Prevalence of pain in hospitalised cancer patients in
advertisement
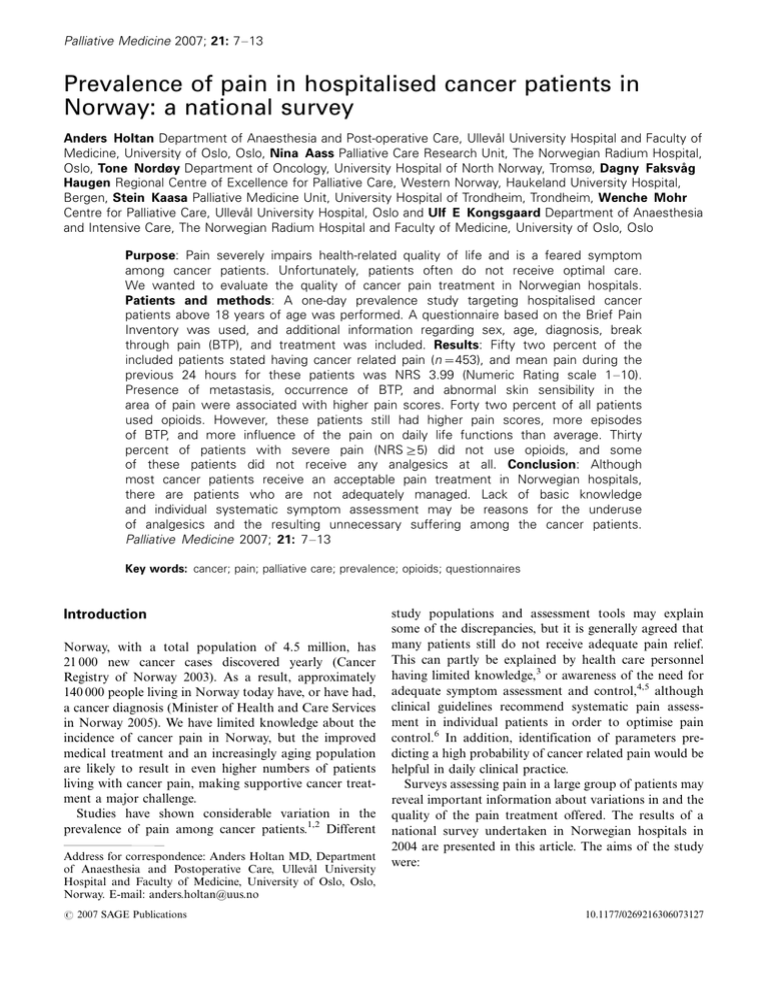
Palliative Medicine 2007; 21: 7 13 Prevalence of pain in hospitalised cancer patients in Norway: a national survey Anders Holtan Department of Anaesthesia and Post-operative Care, Ullevål University Hospital and Faculty of Medicine, University of Oslo, Oslo, Nina Aass Palliative Care Research Unit, The Norwegian Radium Hospital, Oslo, Tone Nordøy Department of Oncology, University Hospital of North Norway, Tromsø, Dagny Faksvåg Haugen Regional Centre of Excellence for Palliative Care, Western Norway, Haukeland University Hospital, Bergen, Stein Kaasa Palliative Medicine Unit, University Hospital of Trondheim, Trondheim, Wenche Mohr Centre for Palliative Care, Ullevål University Hospital, Oslo and Ulf E Kongsgaard Department of Anaesthesia and Intensive Care, The Norwegian Radium Hospital and Faculty of Medicine, University of Oslo, Oslo Purpose: Pain severely impairs health-related quality of life and is a feared symptom among cancer patients. Unfortunately, patients often do not receive optimal care. We wanted to evaluate the quality of cancer pain treatment in Norwegian hospitals. Patients and methods: A one-day prevalence study targeting hospitalised cancer patients above 18 years of age was performed. A questionnaire based on the Brief Pain Inventory was used, and additional information regarding sex, age, diagnosis, break through pain (BTP), and treatment was included. Results: Fifty two percent of the included patients stated having cancer related pain (n /453), and mean pain during the previous 24 hours for these patients was NRS 3.99 (Numeric Rating scale 1 10). Presence of metastasis, occurrence of BTP, and abnormal skin sensibility in the area of pain were associated with higher pain scores. Forty two percent of all patients used opioids. However, these patients still had higher pain scores, more episodes of BTP, and more influence of the pain on daily life functions than average. Thirty percent of patients with severe pain (NRS]/5) did not use opioids, and some of these patients did not receive any analgesics at all. Conclusion: Although most cancer patients receive an acceptable pain treatment in Norwegian hospitals, there are patients who are not adequately managed. Lack of basic knowledge and individual systematic symptom assessment may be reasons for the underuse of analgesics and the resulting unnecessary suffering among the cancer patients. Palliative Medicine 2007; 21: 7 13 Key words: cancer; pain; palliative care; prevalence; opioids; questionnaires Introduction Norway, with a total population of 4.5 million, has 21 000 new cancer cases discovered yearly (Cancer Registry of Norway 2003). As a result, approximately 140 000 people living in Norway today have, or have had, a cancer diagnosis (Minister of Health and Care Services in Norway 2005). We have limited knowledge about the incidence of cancer pain in Norway, but the improved medical treatment and an increasingly aging population are likely to result in even higher numbers of patients living with cancer pain, making supportive cancer treatment a major challenge. Studies have shown considerable variation in the prevalence of pain among cancer patients.1,2 Different Address for correspondence: Anders Holtan MD, Department of Anaesthesia and Postoperative Care, Ullevål University Hospital and Faculty of Medicine, University of Oslo, Oslo, Norway. E-mail: anders.holtan@uus.no # 2007 SAGE Publications study populations and assessment tools may explain some of the discrepancies, but it is generally agreed that many patients still do not receive adequate pain relief. This can partly be explained by health care personnel having limited knowledge,3 or awareness of the need for adequate symptom assessment and control,4,5 although clinical guidelines recommend systematic pain assessment in individual patients in order to optimise pain control.6 In addition, identification of parameters predicting a high probability of cancer related pain would be helpful in daily clinical practice. Surveys assessing pain in a large group of patients may reveal important information about variations in and the quality of the pain treatment offered. The results of a national survey undertaken in Norwegian hospitals in 2004 are presented in this article. The aims of the study were: 10.1177/0269216306073127 8 1) 2) 3) A Holtan et al. To assess pain treatment offered to hospitalised cancer patients on a national basis. To identify objective and reliable measures for cancer related pain. To identify possible factors associated with severe cancer related pain. Patients and methods The target population was all cancer patients ]/18 years of age, hospitalised due to their malignant disease, in any somatic public hospital in the five health care regions in Norway on the day of the study. All patients received oral and written information prior to the study, and informed consent was obtained. Exclusion criteria were: (1) surgery B/24 hours prior to the study; (2) cognitive impairment; (3) patient declining participation; and (4) other reasons. All patients included in the study were anonymous to the central data analysis. Excluded patients, for whom administrative information about age, diagnosis, and use of analgesics was registered, were unidentifiable. The survey was performed as a single day prevalence study, between 08:00 and 12:00 hours in May 2004. All participating hospitals, with the exception of three hospitals in one single region, agreed to participate in the survey on a given date. Due to limited personnel resources, the remaining three hospitals performed the survey on different days the following week. The survey consisted of a questionnaire which was filled in by both patients and investigators. The questionnaire was based on the Brief Pain Inventory (BPI),7 an evaluation tool for cancer related pain which has been translated into Norwegian and validated in Norwegian cancer patients.8 Pain is rated from 0 to 10 using a numerical rating scale (NRS) (0 /no pain, 10/worst possible pain). The experience of pain during the previous 24 hours is assessed as ‘average pain’, ‘least pain’ and ‘worst pain’. In addition, ‘pain right now’ is assessed. Many investigators regard a NRS 5/3 as acceptable and a NRS ]/5 as severe pain.9,10 These levels were, therefore, used as cut-off points in the analysis. The influence of pain on general activity, mood, walking ability, working ability, relationship with other people, sleep, and enjoyment of life were also examined. In addition, the questionnaire covered information regarding sex, age, diagnosis, treatment modality, treatment intention, occurrence of breakthrough pain (BTP), and pain medication. Treatment intention was given as curative, palliative, or unresolved. The questionnaire also included a specific question (for the patient) regarding abnormal skin sensibility in the area of the pain. Questions regarding BTP were: ‘Do you have short episodes of intense pain when your pain treatment otherwise has been generally effective?’, and ‘If yes; how many episodes have you experienced each day (24 hours) on the average?’ The term ‘pain medication’ included both classic analgesics, such as opioids, paracetamol and NSAIDs; and co-analgesics, such as steroids, tri-cyclic antidepressants and antiepileptics. The cancer diagnoses were categorised according to the ICD10 system.11 Some patients had more than one cancer diagnosis and, therefore, were omitted from sub-analyses relating pain and other variables to specific diagnosis. Data are also presented in relation to age and hospital size. Older patients are defined as age 75 years and above and younger as B/75 years. This project was supported by an unrestricted grant from Mundipharma AS, Lysaker, Norway and the Regional Committees for Medical Research Ethics in Norway. The Norwegian Social Science Data Services approved the study. Statistical analyses The statistical program SPSS, version 11.5, was used for statistical analyses. Results in pain-scores are presented as mean values. One-way variance analyses were used to identify differences between groups, and t -tests were thereafter applied to verify these differences. Although the material did not always show a normal distribution, parametric tests were applied due to the large size of the groups. For smaller groups, KruskalWallis and Mann Whitney tests were applied. Categorical data was compared with Pearson’s x2-tests, Fisher’s exact test and linear-by-linear x2-tests. Linear regression analyses were used to determine predictors for higher pain scores/ intensity, and NRS scores were regarded as continual variables in these analyses. A P valueB/0.05 was regarded as statistically significant. Results Patient characteristics A total of 1337 patients, with a mean age of 66 years, from 57 hospitals in all five Norwegian health care regions were accrued (Figure 1). Four small hospitals did not take part in the study due to administrative problems. A total of 872 patients were included and 465 excluded. The reasons for exclusion were: patient refusal (n /158), cognitive impairment (n/148), surgery B/24 hours prior to the study (n/62), and other reasons (n/97). Detailed patient characteristics are presented in Table 1. The most prevalent diagnoses were gastrointestinal, gynaecological, urological, pulmonary, and haematological malignancies. Some 30% of the patients were age 75 or above, and this group had a significant lower inclusion rate (56%) than the younger patients (70%). Females, likewise, had a significant lower inclusion rate compared to males (61.4 versus 70.1%). For other variables, no differences between the included and excluded patients were found. Although the treatment intention was palliative for the Cancer pain in Norwegian hospitals 9 Study target population 61 Norwegian public somatic hospitals 4 hospitals did not participate All patients 1337 patients, 57 Hospitals Excluded patients 465 patients, 50 hospitals Included patients 872 patients*, 55 hospitals Included patients without cancer pain 404 patients* Included patients with cancer pain 453 patients* Figure 1 The term ‘‘all patients’’ is in this article defined as the total number of registered patients, both included patients, who have accepted participating in the study; and the excluded patients. *There is missing information about presence of cancer related pain in 15 included patients Table 1 Descriptive data for the excluded patients, included patients without cancer related pain, and included patients with cancer related pain. The figures show number of patients with percent on the basis of ‘‘all patients (n/1337)’’ in brackets: No of patients* Female Male Missing information regarding sex Age (Mean years) Missing information regarding age Excluded patients Included patients without cancer related pain Included patients with cancer related pain 465 261 192 12 404 196 206 2 453 211 238 4 (100) (56.1) (41.3) (2.6) 67.8 (n /459) 6 (1.3%) (100)* (48.5) (51.0) (0.5) 66.1 (n /404) 0 (100)* (46.6) (52.5) (0.9) 63.4 (n /453) 0 Diagnosis** GI cancer Urological cancer Haematological malignancies Lung cancer Gynaecological cancer Breast cancer Head and neck cancer Other diagnoses Missing information regarding diagnosis 122 (26.2) 77 (16.6) 54 (11.6) 52 (11.2) 32 (6.9) 37 (8.0) 20 (4.3) 82 (17.6) n/1 (0.2) 99 (24.5) 67 (16.6) 70 (17.3) 48 (11.2) 46 (11.4) 27 (6.7) 14 (3.5) 49 (12.1) n /0 113 (24.9) 71 (15.7) 64 (14.1) 57 (12.6) 50 (11.0) 37 (8.2) 20 (4.4) 54 (11.9) n /1 (0.2) Metastases-any localization Bone metastases Liver metastases Lung metastases Brain metastases 153 38 46 22 18 (32.9) (8.2) (9.9) (4.7) (3.8) 108 22 23 11 16 (26.7) (5.4) (5.7) (2.7) (4.0) 170 77 39 24 13 (37.5) (17.0) (8.6) (5.3) (2.9) Treatment intention Palliative Curative Unresolved Missing information regarding treatment intentions 219 114 57 75 (47.1) (24.5) (12.2) (16.1) 182 145 63 14 (45.0) (35.9) (15.6) (3.5) 271 120 49 13 (59.8) (26.5) (10.8) (2.9) Treatment modality Preceding surgery Ongoing radiotherapy Ongoing chemotherapy Missing information regarding treatment modality 202 63 68 62 (43.4) (13.5) (14.6) (13.3) 207 81 120 1 (51.2) (20) (29.7) (0.3) 257 96 103 1 (56.7) (21.2) (22.7) (0.2) *There is missing information about presence of cancer related pain in 15 included patients. **Diagnoses: GI-cancer includes oesophagus, ventricle, jejunum/ileum, colon, rectum, pancreas and liver cancer. Gynaecological cancer includes ovarian, corpus uteri, cervix uteri, and vulva cancer. Urological cancer includes kidney, ureter, bladder, urethra, penis, prostate, and testis cancer. Haematological malignancies include lymphoma, leukaemia, and multiple myeloma. Some patients have more than one diagnosis. 10 A Holtan et al. majority of patients in all hospitals, the relative proportion of this group was especially high in small local hospitals. Cancer related pain A total of 52% of the included patients (n /453) reported pain by answering ‘Yes’ to the opening question: ‘Throughout our lives, most of us have had pain from time to time (such as minor headaches, sprains, and toothaches). Have you had pain other than these everyday kinds of pain today?’.12 The prevalence of pain for patients with advanced disease (metastases or palliative treatment intention) was 61%. The mean scores, using the NRS, for ‘average pain’ score during the last 24 hours for patients who reported pain was 3.99 (SD 2.2), ‘worst pain’ 5.10 (SD 2.6), ‘least pain’ 1.80 (SD 1.9), and ‘pain right now’ 2.56 (SD 2.3). Some 80% of the patients with cancer related pain had an ‘average pain’ scoreB/5 (Figure 2). There was no difference in pain scores between the two age groups. Some 37% (n/322) of the included patients reported having BTP, with a mean of five episodes a day and a median of three. A total of 61 patients reported having six episodes or more of BTP daily. Compared to patients with scores5/3, patients who reported average pain more than three times during the previous 24 hours, more often had a palliative treatment intention. They were also more likely to have episodes of BTP, abnormal skin sensibility in the area of pain, or used any form of opioid-analgesics. Increased pain, measured as a continuous variable, correlated to high scores with regard to the pain’s influence on general activity, mood, walking ability, working ability, relationship to other people, sleep, and enjoyment of life. Patients with BTP and abnormal skin sensibility in the area of pain scored significantly higher on these functional parameters than those without these symptoms. Variables predicting severe cancer pain Certain variables were tested to see whether they were associated with higher pain intensity (Table 3). The variables used in this analysis were partly selected from relevant literature,13 16 and partly chosen from our own clinical experience. The two variables found to be most important in predicting pain, were ‘presence of BTP’ and ‘abnormal skin-sensibility in the area of pain’. Use of analgesics The use of analgesics was registered for both included and excluded patients (Table 2). Of all patients, 28% (n/374) used no analgesics, 4% (n /57) used only coanalgesics, while the rest used traditional analgesics that could be related to steps on the WHO ladder.17 Excluded patients used less analgesic than patients included in the survey (Table 3). The included patients were analysed in more detail: 75% used analgesics. Patients who reported pain used more analgesics compared to patients without pain (Table 2). Of the patients reporting pain, 62% used opioids compared to 24% of the patients without pain. One-third of the included patients who were using weak opioids, corresponding to step 2 on the WHO ladder, also used strong opioids belonging to step 3 on the ladder. Looking at different routes of opioid administration, the oral route was most common (74%, n/284), followed by parenteral (29%, n /111), and transdermal routes (27%, n /104). Of the included patients, 10% (n /88) used both paracetamol and NSAIDs. No difference related to age was found in the use of opioids or NSAIDs. Patients who reported BTP received significantly more analgesics and coanalgesics than patients without BTP. Of the patients reporting pain, 37% did not receive any analgesic at all. Of the patients with mean pain score]/5, 30% (n/54) did not use opioids, and 7% (n/12) did not receive any analgesics. 250 Discussion 200 150 100 50 9 8 7 6 5 4 3 2 1 0 10 M is si ng 0 Figure 2 Dispersion of ‘average’ pain during the last 24 hours for the included patients (n /872), given as NRS (X-axis) and number of patients (Y-axis) This national survey was performed in 57 of 61 Norwegian public hospitals to evaluate the prevalence of pain in hospitalised cancer patients. A total of 1337 cancer patients were registered on the day of the study, of which 872 were included. Of the included patients, 52% reported pain, with mean pain score (NRS 0 10) ‘average pain’ for the preceding 24 hours of 3.99. Of the patients with pain, 20% reported ‘average pain’ as severe ( ]/5). About 60% of the patients reporting pain used strong opioids. Our target population was all cancer patients hospitalised due to their malignant disease on the day of the study. Four smaller hospitals did not take part in the Cancer pain in Norwegian hospitals 11 Table 2 The table demonstrates the use of analgesics, given as the number of patients and columnar percentage. The number of patients in each group that did not use any analgesics is also given: Drug All patients n /1337 Excluded patients n /465 All included patients n /872 Included patients having no cancer related pain n /404 Included patients having cancer related pain n /453 Paracetamol NSAIDs** Weak opioids** Strong opioids** TCA & AE*** Steroids No analgesics 617 191 186 559 117 274 374 190 58 46 177 36 87 157 427 133 140 382 81 187 217 150 42 42 97 16 78 44 272 89 94 281 63 108 167 (46.1) (14.3) (13.9) (41.8) (8.8) (20.5) (28.0) (40.1) (12.5) (9.9) (38.0) (7.7) (18.7) (33.8) (49.9) (15.3) (16.1) (43.8) (9.3) (21.4) (24.8) (37.1) (10.4) (10.4) (24.0) (4.0) (19.3) (10.9) (60.0) (19.6) (20.8) (62.0) (13.9) (23.8) (36.9) *There is missing information about presence of cancer related pain in 15 included patients. **NSAIDs include coxibs. Weak opioids include codeine, dextropropoxyphene, and tramadol. Strong opioids include morphine, oxycodone, fentanyl, buprenorphine, and ketobemidone. ***TCA/tri-cyclic antidepressants, AE/antiepileptics. study. There is, of course, a possibility that a few cancer patients might have been missed in the 57 participating hospitals. The percentage of females and old patients was significantly lower among the included than the excluded patients. More of the included patients used analgesics compared to those not included in the survey. Otherwise, there were no differences between the included and excluded patients. Due to the high number of included patients, we think the material is reliable because of: (1) an overall inclusion rate of 66%; (2) a normal distribution of gender and age; (3) few differences among the regions concerning included patients, inclusion rates, diagnoses, and age; (4) and an overall distribution of diagnoses reflecting the prevalence of the different cancer types in Norway, as described by the Norwegian Cancer Registry.18 To our knowledge a national sample, such as the present series, has never been achieved before. Most prevalence studies are smaller,20 have been performed in smaller groups defined by diagnosis, limited geographical areas, or hospitals.21 In this study, the prevalence of cancer related pain in hospitalised patients was found to be 52%. In a previous Norwegian regional survey, a similar result of 51% was found.22 A review of other studies gave a mean cancer pain prevalence of 40% (range: 18 100%) for the group ‘general adult population’.23 Some of these studies also included outpatients, which may be reflected in a lower prevalence of pain Table 3 Regression analyses were used to identify variables associated with higher NRS. Pain scores were regarded as a continual variable, and mean pain preceding 24 hours were chosen as the dependent variable: Unstandardized Coefficients B (Constant) Gender Age]/75 orB/75 years GI cancer Urological cancer Haematological malignancies Other diagnoses Lung cancer Gynaecological cancer Breast cancer Head and neck cancer Presence of metastases Curative treatment intention Palliative treatment intention Treatment intention unresolved Presence of Break Through Pain Abnormal skin sensitivity* Small Hospitals Medium Hospitals Large Hospitals Dependent Variable: Mean pain 24 hours 3.649 /0.032 0.002 0.151 /5.096 /5.033 /5.179 /4.805 /5.150 /5.164 /4.395 0.133 0.040 0.440 0.555 1.849 1.023 /0.217 /0.028 /0.302 *Abnormal skin sensitivity in the area of pain. Standardized Coefficients Std. Error Beta t Sig. 3.193 0.181 0.006 0.356 2.196 2.200 2.202 2.194 2.201 2.200 2.216 0.198 0.496 0.482 0.516 0.170 0.175 2.190 2.185 2.186 /0.007 0.012 0.026 /0.748 /0.704 /0.614 /0.645 /0.646 /0.974 /0.421 0.026 0.008 0.089 0.076 0.367 0.196 /0.033 /0.006 /0.061 1.143 /0.174 0.355 0.425 /2.320 /2.287 /2.352 /2.190 /2.340 /2.347 /1.984 0.672 0.081 0.913 1.075 10.878 5.855 /0.099 /0.013 /0.138 0.254 0.862 0.723 0.671 0.021 0.022 0.019 0.029 0.020 0.019 0.048 0.502 0.936 0.361 0.283 0.000 0.000 0.921 0.990 0.890 12 A Holtan et al. compared to our findings. In the same review, the prevalence of pain in patients with advanced cancer was 74% (range: 53100%) compared to our findings of 61%. When using the BPI, some patients may answer ‘Yes’ to the opening question (‘Other than these everyday kinds of pain, have you had pain today?’) on a different basis than cancer related pain, ie, due to chronic nonmalignant conditions. However, this is probably relevant for only a small number of patients. The instrument also does not differentiate between disease related and treatment related pain. For some groups of patients, the pain is mostly related to therapy, as in patients with head and neck cancer receiving curative irradiation.19 Furthermore, a one-day prevalence study will not capture the dynamic nature of pain. Our study, for example, did not take into account the length of time the patient had been admitted to the hospital. Pain is one of the symptoms most feared by cancer patients.24,25 In the present study, the ‘average pain’ score for the last 24 hours was close to 4, and 20% of the patients reported ‘average pain’ ]/5. It is also worth mentioning that no differences in pain intensities related to age are shown in this study (Table 3). Former studies have both found,16 and not found,14 that increasing age accompanies increased pain intensity. Even though many patients were using strong opioids, there seems to be an underuse of these drugs. As this was a survey in hospitalised patients, it is not surprising that the parenteral route of opioid administration was often utilised. Patients taking strong opioids had significantly higher NRS scores than patients not using this type of analgesic. Many of the patients on strong opioids also reported having more than six episodes of breakthrough pain per day, which might be a sign of under-dosage. It is, therefore, reasonable to conclude that the use of neither long-acting nor short-acting opioids seems to be optimal. It could be argued that only those few patients who were receiving opioids, but did not report having cancer related pain, have received optimal treatment (n /97). In relation to new knowledge regarding mechanisms in cancer pain, it could also be argued that the use of coanalgesics in our patients group is too low (Table 2). This is supported by our findings that altered skin sensibility of pain (perhaps indicating a neuropathic component?) was one of the variables for predicting severe cancer pain. Thus, there is obviously a potential for improving cancer pain management in Norway. Our findings indicate that the principles of the WHO ladder,26 are not followed, and that patients are suffering as a result. One example illustrating this is that one out of three patients using analgesics from step 2 (weak opioids, ie, codeine), also use strong opioids belonging to step 3 of the ladder. This is normally not regarded as state of the art pain therapy, and this finding may suggest a need for better education in palliative care. A mean NRS score for the previous 24 hours of close to 4 for ‘average pain’ is probably also not satisfactory. On the other hand, the fact that 47% of the included patients reported no pain may seem acceptable. Comparison with other countries is not possible, since no similar studies are known. The prevalence of BTP is highly variable in different study materials.27 In the present series, the prevalence of BTP was 37%. Patients reporting BTP scored worse on all pain and pain-related items. Our findings correspond to results from previous studies, demonstrating that patients with BTP assess their pain as worse than those without BTP, and that they have a poorer quality of life, and a more complex situation.27 The fact that patients with BTP had a higher score on all pain related items, may reflect that many patients did not have adequate fast acting ‘on-demand’ analgesics, that they were on a too low dosage of long-acting opioids, or that they have a more complex pain syndrome with mixed pain or a component of neuropathic pain. Several variables that could predict severe cancer pain were found. Few studies have searched for such positive and negative predictors, and most deal with highly selected populations.13 16 The two most prominent variables for predicting cancer related pain were the existence of BTP and abnormal skin sensibility in the area of pain. These results are similar, in part, to other findings where researchers have found, for example, bone metastases, BTP, and the presence of metastases, associated with higher pain intensity.13,14,16 Conclusion In this study, 52% of the patients reported having cancer related pain with a mean pain score (NRS) for ‘average pain’ the previous 24 hours of 3.99. Patients with BTP, and abnormal skin sensitivity in the area of pain were found more likely to report more pain. Some 42% of all patients used opioids, and these patients had higher pain scores, more episodes of BTP, and had their daily life functions more influenced by pain than those patients not receiving opioids. Many patients reporting severe pain did not use opioids, and some did not receive any analgesics at all. This survey reveals that many hospitalised cancer patients in Norway do not receive adequate pain relief. Health care personnel’s lack of basic knowledge in treatment of pain, insufficient focus on the patients’ pain experience, and inadequate systematic symptom assessment are probably some of the reasons for suboptimal treatment. This is a continuous challenge in basic education and specialist training for all personnel groups caring for cancer patients. New surveys should be performed in order to monitor improvement. Cancer pain in Norwegian hospitals Acknowledgements We have received statistical assistance from biostatistician B Sandstad at The Norwegian Radium Hospital, Oslo, Norway; and administrative assistance and technical equipment offered by the Clinical Research Office, also at The Norwegian Radium Hospital, Oslo, Norway. The project was supported by an unrestricted grant from Mundipharma AS, Lysaker, Norway. 9 10 11 Conflict of Interest Statement Anders Holtan has received payment for his role as lecturer from Mundipharma. All payments less than $4000. Ulf E Kongsgaard has received payments for his role as advisor, member of expert groups, and lecturer from Mundipharma, Swedish Orphan and Pfizer. All payments were lesss than $4000. He has also received research funding from Mundipharma. Stein Kaasa has received payments for his role as advisor and member of expert groups from Janssen-Cilag, Mundipharma and Nycomed. The other authors have no financial or other relationships that might lead to conflict of interests. 12 13 14 15 16 17 References 1 Portenoy RK. Cancer pain. Epidemiology and syndromes. Cancer 1989; 63(11 Suppl): 2298 307. 2 Bonica JJ. Treatment of cancer pain: current status and future needs. In Fields HL ed. Advances in pain research and therapy. Raven Press, 1985: 589 616. 3 Catane R, Cherny NI. Attitudes of medical oncologists toward palliative care for patients with advanced and incurable cancer. Report on a Survey by the European Society of Medical Oncology Taskforce on Palliative and Supportive Care 2003 . American Cancer Society, 2003. 4 Cleeland CS, Gonin R, Hatfield AK, Edmonson JH, Blum RH, Stewart JA, et al . Pain and its treatment in outpatients with metastatic cancer. N Engl J Med 1994; 330(9): 592 96. 5 Melsom H, Wist E. Terminalomsorg til kreftpasienter. [Terminal care of cancer patients]. Tidsskr Nor Laegeforen 2001; 121(22): 2590 92. 6 Jacox A, Carr DB, Payne R. Management of cancer pain. Clinical practice guideline. AHCPR Publication No. 94-1592, 1994. 7 Cleeland CS. Measurement and prevalence of pain in cancer. Semin Oncol Nurs 1985; 1(2): 87 92. 8 Klepstad P, Loge JH, Borchgrevink PC, Mendoza TR, Cleeland CS, Kaasa S. The Norwegian brief pain inventory questionnaire: translation and validation in 18 19 20 21 22 23 24 25 26 27 13 cancer pain patients. J Pain Symptom Manage 2002; 24(5): 51725. Cleeland CS, Nakamura Y, Mendoza TR, Edwards KR, Douglas J, Serlin RE. Dimensions of the impact of cancer pain in a four country sample: new information from multidimensional scaling. Pain 1996; 67(2 3): 267 73. The Norwegian Medical Association. Standard of palliation . i. 29-11-2005. Ref type: Internet communication. ICD-10. (Den internasjonale klassifikasjonen av sykdommer og beslektede helseproblemer ). Statens Helsetilsyn, 1998. Cleeland CS. Pain assessment in cancer. CRC Press, 1991. Strømgren AS. Pain characteristics and treatment outcome for advanced cancer patients during the first week of specialised palliative care. J Pain Symptom Manage 2004; 27(2): 104 13. Rustøen T. The impact of demographic and diseasespecific variables on pain in cancer patients. J Pain Symptom Manage 2003; 26(2): 696 704. Barnabei R. Management of pain in elderly patients with cancer. JAMA 1998; 279(23): 1877 82. Given CW. Predictors of pain at fatigue in the year following diagnosis among elderly cancer patients. J Pain Symptom Manage 2001; 21(6): 456 66. World Health Organization. WHO technical document CAN/84.2 . WHO, 1984. Cancer Registry of Norway. Cancer in Norway. 2003. Chaplin JMMR. A prospective, longitudinal study of pain in head and neck cancer patients. Head Neck 1999; 21(6): 53137. Larue F, Colleau SM, Brasseur L, Cleeland ES. Multicentre study of cancer pain and its treatment in France. BMJ 1995; 310(6986): 1034 37. Higginson IJHJ, Addington-Hall J. Epidemiology of cancer pain. In Syles N, Fallon MT, Patt RB eds. Clinical pain management cancer pain . Arnold, 2003: 21 32. Holtan A, Kongsgaard UE, Ohnstad HO. Smerter hos kreftpasienter innlagt i sykehus-en prevalensundersøkelse i Helse Sør. Tidsskriftet for den norske legeforening 2005; 125(4): 41618. Higginson IJ, Hearn J. A multicenter evaluation of cancer pain control by palliative care teams. J Pain Symptom Manage 1997; 14(1): 29 35. Cleeland CS. The impact of pain on the patient with cancer. Cancer 1984; 54(11 Suppl): 2635 41. Doyle D, Hanks G, MacDonald N. Oxford textbook of palliative medicine. Oxford University Press, 1998. WHO. Cancer pain relief, second edition. World Health Organization, 1996. Aea C. Working Group of an IASP Task Force on Cancer Pain. Breakthrough pain characteristics and syndromes in patients with cancer pain. An international survey. Palliat Med 2004; 18(3):177 83.