mile buffer is meaningless due to impassable mountains or lakes, lines could be redrawn and a remote area declared vulnerable. In another example, if the proportions of elderly and low income households are insufficient to achieve cluster scores making the community vulnerable, but because of patterns of care the proportions of patients actually seen originates disproportionately from those groups, an exception could be made. The technique developed here to assess the implications of place for providing health care services will be useful to three audiences. State government health departments, specifically offices of rural health, can use this approach to identify those places in their states that should be targeted with programs designed to sustain health care providers. These might include loan repayments as financial incentives, technical assistance to providers to help them achieve efficiencies that help survival with lower revenues, incentives to establish regional systems of care, and direct assistance where needed. Federal policy makers can use this approach to identify those places in which providers can qualify for special payment considerations. This technique also identifies places that can be targeted by special federal programs, including placing health care providers committed to locate in under served areas. Finally, health care providers, such as hospital administrators, can use this technique to identify places based on likely revenues, which becomes input into strategic planning. For example, hospitals located in vulnerable communities might approach network arrangements differently than those located in communities with more potential for payment from privately insured patients. Implications for Policy, Delivery or Practice: Implications for Policy, Delivery or Practice: Access to primary health care services in rural areas. Primary Funding Source: Federal Office of Rural Health Policy • Changes in Breastfeeding Patterns among Ethiopian Immigrants to Israel Michal Shani, M.D., Eric Shinwell, M.D. Presented by: Michal Shani, M.D., Family Physician, Department of Family Medicine, Central District, Clalit Health Service, Israel, 3814 N.E. 75th, Suite #2, Seattle, WA 98115; Tel: 206.892.9491; Fax: 206.616.9204; E-mail: shani99@medscape.com Research Objective: To describe the changes in breastfeeding patterns among Ethiopian women following immigration to Israel. Study Design: During the months of February to April 1999 we distributed questionnaires to the mothers in the maternity department in Kaplan Hospital, Rehovot,Israel. The questionnaires included demographic data, questions relating to the desire to breastfeed and questions about previous breastfeeding experience. The women were contacted by phone after 4-6 months and their breastfeeding history was noted. For those women who were still breastfeeding at that time, another phone call was made 12-15 months after delivery. Principal Findings: During the above period there were 733 births in the hospital. Approximately 600 questionnaires were distributed. 515 (85.8%) women responded to the questionnaire. Forty (7.7%) of the women were born in Ethiopia. These women breastfed their child for a longer duration (mean 6.0 months) than the general population (mean 3.9 months, p<0.0004). There was also a decrease in breastfeeding duration between the current (mean 5.6 months) and the previous child (7.9 months, p<0.030). The main reasons for stopping breastfeeding among Ethiopian women were insufficient milk (54.5%), and the child’s refusal to nurse (18.1%). Eighty-five percent of the Ethiopian women did not receive any help concerning breastfeeding outside the maternity hospital. Conclusions: The immigration of Ethiopian Jews to Israel caused a decrease in breastfeeding duration, although it was still longer then the breastfeeding duration of the general population in Israel. The lack of lactation counseling and support may contribute to this trend. The medical authorities in Israel should consider ways to preserve breastfeeding habits among Ethiopian immigrants. Implications for Policy, Delivery or Practice: The medical authorities in Israel should consider ways to preserve breastfeeding habits among Ethiopian immigrants. • Evaluating Accessible and Culturally Competent Hispanic Health Care Windsor Westbrook Sherrill, Ph.D., M.H.A., Rachel Mayo, Ph.D., Linda Crew, M.B.A. Presented by: Windsor Westbrook Sherrill, Ph.D., M.H.A., Assistant Professor, Health Sciences, Clemson University, 528 Edwards Hall, Clemson, SC 29634; Tel: 864.656.0263; Fax: 864-656-6227; E-mail: wsherri@clemson.edu Research Objective: The purpose of the project was to develop a program to address the health care needs of rural, minority, and uninsured/underinsured populations in upstate of SC, particularly Hispanic individuals. Providing culturally appropriate, sensitive, accessible and affordable care is one of the objectives of this HRSA funded program. Study Design: The program brings primary care to the community through (1) mobile health van services and staff with experience in working with the Hispanic popuation, (2) the use of a cultural competence preparatory course for all practitioners, ( 3) the lay health advisor model utilizing members of the Hispanic community as liaisons and outreach workers. Population Studied: Through a three-year grant from HRSA, health services needs of rural, primarily Hispanic patients in the upstate area of SC were assessed and a service program developed. Evaluation was an important component of this study. Principal Findings: There were 900 patient encounters in year one of the project. A majority, 70%, of the patients using program services were uninsured, had no access to regular medical services and lacked up-to-date preventive services such as immunizations and mammograms. Barriers to care for this particular population were accessed as well as disparities in health access, health status and outcomes. Conclusions: For populations particularly difficult to reach in rural areas, several strategies have been developed, implemented and assessed: the "promotora model", mobile health clinic services, and translation and other support services. Improvements in health status among populations have been assessed with particular focus on chronic health problems such as diabetes, hypertension and women's health problems. Implications for Policy, Delivery or Practice: Culturally and linguistically competent primary and preventive health services can improve access and health disparities among medically underserved and minority populations. Improved utilization of health care services and improved health status can be achieved by services which empower individuals and communities to have a role and responsibility in their own health care. The program creating an inclusive partnership with the community is the most effective and sustainable. This unique partnership model as well as evaluation outcomes will be presented. Primary Funding Source: HRSA • Racial Variations in Adjuvant Chemotherapy Regimens for Breast Cancer Melony Sorbero, Ph.D., M.S., M.P.H., Andrew Dick, Ph.D., Jennifer Griggs, M.D., M.P.H. Presented by: Melony Sorbero, Ph.D., M.S., M.P.H., Associate Scientist, RAND Corporation, 201 North Craig Street, Suite 202, Pittsburgh, PA 15213; Tel: 412.683.2300; Fax: 412.683.2800; E-mail: Melony_Sorbero@rand.org Research Objective: Black women have been found to receive lower breast cancer adjuvant chemotherapy dose proportion than white women, but we don’t know whether systematic differences exist in the types of adjuvant chemotherapy regimens received for breast cancer treatment. Anthracyclinecontaining regimens have been shown to have the best efficacy. The purpose of this study is to determine whether black women receiving adjuvant chemotherapy for breast cancer receive the same drug combinations and delivery methods as white women. Study Design: Women with breast cancer were identified using tumor registries at our study sites. Patient and treatment data were collected from oncology medical records, including age, comorbid conditions, tumor characteristics, chemotherapy course and dates of diagnosis and treatment. The six adjuvant chemotherapy regimens were categorized by their delivery method (intravenous vs. oral), and four of the regimens contained an anthracycline. Multinomial logistic regression was used to examine the relationship between patient race and six chemotherapy regimen, controlling for age, comorbidity, tumor characteristics, type of insurance, year of treatment and treatment region. Joint tests of significance were performed to determine the statistical significance of race across regimens. Multivariate logistic regressions were estimated to examine the relationship between race and delivery method, and the relationship between race and receipt of an anthracycline-containing regimen. All analyses included robust standard errors clustering on physician to account for the lack of independence among patients treated by the same medical oncologist. Population Studied: A sample of 745 black and non-Hispanic white women treated with adjuvant chemotherapy for a primary localized or regional breast cancer from 1985-2001 in 11 treatment sites in three regions. Principal Findings: Black women were significantly more likely than white women to receive their chemotherapy intravenously if receiving an anthracycline-containing regimen (p=.02). In bivariate analyses, there was not a significant difference in whether the regimen received contained an anthracycline. Regions varied in their use of regimens. Two regions varied in the use of regimens by race (p<.001) while one (that with the smallest minority population) did not (p=.21). Adjuvant chemotherapy regimen received also varied with nodal status, tumor size, patient age and year of treatment. The use of anthracycline-containing regimens did not vary significantly by region. Blacks in one of the regions were significantly less likely to receive anthracycline-containing regimens than were whites in the region (p<.001). Conclusions: The existence and magnitude of racial differences in the type and quality of adjuvant chemotherapy regimens used in the treatment of breast cancer varied by region. Variations in the types of chemotherapy regimens used in the adjuvant setting may in part account for the poorer breast cancer outcomes experienced by black women. Implications for Policy, Delivery or Practice: Racial variations were larger in areas with greater minority populations. This included a lower use of anthracyclinecontaining regimens for blacks versus whites. We know little about the structural causes for these disparities. More work needs to be done to identify these causes and develop policies to address them. Primary Funding Source: U.S. Army Medical Research and Materiel Command • Rural/Urban and Racial Disparities in Geographic Access to Hospital-Based Perinatal Care in South Carolina John Stewart, M.S., M.P.H., Ana Lopez-DeFede, Ph.D. Presented by: John Stewart, M.S., M.P.H., GIS Manager, Institute for Families in Society, University of South Carolina, 937 Assembly Street, Suite 618, Columbia, SC 29208; Tel: 803.777.5516; Fax: (803) 777-1793; E-mail: jstewart@gwm.sc.edu Research Objective: Identify and map women at risk for poor perinatal outcomes in a South Carolina perinatal care region. Evaluate rural/urban and racial disparities in geographic access to appropriate health services by comparing travel distance to hospital-based perinatal care for at-risk subpopulations. Study Design: Data from the 2000 Census were used to determine the number of African American and White/NonHispanic women at risk for poor perinatal outcomes (women ages 15 to 17 and 35 to 44) in 24,949 rural and urban census blocks comprising the Pee Dee perinatal care region in South Carolina. Using a geographic information system (GIS), area hospitals providing basic and/or specialty perinatal care were geocoded at the street address level. A GIS network tool then was used to determine actual road distance from each populated block centroid (point representing the geographic center of a census block with one or more at-risk women) to the nearest hospital(s) providing basic perinatal care and specialty perinatal services. Population Studied: African American women ages 15 to 17 (N=5,355) and 35 to 44 (N=15,989) and White/Non-Hispanic women ages 15 to 17 (N=6,013) and 35 to 44 (N=26,983) in an eight-county perinatal care region in South Carolina. Principal Findings: On average, rural women live nearly twice as far from hospitals providing basic perinatal care as urban women (ages 15 to 17, 12.4 miles vs. 6.4 miles; ages 35 to 44, 12.3 miles vs. 6.7 miles). Similarly, rural women reside almost two times as far from specialty perinatal care hospitals as urban women (ages 15 to 17, 20.6 miles vs. 11.1 miles; ages 35 to 44, 19.9 miles vs. 10.7 miles). In both rural and urban areas, geographic access to basic perinatal care is similar for African American and White/Non-Hispanic women. On average, however, African American women must travel farther for specialty perinatal care than White/Non-Hispanics (rural: ages 15 to 17, 22.9 miles vs. 18.5 miles; ages 35 to 44, 22.5 miles vs. 18.2 miles; urban: ages 15 to 17, 12.6 miles vs. 9.9 miles; ages 35 to 44, 12.3 miles vs. 9.8 miles). Conclusions: Distance from care may limit access to hospitalbased perinatal services, particularly for rural African American women needing specialty care. GIS technology can be used to evaluate rural/urban and racial disparities in perinatal care accessibility and to locate/allocate services to reduce existing disparities. In addition, a GIS can be used to identify geographically remote at-risk subpopulations, locate community-based perinatal care specialists (e.g., obstetricians, gynecologists) serving remote areas, coordinate neonatal and maternal transportation to and from appropriate perinatal care sites, and target perinatal health education initiatives. Implications for Policy, Delivery or Practice: Enhanced coordination of regional perinatal care to reduce rural/urban and racial disparities in care accessibility and to improve perinatal outcomes for geographically remote at-risk women. Primary Funding Source: SC Department of Health and Human Services • A National Survey of Accessibility of Medical Instrumentation Molly Story, M.S., Jill Winters, Ph.D., R.N., Kris Barnekow, Ph.D., O.T., Brenda Premo, M.B.A., June Isaacson Kailes, M.S.W., Erin Schwier, O.T.D., and Jack Winters, Ph.D. Presented by: Molly Story, M.S., Co-Director, , RERC on Accessible Medical Instrumentation, 3717 Deauville Place, Santa Rosa, CA 95403-0980; Tel: 707.578.6839; Fax: 707.578.9435; E-mail: molly@humanspectrumdesign.com Research Objective: This project is conducting activities to identify the nature of obstacles related to medical instrumentation (and related policies) that prevent people with disabilities from receiving healthcare services. Study Design: A national survey was developed to assess difficulties experienced by people with disabilities as patients using medical instrumentation for healthcare. The project staff employed a range of strategies to recruit a diverse national sample, and preliminary results from the survey are available. A Delphi approach was used to construct the instrument to be distributed in the national survey. The questionnaire asked about experiences respondents have had with fifteen specific categories of medical equipment representing the full range of classifications. The survey was available in a wide variety of formats: as an online form, as a Word form, as a text document, and as a PDF document in either regular or large print that could be printed out and completed by hand. The survey could also be completed over the telephone or in person. Population Studied: To identify obstacles related to medical instrumentation preventing people with disabilities from receiving healthcare services, the questionnaire was disseminated to a diverse array of organizations and individuals throughout the United States. The desired sample for this study needed to contain individuals with disabilities who were diverse in age, abilities, ethnicity, geographic location, and socio-economic status. Principal Findings: As of this writing, only preliminary analyses of the data have been performed. Early results have helped to identify some types of instrumentation that cause difficulties for patients with disabilities when using the healthcare system. For example, of the 93% of respondents with experience with examination tables, 34% had moderate and 33% had extreme difficulty. Eight percent of participants indicated they were impossible to use. Of the 77% with experience using various types of medical chairs, 30% had moderate and 17% had extreme difficulty. Four percent of respondents said chairs were impossible to use. Of the 85% of people with x-ray equipment experience, 32% had moderate and 32% had extreme difficulty. Again, four percent indicated that these machines were impossible to use. More complete survey results will be available for presentation at the Academy Health Annual Research Meeting in June 2004. Conclusions: While the scope of the problem of access to and utilization of healthcare services is vast, one of the major barriers can be identified as the accessibility and usability of medical instrumentation. Unfortunately, the scope of problems resulting from inaccessible equipment has not been documented. To date, there have been few studies focusing on access, utilization, and frequency of use and usability of the medical instrumentation used by and for persons with disabilities. Implications for Policy, Delivery or Practice: Carefully structured national needs assessments are needed in order (a) to improve both access to healthcare services and utilization of these services by individuals with disabilities, and (b) to improve access to healthcare equipment by healthcare providers with disabilities. The activities of the research project described herein will begin to provide this necessary information. Primary Funding Source: NIDRR, U.S. Dept. of Education • Drug Treatment Disparities among African Amerians Carleen Stoskopf, Sc.D., Jong-Deuk Baek, Ph.D., Junho Jeon, M.S. Presented by: Carleen Stoskopf, Sc.D., Professor and Chair, Health Services Policy and Management, University of South Carolina, Arnold School of Public Health, Columbia, SC 29208; Tel: 803.777.4781; Fax: 803.777.1836; E-mail: cstoskopf@sc.edu Research Objective: The objective of this research is to determine if there are significant differences is the drug treament of HIV/AIDS between Whites and other minorities, especially African Americans. Study Design: This study is based on a secondary data analysis using the "HIV Cost and Service Utilization Study" data available from the Health Resources and Services Administration. The use of specific categories of drugs, such as antiretroviral drugs, etc., as well as specific drugs is used as the dependent variable in a series of logistic regressions. Race/ethnicity is the primary independent variable and age, gender, education, employment, income, and insurance status are used as control variables. Because the data is a weighted national sample, SUDDAN was used for the data analysis. Population Studied: This data is based on a national survey of persons who are HIV positive. The sample was collected from a population who had seen at least one medical professional. N = 231,414 (population estimate). Principal Findings: African Americans have a significant risk of not taking antiretroviral drugs (odds ratio = 0.71), anti-CMV (Cytomegalovirus) drugs (odds ratio = 0.54), drugs for treatment of pneumocystis carinii pneumonia and/or protozoal diseases (odds ratio = 0.66), drugs for fungal infections (odds ratio = 0.57), drugs for treating Mycobacterium avium complex (TB/MAC) disease (odds ratio = 0.72), and anit-herpes drugs (odds ratio = 0.57) as compared to Whites. Hispanics are significantly less likely to receive drugs for CMV (odds ratio = 0.30) and TB/MAC (odds ratio = 0.63). Conclusions: African Americans are less likely to receive drug therapies for HIV/AIDS or related illnesses than their White counterparts after controlling for major demographic and social economic status variables such as age, gender, education, employment, income, and insurance status. Other minorities fair better, although Hispanics are less likely to be treated for TB/MAC and CMV. Implications for Policy, Delivery or Practice: African Americans have been found to have different levels and types of treatment for a number of diseases, such as treatment for heart disease (acute and chronic) and various cancers. This data indicates that this pattern is consistent in the treatment of HIV/AIDS. This has serious implications for this vulnerble group since new HIV cases are occurring at a higher rate in minorities. This challenges health care providers and policy makers to develop the means and methods to reach more African Americans with validated treatment regimens. Since the common charactersistics such as demographic and social economic variables do not explain this difference of drug use, it is imperative that further research be conducted into finding the reason(s) African Americans, and to a lesser extent Hispanics, perform so poorly in terms of getting access to treatment or in terms of bridging other barriers such as cultural differences between providers and patients. • Factors Affecting Gender and Racial/Ethnic Differences in the Onset of Depression in Older Adults Joseph Sudano, Jr., Ph.D. Presented by: Joseph Sudano, Jr., Ph.D., Associate Professor, Medicine, Case Western Reserve University, 2500 Metrohealth Drive, Cleveland, OH 44109; Tel: 216.778.1399; Fax: 216.778.3945; E-mail: jsudano@metrohealth.org Research Objective: To (1) determine the independent effect of 8 factors on the onset of depression in older adults; (2) to explain observed racial/ethnic differences in the onset of depression; and (3) to examine whether or not these factors operate differently for women and men. Study Design: Prospective cohort observational study. The data is from the 1994 (wave 2) and 1996 (wave 3) of the Health and Retirement Study (HRS), a nationallyrepresentative sample of U.S. adults age 55-65 as of their 1996 interview. Using self-reports, depression was first defined at each wave using an 8-measure modified CES-D scale, with those respondents scoring 4 or more categorized as depressed. Only respondents categorized as not depressed at wave 2 (1994) were included in the analysis. Independent variables included 1994 baseline information as well as changes in those variables across the study period (2 years). Logistic regression was used to determine the independent effect of socioeconomic status, insurance status, marital status, self-reported overall health, physical limitations, chronic disease, health behaviors and employment in explaining the onset of depression as well as racial/ethnic differences. Stratified analysis examined gender differences in the explanatory factors. Population Studied: 9,824 persons were interviewed in the initial interview in 1992. 8,683 persons responded to both the 1994 and 1996 depression items. A total of 67 persons had incomplete 1994 and 1996 interviews, leaving a total of 6,765 persons were categorized as not depressed as of the 1994 interview and available for analysis in this study. For males, the sample included 2,468 whites, 412 blacks, and 204 Hispanics. For females, 2,836 whites, 593 blacks, and 253 Hispanics. Principal Findings: Incidence of depression between 1994 and 1996 was higher among blacks and Hispanics compared whites, but this relationship held across gender for only Hispanics. Unadjusted odds ratios for onset of depression were 1.47 (95% CI =1.03-2.07) and 2.16 (95% CI=1.37-3.39) for black and Hispanic females, respectively, compared to whites, and 1.39 (95% CI=0.82-2.36) and 2.12 (95% CI=1.40-3.21) for black and Hispanic males, respectively, compared to whites. In the multivariate analysis, the major independent contributors to explaining the onset of depression where lower socio-economic status, loss of insurance, divorce/separation or loss of a spouse, development of a new physical limitation associated with mobility. Marked differences in the independent effect were noted for females compared to males. Most of the effects in the non-stratified analysis seem to have been driven by the effect of these factors on females. Only the marital status changes and the development of new physical difficulties were significant for males. Most of the racial/ethnic differences in onset could be attributed to lower socio-economic status and development of new physical difficulties. Conclusions: Very different explanations for the onset of depression may exist for men and women, in this older population of adults. Socio-economic status and related physical limitations explain the majority of racial/ethnic variations in onset of depression. Implications for Policy, Delivery or Practice: Attention to gender differences in the causes of depression must be emphasized. Social and family stressors as well as the pernicious effects of lower socio-economic status must be recognized and addressed if we are to reduce racial/ethic disparities in mental health. Primary Funding Source: NIA • Relationship between Census-Tract Level Measures of Segregation and Contextual Factors Deleterious to Health Joseph Sudano, Jr., Ph.D., David Litaker, M.D., Ph.D., Natalie Colabianchi, Ph.D. Presented by: Joseph Sudano, Jr., Ph.D., Asst. Professor, Medicine, Case Western Reserve University, 2500 Metrohealth Drive, Cleveland, OH 44109; Tel: 216.778.1399; Fax: 216.778.3945; E-mail: jsudano@metrohealth.org Research Objective: To (1) develop and introduce 2 new measures (or dimensions) of black/white segregation at the census tract level; (2) develop and assess the statistical properties of 3 latent constructs linked to and potentially deleterious to health; (3) describe various levels of segregations across 2 dimensions in terms of economic, physical, and socio-cultural characteristics. Study Design: Descriptive and correlational study using data from the US Census 1990. We developed 2 measures of segregation: (1) a measure of evenness or "S" based on minority population in the census tract relative to the minority population in larger metropolitan area, and (2) a measure of concentration or "C" based the minority density relative to the minority density in the larger metropolitan area. We then conducted factor analysis and determined the alpha statistic (reliability coefficient) for 3 latent "contextual" constructs using census tract level indicators: economic environment (percent above poverty, median family income, percent white collar, percent high school graduates); physical environment (percent home ownership, median housing value, boarded-up houses per 100, median age of housing, where higher levels indicate); and socio-cultural environment (percent femaleheaded household, population density, crowding in housing, percent unemployed). Finally, we categorized the 2 segregation measures into low, medium, and high levels, and assessed the distributional characteristics of the constructs across the levels of segregation. Population Studied: Of the 63,227 census tracts in the US, we first eliminated 20,506 that were not located in a primary statistical metropolitan area (PMSA). Next, we further eliminated an additional 1,295 tracts with missing data on the construct items which left a total of 41,426 census tracts available for this analysis. Principal Findings: Two of the 3 contextual constructs exhibited acceptable reliability: economic environment (alpha = 0.90) and socio-cultural environment (alpha = 0.74). Physical environment (alpha = 0.56) was below the traditional acceptable level of 0.70. All 3 constructs exhibited a positive and linear relationship with both segregation measures: higher levels of unevenness and concentration were associated with worse economic, physical and socio-cultural environments. Conclusions: Among census tracts located in major metropolitan statistical areas, black/white segregation measures of evenness and concentration correlate dramatically with contextual factors potentially adverse to health. Implications for Policy, Delivery or Practice: Public health officials and policy makers should recognize that adverse economic, physical and socio-cultural contextual factors related to segregation are pervasive, and that if these socialstructural factors are not addressed, their "best effort" health initiatives may be undermined. Primary Funding Source: NIA • Differences in Access and Utilization among Hispanics Enrolled in a Community-Based Access Program: Does Level of Acculturation Matter? Erin Taylor, Ph.D., M.P.P., Catherine McLaughlin, Ph.D., Jeffrey Kullgren, M.P.H. Presented by: Erin Taylor, Ph.D., M.P.P., Health Researcher, Mathematica Policy Research, 600 Maryland Avenue, S.W., Suite 550, Washington, DC 20024; Tel: 202.484.5276; Fax: 202.863.1763; E-mail: etaylor@mathematica-mpr.com Research Objective: Although disparities in health care access between Hispanics and non-Hispanics have been well documented in the health services literature, fewer studies have examined how access differs among subgroups of Hispanics. In this study, we investigate whether differences in health care access and utilization exist among Englishspeaking and Spanish-speaking Hispanic enrollees in a community-based health care access program for low-income uninsured adults in Austin, Texas. Study Design: Using self-reported data from a multi-wave telephone survey of enrollees in a health care access program, we present descriptive statistics on access and test whether statistically significant differences exist on these measures both across subgroups of Hispanics and across time. Population Studied: 170 English- and Spanish-speaking Hispanic persons continuously enrolled for 6 months in a health care access program in Austin, Texas who responded to a telephone survey. Upon enrollment into the program, participants were assigned a primary care provider, given an access card to use when seeking medical services, and assigned a sliding fee co-payment schedule for various services. We use the language spoken in the telephone interviews as a proxy for enrollees’ level of acculturation. However, we also examine how access and utilization varies by other acculturation measures, such as enrollees’ nativity and length of residence in the U.S. Principal Findings: At the time of enrollment, a statistically significantly lower rate of Spanish-speaking Hispanics reported having a usual source of care (47 percent), compared to English-speaking Hispanics (63 percent). Among those reporting a usual source, Spanish-speaking Hispanics were more likely to seek care in a safety-net setting, such as a clinic or health center (58 percent versus 35 percent for Englishspeaking Hispanics). Spanish-speaking Hispanics also had lower rates of utilization and preventive care on all measures studied, though some differences were not statistically significant. Moreover, Spanish-speaking Hispanics were significantly more likely never to have had health insurance coverage in the past (78 percent), relative to English-speaking Hispanics (44 percent). At six months after enrollment, several measures of access showed improvement, including the proportion with a usual source of care (statistically significant for both groups); the proportion with unmet prescription drug need (with the decline significant only for English speakers); and the proportion reporting that they were very satisfied with their health care (with a dramatic increase from 47 to 83 percent for Spanish-speaking Hispanics). Conclusions: Results indicate that a larger proportion of Spanish-speaking Hispanic participants in a community-based program studied had experienced difficulties in accessing health care prior to enrollment, relative to English-speaking Hispanics. After being enrolled in an access program for six months, several measures of access improved for both groups. Despite these improvements over time, Spanishspeaking Hispanics still fared worse than their Englishspeaking counterparts on several measures. Implications for Policy, Delivery or Practice: Despite significant improvements in access to care among both English-speaking and Spanish-speaking Hispanics enrolled in a community-based program, differences in access persisted among these two subgroups. With Hispanics now comprising 13 percent of the U.S. population-- the country’s largest minority--health services researchers should make efforts where possible to study differences within subgroups of this growing segment of the population. Primary Funding Source: RWJF • An Evaluation of States’ Capacity to Address Racial and Ethnic Health Disparities: Creating a State Minority Health Report Card Amal Trivedi, M.D., M.P.H., Brian Gibbs, Ph.D., Laurie NsiahJefferson, M.P.H., John Ayanian, M.D., M.P.P., Deborah Prothrow-Stith, M.D. Presented by: Amal Trivedi, M.D., M.P.H., Fellow, Health Care Policy, Harvard Medical School, 180 Longwood Avenue, Boston, MA 02115; Tel: 617.432.3138; E-mail: trivedi@hcp.med.harvard.edu Research Objective: A state minority health report card may provide an important tool to evaluate and promote state policies to reduce health disparities. We analyzed state performance on four measures of minority health: rates of uninsurance for minorities compared to whites, physician diversity, creation of an Office of Minority Health (OMH), and reporting of health data using detailed race/ethnicity categories. Study Design: We used data from the Current Population Survey to determine the relative risk of being uninsured for minorities compared to Whites among non-elderly, lowincome individuals. Using data from the AMA Physician Masterfile and U.S. Census, we calculated the degree to which underrepresented minority physicians (URM) in the state must be increased in order to reflect the state’s underlying demographic population. We contacted all state OMH’s recognized by the federal government to conduct a telephone survey on their funding, staffing, history and activities. We determined the number of racial and ethnic categories states used in reporting all-cause mortality data in their most recent vital statistics publication. Finally we conducted secondary analyses of the data to explore three potential predictors of state performance in minority health - region of the country (East, Midwest, South, and West), per capita government spending, and proportion of minorities within the state. Population Studied: Non-elderly, low-income U.S. residents; U.S. physicians; representatives of state Offices of Minority Health. Principal Findings: Top-quartile states had minimal insurance disparities between minorities and whites; however, minorities who live in bottom-quartile states are 50-100% more likely to be uninsured than Whites. While six states had a proportion of URM physicians that reflected their demographic composition, eighteen states would need to raise their number of URM physicians by a factor of 4.5 to 11 to reach proportional representation. Thirty of fifty states have an office of minority health; however, of these thirty, 6 had no budget and 10 had only one employee. Nearly 50% of states report mortality data using three or fewer racial or ethnic categories, including 30% that report mortality data using a “White-Other”, “Black-White,” or “Black-White-Other” racial breakdown. There was a striking geographic clustering of high and low-performing states with region a significant predictor on all four measures (p<0.05). Percentage of minorities in the state and state fiscal capacity were not significant predictors of performance. Conclusions: States vary tremendously in their capacity to address racial and ethnic health disparities. High and low performing states tend to cluster geographically. Implications for Policy, Delivery or Practice: Future research should be conducted on these and other potential predictors of state variation in minority health policy and connections between state policy and health outcomes for minorities. Primary Funding Source: The California Endowment Primary Funding Source: RWJF • The Relationship between Body Mass Index and Health Services Access for Hispanic Children in a Texas/Mexico Border Population Martha Conkling Tromp, MSPH, Miguel Zuniga, M.D., Ph.D. Presented by: Martha Conkling Tromp, MSPH, Graduate Research Assistant, Policy and Management, School of Rural Public Health, 3000 Briarcrest, Suite 300, Bryan, TX 77802; Tel: 979.458.3031; E-mail: mctromp@srph.tamushsc.edu Research Objective: The use of Body Mass Index, BMI, as a measure of health status is well documented. Among the Hispanic population the increase in obesity and chronic disease is alarming. This study seeks to quantify the relationship between child BMI scores and indicators of health services access. Study Design: The intervention goals of a project taking place in Hidalgo County, Texas are to improve the ability of promotoras, community health workers, to impact health behaviors of Colonia residents and to increase health services access and utilization rates. A preliminary household survey of 646 residents took place from Dec. 2002 to April 2003. Survey respondents were selected randomly through block groups, then households, then residents within households. Interview subjects could be a child, the head of the household, or another adult in the household. Height and weight data were collected during the interview. Population Studied: The children included in the survey totaled 200, from two intervention Colonias and one control Colonia. The 102 females and 98 males ranged in age from 4 to 17 years, with a mean age of 11 years. A BMI and age were available for 117 of the children. Principal Findings: The children’s mean BMI is 24. This is a measure of overweight for children 16 years and up and a measure of obesity in children less than 11 years old. For the girls the BMI range is between 12.2 and 53.1 with a mean of 23.6. The boys have a range of 8.8 to 50.6 with a mean of 25. Body Mass Index is sensitive to age and ethnicity. Children in the 4-8 year age groups have the largest body mass: 71 percent are in the obese range, 11 percent are overweight. Children in the 10-12 year age groups: 41 percent obese and 35 percent overweight. Of the teenagers measured, 69 percent are in the normal weight range. Characteristics of the children with a BMI of 17.5 or more are: 43 percent have 1 or more chronic disease, most live in households earning less than $14,600, and 65 percent of these children do not have health insurance. Conclusions: Children in this population have a high risk of chronic disease as indicated by their BMI scores. Health conditions associated with obesity include diabetes, high blood pressure, high cholesterol, and coronary heart disease, all observed in the adult population of these Colonias. Many of these children have at least one chronic disease and most of them do not have health insurance. Their access to health services are limited by poverty, lack of health insurance and knowledge. Implications for Policy, Delivery or Practice: Initiatives in health care access in Hidalgo County and similar populations should include BMI as a measure to identify those children most at risk. Through policy development this measure can be used by promotoras in prevention efforts in the Colonias and as a catalyst to assist these children and their families to access health services in their communities. • How Do Medicare Beneficiaries’ Assessments of Care Differ by Race and Ethnicity? Jennifer Uhrig, Ph.D., M.H.A., Jeffrey Laufenberg, M.S., Celia Eicheldinger, M.S., Shulamit Bernard, Ph.D. Presented by: Jennifer Uhrig, Ph.D., M.H.A., Health Services Researcher, Health Communication, RTI International, 3040 Cornwallis Road, P.O. Box 12194, Research Triangle Park, NC 27709-2194; Tel: 919.316.3311; Fax: 919.990.8454; E-mail: uhrig@rti.org Research Objective: To examine whether consumer reports and ratings of health care in fee-for-service Medicare vary by race/ethnicity, and to determine whether the consumer reports and ratings change over time. Study Design: We used data from the 2000-2002 National Medicare Fee-for-Service CAHPS surveys. The sample of beneficiaries was drawn from a sampling frame constructed from the CMS Enrollment Data Base. In each of the three years, the frame comprised over 30 million beneficiaries. The number of respondents and response rates for the surveys was 103,551 (64%) in 2000, 117,836 (68%) in 2001, and 122,955 (71%) in 2002, respectively. The combined analysis file contained 344,342 survey respondents. We calculated CAHPS ratings and composites for each racial and ethnic subgroup using the CAHPS 3.4 Survey and Reporting Kit macros. We used two sample tests for differences in proportions for all pairwise comparisons. We used the combined data set and compared all racial categories with white, and Hispanic with Non-Hispanic for each CAHPS rating and composite. We then stratified by year and compared responses within each racial/ethnic group to determine whether trends were present across years. Population Studied: Beneficiaries enrolled in fee-for-service Medicare Principal Findings: Compared with whites, a larger percentage of all minority racial groups reported problems with getting needed care. Asians were more likely than whites to report problems or provide ratings other than a 10 for all measures except Rate Medicare. African-Americans were less likely than whites to report problems or provide ratings other than 10, except for getting needed care. American Indians/Alaska Natives reported worse experiences than did whites for getting needed care, communication and customer service. Hispanics were more likely than non-Hispanics to report problems getting needed care, respect, and care quickly. Reports and ratings were fairly stable among Hispanics, Non-Hispanics, whites, and African-Americans over the 3 years. However, several statistically significant differences emerged between years within racial/ethnic subgroups for some of the measures, and most of the differences indicate downward trends. Conclusions: Our findings show that statistically significant differences in experience and ratings among beneficiaries in FFS Medicare are associated with race and ethnicity. These findings are consistent with those reported in other research. There is often a disconnect between findings from studies that examine disparities in access, utilization and clinical quality versus those that examine patient reports of their experiences and ratings of their care and providers. Attitudes, beliefs, and preferences all impact health-seeking behaviors and likely have an impact on the reports and ratings that individuals provide. It may be that people are using different points of reference when reporting their experiences and providing their ratings. Implications for Policy, Delivery or Practice: It is unclear whether ratings and reports are a direct result of the quality of care received or rather a result of response bias related to cultural differences or different historical frames of reference concentrated within racial/ethnic subgroups. If differences in reports and ratings are not a direct result of the quality of care received, it is not immediately apparent how these measures can be used to monitor quality. Primary Funding Source: CMS • Mapping Inequalities in Access to Health and Health Outcomes in Ontario and the Commonwealth of Virginia Sorina Vlaicu, M.D., M.P.H., Ph.D. Presented by: Sorina Vlaicu, M.D., M.P.H., Ph.D., Assistant Professor, Political Science/Epidemiology and Biostatistics, University of Western Ontario, 30 Augusta Crescent, London, Ontario, N6E2E1; Tel: 519.661.2111 Ext. 85114; E-mail: svlaicu@uwo.ca Research Objective: Improve our understanding of the spatial distribution of various determinants of health. Describe geographical disparities in access to health services and health outcomes in each community and explore how they relate to socio-economic, demographic, political and other determinants of health. Discuss the role that governmental policies play (or could play) in widening or narrowing the gaps between advantaged and disadvantaged groups. Study Design: This research project promotes an innovative look at inequalities in access to health and health outcomes, while looking at the role that governmental policies play in widening (or narrowing) the gap between ‘have’ and ‘havenots.’ The study provides evidence to inform the design of programs, policies and practices by employing a comparative approach. Similar regions from Canada (Province of Ontario) and the United States (Commonwealth of Virginia) are analyzed side-by-side, to isolate the effect of governmental policies (welfare, health, taxation) and national culture on health disparities and approaches used to address them. Health varies with socio-economic status. Recent research has shown that geography matters as well. Where we live not only defines our individual health, but also what we are getting back from the community--support and resources--and even the quantity and quality of health services we have access to. Traditionally focused on differences in income, the research on health disparities has lately embraced a more comprehensive and interdisciplinary approach, by starting to look at all individual and context factors that have a role in creating and maintaining health inequalities in a society. Population Studied: This study defines health as the resultant of biological, physical, socio-economic and cultural characteristics. The research is constructed within a geographical information systems (GIS) rather than classic (linear) framework. GIS allows the geographic linkage of outcome variables (access to health services and health outcomes) with data on population characteristics, such as socio-economic, community and demographic data, census and health surveys with administrative information. By mapping these data, immediate visual information is obtained on spatial variations in health access and outcomes. Principal Findings: Several statistical methods are used to analyze the data, such as descriptive methods (maps) for the spatial distribution of variables, map smoothing techniques (Bayesian smoothing), tests for spatial randomness, and spatial regression. Spatial regression, in particular, provides a valuable tool for statistical inference, because unlike linear regression, it allows for pure spatial correlation to be built into the model. Most analyses on health inequalities have tried to force the same variables—some of which could be spatially, but not linearly correlated—into a regular linear regression model, leading to potentially biased results. Conclusions: By using GIS, this study emphasizes the important role of socio-demographic and economic characteristics in access and health outcomes. Implications for Policy, Delivery or Practice: The comparison between the two countries with a radically different type of health care system (public v. private) also provides decision makers with the information needed to design, implement, and evaluate targeted programs to address health inequalities in their communities. By using small geographic areas as the unit of analysis- zip/postal codes- community involvement in policy development is also encouraged. Primary Funding Source: University internal grant • Hispanic Language and Patient Assessments of Medicare Managed Care Robert Weech-Maldonado, Ph.D., Peter Gutierrez, M.A., Ron Hays, Ph.D. Presented by: Robert Weech-Maldonado, Ph.D., Assistant Professor, Health Policy & Administration, Pennsylvania State University, 116 Henderson Building, University Park, PA 16801; Tel: 814.865.1926; Fax: 8148.63.2905; E-mail: rxw25@psu.edu Research Objective: Hispanics comprise an increasing proportion of the total population. Recent studies using the Medicaid and commercial managed care CAHPS® data show that Hispanics have lower assessments of care than Whites. Furthermore, these studies suggest that language has a stronger effect on assessments of care than Hispanic ethnicity. The present study analyzes the relationship between Hispanics’ primary language (English or Spanish) and assessments of Medicare managed care. Study Design: The data analyzed are from the 2002 CAHPS Medicare Managed Care survey. Data were analyzed using linear regression models. The dependent variables were CAHPS® 2.0 global rating items (personal doctor, specialist, health care, health plan) and multi-item reports of care (getting needed care, timeliness of care, provider communication, staff helpfulness, plan service). The independent variables were race/ethnicity (Hispanic, Whites, African American, Asian, Pacific Islanders, American Indian, White/African American, American Indian/White, Other), survey language (English, Spanish), controlling for gender, age, education, and health status. All regression analyses adjusted standard errors for the clustered nature of the data (using the Huber/White correction). Population Studied: 143,818 adults enrolled in 181 Medicare managed care plans in 2002. Principal Findings: Hispanic English speakers had lower reports of care than Whites for getting needed care (b= -6.18), timeliness of care (b= -6.18), staff helpfulness (b= -2.18), and health plan service (b= -3.18). They also had lower ratings than Whites for specialist (b= -1.92), health care (b= -1.00), and health plan (b= -1.36). However, Hispanic English speakers did not differ from Whites in their reports of provider communication or their ratings for personal doctor. Hispanic Spanish speakers had lower reports of care than Whites for timeliness of care (b= -7.69), provider communication (b= 3.46), and staff helpfulness (b= -4.38). However, they had higher reports of care than Whites for getting needed care (b= 3.97) and plan service (b= 4.39), and higher ratings than Whites for personal doctor (b= 3.97) and health care (b= 2.97). Hispanic Spanish speakers did not differ from Whites in their ratings for specialist and health plan. Conclusions: Primary language affects the experiences with Medicare managed care among Hispanics. Both Hispanic English and Spanish speakers face barriers to care, but the two groups differ in their assessments for various aspects of care. While Hispanic Spanish speakers had lower scores than Whites for provider communication, Hispanic English speakers did not differ from Whites in this assessment of care. On the other hand, while Hispanic English speakers had lower scores than Whites for the health plan-related aspects of care (getting care needed and plan service), Hispanic Spanish speakers had higher scores than Whites for these aspects of care. Similar to previous research with Medicaid managed care CAHPS®, lower reports of care did not translate necessarily into worse ratings of care among Spanish speakers. Implications for Policy, Delivery or Practice: Medicare managed care plans need to address the observed disparities in care among Hispanics as part of their quality improvement efforts. Particular attention should be paid to how primary language affects experiences with provider communication. Primary Funding Source: NIA • Racial/Ethnic and Language Differences in Patient Assessments of Hospital Care Robert Weech-Maldonado, Ph.D., Azza Abu Dagga, MHA, Ron Hays, Ph.D. preferences. The independent variables are race/ethnicity (White, Hispanic, African American, American Indian, Chinese, Vietnamese, Filipino, Other Asian/Pacific Islander, Multiracial, Other Race), survey language (English, Spanish, and Chinese), and primary language spoken at home (English, Spanish, Chinese, Tagalog, Vietnamese, Other), controlling for service type, health insurance, gender, age, education, and health status. All regression analyses adjusted standard errors for weighting (using the linearization approach) and for the clustered nature of the data (using the Huber/White correction). Population Studied: 25,584 adult patients that received medical or surgical care in 179 participating hospitals, representing approximately 48% of hospitals in California. Principal Findings: Racial/ethnic and linguistic minorities reported more problems with hospital care compared to White English speakers, particularly in the areas of coordination of care, emotional support, information and education, and respect for patient preferences. Asian subgroups reported more problems with care compared to other racial/ethnic groups, and among Asians, non-English speakers encountered more problems with their care. This was particularly the case for Vietnamese speakers who reported more problems than Whites for respect for patient preferences (b= 19.11), emotional support (b= 13.10), coordination of care (b= 9.74), and information and education (b= 8.22). Conclusions: This study suggests that racial/ethnic minorities and non-English speakers face barriers to hospital care, even after controlling for health insurance status. Race/ethnicity and language have independent positive associations with reported problems with hospital care. However, language has a stronger positive effect on reported problems, especially among Asians. Implications for Policy, Delivery or Practice: Hospitals should address the observed racial/ethnic and language disparities in care as part of their quality improvement efforts. Staff’s training in cultural competence and use of interpreter services hold promise as particular mechanisms that may help reduce the observed disparities in hospital care. Primary Funding Source: AHRQ Presented by: Robert Weech-Maldonado, Ph.D., Assistant Professor, Health Policy & Administration, Pennsylvania State University, 116 Henderson Building, University Park, PA 16801; Tel: 814.865.1926; Fax: 814.863.2905; E-mail: rxw25@psu.edu Research Objective: Previous studies have shown differences in hospital treatment based on race/ethnicity. However, relatively few studies have examined racial/ethnic differences in patient experiences with inpatient hospital care. This study analyzes whether patient assessments of hospital care vary by race/ethnicity and primary language. Study Design: The data analyzed are from the 2002 Patients’ Evaluation of Performance in California (PEP-C). Data were collected by mail and surveys were administered in English, Spanish, and Chinese. The average response rate for all hospitals was 50%. Data were analyzed using linear regression models. The dependent variables are 7 dimensions of hospital care: coordination of care, continuity and transition, emotional support, information and education, involvement of family and friends, physical comfort, and respect for patient • Racial/Ethnic Differences in Assessments of Managed Care: Medicaid versus Commercial Insurance Status Robert Weech-Maldonado, Ph.D., Marc Elliott, Ph.D., Adetokunbo Oluwole, M.S., Ron Hays, Ph.D. Presented by: Robert Weech-Maldonado, Ph.D., Assistant Professor, Health Policy & Administration, Pennsylvania State University, 116 Henderson Building, University Park, PA 16801; Tel: 814.865.1926; Fax: 814.863.2905; E-mail: rxw25@psu.edu Research Objective: The study of racial/ethnic differences in consumer assessments of managed care plans is important given the high level of managed care penetration in both the public and private health care markets. Recent studies using the CAHPS® data show that racial/ethnic minorities have worse reports of care than Whites in managed care. This study assesses the effect of insurance status (commercial versus Medicaid) on the observed racial/ethnic differences in patient assessments of care. Study Design: The data analyzed are from the National Committee on Quality Assurance (NCQA) Quality Compass 2001. The CAHPS® data were collected by telephone and mail. The average response rate for all plans was 43%. Data were analyzed using linear regression models. The dependent variables were CAHPS® 2.0 global rating items (personal doctor, specialist, health care, health plan) and multi-item reports of care (getting needed care, timeliness of care, provider communication, staff helpfulness, plan service). The independent variables were interactions of race/ethnicity (White, Hispanic, African American, Asian, Pacific Islander, American Indian, White/American Indian, White/African American, White/Asian, and Other Multiracial) and insurance status (Medicaid and commercial), controlling for gender, age, education, and health status. All regression analyses adjusted standard errors for weighting (using the linearization approach) and for the clustered nature of the data (using the Huber/White correction). Population Studied: 229,790 adults enrolled in 368 commercial managed care plans and 31,622 adults enrolled in 94 Medicaid managed care plans in 2000. Principal Findings: Asians in Medicaid plans reported worse experiences with care than their counterparts in commercial plans for getting needed care, timeliness of care, provider communication, and staff helpfulness. In addition, Asians in Medicaid had lower ratings than their commercial counterparts for personal doctor and health care. Hispanics in Medicaid plans had lower scores than their commercial counterparts for getting needed care. Furthermore, the observed disparity in reports and ratings of care for Asians and Hispanics in Medicaid managed care was greater than the disparity observed between Whites in Medicaid and commercial plans. On the other hand, African Americans and Hispanics in Medicaid managed care had higher ratings than their commercial counterparts for personal doctor, specialist, health care, and health plan. Similarly, American Indians and Pacific Islanders in Medicaid had higher ratings than their commercial counterparts for personal doctor and health plan. Conclusions: Race/ethnicity determines patient experiences with managed care. While most racial/ethnic minority groups in Medicaid managed care had similar or better experiences than their counterparts in commercial plans, Asians in Medicaid reported lower patient assessments of care than their commercial counterparts for most dimensions of care. Furthermore, the disparities observed in Asian experiences with care were greater than those observed for whites based on insurance status. Implications for Policy, Delivery or Practice: The observed greater disparity in patient experiences for Asians in Medicaid managed care plans suggests that Medicaid managed care may be ill prepared to face the cultural and linguistic challenges of a growing Asian population. Policymakers should provide incentives to Medicaid managed care plans with the goal of reducing the observed racial/ethnic disparities in care. Primary Funding Source: AHRQ • Finding from the Racial and Ethnic Adult Disparities in Immunization Initiative (READII) 2003 Survey Carla Winston, M.A., Ph.D., Pascale Wortley, M.D., M.P.H. Presented by: Carla Winston, M.A., Ph.D., Epidemiologist, Health Services Research and Evaluation Branch, National Immunization Program / CDC, 1600 Clifton Road, N.E., MS E- 52, Atlanta, GA 30333; Tel: 404.639.6248; Fax: 404.639.8614; E-mail: ctw3@cdc.gov Research Objective: Influenza vaccination is recommended for all people age 65 and over, yet racial/ethnic disparities in coverage persist. We investigated influenza vaccination knowledge, attitudes, and practices among African American, Hispanic, and Caucasian seniors as part of the baseline survey conducted to evaluate the Racial and Ethnic Adult Disparities in Immunization Initiative (READII). Study Design: Using stratified random sampling, we surveyed Medicare beneficiaries in the five READII demonstration sites (Chicago, IL, Rochester, NY, San Antonio, TX, Milwaukee, WI, and 19 counties of the Mississippi delta). From February to April 2003, we conducted a telephone survey using computer assisted interviewing. Population Studied: Seniors were sampled from the Medicare enrollment database according to zip code of residence in demonstration project areas. We oversampled by race/ethnicity to ensure sufficient numbers of completed interviews with African American and Hispanic seniors. Sampling weights reflected the inverse of the probability that a respondent was selected, adjusted for non-response. Data were analyzed using SUDAAN software to account for the complex sampling scheme. Principal Findings: Response rate to the survey was 61%. Of 4633 Medicare beneficiaries surveyed, 22% of African Americans, 15% of Hispanics, and 9% of Caucasians had never received a flu shot. Among those who had never received a flu shot, Caucasians were more likely (65%) than African American (46%) or Hispanic (28%) participants to state they would definitely not get vaccinated in the coming year. Ninety-five percent (95%) of Caucasian seniors knew the flu shot is recommended for people over age 65, compared to 92% of Hispanics and 88% of African Americans. Overall, 55% of respondents reported that a health care provider recommended influenza vaccination during fall or winter 2002; there was no significant difference in provider recommendation by race. Seniors who reported a provider recommendation were more likely to be vaccinated than seniors who did not report a provider recommendation (84% vs. 56%, P <0.0001). Among those who reported provider recommendation, 88% of Caucasians were vaccinated in 2002, compared to 80% of Hispanics and 66% of African Americans. Among those who did not report a provider recommendation, 61% of Caucasians, 50% of Hispanics and 33% of African Americans were vaccinated. Seniors who believed they had previously gotten sick from vaccination were less likely to be currently vaccinated, with African Americans being more likely than Caucasian or Hispanic respondents to report that they had previously gotten sick from influenza vaccination. Conclusions: Provider recommendation for influenza vaccination did not differ by race in our sample and patients who reported a provider recommendation were more likely to be vaccinated than those who did not. However, African American and Hispanic patients were less likely to be vaccinated despite provider recommendation. Implications for Policy, Delivery or Practice: Reasons for vaccination refusal need to be evaluated so that health provider messages regarding vaccination may be tailored to specific patient concerns in order to improve immunization outcomes. Primary Funding Source: CDC, Department of Health and Human Services • Doing More For Some: The Lives Lost by Prioritizing Efficacy Over Equity in Health Care Steven Woolf, M.D., M.P.H., Robert Johnson, Ph.D. Presented by: Steven Woolf, M.D., M.P.H., Professor, Departments of Family Practice, Preventive Medicine and Community Health, Virginia Commonwealth University, 3712 Charles Stewart Drive, Fairfax, VA 22033; Tel: 703.391.2020 Ext. 141; E-mail: swoolf@vcu.edu Research Objective: The outcomes of health care can be improved by making treatments more efficacious and by bridging gaps in the delivery of those treatments to eligible patients (improving equity). For example, lives can be saved—independent of making improvements in drug therapy—by optimizing the degree to which eligible patients receive drug therapy. Lives can also be saved by developing more efficacious drugs, an enterprise that attracts $32 billion annually from the pharmaceutical industry. We sought to determine how much society benefits from each endeavor to determine whether the nation’s predominant investment in the latter is of net benefit to the population. Study Design: Assume that an established drug therapy achieves a given relative risk reduction (RRR) in a health outcome (e.g., mortality) but is delivered to only a fraction of the eligible population. We can demonstrate that developing a more efficacious drug is more beneficial than improving access only if the new RRR exceeds the existing RRR divided by the percent of the population exposed to treatment. We applied this principle in two examples: (a) developing clopidogrel and ticlopidine as an alternative to aspirin for the prevention of stroke, which is received by 58% of the eligible population; and (b) developing newer-generation statins as an alternative to older agents, which are prescribed to 33% of patients with coronary artery disease. Population Studied: Hypothetical population cohorts with a history of (a) transient ischemic attacks or strokes or (b) coronary artery disease. Principal Findings: Developing an antiplatelet alternative to aspirin is more beneficial than improving access to aspirin only if the newer agent can lower stroke incidence by at least 40%—a proportional improvement over aspirin of 74%—but clopidogrel and ticlopidine are only 10-12% more effective than aspirin. Developing a more efficacious statin is more beneficial than improving access to statin therapy only if the newer agents can reduce 5-year coronary artery disease mortality by at least 72%, three times the potency of older agents such as pravastatin and simvastatin. Although relevant mortality data are lacking, we found that rosuvastatin, among the most impressive of the newer statins, is only 26% more effective than pravastatin and 12-18% more effective than simvastatin in lowering LDL cholesterol. We can demonstrate that the lives saved by the incremental superiority of rosuvastatin over pravastatin are only one seventh the number of lives that might be saved by refining care processes such as placing reminders on charts about the need for lipid-lowering therapy. Conclusions: Fewer strokes and cardiac deaths might occur if society invested more in improving access to aspirin and statin therapy than in developing newer antiplatelet and statin alternatives. Implications for Policy, Delivery or Practice: Despite recommendations in major reports (e.g., Crossing the Quality Chasm) about the urgent need to redesign systems of care to improve the delivery of effective health care, the nation continues to divert most of its research resources toward enhancing the “technology” of care. We conclude that lives are put at stake by this disproportion in national priorities. • Social Support and Breast Cancer Survivorship: Disparities across Ethnic Groups Grace Yoo, Ph.D., M.P.H., Caryn Aviv, Ph.D., Ellen Levine, Ph.D., M.P.H. Presented by: Grace Yoo, Ph.D., M.P.H., Associate Professor, Asian American Studies, San Francisco State University, 1600 Holloway, San Francisco, CA 94131; Tel: 415.338.3891; Fax: 415.338.1739; E-mail: gracey@sfsu.edu Research Objective: The investigators are particularly interested in reducing the health disparities that exist in minority communities and in understanding how social supports impacts quality of life among breast cancer survivors from diverse populations. Social support has been documented to help in adjustment and coping with breast cancer and to impact positively on the survivor's health. For breast cancer survivors, access to a supportive environment can prevent long-term psychological difficulties and positively impact general well-being Study Design: Twenty women (5 from each ethnic group) were recruited for in-depth, face to face, qualitative interviews. Population Studied: The participants selected for this study were African American, Asian American, Latina, and white women residing in the San Francisco Bay Area who had been diagnosed with invasive breast cancer (Stage 1 and Stage 2) and had completed treatment. Potential participants were recruited through the UCSF Comprehensive Cancer Center Clinic and local Bay Area non-profit breast cancer community advocacy organizations. Principal Findings: The results of these interviews include the discussion of definition and types of social support used at diagnosis, during treatment, after treatment; psycho-social impact of breast cancer; reactions of family members; and ways of coping. We are also asking the women if they want to give advice to other women diagnosed with breast cancer as well as give recommendations to the community for programs to support breast cancer patients and survivors. Implications for Policy, Delivery or Practice: The findings will contribute to the understanding within the broader health, social services and policy communities of how to best meet the needs of breast cancer survivors from diverse populations. Primary Funding Source: NCI • Hospital Debt Collection Impact on Profitability and Access to Healthcare Mustafa Zeedan Younis, Dr.PH., M.A., M.B.A. Presented by: Mustafa Zeedan Younis, Dr.PH., M.A., M.B.A., Assistant Professor of Health Economic & Finance, Healthcare Administration, Jackson State University, 350 W. Woodrow Wilson Avenue, Jackson, MS 39213; Tel: 504.488.9628; Fax: 504.488.9628; E-mail: younis68@hotmail.com Research Objective: This study examines changes and conditions in hospital financial liquidity and debt collection over a five-year period (1996-2000). Variations in the characteristics of hospital ownership classification are analyzed by regression models to identify differences in cash inflow and financial liquidity. Study Design: Two comparative groups of For- Profits, (F-P) and non-profits (N-P) and are the database for analysis of information that compares all variables by geographic region (e.g. return on assets, uncompensated care, occupancy rate, alos, etc.). Population Studied: 5000 hospitals from the Medicare Cost Report (MCR) minimum data sets. Principal Findings: F-P hospitals were more effective in collecting their debt than their N-P counterparts. This efficiency in collection did add to the F-P hospitals profit margins and financial performance in general. However, these results must be taken with grain of salt, because most N-P hospitals tend to be located in the inner cities and serve a large number of indigent population. Therefore, one may conclude that N-P hospitals' strategy is to provide uncompensated care to its community rather than lacking the effective tools to manage their account receivables. Conclusions: Non-Profit and public hospitals play a major role in supporting healthcare safety net in United States. Implications for Policy, Delivery or Practice: The finding of the study are important to all type of hospital ownership to improve conditions of debt management impacting of profit margin, preserving growth and assuring strength in their financial performance. • Eliminating Health Disparities among Low Income Pregnant Women by Identifying Psychosocial Factors as Predictors of Adverse Outcomes of Pregnancy Rachel Zachariah, R.N., M.S., DNSc Presented by: Rachel Zachariah, R.N., M.S., DNSc, Associate Professor, Bouvé College of Health Science, School of Nursing, Norteastern University, 360 Huntington Avenue, 207H Robinson Hall, Boston, MA 02115; Tel: 617.373.2985; Fax: 617.373.8675; E-mail: r.zachariah@neu.edu Research Objective: The purpose of this research was to examine: (1) the relative strength of attachments with mother/surrogate and husband (partner), other forms of social support, life stress, and anxiety as predictors of lowincome women’s psychological well-being; (2) the impact of these modifiable psychosocial variables on pregnancy outcomes of low-income women. Study Design: Attachments, social support, life stress, anxiety, and psychological well-being of women from obstetric clinic were measured using self-report questionnaires administered between 14 and 22 weeks, and 32 and 42 weeks of pregnancy. The hospital records of the subjects were reviewed to determine pregnancy, labor, delivery, and newborn complications. Data analysis included descriptive statistics, correlational analysis, multiple regression, paired t-tests, and discriminant analyses. Population Studied: One hundred and eleven pregnant women from obstetric clinics, 18 through 35 years of age, Medicaid eligible, between 14 and 22 weeks of pregnancy, without preexisting medical conditions, and fluent in English. Principal Findings: Discriminate analysis was performed to assess the relative contribution of prenatal attachment, trait anxiety, psychological well-being, emotional support, bad life events and the interaction of bad life events with emotional support at Time 1 (early pregnancy) to predict newborn and pregnancy complications. These Time 1 measures significantly classified the Newborn complications in this study (Wilks’ Lambda=.792 Chi-square=17.09 df=7 p=.017). The most important discriminating factors were negative life events and the interaction of emotional support with negative life events. These Time 1 measures also significantly classified the complications of pregnancy in this study (Wilks’ Lambda=.816 Chi-square=14.77 df=7 p=.039). The most important discriminating factors were state anxiety and total functional social supports. Conclusions: The findings of the study support the notion of the presence of positive psychological well-being for those women with stable family relationships, lower anxiety, life stress, and strong social support. The most important factors that discriminated women with complications of pregnancy and complications of the new born were anxiety, social support negative life events and emotional support in interaction with negative life events. Implications for Policy, Delivery or Practice: Identification of modifiable psychosocial risk factors as predictors of adverse outcomes of pregnancy is a major step in reducing negative outcomes of pregnancy for low-income women. Health care policies need to be developed to facilitate augmentation of social support and reduction of life stress and anxiety for lowincome women in order to reduce complications of pregnancy and the new born. Considering the fact that 84% of the subjects were African Americans, public policy should specifically target this population for major interventions during early pregnancy. New ways need to be addressed to generate innovative health promotion strategies to strengthen close attachment relationships and support systems for low-income women during pregnancy. The findings need to be tested with larger sample of low-income pregnant women of different ethnic backgrounds; however, the identification of significant predictors of negative outcomes of pregnancy for the socially high risk low-income pregnant women in this study provides important information for the development of future healthcare policies and effective interventions. Primary Funding Source: National Institutes of Health, AREA Research Grant Invited Papers People with Disabilities: Do They Have the Same Access? Chair: Susan Palsbo, Ph.D. Tuesday, June 8 • 11:15 a.m.-12:45 p.m. • Panelists: Mari-Lynn Drainoni, Boston University; Holly Hollingsworth, Washington University, St. Louis; Trudy Mallison, Northwestern University (no abstracts provided)