In this section Welcome to gether NHS Foundation Trust’s Quality
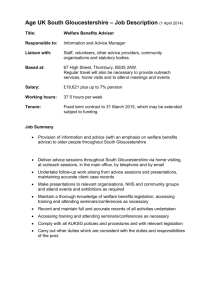
advertisement

Welcome to 2gether NHS Foundation Trust’s Quality Report for 2012/13. The purpose of a Quality Report is to ensure Trust Boards focus on quality improvement as a core function of the organisation. In this section 3 Statement on Quality from the Chief Executive 5 Looking ahead to 2013/14 9 Statements relating to the Quality of the NHS services provided 17 Looking Back: A review of Quality in 2012/13 39 Statements from our Partners on the Quality Report 45 Statement of Directors’ Responsibilities in respect of the Quality Report 49 Independent Auditor’s Report to the Council of Governors on the Quality Report Part 1. Statement on Quality from the Chief Executive Introduction Quality Initiatives 2012/13 Quality Initiatives 2013/14 3 3 3 Part 2a. Looking ahead to 2013/14 Priorities for Improvement 2013/14 5 Part 2b. Statements relating to the Quality of NHS Services Provided Review of Services Participation in Clinical Audits and National Confidential Enquiries Participation in Clinical Research Use of the CQUIN payment framework Statements from the Care Quality Commission Quality of Data 9 10 11 12 15 16 Part 3. Looking Back: A Review of Quality in 2011/12 Priorities for Improvement 2012/13 Domain 1: Preventing people from dying prematurely Domain 2: Enhancing quality of life for people with long-term conditions Domain 3: Helping people to recover from episodes of ill health or following injury Domain 4: Ensuring people have a positive experience of care Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm Summary Report on Quality Measures for 2012/13 Monitor Indicators and Thresholds for 2012/13 Quality Indicators for 2012/13 Community Survey 2012 Staff Survey 2012 PEAT Assessment Results 2011/12 17 18 18 20 22 27 31 33 33 36 37 38 Annex 1. Statements from our Partners on the Quality Account Gloucestershire Health, Community and Care Overview and Scrutiny Committee Herefordshire Health, Community and Care Overview and Scrutiny Committee Gloucestershire Local Involvement Network Healthwatch Herefordshire Gloucestershire Clinical Comissioning Group Herefordshire Clinical Comissioning Group The Royal College of Psychiatrists 39 39 40 41 42 43 43 Annex 2. Statement of Directors’ Responsibilities in respect of the Quality Report 45 Annex 3. Glossary 46 Annex 4. How to contact us 2 Other Comments, Concerns, Complaints and Compliments Alternative Formats 48 48 Independent Auditor’s Report to the Council of Governors on the Quality Report 49 Part 1. Statement on Quality from the Chief Executive Against a backdrop initially of uncertainty and subsequently of knowledge that we would cease being the preferred provider, our practitioners maintained high standards of provision throughout the year delivering some of the best outcomes across the South West of England. From December onwards practitioners worked extremely hard to continue to deliver services and ensure a safe transfer of care to the new provider. This was achieved and we ceased service provision from the end of March 2013. Quality Initiatives 2013/14 Introduction Once again on behalf of the Board and all colleagues within 2gether NHS Foundation Trust it is my pleasure to present our annual Quality Report. As always, this report is a combination of the collective efforts of many clinical and managerial colleagues across the Trust. Our Quality Report last year identified 24 goals and 34 targets across the five domains of quality as detailed in the 2012/13 NHS Operating Framework and NHS Outcomes Framework. Following feedback from service users, carers, our commissioners and LINks, we have streamlined our objectives for 2013/14 into 11 goals and 12 targets. In part 2 of this report you will find those detailed goals and targets - these are the further improvements we have planned for 2013/14. In part 3 you will read how we did against the plans we set out to achieve in our Quality Report last year. Quality Initiatives 2012/13 Whilst 2012/13 has been a challenging year, our frontline staff backed by our support services have once again continued to deliver improvements in the quality of services we provide. Significant progress was made on the 24 goals and 34 targets we set ourselves, with 24 targets achieved. Progress on the ten targets which were not fully achieved is detailed within the report. We have been privileged to have had the opportunity to provide the full range of a prison Healthcare service into HMP Gloucester. Our team of dedicated and skilled practitioners were acknowledged during a Care Quality Commission (CQC) visit to the prison for their excellent work. HMP Gloucester was one of the seven prisons chosen for closure under the reconfiguration plans by the Ministry of Justice and the service provision ceased at the end of the 2012/13 financial year. In June 2012, Gloucestershire Substance Misuse Services were tendered by commissioners. We were unsuccessful at tender and service contracts were awarded to Turning Point. This theme of continuous improvements will continue into 2013/14 and is supported by further investment in our inpatient units and our community bases. It will also be evident in the ongoing professional development and increased number of permanent staff working within our working age adult inpatient services. As we commence 2013/14, our focus is clear: to work ever closer with service users, carers, commissioners and staff to understand the quality indicators that matter most to them. As a provider organisation we only exist to serve service users and carers. They are experts by experience and throughout the year, much of our learning and subsequent improvements have come from their involvement in service planning and evaluation. We are indebted to their continued support. "Health outcomes matter to patients and the public. Measuring and publishing information on health outcomes are important for encouraging improvements in quality". During 2013/14 we will implement ways to help make sure that our adult service users have the opportunity to describe the impact of the interventions they received by completing nationally recognised outcome measures. This will help us to continually understand, from their perspective, the usefulness of the interventions provided and enable us to make any necessary adjustments. It is essential that when individual’s access services that they are as safe as possible. We will build upon the learning from our involvement in the South of England Improving Safety in Mental Health Programme to implement change using reliable improvement technologies. The Francis Report and the failings at Winterbourne View have raised question of confidence in the overall care and support system. Every health and social care practitioner, every manager and every Board member must think carefully about the recommendations that have emerged from the lessons from both of these reports to ensure that they have confidence in the local services they provide and access. 3 Our clinical leadership is leading our organisational self-reflection and action planning to ensure that we can give everyone confidence, that locally, we have a culture that is conducive to ensure the quality of care we provide and that if concerns arise, that there are effective methods of raising these and that they are acted upon. Our clinicians are highly qualified and experienced. They are trained to critically appraise and utilise emerging evidence on effectiveness, to adopt and adapt best practice and to personalise what they do for the unique circumstances of the individual they are supporting with care and compassion. These attributes will be pivotal in embracing the changes ahead of us effectively. Following the introduction of a Carers Charter in 2011, this year service users and clinicians collaborated together to develop our Service User Charter. The charter was launched on World Mental Health Day in October and together with our Carers Charter is a statement of the positive intent to place service users and carers at the centre of everything we do, on every occasion. Overall, the primary goal to which we aspire is to ensure that individuals in our care are safe, obtain the best possible outcomes and when in receipt of services have the experience that we would all wish for a member of our family. As we have stated in previous years our name is a statement of intent; to work together with others. Throughout the year we have benefited from feedback, collaborative discussions, suggestions and challenges from our partners in commissioning, LiNks and shadow Healthwatch as well as other provider organisation colleagues. We are proud to be a part of the NHS. We are also proud that as a Public Interest Corporation we are a membership organisation. Our 7,000 members elect a Council of Governors who play a vital role in ensuring our accountability and connectivity to our local communities in which we serve. We are indebted to our Governors who have given freely of their time energy and skills to assure themselves on behalf of our communities that the quality of services provided is of an appropriate standard. In the coming year, the Trust Board will continue to focus our energy and expertise on ensuring that we consistently deliver and improve the services we provide. This is what our service users and carers deserve; this is what we will work with them and our commissioners to achieve. Shaun Clee Chief Executive 2 gether NHS Foundation Trust 4 Part 2a. Looking ahead to 2013/14 This section of the report looks ahead to our priorities for quality improvement in 2013/14. We have developed our quality priorities for improvement against the five quality areas described in the NHS Outcomes Framework 2013/14. These areas sit under the three key dimensions of effectiveness; user experience and safety and have been approved by the Trust Board following discussions with our key stakeholders. We are aiming to improve outcomes for service users through these actions being mindful that a key national priority is: “Health outcomes matter to patients and the public. Measuring and publishing information on health outcomes are important for encouraging improvements in quality” NHS Outcomes Framework 2013/14 Following feedback from service users, carers, our commissioners and LINks, we have streamlined our objectives for 2013/14 into 11 goals and 12 targets. Outcomes will be measured and monitored with the period of time varying from monthly, quarterly or annually depending what we are measuring and how often the data is collected. How we prioritised our quality improvement initiatives The quality improvements in each area were chosen by considering the requirements and recommendations from the following sources: Documents/Organisations: • NHS Commissioning Board (Everyone Counts: Planning for Patients 2013/14) • The Francis Inquiry (February 2013) • Care Quality Commission (via the Quality Risk Profile and CQC Compliance Reviews at our sites) • Department of Health, with specific reference to ‘No health, without mental health (2011) • Internal inspections • Monitor • King’s Fund report on Quality Accounts • National Institute for Health & Care Excellence publications including their quality standards We strongly value working in partnership and have had feedback on our services during 2012/13 which has informed our choice of quality improvement initiatives for this coming year. The feedback and contributions have come from: • Gloucestershire Local Involvement Network (LINk) • Herefordshire Local Involvement Network (LINk) • Gloucestershire Health, Community and Care Overview and Scrutiny Committee (HCCOSC) and Council colleagues • Herefordshire Overview and Scrutiny Committee and Council colleagues • NHS Gloucestershire and the shadow Clinical Commissioning Group • NHS Herefordshire and the shadow Clinical Commissioning Group • Internal audits • South West Mental Health Patient Safety Improvement Programme • Trust’s Service Experience Committee (comprising of service users and carers) • Trust’s Governors • Trust clinicians and managers The proposed quality initiatives were then considered and agreed by the Governance Committee, which is a sub-committee of the Board and has clinical and managerial representation from across the Trust and is chaired by a Non-Executive Director. This Committee meets formally monthly to consider information relating to quality across all of the services we provide. The priorities for improvement are applicable for services in both Gloucestershire and Herefordshire unless specified, and where they are different it is a reflection of the different quality priorities in each county. 5 Progress on the implementation of each of the quality improvement areas will continue to be reported to the Trust Board every quarter. This information will also be shared with our major stakeholders. These targets represent a small sample of the large number of quality initiatives which are undertaken, but are areas which will potentially have a significant impact on safety and quality. In terms of wider initiatives, the Trust remains an active participant in the South of England Patient Safety Improvement Programme for mental health providers and has challenging CQUIN targets in both counties. The Trust has also reviewed the recommendations from the Francis Report into the Mid Staffordshire Trust and identified areas where we have good assurance and issues we plan to focus on for further work. A group of senior clinicians has met to draw up a plan of actions and areas of work and these will be communicated to staff in a series of road shows which will also provide an opportunity for staff to give feedback and make their own suggestions. This alongside our service experience work will hopefully make the organisation more aware of what it is like to work in the Trust or to receive services. Domain 1: Preventing people from dying prematurely Ensuring that premature death in people with serious mental illness and learning difficulties is reduced remains a key priority; we will carry out the following activities: Goal Target Drivers Minimise the risk of suicide of people who use our services 1.1 Reduce the numbers of deaths relating to identified risk factors of people in contact with services when compared data from previous years. National strategy of zero tolerance of preventable harm Gloucestershire Suicide Prevention Strategy and Action Plan Herefordshire Public Health Report 6 Ensure we follow people up when they leave our inpatient units within 48 hours to reduce risk of harm. 1.2 95% of adults will be followed up by our services within 48 hours of discharge from psychiatric inpatient care Improve the physical health of patients with mental health problems 1.3 70% of community patients with a serious mental illness will have had an annual physical health check (This is a local target. The national target is that 95% CPA service users receive follow up within 7 days) Local and national priorities Our local target of 95% was not met consistently during 2012-13 People with schizophrenia and bipolar disorder die on average 25 years earlier than the general population largely because of physical health problems. Domain 2: Enhancing quality of life for people with long term conditions We will continue to focus on outcomes that are important to those living with long-term conditions. The way we will carry out this objective will be to focus improvements upon the following: Goal Target Drivers Improve the experience of people with dementia in Gloucestershire and Herefordshire 2.1 Improved access to dementia services for Black & Ethnic minority communities through training an agreed number of staff. 70% of an identified group of registered staff will receive this training. (Gloucestershire). Prime Minister’s Dementia Challenge (2012) - enhancing the quality of life for people with dementia. 2.2 Ensure appropriate and timely reviews of prescribed antipsychotic medication for people with dementia living in a care home through three monthly reviews, providing demonstrable evidence of improvement during Quarter 4. (Herefordshire) People will feedback to us whether the service they have received has improved their quality of life. 2.3 90% of adults in contact with services will describe the impact of interventions on their discharge through the completion of nationally recognised outcome measures Children and Young Peoples Services will use mechanisms to gain feedback on whether the service has improved their quality of life. 2.4 Report on improved outcomes of those who use the service Improve the effectiveness of interventions offered by the Trust Implementation of the new National Children’s Improving Access to Psychological Therapy Local priority for Herefordshire to improve services Domain 3: Helping people to recover from episodes of ill health or following injury Central to the service we provide is achieving the best possible outcomes for people who develop treatable conditions. Specifically, we need to help people recover from illness or injury and prevent conditions from becoming more serious. Actions that will be taken to support this objective include: Goal Target Drivers Ensure appropriate access to psychiatric inpatient care 3.1 95% of people will be seen by the Crisis and Home Treatment Team prior to admission, to ensure appropriate access to inpatients services. Department of Health Outcomes Framework - key measure on appropriate access 7 Domain 4: Ensuring people have a positive experience of care Quality of care includes the quality of caring. This means how personal care is provided; the compassion, dignity and respect with which service users are treated, and the extent to which they are given the level of comfort, information and support they require. The Trust is implementing the 6Cs (National Nursing Strategy 2012) throughout the organisation. In our quarterly reports we will report on our development work in this area as well as focusing upon equality and diversity work and partnership working with voluntary agencies in both counties. Goal Target Improve service user experience 4.1 Undertake local surveys of both community and inpatient services by asking the following questions and improve on our 2012/13 scores. • Did you have enough time to discuss your condition, treatment and care? (72%) • Did you find talking with a member of your care team helpful? (49%) • Did we involve your family and carers as much as you would like? (50%) • Has your mental health care service helped you start achieving your treatment goals? (54%) Improve carer experience 4.2 Ensure that 100% of carers are offered assessments Drivers We have identified these questions as they were areas where we achieved a lower score in the 2012/13 national Community Patient Survey Implementation of Trust’s Carers Charter Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm Protecting service users from further harm whilst they are in our care is a fundamental requirement. We seek to ensure a safe environment for service users, staff and everyone else that comes into contact with us. We will achieve this by the following: Goal Target Drivers Minimise the risk of harm to people who use our services 5.1 To reduce the number of serious incidents as a proportion of patients on the trust’s caseload to an annual average of 0.2 incidents per 1000 caseload. National driver of zero tolerance of preventable harm for people who use NHS services (Patient harm serious incidents are reported nationally e.g. pressure ulcers, severe selfharm incidents ) NHS Safety Programme Ensure the safety of patients detained under the Mental Health Act 8 5.2 Reduce the number of patients who are absent without leave from inpatient units who are formally detained by 50%. Baseline to be established and confirmed in Quarter 1 2013 NHS Safety Programme Part 2b. Statements relating to the Quality of NHS Services Provided The following section includes responses to a nationally defined set of statements which are common across all Quality Reports. The statements provide assurance that we are providing services according to national standards, measuring and monitoring the quality of care we provide and are participating in and learning from national projects. Review of Services The purpose of this section of the report is to ensure we have considered the quality of care across all our services which we undertake through comprehensive reports on all services to the Governance Committee (a sub-committee of the Board). During 2012/2013, the 2gether NHS Foundation Trust provided and/or sub-contracted the following NHS services: Gloucestershire Our services are delivered through multidisciplinary and specialist teams. They are: • One stop teams providing care to adults with mental health problems and those with a learning disability • Primary Mental Health Care services • Specialist services including Early Intervention, Crisis Resolution and Home Treatment, Assertive Outreach, Managing Memory, *Prison healthcare, *Substance Misuse and Children and Young People Services • Inpatient care • Improving Access to Psychological Therapies *Following the closure of HMP Gloucester, the Prison Healthcare service ceased to be a service that we provided from 31 March 2013. Also the Substance Misuse Services were transferred to Turning Point from 1 April 2013 following a tendering process by NHS Gloucestershire. Herefordshire We provide a comprehensive range of integrated mental health and social care services across the county. Our services include: • Children and Adolescent Mental Health care • Specialist services including Early Intervention, Assertive Outreach and Crisis Resolution and Home Treatment and Substance Misuse Services • Inpatient care • Improving Access to Psychological Therapies South Gloucestershire During 2012/13, we provided Improving Access to Psychological Therapies services until October 2012. gether NHS Foundation Trust has reviewed all the data available to them on the quality of care in all of these NHS services through a systematic plan of quality reporting and assurance that is considered by the Trust’s Governance Committee and the Board. 2 The income generated by the NHS services reviewed in 2012/13 represents 94.9% of the total income generated from the provision of NHS services by the 2gether NHS Foundation Trust for 2011/12. Participation in Clinical Audits and National Confidential Enquiries During 2012/13, two national clinical audits and four national confidential enquiries covered NHS services that 2 gether NHS Foundation Trust provides. During that period, 2gether NHS Foundation Trust participated in 50% national clinical audits and 100% confidential enquiries of the national clinical audits and national confidential enquiries which we were eligible to participate in. • providing care to adults with mental health problems in Recovery Teams and Older People’s teams 9 The national clinical audits and national confidential enquiries that 2gether NHS Foundation Trust was eligible and participated in during 2012/13 are as follows: National Clinical Audits Clinical Audits Participated - Yes/No National Audit of Psychological Therapies Yes Prescribing Observatory for Mental Health No Reason for no participation Voluntary involvement. The Trust was not a member in 2012-2013 membership period National Confidential Enquiries National Confidential Enquiries Participated - Yes/No Confidential Enquiry into Maternal and Child Health Yes National Confidential Inquiry into Suicide and Homicide by People with Mental Illness Yes Sudden Unexplained Death of Psychiatric Inpatients Study Yes Confidential Inquiry into the Premature Deaths of People with a Learning Disability Yes Reason for no participation The national clinical audits and national confidential enquiries that 2gether NHS Foundation Trust participated in, and for which data collection was completed during 2012/13 are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Clinical Audits No of cases requested No of cases submitted All Not known Confidential Enquiry into Maternal and Child Health Not Available Not Available Not Available National Confidential Inquiry into into Suicide and Homicide by People with Mental Illness Not Available Not Available 98.45% Sudden Unexplained Death of Psychiatric Inpatients Study Not Available Not Available 98.31% Confidential Inquiry into the Premature Deaths of People with a Learning Disability Not Available Not Available Not Available National Audit of Psychological Therapies % cases submitted Report not available. Confidential Enquiries The report for the National Audit of Psychological Therapies has not yet been issued and will be available in October 2013. 10 The participation in these national audits and enquiries demonstrates that as an organisation we want to learn and benchmark our care against other providers to the benefit of the people who use our services. As a result of participating in the national audits we are: Participation in Clinical Research • Ensuring an increased focus on the physical health of people diagnosed with schizophrenia • Reviewing how more people can access psychological therapy services through our Improving Access to Psychological Therapy service • Providing maternal mental health services according to agreed countywide pathways of care Throughout the last twelve months, we have continued to support the recruitment of service users and staff into research approved by an NHS research ethics committee. During 2012/13 the Trust took part in the audit of schizophrenia lead nationally by Rethink. The Trust also participated in the first round of the National Audit of Schizophrenia in autumn 2011, the final report of which was published in April 2012. 2gether NHS Foundation Trust is already enlisted to take part in the second round of this audit due to take place during 2013/14. Clinical audits of our services Within our services there is a high level of clinical participation in local clinical audits, demonstrating our commitment to quality across the organisation. All clinically led local audits are reported to the Governance Committee in summary form to ensure that actions are taken forward and learning is shared widely. During 2012/13, 83 local clinical audits were completed within the Trust. During this process we internally identified 581 recommendations to further improve our practice as part of our commitment to continuous improvement. A further 17 audits were commenced during 2012/13 and are due to be completed early in 2013/14. An extract from one of our internal audits regarding compliance with the Falls Care Pathway (written incorporating the NICE guidance CG21) identified the following: All inpatients in older people services and learning disability services over the age of 40 were included in the audit. In total 45 inpatients were identified and of the 16 criteria the following scores were identified: • • • • 6 (38%) scored 95-100% compliance 2 (13%) scored 90-94% compliance 7 (43%) scored 80-89% compliance 1 (6%) scored 70-79% compliance Overall score 91% Compliance The audit showed that the Falls risk assessment is routinely covered on admission or as part of the Trust initial assessment and all those assessed as being at risk are being referred for physiotherapy treatment. The areas which scored lower included: • Osteoporosis risk • Visual impairment • Home hazard assessment From the audit findings, recommendations were made to further improve quality and patient experience within this area. It is important that we report on our participation in research reflecting our commitment to continuously improve the quality of services that we provide. During 2012/13, there were 242 people recruited (data from the Western Comprehensive Local Research Network - WCLRN). The number has decreased from last year (315 recruits) reflecting that there are less recruiting studies on the National Institute for Health Research (NIHR) portfolio, and greater competition. The Trust currently has a total of 62 registered and approved studies in Gloucestershire which includes a mix of clinical and commercial trials, confidential inquiries, service evaluations and student research. Of these studies, 40 were clinical research based in mental health or dementia during 2012/13, with the addition of 22 service evaluation or student research projects initiated and co-ordinated by Trust staff or students. We continue to participate in research that fits with the Trust core values, which means we are focusing closely on research studies that align with our continuing commitment to improving the quality of care we offer and to making our contribution to wider health improvement. Service change within Herefordshire has meant that active research did not take place during 2012-13 but preparations were made to ensure that research activity can begin during 2013-14. Research Sponsors At the close of 2012/13, we have 28 approved NIHR studies recruiting or active in Gloucestershire. Of these, 17 studies are sponsored by Universities, seven sponsors are from the pharmaceutical industry, two are other NHS Trusts and two are charitable organisations such as the Medical Research Council. This highlights the need for NHS organisations, such as ours, to build strong academic links with those Universities who are research active in mental health in order to help build links for site selection. Examples of the breadth of our research portfolio of activity are listed below. Mental Health • ECHO: Expert Carers Helping Others – a randomised controlled trial of a carer intervention for those with an eating disorder • N-Alive Pilot: NALoxone InVEstigation Prison-based Naloxone-on-release pilot randomised controlled prevention trial: to demonstrate feasibility by recruiting first tenth of 56,000 participants needed to quantify reduction in drugs-related deaths soon after release • DPIM Polymorphisms in Mental Illness: investigating genetic factors involved in schizophrenia, bipolar disorder, alcoholism and autism and exploring possible treatment options 11 • National Confidential Inquiry into Suicide and Homicide by People with Mental Illness • Confidential Inquiry into premature deaths of people with learning disabilities • REFOCUS randomised controlled trial: Developing a recovery focus in mental health services in England • OASIS: Seroquel XL hospital-event monitoring study • Victims of homicide with mental illness • National study of suicide by prisoners • Liberty, equality, capacity: the impact of the Deprivation of Liberty Dementias and Neurodegenerative Disease • A large randomised assessment of the relative cost effectiveness of classes of drugs for Parkinson’s • Brains for Dementia Research We continue to receive support funding from the WCLRN via the Research and Development Consortium for Gloucestershire to provide a research infrastructure within the Trust. Use of the Commissioning for Quality & Innovation (CQUIN) framework The national contractual use of CQUINs is to support the essential focus upon quality improvement in the provision of services and incentivise this through specific quality payments. A proportion of 2gether NHS Foundation Trust’s income in 2012/13 was conditional on achieving quality improvement and innovation goals agreed between 2gether NHS Foundation Trust and NHS Gloucestershire, NHS Herefordshire and NHS South West Specialised Commissioning Group (for the provision of low secure mental health NHS services). • GERAS: Observational Study of costs and resource use of Alzheimer’s disease in Europe • PD Rehab – Parkinson Disease 2012/13 CQUIN Goals Gloucestershire 12 Goal Name Description Goal weighting Expected value Quality Domain Venous thrombo – embolism (VTE) Reduce avoidable death, disability & chronic ill health from VTE 5.00% £91,100 Safety Patient Experience Improve responsiveness to the personal needs of patients (Patient Experience) 19.00% £346,180 Patient Experience NHS Safety Thermometer Improve data collection on pressure ulcers, falls, urinary tract infection in those with a catheter & VTE 5.00% £91,100 Safety Telehealth and Telecare Promote use of this technology to help people live more independently at home 10.00% £182,220 Effectiveness Maternal Mental Health Provide a pathway and staff training to better help expectant mothers who are experiencing mental ill health 14.00% £255,080 Effectiveness Out of County Placements To ensure systems are in place that will allow people to be treated as close to their support networks as possible 3.00% £54,660 Effectiveness Medicines management Falls Make plans to encourage generic prescribing within Primary care Reduce falls within inpatient settings 22.00% £400,840 Effectiveness 10.00% £182,220 Safety Learning Disability Outcomes Develop a tool that captures how interventions result in improvements for the individual or LD population 12.00% £218,640 Patient Experience Herefordshire Goal Name Description Goal weighting Expected value Quality Domain VTE Risk Assessment (Prevention) To reduce avoidable death, disability and chronic ill health from venous thromboembolism (VTE) 5.00% £17,783 Safety NHS Safety Thermometer Improve data collection onpressure ulcers, falls, urinary tract infection in those with a catheter & VTE 5.00% £17,783 Safety Improve responsiveness to the personal needs of patients Improve responsiveness to the personal needs of patients (Patient Experience) 18.00% £64,019 Patient Experience Making Every Contact Count Making every patient contact count through systematic healthy lifestyle advice delivered through frontline staff 12.00% £42,680 Effectiveness Pain Assessment Implementation of a community and inpatient (Cantilupe) pain assessment tool to improve local assessment 30.00% £106,699 Effectiveness Recovery Star To pilot the implementation of recovery star clients of agreed teams 15.00% £53,349 Effectiveness Prevention of suicide Implementation of the NPSA community patient suicide prevention through toolkits 15.00% £53,349 Safety Goal Name Description Goal weighting Expected value Quality Domain Minimum Take Dashboard Aimed at ensuring that implementation and routine use of the required clinical dashboards 25% £9,801 Efficiency Shared pathway and recovery and outcomes Introduce and implement a recovery and outcomes based approach to the care pathway, demonstrating recovery orientated practice 25% £9,801 Patient Experience Implementing a standard secure pathway Introduce and monitor key milestones on the patient pathway to make it efficient and reduce length of stay 25% £9,801 Efficiency Secure forensic care pathway feasibility project Implement, review and feedback on MHCT clustering, 5 Care pathway indicators, and reporting feasibility within a clear reporting structure 25% £9,801 Innovation Low Secure Services The total combined potential value of the income conditional on reaching the targets within the CQUINs during 2012-13 was £2,301,000 of which £2,290,000 has actually been achieved. This is different to the figure provided in the final account due to due the year end figure being agreed by commissioners at the end of Quarter 4 2012-13. In 2011-12 the total potential value of the income conditional on reaching the targets within the CQUINs was £1,321,000 of which £1,306,500 was achieved. 13 2013/14 CQUIN Goals 2013/14 CQUIN Goals CQUIN goals for 2013/14 have been agreed with Gloucestershire and Herefordshire Clinical Commissioning Groups and the National Commissioning Board (for the provision of low secure mental health NHS services). These include: Digital First Initiatives - an innovation which aims to avoid unnecessary face to face appointments Increased use of Telecare/Telehealth Technologies - using technologies to help people live independently Use of NHS Safety Thermometer - a tool to promote, measure and monitor harm free care Patient experience - improving the experience that service users have from our services Effective Communication between Secondary and Primary Health - improved communication between GPs and specialist services Increased use of Recovery Star - tool for promoting service users recovery CAMHS Outcome measure - understanding what helps children and young people best Increased use of LD Outcomes measure - understanding what helps people with a learning disability best Responsiveness to carers of inpatients - making sure that we are listening to and working with carers Carers for people with dementia - making sure that we are listening to and working with carers VTE Monitoring and assessing - a tool to promote, measure and monitor harm free care Encourage use of generic prescribing in Primary Care - working with GPs to promote good use of medicines Physical health of people with mental health problems - promoting annual physical health checks Increased access for BME to community services - ensuring that equality of access to our services is available to the whole community Payment by Results - promoting efficiency, patient choice and best practice Suicide prevention training - providing staff with skills to help support people experiencing suicidal crisis Regular review of elderly patients being prescribed antipsychotic medication - ensuring appropriate use of medicines Low secure care pathway - ensuring the best outcomes for people in our forensic services Provision of Literacy and Numeracy in Low secure unit - improving reading and simple arithmetic 14 Statements from the Care Quality Commission The Care Quality Commission (CQC) is the independent regulator of health and adult social care services in England. From April 2010, all NHS Trusts have been legally required to register with the CQC. Registration is the licence to operate and to be registered, providers must, by law, demonstrate compliance with the requirements of the CQC (Registration) Regulations 2009. The inspection found that people using this service were treated people with respect, provided with safe care and food and drink to meet their individual needs and safeguarded from harm. Comments from patients to the CQC inspectors included: “I feel involved in my care and know my rights” gether NHS Foundation Trust is registered with the CQC with no conditions. This means that the Trust has continued to demonstrate compliance with the regulations and we are registered to provide the following regulated activities: The inspection found that the recording of care was not compliant with the CQC standards and that this was having a minor impact on patients using the service. • Assessment or medical treatment to persons detained under the Mental Health act 1983 • Diagnostic and screening procedures • Treatment of disease, disorder or injury A series of actions were taken and following a review by the CQC of information provided to them by the Trust, the service was judged in February 2013 as being fully compliant. The locations from which the Trust is registered to provide these regulated activities are confirmed on the CQC website www.cqc.org.uk. Review of Westridge Assessment and Treatment Unit 2 The CQC has not taken enforcement action against gether NHS Foundation Trust during 2012/13; however compliance actions were required following one of their inspections during this time period. 2 The Trust continues to receive monthly Quality Risk Profiles from the CQC. The Quality Risk Profile published on 4 April 2013 declares no risk to compliance with any of the 16 essential standard outcome areas for quality and safety above a ‘High Yellow rating’. This is on a scale that increases risk from Low/High red to Low/High Yellow to Low/High Amber to Low/High Red. Low Green being the lowest risk rating and High Red being the highest risk rating. The CQC has monitored the Trust’s compliance with its standards by undertaking the following inspections of services during 2012/13: Review of HMP Gloucester- Prison Healthcare A CQC Inspection of the healthcare provision within the prison took place on 9-12 July 2012, as part of a wider inspection by HMP Inspectorate of HMP Gloucester. The inspection found that the service was compliant in the areas reviewed which included treating people with respect, the provision of safe care which is co-ordinated, appropriately trained and supervised staff with quality monitoring systems in place. During the inspection prisoners spoken with expressed a high level of satisfaction with the health services offered. One person commented: “They’ve really helped me a lot”. Charlton Lane Centre A CQC inspection of Charlton Lane Centre took place on 22 August 2012 as part of the national themed CQC inspections on dignity and nutrition. Charlton Lane provides inpatient care to people with mental health problems as well as physical health problems. “Staff always maintain my privacy and dignity” An unannounced CQC inspection of this in patient service for people with a learning disability took place on 18 December 2012. The inspection found that people using this service were provided with safe care in appropriate environments, were safeguarded from harm, with appropriate levels of staff on duty and quality monitoring systems in place. Relatives told the inspection team that they were happy with the service provided, the skills of the staff and they felt informed and included in the care of those using the service. Mental Health Act monitoring The CQC undertake regular reviews of the use of the Mental Health Act within Trust services – The Mental Health Act Commissioner has visited all of our inpatient services in Gloucestershire and Herefordshire and has forwarded to the Trust reports detailing their findings. We have investigated the points raised within the reports and responded to the CQC detailing the actions that have been put in place to correct those issues. All visit reports made by the Commissioner and the Trust responses are scrutinised initially by the Director of Service Delivery and then by the Trusts Mental Health Act Scrutiny Committee. Changes in service registration with Care Quality Commission for 2013/14 The CQC have been formally informed of the closure of Her Majesty’s Prison – Gloucester, and that the Substance Misuse Services in Gloucestershire were transferred to Turning Point from 1 April 2013 following a tendering process by NHS Gloucestershire. The Trust’s Certificate of Registration with CQC has been updated in relation to the locations from which services are provided. 15 Quality of Data Statement on relevance of Data Quality and actions to improve Data Quality Good quality data underpins the effective provision of care and treatment and is essential to enabling improvements in care. gether NHS Foundation Trust submitted records during 2012/13 to the Secondary Uses Service for inclusion in the Hospital Episode Statistics which are included in the latest published data. 2 The percentage of records in the published data which included: • the patient’s valid NHS number was: 99.8% for admitted patient care (99.1% national); and 99.9% for outpatient care (99% national) • the patient’s valid General Practitioner Registration Code was:100% for admitted patient care (99.9%); and 99.9% for outpatient care (99.3% national) gether NHS Foundation Trust has taken the following actions to improve data quality building on its existing clinical data quality arrangements: 2 • Putting in place new data quality processes resulting in one report covering all services which is held on a shared system so managers can view information by service, team or clinician • Significant increase in the completeness of data capture over and above what has already been achieved throughout 2012/13 • Setting up a new Clinical Information Reference Committee to support the already established RiO (mental health electronic record) Group to continue the review of data quality Information Governance Toolkit Ensuring that patient data is held securely is essential, as such the Trust complies with the NHS requirements on Information Governance and assesses itself annually against the national standards set out in the Information Governance Toolkit which is available on the Health & Social Care Information Centre website: http://systems.hscic.gov.uk/infogov gether NHS Foundation Trust Information Governance Toolkit Assessment Report overall score for 2011/12 was 83% and was graded green (satisfactory). For the 2012/13 version of the Information Governance Toolkit Foundation Trusts were again required to achieve a minimum of Level 2 for each of the 45 indicators. 2 At time of submission on 31 March 2013, of the 45 key indicators: • 22 were at level 3 • 22 were at level 2 • 1 was deemed not relevant to us This produced an overall score of 83%, which is rated green (satisfactory) The Trust’s efforts will remain focussed on maintaining the current level of compliance during 2013/14 and ensuring that the relevant evidence is up to date and reflective of best practice as currently understood, and that good information governance is promoted and embedded in the Trust through the work of the Information Governance and Health Records Committee, the IG Advisory Committee and Trust managers and staff. Clinical Coding Error Rate gether NHS Foundation Trust was not subject to the Payment by Results clinical coding audit during 2012/2013 by the Audit Commission. 2 16 Part 3. Looking Back: A Review of Quality in 2012/13 A Review of Quality in 2012/13 The 2012/13 quality priorities were agreed in May 2012 and published in the Quality Report, and are accessed through the following link: http://www.nhs.uk/Services/Trusts/Overview/DefaultVie w.aspx?id=2769 The quality priorities were grouped under five broad areas of quality improvements. This section of the report outlines the achievements and progress made in each of the five areas against what we said we would do. It also outlines key service developments which have positively impacted on the care we provide. Significant progress was made on the 24 goals and 34 targets we set ourselves, with 24 targets achieved. The report describes the progress made on the 10 targets that we did not achieve or partially achieved relating to: 1. Smoking cessation referrals in Gloucestershire (1.3) 2. Implementation of an IAPT service for HMP Gloucester (2.5) 3. Ensuring improved access to IAPT in Herefordshire (2.6) 4. At least 95% of adult Care Programme Approach (CPA) service users receiving follow-up contact within 48 hours of discharge from psychiatric inpatient care (3.1) 5. Internal service satisfaction survey results (4.1) 6. Achievement of AIMS accreditation in Herefordshire inpatient services (4.4) 7. Reduction in serious harm from falls by 50% (between 2010-13) 8. Zero unexpected deaths in inpatient units. (5.3) 9. Information being made available from a crisis team to an inpatient unit within 4 hours of admission. (5.4) 10.Service users being discharged with relevant information ( 5.5) Since the start of the Commissioning for Quality and Innovation (CQUIN) scheme commenced, 2gether NHS Foundation Trust has worked proactively with its commissioners to ensure that the targets that were being set had a positive benefit for users of its service. It is important to us that we use this scheme to aid quality improvements and that it fits into our commitment to constantly strive to improve quality overall. In January 2011, NICE (now The National Institute for Health and Care Excellence) released Quality Standard 14 which is focused on service user experience in adult mental health. In this standard they stated that high-quality care should be clinically effective, safe and be provided in a way that ensures the service user has the best possible experience of care from the NHS. “The way the staff are here makes it feel more equal, from the patient point of view. They make you feel equal, they don’t talk down to you”. This quality standard describes markers of high quality, cost-effective care that, when delivered collectively, should contribute to improving the effectiveness, safety and experience of care for service users in the following ways: • enhancing quality of life for people with long-term conditions • ensuring that people have a positive experience of care • treating and caring for people in a safe environment and protecting them from avoidable harm • enhancing quality of life for people with care and support needs • ensuring that people have a positive experience of care and support • safeguarding adults whose circumstances make them vulnerable and protecting them from avoidable harm This standard has had a direct impact on what CQUINs were agreed and how we delivered them. 17 Domain 1: Preventing people from dying prematurely In 2012/13 we committed to continue our quality work in reducing the risk of premature death in people with serious mental illness and learning difficulties. We set ourselves three goals with five associated targets, and achieved four targets within this domain. 1.1 Suicide Prevention We aimed to minimise the risk of suicide amongst those with mental disorders through a systematic implementation of sound risk management principles and set ourselves a specific target. Target Year End Achievement To use the National Patient Safety Agency (NPSA) National Suicide Prevention Toolkit for all inpatient units in Herefordshire and Gloucestershire monthly on a sample of patients records.* It is positive to report that the toolkit audit took place in all teams as per the plan and this enabled staff to ensure all patient risk factors are taken account of and learning within in teams * This target relates to Wotton Lawn Hospital and Stonebow Unit To use the NPSA Community Suicide Prevention Toolkit quarterly to audit Crisis & Recovery Teams in Gloucestershire and Herefordshire suicide prevention work 1.2 Promoting healthier lifestyles We wanted to provide more positive health interventions for our service users relating to smoking and drinking and quality improvements have taken place: Staff in Herefordshire and Gloucestershire have undertaken specific Making Every Contact Count training. 162 staff have been trained at Level 1 and 114 at Level 2 in Herefordshire. This has increased the total number of referrals that have been made to stop smoking services this year to: Improving the health of prisoners has been a key objective through accessible primary and mental health services. This has been measured against 32 national prison indicators and at the end of the year before the prison closed the healthcare service was meeting all the indicators. Comments from individuals under our care to CQC inspectors at HMP Gloucester included: • Gloucestershire: 146 against a target of 170 (Not achieved. This target relates to service users in the community. In 2013/14 emphasis will be placed on smoking cessation as part of the physical health check) • Herefordshire: 71 against a target of 62 "There's no problem with the staff, they are very efficient and sort things out quickly." "They let you speak and I feel like they listen to my opinions." Domain 2: Enhancing quality of life for people with long-term conditions We continue to be aware that people who have a mental illness or a learning disability need support to live with their long-term condition and we wanted to make more quality improvements to our service that would assist in this area. In this domain, we set ourselves four goals with seven associated targets, and achieved five of the targets. 2.1 Improving services for people with dementia (Gloucestershire) We wanted to improve dementia services within Gloucestershire by providing appropriate assessments of need and ensuring that people were able to access the appropriate services for them. Staff in Gloucestershire have undertaken specific Telehealth and Telecare training. This will help them to be aware of the benefits of Telecare and Telehealth services and promote the use of this technology to help people live more independently at home. The technology includes personal alarms and health monitoring devices. • Gloucestershire staff trained: 105 against a target of 83 18 2.2 Improving services for people with dementia (Herefordshire) In Herefordshire, reflecting local priorities, we wanted to ensure that service users with a diagnosis of dementia received a thorough pain assessment on admission to hospital and in community teams. Throughout the year we have developed the tool, trained staff and have now embedded it into practice in such a way that all appropriate people are now assessed in this way on admission. 2.3 Improve services for people with a learning disability in Gloucestershire We were concerned that there has been an absence of a tool that that accurately captures how interventions from the Learning Disability (LD) service result in improvements for the individual or population of people using learning disability services. We therefore have worked collaboratively to develop and implement one during the course of this year. Throughout this year we have worked collaboratively and developed a Health Equality framework outcome tool, trained staff, piloted the tool and it has been launched nationally. The scores from within our Trust are showing positive outcomes across all five health equality 2.5 Improve access to psychological therapy services for the wider populations in Gloucestershire In line with principles outlined in ‘No health, without mental health’ (2011), we wanted to make sure that as many people as possible were able to access and benefit from our Improving Access to Psychological Therapies (IAPT) services in Gloucestershire and Herefordshire. Access and recovery rates have improved throughout the year. We also wanted to establish and implement a children’s Improving Access to Psychological Therapies (IAPT) service in Gloucestershire as part of a national pilot. determinant areas with further analysis made possible by the developing electronic data capture tool. Overall a net positive 24% change in the impact of the evidence based determinants of health inequalities was achieved across the sample. 2.4 Improve access to services for adults in Gloucestershire To ensure ease of access to our services we wanted to establish and implement a Contact Centre and monitor the benefits for service users and those referring to the service. The Gloucestershire Contact Centre commenced in May 2012 providing a referral management function for the North Locality initially. The West Locality commenced using the service on the 16 July 2012 and the South Locality service commenced in September. The Contact Centre is continuing to review how systems can be improved and has recently provided access for GP queries related to medication with access to the on call Consultant rota. The service has been positively received evidenced by increased use of the service by GP colleagues. The Contact Centre is now also receiving referrals for the Crisis Teams between 9am-5pm. Our IAPT trainees have now completed their course at Reading University, and work is taking place to ensure participation and feedback from children on this. The service is currently developing routine outcome monitoring and developing a Cognitive Behaviour Therapy (CBT) pathway. Prior to HMP Gloucester closing on March 31 2013, we had also progressed our plans to implement an IAPT service for prisoners within the prison and the service had commenced. With the closure of the prison the target could not, therefore, be realised. Target Year End Achievement (cumulative) To ensure that people in Gloucestershire have improved access to our Improving Access to Psychological Therapies (IAPT) Service Q1 Referrals - 1148 Q2 Referrals - 2640 Q3 Referrals - 4402 Q4 Referrals - 6415 2.6 Improve access to psychological therapy services for the wider populations in Herefordshire In line with ‘No health, without mental health’ (2011) we wanted to make sure that as many people as possible were able to access and benefit from our IAPT services in Herefordshire. At the end of March 2013 there had been 943 new cases accepted against a target of 950 so the target was narrowly missed, but nevertheless not achieved. There were also 599 successful completions of therapy against a target of 600; likewise, whilst this was a marginal deficit, the overall target was not achieved. Progress against targets for 2013/14 will be reviewed monthly by the Trust’s Delivery Committee to maintain a dedicated focus throughout the year. Target Year End Achievement (cumulative) To ensure that people in Herefordshire have improved access to Herefordshire IAPT Q1 Referrals - 270 Q2 Referrals - 503 Q3 Referrals - 657 Q4 Referrals - 943 19 Domain 3: Helping people to recover from episodes of ill health or following injury We continue to strive to provide a service that is achieving the best possible outcomes for people who develop treatable conditions. Specifically, in 2012/13 we wanted to help people recover from illness or injury and prevent conditions from becoming more serious. In this domain, we set ourselves seven goals with eight associated targets, and achieved seven of the targets. 3.1 In order to try to ensure safety of people discharged from our services, we wanted to follow them up within as short space of time as possible, exceeding the set national timescales Target Year End Achievement At least 95% of adult Care Programme Approach (CPA) receiving follow-up contact within 48 hours of discharge from psychiatric inpatient care. We did not achieve this target during 2012/13 so we will be keeping it as a key target for 2013/14 . In April 2013 we will introduce pre discharge planning forms which will identify who is responsible for completing the 48 hour follow up, and have produced guidance for staff for recording this. This target will be monitored monthly via the Countywide Delivery Committee. Gloucestershire Gloucestershire Target (95%) Year end (89%) 89% Herefordshire Herefordshire Target (95%) Year end (70%) 70% This relates to our stretch target of follow up within 48 hours. We have consistently achieved the national target in ensuring that 95% of people on CPA received follow up within 7 days of discharge. 3.2 To ensure effective and responsive services for people with a first episode of psychosis, we wanted to put mechanisms in place that checked people with a first episode of psychosis were being treated by the appropriate teams Target New psychosis cases will be served by early intervention teams* Target (95%) Year End Achievement Gloucestershire Year end (100%) 100% Herefordshire Year end (100%) 100% * Measure defined by Department of Health national standards 20 4 3.3 To ensure appropriate admission to psychiatric inpatient care, we wanted to put mechanisms in place that checked people were consistently being assessed by our Crisis and Home Resolution Treatment Teams, prior to any potential admission (excludes those with organic illnesses). Target Year End Achievement At least 95% of service users admitted to psychiatric inpatient care who had access to crisis resolution home treatment teams* Gloucestershire Target (95%) Year end (100%) 98.6% Herefordshire Year end (100%) 100% 3.4 Recognising the need to ensure inpatients are transferred from hospital beds swiftly when they are fit to leave hospital; we wanted to measure how long we were taking to discharge patients when they are ready to be discharged. Target Year End Achievement Less than 7.5% of inpatient bed days will be a delayed transfer of care when they are ready to leave hospital.* Gloucestershire (1%) Target <7.5% 1% <7.5% 0% 2.5% 5% 7.5% 10% 0% 2.5% 5% 7.5% 10% 7.5% 10% Herefordshire (0.5%) 0.5% 0% 2.5% 5% 3.5 Develop effective recovery services within Herefordshire The Recovery Star is a recognised client centred tool that is used nationally to assist with the recovery process for individuals. We wanted to start using this measure in Herefordshire, with an added intention to continue to build its use in the future. As the days went by I started doing things like going to The Recovery Star is a recognised client centred tool that is used nationally to assist with the recovery process for individuals. college, attending the gym, cooking, going out for walks, going on day trips and, the best of all, I went on holiday. Our target was for 90% of an agreed sample of service users within Herefordshire to have an assessment completed. At the end of Quarter 4, 100% of the sample size were reported as having had an assessment and re-assessment. 21 3.6 Reduce waiting times for children and young people within Gloucestershire Target Year End Achievement 95% of non-urgent tier 3 cases will be seen within eight weeks (children and young people’s services). Target (95%) Current (97%) 97% 3.7 Reduce waiting times for children and young people within Gloucestershire The specialist service continues to engage with children and young people experiencing greater levels of acutity and we continue to ensure we achieve a rapid response. We have received positive feedback from those who use this service and our partners on this. Target Year End Achievement 95% of children referred for crisis home treatment will receive support within 24 hours Target (95%) Current (97%) 97% 3.8 Improve the experience of expectant mothers in need of mental health support in Gloucestershire, through staff training We recognised the need to develop a maternal mental health pathway in Gloucestershire, and train staff in this area in order to provide a better service to expectant mothers who were in need of mental health support. After developing and implementing an operational policy and pathway, a training programme was developed and will continue to be offered to staff. This year: • Gloucestershire staff trained: 108 against a target of 102 Domain 4: Ensuring people have a positive experience of care Quality of care includes the quality of caring reflecting the introduction of the national Nursing Strategy ‘Compassion in Practice – the 6Cs (December 2012) which the Trust has adopted at Board level and across all professions. For us, we are ensuring our commitment to the 6Cs, through the Trust’s Service User and Carer Charters as well as considering what we learn from the Francis Inquiry. As part of this work, it is essential that we gain feedback from those who use our services and we have increased this focus during 2012/13. In this domain, we set ourselves five goals with seven associated targets, and achieved five of the targets with a partial achievement of a further one. 22 4.1 Gain feedback from service users to determine satisfaction levels with the care they are receiving, in order to change the service where appropriate We realise the absolute importance and validity in gaining feedback from people who use our services. Overall this year we have gained feedback on discharge of 196 patients and 526 community patients. Below are a series of results from questions that have been asked of people who use our services in both Gloucestershire and Herefordshire each quarter, these are set against national targets. We chose these questions, as the national survey of mental health patients in 2011 demonstrated that we were not meeting people’s needs in these areas, and we wanted to know if the actions we had taken had made a difference. We did not meet our own targets in some instances but responses exceeded the national average scores in the majority of questions. Seeking feedback from service users remains a high priority with a further satisfaction survey being a quality target for 2013-14. Whilst the same questions have been used for both Gloucestershire and Herefordshire, there were different targets set in both counties. The questions were as follows: 1. Crisis Care - Do you have the number of someone in mental health service that you can call out of office hours? 2. Care Reviews -Were you given a chance to express your views during your Care Review meeting? 3. Medication Explanation - Was your medication explained to you? 4. Feeling Safe - Did you feel safe in our care? 5. Recommending Services - How likely is it that you would recommend this service to friends and family? Inpatient Results Target Year End Achievement Crisis Care Gloucestershire 51% (reflecting the national average 51%) Gloucestershire Inpatient 88% 88% 51% Herefordshire 70% Herefordshire Inpatient 85% 70% 85% Care Reviews Gloucestershire 70% (reflecting the national average 70%) Gloucestershire Inpatient 91% 91% 70% Herefordshire Inpatient 100% Herefordshire 90% 100% 90% Gloucestershire Inpatient 94% Medication Explanation Gloucestershire & Herefordshire 68% (reflecting the national average) 94% Herefordshire Inpatient 92% 68% 92% Feeling Safe Gloucestershire Inpatient 94% Gloucestershire & Herefordshire 90% (reflecting the national average) 90% 94% Herefordshire Inpatient 100% 100% 23 Target Year End Achievement Recommending Services The target was set to increase scores from Quarter 1 scores Gloucestershire 27% 27% Gloucestershire Inpatient 25% 25% 51% Herefordshire 25% Herefordshire Inpatient 77% 25% 77% Community Results Target Year End Achievement Crisis Care Gloucestershire 51% (reflecting the national average 51%) Gloucestershire Inpatient 79% 79% 51% Herefordshire 70% Herefordshire Inpatient 64% 70% 64% Care Reviews Gloucestershire 70% (reflecting the national average 70%) Gloucestershire Inpatient 93% 93% 70% Herefordshire Inpatient 89% Herefordshire 90% 90% 89% Gloucestershire Inpatient 96% Medication Explanation Gloucestershire & Herefordshire 68% (reflecting the national average) 96% Herefordshire Inpatient 98% 68% 98% Feeling Safe Gloucestershire Inpatient 99% Gloucestershire & Herefordshire 90% (reflecting the national average) 90% 99% Herefordshire Inpatient 96% 96% 24 Target Year End Achievement Recommending Services The target was set to increase scores from Quarter 1 scores Gloucestershire 46% Gloucestershire Inpatient 45% 45% 46% Herefordshire 45% Herefordshire Inpatient 45% 45% It is seen that the key target we did not achieve relates to “recommending services”. We will survey a larger sample of service users during 2013/14 and will use iPads to gather this information in real time, thereby providing early feedback to the teams of how the service is viewed by those who use it. This will provide a powerful message to all staff and help to culturally embed the principles of both the Carer’s Charter and the Service User Charter. “The launch of The Carers Charter is the first step in acknowledging the role of Carers. It establishes important principles for guiding clinicians as they work with family and friends of the patients they are treating”. 4.2 Promote dignity in care To promote the dignity of people who use our services, we wanted to sign up to national care campaigns. After holding a workshop on the Kissing it Better initiative in February 2012, staff who attended made pledges to make small changes to improve services. These are being followed up and mentors have been allocated to help implement the changes. As stated above we have embraced the national Nursing Vision ‘Compassion in Practice – the 6Cs (December 2012) commonly called the 6Cs. These are Care, Compassion, Commitment, Competence, Courage and Communication. This vision has been adopted across all the clinical disciplines of health and social care professionals and also across all corporate functions. “Mental health professionals all have a duty to support people on their recovery journeys and can do so by developing values and attitudes that support personal recovery.” The Trust has developed a pledge site where staff can pledge their commitment to deliver care and interact with other staff in line with the principles outlined in the 6Cs. 45% Staff who pledge are being issued with a 6Cs pledge badge as a visible declaration of their commitment to the 6Cs. 4.3 Ensure compliance with the national NHS “Equality Delivery System” covering all nine protected characteristics gether NHS Foundation Trust believes passionately in the equality of the services that it delivers and, to promote this, has four equality objectives in the business plan and the work on translating these objectives into local actions is overseen by the Trust’s Diversity Steering Group. 2 Objective 1 In addition to a data validation exercise commencing in Herefordshire, the same exercise was carried out and completed for Substance Misuse Services. A review of progress will be undertaken early in next year to ensure further actions are taken forward. Objective 2 Our Five Steps to Wellbeing programme has been delivered to members of the Asian and Bengali communities. Sessions were arranged with partner organisations and delivered through interpreters. The delivery of this programme has enabled some of the participants to access support and interventions offered through Let’s Talk, our Improving Access to Psychological Therapies (IAPT) service, which they historically would not have accessed allowing them to receive the right support at the right time. Objective 3 Service user and carer participants took part in the recruitment and selection process for the Director of Finance, Director of Organisational Development and for two non-executive director roles. Feedback from participants was that they enjoyed the process, felt involved and included and that their views were taken into account. Objective 4 Six managers have been trained to deliver 360 degree appraisal as part of supporting managers undertaking the development programme, and those considering placements on the programme for 2013 – 2014. 25 4.4 Provision of high quality inpatient services To ensure we are providing high quality inpatient services, we participate in the Royal College of Psychiatry accreditation process for inpatient services known as AIMS in both Gloucestershire and Herefordshire. Gloucestershire has now received full AIMS accreditation for all of its inpatient services. Herefordshire did not achieve this target within the year but are well on their way to completing this rigorous, time consuming but worthwhile evaluation. To achieve accreditation additional psychology input will need to be secured, and there is an associated action plan in place to gather the necessary evidence to demonstrate that all criteria are fully met. The target for 2013/14 is to apply for accreditation in three months as along as the psychology appointment is made. 4.5 Improve service user experience Service users are rightly at the centre of everything that we do. One of the ways that we wanted to ensure and support this was to have a Service Users Charter which all Trust employees would sign up to. The Service User Charter was successfully launched on World Mental Health Day 10 October 2012. The Charter was endorsed by the Trust Board on the 24 September 2012. Additional awareness raising leaflets to encourage complaints when people are dissatisfied with or concerned about their care have been developed. The number of clients seen by 2gether services in 2012-13 is reported as 26,168 .Taking the complaint number figure of 147 this represents complaints from less that 0.6% of the population served. This is the same percentage figure of complaints that were reported in last year’s Complaints Annual Report. Whilst more complaints were recorded last year (n=178) the organisation reported more people using services last year also. During 2012-13 five complaints were referred to the Parliamentary Health Services Ombudsman which is one more than in the previous two years. None of the cases referred this year were upheld. Figure 1 - Number of complaints by quarter year over a five year period 200 180 160 “I have received excellent support from my employment specialist where I feel without her, I would be very poorly. Always there for me even though she is extremely busy.” 41 37 100 80 21 60 8 15 13 40 20 0 15 2008/09 20 16 2009/10 2010/11 Work has been carried out to raise awareness of the complaints process through increased publicity in clinical areas, public forums and on the Trust’s website. 39 49 2011/12 39 2012/13 This number does not include numbers of people seen by the Improving Access to Psychological Therapies Service (IAPT) now was it represented in the 2011-12 complaints report. 2 It should be noted that the figures quoted in 2011-12 report were an estimate as the electronic records system (RiO) had not been implemented in Herefordshire services at that time. The Service Experience Team continues to develop systematic ways of recording and reporting learning from complaints and other service experience feedback. The following are examples of the learning from complaints that have occurred during 2012/13. You Said In previous years illustrated in Figure 1 - i.e. before April 2011. 2gether NHS Foundation Trust was not providing services to Herefordshire or HMP Gloucester Prison service. 47 Jan - Mar Oct - Dec Jul - Sep Apr - Jun 1 We committed to develop a Volunteers Pathway during 2012/13 to help service users in their on-going recovery A total of 147 complaints were made to the Trust between April 2012 and the end of March 2013. This represents a 17% fall in number from the previous year (see Figure 1) when service provision was at a comparable rate. 33 26 28 Clinical Treatment Complaints 30 23 4.6 Improve service user experience This strategy has been drafted, consulted upon and it is planned that it will be agreed at by the Board in late Spring of 2013. 26 36 120 The presentation of the Service User Charter has now been integrated into staff induction. All managers and staff have been informed of this and the Service User Charter is displayed in over 49 clinical areas in the Trust. The charter has been translated into five different languages and an easy read version is also available. 39 140 “It is not helpful to change medication without a full explanation to patient and family.” We Did A message has been sent to staff that there is a need to communicate with patients and wherever possible with families when medication change is recommended. You Said • Work with new partner organisations including Healthwatch to respond to, take action to rectify situations where indicated and learn feedback “Sometimes staff interaction with patients and carers is perceived as rude and uncaring.” We Did We have launched our Service User Charter in all clinical teams which sets out the expectations of providing a positive service experience. The Service Experience Team will continue to work towards improving the service it provides by managing performance and capturing organisational learning from complaints. In 2012/13 the emphasis on a holistic approach to service experience will continue to: • Learn from the Francis Report and integrate learning into the Trust’s Complaints Policy and clinical practice • Continue to review the complaints process and procedure and to facilitate improvements in service users’ experience across the organisation in partnership with operational services • Report information about the protected characteristics of people who complain about our services in order to better understand the equality of our approach and to fulfil the Equality Delivery Scheme requirements • Refine the system of capturing how satisfied people who complain are with the response they have received from the Service Experience Team of the Trust • Continue to triangulate complaints with concerns, comments and compliments received to gain rich information about potential areas of risk to address and to document in the quarterly Service Experience Reports • Implement a system for learning from complaints across the organisation Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm Protecting service users from further harm whilst they are in our care is a fundamental requirement. We seek to ensure we assess the safety of those who use our services as well as providing a safe environment for service users, staff and everyone else that comes into contact with us. In this domain, we set ourselves five goals with seven associated targets, and fully achieved three targets, with a partial completion of a further one. 5.1 Minimising the risk of venous thromboembolism (VTE) In order to minimise risk and prevent service users coming to harm within our services we set out to ensure that Venous Thromboembolism (VTE) was assessed as a potential danger, on admission, and was dealt with swiftly and appropriately if found to be a concern. Target Year End Achievement Gloucestershire Gloucestershire Assessment Target (90%) Assessment Current (96%) 90% Treatment Target (90%) 96% Treatment Current (100%) 90% 90% 100% Herefordshire Herefordshire Assessment Target (98%) Assessment Current (100%) 100% 98% Treatment Target (98%) Treatment Current (100%) 90% 98% 90% 100% 27 5.2 Minimise the risk of harm to inpatients Our aim was to reduce serious harm from falls by 50% between 2010-2013. This target has not been achieved. From 2010, we have aimed to reduce serious harm from falls by 50% and within Gloucestershire this has been exceeded with an improvement of 66%. From 2011, the organisation expanded and Herefordshire services joined the Trust. The acquisition of new services means that the overall organisational aim has not yet been fully achieved as the roll out of the programme is at different stages of implementation; however a 33% improvement is reported and we are looking to achieve the overall organisational aim of a 50% reduction by March 2014 To assist with this we will look to test ward floor mapping and magnetic falls risk indicators for the patient status whiteboards at the Stonebow Unit in Hereford, we will measure the days between falls in Herefordshire as we do in Gloucestershire and we will set up learning events between Willow Ward at Charlton Lane Hospital and Cantilupe Ward at Stonebow Unit as the inpatient group is very similar, and shared learning will be sensitive to service user need. Since the end of January 2011, 2gether NHS Foundation Trust has been involved in the NHS South West Quality and Safety Improvement Programme for Mental Health. The Trust is part of a group of seven mental health NHS Trusts in the South West of England who are working together to deliver the Patient Safety Programme. The overall aim of the programme is to reduce avoidable harm to inpatients whilst in our care, by making improvements in the way we work, and thereby improving the patients’ experience of what is provided. One of the work streams is on patient, family, and carer communication, as part of this work we had an initiative to ensure that when people are discharged from our services that they had a clear care plan, an updated risk assessment and management plan, summary of key information and a medication list. 5.3 Minimise the risk of harm to inpatients We wanted this to happen 95% of the time. The numbers of service users discharged with all this information has not yet been audited so we did not achieve the specific target; however we have tested initiatives to provide discharge information as outlined below. Our aim was to have no unexpected deaths in our inpatient units. Wotton Lawn Hospital continues to pilot user friendly information for service users which includes the following: Sadly there was one unexpected inpatient death and therefore this target has not been achieved. The serious incident was fully investigated and reviewed by the Strategic Health Authority and the learning cascaded across our Trust and others in the South West area. To minimise the risk of access to ligatures, Kingsholm and Abbey Wards at Wotton Lawn Hospital completed second phase ligature works programmes during 2012/13, works are underway on Dean Ward and Priory Ward has ligature work scheduled for autumn 2013. It has been confirmed that 2gether will become responsible for the estate in Herefordshire in 2013, and a programme of estates work is underway at the Stonebow Unit. A Ligature Policy was approved during 2012 and requires a detailed annual audit of all acute inpatient units to be undertaken by senior clinicians in conjunction with estates, health and safety colleagues and service users who are experts by experience. The results and recommendations from the annual ligature audit will be monitored via the Governance Committee. 5.4 Minimise the risk of harm to inpatients Our aim was to ensure that where the crisis team are supporting a known service user and an admission to an inpatient unit was needed, in 95% of admissions, information would be passed from the crisis team to the ward within four hours. We had hoped that this information could be captured from the electronic health records system (RiO) at the end of the year to see if there had been an improvement but we did not identify a mechanism to extract this data, therefore the target was not achieved. During 2013/14 our Clinical Systems Team will work closely with clinical colleagues to see if a solution to document this can be realised and subsequently audited. 28 5.5 Implementation of the South West Patient Safety Improvement Programme (Discharge Information) • a paper questionnaire was introduced in October 2012 and given out to service users on discharge. These are returned to the ward and the ward manager collates the information. This stays with each ward for them to learn the feedback and plan the next steps as appropriate. A file is kept including this information • credit card size cards were available to give to patients on discharge for a three month period, with the 48 hour follow up appointment on and the details of the relevant crisis service, according to locality. These are currently out of print but being revised to extend the scope of their use beyond Wotton Lawn Hospital. The revised cards will be reintroduced in 2013/14 • a letter being given to the patient from pharmacy on discharge with their current medication • a copy of information being sent to the GP within 48 hours of discharge From April 2013, iPads will be reintroduced to all wards and these will also be used to capture information the experience of patients during their inpatient stay, the other discharge information will continue to be provided. 5.6 Monitor and report the numbers of serious incidents for the purpose of improving safety of services Serious incidents requiring investigation are incidents which occurred in relation to NHS funded services and care resulting in unexpected or avoidable death, or serious harm to service users, staff, visitors or members of the public. Reducing the numbers of these incidents remains a high priority for the Trust and as such it reports and investigates all incidents which occur, monitors trends and makes recommendations to improve care wherever possible. Numbers of serious incidents reported by the Trust have decreased this year; which is, in part, an indication of the vigilance of our staff in maintaining the safety of service users. Figure 1 below shows the absolute number of serious incidents reported by the Trust over a five year period. Number of serious incidents Serious incident rate per 1000 caseload 70 11 60 50 14 40 4 6 20 7 12 23 15 7 10 0 10 6 30 2008/09 18 13 8 2009/10 2010/11 Q4 Q3 Q2 Q1 20 9 13 15 19 2011/12 0.70 0.60 0.50 0.40 0.30 0.20 0.10 0.00 12 2011/12 2012/13 Figure 1 2012/13 Figure 2 It is possible to attribute the increase in reported serious incidents seen from 2011/12 to the Trust expanding its scope from that time to include the provision of mental health services in Herefordshire and prison healthcare in Gloucestershire. The rate of serious incidents per 1000 service users on the Trust caseload has been calculated as shown in Figure 2 above. The most frequently reported serious incidents are suspected suicide, and attempted suicide, this is seen clearly in Figure 3. It is really positive that the numbers of patients in contact with mental health services who died by suicide decreased from 27 in 2011/12 (including two deaths in custody) to 18 in 2012/13 (including two deaths in custody). Initiatives such as the implementation of both the inpatient and community suicide prevention toolkit continue to improve staff awareness of issues associated with suicide. Serious incidents by type 2012-13 Declassified - 2 ECT incident - 1 Serious assault - 3 Infection control ward closure - 3 Natural cause death - 1 Grade 3 pressure ulcer - 4 Police intervention - 1 Absconding - 1 Arson - 2 Suspected suicide (including deaths in custody) - 18 Falls leading to fracture - 4 Deliberate self harm - 4 Attempted suicide 12 Unexpected death - 2 Accidental death - 2 Figure 3 29 Two independent investigation reports were published during 2012/13. These were commissioned by the Strategic Health Authority (SHA) following homicides committed by service users who were under the care of the trust at the time of the incidents, these are as follows: 1. The Independent Investigation into the Care and Treatment of Mr A (the incident occurred in 2008) 2. The Independent Investigation into the Care and Treatment of Mr C (the incident occurred in 2010) Both reports were critical of aspects of the care provided and elements of the Trust’s internal investigation processes at the time, and made recommendations in key areas as follows: • • • • • • • • • • • Clinical risk assessment and management Care Programme Approach Substance misuse Safeguarding Medication and treatment Carers Communications Serious Incident Procedures Clinical supervision Joint working with the police and Governance and management issues The Trust developed detailed action plans in response to these, and had already made many changes to systems and practice in the years between the tragic events occurring and publication of the reports. The NHS safety thermometer continues to be used every month for all service users in older person and learning disability units. 30 There have been no Department of Health defined Never Events within the Trust during 2012-13. Never Events are serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented. The full list of reportable Never Events can be seen at: www.gov.uk/government/news/never-eventslist-update-for-2012-13 5.7 Promote service user safety We were required to implement the NHS Safety Thermometer (which required the monthly submission of data on pressure ulcers, falls, urinary tract infection in those with a catheter and VTE) and pilot the Mental Health Safety Thermometer (which had different harm indicators including violence and aggression). The NHS safety thermometer continues to be used every month for all service users in older person and learning disability units, which we report to the Department of Health (DH) Information Centre. As a provider of mental health and learning disability services, the data general reflects low incidences of harm with the exception of falls which we are already tackling. We have been involved in the piloting of a mental health safety thermometer. This will be reviewed nationally and a decision made as to whether this will be rolled out. Summary Report on Quality Measures for 2012/2013 The following are the quality measures that have been mentioned previously under the 5 main areas which had specific targets. Domain 1: Preventing people from dying prematurely 2011-2012 Actual 2012-2013 Target 2012-2013 Actual 1 Compliance with suicide prevention toolkit in Gloucestershire 100% 100% 100% 2 Compliance with suicide prevention toolkit in Herefordshire 100% 100% 100% 3 Increase in recorded referrals to GSAS Gloucester 179 >170 146 4 Increase in recorded referrals to GSAS Herefordshire. Staff receiving MECC training - Herefordshire - >62 71 >175 276 Compliance with prison indicators - =32 32 2011-2012 Actual 2012-2013 Target 2012-2013 Actual - >83 105 100% >95% 100% 5 Domain 2: Enhancing quality of life for people with long-term conditions 6 Staff receiving Telecare training – Gloucester 7 Assessment of inpatients for pain and distress in Herefordshire 8 Develop a learning disability outcome tool - - Achieved 9 Establish and implement the Contact Centre - - Achieved 10 Establish a Children’s IAPT in Gloucester - - On target 11 Ensure improved access to IAPT in Herefordshire - >950 943 12 Implement an IAPT service for HMP Gloucester - - Not achieved due to prison closure 2011-2012 Actual 2012-2013 Target 2012-2013 Actual - >95% >95% 89% 70% 127% 114% >95% >95% 100% 100% 99% >95% >95% Q4 98% Q4 100% Q4 98.8% Domain 3: Helping people to recover from episodes of ill health or following injury 13 14 15 Adult CPA receiving follow-up within 48 hours of discharge – stretch target Gloucestershire Herefordshire Serving new psychosis cases by early intervention teams Gloucestershire Herefordshire Access to crisis resolution/home treatment services Gloucestershire Herefordshire (combined year-end) 31 16 Delayed Transfer of Care Gloucestershire Herefordshire (combined) 17 Recovery Star - Herefordshire 18 4.2% ≤ 7.5% ≤ 7.5% ≤ 7.5% 1% 0.5% 0.9% - >90% 100% Non-urgent tier 3 cases will be seen within eight weeks (children and young people’s services) 95% 97% 19 Children referred for crisis home treatment will receive support within 24 hours 95% 97% 20 Staff receiving MMH training - Gloucestershire >102 108 2011-2012 Actual 2012-2013 Target 2012-2013 Actual - ≤ Q1 Score ≤ Q1 Score ≤ Q1 Score ≤ Q1 Score Partially achieved Partially achieved Achieved Partially achieved - - Achieved - - Achieved Achieve AIMS accreditation – all older peoples inpatient services Gloucestershire - - Achieved Achieve AIMS accreditation – all inpatient services Herefordshire - - Not achieved Finalise and implement the Service Users Charter - - Achieved Develop a Volunteers Pathway - - On target Domain 4: Ensuring people have a positive experience of care 21 Internal service level results from surveys Gloucestershire Inpatient Gloucestershire Community Herefordshire Inpatient Herefordshire Community 22 Sign up to National Care Campaign 23 Ensure compliance with the national NHS “Equality Delivery System” 24 25 26 27 Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm 28 32 2011-2012 Actual 2012-2013 Target 2012-2013 Actual VTE screening for all adult admissions Gloucestershire Herefordshire 100% 90% 98% 96% 100% VTE prophylaxis for adult admissions at risk Gloucestershire Herefordshire 100% 90% 98% 100% 100% <50% <50% 33% 29 Reduce serious harm from falls by 50% (between 2010-13) 30 Zero unexpected deaths in inpatient units 0 0 1 31 Information available from a crisis team to an inpatient unit within four hours - 95% Not measured 32 Service users discharged with relevant information - 95% Pilot developed Partially achieved 33 Develop and monitor a serious incidents rate - - Achieved 34 Implement the NHS Safety Thermometer - - Achieved Monitor Indicators and Thresholds for 2012/2013 The following table shows the 10 metrics that are monitored during 2011/12. These are the indicators and thresholds from Monitor and follow the standard Department of Health national definitions. Please note that some are also the Trust Quality targets as shown in the previous table, though some may have more stretching targets than Monitor require as a threshold. 2010-2011 Actual 2011-2012 Actual National Threshold 2012-2013 Actual 1 Clostridium Difficile objective 0 0 0 1 2 MRSA bacteraemia objective 0 0 0 0 3 Seven day CPA follow-up after discharge 100% 100% 95% 98.6% 4 CPA formal review within 12 months 100% 96.6% 95% 95.1% 5 Delayed transfer of care 5.9% 4.2% ≤7.5% 0.9% 6 Access to Crisis resolution/home treatment services 97% 99% 90% 98.8% 7 Serving new psychosis cases by early intervention teams 130% G127% H114% 95% 100% 8 MHMDS data completeness: identifiers 99% 99.5% 99% 99.7% 9 MHMDS data completeness: CPA outcomes 50%+ 86.9% 50% 79.7% 10 Learning Disability – six criteria 6 at level 4 6 6 at level 4 6 Quality Indicators 2012 -2013 There are a number of mandated Quality Indicators which organisations providing mental health services are required to report on, and these are detailed below. The comparisons with the national average and both the lowest and highest performing trusts are benchmarked against other mental health service providers. 1. Percentage of patients on CPA who were followed up within seven days after discharge from psychiatric inpatient care gether NHS Foundation Trust considers that this data is as described for the following reasons: 2 that service users are more vulnerable and at higher risk during this time • In recognition of this awareness there is a local stretch target of follow up within 48 hours of discharge from inpatient care gether NHS Foundation Trust has taken the following action to improve this percentage, and so the quality of its services by: 2 • Keeping its local stretch target of follow up within 48 hours as a key quality target for 2013-14 • The Trust performs well against this indicator as staff work hard to provide timely follow up as they are aware Quarter 1 2012-13 Quarter 2 2012-13 Quarter 3 2012-13 Quarter 4 2012-13 100% 100% 99.6% 99.1% National Average 97.5% 97.3% 97.6% 97.3% Lowest Trust 94.9% 89.9% 92.5% 93.6% Highest Trust 100% 100% 100% 100% 2 gether NHS Foundation Trust 33 2. Proportion of admissions to psychiatric inpatient care that were gate kept by Crisis Teams gether NHS Foundation Trust considers that this data is as described for the following reasons: 2 • Whilst the Trust performs well against this indicator, we are a small organisation with a small number of beds; staff respond to individual service user need and help to support them at home wherever possible unless admission is clearly indicated • During 2012, crisis teams also gate kept admissions to older people’s services beds within Gloucestershire gether NHS Foundation Trust has taken the following action to improve this percentage, and so the quality of its services, by: 2 • Ensuring that all teams are aware that they must involve crisis teams at the point of admission even when a service user is transferred from other mental health or general hospitals • Ensuring that the all admitting consultants are aware that they have to admit via the crisis teams to beds within older people’s service beds • On some occasions individuals have been admitted directly from other hospital beds if they have been returned from out of county Quarter 1 2012-13 Quarter 2 2012-13 Quarter 3 2012-13 Quarter 4 2012-13 97.9% 99.4% 97.7% 98.8% 97.8% 98% 98.4% 98.6% Lowest Trust 83% 84.4% 90.7% 20% Highest Trust 100% 100% 100% 100% 2 gether NHS Foundation Trust National Average 3. The percentage of staff employed by, or under contract to, the trust during the reporting period who would recommend the trust as a provider of care to their family or friends gether NHS Foundation Trust considers that this data is as described for the following reasons: 2 • The Trust has been through a significant period of change in the preceding 12 months, services have been reconfigured, and staff are working in new ways • The new ways of working continue to be embedded and staff may not, as yet, have seen the benefits for service users, however the feedback directly from service users and carers suggests that the benefits are being felt gether NHS Foundation Trust has taken the following action to improve this score, and so the quality of its services, by: 2 • Holding focus groups with staff to understand their concerns and agree actions which staff members, their managers, and senior managers within the Trust can take to make a positive difference • Sharing positive feedback from service users and carers with staff, for example feedback from stakeholder events where service users can carers assessed the Trust progress on the outcomes described in the Trust’s Equality Delivery System (Goals 1 and 2 which relate to patient care) • Involving staff in responding to the Francis report though local workshops • Holding staff engagement events NHS Staff Survey 2011 NHS Staff Survey 2012 3.36 3.20 National Median Score 3.42 3.54 Lowest Trust Score 3.07 3.06 Highest Trust Score 3.94 4.06 2 34 gether NHS Foundation Trust Score 4. “Patient experience of community mental health services” indicator score with regard to a patient’s experience of contact with a health or social care worker during the reporting period gether NHS Foundation Trust has taken the following action to improve this score, and so the quality of its services, by: 2 • Scrutinising the 2012 data for both Herefordshire and Gloucestershire further and noting some differences in where developments appear to be needed. This has formed an action plan which was completed collaboratively in September 2012 and cascaded for implementation across operational services through Locality Directors and Service Experience Leads gether NHS Foundation Trust considers that this data is as described for the following reasons: 2 • We are aware that the survey results for 2011 and 2012 do not compare like with like. This is because the 2011 2 gether survey did not include the Herefordshire population. This matter needs to be considered when making conclusions from the numerical data supplied NHS Community Mental Health Survey 2011 NHS Community Mental Health Survey 2012 8.7 8.4 National Average Score not available not available Lowest Score not available 8.2 Highest Score not available 9.1 2 gether NHS Foundation Trust Score 5. The number and rate* of patient safety incidents reported within the trust during the reporting period and the number and percentage of such patient safety incidents that resulted in severe harm or death • The Trust is in the highest 25% of reporters and it is believed that organisations that report more incidents usually have a better and more effective safety culture • There is limited national guidance in assigning categories of harm for mental health providers gether NHS Foundation Trust considers that this data is as described for the following reasons: 2 • If staff reporting an incident do not include all required information, there can be delays in uploading incidents to the NRLS • Not all of the Trust’s reported incidents meet the criteria for uploading to the National Reporting and Learning Systems (NRLS), for example, whilst the trust documents all deaths by natural causes within its risk management system it only uploads those in which natural causes are not suspected. All deaths by suspected suicide are reported in line with the revised CQC guidance effective from 1 April 2012 gether NHS Foundation Trust has taken the following action to improve this rate, and so the quality of its services, by: 2 • Strengthening local guidance to staff regarding data completeness, reporting deadlines and timeliness of upload • NRLS data is published 6 months in arrears; therefore data below for severe harm and death will not correspond with the serious incident information shown in section 5.6 of the Quality Report • Including additional local guidance within the Trust’s Incident Reporting Policy to assist staff in classifying categories of harm October 2011 - March 2012 April 2012 - September 2012 Number Rate Severe Death Number Rate Severe Death 1268 34.6 0/0% 3/0.2% 1503 36.79 2/0.1% 4/0.3% 105,228 19.9 110,360 23.8 Lowest Trust 44 0 0/0% 0/0% 22 0 0/0% 0/0% Highest Trust 6080 86.89 69/2.3% 53/0.9% 6903 70.29 316/8.9% 78/2.6% gether NHS Foundation Trust 2 National 496/0.5% 806/0.8% 831/0.8% 916/0.8% * Rate is the number of incidents reported per 1000 bed days. 35 This year is the first time that this indicator has been required to be included within the Quality Report alongside comparative data provided, where possible, from the Health and Social Care Information Centre. The National Reporting and Learning Service (NRLS) was established in 2003. The system enables patient safety incident reports to be submitted to a national database on a voluntary basis designed to promote learning. It is mandatory for NHS Trusts in England to report all serious patient safety incidents to the Care Quality Commission (CQC) as part of the Care Quality Commission registration process. As there is not a nationally established and regulated approach to reporting and categorising patient safety incidents, different Trusts may choose to apply different approaches and guidance to reporting, categorisation and validation of patient safety incidents. The approach taken to determine the classification of each incident, such as those ‘resulting in severe harm or death’, will often rely on clinical judgement. This judgement may, acceptably, differ between professionals. In addition, the classification of the impact of an incident may be subject to a potentially lengthy investigation which may result in the classification being changed. To avoid duplication of reporting, all incidents resulting in death or severe harm should be reported to the NRLS who then report them to the Care Quality Commission. Although it is not mandatory, it is common practice for NHS Trusts to report patient safety incidents under the NRLS’s voluntary arrangements. This change may not be reported externally and the data held by a Trust may not be the same as that held by the NRLS. Therefore, it may be difficult to explain the differences between the data reported by the Trusts as this may not be comparable. Community Survey 2012 During 2012, the CQC published the results of an independent survey taken in 2012 that tested the experience of our community service users, comparing the results with most other mental health trusts. The results for Gloucestershire and Herefordshire were: Our Score (out of 10) Compared with other Mental Health Trusts Health & Social Care Workers 8.4 About the same Medications 7.5 About the same Talking Therapies 6.1 Worse Care Co-ordinator 8.3 About the same Care Plan 6.9 About the same Care Review 7.4 About the same Day to Day Living 5.6 About the same Crisis Care 5.9 About the same Overall 6.5 About the same Questions about: The survey received replies from 273 of our service users out of 850 who were asked to participate, which represents a response rate of 33% compared with an average for all mental health trusts of 32%. Full details of this survey can be found on the CQC website www.cqc.org.uk. Overall, these results state that we are mainly within the expected range for mental health trusts in all areas, except for one. It is clear we have more to do to improve the experience of people using our services. We have an action plan in place to address this and will monitoring feedback through our local surveys throughout the coming year. We anticipate that the additional actions and initiatives identified earlier in the report will result in further improvements in these scores next year. 36 Staff Survey 2012 Staff Survey 2012 Every year, the Department of Health conducts a national NHS staff survey. The survey is used to gauge how well our staff believe that we treat them and provide good management as described in the staff pledges of the NHS Constitution. The 2012 results were released in March 2013. This year there were 28 Key Findings in the survey compared with 38 the previous year. Of those 28, seven key findings cannot be compared with the previous year’s results because of changes to the format of the survey questions so that comparisons with the 2011 results were not possible for seven key results, leaving 21 for comparative purposes. Of the 21 results which can be compared, staff said that that there was no change in many areas and consequently results were consistent for 15 of the key findings when compared with the previous year. However results are worse than other like-type Trusts. For a further five key findings, results were not as good as the previous year, and one was better. When compared with like-type Trusts in the 28 key areas we were: • • • • Better than average in 3 areas (8) Average in 7 (10) Worse than average in 7 (9) In the lowest 20% in 11 (6) The previous year’s figures are shown in brackets. For the second year running our survey also included staff in our Herefordshire services. However the response rate overall was lower with only 48% of staff in the random sample returning their questionnaire compared with 60% the previous year. The comparison with last year shows that in many areas we are roughly the same, but it is clear that other Trusts have improved relative to us. The five key findings for which the Trust compares most favourably with other mental health/learning disability Trusts in England were: • Working extra hours • Staff witnessing potentially harmful errors, near misses or incidents in last month • Support from immediate managers • Staff experiencing physical violence from patients, relatives or the public in last 12 months • Feeling pressure in last three months to attend work when feeling unwell The five key findings for which the Trust compares least favourably with other mental health/learning disability trusts in England were: • Good communication between senior management and staff • Motivation at work • Staff receiving job relevant training, learning or development in last 12 months • Recommendation of the Trust as a place to work or receive treatment • Having equality and diversity training in last 12 months The above five key findings are included in the eleven key findings where the Trust is in the bottom 20% for like type Trusts. The other six key findings in this category are: • Staff feeling satisfied with the quality of work and patient care they can deliver • Agreeing that their role makes a difference to patients • Work pressure felt by staff • Having well-structured appraisals in the last 12 months • Experiencing work related stress in the last 12 months • Able to contribute to improvements at work 37 Whilst the results of the 2012 survey were disappointing, they were not wholly unexpected in the context of the significant change which services and staff have experienced in the preceding 12 months. The Trust has therefore been pro-active in starting a staff engagement programme which will be co-ordinated and overseen by a Workforce and Organisational Development Committee. This committee will report to the Trust Board Executive Committee and will oversee four work streams of ‘Training’; ‘Culture’; ‘Workforce’ and ‘Staff Engagement’. The Trust Board has approved a set of recommendations which will enable the Trust to respond to the results of the 2012 survey. Three key findings have been set at the priorities, these are ‘stress at work’; ‘communication with senior managers’ and ‘recommendation of the Trust as a place to work and receive treatment’. In respect of these key findings, work has commenced through the running of focus groups led by staff for staff to understand experiences, to enable individuals to identify actions they can take to make a difference, what managers can do and how organisational issues can be addressed. Specific actions have already been identified such as a comprehensive review of the appraisal process to streamline the documentation and ensure the process is meaningful for staff and managers; reviewing and revising the Trust’s recognition programme to include local or more frequent recognition where staff are making a difference to our service users and carers; holding health and wellbeing days for staff; revising and re-publicising our Dignity at Work scheme encouraging staff to seek support and advice on issues at work; and improving course booking processes to ensure staff can more easily book training and supporting managers to release staff. Staff will be asked to participate in both structured conversations and anonymous online surveys on the topics above. Specifically, we will seek ideas from staff on how we can make further improvements in the care we are commissioned to provide and how we can make our Trust a better place to work. The Trust will actively work with Staff Side representatives who are committed to improving the working environment and all feedback will be fed into our new Staff Engagement Committee. We will continue to ask managers what additional support they need and we are planning an additional leadership and development programme for the Autumn. Further details can be found in the Annual Staff Survey section of our Annual Report and Accounts 2012/13. PEAT Assessment Results 2012/13 Every year, our locations are assessed for the quality of the environment, food, and for privacy and dignity. These are known as Patient Environment Action Team (PEAT) assessments. The table below gives a summary of their findings for the eight main inpatient premises during the year. This is the last publication of PEAT results in their current form; following a Government announcement in July 2012 that a new inspection programme will be developed for launch in April 2013. Weighted Environment Score Overall Food Score Overall Privacy & Dignity Score Charlton Lane 4 Good 5 Excellent 5 Excellent Wotton Lawn 4 Good 4 Good 5 Excellent Laurel House 4 Good 5 Excellent 5 Excellent Honeybourne, Cheltenham 4 Good 4 Good 5 Excellent Hollybrook 4 Good 5 Excellent 5 Excellent Westridge 4 Good 5 Excellent 5 Excellent BranchLea Cross, Cheltenham 4 Good 5 Excellent 5 Excellent Stonebow Unit 4 Good 5 Excellent 5 Excellent Site Name 38 Annex 1. Statements from our Partners on the Quality Account We have taken the opportunity of sharing our Quality Account progress and development with many of our partners throughout the year, including the Board of Governors. We are very grateful for the time they have taken to provide helpful comments and suggestions in its content and layout. We have already taken the opportunity to include many of their very useful suggestions and recommendations in the final version of this document. Responses from those partners who have made formal written responses are given below. Gloucestershire Health, Community and Care Overview and Scrutiny Committee Comments on the 2gether NHS Foundation Trust Quality Report 2012/13 The Health, Community and Care Overview and Scrutiny Committee (HCCOSC) welcome the opportunity to comment on the 2gether NHS Foundation Trust’s Quality Account 2012/13. The committee has developed a good working relationship with the 2gether NHS Foundation Trust; and appreciates the open manner in which Trust representatives attend committee meetings. I hope that this will continue into the new council and the new Health and Care Overview and Scrutiny Committee. The Quality Account shows that a lot of work has been undertaken by the Trust during 2012/13; and demonstrates the Trust’s commitment to its service users and their carers. The Winterbourne View and Francis Reports have raised serious concerns regarding the care of patients and damaged people’s confidence in the care system. It is good to see that the Trust has taken forward the issues and lessons discussed into its work planning and leadership team. However, following on from my comments on the structure of the 2011/12 Quality Account, I must again comment that this document is not easily accessible, and suggest that the Trust considers the presentation of this report such that it is more easily understandable. I would like to thank Shaun Clee, Trish Jay and Jane Melton for attending our meetings and answering our questions in a helpful and informative manner. Cllr Stephen McMillan Chairman Herefordshire Health, Community and Care Overview and Scrutiny Committee Comments on the 2gether NHS Foundation Trust Quality Report 2012/13 The Health and Social Care Overview and Scrutiny Committee have created a good working relationship with 2 gether NHS Foundation Trust over the past year. In light of the Francis report and the significant changes to the health care system, it is imperative that this relationship continues to develop and grow. We are now working in a world where transparency and openness is of even more importance than ever. The Committee would like to thank 2gether for their openness and transparency in their reports and in meetings attended. Though the Committee has no specific points to make reference this year’s Quality Accounts, the Committee are changing the way in which they view and comment on Quality Accounts. Later this year the Committee shall invite key stakeholders to a briefing on the content of Quality Reports, recurring themes and areas of improvement. This will then allow the Committee to make a comprehensive and informed response for 2013/2014. It would be of great benefit if the Committee could receive the Quality Reports well within time next year to allow Members to give sufficient scrutiny of the document. I would like to thank Shaun Clee and Colin Merker for their attendance at the Health and Social Care Overview and Scrutiny Committee. Councillor Jeremy Millar, Chair of Health and Social Care Overview and Scrutiny Committee 39 Gloucestershire Local Involvement Network (LINk) Comments on the 2gether NHS Foundation Trust DRAFT Quality Account 2013 Gloucestershire LINk welcomes the opportunity to comment on the draft 2gether NHS Foundation Trust’s 2013 Quality Account. The following comments have been compiled by a group of LINk members. This early draft of the Quality Account does not include a large amount of qualitative data or the CEO’s statement, which makes the comments rather limited. LINk has been aware that there have been improvements in the mental health services for residents of Gloucestershire and feel that the draft does not sufficiently emphasise where the Trust is providing an excellent service and also where improvements have been made. It would be helpful to highlight the transitions/changes which have taken place during this report period. For example, the prison closed in mid-February resulting in incomplete data-sets relating to the effort put into this area of work. As this is a document that is available to the public it might be better if there was an explanation of the ‘Fair Horizons’ model of care or Care Programme approach so that the public can understand the different parts of the mental health services in the county. An example of this is found in the statement that the implementation of a contact centre will improve the service without explaining how this helps. There is a lack of qualitative information which is disappointing especially in relation to this particular area of health. More qualitative evidence would bring the report ‘alive’. Some explanation of how certain issues, such as the number of falls, are being tackled and how positive results have been achieved would be useful. A more consistent approach in the presentation of data would be welcome particularly where data for Gloucestershire and Herefordshire are seen side by side. We would also suggest that specific percentages be used to give a more accurate reflection of the Trust’s efforts into service improvement, especially as achievements have mostly met and exceeded targets. There is a disappointing lack of understanding of Equality Diversity System (EDS) as baselines do not appear to have been set. Moreover, it is not obvious how partnership with other services has improved this engagement with the community. We would very much welcome the establishment and implementation of a Children’s IAPT in Gloucestershire as this was a clear gap in the CYP services provided. We were delighted to see that the inpatient wards for Older Peoples’ services in Gloucestershire had gained accreditation with national standards. The development of the Service User Charter has enabled patients to understand the ethos of the organisation. It is disappointing that only 48% of staff taking part in the random sample returned their questionnaire compared with 60% in the previous year and that one of the key findings that compare least favourably with other Mental Health/Learning Disability Trusts was the ‘motivation at work’ which is reflected in these scores. Unfortunately, the cessation of the LINks on March 31 makes it impossible to do more than make these brief comments which may not be relevant on the completed document. Barbara Marshall Chair of Gloucestershire LINk 28 March 2013 40 Healthwatch - Herefordshire Comments 2012-13 Quality Account for 2 gether NHS Foundation Trust 1. Thank you for the opportunity to comment on the Quality Account. You will be aware that Healthwatch Herefordshire came into being on the 1 April; therefore this response is built on information derived from or collated by the Herefordshire LINk. Healthwatch Herefordshire looks forward to receiving the Quality Account for 2013/14 and making a fuller contribution as we will have data to compare with this Account and knowledge gained during this coming year. 1.1 We would like to acknowledge the work that the Trust has done to build the relationship with partners in Herefordshire to secure better quality services. Attendance at and the reports given to the LINk during the year were well received. The co-ordination of activity with partners to support service users and their carers enabled a clearer understanding of the roles of each organisation and where there were potential gaps in services or the quality was not as it should be. 1.2 This work is not reflected in the Account and would have been an opportunity to demonstrate that the Trust is committed to support the work of others as part of driving up quality. An area identified as a gap in service was the need to listen to Carers concerns about deterioration in the mental health of the person they care for. A report produced jointly by the LINk and Herefordshire Carers Support and subsequent explorations had identified that some carers of people with enduring conditions didn’t know where to contact or felt they had not been listened to, and this had resulted in a crisis incident. We note in the CQUINS section of the Account that this is an area to be monitored and will be of continuing concern. Other parts of the Account refer to crisis care for the service user, showing positive results, maybe cross referencing of some standards would be helpful. 1.3 Participation in clinical research is cited as low in Herefordshire for this period due to service changes; however, we understand that involvement with research has been low in Herefordshire for some time, according to information from the PCRN. With a rural scattered population and transport challenges it is important for Herefordshire people to be offered the same opportunities to engage with research as people in other areas such as Gloucestershire and for this to be facilitated appropriately. 1.4 One aspect not commented upon but with a bearing on one of the CQUIN goals, namely to ‘improve responsiveness to the personal needs of patients’, is initial access to mental health care and support and possibly identification of needs at the first point of access. Recent feedback to Healthwatch indicates that there is a perception that mental healthcare and support is diminishing within the voluntary sector and needs to be picked up by statutory services. In the meantime increasing numbers of people do not know where to go for support and help. Therefore, access to the mental health services pathway may be an area to monitor for the future. 1.5 The Account gives a good record of the quality ‘tool box’, the impact on the longer term benefits to people using the services and their families is less clear and we hope that Healthwatch will have a role in ensuring this is embedded as the goal for us all. Paul Bates Interim Chair Herefordshire Healthwatch 02/05/2013 41 Gloucestershire Clinical Commissioning Group Statement for Quality Account 2 gether NHS Foundation Trust 2012/13 Gloucestershire Clinical Commissioning Group (CCG), on behalf of its predecessor NHS Gloucestershire, has taken the opportunity to review the Quality Account prepared by 2gether NHS Foundation Trust (2gether) for 2012/13. We are pleased that 2gether has been working alongside NHS Gloucestershire and the shadow CCG during 2012/13 to maintain and further improve the quality of commissioned services. gether have engaged with the development of initiatives such as the Map of Medicine and Your Health, Your Care strategy– our shared vision for the future. They have also demonstrated further improvement of the safety, effectiveness and patient experience of services particularly in relation to the successful development of an appropriate Outcome Measure for Learning Disability services and reduction in the number of patient falls within inpatient environments in Gloucestershire. 2 The CCG very much welcome 2gether’s focus on patient experience and quality of care, which demonstrates a joint commitment to delivering high quality compassionate care. We look forward to developing a whole health and social care community clinical programme approach towards commissioning and delivering services, with a strong emphasis on clinical leadership and engagement. Integrated care will be delivered according to agreed pathways and standards, with strong user and carer involvement being evident from prevention to end of life. There are robust arrangements in place with 2gether to agree, monitor and review the quality of services. The Clinical Quality Review Group continues to meet bi-monthly and brings together GPs, senior clinicians and managers from both 2gether and Gloucestershire CCG. We have received assurance throughout the year from 2 gether in relation to key quality issues, both where quality and safety has improved, and where it fell below expectations, remedial plans put in place and learning shared wherever possible. It is the view of the CCG that the Quality Account produced by 2gether does not in general reflect a balanced view of some of the services provided by the Trust. Whilst acknowledging the excellent outcomes delivered by 2gether, the Account would provide a more rounded view of services if the areas for improvement were more clearly identified. For example in respect of children and young people’s services (CYPS) the targets indicated in the report show successful year end outcomes, 95% of non-urgent tier 3 cases will be seen within 8 weeks (CYPS) achieving 97%, however the target for Non-urgent tier 3 cases will be treated within 8 weeks (CYPS) achieved a year end performance of 74%, and did not achieve the target and was not reported in the account. The CCG are aware of the efforts to improve this target but feel as a public document it would be more transparent to clearly highlights areas for improvement and describe actions to improve these services. It was disappointing to see the results of the staff survey indicating the Trust's score was in the lowest 20% when compared with Trusts of a similar type, and a decrease in staff recommendation of the Trust as a place to work or receive treatment which was also in the lowest 20%. The CCG welcome the initiatives described in the report to address these concerns and will be working with 2gether over the next few months to ensure improvement in these key areas. The priorities for 2013/14 have been developed in partnership and Gloucestershire CCG endorse the proposals set out in the Quality Account. The Francis report and the failings at Winterbourne View underline the importance of honesty; transparency and engaging with stakeholders and the CCG are committed to working with 2gether to ensure they are in a strong position to manage both present and future challenges. The CCG will work with 2gether to deliver best value effective care for the people of Gloucestershire. Upholding these values ensures that the population of Gloucestershire will maintain trust and confidence in these core NHS services. Gloucestershire CCG can confirm that we consider that the Quality Account contains accurate information in relation to the quality of services that 2gether NHS Foundation Trust provides to the residents of Gloucestershire. Marion Andrews-Evans Executive Nurse and Quality Lead NHS Gloucestershire Clinical Commissioning Group 42 Herefordshire Clinical Commissioning Group Statement for Quality Account 2012/13 2 gether NHS Foundation Trust Our ref: Ask for: David Farnsworth Tel: 01432 260618 Email: david.farnsworth@herefordshireccg.nhs.uk Herefordshire Clinical Commissioning Group (CCG) is pleased to receive 2gether NHS Foundation Trust quality account for 2012/13 which provides an overview of the quality of services during the period, and sets out priorities for the forthcoming year. Following a review of the information presented, coupled with commissioner led reviews of quality across all providers, the CCG is satisfied with the accuracy of the report. This recognises the Trust commitment to quality and demonstrates further development which mirrors the aspirations of commissioners. The CCG appreciates the renewed focus to improve the physical health of patients with mental health problems, alongside the commitment to reduction in suicide within the service user group. Furthermore, the focus on improving patient experience is welcomed which mirrors wider national learning which increasingly values the voice of service users. Herefordshire CCG has set out a quality framework which includes assurance visits and regular quality review meetings between provider and commissioners to scrutinise and challenge quality. We look forward to continuing this work during the coming year to ensure the delivery of high quality, high performing and safe services for the residents of Herefordshire. Yours sincerely, David Farnsworth Executive Lead Nurse Herefordshire CCG The Royal College of Psychiatrists Statement of Participation in National Quality Improvement Projects managed by The Royal College of Psychiatrists’ Centre for Quality Improvement Participation by Trust National Participation 3 ECT Clinics 93 ECT Clinics Working age adults wards 4 wards 165 wards Psychiatric intensive care units (PICU) 1 PICU 34 PICUs Older people mental health wards 3 wards 57 wards Inpatient learning disability units 2 units 36 units Inpatient rehabilitation units 0 units 36 units 2 services 61 services 0 teams 43 teams April 1 2012 – March 31 2013 CCQI Programme Service accreditation programmes ECT clinics Memory services Psychiatric liaison teams 43 Participation by Trust National Participation 0 units 91 units 2 teams 45 teams 0 communities 83 communities Low secure forensic mental health services 0 services 66 services Medium secure forensic mental health services 0 services 64 services 0 units 15 units April 1 2012 – March 31 2013 CCQI Programme Service quality improvement networks Inpatient child and adolescent units Child and adolescent community MH teams Therapeutic communities Perinatal mental health inpatient units The Royal College of Psychiatrists Statement of Participation in the Prescribing Observatory for Mental Health (POMH) 2 gether NHS Foundation Trust was not a member of POMH in 2012/13 April 1 2012 – March 31 2013 POMH Topic Number of patients enrolled by Trust Number of patients enrolled nationally Prescribing antipsychotics for dementia (Topic 11a) 0 TBC Assessment of the side effects of depot antipsychotics (Topic 6c) 0 TBC Monitoring of patients prescribed lithium (Topic 7c) 0 TBC Prescribing antipsychotics for children & adolescents (Topic 10b) 0 TBC The Royal College of Psychiatrists Statement of Participation in the National Audit of Psychological Therapies April 1 2012 – March 31 2013 2 Number of teams enrolled by Trust gether NHS Foundation Trust 1 Number of teams enrolled nationally TBC Trust Contacts for National Quality Improvement Projects CCQI Programme Name Email ECT Clinic - Gloucestershire Dr Jim Laidlaw jim.laidlaw@glos.nhs.uk Working age adults wards Dr Tiffany Earle tiffany.earle@glos.nhs.uk Psychiatric intensive care units (PICU) Caroline Driscoll caroline.driscoll@glos.nhs.uk Older people mental health wards Sally Simmonds sally.simmonds@herefordpct.nhs.uk Inpatient learning disability units Tim Coupland tim.coupland@glos.nhs.uk Inpatient rehabilitation units Sarah Bennion sarah.bennion@herefordpct.nhs.uk Mathew Page mathew.page@glos.nhs.uk Service Quality Improvement Networks Children & Young Peoples Services 44 Annex 2. Statement of Directors’ Responsibilities in respect of the Quality Report The directors are required under the Health Act 2009 and the National Health Service Quality Accounts Regulations 2010 as amended to prepare Quality Accounts for each financial year. Monitor has issued guidance to NHS foundation trust boards on the form and content of annual Quality Reports (which incorporate the above legal requirements) and on the arrangements that foundation trust boards should put in place to support the data quality for the preparation of the quality report. In preparing the Quality Report, directors are required to take steps to satisfy themselves that: • the content of the Quality Report meets the requirements set out in the NHS Foundation Trust Annual Reporting Manual 2012/13; • the content of the Quality Report is not inconsistent with internal and external sources of information including: o o o o o o o o o o o o Board minutes and papers for the period April 2012 to May 2013 Papers relating to Quality reported to the Board over the period April 2012 to May 2013 Feedback from the Gloucestershire commissioners dated May 2013 Feedback from the Herefordshire commissioners dated May 2013 Feedback from Governors dated April 2013 Feedback from Herefordshire Healthwatch dated 2 May 2013 Feedback from Gloucestershire LINk dated 28 March 2013 The Trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009, dated April 2013; The 2012 national patient survey The 2012 national staff survey The Head of Internal Audit’s annual opinion over the trust’s control environment dated May 2013 CQC quality and risk profiles dated April 2012 to March 2013 • the Quality Report presents a balanced picture of the NHS foundation trust’s performance over the period covered; • the performance information reported in the Quality Report is reliable and accurate; • there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Report, and these controls are subject to review to confirm that they are working effectively in practice; • the data underpinning the measures of performance reported in the Quality Report is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Report has been prepared in accordance with Monitor’s annual reporting guidance - which incorporates the Quality Accounts regulations - (published at www.monitor-nhsft.gov.uk/annualreportingmanual) as well as the standards to support data quality for the preparation of the Quality Report available at www.monitornhsft.gov.uk/annualreportingmanual. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Report. By order of the Board NB: sign and date in any colour ink except black Date: 28 May 2013 Chair Date: 28 May 2013 Chief Executive 45 Annex 3. Glossary AIMS National accreditation for Inpatient Mental Health Services process led by the Royal College of Psychiatrists. It is a standards-based accreditation process for adult inpatient mental health services that encourages organisations to identify and prioritise problems and sets achievable targets for change. CAMHS Child and Adolescent Mental Health Services CBT Cognitive Behavioural Therapy Clinical Commissioning Group CCG CPA Care Programme Approach: a system of delivering community service to those with mental illness CQC Care Quality Commission – the Government body that regulates the quality of services from all providers of NHS care CQUIN Commissioning for Quality & Innovation: this is a way of incentivising NHS organisations by making part of their payments dependent on achieving specific quality goals and targets CRA The Community Reinforcement Approach (CRA) is a comprehensive behavioural programme for treating substance-abuse problems Essence of Care Screening Essence of Care Screening is a method of assessing the risks associated with the condition of a service user so that the most appropriate treatment can be determined 2 gether NHS Trust’s programme to reengineer their services more around their service user’s individual needs in a one-stop shop approach rather than being looked after by many different teams. This will provide much enhanced quality of care Fair Horizons 46 Green Light Mental Health Toolkit A self-audit set of 39 indicators that was initially instigated by the Healthcare Commission (previous regulator to CQC) to measure the quality of the health services provided to people with learning disabilities GRiP Gloucestershire Recovery in Psychosis (GRiP) is 2gether’s specialist early intervention team working with people aged 14-35 who have first episode psychosis GSAS Gloucestershire Smoking Advice Service HCCOSC Health, Community and Care Overview and Scrutiny Committee HoNOS Health of the Nation Outcome Scales – this is the most widely used routine measure of clinical outcome used by English mental health services. IAPT Improving Access to Psychological Therapies Information Governance (IG) Toolkit The IG Toolkit is an online system that allows NHS organisations and partners to assess themselves against a list of 45 Department of Health Information Governance policies and standards The King’s Fund The King’s Fund is a charity that seeks to understand how the health service in England can be improved KUF The National Knowledge and Understanding Framework on Personality Disorder is a national framework to support people to work more effectively with personality disorder LINk Local Involvement Networks (LINks) are groups made up of individuals and community groups, such as faith groups and residents’ associations, working together to improve health and social care services LIPS The Leading Improvement in Patient Safety programme (LIPS) is concerned with building capacity and capability within hospital teams to improve patient safety MECC Making Every Contact Count is about using every opportunity to talk to individuals about improving their health and wellbeing Memory Assessment Service Memory assessment services offer a responsive service to aid the early identification of dementia, and include a full range of assessment, diagnostic, therapeutic and rehabilitation services ensuring an integrated approach to the care of people with dementia and the support of their carers, in partnership with local healthcare, social care and voluntary organisations MHMDS The Mental Health Minimum Data Set is a series of key personal information that should be recorded on the records of every service user Monitor Monitor is the independent regulator of NHS foundation trusts.They are independent of central government and directly accountable to Parliament MRSA Methicillin-resistant Staphylococcus aureus (MRSA) is a bacterium responsible for several difficult-to-treat infections in humans. It is also called multidrug-resistant NHS The National Health Service refers to one or more of the four publicly funded healthcare systems within the United Kingdom. The systems are primarily funded through general taxation rather than requiring private insurance payments. The services provide a comprehensive range of health services, the vast majority of which are free at the point of use for residents of the United Kingdom NICE The National Institute for Health and Care Excellence (previously National Institute for Health and Clinical Excellence) is an independent organisation responsible for providing national guidance on promoting good health and preventing and treating ill health NIHR The National Institute for Health Research supports a health research system in which the NHS supports outstanding individuals, working in world class facilities, conducting leading edge research focused on the needs of patients and the public Tier 3 Children’s Services Services which offer a comprehensive assessment and treatment service based on a skill mix drawn from professionals from the range of disciplines and therapeutic backgrounds (such as the local Children and Young Peoples Service in Gloucestershire and CAMHS in Herefordshire) NPSA The National Patient Safety Agency is a body that leads and contributes to improved, safe patient care by informing, supporting and influencing the health sector NTA The National Treatment Association for Substance Misuse is a special NHS health authority established to improve the availability, capacity and effectiveness of drug treatment in England PCT The Primary Care Trust, which oversees the operations of providers of NHS care. The PCTs responsible for 2gether NHS Foundation Trust are NHS Gloucestershire and NHS Herefordshire. PEAT assessments Patient Environment Action Team assessments are assessments carried out by the NPSA into the quality of the environment, food, and privacy and dignity in every inpatient location PICU POMH-UK Psychiatric Intensive Care Unit QRP The Quality and Risk Profile is a monthly compilation by the CQC of all the evidence about a Trust they have in order to judge the level of risk that the Trust carries to fulfil its obligations of care RiO This is the name of the electronic system for recording service user care notes and related information within 2gether NHS Foundation Trust. In a major exercise, it has been implemented across almost all the Trust’s areas of operation during 2010 Safety Thermometers These are national tools for measuring patient safety. The general Safety Thermometer was introduced for all NHS providers in April 2012. They are required to submit monthly data returns to the NHS Information Centre. The Mental Health Safety Thermometer is still in development SHA Strategic Health Authority SIRI Serious Incident Requiring Investigation, previously known as a “Serious Untoward Incident”. A serious incident is essentially an incident that occurred resulting in serious harm, avoidable death, abuse or serious damage to the reputation of the Trust or NHS. In the context of the Quality Report, we use the standard definition of a Serious Incident given by the NPSA The national Prescribing Observatory for Mental Health is a body that helps specialist mental health Trusts and healthcare organisations improve their prescribing practice 47 Service Users Charter A set of pledges made by 2gether staff about the way in which we will work with people who use our services Step 2 IAPT These interventions include guided self-help (booklets and worksheets) computerised CBT, employment advice, signposting to other services, books on prescription, lifestyle support and group work Step 3 IAPT The Step 3 service will work with people who have been assessed at Step 2, may have undertaken Step 2 interventions or whose needs require more complex interventions possibly on an individual basis, which will provided by High Intensity Therapists VTE Venous thromboembolism is a potentially fatal condition caused when a blood clot (thrombus) forms in a vein. In certain circumstances it is known as Deep Vein Thrombosis Annex 4. How to Contact Us If you have any questions or comments concerning the contents of this report or have any other questions about the Trust and how it operates, please write to: Mr Shaun Clee Chief Executive Officer 2 gether NHS Foundation Trust Rikenel Montpellier Gloucester GL1 1LY Or email: shaun.clee@glos.nhs.uk Alternatively, you may telephone on 01452 894000 or fax on 01452 894001. Other Comments, Concerns, Complaints and Compliments Your views and suggestions are important us. They help us to improve the services we provide. You can give us feedback about our services by: • Speaking to a member of staff directly • Telephoning us on 01452 894673 • Completing our Online Feedback Form at www.2gether.nhs.uk • Completing our Comment, Concern, Complaint, Compliment Leaflet, available from any of our Trust sites or from our website www.2gether.nhs.uk • Using one of the feedback screens at selected Trust sites • Contacting Patient Advice and Liaison Service (PALS) on 0800 0151 548 • Writing to the appropriate service manager or the Trust’s Chief Executive Alternative Formats If you would like a copy of this report in large print, Braille, audio cassette tape or another language, please telephone us on 01452 894000 or fax on 01452 894001. 48 Independent Auditor’s Report to the Council of Governors of 2gether NHS Foundation Trust on the Quality Report We have been engaged by the Council of Governors of 2 gether NHS Foundation Trust to perform an independent assurance engagement in respect of 2gether NHS Foundation Trust’s Quality Report for the year ended 31 March 2013 (the “Quality Report”) and certain performance indicators contained therein. This report, including the conclusion, has been prepared solely for the Council of Governors of 2gether NHS Foundation Trust as a body, to assist the Council of Governors in reporting 2gether NHS Foundation Trust’s quality agenda, performance and activities. We permit the disclosure of this report within the Annual Report for the year ended 31 March 2013, to enable the Council of Governors to demonstrate they have discharged their governance responsibilities by commissioning an independent assurance report in connection with the indicators. To the fullest extent permitted by law, we do not accept or assume responsibility to anyone other than the Council of Governors as a body and 2gether NHS Foundation Trust for our work or this report save where terms are expressly agreed and with our prior consent in writing. Scope and subject matter The indicators for the year ended 31 March 2013 subject to limited assurance consist of the national priority indicators as mandated by Monitor: • Delayed Transfers of Care • Access to Crisis Resolution Teams We refer to these national priority indicators collectively as the “indicators”. Respective responsibilities of the Directors and auditors The Directors are responsible for the content and the preparation of the Quality Report in accordance with the criteria set out in the NHS Foundation Trust Annual Reporting Manual issued by Monitor. Our responsibility is to form a conclusion, based on limited assurance procedures, on whether anything has come to our attention that causes us to believe that: • the Quality Report is not prepared in all material respects in line with the criteria set out in the NHS Foundation Trust Annual Reporting Manual; • the Quality Report is not consistent in all material respects with the following sources: • Board minutes for the period April 2012 to March 2013; • Feedback from Commissioners dated May 2013; • Feedback from local Healthwatch organisations dated May 2013; • The Trust’s 2012/13 complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009; • The Mental Health Patient Survey report 2012; • The National Staff Survey results 2012; 49 • Care Quality Commission quality and risk profiles dated March 2012 – September 2012 and October 2012 – March 2013; • The Head of Internal Audit’s annual opinion over the Trust’s control environment for the year ending 31/03/2013; and • Other papers relating to Quality reported to the Board from April 2012 to March 2013. • The indicators in the Quality Report identified as having been the subject of limited assurance in the Quality Report are not reasonably stated in all material respects in accordance with the NHS Foundation Trust Annual Reporting Manual and the six dimensions of data quality set out in the Detailed Guidance for External Assurance on Quality Reports. We read the Quality Report and consider whether it addresses the content requirements of the NHS Foundation Trust Annual Reporting Manual, and consider the implications for our report if we become aware of any material omissions. We read the other information contained in the Quality Report and consider whether it is materially inconsistent with the documents specified within the detailed guidance. We consider the implications for our report if we become aware of any apparent misstatements or material inconsistencies with those documents (collectively the “documents”). Our responsibilities do not extend to any other information. We are in compliance with the applicable independence and competency requirements of the Institute of Chartered Accountants in England and Wales (ICAEW) Code of Ethics. Our team comprised assurance practitioners and relevant subject matter experts. Assurance work performed We conducted this limited assurance engagement in accordance with International Standard on Assurance Engagements 3000 (Revised) – “Assurance Engagements other than Audits or Reviews of Historical Financial Information” issued by the International Auditing and Assurance Standards Board (“ISAE 3000”). Our limited assurance procedures included: • Evaluating the design and implementation of the key processes and controls for managing and reporting the indicators. • Making enquiries of management • Testing key management controls • Limited testing, on a selective basis, of the data used to calculate the indicator back to supporting documentation • Comparing the content requirements of the NHS Foundation Trust Annual Reporting Manual to the categories reported in the Quality Report. • Reading the documents A limited assurance engagement is smaller in scope than a reasonable assurance engagement. The nature, timing and extend of procedures for gathering sufficient appropriate evidence are deliberately limited relative to a reasonable assurance engagement. Conclusion Limitations • the Quality Report is not prepared in all material respects in line with the criteria set out in the NHS Foundation Trust Annual Reporting Manual; Non-financial performance information is subject to more inherent limitations than financial information, given the characteristics of the subject matter and the methods used for determining such information. The absence of a significant body of established practice on which to draw allows for the selection of different but acceptable measurement techniques which can result in materially different measurements and can impact comparability. The precision of different measurement techniques may also vary. Furthermore, the nature and methods used to determine such information, as well as the measurement criteria and the precision thereof, may change over time. It is important to read the Quality Report in the context of the criteria set out in the NHS Foundation Trust Annual Reporting manual. The scope of our assurance work has not included governance over quality or non-mandated indicators which have been determined locally by 2gether NHS Foundation Trust. Based on the results of our procedures, nothing has come to our attention that causes us to believe that, for the year ended 31 March 2013: • the Quality Report is not consistent in all material respects with the sources specified in the Detailed Guidance for External Assurance on Quality Reports; and • the indicators in the Quality Report subject to limited assurance have not been reasonably stated in all material respects in accordance with the NHS Foundation Trust Annual Reporting Manual. Deloitte LLP Chartered Accountants Bristol Office 28 May 2013 50