Consumer Driven Health Plans: Early evidence of take-up, cost and
advertisement

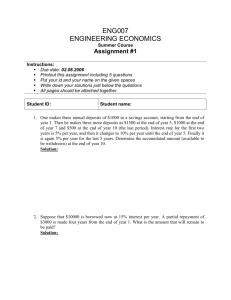
Consumer Driven Health Plans: Early evidence of take-up, cost and utilization and HSA policy implications. Stephen T Parente, Roger Feldman, Jon B Christianson Sponsored by the Robert Wood Johnson Foundation’s Health Care Financing & Organization Initiative (HCFO) February, 2005 Presentation Overview Employer-based Analysis Overview Policy Questions National CDHP Take-up Cost & Utilization Comparisons Over Time National HSA Simulation Policy Implications 1 Employer-based Analysis Overview Analysis started in 2002 with six employers Combined population drawn from 50 states Total covered lives represented: ~250,000 Collect primarily employer HR data and insurance claims data for all plans. New HCFO grant will create a study panel with six total years of CDHP experience 2001-2006. Policy Questions Do CDHPs (in the form of HRAs) have national appeal? What are the longer-run cost & use consequences of CDHPs? Where do they save money? Where are they more expensive? What is the impact on utilization of key services? Do HSAs have potential national appeal? Are HSAs a viable approach to addressing the problem of the uninsured? General Caveat: We are just approaching the half-way point of our research. 2 Nearly National Appeal: States where the study employers’ 1st year CDHP take-up was >5% Take-up >5% 0.1 - 5% 0% Take-up Summary from the Study Employers All states have take-up above 5% with the exception of New York, New England States, Indiana, California and Arizona. Differences may by driven by: Dominance of managed care in CA, AZ Insurer/provider choices in Northeast Not enough data from only six employers Grand experiment in 2005: FEHBP 3 What is the impact of CDHPs on cost & use? Study Design: Reported in 2004, August, Health Services Research. Look at CDHP/PPO/POS cohorts within one large employer for employees over time to see ‘longer run’ impact of CDHP in 2001 & 2002. Control for several factors to ADJUST cost & use estimates: Health status/illness burden/health shocks (cancer, catastrophic accident) Income Family size and dependents Age, gender What was the ADJUSTED impact on provider and patient payment? 2000 Mean 2001 Mean 2002 Mean CDHP Cohort N=531 Total Expenditure Employer Expenditure Employee Expenditure $ 4,396.22 $ 4,005.28 $ 416.51 $ 6,154.36 $ 5,903.61 $ 634.38 $ 8,149.26 $ 7,807.39 $ 792.01 POS Cohort N=1,551 Total Expenditure Employer Expenditure Employee Expenditure $ 5,284.53 $ 4,895.75 $ 394.70 $ 6,773.62 $ 6,227.81 $ 549.32 $ 7,197.50 $ 6,428.83 $ 702.49 PPO Cohort N=1,554 Total Expenditure Employer Expenditure Employee Expenditure $ 5,228.42 $ 4,688.28 $ 511.84 $ 7,050.59 $ 6,349.99 $ 657.16 $ 8,377.78 $ 7,330.94 $ 881.47 Health Plan Cohorts One employer’s results reported in: ST Parente, R Feldman, JB Christianson. Evaluation of the Effect of a Consumer Driven Health Plan on Medical Care Expenditures and Utilization, Health Services Research, Vol. 39, No. 4, Part II, pp. 1189-1209, August 2004. NOTE: These are results from a restricted continuously enrolled sample of 50% to 60% of the total employee population and are not a reflection of the plans’ full PMPM expenditures. Also note: 1) Patient expenditures from the Personal Care Account (PCA) are included in the employer payment category. 2) Consumer payment reflects deductibles, copayments, and coinsurance expenses. 4 What was the ADJUSTED impact on provider & patient payment by different services? Health Plan Cohorts Year 2000 Year 2001 Mean a Mean Year 2002 Mean CDHP Cohort N=531 Hospital Expenditure Physician Expenditure Pharmacy Expenditure $ $ $ 1,369.97 2,093.70 935.29 $ 1,999.25 $ 2,935.84 $ 1,103.72 $ 3,468.53 $ 3,510.83 $ 1,341.78 POS Cohort N=1,551 Hospital Expenditure Physician Expenditure Pharmacy Expenditure $ $ $ 1,842.80 2,381.08 1,107.64 $ 1,796.37 $ 2,959.90 $ 1,498.54 $ 1,956.83 $ 3,088.22 $ 1,640.25 PPO Cohort N=1,554 Hospital Expenditure Physician Expenditure Pharmacy Expenditure $ $ $ 1,779.06 2,245.22 1,007.95 $ 2,049.76 $ 2,834.32 $ 1,484.91 $ 2,367.17 $ 3,294.47 $ 1,789.26 One employer’s results reported in: ST Parente, R Feldman, JB Christianson. Evaluation of the Effect of a Consumer Driven Health Plan on Medical Care Expenditures and Utilization, Health Services Research, Vol. 39, No. 4, Part II, pp. 1189-1209, August 2004. NOTE: These are results from a restricted continuously enrolled sample of 50% to 60% of the total employee population and are not a reflection of the plans’ full PMPM expenditures. Was ADJUSTED service use different for CDHPs? Health Plan Cohorts 2000 Mean 2001 Mean 2002 Mean CDHP Cohort N=531 Hospital Admission Rate Physician Visits Prescriptions Filled 0.05 5.74 18.89 0.10 7.49 22.23 0.16 7.15 25.25 POS Cohort N=1,551 Hospital Admission Rate Physician Visits Prescriptions Filled 0.07 6.75 22.23 0.06 7.56 22.59 0.09 7.29 30.89 PPO Cohort N=1,554 Hospital Admission Rate Physician Visits Prescriptions Filled 0.07 5.78 20.63 0.07 6.54 23.79 0.11 6.95 24.50 One employer’s results reported in: ST Parente, R Feldman, JB Christianson. Evaluation of the Effect of a Consumer Driven Health Plan on Medical Care Expenditures and Utilization, Health Services Research, Vol. 39, No. 4, Part II, pp. 1189-1209, August 2004. NOTE: These are results from a restricted continuously enrolled sample of 50% to 60% of the total employee population and are not a reflection of the plans’ full admissions and prescription drug experience. 5 Results Summary CDHP plan did not have the lowest cost and utilization across all plans. CDHP best (lowest) cost result was for pharmacy. CDHP worse (highest) cost result was for hospital admissions – partially explained by pent-up demand for elective procedures & provider pricing differences across years. Utilization results have no dramatic differences across plan types for pharmacy and physician services. Obvious access to care problem not apparent. CDHP hospital admissions dramatically higher by 2nd year. Using HRA Results to Explore HSA Policy Questions What is the expected take-up rate of HSAs in the individual market? What is the likely impact of the Administration’s proposed HSA subsidies? Take-up rate of HSAs with subsidies Reduction in the number of uninsured Cost of the subsidy What is the impact of other possible subsidy designs? 6 Analysis Design Data Sources Model Estimation MEPS CDHPs eHealthinsurance Estimate plan offerings using insurance data Merge employer data Estimate hedonic premium regression Estimate plan choice regression Assign plan choices to full MEPS sample Choice set Assignment/ Use parameter estimates Prediction to predict plan choice Define HSA plan design & premium probabilities for MEPS Policy Simulation Calibrate take-up rates Simulate impact of proposed policies Status Quo* Impact of MMA 2003 Preliminary Results Plan Choice INDIVIDUAL MARKET EMPLOYER INSURANCE OFFERED MARKET Status Quo Population % Status Quo Project Pop. HSA-Full Price PPO_High $$ PPO_Low $$ PPO_Medium $$ Uninsured 16% 23% 1% 6% 54% 9,877,798 14,344,204 819,464 3,880,982 34,313,001 HMO HRA HSA-Shared Prem HSA-Full Price PPO_High $$ PPO_Low $$ PPO_Medium $$ Turned Down 30% 2% 1% 1% 7% 2% 43% 14% 25,564,398 1,757,424 507,307 597,724 6,194,696 1,598,877 36,252,356 12,246,802 NOTE: Population is 18-64, non public insurance * Status Quo population is defined as 2005 population facing no tax subsidies. 7 Diminishing Subsidy Returns 16,000,000 14,005,598 Previously Uninsured 14,000,000 Sim #2 12,000,000 Sim #3 10,841,110 10,000,000 8,000,000 6,000,000 Sim #1 4,191,441 4,000,000 2,000,000 0 0 $0 $10,000,0 $20,000,0 $30,000,0 $40,000,0 $50,000,0 $60,000,0 $70,000,0 $80,000,0 00,000 00,000 00,000 00,000 00,000 00,000 00,000 00,000 Subsidy Cost HSA Simulation Implications Without any subsidies, the 2003 MMA HSAs could have a take-up of ~10 million. Hypothetical tax subsidies for HSAs could increase coverage among the uninsured from 4 to 14 million. Offering a free premium HSA to the non-working population covered by public programs reduces the uninsured, but less efficiently than income targeted subsidies. 8 Summary For study employers, almost all states had some CDHP take-up – many with 5% or more take-up in the first year offered. Cost results are mixed. Lower costs initially – but rapid rise in expenditures, adjusting for case-mix and demographics. Utilization results are not extraordinarily different in pharmacy and physician services, but significantly higher for admissions. HSA take-up, based on HRA experience and actual 2005 HSA premiums, could be quite substantial. Administration proposals to use HSAs as a mechanism to substantially reduce the number of uninsured may be viable depending on the level of subsidy provided. All future results will be VERY dependent on benefit design: premiums, account/deductible gap, coinsurance. 9