Session Overview Community Health Centers Implementing EHRs: Lessons Learned
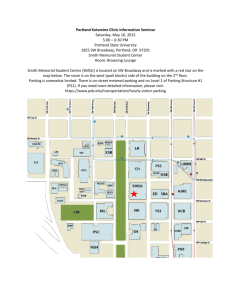
advertisement
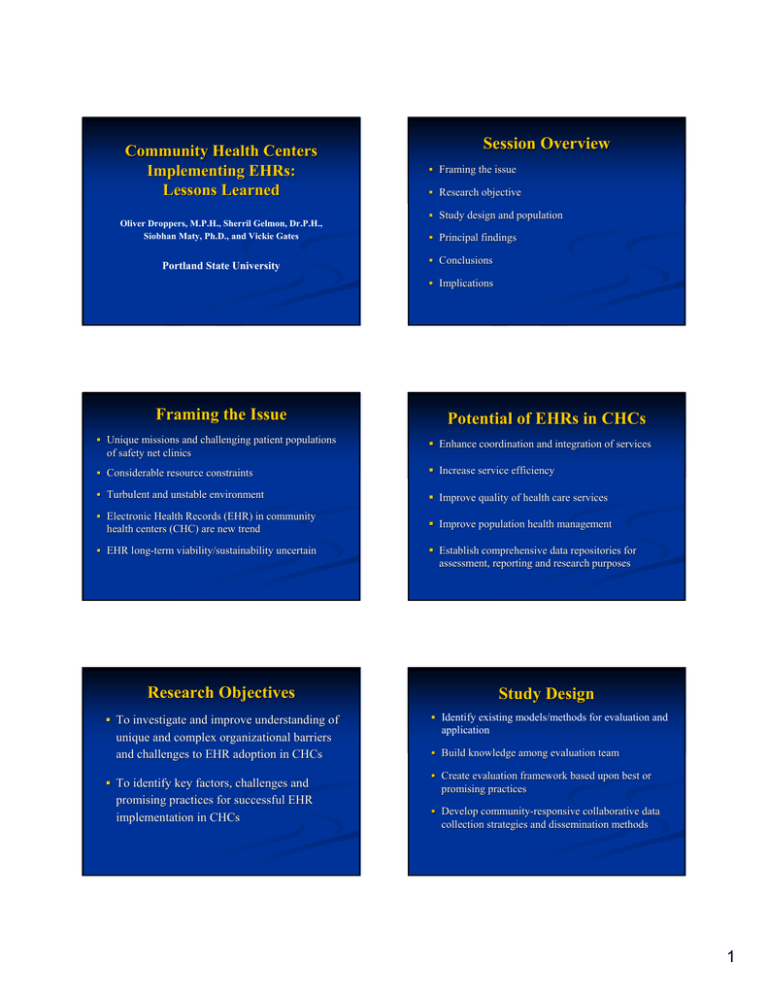
Community Health Centers Implementing EHRs: Lessons Learned Oliver Droppers, M.P.H., Sherril Gelmon, Dr.P.H., Siobhan Maty, Ph.D., and Vickie Gates Portland State University Session Overview Framing the issue Research objective Study design and population Principal findings Conclusions Implications Framing the Issue Unique missions and challenging patient populations of safety net clinics Potential of EHRs in CHCs Enhance coordination and integration of services Considerable resource constraints Increase service efficiency Turbulent and unstable environment Improve quality of health care services Electronic Health Records (EHR) in community health centers (CHC) are new trend EHR longlong-term viability/sustainability uncertain Improve population health management Establish comprehensive data repositories for assessment, reporting and research purposes Research Objectives Study Design To investigate and improve understanding of Identify existing models/methods for evaluation and unique and complex organizational barriers and challenges to EHR adoption in CHCs To identify key factors, challenges and promising practices for successful EHR implementation in CHCs application Build knowledge among evaluation team Create evaluation framework based upon best or promising practices Develop communitycommunity-responsive collaborative data collection strategies and dissemination methods 1 Population Studied Two federally qualified communitycommunity-based health centers operated by a county health department Each center employs 4040-50 fullfull-time staff members Centers serve medically uninsured and underserved populations in Portland, OR Principal Findings: Challenges Significant impact on staff and providers Use of EHR among certain provider groups “problematic” problematic” ProviderProvider-patient interaction changes Need adequate provision of ongoing and continuous training and IT support Regular modifications required to respond to specific needs and patient populations at CHCs Principal Findings: Benefits Improved quality of patient care Increased ease in accessibility and reliability of patients’ patients’ medical records Improved legibility, decreased errors Improved processes for internal communications, patient followfollow-up, tracking events, patient referrals, ordering and accessibility of lab results Overall EHR has been a positive change for patients, staff and providers Implications for CHCs EHRs can potentially improve overall quality of care provided by CHCs EHRs are a complex, multifunctional, and challenging technology for any CHC Conclusions: Organizational Success Factors Strong organizational infrastructure Committed administrative and clinical leadership Existence of clear strategic implementation plan Carefully redesigned organizational processes and workflows Comprehensive training of staff prior to, during, and after implementation Adequate endend-user IT support Ability to respond and adapt rapidly to barriers/changes For Further Information Oliver Droppers, Graduate Research Assistant, Portland State University, odropper@pdx. odropper@pdx.edu Sherril Gelmon, Professor of Public Health, Portland State University, University, gelmons@pdx.edu Successful adoption of EHRs in the safety net context requires: • Strong organizational infrastructure and commitment • Significant capacity for effective change management and ongoing learning • Adequate human and technological resources Supported by the Kaiser Community Fund and the Northwest Health Foundation Our thanks to the staff of the North Portland and MidMid-County Health Centers, Multnomah County Health Department 2