HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis MIT OpenCourseWare .
advertisement

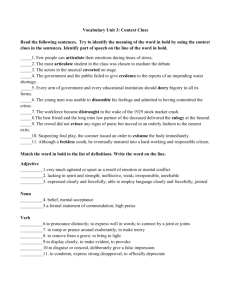
MIT OpenCourseWare http://ocw.mit.edu HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis Fall 2006 For information about citing these materials or our Terms of Use, visit: http://ocw.mit.edu/terms. HST.583: Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006 Harvard-MIT Division of Health Sciences and Technology Course Director: Dr. Randy Gollub. Quantitative fMRI Lecture: BOLD, CBV, & ASL Questions: BOLD 1. We know that R2 = 1/T2. If we want to measure the BOLD relaxation rate, why not approach this problem by using different values of TE and then fitting for T2, rather than using the hypercapnia calibration method? 2. Roughly, how much of the total relaxation rate at 1.5 Tesla is due to the BOLD effect (e.g., express BOLD effect as a percentage of the total effect)? 3. What does the BOLD resting state relaxation rate (equivalently, maximum possible BOLD signal) depend upon in terms of basal physiology? Give multiple answers in terms of physiological variables, with and without coupling assumptions. 4. Draw a plot of BOLD CNR versus echo time. Where is the maximum? Suppose you have problems with image artifacts, and you find that the images are much better using an echo time that is only half as large as the echo time you were told (by some dumb physicist) should be used maximize CNR. How much CNR do you lose with the smaller value of TE? 5. Suppose that you perform a task with and without pretreatment by a drug. With drug pretreatment, the BOLD response is smaller. Give 2 possible interpretations. 6. Suppose you are attempting to image the acute effects to a drug that is known to depress respiration, leading to an increase in PaCO2. Thus, one should expect the response to contain nonspecific vascular effects in addition to potential hemodynamic responses modulated by changes in neural activity. Will the nonspecific effects be more problematic (larger relative to neuronally modulated signals) using BOLD signal or CBF, and why? 7. When might “typical” coupling relationships between CBF and CBV not hold? How about CBF versus CMRO2? Questions: CBV 1. What is the baseline BOLD relaxation rate at 1.5 Tesla? Based upon the BOLD relaxation rate at this field strength, and assuming we use an echo time of 40 ms, how much larger could we make the “amplification factor” using contrast agent? How could we further increase the detection power (CNR) of the CBV method by manipulating the echo time and agent dose? 2. During a functional challenge using a contrast agent, BOLD effects occur in addition to swelling of vessels. How can we estimate this “BOLD contamination” in CBV-weighted fMRI? 3. Could we measure CBV by T1? If so, would this method be more or less sensitive to functional changes than a T2 or T2* method? 4. The use of exogenous contrast agent makes fMRI using T2 or T2* methods much more sensitive than BOLD fMRI at clinical field strengths. Can you explain why the relative sensitivity of these two methods (BOLD versus CBV) depends upon B0? Dose of contrast agent? Basal CBV? TE? Stimulus presentation rate? Questions: ASL 1. Could we detect CBF through T2, rather than T1? What are the major conceptual problems with this suggestion? One-word hints: 1) time scale, 2) coherence 2. What problem might one encounter when applying ASL to stroke? 1 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. Measuring CBV and Hbr through transverse relaxation • Relaxation has components independent & dependent upon agent • Agent-dependent relaxation occurs at rates roughly ~ [A] R Total = R Static + R Agent 2 2 2 , R2 = 1 T2 = R Static + k[A] 2 MRI signal: ! S(t) = S0 e "T E R Static 2 e "T E R Agent (t) 2 1) Suppose we inject exogenous contrast agent. Then we know the pre-injection signal, ! R Agent (t) = " 2 SPRE = S0 e "T E R Static 2 1 # S(t) & ln% ( TE $ SPRE ' ! ! Agent 2 Agent 2 R R (t) (0) = [A](t) [A](0) = V(t) "V(t) = 1+ V(0) V(0) ∴ We can measure ΔV/V versus time using injected agent 2) ! How about BOLD signal? Problem: We can’t easily separate R2Agent from R2Static. → See BOLD model & “hypercapnia calibration” 2 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. BOLD model Goal: relate [Hbr] to CBF (F), CBV (V), and CMRO2 (M) (1) [Hbr] = = ! (2) dO 2 dt " IN [HbT] " [HbO] (1" Y) [HbT] dO 2 dt = OUT dO 2 dt USED OR F [O 2 ] ART (1" Y) = M ! (1& 2) [Hbr ] " M[HbT] F So, functional changes in deoxyhemoglobin are … ! Hbr(t) M(t) = Hbr(0) M(0) (1 HbT(t) " F(t) % $ ' HbT(0) #F(0) & Linearize: drop terms of order small2, and HbT → V ! "Hbr(t) "M(t) "V(t) "F(t) = + # Hbr(0) M(0) V(0) F(0) "R 2 (t) = k " [Hbr ](t) "S ii) Convert to percent signal change: S # $ TE "R 2 i) Convert to BOLD: ! $ "F(t) ! "S(t) "S(t) "V(t) = # & S(0) BOLD,% S(0) BOLD, Max% % F(0) V(0) # "M(t) ' ) M(0) ( ! ! 3 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. “Hypercapnia calibration” for BOLD Goal: BOLD determine BOLD basal relaxation rate, R 2 • Equivalent to basal [Hbr] • Equivalent to maximum obtainable BOLD signal ! Start with BOLD equation: $ "F(t) "S(t) "S(t) "V(t) = # & S(0) BOLD,% S(0) BOLD, Max% % F(0) V(0) # "M(t) ' ) M(0) ( Assumptions 1) ! 2) 3) CMRO2 does not change during hypercapnia. All measurements are performed between steady states to avoid transients (undershoot, etc.) CBF and CBV are coupled (human fMRI cannot easily measure CBV) 2-step procedure in humans: 1) 2) Measure BOLD signal and ΔF/F for hypercapnia → R BOLD or maximum BOLD signal, above 2 Repeat BOLD and ΔF/F for a task → ΔM/M (once the calibration factor is determined in step 1) ! Coupling relationships (normal physiology) Question:Are the contributors to BOLD (F,V,M) independent? Regional relationships, basal physiology: • V(r) = kvf F(r) • M(r) = kmf F(r) everything is linear! Functional relationships: K1 V(t) " F(t) % =$ ' V(0) #F(0) & , or (V(t) (F(t) ) K1 V(0) F(0) (M(t) (F(t) ) K2 M(0) F(0) K1 ~ 0.35, K2 ∈ (0.3,0.5), so assume K2 ~ 0.35 for simplicity Inserting into BOLD equation (above): BOLD ! Hypercapnia = BOLD 0 (.65 "F F) , "M M = 0 BOLDTask = BOLD0 (.30 "F F) #BOLDHypercapnia $ 2 BOLDTask (for matched "F/F) 4 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. Sensitivity of T2 (or T2*) fMRI Goal: Understand basic relationships for BOLD, CBV fMRI CNR = contrast to noise ratio It is useful to break this into SNR and the relative signal change: CNR = SNR "S S • SNR depends upon quantities of interest as a decaying exponential • Percentages signal changes depend linearly upon quantities of interest CNR " x e#x , x = TE , dose, rCBV ! ∴ Maximizing CNR is a balance between SNR and relative signal change MRI signal: ! Relative change: Agent Static e"TE R 2 S(t) = S0 e"TE R 2 (t) exp(#TER Agent (t)) "S S(t) # S(0) 2 = = #1 S S(0) exp(#TER Agent (0) ) 2 ! Agent = e#TE "R 2 (t) #1 $ # TE"R Agent (t) 2 • BOLD CNR is maximized @ TE=T2 SNR !S/S CNR relative units ! • CNR is rather flat versus TE, so choose a somewhat smaller value to minimize signal loss in short T2* regions probablity Below T2* distribution at 9.4T 0 1 2 TE / T2 3 0 5 10 20 30 40 T2* (ms) Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. Sensitivity (continued) CNR = SNR "S S Use expressions on previous page, and rearrange terms: Static CNR = !"S0e"TE R 2 Agent TER Agent (0) e"TE R 2 2 ↑ SCALE #R 2 (t) R Agent (0) 2 (0) ↑ AMPLIFICATION ↑ ACTIVATION ! For global CBV, plot versus dose or field For fixed dose or field, plot versus rCBV large vessels Tissue amplification factor amplification factor 0.4 ~ BOLD, 1.5 T 0 1 0.3 0.2 0.1 0 0 2 TE R2Agent IRON fMRI BOLD fMRI 1 2 3 relative CBV 6 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. Arterial spin labeling (ASL) • Analogies: similar to microspheres or diffusible tracers • Examples: PET-CBF using [15O]-water, autoradiography using iodoantipyrene delivery = F C A (t) Principle: total tracer Q(" ) = F " #C o A (t) dt For ASL, the label is magnetic via inversion ! Differences between PET-CBF and ASL Background Decay Time PET-CBF << label minutes (>> longer than MTT) ASL >> label seconds (~ same as MTT) Repeated measurements minutes seconds 7 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA. R1Apparent = R1Static + F " , " # 1 R1Static = 1 T1 F ~ 60 ~ 1 sec$1 ml 100g $ min ~ .01 sec$1 ∴ F << R1 ASL techniques must address these issues: ! 1. Accurate subtraction of “background” a. Static tissue b. Magnetization transfer (tagging induces off-resonance saturation of image volume 2. Minimizing errors induced by variable blood transit times ~ T1 3. Label must be applied in time, not in space Measuring CBF Difference signal: "S = SControl # SLabel $ 2 % S0 , % & labeling efficiency ! From Buxton, JMRI 2005; 22:723-726 "S(t) = F 2#S 0 $ e%t/T1 8 Cite as: Joe Mandeville, HST.583 Functional Magnetic Resonance Imaging: Data Acquisition and Analysis, Fall 2006. (Massachusetts Institute of Technology: MIT OpenCourseWare), http://ocw.mit.edu (Accessed MM DD, YYYY). License: Creative Commons BY-NC-SA.