Norfolk and Suffolk
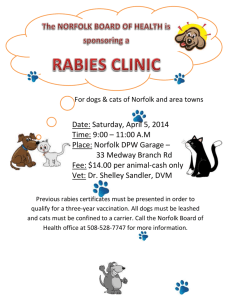
advertisement

Norfolk and Suffolk NHS Foundation Trust Norfolk and Suffolk NHS Foundation Trust Hellesdon Hospital Drayton High Road Norwich NR6 5BE Tel: 01603 421421 Web: www.nsft.uk Norfolk and Suffolk NHS Foundation Trust values and celebrates the diversity of all the communities we serve. We are fully committed to ensuring that all people have equality of opportunity to access our service, irrespective of their age, gender, ethnicity, race, disability, religion or belief, sexual orientation, marital or civil partnership or social & economic status. If you would like this leaflet in large print, audio, Braille, alternative format or a different language, please contact PALS and we will do our best to help. Email: PALS@nsft.nhs.uk or call: PALS Freephone 0800 279 7257 © 2015 NSFT. All rights reserved. NSFT Comms/15/016. GFX 3770 Quality Account 2014-15 Contents Page 2014-15 Statement of Directors’ Responsibilities in respect of the Quality Report Independent Auditor’s Report Statement from the Chief Executive Information about the quality account Looking forward Feedback on Quality Priorities 2014-15 Statements of Assurance from the Board Review of Services Research Commissioning and Quality Innovation Goals (CQUIN) agreed with Commissioners Statements from the Care Quality Commission (CQC) Data Quality Quality Initiatives Implementing Recovery through Organisational Change (ImROC) Crisis Care Child Family and Young People Pathway Drug and Alcohol Services Secure Services Learning Disability Services National Recognition Quality indicators Key Quality Indicators Evaluation of Patient Safety Infection Prevention and Control (IPAC) Activities Physical Health Sign Up to Safety Plan Positive and Proactive Care Evaluation of Clinical Effectiveness Evaluation of Patient Experience Serious Incidents (SIs) Patient Led Assessments of the Care Environment (PLACE) Service User Survey Staff Survey Commissioners and Stakeholder Comments NSFT Governors NHS South Norfolk CCG, on behalf of the Norfolk CCGs Great Yarmouth & Waveney Clinical Commissioning Group Healthwatch Suffolk Healthwatch Norfolk Health Overview and Scrutiny Committee Key and glossary How you can get involved 2 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 3 4 6 8 8 9 13 13 18 18 19 20 20 20 22 23 23 23 24 24 26 31 32 33 33 33 33 33 35 38 39 40 42 43 43 44 44 45 48 48 49 49 Quality Account 2014 -15 Norfolk and Suffolk NHS Foundation Trust 2014-15 Statement of Directors’ Responsibilities in respect of the Quality Report – CQC Intelligent Monitoring Report dated November 2014 The Directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations to prepare Quality Accounts for each financial year. Monitor has issued guidance to NHS Foundation Trust Boards on the form and content of annual quality reports (which incorporate the above legal requirements) and on the arrangements that NHS Foundation Trust Boards should put in place to support the data quality for the preparation of the Quality Report. In preparing the Quality Report, Directors are required to take steps to satisfy themselves that: • The Quality Report presents a balanced picture of the NHS Foundation Trust’s performance over the period covered • The performance information reported in the Quality Report is reliable and accurate • There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Report, and these controls are subject to review to confirm that they are working effectively in practice • The data underpinning the measures of performance reported in the Quality Report is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review • The content of the Quality Report meets the requirements set out in the NHS Foundation Trust Annual Reporting Manual 2014-15 and supporting guidance • The content of the Quality Report is not inconsistent with internal and external sources of information including: – Board minutes and papers for the period April 2014 to March 2015 – Papers relating to Quality reported to the Board over the period April 2014 to March 2015 – Feedback from commissioners dated April 2015 – Feedback from governors dated May 2015 – Feedback from local Healthwatch organisations dated May 2015 – Feedback from Overview and Scrutiny Committee dated May 2015 – The Trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009, dated May 2015 – The national patient survey published 2014 – The 2014 national staff survey published February 2015 – The Head of Internal Audit’s annual opinion over the Trust’s control environment dated May 2015 The Quality Report has been prepared in accordance with Monitor’s annual reporting guidance (which incorporates the Quality Accounts regulations) as well as the standards to support data quality for the preparation of the Quality Report (available at www.monitor.gov.uk/annualreportingmanual) The Directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Report. By order of the Board Date Chairman Date Chief Executive Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 3 Independent Auditor’s Report to the Board of Governors of Norfolk and Suffolk NHS Foundation Trust on the Quality Report We have been engaged by the Board of Governors of Norfolk and Suffolk NHS Foundation Trust to perform an independent assurance engagement in respect of Norfolk and Suffolk NHS Foundation Trust’s Quality Report for the year ended 31 March 2015 (the “Quality Report”) and certain performance indicators contained therein. Scope and subject matter The indicators for the year ended 31 March 2015 subject to limited assurance consist of the national priority indicators as mandated by Monitor: • 100% of Care Programme Approach (CPA) patients receive follow-up contact within seven days of discharge; and • Minimising delayed transfer of care. We refer to these national priority indicators collectively as the “indicators”. Respective responsibilities of the Directors and auditors The Directors are responsible for the content and the preparation of the Quality Report in accordance with the criteria set out in the NHS Foundation Trust Annual Reporting Manual issued by Monitor. Our responsibility is to form a conclusion, based on limited assurance procedures, on whether anything has come to our attention that causes us to believe that: • the Quality Report is not prepared in all material respects in line with the criteria set out in the NHS Foundation Trust Annual Reporting Manual; • the Quality Report is not consistent in all material respects with the sources - specified in the Detailed Guidance for External Assurance on Quality Reports; and. • the indicators in the Quality Report identified as having been the subject of limited assurance in the Quality Report are not 4 Norfolk and Suffolk NHS Foundation Trust Quality Account reasonably stated in all material respects in accordance with the NHS Foundation Trust Annual Reporting Manual and the six dimensions of data quality set out in the Detailed Guidance for External Assurance on Quality Reports. We read the Quality Report and consider whether it addresses the content requirements of the NHS Foundation Trust Annual Reporting Manual, and consider the implications for our report if we become aware of any material omissions. We read the other information contained in the Quality Report and consider whether it is materially inconsistent with: • Board minutes for the period April 2014 to May 2015; • Papers relating to Quality reported to the Board over the period April 2014 to May 2015; • Feedback from Commissioners dated May 2015; • Feedback from Governors dated May 2015; • Feedback from local Healthwatch organisations dated May 2015; • Feedback from Overview and Scrutiny Committee dated May 2015; • The Trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009, 2014-15; • The 2014-15 national patient survey; • The 2014-15 national staff survey; • Care Quality Commission intelligent monitoring report; and • The 2014-15 Head of Internal Audit’s annual opinion over the Trust’s control environment. We consider the implications for our report if we become aware of any apparent misstatements or material inconsistencies with those documents (collectively, the “documents”). Our responsibilities do not extend to any other information. We are in compliance with the applicable independence and competency requirements of the Institute of Chartered Accountants in England and Wales (ICAEW) Code of Ethics. Our team comprised assurance practitioners and relevant subject matter experts. This report, including the conclusion, has been prepared solely for the Board of Governors of Norfolk and Suffolk NHS April 2014 to March 2015 QA 2015 040615 numbered for insertion to ARA :Layout 1 09/06/2015 08:26 Page 31 Governors of Norfolk and Suffolk NHS Foundation Trust as a body, to assist the Board of Governors in reporting Norfolk and Suffolk NHS Foundation Trust’s quality agenda, performance and activities. We permit the disclosure of this report within the Annual Report for the year ended 31 March 2015, to enable the Board of Governors to demonstrate they have discharged their governance responsibilities by commissioning an independent assurance report in connection with the indicators. To the fullest extent permitted by law, we do not accept or assume responsibility to anyone other than the Board of Governors as a body and Norfolk and Suffolk NHS Foundation Trust for our work or this report save where terms are expressly agreed and with our prior consent in writing. Assurance work performed We conducted this limited assurance engagement in accordance with International Standard on Assurance Engagements 3000 (Revised) – ‘Assurance Engagements other than Audits or Reviews of Historical Financial Information’ issued by the International Auditing and Assurance Standards Board (‘ISAE 3000’). Our limited assurance procedures included: • Evaluating the design and implementation of the key processes and controls for managing and reporting the indicators. • Making enquiries of management. • Testing key management controls. • Limited testing, on a selective basis, of the data used to calculate the indicator back to supporting documentation. • Comparing the content requirements of the NHS Foundation Trust Annual Reporting Manual to the categories reported in the Quality Report. • Reading the documents. A limited assurance engagement is smaller in scope than a reasonable assurance engagement. The nature, timing and extent of procedures for gathering sufficient appropriate evidence are deliberately limited relative to a reasonable assurance engagement. Limitations Non-financial performance information is subject to more inherent limitations than financial information, given the characteristics of the subject matter and the methods used for determining such information. The absence of a significant body of established practice on which to draw allows for the selection of different but acceptable measurement techniques which can result in materially different measurements and can impact comparability. The precision of different measurement techniques may also vary. Furthermore, the nature and methods used to determine such information, as well as the measurement criteria and the precision thereof, may change over time. It is important to read the Quality Report in the context of the criteria set out in the NHS Foundation Trust Annual Reporting Manual. The scope of our assurance work has not included governance over quality or nonmandated indicators which have been determined locally by Norfolk and Suffolk NHS Foundation Trust. Conclusion Based on the results of our procedures, nothing has come to our attention that causes us to believe that, for the year ended 31 March 2015: • the Quality Report is not prepared in all material respects in line with the criteria set out in the NHS Foundation Trust Annual Reporting Manual; • the Quality Report is not consistent in all material respects with the sources specified above; and • the indicators in the Quality Report subject to limited assurance have not been reasonably stated in all material respects in accordance with the NHS Foundation Trust Annual Reporting Manual. KPMG LLP Statutory Auditor 6 Lower Brook Street, Ipswich, Suffolk. IP4 1AP 27 May 2015 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 31 Statement from the Chief Executive This has been a challenging 12 months for our Trust, and we recognise that the high quality standards that we aspire to achieve have not always been met. That is a personal disappointment to me and I know it is to my colleagues on the Trust Board. The commitment of our Board is that 2015-16 and beyond is going to be a time of improvement, with a clear focus on quality and of improving the working lives of our staff. On inspecting us in October 2014, the Care Quality Commission (CQC) stated in its report: ‘Overall, we saw that staff were kind, caring and responsive to people and were skilled in the delivery of care’. To have skilled and competent staff, who care and respond to the needs of our service users is the starting point for our achieving high quality standards. Our Board has described the end of 2014-15 as our ‘turning point’. This will be the point from where we demonstrate that we learn from our mistakes and ensure they are not repeated. We will ensure that our day to day practices offer high quality, safe services which are the norm not the exception. Most significantly, we will celebrate and share our successes with our service users, carers and commissioners. We will continue to give full credit to our staff to motivate them to continue to deliver ever increasing levels of quality. Some of the key quality improvements and achievements we have already made include: • A safe staffing review for in-patient areas was completed and £2.6m investment made into recruiting more staff. • 16 new doctors have been recruited to improve services and reduce locum use. • A new 12-bed mental health assessment ward opened in March to reduce out of area placements. • In partnership with MIND, we introduced a mental health crisis telephone line, available seven-days-a-week in Norfolk. • Significantly reducing out of area placements of our service users • Our Trust has been awarded the five-year contract for the new Norfolk and Waveney Wellbeing service. 6 Norfolk and Suffolk NHS Foundation Trust Quality Account • We have been awarded the new £1.3m Liaison and Diversion contract, offering early intervention, and diverting people, who require mental health services, away from the criminal justice system. But we know there is still much work to be done. The CQC inspection report also rated our Trust overall as ‘inadequate’ and recommended to our regulator, Monitor, that we were put in to ‘special measures’, which was enacted in February 2015. The report highlighted the need to improve staff morale, staffing levels, bed availability, staff training and visible leadership across our Trust. It held no surprises for us and, although much work had already begun to address many of these issues when the report was published in January this year, further improvements will be delivered over the coming months. I am more confident that as we enter a period of stability and support that ‘special measures’ offers us, we are in a better position to meet the challenges we face than we have ever been before. Our Quality Improvement Plan and the Quality Goals outlined within this Quality Account will provide the framework for our continued progress. We know what is important, we understand where we got it wrong and we are putting it right; these priorities and plan will ensure we stay on track. Our Board recognises that being truly visible leaders who are ready to listen and respond, as well as lead, has to be our approach moving forward and with that approach we have been able to address, quickly and effectively, a number of issues raised by the CQC. We must not ignore the other positive elements of the inspectors’ report highlighting areas of existing good practice, such as: • The Dementia Intensive Support Team (DIST) introduced an innovative helpline to provide advice to carers and care homes. The team was recognised for their achievements by being shortlisted for a Positive Practice in Mental Health Award 2014. • Examples of innovative multi-disciplinary working within our Child, Family and Young People services. The young people’s April 2014 to March 2015 in-patient unit was also commended last year, following assessment by the Quality Network for In-patient CAMHS, which praised the collaboration between staff and service users, and staff morale. • By collaborating with Norfolk and Suffolk Constabularies, we are helping to reduce the number of people unnecessarily detained under Section 136. In Norfolk, a team of qualified mental health nurses are working in the police control room and in Suffolk, nurses work with police officers in a triage car which can attend incidents around the county. • Our Dementia and Complexity in Later Life teams (DCLL) have integrated with GPs and social workers to improve outcomes for patients, and as part of the Health Foundation’s two-year project ‘Closing the Gap in Patient Safety’, will be looking at preventing falls and medication errors among people using dementia care services. All of this is a real testament to the commitment and professionalism of our staff and on behalf of the Board I’d like to acknowledge their ongoing support and dedication. It will be critical to work with staff, service users, our Governors, commissioners and other stakeholders, to continue to build on quality improvements to our services. We will continue to listen, to learn, to improve and to raise the bar on quality through 2015-16 and beyond. Statement of accuracy I confirm that to the best of my knowledge, the information contained in this document is accurate. Michael Scott Chief Executive Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 7 Information about the quality account The purpose of the quality account is to ensure that NHS organisations are accountable for the quality of services they provide. The quality account is a way in which the Board of Directors demonstrates that it takes seriously its responsibilities for promoting, monitoring and leading on quality. It includes several quality priorities explicitly agreed by the Board of Directors for 2014-15. These were identified in a process which began with stakeholder consultation followed by widespread dissemination of options and collation of feedback. Seclusion and restrictive interventions: Use of restrictive interventions will reduce to below the national benchmarking average by 1 April 2016. This priority will be led by the Director of Nursing, Quality and Patient Safety. Physical health 95% of service users admitted to a ward for more than 24 hours will receive a physical health check. This will be recorded on the service user (patient) record (Lorenzo) along with any action plan if a physical health need is identified. Looking forward Priorities for Improvement in 2015-16 *This plan can be found on NHS Choices website at http://www. nhs.uk/NHS England/ special measures/ Documents/ May%20 2015/ norfolk-and -suffolk-action -plan-may -2015.pdf 8 This is the section of the Trust’s Quality Account that looks forward to 2015-16 and identifies our goals for improvement. The rationale for why these goals have been chosen and how progress will be monitored is described below. Our Trust has agreed a number of priorities which support our Quality Improvement Plan and which include goals to improve practice, where deficits have been identified from the service user survey, local and national clinical audits and local feedback, including complaints and serious incident investigations. The priorities our Trust has agreed will help us to improve the quality of care we offer. They are based on feedback from service users and carers who have told us how services could be improved. We have also looked at what we can learn from complaints and incidents, and from national research into good practice. Each of these priorities will support our Quality Improvement Plan and each will be led by an Executive Director to ensure progress is made. This progress will be reported to our full Board of Directors four times a year. This priority will be led by the Norfolk and Suffolk Operations Directors, supported by the Physical Health Team. Patient Experience (Reference: Quality Improvement Plan RE6)* Trust service users (with Care Programme Approach entitlements) will report that they were involved in their care plans at a level at or above the national benchmarking average when the 2016 results are published. This will be measured via the Service User Survey, ‘Have you agreed with someone from NHS mental health services what care you will receive?’ Clinical Effectiveness (Reference: Quality improvement Plan SA9)* All locality governance groups will be able to demonstrate that learning from incidents has led to changes in practice by 1 October 2015. Patient safety (Reference: Quality Improvement Plan SA4)* Norfolk and Suffolk NHS Foundation Trust Quality Account This priority will be led by the Norfolk and Suffolk Operations Directors and all managers will take action and respond to information coming from the Patient Safety Team. April 2014 to March 2015 Feedback on Quality Priorities 2014-15 The Quality Account published in 2014 identified five new quality targets, with a further three quality targets carried forward from 2013-14. This section demonstrates the progress that has been made in the past 12 months. Patient Safety Priority 1 – To implement a system that ensures that all patients/service users in contact with mental health services access relevant physical healthcare screening and services. Where we were: This priority arose from the National Audit of Schizophrenia published in 2012. Following discussion with commissioners a number of systems were put in place for community patients which acknowledged that our Trust carried responsibility for the physical health of its service users, usually in partnership with primary care services. Where we are now: In 2014-15, this priority was clarified as the implementation of the Lester Tool and adopted as a National CQUIN target. Results of round two of the National Audit identified that the Trust performance in monitoring the five cardio-metabolic health risk factors had improved and the Trust had moved from 53rd position to 39th position out of the 64 organisations taking part. Although this identifies an improved position nationally, completion of all five elements of the tool remained low and an action plan was put in place and led by the Physical Health Strategy Group. Our Trust has subsequently submitted data to a follow up audit and the results are awaited. Priority 2 – Being able to access services quickly. Where we were: This priority was identified by service users responding to a consultation and reflected the view that there were delays in accessing NSFT services following referral. Where we are now: The following table identifies the waiting times for services in the three commissioned areas of the Trust, as of 31 March 2015. The target in all cases is for 100% of patients to be seen within the number of days stated in the contract. (QA1) IAPT Services - seen within 28 days of referral Month Jan Feb Mar Qtr Gt Yarmouth & Waveney 80.58% 94.30% 97.85% 88.87% Norfolk 95.76% 100.00% 99.85% 98.49% Suffolk 99.80% 99.84% 99.35% 99.63% Trust 93.05% 99.00% 99.34% 97.10% Suffolk 97.25% 97.83% 98.23% 97.76% Trust 98.63% 98.76% 98.57% 98.65% (QA2) Secondary Care Services - seen within 18 weeks of referral Month Jan Feb Mar Qtr Gt Yarmouth & Waveney 100.00% 99.73% 100.00% 99.92% Norfolk 99.03% 98.99% 98.19% 98.73% Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 9 Priority 3 – Being confident that the Trust learns from mistakes and puts in place plans to reduce similar risks. Where we were: The Francis Inquiry in 2013 identified the need for organisations to have a greater openness and ‘candour’ with service users and patients when safety incidents occur. While our Trust did have a process for investigating safety incidents, it had not fully demonstrated that actions from investigations were being completed or that lessons learned were being shared. Where we are now: The recent Care Quality Commission (CQC) report identified that this issue was still a cause for concern, and this priority has been included in the Trust’s Quality Improvement Plan to ensure action is taken. Our Trust has also implemented a policy to ensure that ‘Duty of Candour’ is applied and that evidence that action is being taken is regularly presented to our Board. Patient Experience Priority 4 – Being able to contact a mental health worker out of hours, and the inclusion of emergency contact details in Crisis or Contingency Plans for service users. although when plans were in place they were found to be of high quality and to contain the relevant contact numbers. Although our Trust produced general information about its services, there was, at times, a lack of direct contact numbers for clinical teams for our service users in a crisis or out of hours. “Crisis team are not a helpful service for a person in a real crisis” “My care plan was discussed fully and I was involved” Where we are now: The guidance remains consistent that all service users should have a Crisis, Contingency or Recovery Plan and this should contain contact details for emergencies and out of hours. Monitoring this will become easier with the roll out of a single online patient/service user record (Lorenzo) in Spring 2015, where plans will be recorded. In the meantime, a small audit of community teams was undertaken in February 2015. Although a relatively small sample of 51 cases is not fully representative, the cases were drawn from teams right across our localities. This audit has shown that the number of service users having a crisis plan has increased, but only 55% of the plans contain the contact numbers. Where we were: Audit demonstrated that less than 50% of our service users had a Crisis Plan in place, (QA3) Combined Total (n = 51) Central Norfolk West Norfolk East Suffolk West Suffolk (n = 9) Gt Yarmouth & Waveney (n = 6) (n = 51) (n = 51) (n = 51) 7/9 (78%) 3/6 (50%) 9/12 (75%) 10/12 (83%) There is a Crisis / Contingency Plan in place 40/51 (78%) 11/12 (92%) The Crisis / Contingency Plan includes specific telephone contact details out of working hours in case of emergency 22/40 (55%) 10 7/11 (64%) Norfolk and Suffolk NHS Foundation Trust Quality Account 3/7 (43%) April 2014 to March 2015 1/3 (33%) 5/9 (56%) 6/10 (60%) In addition, in January 2015 a 6pm to 8am crisis support line was launched in Norfolk in partnership with MIND. All service users are given the contact number. If the support line proves successful, ongoing funding will be sought and plans to roll out a similar support line in Suffolk will be discussed. Priority 5 – All in-patient areas will have a programme of activities which will be available seven days a week including evenings. Where we were: Feedback from our 2013 National Service User Survey showed our Trust to be in the top 20% of mental health trusts for providing activities both at weekends and during the week. However, staffing shortages in some areas were leading to the programme not being delivered consistently. Where we are now: The original TOC guide was launched in July 2010 to build on good practice and to include and recognise carers as partners in care. NSFT signed up as official members of the TOC scheme in May 2014. By signing up to the TOC membership scheme, our Trust has committed to ensuring that carers are valued for the vital role they play and are identified as equal partners in care. Since signing up to the scheme, our service lines have taken an active role in ensuring that self-assessments are in place and the carer’s role is acknowledged and supported. Our teams have also set up monitoring groups where self-assessments can be discussed locally, good practice shared and any issues addressed. Oversight is provided at a strategic level by the Carers Leads Advisory group. Clinical Effectiveness Where we are now: This priority was set without a clear and measurable goal and a new method of measurement has been implemented through the use of an individual monitoring form. This form has been introduced for all in-patients and is used in conjunction with daily ward meetings, which enable service users to discuss activities for the day and for the staff to tailor the programme accordingly. The form will demonstrate the activity that is available and taken up by the service user and may also be used in reviews to identify changes in mental state. Priority 6 – The Trust will use the Triangle of Care (TOC) self-assessment tool as a starting point before consulting with carers on an appropriate action plan. Its implementation and effectiveness will be monitored and reported to carers, service users and commissioners. Where we were: Local feedback identified that carers were not always involved or considered in the care of the service user. While a number of initiatives were in place to improve the situation, the implementation was variable across the Trust. Priority 7 – When a new medication is prescribed, the prescriber should always discuss this with the service user first. Information leaflets should be given and this should be recorded in the service user’s record. Where we were: The National Service User Survey and the National Audit of Schizophrenia both indicated that some service users did not feel that they were consulted in changes to their medication or given enough information. Where we are now: The National In-patient Survey in 2014 revealed that: • Patients reporting that the purpose of their medication had been explained in a way that they could understand decreased from 45% to 34%. • Patients reporting being fully informed about the side effects of the medication dropped from 34% to 19%. For both responses the Trust’s score fell within the lowest 20% of trust scores. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 11 QA 2015 040615 numbered for insertion to ARA :Layout 1 09/06/2015 10:31 Page 38 (QA4) Q24 Purposes of medications explained completely Q25 Told completely about the side effects of the medication 0% 10% Denotes Trust’s position within the above ratings 20% Best performing Trusts The Trust is disappointed in these results but notes that many of the respondents would have accessed services in 2013, and improvements have been made since then. An audit carried out in March 2015 has identified that 82% of service users were engaged in a discussion about their medication and 56% reported having the side effects explained. Following the results of the service user survey, a Trust-wide action plan has been put in place and progress will be reported to Senior Management Forum. Priority 8 – Having a care coordinator who gets to know you and can ensure continuity of care. 30% 40% About the same 50% 60% 70% Worst performing Trust Where we were: This priority was identified by service users during a period of time when there was a major service restructuring programme in place, with movement of care coordinators between teams having a real impact on service users. “I feel that I have been left high and dry after my change of care coordinator” Where we are now: Whilst recognising the importance of this priority, there is no straightforward way of measuring achievement. The Trust do regularly collect data on the number of cases awaiting care coordinator allocation, and this information is provided as an indication of our performance against this priority. (QA5) Unallocated cases in the last three months of 2014-15 Locality Number of cases (Jan 15) Number of cases (Feb 2015) Number of cases (March 15) 270 196 109 53 174 20 51 267 162 98 61 189 6 51 286 188 141 0 221 6 0 Central adult Central CFYP Coast adult Coast DCLL West adult West CFYP West DCLL This issue is predominantly related to care in Norfolk where a number of initiatives have been put in place to mitigate the risks to service users: • Allocation of £2.6 million to provide additional staff. 12 Norfolk and Suffolk NHS Foundation Trust Quality Account • All relevant staff in service teams can access all cases, ensuring any member of the team can provide assistance to a service user when required. • Service users can access groups within the Norfolk Wellbeing service if appropriate. April 2014 to March 2015 Statements of Assurance from the Board The wording in the following statements is required in the DH regulations for producing Quality Accounts. The statements are required nationally to enable the public to compare the performance of individual trusts and are therefore common across all Quality Accounts. We have provided some explanation of the terms used in the glossary, but if you would like any further explanation please contact the Patient Advice and Liaison Service (PALS) on Freephone 0800 279 7257. Review of Services During 2014-15 NSFT provided and/or subcontracted eight NHS services: adult services, children’s services, drug and alcohol services, improving access to psychological therapies (IAPT), learning disability services and (QA6) older people’s services. The Trust also provides forensic and Tier 4 Child and Adolescent Mental Health Services (CAMHS) commissioned by NHS England rather than local CCGs. The Trust has reviewed all the data available on the quality of care in all of these services. The income generated by the NHS services reviewed in 2014-15 represents 92.06% of the total income generated from the provision of NHS services by the Trust for 2014-15. The quality of care the Trust has provided has been reviewed in a number of ways. This is via the collection of systematic performance data against Monitor, CQC and CCG quality targets as well as clinical audits, surveys, analysis of complaints and serious incident data, and informal feedback from service users and carers. However data is gathered, the Trust system of meetings ensures that it is reported, and that action plans for improvement are put in place where needed. Quality of care review methods Data type Lead Reported to Action Clinical Audit Audit lead Quality Governance Committe • Action plan developed and implemented by relevant lead clinician. • This is then monitored by the audit department and a re-audit undertaken as indicated to demonstrate that the plan has improved the service. • Locality Governance dashboards incorporating audit compliance and audit results databases are updated monthly and shared with Localities to enable them to compare their performance with other areas and to see, at a glance, where further action is required. Complaint Complaints manager Quality Governance Committee • Action plan developed and implemented by relevant manager. • Where there is learning for other areas, the action plan is shared through a variety of mechanisms including access to the plan and the production of themes that are shared with all areas, policy amendments and adjustments to training packages. Feedback from visits Non-executive Modern matrons Directors and ward managers • Action plan developed to resolve any issues that arise. Feedback Head of Governance • Quality Improvement visits carried out by clinicians, governors, commissioners and partner agency representatives. Quality Governance Committee Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 13 During 2014-15, one national clinical audit and one national confidential enquiry* covered NHS services that the Trust delivered (in terms of collecting patient level data). During that period, NSFT did not take part in the national clinical audit: Prescribing Observatory for Mental Health (POMH)**. * A national confidential enquiry is a nationwide review of clinical practice which when completed leads to recommendations for improvement. ** The Trust has not to date participated in the POMH audits as these are audits prescribed by the Observatory and were not considered to be relevant to the priorities of the Trust. The Trust will participate in the audits commencing in February 2015 and the results will be reported in the 2015-16 Quality Account. The national clinical audits and national confidential enquiries that the Trust was eligible to participate in during 2014-15 were: • Prescribing Observatory for Mental Health: prescribing topics in mental health services. • Mental health clinical outcome review programme: National Confidential Inquiry into Suicide and Homicide by People with Mental Illness (NCISH). The national clinical audits and national confidential enquiries that NSFT actually participated in during 2014-15 are as follows: • Mental health clinical outcome review programme: National Confidential Inquiry into Suicide and Homicide by People with Mental Illness (NCISH). The national clinical audits and national confidential enquiries that the Trust participated in, and for which data collection was completed during 2014-15, are listed below, alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. (QA7) National Confidential Enquiries 14 Name Completed and status Number of cases and percentage of registered cases required National Confidential Inquiry Into Suicide and Homicide by People with Mental Illness Continuous audit N/A Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 The reports of two national clinical audits carried out by NSFT were reviewed in 2014-15 and the Trust intends to take the following actions or has taken action to improve the quality of healthcare provided: (QA8) Actions following audit National audit of psychological therapies (published 2012-13) Actions reported in 2014 Progress against actions Improving access for older people by: Implementing a training programme for IAPT team members in working with older adults (Great Yarmouth and Waveney (GY&W)). All staff have now attended training Providing workshops within residential and sheltered housing (Norwich). These sessions have now been delivered. Improving accessibility by: Extending hours within the day in which interventions can be provided by therapists (West Norfolk & GY&W). The service is now provided from 8am to 8pm. Development and provision of resources in a range of languages. IAPT services across the Trust are working together to collate therapy resources in other languages. Interpreting services are accessed where the need for this is identified. Consulting with service user forums regarding the report findings. The report findings have been shared with the forums. Adapting Patient Experience Questionnaire to capture feedback from those dropping out of treatment with follow up. Where service users do not automatically opt in to the service within two weeks of receipt of the referral, they are contacted by telephone. Plans to evaluate the Ready to Change programme; a new way to deliver guided self-help for people with mild / moderate depression and / or anxiety (Suffolk Wellbeing service). Six-month evaluation incorporating data as well as staff and service user feedback. This model is now being adopted across Suffolk. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 15 (QA8 continued) National audit of schizophrenia: (Second round) Actions reported in 2014 Progress against actions Following the publication of the report, a time limited steering group was set up to review the findings and coordinate actions. This steering group acknowledged that most of the actions required were already in progress through other pieces of work in the Trust. The steering group is due to end in April 2015 and a report will be produced, summarising the actions completed and the reporting mechanism for further actions. Action plans include Improving carers satisfaction with the support and information they receive through application of the Triangle of Care and support of Service User/Carer Forums. Providing information and supporting decision making about medication though education and training of medical staff, medicine information sessions in in-patient areas. Supporting best practice in the prescribing of antipsychotic medication through medical staff training plan, development of prescribing guidelines and alerts on prescription cards to prompt reviews. The review into availability and use of psychological therapies will be coordinated by Lead Clinicians. Monitoring and interventions for physical health problems through shared care protocols with primary care, named physical health leads in each locality and a physical health champion for each team, physical health monitoring in clozapine and depot clinics. 16 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 The reports of 70 local clinical audits were reviewed by the provider in 2014-15 and NSFT intends to take the following actions to improve the quality of healthcare provided in relation to the three audits selected: (QA9) Actions following audit Actions Taken Audit Title Suicide Prevention: The Trust has continued to undertake monthly audits which have measured its progress against nationally approved standards using evidence-based audit tools (National Patient Safety Agency (NPSA) Preventing Suicide Toolkit) for in-patient wards and a purposive sample* of community teams. Charge Nurses and Community Team Leaders take immediate action following any audited practice that falls below 100% compliance. Action plans in in-patient wards have related to giving information about medications to service users, discharge planning, contingency planning, discharge CPA reviews, care planning and risk assessment for changes in observation levels and involving service users and carers in discharge planning. Actions in Community Teams have included: timely reviews of assessments, recording service users’ involvement in care planning, accessibility of risk assessments, identification of lead professionals, completion of data protection act forms, involvement of carers in assessment process. Additional Observations: The Trust undertakes bi annual audits of Additional Observations. Data is collected by the Modern Matrons for their service and action plans are submitted at point of data submission. Actions have included: monitoring and scrutiny of observation records by team leaders, monitoring of adherence to requirement to review care plans as observation levels change, local re auditing to measure compliance. Medical Staff Audits: Medical staff have completed many audits throughout the year, and participated in Trust wide audits. Topics have included: admission summaries, blood test monitoring, clozapine monitoring, clinical coding, health records, use of MHA, ADHD, smoking rates in an in-patient area, medication prescribing for dementia. Actions resulting from an audit of Physical examination and investigations for psychiatry in-patients at Woodlands Unit, Ipswich Hospital included: the development of a pro-forma to guide and record physical health parameters on admission following multi professional team feedback. * A purposive sample is a sample of people who have the characteristics that are required for the study Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 17 The Trust participates in the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness as previously documented, with excellent compliance scores. Should the Trust have a serious incident resulting in a child’s death or near miss, this would be referred to the Norfolk and Suffolk Safeguarding Children’s Boards for consideration under the Serious Case Review (SCR) guidance as outlined in Working Together to Safeguarding Children 2013, and be reported in the three-year national report. For the period being looked at there has been one SCR involving a child known to the Trust in Suffolk, and to which the Trust contributed as part of the management review. As a member of the Norfolk and Suffolk Safeguarding Child and Adult Boards: the Trust will take account of all recommendations arising from SCRs, regardless of whether or not Trust services were involved. The Trust is currently participating in an Adult SCR involving two adults known to Suffolk services, and a further joint Suffolk and Norfolk Adult SCR related to a service user known to the Trust in both counties. Research The number of patients receiving NHS services provided or sub-contracted by the Trust from April 2014 to March 2015, who were recruited during that period to participate in research approved by a research ethics committee, was 250. To support research in the Trust, NSFT Research has launched a new online referral system and register which enables clinicians to support all service users to take part in research. This has also been a successful year for research capacity with several Trust members obtaining places on national research MSc, PhD and Fellowship schemes. The launch of the service user, carer and public involvement in research initiative (inspire) has proven to be very popular, with 40 current members across Norfolk and Suffolk. Commissioning and Quality Innovation Goals (CQUIN) agreed with Commissioners A proportion of the Trust’s income in 2014-15 was conditional on achieving quality 18 Norfolk and Suffolk NHS Foundation Trust Quality Account improvement and innovation goals agreed between the Trust and any person or body with which it entered into a contract, agreement or arrangement for the provision of NHS services, through the Commissioning for Quality and Innovation (CQUIN) payment framework. The Trust has a contract with Norfolk* (CCG), Suffolk CCG and Cambridge and Peterborough CCG for the provision of mental health services to the population of Norfolk and Suffolk, and with NHS England (specialist) Commissioning Group for the provision of low and medium secure services and Tier 4 Child and Adolescent Mental Health Service. The Trust has a contract with Norfolk* and with Great Yarmouth and Waveney CCGs for the provision of Increased Access to Psychological Therapy (IAPT) services. In addition, Norfolk Public Health commissions the Norfolk Recovery Partnership (NRP) for drug and alcohol services for prisons and community. For the contract with Norfolk* and with Great Yarmouth and Waveney CCGs, a total of seven goals to improve quality were agreed as part of the main contract and a further four goals attributed to the contract to provide IAPT services. The eleven goals agreed accounted for 1.5% of the total contract value and an additional 1% was allocated to system wide indicators. The rationale for these goals included suggestions from service user feedback as well as pre-defined national priorities. The goals covered all services delivered by the Trust and the three domains of quality: patient experience, patient safety and clinical effectiveness. The CQUIN contract with Suffolk CCGs included eight goals covering the full value of the scheme. The goals covered a range of topics including, wellbeing, IAPT, data collection for the national patient safety thermometer**, increased efficiency of psychiatric liaison services and raising awareness in police services. A total of seven goals to improve quality were nationally agreed for secure services by the 10 regional area teams. This covered a diversity of goals including an education and training package and assuring the appropriateness of unplanned admissions. Further details of the agreed goals for 201415 and for the following 12 month period are available electronically on request from the contracts department on 01603 421251. April 2014 to March 2015 QA 2015 030615:Layout 1 09/06/2015 08:57 Page 19 The value of the scheme represents 2.5% of the total contract value and approximately 84% compliance has been achieved in Norfolk and Suffolk. The income received which was conditional upon achieving quality improvement and innovation goals in the main contracts 2014-15 is forecast to be £4,182,137 this compares with the income received in 2013-14 which was £4,165,914. *Comprising South Norfolk, North Norfolk, West Norfolk and Norwich City Clinical Commissioning Groups **Patient safety thermometer is a national patient safety initiative which records a number of safety concerns that measure the provision of ‘harm free care’ including pressure ulcers and falls ***Monitor is the regulator for Foundation Trusts (QA10) CQC Ratings This rating led to the CQC recommending to Monitor*** that the Trust be placed in ‘special measures’. This means that an Improvement Director has been appointed and the Trust will work with a buddy trust to learn from them. A Quality Improvement Plan is now in place and is being monitored by the Trust Board and reviewed at monthly meetings with Monitor and the CQC. Statements from the Care Quality Commission (CQC) The Trust is required to register with the Care Quality Commission (CQC). Its current registration status is ‘registered to provide assessment or medical treatment for persons detained under the Mental Health Act 1983 and treatment of disease, disorder or injury’. The CQC has taken enforcement action against NSFT during 2014-15 and in February 2015 the Trust was put into ‘special measures’. The Trust has not been eligible for any special reviews or investigations by the CQC during 2014-15. During 2014-15, the CQC undertook a number of visits to the Trust to check compliance with registration against the essential standards and compliance with the Mental Health Act for people detained. This culminated in a ‘Comprehensive inspection’ in October 2014 which inspected the Trust and produced a report for each service line. The Trust then received a rating for each service line against the five domains of: Safe, Effective, Responsive, Caring and Well-led. The ratings received are shown below: All of the CQC reports are available at www.cqc.org.uk. The CQC visited all of the registered sites and inspected all in patient areas and a selection of community teams in line with their policy. The new reporting method reflects the service provided rather than the location, but the reports do identify the location where practice is commented on. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 19 Data Quality Norfolk and Suffolk NHS Foundation Trust will be taking the following actions to improve data quality: • Excellent data quality is essential to the delivery of excellent quality care. NSFT will continue to ensure data quality improvements are made to support services through provision of easily accessible available performance reporting through Abacus and MIS, the Trust’s business intelligence reporting systems, overseen by the Data Quality Group. • These systems provide daily updates which are accessed by business support staff. Any data quality issues can be passed to the appropriate staff member for correction. • A monthly data quality meeting is held and attended by a wide range of staff to discuss data quality issues, new updates where applicable and Information Standards Board changes which may affect reporting and therefore data quality. • Data quality is also mentioned in staff job descriptions, ensuring that staff are held accountable for data quality. • Norfolk and Suffolk NHS Foundation Trust submitted records during 2014-15 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data: • Which included the patient’s valid NHS number was 94.98% for admitted patient care: – Not applicable for out-patient care – Not applicable for accident and emergency care • Which included the patient’s valid General Medical Practice Code was 99.89% for admitted patient care: – Not applicable for out-patient care. – Not applicable for accident and emergency care. NSFT information governance assessment reports the overall score for 2014-15, submitted in March 2015, was 80% and was graded ‘not satisfactory / red’ under national information governance rules. 20 Norfolk and Suffolk NHS Foundation Trust Quality Account Action plans are being developed with regards to those requirements that did not achieve Level 2. This is monitored at the Information Governance Committee with the expectation that these improvements will be in place before the next submission due in March 2016. The Information Governance Risk Register, and also information governance related incidents that are reported through the Trust Datix reporting system, are continuously reviewed and reported quarterly to the Information Governance Committee for action. The information quality and records management attainment levels assessed within the information governance toolkit provide an overall measure of the quality of data systems, standards and processes within an organisation. Further details on information governance can be found at www.commissioningforhealth.nhs.uk The Trust was not subject to the payment by results clinical coding audit during 2014-15 by the Audit Commission. Quality Initiatives This section summarises quality information specific to Norfolk and Suffolk NHS Foundation Trust. Key Performance and Developments during 2014-15 This section allows the Trust to highlight quality matters from 2014-15 that have not been addressed elsewhere in the report. The Quality Account has already highlighted specific areas where quality is not as high as the Trust would expect; however, there are many areas of excellent and innovative practice. Implementing Recovery through Organisational Change (ImROC) The Trust has taken part in the national ImROC initiative which aims to put people with mental health problems at the heart of service delivery and to enable them to rediscover a sense of wellbeing and purpose in their lives. An important channel of this initiative has been the continued success of our Recovery College. The College was set up in September 2013 to deliver a range of courses and April 2014 to March 2015 424 service users, carers or supporters having taken part. The Recovery College is overseen by a steering group in which service users, carers, staff and governors are all represented. Evaluation of the courses has been very positive (409 respondents): workshops to empower people with mental health challenges to become experts in their own recovery. The success of the College has seen the number of tutors grow from seven staff and five peer tutors to 19 staff and 19 peer tutors by the end of the first year. In the four terms the College has been operating, its programme has expanded to deliver courses across all five localities with 411 staff and (QA11) How would you describe the value of the course for your own recovery or for the recovery of someone you support? 1% Excellent 34% Good Poor 65% What next for 2015-16 Targets for year two of the Recovery College include: • Collaborating with partners to produce workshops which focus on dementia and older peoples services, forensic services, youth services, drugs and alcohol services. • Working with Equal Lives and the Shaw Trust to create courses on mental health, employment and work. • Working with Cambridgeshire and Peterborough NHS Foundation Trust (CPFT) to share some courses already co-produced and to develop further courses on relationships and intimacy, and music and mental wellbeing. • Seeking other opportunities to increase partnership, co-production and delivery of courses. • We have extended the eligibility to access courses to include service users who have been discharged from services (and who have a discharge care plan) for up to one year post discharge and will continue to identify ways of widening the eligibility criteria further. • Continue to evaluate student experience. • Identification of a process to measure recovery outcomes for students and peer tutors. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 21 Crisis Care Crisis care is a priority for the Trust and in addition establishing the crisis telephone line mentioned on page 6, the Trust has signed up to the Crisis Care Concordat in both Norfolk and Suffolk. This is a national programme which brings together NHS trusts, local authorities and the police to review crisis care as a system-wide issue in order to develop shared goals and a collaborative approach. Norfolk In addition to reflecting the crisis care priorities outlined in this report, an important outcome of the Norfolk Concordat is the provision of a mental health team within the Norfolk Constabulary Contact and Control room. The team consists of four staff who are able to speak to service users and provide professional, specialised advice. The team ensure callers receive the best and most appropriate care and can reduce the need for involvement by the police. The team monitors performance and has reported a 30% drop in the number of people detained under section 136*. This is a positive step towards meeting the objectives of the Safer Place to Be report, published in October 2014 following a survey of all health-based places of safety across the country. http://www.cqc.org.uk/content/safer-place-be *Section 136 is a section of the MHA which enables a police officer to remove a person to a place of safety to undergo a mental health assessment. Suffolk In Suffolk the action plan for the Concordat covers a range of issues that are being addressed in collaboration with the local authority and police. These include: service user involvement, the use of section 136 and improving the knowledge of professionals involved in primary care to help them to manage people who may be at risk of committing suicide. In addition, we are currently evaluating a CQUIN initiative which sees staff from our Trust linked with police to assess care needs in 22 Norfolk and Suffolk NHS Foundation Trust Quality Account a crisis situation. As we have seen in the Norfolk scheme, working with police has also reduced the number of people detained under section 136. Improving access to psychological therapies in Suffolk As part of the IAPT agenda, we are taking active steps to ensure access to our wellbeing services is as easy as possible, including: • 24/7 online self-referral system available in multiple languages • Parts of the service being accessible without a need for an assessment • Providing workshops to community groups, workplaces and colleges • An active presence on social media We are involving service users in the development and maintenance of the service by seeking feedback via Patient Experience Questionnaires and inviting previous service users to attend our service user group. A recent example of this work was a SPEAK poster developed by the service user group to encourage more people to seek help for stress, anxiety and/or depression. This poster is also being used as a template to advertise our new developments aimed at increasing access to psychological therapies for people with long term physical health conditions. Improving access for Black and Minority Ethnic (BME) service users Through innovative working with third sector partners VoiceAbility, the Suffolk Wellbeing Service (SWS) has achieved a 16% access rate to its services by the BME community in Suffolk. VoiceAbility is an advocacy group that aims to bring together organisations to support people facing disadvantage and discrimination (www.voiceability.org). SWS has engaged with community networks to raise awareness of the services they offer and routes to access them. Building strong links with the BME community has also enabled SWS to deliver culturally sensitive Stress Management workshops in community venues, providing services in an environment where people feel safe and empowered. April 2014 to March 2015 Child, Family and Young People Pathway Friends and Family Pathway The Central Norfolk Early Intervention Team has begun a pilot scheme which aims to ensure that all carers have equal and consistent access to support services. The Family Involvement Team, with consent from the service user, can offer the family: • Initial telephone or face to face meeting to answer questions and discuss any concerns. • Information packs, including guidance on: the Team, medication, unusual experiences, support services available to carers, family work offered by the Team and details of the Friends and Family Group (a rolling group, held monthly and facilitated by staff). • Six follow up sessions to look in more detail at the family’s role in supporting the service user. The Team has received positive informal feedback and the success of the pilot will be evaluated using future feedback collected regarding the Friends and Family pathway. users received a consistent and effective approach to their care. The POG tool enables staff to evaluate service users by ‘risk’, ‘motivation’ and ‘need’, and to group their clients accordingly. The tool incorporates information from previous assessments as well as subsequent engagements to assign a client to either Purple (Intensive), Orange (Enhanced) or Green (Standard) groups. Staff can then determine the appropriate level and intensity of engagement each service user requires. The benefits of the POG tool are: • Enables staff to accurately and effectively prioritise their time and caseload. • Gives staff ownership of their caseload and it’s management. • Provides insight into service users motivation and engagement with treatment. • Supports the progress of service users through the service, particularly those engaged with the service for long periods of time. • Assists managers in monitoring workload and allocation of new client work. Secure Services School Twilight Sessions This service offers free, direct access to specialist mental health professionals, consultation and training for teachers and other school staff. The sessions include information on topics such as self-harm and eating disorders, as well as the opportunity to ask questions. Drug and Alcohol Services Drug and alcohol services are provided by the Trust in partnership with the Matthew Project and RAPt, collectively known as the Norfolk Recovery Partnership (NRP). POG Rating System Due to growing caseloads, it was recognised that a tool was needed to assist staff to make best use of their time and to ensure service 2014-15 has been a challenging year for Secure Services, but also a productive one: • The service has developed a strategy for supporting carers and a Steering Group is working through the ‘Triangle of Care’ actions with the support of carers themselves, a champion from each area and involvement from Suffolk Family Carers. • The service has developed a strategy for improving staff wellbeing and engagement, introducing a quarterly staff forum and staff recognition scheme. • In June 2014, the Trust commissioned a ‘Review of progress made following the Exploratory Review relating to three in-patient deaths within Secure Services in 2013’. It revealed that, of the 14 recommendations made in the Exploratory Review, 12 have been implemented fully and two require further work to complete. The reviewer noted that a number of other positive changes have Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 23 occurred and commended the management team and the service for the progress made. • Each area of the Service has strengthened its Service User involvement throughout 2014 with attendance at forums increasing. • In 2014 we introduced Quarterly Learning Events – half day service-wide events which focus on governance and quality. • In April 2014 we started a NHS England funded partnership with HMP Wayland to develop a PIPE (Psychologically Informed Planned Environment) and the country’s first Category C Personality Disorder Assessment & Treatment Service which officially opened in February 2015. Learning Disability Services Bowel Care Passport Our Suffolk Adult Learning Disability Service has developed an innovative tool to improve patient care, in response to the findings of the Confidential Inquiry and two local serious case reviews relating to the premature and preventable deaths of people with a learning disability. The ‘bowel care passport’ acts as a care plan and a guidance document to ensure all care providers know how to best support the individual with bowel care. Service users own the passport which is used to share information with their GP and other health providers when accessing services. The passport was developed in consultation with service users, staff and bowel care specialists at Ipswich Hospital. chaired by service users and supported by the Modern Matron and IMPACT advocacy service. *The Trust is not commissioned to provide learning disability services in Norfolk. LISTEN Staff from East Suffolk worked with service users and carers to respond proactively to complaints regarding service users’ experiences of crisis care. The LISTEN (Listen, Involve, Shared, Time, Empathise, Next) acronym was developed to remind staff of the key issues to consider when communicating with service users and carers. Posters and prompt cards were printed and distributed to staff throughout the Trust. CRAM In East Suffolk, it was recognised that there was a need to improve the clinical quality of patient records. A local audit was devised to consider each of the teams and identify areas of strength and weaknesses. Individual action plans were developed in response to these findings. The outcomes of the action plans were re-examined and revealed that one inpatient team had shown significant improvement. The model employed by this team was then shared as best practice with other teams. The successful approach involves using the CRAM acronym within patient notes to remind staff to consider care plan, risk assessment, activity and mental state. LD Service User Forums National Recognition Some people using our learning disability services reported that the mental health forums were not representative and were too difficult to understand. To ensure that people with a learning disability were empowered to contribute to the work of our Trust, we set up dedicated service user forums in both Waveney and Suffolk.* Service users meet monthly to discuss the care they receive from NSFT, and they are invited to contribute to discussions about changes to the service. Both forums are 24 Norfolk and Suffolk NHS Foundation Trust Quality Account AIMS (Accreditation for In-patient Mental Health Services) accreditation In February 2015 Waveney ward at Hellesdon Hospital attained AIMS accreditation, joining several other wards across the Trust which have already been awarded this standard. The AIMS accreditation is a standards-based accreditation programme designed to improve the quality of care in in-patient mental health April 2014 to March 2015 wards run by the Royal College of Psychiatrists. Further information can be found at: http://www.rcpsych.ac.uk/workinpsychiatry/qu alityimprovement/qualityandaccreditation/psyc hiatricwards/aims.aspx East Suffolk Excellent accreditation for ECT team In February 2015 the East Suffolk Electro Convulsive Therapy (ECT) team based at Woodlands received a renewed accreditation of ‘excellent’ from the Royal College of Psychiatrists Centre For Quality Improvement (CCQI). This is a voluntary accreditation scheme which ensures that the best standards of care are provided to service users who receive ECT therapy. Further information about the scheme can be found at: http://www.rcpsych.ac.uk/workinpsychiatry/qu alityimprovement/qualityandaccreditation/ectcl inics/ectas/ectasstandards.aspx Fermoy Unit, Queen Elizabeth Hospital; Frank Curtis NSFT Library and NSFT Research Team, Hellesdon Hospital; Sandringham and Blickling Wards, Julian Hospital Two of our nominees – Sandringham and Blickling Wards and also Steve Birt – were specially selected for the Outstanding Contribution to Learning award. Sandringham and Blickling Wards were praised for their contribution to an innovative pilot project called ‘Collaborative Learning in Practice’ (CLiP), which enables clinical areas to host an increased number of student nurses by utilising a coaching model to provide comprehensive support and guidance. The Trust is delighted that Steve Birt was awarded both the Learning Support Award and the award for Outstanding Contribution to Learning in recognition of his approach to mentoring and vital role in the support of students. Woodlands Safewards Model The team’s Lead Nurse, who chairs the Trust wide ECT special interest group, has also become an honorary member of (NALNECT) National Association of Lead Nurses for ECT. Workforce Partnership Practice Education and Learning Support Awards Four individuals and three teams from our Trust were nominated for regional excellence awards in recognition of their contribution to supporting learning and education. The awards, which were presented on 16 March 2015, saw nominations for: • Mentor / Practice Teacher Award: Melanie Grose, Criminal Justice Mental Health Liaison Practitioner; Ronnie Simpson, Staff Nurse, Blickling Ward • Learning Support Award – Foundation degree: Steve Birt, Care Pathway and Discharge Nurse, Assessment and Treatment Service, Bury St Edmunds • Learning Support Award – Apprenticeships: James Lunny, Education and Development Team • Team Award: Mental Health Liaison Team, Woodlands, which provides the base for acute mental health services in East Suffolk, has become the first unit in the Trust to adopt the Safewards model. The model encourages service users and staff to work together to reduce factors such as aggression and selfharm. A Department of Health paper stated that the Safewards model had ‘demonstrated significant effectiveness in achieving reductions in incidents of conflict and the use of physical restraint…’ and it is employed as best practice across a number of mental health trusts. Staff at Woodlands received an initial introduction to the 10 interventions outlined in the model, with ongoing support for implementation of the Safewards approach being delivered by staff champions and through monthly progress reviews. The model is now being adopted across the Trust. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 25 • Data is submitted to commissioners where it is scrutinised and challenged where necessary. Quality Indicators Seven Day Follow Up This indicator is described as “The percentage of patients on CPA who are followed up within seven days after discharge from psychiatric in-patient care”. NSFT considers that this data is as described for the following reasons: • NSFT has robust systems in place to check the quality of data. NSFT has taken the following actions to improve this percentage, and so the quality of its services, by: • Business Support Managers check the systems and liaise with clinical staff to check any data that appears to be outside normal parameters. • Data is discussed at local management groups as well as Trust wide performance groups. (QA12) Prescribed information Related NHS Outcomes framework domain 2012-13 2013-14 2014-15 The percentage of patients on CPA who were followed up within seven days after discharge from psychiatric in-patient care. Preventing people from dying prematurely. 95.9% 97.89% 98.57% This is a national definition reported to Monitor. Enhancing quality of life for people with long term conditions. Target 95% The latest available data produced by NHS England shows that the national average score for the period October to December 2014 was 97.3%. The highest performing area scored 99.6% and the lowest area scored 94.9%. • NSFT has robust systems in place to check the quality of data. • Data is submitted to commissioners where it is scrutinised and challenged where necessary. Access to CRHT NSFT has taken the following actions to improve this percentage, and so the quality of its services, by: This indicator is described as “The proportion of in-patient admissions gate kept by the crisis resolution home treatment teams”. NSFT considers that this data is as described for the following reasons: 26 Norfolk and Suffolk NHS Foundation Trust Quality Account • Business Support Managers check the systems and liaise with clinical staff to check any data that appears to be outside normal parameters. • Data is discussed at local management groups as well as Trust wide performance groups. April 2014 to March 2015 (QA13) Prescribed information Related NHS Outcomes framework domain 2012-13 2013-14 2014-15 The percentage of admissions to acute wards for which CRHT acted as gatekeeper. Enhancing quality of life for people with long term conditions. 92.40% 99.69% 97.46% This is a national definition reported to Monitor. Target 95% The latest available data produced by NHS England shows that the national average for the period October to December 2014 was 97.8%. The highest performing area scored 100% and the lowest performing area scored 82.5%. Readmission Rates NSFT considers that this data is as described for the following reasons: • NSFT has robust systems in place to check the quality of data. NSFT has taken the following actions to improve this percentage, and so the quality of its services by: • Ensuring that discharge planning is robust and that the discharge policy is followed. • Ensuring patients receive a follow up visit within seven days of discharge and telephone contact within 48 hours of discharge. (QA14) Prescribed information Related NHS Outcomes framework domain The percentage of patients aged Helping people to recover from episodes of ill health or following injury. 0-15 16 or over readmitted to a hospital which forms part of the Trust within 28 days of being discharged from a hospital which forms part of the Trust. 2012-13 No 2013-14 2014-15 5.9%** No re-admissions. 5.3% 7.87% admissions* 6.2% * NSFT did not have beds for under 14s in 2012-13 ** The number of readmissions refers to the specialist tier 4 CAMHS unit which was not opened in previous years Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 27 It should be noted that the Monitor guidance has been changed and that in previous years the ages reported were 0-14 and 15 and over. This does not affect the reported numbers as the Trust does not admit people under 16 to adult beds. Staff Survey The national NHS Staff Survey is a mandatory requirement for NHS organisations, with results being used by NSFT to understand the views of its staff and to inform improvements in the workforce arena. The most recent survey took place in September to October 2014, with results published on 24 February 2015. (QA15) Prescribed information Related NHS Outcomes framework domain 2012 2013 2014 Staff employed by, or under contract to, the Trust during the reporting period who would recommend the Trust as a provider of care to their family or friends. Ensuring that people have a positive experience of care 3.32 3.08 2.99 National average: 3.57. Top scoring Trust: 4.15. The scores achieved are from a maximum possible score of five. NSFT considers that this data is as described for the following reasons: • In order to get feedback from as many staff as possible, for the first time, NSFT undertook the survey as a census of all employed staff. In previous years it has undertaken a sample survey. Whilst the percentage response rate is therefore lower than previous years, the number of staff who responded is far more representative than in previous years (1,336 staff responded out of 3,676 staff surveyed in 2014 compared to 341 out of 840 staff surveyed in 2013). • Whilst recognising the significant level of organisational change that had impacted staff in the 12 months prior to the survey, NSFT is disappointed by the results. The results, however, highlight issues that the Trust is already aware of and is addressing. These issues reflect feedback also received from the CQC inspection that was held at the same time as the survey. Improving staff engagement is an absolute priority of NSFT. 28 Norfolk and Suffolk NHS Foundation Trust Quality Account NSFT is taking the following actions to improve this percentage, and so the quality of its services, by: • Engaging independent consultants to work with NSFT to review its values and behaviours. • Reviewing its operating model and developing a responsibilities and accountabilities framework to support this. • Investing in leadership and management development. • Continuing to implement its Wellbeing Strategy including the roll out of Wellbeing Weeks across the Trust and the Healthy Worker training programme. • Implementing a fifteen point plan endorsed by the Board of Directors to improve staff engagement. • Implementing its Recruitment and Retention Strategy to fill vacancies, including additional posts added to the establishment to support safer staffing, and to improve the retention of staff. • Reviewing its mandatory training strategy and moving to a more competencybased approach. April 2014 to March 2015 NSFT has taken the following actions to improve this percentage, and so the quality of its services, by: Community Service User Survey NSFT considers that this data is as described for the following reasons: • The Trust commissions an outside agency, Quality Health, which is an ‘approved provider’ to undertake the survey. • Action plan for improvement is monitored at the Senior Managers Forum and Locality governance meetings. • It should be noted that the sample is drawn from service users accessing services before the results of the previous survey are known. We would therefore not expect to see any improvements as a result of the action plan in the next survey. (QA16) Prescribed information Related NHS Outcomes framework domain 2012 2013 2014 The trust “patient experience of community mental health services” indicator score with regard to a patient’s experience of contact with a health or social care worker. Enhancing quality of life for people with long term conditions. NWMHFT NSFT NSFT 8.7 8.6 7.5 Ensuring that people have a positive experience of care. SMHP 8.8 Range of scores: 7.3 – 8.4. The scores achieved are from a maximum possible score of ten. Incident Reporting NSFT has taken the following actions to improve this percentage, and so the quality of its services, by: NSFT considers that this data is as described for the following reasons: • Staff report all incidents using the electronic Datix system. • All incident reports are reviewed by the Risk Management Team and clinical managers required to investigate and sign off each incident before closing the event. • Health, safety and security audits are carried out on all Trust premises which include a review of incident reporting trends. • These are subject to discussion at the Incident and Patient Safety Group meetings. • Staff are encouraged to report all incidents and the Trust has recently introduced an upgrade to the report form and Datix dashboard, which provides clinical managers with a live overview of the reported incidents in their area. • Incidents are reviewed by the patient safety team to identify themes and patterns, working with clinical areas and stakeholders, such as the police, to implement changes where required. • Serious Incidents are managed in accordance with national guidance. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 29 (QA17) Related NHS Outcomes framework domain 1 October 2012 to 31 March 2013 1 April 2013 to 30 Sept 2013 1 October 2013 1 April 2014 to to 31 March 2014 30 Sept 2014 1 October 2014 to 31 March 2015 Treating and caring for people in a safe environment and protecting them from avoidable harm 2,835 incidents* reported. 3,395 incidents* reported. 4,065 incidents* 4183 incidents* reported. reported. 4,018 incidents reported 42.2 incidents per 1000 occupied bed days.** 31.63 incidents per 1000 occupied bed days.** 37.87 incidents per 1000 occupied bed days.** 55.48 incidents per 1000 bed days.** 3 incidents (0.07%) led to severe harm 7 incidents (0.25%) led to severe harm. National average 0.5%. 7 incidents (0.2%) led to severe harm. 3 incidents (0.07%) led to severe harm. 3 incidents (0.1%) led to severe harm. 8 incidents (0.2%) led to a death 10 incidents (0.35%) led to a death. 25 incidents (0.7%) led to a death. 7 incidents (0.2%) led to a death. National average 0.3%. 6 incidents (0.1%) led to a death. National average 0.8%. NB. The reporting rate of 42.2 incidents is rated 5th out of 55 mental health organisations and puts the Trust in the top 25%. National average 0.7%. NB. The reporting rate of 31.63 incidents is rated 20th out of 55 mental health organisations and puts the Trust in the middle 50%. NB. The reporting rate of 37.87 incidents is rated 12th out of 56 mental health organisations and puts the Trust in the top 25%. Differences between the National Reporting and Learning System (NRLS) data for deaths and the figure for Serious Incidents are due to the different reporting requirements. NRLS guidance requires that only deaths of suspected suicide are reported to the system, whereas Serious Incident reporting will include all forms of unexpected death (e.g. incidents where information suggests it may be due to an accidental overdose). * An incident is defined as “any unintended or unexpected incident which could have, or did, lead to harm for one or more patients 30 Norfolk and Suffolk NHS Foundation Trust Quality Account NB. The reporting rate of 55.48 incidents is rated 10th out of 54 mental health organisations and puts the Trust in the top 25%. NB. This data is subject to change following final ratification and report from NRLS. receiving NHS-funded healthcare”. (www.nrls.npsa.nhs.uk) Organisations that report more incidents usually have a better and more effective safety culture because they are aware of the problems and able to act to improve. ** A bed day is used as a measure to enable comparison between Trusts of different sizes. The measurement accounts for differences in the number of beds a hospital may have and just considers the days the beds were occupied. April 2014 to March 2015 Key Quality Indicators The Board receives regular reports on the quality of services which are measured through the domains of patient safety, clinical effectiveness and patient experience. Key performance indicators (KPIs) are identified by the Board as internally generated or enforced by contractual obligations with partner organisations. These indicators are reported in a monthly business performance report, and other measures of quality are reported through the reporting system to evaluate services. The indicators reported here have not been changed following the 2013-14 Quality Account to provide consistency and enable comparisons to be made. (QA18) Key performance indicator Target Trust position 2012-13 Trust position 2013-14 Trust position 2014-15 95% 95.9% 97.89% 98.57% 4.1 7.61 7.31 5.72 3.8 2.74 2.74 4.19 95% 92.40% 99.69% 97.46% <7.5% 4.55% 4.80% 4.55% No admissions 6.2% 5.9%* 5.3% No readmissions 97.55% 99 15 0 98.05% 72 17 0 96.71% 78 12 0 137.65% 131.76% Patient safety • Seven-day follow up of service users following their discharge from in-patient services. • Absconsions of detained patients from Adult wards as a ratio of 100 detained patients. • Ratio of in-patient serious untoward incidents (e.g. suicide) per 10,000 occupied bed days. Clinical effectiveness • Access to crisis resolution and home treatment services. • Delayed transfers of care, relating to other support needs (like housing) following discharge from hospital. The increased numbers of delayed transfers are attributable to a reduction in capacity and funding in social care though the number remains within target. • Readmission rates Age 0-15 Age 16+ Patient experience • CPA patients having formal review within 12 months. 95% • Waiting times. Number of people waiting 18 weeks or greater. • Number of under-18 year old admissions to adult acute ward. • Number of under-16 year old patients admitted 0 to adult acute wards. • Meeting commitment to serve new psychosis cases 95% by early intervention teams. * The number of readmissions refers to the specialist tier 4 CAMHS unit which was not opened in previous years Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 31 Evaluation of Patient Safety The Trust continues to report all Serious Incidents on receipt of an initial report. This is reported as good practice by the National Patient Safety Agency. The latest report from the National Reporting and Learning System for the period April 2014 to September 2014 shows that the Trust is the 10th highest reporter of all 56 mental health trusts in that period. (QA19) Are you actively encouraging reporting of incidents? The comparative reporting rate summary shown below provides an overview of incidents reported by NHS organisations to the National Reporting and Learning System (NRLS) occurring between 01 April 2014 to 30 September 2014. Your organisation reported 4,183 incidents (rate of 55.48) during this period. Organisations Figure 1: Comparative reporting rate per 1,000 bed days for 56 mental health organisations 0 20 40 60 80 100 Reporting rate (per 1,000 bed days) Your organisation’s reporting rate Highest 25% of reporters Middle 25% of reporters Lowest 25% of reporters Source: NHS national Reporting and Learning System. www.nrls.npsa.nhs.uk/patient-safety-data The median reporting rate for this cluster is 32.82 incidents per 1,000 bed days. 32 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 Infection Prevention and Control (IPAC) Activities The IPAC annual work plan is devised to identify and implement activity which will deliver the priorities described in key documents and guidance, including: the Health and Social Care Act 2008 (rev.2010), CQC Regulation 12 objective 8, national best practice standards. The completion of the IPAC annual work plan is overseen by the IPAC Committee, the Quality Governance Committee and the Trust Board. Key achievements resulting from implementation of the IPAC plan for 2014-15 have been: • An improved training programme for our local infection prevention and control supporters (LIPACS) to enable them to more effectively monitor and manage their environment and support local staff. • Modification of the hand hygiene tool to improve suitability for community teams. • A programme of audits to raise awareness of standards and address deficits. There has been one confirmed outbreak of Norovirus infection involving a significant number of staff and patients. All standard IPAC interventions were applied with additional focus on cleaning objects handled, such as keys, and on staff behaviour, such as chewing pens. There have been no cases of MRSA bacteraemia or of Clostridium difficile attributed to the Trust. Patients identified as being colonised with MRSA have been treated according to Trust guidance. The priorities for the forthcoming year include: • Improving compliance with mandatory education in IPAC procedures through a range of learning and assessment opportunities. • Improved focus to ensure actions identified by audit are implemented and completed. • Strengthening the role of the LIPACS within clinical teams. Physical Health Our Physical Health Strategy Group (PHSG), which includes representatives from all localities and staff groups within our Trust, aims to improve the focus on physical health throughout the Trust by creating effective initiatives which are implemented uniformly across the services. The PHSG has commissioned task and finish groups to address a range of issues including in-patient areas, community teams, Clozapine clinics and smoking cessation. The group reports to the Quality Governance Committee and to the Trust Board. Key achievements this year have been: • Demonstrated improvements in the completion of documentation relating to a patient’s physical health and evidence of actions taken where physical health problems have been identified. • Opportunities for all staff, either at the University of East Anglia, University Campus Suffolk or at local and ward level, to undertake education and training appropriate to the needs of their service. • Scenario training delivered within wards to assist staff to recognise when a patient is deteriorating and to practice resuscitation response. • Improving the knowledge of local physical health link staff through forum activities and individual supervision. • Engagement with community teams and the decision to implement the national Rethink tool ‘My Physical Health’ as a document for raising and addressing physical health issues. • The launch of a Recovery College module focusing on physical health. Some of the priorities for the coming year are to: • Develop pathways for focusing on physical health to aid collaboration between primary care and mental health services. • Establish a multidisciplinary health and wellbeing working group as a sub-group of the PHSG. This will focus on diet and exercise and modifiable behaviours such as smoking, alcohol and drug use. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 33 • Develop care plans specifically to ensure standardised care for patients with longterm conditions. • Work within the current networks to ensure patients at the end of life are identified and receive the best evidence-based care, supported by other agencies and using standard documentation recognised by all care providers. Sign Up to Safety Plan In October 2014 the Trust signed up to the National Patient Safety First Campaign to demonstrate our commitment to continuously drive forward improvements in patient safety. This initiative will be led by the Director of Nursing, Quality and Patient Safety, and the Chief Executive will have continued oversight of progress. The six key areas identified to improve safety are: • Reduce the number of service user to service user assaults within older people’s in-patient services. • Reduce harm resulting from falls. • Provide in-patient services that are safe for service users. • Provide an environment that reduces the risk of harm. • To ensure the Trust embeds a safety culture based on openness transparency and learning from previous incidents. • To improve the community mental health teams performance in updating risk assessments in line with policy and best practice. Positive and Proactive Care In April 2014 the DH published the report ‘Positive and Proactive Care’ focusing on the need to reduce the use of restrictive interventions (restraint) by staff in mental health trusts. ‘Restraint’ describes a range of interventions, from touching a person’s arm to full restraint in which staff use validated methods to prevent assaults and self-harm. As noted on page 30, our Trust has a high rate of incident reporting and any episode of 34 Norfolk and Suffolk NHS Foundation Trust Quality Account restraint is recorded. The Trust has been identified as a high user of restraint and has now put in place a plan to reduce the use of restrictive interventions over the next 18 months. Evaluation of Clinical Effectiveness Our clinical effectiveness strategy sets out the structures and processes for ensuring clinical effectiveness across the Trust. The implementation of NICE guidance and adopting nationally agreed best practice is central to ensuring good quality outcomes for patients. NICE guidance for 2014 included: • Medications – discussed by our Drug and Therapeutics Committee. • Products designed to prevent pressure ulcers – discussed in the Physical Health Group. • Psychosis and schizophrenia in adults, bipolar disorder, delirium and autism in adults – reviewed and implemented where appropriate. The Trust audit schedule includes audits that measure compliance against the NICE guidance and best practice. Where noncompliance is identified, an action plan to improve is implemented and incorporated into the audit cycle. Monitor identifies a number of measures of clinical effectiveness including access to crisis resolution and home treatment teams before a person is admitted to hospital, and ensuring service users are followed up within seven days of discharge from an in-patient ward. These are reported to Monitor and the Trust continues to report excellent compliance with the targets. See page 26 to 27. The reports by CQC indicated that clinical effectiveness within the Trust was affected by poor levels of appraisal and supervision, as well as mandatory and specialist training. These issues are being addressed as part of our Quality Improvement Plan. April 2014 to March 2015 Evaluation of Patient Experience Service User and Carer Involvement Our Trust values the role played by service users and carers who engage in a number of ways to provide feedback and contribute to improvements. Our Trust has groups for adult mental health service users and carers across the region, in West Norfolk, City and South Norfolk, North Norfolk, Great Yarmouth and Waveney, East Suffolk and West Suffolk. The groups are open to people who are using or who have used mental health services and their carers. Service users and carers from our locality groups play an important role in influencing developments within the Trust and are actively involved in the interview process for appointing new staff. Other areas where our service users have been involved include: • Consultation on the development of a new 12-bed assessment ward based at our Hellesdon Hospital site and supporting the development of the assessment ward at the Wedgwood Unit. • Implementing a new Trust-wide patient record system, Lorenzo. • Contributing to the development of a community action plan to improve services. • Training for new ward staff in complaints and communication. • Working with staff to produce service specific leaflets for both in-patient and community services. • Working with staff to develop the LISTEN cards and posters, which describes the approach to how service users wish to be involved in their care. Our wellbeing services have locality groups in West Norfolk, Great Yarmouth and Waveney, East and West Suffolk. The Norfolk Central group will be re-launching in April 2015. Wellbeing groups have been actively involved in: • Developing a website and social media platform. • Wellbeing governance and team management meetings. • Attending and reviewing current workshops and providing feedback and recommendations. Two new groups for people with a learning disability have been developed in Lowestoft and Stowmarket, the groups are open to people who are using our learning disability services, plans for future work include: • Working with staff to produce learning disability specific courses at our Recovery College. • Being involved in the recruitment of new staff. • Working on a poster to advertise the group. The Norfolk Youth Council is fully established and meets monthly in Norwich with separate locality groups across the county. In Suffolk the group meets fortnightly and is currently developing locality-based groups. Some of the Youth Councils’ achievements in 2014-15 include: • Co-produced the job description for peer support worker for youth pathway and participated in recruitment panels. • Delivered a workshop for Ipswich hospital staff concerning young people’s experiences in A&E. • Worked with A&E Managers to identify a suitable area of the A&E to be used by young people. • Collaborated with Mental Health Liaison Nurse to produce written information for young people. • Contributed to a module regarding psychosis delivered to fourth-year medical students at University of East Anglia. • Delivered a workshop for year 10 students at Coplestone High School for the school mental health day. • Contributed to a Recovery College group which is looking into developing courses for young people. • Two Norfolk youth council members attended a European Parliament sponsored project in Rome in March, 2015 to create guidelines for improving care and access for young people with mental health needs. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 35 • Plan for eight members of the Norfolk Youth Council to attend the International Association of Youth Mental Health in Canada in October 2015. Service User and Carer Involvement Strategy Our Trust values the role played by service users and carers who engage in a number of ways to provide feedback and contribute to improvements. A project group, incorporating representatives from our Trust wide forums, service user and carer governors, members of the Board of Directors, NSFT staff and stakeholders, has developed a new service user and carer involvement strategy called ‘Improving Services Together’. The strategy outlines our commitment to: • Providing opportunities for service users and carers to have their say in Trust business. • Providing opportunities for service users and carers to use their skills to develop services. • Changing the way we provide services in line with our commitment to organisational change. • Strengthening our links with our partner agencies. • Reaching out to diverse and underrepresented groups. • Ensuring that service users and carers are involved in monitoring of the Trust’s strategy and in judging its effectiveness. The Trust continues to work with a number of agencies that represent service user and carer views, these include: Suffolk Family Carers, Suffolk User Forum, Carers Agency partnership and Healthwatch. Friends and Family Test (FFT) Both the Francis report, regarding Mid Staffordshire NHS Foundation Trust (2013), and the Berwick Report, ‘Improving the safety of patients in England’ (2013), highlighted the need for patients to be more engaged and their voices to be heard regarding the service they receive within the NHS. The Friends and Family Test (FFT) was devised to address this, and to determine patient satisfaction with NHS services. The Department of Health stipulated that all mental health and community services offer the test by January 1, 2015. The FFT was implemented across our Trust on 1 October, 2014. The primary aims of the FFT are to: • Gather feedback from patients immediately, or soon after, care has been received. • Provide a broad measure of patient experience that can be used alongside other data. • Identify areas where improvements can be made and practical action can be taken. • Empower patients to make informed choices about their care. The FFT consists of one key question: ‘How likely are you to recommend our service / team to friends and family if they needed similar care or treatment?’ with responses ranging from ‘extremely likely’ to ‘extremely unlikely’. Service users also have the option to answer ‘don’t know’. Cards have been designed to capture responses to the FFT; one for in-patients and one for community-based services. The cards are filled out at the point of discharge from in-patient services, and intermittently for all community-based services. (QA20) How likely are you to recommend our service / team 100 80 % 56% 60 40 26.8% 20 5.3% 3.6% 3% 5.3% Extremely unlikely Don’t know 0 Extremely likely 36 Likely Norfolk and Suffolk NHS Foundation Trust Quality Account Neither likely nor unlikely Unlikely April 2014 to March 2015 The bar graph (QA20) shows responses to the FFT received by the Trust from 1 October, 2014 to February 2, 2015. It demonstrates that 56% of service users and carers would be ‘extremely likely’ to recommend the service they received and 26.8% would ‘likely’ recommend the service. The following table identifies the number of responses received from service users since the FFT was launched in October 2014. (QA21) Month October 2014 November 2014 December 2014 January 2015 February 2015 Response Numbers 300 46 30 38 24 It is disappointing that the response rates have declined but the Trust is working hard to increase the response rates and improve engagement with service users and carers through the following: • Reviewing the format of the current questionnaire to make it more user friendly and engaging. • Increasing communication to all staff and patients to demonstrate the positive changes that have been made following feedback. • Considering the use of other feedback methods, such as the use of texting and using volunteers to gather feedback. Services will be expected to use the information to make improvements in their areas and a ‘You Said – We Did’ poster will be developed to enable services to show what changes have been made in response to feedback. By demonstrating the positive impact of communicating feedback, we hope to encourage more service users to complete the FFT. “The team that came out were excellent and covered everything.” “I was treated with respect and empathy and instantly felt I had made the correct decision in seeking help.” “Need better equipment and facilities.” Complaints Our Trust is committed to using complaints as a means by which learning and development can occur. Our Trust aims to consider complaints in an open and transparent way. At the time of reporting (April 2015), our Trust had logged as received 608 complaints during April 2014 – March 2015 (544 in 2013-14). The majority of complaints related to “all aspects of clinical care” (43%), followed by “attitude of staff” (22%). At the time of reporting 523 complaints have been responded to. Of these complaints 26% were upheld, 25% were partially upheld and 33% were not upheld by our Trust. 16% of complaints were stood down for reasons including the service user not providing consent to a complaint being made on their behalf, the complainant not confirming the details of their complaint and the complaint was found to refer to another agency. Our Trust has been informed that following the response to a complaint, eight complainants requested review of their complaint by the Parliamentary and Health Service Ombudsman (one to the Local Government Ombudsman). The Ombudsman requested information from our Trust to assist their investigation. During this year our Trust has implemented changes to the Complaints Procedure in order to develop the experience and response to complainants. This has included all complaint responses going through a quality check by the Complaints team prior to the Chief Executive viewing and signing all letters. Feedback from the Trust’s Board of Governors observed this has contributed to an improvement in the tone, sensitivity and completeness of response letters. Our Trust’s Non-Executive Directors continued to view a sample of complaints on a monthly basis. Learning from Complaints The CQC published its inspection report in February 2015. The inspection findings conclude there was limited evidence to demonstrate the Trust implemented learning from Serious Incidents (SIs), Complaints and other patient safety indicators. It is the Trust's contention that it does learn from SIs, complaints and other patient safety incidents. System changes often result in the Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 37 form of policy amendments, adjustment to training and clinical care pathways. Learning is also shared via a quarterly Patient Safety Newsletter and sections at Trust forums (Nursing Leadership and Modern Matrons). However, the external inspection has prompted reflection and review of the current actions and how this critical area can be developed. Actions The following outlines four actions which have been implemented and will be evaluated as part of the Quality Improvement Plan: manner) that patient safety information has reached their level / awareness. The aim is to receive assurance that information is reaching the targeted areas and to identify any blockages in the flow of information. The Trust’s Patient Advice and Liaison Service (PALS) continues to be available to provide support to service users, carers and members of the general public who seek to find information or to resolve their concerns without the desire or need to use the complaints procedure. PALS can be contacted on 0800 279 7257. Serious Incidents (SIs) Communicating learning • Increase frequency of Patient Safety Newsletter from quarterly to bi-monthly. • On the alternate month, send an e-bulletin to managers and clinical leads. • Refresh the Patient Safety intranet page, ensuring high quality, accessible information is available to all staff. • Provide learning summaries to Trust forums (e.g. Nursing, Modern Matrons) and put the presentation onto the Trust intranet. Supporting managers to enhance their understanding and role within Patient Safety • Create a tips / guidance booklet for managers with practical ways in which they can drive patient safety and quality to be high on the agenda of their respective clinical teams. • Creation and distribution of a ‘lessons learnt’ poster which clinical teams will be able to use to share learning with staff in a succinct visual way. Connection with localities • The implementation of the Governance business partner model will support direct channel of information from patient safety indicators. Assurance learning has reached all levels • To implement a system or process of checking with staff (in a safe confidential 38 Norfolk and Suffolk NHS Foundation Trust Quality Account Our Trust continues to report all Serious Incidents (SIs) in accordance with national guidance. Incidents may subsequently be stood down if an explainable cause is identified i.e. if a death is found to be as a result of physical or natural causes. From April 2014 to March 2015, 228 (172 in 2013-14) SIs were reported by NSFT, of which 139 (130 community and nine in-patient) were unexpected deaths. At the time of reporting, 15 have been determined to be due to a natural cause. The remaining SIs involved service users who were accessing a range of in-patient and community services across our Trust. They were engaged with services at the time of their death or had been discharged within the previous six months. Our Trust uses Root Cause Analysis methodology to consider the timeline and factors that influenced an incident. Through group review the analysis identifies learning actions. In the past year our Trust has strengthened oversight for a number of Serious Incidents through the engagement of Executive and Non-Executive Directors in setting the terms of the investigation and agreeing the final report. Learning from Serious Incidents plays a critical role in developing services. Examples of learning include adjusting the level of observations for people experiencing acute periods of distress requiring restrictive intervention and affirming the actions required of staff when a service user misses an appointment. This is important because evidence informs us that missing an appointment can be an indicator of increasing April 2014 to March 2015 Patient Led Assessments of the Care Environment (PLACE) risk. Learning from Serious Incidents has also contributed to the design of clinical forms for the single electronic health record system. PLACE assessments are undertaken by the Trust on an annual basis and include service users as part of the inspection teams. For the assessments carried out in 2014, when benchmarked nationally against the other 49 mental health trusts, the Trust performed as follows: (QA22) Criteria National Benchmark NSFT Score National Score Mental Health 99.63% 91.57% 89.22% 97.56% 97.75% 85.42% 88.90% 88.78% 10th 20th 28th 6th Cleanliness Food Privacy and Dignity Condition, Appearance and Maintenance It should be noted that, due to changes in the assessment methodology and scoring for the Food and Privacy, Dignity and Wellbeing sections, comparison between 2013 and 2014 is not possible. The scores attained were as follows: (QA23) PLACE Evaluation results Location Cleanliness 2013 2014 National Overall average Ward 95.75% Org Food 2013 National average 85.41% Privacy, Dignity Condition, Appearance and Wellbeing and Maintenance 2014 Overall ward org 2013 2014 2013 2014 National average 88.9% Overall ward org National average 88.78% Overall ward org Wedgwood 99.48% 99.94% 97.88% 86.70% 93.68% 85.85% 96.25% 90.35% Carlton Court 99.48% 99.48% 97.18% 96.20% 95.71% 92.06% 97.50% 99.62% Fermoy Unit 97.46% 99.03% 96.83% 90.00% 89.14% 81.67% 83.33% 98.36% Hellesdon Hospital 98.73% 99.11% 96.45% 95.15% Meadowlands 99.40% Chatterton House 99.07% Woodlands 99.25% 99.95% 96.21% St Clements Hospital 99.44% 99.33% 97.31% 86.37% 97.58% 73.61% 90.91% 92.16% The Julian Hospital 99.14% 99.95% 96.34% 93.50% 92.66% 91.83% 95.38% 99.35% The Norvic Clinic 98.94% 99.66% 96.38% 93.77% 97.57% 95.11% 97.83% 99.72% Northgate Hospital 99.63% 99.06% 96.77% 95.06% 94.71% 87.38% 94.74% 99.18% – 97.16% – 95.31% 93.07% 91.12% 92.86% 99.03% – 94.55% – 85.34% – – 83.45% – 88.39% – 97.22% 86.86% 89.84% 97.76% 87.05% The blanked out boxes indicate that Chatterton House and Meadowlands are no longer used for in-patients. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 39 The reduction of the scores noted for the Wedgwood unit is due to major building works being underway at the time which impacted on the environment and quality of dining experience, however, the food satisfaction at ward level score remained high (93.46%). The scores for cleanliness were above the 2013 national average for all sites assessed except Northgate and St Clements which both showed a slight deterioration. Both sites receive regular visits from the Quality Assurance department within the facilities team, and improvement has been seen with no complaints from service users or staff. The 2014 survey questionnaire was substantially redeveloped and updated in order to reflect changes in policy, best practice and patterns of service. New questions have been added to the questionnaire, and existing questions modified. This means that for all questions, the results from the 2014 survey are not comparable with the results from previous surveys. Community Survey A response rate of 32% was achieved; the national average was 29%. Further information about the survey can be accessed via the CQC website on http://www.cqc.org.uk/content/communitymental-health-survey-2014 or type ‘service user survey’ into the CQC website search box. This national survey enables the Trust to be benchmarked against other mental health trusts. The survey questions are grouped into nine sections and the table below shows the Trust scores compared to other mental health trusts. Service User Survey The CQC requires Trusts to undertake national service user surveys each year and this survey involved 57 mental health NHS Trusts. This is the second year in which our Trust has undertaken a survey of service users in the community, and a survey of in-patients. (QA24) S1. Your Health and Social Care Workers 0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10 S2. Organising your care S3. Planning your care S4. Reviewing your care Worse S5. Changes in who you see Worse 0 1 2 3 4 5 6 7 8 9 About the same 10 S6. Crisis Care Worse 0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10 0 1 2 3 4 5 6 7 8 9 10 S7. Treatments S8. Other areas of life Best performing Trusts Worst performing Trust Denotes Trust’s position within the above ratings 'Better/Worse' Only displayed when this trust is better / worse than most other trusts S9. Overall These results are subject to an action plan which was developed by the Senior Managers Forum, which will continue to monitor 40 Norfolk and Suffolk NHS Foundation Trust Quality Account progress, and also locality-based action plans which will be monitored within the Locality Governance meeting. April 2014 to March 2015 (QA26) – Q51 Patients’ long-standing medical conditions In-patient Survey This survey is not a mandatory requirement and was undertaken by 23 mental health trusts. The data is presented differently to the community survey and can only be compared with the 23 Trusts who participated. A response rate of 27% was achieved by our Trust. Key findings There was a decrease in the number of people rating their care as excellent from 27% in 2013 to 17% in 2014. The percentage of people who rated their care as either ‘excellent, very good or good in 2013 was 74% with a decrease to 70% in 2014. Deafness or severe hearing impairment Blindness or partially sighted A long-standing physical condition A learning disability A long-standing illness, such as cancer, HIV, diabetes, chronic heart disease, or epilepsy No, I don’t have a long standing condition (QA25) – Q47 Level of care rating This year the full results of the in-patient survey have been broken down and attributed to the individual wards. This enables our wards to implement a targeted action plan for improvement. It should be noted however that the numbers responding are small so may not be fully representative. Excellent Very good Good Fair Poor The survey also asks respondents about any long-standing conditions which are important to consider in the effective delivery of comprehensive care. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 41 Staff Survey (QA27) Summary of the response rate and the four best and worst key findings for the Trust 2012-13 2013-14 Trust (published Oct 13) (published Oct 14) Improvement (+) Response Rate Trust National Average * Trust National Deterioration (–) Average* 41% 36% 50% 42% -5% Top two ranking scores NB: While guidance requires the Trust to report the top four scores, unfortunately NSFT is only able to report two scores in the top scoring section of the report % of staff experiencing physical violence from staff in the last 12 months % of staff having equality and diversity training in last 12 months Bottom four ranking scores % of staff agreeing that their role makes a difference to patients Staff recommendation of the Trust as a place to work or receive treatment % of staff having well-structured appraisals in last 12 months Staff motivation 2% 3% 6% 4% +4% 73% 67% 71% 67% -2% 88% 90% 83% 89% -5% 3.08 3.55 2.99 3.41 -0.09 35% 42% 24% 37% -11% 3.65 3.85 3.62 3.79 -0.03 * National average scores are for mental health / learning disability trusts. Future Priorities and Targets As set out under the commentary on page 28, improving workforce engagement is one of three core strategic workforce priorities. The Trust recognises that the previous 12 months has been a particularly difficult time for its staff in the context of an unprecedented level of organisational change to support the Trust’s Service Strategy. The majority of the required change has now been implemented, leading to a greater level of stability for most staff over the coming year. Detailed plans are being developed to support the 2014 to 2019 Workforce and Organisational Development Strategy in regard to each of the priority areas: staff engagement, flexible workforce and skilled workforce. 42 Norfolk and Suffolk NHS Foundation Trust Quality Account The focus areas for the staff engagement strategy are as set out above, which includes promoting a safe and healthy working environment. In addition to the Trust-wide approach to improving staff engagement, existing Locality Workforce Plans will be reviewed to respond to area specific priorities highlighted by the Staff Survey results. The Trust is committed to making improvements across all Key Findings as benchmarked against previous Staff Survey results and other mental health trusts. Progress will be monitored taking account of the measures set out under the commentary above. Further information about the survey, and a full breakdown of results, can be accessed via a dedicated website on http://www.nhsstaffsurveys.com. April 2014 to March 2015 Commissioners and Stakeholder Comments The comments received from commissioners and stakeholders are appreciated by the Trust and are used to inform and improve subsequent accounts. In some cases where minor changes are suggested, these have been incorporated for this year but in other cases, where more substantial changes are suggested, these have not been included but will inform change next year. It should also be noted that the Quality Account will be published separately and the layout will change accordingly. NSFT Governors ‘The comments below are submitted by representatives of the Norfolk and Suffolk Foundation Trust’s governors: Members of the NSFT’s governors have scrutinised the Trust’s 2014-2015 Quality Account. We acknowledge the care taken to gather and compile this data and are assured of its integrity. The Account analyses the key challenges facing the Trust and describes action plans and monitoring processes to deal with them. Rising demand for services have resulted in pressure on the availability of beds, whilst staffing shortages have likewise affected clinical care in the community. The reorganisation of services which took place in response to a reduction (in real terms) of funding has proved a challenge to both staff and service users. There is currently the added pressure of scrutiny by the Care Quality Commission and MONITOR. The Trust Board has assured the governors that it is striving to regain stability, whilst maintaining and improving the quality of its services. The governors acknowledge the Trust’s focus on recruitment during the current national shortage and availability of clinical staff and the difficulties in attracting staff to the area we serve. In accordance with CQC, we acknowledge the excellence, dedication and resilience of our present clinical staff. The governors continue to support the implementation of the Triangle of Care and the growth of IMROC (implementing recovery through organisational change). The governors continue to represent and communicate public opinion to the nonexecutive directors of the Trust and, when appropriate, challenge the executive strategic decisions they oversee. We aim to uphold the Trust’s ethos in its delivery of the Trust strategy. We are particularly concerned in monitoring the Board’s current Quality Improvement Plan and quality goals as described in the Quality Account. The governors appreciate transparency of the information shared with us by the Board that facilitates us in our responsibilities of representing service users, carers, staff and the public we serve. The governors continue to both challenge and encourage the Trust in its endeavour to deliver quality services in safe environments, both inpatient and to the majority of its service users living in the community. We support the priorities stated in the Quality Account in regards to provision of prompt services to people in crisis and the provision of quality care plans for all of its service users. We support the Trust’s use of service user and staff surveys and in developing a responsive and reflective complaints process. Also we exhort the Trust’s focus on physical health and its participation in national research into good practice, particularly around schizophrenia. The governors share the Trust’s determination in its continued attempt to improve the quality of patient care, dignity and respect. The governors acknowledge the Chief Executive Officer’s recognition of the challenges faced by the Trust and the improvements that have been achieved at the time of writing this response. We also appreciate and find useful the comments in the report on the Quality Account provided by both Norfolk and Suffolk Healthwatch.’ Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 43 NHS South Norfolk CCG, on behalf of the Norfolk CCGs NHS South Norfolk CCG, on behalf of the Norfolk CCGs, is pleased to support the Trust in its publication of the 2014-15 Quality Account. Having reviewed the mandatory detail of the report, we are satisfied that the Quality Account incorporates the mandated elements required, based on available data. The CCG recognises that the Trust has experienced significant challenges over 2014-15, including a new style of CQC inspection that occurred during October 2014 rating the Trust overall as inadequate. The Trust was subsequently put into ‘special measures’ in February 2015 by Monitor, the Trust’s regulator. The CCG believes that this will trigger a very significant year of change for the Trust, where turnaround is a necessity and a follow up CQC visit in about a year’s time. The CCG has been actively involved in supporting the Trust with continuous monitoring through Clinical Quality Review Meetings (CQRM’s) and supporting the Safewards work through a local Commissioning for Quality and Innovation (CQUIN) scheme for 2015-16. The Trust has an excellent history of appropriate reporting of Serious Incidents, which is indicative of its open and transparent approach around issues affecting patient safety. There is however further work that needs to be achieved in relation to ensuring that learning from these serious incidents is embedded into practice and service delivery. The Trust has always demonstrated excellent engagement and working relationships with the CCG in matters relating to patient safety and has welcomed challenges posed by the CCG in this area to ensure services are safe for patients. Throughout 2014-15 we have continued to see a number of patients who have had to transfer out of county in order to access acute in-patient care. The Trust committed to end this during 2014-15. Whilst numbers were significantly reduced, this has not yet been achieved. The CCGs note the Trust has a new 12-bed mental health assessment ward in March 2015 to help reduce out of area placements. The CCG also notes the quality priorities identified for 2015-16 and would prefer that workforce should feature within these. The 44 Norfolk and Suffolk NHS Foundation Trust Quality Account CQC identified a number of areas of concern in regards to workforce from staff morale, staffing levels, training and leadership issues which all have a direct impact on patient safety. The quality of services can be assured to be safe and responsive with a well-trained, valued and motivated staff group. The CCG looks forward to continuing to working in a positive and collaborative manner with the Trust to continue improvements in patient care during the coming year. Great Yarmouth & Waveney Clinical Commissioning Group Great Yarmouth & Waveney Clinical Commissioning Group as a commissioning organisation of NSFT supports the organisation in its publication of a Quality Account for 2014-15. We are satisfied that the Quality Account incorporates the mandated elements required based on available data. The information contained within the Quality Account is reflective of the Trust over the previous 12 month period. In our review we have taken account of the clinical quality and safety improvement priorities identified for 2015-16 and support the identified improvement objectives in the quality and safety of care provided to Great Yarmouth & Waveney residents. The Trust will do this by: Improving Patient Safety; The Trust Board’s aim is to reduce the use of restrictive interventions to below the national benchmarking average by 1 April 2016. The Trust Board’s aim is that 95% of service users admitted to a ward for more than 24 hours will receive a physical health check. Improving Patient Experience; The Trust Board will measure service user’s involvement with their care through the Service User Survey to ensure that this is at a level at or above the national benchmarking average when the 2016 results are published. Service users will be asked ‘Have you agreed with someone from NHS mental health services what care you will receive?’ April 2014 to March 2015 Improving Clinical Effectiveness; The Trust Board will actively monitor the implementation of actions arising from Serious Incident investigations and the correct application of the Duty of Candour. The CCG expects that this will result in the sharing of learning from incidents that informs changes in practice and decision making. We note that learning from incidents has been included as a priority in the Trust’s Quality Improvement Plan and that a Duty of Candour Policy has been implemented during 2014-15. Great Yarmouth and Waveney CCG also notes the quality priorities identified for 2014-15 and in particular the deterioration in feedback from patients about explanations of prescribed medications. The CCG does recognize that there may be a delayed measurable improvement due to the timings on the national surveys. We anticipate improvements within the next published survey as a result of the clinical improvements being made. The Trust has stated that, for the second year running, it has not participated in the Prescribing Observatory for Mental Health clinical audit as these were not considered to be relevant priorities of the Trust during 2014-15. The CCG looks forward to receiving the results of these audits which the Trust intended to commence in February 2015. We recognise the challenge of being placed in Special Measures by Monitor puts the Trust under great scrutiny and challenge; the CCG would like to acknowledge and commend the Trust on its openness and transparency within the Quality Account about the outcomes of the Care Quality Commission inspection in October 2014 and commitment to making the required improvements. The CCG would also like to acknowledge the areas of good practice observed during the inspection. The CCG asks that the section within the report about the Care Quality Commission inspections undertaken in 2014-15 be developed further to include a list of all services and locations inspected by the CQC with a brief overview of the outcomes. Where there has been areas of non-compliance, we request that the Trust clearly states what these consist of and what the Trust is doing / has done to address these concerns. The CCG believes that the Annual Quality Account presents the Trust with an opportunity to share with service users the significant service changes that have occurred within 2014-15 and provide an update on how these service changes continue to be monitored. Recognition of patient engagement and the voice of the service user are requested to be included. The Great Yarmouth & Waveney Clinical Commissioning Group looks forward to working with the NSFT during 2015-16. Healthwatch Suffolk The CQC inspection of the Norfolk and Suffolk Foundation Trust in October 2014 raised some significant concerns about performance. This quality account reflects some of these challenges and sets out plans to address the issues raised. It is imperative that services are well-led and this requires staff at all levels to communicate openly and effectively without fear of reprisal. It is evident that some staff have not felt valued or listened to by senior staff. Feedback on 2014-15 Quality Priorities For a number of these priorities, progress is limited or there is insufficient data yet available to judge how much progress has been made. This seems to be recognized in particular for priorities 1 and 3 which essentially continue in 2015-16. Evidence of adequate progress on priority 4 (small audit, limited improvement on care plans), priority 5 (introduction of a form but has the staffing issue been resolved?) and priority 6 (how widely is the TOC tool used?) is also lacking. On priority 7 the scale/reliability of the audit in March 2015, reporting improvements in service user involvement in their medication planning, is not described. On priority 8, Healthwatch Suffolk, while recognizing that there were particular problems during the period of major service restructuring, is by no means convinced that the ongoing problem of continuity in care coordination is one confined to Norfolk. We would like to see more evidence that this problem is being overcome by ensuring adequate training, organisation and resourcing of teams within the Trust. This priority is Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 45 related to the 2015-16 Patient Experience priority on service user involvement in care planning which it is suggested could be widened to address the care continuity aspect. On priority 2, the waiting times as of 31st March show that mandatory requirements are almost being achieved and it is to be hoped that at least this level of performance will be consolidated. The results of a Healthwatch Suffolk survey of the Access and Assessment Service in 2014 show that service users were generally satisfied with the amount of time they had to wait to book an appointment within the Trust. However, service users were still concerned at waiting times for subsequently receiving treatment with almost 9 out of 10 service users still waiting at the time they were polled, often also lacking adequate communications on what was happening. Quality priorities 2015-16 The proposed quality priorities make reference to meeting national benchmarking averages. Many readers however will not know what these are and they need to be spelled out and enumerated in the text. The priority descriptions are very short and technical. Reference to the Trust Quality Improvement Plan (a separate document) is actually necessary to be able to understand what is intended. Précised text from the latter should be added to provide a fuller description for each priority. Patient experience - Quality improvement plan reference RE6 It is notable that response rates to the Family and Friends Test (FFT) have declined and therefore it is questionable how representative these views are of the organisation as a whole. Healthwatch Suffolk would therefore encourage the Trust to seek more innovative ways of gathering this data. It is also evident that improving staff engagement must be a priority for the Norfolk and Suffolk Foundation Trust. The staff survey FFT falls below that national average, indicting a lack of confidence by staff in the trusts ability to deliver acceptable services, again the response rates remain low. 46 Norfolk and Suffolk NHS Foundation Trust Quality Account Healthwatch Suffolk’s project exploring patient experiences of accessing the Norfolk and Suffolk Foundation Trust services via the Access and Assessment Team (AAT) indicate that there remains confusion about processes within the trust, this may be in part due to the reorganisation of services, but reflects the need for better communication with patients to avoid stress and anxiety at the point of entry into or between the Norfolk and Suffolk Foundation Trust services which was highlighted during Healthwatch telephone interviews. Experiences reported to Healthwatch Suffolk also highlight a lack of consistency in staff seeing patients, a sense of uncertainty about the purpose of interventions, limited co-production of care plans with patients, a lack of information and support for carers and in some cases such a lack of compassion and understanding that patients and their carers came away feeling worse after appointments. Many of these concerns are indicative of resourcing problems and / or poor management. However, while benchmarking against the 2016 service user survey is a good idea, we are concerned at the delay involved before this feedback is obtained. We suggest that additional means of monitoring progress are identified to provide nearer term, and ongoing, feedback on service user experience. The CQC did not dispute in its inspection that the Norfolk and Suffolk Foundation Trust’s staff are, on the whole, caring. This is backed up by the Healthwatch Suffolk Survey which shows 92% of patients agreeing that they had been treated with respect and dignity at all times and 76% feelings that their views were listened to, although there is room for improvement. It appears that around half those surveyed had not actually commenced the treatment they require. The Quality Improvement Plan more widely addresses the quality of services delivered by Community teams including the implementation of the Waves model and a crisis support line for service users with personality disorder. Lack of provision for personality disorder has been a key concern flagged to Healthwatch by services users and we would like to see an additional priority defined to cover this area under the `Patient Experience` heading. More generally, the issue of Crisis Care has been an area where service users have raised April 2014 to March 2015 serious concerns in the past with both Healthwatch Suffolk and Suffolk User Forum and dialogues with senior Trust staff have led to various initiatives and pilots, carried forward under the Crisis Concordat, and we would like to see final implementation and embedding of these developments as a key priority for 2015-16. Key aspects are: • an appropriate place of safety for service users in crisis to go to which is not a police cell, even when under the influence of alcohol or drugs • psychiatric liaison available in all A&E departments in timely fashion – say within one hour • a 24/7 Suffolk wide crisis telephone line manned by suitably trained and empathetic staff • proactive planning of community care to avoid relapse after crisis and, where necessary, to enable rapid return to secondary Norfolk and Suffolk Foundation Trust care to avoid serious deterioration of health Patient safety - Quality improvement plan reference SA4 We fully support the CQC view that ““Use of restrictive interventions will reduce to below the national benchmarking average by 01.04.16” is an essential priority. The target that 95% of service users admitted to the ward where they stay for more than 24 hours will have a physical health check is welcomed, given the risks of comorbid long term conditions, however a timescale should be associated with this objective and any steps taken and planned should be recorded in the Care Plan. Clinical effectiveness - Quality improvement plan reference SA9 The priority that “all locality governance groups are able to demonstrate that learning from incidents has led to changes in practice by 01.10.15” appears focused on reducing Serious Incidents and complaints and is certainly an area of improvement that we would support. The question is however what will be the measure as to whether a sufficient change in practice has been achieved by the date indicated? Would this be that all relevant staff will report a debriefing has taken place following a serious incident and identify what they have learnt? The CQC identified concerns about the ability of staff to learn from complaints and incidents and whilst a plan to improve this is now in place, this will require a whole system approach that ensures transparency and changes to the way in which staff view, manage and learn from complaints. Additional comments The draft text lacks both a contents page, laying out the general structure of the document, and a numbering scheme making it difficult to identify the context of individual sections. The document is also full of jargon and is essentially structured to meet internal NHS reporting requirements. It is not, in its present form appropriate for service users, carers or the general public. While it is appreciated that the Trust is required to report to a certain format it is suggested that a more readable document could be achieved by making greater use of charts and diagrams to present information and highlighted text boxes on each page to summarise main points in simple language. It is also strongly recommended that the Trust produce a shorter `easy read` version of the final Quality Account, specifically designed for service users and carers, in order to reach a wider stakeholder audience. It was pleasing to read about the success of the Recovery College and the improvements to the Improving Access to Psychological Therapies (IAPT) services, which also includes service user involvement and improved methods of access. There is evidence of service user involvement in the planning of services, such as the learning disability forums and some positive examples of innovative and collaborative approaches to delivering services was evident. The CQC has highlighted some areas of excellent practice and other areas where significant improvements must be made. Ensuring that staff voices are heard and that their views are acted upon to improve services is essential, as is the on-going involvement of patients and their carers in the planning and Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 47 delivering of services to ensure that services are responsive to the needs of the local population in Suffolk. Where innovative staff have developed new initiatives and tools these could be shared more proactively across the trust. Healthwatch Suffolk looks forward to seeing the Norfolk and Suffolk Foundation Trust achieve its goals for the coming year and is eager to work with the Trust in helping it to achieve those goals. Healthwatch Norfolk Healthwatch Norfolk appreciates the opportunity to make early comments on the Quality Account in order to influence the substance of the report. We also appreciate the increased pressures on NSFT from reduced funding, rising demand and external inspection; and are particularly concerned that increased pressure to meet particular targets detracts from the wider objective of providing the best service for users. Patient safety We agree that reducing seclusion and restrictive intervention is a key priority but ask that the potential knock-on effect on incidents is carefully analysed. Monitoring physical health is also a key priority but as part of a general concern about treating the whole patient with potentially a combination of mental, physical and social care needs. We are particularly concerned that with the pressure on beds and the need to move patients between services, that this bigger picture may be lost by over-emphasis on a particular target. Meeting the 95% target for physical health but missing some in the 5% category with significant physical health problems would not constitute success. Patient experience Clinical effectiveness We agree the importance of demonstrating learning from incidents by changing practice where relevant. Feedback on Quality Priorities 2014-15 Ensuring that 100% of patients are seen within the number of days stated in the contract and that patients are correctly allocated to the various priority queues remains a key priority. Will an Executive Director be responsible for this target? The follow-on in 2015-16 from the priority 4 (being able to contact a mental health worker out of hours) is not entirely clear. • Is the service only available to users with a crisis plan? • Will the service be available in Norfolk throughout 2015-16? • Will the service be available at weekends? • What are the contingency arrangements for users, carers and members of the public not covered by the service? We will continue to work with the Trust to ensure that the views of patients, carers and their families are taken into account and to make recommendation for change where appropriate. Health Overview and Scrutiny Committee The Norfolk Health Overview and Scrutiny Committee has decided not to comment on any of the Norfolk provider Trusts' Quality Accounts for 2014-15 and would like to stress that this should in no way be taken as a negative comment. The Committee has taken the view that it is appropriate for Healthwatch Norfolk to consider the Quality Accounts and comment accordingly. We agree the importance of involving users, and where relevant their carers, in their care plans while also seeking that 100% of users actually have a care plan. 48 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 Key and glossary AAT BMI CAMHS CPA CQC CQUIN CRHT DH IAPT IPAC KPI LIPACS NCE NCISH NHSLA NICE NPSA NSFT NWMHFT PALS PbR PC-MIS PEAT PET PLACE POMH QRP RAPt RCA SCR SI VTE Access and Assessment team Body mass index Child and Adolescent Mental Health Service Care programme approach Care Quality Commission Commissioning for Quality and Innovation Crisis resolution and home treatment Department of Health Improving access to psychological therapies Infection prevention and control Key performance indicator Local infection control prevention and control supporter National confidential enquiry National confidential enquiry into suicide and homicide for people with mental illness NHS Litigation Authority. National Institute of Health and Care Excellence National Patient Safety Agency Norfolk and Suffolk NHS Foundation Trust Norfolk and Waveney Mental Health Foundation Trust Patients’ Advice and Liaison Service Payment by results Patient case management information system Patient Environment Action Team Patient experience tracker Patient led assessment of the care environment Prescribing Observatory for Mental Health Quality and risk profile Rehabilitation of Addicted Prisoners Trust Root cause analysis. Serious case review Serious incident Venous thrombo embolism How you can get involved As a member of Norfolk and Suffolk NHS Foundation Trust, individuals can help shape the way the Trust plans and provides mental health services in Norfolk and Suffolk. Membership is free, and members will receive regular information about the Trust’s plans and developments. They will be invited to public meetings and receive a copy of our newsletter, Insight. Members are also able to stand for election as a governor, or vote in our annual governor elections. Join now by calling 0870 707 1647. Alternatively, visit www.nsft.nhs.uk to sign up on line. Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 49 50 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 Norfolk and Suffolk NHS Foundation Trust Quality Account April 2014 to March 2015 51 Norfolk and Suffolk NHS Foundation Trust Norfolk and Suffolk NHS Foundation Trust Hellesdon Hospital Drayton High Road Norwich NR6 5BE Tel: 01603 421421 Web: www.nsft.uk Norfolk and Suffolk NHS Foundation Trust values and celebrates the diversity of all the communities we serve. We are fully committed to ensuring that all people have equality of opportunity to access our service, irrespective of their age, gender, ethnicity, race, disability, religion or belief, sexual orientation, marital or civil partnership or social & economic status. If you would like this leaflet in large print, audio, Braille, alternative format or a different language, please contact PALS and we will do our best to help. Email: PALS@nsft.nhs.uk or call: PALS Freephone 0800 279 7257 © 2015 NSFT. All rights reserved. NSFT Comms/15/016. GFX 3770 Quality Account 2014-15