SIMULTANEOUS
mTc-MDP/l 2 I-MIBG IMAGING OF NEUROBLASTOMA USING
ARCMVES
SPECT-CT
99
By
Jose P. Pdrez-Gutierrez
SUBMITTED TO THE DEPARTMENT OF NUCLEAR SCIENCE AND ENGINEERING
IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREES OF
BACHELOR OF SCIENCE IN NUCLEAR SCIENCE AND ENGINEERING
AND
MASTER OF SCIENCE IN NUCLEAR SCIENCE AND ENGINEERING
AT THE
OF TECHNOLOGY
INSTITUTE
MASSACHUSETTS
SEPTEMBER 2011
C 2011 Massachusetts Institute of Technology
All rights reserved
Signature of Author:
V7
Jose P. Perez-Gutierrez
Department of Nuclear Science and Engineering
August 11, 2011
Certified by :
~v
Jinsong Ouyang
Assistant Professor of Radiology, Department of Radiology, Harvard Medical School
Thesis Supervisor
Certified by:
Richard Lanza
enor Research Scie
ist,
epartment of Nuclear Science and Engineering, MIT
Thesis Reader
Accepted by:__________
Mujid S. Kazimi
MIT
Engineering,
Nuclear
of
TEPCO Professor of Nuclear En 'neerin , Department
Chai , epartment Committee on Graduate Students
2
SIMULTANEOUS
99 mTc-MDP/ 23I-MIBG
IMAGING OF NEUROBLASTOMA USING
SPECT-CT
By
P.
Perez-Gutierrez
Jose
SUBMITTED TO THE DEPARTMENT OF NUCLEAR SCIENCE AND ENGINEERING IN
PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE DEGREES OF
BACHELOR OF SCIENCE IN NUCLEAR SCIENCE AND ENGINEERING AND MASTER
OF SCIENCE IN NUCLEAR SCIENCE AND ENGINEERING
Abstract
Simultaneous 99mTc-MDP/ 1 3I-MIBG SPECT has the potential to replace current clinical
sequential acquisitions of 99 mTc-MDP and 12 I-MIBG SPECT studies, and therefore has great
potential to reduce imaging time, sedation time, and injection dose on patients with
neuroblastoma. Simultaneous 99mTc/I 231 imaging is challenging because of the crosstalk between
the 99mTc and 1231 photo-peak windows due to down-scatter of 1231 photons (159keV) to the 99mTc
(140keV) photo-peak window and limited energy resolution of the scanner. Additionally, the
counts of detected photons are limited because the injection dose as well as scan time are limited
for neuroblastoma patients and scan acquisition cannot be performed for at least 24 hours after
123 1-MIBG injection. These factors hinder the separation of images of these two radionuclides.
An enhanced fast Monte Carlo based joint ordered-subset expectation maximization
(MC-JOSEM) reconstruction algorithm has been been developed for simultaneous 99mTc/I 2 3
imaging by Ouyang, El Fakhri, and Moore (2007). MC-JOSEM incorporates attenuation into a
full system matrix to greatly improve image accuracy and include both primary and scattered
photons in the reconstruction process to significantly reduce image noise.
Separate 99mTc-MDP and 123 I-MIBG Monte Carlo simulations were performed. For each
isotope, noise-free projection data sets were generated first. Lesions were then added to the 99mTc
and 2I data separately. Mimicked dual-isotope data were then generated by combining the
99mTc and 1231 data. Images for single-isotope and dual-isotope were reconstructed by using
standard clinical single-isotope OSEM and MC-JOSEM, respectively. Channel Hotelling
observer (CHO) was used to calculate lesion detectability. On average, the CHO SNR obtained
from dual-isotope studies is close to that of single-isotope studies for each radionuclide. (SNR:
3.521 for dual-isotope versus 3.828 for single-isotope). Hence, simultaneous 99mTc-MDP/ 23 1_
MIBG has the potential to replace sequential 99mTc-MDP and 12 3I-MIBG for neuroblastoma
imaging.
Thesis Supervisor: Jinsong Ouyang
Title: Assistant Professor of Radiology, Department of Radiology, Harvard Medical School
Thesis Reader: Richard Lanza
Title: Senior Research Scientist, Department of Nuclear Science and Engineering, MIT
3
Acknowledeements
I would like to express my deepest gratitude to Dr. Jinsong Ouyang, my thesis supervisor, for
his help, guidance and support throughout this work. Working with you was very enriching to my
knowledge and experience. Your kindness, patience and understanding made it possible to overcome
all the hardships while finishing this work.
I would also like to acknowledge professor Richard Lanza and Dr. Georges El Fakhri, my
thesis readers, for guiding me in the right direction from the start of this endeavor. Thank you
also for your helpful comments on the thesis. Your encouragement and support is much
appreciated.
I would also like to thank some very special professors I had along my MIT career.
Professor Jacquelyn Yanch, you were a great professor, advisor, and mentor; your counsel
guided my path through MIT, and I am very grateful for it. Dr. Gordon Kohse, thank you for
always having time to meet with me to discuss various topics, and counsel me; your patience is
very well appreciated. Dr. Phillip Zhe-Sun, thank you for providing me with a strong foundation
in biomedical imaging, and for being a great friend. Professor Alan Jasanoff, thank you for
further strengthening my background in biomedical imaging.
I would like to thank my best friend, Osvaldo Laurido-Soto, for always being there for
me. More than a friend, you are like a brother to me, and I am lucky to have you in my life.
No words can describe my gratitude towards my dearest, closest, and most important
people in my life: my mother, Brunilda Gutierrez-Kercad6; my father, Jose R. Perez-Anzalota;
and my sister, Brunelle Perez-Gutidrrez. Not a moment has passed in my life that I haven't felt
your endless love and care for me. I wouldn't be here without you. I owe you everything, and to
you I dedicate this thesis.
4
Table of Contents
A bstract .....................................................................
Acknow ledgem ent ............................................................
Table of C ontents .............................................................
List of Figures ................................................................
List of Tables ................................................................
1 Introduction ..............................................................
2 Literature Review .........................................................
2.1 Nuclear Medical Imaging Overview ........................................
2.2 SPECT ...............................................................
2.2.1 Designs and Principles of Operation ..................................
2.2.2 Image Acquisition ...............................................
2.2.3 Gamma Camera .................................................
2.2.4 Scintillation Detection ..........................................
2.2.5 Collimation ......................................................
2.3 Image-degrading Effects in SPECT .......................................
2.3.1 Photon Interactions with Matter .....................................
2.3.2 Collimator Blurring .............................................
2.3.3 Poisson Noise ...................................................
2.3.4 Other Image-Degrading Effects .....................................
2.4 SPECT Monte Carlo Simulation ..........................................
2.4.1 GATE Program for SPECT Simulation ...............................
2.4.2 Computational Human Phantoms ....................................
2.4.3 SPECT Reconstruction ............................................
2.5 Simultaneous Dual-Isotope SPECT .......................................
2.5.1 Simultaneous 99mTc/I 231 Neuroblastoma SPECT Imaging ..................
2.5.2 Down-scatter and Cross Talk ......................................
2.5.3 Image Reconstruction in Dual-Isotope SPECT ..........................
3.1
MC (GATE) Simulation of Simultaneous
mTc/
32
33
36
37
39
40
42
3 M ethods .................................................................
99
3
4
5
6
9
10
12
12
13
14
15
17
18
19
20
20
28
30
31
31
32
12 3
1 Studies .....................
3.1.1 SPECT System Specifications ......................................
3.1.2 NCAT Phantom Specifications ......................................
3.1.3 99mTc and 1231 SPECT Simulations ...................................
42
42
42
43
3.2 Reconstruction Methods for Simultaneous 99mTc/ 1231 Studies ....................
3.3 Lesion Detectability Comparison ........................................
4 Results and Discussion .....................................................
4.1 MC (GATE) Simulation of Simultaneous 99mTc/ 12 31 Studies .....................
4.2 Reconstruction of Simultaneous 99mTc/ 1231 Studies ............................
4.3 Lesion Detectability Comparison ........................................
5 Conclusions and Future Projections..........................................53
45
47
49
49
50
51
6 W orks Cited ..............................................................
54
5
List of Figures
Figure 2.1. Siemens Symbia T6 SPECT-CT Scanner. The Symbia TruePoint SPECT-CT
combines variable angle dual-detector SPECT with 6-slice CT for rapid, accurate attenuation
correction, precise localization, and advanced CT applications in cardiology, oncology, and
neurology. Source: Siemens Global Website: www.medical.siemens.com................. 15
Figure 2.2. (A) Circular and (B) body-contour orbits in SPECT (from Bushberg et al. 2002). .16
Figure 2.3. Gamma Camera. This schematic shows a NaI(Tl) crystal scintillation camera
detector. A scintillation camera contains a disk-shaped or rectangular thallium-activated sodium
iodide, NaI(TI), crystal, typically 0.95-cm thick, optically coupled to a large number (typically
37 to 91) of 5.1- to 7.6-cm diameter photomultiplier tubes (PMTs). The PMT are connected to
pre-amplifiers that connect to a circuit that analyze the data (position encoding and pulse-height
analysis) (from Bushberg et al. 2002) .............................................
18
Figure 2.4. Ways that Photons Interact with a Scintillation Camera. All of these, other than
the ones depicted in the upper left, cause a loss of contrast and spatial resolution. However,
interactions by photons that have scattered though large angles and many coincident interactions
are rejected by pulse height discrimination circuits (from Bushberg et al. 2002)............ 21
Figure 2.5. Mass Attenuation Coefficient as a Function of Energy. This graph shows the
Rayleigh, photoelectric, Compton, pair production, and total mass attenuation coefficients for
soft tissue (Z=7) as a function of energy (from Bushberg et al. 2002)..................... 22
Figure 2.6. Photoelectric Effect. Left: The diagram shows a 100-keV photon is undergoing
photoelectric absorption with an iodine atom. In this case, the K-shell electron is ejected with a
kinetic energy equal to the difference between the incident photon energy and the K-shell
binding energy of 34: 66 keV. Right: The vacancy created in the K shell results in the transition
of an electron from the L shell to the K shell. The difference in their binding energies, (i.e., 34
and 5 keV), results in a 29-keV Ka characteristic x-ray. This electron cascade will continue
resulting in the production of other characteristic x-rays of lower energies. Note that the sum of
the characteristic x-ray energies equals the binding energy of the ejected photoelectrons.
Although not shown on this diagram, Auger electrons of various energies could be emitted in
lieu of the characteristic x-ray emissions (from Bushberg et al. 2002)....................
23
6
Figure 2.7. Compton Scattering. The diagram shows the incident photon with energy E0 ,
interacting with a valence shell electron that results in the ejection of the Compton electron (Be-)
and the simultaneous emission of a Compton scattered photon (Esc) emerging at an angle, 0,
relative to the trajectory of the incident photon. K, L, and M are electron shells (from Bushberg et
a. 2002).....................................................................25
Figure 2.8. Compton Scattering Probabilities. This is a polar plot of the number of photons
(incident from the left) Compton scattered into a unit solid angle at the scattering angle, 0. The
curves are shown for the indicated initial energies (from Knoll 2000)....................
26
Figure 2.9. Collimator Line Spread Function (LSF). The full-width-at-half-maximum
(FWHM) of the line spread function (LSF) gives the resolution of the collimator (from Bushberg
etal. 2002)..................................................................
29
Figure 2.10. Collimator Line Spread Function. The diagram shows the line spread function
(LSF) of a parallel-hole collimator as a function of source-to-collimator distance. The width of
the LSF increases with distance. Nevertheless, the area under the LSF (total number of counts)
does not decrease significantly with distance (from Bushberg et al. 2002).................
30
Figure 2.11. 99 mTc and 12I Energy Spectra. The graph shows a sample energy spectrum
indicating detected scattered, unscattered, and total Tc-99m and 1231 photons. The graph also
indicates the photo-peak energy windows for 99mTc (129-148 keV) and 123I (148-175 keV)
(from Du et al. 2003)......................................................
40
Figure 3.1. CT Images of the NCAT Phantom. Left: Coronal section. Middle: Transverse
section. Left: Sagittal section.................................................
43
Figure 4.1. Single-Isotope and Dual-Isotope Projection Data. The top and bottom rows give
the 99mTc-MDP and 23I1-MIBG projection data, respectively. The left and right columns show the
single-isotope and dual-isotope data, respectively. All images correspond to the same projection
angle....................................................................
49
Figure 4.2. Comparison of Reconstructed Images After Three Iterations. The top
bottom rows give the 99mTc-MDP and 123I-MIBG reconstructed data, respectively. The left
right slices correspond to the SI-OSEM and MC-JOSEM reconstructions, respectively.
images correspond to the same transverse slice in the reconstructed data..................
7
and
and
All
50
Figure 4.3. Comparison of SNR of Lesions in 99 mTc-MDP Reconstructed Images After
Three Iterations. The blue striped and red diamonds bars correspond to SI-OSEM and MC52
JOSEM, respectively...........................................................
Figure 4.4. Comparison of SNR of Lesions in
1 23
1-MIBG Reconstructed Images After Three
Iterations. The blue striped and red diamonds bars correspond to SI-OSEM and MC-JOSEM,
52
respectively ..................................................................
8
List of Tables
Table 3.1. Relative Activity Concentration for Different Body Parts ............................
43
Table 3.2. Ratio of Tumors Maximum SUV (Lesions Present) to Mean Background SUV (Lesion Absent) at
Same Location in Lesion-Absent Data .................................................
45
9
1
Introduction
Neuroblastoma is the most common extracranial solid cancer in childhood and the most
common cancer in infancy (Gelfand 1993). This disease frequently metastasizes to bone marrow
(most likely), liver and other organs. Precise staging of the disease is essential to ensure the most
appropriate treatment plan. The current battery of imaging tests for staging and re-staging
combines separately acquired 99mTc-methylene diphosphonate (99mTc-MDP) scintigraphy,
1231_
metaiodobenzylguanidine (12 3I-MIBG) scintigraphy, and computed tomography (CT) imaging.
Planar scintigraphy images, which cannot be anatomically co-registered to CT, have low spatial
resolution and do not provide precise anatomic localization, resulting in lower sensitivity for
lesion detection as compared to tomographic imaging techniques. Although not as frequent as
scintigraphy imaging, separately acquired
99mTc-MDP
and
123 I-MIBG
single photon emission
computed tomography (SPECT) are also used to image neuroblastoma patients. Although current
clinical approaches offer high sensitivity and specificity for imaging primary and metastatic
deposits of neuroblastoma, it is desirable to reduce the number of scans for each staging and restaging because 75% neuroblastoma cases are diagnosed in children of five years-old or younger,
and these children typically require sedation or general anesthesia during imaging.
Simultaneous acquisition of 99mTc-MDP/l 23I-MIBG SPECT has the potential of halving
the imaging time, avoiding repositioning of the patient and multiple sedations, and yielding
perfectly registered MDP and MIBG images. However, simultaneous
challenging because of the crosstalk between the
down-scatter of
123I
photons (159keV) to the
99mTc
99mTc
and
1231
99mTc/ 2 31
imaging is
photo-peak windows due to
(140keV) photo-peak window and limited
energy resolution of the scanner. Additionally, the counts of detected photons are limited
10
because the injection dose as well as scan time are limited for neuroblastoma patients and scan
12 3 I-MIBG
acquisition cannot be performed for at least 24 hours after
injection.
A fast Monte Carlo based joint ordered-subset expectation maximization (MC-JOSEM)
reconstruction algorithm has been developed for simultaneous
99mTc/12 3
1
imaging (Ouyang, El
Fakhri, and Moore 2007). In MC-JOSEM, two photo-peak projections at 129-148 keV and
148-175 keV are first used to reconstruct initial
99mTc
and
123I
images, respectively, using
standard OSEM, while modeling the attenuation map and the detector point spread function
(PSF) in both the projector and back-projector. The scatter and crosstalk contributions to all
energy windows are then estimated using a fast MC algorithm while using as starting images the
99mTc and 1231 images reconstructed with standard OSEM. The estimation of the scatter and
crosstalk contributions is included when forward-projecting to preserve Poisson statistics.
Finally, JOSEM is used to reconstruct both 99mTc and
123I
images from both energy windows.
MC-JOSEM incorporates attenuation into a full system matrix to greatly improve image
accuracy and include both primary and scattered photons in the reconstruction process to
significantly reduce image noise. The objective of this thesis is to perform separate
and
123 I-MIBG
99mTc-MDP
Monte Carlo simulations and compare the lesion detectability of mimicked dual-
isotope images reconstructed using MC-JOSEM to the lesion detectability of sequential singleisotope images.
11
2
Literature Review
2.1
Nuclear Medicine Imaging Overview
Nuclear medicine imaging is based on detecting nuclear radiation emitted from the body
after injecting a radiolabeled biomolecule (radiopharmaceutical)into the body to tag a specific
biochemical function. Nuclear medicine imaging produces images of the distribution of
radionuclides in patients. To form a projection image, an imaging system must determine not
only the photon flux density (number of y-rays per unit area) at each point in the image plane,
but also the directions of the detected photons (Cho, Jones, and Singh 1993; Webb 1988). In xray transmission imaging, the primary photons travel known paths diverging radially from a
point (the focal spot of the x-ray tube). In contrast, the y-rays from the radionuclide at each
portion of a patient are emitted isotropically (equally in all directions) (Cho, Jones, and Singh
1993). Nuclear medicine instruments designed to image y-ray-emitting radionuclides use
collimators that permit photons following certain trajectories to reach the detector but absorb
most of the rest. A heavy price is paid for using collimation: the vast majority (typically well
over 99.95%) of emitted photons are wasted (Bushberg et al. 2002). Thus, collimation severely
limits the performance of these devices.
The earliest successful nuclear medicine imaging device, the rectilinear scanner, which
dominated nuclear imaging from the early 1950s through the late 1960s, used a single moving
radiation detector to sample the photon fluence at a small region of the image plane at a time.
This limitation was improved upon by the use of a large-area position-sensitive detector (a
detector indicating the location of each interaction) to sample simultaneously the photon fluence
over the entire image plane. The Anger scintillation camera, which currently dominates nuclear
12
imaging, is an example of the latter method. The scanning detector system is less expensive, but
the position-sensitive detector system permits more rapid image acquisition and has replaced
single scanning detector systems (Bushberg et al. 2002). Nuclear imaging devices using gasfilled detectors (such as proportional counters) have been developed. Unfortunately, the low
densities of gases, even when pressurized, yield low detection efficiencies for y-ray energies
commonly used in nuclear imaging. To obtain a sufficient number of interactions to form
statistically valid images without imparting an excessive radiation dose to the patient, nearly all
nuclear imaging devices in routine clinical use utilize solid inorganic scintillators as detectors
because of their superior detection efficiency (Bushberg et al. 2002). The attenuation of x-rays in
the patient is useful in radiography and fluoroscopy, and, in fact, is necessary for image
formation. However, in nuclear imaging, attenuation is usually a hindrance because it causes a
loss of information and, especially when it is very non-uniform, it is a source of artifacts (Cho,
Jones, and Singh 1993).
In general, nuclear medicine imaging may be divided into three categories: (i) planar
imaging, (ii) single photon emission computed tomography (SPECT), and (iii) positron emission
tomography (PET). This thesis focuses on SPECT; hence, the other two modalities will not be
discussed.
2.2
SPECT
Single Photon Emission Computed Tomography (SPECT) is one of the major methods
used to assess physiological function by visualizing and analyzing the 3D special distribution of
radiopharmaceuticals in patients. SPECT, as its first three initials imply, is based on the detection
of single gamma photons that are emitted from a radiopharmaceutical. These photons are
13
generally in the energy range of several tens to a few hundred keV. Because a
radiopharmaceutical concentrates in regions in which it undergoes biological use, SPECT is
capable of measuring quantitatively biological and metabolic functions in the body. Therefore,
SPECT images mainly portray functional properties of organs and tissues. For example, SPECT
is able to non-invasively measure organ perfusion, metabolic function, receptor density and drug
delivery. Important clinical areas for SPECT imaging are oncology, neurology, and cardiology.
For instance, in oncology, SPECT is used to detect tumors. The radiopharmaceuticals are
generally administered to the patient by injection; afterwards, tomographic images can be
reconstructed from projection data acquired at discrete angles around the patient. The quality of
the reconstructed SPECT image is degraded by factors such as photon attenuation, collimator
blurring and the detection of scattered photons. Most SPECT studies only give functional data, in
contrast to x-ray computed tomography (CT), which primarily produces images of anatomical
structures in the human body. Therefore, it is useful to combine SPECT with transmission CT.
SPECT-CT combines the functional data from SPECT with the high-resolution anatomical detail
from a multi-slice diagnostic CT scanner.
2.2.1
Designs and Principles of Operation
SPECT generates transverse images depicting the distribution of Y-ray-emitting nuclides
in patients. Standard planar projection images are acquired from an arc of 1800 (most cardiac
SPECT) or 360* (most non-cardiac SPECT) about the patient (Bushberg et al. 2002). Although
any collimated imaging device could obtain these images, the vast majority of SPECT systems
use one or more scintillation camera heads that revolve about the patient. The SPECT system's
digital computer then reconstructs the transverse images, using either filtered back-projection or
14
iterative reconstruction methods, which are described later. Figure 2.1 shows a multi-head
SPECT-CT system.
Figure 2.1. Siemens Symbia T6 SPECT-CT Scanner. The Symbia TruePoint SPECT-CT combines
variable angle dual-detector SPECT with 6-slice CT for rapid, accurate attenuation correction, precise
localization, and advanced CT applications in cardiology, oncology, and neurology. Source: Siemens
Global Website: www.medical.siemens.com.
2.2.2
Image Acquisition
The detector heads of a SPECT system revolve about the patient, acquiring projection
images from evenly spaced angles. The heads may acquire the images while moving
(continuous acquisition) or may stop at predefined angles to acquire the images ("step and
shoot" acquisition). For an overview of the modes of image acquisition, see Bushberg et al.
(2002). If the detector heads of a SPECT system produced ideal projection images (i.e., no
attenuation by the patient and no degradation of spatial resolution with distance from the
15
camera), projection images from opposite sides of the patient would be mirror images and
projection images over a 1800 arc would be sufficient for transverse image reconstruction
(Bushberg et al. 2002). However, in SPECT, attenuation greatly reduces the number of photons
from activity in the half of the patient opposite the camera head, and this information is greatly
blurred by the distance from the collimator. Therefore, for most non-cardiac studies, such as a
tumor scan, the projection images are acquired over a complete revolution (360*) about the
patient.
The camera heads on older SPECT systems followed circular orbits around the patient
while acquiring images. Circular orbits are satisfactory for SPECT imaging of the brain, but
cause a loss of spatial resolution in body imaging because the circular orbit causes the camera
head to be many centimeters away from the surface of the body during the anterior and posterior
portions of its orbit, as shown in Figure 2.2.
A
Circula orbit
Body contour orbit
B
Figure 2.2. (A) Circular and (B) body-contour orbits in SPECT (from Bushberg et al. 2002)
Newer SPECT systems provide noncircular orbits (also called "body contouring") that
keep the camera heads in close proximity to the surface of the body throughout the orbit. For
some systems, the technologist specifies the noncircular orbit by placing the camera head as
16
close as possible to the patient at several angles, from which the camera's computer determines
the orbit. Other systems perform automatic body contouring, using sensors on the camera heads
to determine their proximity to the patient.
2.2.3
Gamma Camera
A SPECT scanner uses a gamma camera to detect the photons emitted from the
radiopharmaceutical. The modem gamma camera, shown in Figure 2.3, consists of a collimator,
a large-area NaI(Tl) crystal, a light guide for optically coupling the photomultipliers to the
crystal and circuits for position encoding and pulse-height analysis. A lead shield surrounds the
entire camera in order to prevent the measurement of background radiation from outside the field
of view of the camera. Most SPECT systems consist of one or more gamma cameras which are
mounted on a frame in such a way that they can rotate around the patient. The data required for
the reconstruction of the source distribution are obtained by the acquisition of planar gamma
camera images at a sufficient number of angles around the patient. Because of the large field of
view of these scintillation cameras (typically 40x50 cm), a large part of the patient can be
examined in one scan. Since the scintillation detectors used in this modality are incapable of
determining the direction of the incoming photons, SPECT system cameras are always provided
with a collimator. A collimator is usually a slab of lead with several tens of thousands of holes
covering the entire detector surface. These holes are typically a few centimeters long and a few
millimeters in diameter. Since few photons are able to traverse the lead, it is mainly the photons
traversing the holes that are detected. The elongated geometry of the holes ensures that the
direction of the detected photons is well determined. This information is essential in order to
reconstruct the distribution of the radiopharmaceuticals.
Unfortunately, this directional
information is achieved at great cost, namely a tremendous loss of sensitivity (number of
17
detected photons). The typical sensitivity of a gamma camera is about 5x 104, meaning that 5 out
of 10,000 emitted photons will actually traverse the collimator and be detected (Bushberg et al.
2002; Cho, Jones, and Singh 1993; de Jong 2001; Webb 1988). Accordingly, as aforementioned,
collimation severely limits the performance of these devices, and is the major reason why
counting statistics in SPECT images are poor.
Analog Vo~tag puls to 0Mur sntai*
Pm
PMT
PMT
P"m
PMT
PMT
I
Pm
PMT
PMT
~
PMT
tube
Ludb "g
-0
Figure 2.3. Gamma Camera. This schematic shows a NaI(Tl) crystal scintillation camera detector. A
scintillation camera contains a disk-shaped or rectangular thallium-activated sodium iodide, NaI(TI),
crystal, typically 0.95-cm thick, optically coupled to a large number (typically 37 to 91) of 5.1- to 7.6-cm
diameter photomultiplier tubes (PMTs). The PMT are connected to pre-amplifiers that connect to a circuit
that analyze the data (position encoding and pulse-height analysis) (from Bushberg et al. 2002).
2.2.4
Scintillation Detection
Scintillation detection is currently the main technique for y-radiation detection in nuclear
medical imaging. It is based on the emission of visible or near-visible light from scintillation
crystals when energy is absorbed from ionizing radiation. This emission of light is a result of
inelastic collisions between secondary electrons and other atomic electrons. The photomultiplier
tubes amplify the light and convert it into electrical pulses.
A property of many inorganic scintillators is that the light emission is proportional to the
18
energy deposit in the material. This property allows measuring the energy of the detected
photons. A typical value of the energy resolution of scintillation detectors used in modem
gamma cameras is about 10% for photon energies of 100-200 keV (Phelps and Sorenson 1987).
Therefore, one can discriminate (only to a limited extent) by applying a photo-peak window,
between unscattered photons (primaryphotons) and photons that have scattered and have thereby
lost energy. The width of this window is normally 15-20% of the photo-peak energy. Hence, a
large fraction of primary photons can be collected, but a significant part of the photons detected
in the photo-peak window have undergone scattering.
2.2.5
Collimation
To filter further the scattered photons, gamma cameras use collimators. The collimator of
a scintillation gamma camera forms the projection image by permitting y-ray photons
approaching the camera from certain directions to reach the crystal, while absorbing most of the
other photons. Collimators are made of high atomic number, high-density materials, usually lead.
Because each clinical study has different requirements for field of view (FOV), the choice of
radiopharmaceutical and associated dose, the best method for collimation differs for each type of
study. Therefore, several types of collimators have been developed to achieve an adequate
compromise between spatial resolution, sensitivity and accuracy. The most commonly used
collimator is the parallel-hole collimator, which contains thousands of parallel holes. This
collimator is suitable for almost all studies and permits the use of relatively simple and fast
reconstruction techniques, and will be the one used for this study. Other collimator types include
fan-beam, cone-beam and pinhole collimators.
19
2.3
Image-degrading Effects in SPECT
The detection of photons in SPECT is seriously affected various factors: photon
interactions with atoms inside the patient (photon attenuation and scattering), or with atoms of
the detector crystal (mainly Compton scattering and photoelectric effect); inaccuracy of the
collimator (collimator blurring); and noise (mainly due to the Poisson nature of the photon
emissions) (Bushberg et al. 2002; de Jong 2001). Accordingly, it is very difficult to obtain high
quality and quantitatively accurate SPECT images. As will be shown in the following
subsections, each factor is a well-understood physical phenomenon, and therefore corrections
can be made for each of these image-degrading effects during reconstruction.
2.3.1
Photon Interactions with Matter
An important image degrading effect in SPECT is the interaction of photons with tissue.
Scatter results in the detection of 'incorrect' photons and is also the cause of the attenuation
effect. These effects are explained in Figure 2.4.
A photon can penetrate matter without interaction, it can be absorbed and it can scatter
and thereby lose a certain amount of energy. If a photon is scattered and then detected in the
photo-peak energy window, this may lead to detection at a detector position that suggests an
incorrect emission point. Scattering causes severe degradation of the contrast and quantitative
accuracy of the reconstructed image if scatter events are not corrected for.
Mainly four processes describe the interactions of photons with matter: Rayleigh
scattering, photoelectric effect, Compton scattering, and pair production (Phelps 1987; Shultis
and Faw 2008). Each process occurs with a probability that strongly depends on parameters like
photon energy, the electron density of the material or the differential cross-section per atom. The
total probability for the occurrence of any of the processes is therefore the sum of the cross-
20
sections for the different processes. An easier way of analyzing the probabilities of interactions
(and cross-sections) is by analyzing the linear or mass attenuation coefficients, both of which are
c~
sc
amp pMWkMW
r In Pad"t
I
I
Figure 2.4. Ways that Photons Interact with a Scintillation Camera. All of these, other than the ones
depicted in the upper left, cause a loss of contrast and spatial resolution. However, interactions by photons
that have scattered though large angles and many coincident interactions are rejected by pulse height
discrimination circuits (from Bushberg et al. 2002).
directly proportional to the cross-section (Shultis and Faw 2008). For more information about
cross-sections and attenuation coefficients, see Knoll (2000), Sultis and Faw (2008), and
Bushberg et al (2002). Figure 2.5 shows the mass-attenuation coefficient for soft tissue (Z=7) of
the aforementioned interactions and the total mass attenuation coefficient. From Figure 2.5, it is
21
clear that, for photons with energy of 50-1000 keV, the most probable interaction process is
Compton scattering. In heavier materials such as the collimator lead and detector crystal, and at
low energies, below 100 keV, photoelectric absorption also becomes significant. Therefore, only
Compton scattering and photoelectric absorption need to be modeled for an accurate description
of photon interaction in SPECT.
10
3
-
0
0
E
C
S
0
0.3
0
0.1
/Total
Photoelectrc
0
0.03
0.01
0.003
0.001
I
RleighCopn
-
10
-
-
-
-
1,000
10
-a-r
10,000
Energy (keV)
Figure 2.5. Mass Attenuation Coefficient as a Function of Energy. This graph shows the Rayleigh,
photoelectric, Compton, pair production, and total mass attenuation coefficients for soft tissue (Z=7) as a
function of energy (from Bushberg et al. 2002).
The Photoelectric Effect
In the photoelectric effect, a photon undergoes an interaction with an absorber atom in
22
which the photon completely disappears. The energy of the photon is transferred completely to
the atomic electron. If the photon's energy is higher than the binding energy of the electron, the
photoelectron can be ejected from the electron shell. The photon interacts with the atom as a
whole and cannot take place with free electrons (Knoll 2000). For y-rays of sufficient energy, the
most probable origin of the photoelectron is the most tightly bound or K shell of the atom. The
kinetic energy of the ejected photoelectron (Ee) is given by
Ee = hv - Eb,
(1)
where Eb represents the binding energy of the electron and hv is the energy of the incoming
photon. For y-rays with energy more than a few hundred keV, the photoelectron carries off the
majority of the original photon energy.
(
Binding Energy (keV)
skeVPhoolctron
A
100 keV
B
photon
C
A: 0.6 keV (N-+M)
X1<4 < X
<X
B: 4A keV (M-L)
C: 29 keV (L -K)
Figure 2.6. Photoelectric Effect. Left: The diagram shows a 100-keV photon is undergoing photoelectric
absorption with an iodine atom. In this case, the K-shell electron is ejected with a kinetic energy equal to
the difference between the incident photon energy and the K-shell binding energy of 34: 66 keV. Right:
The vacancy created in the K shell results in the transition of an electron from the L shell to the K shell. The
difference in their binding energies, (i.e., 34 and 5 keV), results in a 29-keV K, characteristic x-ray. This
electron cascade will continue resulting in the production of other characteristic x-rays of lower energies.
Note that the sum of the characteristic x-ray energies equals the binding energy of the ejected
photoelectrons. Although not shown on this diagram, Auger electrons of various energies could be emitted
in lieu of the characteristic x-ray emissions (from Bushberg et al. 2002).
23
The ejection of a photoelectron causes a vacancy in the electron shell. An electron from a
shell with a lower binding energy will fill this vacancy. This creates another vacancy, which, in
turn, is filled by an electron from an even lower binding energy shell. Thus, an electron cascade
from outer to inner shells occurs. The difference in binding energy is released as either
characteristic x-rays or auger electrons. The photoelectric effect and subsequent characteristic xray emission is summarized in a schematic in Figure 2.6. Characteristic x-ray emission is more
probable for high-Z materials, such as lead (Pb-82). The binding energy of the lead K-shell is
88 keV and the energies of the relevant characteristic x-rays (Pb x-rays) are 75 keV, 73 keV and
85 keV. For instance, this can result in the absorption of a 140 keV causing the emission and
possible detection of an x-ray with much lower energy.
Compton Scattering
Compton scattering occurs when an incident photon interacts with an orbital electron,
producing a scattered photon of lower energy and a free recoil electron (Knoll 2000). This
interaction is most likely to occur between photons and outer (valence) shell electrons, as seen in
Figure 2.7. The electron is ejected from the atom, and the photon is scattered with some
reduction in energy.
As with all types of interactions, both energy and momentum must be conserved. Thus
the energy of the incident photon (E0 ) is equal to the sum of the energy of the scattered photon
(Esc) and the kinetic energy of the ejected electron (E,_):
E0 = Esc + Ee..
(2)
The binding energy of the electron that was ejected is comparatively small and can be ignored.
Compton scattering results in the ionization of the atom and a division of the incident photon
energy between the scattered photon and ejected electron. The ejected electron will lose its
24
C~p~nSo.UU~O
Voko00 W0Fone
0.
initphotona.2
Figure 2.7. Compton Scattering. The diagram shows the incident photon with energy E0, interacting with
a valence shell electron that results in the ejection of the Compton electron (E,) and the simultaneous
emission of a Compton scattered photon (E,,) emerging at an angle, 0, relative to the trajectory of the
incident photon. K, L, and M are electron shells (from Bushberg et a. 2002).
kinetic energy via excitation and ionization of atoms in the surrounding material. The Compton
scattered photon may traverse the medium without interaction or may undergo subsequent
interactions such as Compton scattering, photoelectric absorption, or Rayleigh scattering. The
Compton scattered photon is scattered by an angle 6 relative to its incident direction and loses
energy, which is then transferred to the electron. The scattered photon energy (Ese) is given by
Esc =
1+
E,
E
,
" 22 (1 - cos 0)
moC
25
(3)
where E, is the incident photon energy and moc 2 is the rest mass of the electron. From Eq. 3, it is
evident that the maximum amount of energy is transferred to the electron when the photon is
backscattered (0 = 1800) and that little energy is lost by the photon when 0 ~ 0*.
go.
Figure 2.8. Compton Scattering Probabilities. This is a polar plot of the number of photons (incident
from the left) Compton scattered into a unit solid angle at the scattering angle, 0. The curves are shown for
the indicated initial energies (from Knoll 2000).
The angular distribution can be described by the Klein-Nishina formula, which relates the
differential cross-section, or scatter probability, to the scatter angle. As the incident photon
26
energy increases, both scattered photons and electrons are scattered more toward the forward
direction, as seen in Figure 2.8. A comprehensive description of Compton scatter is given in
Knoll (2000).
Compton scattering is the predominant interaction of x-ray and y-ray photons with soft
tissue in the diagnostic energy range. In fact, Compton scattering not only predominates in the
diagnostic energy range above 26 keV in soft tissue, but also continues to predominate well
beyond diagnostic energies to approximately 30 MeV.
Attenuation
Attenuation is the removal of photons from a beam of x- or y-rays as it passes through
matter. Attenuation is caused by both absorption and scattering of the primary photons. The
interaction mechanisms discussed previously contribute in varying degrees to the attenuation. At
low photon energies (less than 26 keV), the photoelectric effect dominates the attenuation
processes in soft tissue. However, as previously discussed, photoelectric absorption is highly
dependent on photon energy and the atomic number of the absorber. When higher energy
photons interact with low-Z materials (e.g., soft tissue), Compton scattering dominates
(Figure 2.5). Attenuation depends on the total length of the tissue that has to be traversed and on
the type of tissue involved. The attenuation of a narrow beam of photons passing through a nonhomogeneous medium of thickness d is given by
=
e
ef
(r)dr
(4)
where ip is the photon flux after attenuation,*, is the incident photon flux and i(r) is the linear
attenuation coefficient (the total sum of all possible differential cross-sections). For water, the
linear attenuation coefficient, pU, is approximately 0.152 cmf for 140-keV y-rays (Manglos et al.
1987).
27
As mentioned before, the attenuation of x-rays in the patient is useful in radiography and
fluoroscopy, and, in fact, is necessary for image formation. However, in nuclear imaging,
attenuation degrades the image because it causes loss of information and artifacts if not corrected
properly (especially when it is very non-uniform). In standard SPECT scanning, the attenuation
coefficients are obtained by a separate transmission measurement using an external source of yrays. In SPECT-CT scanning, the attenuation coefficients are measured with x-ray transmission;
the attenuation coefficients for the lower-energy x-rays are remapped to estimate the values for yrays.
2.3.2
Collimator Blurring
Because collimator holes are not infinitely narrow, the photons that traverse the
collimator will not all come from a direction that is exactly aligned with the holes. This leads to a
substantial loss of resolution in the gamma camera images and in the reconstructions. The
acceptance angle of a collimator is defined by the fraction of the size of the hole and its diameter.
Although decreasing the acceptance angle would decrease the collimator blurring, it would also
greatly decrease the sensitivity of the collimator. It can be shown that a twofold increase of the
collimator resolution would decrease the sensitivity by a factor of about four (Metz, Atkins, and
Beck 1980). Therefore, a compromise has to be found between collimator resolution and
sensitivity, and this is the single most significant limitation on scintillation camera performance
(Bushberg et al. 2002).
The collimator resolution can be measured by the line-spreadfunction(LSF) formed by a
line source at a distance, and is defined to be the full-width-at-half-maximum (FWHM) of the
LSF (see Figure 2.9). The collimator's resolution, when corrected for magnification, is degraded
(FWHM of the LSF increases) as the collimator-to-object distance increases (Cho, Jones, and
28
Singh 1993). Therefore, it is important to position the camera as close as possible to the patient
(see Figure 2.10).
Projmme01 radsont
III
III
Figure 2.9. Collimator Line Spread Function (LSF). The full-width-at-half-maximum (FWHM) of the
line spread function (LSF) gives the resolution of the collimator (from Bushberg et al. 2002).
In 2D, the LSF becomes the point-spreadfunction (PSF). The PSF has the same
properties of the LSF, but the mathematical operations are performed in two dimensions.
Accurate mathematical descriptions of collimator blurring, efficiency, and resolution can be
found in Bushberg et al. (2002); Cho, Jones, and Singh (1993); Metz, Atkins, and Beck (1980);
and Tsui and Simmons (1988).
29
11s Amd0In
vdraW
I
Lwsumce
Figure 2.10. Collimator Line Spread Function. The diagram shows the line spread function (LSF) of a
parallel-hole collimator as a function of source-to-collimator distance. The width of the LSF increases with
distance. Nevertheless, the area under the LSF (total number of counts) does not decrease significantly with
distance (from Bushberg et al. 2002).
2.3.3
Poisson Noise
The emission of photons in radioactive decay is a Poisson distribution process. This fact
implies that the measurements of the projections also include Poisson noise. Since the variance
of Poisson noise is proportional to the mean activity, the acquisition of a high number of counts
will increase the signal-to-noise ratio. However, the counts are small in SPECT, in part because
of the isotropic nature of radioactive decay, and because of the sensitivity and efficiency of the
detector. Decreasing the duration of the scan decreases costs, patient discomfort and the
possibility of patient movement. Decreasing the radiation dose also decreases costs and patient
discomfort. Hence, for financial and health reasons, the quality of a SPECT image is minimized
to the point were interpretation becomes questionable ('As Low As Reasonable Achievable').
Therefore, a low signal-to-noise ratio is inherent to a SPECT image and noise thus is major cause
30
of image degradation (de Jong 2001).
2.3.4
Other Image-Degrading Effects
Other instrumentation-related processes influencing the quality of SPECT images are
nonlinearities and non-uniformities of the detector and inaccuracy of the center of rotation of the
detector. Correction methods for these effects exist. Therefore, their influence is relatively small
compared to effects of collimator blurring, photon scattering and Poisson noise. Finally, image
quality can be significantly affected by biological factors such as tracer kinetics and target
specificity, and by patient and/or organ movement during image acquisition.
2.4
SPECT Monte Carlo Simulation
Since the processes involved in SPECT (gamma radioactive decay and subsequent
photon interactions with matter) are stochastic in nature, Monte Carlo (MC) methods are used to
simulate SPECT. MC methods are a class of computational algorithms that rely on repeated
random sampling to compute their results. MC simulation can be described as a statistical
simulation method based on random sampling of probability density functions (PDF). For
example, such a PDF(x) can describe the photon path length x up to the next interaction with
matter. MC simulation was first used during the World War II Manhattan project. Von Neumann
named it Monte Carlo simulation because of the similarity between statistical simulation and
games of chance, and because the city in the principality of Monaco was a center for gambling
(Zaidi 1999).
Constructing a cumulated probability density function (CPDF(x)) allows sampling
a PDF(x), normalized by integration over its definition range [a, b]:
31
CPDF(x) = fXPDF(x')dx'.
(5)
A random variable x can be sampled by substituting a random number in the range of
[0,1) for CPDF(x) and solve the equation for x. If PDF(x) is analytically integrable, x can be
sampled in a straightforward manner. Often the PDF(x) is too complex to allow analytic
integration, as in the case of the Klein-Nishina formula which describes the probability of
Compton scattering over angle 0. In such cases, the CPDF(x) can be described numerically. An
overview of the MC method and its applications to SPECT scatter simulation are given in
Raeside(1976); Ljungberg, Strand, and King (1998); and Zaidi (1999).
2.4.1
GATE Program for SPECT Simulation
In nuclear and high-energy physics, one of the most used MC methods is Geant4 (for
GEometry ANd Tracking), a platform for the simulation of the passage of particles through
matter. Geant4 includes facilities for handling geometries, tracking, detector response, run
management, visualization, and user interface. More specific Geant4 applications have been
developed for emission tomography studies: the GATE (Geant4 Application for Tomographic
Emission). GATE combines a powerful simulation core, the Geant4 toolkit, with newly
developed software components dedicated to nuclear medicine. In particular, it models the
passing of time during real acquisitions, allowing it to handle dynamic systems such as decaying
source distributions or moving detectors.
2.4.2
Computational Human Phantoms
Computational human phantoms are models of the human body used in computerized
analysis. Since the 1960s, the radiological science community has developed and applied these
models for ionizing radiation dosimetry studies. These models have become increasingly
accurate with respect to the internal structure of the human body. As computing evolved, so did
32
the phantoms: phantoms based on simple quadratic equations evolved to voxelized phantoms,
which were based on actual medical images of the human body. The newest models are based on
more advanced mathematics, such as Non-Uniform Rational Basic-Splines (NURBS) and
polygon meshes, which allow for 4D phantoms, where simulations can take place not only in
3-dimensional space, but also in time. Phantoms have been developed for a wide variety of
humans, from children to adolescents to adults, male and female, as well as pregnant women.
With such a variety of phantoms, many kinds of simulations can be run, from dose received from
medical imaging procedures to nuclear medicine simulations.
William P. Segars (2002) created the NURBS-based cardiac-torso (NCAT) phantom that
is based on digitized CT acquisitions of normal patients. The flexibility of the anthropomorphic
NCAT phantom allows researchers to generate realistic simulations of patients characterized by
different size, weight, and individual organ sizes.
2.4.3
SPECT Reconstruction
The purpose of tomographic reconstruction is to obtain cross-sections of an object from
projections of that object. Two different approaches are commonly used for reconstruction in
SPECT. Until recently, filtered back-projection (FBP) was the universal method because of its
simplicity and speed. Iterative reconstruction techniques permit the modeling of all imagedegrading factors and are therefore more accurate, but require much longer computation time.
The acceleration that has been accomplished for these techniques over the last decade has
brought them into the range of clinical application.
Iterative Reconstruction
Iterative reconstruction algorithms estimate projection data by means of a forward
projector, using an initial estimate of the activity distribution. These calculated projections are
33
compared to the measured projections. On the basis of this comparison, one can obtain a better
estimate of the image using an update step. This process of forward projection, comparison and
updating can be iterated until an acceptable image is obtained (de Jong 2001). The transition
matrix that is used in the iterative algorithm represents the model of forward projection. The
more accurate this transition matrix is modeled, the better the agreement will be between the
estimated images and the real activity distribution.
SPECT projection data are severely affected by Poisson noise, which implies that lowpixel-count values give a less accurate prediction of the time-average photon flux received in the
pixel. A possible way to model the Poisson nature of the measurements is to treat the data as
stochastic variables and not as exact measurements; noise-free projections are taken as the mean
of the Poisson distributions. Calculating the maximum likelihood estimate of the emission
distribution that generated the measured projections takes into account the Poisson nature of the
projections. Without making any a priori assumptions about the activity distribution, the
statistically most likely emission distribution can be calculated using the maximum likelihood
expectation maximization (MLEM) algorithm (Dempster, Liard, and Rubin 1977; Lange and
Carson 1984; Shepp and Vardi 1982). The MLEM algorithm updates all image elements i of the
estimated image at iteration k + 1 according to
~k+1
=
__
cJp;j
(5)
Z j ci; ZJ Zi ci;\(5
where Ak represents the kth image estimate, C = {cij} represents the transition matrix, P = {p;}
represents the measured data, and
ZE
cijl4 is the projection bin j after forward projection of the
k-th image estimate.
This algorithm has the following important properties: (i) in every iteration, the algorithm
increases the likelihood that the image estimate will generate the measured data (according to the
34
transition matrix used); (ii) image elements in each iteration are constrained to remain positive;
(iii) the algorithm takes into account the Poisson nature of the noise in the projection data. These
features of the MLEM algorithm lead to images that are less noisy than images reconstructed
using FBP (de Jong 2001).
A drawback of MLEM is that reconstruction is extremely slow, especially when accurate
transition matrices are used. In order to render MLEM fast enough to be used in a clinical
setting, the scheme is often accelerated, for example using block iterative methods like the
ordered subsets expectation maximization (OSEM) algorithm of Hudson and Larkin (1994),
which has become the standard clinical iterative reconstruction algorithm. OSEM involves
grouping projection data into an ordered sequence of sub-sets. The EM algorithm is then applied
to each subset, and the result is used as the starting estimate for processing the next estimate. It
has been shown that OSEM can reach acceleration factors that are close to the number of subsets
used (Hudson and Larkin 1994; Kamphuis, Beekman, and Viergever 1996), while achieving
image quality that is similar to standard MLEM. An additional decrease of the reconstruction
time can be achieved using a less complex transition matrix for the update step than for the
forward projection step (Kamphuis et al. 1998). This approach is also known as the dual-matrix
method. Overviews of accelerated EM algorithms are given in Hutton, Hudson, and Beekman
(1997), and Leahy and Qi (2000).
Calculation of the Transition Matrix
The transition matrix describes the forward projection and re-projection used in iterative
SPECT reconstruction. The generation of an accurate transition matrix requires an accurate
method for calculating photon transport in SPECT and an estimate of the density distribution of
the patient, which can be represented by a transmission CT map. Acquisition of a transmission
35
CT image has become a common part of the total SPECT acquisition protocol. Other arguments
for acquisition of a transmission CT image are improved anatomical localization of activity (e.g.
in tumors and infectious foci), registration with other imaging modalities and dose calculations.
2.5
Simultaneous Dual-Isotope SPECT
As above-mentioned, in SPECT, a radiopharmaceutical is administered to the patient; it is
then distributed through the body in a way determined by the properties of that
radiopharmaceutical and by the anatomy and physiology of the patient. Sometimes, it is
important to monitor two different physiological functions or one function under different
physical or medical conditions. These assessments can be achieved by performing two
independent SPECT studies or using two different radioisotopes in a single imaging session; the
latter is called simultaneous dual-isotope SPECT. When two different radiopharmaceuticals are
used with distinguishable emission energies, the data for both tracers can also be acquired
simultaneously using different energy windows. Simultaneous acquisition of projection data
from two isotopes has the advantage that it allows measurement of two potentially related
processes at the same time. This may add additional diagnostic information and, in addition,
there are practical advantages such as shorter time needed for the study, doubled hardware
throughput, reduced patient discomfort, and common patient motion in the two studies.
Furthermore, simultaneous acquisition ensures perfect co-registration between the images for
each isotope. However, due to scatter in the patient and gamma camera and the poor energy
resolution of conventional gamma cameras, dual-isotope SPECT will result in crosstalk
contamination of the two sets of projection data.
Dual-isotope SPECT studies have a wide range of uses; these include tumor detection,
36
the
evaluation
of
myocardial
viability
and
perfusion,
and
brain
function.
The
radiopharmaceuticals used for these studies include a number of combinations, for example,
99
mTc/ 20oTl,
99
mTc/"lln 20 1T/"1 1n, 99mTc/12 31,
99mTc-MDP/1 23 I-MIBG
2.5.1
99
mTc/s"mKr,
and "F/
9
'Tc. This thesis focuses on
imaging for neuroblastoma.
Simultaneous
99
mTc/ 123 I
Neuroblastoma SPECT Imaging
Neuroblastoma is the most common extracranial solid cancer in childhood and the most
common cancer in infancy (Gelfand 1993). The most common study to detect neuroendocrine
tumors, such as pheochromocytoma
and neuroblastoma, involves the use of the 1231
metaiodobenzylguanidine ( 123 1-MIBG) in planar scintigraphy (Shapiro et al. 1985; Hoefnagel et
al. 1987; Gelfand 1993).
123 1-MIBG
scintigraphy is useful not only for identifying the primary
tumors, but also to monitor the pattern of metastatic spread (with an overall 92% sensitivity and
96% specificity) and response to treatment (Rufini, Calcagni, and Baum 2006). Neuroblastoma
frequently metastasizes to bone marrow (most likely); therefore, 99Tc-methylene diphosphonate
(9 9mTc-MDP) bone scintigraphy is used to verify tumor metastasis to the bone.
Although not as frequent as scintigraphy imaging, separately acquired
12 3
99mTc-MDP
and
I-MIBG SPECT are also used to image neuroblastoma patients. The separately-acquired
99mTc-MDP and 123I-MIBG SPECT studies are performed in several steps as follows:
(1)
Inject a dose of 99mTc-MDP (10.57 MBq/kg, minimum 185 MBq, maximum 740 MBq).
(2)
Two to three hours later, take a twenty-minute whole-body SPECT scan and a noncontrast-enhanced low-dose CT scan for attenuation correction.
37
(3)
Administer a dose of
12
I-MIBG (7.5 MBq/kg, minimum 37 MBq, maximum 370 MBq)
intravenously over 10 minutes.t
(4)
Twenty-four (24) hours later, take a twenty-minute whole-body SPECT scan and a noncontrast-enhanced low-dose CT scan for attenuation correction.:
The current clinical approaches descried above offer high sensitivity and specificity for
imaging primary and metastatic deposits of neuroblastoma, but they have many limitations.
Firstly, multiple scans are needed for each staging and re-staging work-up. These scans are
usually performed on different scanners on different days. It is desirable to reduce the number of
scans for each staging and re-staging because seventy-five percent (75%) of neuroblastoma cases
are diagnosed in children of five-years-old or younger, and these children typically require
sedation or general anesthesia during imaging (Gelfand 1993). These sedations can cause
significant stress and risk to these very young patients who have difficulty remaining motionless
during imaging. Additionally, specialized pediatric anesthesiologists and nurses are required,
which in most hospitals are a limited resource that must be shared with pediatric surgery and
other departments. There is often a long wait time to schedule pediatric sedation or general
anesthetic imaging studies due to the limited availability of these specialists. It is therefore very
desirable to acquire all three scans at the same time on the same scanner, which will minimize
the time spent in hospital, avoid repositioning the patient between scans, and eliminate the need
for multiple sedations and general anesthesia. Secondly, planar scintigraphy images, which
cannot be anatomically co-registered to CT, have low spatial resolution and do not provide
precise anatomic localization, resulting in lower sensitivity for lesion detection as compared to
t At least one week before the 123I-MIBG scan, the physicians give the parents a list of drugs known to
inhibit MIBG uptake with instructions that children should avoid them. Also, the physicians give potassium
iodide orally to the patient before the 23I-MIBG study to prevent hypothyroidism.
*Note that the patient has to go home and return during the twenty-four-hour period.
38
tomographic imaging techniques, especially for small tumors (Rufini et al. 1995). Thirdly,
because the
99
mTc-MDP,
12 31-MIBG scan, and CT scan are acquired on different days, and
usually on different scanners, any attempt to co-register their respective images for anatomic
localization would be technically difficult and inaccurate.
To reduce imaging time, sedation time, and injection dose, the patients can be imaged
3
SPECT in addition to a non-contrastusing simultaneous acquisition of 99mTc-MDP/l 21I-MIBG
enhanced CT on a combined SPECT-CT scanner. A single SPECT scan produces both
MDP and
99mTc-
12 3
I-MIBG images, which are perfectly registered and under the exact same patient
conditions. Additionally, it has the advantage that a CT scan, which is registered to the SPECT
99mTc/1231
scan, can be acquired without repositioning the patient. However, simultaneous
imaging is challenging because of the crosstalk between the 99mTc and
due to down-scatter of
1231
photons (159keV) to the
99mTc
1231
photo-peak windows
(140keV) photo-peak window and
limited energy resolution of the scanner. Additionally, the counts of detected photons are limited
because the injection dose as well as scan time are limited for neuroblastoma patients and scan
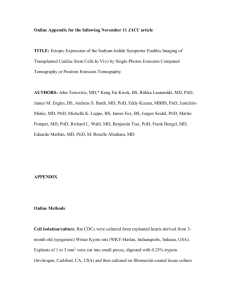
acquisition cannot be performed for at least 24 hours after 123 1-MIBG injection. Figure 2.11
shows the 99 mTc and
2.5.2
1231
energy spectra, emphasizing the photo-peak windows.
Down-scatter and Crosstalk
A major image degrading effect in dual-isotope SPECT is the appearance of photons of
one isotope in the energy window of the other isotope. In the case of simultaneous
99mTc/ 2 31
imaging, there is substantial down-scatter of 1231 photons (159keV) to the 99mTc (l40keV) photopeak window in the region of 129-148 keV. This is demonstrated by the sample
1231
energy
spectrum shown in Figure 2.11. This energy spectrum also shows the energy windows used in
this thesis. The largest component of this down-scatter is due to
39
1231
photons losing energy in
Compton scatter events in the patient. Not only are down-scattered
1231
photons detected in the
99mTc window, but also, equally importantly, primary photons of each radionuclide are detected
in the wrong window (cross talk), making challenging the energy discrimination between them
(Ouyang, El Fakhri, and Moore 2007).
Tc99m
-Unscanere
-
Tc00m photon
Scatmd Tc00 photon
1123
1123 photon
d 1123 photon
-Unscttered
-- Sc
40000
I,
I
c10
120
140
100
180
Energy (iNV)
99
mTc and 123I Energy Spectra. The graph shows a sample energy spectrum indicating
detected scattered, unscattered, and total Tc-99m and 1231 photons. The graph also indicates the photo-peak
energy windows for 99mTc (129-148 keV) and 123I (148-175 keV) (from Du et al. 2003).
Figure 2.11.
2.5.3
Image Reconstruction in Dual-Isotope SPECT
Image reconstruction in dual-isotope SPECT is rapidly evolving in the tomographic
imaging research field. Many methods for dual-isotope SPECT reconstruction have been created
40
recently, and more are being created (Ouyang et al. 2009). As stated above, the difficult parts
about simultaneous
99mTc/ 2 1
imaging are the down-scatter and cross talk between both isotopes'
energy windows. Reconstruction methods that correct for these problems have been created and
tested successfully (de Jong 2007; El Fakhri et al. 2001; de Jong 2007; Ouyang, El Fakhri, and
Moore 2007; Zheng et al. 2004). Recently, researchers have developed a reconstruction method
that incorporates a fast Monte Carlo (MC) simulation method into a joint ordered-subset
expectation maximization (JOSEM) approach, or MC-JOSEM (Ouyang, El Fakhri, and Moore
2007). The MC simulation method accurately models all physical factors involved in image
formation while also incorporating patient-specific activity distributions. Hence, MC-JOSEM
compensates simultaneously for scatter and cross talk, as well as for collimator penetration and
collimator and detector scatters (Ouyang et al. 2009).
The objective of this thesis is to compare the lesion detectability of mimicked dualisotope images reconstructed using MC-JOSEM to the lesion detectability of sequential singleisotope images.
41
3 Methods
3.1
MC (GATE) Simulation of Simultaneous
9 9 mTC/I 2 3 1
Studies
Full Monte Carlo simulations were performed using the GATE program to accurately
model
a Siemens
SPECT camera (Siemens
T6
SPECT-CT).
An NCAT phantom
(anthropomorphic digital phantom) was used to simulate realistic separate noise-free
and
12 3I-MIBG
99mTc-MDP
whole-body SPECT scans with lesions at different locations using realistic
activity distributions. These two separate SPECT scans were combined to mimic dualradionuclide SPECT scans.
3.1.1
SPECT System Specifications
Using the GATE program, a dual-head Siemens T6 SPECT-CT (see Figure 2.1) system
was modeled for the data acquisition. Each gamma camera was modeled with a Low Energy
Low Penetration (LELP) parallel-hexagonal-hole collimator with face-to-face (F2F) distance of
1.11 mm, septal thickness of 0.16 mm, and hole length of 24.05 mm. Each NaI(Tl) detector
crystal was 0.95-cm thick. The detectors have an energy resolution of 10% at 140 keV. A dualhead, fixed 1800 configuration was used. Each head rotated 1800 in 3.75* intervals, giving
48 views. Hence, there were a total of 96 projections covering a 3600 angular range for each
acquisition, and each projection was a 128x128 matrix with a pixel size of 2.7x2.7 mm2. Data
was acquired in frame mode for two energy windows: 129-148 keV, Othe
window and 148-175 keV, the
3.1.2
123
99mTc
photo-peak
photo-peak window.
NCAT Phantom Specifications
The anthropomorphic NCAT phantom was used to generate an index image, where each
tissue or organ is assigned an integer. Each index was assigned a concentration value and
42
material name (for linear attenuation coefficient), modeling the activity distributions based on
previously reported MGH clinical studies of
99 mTc-MDP
and ' 3 I-MIBG. Figure 3.1 gives
coronal, transverse, and sagittal sections of the CT images of the NCAT phantom.
Figure 3.1. CT Images of the NCAT Phantom. Left: Coronal section. Middle: Transverse section. Left:
Sagittal section.
Table 3.1 summarizes the most important tissues or organs with the appropriate relative activity
concentration of 99mTc-MDP and 12 1-MIBG. Also, five tumors were simulated inside the body,
but their activity concentrations were adjusted before reconstruction for an appropriate lesion
detectability comparison.
Table 3.1. Relative Activity Concentration for Different Body Parts
Body Part
""'Tc-MDP Relative Activity
Heart
5
Lungs
2
Liver
5
Spine
80
Kidney
5
Soft-tissue
5
3.1.3
2
1 1I-MIBG
Relative Activity
20
5
25
5
5
5
99mTc and mI SPECT Simulations
Full Monte Carlo simulations were performed to simulate
99mTc-MDP
and
2 1-MIBG
SPECT studies separately using the GATE program. The tumor simulation was also performed
43
separately. Five tumors were simulated: TI in the left lung, T2 in the liver, T3 in the spine, T4 in
soft tissue, and T5 in the pelvis. All simulations were performed with the same scan time.
Scattered photons were followed up to eight orders of scatter. Only
123
99
mTc
140-keV photons and
159-keV photons were simulated. The low-abundance high-energy mI photons above 159
keV were not simulated for simplicity. The simulations included all details of the photon
transport through the torso (using anthropomorphic attenuation values), collimator, and detector.
Compton scatter, coherent scatter, and penetration through the collimator septa, as well as
backscatter from camera components behind the NaI(Tl) crystal, were also simulated.
For each isotope, noise-free projection data sets were generated first for each of the two
energy windows. Lesions were added to the 99mTc and
were then generated by combining the 99mTc and
129-151 keV window were three times the total
123
1231
1231
data separately. Dual-isotope data
data so that the total
99 mTc
counts in the
counts in the 159-175 keV window to
mimic a clinical dual-isotope torso SPECT setting. The projections were scaled so that the total
number of
99mTc
counts in the 129-151 keV window was 12x 106, which was consistent with
statistics observed in previous patient studies. The projections were also scaled so that the lesions
were barely visible, so that a proper comparison of lesion detectability after reconstruction could
be conducted. The 99mTc-MDP dual-isotope data was generated by combining the
present data with the
123I
generated by combining the
lesion-absent data, whereas the
1231
lesion-present data with the
23 1-MIBG
99mTc
99mTc
lesion-
dual-isotope data was
lesion-absent data. Table 3.2
summarizes the maximum standardized uptake value (SUV) of each tumor relative to the mean
background SUV of the appropriate location in the reconstructed image without lesions, defined
as follows:
Ratio =
suvmax(tumor)
SUVmean(backbround)
44
Sixteen noisy data sets, consisting of 96 projections each, were generated from the
"noise-free" projections using a Poisson pseudo-random noise generator.
Table 3.2. Ratio of Tumors Maximum SUV (Lesions Present) to Mean Background SUV (Lesion
Absent) at Same Location in Lesion-Absent Data
123
I-MIBG
""'Tc-MDP
Tumor (location)
TI (left lung)
T2 (liver)
T3 (spine)
T4 (soft tissue)
T5 (pelvis)
3.2
1.92
2.78
2.70
4.26
2.63
2.39
2.71
3.30
3.33
1.77
Reconstruction Methods for Simultaneous
99
mTc/ 123 I
Studies
For each of the 16 noise realizations of the dual-isotope data and each of the sequential
single-isotope data, two reconstruction methods were implemented for comparisons:
(1)
After creating the mimicked dual-isotope data, the photo-peak-energy-window projections
(129-148 keV for 99mTc and 148-175 keV for
1231)
were reconstructed independently using
standard OSEM while modeling the attenuation map and the collimator detector PSF but
without scatter correction. The dual-isotope
99mTc
and
123
images after three iterations
were used as starting images for the fast MC algorithm to estimate scatter and cross-talk
contributions to both photo-peak energy windows. One hundred million photon histories
were generated based on these two starting images to estimate scatter contributions for each
of the 96 projection angles. Scatter maps were simulated at each projection angle for many
energy windows, denoted as object energy windows (OEWs), throughout the entire energy
spectrum for all the primary and scattered photons that have non-negligible probability of
being detected in the two detected energy windows (DEWs) used by the scanner. These
scatter maps were then blurred by the PSFs to form the projection for each DEW to obtain
§ The PSFs mentioned in the reconstruction methods are described in detail in Ouyang et al. (2009)
45
the scatter and crosstalk estimates. Then, a joint OSEM incorporating two radionuclides
and two DEWs was performed with three additional iterations for each noise realization.
The simulated PSFs and attenuation corrections were included in both the forwardprojection and back-projection. The fast MC-estimated scatter contributions, which were
calculated only once, were added to the estimates of primary photon projections during the
forward-projection step of each iteration. For the joint OSEM, each forward projection has
contributions from both isotopes, in which each back-projection has contribution from both
DEWs. This is different from the standard OSEM procedure described above, in which
only one radionuclide and one DEW are involved in the reconstruction process. This
algorithm is denoted as MC-JOSEM. The detector PSFs were simulated separately for a
sphere source in air. All the physical processes in the detector materials, including
penetration and scatter in the collimator, the NaI(Tl) crystal, and the materials behind the
crystal, were modeled. The sphere source has the same volume as a voxel (19.7 mm 3 ). The
PSFs were represented by a five-dimensional array indexed by OEW, DEW, source-tocollimator distance (32 bins from 0.2 to 48.2 cm), and a two-dimensional detector "kernel"
(2.7x2.7 mm 2 sampling). Each kernel was represented by a 63x63 pixel array; however,
only one 32x32 quadrant needed to be stored owing to symmetry.
(2)
The sequential single-isotope projections were reconstructed independently using their
respective photo-peak-energy-windows (129-148 keV for
99mTc
and 148-175 keV for
1231)
with standard OSEM while modeling the attenuation map and the collimator detector PSF
using the fast MC method for scatter correction. This is the gold standard for this study. It
will be denoted as SI-OSEM in this thesis.
46
For all reconstructions in this study, eight subsets were used with eight projections per
subset. In both the projector and back-projector, the attenuation map and the detector PSF were
modeled. The reconstructed image volume consisted of 128x128x128, 2.7-mm cubic voxels.
3.3
Lesion Detectability Comparison
The dual-isotope simulated studies were compared to the sequential single-isotope studies
on the basis of the performance of a model observer in detecting the presence of a lesion of
unknown size and shape on an anatomic background for all 16 noise realizations. The model
observer was a 3D three-channel Hotelling observer (CHO), by which a 32x32 pixel sub-image
data was processed through the frequency channels that were designed to mimic the human
visual system (Abbey and Barrett 2001). The 32x32 image corresponded to the slice with the
greatest signal from a lesion located in pixel (16,16) at the center of the image (only one lesion
was present in any 32x32 image). The CHO signal-to-noise ratio (SNR) is given by
(2)
SNCRHO = (Wf)T S2 (Af),
where, Af is the mean inter-class channel output difference vector, and S2 is the intra-class
scatter matrix, calculated from the (channelized) covariance matrices Mi and M2 of the two
classes (lesion-present and lesion-absent) being discriminated by S2
=
M1+M2
2
A three-channel (sparse) difference-of-Gaussians Hotelling observer (Abbey and Barrett
2001) was used. The (radially symmetric) channel profiles Co, C1 , and C2 were given by
1f pj
2
C(p) =e
where p is the spatial frequency,
j
2kz
1 p
2
e
2
= 1, 2, ..., N indexes the channels, a = o 2j1-,
(3)
and
ao = 0.052. The parameters of this observer model were appropriate for a viewing distance of
47
60 cm and a displayed pixel size of 0.51 mm. Doubling the diagonal elements of the channel
covariance matrix incorporated the effect of the observer noise on task performance. Since the
same images were used for both the training set and evaluation set for this study, a potential bias
in the CHO SNR estimates was introduced. Any such bias, however, was the same for both
sequential and simultaneous dual-isotope studies, and could therefore not affect the conclusions.
The lesion detectability performance estimated with the CHO, dA, can be related to the
corresponding area under the receiving operator characteristic curve (Az) by:
dA = 2 erf~ 1 (2Az - 1),
where erf-1 is the inverse error function.
48
(4)
4
Results and Discussion
4.1
MC (GATE) Simulation of Simultaneous
99
mTc/ 2 3 1
Studies
After the MC (GATE) simulation was finished, the projection data was analyzed, and the
tumors were combined with the 9 9mTc and
1231
data as aforementioned. Figure 4.1 shows single-
isotope and dual-isotope projection data for 99mTc-MDP and
123
I-MIBG.
16
12
"'"TC-MDP
4
0
16
L
12
23 1-MIBG
S
4
0
Dual-Isotope
Single-Isotope
99
Figure 4.1. Single-Isotope and Dual-Isotope Projection Data. The top and bottom rows give the mTc2
MDP and 1-MIBG projection data, respectively. The left and right columns show the single-isotope and
dual-isotope data, respectively. All images correspond to the same projection angle.
49
As shown in the images, the projections were also scaled so that the lesions were barely
visible, so that a proper comparison of lesion detectability after reconstruction could be
conducted.
4.2
Reconstruction of Simultaneous
99
mTC/1 2 3 1
Studies
Each of the 16 noise realizations of the dual-isotope data and each of the sequential
single-isotope data were reconstructed using MC-JOSEM and the SI-OSEM respectively.
16
12
"'TC-MDP
4
S
16
12
231-MIBG
Li 4
0
MC-JOSEM
SI-OSEM
Figure 4.2. Comparison of Reconstructed Images After Three Iterations. The top and bottom rows give
the 9 9mTc-MDP and 2 3I-MIBG reconstructed data, respectively. The left and right slices correspond to the
SI-OSEM and MC-JOSEM reconstructions, respectively. All images correspond to the same transverse
slice in the reconstructed data.
50
Figure 4.2 shows a transverse slice though the torso of the
99mTc-MDP
and
12 1-MIBG
reconstructed images of both single-isotope and dual-isotope data, reconstructed with SI-OSEM
and MC-JOSEM, respectively. The images reconstructed with MC-JOSEM were close to the
images reconstructed with SI-OSEM. This finding is confirmed by the quantitative analysis
studies shown below.
Lesion Detectability Comparison
4.3
The lesion detectability from the MC-JOSEM reconstruction was compared to that of SIOSEM gold standard reconstruction algorithm on the basis of the SNR of lesions. Figures 4.3
and 4.4 show the comparison between SNR of lesions in reconstructed images for
and
99 mTc-MDP
I-MIBG, respectively. The SNR of lesions in MC-JOSEM-reconstructed images is close
12 3
23
to that of SI-OSEM-reconstructed images for both 99mTc-MDP and 1 1-MIBG. It is also evident
that SNR is lesion-dependent (it depends on contrast, location, and other factors). Because of the
CHO uncertainty and the lesion-dependability of the SNR, it is not surprising that the MCJOSEM SNR can be higher than the SI-OSEM SNR for one of the lesions.
On average, the SNR obtained from dual-isotope studies is only 5.77% and 10.61% lower
than single-isotope studies for
99
mTc-MDP/l
3
99mTc-MDP
and
I-MIBG,
123
respectively. Hence, simultaneous
I-MIBG has the potential to replace sequential
neuroblastoma imaging.
51
99mTc-MDP
and
12 3I-MIBG
for
-
SI-SM
8
*6MC-JOSEM
6
cC-
0
5
4
(-C
Xz
3
-**4
Ln
-
-
0
Tumor I
Tumor 2
Tu- r3
Tumor4
Tumor 5
99
Figure 4.3. Comparison of SNR of Lesions in mTc-MDP Reconstructed Images After Three
Iterations. The blue striped and red diamonds bars correspond to SI-OSEM and MC-JOSEM, respectively.
8
7
6
C
C
-
4
SI-SEM
'MC-JOS&M
3
0
0
**4
zCd,
=--***4
:*4
***4
ZvZV41rl
Tumor I
Tumor 2
Tumor 3
Tumor 4
23
1 I-MIBG
Tumor S
Figure 4.4. Comparison of SNR of Lesions in
Reconstructed Images After Three
Iterations. The blue striped and red diamonds bars correspond to SI-OSEM and MC-JOSEM, respectively.
52
5
Conclusions and Future Projections
The MC-JOSEM reconstruction algorithm was applied to simultaneous
'Tc/'I-
simulated data and its lesion detectability was compared to that of the standard single-isotope
reconstruction algorithm. The lesion detectability of from the MC-JOSEM reconstruction
99
algorithm is close to the single-isotope golden standard reconstruction algorithm for both mTc-
MDP and
I-MIBG. Therefore, simultaneous ""'Tc-MDP/'2I-MIBG has the potential to replace
12 3
sequential "'"Tc-MDP and
l'I-MIBG
for neuroblastoma imaging.
Future studies include dose-reduction calculations of dual-isotope SPECT compared to
single-isotope SPECT, and applying MC-JOSEM to
real patient data.
53
99mTc-MDP/12 3I-MIBG
phantom data and
6
Works Cited
Abbey, C. K., Barrett, H. H. "Human- and model-observer performance in ramp-spectrum noise;
effects of regularization and object variability." Journal of the Optical Society of America
A, Vol. 18 (2001): 473-488.
Bushberg, J. T. et al. The Essential Physics of Medical Imaging. Philadelphia, PA: Lippincott
Williams & Wilkins, 2002.
Cho, Z., Jones, J. P., and Singh, M. Foundations of Medical Imaging. New York, NY: John
Wiley & Sons, Inc., 1993.
de Jong, H. W. A. M. "Accelerated Monte Carlo simulation for scatter correction in SPECT."
Febodruk BV, Ensede, 2001.
Dempster, A. P., Liard, N. M., and Rubin, D. B. "Maximum Likelihood from incomplete data via
the EM-algorithm." Journal of the Royal Statistical Society, Vol. 39 (1977): 1-38.
Du, Y. et al. "Optimization of acquisition energy windows in simultaneous
99mTc/ 12 3I
brain
SPECT." IEEE Transactions in Nuclear Science, Vol. 50 (2003): 1556-1561.
El Fakhri, G. et al. "Absolute Activity Quantitation in Simultaneous
1/99mTc Brain SPECT."
12 3
Journal of Nuclear Medicine, Vol. 42 (2001): 300-308.
Gelfand, M. "Metaiodobenzylguanidine in children." Seminar in Nuclear Medicine. Vol. 23
(1993): 231-242.
Hoefnagel, C. A. et al. "Radionuclide diagnosis and therapy of neural crest tumors using iodine131 -metaiodobenzylguanidine." Journal of Nuclear Medicine, Vol. 28 (1987): 308-314.
Hudson, H. M. and Larkin, R. S. "Accelerated image reconstruction using ordered subsets of
projection data." IEEE Transactions in Medical Imaging, Vol. 13 (1994): 601-609.
Hutton, B. F., Hudson, H. M., and Beekman, F. J. "A Clinical Perspective of Accelerated
54
Statistical Re- construction." European Journal of Nuclear Medicine, Vol. 24 (1997):
797-808.
Kamphuis, C., Beekman, F. J., and Viergever, M. A. "Evaluation of OSEM for ID, 2D and fully
3D SPECT Reconstruction." IEEE Transactions in Medical Imaging, Vol. 43 (1996):
2018-2024.
Kamphuis, C. et al. "Dual Matrix Ordered Subset Reconstruction for Accelerated 3D Scatter
Correction in SPECT." European Journal of Nuclear Medicine, Vol. 25 (1998): 8-18.
Knoll, G. Radiation Detection and Measurement
3 rd.
Hoboken, NJ: John Wiley & Sons, Inc.,
2000.
Lange, K. and Carson, R. "EM Reconstruction algorithms for emission and transmission
tomography." Journal of Computed Assisted Tomography. Vol. 8 (1984): 306-316.
Leahy, L. M. and Qi, J. "Statistical approaches in quantitative positron emission tomography."
Statistical Computation, Vol. 10 (2000): 147-165.
Ljungberg, M., Strand S. E., and King, M. A. Monte Carlo Calculations in Nuclear Medicine.
Bristol, UK: IOP Publishing, 1998.
Ouyang, J., El Fakhri, G., and Moore, S. C. "Fast Monte Carlo based joint iterative
reconstruction for simultaneous
99
mTc/1 2 3 I SPECT imaging." Medical Physics. Vol. 34,
No. 8 (2007): 3263-3272.
Ouyang, J. et al. "Quantitative simultaneous
99mTc/ 2
1
cardiac SPECT using MC-JOSEM."
Medical Physics, Vol. 36, No. 2 (2009): 602-611.
Metz, C. E., Atkins, F. B., and Beck, R. N. "The geometric transfer function component for
scintillation camera collimators with straight parallel holes." Physics in Medicine and
Biology, Vol. 25 (1980): 1059-1070.
55
Manglos, S. H. et al. "Experimentally measured scatter fractions and energy spectra as a test of
Monte Carlo simulations." Physics in Medicine and Biology, Vol. 32 (1987): 335-343.
Phelps, M. E. and Sorenson, J. A. Physics in Nuclear Medicine, New York, NY: Grune &
Stratton, 1987.
Raeside, R. E. "Monte Carlo principles and applications." Physics in Medicine and Biology. Vol.
21, No. 2 (1976): 181-197.
Rufini, V., Calcagni, M. L., Baum, R. P., "Imaging of neuroendocrine tumors." Seminar in
Nuclear Medicine, Vol. 36 (2006): 228-247.
Rufini, V. et al. "Iodine-123-MIBG scintigraphy in neuroblastoma: a comparison between planar
and SPECT imaging." Journal of Nuclear Medicine, Vol. 39 (1995): 25-28.
Segars, W. P., Lalush, D., and Tsui, B. "A realistic spline-based dynamic heart phantom." IEEE
Transactions on Nuclear Science, Vol. 46 (2002): 503-506.
Shapiro, B. et al. "Iodine-131-metaiodobenzylguanidine
for the locating of suspected
pheochromocytoma: experience in 400 cases." Journal of Nuclear Medicine, Vol. 26
(1985): 576-585.
Shepp, L. A. and Vardi, Y. "Maximum likelihood reconstruction for emission tomography."
IEEE Transactions in Medical Imaging, Vol. 1 (1982): 113-122.
Shultis, J. K. and Faw, R. E. Fundamentals of Nuclear Science and Engineering. 2 "d.Boca Raton,
FL: Taylor & Francis Group, LLC, 2008.
Tsui, B. M. W. and Simmons, G. H. "Collimator design, properties and characteristics." The
Scintillation Camera. New York, NY: The Society of Nuclear Medicine, 1988.
Webb, S. The Physics of Medical Imaging. Philadelphia, PA: Institute of Physics Publishing,
1988.
56
Zaidi, H. "Relevance of accurate Monte Carlo modeling in nuclear medical imaging." Medical
Physics, Vol. 26 (1999): 574-608.
Zheng, X. M. et al. "Correction for crosstalk contaminations in dual radionuclide 99mTc and 123
images using artificial neural network." IEEE Transactions on Nuclear Science, Vol. 51
(2004): 2649-2653.
57