Reforming Health Care Delivery Through Payment Change and
advertisement

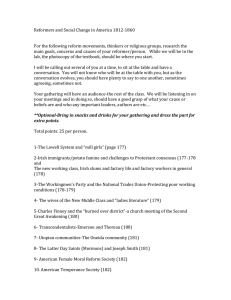
Reforming Health Care Delivery Through Payment Change and Transparency: Innovations in Minnesota and Massachusetts Anne K. Gauthier Kristin Sims-Kastelein Academy Health Annual Conference State Health Policy Research Interest Group June 26, 2010 This project is supported by The Commonwealth Fund. 1 Overview & Objectives Project Methodology Minnesota’s Legislation Findings: Progress to date and implementation challenges Massachusetts’s Legislation and Major Recommendations Findings: Current status and implementation challenges Key Lessons from Each State Concluding Analysis: Cross Cutting Themes Study Design & Project Methodology Extensive document review of the two states’ initiatives Legislation, key workgroup reports, news articles, literature review 34 semi-structured telephone interviews with high level state officials and private sector executives Interview lasted roughly 60 minutes Recorded, transcribed, and analyzed to identify key themes, issues, and lessons Separate case studies written; analysis of crosscutting themes Minnesota’s Landmark Legislation, 2008: Price and Quality Transparency Statewide Measures and All-Payer Database What it is: Standardized set of quality measures for health care providers across the state. Collection and use of all-payer encounter data and contracted prices Provider Peer Grouping What it is: A method of for comparing health care providers based on a combination of risk-adjusted cost and quality. Transparent ranking of providers based on a combination of risk-adjusted cost and quality Minnesota’s Landmark Legislation, 2008: Delivery and Payment Redesign Baskets of Care What it is: A collection of services, paid separately under fee-for-service, but combined by a provider in delivery of a full diagnostic or treatment procedure. Uniform definitions and quality measurements for 7 baskets Quality Incentive Payments What it is: A statewide system of quality-based incentive payment to health care providers. Initial focus on diabetes, vascular care, depression, AMI, heart attack, pneumonia care Health Care Homes What it is: A primary care approach where providers, families, and patients work in partnership to improve health outcomes and quality of life. Voluntary certification. Certification tied to incentive payment for coordinated care. 5 Minnesota Findings: Standardized Quality Measures and All-Payer Database Progress to date n tio c olle C ta Da Sept. 2009: Uniform definitions and measure have been developed Registration of medical groups underway January 2010: providers began submitting data on the measures July 2010: data on the measures will publically reported So ftw are Implementation Challenges 100% physician participation Lack of enforcement mechanism Technical issues in exactly what is reported and how Analysis Minnesota Findings: Provider Peer Grouping Progress to Date July 2009: Collection of third-party administrators and health plans encounter data June 2010: Data distributed to providers Implementation Challenges Technical details How do you score high cost/ high quality versus low cost/low quality? How do you weigh process measures versus outcome measures? Program design How should like organizations be grouped? How is location being taken into account? Impact on access Are rural providers to be unfairly penalized? Minnesota Findings: Baskets of Care Progress to Date Dec. 2009 MDH finalized Baskets Jan 2010: Providers can offer baskets. Price cannot vary by payer. Implementation Challenges Definitions – balance breadth with simplicity Operational – payment, combining different systems, and more Voluntary – will they be used? 7 (+ 1) baskets of care Total Knee Replacement Low Back Pain Obstetric Care Preventative Care (Adults & Children) Diabetes and Pre-Diabetes Asthma Minnesota Findings: Quality Incentive Based Payments Progress to Date July 2009: Rules for implementation January 2010: Health plans use standard quality measures. Providers submit measures electronically July 2010: First public quality reports published. Public programs use quality incentive payment system Implementation Challenges Risk adjustment Applies only to state programs Alignment with existing pay for performance programs Minnesota Findings: Health Care Homes (HCH) Progress to Date/Next Steps HCH certification criteria Access and communication Use of registries Care coordination Care planning Practice level quality improvement November 2009: HCH criteria finalized January 2010: Care coordination methodology finalized July 2010: Care coordination payment begin for public programs and health plans. Health plans have HCH available in network. Implementation Challenges Conceptual definition varies Debate over coordination payments Massachusetts’ 2008 Legislation : Chapter 305 Payment and Delivery Redesign Established the Special Commission on the Health Care Payment System Strengthened role of the Health Care Quality and Cost Council to "promote public transparency of the quality and cost of health care in the commonwealth“ Other Key Legislative Provisions Creation the Massachusetts e-Health Institute Charging DPH to develop, implement, and promotion of an evidence-based outreach about cost-effective utilization of prescription drugs Uniform reporting Establishment of a Medicaid medical home demonstration Annual public hearings from providers and hospitals on cost containment and quality Recommendations of the Special Commission on the Health Care Payment System All payers move to a global payment system within 5 years Development of Accountable Care Organizations (ACOs) Focus on patient-centered primary care Preservation of patient choice Cost and quality reporting Risk-sharing between ACOs and payers Development of risk adjustment models Widespread adoption of medical homes Creation of an independent entity to oversee implementation and transition strategy 12 Health Care Quality & Cost Council’s Roadmap to Cost Containment Comprehensive reform phased in over 10 years 1. All payers increase use of payment methodologies that support health care delivery redesign: • 2. 3. Statewide adoption of global payments HCQCC should set cost control targets and monitor cost growth. • 4. P4P, episode-based payments, medical homes, and reduced payments for avoidable hospitalization and preventable readmissions Explore rate regulation if cost targets are not met. Continue state efforts to work with CMS on alternative payment models and system redesign. Massachusetts Findings: Bold Consensus: Wow! How? Special Payment Commission’s unanimous endorsement of global payment signaled understanding that transparency will not control costs alone Ambitious recommendations still quite conceptual; many details still to come Stakeholders (especially hospitals and physicians) given political cover through Commission process Media spotlight provided additional support: national leader on access, Boston Globe series on Partners’ prices, and overall cost trends All the way to global payment? What about episodes? Massachusetts Findings: Technical and Environmental Issues Further legislation needed? Yes, say most observers Independent entity to oversee implementation will be critical Significant activity led by the private sector helping to prepare market Composition is contentious Numerous specific decisions to come identified by Special Payment Commission and many more by stakeholders Moderately strong support for transition strategy recommendations Blue Cross’s Alternative Quality Contract helpful in changing provider payment “mindset” Reorganization and alignment of hospitals & physicians Rate regulation “stick” recommendation by HCQCC does not have wide support, but limits on insurer administrative costs appears to have “legs” 15 Current Status of Massachusetts’ Payment Reform April 2010: Attorney General denied insurance rate increases March 2010: Cost Hearings May 2010: Senate passed legislation to control health care premiums; payment reform NOT included State leaders plan, private leaders continue discussions and pilots Minnesota’s Lessons Passing Major Reform Leadership, leadership and leadership System reform is bipartisan issue Articulation of clear goals motivates action – Triple Aim resonated Good data on variation and cost coupled with personal stories instrumental in building shared sense that status quo unacceptable Mutually valued public-private partnerships to gain critical mass and buyin for the process Major reform element: “total cost of care” introduced too late to gain stakeholder support, was poorly written, and misunderstood Minnesota’s Lessons Payment and Transparency Reforms: A Solid Base Hit Care coordination, episodes of care and value based payments are essential building blocks for future reform Alignment with other existing reporting and payment pilots bolsters work already done An imperfect package is far preferable to a “do nothing” alternative but will it work as a package? Ambitious timetable fueled action and promoted efficiency but didn’t allow time to simplify package Despite the significant collaboration already underway in Minnesota, the legislation has potential to accelerate efforts and improve impact Will enough stakeholders be affected? (and what about Medicare?) Massachusetts’ Lessons Culture of Reform Provides Momentum, Recommendations to Actions Still Tough Political landscape and active reform culture have no doubt shaped the current discussion Unique and expensive health care environment and role of provider as major employer makes controlling costs imperative and difficult Consensus that MA needed to tackle access before costs (“Reform I” did not produce individual winners & losers) Leadership, leadership, and leadership Major bill with infrastructure steps and a high profile Commission and a short timeframe creates momentum Stakeholders signed on to bold recommendations of Commission; later, they supported slower and voluntary adoption and other reforms, along lines of Roadmap report Massachusetts’ Lessons Global Payment in 5 Years? Made Sense But Not the Whole Answer A significant first step in payment reform is deep understanding of FFS payment problems – restating the problem is critical Why go right to global payment? Building a system of episode-based payment would take just as long and is seen only as an interim step The devil is always in the details: What will the ACO’s look like? Can they be virtual? How can gains be shared? The stakeholder tensions: which reforms are most critical for controlling costs? Relative impact of administrative simplification, malpractice reform, consumer incentives – and rate regulation (HCQCC) versus payment reform Cross-Cutting Themes (1) Both states provide models for replication – what they passed or recommended and in how they’ve brought stakeholders along Payment change and transparency reforms: Require an upfront financial investment Critical decisions in implementation – that will reflect local culture and Should start with a core set of measures, add over time – selection process is as important as the measures selected. Payment reform legislated or not? May depend on the culture of the state. But the building blocks -- quality and cost measure and reports on providers and plans need to span system. Cross-Cutting Themes (2) Leadership, leadership, and leadership Timing is everything: In MN, “level 3, total cost of care payment” was ahead of its time in early 2008; MA had another year of national conversation to assist Role of payment reform and transparency in delivery system reform – and need for delivery reform – now more understood than ever. But winners & losers make the road tough. Multiple opportunities in national health reform to propel these states’ efforts on a multi-payer basis! Contact Information and Sources • Anne Gauthier Senior Fellow National Academy for State Health Policy 202-903-0101 agauthier@nashp.org • Kristin Sims-Kastelein 207-874-6524 ksimskastelein@gmail.com www.nashp.org Gauthier, Anne and Cullen, Ann, “Reforming Health Care Delivery Through payment Change and Transparency: Minnesota’s Innovations, “ The Commonwealth Fund #1375, April 2010. Gauthier, Anne and Sims-Kastelein, Kristin, “Health Care Reform Phase Two in Massachusetts: The Road to Payment Reform and Restructured Health Care Delivery,” The Commonwealth Fund, forthcoming.