Transition of Care Program: Connecting the Dots
advertisement
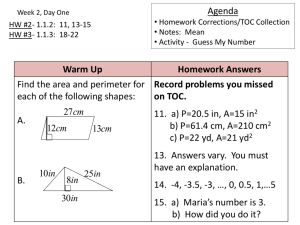
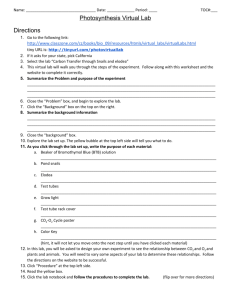
Transition of Care Program: Connecting the Dots Transition of Care Program: Connecting the Dots June 26, 2010 David Kelley, M.D. Chief Medical Officer Pennsylvania Department of Public Welfare Office of Medical Assistance Programs Bureau of Fee-For-Service Programs c-dakelley@state.pa.us Transition of Care Program: Connecting the Dots Key Facts and Timeline • September-October 2009 Initiated and completed program planning and design, including identification of preferred pilot site ERIE WARREN McKEAN SUSQUEHANNA BRADFORD TIOGA POTTER WAYNE CRAWFORD FOREST • November–December 2009 Initial meetings with Williamsport Regional Medical Center WYOMING ELK VENANGO CAMERON CLINTON LUZERNE COLUMBIA JEFFERSON CLARION LAWRENCE MONROE MONTOUR CLEARFIELD BUTLER UNION CENTRE CARBON ARMSTRONG SNYDER NORTHUMBERLAND NORTHAMPTON BEAVER INDIANA MIFFLIN JUNIATA CAMBRIA SCHUYLKILL BLAIR LEHIGH BERKS PERRY WESTMORELAND DAUPHIN BUCKS LEBANON HUNTINGDON MONTGOMERY WASHINGTON CUMBERLAND LANCASTER SOMERSET GREENE – Hired and trained nurse manager – Completed arrangements with hospital PIKE LYCOMING MERCER ALLEGHENY • January-March 2010 LACKAWANNA SULLIVAN FAYETTE CHESTER BEDFORD FULTON PHILADELPHIA YORK FRANKLIN ADAMS DELAWARE ACCESS Plus and Voluntary Managed Care ACCESS Plus only Health Choices Region • March 29, 2010 Launched pilot program 2 Transition of Care Program: Connecting the Dots Why Transition of Care (ToC)? • Patients transitioning from one setting of care to another are at risk of poorer outcomes due to: –Miscommunication between multiple providers, patients, family and caregivers –Medication changes –Lack of understanding of discharge instructions • Dedicated resources focused on the immediate transition period have demonstrated improved patient outcomes –Coleman Care Transitions Intervention –Naylor Transitional Care Model –Boston Medical Center Re-engineered Discharge Project 3 Transition of Care Program: Connecting the Dots ToC Program Goal and Focus Manage patient transitions from acute care through community-based care to improve quality of care and, ultimately, the patient’s experience and health status, thereby reducing days in post-acute care, hospital readmissions and emergency department visits. 1 – 6 weeks post‐discharge 4 Transition of Care Program: Connecting the Dots ToC Program Scope and Role • Population – ACCESS Plus (Enhanced Primary Care Case Management program) enrollees admitted to Williamsport Regional Medical Center – Excludes maternity and newborns (other programs serve these patients) • Transition of Care Manager Role – Improve coordination among key stakeholders prior to, during, and immediately after transitions from one care setting to another – Key stakeholders include: • Patient/family/caregivers • Primary care physician and other treating physicians • Hospital and post-acute care facilities • ACCESS Plus disease management • Pharmacy services (internal and external) • Intense medical case management unit (IMCM) • Medical assistance transportation program (STEP) 5 Transition of Care Program: Connecting the Dots Process Overview End NO Admission notification via daily census report Meets program eligibility criteria? Discharge to PCP Refer to IMCM or Disease Management (if appropriate) YES Evaluate medical record and condition Will patient benefit from ToC program? Conduct post‐ discharge home visit(s) and phone calls Follow patient in hospital and other post‐ acute setting Meet with patient* and describe ToC program YES Agreement to participate? NO End * Patient may mean patient or family/caregiver 6 Transition of Care Program: Connecting the Dots Benefits of ToC Program • Medical Assistance Program and Consumers – Fill unmet need(s) for ACCESS Plus consumers – Focus on improving quality of care and health outcomes – Strengthen partnership between the Department and the Hospital • Hospital – Reduce readmissions – Single point of contact for hospitalized consumers – Onsite Medical Assistance resource 7 Transition of Care Program: Connecting the Dots ToC Program Measurement • Efficiency/Cost/Utilization – Hospital Readmission Rates – Emergency Room Visits – Post Acute Facility Days/ Services – Expected vs Actual Spending – PMPM Rates – Post-acute Service Utilization • Program Utilization – Program Volume – Opt Out Rate • Quality – Consumer Satisfaction Survey – Medication Reconciliation – Adverse Events – Mortality 8 Transition of Care Program: Connecting the Dots Results to Date • ToC Program went live Monday 3/29/10 – Through 6/4/10 (10 weeks of operation), ToC Manager has: – Screened 49 consumers – Offered ToC services to 46 consumers – Enrolled 46 consumers – Discharged 21 consumers • All enrolled consumers have received post-discharge follow up, including health education/wellness promotion, diet, medications, reminders about follow up appointments, etc. • Nine consumers received counseling and/or assistance regarding smoking cessation (e.g., Chantix, nicotine replacement) 9 Transition of Care Program: Connecting the Dots Results to Date (continued) Percentage of Enrollees by Type of Assistance Other healthcare services Supplies and equipment Assistance with medication Diagnostic testing Assistance with PCP Transportation assistance Social/non‐health assistance 0% 5% 10% 15% 20% 25% 30% 35% 40% n = 33 ToC enrolled consumers 10 Transition of Care Program: Connecting the Dots Results to Date (continued) • Sample vignettes include: – Diabetic with high blood pressure was instructed at discharge to check blood sugars twice a day, but not given prescription for glucometer. ToC Manager obtained glucometer from Diabetes Educator, took it to him and instructed him on proper use. Also followed him to make sure he kept all his doctor appointments, went to the lab for his blood work, and had transportation there. He had a cold and was taking an OTC cold medicine that was affecting his blood sugars and blood pressure. ToC Manager instructed him on recommended cold medications. – Consumer admitted with CHF exacerbation was discharged with Altace, a medication not on formulary and pharmacy did not fill it or call the doctor. When ToC Manager called the day after discharge she had no heart medication. ToC Manager called the pharmacy to get a 5 day supply of Altace, then contacted the physician who ordered a comparable (formulary) medication. 11 Transition of Care Program: Connecting the Dots Results to Date (continued) • Sample vignettes include: – Consumer with liver failure was discharged and informed that he needed to see a liver specialist at a nearby larger medical center. Consumer’s father handles his affairs, and the father kept waiting for the specialist to call him. The consumer needed immediate medical care, so ToC Manager instructed them to go to the ER at the medical center. Consumer’s father was told at the medical center that if treatment was not provided that day, the consumer may have died. – Diabetic with cardiac complications was discharged with a list of medications from the hospital that was different from his previous regimen. When ToC Manager called him and reviewed medications, he was doubling up on some medications that were prescribed with different doses and was taking the new dose along with the old dose. He also required encouragement to follow up with his PCP. ToC Manager also reviewed low cholesterol, low sodium, diabetic diet. 12 Transition of Care Program: Connecting the Dots Results to Date (continued) • Sample vignettes include: – Consumer was obese individual admitted for total knee replacement and discharged with home PT. ToC Manager coordinated with physician and home health agency to have PT and blood work at home until she was able to get out of her house safely. After 3 days, home health agency did not start therapy, so ToC Manager contacted agency and they initiated services that evening. Consumer also needed raised toilet seat and bars for the bathroom which ToC Manager assisted with. – Consumer admitted with pneumonia and severe COPD with malnutrition. He needed dental care which was affecting his eating. ToC Manager set up dental appointment. He also had several doctors to follow up with and did not know the address or phone number of one physician. ToC Manager obtained physician’s contact information for the family, and also addressed many questions about medications. 13 Transition of Care Program: Connecting the Dots Results to Date (continued) • Sample vignettes include: – Consumer admitted with respiratory failure and needed new BiPAP at home. ToC Manager coordinated with the physician and DME company about which equipment would be best because she now required BiPAP during the day. Consumer also wanted a living will, which ToC Manager assisted with completing, made copies for her and dropped one off at her physician’s office. Consumer would benefit from having a power scooter, so ToC Manager obtained prescription and coordinated with DME vendor. Also set her up for STEP transportation and assisted in obtaining a bedside commode and shower chair. – Consumer has new diagnosis of lupus and requires frequent monitoring of bleeding times. She sees a cardiologist at a nearby medical center and they can do finger sticks there, but the local lab could only do venipuncture. ToC manager worked with the Coumadin clinic to obtain home finger stick equipment that she will enable consumer to check her own PT/INR and call in results to cardiologist, saving both time and energy. 14 Transition of Care Program: Connecting the Dots Key Program Design Considerations • Selection of hospital partner – Sufficient patient census to support activity of one ToC Manager (Williamsport has approximately 500 non-obstetric or newborn discharges annually) – “Solo” provider for service area – 90+ percent of consumers live within 30 miles of hospital – Interested/excited about program potential • Selection of ToC Manager – Previous discharge planning and/or home care experience (case management experience preferred) – Excellent communication and problem-solving skills – Ability to work autonomously – Knowledgeable about local area and resources • Allow sufficient time for discussions and preparations with hospital 15 Transition of Care Program: Connecting the Dots Questions and Answers 16