Document 11206655
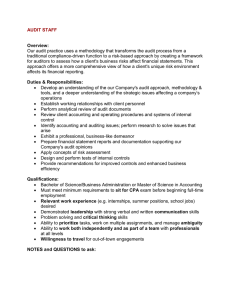
advertisement

Contents Section 1 Section 2 Section 3 Goal 1 Goal 2 Page 1.1 Introduction to Quality Account 4 1.2 Statement of Directors 5 1.3 Foreword from the Chief Executive 6 1.4 About our Services, Our Mission, Vision and Values 10 1.5 Executive Summary 12 Our Quality Priorities 2.1 Achievements 2013/2014 28 2.2 Priorities for Improvement Areas 30 2.3 Governance Statement 31 2.4 Our Quality Priorities 34 2.5 Quality Aspirations and Goals 39 Our Progress 3.1 Performance 2013/2014 42 3.2 CQUINs 43 3.3 A year on from Francis 44 3.4 Introduction to progress of Quality Goals Measurable year on year improvement in every area of patient safety in community services. Safe Care Deliverables 45 Infection Prevention and Control 49 Harm Free Care 53 Pressure Ulcer Prevention and Management 55 Venous Thrombo-embolism 58 Falls Prevention and Reduction 59 Patient Safety Walkabouts 62 Safeguarding 64 Early Warning Trigger Tool 68 Safe Medicines Management To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time. Transfer of Care 69 Improving End of Life Care 75 Page 2 of 153 47 73 Morbidity and Mortality 78 Acute Pain 80 Dementia 82 Children & Young People 85 National Institute for Health & Care Excellence Measurable year on year improvement in patient experience, engagement and satisfaction. Improving Patient Feedback 91 Improving Nutrition and Hydration 97 CNO Caring with compassion strategy 100 Improving Health and Wellbeing 102 Promoting a culture of accountability and openness. Information Governance 107 Clinical Audit 110 Research 115 Serious Incidents 117 Understanding Claims 119 Care Quality Commission 121 Improving delivery, capacity and capability in all areas. Improving Clinical Education and Standards 124 Workforce 127 Transformation 132 Summary of Responses 135 Appendix A Progress on Francis 142 Appendix B CQUINs schedule 148 Appendix C Audit Examples 149 Goal 3 Goal 4 Goal 5 Page 3 of 153 93 SECTION 1 1.1 What is a Quality Account? Quality Accounts are annual reports that all providers of NHS services in England have a statutory duty to produce to the public about the quality of services they deliver and their plans for improvement. The purpose of the Quality Account: Public accountability is increased and quality improved within NHS organisations so that the public can hold providers to account for the quality of services they deliver. Patient and cares can make informed choices about their providers of healthcare. Boards of providers review their performance over the previous year, identify areas for improvement, and publish that information, along with a commitment to you about how those improvements will be made and monitored over the next year. The three important quality improvement areas: Patient safety Clinical effectiveness (how well the care provided works) Patient experience (how patients experience the care they receive) Some of the information in a Quality Account is mandatory but most is decided by patients and staff. This Quality Account contains information about the quality of our services, the improvements we have made during 2013/14 and sets out our key priorities for next year. This report includes the comments of our external stakeholders on how well they think we are doing including: Clinical Commissioning Groups Kent County Council Healthwatch Kent Page 4 of 153 1.2 2013/14 Statement of Director Responsibilities in Respect to the Quality Report The Trust’s Directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations 2010 to prepare Quality Accounts for each financial year. National guidance has been issued on the form and content of annual quality accounts (which incorporate the above legal requirements) and on the arrangements that Boards should put in place to support the data quality for the preparation of the Quality Account. In preparing the Quality Account, directors are required to take steps to satisfy themselves that the content of the Quality Account meets the requirements set out. The content of the Quality Account is not inconsistent with internal and external sources of information including: Board minutes and papers for the period April 2013 to March 2014 Papers relating to quality reported to the Quality Committee over the period April 2013 to March 2014 Feedback from commissioners – May 2014 The Trust’s complaints reports 2013/14 The national staff survey 2013/ 2014 CQC quality and risk profile 2013/14 Feedback from governors Feedback from Healthwatch organisations – May 2014 The national patient survey 2013 The head of internal audit‘s opinion over the trust’s control environment dated 2013/14 The performance information reported in the Quality Account is reliable and accurate There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Account has been prepared in accordance with 2013/14 reporting guidance (which incorporates the Quality Accounts regulations) The Directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Account. Page 5 of 153 1.3 Foreword from the Chief Executive Welcome to our third Quality Account from Kent Community Health NHS Trust (KCHT). This publication describes just how seriously we consider quality and safety issues and how we continually work to improve care to patients and families. We want to make users confident of the quality of our services and we aim to continue to deliver the very best healthcare to people in the community and closer to home. The quality account is one of the most important documents that we publish each year and sets out the priority areas that we need to focus on. These have been identified by patients, staff and partner organisations. By comparing ourselves with other organisations we can identify areas where we can further improve and consistently deliver high standards of care. This includes communication with our patients, relatives, commissioners and partner organisations. We also need to ensure that our staff have the right skills and competences; we are able to contribute to plans and have the right capacity to fulfil our role within the health and social care system. Care regulations have been amended and are reflected in this account. To ensure that the Trust responds to central changes we closely follow Department of Health requirements and respond positively to the recommendations in national publications, as well as listening and responding to what our staff, patients and commissioners say. In this document we outline the progress that we made in 2013/14 and areas where we need to improve further. This year we have developed our Quality Strategy which clearly sets out the four quality aspirations which we will be aspiring to achieve, underpinned by a well-led, open culture. 1. 2. 3. 4. Equal partnerships between patients, their families and the delivery of KCHT services which respect individual needs and values and demonstrates care, compassion, continuity and shared decision-making. There will be no avoidable injury or harm to people who receive KCHT services and a safe, clean environment will be provided at all times Treatment, interventions, support and services will be appropriate and effective, provided at the right time, by the right person with the right skills and wasteful and harmful variation in care will be eradicated. A culture of transparency and openness through learning, sharing and innovation. This will be a cornerstone in driving and sustaining excellent care, through robust governance, leadership and accountability at all levels. Underpinning the quality aspirations will be the priorities for improvement in 2014/15 which were agreed following discussions with our patients, staff, shadow governors, Trust members and partners and reflect what was important to them. The quality goals for Page 6 of 153 2014/15 focus on the three pillars of patient safety, clinical effectiveness and patient experience and the continued need to develop our staff and our culture. We recognise how important it is for us to continue to build on our partnerships with our commissioners and GP colleagues, all providers, the county and district councils, the voluntary sector and our communities in order to make a real difference to people’s lives and experience of the wider health economy. We work closely with the people who use our services and their carers and families. With their involvement and that of our Trust shadow governors and members and voluntary groups we are working together to improve services. This year has seen many improvements in the Trust including new models of care which have resulted in the restructuring of most of our teams. It has been a challenging time for staff but they have worked hard to implement initiatives which are designed to improve quality and you will find many examples detailed in case studies in this Quality Account. Our work with our partners to deliver integrated care pathways and to achieve the best possible outcomes for patients has been recognised by the Department of Health which chose Kent as one of fourteen pioneers in the country to take forward the integration of health and social care. The Trust has made favourable progress during the past 12 months, although we still need to continue to make improvements. There is more work to be done in reducing patient harms, such as pressure ulcers and medication errors; we need to improve recruitment and retention of staff, staff competencies, mandatory training and staff morale. It is also critical that patients, their families and members of staff at whatever level they work, should feel confident to raise concerns within a safe environment and that something will happen as a result. It is the most basic ingredient of our duty of care. We will spend more time talking with staff, through organised listening events, informal walkabouts and team meetings to support a more open culture. It is critical that we focus on the culture of the organisation and ensure that it is founded on the Chief Nursing officer 6Cs; care, compassion, courage, communication, competence and commitment. It has been a key priority for 2013/14 and will be a high priority for next year to ensure that we encourage a culture within the Trust where everybody feels able to provide first class care every time, for every patient and their family. We want to continue to be open and to learn when things go wrong and ensure that all staff have the required competence to deliver what is expected by patients and their families. We need to ensure good communication and treat everybody with compassion and with a commitment to always do the best that we can. Page 7 of 153 The Trust has a clear vision and value-based framework to ensure that strong leadership, at all levels, remains key to realising our vision. There is a continued emphasis on leadership and management at every level of the organisation. We also recognise the need for a culture that permeates every level of the organisation. We want to recruit and retain the highest quality of staff and invest in their continued development, so they can reinforce the standards and commitment to quality patient care. We recognise there is still further work to do and we will continue to build our standards and value base supported by robust appraisals. Turnover has remained a key issue but this has been expected in a year of transition and change. We will monitor this closely and take action to address any particular areas of concern. We have focused on reducing the number of days lost to sickness absence this year as we see this as an important way to improve quality of life and reduce costs. It will continue to be a focus of activity next year. We continue to reduce further the numbers of hospital acquired infections. In 2013/14 we had the lowest numbers of Clostridium difficile ever. However, recognising that one is too many, we continue to scrutinise every case to ensure learning to prevent these infections. We also had a major focus on reducing the number of pressure ulcers and we have increased the number of teams with reduced incidents of pressure ulcers. We still have teams that need to improve and unfortunately this meant that we exceeded our trajectory. The Director of Nursing and Quality continues to work with clinical teams to understand the causes and put in measures to do all we can to drive down incidences. 2014/15 is going to be an extremely challenging but also exciting year for the Trust. We are committed to improving patient and staff experience in all aspects of our performance. We will be assessed by the Care Quality Commission in June 2014. The assessment will focus on whether our services are safe, effective, caring, responsive and well-led. In 2014/2015, the cost improvement programme will be a challenge. We are confident our quality and transformation plans will enable us to reduce costs and to continue to deliver effective and efficient services to meet current and future demands. Our progress against the quality goals in 2014/15 will be monitored by the Board and reported through our governance systems, especially the Quality Committee which reviews information and performance of local teams through to the board on a monthly basis. I want to take this opportunity to thank all our staff for continually striving to improve the care that they deliver; staff and service users for providing valuable feedback on our services as well as colleagues for their continued partnership working. Page 8 of 153 Declaration The Chief Executive should be the accountable officer for the Trust and that responsibility includes accountability for clinical governance and hence the quality and safety of care delivered by the Trust. The information in this Quality Account is provided from our data management and our quality improvement systems and to the best of my knowledge is accurate and provides a true reflection of our organisation. Marion Dinwoodie Chief Executive Page 9 of 153 1.4 About our Services Kent Community Health NHS Trust is one of the largest providers of NHS care in patients’ homes and the community in England. We provide care for patients in their own homes and in other locations, including GP surgeries, nursing homes, health clinics, community hospitals, minor injury units and children’s centres. Our 5,400 strong workforce includes doctors, community nurses, dieticians, health visitors, dentists, podiatrists, occupational therapists, physiotherapists, family therapists, clinical psychologists, speech and language therapists, radiographers, pharmacists, health trainers, health improvement specialists and many more. Our services are commissioned by clinical commissioning groups, local authorities and NHS England, mostly in Kent, but also in neighbouring areas. The Trust provides services for children and adults to support them to stay healthy, manage their long-term health conditions, help them avoid going into hospital and, when they have needed to be in hospital, help them to get home quickly. Advice and support for children’s emotional and physical health and wellbeing is available from a range of services, including health visitors, by attending one of the Trust’s parenting support groups in children’s centres or from our school-based nurses. Our health and wellbeing services support people to make positive lifestyle choices. Help is available to increase exercise, eat healthily, quit smoking and assist with wider health and social needs. Sexual health services encourage safe sex and provide contraception, family planning and treatment. If people do become ill and need treatment, there are seven minor injury units across Kent, which treat a range of minor illnesses and injuries. We also provide emergency and specialist dental treatment, wheelchairs and other specialist equipment. A range of specialist services, including physiotherapy, podiatry, orthopaedics and chronic pain are provided in the community so that people can get treatment close to home. Nursing and therapy teams provide care in people’s homes and help in managing longterm conditions, so they don’t have to go into hospital unnecessarily. We have a rapid response service 24-hours-a day, seven-days-a-week where experienced nurses, following a request from a GP or other health professional, assess a patient’s needs within two hours and put a package of care in place to enable the patient to stay at home rather than go to hospital. Page 10 of 153 More complex care for people, who otherwise would have needed to go into hospital, called step-up care, is also provided in the county’s 12 community hospitals. If people do need in-patient care in an acute hospital, for example while recovering from an illness, our staff support people to get back home by providing rehabilitation at home and in community hospitals. We provide specialist care in the community, for example for seriously ill children or rehabilitation following a serious illness or injury and provide care for disabled children and adults. For more information about the Trust’s full range of services please visit our website www.kentcht.nhs.uk or contact us using the information on the back of this report. Our Mission, Vision and Values Our mission is to provide high-quality, value for money community-based services to prevent people from becoming unwell, to avoid people going into hospital or to leave earlier and to provide support closer to home. Kent Community Health NHS Trust’s vision is to be the provider of choice by delivering excellent care and improving the health of our communities. We will achieve this through these five core values: Caring with compassion Listening, responding and empowering Leading through partnerships Learning, sharing and innovating Striving for excellence. Our Strategic Goals Preventing people from becoming unwell and dying prematurely by improving the health of the population through universal targeted services. Enhancing the quality of life for people with long-term conditions by providing integrated services to enable them to manage their condition and maintain their health Helping people recover from periods of ill health or following injury through the provision of responsive community services. Ensuring that people have a positive experience of care and improved health outcomes by delivering excellent healthcare. Ensuring people receive safe care through best practice. Page 11 of 153 1.5 Executive Summary This is our third Quality Account as Kent Community Health NHS Trust. It details our achievements against the key areas of quality improvement set for 2013/14 and where we need to make further improvements. In the last twelve months the Trust has made good progress in delivering high quality care, however there is more work to be done in 2014/2015. Our staff have worked hard to reduce harm to our patients and have received training in a range of topics that support safe, person-centred care. We have implemented the Quality Strategy and held a range of staff engagement events. Preparation for CQC visits was undertaken through a programme of visits and along with an Early Warning Trigger Tool, has helped to identify further areas for improvement. Care strategies for dementia, end of life care and acute pain have been developed and awareness of issues important to patients, carers and staff have been raised. We still need to continue to make improvements in areas such as pressure ulcers, wound management and medication errors, we need to improve recruitment and retention of staff, staff competencies, mandatory training and staff morale. It is also critical that patients, their families and members of staff at whatever level they work, should feel confident to raise concerns within a safe environment and that something will happen as a result. It is the most basic ingredient of our duty of care. We will spend more time talking with staff, through organised listening events, informal walkabouts and team meetings to support a more open culture. It is critical that we focus on the culture of the organisation and ensure that it is founded on the Compassion in Care Strategy. This has been a key priority for 2013/14 and will be a high priority for next year to ensure that we encourage a culture within the Trust where everybody feels able to provide first class care every time, for every patient and their families. Performance and progress in 2013/14 against each goal will be summarised. The key improvement areas for 2014/15 are detailed in the main report. Page 12 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in Community Services Quality Goal 1 2013/14 HCAI Infection control Overall Performance against Goals Improvements required 33% Reduction C Diff on 2013/14 Target Achieved 40% Zero MRSA 2013/14 Hand IPC CAUTIs MRSA Hygiene Mandatory and UTIs Screening Compliance Training 50% 100% 95% 95% reduction Not fully achieved 99% 1 case 82% 73.6% Achieved Good progress has been made achieving a 40% reduction in C.diff and a 50% reduction in CAUTIs and UTIs. There was one case of MRSA bacterium attributable to KCHT this year and MRSA screening compliance was below 100% for 3 months. Overall there are areas where we have not performed as well this year with Hand Hygiene and Infection Prevention training below the compliance target. Our PLACE results were low compared to the National average. The Trust recognises these are priority areas and there are improvement actions in place to ensure patient safety. Cleanliness Food and Hydration Privacy, Dignity and Wellbeing Condition and Appearance National Results 95.74% 84.98% 88.87% 88.75% KCHT Results 88.94% 86.05% 81.78% 77.89% Quality Goal 1 2013/14 Harm Free Care Overall Performance against Goals Achieved Target to Achieve National 95% HFC Target to Achieve 95% New Harms Achieved 98% We have performed very well in the delivery of harm free care and have been above the national and regional average consistently throughout the year. We have seen a 2.5% reduction in harms compared to the 2012/13 position. Quality Goal 1 2013/14 Falls Performance 10% Reduction in all against Falls Aims/Objectives Achieved 7% 10% Reduction in Falls with Harms 14% Reduction in Falls Leading to Fractures 42.85% Falls have reduced considerably and in the community hospitals there has been a significant reduction in falls with harm. We have seen a 42.85% reduction in the number of falls resulting in a fracture. There was an average of 6.85 falls per 1000 occupied bed days Page 13 of 153 (OBD) for 2013/14 which compares favourably against the national benchmark of 8.6 falls per 1000 OBD for community hospitals (NRLS benchmarking data 2010). Performance Zero Avoidable Quality Goal 1 Grade 3 AND 4 against 2013/14 Aims/Objectives Pressure Ulcers Pressure Ulcer Prevention and Management Improvements required 57 Reduction in Pressure Ulcers by 20% of Poor Performing Areas 81% of Teams Achieved Zero Aspirant Foundation Trust Benchmark 20.9 KCHT Average Monthly Attributable Avoidable 12.7 There has an overall reduction in the numbers of pressure ulcers within KCHT. However the zero avoidable grade 3 and 4 pressure ulcers target was not met. 81% of teams (including Long Term Services, intermediate care, podiatry and community hospitals) achieved zero. 7% of teams had one pressure ulcer and sustained improvement and 12% had two or more. Work has begun in teams where there have been avoidable pressure ulcers and we will continue to ensure quality improvements are sustained. Good practice has been identified; actions taken in response included an easy access guide to the prevention and management of pressure ulcers; leaflets for formal and informal carers on prevention of pressure damage; eLearning for Waterlow (risk assessment tool) and implementation of the Quality Nurse Indicators. A strengthened Tissue Viability Team is now in place and will be led by a Nurse Consultant. The reduction of pressure ulcers remains a high priority for the Trust and we proactively develop initiatives to raise awareness of risks and to prevent harm. Quality Goal 1 2013/14 Performance against Aims/Objectives 100% of VTE Assessment Completed within 24 hours VTE Achieved 97% Our average compliance for the assessment of venous thrombo-embolism risk (VTE) within 24 hours of admission was 97% and we will continue to aim for 100%. All staff have been trained and competency assessed and no patient has suffered a VTE under our care. Page 14 of 153 Quality Goal 1 2013/14 Performance against Aims/Objectives Review Patient Safety Walkabouts Patient Safety Walkabouts Achieved Achieved A refreshed programme of Patient Safety Walkabouts took place in 2013/14 and a pre-visit survey was developed. Since July 2013, 324 surveys had been completed which resulted in a 54% increase in feedback by staff. Key results highlighted 5 action areas: communication, service development, IT, quality and safety and risk management. These visits have led to changes and raised awareness of the importance of the right equipment, insulin administration and team communication. Quality Goal 1 2013/14 Safeguarding Adults, Children and MCA/DoLs Performance against Aims/Objectives Improvements required Decrease in the Number of Cases Implicating KCHT Safeguarding Concerns To Improve on To Improve on To Improve Safeguarding Safeguarding on MCA Children Adults Training Training Training Position 80% Position 80% Position 79% Target 85% Target is 85% Target 85% 49 89% 80% 89% Work continues in partnership with Kent Social Care services; in the last 12 months there has been a steady increase in the number of children subject to a Child Protection Plan. This upward trend is due to a number of factors, the application of the multi-agency thresholds and statutory assessments and continued application of the Common Assessment Framework by our staff. 255 adult protection alerts were raised by KCHT and the numbers of cases where our services were implicated has risen. Nine of these were confirmed. To ensure patients under our care do not sustain harm, lessons learned have been cascaded. Awareness of the Mental Capacity Act and Deprivation of Liberty Safeguards has increased through a variety of initiatives to support frontline staff. This is a key priority area. Safeguarding training compliance was a focus for improvement in 2013/14 and although we have made progress the adult safeguarding training compliance figure has not been achieved. Continued efforts will be made to improve compliance. Page 15 of 153 Quality Goal 1 2013/14 Safe Medicines Management Performance against Aims/Objectives Improvements required Improve Medication National Target Improve Incident Reporting Flu Vaccinations Optimisation of on 2012/13 Figures 75% Medicines by 20% 16% increase 49% Not achieved Good progress has been made; safe medicine incident reports have increased by 16%. Of these incidents 87% did not result in any harm; 11% were low harm incidents and 1% were moderate harm. These predominantly related to administration errors and missed doses. A detailed action plan has been developed to help eradicate errors and prevent harm. KCHT had a successful staff flu vaccination programme with an increase in take up from 17% in 2012/13 to 49%, although significant progress was made we did not meet the national target. Performance against the agreed metric for 2013/14 to improve optimisation of medicines by 20% was not achieved. The Trust has developed a medicines optimisation strategy which has 6 overarching objectives and includes measurable key performance indictors to ensure progress can be monitored in 2014/15. Quality Goal 1 2013/14 Early Warning Trigger Tool Performance against Aims/Objectives Implement the Early Warning Trigger Tool across all services Achieved Achieved An early warning trigger tool has been developed to identify teams where quality performance is deviating from expected standards and to enable help and support to be targeted, to provide a level of assurance of quality throughout the implementation of change and service redesign. This has been implemented across all services. The tool has highlighted various areas where there have been concerns in some teams and rapid support has been provided. Further work is required on the early warning trigger tool and the indicators need to be refined following its implementation and review. Page 16 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time. Quality Goal 2 2013/14 Transfer of Care Improve Incident Improving Transfer of Reporting System Performance Care by developing to Support Discharge Passport against care pathways in four Analysis of Aims/Objectives areas Transfer of Care Incidents Improvements Not fully achieved baseline Achieved Not achieved required work is in place Transfer of care is an area where patients and carers would like to see improvements. Our transfer of care policy has been implemented across all services. We have improved the reporting system which is enabling us to monitor and analyse such incidents in more detail. Work continues with other providers to develop integrated care pathways and improve the transition pathway for children moving into adult services. Progress has been made and we will continue to build on what we have achieved. There were 697 transfers of care incidents from external providers of which 46% were related to pressure ulcers and 25% were related to admission, transfer and discharge issues. Internally, the majority of transfer of care incidents involved medication. We will be prioritising this area during 2014/15 to ensure we improve the transfer of care process for patients, carers and staff. Quality Goal 2 2013/14 End of Life Performance against Aims/Objectives Achieved Develop an End of Life Strategy Achieved To w ork with our h ospice c olleagues Achieved 90% of Patients Die in their Preferred Place Achieved We have made significant progress in End of Life and developed an End of Life Strategy with key stakeholders including patients, carers, the public, our staff and Hospice colleagues for both adults and children. The focus is on ensuring our workforce has the skills and competency required to deliver safe effective care. The significant national review of the Liverpool Care Pathway has resulted in the phasing out of the LCP and a greater emphasis on the development of individualised care plans for each patient. Policies and procedures have been updated throughout the year. Page 17 of 153 Quality Goal 2 2013/14 NICE Performance against Aims/Objectives Achieved Technological Appraisals to be 100% Compliant Achieved Twenty-eight quality standards were issued for 2013/14 of which 22 were relevant to our services along with 30 guidelines. A group has been set up with key stakeholders to receive, review and agree actions; this group includes patient and public representatives. Quality Goal 2 2013/14 Acute Pain Performance against Aims/Objectives Achieved Pain Audit Achieved In response to patient feedback effective management of acute pain was identified as a developmental goal for 2013/14. A pain audit highlighted that in 94% of cases a holistic assessment was undertaken within 24 hours of first contact. An assessment of pain was included and evidence showed that previous effective pain management was discussed with patients. Medicines management teams have developed training packages for staff and we now have a pharmacist on call 24 hours a day over 365 days to support and advise staff on the management of pain. Quality Goal 2 2013/14 Dementia Performance against Aims/Objectives Dementia Strategy Achieved Achieved Dementia Awareness Training Across All Community Hospitals Achieved Ensuring that we address the needs of the growing number of people with Dementia was a developmental goal and we have made excellent progress this year. We have developed a Dementia Strategy and an associated care pathway. Dementia Support Nurses led by a Nurse Consultant have delivered training and raised awareness with staff from a wide range of services and disciplines across the Trust. Staff attending training sessions fed back that they felt confident in recognising the early signs of dementia and how to communicate with a person with dementia. Page 18 of 153 Quality Goal 2 2013/14 Children and Young People Increase the Number of Families Performance Offer of Universal Benefitting from Services across against Family Nurse Kent Aims/Objectives Partnership Programme Successful expansion 100% achieved Roll out the Early Intervention and Prevention Models Achieved There has been considerable progress made within Children and Young People’s services. The Trust has received further investment for expansion of the Family Nurse Partnership programme to provide intensive early parenting support for 250 teen parents. Health Visiting services have achieved a 100% offer of universal services and these are now Health Visiting Lead roles for domestic abuse and perinatal mental health, supporting over 200 families with children under 5 experiencing domestic abuse. The Active Baby programme supporting cognitive development and positive parenting has been rolled out across the teams and early years’ settings. Our School Nursing teams were the best performing in the SE Coast region achieving high uptakes of immunisations and growth measurement, and winning national recognition for a multi-agency toilet training project. Children’s integrated therapy services have extended into East Sussex and implemented regular assessment clinics for all disciplines to meet referral targets; urgent referrals are now allocated and seen within two weeks of referral. Quality Goal 2 2013/14 Morbidity and Mortality Performance against Aims/Objectives Achieved Strengthen Morbidity and Mortality in Community Hospitals Achieved Progress has continued throughout the year and following a review of end of life care More Care Less Pathway (2013) and the Francis report, a procedure to review all deaths within the 12 community hospitals is in place. 90% of deaths related to patients who were admitted for end of life care and 10% were patients whose death was unexpected. No cause for concern was found in their care and treatment. Key findings from the reviews have been included into on-going action plans. Audits of The Deteriorating Patient Policy and Resuscitation were completed. As a consequence a review of the competency-based training on Basic Life Support, was completed resulting in the inclusion of management of the deteriorating patient, team communication and revision of the National Early Warning Score (NEWS) competency framework. Further work is required to ensure the audit recommendations and actions are embedded into practice to safeguard patients. Page 19 of 153 Goal 3: Measurable year on year improvement in patient experience, engagement and satisfaction. Quality Goal 3 2013/14 Performance against Aims/Objectives 20% of Patients undertake Friends and Family Scores and Achieve a Result of +80 per month on the Net Promoter Score Over 95% Patient Satisfaction in all Service Areas using Meridian Surveys and at least 15% Coverage Achieved B Achieved Improving patient feedback Stakeholder Engagement Increase by 15% Achieved The Trust captures patient feedback in real-time using iPads with ‘Meridian’ software. Feedback is consistently positive with around 1 complaint for every 10,000 patient contacts. The number of complaints increased to 362 compared to 301 in 2012/13 in common with other Kent trusts. This may reflect increased publicity about how to complain as we encourage people to give their feedback so that we can learn from it and improve patient experience. Learning from complaints has inspired changes to several referral, appointment and communication processes. The Trust’s overall patient experience score this year is 95% and we can be assured that overall most patients have a positive experience. We are one of the first trusts to introduce the NHS Friends and Family Test. KCHT’s overall score is positive and above the benchmark for aspirant Community Foundation Trusts The Trust has also made significant progress in actively engaging with stakeholders and exceeded the targets for 2013/14. Quality Goal 3 2013/14 Improve Nutrition and Hydration Performance against Aims/Objectives Implement Nursing Indicators in 100% of Community Hospitals including Nutrition and Hydration and Pain Indicators Achieved Achieved Evaluate and Action the Results of the Hydrant Project Achieved The Trust has an on-going commitment to ensuring patients receive the best nutritional support and has established a Nutrition and Hydration Group with a comprehensive action plan in place. In 2013/2014 we took part in a Department of Health pilot project that Page 20 of 153 demonstrated that a multi-disciplinary approach is needed to support hydration and has led to a variety of initiatives being implemented. A range of Nutrition and Hydration resources are available. Admission questionnaires now identify inpatient choices and new menus and drinks have been introduced across the community hospitals. Quality Goal 3 2013/14 Caring with compassion Performance against Aims/Objectives Achieved Implement the Six Areas of the Chief Nursing Officer Caring and Compassion Strategy Achieved KCHT Definition of Compassionate Care Achieved The Trust held a series of engagement events with patient, carers, public and staff to define a KCHT definition of compassionate care which was launched at our 1 st Class care Conference which was attended by the Chief Nursing Officer of England. Implementation of the Caring with Compassion Strategy is underway and a robust action plan is in place. Quality Goal 3 2013/14 Improve Health and Wellbeing Performance against Aims/Objectives Achieved 95% of Patients Asked about Smoking as Part of their Assessment Achieved 90% Offered Referral to Stop Smoking Services Achieved Healthy weight is vital for long-term health and wellbeing and can prevent long-term conditions such as hypertension, heart disease, type 2 diabetes and certain types of cancer. During 2013/2014 32,000 people had health checks with the Trust’s Health Checks Team who collaborated with GPs, pharmacies and other providers. The Stop Smoking service received on average 92% patient satisfaction and has reviewed its service model. The team has strengthened its links with Kent and Medway NHS and Social Care Partnership Trust, which has agreed to become smoke free next year. The Health Trainer service saw over 4,800 new self-referring clients, achieving excellent outcomes with 73% of all goals set being fully or partly achieved. In partnership with schools, pharmacies, community centres and GPs in areas of greatest need, the Healthy Weight team delivered specific programmes for adults with a high body mass index, families and children, providing practical help. KCHT’s integrated sexual health services enabled service users to access all the services they need in one visit with implementation of a Hub and Spoke model in 35 sites across Kent and Medway. Staff have undergone training to develop new competencies to allow them to work across the breadth of the service. Service developments include using social media to encourage patient participation. Page 21 of 153 Goal 4: Promoting a culture of accountability and openness. Quality Goal 4 2013/14 Care Quality Commission Performance against Aims/Objectives Achieved Maintain Registration of 34 Locations without Conditions Achieved KCHT is required to maintain registration with the Care Quality Commission (CQC) and has 34 locations registered. The CQC has not taken any enforcement action against us in 2013/14. We have not participated in any special reviews or investigations by the CQC during this reporting period. We continue to be registered with the CQC without conditions. The Trust has a robust assurance process that requires services and subject matter experts (in areas such as safeguarding, medicines, consent, learning and development and equality and diversity) to self-assess compliance against the CQC’s 16 Quality and Safety Outcomes. The Trust’s mock CQC inspection tools have been re-designed and are now based on the CQC’s new five domains – Caring, Effective, Responsive, Well-led and Safe. Training and awareness material is being developed to raise awareness amongst staff. The Trust will be inspected by the CQC in June 2014. Quality Goal 4 2013/14 Serious Incidents Performance against Aims/Objectives Achieved Improve Incident Implement in Full Reporting across the the “Being Open” Organisation By 10% Policy in All Incidents 7.6% Achieved Reduce the Number OF Serious Incidents Reduction of 5 In 2013/14 the Trust had total of 79 SIs compared to the 82 reported in the previous year. The largest proportion related to pressure ulcers and there have been information governance and falls serious incidents. The Trust has maintained 100% compliance with the national targets for the completion of SI investigations. The Trust has had no Never Events. Page 22 of 153 The Being Open policy and the principles of transparency and candour are embedded into the serious incident investigation process. A plan of action to ensure the organisation learns lessons from all incidents/near misses/complaints and claims to improve patient experience and patient/staff safety for the future is in place and is a key quality priority for 2014/15. Claims During the year 2013/14 the Trust had seven clinical claims. In one case we admitted the care given was not of an acceptable standard. To ensure consistently high standards of care, the clinical service held a ‘back to basics’ training day and shared the lessons learned throughout the Trust. Five clinical claims are still being investigated. We also had four non-clinical claims made against us in this period. One claim was repudiated and the other three are still being investigated. Inquests Reports on Action to Prevent Future Deaths (PFDs) place the Coroner under a statutory duty to issue a report to any person or organisation where, in the opinion of the Coroner, action should be taken to prevent future deaths. The Trust has received one such report in 2013/14. The report related to communication between healthcare providers and the holistic training of district nurses. Actions have been taken to mitigate risks in the future and lessons learned have been shared across the trust. Data Quality Effective delivery of patient care relies on good quality information and is essential if improvements in the quality of care are to be made. The Information Quality Improvement Group is driving the implementation of the Data Quality Policy, ensuring standard operating procedures and best practice is followed, data quality audits are reviewed and action plans monitored. Information Governance KCHT’s Information Governance Assessment Report’s overall score for 2013/14 was 81% and was graded satisfactory and green exceeding the previous year’s score by 6%. All requirements have met the minimum level 2 compliance and the IGTA is rated as “Satisfactory”. The work plan for 2014/15 will include continued auditing of compliance. Page 23 of 153 Audit During 2013/14 KCHT participated in 100% of the national audits which it was eligible to participate in. For 2013/14 there were no national confidential enquiries that KCHT was eligible to participate in. However, for 2014/15 there are already 3 national confidential enquiries that are relevant to KCHT. These include Lower Limb Amputation, Mortality Review and Sepsis. The Falls and Bone Health in Older People and the National Audit of Treatment & Care of HIV infected inpatients are the two national audits that were reviewed by KCHT in 2013/14 and actions to improve the quality of healthcare will be taken. For a clinical audit to be recorded as complete by the Trust every single action identified from the audit must be implemented. At the end of 2013/14 350 actions designed to improve the quality of care for our patients had been implemented. There were many areas of good practice and positive outcomes for patients. Outcomes for patients and staff are now included against all recommendations in an action plan. This encourages auditors to focus on the audit output rather than the process of action planning and managing change so there is a clear understanding of how each action from the audit will improve care for our patients. The audit programme for 2014/15 was approved by the Clinical Audit Group on 20 th March 2014 and consists of 160 clinical audits. Research and Development During 2013/14 Kent Community Health NHS Trust has participated in 45 research studies, 19 of these are classified by the National Institute of Health Research as portfolio studies. Portfolio studies are high quality clinical research studies that are eligible for support from the National Institute of Health Research Clinical Research Network in England. There was 36 clinical staff at KCHT participating in the Research Ethics Committee during 2013/14. Links have been strengthened between Research and Clinical Audit in order to contribute to increased clinical effectiveness within KCHT. Page 24 of 153 Goal 5: Improving delivery capacity and capability in all areas. Quality Goal 2 2013/14 CEST Performance against Aims/Objectives Achieved Mentorship Updates Compliance 85% Achieved Implement Person Centered Care Planning in at least 50% of Services To continue to improve The delivery of consistently high quality care requires an educated, skilled, competent workforce working to evidence-based practice standards. Significant progress has been made and a Clinical Competency Framework developed where the core domain includes holistic assessment, person-centred care planning/goal setting, record keeping and safeguarding. A clinical induction programme has been developed and focuses on standards, competencies and practice outcomes. Action learning sets enabling time reflection, sharing experiences, learning and networking are incorporated in the Trust’s preceptorship programme. In light of the Cavendish review the Trust has reviewed the Health Care Support Worker Programme and developed an associated strategy and career progression framework for implementation in 2014. There has been an increased focus on the quality assurance of education and training and on improving the quality and delivery of training sessions. In 2012/13 the compliance figure for mentorship updates was below target. It has been successfully achieved for this year. Across the organisation the level of access to clinical supervision has been variable. A review of the policy resulted in a revised framework for staff. The Trust has successfully developed a Post Graduate Certificate in Community Health in partnership with the University of Kent which will deliver essential education flexibly and at a standard equal to Higher Education Institutes. Page 25 of 153 Performance Quality Goal 5 against 2013/14 Aims/Objectives Workforce Improvements required Mandatory Training 85% Compliance in all 10 areas Reduction in Sickness Absence to 3.75% Fire and Moving and Handling Training did not Meet the Target 4.25 % Reduction in Average Recruitment Timescales from 10.5 weeks Achieved 7.6 weeks Staff Survey Results 2 % lower than National Average Training is a key priority for the organisation and fundamental to high quality care. Our mandatory training compliance figure is 85%, eight of the ten areas of training have achieved the target, however Fire training and Moving and Handling training did not meet the target. Where compliance is below 85% teams are being targeted to discuss why compliance is not being achieved and to find alternative ways of providing training. Recruitment and retention is a key focus for the Trust to increase our permanent workforce and reduce the amount of temporary staff. The Trust is recruiting staff more quickly and strong relationships with local Universities will enable us to recruit and support newly qualified clinicians. We are currently exploring the option of overseas recruitment and Return to Practice to support those areas with the most difficulties in recruiting staff. A variety of initiatives and incentives have been implemented to attract new staff into KCHT and to support retention of existing staff. The Trust has developed a framework for managers (The KCHT Manager) aligned to KCHT values and outstanding leadership and management behaviours. The Trust recognises good leadership is fundamental to the delivery of quality care. The 2013 staff survey results were disappointing in some areas but demonstrated that 73% of staff feel satisfied with the quality of work and patient care they are able to deliver which is 2% lower than the national 2013 average for community trusts. Directorates have developed action plans to address any issues raised. The Trust concerns regarding workforce and morale are a key quality priority for 2014/15. Page 26 of 153 Transformation The Transformation Team is driving forward service improvement and partnership work to support the Trust in securing quality, clinical and financial sustainability. Highlights of this work in 2013/14 were: The development of the intermediate care model, which supports people to avoid admission to an acute hospital by providing urgent support, either at home or in a community inpatient unit; A new model of more intensive support in the community; The implementation of the productive community services programme in 220 teams and the e-rostering system to ensure safe levels of staffing. The Kent Health and Social Care Integration Programme were recognised as one of fourteen Integration Pioneers by the Department of Health in 2013. Throughout the year the Trust has shared its integration work with other organisations around the UK, and presented at major national conferences. In summary, following the progress and areas for improvement identified through this quality account, the Trust will continue to achieve the five overarching quality goals and there will be six key focus areas for quality improvement which are: Improving staff morale and recruitment/retention; Learning from mistakes to improve safety; Improving the implementation of the Mental Capacity Act; Reducing the number of medication errors; Wound medicine Continue to develop integrated pathways. Page 27 of 153 SECTION 2 – OUR QUALITY PRIORITIES 2.1 Achievements in 2013/14 Harm Free Care Safety Thermometer We have surveyed 37,835 patients, achieving the Safety Thermometer target of 95% harm free care and a 2.5% reduction in all harms, above the National and Regional benchmarks. Falls 14% reduction in attributable falls for community hospital inpatients 31% reduction in falls resulting in harm and 43% reduction in severe harm falls KCHT hosted a successful Falls Conference that was highlighted in a national journal. Our award-winning Colours Reducing Falls programme is helping to identify people at risk of falling in hospital. Pressure Ulcers 81% of teams have achieved zero attributable-avoidable grade 3 and 4 pressure ulcers. Never Events No never events. Health Visiting and School Nursing Increased the number of Health Visitors by 12% to 243.71 in 2013-2014 Implementation of the Active Baby provided “champion” training to 550 health visitors, children’s centre and early year’s staff 85% children in the original pilot area are reported as “starting school ready to learn” compared to 25% four years ago. The Clean and Dry initiative to improve toilet training has won national recognition, media and conference coverage. Post Graduate Certificate in Community Health Designed in partnership between the Trust and the University of Kent Focuses on clinical education and assurance of competent practice. Page 28 of 153 End of Life and Dementia Appointed a Dementia Nurse Consultant and a Nurse Consultant for End of Life Care. Developed a Dementia Strategy for KCHT. Developed and implemented the End of Life Strategy and pathway in partnership with key stakeholders. Pain A chronic knee pain programme developed in Kent was praised by the National Institute for Health and Care Excellence. “A Step into Placement” An evaluation of a student’s placement based on the 15 step initiative commended by the Nursing and Midwifery Council in January 2014. Page 29 of 153 2.2 Priorities for Improvement Areas Improving staff morale and recruitment and retention (safety, effectiveness patient experience) Staff morale and the delivery of safe, high quality care are well documented. Staff survey results show there are areas where staff morale is below average and needs to improve. Learning from mistakes to improve safety To stay effective, innovate and address care issues organisations must learn rapidly to avoid mistakes recurring and build sustainability. The Trust needs to strengthen the methods and scale of organisational learning and this will underpin all of the key quality improvements for 2014/15. Improve implementation of the Mental Capacity Act (MCA 2007) We must do more to ensure that staff understand the Act, its application and what it means for the care and treatment of people. Reduce the number of medication errors and increase optimisation of medicines We know that KCHT has had a number of medication incidents in 2013/14 that have caused harm to patients and therefore it is a priority to improve and reduce this avoidable harm. Wound Medicine Last year we committed to eliminating avoidable category 3 and 4 pressure ulcers. We must continue to strive to reach this goal. Continue to develop Integrated Care pathways and ways of working CQUINS for 2014/15 are focused on diabetes, chronic obstructive pulmonary disease, heart failure and fragility pathways. KCHT has begun this work and needs to continue it in the coming year. Page 30 of 153 2.3 Governance Statement Significant Issues Our Annual Governance Statement for 2012/13 highlighted four significant issues. The first was a loss of patient records during archiving, the second was poor maintenance of the Trust’s hydrotherapy pools, the third was related to the prevalence of pressure ulcers and the fourth concerned a delay in the identification of a deteriorating patient. Clear action plans have been developed and implemented as a result of these issues. Training on the treatment of deteriorating patients is available to staff and is being rolled out to relevant services. Pressure ulcers remain an issue in some localities but there has been a marked improvement in reporting and in the prevention of grade three and four ulcers. The Information Governance team provide support to any team that relocates and the Trust has a clear policy relating to archiving records. Eighty seven per cent of all staff (calculated including those on maternity and sick leave) have received mandatory Information Governance training. For the year 2013/14 the following significant issues have been identified: Significant Issue Description: Remedial Action Taken and Plans for Mitigation: The Trust was issued with a Prevention of Future Death Report following a Coroner’s inquest in December 2013 relating to the death of a patient in December 2011. The report was critical of communications between the Trust and out of hours GP services and training of district nurses in relation to symptoms of bleeding. The Trust has worked with the out of hours provider concerned to ensure that they have multiple communications options for the relevant service 24 hours a day. The Clinical Education and Standards Team was set up in May 2013. It is led by the deputy Director of Nursing and Quality and aims to support staff in providing high quality care. Since the inquest, the nurses in the team that were responsible for the deceased’s care have received clinical supervision from their manager and the head of service. This included the delivery of injections and anticoagulants. Page 31 of 153 Significant Issue Description: Remedial Action Taken and Plans for Mitigation: In November 2013 the HSE conducted an investigation following an incident at Sheppey Community Hospital where a patient fell from his bed due to a problem with the bed rails. Fortunately the patient did not suffer any significant injuries and returned to the ward that same evening and was discharged as was planned prior to the incident. As a result of their findings, the HSE issued an Improvement Notice on 4 December 2013 requiring a full review of the following: The suitability of bed rails and their compatibility with mattresses Assurance that all bed rail dimensions meet current British Standards Staff were appropriately trained in the assessment, use and checking of bed rails A system of planned preventative maintenance for all bed rails Written procedures for assessment of bed rail requirements against the needs of the patient Evidence of management checks, monitoring and review of bed rail safety An action plan to address the issues has been developed and is overseen by the Adults Directorate Quality Group. A formal response has been sent to the HSE describing the actions that the Trust is taking as a result of the incident. While clear progress has been made in the year with regard to pressure ulcers, concern still exists in some areas either due to delays of reporting incidents or in relation to prevalence in specific geographical areas. Each pressure ulcer occurrence is subject to an immediate and in depth root cause analysis with an action plan which includes wider dissemination of lessons learnt. These action plans are reviewed by the Director of Nursing and Quality and the Director of Operations, Adults. There is an overarching Trust action plan and Pressure Ulcer Project Board in place led by the Director of Nursing and Quality. The Board oversees progress and trends in this area which are reported at all formal and informal meetings. During the year, specific actions taken have included tendering and awarding a new contract for the provision of pressure relieving mattresses; developing closer working relationships with nursing homes, improving patient information; targeting training being provided to teams regarding reporting and management action taken where appropriate. A number of services across the Trust are suffering from high vacancies and turnover. This in turn exposes the Trust to the risk that safety and quality of care may be compromised. The Trust has been working to reduce vacancy levels in the affected services and localities. Human Resources provide specific support to managers struggling to recruit. Targeted recruitment campaigns are run in areas where normal procedures are not filling vacancies. The Trust also has a programme to support nurses who wish to return to practice. All staff complete an exit questionnaire when they leave the Trust in order to understand why people leave. The Trust has a workforce in which a significant proportion of staff are approaching retirement age, and changes to service provision may lead to staff leaving as a result. Page 32 of 153 Significant Issue Description: Remedial Action Taken and Plans for Mitigation: Some indicators show that staff morale is low in some areas of the Trust. This includes the annual staff survey and feedback from internal engagement programmes. The Trust is not achieving the expected targets in relation to the completion of statutory and mandatory training. The Trust has a communications and engagement strategy and associated action plan. Actions that the Trust has taken to address staff morale include: Working with staff to discuss our vision and values Enhanced engagement programme to listen to staff views and demonstrate subsequent actions Developing a consistent framework for appraisals supported by a clear description of the behaviours we expect from staff and managers. The first cohort of managers is going through the KCHT manager programme An organisational-wide staff awards scheme which is growing in momentum and new quarterly awards to reward good patient feedback. New structures that support greater team working and a new auditable structure for team meetings and the cascade of communications. A task and finish group addressing the burden of paperwork and reporting required from front-line staff so they have more time to devote to patients Significant action has been taken in year to address these areas and although progress is noted, this has not been sufficient. Action being taken includes: On-going review of mandatory training requirements Expanded methods to deliver training including elearning, out of hours training and targeted training delivered at convenient locations Increases in number of trainers available Data cleansing and data quality assessments. Page 33 of 153 2.4 Our Quality Priorities for 2014/15 KCHT has chosen 6 priority areas for improvement which have been identified against our overall performance for 2013/14. These also reflect feedback received from key stakeholders, are underpinned by the strategic objectives and link to our quality aspirations and quality goals. All link to the three elements of quality – Patient Safety, Clinical Effectiveness and Patient Experience 1. Improving Staff Morale and Recruitment and Retention (Safety, Effectiveness Patient Experience) Why is this a priority? Links to: Quality Aspirations 3 & 4, Quality Goals 2,4,5 The Trust recognises that it is important that as an employer we are providing a positive experience for staff and that staff are proud to work with us. We know that the relationship between staff morale and the delivery of safe, high quality care is well documented. The results from the staff survey demonstrate that there are areas where we are below average and we need to improve. We also know that we need to reduce the level of vacancies and increase staff retention as well as implementing the national recommendations regarding safer staffing. We are also committed to ensuring that we have the right staff, with the right skills, in the right place with the right competencies and this requires further effort. Developing capability and capacity to deliver: Implement the recruitment and retention strategy and workforce plan Overseas recruitment campaign. Increase the number of staff undergoing the community nursing qualification. Increased focus on leadership and management training, to recognise that high quality leadership training needs to be supported at all levels. Implement a new bank system to support temporary staffing. Organisational refocus to ensure that the human resources teams are appropriately aligned to support the operational teams. Promote improved engagement with the staff health and wellbeing strategy. Implement performance related pay progression alongside the Values into Action Framework. Continue to link performance (including our values) to pay for the rest of the organisation. Education services available to staff to ensure evidenced-based practice including elearning solutions. Roll out the competency frameworks across the organisation. Page 34 of 153 2. Reduce sickness absence to below 3.75%. absence. Improve staff engagement. Appraisal rates to be above 85%. There will be a focus on short term Learning from Mistakes to Improve Safety (Safety) Why is this a priority? Links to: Quality Aspirations 2, 4 Quality Goals 4, 5 A learning organisation not only values and encourages learning from its own experiences, but looks beyond itself for lessons and avoids complacency. This is one of the key elements identified in improving safety management, leadership and safety culture. The Trust recognises that it needs to work in an environment of rapid and accelerating change, growing public expectations, increasing demands, expanding workloads and continued resource constraints. To stay effective and innovate and address care issues organisations must learn rapidly and build sustainability. The Trust understands the importance of a culture where staff see the need to report any incident affecting patients, the staff or the environment. By investigating each incident, the lessons learned from such investigations can be communicated widely and recommendations implemented swiftly. The Trust acknowledges that for some incidents the organisation has been a passive learner, where lessons are identified but not put into practice, rather than learning actively, where those lessons are embedded into an organisation’s culture and practices. Developing capability and capacity to deliver: For nursing posts encompass the 6cs approach as laid out by the chief nursing officer. Setting a refreshed culture for the organisation (Values into Action Framework). Improved clinical supervision. Continue with “being open”- communicating honestly and openly with patients and their families when things go wrong. Fair blame - we need to continue to ensure that staff are confident in the fairness of the system in order to further develop a culture whereby incidents are routinely reported and investigated. Continue with “Schwartz rounds.” Continue to share best practice and support staff. Page 35 of 153 3. Improve Implementation of the Mental Capacity Act (MCA 2007) (Patient Experience, Safety) Why is this a priority? Links to: Quality Aspirations 1,2 Quality Goals 2,3,4,5 The Mental Capacity Act is a very important mechanism for protecting the rights of people who do not have the ability (mental capacity) to make certain decisions for themselves. Understanding the Mental Capacity Act and the way it is applied is critical to good quality, safe care. Similar to the national picture, we know that within KCHT we have varied compliance with training and with understanding and application of the Mental Capacity Act and Deprivation of Liberties safeguards. We must therefore do more to ensure that staff understand the Act and its application and what it means for the care and treatment of people. Developing capability and capacity to deliver: 4. A dedicated MCA lead has been recruited. The safeguarding teams have had MCA strengthened in their roles and responsibilities. Standardise MCA assessment and documentation in all areas of the Trust to prevent variation in practice. Increase compliance with MCA training and the number of staff trained in level 3 MCA Implement the MCA actions identified by internal audit. Improve the education and training of temporary staff in MCA awareness . Ensure that staff who have completed MCA training have competencies signed off and assessed. Reduce the Number of Medication Errors and Increase Optimisation of Medicines (Safety, Effectiveness and Patient Experience) Why is this a priority? Links to: Quality Aspirations 2,3 Quality Goals 1,2,4 Medicines play a crucial role in maintaining health, preventing illness, managing chronic conditions and curing disease and are a valuable resource in the NHS. It is crucial that patients get the best quality outcomes from medicines. However, the evidence shows that up to 50% of patients do not take their medicines as intended. We waste over £300 million worth of medicines a year and safety data indicates we could do better at preventing avoidable harm from prescribed medication. Effective medicines optimisation is essential to solving this. We also know that KCHT has had a number of medication incidents in Page 36 of 153 2013/14 that have caused harm to patients and therefore it is a priority to improve and reduce this avoidable harm. Developing capability and capacity to deliver: 5. Implement the medicines optimisation strategy 6 key goals and objectives for 2014/5. Improve the support for staff through the Medicines information service and pharmacy support in Community Hospitals. Increase reporting and learning from medication incidents. Minimise dosing errors and omitted dosage using a peer review process. Increase information to patients on administration of medicines. Wound Medicine (Effectiveness, Patient Experience) Why is this a priority? Links to: Quality Aspirations 1,2,3 Quality Goals 1,2,3,4,5 The integrity of skin is vital to patients’ physical and psychological health and it is something that is taken for granted until it is damaged. A holistic approach means a relationship, between the patient, the wound and the treatment. The aim of wound management is to provide the optimum environment for the natural healing process to occur. The challenges of wound management suggest that clinical governance, pain management from wounds and improving quality of life through effective wound care are intricately linked. In the past wound management has not always been well managed. As the management of patients’ wounds comprises 60% of the community nurses workload it is essential that we ensure the effectiveness of our care to improve patient experience. Equally last year we committed to eliminating avoidable grade 3 and grade 4 pressure ulcers. Therefore we must continue to reach this goal as a priority this year. Developing capability and capacity to deliver: Expand tissue viability team resource. Ensure all staff are trained and competent in wound care Increase and ensure compliance with the first choice dressing list Continue the campaign on nutrition and hydration to aid healing. Implement the wound medicine project and the integrated care pathways for wound care Deliver a specific wound medicine module for wound medicine in conjunction with the University of Kent. Work with industry and international partners on best practice. Page 37 of 153 6. Continue to Develop Integrated Care pathways and Ways of Working (Safety, Effectiveness and Patient Experience) Why is this a priority? Links to: Quality Aspirations 1,3 Quality Goals 2,3,5 Integration is about the management and delivery of health services so that clients receive a continuum of preventative and curative services according to their needs, over time and across different levels of the health system, to provide good quality care. Nationally we recognise that often the patient’s journey has too many steps and that we need to ensure that it is as seamless as possible and that the patient receives the right care, at the right time, from the right person, particularly in supporting long-term conditions. This means working in close collaboration with partner organisations. CQUINs for 2014/15 are focussed on Diabetes, Chronic Obstructive Pulmonary Disease, Heart Failure and fragility pathways. KCHT began this work in a number of areas in 2013/14 and needs to continue to develop this work in the coming year, is key to supporting and maintaining people’s health and wellbeing closer to home and working as part of the wider health economy in reducing the burden on secondary care. Developing capability and capacity to deliver (safety, effectiveness and patient experience) Develop new models of care and patient pathways in 4 key areas Implement the End of Life Care Strategy and Dementia Strategy. Improved utilisation of community beds. Improve discharge skill and competencies to support timely discharge and transfers Continue with the Rapid Response Scheme in North Kent to support prevention of hospital admissions. Increase health and wellbeing support in localities. Increase intravenous support in the community to allow care closer to home. How will we monitor and report our improvements? Each improvement priority and goal will have an underlying improvement action plan with key metrics, performance and quality indicators and outcome measures. These will be monitored and reported to the Trust Quality Committee and the Trust’s Board, through the relevant committees and based on benchmarking against other provider services, as detailed in the quality aspirations dashboard (section 2.4). Page 38 of 153 2.5 Quality Aspirations Dashboard Quality Aspirations and Goals - 2014/2015 1.Equal partnerships between patients, their families and the delivery of KCHT services which respect individual needs and values and demonstrate care, compassion, continuity and shared decisionmaking 2.There will be no injury or harm to people who receive KCHT services and a safe, clean environment will be provided at all time 3. Treatment , interventions, support and services will be appropriate and effective, provided at the right time, by the right person with the right skills, wasteful and harmful variation in care will be eradicated 4. A culture of transparency and openness through learning, sharing and innovation. This will be a cornerstone in driving and sustaining excellent care through governance , leadership and accountability at all levels Goal 1 – Patient Safety Measurable year on year improvement in every area of patient safety in community services Goal 2 – Clinical Effectiveness To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Goal 3 – Patient Experience Measurable year on year improvements in patient experience, engagement and satisfaction Goal 4 – Links in with Goal 1, 2 & 3 Promoting a culture of accountability and openness Goal 5 – Links in with Goal 1, 2&3 Improving delivery, capacity and capability in all areas Reduction in catheter associated urinary tract infections in the community by 10% of the baseline (established during qtr2 ) Improve transfer of care by developing care pathways in four area- Diabetes, COPD, Heart Failure, End of Life care and Frail elderly 15% of patients undertake friend and family scores and achieve a result of + 75 per month on the NET Promoter Score Decrease the numbers of cases implicating KCHT in safeguarding concerns against the 2013/14 baseline 70% of all clinical staff across all services to be assessed on core competencies Falls prevention and reduction by 10% and 10% reduction in falls with harm. SBAR to be rolled out across all services for transfer of care by qtr 4 2015 Over 95% patient satisfaction in all service areas using Meridian surveys and at least 50% coverage Improve recruitment and retention process and decrease vacancies to less than 4 % Implementation of safer nursing staffing tool in community hospitals Page 39 of 153 Goal 1 – Patient Safety Measurable year on year improvement in every area of patient safety in community services Goal 2 – Clinical Effectiveness To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Goal 3 – Patient Experience Measurable year on year improvements in patient experience, engagement and satisfaction Goal 4 – Links in with Goal 1, 2 & 3 Promoting a culture of accountability and openness Goal 5 – Links in with Goal 1, 2&3 Improving delivery, capacity and capability in all areas Reduction in all attributable avoidable and unavoidable Pressure Ulcers by 20%, trajectories to be set for each locality 10% reduction in transfer of care issues internally Implement person centred care planning in 50% of services Improve incident reporting across the organisation by 10% Mandatory training compliance at 85% across the organisation 50% reduction in attributable avoidable grade 3 & 4 pressure ulcers set against 2013/14 numbers 95% of medications to be reconciled within 24 hours – community hospitals Embed the six areas of the CNO Caring and compassion strategy Embed the See something Say something campaign (whistleblowing) - measure through responses 10% reduction in agency use Safety thermometer 20 % reduction in new harm pressure ulcers and 5 % reduction in old harm pressure ulcers 95% of medications to be reconciled within 24 hours – community hospitals Develop and implement nurse indicators across children and young person’s services Strengthen morbidity and mortality reporting in community hospitals Ensure that every service redesign and cost improvement plan is quality impact assessed Deliver 95% harm free care Reduction in medication 20 % of patients feedback on errors causing harm by 15% on their experience in relation 2013/14 baseline to wound care Reduction in serious incidents by 50% Increase the number of health visitors to 342 by March 2015. Implement an early warning trigger tool at team level across all services 100 % of VTE assessments to be completed within 24 hours of admission Reduction in complaints implicating clinical care by 10% from 13/14 Reduction in sickness absence to 3.75% Implement end of life strategy goals Page 40 of 153 Goal 1 – Patient Safety Measurable year on year improvement in every area of patient safety in community services Goal 2 – Clinical Effectiveness To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Goal 3 – Patient Experience Measurable year on year improvements in patient experience, engagement and satisfaction Goal 4 – Links in with Goal 1, 2 & 3 Promoting a culture of accountability and openness Goal 5 – Links in with Goal 1, 2&3 Improving delivery, capacity and capability in all areas Reduce the length of stay to 21 days in community hospitals 85% compliance with MCA training across the organisation and 70 % of clinical staff competency assessed Implement dementia strategy goals Reduction in coroners inquests implicating KCHT Trust wide appraisal for all staff at 85% Early implementation of the medication safety thermometer To establish a baseline for healing rates Implement “clean and dry” to all school nurses 85% compliance with DoLs training and 85% community hospital matrons, junior matrons and clinical sisters will have been competency assessed To implement the agreed standard for clinical and managerial supervision. 95% of staff will be receiving supervision by end of 2015. Increase the uptake of staff flu vaccination by 20% Introduce situation, background, action and recommendation as a communication handover tool. Implementation of the Family and Friends Test for staff Reduce agency staffing by 10% Reduce turnover to less than 10% Increase PLACE scores to achieve national best practice in all areas, where estate allows Develop a discharge passport for transfers of care Variances to be below 3% Improve compliance to agreed benchmarks for all statutory and mandatory training Page 41 of 153 Section 3 - Progress against 2013/14 priorities 3.1 KCHT Performance Measures Over 3,700 patients identified as having Chlamydia following screening and offered treatment Over 119,000 patients have been treated at our MIUs and WIC, 320 a day on average, 7 days a week Over 6,000 patients supported to quit smoking New referrals were seen within 18 weeks in our consultant-led services in 97.4% of cases All Cost Improvement Plans were Quality Impact Assessed Nearly 500,000 patient contacts were for planned therapy in a clinic setting Over 3,200 patients were admitted to Community Hospitals More then Care was provided by over 3,600 staff from many professions 3 million patient contacts were provided in the community 16,500 new born babies were seen by our Health Visitors The median length of stay in our Community Hospitals was 23.2 days Over 1.6 million More than of our patient contacts were provided in the patients’ own place of residence Health Checks have been carried out across Kent We significantly exceeded the 50% data quality target for Referral to Treatment Page 42 of 153 30,000 Our C-difficile reduction target was met for 2013/14, reducing from 11 to 8 cases. 3.2 Commissioning for Quality and Innovation Statement Commissioning for Quality and Innovation A proportion of Kent Community NHS Health Trust’s income in 2013/14 was conditional on achieving quality improvement and innovation (CQUIN) goals agreed with NHS Kent and Medway through the CQUIN of all CQUIN goals for 2013/14 93% was achieved. Further details of the agreed goals and performance against those goals for 2013/14 and 2014/15 are available in our performance reports to the Board on our website www.kentcht.nhs.uk See Appendix B The CQUIN framework aims to ensure that there is a shift in quality within the NHS and stretch targets are set. This means that payments are made to providers upon the achievement of the nationally and locally agreed quality goals. CQUIN was 2.5% of applicable contracts, namely CCG contracts, totalling £3,678k of which we achieved £3,415k (93%). CQUINS for 2014/15 are focused on diabetes, chronic obstructive pulmonary disease, heart failure and fragility pathways. KCHT has begun this work and needs to continue in the coming year. Page 43 of 153 3.3 A year on from Francis Our progress on Francis The Francis report was published in February 2013 and had 290 recommendations for action across the NHS – both locally and nationally. The Trust conducted its initial assessment against the Francis report in February 2013 and subsequently self-assessed against additional reviews and have added any recommendations to the Francis action plan. These are listed below: Patients First and Foremost: Government’s initial response to the Francis report March 2013 Health Education England Mandate – April 2013 Children and Young People’s Forum – May 2013 Cavendish review of Health Care Assistants – July 2013 Review of the Liverpool Care Pathway – July 2013 Keogh review of mortality/morbidity – July 2013 Berwick report – August 2013 After Francis: Making a Difference – September 2013 Clwyd Hart review of complaints – October 2013 Keogh review of urgent care – November 2013 National Quality Board Safer Staffing Levels guidance – November 2013 Hard Truths: Government response to Francis – January 2014 The actions for KCHT have been themed as follows: Creating the right culture Putting the Patient first Fundamental Standards of Behaviour Accountability of Directors Performance Management and Oversight Patient, Public and Local Scrutiny Effective Complaints Handling Openness, Transparency and Candour Nursing Leadership Caring for Older People Information Progress has been made in all areas throughout 2013-14 and future plans are in place for 2014/15. (A summary of progress is in Appendix A). Page 44 of 153 3.4 Progress of Quality Goals The following section of the report provides more detail on the achievements of the individual goals, as summarised in the executive summary, against each of the five overall goals. There are a variety of subject areas underneath each goal which support delivery and attainment. Each subject area will provide an update on progress made during 2013/14 and will highlight the priority areas for continual improvement for 2014/15. Goal 1 Measurable year on year improvement in every area of patient safety in community services. This section includes a variety of key subject areas which support the Trust in achieving the overarching goal, with the primary focus on Patient Safety and Reduction of Harms to ensure safe care. Goal 2 To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time. Within this section the key subject areas are End of Life, Dementia, NICE, Children and Young People and Transfer of Care, all of which are fundamental in achieving this goal. Goal 3 Measurable year on year improvement in patient experience, engagement and satisfaction – This is important for the Trust to ensure we are delivering services that are patient centred. The subjects which support the Trust in achieving this goal are Patient Feedback, Complaints, Nutrition and Hydration, Caring with Compassion and Health and Wellbeing. Goal 4 Promoting a culture of accountability and openness. This is a high priority for the Trust to ensure we are transparent and a learning organisation. The subject areas which contribute to this goal are Serious Incidents, Claims, CQC, Information Governance, Clinical Audit and Research. Goal 5 Improving delivery, capacity and capability in all areas. This is fundamental to ensuring safe, effective delivery of high quality care and providing a good experience for people who use KCHT services. The main subject areas which support this goal are Clinical Education, Workforce and Transformation. Page 45 of 153 Each of these goals link to the NHS Outcome frameworks five domains and KCHT strategic objectives and are aligned to the three key elements of quality – patient safety, patient experience and clinical effectiveness. Page 46 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Safe Care Deliverables Mandatory Statement – Safe Care When compared to 2012/13 the overall number of incidents has reduced in 2013/14, but the rate of incidents remain consistent against activity. We want to do better and will continue to strive to reduce incidents of harm. The Trust’s rate of patient safety incidents is 1 per 1,000 patient contacts and of this 0.2% resulted in severe harm or death, which is a reduction compared with 0.3% in 2012/13. The reduction in severe harms is due to the significant reduction in the number of falls in this level of harm. KCHT reports all attributable patient safety incidents to the NRLS (National Reporting and Learning System). This data is shared with other organisations, such as the HSCIC (Health and Social Care Information Centre). A summary of the data reported to the NRLS during 2013/14 is shown below. To provide context, the rate of incidents per 1000 patient contacts is detailed in the table below. Number of incidents Per 1000 contacts Percentage None (No harm to patient(s) 1612 0.5979 40.0% Low (Minimal harm - patient(s) required extra observation or minor treatment) 1552 0.5756 38.5% Moderate (Short term harm - patient(s) required further treatment, or procedure) 859 0.3186 21.3% Severe (Permanent or long term harm) 6 0.0022 0.1% Death (Caused by the Patient Incident) 1 0.0004 <0.1% 4030 1.4947 100% 2013/14 Total Page 47 of 153 A patient death occurred during an influenza outbreak and a full root cause analysis investigation has been undertaken. Following the investigation it was not possible to confirm whether or not the patient’s death was related to the flu, however lessons learnt have been shared throughout the organisation. When compared to 2012/13, the number of incidents has increased from 3744 to 4030 (an increase of 8%) due to a drive to improve incident reporting. The level of harm has reduced. The table below shows the 2012/13 incident figures 2012/13 Attributable Patient Incidents Pressure ulcers (number of forms) Falls SafeMed Severe Harm Death Harm Total Severe and Death Apr 328 May 366 Jun 324 Jul 321 Aug 372 Sep 278 Oct 282 Nov 288 Dec 265 Jan 308 Feb 280 Mar TOTAL 3744 332 137 155 121 113 137 90 90 88 90 108 100 101 1330 62 64 73 61 71 63 72 51 50 79 59 70 775 59 42 57 68 73 51 46 50 42 39 40 53 620 1 0 0 0 1 0 2 2 1 0 0 3 10 0 0 0 0 0 0 0 0 0 0 0 0 0 1 0 0 0 1 0 2 2 1 0 0 3 10 2865 227 264 264 224 254 227 230 259 254 198 241 222 Patient contacts (1000s) 1.3 1.4 1.4 1.2 1.4 1.5 1.2 1.2 1.1 1.0 1.6 1.2 1.5 Incident Rate per 1000 patient contacts 0.3% 0.3 0.0 0.0 0.0 0.3 0.0 0.7 0.7 0.4 0.0 0.0 0.9 % of Severe and Death Incidents *There is a slight variance to the data reported in the 2012/13 Quality Account. The main difference occurs within the Safe Medicines figures which have been corrected following audit. Other variations are due to incidents being reported after the 2012/13 Quality Account was produced The table below shows the 2013/14 incident figures 2013/14 Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar Total Attributable Patient Incidents 314 317 359 359 324 341 360 317 284 357 328 370 4030 Pressure ulcers (number of forms) 109 110 109 102 74 95 133 106 85 104 111 117 1255 Falls 55 64 66 77 37 67 56 47 53 74 61 67 724 *SafeMed 45 48 63 62 85 75 58 62 62 65 61 56 742 Severe Harm 1 0 1 1 0 1 1 0 0 1 0 0 6 Death Harm 0 0 0 0 0 0 0 0 0 0 1 0 1 Total Severe and Death 1 0 1 1 0 1 1 0 0 1 1 0 7 Patient contacts (1000) 228 242 234 251 205 226 250 239 199 223 188 213 2483 Incident Rate per 1000 patient contacts % of Severe and Death Incidents 1.4 1.3 1.5 1.4 1.6 1.5 1.4 1.3 1.4 1.6 1.7 1.7 1.6 0.3 0 0.3 0.3 0 0.3 0.3 0 0 0.3 0.3 0 0.2% We will to strive to improve and reduce the number of harm incidents and build upon the improvements we have made during 2013/14, as detailed in our key priorities. Page 48 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Infection Prevention and Control Reduction in Health Care Associate Infections The Quality Goal 2013/14: No one to contract MRSA in any of our community hospitals and to reduce Clostridium Difficle by 33%. How did we perform in 2013/14? Our plan was to improve our performance by 33% of C difficile (C.diff) incidents. Target 2013/14 33% reduction Achieved 40% In 2012/13 there were 14 cases which reduced to 8 cases in 2013/14. The Trusts’ rate of c.diff infection decreased from 15.1 per 100,000 bed days in 2012/13 to 9.1 cases per 100,000 occupied bed days in 2013/14 which compares favourably against neighbouring Acute Trust rates (published data rate to November 2013): Local acute Trust rates for comparison: Dartford and Gravesham 10.09 per 100,000 occupied bed days EKHUFT 16 per 100,000 occupied bed days Maidstone and Tonbridge Wells – 18.63 per 100,000 occupied bed days Medway Maritime 8.2 per 100,000 occupied bed days A root cause analysis (RCA) is completed for all incidents of Clostridium difficile to understand the contributory factors and that lessons learned are clarified and implemented. Of 8 cases, only one was deemed to be avoidable and new policies and procedures for contractors have been improved. Antimicrobial Stewardship – (UK Five Year Antimicrobial Resistance Strategy 2013– 2018) is a key contributor to reducing C difficle and the Trust has undertaken a gap analysis to ensure that all best practice is followed. The Trust has further strengthened efforts on appropriate prescribing to aid reduction in cases of Clostridium difficile and antimicrobial resistance and will continue to audit year on year. Methicillin Resistant Staphylococcus Aureus (MRSA) – Target 2013/14 Zero Not achieved 1 case Page 49 of 153 One MRSA bacteraemia (blood stream infection) was attributed to the Trust in April 2013. A full root cause analysis was carried out and as a result further screening and skin cleansing was implemented. MRSA Screening is carried out on all patients who are admitted to community hospitals from home to reduce the risk of spreading infection. Target 2013/14 100% Not fully achieved 99% Three patients that should have been screened were not which led to an overall achievement of 99%. As a result improvements were made in the orientation and induction programme for agency staff. Escherichia coli - There have been zero cases of E. coli blood stream infection within KCHT There were eight outbreaks of norovirus in five of the community hospitals which reflected norovirus in the community and there was one outbreak of influenza. These were all well managed and contained. Issues of isolation and ward layout that make isolation of patients difficult are being addressed with the estates team and commissioners. The influenza outbreak RCA identified lessons to be learned and these are being implemented to reduce further risks One patient died during this outbreak. This was reported as an SI and a full root cause analysis investigation was completed. It was not possible to confirm whether or not the patient’s death was related to the flu, however lessons learned have been shared throughout the organisation. Infection Prevention and Control Training Hand hygiene is the single most important measure in reducing the spread of infection and is a priority for KCHT. Overall compliance Hand Hygiene 82% Clinical staff compliance: 82.5% Target 2013/14 85% Not achieved 82% Overall compliance IPC Mandatory training 73.6% Clinical staff compliance: 65% Target 2013/14 85% Not achieved 74 % Page 50 of 153 The target of 85% reflects staff on maternity leave, career breaks or vacant posts. The Director of Infection Prevention and Control wrote to all non-compliant staff in September 2013 to directly address non-compliance. A review of the training programmes and targeting teams with poor performance is a priority for the next year. The Infection Prevention and Control team aims to achieve full compliance by August 2014. Hospital Acquired Catheter Associated Urinary Tract infections (CAUTIs) and Urinary Tract Infections (UTIs) Target 2013/14 50% reduction Achieved The plan for 13/14 was to reduce CAUTIs and UTIs. There was a significant decrease of CAUTIs by 50%, this rate has been sustained but there has been no further decrease in the last year. The reported cases remain significantly low averaging 3.5 per month. For UTIs there was a 15% overall reduction. Patient Led Assessment of the Care Environment (PLACE). These visits replaced the Patient Environment Action Team (PEAT) inspections. The assessment covers privacy and dignity, wellbeing, food, cleanliness and general maintenance of all areas of community hospitals where care is delivered. Visits are conducted by a team of 50% patient representatives and 50% of Trust staff. The overall scores are shown in the table below. National Results KCHT results Cleanliness Food and Hydration Privacy, Dignity and Wellbeing Condition and appearance 95.74% 84.98% 88.87% 88.75% 88.94% 86.05% 81.78% 77.89% The Trust performed in the lower quartile nationally and is very disappointed with the results. Whilst some issues relate to the age and condition of the estate, which is being addressed by the landlords, The Trust has taken actions to improve the performance of cleanliness, food and nutrition by introducing new menus and a specific campaign on nutrition and hydration. The Trust has introduced changes to some of the ward configuration and estates and is confident that these will be reflected in future assessments: Management of Healthcare Waste - updated Waste guidance issued by the Department of Health: HTM 07-01 Safe Management of Healthcare Waste was reviewed against Page 51 of 153 KCHT standards and practice and KCHT has been found to be fully compliant with the guidance. No waste generated by healthcare workers will be left within a patient’s home without their consent. Goals for 2014/2015: Reduce Clostridium Difficile to no more than 7 cases. Catheter Acquired Urinary Tract Infections and Urinary Tract Infections to reduce by a further 10%. Ensure 100% compliance with MRSA screening. Increase the percentage scores on the PLACE audit to at least the national average. Ensure full compliance with hand hygiene and improve compliance with infection prevention training. Increase the percentage uptake of staff flu vaccinations. The following case study highlights one of the achievements for 2013/14. Case studies ‘C Diff green card rolled out to protect patients’ Page 52 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Harm Free Care Delivering harm free care is important to KCHT as we do not want to cause harm to any patient or their family. The Trust wants to improve quality and engage staff in thinking about how they can help reduce harms even further. How did we perform 2013/14? We have successfully increased the percentage of Harm Free Care (HFC) above the national average for 2013/14 and exceeded the KCHT benchmark. The safety thermometer that measures harm free care focuses on four harms: Falls Preventable pressure ulcers Venous thrombo-embolism (VTE) Catheter acquired infections (CAUTI) The graphs below show our position against last year and the national benchmark. 37,835 patients were surveyed for the year, an increase of 18.7% compared to 2012/13 with a 2.5% reduction in harms for 2013/14, which is above the National and Regional benchmarks. KCHT Patients Surveyed KCHT Position Average National Position Average Regional Position Average 2013-14 37835 95.42 93.04 93.70 Page 53 of 153 2012-13 % Variance 31874 ↑18.70% 92.92 ↑2.50% 92.61 0.42% 91.59 2.11% The main category of harm remains new and old pressure ulcers even though there has been a reduction in both for 2013/14. There is on-going work to reduce pressure ulcers, (covered in another section of the report. In addition the Trust is working collaboratively with CCGs, Acute Trusts and social care to have a whole systems approach to the reduction of harms. The table below shows the improvement of each individual harm in comparison to last year. Harm Total Old PU Total New PU Total Falls with Harm Total New VTE Total Catheter & NEW UTI Total Catheter & OLD UTI 2012-13 2013-14 4.38 1.33 0.57 0.37 0.31 0.23 3.31 0.72 0.25 0.08 0.15 0.13 Workshops with clinical staff have focused on reinforcing the importance of teams using their safety thermometer results to inform quality improvements and reduce harms. Goals for 2014/2015: To be an early implementer of the new national medication safety thermometer tool. To maintain and improve 95% and above Harm Free Care for new harms. To reduce the number of new harm pressure ulcers by 20%. To reduce the number of old pressure ulcers by 5% by working in partnership across the whole system. Page 54 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Pressure Ulcer Prevention and Management Zero attributable and avoidable pressure ulcers The development of pressure damage has a profoundly negative effect on all aspects of a person’s life and is very distressing for patients, carers and their families. The reduction of pressure ulcer incidents has been a key priority for the Trust and a key goal for staff. How did we perform in 2013/14? 2013/14 Progress Inherited Pressure Ulcers (Non attributable Pressure Ulcers attributable to KCHT Aspirant Foundation Trust Benchmark Monthly average of attributable avoidable 20.9 Pressure Ulcers 2% ↓ 7.2 % ↓ KCHT position 12.7 The results for this year have seen some positive improvements but we have much more work to do. The number of pressure ulcers which KCHT inherited from other care providers has reduced by 2% which reflects the overall priority across the whole health economy. The number of attributable avoidable and unavoidable pressure ulcers grade 2, 3 and 4 has reduced by 7.21 % compared to 2012/13, as shown in the graph below. 250 2012/13 Yes (Attributable) 200 150 2013/14 Yes (Attributable) 100 2012/13 Yes (Attributable) Average 50 0 Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar 2013/14 Yes (Attributable) Average The number of attributable avoidable grade 2, 3 and 4 pressure ulcers reported on average per month was 12.7 which compares favourably against the Aspirant Community Page 55 of 153 Foundation Trust benchmark of 20.9 per month (Feb 2014 publication) however as a Trust it is our priority to reduce all avoidable pressure ulcers. Eighty-one per cent of the total of 144 teams achieved zero Grade 3 and 4 pressure ulcers in community hospital wards, short-term and long-term services). 7% of teams had one avoidable grade 3& 4 pressure ulcer and 12% of teams had two or more. These teams will be subjected to an intensive support programme to ensure lessons are learned and embedded into practice. Work has already begun in many of these teams to ensure quality improvements are sustained. Root cause analysis investigations are completed on pressure ulcers classified as serious incidents, so we can understand why it has happened and learn the lessons. We have completed a detailed analysis of attributable avoidable and unavoidable pressure ulcers across all services. There has been targeted support including holistic assessment, caseload management support, accountability sessions, tissue viability training, competency assessments and the implementation of nurse indicators in teams where there have been two or more attributable avoidable grade 3& 4 pressure ulcers. A sample of teams who had achieved zero avoidable pressure ulcers were visited which highlighted areas of best practice that have been factored into the pressure ulcer standard. A repeat audit was completed on compliance with the pressure ulcer standard for attributable unavoidable pressure ulcers which had been classified as all interventions in place and non-concordant. It highlighted evidence of good practice including clear evidence of shared care between podiatry, nursing and patient choices. In non-concordant patients there was evidence of negotiation and risk assessments. Page 56 of 153 Although the audit highlighted some good practice there is still work to do to improve practice. In response to the findings the following actions were implemented: A top tips handbook for the prevention and management of pressure ulcers. A leaflet on the prevention of pressure damage for formal and informal carers developed in partnership with them. Partnership working will aim to address the shared care issues associated with pressure damage. A high profile campaign on the reduction of pressure ulcers, including screensavers on all computers. Developing an eLearning tool for Waterlow (risk assessment tool). Holistic assessment training has been developed. Nurse indicators and standards. A nurse consultant for tissue viability will be employed and the tissue viability team has been strengthened. Goals for 2014/2015: Work has continued with other providers and clinical commissioning groups to address the issues. A CQUIN for 2014/15 has been designed to support the wider health economy focus on the reduction of pressure ulcers: To identify further learning from teams who have achieved zero avoidable grade 3 and 4 pressure ulcers. Reduction in unavoidable pressure ulcers “all interventions in place” and “nonconcordant” by 20%. 20% reduction in avoidable grade 2 pressure ulcers. 50% reduction grade 3 and 4 pressure ulcers aiming for zero. Page 57 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Venous Thrombo-embolism ( VTE) All patients admitted into community hospitals should have a venous thrombo-embolism risk assessment completed within 24 hours to see if they are at risk of developing a blood clot. Preventative treatment using daily injections helps to dramatically reduce the risk. We had no preventable VTE events or deaths in 2013/2014 and on average the Trust is achieving 97% compliance. Work continues to ensure processes are robust to ensure all patients are assessed within 24 hours to achieve 100% of the target. Target Progress 100% 97% not achieved All established qualified staff have been trained and competency assessed. programme for new staff is in place and part of their induction. VTE Screenings Target Actual (2013-14) Actual (2012-13) A rolling Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 100% 95% 95% 96% 98% 95% 95% 98% 100% 98.00% 98% 96% 100% 90% 98% 96% 95% 96% 96% 99% Goals for 2014/2015: 100% of assessments to be completed within 24 hours. Revision of the VTE assessment tool to improve evidence of decision-making. Patient information leaflet to be given to all patients at the time of assessment. All patients at risk of VTE are to have a care plan in place. A rapid cycle audit will take place to ensure all recommendations are embedded. Page 58 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Falls Prevention and Reduction by 10% and 10% reduction in falls resulting in falls with harm Falls can happen at any age but are more common when we get older. The cause of falls includes many factors and reducing the risk of falls requires thorough assessment and planning. How did we do in 2013/14? The KCHT falls rate is variable and influenced by a combination of factors. Services aim to achieve a balance between promoting independent mobility through rehabilitation and the on-going risk of falls. Target 2013/14 10% reduction in falls 7% We have seen a 7% reduction in all falls reported this year compared to the 2012/13 figures. There has been a 14% decrease in the number of inpatient falls in community hospitals in 2013/14. The table below clearly demonstrates improvements against the 2012/13 position. Target 2013/14 10% reduction in Community Hospital falls Achieved 14% KCHT achieved an average of 6.85 falls per 1000 Occupied Bed Days (OBD) for 2013/14. This figure compares favourably against the national benchmark of 8.6 falls per 1,000 OBD for community hospitals (NRLS benchmarking data 2010). Service transformation within community hospitals to reduce the number of falls has led to a decrease in overall terms by 31.41% and a 42.85% reduction in fractures compared to last year (as seen in the chart overleaf). We will continue to strive for further reductions in both of these areas in the next year. Page 59 of 153 From January 2014 the podiatry service joined a national falls research programme sponsored by the University of York, the REFORM study (Reducing Falls with Orthoses and a multifaceted podiatry intervention). Goals for 2014/2015: This year KCHT will trial “The Canadian Safer Home Tool” using two pilot sites in East and West Kent. The tool is internationally validated and will provide an assessment of falls risks in the domiciliary setting. In addition KCHT will: Reduce the number of falls by a further 10%. Reduce the number of falls with harm by a further 10%. Review comfort rounds and the use of the quality risk indicators tool in relation to falls. Undertake observational audits in all community hospitals to determine any key triggers for falls. Increase medications reviews to help support a reduction in falls. Focus awareness on medication starting with fall awareness week in June. Focus support interventions on people with dementia. Review the environment in all wards, such as signage. Page 60 of 153 Case study ‘June gets a greenbelt’ An innovative new wristband scheme which has cut falls at the Livingstone hospital by 50 per cent is to be rolled out across Kent. Colours Reducing Falls is an award-winning programme where all patients are assessed by the physiotherapy team, which decides how much help they need and what their risk of falling might be. They are given a red, yellow or green wrist band to alert other staff. Senior Physiotherapist Sam Gohir at the Livingstone Hospital in Dartford said, “We trialed this programme two years ago as a simple way of making sure all staff in our hospital knew the needs of every patient. It allows us to take into account all the factors that might affect a patient’s fall risk, such as if they have dementia, mobility issues or a lack of confidence. “It has worked fantastically well and in the first six months, the number of falls at the Livingstone had reduced by 50 per cent.” June Gildea, 75, from Gravesend, suffered a fall at her home and fractured her hip. She said: "The staff have been really supportive and it has encouraged me to work hard and do my exercises and move up to the green band. I felt like I had won a medal when they promoted me! It has given me the confidence to know I will be ok when it’s time to go home.” Now the team behind the scheme has been recognised by the Community Hospitals Association (CHA) for the effective and simple way they have improved patient care. The system has been so successful that it has also been launched on the Sapphire Unit at Gravesham Community Hospital and will be rolled out across all community hospitals run by Kent Community Health NHS Trust. Page 61 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Patient Safety Walkabouts (PSW) In 2013/14, 43 Patient Safety Walkabouts (PSW) took place. Patient Safety Walkabouts are weekly visits to a team by a member of the executive and non-executive team to discuss and engage with staff on areas of patient safety. As part of the visit and in order to be as inclusive as possible a pre-visit survey is sent to teams prior to the walkabout, so that staff who may not be able to attend the walkabout can give their views on safety, quality, effectiveness, innovation and aspiration. The survey results highlighted the following top 5 action areas: Communication: This was a recurrent issue related to ensuring that there is adequate and regular communication from team leaders/managers addressing policy changes, Lessons Learned, the Trust core brief and staff concerns around service redesign/restructuring and relocation. Actions were resolved for example by arranging executive visits, reinstating team meetings and strengthening and changing the engagement and communication plan. Service development: These actions covered a range of issues which included the desire to understand best practice in comparable teams; the potential for development of support roles such as dietetic assistants or phlebotomists; marketing services and identifying or rectifying gaps or inequity in service provision. As a result a number of support roles have been introduced. Best practice is being used to support good practice, such as pressure ulcers and a review of staffing has taken place. IT: Information technology actions mitigated frequent concerns around implementation and training for Community Information System (CIS), adequate IT access in integrated teams and issues pertaining to out of hours systems and out of base connection problems. These are being addressed as part of the overall implementation of the system as they are highlighted. Quality and safety: Issues highlighted included a variety of issues such as confidentiality in public waiting areas, understanding and using performance data with teams to support improvement, raising awareness of the Francis report, and escalating concerns around gaps in provision, practice or awareness. A number of interventions have been put in place, for example changes in awaiting areas, escalation frameworks and locality-based scorecards. Page 62 of 153 Risk management: Issues raised by staff involved staff risk management such as moving and handling, conflict resolution, lone working risks, adequate staffing levels and raising awareness of team risk registers. Considerable work has been undertaken including in the areas identified, safety reviews have been undertaken and support has been given to teams on risk registers. The visits have enabled staff to voice their concerns and raise issues that pertain to practice. This supports the culture of openness as recommended by Francis. Actions that have supported patient care include raised awareness of requisitioning the right equipment, highlighting issues around Insulin administration in the community and improving board to floor communication. Goals for 2014/2015: A revised quality and safety visit programme to encompass more staff and less bureaucracy. Increased visibility of the Executive and Board through executive road shows Improved communication with all teams, by improving communication channels and methods Continue to address issues raised by staff at the walkabout in timely manner Page 63 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Safeguarding Decrease the number of safeguarding cases implicating KCHT in safeguarding concerns The Trust recognises its responsibility to prevent abuse of adults and children who are at risk. Safeguarding is a fundamental part of patient safety and healthcare professionals have a key role in identification of safeguarding concerns and responding appropriately to them. Safeguarding Children We have continued to work closely with our partners in Kent Social Care services, to ensure staff, understand the multi-agency thresholds that have been developed to help them identify and manage safeguarding and child protection concerns. A multi-agency review of Kent and Medway Threshold Criteria for Children in Need was completed in 2013, to evidence that existing arrangements to safeguard and protect the most vulnerable children living or visiting the counties reflect their needs. In the last 12 months there has been a steady increase in the number of children made subject to a Child Protection Plan (CPP). This upward trend is due to a number of factors, including: improvements made by KCHT practitioners in applying the multi-agency child-inneed thresholds and statutory assessment framework for child protection the continued application of the Common Assessment Framework (CAF), by KCHT practitioners. the Kent Safeguarding Children’s Board redefined its strategic objectives to state that all children who were identified at risk of significant harm should be made subject to CPP proceedings, which resulted in a review of such cases against the afore-mentioned thresholds Safeguarding Adults During 2013/14, KCHT raised 226 Adult Protection (AP) alerts involving other agencies, carers compared to 255 alerts raised in the previous 12 months. In the same period 65 Adult Protection alerts were raised against KCHT, either by another agency (9), or KCHT itself (56). The details of the cases raised against KCHT services were as follows: Page 64 of 153 Types of abuse Number of Adult Protection alerts Neglect 53 (29 pressure ulcers) Financial 1 Physical 8 Sexual 3 Outcomes of alerts raised against KCHT The 65 Adult protection alerts for 2013/14 is a significant increase in activity compared to the 49 alerts raised during 2012/13. This increased reporting reflects the continued awareness that our frontline services have as to their safeguarding responsibilities and what constitutes a safeguarding concern. This is borne out by the increase in the number of practitioners contacting our internal SG service, for advice and/or to share concerns. Closed - abuse confirmed 14 Closed - abuse discounted 27 Closed – insufficient evidence 4 Cases still open/under investigation by KCC 20 8/14 confirmed abuse cases were classified as a Serious Incident Requiring Investigation (SI), 7/9 were investigated under the category of neglect 1/9 was investigated under sexual abuse. Root Cause Analysis (RCA) investigation findings are used to formulate a robust action plan to ensure organisational learning is embedded; learning is shared through the Lessons Learnt Newsletter and included in training programmes to prevent such an incident happening again. The key learning opportunities and outcomes from the cases investigated through the SI process, included The need to improve shared care arrangements with care home staff Page 65 of 153 The need for staff to have a better understanding of safeguarding policy and procedure, to support earlier identification of concerns and timely liaison with KCHT Safeguarding services and KCC Review of staffing levels and handover arrangements, to support the provision of safe care The need to seek specialist advice, at an earlier stage in the patients care, to support the early identification, escalation and management of complex needs A review of staff competencies, to ensure the application of learning to practice and patients will be cared for by trained and experienced staff The need to access safeguarding training, to ensure that the patient’s best interest is at the heart of care being provided The need to have robust contract monitoring arrangements in place, that will immediately highlight possible delays in equipment delivery and mitigate associated risks of harm Mental Capacity Act/Deprivation of Liberty Safeguards (MCA/DoLS) Last year, each of the Community Hospitals was allocated a named Safeguarding practitioner from the Safeguarding Team. During core hours our Safeguarding service provides same day telephone advice regarding any urgent MCA/DoLS issues/concerns and has regular presence at ward rounds and multi-disciplinary meetings. This input from the Safeguarding service has increased associated frontline teams’ awareness of MCA, increased safeguarding consultations, reporting of MCA concerns and consideration of DoLS applications. There are MCA link nurses, to provide local leadership around MCA and to act as a first line resource to their colleagues. Last year our Community Hospitals had 1 DoLS application authorised by the Supervisory Body. The achievements from this initiative include: Increased sign-off of MCA competencies for band 6/7/8 practitioners MCA prompt cards. Bespoke MCA training sessions provided Best interest meetings taking place at the request of KCHT staff. Safeguarding Operational Manual published Alignment of designated Safeguarding Specialist Practitioners to each community hospital - Work will continue into next year, to support the MCA link nurses to consolidate their role, ensuring that they are confident in undertaking regular case review. This will provide the Trust with assurance that care plans, records and patient care reflects the principles of the MCA. Page 66 of 153 Improve Safeguarding training compliance – remains a key priority and a rolling programme of Safeguarding training sessions is made available to staff across the Trust practitioners have been reminded of their professional responsibilities to safeguard and protect vulnerable adults and children. The table below shows the overall training compliance. Safeguarding Training – target 85% 12/13 13/14 80% 89% Safeguarding children training 79% 80% Safeguarding adults training 80% 89% Mental Capacity Act (MCA) Training To address the remaining (overall and module specific) compliance gaps: Safeguarding and Mental Capacity Act training packages, included e-learning (which has been endorsed by the Department of Health) have been made available and will support face to face sessions to ensure compliance. Goals for 2014/2015: Ensuring that all staff are compliant with safeguarding/MCA and DoLS training and that KCHT’s target is reached and maintained. Reducing the number of cases of avoidable harm remains a priority for KCHT in 2014/15 Supporting MCA link nurses to consolidate their role within Community Hospitals Achieve and maintain corporate compliance for all safeguarding training and ensure robust action plans are in place and delivered against by each service that continues to show non-compliance. 85% of community hospital band 6 and 7 practitioners to have their competency assessed for DoLS Review our MCA training to embed MCA into Consent and Safeguarding Children training. Page 67 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Early Warning Trigger Tool ( EWTT) An Early Warning Trigger Tool (EWTT) has been developed to identify teams where quality performance is deviating from expected standards and to enable help and support to be targeted to provide a level of assurance of quality throughout the implementation of change and service redesign. The EWTT has been rolled out across all services at locality level and has been in place since October 2013. Patient safety and ensuring patients suffer no harm is a key priority for the trust and this tool helps to identify areas where safety maybe compromised through a range of indictors. There are pockets of teams where we have had concerns during the year and rapid support, guidance, training, competency assessments, review, recommendations and actions of systems and processes and resource management has been provided. The outcomes of intensive support has improved the delivery of quality care and reduced harm to patients, improved patient and staff experience. There are some key areas where there could be potential risks and action plans are in place and on-going monitoring through the EWTT and a variety of assurance metrics The thresholds of tolerance have been set with clear actions stipulated at each level for the service / hospital. Clear action plans are put in place whenever there is a breach in standards. Goals for 2014/2015: Further work is required on the EWTT and the indictors need to be refined following its implementation and our learning. To develop team-level reporting, as the aggregated score at locality level is masking team level sensitivity. Develop the escalation framework and rapid response support framework to support teams identified in need of improvement. Page 68 of 153 Goal 1: Measurable year on year improvement in every area of patient safety in community services. Delivering Safe Medicine Management Making sure patients get the right medicines at the right time is important to us, whether at home or in hospital, to keep patients safe in our care. Data indicates that incorrect administration of medicines results in 10-20% of hospital admissions. There has been a 16% increase in attributable safe medicine incidents reported in 2013/14 compared to 2012/13. This is largely due to increase reporting of medication incidents within KCHT which is positive as previously not all areas reported consistently. The table below shows 87% of these incidents did not result in harm to patients. The low and moderate harms are predominately related to administration errors and missed doses of medication which are unacceptable for patients. There is an organisational action plan in place to address the root causes of these incidents. This is a priority area for improvement for 2014/15. 2013/14 None Low Moderate Severe Death Level of harm by percentage 88% 11% 1% 0% 0% Level of harm by numbers 649 85 8 0 0 Performance against the agreed metric for 2013/14 to improve optimisation of medicines by 20% was not achieved. The Trust has developed a medicine optimisation strategy which has 6 overarching objectives and includes measurable key performance indictors to ensure progress can be monitored in 2014/15. Medicines Management undertook a number of actions to improve the management of medicines which included: Development of community medicines management administration documentation and a Paediatric palliative care chart has been developed in collaboration with local and tertiary paediatric palliative care providers to help improve the management of medicines for patients. Improved medicine training so that staff understand the impact of medicines on patients Pharmacy has worked with the University of Kent to develop an injectable medicine a module as part of the Postgraduate Certificate in Community Health Care. KCHT is compliant with the NHS England patient safety requirements (formally NPSA) and has introduced the new syringe drivers that will improve patient safety Page 69 of 153 In September 2013 KCHT became the first community health trust to have a medicines information service registered and accredited with United Kingdom Medicines Information. This service helps staff to discuss patient medicines and issues with a pharmacist to ensure best use. An external audit of systems and processes associated with the management of controlled drugs provided significant assurance. A successful staff flu vaccination programme was led by the Medicines management team which resulted in a doubling of uptake amongst KCHT front-line staff by using innovate ideas. Unfortunately whilst the Trust made a significant improvement from 17% in 2012/13 to 49 % in 2013/14 we, it did not meet the national target of 75% but was short listed for a national NHS Employers award, for the innovative approaches used. The first pre-registration pharmacy technician to be trained in Community services registered with the General Pharmaceutical Council and a second student began training in January 2014. A number of areas of risk associated with the management of medicines have been identified through audit, incident reporting and medicines information enquiries and actions put in place to address them. Patients missing doses or receiving drugs at the wrong frequency, this is being addressed on an individual basis and is part of an organisational action plan to eliminate these errors. Agency staff do not always have sufficient skills to administer medicines safely. This has been addressed through contracts with the agencies and on line training packages Wards/services being non-compliant with medicines policies, following each service audit, individual service action plans are put in place to address the issues identified. The annual omitted dose audit showed that actions that have been implemented during the previous twelve months have led to a reduction in omitted doses; work to implement additional actions both in inpatient and domiciliary settings to further reduce the occurrence of omitted doses. All incidents that have resulted in any harm to patients however minor have been investigated and actions taken to prevent similar incidents with the result that levels of harm from medicines is low. The Patient Experience Policies for the use of patients own medication and self-administration have been updated and work to promote self-administration in community hospitals has taken place. Patients have been supported in domiciliary settings to enable correct use of medicines and prevent hospital admissions as part of different locality projects with much success. Page 70 of 153 Goals for 2014/15: The Trust has developed a medicines optimisation strategy with the following objectives to be implemented in 14/15, which will support the areas identified as risk. Objective 1: Strategic, Risk and Governance KCHT will make medicines optimisation an integral part of the Trust’s medicines strategy, systems, working practices and culture at all levels. Objective 2: Safe Use of Medicines KCHT will have systems, processes and practices designed and in place to prevent or reduce the risk to patients from medicines. Objective 3: Effective Choice of Medicines and Patient Outcomes KCHT will have systems and processes in place to deliver good clinical outcomes through effective medicines optimisation supported by robust local decision making. Objective 4: The Patient Experience KCHT will involve patients (and carers) in the decisions made about their medicines and support them to take medicines as intended. Objective 5: Environment for Medicines Optimisation KCHT will continually work towards improving health environments that support optimal use of medicines and secure the best outcomes for patients. Objective 6: Workforce for Medicines Optimisation KCHT will have in place workforce planning, development and education and training to support the optimal use of medicines to ensure that services are delivered by competent and well trained staff. All of the overarching objectives are supported by detailed actions underpinning the strategy. Page 71 of 153 SUMMARY Goal 1: Measurable year on year improvement in every area of patient safety in community services The summary of performance against goal 1 has overall been very positive with many targets achieved and progress has been made in reducing harms to patients. However, the Trust still has a significant amount of work to do to sustain and continue to improve patient safety. Infection prevention and safeguarding adults training, PLACE results, medicine errors and reduction in attributable pressure ulcers are the key areas requiring improvements to ensure patients are not harmed. The goals and measures for 2014/15 within goal 1 will ensure there are improvements in these areas to minimise risk to patients and improvements made are sustained and embedded into practice. Page 72 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Transfer of Care Transfer of Care is an area patient and carers would like to see improvements and is a key priority for the organisation. During 2013/2014 a total of 697 transfers of care incidents occurred from external providers to KCHT. 46% of these were related to pressure ulcers and 25% were related to admission, transfer and discharge issues. Work continues with health economy partners to identify barriers to safe transfers of care and implement solutions such as a new Transfer of Care form for reporting concerns. Whilst the reporting has been robust, we have not achieved all the aspirations that were set for this year. The graph below shows the transfer of care issues. The internal transfer of care incidents related to: 28% Safe Medicine Incidents 20% Access, Appointment, Admission, Transfer, Discharge 16% Pressure Ulcers 16% Treatment, Procedure 7% Patient Information 13% Other A review of the incident reporting system took place to improve data capture of transfer of care issues. Since June there were 143 transfers of care issues involving KCHT services .The main issue internally is communication and a new communication tool is to be used to improve internal and external communication and will be rolled out during 2014. Page 73 of 153 A review of incidents citing communication as a contributory factor reveals that the main issues are delays or failures in referral process to community teams. This can result in missed visits, omissions of medications, pressure area / ulcer deterioration and delays in following up of vulnerable patients. These areas are being addressed by the introduction of a caseload management tool, a quality risk indicator and enhanced pharmacy support in addition to the actions in the pressure ulcer action plan. Goals for 2014/2015: Further Transfer of Care audit 2014/15 against the policy Complete implementation of Situation Background Action Recommendation (SBAR) communication model for handover across all services. 20% Reduction of attributable transfer of care issues internally. Improve data capture to enable focus on quality improvements. Work with external partners to reduce the number of transfer of care issues that impact on patients. Develop a patient held discharge passport. Page 74 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Improving End of Life Care 90% of patients die in their preferred place Target 90% patients died in Achieved their preferred place The Trust is committed to improving and embedding best practice in all areas of end of life care for patients and relatives/carers. The Trust appointed a Nurse Consultant for End of Life Care in June 2013 to lead the development and implementation of an end of life strategy to improve the care to patients and their families. The strategy has been developed with key stakeholders including patients; carers; staff; the public and hospice colleagues. On a national level it has been an important year for end of life care following the review of the Liverpool Care Pathway (LCP). The review undertaken resulted in the pathway being phased out with focus now on staff assessing patients and creating an individualised care plan. An audit was undertaken to identify the scope of the gaps in best practice, compliance with LCP and a baseline on which to focus improvement actions and develop a response to the removal of the LCP. Information on the decisions regarding reassessment and actions taken indicates that decisions to continue treatments or not were not always preceded by an assessment. A key strand of the strategy is to focus on ensuring that the workforce has the skills and competencies required to appropriately care for this vulnerable group of patients. Related competency assessments to match the skills required to provide safe, effective care have been developed and approved for implementation. The education and training programmes have been reviewed to enable our workforce to have the skills they require: For all new staff who provide clinical care to patients so that they have the fundamental skills to care for patients who may be at end of life or have long-term conditions and health issues that may make them consider their wishes for the future On how to care for patients to ensure they have appropriate medication to keep them comfortable at end of life To help staff have the difficult conversations about dying with individuals and families To enable our staff to discuss ‘Do not Resuscitate’ and to be able to work with the lead clinicians to complete the appropriate documents to allow for a Natural death. Page 75 of 153 The Trust has worked in partnership with colleagues at the University of Kent and Canterbury Christchurch University (CCU) to develop and deliver education and training on end of life care to nurses and doctors across the county. The Trust secured funding to develop an online training programme to support the public and health and social care staff to gain understanding and insight into Advance Care Planning. The Trust has benefited from collaboration with local Hospices including Demelza House and the CHYPs team for North Kent to help individuals including children plan for their future. Policies and procedures have been updated and new policies developed to ensure staff have the appropriate best guidance for end of life care. This includes a policy for care after death, ‘do not resuscitate orders’, and another focussing on verification of death. Regular forums have been established to allow colleagues from the local Hospices, third sector providers (such as Marie Curie and Macmillan) and commissioners for end of life care to discuss issues and areas for improvement. The aim is for the various stakeholders to work together to make sure patients are getting the right care and future developments meet the needs of the whole community. The Trust has already started using an electronic system such as the ‘Share my Care’ record which identifies patients’ wishes at end of life across local health providers. The community nursing staff have also been involved in a research project to help better understand carers’ needs for those caring for a family member or friend at end of life. The National study is led by the University of Manchester and aims to improve the support carers receive at end of life. In Dartford and Gravesham, staff have been involved in a project known as “Planning for Change”, a case management pilot to help identify those who are nearing the end of life to help support them and get appropriate care and plans in place. In West Kent, staff have been working to develop a rapid response service which aims to support patients including those nearing the end of their life to enable them to be cared for at home. Goals for 2014/2015: Improve written information and communication on support at end of life; Implementing the strategy to improve the experience for patients and those close to them (End of Life Strategy available) Take forward the work already underway to make sure our staff have the appropriate training and the right skills to provide the right care Listen to patients and their relatives and increase the opportunities for them to feedback to us Page 76 of 153 Review more data and information to ensure we provide high quality care. We will do this via our new community information system Improve ways of involving and assessing carers needs Improve discussions and documentation on patients preferences and choices including spiritual and religious needs Page 77 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Morbidity and Mortality Following the review of end of life care, More Care Less Pathway (2013) and the Francis report, we instigated a procedure to review all deaths within the 12 community hospitals to identify any areas of concern and to learn lessons to improve care and treatment. There were 52 deaths in community hospitals. 90% of these were patients admitted for end of life care, the other 10% were patients who were still undergoing active rehabilitation and the death was unexpected, but no cause for concern was found in any of the cases Key findings from the reviews for 2014 highlighted the following: • • • • • • Senior staff are committed to making sure staff are supported to manage care of patients at end of life The majority of the care provided was supportive and staff felt they had enabled patients to achieve a ‘good death’ KCHT currently has a lack of information for patients and relatives regarding Do Not Resuscitate Orders and end of life care planning Staff need to develop skills to recognise changes which suggest a patient is in their last days of life Lack of communication with families and updating on progress or change in symptoms Transfer of care into community hospital beds for end of life care could be improved. Work has continued throughout the year to assure that the implementation of The Deteriorating Patient Policy is embedded into practice and audit has been undertaken with a further audit on Resuscitation scenarios. Both these audits highlighted key issues including: discussions regarding DNA CPR decisions need to be documented in the patient records (using the MCA framework is the patient lacks capacity); staff competence in completing the National Early Warning Score (NEWS); actions taken when a patient’s condition deteriorates needs to be clearly documented and evaluated; poor team communication in resuscitation event. Detailed action plans are in place and a review of the competency based training on Basic Life Support which includes recognition of the deteriorating patient. This has resulted in revision and further development of the training to incorporate management and of a deteriorating patient and team communication. The competency assessment framework has been reviewed for NEWS. Page 78 of 153 Further work is required to ensure the audit recommendations and actions are embedded into practice to safeguard the patients. Goals for 2014/15: Implementation of End of Life training which includes recognising when a patient’s at end of life and competency assessments for clinical staff Developing information leaflets for patients and relatives on end of life care planning and Do Not Resuscitate Orders To work in partnership with our commissioners and other health and social care providers to improve transfer of care To continue to review mortality and morbidity To implement standard mortality rate reviews in all community hospitals. Revised competency based training for basic life support (BLS) will be included in clinical induction All community clinical staff to have completed training and competency by March 2015 target 85% compliance Revised BLS incorporating management and recognition of the deteriorating, patient, communication, National Early Warning Score and escalation and associated competencies to be rolled out. All clinical staff in Community Hospitals to have completed the revised BLS training and to be assessed as competent to achieve the 85% target by March 2015. Page 79 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Acute Pain Key National guidance recommends ensuring people feel supported to manage their condition and improve functional ability for people with Long Term Conditions and ensure people have a positive experience of care. Last year patient feedback identified that acute pain was an area that they wished the Trust to focus on. As a result the Trust concentrated on a pain audit to understand how pain was managed with patients. The pain audit showed 94% of patients received a holistic assessment within 24 hours of the first contact including pain assessment. 53% of the patients reviewed had an initial assessment that included what had worked well in the past in managing their pain. In 40% of patients, pain intensity was assessed using numerical scales. In 19% of patients this was not assessed at all which identified a key area that required improvement. The patient's preference for managing their pain was recorded in 43% of patients’ records. A communication aid was required for 3% of patients (those that had learning disabilities) to help assess their pain and its use and was recorded in the patients case notes. 83% of records showed that a patient's plan of care had been developed and discussed with the patient and/or their carer and agreed. An end of life audit undertaken this year showed that in 100 patients, 97% had appropriate pain relief prescribed. Children’s services were also audited on pain assessment and treatment. 67% of the children had a learning disability. 75% of those reviewed had a holistic assessment with pain assessed at the initial contact. In 50% of cases a pain assessment tool was used. Of these 50% of the assessments used the FACE tool whilst 33% used a numbers scale. In 100% of the case notes reviewed the risks and benefits of treatment had been discussed with the child/young person and/or parent as well as possible alternatives for treatment. An action plan is in place following the audit to address the issues highlighted. We now have a pharmacist on call 24 hours a day, 365 days a year for advice if required regarding medication which includes guidance on appropriate pain management for patients. Extensive training on syringe drivers and new equipment purchased to ensure patients at end of life have access to appropriate pain treatment. Page 80 of 153 The medicines management team has developed training packages using on line training and blended learning to train staff in use of medication. Goals for 2014/2015: Progress a task and finish group to take a lead on pain management and assessment. Develop a practice standard for pain Identify and implement suitable assessment tools and pain scoring charts that can be utilised as the basis for effective pain management. The tools will be suitable for children and those with disabilities including blind people and those with dementia. Develop a training package on assessing and managing acute and chronic pain 20% improvement in audit results especially in assessment of pain. Page 81 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Dementia The number of patients diagnosed with dementia is increasing, so ensuring that they receive appropriate care is important. In August 2013 the Trust appointed a Nurse Consultant for Dementia jointly with the University of Greenwich. In addition she leads the Dementia Cluster within the Centre of Positive Ageing at the university. The Nurse Consultant successfully acquired a place on the first HE KSS / BSMS Primary Care Dementia Fellowship Programme led by Professor Sube Banerjee with the development of collaborative working across KSS which is exciting for the Trust. A Dementia Strategy for KCHT has been developed through a Dementia Steering Group and consultation at the First Class Care Conference (2013) and includes clinical representation across KCHT’s workforce and the third sector such as Dementia UK and patients/users. A Dementia Care Pathway has been developed, an electronic resource for staff to use to support patients and their families/carers affected by dementia. Dementia awareness across the 12 community hospitals has been addressed through the implementation of the Butterfly Scheme, the development of dementia champions and dementia awareness training for all patient-facing staff. The Butterfly Scheme includes a symbol of a butterfly which can be attached to patient notes, or by their bedside, for patients with a possible diagnosis of dementia, to highlight this to all staff, while maintaining a level of confidentiality. The symbol of the butterfly will remind staff to use the REACH approach in communication: Remind the patient what has led to this moment Explain what is about to happen Arrange the bedside area to make sense and be assessable to the patient Check well-being, especially cleanliness and hydration History must always be verified Dementia awareness training has initially focused on community hospital staff, now this is completed the training will be adapted and delivered to community nursing staff. Following the completion of the training, staff voluntarily completed a dementia awareness questionnaire, with 521 responses. Staff attending training sessions feel confident in Page 82 of 153 recognising the early signs of dementia and how to communicate with a person with dementia. Case study Film stars and fish tanks for Edenbridge hospital With black and white film star pictures on the wall, you’d be forgiven for not realising you had stepped inside Edenbridge and District War Memorial Hospital. But the new look and feel is all thanks to a new initiative by Kent Community Health NHS Trust to provide a friendlier environment for patients with dementia to recuperate in. The day room has been overhauled to create a calm and relaxing atmosphere for patients, encouraging them to socialise and become more independent. Other improvements include open seating areas so patients can chat to each other more easily, improved access to books, magazines, television, music and information leaflets, a fish tank, better access to tea and coffee which they can help themselves to and black and white pictures of classic film stars on the main corridor walls. Rachel Daykin, Clinical Support Nurse Dementia Care, has been leading the changes with the hospital team and has also been involved in training all staff who come into contact with patients with dementia, including cooks, cleaners and porters. Page 83 of 153 She said: “It’s really fantastic to see the changes that have been made at Edenbridge hospital. Before the improvements, the day room looked very dull and dark and it was completely uninviting for patients. It was like a boardroom! “It’s really important we provide a relaxing and supportive environment for our patients and I know the changes have extended beyond the day room onto the ward. This is really positive for all our patients, but especially those who have dementia as it can be really frightening and isolating having to spend time in a hospital in unfamiliar surroundings. The black and white pictures are my favourite feature; they encourage people to reminisce and provide them with something familiar to talk about.” June Simmons, 70, from Tunbridge Wells, has been a patient at Edenbridge hospital for two weeks. She started to feel very short of breath in December last year and by the time she was admitted to Pembury Hospital she could no longer walk. She was diagnosed with arrhythmia and offered the chance to go to Edenbridge for rehabilitation before returning home. She said: “I came here for rehab after staying at Pembury Hospital and they have done a marvellous job helping me to walk again. As soon as I could walk with the frame they brought me into the day room to have dinner. It’s a lovely space to come and relax and chat. “I am agoraphobic so don’t go out much at home and I will really miss all the friendly chats in this room. I have made some really nice friends, felt 100 per cent supported and don’t want to go home!” Goals for 2014/2015: Focus on community staff to complete dementia awareness training with a pre- and post-audit dementia knowledge questionnaire. Continued support of community hospital staff to maintain development of the Butterfly Scheme and implementation of intermediate dementia training for clinical staff. Further development of the Dementia Care Pathway with information to support practitioners, and people living with dementia and their carers/families. Easy access to relevant information and the creation of a blog regarding dementia. Page 84 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time Children and Young People The Trust provides services for children and adults to support them to stay healthy, manage their long-term health conditions, help them avoid going into hospital and, when they have needed to be in hospital, help them to get home quickly. We deliver Children’s integrated therapy services outside of Kent in East Sussex. There is a large geographical spread of services, including areas of urban deprivation, and sparsely populated rural communities. We offer a range of hub and spoke service provision from clinics, as well as offering home and school based community visits – to ensure we see the child and family in a setting that is best suited to their clinical and social needs, and delivers care closer to home and school. Waiting List Initiative East Sussex Children’s Integrated Therapy Service In April 2013, KCHT took responsibility for the delivery of Children’s Integrated Therapy services in East Sussex. At the point of transfer to KCHT, there were 851 children found to be on waiting lists to see Occupational Therapy, Physiotherapy and Speech and Language Therapy. Some children had been waiting for nearly two years for an appointment. In discussion with commissioners, we agreed to carry out a waiting list initiative to clear all waits within nine months. This not only assessed children, but offered them a further three follow-up therapy appointments to complete therapy and discharge or to start therapy and, if required, transfer the child to the new service for on-going care. The waiting list initiative was successfully completed at the end of September 2013. A new system has been established to screen, prioritise and allocate all referrals to the service from 1 April 2013. New regular assessment clinics for all disciplines have been established to meet the target for assessment within 18 weeks of referral. In addition, any urgent referrals are now allocated and seen within two weeks of referral. Family Nurse Partnership This is a licensed researched based national programme specifically targeted to First Time parents aged 19 and under having their first baby. Each programme has 4 nurses working with up to 25 young parents each, in a researched, strength based parenting programme which can make a real difference to these young parents and the outcomes for their babies. The research base shows that where the Family Nurses can engage young people the outcomes it achieves are healthier pregnancies, better long term health and social outcomes such as reduced smoking, increased breast feeding, reduced substance use, Page 85 of 153 reduced post natal depression and achieves healthier relationships for the parents. Many engage in education or employment following the birth of their babies. For their babies there are reduced hospital admissions, reduced A&E and GP attendances, better immunisation, and greater safety in the home, greater school readiness and school attendance and in America where the programme has been in place for 30 years the children achieve better education attainment, more likely to find employment and reduce criminality. Many of these young parents have been school refusers and are Looked after Children and frequently do not engage with services. Our first team of 4 nurses and 1 Supervisor was established in January 2012 and within 12 months they had engaged 96 families onto the programme and achieved higher that national average engagement and retention rates with the young parents. Our first family will graduate from the programme later this month. Our licence to recruit up to another 100 families with an additional 4 nurses from January 2013 has commenced the fastest national expansion to the programme. We currently have 157 parents on the programme. Currently the service is provided in the following districts Swale, Thanet, Maidstone, Tonbridge and Malling which have the highest rates for young parents across the county. We have recently been granted further license for 1 supervisor and an additional 75 families which will expand the team by 3 Family Nurses, recruitment of the appropriate families will commence in Jan 2015 due to the licensing and training requirements for the team. Districts where the service will be expanded into are currently being negotiated with commissioners and the National FNP team. Universal Services The Children’s Universal Service includes Health Visiting, Family Nurse Partnership, School Nursing and Children in Care Nurses. The Trust now has 253.87 Health Visitors [HV] in post compared to 217 in 2012/13 and there are currently 106 students in training, they have the support of specialist mentors and their Practice Teacher which provides a ‘team around the student‘ model of delivery. This approach has been recognised and complimented at the recent NMC inspection with one of our partner HEIs. The students will qualify in September 14 and January 15, we intend offering all our students full time employment within the Trust. In the past year we have worked with the local universities to provide a variety of bespoke ‘return to practice’ courses with 8 Health Visitors completing and joining the team we have also been successful in attracting a further 15 qualified Health Visitors from out of area. Page 86 of 153 We recognise that having so many newly qualified staff, that it is even more important that we retain our experienced health visitors to provide support both to clients and staff. Therefore we have developed lead roles in areas such as domestic abuse and perinatal mental health which provides intense early support for families and early referral to safeguarding. The Domestic Abuse leads have been supporting over 200 families with children under 5 who are experiencing Domestic Abuse. By 2015 the increase in Health Visitors will ensure that all families in Kent are offered all the elements of the Universal Healthy Child programme, which will include an antenatal support visit to all parents, a new birth visit, a postnatal mental health assessment, a one year and two and half year development check. The needs of the children and families will be assessed and monitored and any additional support will be provided by the team or if required an onward referral made. Using initiatives such as Active Baby, the service will aim to help all children have a smooth transition from early year into school years. Active Baby - It is acknowledged that the start of life is a crucial time for children and parents, in laying the foundations of good health and wellbeing in later years. A child’s early experience and environment influences their brain development during these early years, when warm, positive parenting helps create a strong foundation for the future. Active baby promotes cognitive development through movement and positive parenting through interaction. This work has highlighted a growing issue of children arriving at school ill prepared to learn. This includes issues such as poor toilet control. Health Visitors and School Nurses have responded to these issues by developing a programme to support children and families. All health visitors will be trained to promote ‘active baby’ and all children centre and early year’s staff will be trained in this approach. Our lead Health Visitor Active Learner has now provided “champion” training to health visitors, children’s centres and some early years settings a total of over 550 staff across these settings in Kent have been trained to offer families these crucial messages for their baby’s development. 85% children in the original pilot area are reported by teachers as “starting school ready to learn” as opposed to a figure of around 25% four years ago. Children in Care Specialist Nurse The nurses provide all children in care with a review health assessment; they monitor the health status of children and young people and help them to identify any health issues that may exist. They work with the children and if appropriate the carers, to develop health care plans that will highlight any issues, they make recommendations and if required referrals to other health services, these plans are then monitored and reviewed as appropriate. The following is just some of the feedback from the client experience: “I was impressed with the service and the care and attention my children received” Page 87 of 153 “The Nurse was very friendly and polite” “The Nurse was funny and fun” “The Nurse was very kind and didn’t make me feel insecure about my weight” “The Nurse understood what I had to say even though some things were hard to talk about, she listened and understood” Agreed goals for 2014/15: Further expansion of Family Nurse Partnership programme to increase to maximize capacity for 250 parents by March 2015. Increase Health Visitors to 342.2 by March 2015. Further develop the health visiting lead roles for CONI, Infant Feeding and Safeguarding Health visitor active learner training will continue to increase the training to 1000 staff School Nursing In School Nursing there are currently 106 students and the team has increased the Practice Teacher capacity to 33. We have developed an innovative Specialist Mentor and Team around the Practice Teacher model of delivery. This approach has been recognised and complimented at the recent NMC inspection with one of our partner HEIs. Clean and Dry was one of two Early Implementer Site Projects focussed on transition from early years to school. School nurses and Health Visitors identified that a large number of children in the Dover/Deal area were starting school in nappies, not having been toilet trained. ‘Clean and Dry’ is a multi-agency approach to supporting parents in toilet training. The project won national recognition and media coverage, with staff presenting at DH conferences nationwide. In addition HPV vaccinations in Kent school totalled 95.5%. Average uptake for all 3 vaccines was 87%, higher than the England average. KCHT school nursing teams were the best performing in the SE Coast region. National Child Measurement Programme (NCMP) uptake academic year 2012/13 – KCHT school nursing teams achieved over 90% uptake in both Year 6 and Year 7, exceeding the target. In recognition of the important role school nurses have to play in the delivery of the Healthy Child Programme, KCC commissioners invested in an additional 4 whole time equivalent all year round SCPHN (school nursing) for the West of Kent. 2013 School Nursing Conference was held with Viv Bennett, Director of Nursing at the DH and Public Health England as the Key Note speaker. Page 88 of 153 Clean and Dry Clean, Dry and Ready for School is a new initiative by Kent Community Health NHS Trust. School nurses and health visitors are working with nurseries and primary schools to identify children who need help with toilet training before starting school and those not yet clean and dry at school. The pilot initially involved KCHT working with two nurseries attached to two schools – Warden House Primary School in Deal, Bright Sparks Preschool in Deal and Shatterlocks Infants School and Nursery in Dover. It’s been so successful it’s now being rolled out across Kent. School Nurse Practice Teacher Chris Beer said: “We had lots of contact from schools saying they were seeing a rising number of children starting school who were still wearing nappies and children who were not staying clean and dry during the day. “We looked at 18 schools and found 24 children who were not toilet trained. While the odd accident is acceptable, we want to make sure children and parents are supported so children are clean and dry before they start school and therefore ready to learn.” One of the main problems can be that children are not drinking enough fluid during the day. “What we hope is that by working with children who are struggling early on in nursery, we can support them so by the time they get to school they will be clean and dry and can concentrate on learning.” The team is also looking at how through children's centres, it can reach those children who do not attend nurseries, by holding coffee mornings when they start schools to meet with parents. Page 89 of 153 Goals for 2014/15 Expand the existing Immunisation Team Introduce a Band 5 Development programme to support recruitment onto SCPHN programme and retention of staff Roll-out ‘Clean and Dry’ training to all School Nurses to support transition from early years to school Develop a transition pathway from Year 6 to Year 7 Develop an integrated School Nursing/Healthy Schools framework for the delivery of HCP. Expand the delivery of the initial assessments core service across KCHT Page 90 of 153 Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time National Institute for Health and Care Excellence (NICE) Compliance with Assessments KCHT receives information from NICE for distribution, assessment and implementation across the organisation which sets out best practice standards. The organisation receives the following on a monthly basis from NICE: • • • • • Interventional procedures (relate mostly to surgical procedures) Technological appraisals (these mainly relate to new medicines and must be acted on by law) Medical technologies (relating to medical equipment) and diagnostics Clinical guidelines (these usually contain many recommendations) Quality standards (these mainly relate to the priorities to be focussed on in the clinical guidelines). The Care Quality Commission (CQC), in its document, A New Start, June 2013, advised that it will monitor and assess standards of quality, will work with NICE to ensure these align with the NICE Quality Standards and provide a comprehensive spectrum of standards, as recommended by Robert Francis. 28 quality standards were issued in 2013/14. Of these, 22 were relevant to KCHT and standards of practice have been reviewed against the standards. Goals for 2014/2015: • To implement commissioned standards as identified by NICE Page 91 of 153 SUMMARY Goal 2: To improve outcomes by developing integrated care pathways ensuring the right care, right place, right person, right time The Trust has made significant progress this year on End of Life and Dementia with strategies in place. Baseline work has been completed to continue to build upon for next year. Children and Young people’s services have performed extremely well across all initiatives to ensure positive health outcomes. Transfer of care is an area where we will need to strengthen to ensure all transfers are safe and transition from children’s to adult services are seamless. Recognition and management of the deteriorating patient is a key area where the trust has to continue to focus on next year. All areas have key goals to meet throughout 2014/15 to ensure sustainability of quality and patient outcomes. Page 92 of 153 Goal 3: Measurable year on year improvement in patient experience, engagement and satisfaction Improving Patient Feedback The Trust takes patient experience and complaints very seriously and works hard to act on that feedback to make improvements for all patients. We are using 230 iPads with ‘Meridian’ software to capture patient feedback in real-time in people’s homes and at clinics and community hospitals. Feedback is consistently positive. We receive around 1 complaint for every 10,000 patient contacts. KCHT receives relatively few complaints relative to patient contacts; however, the overall number of complaints has increased during 2013/14 to 362 compared to 301 in 2012/13. This trend is in common with other NHS trusts in Kent and may also reflect increased publicity about how to complain. The trust encourages people to give their feedback, whether it is good or bad, so that we can learn from it and improve the patient experience. The number of complaints varies across localities. 289 of the 362 complaints for 2013/14 were reported in the KO41 an annual return to the Department of Health and required some form of investigation to resolve. There have been four complaints reported where the patient has suffered harm and these have been raised as serious incidents and full root cause analysis investigations have been completed. Learning from complaints has resulted in a variety of service improvements and changes to improve our patients experience such as: Improvements to appointment systems in community paediatrics. Intermediate Care Therapy services have been extended to seven days a week in some localities. Promotion of local referral numbers / point of contact for community nursing. Service user involvement in Dental services. Podiatry provided a facility for patients to leave voicemail when reception was not staffed. Whilst the main subject continues to be clinical treatment, there has been an increase in complaints about waiting times either for assessment or follow-up appointments relating to a number of services, but in particular to Children’s Speech and Language Therapy in some areas, Podiatry across Kent and Dental services in prisons. A deep dive report was presented to the Trust’s Quality Committee and the improvement plan was approved. Complaints about waiting times have reduced since October 2013, and therefore it is likely that the actions are proving effective. Page 93 of 153 The number of complaints per service needs to be viewed in the context of the number of patient contacts. For example, in January 2014 Community Nursing services in Kent had one complaint per 4,286 contacts whereas Dental had one per 2,008 contacts. Patient Experience - The Trust’s overall patient experience score for April 2013 to March 2014 is 95% based on 57,362 surveys. Overall patient experience is very positive, and the amount of patient feedback collected each quarter is now more than the Trust collected on a yearly basis in 2011/12. Therefore we can be assured that overall most patients have a positive experience. There has been an improvement in patients reporting they feel involved in decisions about their care and treatment compared with 2012/13. A variety of actions from patient experience feedback have been implemented In Livingstone Community Hospital a privacy room for patient discussions and private matters has been provided. Eye masks/pads have been provided for patients who have difficulty sleeping. At Whitstable and Tankerton Community Hospital a HCA now has one shift per week dedicated to doing activities with patients on Friends Ward. At Tonbridge Community Hospital a second phone has been provided to take incoming calls and more activities are taking place at the weekend. At Faversham Cottage Hospital volunteers are now coming in at supper time to assist patients. In Adult Musculoskeletal Physiotherapy a room is now available to hold sensitive conversations. In Community Orthopaedic and Chronic Pain ICATS texts are being sent to patients advising them of appointments booked an additional Podiatrist has now been recruited School nurses now request a private room to be available after school Chlamydia assemblies and information is now available to signpost young people to other venues where testing can be provided. Sexual Health has a choice of walk-in slots as well as booked appointments. Friends and Family Test We are one of the first Community Services Trust’s in the country to introduce the NHS Friends and Family Test which is included in all KCHTs services surveys. Patient’s clients are asked if based on their experience today, would they recommend the service to their friends and family. The scores are calculated based on a range of answers. Page 94 of 153 The maximum score is +100 and the minimum is -100. KCHTs had an overall score of +77, which is positive and is above the benchmark of +75 for aspirant Community Foundation Trusts (ACFT) recorded up to February 2014. We will strive to continue to improve our score during 2014/2015. Area Trust-wide FFT Score Total Responses +77 15,688 Extremely Likely Likely 12,320 2,948 Neither Likely or Unlikely Unlikely 203 51 Extremely Don't Unlikely Know 51 115 Stakeholder Engagement The Trust has made significant progress in actively engaging with stakeholders and has exceeded the targets for 2013/14. Target Increase members on patient engagement network by 20% Increase membership to reflect the local population Increase groups/reps on a further 10 services Recruited 2,673 new members in total. Achieved by 55% Increased members who are listed as working class or non-working by 134. Increased male members by 556. Achieved increase to 13 Increased members aged 22 and over by 1,626. The Trust engages with stakeholders in a number of ways, and generally receives very positive feedback about the quality of care and positive attitude of our staff. This includes: An on-going programme of attendance at voluntary and community sector events and forums, with information stands, and as guest speakers. Examples of the 77 events attended in 2013/14 include the Nepalese community event in Ashford, Kent County Show, launch of the information service in Dartford, Dartford Elders Forum, Gravesham Over 50s Forum, Ethnic Minority Independence Council forum meetings and community event in Canterbury, Roma event in Dover, Little Forest Children’s Centre in Tunbridge Wells, Fibromyalgia group in Swale and Tunbridge Wells, and Tunbridge Wells Access Group. A Patient Engagement Network with 130 members, 32 of who are involved in attending the Trust’s committees and working groups as patient/public reps. Others sit on Page 95 of 153 interview panels; take part in PLACE visits; and assist the patient information team to develop user-friendly patient information. Work with the District Partnership Groups (people with learning disabilities) to develop Easy Read information, including patient leaflets, posters and an Easy Read version of the Trust’s quarterly Community Health magazine. A Patient Experience Committee which oversees all our patient experience and public engagement. This has places for 14 patient/public representatives. We have a Memorandum of Understanding with Healthwatch Kent. We have attended a training session with their prospective volunteers to talk about KCHT and NHS, and Healthwatch have two places on our Patient Experience Committee. We have met all but one of the CCG Board Lay Members, and attended one of their lay members meetings at the invitation of the South Kent Coast Lay Member. Within Children’s Therapy services in Kent and East Sussex, we will be expanding current levels of parental engagement and feedback through use of parent and carer forums for disabled children or those with long term conditions. We co-ordinate a quarterly forum of patient and public engagement leads from NHS Trusts across Kent. CCG Board Lay Members and Healthwatch are invited to attend these meetings. Goals for 2014/2015: Improve patient experience in services that are not reaching the Trust’s target Support services to make changes as a result of patient feedback including complaints and ensure that changes impact positively on “protected groups.” Ensure all services have clear and accessible patient information both online and printed, e.g. community hospital booklet, patients in community. Support services to improve information to patients and carers about further support available. To continue to improve KCHT Friends and Family Test score. To improve engagement with hard to reach groups. Page 96 of 153 Goal 3: Measurable year on year improvement in patient experience, engagement and satisfaction Improve Nutrition and Hydration Malnutrition continues to affect over 3 million people in the UK with approximately 1.3 million being over the age of 65. The Trust has an on-going commitment to ensuring patients receive the best nutritional support and risks associated with malnutrition are identified and acted upon. The Trust has an established Nutrition and Hydration Group which has a comprehensive action plan in place that includes: A malnutrition universal screening tool to risk score for malnutrition. Nutrition policies. Admission questionnaire for patients and their carers to support personalised care planning. Nutritional resources available for nursing staff to leave with patients. Dietetic referral system for all community hospitals. Hydration focus for community hospitals – a standard of seven daily drinks are offered to our patients as well as the water jugs. A Nutrition and Hydration Nursing handbook for all nurses. This holds first line actions for staff to take in the prevention of malnutrition and dehydration. The Hydrant is a hands free hydration system which the Trust trialled as part of our commitment to improving hydration. The overall awareness of the importance of hydration amongst staff has increased. It has shown that a multidisciplinary approach is needed to support hydration. The project has led to a variety of initiates being implemented. Ensure that every patient has a nutritional care plan specific to their needs – ongoing action to increase awareness and knowledge regarding patients’ nutritional needs and personalised care plan. Nutrition training modules are currently being rolled out. The aim is to establish 100% compliance of identified staff to be trained in Nutrition and Hydration by the end of 2014. New menus As part of the campaign new menus have been introduced and these include: Seasonal menus – and easy to read menu booklets. 24 hour / 7days week hot meal availability. Page 97 of 153 New crockery and mats (to support Dementia friendly initiatives). Wider range of snacks and drinks available in snack cupboards. Wider range of puree and modified consistency diet options. Afternoon tea with homemade cake daily. Cooked breakfast at weekends. The menus have been assured by the Dieticians and Speech and Language therapists for nutritional quality and safety. Other Activities Nutrition and Hydration Week Nutrition and Hydration is essential to patient care and in 2014/15, our new campaign was launched with tea parties across the Trust during this year’s worldwide Nutrition and Hydration week 17 – 23 March 2014. The aim of the Nutrition and Hydration Week 2014 was to: Raise awareness and improve understanding of the vital importance of good nutrition and hydration. Illustrate how people can improve their quality of life by making changes to eating and drinking habits. Show staff the preventative role they can play in reducing malnutrition-related illnesses. This event launched our Nutrition and Hydration 2014 yearlong campaign. The event was a success for patients and staff. Page 98 of 153 Goals for 2014/2015: Aims for 2014/15 are to achieve the following outcomes: 1000 KCHT nursing and allied health professionals to have attended face to face nutrition and hydration training by March 2015. 50% of Health Care Assistants to have accessed face to face nutrition and hydration training by March 2015. Nutrition and Hydration information to be available in community hospitals discharge packs by August 2014. Ensure all community hospitals are using coloured crockery/coloured mats and offering finger foods for patients with dementia by October 2014. Audit hydration practices in community hospitals by January 2015 Audit the completion of MUST (assessment of nutritional status), referrals to dieticians and nutritional care plans by March 2015. Case study ‘Importance of nutrition and hydration highlighted across hospitals’ Community hospital staff across Kent pulled out all the stops to dress up as traditional tea maids and serve patients drinks, homemade cakes, and fruit to highlight how important the right food and drink is to recovery. The event, led by manager Tiffany Maxted and our Nutrition and Dietetics Service, was organised to celebrate this year’s Nutrition and Hydration week in March 2014. Page 99 of 153 Goal 3: Measurable year on year improvement in patient experience, engagement and satisfaction Implement the six areas of the CNO Caring with Compassion strategy The implementation of the Caring with Compassion strategy was launched with a series of engagement events with patients, carers and staff to define ‘compassionate care’ for Kent. The level of involvement was extremely high and the final definition was launched at the 1st Class Care Conference in November 2013 which was attended by the Chief Nursing Officer of England and the Chief Executive Officer of the Patient Association. KCHT definition for Compassionate Care: “Hear my story, respect me, be kind, acknowledge my wishes, respond and understand my needs and care like you mean it, because you do.” KCHT has made 2 DVDs highlighting compassionate care, and supported further development of “Sit and See™” tool with the author to ensure it met the needs of a community trust. It is an observational tool which aims to capture the quality of interaction between patients and staff as Positive, Passive or Poor. A robust action plan has been developed to support the implementation of the strategy including: Care – integrated care pathways. Compassion – align 15 Steps, Dignity and Respect standard, PLACE inspection. Courage – “Seen Something, Say Something” campaign encouraging staff to raise concerns. Competence – development of competency framework and role profiles; developing community nursing tools to support competency and safe staffing and part of a project with the University of Kent in developing a shared purpose framework and community nursing tool. Communication – introduction of SBAR (Situation, Background, Assessment, Recommendation) as the Trust communication tool for staff. Commitment – the development of professional practice standards clarifying expectation for staff in relation to specific areas of practice; introduction of values based recruitment. Page 100 of 153 Goals for 2014/2015: Roll out the observational “Sit and See™ tool” in practice and evaluate the findings in community hospitals by end of quarter two. Continue to support national and local developments in staffing competencies for community nursing by March 15. Further develop the competency frameworks across all areas of the Trust by March 15. Develop a culture where everybody feels able to deliver first class care through the implementation of the culture change plan. Communication that is focused on the patient and their family - this will be measured through patient questionnaires. Treat everybody with compassion with a commitment to do the best we can - this will be measured through patient experience, staff survey and appraisal. Page 101 of 153 Goal 3: Measurable year on year improvement in patient experience, engagement and satisfaction Improving Health and Wellbeing The Health Checks Team has given health checks to 32,000 people (34% uptake of invitations sent) and is aiming to achieve a minimum of 50% of NHS Health Checks from the invited population next year. The team worked closely with GPs, pharmacies and other providers to ensure the invites were sent in a staggered way to prevent any long waiting times, all clients received an appointment within 4 weeks of a request. The team received positive comments on the service by their clients. The NHS Health Check programme aims to help prevent heart disease, stroke, diabetes, kidney disease and certain types of dementia. Everyone between the ages of 40 and 74, who has not already been diagnosed with one of these conditions or have certain risk factors, will be invited (once every five years) to have a check to assess their risk of heart disease, stroke, kidney disease and diabetes and will be given support and advice to help them reduce or manage that risk. The Stop Smoking service has received an average of 92% positive patient experience this year. The team has reviewed its service model and has linked in to the health trainer service for on-going behavioural support to prevent relapse and more targeted work in areas such as mental health. The team has strengthened their links with Kent and Medway Partnership Trust which has agreed to become smoke free next year. There are only two mental health trusts in the country which are smoke free. Target 2013/14 95% of patient asked about smoking as part of their assessment 90 % of patient asked were offered a referral to stop smoking services Achieved Achieved The Health Trainer Service has seen over 4,800 new self-referring clients this year. Clients have been achieving excellent outcomes with 73% of all goals set being fully or partly achieved. The service sign posted clients for additional support for weight management, stop smoking, increasing physical activity and social care support such as housing, benefits and education. Clients have reported over 98% satisfaction with the service. Page 102 of 153 Healthy Weight - The Healthy Weight team deliver specific programmes for families, young children and adults with a body mass index (BMI ) from 25 – 40+. The team will also coordinate the delivery of community schemes including East Kent Health Walks, an Exercise Referral Scheme and Fresh Start, a community weight management programme. Working in partnership with schools, pharmacies, community centres and GPs we provide sensible, practical help and advice to anyone wanting to change to a healthier lifestyle. We specialise in assisting the most vulnerable populations in the areas of greatest need. There is significant evidence that being a healthy weight is vital for long term health and wellbeing and can prevent long term conditions such as hypertension, heart disease, type 2 diabetes and certain types of cancer. We have good engagement with over 90% client satisfaction and we work with our external providers who deliver services on behalf of KCHT to conduct patient satisfaction and experience feedback to enhance our services further. Self-Management - KCHT has developed a Self-Management Steering Group which is progressing well and has developed the “Making every contact count strategy” which sets ten priorities to improve pathways, develop easy referral processes, enhance training provision to staff, to provide holistic support and strengthen services for self-management to promote independence. Sexual Health - integrated sexual health services allows service users to access all the services they need in one visit and implementation of a Hub and Spoke model is underway. There are 35 different sites across Kent and Medway and over 100 clinical sessions per week. Screening supports Public Health targets to increase the early diagnosis of HIV and increase diagnosis of Chlamydia. Staff have developed new competencies to allow them to work across the breadth of the service. Feedback from patients shows that they appreciate the services being on one site, which was in response to the negative comments regarding waiting times. The service is also aiming to increase patient participation through social media including Twitter and Facebook. Page 103 of 153 Case study Tilly happy to be in the spotlight after help from Healthy Weight Team Chirpy teenager Tilly Penn used to refuse to pose for family snaps – now she’s thrilled with her professional portfolio photos for a London acting agency and is feeling fit, healthy and fabulous – with help from the Healthy Weight Team at Kent Community Health NHS Trust. “I was never the skinniest girl in the class,” smiles 13-year-old Tilly, who lives with her mum Nina in Dover. “But I’d always loved PE until a couple of accidents put me out of action and the weight started to creep up.” In a series of unfortunate events, two years ago Tilly broke her arm and then suffered a fractured leg the following year. “Basically in years seven and eight at school I couldn’t take part in PE or do any exercise at all,” said the One Direction fanatic and Dover Grammar School student. “But I met the Healthy Weight Team at a school sports open day and was told about Ready Steady Go. I thought, ‘I could give that a go’.” Mum Nina works for P&O ferries at Dover docks and was the first to admit that the family had got into some bad habits when it came to mealtimes. “Because of my shift work I often opted for takeaways or ready meals for me and Tilly. We both wanted to be motivated to stay healthy, that’s where Ready Steady Go came in.” Tilly and Nina started the programme in January 2013 at a local school. “It was really good fun,” said Tilly. “I was worried at first but I met some really nice people and we made lots of friends.” Ready Steady Go is a free, fun course, which covers healthy eating, being more active and changing family routines to encourage the whole family to take steps towards a healthier future. “The programme showed us that cooking from scratch didn’t have to be hard work, we just needed to plan ahead and be a bit more organised,” says Nina. “Now I watch the portion sizes and we always eat together at the table. It’s made a real difference.” “I’ve got loads more energy now,” says Tilly. “I eat breakfast every day and I usually walk to school. I’ve even improved my grades.” Tilly also gets out and about in Dover harbour twice a week to take part in a rowing club, which she loves. “I’ve been going for five weeks and I really enjoy the exercise and the fresh air. I’m glad we did Ready Steady Go and I’d recommend it to any family that wants to be healthier.” Page 104 of 153 Goals for 2014/2015: Increase target numbers of smokers successfully quitting by developing and implementing a new Stop Smoking model with commissioners. The focus will be on behaviour change and harm reduction as well as quitting. Develop and implement Every Contact Counts strategy. Enhance health improvement services for mental health clients addressing the recommendations within “Closing the Gap.” Implement electronic records for all services including Sexual Health. To continue to access the target population at risk of chlamydia to screen and treat. Page 105 of 153 SUMMARY Goal 3: Measurable year on year improvement in patient experience, engagement and satisfaction Overall the Trust has made positive progress against this goal with complaints increasing which is positive and resulting in changes in practice. Patient experience is very positive and achieved the target with Friends and Family Test results comparing positively against Aspirant Foundation Trust. Trust stakeholder engagement has increased considerably. Nutrition and hydration is fundamental to quality care and steady progress has been made and continued work is planned for 2014/15. All health and wellbeing initiatives have demonstrated achievements. The Caring with Compassion strategy is being implemented and progress continues. Goals for 2014/15 all aim to ensure we improve on the good work we have achieved and clearly demonstrate we are listening to our key stakeholders. Page 106 of 153 Goal 4: Promoting a culture of accountability and openness Information Governance Data Quality Statement Effective delivery of patient care relies on good quality information and is essential if improvements in quality of care are to be made. Historically the quality of data captured by services working in a community setting has been poor due to a lack of investment in information systems. Background and Requirements The Trust has a number of statutory responsibilities relating to the collection and reporting of information. These range from the requirement to complete a number of national returns, to the need to collect specific data sets for various services that the Trust provides. There are also a number of local contractual requirements such as the need to supply a number of local commissioning data sets commissioners on a monthly basis covering the activities of many services the Trust provides. The Trust is also required to accurately report levels of activity and performance against a number of key performance indicators and as well as reporting achievement against the national and local CQUINs and reenablement schemes. The Trust is also required to provide accurate information internally to support clinical and business decision making. KCHT is taking the following actions to improve data quality: Assurance Policy: KCHT has a Data Quality Policy in place which is intended to raise the profile of data quality and the subsequent information derived from it within the Trust. Basic principles outlining the roles and responsibilities of staff the need to have a robust data quality audits and governance arrangements for monitoring the policy implementation. Governance: The Information Quality Improvement Group (IQIG) meets on a quarterly basis and has a membership which includes all ‘key’ information system leads, Information Governance and Information Technology teams. The focus of the group to drive the implementation of the data quality policy, ensure standard operating procedures and best practice are followed and to review data quality audits and associated action plans. The Information Quality Assurance Group (IQAG) oversees improvements in data quality and completeness to provide assurance to internal and external stakeholders. Action Plans: There are various action plans in place that aim to improve data quality relating to the Trust’s corporate and clinical systems. These range from system specific Page 107 of 153 plans put in place following audits, to higher level plans covering local or national data sets / data standards. Monitoring: Internally data quality action plans are monitored via the IQIG and the IQAG. The Trust’s commissioners also monitor a ‘Data Quality Improvement Plan’ which forms part of the contract. Reporting: The data quality and completeness indicators included in Monitor’s Compliance Framework have been incorporated into the Trust’s Integrated Performance Report. In addition, data quality star ratings have been added to this report along with a number of data quality indicators to raise the visibility of data quality within the organisation. KCHT currently has no single, centralised, integrated patient records system in place. Implementation of a new Community Information System (CIS) will address many of the data quality issues within the Trust, as the system has been configured to comply with all relevant data standards. The system will be fully implemented during 2014/15. NHS Number and General Medical Practice Code Validity Statement Kent Community Health NHS Trust submitted records during April 2013 to March 2014 to the Secondary Uses Service (SUS) for inclusion in the Hospital Episode Statistics which are included in the latest published data. The percentage of records in the published data which included the patient’s valid NHS number was 99.8% for admitted patient care. The percentage of records in the published data which included the patient’s valid General Medical Practice Code was 100% for admitted patient care. It should be highlighted that data are currently only submitted to SUS for ten of the twelve Community Hospitals which KCHT has responsibility for. The Trust will be deploying a new system to all twelve hospitals during 2014/15 which will enable SUS to be collected and submitted. Page 108 of 153 Payment by Results Statement KCHT has not been subject to the Payment by Results clinical coding audit during the reporting period 2013/14. Additional Statements During 2013-2014 the Kent Community Health NHS Trust provided and/or sub-contracted 62 relevant health services. The Kent Community Health NHS Trust has reviewed all the data available to them on the quality of care in of these 62 relevant health services. All services are subject to a contract. The income generated by the relevant health services reviewed in 2013-2014 represents c.94% per cent of the total income generated from the provision of relevant health services. Information Governance Statement KCHT Information Governance Assessment Report overall score for 2013/14 was 81% and was graded satisfactory and green. Kent Community Health NHS Trust has shown significant improvement in the Information Governance Toolkit Assessment (IGTA) for the period 2013/14. The compliance score submitted for 2013/14 is 81%, exceeding the previous year’s score by 6%. All requirements have met the minimum level 2 compliance, and the IGTA is rated as “satisfactory”. The work plan for 2014/15 will include continued auditing of compliance. Page 109 of 153 Goal 4: Promoting a culture of accountability and openness Clinical Audit By the start of each financial year KCHT has agreed an appropriate planned programme clinical audit activity designed to assess our performance against local and national standards of care. Statement During 2013/14 two national clinical audits covered NHS services that KCHT provided. During that period KCHT participated in 100% of the national clinical audits it was eligible to participate in. The national clinical audits KCHT is eligible to participate in during 2013/14 were as follows: National Epilepsy Audit – this did not relate to core business of the Trust and therefore no eligible patients were identified. However, we will re-evaluate our applicability of this audit in 2014/15. to the Trust. Sentinel Stroke National Audit Programme For 2013/14 there were no national confidential enquiries that KCHT was eligible to participate in. However, for 2014/15 there are already 3 national confidential enquiries that are relevant to KCHT. These include: 1. Lower Limb Amputation – organisational survey 2. Mortality Review 3. Sepsis – organisational survey The reports of two national clinical audits were reviewed by KCHT in 2013/14 and KCHT intends to take the following actions to improve the quality of healthcare provided. Page 110 of 153 National Clinical Audit Title Findings/outcomes Falls and bone health in older people Falls screening tool 1 to be incorporated into the new electronic community information system to ensure all patients receive relevant falls assessment The screening tool will be on the staff intranet for easy staff access in the interim Online training is available through the staff intranet for community hospitals staff and has been added to the training needs analysis under essential to role Falls awareness training is being introduced for all clinical staff within KCHT A patient leaflet and booklet to provide advice about falls prevention has been developed. The outcome for patient will be improved screening, risk assessment and tailored care package. KCHT has proposed an annual inpatient HIV audit is undertaken with the acute trust. However, KCHT do not manage HIV inpatient services. In line with other providers, and good practice, HIV inpatients are jointly managed under the care of an HIV consultant with an admitting Consultant. Complex inpatients are transferred to a tertiary HIV centre in line with locally agreed pathways. The outcome is that the testing for HIV is now more widely promoted through a variety of training methods and community events resulting in earlier detection and treatment. National audit of Treatment & Care of HIV infected inpatients EFFECTIVNESS OF THE LOCAL AUDIT PROGRAMME In order for a clinical audit to be recorded as complete by the Trust every single action identified from the audit must be implemented. At the end of 2013/14 350 actions designed to improve the quality of care for our patients had been implemented as a result of clinical audit. Examples of actions undertaken or planned include: Ensure that key data requirements for record keeping are incorporated as mandatory fields in our new Community Information System. Musculoskeletal Physiotherapy to introduce a Whiplash Assessment Form. Community Orthopaedics to introduce waiting list system to monitor follow ups after MRI and confirm the serious pathology pathway. Mandatory workshops have been introduced for all staff required to monitor Telehealth to ensure staff competency and capability and to ensure that we continue to deliver high quality care to our patients. Page 111 of 153 Redesign consent audit instrument to reflect patient impact and assurance in line with CQC Outcome 2 Standards testing design to ensure reliability and clarity in use. Implementation of a monitoring system for wards incorporating review of hydration practices through the nurse indicators. The Fresh Start Programme will be monitored to ensure adherence to inclusion criteria to ensure that all clients with a BMI in excess of 35 are referred to dietetics. This will improve the criteria pathway and ensure the relevant service meets the clients’ needs. Datix incident reporting to record being open for all patient safety incidents. Increase the awareness and use of Antimicrobial Guidance. Improve clinical coding to better capture all post exposure prophylaxis consultations. Areas of good practice and positive outcomes for patients identified by local clinical audit include: Documentation audit highlighted that staff are aware of and able to apply the principles of good record keeping taking into account information governance and relevant professional standards. Whiplash Audit showed that there are very positive treatment outcomes for patients suffering from whiplash following treatment by Musculoskeletal Physiotherapy. Management of MRI referrals in Community Orthopaedics Audit demonstrated that regular review of referral criteria has been undertaken to ensure appropriateness of referrals. Telehealth re-audit confirmed that Kent Community Health Trust is seen as a national leader in relation to Telehealth. We have hosted many other organisations to visit and review our systems and processes. We were one of the first organisations to develop protocols and policies to support the monitoring for patients using Telehealth – therefore the implications of this audit will be felt Trust wide and we must ensure our st monitoring processes are robust and 1 class. Consent audit demonstrated positive results in terms of patients receiving information regarding their care, treatment and support options and information on the benefits and risks. Hydration in Community Hospitals Audit led to the introduction of nutrition and hydration prompts. These are used to identify patients’ needs on admission to the ward and support individualised care planning. Fresh Start Audit showed that 99% of clients on the Fresh Start Programme achieved their weight loss/maintenance goals. Being Open Audit demonstrated that 95% of staff are aware of the principles of Being Open. Audit to Identify Appropriate Prescribing for patients with Bacterial Infections demonstrated that there is excellent awareness of the associated risk with the concurrent use of stomach acid suppressants and antimicrobials amongst prescribers and staff. Page 112 of 153 Re-audit of HIV Post Exposure Prophylaxis demonstrated that there has been a significant improvement of the appropriate prescribing of post exposure prophylaxis from 69% in 2009 to 90% in 2013. OTHER ACHIEVEMENTS FOR CLINICAL AUDIT KPI’s were introduced around number of due audit recommendations implemented (set at >=80% to receive green RAG rating). Trust position at end of financial year was 85%. Outcomes for patients and staff are now included against all recommendations in an action plan. The Clinical Audit Group and Department have enjoyed the continued support and input of 2 patient representatives. Strategic Clinical Audit Co-ordinator now Chairs South East Clinical Effectiveness Network (SECEN) and feeds into the National Quality Improvement Clinical Audit Network which helps to drive the national clinical audit agenda. Through Chairing SECEN the Strategic Clinical Audit Co-ordinator was involved in presenting at the Healthcare Quality Improvement Annual National Conference. In addition, a poster was also presented at this national conference on the KCHT Clinical Audit Action Plan Monitoring Process. CONCLUSION Where concerns are identified in relation to individual audits by the Clinical Audit Department but are not addressed by recommendations formulated by the project lead, this will be escalated to the appropriate directorate group responsible for clinical audit. Where issues remain outstanding these are escalated to the Medical Director and the Clinical Audit Group. Outcomes for patients and staff are now included against all recommendations in an action plan. This encourages auditors to focus on the on the audit output rather than the process of action planning and managing change i.e. there is a clear understanding of how each action from the audit will improve care for our patients. AUDIT PROGRAMME 2014/15 The audit programme for 2014/15 was approved by the Clinical Audit Group on 20 th March 2014 and consists of 160 clinical audits. Forward Planning sessions were held by the Clinical Audit Department and Head of Risk Management with Directorates in order to ensure that the programme for 2014/15 was systematically prioritised by using the HQIP 4step prioritisation model as outlined below: Priority 1 – External “must do” audits e.g. national audits, CQUIN audits, audits of NICE Guidance or other national priority areas. Page 113 of 153 Priority 2 – Internal “must do” audits e.g. audits focussed on risk and quality issues identified from a number of sources such as clinical governance, risk registers and complaints data. Priority 3 – Directorate Priorities Priority 4 – Clinician Interest This ensures that the KCHT Clinical Audit Programme for 2014/15 reflects relevant national priorities and is informed by local quality and risk issues. Page 114 of 153 Goal 4: Promoting a culture of accountability and openness Research and Development Research and Development Account for 2013/14 Participation in clinical research demonstrates Kent Community Health NHS Trust commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Our clinical staff stay abreast of the latest possible treatment possibilities and active participation in research leads to successful patient outcomes. During 2013/14 Kent Community Health NHS Trust has participated in 45 research studies, 19 of these are classified by the National Institute of Health Research as portfolio studies. Portfolio studies are high quality clinical research studies that are eligible for support from the National Institute of Health Research Clinical Research Network in England. Statement Kent Community Health NHS Trust has become involved in 7 new portfolio research projects during 2013/14. Total patient recruitment for portfolio studies for participation in research approved by a research ethics committee for this period is 149. Statement The portfolio studies cited above the number of patients receiving NHS services provided or sub-contracted by Kent Community Health NHS Trust in 2013/14 that were recruited during that period to participate in research approved by a research ethics committee was 52. The improvement in patient health outcomes demonstrates that a commitment to clinical research leads to better treatments for patients. There was 36 clinical staff at Kent Community Health NHS Trust participating in research approved by a Research Ethics Committee during 2013/14. In the last three years, no publications have resulted from our involvement in NIHR research. However, KCHT has a commitment to transparency and a desire to improve patient outcomes and experience across the NHS and we will be encouraging our researchers to publish relevant findings in the future. Page 115 of 153 In 2013/14 links have been strengthened between Research and Clinical Audit in order to contribute to increased clinical effectiveness within KCHT. Goals for 2014/15: For 2014/15 we have increased the resources for research within KCHT including the recent recruitment of an experienced Senior Research Nurse who will help to deliver on our research priorities action plan which is focussed on the following 3 areas: Review of existing arrangements to embed robust research structures within KCHT. Establishment/re-establishment of links within and without KCHT to ensure stakeholder engagement. Raising the profile of research and ensuring lessons learnt approach to research findings. Our engagement with clinical research demonstrates Kent Community Health NHS Trusts commitment to testing and offering the latest medical treatments and techniques. Page 116 of 153 Goal 4: Promoting a culture of accountability and openness Serious Incidents The Trust remains committed to reducing the levels of preventable harms and developing the Trust as a learning organisation where staff feel empowered to openly discuss incidents and learn lessons. The Trust has focused on strengthening these values and being explicit about the behaviours required to embed this into the Trusts culture. In 2013/14 the Trust had total of 79 serious incidents compared to the 82 reported in the previous year. The largest proportion relate to pressure ulcers. The Trust has maintained 100% compliance with the national targets for the completion of SI investigations. The Trust has had no never events. Root Cause Analysis (RCA) KCHT embedded the Being Open policy and the principles of transparency and candour into the Serious Incident investigation process. Every Serious Incident is investigated using RCA process to ascertain the possible reasons leading to a Serious Incident. Patients and their relatives/carers are advised of the incident and involved in the investigation and clarification is attained on the level of involvement and feedback the patient and their relatives/carers wish to have. This year the drive has been to increase staff participation in the investigation process and learning for students and staff within all disciplines. Heads of Service are expected to complete 72 hour Report to encourage immediate action and learning in response to the incident. The highest prevalence of Serious Incidents are: Pressure ulcers 57% Information Governance (IG) 14% Falls 11% The classification of an Information Governance Incident has been expanded and it was expected this would increase the overall number of Information Governance Serious Incidents. Compared to 2012/13 there were five fewer pressure ulcer Serious Incidents reported in 2013/14. Lessons Learnt The serious incident team have developed a plan of action to ensure the organisation learns lessons from all incidents/near misses/complaints and claims to improve patient experience and patient/staff safety for future. Page 117 of 153 The emphasis for every incident is to establish what has happened and not who is to blame. At times, the investigation may uncover actions from an individual which require further action and investigation to establish more details. This is always carried out in collaboration with the operational teams and the employee relations team. The lessons learnt newsletter is published quarterly and weekly information and learning is shared through the communication bulletin. Below are some of the recommendations and actions that have arisen from the investigations: Pressure Ulcer Serious Incidents Handover processes must be robust Staff should put equipment provision/delays on the incident reporting Staff should refer to specialists for expert help All wounds to be photographed at the time of discovery Falls Holistic assessments and reassessments must be completed relating to patients at risk of falls and when patients are re-referred or if the patient’s condition changes. All equipment should be checked on every shift to make sure it is working correctly. Consent must be gained from patients for the use of sensor mats. Information Governance Person identifiable information should not be kept at a non-KCHT site. Staff must always follow the safe haven fax procedure The pre-programmed fax number facility must be used to store the fax number for frequently used numbers. Staff must ensure they only transport the minimum amount of information needed to complete the visit and ensure that it is transported and stored in accordance with the Records Management Policy. Goals for 2014/2015: No never events. Embedding learning from incidents. Twenty per cent reduction in reported SIs Incidents due to an intended reduction in pressure ulcers. Serious Incidents as a rate per occupied bed days/contacts will be reported quarterly to the Quality Committee and Trust Board to allow benchmarking with other similar providers. The Serious Incidents Team will engage with staff at focus groups to identify innovative methods of sharing lessons learned. The Being Open Policy will be audited. Page 118 of 153 Goal 4: Promoting a culture of accountability and openness Understanding Claims During the year 2013/14 the Trust had seven clinical claims. In one case we have admitted the care given was not of an acceptable standard. To ensure consistently high standards of care, the clinical service held a ‘back to basics’ training day and shared the lessons learnt throughout the Trust. Five clinical claims are still being investigated. We also had four non-clinical claims made against us in this period. One claim was repudiated and the other three are still being investigated. Inquests: ‘Rule 43’ reports have been replaced with ‘Reports on Action to Prevent Future Deaths’ (PFDs). PFDs place the Coroner under a statutory duty to issue a report to any person or organisation where, in the opinion of the Coroner, action should be taken to prevent future deaths. These reports can be issued before or during the inquest. It is important that the Trust fully and swiftly investigates the circumstances of any deaths, identifies any action that can be undertaken to reduce future deaths and puts in place a plan to carry out the actions. The Trust has received one such report in 2013/14. The report related to communication between healthcare providers and the holistic training of district nurses. The Coroner’s specific concerns were: The out of hours GP service (OOH GPs) had difficulties in contacting the district nursing service and the Coroner considered that improved methods of both oral and written communication between OOH GPs and the district nurses must be put in place. The training of district nurses must now include that a patient should be examined if symptoms of bleeding have been reported. In our response, we explained that subsequent to the incident the relevant Head of Service had provided to the OOH GPs full 24 hour contact details for her team. These details were published by the OOH GPs on their intranet and were circulated to relevant staff. A KCHT representative also attends the OOH GPs clinical governance meetings. Clinical Education and Standards Team (CEST) has begun rolling out a programme of training in holistic care and all community nurses will undergo this training. In addition, the Trust has introduced new patient documentation which will support this process (The Health and Social Care Record: Bi-Overview Booklet). This documentation Page 119 of 153 has been developed in partnership with Kent County Council and has been designed to allow our clinicians to document a full assessment of the clinical needs of each patient. All staff who is expected to use Bi-Overview has received appropriate training on the documentation. Goals for 2014/2015: More involvement in training of staff, including clinical record keeping, statement writing and court skills in order to assist staff generally. To reduce the number of coroners cases implicating KCHT. Page 120 of 153 Goal 4: Promoting a culture of accountability and openness Care Quality Commission Statement KCHT is required to maintain registration with CQC and has 34 locations registered. We continue to be registered with the Care Quality Commission without conditions. A condition of registration can be imposed upon a provider where there is evidence that they are not compliant, to limit or restrict what they can do. The CQC has not taken any enforcement action against us in 2013/14 We have not participated in any special reviews or investigations by the CQC during this reporting period. The Trust has a robust assurance process that requires services and subject matter experts (in areas such as safeguarding, medicines, consent, learning and development and equality and diversity) to self-assess compliance against the CQC’s 16 Quality and Safety Outcomes. Improvements September to December 2013 During this quarter work began within the Standards Assurance Team to consider the recent, significant changes to the CQC’s inspection model. The key lines of enquiry used during inspections of acute Trusts have been reviewed (a community trust model has not yet been published) and an organisational level selfassessment undertaken so that indications of gaps could be identified. The Trust’s mock CQC inspection tools have been re-designed and are now based on the CQC’s new five domains – Caring, Effective, Responsive, Well-led and Safe. Training and awareness material is being developed to raise awareness amongst staff. The Trust will be inspected by the CQC during 2014. Page 121 of 153 CQC inspections The CQC inspected two of our services this year and the results are shown below: Outcome Outcome 1 Respecting and involving people who use services Outcome 4 Care and welfare of people who use services Outcome 7 Safeguarding Edenbridge Hospital 22.04.13 Hawkhurst Hospital 07.06.13 Compliant Compliant Compliant Compliant Outcome 13 Staffing Outcome 14: Supporting workers Outcome 16: Assessing and monitoring the quality of services Outcome 21: Records Compliant Compliant Compliant Compliant Compliant The CQC’s Quality and Risk Profile (QRP) for the Trust is updated by the CQC nine times each year. Each new version is reviewed to ensure any areas of concern have been addressed. The data available to the CQC to populate the QRP has increased since last year. The majority of items on the QRP are either positive (70 items) or neutral (144 items). These data items relate to areas such as positive comments from CQC reviews and inspections, Information Governance Toolkit results, Food Standards Agency ratings, positive staff survey results, our responses to safety alerts from the Medicines and Healthcare products Regulatory Agency (MHRA), and positive comments left by patients on NHS Choices. There are currently 39 negative data items within the QRP. The main themes of these negative items are: 13 relate to issues identified during CQC review/inspection, 13 relate to negative comments left on NHS Choices or the CQC's web form and 6 relate to Staff Survey results and actions have been taken to address these negative items. Goals for 2014/15: The Trust will be inspected by CQC in June 2014 and aims to achieve “good” to “outstanding” rating. Page 122 of 153 SUMMARY Goal 4: Promoting a culture of accountability and openness The overall summary for this goal shows good progress with many targets achieved. We have had no never events however the number of serious incidents has not sufficiently reduced which is a concern for the trust. Ensuring lessons learnt are being embedded into practice is a priority for the Trust to minimise the risk to patients and avoidable harm. The trust received one “Report on Action to Prevent Future Deaths’ issued by the coroner which is unacceptable and work will continue to ensure these lessons are embedded to protect patients. All goals for 2014/15 are set to ensure improvements will be made. Page 123 of 153 Goal 5: Improving delivery capacity and capability in all areas Clinical Education and Standards Clinical Education and Standards The delivery of consistently high quality care requires an educated, skilled, competent workforce to evidence based practice standards. The trust is committed to the development of the workforce and has developed strong partnerships with Higher Education Institution (HEI) providers and clinical experts to develop a robust education and workforce development programme. Competency Framework - The Clinical Education and Standards Team (CEST) has been developing the Clinical Competency Framework with Clinical Operations. The aim of the framework is to reflect the professional standards, clinical competencies and the practice outcomes expected of staff members from bands 2-7. Each role profile makes explicit to staff their personal responsibilities in patient care. The core domain includes holistic assessment, care planning/goal setting, record keeping and safeguarding. For staff in band 6 and 7 roles the profiles include clinical leadership and management competencies to ensure that quality of services are monitored and measured locally by the teams. The role profile details the competency requirements, development opportunities and the assessment process to meet the standards required for high quality care. The framework will be supported by a robust education and training programme which will include: The framework will provide the structure to support staff to prepare the necessary evidence required for Revalidation that is to be introduced to non-medical professionals starting with nursing in 2015. It will provide assurance to the organisation that staff have clarity of role, competencies and behaviours. The framework has been aligned to the Values into Action framework and will detail the behaviours that will be required to each domain. The framework has also been mapped to CQC, Nursing & Midwifery Council (NMC) and National Occupational Standards. Clinical Induction Programme – in 2014 the trust will introduce the programme which will establish the competency framework with staff on commencing with the trust. It will focus on the standards, competencies and practice outcomes for the high risk areas such as: Holistic Assessment and Person Centred Care Planning/Goal Setting. Pressure Ulcer prevention and management; and general wound management and 1 st Choice Dressings. Diabetes management. Falls prevention. Page 124 of 153 Preceptorship Programme – Newly qualified staff need a period of support and supervision through the transition period. The trust has a programme in place which provides staff with education and training but more importantly dedicated Action Learning sets which enable them to have time for reflection, sharing experiences and learning and networking. Health Care Support Worker Programme (HCSW) – the Trust has a long standing history of delivering HCSW programmes in nursing and Allied Healthcare Professionals (AHPs). In 2013 the Francis Report recommended that a review be undertaken of HCSW education and the Cavendish Review followed. The Trust programmes have been reviewed against the Cavendish Report (2013) and the regional Health Care Support Worker Career Progression Strategy. The Trust has developed a Health Care Support Worker strategy and career progression framework for implementation in 2014. The revised programme has strengthened the education and competencies relating to the high risk areas of practice. Quality Improvement Development Programme In 2013 the first cohort of nursing delegates commenced a Quality Improvement Development Programme and completed Quality Improvement Projects. The aim of the programme is to provide mentoring to staff in clinical leadership roles to lead and manage change and make improvements within their area of practice. Validation In August 2012 it was agreed that all learning opportunities in KCHT should be standardised to ensure the provision and expectation of 1st Class clinical education every time to ensure: Lessons learnt from incidents and complaints are incorporated in to training programmes. Focus is placed on competency assessment in practice. Clarity on the patient outcomes measures that the training will impact upon That training is fit for purpose. Standardisation in relation to templates. Application of appropriate teaching methods. There has been an increased focus on the quality assurance of education and training and on improving the quality and delivery of training sessions. The next phase of this quality assurance process will focus on the impact the training has on clinical practices. The quality assurance model will link in with the clinical competencies to help drive standards up even further. An evaluation of the outcomes will be provided on a quarterly basis through 2014/15. Page 125 of 153 CEST has also developed an assurance visit tool to ensure that students, preceptees and other learners have the support and the environment that promotes learning. Mentorship – the NMC mandate that registrants who supervise teach and assess students undertake an annual Mentor update. During this year the non-compliance has been rectified with compliance over 85%. Across KCHT allied health professionals have a high level of compliance. In recognition of NMC best practice AHPs have agreed to work to the same standard and work is underway to incorporate roles equivalent to Mentors onto the register. The NMC completed a quality placement assessment in January for Canterbury Christ Church University and February for University of Greenwich and no immediate concerns were identified. Clinical Supervision – Clinical supervision is a relationship based clinical education that brings practitioners and skilled trained supervisors and/or peers together to reflect on practice. Supervision aims to identify solutions to problems, improve practice and increase understanding of professional issues. Across the organisation the level of access to Clinical Supervision has been variable and sometimes undervalued by staff. Work has been undertaken to review the policy, the models in place across the Trust and develop a revised framework for staff. Post Graduate Certificate in Community Health in partnership with the University of Kent– The development of this model focused on high priority areas of clinical practice, designed in response to gaps in clinical education and assurance related to competent practice which correlates directly to patient outcomes. The Trust will be able to deliver essential education flexibly and at a standard equal to Higher Education Institutes. The delivered programme is focused on work based learning and the application of Trust values and objectives. Rewards staff with academic credits without additional attendance at educational institutions. It will also support the desire to increase innovation and research activity. Goals for 2014/2015: Ninety-five per cent of all clinical staff to have individual competency role profiles with relevant assessment tools. NMC Mentors to maintain compliance at 85%. Development of career pathways for unregistered workforce through the strategy. 75% of newly appointed unregistered clinical support workers will be on a career development pathway by March 2015. Increase of 25 Non-Medical Prescribers within Long Term Conditions by March 2015. Implementing Post Graduate Certificate in Community Health Care in partnership with University of Kent by September 2014. Page 126 of 153 Goal 5 - Improving delivery capacity and capability in all areas Workforce KCHT strives to be a high performing sustainable organisation, delivering safe quality services to our patients. Our staff are the critical factor in achieving this. We therefore need our staff to perform at the highest level possible at all times. Trust wide appraisal compliance was 82% which fell below our target of 95%. Work continues to improve this compliance figure. Appraisals are key to ensuring staff understand their role and objectives for the forthcoming year with support identified to help them achieve these. This year the Trust has linked performance to pay for Bands 7 and above with a view to rolling this out to all staff by April 2015. Staff are rated against their compliance with mandatory training, performance against objectives, the achievement of their personal development plan and an assessment of behaviours against our Values. The focus of this framework is to create a high performing organisation with equal opportunity for all staff to reach the higher performance categories. Training Is a key priority for the organisation and fundamental to high quality care. Our mandatory training compliance figure is 85% and some areas have seen a considerable improvement on attaining this target compared to 2012/13. 12/13 Year End 13/14 Year End Training - Mandatory - Induction 99.00% 100.00% Training - Mandatory - Information Governance 88.00% 87.00% Training - Mandatory - Fire - Community Hosp. 77.00% 75.00% Training - Mandatory - Fire - Non Community Hosp. 91.00% 88.00% Training - Mandatory - Moving and Handling: Client 78.00% 79.00% Training - Mandatory - Moving and Handling: Object 90.00% 94.00% Training - Mandatory - Health & Safety 95.00% 97.00% Training - Mandatory - Equality & Diversity 86.00% 91.00% Training - Mandatory - Safeguarding Adults Basic 94.00% 97.00% Mandatory Training: MCA Basic Awareness 99.00% 100.00% Page 127 of 153 Services below 85% and are being targeted to discuss the reasons as to why compliance is not being achieved and identifying alternative ways of providing training updates. Our aim is to be compliant in all areas of mandatory training by June 2015. Recruitment and Retention A key focus has been to increase our permanent workforce and reduce the amount of temporary staff. An action plan is in place to ensure values are aligned to those of KCHT. The Trust is recruiting staff quicker having reduced our average recruitment timescales from 10.5 weeks (November 2013) to 7.6 weeks (March 2014). Retention of staff continues to be a challenge and preceptorship programme and close working relationships with local Universities will enable us to recruit and support newly qualified clinicians. New staff are surveyed after their first six weeks in post. This data will help us review our induction period. Our workforce of the future needs to be responsive and flexible to rapid and constant change. We are introducing a model for potential recruits to rate themselves against our Values prior to application. We are currently exploring the option of overseas recruitment and Return to Practice to support those areas with the most difficulties in recruiting staff. Leadership Good leadership is key for our staff and many of our existing managers have already taken part in extensive management development programmes. KCHT wants to assess the current capability and future potential of leaders and managers and to use this information to understand how they can improve their Management capability to inform succession planning activities. A framework for managers (The KCHT Manager) has been developed in which the Trust Values are described in terms of outstanding leadership and management behaviours. All managers will go through a diagnostic against this framework using a questionnaire aligned to these behaviours which will inform targeted development. Staff Survey A full census for the 2013 staff survey was undertaken which meant that 5054 staff were issued with a self-completion questionnaire. The 2013 staff survey demonstrated that 73% of staff feel satisfied with the quality of work and patient care they are able to deliver which is 2% lower than the national 2013 average for community trusts. Within that score are the following results: Page 128 of 153 Seventy-one per cent feel they are able to do their job to a standard they are personally pleased with; Eighty-two per cent are satisfied with the quality of care they give to patients/service users; Sixty-four per cent feel they are able to deliver the care they aspire to. Each of these scores is below the 2013 benchmark and was targeted for action in Operational Directorate action plans following the 2012 survey. Eighty-nine per cent (89%) of staff agree that their role makes a difference to patients and 69% feel they are able to contribute to improvements at work. There are clear areas that require improvement and the Organisation Development Business Partners (ODBP’s) are working with their directorates to develop action plans to address any issues raised. The aim of the actions is to create an environment where staff: Feel that high quality is recognised. Understand the context in which they work including commissioning expectations. Are engaged by their line managers in shaping the services and solutions to address the challenges they face. Recognise their personal responsibilities and are held to account by the whole team. Help staff recognise the impact their role has on patients. Help staff understand the environment in which they deliver care, the scope of the service they are commissioned to deliver, and provide positive recognition for teams and individuals delivering an excellent service. Create a culture where incidents reported match the results of the staff survey so that incidents can be investigated and dealt with at the time they occur. Create an environment where staff and managers understand their responsibilities under the Attendance Management Policy, and managers are confident in supporting absence and managing performance. There are varieties of actions to be taken, some of which are: Implementation of ‘Talking Points’ to improve trust, openness and accountability within teams. Local staff engagement sessions (targeting hard to reach staff) run by ADs and CSDs to cover: o Service achievements o Commissioning intentions and challenges o Requesting feedback and ideas from staff Page 129 of 153 What are they doing to address the challenges eg recruitment, service changes? Develop an understanding in clinicians of their leadership and management responsibilities through the implementation of a first line management programme. Continue the emphasis on high quality appraisals through the audit of Band 7. Recognise high quality work through awards, articles in magazines, weekly bulletins and positive media stories. Improving Morale Our staff engagement score in the 2013 staff survey has increased slightly to 3.69, although it remains below the national average score of 3.71. Sickness absence (including stress) rate has reduced although along with our level of turnover and retention of staff remain key concerns and an element of our workforce strategy. The Trust’s Staff Engagement Strategy has a number of strands: A very visible “we are listening” campaign to continue to listen and make changes in response to staff feedback. We need to continue to find ways to celebrate success and recognise staff achievements. Support for managers to engage well with their teams and support them through organisational change this includes the KCHT Manager diagnostic described above and further management development training including training for managers in having difficult conversations, resolving disagreements and holding others to account. Engagement has improved with managers and operational managers have been going back to the front-line and experiencing the challenges faced by staff. Staff Friends and Family Survey has been rolled out across the Trust. The survey will be carried out quarterly and along with other measures such as turnover rates, will provide a useful measure of how staff view our service and the Trust as a place for treatment and to work. Equality Delivery System We have significantly increased the visibility of Staff Networks and introduced a new Staff Disability Network. Communication between the Networks and senior management teams has improved with an identified member of the Executive team at each network. All networks work much closer together to share common themes and ideas and have developed simplified ways to allow for quicker responses to feedback and requests. The Disability Network has developed a Health and Well Being passport for staff to help the conversations with managers on reasonable adjustments. Page 130 of 153 Our website aims to improve our image towards diversity and we are discussing recruitment strategies with our Networks to support on-going improvements to our recruitment processes. This year we have simplified our Equality analysis with workshops to help our staff understand the value of understanding the equality impact of the work they do. Goals for 2014/2015: We need to recruit more staff, develop staff, retain skilled staff and keep those in employment at work by: Linking performance to pay for the rest of our organisation by April 2015. Improving our staff survey results through the implementation of our Staff engagement strategy using the results of our Friends and Family test for staff. Continue to focus on reducing our vacancy rate through a planned approach to recruitment and retention. Reducing sickness absence with a focus on short term absence. Page 131 of 153 Goal 5: Improving delivery capacity and capability in all areas Transformation The Transformation Team is driving forward service improvement and partnership work to support the Trust in securing quality, clinical and financial sustainability. This work forms the Trust’s Transformation Framework, known as ‘The Human Touch’ which is a framework to transform: Models and pathways of care, so that care is integrated around the patient. The times and places where we deliver care, so that it is 24/7, close as possible to home and make best use of technology. Our people, so that we have a culture of continual service improvement. Our clinical systems, so that we use technology to support services to be safer and more efficient. Our partnerships, so that we tackle the challenges and opportunities facing health and social care together, making the best use of all our resources. Highlights of this work in 2013/14 include: Developing the intermediate care model which supports people to avoid admission to an acute hospital by providing urgent support either at home or in a community inpatient unit. It also supports early discharge from an acute hospital for rehabilitation, at home or for a short rehabilitative stay in a community Hospital. In 2013/14 a new model of more intensive support in the community was developed including: Expanding the therapy services to a 24/7 model. Reducing length of stay to 18 days. Enhancing the health and well-being support and social activities available. Increasing the use of advanced nursing skills such as IV therapy closer to home. Implementing the productive community services programme across 220 teams. Implementing the e rostering system to ensure safe levels of staffing. Transforming our partnerships: Integration Pioneer The Kent Health and Social Care Integration Programme was recognised as one of fourteen Integration Pioneers by the Department of Health in 2013. With the Trust’s partners at Kent County Council and Kent and Medway Partnership Trust, the Adult Operations Directorate, corporate teams and transformation team has continued to drive forward the main mechanisms for integration: Page 132 of 153 Risk stratification to identify high risk patients. Integrated teams across all CCG localities. Multi-disciplinary teams (MDTs) meetings, led by either the GP or Community Matron and involving all partners take place regularly. Health and social care co-ordinators support the co-ordination of Local referral units are being established to provide a single, co-ordinated point of access. Throughout the year the Trust has shared its integration work with other organisations around the UK, and presented at major national conferences. Goals for 2014/2015: Transforming our models of care: Support services to undertake service redesign to increase quality, patient experience and productivity, including Musco Skeletal services, intensive intermediate care, long-term conditions, and self-management services. Transforming the times and places where we give care: Supporting the development of a service led strategy through mapping opportunities for services to work collaboratively in community based buildings. Transforming our people: Develop and implement transformation skills package to improve skills of staff in undertaking service redesign and project management. Transforming our clinical support systems: Complete implementation of e-rostering by March 2015. Page 133 of 153 SUMMARY Goal 5: Improving delivery capacity and capability in all areas Progress has been made with the development of a Trust wide clinical competency framework. However, overall performance against this goal has not progressed as well as we would have wanted. Compliance with mandatory training in two areas was not achieved. Recruitment and retention continues to be an area of concern, along with staff morale and these issues will be a key priority for 2014/15 to ensure that this goal is met. Page 134 of 153 SUMMARY OF RESPONSES From: Alison Smith [mailto:Alison.Smith@eastsussex.gov.uk] Sent: 15 May 2014 17:06 To: Clive Tracey Cc: Thomas Jo (NHS HASTINGS AND ROTHER CCG) Subject: Feedback on th Quality Account Hi Clive, Thank you for sharing this with me and I have now had a chance to review the document and consider the content. I am responding on behalf of the 3 East Sussex CCGs and the Local Authority as the joint commissioner and the lead for your contract for the provision of the childrens integrated therapy services (2013) and paediatric equipment (since 1 April2014) The document talks about the quality goals and I am pleased that in this section the Trust wishes to build on partnerships with commissioners and GPs and that you will aim to deliver integrated care pathways working with partners. The 6 priorities for improvement are areas that commissioners would want to see included and see services deliver. It would have been nice to see some reference to children and CITs here and include the importance of delivering services closer to home/school etc. I would have also liked to see some reference in the document to the geographical spread of you services and how you acknowledge some difference between areas by working in slightly different ways to reflect this. In the section on Quality Aspirations and Goals 2014/15, would it be possible to include CITs here e.g around patient experience and engagement with parent /carer forums. A piece on CITS in the Children and young people section pages 86-88 would have been helpful too especially as you did so well on achieving the waiting list challenge! I hope these comments are helpful Best wishes alison Alison Smith Strategic Lead for health for Children and Maternity-East Sussex 01273 335109 mobile-07801 838590 E1C, County Hall,St Anne's Crescent, Lewes,East Sussex BN7 1UE Page 135 of 153 Healthwatch Kent response to the Quality Account for Kent Community Health Trust As the independent champion for the views of patients and social care users in Kent we have read the Quality Accounts with great interest. Our role is to help patients and the public to get the best out of their local health and social care services and the Quality Account report is a key tool for enabling the public to understand how their services are being improved. With this in mind, we enlisted members of the public and Healthwatch staff and volunteers to read, digest and comment on your Quality Account to ensure we have a full and balanced commentary which represents the view of the public. On reading the Accounts, our initial feedback is that the accounts are very lengthy and not written in plain English making this hard for the general public to read, understand and digest. This is not a problem unique to the Community Health Trust as we have seen similar issues with all the Quality Accounts from Kent providers. For future reports we would like to work with you, and other providers, to ensure the reports are accessible and understandable for a wider audience. For this year, a list of acronyms would help. The report references on a number of occasions, engagement with the public and patients and it clearly demonstrates that the Trust is very patient focused. We have also found this to be the case in our dealing with the Trust over the past year. We would like to hear more detail about how you are reaching seldom heard communities and we would be happy to help you to develop ideas for the year ahead as this is such a vital part of your work. The report clearly states the achievements made and the areas for improvement. Healthwatch Kent has signed a Memorandum of Understanding with Kent Community Health Trust and we have found them to be extremely welcoming and supportive of the work that Healthwatch does. The Trust is always looking for new ways to engage with and listen to the public. In summary, we would like to see more detail about how you involve patients and the public from all seldom heard communities in decisions about the provision, development and quality of the services you provide. We hope to continue and develop our relationship with the Trust to ensure we can help you with this. Healthwatch Kent May 2014 Page 136 of 153 Page 137 of 153 Page 138 of 153 Page 139 of 153 Page 140 of 153 Page 141 of 153 PROGRESS ON FRANCIS APPENDIX A Theme Progress Creating the Right Culture Plan for Future Schwartz rounds have commenced – these sessions are led by the Director of Nursing and Quality. Staff are asked to focus on how they felt during an event (rather than focussing on what happened) and are an evidence based method of supporting staff to examine and reflect about an experience. Staff engagement metrics have been identified which give the leaders within the organisation a ‘barometer’ of how the staff feel. This is used as one measurement in an Early Warning Trigger Tool which guides the Board to where there may be risks to quality and safety and act to remedy a situation as it emerges rather than wait for an incident to occur. The Executive Team has embarked on several approaches to staff engagement throughout the year – the Director of Nursing and Quality met with staff across all localities to present the findings of the Francis report to them, outline the KCHT strategy to embed the learning and give them an opportunity to ask questions and raise concerns. The Medical Director has introduced monthly Clinical Governance Review meetings. This is a forum for clinical staff to share complex case studies with their peers and challenge each other in a safe environment. Clinical audit results are presented at this forum to increase learning and encourage peer review. Page 142 of 153 A ‘You Said We Did’ section will be developed on Staff zone to give staff a response to suggestions they make to the Executive Team. The Executive Team are hosting a series of road shows across the Region to give staff an opportunity to ask questions and give suggestions. The Nursing and Quality team are planning an update on the Trusts response to Francis and presenting this at team meetings to ensure that staff feel involved in the action plan and can feel part of it. Theme Progress Putting the Patient first Plan for Future The Named Nurse System is in use at every community hospital to ensure patients and relatives have a named professional to discuss their care with. The NHS Constitution has been widely publicised and referred to across KCHT. Every member of staff received a letter from the Director of Human Resources highlighting their responsibilities. KCHT has embraced and embedded the 6 Cs – Care, Compassion, Communication, Courage, Competence and Commitment – which was introduced by the Chief Nursing Officer for England. This was celebrated at the Nursing and Quality Conference which the CNO attended as the guest of honour. KCHT has publicised the #hellomynameis campaign to all staff and tested staff response and patient response through feedback questionnaires. Both staff and patients have responded positively to this Patient stories have been widely used for all staff groups to ensure all staff have a patient focus no matter what their role or function is. The range of clinical education has increased to allow staff to develop their skill set and deliver high quality patient care. A set of core competencies have been identified for each role within the organisation. This will ensure that the patient receives care from competent staff. The Trust is compliant with the National Quality Board staffing guidance Page 143 of 153 A Named Professional system is to be implemented in the community setting – in some cases this may be the GP or Social Worker The Trust will work towards every person with a long-term condition being offered a personalised care plan – to be agreed with their lead clinician – by April 2015 National guidance is expected to be introduced to reduce malnutrition in older people. The Trust will adopt this. The Trust will continue to develop a multi-disciplinary, multiorganisational diabetes pathway to improve patient experience The Trust will further develop the dementia friendly care environment The Trust will await the NICE guidance on safe staffing levels and implement this where applicable. Theme Progress Fundamental Standards of Behaviour Accountability of Directors Performance Management and Oversight Plan for Future All contractors providing outsourced services have had contracts and codes of behaviour reviewed to ensure that patient safety and quality is included to embed KCHT values and expectations. The Marsden Manual of clinical procedures has been made available to all staff to ensure evidenced based, up-to-date procedures and guidance is used for patient care. The clinical audit programme has examined adherence to quality standards and clinical procedures e.g. Intra-venous drug administration. A portfolio of practice standards is under development and will be added to as new standards are developed The KCHT Board complies with the NHS Healthy Board guidance The Trust has committed to Staff Engagement The Trust has appointed shadow Governors from both public and staff groups. The Board are committed to the CQC’s Fundamental Standards The Trust has continued to embrace the Foundation Trust process Job Descriptions have been reviewed and altered to ensure line management structures show accountability The National Quality Board has introduced Quality Surveillance Groups which are attended by commissioners, regulatory bodies and NHS England to hold providers to account All staff are subject to competency assessments Performance related Pay Progression for Band 7 and above has been introduced from 1 April 2014 Page 144 of 153 When policies/ procedures are reviewed in KCHT, guidance or advice from professional bodies e.g. NMC, GMC will be included where appropriate. Healthcare assistants (HCA) to develop a code of conduct Continue to adhere to the Fit and Proper Persons guidance for application of Board members and Executives. The Performance related Pay Progression for all staff grades will commence in April 2015 Theme Progress Patient, Public and Local Scrutiny Effective Handling Complaints Openness, Transparency and Candour Plan for Future The Trust has embraced patient involvement at committee level e.g. Medicines Management The Patient engagement group is a successful long standing group The Trust use Internal audit to provide objective scrutiny A gap analysis of the Clwyd Hart recommendations was undertaken and actions taken to reach compliance The Chief Executive has sight of all complaints The Customer Care Strategy was refreshed this year. There is clinical involvement in complaints whenever possible The Being Open policy has been refreshed to take into account new National recommendations All staff are asked about Being Open when reporting any incident The Being Open audit shows 100% compliance with Being Open in the Serious Incident process Lessons to be Learned are included on the public website The Trust has introduced a confidential telephone line for staff who wish to whistle blow – ‘Seen Something Say Something’ Page 145 of 153 The Director of Nursing and Quality has commissioned internal audit to complete an audit of the Francis action plan A patient representative is being recruited for the Quality Committee The Trust will increase the involvement from Staff and Public Governor’s throughout 2014/15. A sample of patients will be asked for feedback about how their complaint was handled to scrutinise satisfaction with the service after completion. The Duty of Candour responsibilities will continue to be reviewed as National guidance is published. Theme Progress Nursing Leadership Plan for Future There has been collaboration with a local university to deliver post graduate education within KCHT Health Care Assistants are given the opportunity to gain an NVQ certificate. Staff have an opportunity for Health Visiting qualification Band 6 Clinical sisters in Community Hospitals are supernumery An Enhanced Rapid Response service provides staff with an opportunity to extend their clinical skills KCHT has developed a Manager programme of education. The first cohort of managers have positively evaluated the programme The Trust has commissioned a bespoke toolkit for managers to build trust within their teams. This is called Talking points The NHS Leadership Academy courses are promoted to relevant staff The Trust has continued to use the influencer strategy to embrace change. Page 146 of 153 The Trust are collaborating to give staff an opportunity to gain a Diploma in Community Nursing The Trust will continue to promote the National and local leadership opportunities and support staff into leadership positions through effective appraisal. Theme Progress Caring for Older People Plan for Future A Care of the Dying pathway and End of Life strategy have been agreed A Nurse Consultant specialising in Dementia has led a steering group to improve the experience of patients with dementia in the Trust. The Medical Director is chairing a whole systems diabetes strategy group to develop a multi-organisational diabetes pathway The Trust has won an award for the Community Geriatrician programme which is part of the programme of work to improve the specialist care for older people. The success of the falls reduction strategy has continued throughout the year Page 147 of 153 The Deputy Director of Nursing is collaborating with a local university to develop a specialist course in caring for the older person APPENDIX B CQUIN DASHBOARD Page 148 of 153 Appendix C AUDIT EXAMPLES FOR OTHER SECTIONS OF THE QUALITY ACCOUNTS Examples of audits that map to the Quality Account Reports sections are included below: Pressure Ulcers The Management of Pressure Ulcers Audit Audit Purpose/ Background Outcomes/ Findings This audit was undertaken to gain assurance that best practice guidance relating to pressure ulcers and Band 7 responsibilities is being followed and evidenced through documentation. Furthermore to identify where current practice in assessment, care planning, delivery and recording can improve and provide assurance to Board and external stakeholders. The aim of the audit was to reduce avoidable patient harm through prevention, early assessment and risk reduction. 81% of the reported pressure ulcers were unavoidable 100% of Pressure ulcer risk assessments were completed. 90% Holistic assessment of the patient was completed on initial visit 95% MUST nutritional screening undertaken at initial visit. Malnutrition Universal Screening Tool (MUST) 85% of patients/carers were given documented evidence of pressure ulcer information highlighting the risks and benefits 66% of patients had been holistically reassessed/reviewed 4 weekly or more frequently if their condition had changed or deteriorated. 71% of equipment was regularly monitored for its effectiveness, in line with the care plan ensuring it continues to reduce risk of pressure damage and meet the patient’s needs 90% of patients had an individualised comprehensive wound care plan which had been agreed with the patient. Updated Framework document now includes a section for signoff by Head of Service review, when appropriate Audit findings shared with Heads of Service for discussion with Team Leaders and staff including the need to document care and action taken Rapid cycle audit undertaken to evidence where improvements have been made. Page 149 of 153 Pressure Ulcers Re-Audit CG29: NICE guidance on pressure ulcer management Audit Purpose / Background Findings/Outcomes A recommendation from the pressure ulcer validation audit reported in June 2012 was to repeat a pressure ulcer validation based on the audit methodology, to review the implementation of the changes recommended and provide assurance. Assurance was provided with regard to the decisions the Team Leaders were making/reporting. The validation audit agreed with 100% of the decisions ‘that the pressure ulcers were unavoidable.’ Following the Pressure Ulcer Audit reported December 2012, one of the objectives was to undertake a rapid cycle audit of records of patients at risk of developing pressure ulcers, reviewing standards not fully met in this original audit The conclusions that 78% were unavoidable, due to ‘all preventative measures being in place’ and 21% were unavoidable, due to ‘the patient having capacity but was non concordant.’ This is an improvement to the results found in the previous validation audit reported September 2012 where 77% of the pressure ulcer decisions were validated as accurate compared to the re-audit where there was 100%. A handbook of Top Tips in Prevention and Management of Pressure Ulcers for all clinical staff has been developed to further aid understanding. Falls Audit and Falls CQUIN audit CG21: NICE Clinical Guidance on Falls (CG21) (replaced by CG161) Audit Purpose / Background Findings/Outcomes KCHT seeks to identify those adults at risk of falling and at time of audit were using Falls Screening Tool 1 as part of the admissions procedure. If the screening tool indicates an increased risk of falls then advice or referral to an appropriate service for further assessment can be given. Assessments should identify the risk factors for falls and osteoporosis and offer appropriate interventions to reduce the risk of falling. The audit was undertaken to ensure that all patients of 65 or older are appropriately screened and treated or referred on as appropriate. Falls CQUIN audit- P/049/13 the CQUIN compliance was met as shown: o 99% of patients aged 65 and over were assessed for the risk of falling at first assessment – Standard 95% o 97% of those at risk of falling were referred for further assessment or support or had a full falls care plan in place – Standard 90% Availability of the falls prevention leaflets has been increased The falls screening tool 1 questions are now included in the Functional Analysis of the Care Environment (FACE) documentation. Page 150 of 153 Nutrition and Hydration Puree Diets in Community Hospitals P/077/12 Audit Purpose/ Background Outcomes/ Findings The Dysphagia Diet in Community Hospital audit was undertaken to gain assurance that texture modified diets for dysphagia patients were prepared to the standards described in the dysphagia diet food texture descriptors developed by the National Patient Safety Agency. The aim was to reduce the risk of harm through aspiration by ensuring that texture modified diets provided to patients: Are the correct consistency. Decrease the number of patients inappropriately started on texture modified diets. Identify the best model of food provision. 162 patients were audited, with 14% found to be on a modified diet or enteral feed. All those started on this diet due to swallowing difficulties had been assessed by the Speech and Language Therapist. There was a lack of up to date training in dysphagia; a training package is now under development by Speech and Language Therapy 25 thick pureed meals across nine hospitals were audited against the Dysphagia Diet Food Texture Descriptors. Four meals failed the standards. Hotel services are to introduce regular spot check monitoring of pureed and soft meals. 100% of meals should meet the standards listed Little detail was recorded on the meal systems in use at the different sites. Insufficient information was provided on fork mashable meals, further audit is recommended. Outcome was the introduction of new equipment for producing puree diets. This has standardised pureed meal preparation. Page 151 of 153 Hydration in Community Hospitals Audit Purpose/ Background Outcomes/ Findings The Hydration in Community Hospitals audit was undertaken to ensure that best practice in hydration for community hospital patients was being followed. The audit aimed to: Ensure adequate fluids are being provided Ensure care plans and systems are in place for those at risk Ensure accurate documentation of hydration needs The number of hot drinks offered daily varies representing a historical difference in catering systems and guidance between east and west Kent. The policy is being revised to ensure standardisation with the recommendation for at least eight hot drink rounds of 200ml to be offered daily and water jugs to be changed at least twice daily. The assessment and documentation of hydration needs was hugely variable between the different wards and there was no standard format to this assessment. Standard assessment for hydration risk has been developed and implemented on community hospital wards Nutrition and hydration practice to be monitored on ward monthly and reported to the Community Nutrition Steering Group Health Visiting and Safeguarding Antenatal / Postnatal Communication and Risk Assessment Audit –I/001/11 Audit Purpose / Background Findings/Outcomes This audit was commissioned from a serious case review learning implementation and monitoring group. The purpose of the audit was to ensure that the Antenatal / Postnatal Communication and Risk Assessment guidance implemented in January 2011 was being followed by Midwives, Health Visitors and GPs in East Kent. This was an interface audit between East Kent Hospitals and Kent Community Health NHS Trust as there was insufficient capacity (within PCT) for GP’s to take part in the audit. This audit provided clear evidence that Midwives are using the communication tool (Concern and Vulnerability form) effectively and copies are being sent in accordance with the Protocol. Midwives now have the up to date contact address for each of the six Health Visiting Districts A notification form had not been completed by the Health Visitor and sent to the GP in 23 cases. The form has been re-launched to Health Visitors in all six districts Daily allocation of new births has been introduced to increase the number of visits being undertaken within 14 days of the birth Page 152 of 153 End of Life Care QS13: NICE Quality Standard on end of life care for adults Audit Purpose / Background Findings/Outcomes This audit was undertaken: To ensure that all palliative care patients who are at the end of life and their families or carers, have their care, treatment and support needs met by being given a high standard of appropriate care. To ensure that end of life care follows nationally recognised standards of best practice and to verify that patients died in their preferred place of care where possible. To provide evidence for the end of life quality goal for the Quality Accounts. 24% of patients are not included on a GP palliative care register. Potential risk has been communicated to Clinical Commissioning Group’s. The majority of patients (89%) were involved in deciding their end of life care plan. The audit demonstrates that in a minority of cases improvements could be made in assessing a patient’s capacity to understand explanations and communicating with the patients regarding their end of life care. A patient carer survey will be developed to ensure involvement in discussions. 98% of patients (who were able to understand) were fully aware of their diagnosis and that they were believed to be in the dying phase. In the community hospitals 29% of carers were given verbal and written information on the support available to them and in the community 12% were given verbal and written information. Appropriate information leaflets for patients/relatives have been developed. OTHER CLINICAL AUDIT EXAMPLES Medical Devices Survey Survey Purpose / Background Findings/Outcomes The Medical Devices Survey was undertaken to ensure compliance with Medicines and Healthcare Products Regulatory Agency (MHRA) guidelines and to provide assurance against Care Quality Commission’s Registration Standard, Outcome 11, safety, availability and suitability of equipment. This is the second consecutive year that the survey has been undertaken Trust wide to ensure that the Medical Devices policy is understood and followed by all staff where appropriate. The purpose of the survey was to assess and minimise the risk for both staff and patients who use and prescribe medical devices. 68% of staff correctly identified the symbol that is used to identify a medical device can only be used once. 88% of staff got the definition of a single use device correct Training was provided in 67% of cases if staff prescribe medical devices, while it was provided in 76% of cases if staff use medical devices The Single Use Poster will be distributed to all Services. The Medical Devices Manager will deliver the Single Use presentation at directorate meetings The process for reporting a fault and or repair will be clearly written in the Medical Devices Policy. Page 153 of 153