Do Patients of Racial/Ethnic Minority and Lower SES Use Depression Care
advertisement
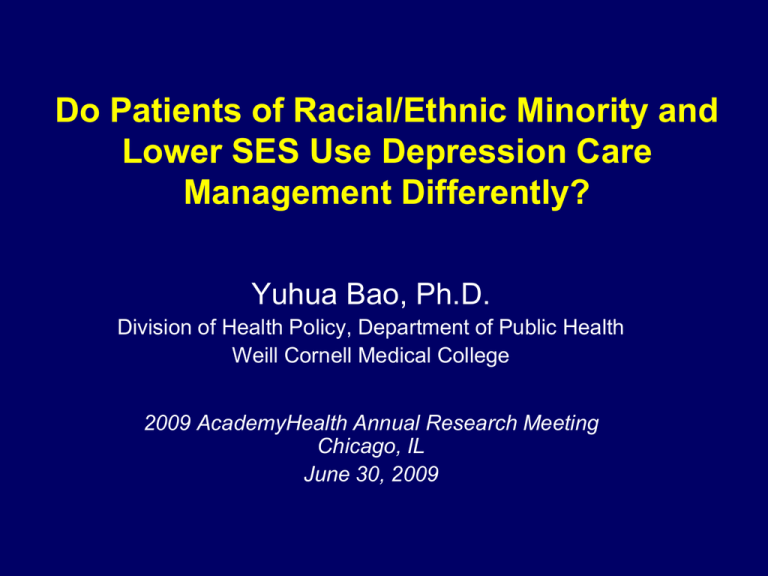
Do Patients of Racial/Ethnic Minority and Lower SES Use Depression Care Management Differently? Yuhua Bao, Ph.D. Division of Health Policy, Department of Public Health Weill Cornell Medical College 2009 AcademyHealth Annual Research Meeting Chicago, IL June 30, 2009 Acknowledgement The following people provided helpful discussion and guidance (in alphabetical order) Martha L. Bruce, Ph.D. Julie M. Donohue, Ph.D. Edward P. Post, M.D., Ph.D. Thomas R. Ten Have, Ph.D. I thank the PROSPECT team for granting me access to the PROSPECT data, and participants at the Weill Cornell Health Policy/Outcomes and Geriatric Psychiatry research-in-progress seminars, for helpful comments. Funding from the Pfizer Scholars Grant in Health Policy supported my time in managing the PROSPECT intervention data. 2 Collaborative Depression Care Management (DCM) Model • A team of clinicians – Depression care manager – Primary care physician (PCP) – Consulting psychiatrist • Care manager – Works with PCP and patient to establish a treatment plan – Follows up with patient to • Assess depression symptoms • Monitor medication effectiveness and side effects • Promote medication adherence – Revise treatment plan and/or consult with psychiatrist • Over 30 RCTs provided strong evidence for efficacy of the model • Offers potential to compensate for poor selfmanagement and ineffective physician-patient communication 3 Racial/Ethnic and Socioeconomic Disparities in Depression Care • Previous studies found persistent disparities in – Access to depression care – Level of guideline-concordant, appropriate care • Underlying mechanisms are likely multi-fold – Health care systems level – Patient population level – Care encounter level • Health literacy / understanding of treatment strategies • Self-management and treatment compliance • Physician bias/stereotype 4 Racial/Ethnic and Socioeconomic Disparities in Depression Care • Previous studies found persistent disparities in – Access to depression care in specialty and non-specialty settings – Level of guideline-concordant, appropriate care • Underlying mechanisms are likely multi-fold – Health care systems level – Patient population level – Care encounter level • Health literacy / understanding of treatment strategies • Self-management and treatment compliance • Physician bias/stereotype Can collaborative DCM help? 5 Research Questions of Interest Research Question 1 Do patients of racial/ethnic minority and lower SES use collaborative DCM differently? Research Question 2 Does DCM help these patients more in improving treatment processes such as antidepressant medication? Research Question 3 Does DCM help patients of racial/ethnic minority and lower SES more in improving their depression treatment outcomes? 6 Research Questions of Interest Research Question 1 Do patients of racial/ethnic minority and lower SES use collaborative DCM differently? Research Question 2 Does DCM help patients of racial/ethnic minority and lower SES more in improving antidepressant medication? Research Question 3 Does DCM help patients of racial/ethnic minority and lower SES more in improving their depression treatment outcomes? 7 The PROSPECT Study • A multi-site, clinic randomized controlled trial of DCM – Older depressed primary care patients (60+) – 20 primary care practices at 3 different sites – No special accommodations for minority patients • All patients need be able to communicate in English • Research funding supported DCM for up to 2 years – Thus taking out the “access to care” factor • N=599 with major or clinically significant minor depression at baseline 8 Racial/Ethnic and Education Breakdown of Prospect Sample Race/ Ethnicity Education N % White 419 70% African American 163 Other 67% 27% NonHispanic white 16 3% Minority 33% Hispanic 26 4% Less than high school 155 26% High school 204 34% Some college 238 40% 9 Data and Measures • The Intervention Checklist (ITCK) Data – ITCK forms filled out periodically by care managers for each patient – Documented • # of care manager contacts with patient, PCP, and family members • Care manager time spent one each type of activities – – – – – Patient assessment Medication management (effectiveness and side effects) Care coordination Administrative tasks Other (including patient and family education) – All measures aggregated to 3-month intervals • PROSPECT baseline research interview – Baseline depression diagnosis and severity – Social and demographic data 10 Analytical Approaches • Descriptive analysis of DCM use by patient race/ethnicity and education – Ever used DCM – Care manager contacts and time • Negative binomial regressions of care manager contacts and time during each quarter of the first year – As a function of: • minority, education, quarter of the year • Minority x quarter, education x quarter – Control for patient demographics, baseline depressive symptoms, Charlson comorbidity score, and study site indicators – Robust standard errors – Adjusted Incident Rate Ratios (IRRs) between groups e.g. IRR(minority/white)=2: minority patients use twice as much DCM as whites during a given time interval 11 Baseline Depression by Patient Race/Ethnicity and Education Minority NonHispanic White Less Than High School High School Some College 17.9 18.0 19.1 18.0 17.1 % Major depression 68.7% 65.2% 68.4% 70.1% 61.3% % With suicidal ideation 22.6% 26.4% 27.1% 24.5% 24.4% HDRS score HDRS: Hamilton Depression Rating Scale 12 Ever Used DCM 100 90 88.6 88.5 < high school high school 91.6 80 % 70 60 50 40 30 20 some college 13 Care Manager Contacts and Time An example Number of Contacts w/ Patient By Education Num ber of Contacts w / Patient By Race/Ethnicity 12.0 12.0 < High school Minority 10.0 10.0 8.0 8.0 NonHispanic w hite 6.0 4.0 High school 6.0 4.0 Som e college 2.0 2.0 0 3 6 Months 9 12 0 3 6 9 12 Months 14 Adjusted Minority/White Differences in DCM Use Adjusted Incident Rate Ratios (IRRs) 0-3 mo. 3-6 mo. 6-9 mo. 9-12 mo. Patient 1.2 [1.0, 1.4] 1.2 [0.9, 1.6] 0.9 [0.6, 1.2] 0.7 [0.5, 1.0] PCP 1.0 [0.8, 1.2] 0.9 [0.6, 1.4] 0.8 [0.5, 1.2] 0.6 [0.4, 1.1] Family Members 1.5 [0.8, 3.0] 1.0 [0.5, 2.2] 1.0 [0.5, 2.0] 1.0 [0.4, 2.3] Patient Assessment 1.0 [0.8, 1.2] 0.9 [0.7, 1.3] 0.7 [0.5, 0.9] 0.6 [0.4, 0.9] Medication Management 1.3 [1.0, 1.7] 1.3 [0.9, 2.0] 0.8 [0.5, 1.1] 0.6 [0.4, 1.0] Care Coordination 0.7 [0.5, 1.1] 0.8 [0.5, 1.5] 0.3 [0.2, 0.7] 0.7 [0.4, 1.4] Contacts Time Results based on negative binomial models with robust standard errors with clusters specified at the patient level. Ninety-five percent confidence intervals of IRRs are shown in square brackets. 15 Adjusted Less Than High School/Some College Differences in DCM Use Adjusted Incident Rate Ratios (IRRs) 0-3 mo. 3-6 mo. 6-9 mo. 9-12 mo. Patient 1.1 [0.9, 1.3] 1.1 [0.8, 1.5] 1.0 [0.7, 1.5] 1.0 [0.7, 1.4] PCP 1.0 [0.8, 1.3] 1.2 [0.7, 1.8] 1.3 [0.8, 2.2] 1.4 [0.7, 2.6] Family Members 1.8 [0.8, 3.9] 4.7 [2.0, 11.4] 2.4 [1.0, 5.5] 5.1 [1.8, 14.4] Patient Assessment 1.0 [0.8, 1.2] 1.2 [0.9, 1.6] 1.0 [0.8, 1.4] 1.1 [0.8, 1.7] Medication Management 0.9 [0.7, 1.1] 1.1 [0.8, 1.7] 1.1 [0.7, 1.6] 1.1 [0.7, 1.7] Care Coordination 1.1 [0.7, 1.6] 1.5 [0.8, 2.8] 1.7 [0.8, 3.7] 1.0 [0.5, 2.2] Contacts Time Results based on negative binomial models with robust standard errors with clusters specified at the patient level.16 Ninety-five percent confidence intervals of IRRs are shown in square brackets. Adjusted High School/Some College Differences in DCM Use Adjusted Incident Rate Ratios (IRRs) 0-3 mo. 3-6 mo. 6-9 mo. 9-12 mo. Patient 1.0 [0.9, 1.2] 1.0 [0.7, 1.3] 1.1 [0.8, 1.5] 1.3 [0.8, 2.0] PCP 0.9 [0.7, 1.2] 1.0 [0.6, 1.5] 1.2 [0.7, 2.0] 2.1 [1.1, 4.3] Family Members 1.3 [0.6, 2.5] 1.3 [0.5, 3.4] 1.0 [0.4, 2.9] 2.1 [0.7, 6.5] Patient Assessment 1.0 [0.8, 1.2] 1.0 [0.7, 1.3] 1.1 [0.8, 1.5] 1.1 [0.7, 1.6] Medication Management 1.0 [0.7, 1.3] 1.2 [0.8, 1.7] 1.2 [0.9, 1.7] 1.4 [0.9, 2.2] Care Coordination 0.8 [0.5, 1.1] 1.3 [0.7, 2.4] 1.4 [0.7, 2.7] 2.0 [0.9, 4.3] Contacts Time Results based on negative binomial models with robust standard errors with clusters specified at the patient level.17 Ninety-five percent confidence intervals of IRRs are shown in square brackets. Study Limitations • DCM contact and time not recorded for each care manager contact, calling into question – Accuracy of recorded DCM use – Consistency between study sites • Strategies to mitigate data limitation – Grouping DCM use by time intervals – Controlling for study site fixed effects • Group differences reflect relative use as long as recording pattern is consistent within sites 18 Summary of Findings & Implications • Racial/ethnic differences: – Minority patients had comparable or slightly higher use of DCM in the first 6 months – Over time, DCM use declined much more rapidly among minorities • Educational differences: – DCM use comparable between educational groups throughout the first year, with one exception • Much more intensive care manager contacts with family members of patients with the lowest education • Implications – Collaborative DCM effective in engaging all patient groups in treatment – Cultural differences associated with race/ethnicity remain a barrier to engaging minority patients in longer-term depression treatment – Engaging family members seemed necessary and important for the less educated 19