2014/15 Quality Account Looking after you locally
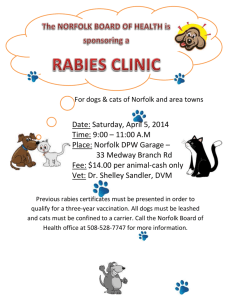
advertisement

Quality Account 2014/15 Looking after you locally Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part One PART 1 PART 2 2 PART 3 Contents Part One 1. Message from the Chair 2. Foreword by the Chief Executive 3. Statement from the Director of Nursing and Quality 4.Our vision, our strategic priorities and our services 3 4 3. 5 4. 6 Part Two 1. 2. Priorities for improvement 2015/16 1.1 Quality Goals 1.2 Commissioning for Quality and Innovation (CQuIN) 1.3 Integration programme 1.4 Transformation programme Mandated statements of assurance 2.1 Review of services 2.2 Participation in clinical audit 2.3 Participation in clinical research 2.4 Goals agreed with commissioners 2.5 Statement from Care Quality Commission (CQC) 2.6 Data quality 2.7 Information Governance toolkit attainment levels 2.8 Clinical coding error rates 2.9 Core Quality Account Indicators 8 9 11 11 12 14 16 17 17 19 20 20 21 Part Three 1. Review of quality performance in 2014/15 1.1Summary/Introduction 1.2 Care Quality Commission (CQC) Inspection 1.3 Service developments 1.4 Transformation programme 1.5 Achievement of our Quality Goals 1.6 Commissioning for Quality Innovation (CQuIN) 2. A Well-led organisation 2.1Introduction 2.2 Student Nurses 2.3 National Apprenticeship week 2.4 Staff Achievements 2.5 NHS Staff survey 2014 5. 6. 22 22 24 26 27 7. 28 29 29 30 30 31 8. 2.6 Health & wellbeing at work 2.7 Compliments and thanks 2.8 Clinical Ethics Group 32 33 34 Responsive services 3.1 Review of Quality performance for 2014/15 35 Caring services (Patient Experience) 4.1Summary 4.2 Patient and carer involvement 4.3 Patient voice at Board 4.4 Friends and Family Test 4.5 Patient Opinion 4.6 Local patient surveys 4.7 Complaints and compliments 4.8 Patient led assessment of the care environment (PLACE) 38 39 39 41 42 43 43 44 Safe services 5.1Introduction 5.2 Safe staffing 5.3 Being Open (duty of candour) 5.4 Norfolk Harm free care project 5.5 National Safety Thermometer 5.6 Management and learning from incidents 5.7 Mortality panel review 5.8 Never Events 5.9 Central Alerts 5.10Infection prevention and control 5.11Medicines management 5.12Safeguarding children and adults 46 46 47 48 49 50 52 52 52 52 55 56 Effective services 6.1Introduction 6.2 Implementation of NICE guidance 6.3 Clinical Audit programme 6.4 Trust Research Performance 6.5 Specialist Palliative Care 58 59 62 64 65 Explanation of who has been involved in this Quality Account 7.1Introduction 7.2 Norwich Clinical Commissioning Group 7.3 Healthwatch Norfolk 7.4 Norfolk Health Overview and Scrutiny Committee 66 67 68 68 Directors’ Declarations69 Glossary of terms 70 Part One Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part One PART 1 PART 2 3 PART 3 1. Message from the Chair Community. Compassion. Creativity. These are the three values we developed with our staff and public during 2014/15, and they are central to how we approach delivering excellent care closer to home for our patients. This is what we mean by creativity. Finding clever ways to improve the care we provide for the communities we serve as cost-effectively as possible. As the new Chief Executive of NHS England, Simon Stevens, has advocated, we really do need to “think like a patient, act like a taxpayer.” This year also saw us embrace the need to integrate health with social care through the development of an integrated management team with Norfolk County Council’s Adult Social Services. Our new values are the high cultural standards we set for ourselves and, on behalf of the Board of Norfolk Community Health and Care NHS Trust, I am pleased to report in our Quality Account for 2014/15 that we are living up to those values. In terms of community, we continue to look after the needs of a population of 882,000 across Norfolk, and we also started to provide services in Suffolk. Building on our expertise in Norfolk with early supported discharge for people who have had strokes, we won a three year contract to provide similar services to stroke patients in Suffolk. The Care Quality Commission (CQC) inspected our services during the year and rated us as Good. That positive CQC rating reflects the care and dedication of our staff and highlights just how focused everyone is on delivering compassionate, high quality patient care. As an NHS community provider we have worked hard over the past year to develop creative ways of making our services more efficient. This does not simply mean saving money, but looking at how we can improve the care we provide for the communities we serve. Our Transformation programme has set out to help give our frontline NHS staff the tools they need to get the job done more effectively. Serving large rural and urban populations presents our staff with challenges in terms of the time they spend travelling between their work bases and their patients. The Transformation programme has seen us invest in information technology that allows our community nursing and therapy teams to update patient records, remotely and in real-time. This has increased their productive time by cutting down on the need to return to base to update records. The result? Time spent with patients has gone up to nearly 63 per cent. This is good for our patients and good for our staff. We also appointed our new Chief Executive, Roisin Fallon-Williams. Roisin has proved to be a real asset and has demonstrated her commitment to always do the very best for local people and patients, and our staff. Looking to the future, NHS England has presented its ‘Five Year Forward View’ and we can see the challenges and opportunities ahead. Meeting those challenges will not be easy but we are in a strong position, we are in charge of our destiny, and we remain committed to looking after you locally. Ken Applegate Chair Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part One PART 1 PART 2 4 PART 3 2. Foreword by the Chief Executive Although I only joined Norfolk Community Health and Care NHS Trust (NCH&C) in the autumn, I am fully aware of all of the excellent work that has been taking place across the Trust. I have been impressed by the way colleagues embrace our vision to improve the quality of people’s lives, in their homes and in the community through the best in integrated health and social care. The theme of integration will be a defining one for us in the year ahead. Work on our integration with Norfolk County Council’s Adult Social Services teams has taken significant strides forward, with a new integrated care management structure in place and bedding in. In the autumn, NHS England’s Chief Executive Simon Stevens unveiled his vision for the future through the publication of the ‘Five Year Forward View’ which looks towards a breaking down of boundaries between primary care and hospitals, between physical and mental health, and between health and social care. It means developing models of care built around the needs of patients rather than on historical or professional divides. At NCH&C this is music to our ears and we need to act now, with our partners in both health and social care, to respond with local flexibility and innovation. It really is up to us to embrace the integration agenda and make it work for our patients and our staff. There will be those that say integration is just the latest buzzword. At a recent Board meeting, however, we heard from frontline colleagues in our Learning Disability service in east Norfolk about the many benefits they felt had been delivered for service users through the integration of health and social care staff around ten years ago. It is not an easy thing to do and it doesn’t happen overnight, but they were very clear about the benefits of working side by side. This year, we also expanded our geographical boundary with the launch of a new Early Supported Discharge service in Suffolk, to allow patients who have had a stroke to return home from acute hospital faster and receive specialist rehabilitation in their own homes. This type of service is all about working across organisational boundaries and focusing on the needs of the patients. Financial stability is the other major challenge facing every NHS organisation. Although we are in relatively good financial shape, delivering our cost improvement programmes will be a major challenge, and we will work hard to not compromise on quality and safety in the delivery of care to patients. I would like to thank everyone for their part in helping us to deliver a service to the people in Norfolk and Suffolk, which is focused on providing safe and effective care while offering a consistent and positive experience to those who use our services. Roisin Fallon-Williams Chief Executive Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part One PART 1 PART 2 5 PART 3 3. Statement from the Director of Nursing and Quality The care, commitment and compassion of our frontline staff have made possible the continued success of our quality achievements contained within this Quality Account. I am proud of all our staff for the valuable work they do every day. We know that nationally the pressures and demands for services are high across health and social care systems; despite this we know that our patients are safe in our care. The Care Quality Commission (CQC) found that our services were caring across the board. Our staff spoke with compassion, dignity and respect regarding the patients that they cared for, and all services inspected demonstrated compassionate care. Looking back over the last year, our staff have involved themselves actively and positively in the many challenges we have developed to transform the way that services are delivered to our patients. Our staff have supported new projects such as the Virtual Wards, extra winter beds, and the intravenous therapy team in the central localities. In addition, our staff have driven the expansion of our Children’s Community Nursing Team and redesign of School Nursing and Health Visiting. I am also pleased to report colleagues have supported the increase in the numbers of students in practice and have piloted new models of support, such as Collaborative Learning in Practice where students are enabled to have greater responsibility of care under the supervision of our experienced staff. Looking forward to the coming year, we will be implementing the new Nursing and Midwifery Council ‘Code of Practice’ for Nurses to ensure they are meeting the required standards. We will also take forward the recommendations from Lord Willis’s ‘Raising the Bar’ report which looks at the way that we support, educate and train our staff to ensure that we are continuing to provide a world class health and care workforce. Our staff remain the key to successful delivery of our services now and in the future. Anna Morgan Director of Nursing and Quality Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part One PART 1 PART 2 PART 3 4. Our vision, our strategic objectives and values 4.1 Our vision 4.2 Our strategic objectives Our vision is to ‘improve the quality of people’s lives, in their homes and community by providing the best in integrated health and social care’. We often sum this up as ‘Looking after you locally’. Improving OUR QUALITY through… The starting point for us is the patient: this means that quality is at the heart of everything we do. Our services are built up around the patient, working closely with GP partners both as commissioners and providers. Wherever possible, our services are delivered in an integrated way with social care. We are therefore part of an extended primary care team focused around the patient. The patient should experience care as if it were from one organisation, seeing the least number of staff necessary and not having to repeatedly tell their story. NCH&C aims to lead out of hospital community healthcare, giving children a better start and adults greater independence - we typically do so in their own home or place of choosing. This, combined with the fact that we are a major employer and operate from multiple sites, means that we are both in and of the community. Our staff are drawn from local communities and have local knowledge. We want to work with communities, not just serving their needs, but recognising that we have a role to empower communities to make the most of the resources within them. Our vision will be delivered through the achievement of a number of longer term, strategic objectives. The Board has agreed three interconnected and mutually dependent strategic priorities to achieve the Trust’s vision. Delivering our vision and quality goals can only be achieved by having a well-informed, engaged workforce which understands, and is motivated to help us deliver, our strategic objectives. • D elivering harm free, clinically effective and compassionate care • Involving patients and the public and delivering excellent patient experience Enabling OUR PEOPLE through… • Inspiring staff and staff engagement • Empowering staff to speak out and put things right • Ensuring the right staff, with the right skills are available to deliver compassionate care • Integrating delivery with social and primary care and having effective partnerships with other organisations • Transforming services • Demonstrating effective leadership Securing OUR FUTURE through… • Delivering what commissioners require • Delivering a financially sustainable organisation • Investing in infrastructure • Growth 6 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part One PART 1 PART 2 7 PART 3 4.3 Our values Our values have formed a behavioural framework for our staff in how they treat our patients and each other, and are the foundation to our delivering our strategic objectives. These values will underpin all communication principles for our Trust, forming the backbone of our key messages. Everything we communicate will have a clear association with one or more of our values. Community • As a Trust, we enhance the lives of our patients through our commitment, support and education • We are proud to serve our local community by providing integrated quality services with our partner organisations • We respect and value the trust we are given to enter our patients’ homes and lives Compassion • We provide compassionate, coordinated and personalised quality care that is safe and effective • We empower and educate our patients and their carers in the effective delivery and management of their own independence, health and wellbeing • We are dedicated to holistic, compassionate care and demonstrate this through our commitment to our personal and professional development Creativity • Our expertise, commitment and creativity are key to the successful delivery of our services • We are always open to new ideas that support us in delivering effective, compassionate care to our patients • We continuously innovate and implement efficient delivery of care The diagram above shows how our objectives and values are integrated with each other and wrap around our patients Part Two Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 8 PART 3 1. Priorities for improvement 2015/16 1.1 Quality Goals High quality care means care that is as safe and effective as possible, where patients are in control and are treated with compassion, dignity and respect; their experience of care being as important as the outcomes of care. High quality care also means focusing on the prevention of illness. We believe that everyone within NCH&C has a role to play in supporting this ethos – this is not just about clinical staff and how they care for patients. Administrative and support staff are also able to contribute in a number of ways – simple things like answering a phone for a colleague can make a real difference. The three domains of high quality care are defined nationally as being: 1.Patient Safety: The first dimension of quality must be that we do no harm to patients. This means ensuring that the environment is safe and clean, and reducing avoidable harm such as drug errors. 2.Patient Experience: Quality of care includes the quality of caring. This means how personal care is – the compassion, dignity and respect with which patients are treated. This can be improved by analysing and understanding patient satisfaction levels and experience. 3.Effectiveness of Care: This means understanding the success rates of different treatments for different conditions. Assessing this will include clinical measures such as mortality or survival rates, complication rates and measures of clinical improvement. Just as important is the effectiveness of care from the patient’s own perspective. Examples include improvement in pain scores or returning to work after treatment. Clinical effectiveness may also extend to people’s well-being and ability to live independent lives. In order to support high quality care, each year we focus on key Quality Goals. These goals are intended to inform the practice of each member of staff across all three domains of quality. After consultation with staff, patients and the wider public we have developed the following goals for 2015/16. At this stage, the goals are of a strategic nature, and it is expected that local teams will identify what each goal means for them and their practice. The Quality Goals have been set under the same headings. They are: 1.Safe services (harm free care): This domain includes actions focussing on the safety thermometer, falls causing harm in our inpatient units, pressure ulcers, VTEs, catheter acquired infections, effective use of medicines, and increasing the percentage of patients receiving harm free care. 2.Clinically effective services: This domain looks at improving clinical effectiveness and demonstrating improvement through the clinical audit programme for 2015/16. It also includes focus on NICE guidance and the quality standard for Dementia. 3.Patient experience and involvement: This domain seeks to increase the involvement of patients, their families and carers in how services are delivered and improved. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 1.2 Commissioning for Quality and Innovation (CQuIN) 2015/16 CQuIN indicators are contractual commitments, some are nationally mandated and some are developed in partnership with our various commissioners. They are intended to improve quality and encourage innovation within key areas of local services. If these indicators are achieved, they attract additional funding that can be used to make further improvements. The CQuIN indicators for 2015/16 that have been negotiated and agreed with our commissioners are as follows; 1.2.1 National Indicator - Dementia a.Find, assess, investigate, refer and inform b.Dementia training for staff c. Dementia support for carers 1.2.2 End of Life Care (a Pan-Norfolk indicator) To ensure the priorities of care of ‘One Chance to Get it Right’ correlate with the 16 Quality Statements and are implemented throughout the community and inpatient units. 1.2.3 Patient Self-Administration of Clexane (west Norfolk CCG) Clexane is a brand name for a medicine used to treat a number of conditions; angina, blood clotting, heart attack To develop a pathway to promote the selfadministration of Clexane injections by a designated cohort of patients in the community setting. Pre-elective surgery patients as part of their postoperative community care would be given the choice to self-administer their Clexane. As part of this pathway the patient would also have the option of a relative/ carer to administer the Clexane. PART 2 9 PART 3 1.2.4 ‘Your Village’ Improved Collaboration and Integration (Norwich CCG) To adopt the traditional ‘Village Style’ District Nursing approach through collaborative and integrated working with Primary Care, Third Sector Providers and Voluntary/ Community Sectors. To align current and existing services with the ambitions and objectives of the ‘Your Norwich Programme’. The scheme is designed to facilitate working together in four city clusters and to provide improved communication and integration with Primary Care and other local services, such as Care Homes. 1.2.5 Lower Limb Care & Management (North Norfolk CCG) To create a responsive and integrated local service for the Care & Management of Lower Limb Ulcers, including those identified as a Diabetic Foot Ulcer. This will enable a greater patient choice within the locality and will develop and retain the skill and competency of all involved. To ensure that all patients presenting with a lower limb ulcer receive a timely holistic assessment and accurate diagnosis by a healthcare professional trained in lower limb care and management, in order to achieve improved healing times. To ensure all staff that are responsible for lower limb management are competent in the management of these patients including the application of compression bandages and hosiery. 1.2.6 Improved Integration – Supporting Independence for Older People (South Norfolk CCG) To improve relationships and promote a culture of continuous improvement in the multi-disciplinary teams in order to maximise independence and decrease avoidable admissions for the most vulnerable patients. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 1.2.7 In-reach into acute hospital for amputees (Great Yarmouth & Waveney CCG) To enable patients to meet with a key member of the Pine Cottage clinical team prior to their discharge from the acute hospital. It is aimed at providing information to patients, giving them the opportunity to ask questions, provide reassurance and empowering patients to take part in decision making around their rehabilitation at a much earlier stage. 1.2.8 Prosthetics Service (NHS England Specialist commissioning) To ensure patients are triaged within four weeks and a multi-disciplinary team meeting is held within six weeks of receipt of referral. 1.2.9 Environmental controls (NHS England Specialist commissioning) Provision of training for stakeholders and staff. PART 2 10 PART 3 1.2.10 Child Health information systems; Newborn and Infant Physical Examination (NIPE) 72 hour (NHS England) NIPE 72 hour screening information to be shared by maternity services and recorded onto SystmOne (electronic patient record system) by the Community Health information systems team. 1.2.11 Suffolk Early Supported Discharge (Ipswich and East Suffolk CCG) Support and training for carers of service users. To improve the quality of life and carer experience of people who care for patients who have had a stroke. 1.2.12 Admission avoidance – (North Norfolk CCG) Reducing the proportion of avoidable emergency admissions to hospital. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 11 PART 3 1.3 Integration programme for 2015/16 1.4 Transformation programme for 2015/16 In November 2014, a Section 75 Agreement was signed between Norfolk County Council and NCH&C providing the architecture for integrated working. On two days in January 2015, approximately 100 staff came together to debate and design what Sustainable Models of Care could be for NCH&C. Delegates from operational and support services were joined by external observers from HealthWatch and commissioning organisations to consider five themes: frail elderly pathway, end of life care, musculo-skeletel services, children’s services, and specialist services. This builds on a long history of joint working between the two organisations, via joint Learning Disability (LD) teams for some years, participation in the Integrated Care Organisation pilots and more recently the Integrated Management Structure in the West. We now have a totally Integrated Senior Management Structure, with a Director of Integrated Care, Deputy, four Assistant Directors and four Heads of Integration. These managers have a joint and equal responsibility for both Health and Social Care Adult Services. We are now moving to Phase 2 for the Integration Pathway during 2015. We will further integrate functions and pathways where it makes sense. Work streams will include: • Single point of access • IT arrangements • Joint Care Plan • Generic worker We aim to achieve a more seamless service for the person receiving our services, and a more efficient and cost effective way of working. We will also include other partners as we progress. Roisin Fallon-Williams, Chief Executive, launched the events by describing the quality of services and the scale of the financial challenge – the need to make cost improvement savings of £12.7 million over the next two years. The groups were asked to consider what services should look like in the future to ensure that they were clinically and financially sustainable. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 12 PART 3 2. Mandated statements of assurance 2.1 Review of services During the period April 2014 to March 2015, NCH&C held contracts for 64 service specifications, covering 33 broad service areas as follows: Community Nursing Smoking Cessation Admission Avoidance Dental Services Rehabilitation Adult Learning Disabilities Palliative and End of Life Care Health Visiting Service Long Term Conditions Management School Nursing Musculoskeletal Services SureStart Care Management Children’s Community Nursing Specialist Neuro- rehabilitation Children’s Therapies Stroke Rehabilitation Community Paediatrics Amputee and post surgical rehabilitation Children’s Short Breaks ‘Hard to reach’ Community Care Clinical Support Services Diagnostics Norfolk Early Supported Discharge Adult Speech & Language Therapy Suffolk Early Supported Discharge Podiatry Environmental Controls Podiatric Surgery Rapid Assessment Team Wheelchair Assessment IPAC Liaison Nurse Continence NCH&C has reviewed all the data available to them on the quality of the care in all of these NHS services. The income generated by the NHS services reviewed in 2014/15 represents 100% of the total income generated from the provision of NHS services by NCH&C for 2014/15. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 Narrative The Trust Board receives a monthly Integrated Performance Report (IPR), which focuses on a number of domains, including patient experience, safety, quality and risk. The data is presented in a dashboard format, using Red-Amber-Green (RAG) ratings to highlight any areas of adverse performance against agreed targets, standards and thresholds, and is supported by a narrative explaining the reason for the variance, and actions being taken to mitigate future risks impacting on performance. The Board also receives a monthly Quality Assurance and Risk report which provides more operational detail and context on those areas reported in the IPR. This report is also presented to the Quality and Risk Assurance Committee, and includes the following areas: • Serious Incidents Requiring Investigation (SIRIs) • Medication Incidents • Falls causing harm • National Safety Thermometer data • Pressure Ulcers • Infection rates • Patient Experience surveys (including the Friends and Family Test and Patient Opinion) • Complaints and compliments • Results of external scrutiny (e.g., Care Quality Commission, National Patient Safety Agency) • Quality assurance assessments • Corporate risk register PART 2 13 PART 3 Aspirant community foundation trust benchmarking report NCH&C is part of a group of 13 community trusts who have agreed to share data in order to benchmark performance against one another to stimulate debate and identify opportunities for sharing best practice. This monthly report includes a number of patient safety and quality indicators, as well as other finance and performance measures. Cost improvement plan quality indicator assessment dashboard A Cost Improvement Plan Quality Indicator Assessment (CIP QIA) dashboard has been developed to highlight to the Quality and Risk Assurance Committee, Trust-wide quality indicators and standards that can be tracked over time. The indicators presented are at an aggregate Trustwide level, and they can be found within a number of individual schemes. Thus, they are intended to highlight where a quality issue may be emerging, which will enable drill down to a specific scheme, area or locality. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 PART 3 2.2 Participation in clinical audit During that period, NCH&C participated in 100% of national clinical audits which it was eligible to participate in. During April 2014 to March 2015, 2 national clinical audits and 0 confidential enquiries covered NHS services that NCH&C provides. The national clinical audits that NCH&C was eligible to participate in during April 2014 to March 2015 are as follows: Name of National Audit Lead Organisation Included participation from NCH&C? National Audit of Intermediate Care NHS Benchmarking Network Yes Sentinel Stroke National Audit Programme (SSNAP) Royal College of Physicians (London) Yes Title of National Confidential Enquiry Applicable to NCH&C? Included participation from NCH&C? None applicable n/a n/a The national clinical audits that NCH&C participated in, and for which data collection was completed during April 2014 to March 2015, are listed below alongside the number of cases submitted to each audit or enquiry as a percentage of the number of registered cases required by the terms of that audit or enquiry. Name Lead Organisation Percentage National Audit of Intermediate Care NHS Benchmarking Network 100% Sentinel Stroke National Audit Programme (SSNAP) Royal College of Physicians (London) n/a 14 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 15 PART 3 The reports of five national clinical audits were reviewed by the provider April 2014 to March 2015, and NCH&C intends to take the following actions to improve the quality of healthcare provided: Name Lead Organisation Actions National Audit of Intermediate Care 2014 NHS Benchmarking Network None Sentinel Stroke National Audit Programme (SSNAP) – Fourth Report May 2014 / Acute Organisation Report December 2014 Royal College of Physicians (London) Continue to review Early Supported Discharge service and stroke ward against relevant NICE guidance and support participation in SSNAP audit National care of the dying audit for hospitals, England May 2014 Royal College of Physicians (RCP) / Marie Curie Palliative Care Institute Liverpool (MCPCIL) Review Trust services against NICE end of life quality standard National COPD Audit Programme November 2014 / February 2015 Royal College of Physicians None National Diabetes Audit 2012–2013 Report 2: Complications and Mortality Diabetes UK None 2.2.1 Local clinical audits The reports of 40 local clinical audits were reviewed by the provider during the period from April 2014 to March 2015, and NCH&C intends to take the following actions to improve the quality of healthcare provided. • Improve written information available for patients and families about ‘do not attempt cardio-pulmonary resuscitation’ orders • Increase the use of pressure ulcer prevention plans • Introduce a ‘named nurse for the day’ notice by the entrance of each patient room on the stroke ward • Ensure that patients with Parkinson’s disease have an opportunity to discuss end of life preferences and concerns • Enhance the depth and breadth of information contained in child protection referrals • Offer more Chronic Obstructive Pulmonary Disorder (COPD) patients the opportunity to use self-management plans • Continue the process of reducing the use of abbreviations in clinical records • Introduce the ‘activities of daily living’ assessment as a measure of rehabilitation progress in the STEPS service • Revise and improve the Trust’s pain assessment tool • Revise the Trust’s assessment process for Dysphagia to meet new national guidance • Extend the roll-out of the new referral process for patients with memory problems for dementia assessment Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 2.3 Participation in clinical research The number of patients receiving NHS services provided, or sub-contracted, by NCH&C in 2014/15 who were recruited during that period to participate in research approved by a research ethics committee, was 427 (compared with 453 in 2013/14). Participation in clinical research demonstrates NCH&C’s commitment to improving the quality of care we offer and to making our contribution to wider health improvement. We have developed further infrastructure within the Trust over the last 12 months to allow easier access for staff and patients to research, and will continue to take these forward into 2015/16. We were involved in 55 research studies during 2014/15, similar to last year; this includes 17 studies that were new in 2014/15 and 38 ongoing from previous years. The National Institute for Health Research (NIHR) supported 58% of these studies through its research networks. Throughout 2014/15 we have taken steps to embed research as core Trust activity and encouraged staff to engage with local clinical research networks. The Trust has recently opened a dedicated clinical research room and trained dedicated research nurses to support the delivery of research within the Trust. The Trust’s first Research Conference was held in September 2014 and feedback was overwhelmingly positive, particularly for the emphasis on networking and linking together interested individuals. The Trust is actively engaging with the new Clinical Research Network (Eastern), and NCH&C has been selected as a pilot site for the introduction of research patient ambassadors. PART 2 16 PART 3 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 2.4 Goals agreed with commissioners Use of the Commissioning for Quality and Innovation (CQuIN) payment framework A proportion of NCH&C’s income for April 2014 and March 2015 was conditional on achieving quality improvement and innovation goals agreed between NCH&C and any person or body that we entered into a contract, agreement or arrangement with for the provision of NHS services, through the CQuIN payment framework. Details of NCH&C’s achievements against the agreed CQuIN indicators for April 2014 to March 2015 are set out in Part 3, section 1.6. The CQuIN indicators agreed with our commissioners for the forthcoming year (April 2015 - March 2016) can be found in Part 2, Section 1.2. PART 2 17 PART 3 2.5 Statement from the Care Quality Commission (CQC) NCH&C is required to register with the CQC and its current registration certificate issued on 25th February 2014, confirms that the Trust is registered to provide the following Regulated Activities: 1. Assessment or medical treatment for persons detained under the Mental Health Act 1983 2. Diagnostic and screening procedures 3. Family planning 4. Surgical procedures 5. Treatment of disease, disorder or injury 6. Personal care The only conditions of registration are that these regulated activities may only be provided from the following registered locations: Registered Locations Regulated Activity (see above) Cranmer House 1, 2, 5 Little Acorns (Children’s respite) 5 Mill Lodge (Adult respite) 5 Provider Services HQ 1, 2, 3, 5, 6 Squirrels (Children’s respite) 5 Benjamin Court 1, 2, 5 Colman Hospital 1, 2, 5 Dereham Hospital 1, 2, 5 Kelling Hospital 1, 2, 5 North Walsham Hospital 1, 2, 5 Norwich Community Hospital 1, 2, 4, 5 Ogden Court 1, 2, 5 Swaffham Community Hospital 1, 2, 5 The CQC has not taken enforcement actions against NCH&C during the period April 2014 to March 2015. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 2.5.1 Inspections by the CQC Mill Lodge, (Adult respite), Taverham (RY3X4) was inspected by the CQC in June 2014, and the following standards were assessed as being met: • Consent to care and treatment PART 2 18 PART 3 All NCH&C’s services were inspected in September 2014 as part of the second pilot phase of the new inspection process CQC introduced for community health services. Please refer to Part 3, section 1.2, Responsive services, for further details. The Trust received an overall rating of GOOD broken down as below: • Care and welfare of people who use services • Safety and suitability of premises • Staffing • Assessing and monitoring the quality of service provision NCH&C OVERALL RATING Overall rating Safe Caring Effective Responsive Well-led GOOD Requires Improvement GOOD GOOD GOOD GOOD The CQC identified three ‘Must do’s’ which the Trust were required to address, these were: 1.Regulation 18 Consent to care and treatment The Trust MUST ensure all clinical staff understand how the Mental Capacity Act applies to their work and develop a mechanism to monitor compliance of the MCA. These actions, which relate to mental capacity, are all complete. However it is recognised that this area requires ongoing training especially as it also relates to Deprivation of Liberty Safeguards (DOLS) and the implementation of new guidance, as it becomes available. 2.Regulation 13 Management of Medicines The Trust MUST carry out a review of medicines management to ensure there are suitable arrangements in place to safely manage medicines. All these actions have been completed which included; updating standard operating procedures, undertaking local audits and the negotiation of a new pharmacy service level agreement with a partner provider. 3.Regulation 9 Care and Welfare of people who use services - The Trust MUST ensure that all patients have a clear care plan in place which takes account of their individual needs and ensures their welfare and safety. An initial review of all inpatient care plans and audit was completed immediately. The current assessment tool has been modified to underpin a personalised care plan. The welcome pack has been updated to use a standardised key message regarding individualised care planning. These actions are all complete. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 2.6 Data quality High quality information underpins the effective and safe delivery of patient care and is key if improvements in quality of care are to be made. Improving data quality, which includes the quality of demographic, ethnicity and other equality data, should improve patient care and improve value for money. PART 2 19 PART 3 2.6.1 NHS Number and General Medical Practice Code Validity NCH&C submitted records during 2014/15 to the Secondary Use System (SUS) for inclusion in the Hospital Episode Statistics (HES) which are included in the latest published data under the organisation code RY3. The percentage of records in the published data which: NCH&C is taking the following actions to improve data quality: (i) Included the patient’s valid NHS number was: 100% for admitted patient care (APC) • A range of data quality reports have been designed to monitor a range of key performance indicators on a weekly and monthly basis (ii) Included the patient’s valid General Medical Practice code was: 100% for (APC) • The Secondary Uses Service (SUS) dashboards are reviewed regularly in relation to a number of national key indicators • A selection of these indicators are also reported to the Data Quality Forum, where operational services are held to account for the quality of data held on the Patient Administration System (PAS) and SystmOne (electronic patient record) • These reports are held on a networked drive and can also be viewed on an Intranet portal to ensure they are accessible to key staff involved in the monitoring and reporting of performance and activity data The Trust has a Data Quality Strategy which will be critical to a number of the Trust’s priorities and objectives, including improving the quality of patient care, compliance with the NHS Information Governance (IG) Toolkit version 11 for 2014/15 and the need to monitor the Community Information Data Set (CIDS). This strategy is underpinned by a Data Quality policy which is subject to annual review. The purpose of this policy is to ensure the highest standards of data quality throughout NCH&C are achieved and maintained. This policy is for all staff collecting and using data and they must adhere to the local and national standards as laid out. The Trust has an internal audit on data quality carried out each year by PricewaterhouseCoopers. The report for 2014-15 returned a Low Risk opinion. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 20 PART 3 2.7 Information Governance 2.8 Clinical coding error rate Toolkit attainment levels NCH&C was not subject to the Payment by Results (PbR) On March 31, 2015, the Trust declared overall compliance at Level 2 against 26 of the 38 requirements of the 2014/15 Information Governance Toolkit (IGT) v12, and the Board noted the Level 3 progress in the submission of the IGT v12 for 2014/15. The remaining 12 requirements are maintained at Level 3 which gives the Trust’s overall score as 76%. clinical coding audit during 2014/15. Evidence has been submitted to cover the following six areas where assurance is required: • Information Governance management • Confidentiality and Data Protection • Information Security • Clinical Information • Secondary User Information • Corporate Information The Information Governance Toolkit is available on the Connecting for Health website: (www.igt.connectingforhealth.nhs.uk) The Information Quality and Records Management attainment levels assessed within the Information Governance Toolkit provide an overall measure of the quality of data systems, standards and processes within an organisation. Assessment Stage Level 0 Level 1 Level 2 Level 3 Not Relevant Total Req’ts Overall Score Self-assessed Grade Version 12 (2014-2015) Final 0 0 26 12 [1] 38 76% Satisfactory Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Two PART 1 PART 2 21 PART 3 2.9 The Core Quality Account indicators Prescribed Information Related NHS Outcomes Framework domain and who will report on them Data / output The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the percentage of patients aged; 3: Helping people to recover from episodes of ill health or following injury NCH&C considers that this data is as described for the following reasons: All trusts NCH&C does not re-admit patients aged 16 or over following discharge. All admissions to the Trust’s beds are received from acute trusts or from the patient’s usual place of residence 5: Treating and caring for people in a safe environment and protecting them from avoidable harm. NCH&C considers that this data is as described for the following reasons: (i) 0 to 15; and (ii) 16 or over, readmitted to a hospital which forms part of the trust within 28 days of being discharged from a hospital which forms part of the trust during the reporting period The data made available to the National Health Service trust or NHS foundation trust by the Health and Social Care Information Centre with regard to the number and, where available, rate of patient safety incidents reported within the trust during the reporting period, and the numbers and percentage of such patient safety incidents that resulted avoidable harm in severe harm or death All trusts Table 1 below; represents the rate of patient safety incidents reported against the number of face-to-face contacts with patients, expressed as a rate per 1,000 Number of patient safety incidents 2014/15 Harm 2014 Apr 2014 May 2014 Jun 2014 July 2014 Aug 2014 Sept 2014 Oct 2014 Nov 2014 Dec 2015 Jan 2015 Feb 2015 Mar Total No 193 253 262 269 251 217 295 276 279 255 225 198 2973 Low 277 330 306 312 296 292 315 289 313 352 297 288 3667 Moderate 78 100 78 90 85 106 90 110 98 119 104 84 1142 Severe 2 6 5 5 4 8 4 3 5 5 2 2 51 Unexpected 0 Death 1 0 0 0 0 1 0 1 1 1 1 6 Total 690 651 676 636 623 705 678 696 732 629 573 7839 7.2 7.5 7.5 7.1 8.6 7.0 550 Total incidents in clinical areas per 1,000 patient contacts 5.6 7.3 6.9 6.7 7.2 6.5 6.9 Part Three Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 22 PART 3 1. Review of quality performance in 2014/15 1.1 Summary/Introduction ‘Quality is at the heart of everything we do’ and this is demonstrated throughout the organisation across all services. We have measurably improved the quality of our services in 2014/15, delivering better health outcomes, high standards of safety, leading to excellent patient experience and more patient involvement. This was in line with our Quality Improvement Strategy 2014/16 and confirmed by our CQC inspection in September 2014. 1.2 The Care Quality Commission Inspection In September 2014, NCH&C underwent one of the ‘new style’ CQC inspections of all its services under the following headings; • Community Dental • Adult inpatients • Community Adults services • Children, young people and families • End of life care The Trust is incredibly proud of its overall GOOD rating which was broken down as follows; NCH&C Overall rating Overall rating Safe Caring Effective Well-led GOOD Requires improvement GOOD GOOD GOOD Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 23 PART 3 NCH&C was encouraged by the positive feedback received by the CQC and this outcome supports the view that ‘Quality Counts’ at the Trust. The results will inform an improvement plan to ensure that the Trust is able to provide assurance of the safety and quality of its services. We welcome the opportunity the inspection finding presents for learning, and intend to ensure improvements are made. The three compliance actions were all completed by the end of February 2015 with a new pharmacy service level agreement being agreed and signed with a partner provider by the end of March 2015 (see Part 2, section 2.5.1, Inspections by the CQC, for more information). • The care and compassion shown to patients by staff in all of the areas inspected A number of ‘should do’s’ were also identified and the top 5 actions include the following; 1.Refurbishment of Squirrels Children’s Respite Centre (completed 11/12/14) 2.Continue the action already in place to improve the recruitment process and staffing levels in all of the services (comprehensive analysis and planning continues and wider system approach is in place) 3.Carry out a risk assessment of faith leaders who have not been subject to Disclosure and Barring Service (DBS) checks (the chaplaincy provision has been reviewed and confirmed that all employed by NCH&C have DBS checks in place). All other multi-faith leads that we use have had DBS checks undertaken by their employing organisation 4.Increase the number of nursing staff who participate in clinical supervision (a policy on a page has been developed and launched, and master classes for ‘train the trainer’ are being rolled out) 5.Review clinical leadership within inpatient settings and ensure all clinical leaders have opportunities for leadership development programmes. In addition to our current leader development programme REAL, the Trust is working with the Trust Development Authority and the Leadership Academy to devise a new programme for ward managers The following are highlights of good practice identified by the CQC; • Our Trust’s mortality review process was a proactive initiative for a community service • The level of multi-disciplinary and multi-agency team working within the end of life and children’s service was exceptionally good • A ‘silver call’ daily multi-agency discharge planning teleconference had been introduced in the West Locality which promoted patient discharges at the earliest stage possible • A daily capacity reporting tool had been developed which enabled managers to have an ‘at a glance’ overview of the staffing pressure points with the ability to divert resources where they were needed most • An outstanding approach to the development of pathways within the school nursing team based on NICE guidance • The Starfish plus team was an excellent example of a responsive service • The ability of the community dental service to adapt care and treatment in order to meet people’s individual needs • We are an integrated provider of health and social care with an agreed joint management structure with Norfolk County Council Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 1.3 Service Developments 1.3.1 Urgent Care Centre (UCC) The UCC commenced at the end of October 2014 as a joint Clinical Commissioning Group (CCG), two year funded project involving NCH&C, the Norfolk and Norwich University Hospital (NNUH), Norfolk and Suffolk NHS Trust, Norwich Practices Limited, Norfolk County Council and Norfolk First Response. As the project involves NNUH premises and facilities NCH&C agreed to their leading the project. We are providing a therapy and nurse-led Early Intervention team who are assessing acute frail elderly arrivals in the Accident & Emergency (A&E) department at the same time as the patients are medically assessed. This pattern of working on the pilot scheme in 2013 resulted in the discharge of an additional patient daily compared with previous efforts. The additional 30 patients a month whose admissions were avoided do make a significant impact on admission numbers over a year. Providing a care assistant led discharge car also aids prompt and safe return home for patients when needed. We also provide nursing oversight of the centre and support to the GP along with triage of cases presenting in A&E to the centre with experienced community nurses. Norwich practices are providing GP cover, and we now have a mental health multidisciplinary team in place and more social work support to the benefit of the UCC and A&E combined. We are seeing over 30 patients daily – around 10-12% of the A&E workload and are pleased that we have had no four hour breaches despite some quite complex cases. PART 2 24 PART 3 1.3.2Hospital care at home service (Virtual Ward) The hospital care at home service (Virtual Ward) was recommended for continuation of funding at the West System Resilience Group. All agencies supported the proposal, so the service will now continue with a 20 bed capacity. The highlights for February 2015 were; • 113 patients were admitted in February. 28 were admitted from the community and 85 were admitted from the Queen Elizabeth Hospital • Average length of stay was 5 days (target is maximum 6 days) • Occupancy was 112% (relates to timings and number of discharges in a day) • 7 patients were readmitted from the hospital care at home service to QEH during February. 1 community patient was admitted to QEH • Patient and carer feedback has been very positive. Friends and Family Test score 100% The Home Ward service in Norwich is undergoing redesign to offer an enhanced rapid response service and to provide community IV services in Norwich. The service has increased its referral pathways and now accepts referrals from case managers, community matrons, the A&D early intervention team, the community liaison team, Priscilla Bacon Lodge and the care at home team. The project team are currently working with Norfolk First Support (NFS) to enable a seamless transfer from the Home Ward to their service. In addition, they aim to offer a step-up pathway if NFS clients require extra nursing and therapy support to prevent admission to acute care. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 1.3.3Ensuring the best end of life care New measures are being introduced across the county to help ensure patients can receive joined–up care at the end of their lives. Following withdrawal of the Liverpool Care Pathway last year, we have revised our End of Life policy which explains how we have adopted five new priorities for care in line with the ‘one chance to get it right’ national guidance. In addition to the revised policy, new documentation will be rolled out to replace the ‘Yellow folder’ which our Trust was instrumental in helping to develop. This new pack gives patients the opportunity to complete an advance care plan and record their choices about their future care and place of death, as well as their preferences about resuscitation, if they wish. Its aim is to standardise the documentation used for all patients, regardless of where they live, to help GPs and health and social care staff to work across boundaries and provide the best possible end of life care in line with each individual’s wishes. PART 2 25 PART 3 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 1.4 Transformation programme PART 2 26 PART 3 1.4.1Hub and spoke working The Transformation programme is ambitious, involving large scale change, to deliver improved care for patients. This has been achieved by a clinical and systems re-design, by investing in technology and improving our efficiency. We have invested in staff capacity and capability, to ensure that they have the right tools to deliver excellent, quality care. Better deployment of staff and improved use of management information will also improve productivity and our competitiveness. A lot has been achieved, but there is still work to do in areas which will require continued support. We are also committed to learning lessons from the programme which will improve our efforts in the future. Transformation has reduced clinical time spent on administrative duties and greater recognition of admin and clinical roles... Kerry Jones, Locality Operational Manager, West Locality We have introduced a hub and spoke model for each locality. Clinical staff can drop in to any spoke to use the facilities, for handovers and to replenish stock. The hub has created a single point of contact for the locality and currently, Community Nursing and Therapy teams have transformed into this new way of working. The Continence Service and MSK service will also align to hubs. Mobile working has been developed in tandem with working on a hub and spoke basis. From the hub perspective, there has been a streamlining of processes and bringing them together in one location. This makes it easier to monitor and support the work that we do so that there can be an oversight of patient care. Working in hubs will standardise the processes that support all services. By centralising these people and processes, and channelling the work through a single point of referral we improve; • Consistency of working processes across the teams in all areas • Coordinated administrative cover to support that service in the event of sickness and absence • Consistent support for all services • Skills and information sharing £1.9m efficiencies created within Community Nursing and Therapy to date 716 152 Care Plans developed 99% staff trained in SystmOne Optimisation (Mar-Dec 2014) of our patients in CN&T, post Transformation, would recommend NCH&C to their friends and family (Dec 2014) 4 Recorded patient-facing time has increased from locality hubs have been created 36% to 62% and continues to rise 60 teams using eRostering 270+ engagement sessions held since January 2013 1100+ eBooks will have been issued to staff by March 2015 1270 Queries sent to the localities’ mailbox 95% of care recorded is entered within 24 hours with over 45% recorded in real time with patients (Jan 2015) 400+ people undertook core competency training Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 1.5 Achievement of our Quality Goals 2014/15 Our Quality Goals for 2014/15 covered key areas such as reducing falls and pressure ulcers, referral to treatment times, length of stay, clinical effectiveness and patient experience. These goals were developed following consultation with staff, patients and stakeholders and the wider public, and help to ensure that we deliver excellent harm free care. The goals were developed to tie into the CQC’s five quality domains of; safe, effective, caring, responsive to people’s needs and well-led. 1.5.1 Safe, (harm free care) • We increased the percentage of patients with harm free care (new harms only) throughout the year •We ensured that the number of falls causing harm to patients in our inpatient units were below national rates • We ensured that all patients were assessed for their risk of falling on admission to our inpatient units • We ensured that all inpatients received a pressure ulcer assessment using the Waterlow risk tool within six hours of admission • We worked hard to ensure that patients, in our inpatient units and in their own homes, did not acquire avoidable pressure ulcers and we continued to support and train all our staff in the prevention and management of pressure ulcers • We ensured that, where appropriate, patients in our inpatient units had a venous thromboembolism (VTE) risk assessment undertaken during their inpatient stay • We created a group to lead on a project to reduce the incidence of catheter acquired infections. The project to raise awareness and train staff on the prevention and management of catheter acquired infections continues into 2015/16 •W e worked to ensure the effective use of medicines by developing a medicines’ optimisation strategy, all patients’ medications are checked by a pharmacist on admission to our inpatient units, and we have raised staff awareness of the NCH&C medication formulary to increase the effectiveness of prescribing • We have worked with Community Children’s Services to ensure that all clinical staff receive safeguarding supervision in accordance with Trust policy PART 2 27 PART 3 1.5.2 Effective care • We have reviewed Trust services against key NICE Quality Standards including: Dementia; Stroke; VTE prevention; End of Life Care for Adults; and the Health and Wellbeing of Looked After Children and Young People • We have also included audits of NICE guidance into our annual clinical audit plan 1.5.3 Caring services We improved our Friends and Family Test score (how likely are patients to recommend our services) in both the inpatient units and community nursing and therapy teams. We also responded to all submissions provided by patients/public on to our Patient Opinion website. 1.5.4 Responsive to people’s needs We worked hard to ensure that our Trust and individual service performance was equal to, or above, the target for completed pathways. Nearly all patients referred to us commenced treatment within 18 weeks of referral. 1.5.5 Well Led • We implemented the ‘Friends and Family Test’ for staff (asking how likely staff are to recommend our organisation as a good place to work), we reviewed the results of the short staff surveys and took action to improve staff experience • We developed and instigated an Organisation Development Strategy, which included the revision of the staff behaviour framework to support our ‘Community’ organisational value and to embed a positive culture throughout the Trust • We implemented a strategy to improve our staff training compliance figures for mandatory and clinical subjects and have achieved our contractual targets • We reviewed and implemented the ‘Safe Staffing’ requirements in the inpatient units using the RCN ‘Safe Staffing for Older People Toolkit’ and created a discharge coordinator role to support patient discharges with positive results Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 1.6 Achievement of our Commissioning for Quality Innovation (CQuIN) indicators for 2014/15 5. Breastfeeding initiative – UNICEF 3 CQuIN indicators are contractual commitments, some are nationally mandated and some are developed in partnership with our commissioners. They are intended to improve quality and encourage innovation within key areas of local services. If these indicators are achieved they attract additional funding that can be used to make further improvements. The indicators for 2014/15 cover the three quality domains of patient experience, patient safety and clinical effectiveness. Achievements are summarised below; 7. Neurology 1. Staff Friends and Family Test To encourage and improve service delivery, and that all staff should have the opportunity to feedback their views on their organisation. 2. Friends and Family Test – Early Implementation To improve the experience of patients in line with Domain 4 of the NHS Outcomes Framework. The Friends and Family Test will provide timely, granular feedback from patients about their experience. To roll-out to Community Nursing and Therapy services, Muskulo-skeletal physiotherapy and inpatient units. 2.1 Friends and Family – Phased expansion To improve the experience of patients in line with Domain 4 of the NHS Outcomes Framework. The Friends and Family Test will provide timely, granular feedback from patients about their experience. Phased expansion, but to exclude Adult Speech and Language and Lymphoedema service. 3. NHS Safety Thermometer To measure and reduce harm. It is recommended that organisations prioritise improvement in pressure ulcer prevalence. 4. Inpatient Beds Dashboard To develop an inpatient Data Management Information System. This dashboard will enable commissioners and providers to support improved system flow by making sound and rapid operational decisions. 28 PART 3 NCH&C contribution across Norfolk to help increase the numbers of women initiating breastfeeding in line with the Department of Health target of 2% increase per annum. 6. Lymphoedema Roll out of specialist service to include pre assessments in the West locality. This will improve patient experience, bringing care closer to home to reduce unnecessary admissions. Expansion of existing service to provide a specialist nurse for patients with Multiple Sclerosis. This service will support patients experiencing problems with relapse, ongoing symptoms and worsening of their condition who would otherwise be admitted to hospital. 8. Development of sepsis education To develop and produce a clinical competency training programme for inpatient units and community teams. 9. Integrated care co-ordination To develop working seven days allowing the co-ordination of placements from the acute trust into the community setting over a seven day week. 10. Dementia Provision of tiered training at three different levels to encapsulate all ranges of staff from non-clinical through to dementia link worker. 11. Prosthetics All new patients referred in to the service are to be triaged within four weeks and offered a multi-disciplinary team (MDT) assessment within a maximum of six weeks from receipt of the referral. The Trust achieved 100% against all the indicators except; Indicator 6. Lymphodoema which achieved 93.7% Indicator 8. Sepsis Education which achieved 90% Indicator 9. Integrated care coordination which achieved 75% As a result of implementing these indicators during the year, it is anticipated that the Trust will receive £2,332,000 in additional income. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 29 PART 3 2. A well-led organisation 2.1 Introduction “It’s all about our staff...” said Roisin Fallon-Williams, our Chief Executive, in the March edition of the Exchange. Our staff play a prominent role in the organisation and we take time out to celebrate the success of our colleagues. Whether this is through the progression of their careers, giving up their own time to share best practice, or being acknowledged for the outstanding work that they do by being nominated for regional awards. 2.2 Student nurses We welcomed our largest ever single cohort of student nurses who will be taking up roles across the county to help prepare them for their first jobs after they have qualified. A total of 80 students – twice the usual headcount – started work at the end of November 2014, most are in the second year of a three year degree course at the University of East Anglia (UEA). They are completing a 12-week placement so that they can gain direct experience of patient care, with added responsibility and autonomy. This means that they will be better prepared for their first jobs as qualified nurses. Taking on the super-sized group has been made possible following the introduction of a new Collaborative Learning in Practice (CLiP) initiative, being piloted by NCH&C in a number of hospitals in the county. Whereas previously, training consisted of a ‘one nurse to one student’ model, the new initiative allows more student nurses to be taken on and trained at the same time. Launched in May this year, CLiP was piloted at North Walsham and District War Memorial Hospital, Community Nursing Teams in North Norfolk, and Alder Ward in the Mulberry Unit at Norwich Community Hospital. It has now been expanded to include Community Nursing Teams in Norwich and South Norfolk. In total, 65 of the students will be trained under the new model, with 15 receiving training under the traditional model. CLiP has been developed in partnership with NCH&C, the UEA and Health Education East of England (HEEoE). It gives students the chance to run a learning bay or small community caseload, while taking on responsibility for planning and delivering care under the guidance of a registered nurse. The aim is to provide a different experience for the students, as well as essential practical skills, helping build their confidence before they qualify. This style of training has also been shown to improve quality of care elsewhere on the ward by giving other staff more time to spend with their patients. Marcia Perry, Deputy Director of Nursing and Quality, said: “It means we are providing trainee nurses with a positive experience of community services. We’re shaping practitioners for the future that will hopefully want to come and work with us in the community and will be better prepared for the role. “Staff recognise the importance of investing in training the future generation, and the patients love it! They are able to build a relationship with student nurses over the 12 weeks. Students work in pairs and have dedicated and focused time each shift where they can assess and plan care for their patients.” We will review the placement, alongside the formal evaluation by HEEoE, in order to continue to improve and plan for future cohorts of students. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 2.3 National Apprenticeship Week The Trust marked National Apprenticeship Week, from 9 - 13 March 2015, by celebrating the success of our apprentices, and our apprenticeship programme, with a variety of events reaching thousands of potential apprentices. 2.4 Staff achievements 2.4.1 Laying their career foundations PART 2 30 PART 3 2.4.3 Staff shortlisted for regional awards Staff from across NCH&C were shortlisted for regional awards in recognition of their contribution to supporting learning and education across the organisation. The awards, run by the Norfolk and Suffolk Workforce Partnership, recognise individuals and teams who have made an outstanding contribution to the overall growth, development and education of pre-registration healthcare students and learners. A total of seven teams and individuals have been named as finalists in the Practice Education and Learning Support Awards 2015. They are; Learning Support Award – Apprenticeships: Congratulations went out to two members of staff who have successfully completed foundation degrees in Health Studies. Kate Mawby and Wayne Lowe, both Nursing / Therapy Assistants working in the Specialist Amputee Rehabilitation Service in Pine Cottage, Norwich, studied for two years to earn the qualification, which is designed to be the ideal first level in higher education for healthcare workers. • Pippa Bennett, Bands 1-4 Development Officer 2.4.2 Kelling trio the first to complete Level Three Diploma • Thetford Community Nursing Team Three members of staff celebrated being the first in our Trust to have successfully completed a Level Three Diploma in Clinical Healthcare Support. The trio, Heidi Ris, Dawn Shailes and Julie Harris, who are all Healthcare Assistants at Kelling Hospital in North Norfolk, embarked on the 18 month course to gain the qualification which demonstrates knowledge and competence in healthcare. • Children’s Speech and Language Therapy Service • Francesca Norton, Career Development Facilitator • Pamela Lacey, Senior Staff Nurse Mentor/Practice Teacher and Outstanding Contribution to Learning: • Lorna Young, Staff Nurse Team Award: • Caroline House, Specialist Neurological Rehabilitation Nursing Team 2.4.4 Sally Tyler is honoured with an MBE One of our Children’s Epilepsy specialist nurses paid tribute to the hardworking team around her after being named as a Member of the British Empire (MBE) in the Queen’s New Year’s Honours list. Sally has worked in this role since 2001, and provides an holistic service for young people aged up to 19 in central Norfolk. Anna Morgan, NCH&C’s Director of Nursing and Quality, said; “ We are absolutely delighted that Sally has been recognised in this way. She provides a fantastic service to children and young people with epilepsy, as well as their families and carers, and ensures they receive the treatment, advice and support they need to live with the condition.” Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 PART 3 2.4.5 Health Visiting 2.5 NHS Staff Survey 2014 Our health visitors have won three awards for their excellence in mentoring students who have been training to become health visitors. The health visitors were presented with their awards on Friday, March 6, 2015 by Professor Viv Bennett, Director of Nursing at the Department of Health. The winners from the Trust were; The 2014 National Staff Survey has provided an invaluable insight into the views of our staff following publication of the results last month by NHS England. •K ate Hillman: Workplace Advisor Award for supporting the Building Community Capacity programme • Glenda Booth: Preceptorship Award for her support to newly qualified Health Visitors and pioneering work with the Institute of Health Visiting (iHV) • All Health Visitor Practice Teachers from across the region were recognised for their hard work with the ‘Team Award for Excellence’. 2.4.6 Speech and Language Therapy (SLT) The SLT team won the team award in the Norfolk and Suffolk Workforce Partnership Practice Education and Learning Support Awards. The awards ceremony was held at Dunston Hall, Norwich, on 16 March 2015, and the SLT team was presented with the Team Award in recognition of its dedication and commitment to student training. The award recognised that University of East Anglia students are routinely welcomed into the team with close liaison between educators to capitalise on learning opportunities. Therapists provide students with essential experiences in clinical decision-making, therapy delivery, inter-disciplinary working and interacting with the people who use our service. Therapists collaborate with students to plan their goals and enhance their personal learning. The SLT team advocates high-quality, accessible care for all and is dedicated to developing confident and competent practitioners of the future. Libby ffrench Mullen, Specialist Speech and Language Therapist, collected the award on behalf of her colleagues. 31 Nearly 300 NHS organisations in England took part in the 2014 survey, and in our Trust a random selection of 800 staff were invited to complete an on-line questionnaire relating to the NHS constitution. Nineteen Community Trusts participated in the survey, which enables NCH&C to compare its results against the national NHS picture and other community trusts. 2.5.1 Overview The overall results show that the scores are not statistically different to our 2013 results. However, when compared to other community trusts, they have moved further and faster with their results. This is in the context of significant change and cost pressures across the NHS. Our response rate has decreased from 55% in 2013 to 36% in 2014. This is reflective of a decrease in the national response rate (from 49% to 47% respectively) and may have been affected by a move from a paper questionnaire to an e-mail questionnaire for the very first time. Analysis of the figures show that NCH&C’s overall staff engagement score is 3.60 compared with 3.65 in 2013 and the average for community trusts of 3.75 in 2014 (scores are between 1 to 5, with the highest figure being positive). Overall, of the 29 Key Findings, NCH&C scored average or better than average in 9 and below average in 20 when compared to other community trusts. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 2.5.2 Top ranking scores Our top ranking scores included; • 91% of staff having had an appraisal in the last 12 months • 94% of staff reported an error, near miss or incident in the last month, and • 74% of staff feel secure to raise concerns • 94% of staff had received equality and diversity training in the last 12 months • 84% of staff had health and safety training in the last 12 months 2.5.3 Areas for development There are, however, areas for improvement required when comparing ourselves against other community trusts, specifically around work pressure felt by staff. 3.32 remains at the same level as our 2013 result but behind the community trust average of 3.11. Furthermore, staff recommending our Trust as a place of work or to receive treatment has declined to 3.42, compared with the community average of 3.66. 2.5.4 Next steps We held a number of staff survey workshops during March 2015 to gather employees’ thoughts and opinions on the results to help shape our action plans going forward. PART 2 32 PART 3 2.6 Health and wellbeing at work Staff interested in promoting health and wellbeing in the workplace are being encouraged to join a new group and help drive through a range of exciting new initiatives designed to make a difference to their colleagues at NCH&C. A group is being set up to help drive our Trust’s Health and Wellbeing strategy, which will ensure NCH&C continues to take a positive and engaging approach to enhancing the wellbeing of all our employees. The next part of the process will see our Trust use the NHS Wellbeing Charter Self-assessment Tool to see how well we are performing against key standards, and where action can be taken to improve still further. The assessment will look at a number of issues, including; leadership, absence management, mental health, smoking and tobacco, physical activity and healthy eating. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 2.7 Compliments and thanks Below is a selection of the compliments and thanks we have received from our patients and stakeholders. Benjamin Court, North I would just like to say thank you for all the kindness, love and excellent care you gave my mum in the last few days of her life. It was a great comfort that she was able to spend them in a safe, loving environment… PART 2 PART 3 Thetford Leg Club, South Norfolk To all the nurses and staff at the Thetford Leg Club, thank you for the kindness you have shown me over the past few weeks… Alder Ward, Mulberry Unit, NCH Thank you for everything – all your help and all your kindness to me. I will always remember you and I will miss you… Dental Access Centre, King’s Lynn To all the staff at Benjamin Court, thank you for your excellent care when looking after mum... An excellent service - prompt, relaxed and relatively painless. If only the whole dental service could be like this… District Nurses, South East Foxley Ward, Dereham Hospital I just wanted to thank the District Nurses who made the last three weeks of my father’s life so much easier and comfortable. I am so very grateful to you all for your help and care… A very big thank you to all the team for your skill, kindness and encouragement during my stay with you. I count myself very lucky to have been in your care. I hope Foxley Ward will be available for many others after me, for the benefit of the community… MSK Physio, Norwich I came in feeling so frustrated with my back and neck problems and the patience and understanding I received has been exceptional… Occupational Therapy, Aylsham The therapist gave me invaluable help and advice as I have mobility problems. They were very kind and provided me with aids and I now have more confidence and can move without pain… Community Nursing &Therapy, Norwich Just a note to say a very grateful thank you for the very prompt and caring service given by the district nurses to my mother during her final days... Family Nurse Partnership (FNP) Thank you for being my FNP nurse, I wouldn’t have it any other way. Thank you for all your help and support... Physiotherapy, West Norfolk The pain and my strength improved greatly within a short time. The advice of recommended diligent exercise by my physiotherapist was key to my success... 33 Lymphodema Team, Swaffham Hospital Excellent service. The therapist has always been caring, helpful, hardworking and professional... Occupational Therapy Team, Norwich Thank you for being a great OT, albeit for a short time. We are very grateful for your care, patience and your listening ear… Physiotherapy Team, Kelling Hospital I am 63. In the last 30 years I visited the Kelling Hospital physiotherapy department on four occasions. As ever, they are thorough, charming, understanding and do a great job. I have now finished my treatment, with good advice and exercises to go away and continue on my own. I’m feeling a lot better… Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 34 PART 3 2.8 Clinical Ethics Group Since its inception, the CEG has received few enquiries relating to acute/hot cases. The Clinical Ethics Group (CEG) for NCH&C had its first meeting in September 2012 and has continued to meet quarterly since then. The meetings are well attended with lively conversations and discussions. The important links with Norfolk & Norwich University Hospitals NHS Foundation Trust (NNUH) Clinical Ethics Group remain strong. Nevertheless, there appears to be no shortage of complex case discussions covering a wide area of service delivery. These discussions are minuted in brief, and to date, it is left to the presenting clinician to include information about a CEG discussion in the patient’s records as appropriate. This will be further considered in the meetings to be held in 2015. The underlying objective is to provide a framework of support for all of our clinicians, dispersed throughout the Trust, to encourage the sharing of complex clinical situations, and ultimately to improve the care, safety and quality of care for our patients by enabling our staff. During the coming year the CEG will continue to progress this work by: NCH&C joined the UK Clinical Ethics Network (UKCEN) in December 2014, and according to the web site (www.ukcen.net), we are the only community trust with membership. The core functions of the CEG are: • To embed ethics in NCH&C • To continue with the joint meetings with NNUH • To consider ‘hot cases’ and promote discussion of historic cases • To develop the function of scrutiny of relevant Trust polices • To discuss subject areas (as opposed to individual cases) which over the past year have included: –– Mental Capacity Act –– Deprivation of Liberties –– End of Life Policy and related matters • Running a programme of Trust-wide road shows entitled ‘Ethics in Action’ • Agree the recording of case discussions and how these may lead on to generic discussion • Develop a Trust CEG intranet ‘room’ • Formalise the CEG’s involvement with the development and scrutiny of Trust policies • Consider the role of a CEG more broadly within a community trust and test this through UKCEN and through the Aspirant Community Trust Benchmarking Group In March 2015, some of the CEG members attended a regional clinical ethics workshop facilitated by UKCEN. This workshop was aimed at clinical ethics committee members, and included ethical case study presentations from each group. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 35 PART 3 3. Responsive services 3.1 Review of quality performance in 2014/15 The specialist epilepsy service is comprised of two members of staff. Unusually high sickness levels in the team led to an increase in waiting times, which was resolved by the end of the year. 3.1.1 Summary Three families out of a total of 19 had to wait over 18 weeks for their home based short breaks nursing service to commence, following their referral to the team. There have been no breaches of the 18 week target since October 2014. One of the key performance targets for the Trust is the 18 week wait Referral to Treatment (RTT) target, where 95% of non-admitted patients should receive a definitive treatment or intervention within 18 weeks of referral. NCH&C reports 18 week wait compliance for 26 services. Overall, the Trust met this target for 2014/15 with a performance of 97%. However, four services saw their RTT performance fall below the agreed target for the year: • Musculoskeletal (MSK) physiotherapy (93%) • Podiatric surgery (67%) • Specialist epilepsy nursing (84%) • Children’s Shortbreaks Home Based Nursing Service (84%) MSK physiotherapy teams have increased the number of clinics in order to manage the increase in demand which they faced at the start of the year. This has seen them reduce the number of patients waiting over 18 weeks from 633 at their peak, to 148 at the end of the year. The podiatric surgery service changed its clinical pathway during 2014/15, resulting in the patients requiring surgery being seen at the Norfolk and Norwich University Hospital (NNUH). This change in pathway, combined with staff absence, resulted in an increase in the waiting list size and waiting time. By the end of the year, all patients waiting for surgery had either been seen by services in Suffolk, or had been transferred to the NNUH or providers in Suffolk. No patient has waited more than 52 weeks for any treatment, and NCH&C has improved and maintained waiting times for diagnostics, with less than 1% of patients waiting longer than 6 weeks. In 2014/15, there were seven reported cases of Clostridium difficile against an annual ceiling of five cases. There have been no reported cases of MRSA bacteraemia since July 2012. The Trust agreed an annual ceiling of no more than 4.0 injurious falls per 1,000 Occupied Bed Days (OBDs). Despite in-month variation across the Trust’s inpatient units, the overall performance year to date was 3.6 falls per 1,000 OBDs. All community service providers are required to report the level of Venous-Thromboembolism (VTE) assessments for patients admitted to its community hospitals. The Trust achieved the 95% target for 2014/15. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 36 PART 3 3.1.2 Meeting targets 2014/15 Indicator Target or upper ceiling Annual performance Trend Injurious falls Number of falls resulting in harm per 1,000 Occupied Bed Days to be less than 4.0 3.6 Stable Venous Thromboembolism (VTE) assessments At least 95% of admissions have a VTE assessment 97.2% Stable 18 week wait referral to treatment 95% patients receiving definitive treatment within 18 weeks of referral 97% Declining 3.1.3 Areas of non-delivery We set some ambitious targets for 2014/15, and have not met them in all cases. Clostridium difficile In 2014/15, there were seven reported cases of Clostridium difficile against an annual ceiling of five cases. All reported cases have been subject to Root Cause Analysis (RCA) to review lessons learned. There has been no link between the cases, and the increase reflects a general increase observed across Norfolk in 2014/15. In recognition, the ceiling for 2015/16 has been increased to seven. Harm free care We have continued to use the national NHS Safety Thermometer to measure how many patients were harm free during their care with NCH&C. Our Board set a target of 97% of patients not being harmed whilst in our care. Harm in this case is defined as patients who develop a pressure ulcer, a catheter acquired urinary tract infection or who fall. We achieved a harm free care rate of 96.7%. Delayed discharges Throughout the year, the number of patients whose discharge was delayed for non-medical reasons occupied an average of 6.2% of the Trust’s community hospital beds. This was above the Trust’s target of 5%. Analysis of the data has shown delays have been attributable to both health service related reasons (including patient and family choice and waiting for continuing healthcare assessments and placements), as well as social care delays. We are working in partnership with social care and the acute trusts to reduce the number of delayed discharges from our hospitals. Smoking cessation The service agreed an annual target for 2014/15 of 2,000 quits with its commissioner, Norfolk County Council. The Trust has struggled to generate the number of referrals required into this service to meet this target and as a result has only generated 1,550 quits. Commissioners have recognised that demand for these services has reduced nationally, and as a result are reducing the target next year to 1,251 which the Trust is confident it will meet. Health visitor recruitment and KPIs We had a target to recruit 169 health visitors by March 2015. The final position was an establishment of 159 whole time equivalent staff in post. This was despite specific recruitment campaigns, a major training programme, and rolling adverts on NHS jobs. The Trust has also failed to meet the KPIs for the 14 day, 12 month, and two and a half year reviews that each child should receive. An action plan has been developed and additional resources targeted on improving our systems and processes to ensure that these targets are met for 2015/16. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 37 PART 3 3.1.4 Missing targets 2014/15 Indicator Target or upper ceiling Annual performance Trend Clostridium difficile Five cases or less during 2014/15 (cumulative) 7 cases Declining % Patients who are harm free At least 97% of patients are harm free according to the Safety Thermometer 96.7% Improving Delayed transfers of care No more than 5.4% of beds occupied by patients whose discharge is delayed for non-medical reasons 6.3% Stable Smoking cessation service Achieve a minimum of 2000 quits per annum Estimated quits to March 1,550 Stable Health visiting New birth visits in 14 days (95%) 90% (Q4) Improving 12 month reviews (95%) 90% (Q4) 2.5 year reviews (90%) 73% (Q4) 3.1.5 Mixed sex accommodation requirements NCH&C is compliant with mixed sex accommodation requirements. No breaches were reported during 2014/15 and the Trust will be declaring continued compliance against this standard. 3.1.6 Self certification Our Board has risk assessed itself against on-going compliance with Monitor’s NHS Provider Licence in preparation for FT status. Compliance with all relevant conditions has been confirmed and validated with evidence. The Trust is therefore also compliant with those conditions identified by the TDA as being relevant to NHS Trusts. The Board has confirmed compliance with all TDA Board Statements, with the exception of statement 10 which relates to achieving all commissioner targets. The target for smoking cessation has not been achieved, and the Trust has not met the 18 week target for podiatric surgery. There is a plan in place to get performance back on trajectory in the coming year and maintain targets over the next two years, subject to further negotiations with commissioners. The Board considers the TDA governance declarations and Board statements every month. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 38 PART 3 4. C aring services Patient Experience 4.1 Summary Our vision for Patient Experience and Involvement is that NCH&C is a patient focused organisation actively seeking the views of our patients and carers, and engaging them in shaping and developing our services whilst consistently providing high level, quality care. We want our patients to have the very best experience of community services in the East of England. NCH&C has been innovative and successful in using new methodologies and techniques to capture the views and experiences of our diverse community patient and carer population. This feedback has been used to promote, share and celebrate good safe quality care and high levels of satisfaction, but also to make improvements where they are needed and inform service redesign and business development. It is against this backdrop that the three priority themes have been identified: 1. Ensuring a systematic approach to capturing feedback – empowering staff with knowledge of how to capture patient experience feedback, the tools and techniques with which to do it and ensuring this informs a Trust-wide plan. 2. Action for improvement – using patient experience information alongside other quality data to make demonstrable improvements to care. 3. Building meaningful and systematic engagement and involvement - spreading and building on where good engagement and involvement of our patients, carers and Members exists and supporting development across the Trust. To turn these themes into reality a number of specific goals/workstreams have been identified. These will inform the development of annual implementation plans. 1. Capture and use the views and experiences of patients, families and carers, service user groups, Healthwatch and other voluntary groups in the evaluation, delivery, improvement and development of our services. Success will be measured by citing increased examples of how services have been improved as a result and increased involvement in developing services. 2.Develop and implement effective mechanisms for capturing and measuring patient experience and involvement. Success will be measured by extending the range (e.g. social media) and scope (across a wider range of services) of how we capture feedback, and demonstrating improvement in measures such as the Friends and Family Test. 3.Develop effective mechanisms for feeding back to our patients, families and carers and commissioners what we have done as a result of their feedback and involvement. Success will be measured by demonstrating improved and increased profile of what actions have been taken, and increased visibility and transparency of when things go well (compliments) as well as when things go wrong (e.g. complaints). 4.Develop a staff culture where listening to and acting upon the patient experience is embedded into everyday practice and informs organisational development. Success will be measured by an increase in participation in initiatives and profile. 5.Empower staff with the knowledge, tools and techniques available to carry out effective patient experience and involvement. Success will be measured by the number of available tools and the evaluation of their use. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 39 PART 3 Patient experience information is also included in the monthly Quality Assurance & Risk report and includes; 4.3 Patient Voice at Board •A n update on responses to the Friends and Family Test, including comments from patients and actions taken 4.3.1 Introduction • A review of patient’s stories uploaded onto the Patient Opinion website (www.patientopinion.org.uk) and actions taken by staff The Patient Voice programme has been part of NCH&C Board agenda since April 2012. The main benefit is that it helps to ground discussions in the reality of patient care. Patients are truly put at the heart of discussions as stories are powerful reminders of the context within which Board members are making decisions. Board members are able to see how their decisions impact on patients and carers, and helps them to better understand the complexities of day to day life at an operational level. • The Patient Voice at Board a regular feature at the beginning of every Board meeting • Complaints information including numbers, themes and trends and a summary of learning from these • Compliments received from patients, relatives and carers 4.2 Patient and carer involvement Patient and carer involvement in service redesign is becoming increasingly important. The first of a new style of ‘deep dive’ focus groups for patients and their carers recently took place for MSK Physiotherapy, MSK Occupational Therapy and Orthopaedic Triage. The feedback is being collated and will be shared with service leads to inform the redesign of the service. This work will also provide the basis of a toolkit for conducting focus groups. A Patient Experience learning event was held in March 2015 for staff and the key objectives included; • How to support patient/carer involvement • Patient experience and involvement - networking / learning / sharing good practice and problem solving The Patient Voice at Board is heard at the very start of the meeting before other items on the agenda. Board members have reflected that this is very valuable and reminds them of the core business of putting patients, their carers and families at the centre of delivering high quality care. It helps to highlight what the elements are of a good patient experience, directly from the patient, and how we can replicate this across the Trust, but equally to address areas where there have been poor experiences and how the Trust can support staff with delivering improvements. From November 2013 to February 2015 there have been 14 stories heard at Board, five of which were patients, three were parents/carers with their children, four were carers/family members, one was a case study given by a member of staff, and one from an external organisation describing how they receive stories from the public. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 4.3.2 What has changed as a result of Patient Voice at Board? Smokefree Norfolk service We have worked closely with commissioners to redesign this service to ensure that our staff can continue to deliver a service that we feel passionate about in influencing healthier lifestyles for our patients. The new contract from April 2015 enables us to deliver more training to other providers as well as retaining our specialist interventions. Intravenous Therapy Service This service continues to be supported by patients who are able to receive more care at home. We have developed stronger relationships with the NNUH as a result, and there is better joint working between our clinical teams and the outpatient departments. Patient with Neurological Condition The experience shared by this patient has informed the care strategy work and the case management level of care that we are taking forward this year. PART 2 40 PART 3 Urgent Care Unit This experience has been reflected into the second phase model of care now provided at the UCC. There has also been a lot of work this year with all clinical teams across adults and children’s services on the Sepsis pathway. New guidance and standard operating procedures are in place. MSK Physiotherapy The delays and early difficulties experienced by this patient have been used to inform a new integrated model of MSK with a triage service that will ensure patients are put on the appropriate pathway at the earliest time. A service user focus group has also been held to develop the model further and serve as a group that can feedback during the implementation phase of the new model. Breastfeeding The ideas generated from the peer support workers have been used to inform the Healthy Child Pathway (HCP) tender and enabled us to develop clearer career pathways for this valuable group. Conclusion and next steps The Patient Voice has been extremely valuable for the Board as it enables them to hear about and understand the experience of care directly from the patient or carer. We will continue to have a Patient Voice at every Board meeting, and use these experiences along-side the wealth of other patient experience feedback to systematically improve care and service delivery. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 4.4 Friends and Family Test (FFT) One of the main areas of focus is the implementation of the Friends and Family Test (FFT). The Trust has made huge progress with FFT across all services, and as a result we have achieved 100% of our Commissioning for Quality and Innovation (CQuIN) indicators. With FFT well underway, the focus will shift to closer monitoring of results, increasing low response rates and taking action as a result of feedback from patients. To assist this, a new monthly monitoring programme is being set up and services that are doing well will be highlighted in the monthly staff newsletter. 97% would recommend our services FFT results for 2014/15 In total, NCH&C received 5162 responses and of these 4648 comments were left with an overall percentage of 97% recommending our services. Overall, the most positive comments received were for care and treatment (3142), and time/appointment delays received the most negative comments (176). Extremely Likely (83.6%) Likely (13.6%) Neither likely nor unlikely (1.2%) Unlikely (0.4%) Extremely unlikely (0.3%) Don’t know (0.3%) 41 PART 3 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 4.5 Patient Opinion Patient Opinion (www.patientopinion.org.uk) allows service users to feedback on their experiences via a web-based tool and enables staff to interact with patients to help improve care. This tool will be rolled out to more services through 2014/15. In 2014/15, there were 29 stories posted on Patient Opinion, some of which were not directly related to NCH&C services. These were highlighted to the most appropriate organisation for acknowledgement and follow up. • 13 stories were wholly positive • 10 stories were wholly negative • 6 stories were a combination of positive and negative • 6 of the 13 positive stories praised care, treatment and professionalism at the Pine Cottage specialist amputee rehabilitation service • Other positive stories praised and thanked community physiotherapy, Dereham, Swaffham and North Walsham Cottage Hospitals • Two of the negative stories related to health visiting regarding identification of tongue tie and subsequent follow up with the parent. Both of these stories were directly responded to by the health visiting lead and have led to changes being planned in the service PART 2 42 PART 3 • Of the other negative stories, they related to a range of different services and concerns including care at North Walsham and Swaffham Community Hospitals, NHS funding for eye tests and glasses in school nursing, access to district nursing, end of life information for a carer and pre x-ray questions prior to podiatric surgery • Of the rest of the stories, which were a combination of positive and negative experiences, these often praised the clinicians for excellent clinical care and treatment, but had less positive experiences of waiting times (MSK physiotherapy), privacy and dignity (Beetley Unit, Dereham Hospital) and information about appointments at a GP reception (community physiotherapy but unknown location) All stories on Patient Opinion are responded to online by the relevant member of staff - where further information is required, the author is asked to contact the Patient Advice and Liaison Service (PALS). We will be exploring ways in the coming year of increasing promotion and uptake in the use of Patient opinion across the Trust, and in sharing good practice in responding online to ensure an open dialogue approach to stories which leads to improvements in care. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 Highlights from this survey: • 96% response rate • 100% reported that they were treated politely and with respect • 98% felt they had received a thorough assessment • 100% felt they could discuss worries or concerns • 93% felt they were involved in decisions about their care It was clear how much the service was valued by those assessed, and a number of people expressed their gratitude, describing a ‘caring’ and ‘excellent’ service. As a result of the survey, a patient information leaflet including service contact details will be included in new referral paperwork pack. Further work needs to be done regarding the number of patients who are not receiving a referral on discharge from hospital promptly. Education and promotion work has been undertaken but this remains an ongoing issue. This is an area under review as part of the COPD pathway review with West Norfolk CCG. Re-enablement Services; conducted a carer survey during November and December 2014. Five of the six carers to respond said the service was good and two responders described the service as “excellent” and “fantastic”. There was a negative comment about the patient transport service which the team reported to the transport manager and G4S. 4.7 Complaints and compliments From 1 April 2014 to 31 March 2015, we received 271 complaints, in comparison to 207 during the year 2013/2014. As in the previous year, there was a spike in complaints during October 2014 (36 complaints were received, compared to 33 complaints during October 2013). Patient compliments are also measured and this year the Trust has received around 1,160 compliments. Numerous discussions around complaint themes have been held, but there does not appear to be any specific explanation for the increase in numbers. Complaints are generally spread across all localities, although the introduction of the locality hubs this year has seen slight increases in complaints in a couple of the localities. The table below shows the number of complaints received on a month by month basis: 40 35 30 25 20 15 10 5 0 pr -1 M 4 ay -1 Ju 4 n1 Ju 4 l-1 A 4 ug -1 Se 4 p1 O 4 ct -1 N 4 ov -1 D 4 ec -1 Ja 4 n1 Fe 5 b15 M ar -1 5 West Norfolk Chronic Pulmonary Obstructive Disorder (COPD) service; the service conducted a redesigned patient satisfaction survey from October 1, 2013 to September 30, 2014. One of the main objectives was to identify if changes made to the assessment process following previous patient experience reports have been beneficial (use of quality of life tool). The survey was distributed to all patients referred to the COPD Nursing team who received a home visit from West Norfolk COPD Team. PART 3 A 4.6 Local patient surveys PART 2 43 A continual process of learning from complaints is in place. These are collated from the Investigating Officer following completion of a complaint investigation, and overseen by both the Quality and Risk Assurance Committee, and the Trust Board. Further evidence is now starting to be collated so that evidence is produced of the learning that is put in place, and reporting will start on this early in the 2015-16 financial year. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 4.8 Patient Led Assessments of the Care Environment Patient-Led Assessments of the Care Environment (PLACE) are a self-assessment of a range of nonclinical services which contribute to the environment in which healthcare is delivered in both the NHS and independent / private healthcare sector in England. The Health and Social Care Information Centre (HSCIC) requires trusts to self assess their patient environment annually using an assessment tool which reflects needs of its various stakeholders and the policy priorities of Ministers and the CQC. Analysis has shown that despite changes to assessment criteria and methodology between 2013 and 2014, our Trust’s performance has improved in three areas Cleanliness, Food, and Condition, Appearance and Maintenance, but deteriorated in one area, Privacy, Dignity and Wellbeing. The Estates strategy has provided focus on investment in the Trust’s estate, improving maintenance and condition of buildings, particularly areas used for patients delivering improvement during 2014 at a rate higher than the national average. Privacy, Dignity and Wellbeing will form the core focus in 2014/15, with action planned through the Trust’s Patient Environment & Nutrition Group (PENG). The highest scoring locations for 2014 were: • Benjamin Court and Cranmer House scoring 100% in Cleanliness • Colman Hospital, Cranmer House and Dereham Hospital all scoring within the upper quartile (above 95.50%) for Food • North Walsham Hospital scoring 93.06% for Privacy, Dignity and Wellbeing • Benjamin Court and Swaffham Hospital scoring within the inter quartile range for Condition, Appearance and Maintenance PART 2 44 PART 3 The lowest scoring locations for 2014 were: •D ereham Hospital, North Walsham Hospital, Ogden Court and Swaffham Hospital, scoring within the lower quartile for Cleanliness but improving since 2013 • Benjamin Court, Kelling Hospital and Ogden Court scoring below the middle quartile for Food (91.73%) but improving since 2013 • Cranmer House, Dereham Hospital, Kelling Hospital, Norwich Community Hospital and Ogden Court scoring within the lower quartile for Privacy, Dignity and Wellbeing. However, all except Dereham Hospital have improved since 2013 • All, except Colman and Swaffham Hospitals scoring within the lower quartile for Condition, Appearance and Maintenance. However Benjamin Court, Cranmer House, Kelling Hospital and Norwich Community Hospital have improved since 2013 The largest contributing factors to lower scores in the Privacy, Dignity and Wellbeing category include the poor way finding and signposting facilities, underutilised dayrooms and courtyards, and a lack of WiFi and individual TV / radios for patients. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 PART 3 Below is a summary of detailed scores by site for 2014. These scores are risk assessed to show whether they fall above or below the national average. Site Name Cleanliness % Food % Privacy, Dignity & Wellbeing % Condition, Appearance & Maintenance % Benjamin Court 100 89.52 82.14 82.64 Colman Hospital 97.48 98.62 85.11 93.16 Cranmer House 100 97.9 80.16 80.51 Dereham Hospital 95.53 95.64 75.00 70.18 Kelling Hospital 99.10 89.98 75.76 79.73 North Walsham Hospital 92.67 95.13 93.06 85.71 Norwich Community Hospital 98.19 92.86 74.07 83.33 Ogden Court 88.89 87.23 73.81 66.00 Swaffham Community Hospital 96.34 93.24 87.14 91.96 AVERAGE SCORE 96.47 93.35 80.69 81.47 below national average for 2014 above national average for 2014 45 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 46 PART 3 5 Safe services 5.1 Introduction 5.2 Safe staffing The CQC inspected our services in September 2014, and whilst the organisation was rated GOOD overall, the CQC identified some concerns regarding the safety of services, and judged this to require some improvement. There has been an increasing focus on both ensuring and evidencing safe staffing levels in inpatient units both by the media and the public. Key guidance in relation to safe staffing was published in November 2013, by National Quality Board entitled ‘How to ensure the right people, with the right skills, are in the right place at the right time’. The key areas related to: 1.The refurbishment of Squirrels residential respite unit for children Response: this work had already been identified in the estates plan and the work was brought forward and completed by the end of December 2014 2.Responsibilities regarding the Mental Capacity Act 2005 (MCA) Response: a guidance document on the 2-stage MCA assessment as a rapid guide and support tool to all staff was created and circulated. Specific MCA training provided to qualified clinical staff in inpatient units as a priority, and a MCA Deprivation of Liberty Safeguarding (DOLS) checklist developed to support staff while national policy is being developed and in line with new legislation 3.Management of medicines in inpatient units, relating to storage and stock control systems Response: Standard operating procedures relating to ordering and storage of medicines and for the management of controlled drugs have been developed. An updated service level agreement is in place for pharmacy services. 4.At the time of the inspection, the Trust could not be assured that all faith leaders had been subject to Disclosure and Barring Service (DBS) checks Response: A review of all faith leaders was undertaken and it was confirmed that all faith leaders had appropriate checks under DBS NCH&C are confident that following completion of the CQC compliance action plan, positive steps continue to be taken to improve the safety and quality of all our services. This section highlights the work that has been undertaken during 2014/15. The new guidance sets out a series of expectations in relation to the role of the Board in ensuring safe staffing, and since April 2014 the Trust has completed the required monthly submission of it safe staffing reports via the agreed “UNIFY” system. This information is also published on the Trust intranet page. We continue to maintain a high standard of patient care, safety and experience. This is evidenced in many ways such as low incident levels, positive external reviews, Patient Safety Thermometer and Friends and Family Test scores. The Trust is committed to ensuring that the levels of nursing staff, including registered nurses, and care support staff, are appropriate and meet the needs of patients across the settings within which we provide services. There is no clear guidance or specific modelling tools available for community trusts to use to assist in determining safe staffing levels, with the exception of our specialist rehabilitation units. However, an appropriate skill mix and level of nursing staff to provide safe and effective care is ensured. These levels of staff are viewed along with ‘registered nurse to patient ratios’, the percentage skill mix ratio of registered nurses to care support staff and the numbers per shift to provide safe, effective patient care. The specialist rehabilitation units use patient dependency tools to demonstrate the level of intensity of care for each individual patient, and that in turn sets out the staffing and payment structure. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 •A ll in-patient units have reviewed staffing levels across all of our rehabilitation units using the RCN toolkit ‘Safe staffing for older people’s wards’ to compare and potentially determine the correct levels of staff for the required standard of patient care within these settings • Community teams utilise recent Interim Management and Support (IMAS) work completed locally which presents a baseline and model for community nursing, and for the first time sets clear levels of activity for nursing teams as agreed with commissioners The Director of Nursing and Quality reports monthly to the Trust Board regarding the actual nurse staffing levels, against the established staff levels, on a shift by shift, unit by unit basis. This account includes monitoring the numbers of shifts that have been escalated, triangulated against the workforce and quality metrics to indicate if there are issues that require improvement i.e. high levels of maternity leave or short notice sickness. As new guidance and tools that are appropriate for community settings and specialist areas are developed, reviews of staffing levels will be undertaken. The on-going work within transformation also supports regular overview of the work and activity in relation to each member of staff and team. The transformation model supports staff in the allocation of appropriate levels of work, sufficient time to complete and that staff work within contracted hours. This is further supported by e- rostering as this is rolled out across all units and teams. PART 2 47 PART 3 5.3 Being Open (Duty of Candour) The Trust has developed an updated Being Open (Duty of Candour) policy which describes the process for staff to communicate with patients, their relatives or carers following an incident causing moderate or severe harm (or unexpected death) which uses the National Patient Safety Agency definitions; • Moderate harm incidents (short term harm, patient required further treatment or procedure – e.g. grade 3 pressure ulcers, some patient falls and medication errors) • Severe harm incidents (permanent or long term harm). All currently reported as SIRIs • Death incidents (any unexpected or unintended incident which caused the death of one or more persons). All currently reported as SIRIs We recognise that promoting a culture of being open is a prerequisite to improving patient safety and the quality of healthcare systems. For patients, effective communication starts from a healthcare need being identified and continues throughout their treatment. For staff, there is an ethical responsibility to maintain honest and open communication with patients and carers even when things go wrong. The terms of this requirement have been based on the 10 principles of ‘Being Open’ policy published by the National Patient Safety Agency (NPSA) in November 2009. 1.Acknowledgement 2.Truthfulness, timeliness and clarity of communication 6.Risk management and systems improvement 7.Multidisciplinary responsibility 3.Apology 8.Clinical governance 4.Recognising patient and carer expectations 9.Confidentiality 10.Continuity of care 5.Professional support NCH&C has been compliant with the requirements of a Duty of Candour during 2014/15, and in line with its policy continues to support clinicians to be open and honest with patients when things go wrong. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.4 Norfolk Harm Free Care project From September 2013 to September 2014, NCH&C have been helping to deliver an innovative, new scheme to improve health outcomes for Norfolk care and nursing home residents which was funded by Norfolk County Council (NCC) for 12 months. The Harm Free Care (HFC) Project is looking to reduce people’s risk of suffering a pressure ulcer, infection linked to urinary catheters, or falls. These three major harms can particularly occur in vulnerable, elderly and frail residents. Working in partnership with the Norfolk Harm Free Care Board, NCH&C joined up with NCC to commission the development of an assessment tool and supporting guidance and information for care homes, which consisted of; • Training for care home staff in addressing the three priority areas of harm • A paper assessment tool • A ‘guide to harm free care’ paper booklet and ‘bundle’ to detail a series of evidence based interventions for the care team to implement • A website to serve as a repository of information to support the carer by providing direction and guidance in using the assessment tool PART 2 48 PART 3 An online resource centre has also been developed to signpost people to local and national learning resources, while a Guide to Harm Free Care for patients and the public has been developed and made available. A total of nine care homes in Norfolk were involved in the new scheme. The evaluation of the project has been carried out in conjunction with the HFC Project Manager, NCH&C Clinical Audit and Effectiveness Team and NCC Public Health information Team. Achievements include; • The production of a local HFC Assessment Tool • Publication of a local HFC Guide to Practice booklet • The construction of a website of HFC information and guidance • Evidence to detail compliance with key outcome frameworks • Patient and service user engagement and involvement (e.g. Older People’s Forum, Suffolk and Norfolk Partnership, Carers’ Partnership, Independent Care) • E ngagement with the management teams of nine care homes and integration of health and social care models • Unilateral pathways of care to complement NCH&C’s transformation programme • Potential future partnership working with other healthcare trusts Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.5 National Safety Thermometer PART 2 49 PART 3 During March 2015, the Trust sampled 908 patients. The results indicated that the overall proportion of patients receiving ‘harm free care’ was 90.4%. Furthermore, the percentage of ‘new harm free care’ was 96.9%, just below the Trust’s Quality Goal target of 97%. It should be noted, that the reported figure is based on a sample undertaken on a specified day in the month, and will therefore depend on the sample size and the case-mix or complexity of patients sampled. The Safety Thermometer is a national measurement tool, developed by the NHS for the NHS, to provide a monthly ‘temperature check’ on harm which can be used alongside other methods, such as analysing incidents, to improve how the Trust treats it patients. The table below shows the data collected (in percentages) on one day a month from April 2014 to March 2015 against each of the ‘harms’: The safety thermometer focuses on four areas of harm; 1.Catheter Acquired Urinary Tract Infections (CAUTI) 2.Falls 3.Pressure ulcers (avoidable and unavoidable) 4.Venous Thrombo-embolisms (VTEs) (blood clots) Apr May Jun Jul Aug Sep Oct Nov Dec Jan Feb Mar 14 14 14 14 14 14 14 14 14 15 15 15 Harm Free 90.4 90.3 90.4 90.1 89.0 90.0 90.2 90.7 90.2 88.7 91.6 90.4 Pressure Ulcers 8.2 7.7 7.8 8.3 8.6 8.2 9.1 7.4 8.2 10.5 6.9 7.9 Pressure Ulcers (New) 1.5 1.7 0.9 2.3 3.4 2.8 1.5 2.7 2.6 1.5 1.2 1.6 Patients Falls 1.2 4.2 2.7 2.3 3.4 2.8 1.5 2.7 2.6 1.5 1.2 1.7 Falls with Harm 0.1 2.0 1.2 1.1 1.9 1.6 0.6 1.4 1.3 0.3 1.0 0.5 Catheters & UTIs 1.4 0.8 1.1 0.9 1.0 0.6 0.1 0.5 0.4 0.5 0.7 0.9 New VTEs 0.1 0.2 0.0 0.1 0.0 0.0 0.1 0.0 0.1 0.1 0.2 0.4 Harmed (New or Old) 9.6 9.7 9.6 9.9 11.0 10.0 9.8 9.3 9.8 11.3 8.4 9.6 Harmed (New) 2.6 4.0 2.9 4.1 5.3 2.7 2.9 3.0 3.8 2.3 3.0 3.1 Patients Sampled 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0 100.0 (New or Old) (New or Old) Harm Free (% of Patients) 92 91 91.6 90.4 90.3 90.4 90.7 90.1 90.0 90 90.2 90.4 90.2 89.0 88.7 89 88 M ar -1 5 15 bFe 15 Ja n- 4 ec D -1 ov N -1 4 4 -1 ct O 14 Se p- 4 ug -1 A l-1 4 Ju 14 nJu 4 -1 ay M A pr -1 4 87 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.6 Management and learning from incidents 60 50 -1 4 p14 O ct -1 N 4 ov -1 D 4 ec -1 Ja 4 n1 Fe 5 b1 M 5 ar -1 5 Se 4 l-1 ug Ju A 4 14 n- Ju -1 ay M A pr -1 4 0 Total SIRIs Pressure ulcers Other SIRIs reported by Type (Excluding Pressure Ulcers) 5 4 3 2 1 pr -1 M 4 ay -1 Ju 4 n1 Ju 4 l-1 4 A ug -1 Se 4 p1 O 4 ct -1 N 4 ov -1 D 4 ec -1 Ja 4 n1 Fe 5 b15 M ar -1 5 0 A All serious incidents are investigated using root cause analysis methodology. We aim to submit our 3 day and 45 day reports to our commissioners on time, and we have not reported any 45 day reports outside this timeframe during 2014/15. 30 10 Number Between April 2014 and March 2015, 379 SIRIs were reported, 360 of which were grade 3 and grade 4 pressure ulcers. 40 20 The policy contains flowcharts for reporting incidents and serious incidents requiring investigation (SIRIs), (as defined by the National Patient Safety Agency), and describes the process for escalation through the DATIX Incident Management System, assignment of an investigator and level of investigation required through to the final approval of the incident. We report monthly on all levels of incidents, including any learning and actions taken to the Trust Board in public throughout 2014/15. These reports are available on our Trust’s website (www.norfolkcommunityhealthandcare.nhs.uk). PART 3 SIRIs reported by Type April 2014 to March 2015 Number NCH&C has an NHS Litigation Authority accredited, Board approved, Incident Reporting, Investigation and Management policy in place which reflects the reporting requirements of the National Reporting and Learning System (NRLS), which is monitored by the Trust Development Agency (TDA) and the CQC. PART 2 50 Unexpected death Infection control Accident - Slip/Trip/Fall Staffing Medication Other Information Governance Accident - Other Allegation of Abuse Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 51 PART 3 5.6.1 Pressure Ulcers prevention 5.6.2 Tackling falls and dementia Staff were reminded of the steps which can be taken to avoid and manage pressure ulcers as part of an international campaign to ‘Stop the pressure’. This month long campaign has been designed to eliminate avoidable pressure ulcers in healthcare settings and care homes across the world. During November 2014, NCH&C ran a ‘Think Waterlow’ campaign to raise awareness of the steps which can be taken to avoid and manage pressure ulcers. Staff are consistently being reminded about the importance of completing a risk assessment by using the Waterlow assessment tool within six hours of the patient’s admission, and during initial contact with patients in the community. Staff have performed well against two important targets designed to ensure patients with suspected dementia and those at risk of a fall get the best possible care. Staff in the north locality referred 100% of inpatients with a clinical presentation of dementia for further medical assessment, in line with the CQuIN target introduced last year. Across the Trust, high scores have also been recorded against a 2014/15 key performance indicator, which aims to ensure all patients are screened for risk of falling, with those at high risk offered an holistic assessment. In addition, a special conference was held in November 2014, on international Stop the Pressure Day, with special speakers who spoke about incontinence, moisture lesions and the importance of protecting the skin. The PUVG also identifies learning points which will be included within the overarching Pressure Ulcer Action Plan. The action and learning points arising from the PUVG recently are; • Inconsistencies of Waterlow scoring • Capacity within operational teams 3 2 1 4 ay pr -1 -1 Ju 4 n14 Ju l-1 4 A ug -1 Se 4 p1 O 4 ct -1 N 4 ov -1 D 4 ec -1 Ja 4 n1 Fe 5 b1 M 5 ar -1 5 0 M The Pressure Ulcer Validation Group (PUVG) continues to meet on a fortnightly basis to review Pressure Ulcer Root Cause Analysis (RCA) and validate the avoidable/ unavoidable decision. 4 A Our Tissue Viability Nurse said; “Reducing pressure ulcers is a quality indicator and a quality goal for the Trust. If patients develop pressure ulcers which are avoidable, we need to be able to demonstrate we have done everything possible to prevent them.” 5 Falls per ‘000 OBS An updated staff information booklet called ‘Preventing and managing pressure ulcers’ was distributed on the day, and also sent to all modern matrons. Injurious Falls per ‘000/OBDs Performance - Inpatient Units 2014/15 performance 2013/14 average 2014/15 target Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.7 Mortality Review Group (MRG) We reported two unexpected deaths of patients in our inpatient units as SIRIs between April 2014 and March 2015, and these were investigated using root cause analysis. These incidents are further reviewed through our mortality review panels alongside all reported deaths. Dr Katie Soden (PBL consultant) has started formal mortality reviews. Over the next months, the MRG will initiate a process for local reviews whereby all inpatient units will undertake a first stage review shortly after the patient’s death, led by the consultant at the regular multi-disciplinary team meetings. The MRG will receive these reviews and alongside others, as described previously, (e.g. unexpected deaths) complete a review focussing on the learning and its dissemination. The Mortality Review policy and the proforma will not require significant change. The objective is to improve the ownership, the understanding and the learning across the Trust. The MRG continues to meet regularly. No significant clinical or quality issues have arisen from any of the recent reviews. Joint reviews with NNUH continue. In February 2015, the medical director attended a meeting alongside 19 other community trusts to discuss what is now referred to as ‘Mortality governance in the community: a care quality journey’. The title intends to describe a supportive, ‘no blame’ continual improvement culture, rather than a performance monitoring process, whose primary objective is to improve quality of care throughout inpatient settings, outside of acute hospitals. A number of trusts presented their work, and the attendees agreed to focus on the tools and frameworks used by NCH&C, as well as Torbay and South Devon and Lincolnshire community trusts. It was agreed to consider community hospital inpatients only at this stage, and not patients dying either in their own homes or other care settings. There was much interest in developing common reporting and analytical tools, and a plan to meet quarterly to share and develop the process. PART 2 52 PART 3 5.8 Never Events Never Events are defined by the Department of Health as ‘serious, largely preventable patient safety incidents that should not occur if the available preventative measures have been implemented by healthcare providers’. The Trust is pleased to report that there have not been any ‘Never Events’ during 2014/15 (or in any preceding years). 5.9 Central Alerts Central Alerts are cascaded to the appropriate service areas for action, and the Executive Directors’ Team (EDT) monitors their communication and supporting actions on a monthly basis in conjunction with the General Health & Safety Committee. 5.10 Infection prevention and control (IPAC) Our Trust’s nominated Director of Infection Prevention and Control (DIPC), currently the Medical Director, has Board level responsibility for infection control. The Deputy DIPC is responsible for the IPAC team, and the strategic and operational planning of the service across the Trust. A consultant microbiologist, contracted from the local acute trust as the infection control doctor, provides advice and support to the team as necessary. The organisation is locality based and the IPAC team work autonomously within each locality, whilst being centrally based. This gives each area an identifiable member of the IPAC team, whilst also having access to the whole team. Gaps in clinical practice, staff knowledge, environment or equipment are identified locally and discussed centrally for either a Trustwide or local solution. The Infection Control Committee, chaired by the DIPC or Deputy DIPC, is held on a quarterly basis and is attended by internal and external staff, including clinical and non-clinical. This committee reports to the Quality and Risk Assurance Committee (QRAC). Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 The work of the IPAC team is led by a detailed Annual Plan, which is reviewed and measured against the requirements set within the Health and Social Care Act, ensuring the Trust meets its obligations and is able to assure the Board that the organisation is meeting all standards. A large part of organisational assurance comes via the completion of regular auditing of clinical practice. ‘Clean, Safe Care’ (2008) identifies a set of IPAC audit tools, ‘Essential Steps’ to monitor clinical practices and gaps in practice. NCH&C has undertaken these audits until recently when, in discussion with the commissioners, ‘Essential Steps’ were replaced with a more comprehensive set of audit tools. All teams within NCH&C are now assessed for the most appropriate audits for their service and follow a bespoke programme of audit. This has led to more meaningful data which allows greater learning across the organisation. This data is analysed on a quarterly basis with exception reporting via the Infection Control Committee, and persistent areas of risk and/or concern escalated via the risk register and QRAC. All alert organisms are fully investigated with a root cause analysis completed with learning identified and shared with staff. Multi-disciplinary meetings ensure a 360 view of the case is considered and appropriate staff take learning back to their areas of work. Public Health plays a key role throughout these investigations ensuring appropriate challenge throughout the process. PART 2 53 PART 3 There is a suite (21 in total) of IPAC policies, as dictated by the Health and Social Care Act, which are regularly reviewed by the IPAC team, consulted on by the Infection Control Committee, approved by Clinical Policy Group, and ratified by Quality and Risk Assurance Committee. There is routine oversight by a consultant microbiologist and, where necessary and appropriate, a consultant virologist. All policies are held on the intranet for staff to access at any time required and, for the more commonplace policies, we are also moving to a policy on a page for ease of use. Training of all staff from Board to ward and beyond is a key focus within the IPAC department, and one which has continued as a face to face service rather than e-learning due to the differing services and environments involved. All staff receive IPAC training as part of induction and are identified as requiring a mandatory annual update if necessary. Training is reviewed each year to improve delivery and content, and to ensure staff receive the information on the most current issues at any given time. The IPAC team network through a variety of areas locally, regionally and nationally. There are good network links within the county covering acute hospitals, mental health trust, primary care, public health, ambulance service and private care homes. Cross boundary working ensures all providers are working towards mutual high standards, sharing best practice and planning together to ensure the best possible pathway for the patient. The two key areas of monitoring concern MRSA bacteraemia and Clostridium difficile infection. NCH&C, along with all other health care providers, has a zero tolerance of MRSA bacteraemia and therefore the ceiling is nil. NCH&C’s end of year figures are zero. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.10.1 Clostridium difficile (C. diff) The C. diff ceiling for 2014-15 is five cases. NCH&C has seen great reductions in cases of C. diff over the last 10+ years (see table) Year C. Difficile figures for the year 2004-5 143 2005-6 15 2006-7 19 2007-8 36 2008-9 13 2009-10 19 2010-11 9 2011-12 8 2012-13 3 2013-14 3 2014-15 7 NCH&C has followed the national trend in reduction of C. diff figures, through increased training, increased IPAC team, heightened awareness and a greatly improved environment. Our seven cases for 2014-15 have shown a disappointing rise, however, this has been a common trend locally and nationally. This has been recognised in the release of the new 2015-16 ceilings, which have increased across the board with a ceiling of seven for NCH&C. PART 2 54 PART 3 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.11 Medicines management There have been 549 medication incidents reported during 2014/15, 97% of these incidents caused no harm or low harm - none caused severe harm to patients. 14 moderate harm incidents were reported, these were: • 3 incidents involving prescribing for end of life patients in the community • 2 incidents involving the administration of medicines via syringe drivers • 3 adverse drug reactions • Delay by care home in obtaining urgent antibiotics • Insulin administered incorrectly by patient • Insulin administered incorrectly by nurse • 2 incidents on transfer of care This level of incidents is set against an estimated 200,000 prescriptions written or medicines administered each month. The following graph shows the trend of severity since April 2014: Breakdown of medication incident trends by severity 60 PART 2 55 PART 3 5.11.1 Controlled drugs incidents All controlled drugs incidents are reviewed by the Trust’s Accountable Officer for Controlled Drugs, and if necessary reported to external agencies. There were 87 incidents involving controlled drugs reported during 2014/15, broken down by severity and type of incident. No harm incidents included: •C ontrolled drug recording or stock issues (25 incidents) • Missed or delayed doses (10 incidents) • Prescribing issues (10 incidents) • Transfer of care issues (8 incidents) • Administration errors (8 incidents) Low harm incidents included: • Issues with administration via syringe driver (4 incidents) • Incorrect use of controlled drugs by patient / carer (4 incidents) • Missed dose of medicine • Adverse drug reaction There were 6 incidents causing moderate harm to patients (described above) and no severe harm incidents. Further analysis of incident breakdown is reviewed through the Trust’s Medication Safety Report at the Medicines Management Committee. 50 40 This report reviews the trends in medicines incidents and looks in more detail at incidents relating to: 30 20 • Controlled drugs 10 • Omitted and delayed doses of medicines Number of controlled drug incidents by month and severity 12 8 4 Ju 4 n1 Ju 4 l-1 4 A ug -1 Se 4 p1 O 4 ct -1 N 4 ov -1 D 4 ec -1 Ja 4 n1 Fe 5 b15 M ar -1 5 -1 4 0 ay Total M Low harm • Syringe driver incidents pr -1 Moderate harm • Moderate or severe harm incidents A No harm • Insulin incidents Number A pr -1 M 4 ay -1 Ju 4 n1 Ju 4 l-1 A 4 ug -1 Se 4 p1 O 4 ct -1 N 4 ov -1 D 4 ec -1 Ja 4 n1 Fe 5 b1 M 5 ar -1 5 0 No harm Low harm Moderate harm Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.12 Safeguarding children and adults We have a duty to comply with national and local legislation and policy. Our work is underpinned in particular by the implementation of the ‘No Secrets’ (Department of Health 2000 & 2011) multi-agency guidance in relation to adults, the Children’s Act (2004), and Working Together to Safeguard Children statutory guidance (Department of Health 2006 & 2013). We contribute to performance and quality measures as requested by the Care Quality Commission (CQC), Norfolk Safeguarding Adults Board, Norfolk Safeguarding Children Board (NSCB) and the Norfolk Clinical Commissioning Groups (CCG’s). The monitoring requirements are reflected in the respective trust safeguarding adults and children’s work plans, which aim to capture all of the expectations of the bodies above in respect of safeguarding. Progress against these plans is in turn monitored quarterly by the Quality and Risk Assurance Committee (QRAC). Since September 2013, inspection of safeguarding processes and case management in health organisations has been undertaken jointly by regulators OFSTED and CQC. 5.12.1 Working in partnership with other organisations The safeguarding children team has played a key role in improving multi agency working by contributing to a number of working groups to take forward Norfolk wide initiatives. This includes contributing to the development of a neglect strategy and plans are now in place to progress the development of Trust neglect champions, and also support the delivery of Graded Care Profile training to staff. This training will support the identification and management of cases where children are subjects of neglect. The safeguarding children team has also contributed to the development of a Norfolk-wide Domestic Abuse strategy. Other developments have included a joint working project with the local authority to improve joint working between social workers and health visitors, and this model has been evaluated well and subsequently embedded in practice. PART 2 56 PART 3 The safeguarding adult lead remains an active member of the Safeguarding Adult sub groups for: Mental Capacity; Deprivation of Liberty (DOLs). Training and health outcomes from these groups include; standardising basic training principles for all training providers and validating training courses; development of assessment criteria and guidance for the new DOL’s judgement outcomes. 5.12.2 Serious Case Reviews Norfolk Safeguarding Children Board authorised four Serious Case Reviews (SCRs) during 2014. The Trust has contributed to all of these as employer of staff involved in the cases. Director or deputy director level membership of each SCR panel has been provided, together with the Individual Management Reviews written by the safeguarding team. Publication of the overview reports will trigger action plans across all agencies, including the Trust, where implementation of recommendations is monitored by QRAC. The safeguarding team has continued to present learning at dissemination events arising from previous multi-agency reviews. A requirement for The Norfolk Safeguarding Adult Board, stipulated within the Care Bill (Department of Health 2013), is to implement SCRs for adult safeguarding cases. Processes have commenced to develop a multiagency procedural framework in line with the Children’s Board SCR process. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 5.12.3 Health visiting (HV) and school nursing The safeguarding children team continues to contribute to the HV Implementation plan for the Trust with training of new health visitors, new team leaders, and supporting the safeguarding supervision of front line staff. With increased numbers of health visitors, our focus is to ensure good safeguarding practice across the spectrum of work, from early intervention with families, to formal child protection procedures. The safeguarding children team have worked with senior children’s services managers around managing constraints within school nursing, and the development of an action plan to ensure robust systems and processes are in place to underpin safeguarding children. The deficit in school nurse numbers is on the safeguarding risk register. The work of school nursing in supporting children and young people of school age, including those at risk of sexual abuse and exploitation, is very important. PART 2 57 PART 3 5.12.4 Securing of Sexual Assault Referral Centre (SARC) contract for 2015 The Trust was pleased to learn their recent proposal for the delivery of a SARC service for under 13 year olds has been accepted by NHS England. This is an opportunity for the Trust to build on its long standing reputation for child protection work, and ensure a high quality service for children and young people at a most difficult and vulnerable time. The new service will be delivered by our experienced team of paediatricians at the newly developed children’s SARC in partnership with Norfolk Constabulary and the existing adult SARC service. In addition, the Trust has been asked by NHS England to investigate the possibilities for the setting up of a similar service in Suffolk and a business case with this aim is currently being prepared. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 58 PART 3 6. Effective services 6.1 Introduction Most measures are used internally; however, some are used to compare with other similar services elsewhere. Quality care can be described as care which is delivered according to the best evidence as to what is clinically effective in improving an individual’s health outcomes. NICE provides advice and support on putting NICE guidance and standards into practice through its implementation programme, and it collates and accredits high quality health guidance, research and information to help health and social care professionals deliver the best patient care through NHS Evidence. There are a number of examples where clinical effectiveness measures are currently used in the Trust. Most of these are benchmarking or Patient Reporting Outcome Measures (PROMS); however, there are also some examples of patient or carer experience and research. Other examples include: • The use of the Measure Your Own Medical Outcome Profile (MYMOP) across a number of services • In specialist rehabilitation, several tools are used including the following which are used for inpatient outcome measurement: –– U nited Kingdom Rehabilitation Outcomes Collaborative (UK ROC) –– Rehabilitation Complexity Score (RCS) –– Neurological Impairment Scale (NIS) –– Northwick Park Therapy Dependency Score –– Northwick Park Nursing Dependency Score –– Northwick Park Care Needs Assessment –– Goal Attainment Scale (GAS) for inpatients For outpatients in specialist rehabilitation: –– Needs and Provisions Complexity Score (NPCS) –– Neurological impairment scale (NIS) –– Northwick Park Nursing Dependency Score –– N orthwick Park Care Needs Assessment and the Goal Attainment Scale –– C hildren’s Services and Children’s Speech and Language Therapy both use the East Kent Outcomes Scale which is an outcome measures system used to identify goals and timetables, and an intervention plan with the family of patients Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 6.2 Implementation of NICE guidance 2014/15 There has been a total of 141 pieces of NICE guidance published in the period April 2014 to March 2015. NICE guidance is published once a month, and then filtered by the Trust’s NICE lead to remove guidance not applicable to Trust services. PART 2 59 PART 3 Guidance is then reviewed in more detail by the NICE Review Group and sent to relevant services for assessment and, if appropriate, risk assessment and action planning. The following NICE guidelines issued have been deemed relevant to the Trust: Date Ref Name Apr-14 CG179 Pressure ulcers Apr-14 PH52 Needle and syringe programmes Jun-14 CG180 Atrial fibrillation: the management of atrial fibrillation Jul-14 CG181 Lipid modification: cardiovascular risk assessment and the modification of blood lipids for the primary and secondary prevention of cardiovascular disease (CG181) Jul-14 CG182 Chronic kidney disease (CG182) Sep-14 CG183 Drug allergy: diagnosis and management of drug allergy in adults, children and young people Sep-14 CG184 Dyspepsia and gastro-oesophageal reflux disease Sep-14 CG185 Bipolar disorder: the assessment and management of bipolar disorder in adults, children and young people in primary and secondary care Oct-14 CG186 Multiple sclerosis Nov-14 CG189 Obesity: identification, assessment and management of overweight and obesity in children, young people and adults Nov-14 PH56 Vitamin D: increasing supplement use among at-risk groups Dec-14 CG191 Pneumonia Dec-14 CG192 Antenatal and postnatal mental health: clinical management and service guidance Dec-14 CG37 Postnatal care Jan-15 NG1 Gastro-oesophageal reflux disease: recognition, diagnosis and management in children and young people Mar-15 NG7 Maintaining a healthy weight and preventing excess weight gain among adults and children Mar-15 NG6 Excess winter deaths and morbidity and the health risks associated with cold homes Mar-15 NG5 Medicines optimisation: the safe and effective use of medicines to enable the best possible outcomes Mar-15 CG28 Depression in children and young people: identification and management in primary, community and secondary care Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 All relevant guidance is reviewed by the applicable services and risk assessed. Guidance that is particularly pertinent to a Trust service will be reviewed in depth and, for example, have a baseline assessment tool completed or a clinical audit planned. PART 2 60 PART 3 The following technology guidance has been deemed relevant to the Trust: Date Ref Name Jun-14 MTG19 The geko device for reducing the risk of venous thromboembolism Jun-14 TA315 Canagliflozin in combination therapy for treating type 2 diabetes Jul-14 TA318 Lubiprostone for treating chronic idiopathic constipation (TA318) Nov-14 MTG20 Parafricta bootees and undergarments to reduce skin breakdown in people with or at risk of pressure ulcers Dec-14 TA327 Dabigatran etexilate for the treatment and secondary prevention of deep vein thrombosis and/or pulmonary embolism Mar-15 TA336 Empagliflozin in combination therapy for treating type 2 diabetes Mar-15 TA335 Rivaroxaban for preventing adverse outcomes after acute management of acute coronary syndrome Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 As per the management of NICE guidance process, all TAs (technology appraisals) are reviewed and recommendations made to commissioners by the Therapeutics Advisory Group (TAG). PART 2 61 PART 3 All TAs for medicines that are applicable to Trust services have been added to the Trust medicines formulary. The following NICE Quality Standards have been deemed relevant to the Trust: Date Ref Name Apr-14 QS59 Antisocial behaviour and conduct disorders in children and young people Apr-14 QS61 Infection prevention and control May-14 QS62 Constipation in children and young people Jul-14 QS63 Delirium Jul-14 QS64 Feverish illness in children under 5 years Aug-14 QS66 Intravenous fluid therapy in adults in hospital Sep-14 QS68 Acute coronary syndromes (including myocardial infarction) Sep-14 QS70 Nocturnal enuresis (bedwetting) in children and young people Oct-14 QS71 Transient loss of consciousness Oct-14 QS74 Head injury Nov-14 QS5 Chronic kidney disease Jan-15 QS77 Urinary incontinence in women Jan-15 QS79 Idiopathic pulmonary fibrosis Mar-15 QS84 Physical activity: encouraging activity in all people in contact with the NHS Mar-15 QS82 Smoking: reducing tobacco use Mar-15 QS86 Falls in older people: assessment after a fall and preventing further falls Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 6.3 Clinical Audit programme 2014/15 Definition of clinical audit — a quality improvement cycle that involves measurement of the effectiveness of healthcare against agreed and proven standards for high quality, and taking action to bring practice in line with these standards so as to improve the quality of care and health outcomes. Clinical audit measures existing practice against evidence-based clinical standards. The annual clinical audit plan was approved by the Trust in April 2014. This contained 45 clinical audits across the Trust’s wide variety of services. The audit plan is broken down into various sections depending on the origin of the audit. A further 13 clinical audits PART 2 62 PART 3 1. Identify problem or issue 5. Implementing change 4. Compare performance with criteria & standards 2. Set criteria & standards 3. Observe practice / data collection were submitted during the year that were not included within the initial plan. The following table shows the breakdown (final figures are in brackets): Audit type Description Number of audits National clinical audits These are national audits the Trust participate in 3 (5) Commissioner priorities These audits are specifically requested by the commissioners of our services to provide analysis or assurance of a service 6 (6) NICE guidance These are audits of the Trust’s services against specific pieces of NICE guidance 18 (21) Trust priorities These are Trust wide audits of the Trust’s services against other guidance or standards that are considered a priority for the Trust 11 (17) Clinical service evaluations These are service evaluation audits and so measure the quality of a service rather than the outcome for the patient 7 (8) Clinical audits measure care provided against evidencebased standards. Where the target percentage is met the audit is said to have achieved ‘high assurance’, if the results fall short of the target the audit is moderate or low assurance depending on the distance from the target. The following table outlines the clinical audit results for 2014-15: Audits completed High assurance 6 Moderate assurance 13 Low assurance 9 No assurance level determined 10 Report not yet submitted 6 Audits cancelled 13 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 The increase in low assurance audits is due to services being challenged this year to develop new topics for clinical audits, and focus on new NICE guidance or clinical issues that they had identified as needing to be improved (for example from incidents or risks). All low assurance audits will be repeated in next year’s clinical audit plan to monitor for improvement. Some clinical audits did not determine an assurance level, due to their design, and five of these are national audits which do not use assurance levels. PART 2 PART 3 Some audits were cancelled during the year, either because the standard they were intending to measure was no longer pertinent to the service, they were merged with other audits for simplicity, or data collection took longer than anticipated and the audit has been continued into the 2015-16 clinical audit plan. All clinical audits are reviewed by the relevant Trust committee and any recommended actions reviewed for implementation. Examples of clinical audits completed in 2014-15 Clinical audit of ‘Do not attempt resuscitation’ orders in inpatient units • Overall compliance for the 12 standards increased from 77% last year to 86% • Improvements were seen in 9 standards, including quality of the discussions with patients and staff • Further improvements needed in the amount of detail recorded in patient notes Clinical audit of pressure ulcers • High assurance on 9 out of 10 standards measured (based on NICE guidance) Antibiotic prescribing audit • High assurance on the prescribing of antibiotics against the Trust formulary and prescribing standards Clinical audit of treatment of hypertension in the inpatient rehabilitation service • Assessed treatment of hypertension against current NICE guidance Clinical audit of ‘looked after children’ care plans • Good completion of health history and immunisation status • Improvement needed on the use of pressure ulcer prevention plans • Only around half of patients were on the treatment recommended by NICE • All medicines initiated prior to admission - liaison with patients GP required •Improvement needed in the recording of contact PREFERENCES, recording of care plan reviews and place of education •Strengths and difficulties questionnaire to be introduced into care plans Clinical audit of Parkinson’s disease treatment - south locality neurology service 63 • High assurance on the 8 standards measured, based on NICE guidance on Parkinson’s disease • Improvements to be made around offering discussion of end of life wishes / concerns with the team Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 6.4 Trust Research Performance We continue to be successful in recruiting patients into studies, and NCH&C is already one of the most active recruiters for National Institute for Health Research (NIHR) studies among the community trusts. Our aspiration is to be an acknowledged national leader in research among community based NHS organisations, and the Trust has many opportunities for further active engagement in this area. The 2013/14 national research recruitment figures were released in March and NCH&C achieved 435 recruits into research, making NCH&C the third highest recruiting community Trust and the first in the eastern region. There are currently 15 studies open within the Trust. A further four are being set-up. The Trust has recruited 405 patients into clinical research in the period April 2014 to February 2015, which is slightly under target (the Trust sets itself a target of 500 recruits into research each year), but with existing projects recruiting well we anticipate reaching the target by the end of March 2015. The research team is also undertaking projects to increase the Trust’s capacity to undertake research or improve the quality of our research: • Research ambassadors: 3 – 4 volunteers are being recruited to act as patient ambassadors to promote research awareness and participation amongst patient groups • Bank research nurses: 3 bank nurses are being trained in research and developed to help deliver on more research studies. This will increase our capacity to undertake studies and ensure we are able to use resources flexibly • Physiotherapy research clinics: bank physiotherapists have also been identified to work in research clinics. This will start at North Walsham, and the clinic will ‘fast track’ shoulder pain referrals and offer participation in a shoulder pain study. The clinic will retain management of all patients referred to it, even if they decline research participation therefore supporting operational team capacity • Good Clinical Practice (GCP): a further 13 NCH&C staff have been training in GCP – ensuring that they are ready to take on research when appropriate projects become available PART 2 64 PART 3 6.4.1 Research conference The first ever research conference organised to celebrate the research carried out by NCH&C, while developing new opportunities for collaborative working, was hailed a success after attracting delegates from across the eastern region. The ‘Reach out to Research’ event took place in September 2014, and was organised by the research department to engage with current and new partners through activities ranging from table top conferencing to speed networking. Feedback from those attending was positive, with patient representatives describing the conference as “the most informative and valuable NHS event attended”. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 6.5 Specialist Palliative Care The multi-disciplinary specialist palliative care team have monthly clinical governance meetings attended by representatives from all aspects of the service including the inpatient unit, the Rowan Centre day unit and the community service. Both clinical effectiveness and clinical audit are essential components of the clinical governance agenda and the team actively encourage all staff to be involved. Over the last year, the team have had a working group looking at the pain tools that are actively used within the inpatient unit. They have been involved with some national research regarding the use of the Carer Support Needs Assessment Tool (CSNAT) – this is seen as important as supporting carers as an integral part of the service the team provide. Recent audits have been undertaken against service guidelines regarding the use of methadone, bisphosphonates and paracentesis to ensure that the care provided is of the very highest standard. At present, the team are currently exploring IPOS as a symptom control outcome measure in line with national work on this. As well as taking part in the wider Trust patient experience work, the specialist palliative care team have also undertaken specific work with their patient group. They have undertaken a survey of patients admitted to Priscilla Bacon Lodge looking at the things that are most important to them including symptom control, the environment and the daily routine on the ward. The team have a very active service user steering group and are also involved in reflective case discussions both at Gold Standard Framework meetings and on site multidisciplinary team (MDT) meetings. The team are also part of the Palliative Care Academy for Norfolk and the Suffolk Research Group. PART 2 65 PART 3 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 66 PART 3 7. E xplanation of who has been involved in this Quality Account 7.1 Introduction There are a number of mechanisms for stakeholders, patients and the public to be involved in the work of the Trust throughout the year. For example; Norfolk Healthwatch and public involvement at Trust Board meetings and other committees, including Quality and Risk Assurance Committee, Patient Experience Steering Group and PLACE inspections. There is also patient and public involvement in discussions regarding service re-design and transformation. Development of the annual plan, priorities and quality goals was achieved in conjunction with the executive directors, assistant directors, heads of service and clinicians through a number of staff workshops and discussions at the Management Forum. Involvement of staff and public Governors and external stakeholders was through an online survey. The staff and public Governors received a draft version of the Quality Account at their Council of Governor’s meeting in May 2015 and further discussions are taking place to agree how the Governors wish to be involved in the development of the Quality Account in future. Third party commentary received from the Norfolk Clinical Commissioning Groups Norfolk Healthwatch and Norfolk Health Overview and Scrutiny Committee are presented below; Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 7.2 Statement from NHS Norwich, north Norfolk, west Norfolk and south Norfolk Clinical Commissioning Groups The Central Norfolk Commissioners for the NCH&C are very pleased to support the community trust in its publication of a Quality Account for 2014/15. We have reviewed the mandatory data elements within this account and can confirm that those included are consistent with the requirements. The report presents detailed and comprehensive information relating to the quality and safety of care delivered within the priority areas identified by the Trust. The Trust has been under significant pressure brought about by the increase in acuity of patients received by them, in part due to the over-all increased pressure in the Norfolk-wide system. The clinical and managerial staff have worked hard to ensure that standards are maintained and that patients are treated as individuals and with compassion. This is reflected in the consistent high scores in the ‘Friends & Family Test’. The Trust has played an active part in working with system partners to increase flow and pressures internally as well as elsewhere. We commend staff for their hard work and dedication to the patients that they serve. The report provides a balanced account of outcomes, highlighting successes and noting areas where further improvements are required and the steps in place to ensure that targets are met. There is a clear ethos of continuous improvement. It is clear that the priorities are relevant and appropriate; however it is felt that further work is still required to ensure that pressure ulcers and quality issues with the new ‘locality hub model’ decrease and a continued focus on recruitment and retention of a skilled workforce is maintained. NCH&C has had a positive impact upon the quality and safety of patient care in helping to evolve an open, crossorganisational improvement culture. PART 2 67 PART 3 Of particular note continues to be the Trust’s active participation in the monthly Clinical Quality and Review meetings. Here both provider and commissioner senior clinicians and managers review and constructively challenge the quality and safety performance of the Trust. The Trust takes these meetings very seriously and they are attended by both the Nursing Director and the Medical Director (as necessary). These meetings remain vital to assuring the local population that services contracted from the Trust are safe and of good quality. They enable discussions concerning new initiatives and current practice. They also provide a vehicle for constructive challenge regarding performance as appropriate. There has been a notably high level of candour and transparency that has allowed for issues to be openly aired and addressed effectively. The Trust’s innovative use of mortality review meetings has continued throughout the year and has been welcomed by patients, staff, governors and management alike. A recent CQC inspection was positive and identifies general improvements that are reflective of the hard work undertaken. We look forward to continuing to support and constructively challenge NCH&C in the pursuit of continuous improvement in the coming year. Jo Smithson, Interim Chief Executive Officer, NHS Norwich CCG (also on behalf of south Norfolk, west Norfolk and north Norfolk CCGs) Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 7.3 Healthwatch Norfolk Healthwatch Norfolk appreciates the opportunity to make comments on the Quality Account. We welcome the introduction of the values of community, compassion and creativity to develop a patient-centre model of care, and its use as the basis for the delivery of national and local quality requirements. The use of patient experience and what has happened as a result and the recognition of the achievements of staff give a clear message about the Trust’s culture. We welcome the comprehensive nature of Norfolk Community Health and Care’s Quality Account for 2014/15 and its honesty in discussing areas of difficulty as well as the Trust’s successes. We look forward to seeing the results of the Trust’s work to improve the results of the staff survey. The explanation of the sources of quality goals and indicators is particularly helpful, including the CQuINs negotiated with the different Clinical Commissioning Groups (CCGs). The number of CCGs in Norfolk provides good opportunities for innovation; we will be interested to see how the experiences from delivering the CQuINs is evaluated and disseminated across the county. We would be concerned if these initiatives led to inequalities in service provision for individual client groups across the county. We are pleased to see the growth in the Trust’s collaboration with other organisations within the health and social care system within Norfolk, particularly the development of integration in community services, and its participation in national initiatives to improve quality and safety of care. PART 2 68 PART 3 We have found that the level of detail, the repetition and the use of language make the Quality Account difficult to follow at times; the document assumes a level of understanding that may not be found among the general public. Where data on quality indicators has been collected over a number of years it would be helpful to give more than one year’s data to demonstrate improvements in service delivery over time. We will continue to work with Norfolk Community Health and Care to ensure that the views of patients, carers and their families are taken into account and to make recommendation for change where appropriate. Alex Stewart, Chief Executive 7.4 Norfolk Health Overview and Scrutiny Committee The Norfolk Health Overview and Scrutiny Committee has decided not to comment on any of the Norfolk provider Trusts’ Quality Accounts for 2014-15 and would like to stress that this should in no way be taken as a negative comment. The Committee has taken the view that it is appropriate for Healthwatch Norfolk to consider the Quality Accounts and comment accordingly. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Part Three PART 1 PART 2 8. Directors’ Declaration The following is a declaration; signed by all directors in office at the date of the account, certifying that they believe the contents to be true, or a statement of explanation as to the reasons any such director is unable or has refused to sign such a declaration. I believe the contents of this Quality Account 2014/15 to be true: Executive Directors Name: Roisin Fallon-Williams Chief Executive Name: Roy Clarke Director of Finance Name: Dr Rosalyn Proops Medical Director Name: Anna Morgan Director of Nursing and Quality Name: Paul Cracknell Director of Strategy and Transformation Name: Matt Colmer Director of Performance and Information Non-Executive Directors Name: Ken Applegate Chairman Name: Alex Robinson Non-Executive Director Name: Professor Ian Harvey Non-Executive Director Name: Derek Allwood Non-Executive Director Name: Heather Peck Non-Executive Director Name: Amanda Reynolds Non-Executive Director Name: Geoff Rivers Designate Non-Executive Director 69 PART 3 Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Glossary 70 Glossary of terms AHP Allied Health Professionals Allied Health Professionals (such as Physiotherapists, Occupational Therapists, Speech and Language Therapists, Podiatrists) provide treatment and help rehabilitate adults and children who are ill, have disabilities or special needs, to live life as fully as possible. They often manage their own caseloads. AQP Any Qualified Provider When a service is opened up to choice of ‘Any Qualified Provider’, patients can choose from a range of providers all of whom meet NHS standards and price. BAF Board Assurance Framework The Board Assurance Framework provides a record of the principal strategic risks to the Trust achieving its objectives. It identifies the controls in place, the methods of assurance and the control and assurance gaps. BGAF Board Governance Assurance Framework A key part of achieving FT authorisation is passing a rigorous assessment of board capability and capacity by Monitor, the Foundation Trust regulator. To support aspiring Foundation Trusts to meet this competency, the Department of Health has developed a mandatory board governance assurance framework in partnership with existing Foundation Trusts and other stakeholders. BNF British National Formulary The British National Formulary provide UK healthcare professionals with authoritative and practical information on the selection and clinical use of medicines in a clear, concise and accessible manner. C. Diff Clostridium Difficile A form of bacteria that is present naturally in the gut of around 2/3s of children and 3% of adults. On their own, they are harmless, but under the presence of some antibiotics, they will multiply and produce toxins (poisons), which cause illness such as diarrhoea and fever. At this point, a person is said to be infected with C. difficile. CADS Community Alcohol and Drug Service The main aim of the service is to reduce problems related to drugs and alcohol misuse, and support recovery. In order to do this CADS provides a range of modalities including advice and information, community and specialist prescribing, structured psychosocial interventions, structured treatments, harm reduction interventions and aftercare. CAUTI Catheter-acquired Urinary Tract Infection A bladder infection that has occurred as a direct result of the presence of an indwelling catheter (a mechanism used initially to help the bladder) CCG Clinical Commissioning Group These are groups of GPs that, from April 2013, are responsible for planning and designing local health services in England. They will do this by “commissioning“or buying health and care services. CIP Cost Improvement Plan/Programme The formal identification of an action which reduces the budgeted cost base of the organisation. It can relate to either pay or non pay costs. CN&T Community Nursing and Therapy Home delivered nursing and therapy services and interventions for Adults such as; wound dressings, end of life care, rehabilitation programmes. CQC Care Quality Commission An organisation that checks whether hospitals, care homes and care services are meeting government standards. CQuIN Commissioning for Quality and Innovation The Commissioning for Quality and Innovation payment framework enables commissioners to reward excellence, by linking a proportion of English healthcare providers’ income to the achievement of local quality improvement goals. Norfolk Community Health and Care NHS Trust Quality Account 2014/15 – Glossary 71 COPD Chronic Obstructive Pulmonary Disease DoL Chronic obstructive pulmonary disease (COPD) is the name for a collection of lung diseases including chronic bronchitis, emphysema and chronic obstructive airways disease. People with COPD have trouble breathing in and out. This is referred to as airflow obstruction. DoL has no simple definition as what qualifies as deprivation of liberty, it originates from case law rather than definitive acts of parliament. Under the MCA though it is now clear that someone cannot be made to do something that they are resisting and a full assessment should be made to enable decisions to deprive someone from a liberty for their own safety or well-being. CRR Corporate Risk Register The Corporate risk register is the aggregation of the local team and corporate department risk registers where the residual risk score is more than 12. It includes any additional sources of risk such as external or internal reviews. DPA Deprivation of Liberty Data Protection Act (1998) The Data Protection Act 1998 requires every organisation processing personal data to register with the Information Commissioner’s Office, unless they are exempt. CSSD Central Sterile Service Department EDT A service that provides sterilisation for equipment used by community services e.g. scissors, scalpels, tool nail cutters. The Team of Executive Directors of Norfolk Community Health and Care NHS Trust, that meets weekly. CSP Chartered Society of Physiotherapy The Chartered Society of Physiotherapy (CSP) is the professional, educational and trade union body for the UK’s 50,000 chartered physiotherapists, physiotherapy students and support workers. DASH Disability and Specialist Health Pathway The DASH service pathways are for children with medical, neuro developmental disorders and long term health conditions who require additional or specialist healthcare and whose needs cannot be met by the Healthy Child Pathway Datix DATIX risk and incident database DATIX is a web-based risk management monitoring tool that aids NCH&C staff in the reporting and management of incidents, risk, complaints and PALS enquires. Executive Directors Team EPRREmergency Preparedness, Resilience and Response In April 2013 NHS England introduced the EPRR Core Standards detailing the roles and responsibilities involved in EPRR, Major Incident and Service Continuity planning, partnership working, resource allocation and staff competencies. EWTT Early Warning Trigger Tool The Early Warning Trigger Tool is designed to capture and bring together all of the factors that could impact on the quality and safety of clinical services, to identify services that may be at risk, and to help prevent serious incidents and patient safety issues in the future. It is part of a package of measures being used to ensure that quality and patient safety remain a key priority for NCH&C. FFT Family and Friends Test A nationally driven patient satisfaction survey using the question ‘would you recommend this service to your friends and family?’ FOIA Freedom of Information Act (2000) The Freedom of Information Act 2000 is an Act of Parliament that creates a public “right of access” to information held by public authorities. Norfolk Community Health and Care NHS Trust FT Foundation Trust NHS foundation trusts are not-for-profit, public benefit corporations. FTN Foundation Trust Network The Foundation Trust Network is the membership organisation for NHS public provider trusts. They represent every variety of trust, from large acute and specialist hospitals through to community, ambulance and mental health trusts. Members provide the full range of NHS services in hospitals, the community and at home. IAG Intelligent Application Gateway A remote access method for access to IT services from outside the Trust. IBP Integrated Business Plan Document setting out the five year strategy of the Trust. ICO Integrated Care Organisation This will build on the Integrated Care Organisation pilot, the work in the West of the county and the work of the current health and social care integration project. KPMG have been commissioned to develop an options appraisal which highlights the benefits and risks of moving further on integration or continuing with our current processes. IG Information Governance Information Governance ensures necessary safeguards for, and appropriate use of, patient and personal information. IG Toolkit Information Governance Toolkit The Information Governance Toolkit is an online system which allows NHS organisations and partners to assess themselves against Department of Health Information, Governance policies and standards. It also allows members of the public to view participating organisations’ Information Governance Toolkit assessments. Quality Account 2014/15 – Glossary 72 IMCA Independent Mental Capacity Advocate Introduced by the MCA 2005: Service that helps particularly vulnerable people who lack the capacity to make important decisions about serious medical treatment and changes of accommodation, and who have no family or friends that it would be appropriate to consult about those decisions. The role of the Independent Mental Capacity Advocate (IMCA) is to work with and support people who lack capacity, and represent their views to those who are working out their best interests. INR International Normalised Ratio A laboratory measurement of how long it takes blood to form a clot. It is used to determine the effects of oral anticoagulants (an anticoagulant is a substance that prevents clotting of blood) on the clotting system. IPR Integrated Performance Report A report used to assure the Trust Board of organisational performance, to flag exceptions to the achievement of performance standards and corrective action as appropriate. KPI Key Performance Indicator Key performance indicators help an organisation to define and measure progress towards organisational goals. LADO Local Authority Designated Officer The role of the LADO is set out in the HM Government guidance Working Together to Safeguard Children (2013). They work within the County Council’s Children’s Services and should be alerted to all cases in which it is alleged that a person who works with children has: • behaved in a way that has harmed, or may have harmed, a child • possibly committed a criminal offence against children, or related to a child • behaved towards a child or children in a way that indicates s/he is unsuitable to work with children LD Learning Disability A learning disability affects the way a person learns new things in any area of life. It affects the way they understand information and how they communicate. Norfolk Community Health and Care NHS Trust MCA Mental Capacity Act 2005 The Mental Capacity Act (MCA) provides a framework to empower and protect people who may lack capacity to make some decisions for themselves. It states that: • you should have as much help as possible to make your own decisions • people should assess if you can make a particular decision • e ven if you cannot make a complicated decision for yourself, this does not mean that you cannot make more straightforward decisions • e ven if someone has to make a decision on your behalf you must still be involved in this as much as possible • a nyone making a decision on your behalf must do so in your best interests MCA often applies to people with a: learning disability, dementia, mental health problem, brain injury and stroke MRG Mortality Review Group All deaths (including unexpected deaths) are reviewed by the MRG to ensure that any trends are appropriately disseminated MRSA Methicillin-resistant Staphylococcus Aureus A bacterium responsible for several difficult-to-treat infections in humans due to its resistance to methicillin and other beta-lactam antibiotics. MRSA is especially troublesome in hospitals and nursing homers, where patients with open wounds, invasive devices, and weakened immune systems are at greater risk of infection than the general public. MUST Malnutrition Universal Screening Tool This is a five-step screening tool to identify adults who are malnourished, at risk of malnutrition or obese. It also includes management guidelines which can be used to develop a care plan. NED Non Executive Director A non-executive director is a member of the board appointed by the Appointments Commission, to hold the Executive to account, bring independence, external skills and perspectives and challenge on strategy development, risk management, shaping culture, and the integrity of financial and quality intelligence. Quality Account 2014/15 – Glossary 73 NHSLANational Health Service Litigation Authority The NHSLA is a Special Health Authority that administers the Clinical Negligence Scheme for Trusts (CNST) which provides indemnity to its members and their employees in respect of clinical negligence claims. They are also responsible for resolving disputes between practitioners and primary care trusts, giving advice to the NHS on human rights case law and handling equal pay claims on behalf of the NHS. The NHSLA also aims to help and support the NHS to improve patient and staff safety through learning from claims. NICENational Institute for Health and Clinical Excellence The National Institute for Health and Clinical Excellence provides independent, authoritative and evidencebased guidance on the most effective ways to prevent, diagnose and treat disease and ill health, reducing inequalities and variation. NPSNet Promoter Score Net promoter score is a key measure of individual, team and corporate performance and is used to drive up positive patient experience. NPSANational Patient Safety Agency The National Patient Safety Agency leads and contributes to improved, safe patient care by informing, supporting and influencing the health sector. NRLS National Reporting and Learning System Through the National Reporting and Learning System, the Patient Safety Division collects confidential reports of patient safety incidents from healthcare staff across England and Wales. Clinicians and safety experts help analyse these reports to identify common risks and opportunities to improve patient safety. OD Organisational Development Plan that which sets out ambitions for the organisation and its staff. PALS Patient Advice and Liaison Service The Patient Advice and Liaison Service has been introduced to ensure that the NHS listens to patients, their relatives, carers and friends, and answers their questions and resolves their concerns as quickly as possible. Norfolk Community Health and Care NHS Trust PAS Patient Administration System An information collection system that acute and community hospitals use to collect patient related data. PEAT Patient Environment Action Team This is an annual assessment of inpatient healthcare sites in England that have more than 10 beds. The assessment teams must be comprised of more than 50% lay members/patients. It is a benchmarking tool to ensure improvements are made in the non-clinical aspects of patient care including environment, food, privacy and dignity. The assessment results help to highlight areas for improvement and share best practice across healthcare organisations in England. PLACEPatient-Led Assessments of the Care Environment Details are being finalised but the new assessments were piloted in October. A total of 68 hospitals were involved in pilot PLACE assessments. The Pilot assessments ran from 1 October to 12 October 2012. The assessments will be similar to the PEAT inspections but with more lay members/patients on the teams (over 50% of the team members must be patients). PMO Project Management Office A department or group that defines and maintains the standards of process, generally related to project management, or a particular project, within the organisation. QIPPQuality, Innovation, Productivity and Prevention Quality, Innovation, Productivity and Prevention is a large scale transformational programme for the NHS, involving all NHS staff, clinicians, patients and the voluntary sector. It will improve the quality of care the NHS delivers while making up to £20billion of efficiency savings by 2014-15, which will be reinvested in frontline care. RATs Rapid Access Team A team of nurses, therapists and social workers who respond quickly to patients who are admitted to accident and emergency at the Queen Elizabeth Hospital to find alternative solutions to enable patients to be cared for at home. Quality Account 2014/15 – Glossary RCA 74 Root Cause Analysis RCA is a process designed for use in investigating and categorising the root causes of events. When incidents happen, it is important that lessons are learned across the NHS to prevent the same incident occurring elsewhere. Root Cause Analysis investigation is a well recognised way of doing this. SARC Root Cause Analysis SARCs are specialist medical and forensic services for anyone who has been raped or sexually assaulted.They aim to be a one-stop service, providing the following under one roof: medical care and forensic examination following assault/rape and, in some locations, sexual health services. Medical Services are free of charge and provided to women, men, young people and children. SHA Strategic Health Authority NHS East of England is the regional headquarters of the NHS, and provides strategic leadership to all NHS organisations across the six counties. It is ultimately accountable to the Secretary of State for Health. SIRI Serious Incident Requiring Investigation The former National Patient Safety Agency has developed a national framework for serious incidents in the NHS, titled ‘National Framework for Reporting and Learning from Serious Incidents requiring Investigation’. An incident or event or circumstance that could have resulted, or did result, in unnecessary damage, loss or harm such as physical or mental injury to a patient, staff, visitors or members of the public. A serious incident requiring investigation is defined as an incident that occurred in relation to NHS-funded services and care resulting in for example Unexpected or avoidable death of one or more patients, staff, visitors or members of the public; Serious harm to one or more patients, staff, visitors or members of the public etc. SM Solihull Model Solihull Approach is an integrated model of working, open learning resource packs and training programme for care professionals working with families, babies, children and young people who are affected by emotional and behavioural difficulties. Norfolk Community Health and Care NHS Trust STEIS Strategic Executive Information System A system to collect data for the Department of Health. All serious incidents requiring investigation (SIRIs) are recorded onto this system by all NHS organisations SOP Standard Operating Procedure A SOP is a description of what staff are required to do in a particular situation; this may be to fulfil the requirements of a guideline, policy, procedure or national guidance. It contains the specific steps to be followed to complete the required procedure SystmOneSystmOne SystmOne is a centralised clinical system that provides healthcare professionals with a complete management system. TDA Trust Development Authority The NHS TDA will play its part in safeguarding the core values of the NHS, ensuring a fair and comprehensive service across the country and promoting the NHS Constitution. It will be accountable nationally for the outcomes achieved by NHS Trusts and for financial stewardship within the NHS Trust system as it is wound down. TMT Trust Management Team A Team that comprises the Executive Directors, Deputy and Assistant Directors of the Trust. TTO “To Take Out” This is the literal meaning Other Trusts sometimes use the term “TTA” – “to take away”. It relates to medications to take home. Quality Account 2014/15 – Glossary 75 TUPETransfer of Undertakings (Protection of Employment) Regulations 2006 The purpose of the Transfer of Undertakings (Protection of Employment) Regulations is to protect employees if ownership of their employer changes hands. UCC Urgent Care Centre During 2013 plans were developed with other providers across the county in conjunction with the Urgent Care Network and CCGs, to set up an Urgent Care Unit at the Norfolk and Norwich University Hospital. The unit was piloted in November and December over two weekends and went live on 20 January 2014, to run over the period of winter pressures. VTE Venous Thromboembolism A blood clot that forms within a vein. WaterlowPressure Ulcer Risk Assessment and Prevention Tool Waterlow pressure ulcer risk assessment/prevention policy tool is, by far, the most frequently used system in the U.K. and it is also the most easily understood and used by nurses dealing directly with patient/clients to assess risks of the individual. XenApp XenApp XenApp is a type of software programme that runs on a PC or laptop to allow users to connect to their corporate applications. It can host applications on central servers and allow users to interact with them remotely or deliver them to user devices for local execution. Head Office: Elliot House, 130 Ber Street, Norwich NR1 3FR Online: www.norfolkcommunityhealthandcare.nhs.uk Telephone: 01603 697300