Quality Account 2014 – 2015
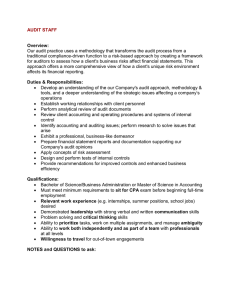
advertisement

Quality Account 2014 – 2015 PART 1 Statement on Quality from Chief Executive and Chairman Introduction Calderstones Partnership NHS Foundation Trust is a specialist learning disability service, authorised on the 1st April 2009 by Monitor the Independent Regulator for Foundation Trusts. The Trust provides forensic and high support services to people with learning disabilities. We are pleased to present on behalf of the Board the Trust’s annual Quality Account for 2014-2015. This publication provides the detail on how we have improved the quality of services as outlined within last year’s Quality Account, together with the forthcoming year’s quality improvement priorities. We have a continued commitment to deliver high quality person centred services to people with learning disabilities, who have complex and challenging needs. For those that require care in a secure environment the level of security is based on the least restrictive option, commensurate with the degree of risk to the service user, staff and public. The purpose of our Quality Account is twofold. Firstly to demonstrate accountability to our service users, carers, commissioners, staff and the public for the quality of services we deliver. Secondly, to ensure the Trust Board assesses and reports on quality across all of the healthcare services we provide. It demonstrates that the leaders, Clinicians, Governors and staff are committed to continuous, evidencebased quality improvement. The principle aims of this publication are to demonstrate: • That we continuously review the quality of our services • That we are transparent in our reporting of this information, reporting both where we are doing well, and where improvement is needed. • The improvements plans we have for the forthcoming year • How we provide information on the quality of services to service users and other stakeholders, inclusive of our governors • Our organisational accountability to the Service Users, Commissioners, Staff, Governors and other relevant stakeholders. • How we enable Service Users, Commissioners, Staff, Governors and other relevant stakeholders to review your services, comment on performance and identify priorities for improvement. 1 Our mission as a Foundation Trust is to promote recovery and quality of life through effective, innovative and caring health, social care and specialist community services. The best interests of our service users are at the heart of this. Our vision, 'changing lives through excellence’, has been defined by our three clear strategic aspirations: To deliver life-changing outcomes for our service users To be the provider of choice for learning disability services To be recognised nationally as the industry lead for learning disability services The Trust’s commitment to continuous quality improvement is based on its shared values of: Trust - We keep our promises Excellence - We continuously strive to deliver the highest standards of care Compassion - We show empathy and are sympathetic to the needs of others Respect - We engage, listen to and value the contribution of others Ownership - We are responsible and accountable for our individual and collective actions Communication - We are open and honest in our communication Partnership - We work together with clients, carers, colleagues, commissioners and communities It is a year since we introduced our Clinical Quality Strategy which underpins the Trust’s Quality Account. This provides us with the opportunity to reflect on the past year to both highlight the key achievements and forthcoming challenges for 2015 2016. There has also been a significant improvement in the provision of physical healthcare with an extensive review of the annual health check and the monitoring of people taking antipsychotic medicines. There has been an emphasis on embedding organisational learning across the Trust; we hosted our first learning event in October 2014 focusing upon the family/carer experience. Whilst this was challenging for our staff there has been an increased momentum to build and develop our engagement with families and carers. The organisational learning event and the Triangle of Care have been a platform on which to improve our partnership working with families and carers. At an event in March 2015, a large number of family members attended to hear about future strategy and to discuss all aspects of care with directors, senior staff and experts. Carers voiced their views and agreed to move forward with their involvement in our services and learning disability provision. We also announced that the Carers' Trust have awarded Calderstones their Gold Star; a powerful 2 recognition of our partnership with family members. We were proud to share that with carers and recognise the work we do together. We are particularly proud as an organisation of the achievements of the service user activist group ‘The Avenue’. The Avenue, a Lesbian Gay Bisexual and Transgender group was set up following a direct request from service users with these backgrounds for a support group, to tackle stigma and as a forum for service users to talk about things to do with their sexuality in a non-judgemental and safe setting. In a recent research study related to the group the outcome was that service users reported improved self-esteem and self-confidence: these factors are thought to influence some forms of offending, so it is important to tackle them. The Avenue was shortlisted for a major national award in the ‘Tackling Stigma’ category National Service User Awards 2015. Another of our service user led groups is the ‘Media Crew’, which is made up of service users from across the Trust. They design and create their own information, including pamphlets and videos about Calderstones. The Media Crew are systematically producing a range of accessible information including the “Welcome to Calderstones pack”. They have developed in film and song a description from a service user perspective of the importance of working in partnership with staff to move along their care pathway. The Trust is committed to investing in modern facilities that meet national specification. The provision of modern purpose built units at Maplewood has enabled us to decommission our oldest facilities at Chestnut Drive. We are also making major changes to West Drive, redesigning our wards, and putting new facilities in place. Fundamental to delivering clinical quality has been the programme of themed director visits to clinical areas. These visits have highlighted issues for wards with regards to food quality and recruitment challenges, and also emphasised the areas of good practice, such as the quality of agency staff induction and the improvements in the ward environments. Whilst acknowledging the achievement from the 2014 2015 period the Care Quality Commission Review together with our Specialist Commissioners Performance Quality Reviews have required us to focus upon key themes. The feedback from these sources include a number of issues which the Clinical Quality Strategy already acknowledges, however, there are other areas that require a sharper focus in the forthcoming year and feature within the priorities for improvement in 2015-2016 detailed in this Quality Account. These themes include ensuring the Trust achieves and maintains high standards of cleanliness, improving the governance systems with regards to Mental Health Act administration, and reviewing the workforce in terms of capacity and capability to deliver safe and effective care. In addition, following the publication of the Department of Health ‘Positive and Safe’ (April 2014), ensuring the Trust delivers its objective to reduce restrictive practices and eliminate prone restraint. Furthermore, we want to build on our commitment to ‘patient safety’ through the national ‘Sign Up to Safety’ campaign. We have committed to focus on areas that include improving 3 our environments to make medicine administration safer, reducing all omitted medicines, ensuring the reduction of restrictive practices are clinically led, embedding and improving organisational learning by continuing to host learning events, and developing safer seclusion environments through technological developments. The annual staff survey is an important activity in understanding the things that are important to staff. It is the cornerstone of ensuring that the principles and values set out within the NHS Constitution are maintained. Furthermore as part of the NHS in England the 7 pledges outline what staff should expect from NHS employers. The pledges are part of the commitment of the NHS to provide high-quality working environments for staff. Calderstones is proud of its organisational development activity and a key activity is the Trust’s communication strategy which has played an important role. The Trust is committed to engaging with service users, people who work with us as well as local people, communities and other stakeholders to improve services and make changes that are beneficial to all. Our vision, strategic aspirations, values and behaviours set out an organisational commitment. The benefits of effective engagement are very relevant for the transformation of the Trust. The staff survey results for 2014 evidence the importance of a culture of engagement and the Trust’s position in the top 20% for engagement. We appreciate that if people who work for us are fully engaged in the vision they are more likely to maintain performance through change and challenge. They are also more likely to contribute to innovation, business improvement, and provide higher rates of discretionary effort. Furthermore, effective engagement is also an opportunity to improve the organisation brand within the local community and will attract and retain talent. The staff survey will further inform the Trust through local action plans of how to respond and build upon the results. We have implemented a range of innovative staff consultation programmes. These include devising a Staff Charter; the Chief Executive’s “Big Conversation” and “Big Breakfasts Meetings”; implementation of regular ward visits from senior managers; a refreshed staff suggestion scheme; staff awards that supported innovation and Trust Values was launched; and a range of meaningful activity to engage staff at all levels was put in place to discuss the key issues in the organisation. We have a commitment to listen and act upon the things that are important to our workforce. As part of the wider organisational development activities; the Trust is committed to implementing new and innovative ways of working. In 2015, the Executive Team will participate in an Executive Development Tool; the Trust will implement a Cultural Assessment and will ensure that all first line managers receive leadership training. Our vision for delivering continuous quality improvement is to ensure that efficiencies drive quality as opposed to efficiencies delivered at the cost of quality. As a Trust, we have embedded vision, values, and strategic direction. We continue to invest in our staff through leadership programmes to ensure they have the knowledge, skills and capacity to meet the challenges of ensuring our services are efficient, high quality and good value. This quality account ensures we have a system in place to ensure implementation and measurement of our quality priorities. 4 As the Chief Executive and Chairman, we are proud to lead the Trust’s commitment to clinical quality and work with key partners, which include the people who use our services, staff, the Board, Governors and Commissioners. The Trust’s aspiration is to deliver the highest possible standards of clinical quality and deliver our vision of “changing lives through excellence”. The directors are required under the Health Act 2009 and the National Health Service Quality Accounts Regulations to prepare quality accounts for each financial year. Monitor has issued guidance to NHS foundation trust boards on the form and content of annual Quality Reports (which incorporate the above legal requirements) and on the arrangements that NHS foundation trust boards should put in place to support data quality for the preparation of the Quality Report. The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Report. By order of the Board NB: sign and date in any colour ink except black Mark Hindle Chief Executive Rupert Nichols Chairman 5 PART 2 2.1 Priorities for Improvement 2015-2016 The Quality Priorities outlined within this year’s Quality Account have been developed in consultation with a number of stakeholders, not only reflecting what is important to people using our services, staff and governors, but are also aligned to the CQC inspection in 2014, the Improving Lives Review as part of the Winterbourne Joint Improvement Programme and the Trust’s strategic objectives for quality. Our Clinical Quality Strategy 2013-2018 (revised 2014) describes the detail of how we will ensure quality remains at the heart of how we plan and deliver our services over the next five years. This Clinical Quality Strategy 2013 - 2018 brings together all the aspects that contribute to high quality services: our five year Integrated Business Plan (IBP); Workforce Strategy, Commissioning for Quality and Innovation Schemes (CQUIN), Quality Account, and Carer Strategy. It describes the intentions of our Trust to continually improve the quality of our services and the experiences of people who use our services. Implementation of the Clinical Quality Strategy includes: • Agreeing and promoting quality priorities within services to meet the Trust strategic goal • Raising awareness of what drives quality by defining our quality priorities • Promoting leadership at all levels to deliver the quality priorities • Creating an understanding of the role and contribution every staff member can make to improving quality • Promoting individual responsibility for taking action to improve safety, experience and outcomes for the people who use our services, their families and staff We have defined what ‘quality’ means to the Trust through the following five commitments: • Commitment 1: Maintaining the very highest standards of care We will demonstrate this by comparing ourselves with other services, checking and auditing that we are meeting our own and national standards, and acting on and learning from feedback from the people who use our services. 6 • Commitment 2: A promise to continuously strive to improve the quality of services We will demonstrate this by active involvement in research at a local, national and international level. We will continue to invest in developing services that are modern and fit for purpose. In addition, we will keep our staff up to date with the specialist knowledge to deliver best practice in the treatment and care of the people who use our services. • Commitment 3: Responding to the changing needs of people who use our services and those who commission them We will demonstrate this by engaging and working collaboratively with people who use our services, their families and carers, and our commissioners. We will be the forefront of developing services by responding to the needs of the population we serve and develop effective treatment and therapy to ensure they progress as quickly as possible • Commitment 4: Safeguarding the welfare of the people we care for We will demonstrate this by ensuring we understand the risks that affect the people we care for and develop plans to protect and ensure the safety of all who use our services. • Commitment 5: Listening and responding to the people we care for, their families and carers, staff and partners We will demonstrate this by offering choices and opportunities to the people we care for to influence service delivery and their own personal treatment and care. We will ensure that treatment and care is personalised, flexible and responsive to each and every individual. Our Clinical Quality Strategy also takes account of the quality framework as outlined within High Quality Care for All (DH, 2008): • Patient Experience • Patient Safety • Clinical Effectiveness 7 The priorities for 2015-2016 also include the Commissioning for Quality and Innovation (CQUIN) payment framework. The CQUIN payment framework enables commissioners to reward excellence, by linking a proportion of English healthcare providers' income to the achievement of local quality improvement goals. Title: Priority 1: Positive and Safe at Calderstones Why are we doing it? In April 2014, under the auspices of the national Positive and Safe Programme, the Department of Health published the guidance framework ‘Positive and Proactive Care: Reducing the Need for Restrictive Interventions’. The guidance required providers of health and social care services to develop organisational restrictive intervention reduction plans, with a particular emphasis on the elimination altogether of prone restraint. Development of a more therapeutic culture, together with an explicit focus on recovery and positive behavioural support, were highlighted as key components of strategy. The revised Mental Health Act Code of Practice, which comes into effect in April 2015, builds on the guidance set out in Positive and Proactive Care, and provides further direction on achieving best practice. The Trust’s response is described within the ‘Positive and Safe at Calderstones’ programme, which was agreed by the Executive Management Team in November 2014, and is reported to the Quality and Risk Committee on a monthly basis. How will we measure success? The programme is comprised of three constituent projects. The first of these aims to create a more conducive and therapeutic culture and promote excellent nursing practice through systematic implementation of the ‘Safewards’ model, created by Professor Len Bowers. The second focuses on workforce development, through roll out of a competence framework for positive behavioural support. This will have two key elements: the principles of applied behavioural analysis, captured within primary and secondary preventative strategies; and review of tertiary strategies, with a particular focus on physical intervention and development of viable alternatives to prone restraint. The third and final project is concerned with the use of data to inform good practice. Monitoring overall trends in the frequency of restrictive interventions, and sharing this information with frontline staff is a key workstream, together with a series of audits designed to measure the quality of our positive behavioural support plans, post-incident debriefs, and the extent of service user, family and carer involvement in treatment and care planning. Success will be measured in two main ways: process and outcome. In terms of process, each project now has a detailed project plan with key deliverables and 8 timescales clearly identified. Project groups provide a monthly highlight report to the programme board, detailing their progress against delivery of the milestones, which in turn is reported to the Trust’s Quality and Risk Committee. In terms of outcome, the ultimate test of the success of the programme is being monitored through ongoing measurement of the frequency of restrictive interventions against the trajectories one would expect to see following implementation of Safewards and positive behavioural support. Other performance indicators will also include comparison of before and after measures relating to staff and service injuries, sickness absence, and patient reported outcome measures. Priority 2:Credits 4 Cleaning (C4C) Why are we doing it? A clean, uncluttered, and attractive environment can make a lot of difference for a person’s attitude and overall mood, and ultimately their recovery. A clean environment is fundamental to promoting self-care and maximising independence for a lasting recovery. The Health and Social Care Act 2008 (Regulated Activities) Regulations 2014 Regulation 15 Premises and equipment states all premises must be ‘clean’. The National Specification for Cleanliness in the NHS: A Framework for Setting and Measuring Performance Outcomes (NPSA 2007) is a key priority for the NHS. Alongside the Code of Practice on the Prevention and Control of Infections and related guidance (DoH 2010), places further responsibility on NHS Trusts to ensure that local provision of cleaning services are adequately resourced and defined through strategic cleaning plans and schedules. This ensures that service users the public and staff know what they can expect. Improving and sustaining levels of cleanliness is important if the Trust is to improve the overall quality of care and experience of people and staff using our services. In the 2014 CQC inspection, it was highlighted as an area that must be improved by the Trust. The Ward Manager has a key role in ensuring that national standards of cleanliness are consistently achieved and that the experience of people using our services are not overshadowed or recovery delayed because of a failure to provide a clean safe environment. The C4C software, was produced with the support of the Department of Health, for the NHS by the NHS, it assist Domestic Services Managers, Clinical Nurse Managers and Ward Managers to set, flex and manage cleaning specifications and standards in Hospitals; monitor performance and comply with National Standards. Enable the Clinical Nurse Manager or Ward Manager to regularly adjust their 9 functional area cleaning specification to meet the changing needs of their service users. How will we measure success? • • • • • By identifying a cleaning specification for all areas Ensuring that all cleaning services are properly deployed and balanced across all areas of the Trust Providing a comprehensive management tool to produce reports on almost any aspect of cleaning Ensuring that monthly monitoring leads to significant improvement in the standards of cleaning particularly across ward areas Improved feedback scores on standards of cleanliness from people using our services Priority 3: Ward Accreditation Scheme Why are we doing it? There is an emphasis within NHS services to ensure that minimum standards of care are met through regulation. However, it is equally important to ensure there is a coherent and comprehensive approach to recognising teams that provide excellent standards of care. Ward Accreditation is a way of recognising the teams that focus upon improving quality and has the potential to initiate healthy competition among clinicians to provide the better care Following Winterbourne, the Francis Inquiry and other reports into the failures of the health systems in England, ward accreditation is gathering momentum. For Calderstones partnership NHS FT the recommendation was raised following the CQC inspection in 2014 and was advocated as a system whereby the Board could obtain assurance on quality, safety and compliance of services. Ward Accreditation Schemes: • • • • Improve quality, experience and safety Provide a level of assurance about the quality of care and standards on wards Inspire trust and confidence for service users, families and key stakeholders in the quality of care Support clinical managers to understand how they deliver care, identify what works well, and where further improvements are needed. 10 How will we measure success? In 2015-2016 the Trust will ensure: • • • • • • • A framework of standards is developed that supports quality improvement and regulation compliance All clinical areas are assessed the framework of standards There are demonstrable improvements in services as a result of assessment A process to improve quality, experience and patient safety To provide a level of assurance about the quality of care and standards on wards To inspire trust and confidence for service users, families and key stakeholders in the quality of care To support clinical managers to understand how they deliver care, identify what works well and where further improvements are needed. Priority 4:Eliminating Omitted Medicines without Clinical Reason Why are we doing it? The Francis Report into Mid Staffordshire Hospitals recommends ensuring that medicines are given on time and that it is the responsibility of the ward manager to ensure this happens. Although the NPSA Rapid Response Report 009 Reducing Harm from omitted and delayed medicines in hospital came out in February 2010 citing an incidence for omitted doses of 5% it would appear there is still room for improvement. Omitted medicines are still seen in reports to the National Patient Safety Agency (NPSA). The NPSA as part of NHS England in the Patient Safety Directorate is introducing a Medicines Safety Thermometer, which will include Omitted Medicines. Locally the Trust has been extensively monitoring omitted medicines over the last year with particular emphasis on critical medicine omissions. For 2015-2016 we want to focus our attention on all medicine omissions. This involves reviewing the supply, prescription and administration of medicines. There are planned changes to the Medicine Administration Card to ensure clearer prescriptions and easier to follow for nurses in the administration process. We are also reviewing administration processes to review to ensure less distraction. There is also ongoing reviews of supply from pharmacy services. 11 How will we measure success? In 2014 the numbers of omitted medicines have been volatile and there has been no pattern of consistent improvement. Figure 1 Omitted Medicines without Clinical reason in 2014 This project aims to ensure that omitted medicines of any type becomes a rare event Priority 5: Integrated Treatment and Care Planning Why are we doing it? The Trust’s CQC Inspection in 2014 highlighted concerns with the treatment, care and support planning for the people using our services. Whilst committed to partnership and involvement the overall judgement was that the Trust’s systems included multiple formulations; different perceptions of the service users and no central resource or document. This made it difficult to demonstrate how the service user was moving through the care pathway and how they were co-creators in their plans. This has also been acknowledged through local audit processes. The Trust will review the care planning process to ensure clear evidence for: • • • • • • Whole Person Approach Comprehensive Assessment Identify Dynamic Factors Targeted needs Treatment Hierarchy and priority needs Co-creation 12 • • • Strengths and abilities Multidisciplinary Single source documentation How will we measure success? The Trust will solicit feedback from key stakeholders which includes service users, carers and families and key stakeholders to test if we are meeting are key objectives as outlined above. The Trust also anticipates an improvement in audit results given the single source documentation should make evidence easier to locate. Priority 6: National Offender Management Project Why are we doing it? For several years the Trust has been leading a national piece of work on behalf of the National Offender Management Service (NOMS) to improve outcomes for offenders with leaning disability. Most recently, this has been in the form a jointly funded project to work with prisons and probation services to improve delivery. To date the project, which is led by the Forensic Support Service, has successfully developed a range of tools to enhance practice , lead the development of a clear practice framework and helped NOMS to revise its national strategy. Work on implementation across all prisons and probation services, is currently under way at NOMS. The project was scheduled to finish at the end of March, but has now been extended in order to support two important pieces of work across prisons. How will we measure success? The first is the national review of suicide and self-harm. NOMS has established and requested Calderstones to lead a workstream reviewing the experience and needs of offenders with learning disability. It is expected that this work will produce recommendations by October. The second strand is for the project to support a broader Safer Custody Review at NOMS, with a specific emphasis on improving reception and induction processes for offenders with learning disabilities. 13 Priority 7: Commissioning for Quality and Innovation (CQUIN) 2015-2016 The Commissioning for Quality and Innovation (CQUIN) aims to enhance the treatment and care pathway through the work delivered as part of a payment framework. A proportion of the Trust’s income in 2015-2016 will be conditional upon achieving quality improvement and innovation goals agreed between the Trust and the commissioners through the payment framework. The Trust is committed to improving the quality of services through the innovation and improvement scheme. The CQUIN Projects for 2015-2016 for NHS England and East Lancashire CCG include: • • • • • Secure Service Users active engagement programme Supporting service users in secure/specialised services to stop smoking Supporting Carer involvement in Mental Health Improving Physical Healthcare to reduce premature mortality in people with severe mental illness o Cardio Metabolic Assessment and treatment for patients with psychoses Care & Treatment reviews (CTR) task & finish group 14 Part 2.2 2.2.1 Review of Services Statement of Assurance from the Board During the reporting period 2014-205 Calderstones Partnership NHS Foundation Trust provided for people with a learning disability: • Specialist on-site in-patient services inclusive of: Assessment and treatment service Secure service provision Enhanced services Rehabilitation services • Specialist forensic outreach support service Calderstones has reviewed all the data that is available to them on the quality of care in the above NHS services (inclusive of social care provision). The income generated by the NHS services reviewed in the reporting period 2014-2015 represents 89.23% of the total income generated from the provision of NHS services by the Trust for the reporting period 2014-2015 2.2.2 Participation in Clinical Audits During 2014-2015 the Trust was not eligible to participate in 1 national clinical audit 83 cases were submitted which is 100% of eligible cases. The national clinical audit that Calderstones Partnership was eligible to participate in during 2014-2015 was Physical Healthcare: National Schizophrenia Audit. The report has not yet been published but Calderstones Partnership will address any recommendations made in respect of the audit. There was a nil return for the Trust response to the National Confidential Inquiry into Suicide and Homicide by People with Mental Illness (CISH) covered NHS services that the Trust provides. The reports of 32 local clinical audits were reviewed by the provider in 2014-2015 and the Trust intends to take action to improve the quality of healthcare provided [See Appendix C for list of clinical audit topics and brief synopsis] All of the Trust’s clinical audits are presented to and reviewed by the multidisciplinary Clinical Audit Committee. Selective reports are presented to the Quality and Risk Committee (as a subcommittee of the Trust Board) and provide the assurance that quality issues are being addressed at Board level. The Trust encourages all 15 services to be quality focused and as such encourages all clinical areas and disciplines to participate in the review of services through clinical audit. 2.3.3 Participation in Clinical Research The number of patients receiving NHS services provided or sub contracted by Calderstones Partnership NHS Foundation Trust in 2014-2015 that were recruited during that period to participate in research approved by a research ethics committee was 75. Other studies have recruited staff numbers (19 participants), and family/carers of people supported by the Trust (3 participants so far). The level of participation in clinical research demonstrates Calderstones Partnership NHS Foundation Trust’s commitment to improving the quality of care offered and to make a contribution to wider health improvement. Calderstones Partnership NHS Foundation Trust was involved in conducting 15 clinical research studies. The Trust completed 100% of these studies as designed within the agreed time and to the agreed recruitment target. The Trust used national systems to manage the studies in proportion to risk. Of the 15 studies given permission to start, 15 were given permission by an authorised person less than 30 days from receipt of a valid complete application. 15 of the studies were established and managed under national model agreements and 2 of the 15 eligible research involved used a Research Passport. In 2014-2015 the National Institute for Health Research (NIHR) supported 2 of these studies through its research networks, with 2 further external studies also given permission from Calderstones through the NIHR portfolio. 2 of the 15 studies recruiting in 2014-2015 were registered on the NIHR portfolio and recruited a total of 5 people (4 patients and 1 staff). In total 5 studies on the NIHR portfolio remain open and eligible to recruit from the Trust; 2 closed during 2014/15. In the last three years 25 publications have resulted from our involvement in clinical research or innovative practice at Calderstones, helping to improve patient outcomes and experience in this specialist field. Of these, 1 paper and 2 book chapters in 2014-2015 relate to the first NIHR portfolio study sponsored by Calderstones and there have been further papers and conference / exhibition / workshop papers submitted in relation to this study during 2014-2015. The Trust has established working partnership links with Lancaster University and continues to be a member organisation of the Lancaster Health Hub (formerly known as the Clinical Research Hub), working collaboratively in developing research proposals. 16 2.3.4 Goals Agreed with Commissioners – The Use of CQUIN Payment Framework A proportion of the Trust’s income in 2014-2015 was conditional on achieving quality improvement and innovation goals agreed between the Trust, NHS England – North of England Specialised Commissioning and East Lancashire CCG (on behalf of 17 Associate CCGs within the North West). The amount of income for 2015/16 is £34.4m and is conditional upon achieving quality improvement and innovation. The Trust achieved the indicators in 2014/15 and successfully received the payment of £877k. Table 1 2014-2015 Payment Schedule for CQUIN Goals Contract Income East Lancashire CCG (on behalf of 17 North West Associate CCGs) 2014-2015 Contract CQUIN Total North of England Specialised Commissioning £000 £000 8,182 26,863 205 672 8,387 27,535 The Trust continues to work with the North of England Specialised Commissioning Team and the Clinical Commissioning Groups (CCGs), to agree goals that reflect measured improvements in the performance of quality The Trust is required to undertake a CQUIN Programme for the period 2015-2016 which is 2.5% of contracted income which amounts to £839k. 2.3.5 Statements from the Care Quality Commission The Trust is required to register with the Care Quality Commission and its current registration status is registered to carry out the following regulated activities: 17 • Treatment of disease, disorder or injury • Assessment or medical treatment for persons detained under the Mental Health Act 1983 • Accommodation for persons who require nursing or personal care The Trust is registered without conditions. During 2013-14, the Trust identified serious weaknesses in its overall governance processes and following the commission of an independent review by Deloitte and receipt of an enforcement notice from Monitor, a significant amount of improvement work was carried out during 2014-15. These areas of weakness were addressed and the final Quality Governance Assurance Framework recommendation was signed off during quarter three period (October to December) 2014-15. The improvements made include: • • • • • • • • • Appointment of a substantive Company Secretary The creation of a new Assistant Company Secretary post Restructure of the Trust Secretariat to provide adequate support to Board and Governors in discharging their statutory responsibilities Appointment of two Non-Executive Directors to the Board, representing an increased capacity of one NED Separation of the Director of Nursing role from the Director of Operations role resulting in the appointment of an Executive Director of Nursing & Quality The delivery of an ongoing comprehensive Board Development Programme to address the identified areas for improvement of individual Board members and the Board collectively The implementation of the revised protocol for the maintenance and monitoring by the Board of the BAF The completion of the review of Board Committees to support the governance and escalation framework The embedding of a restructured and augmented Trust Secretariat to ensure that the Board and Governors are appropriately supported to deliver their responsibilities On 29 April 2015, Monitor issued a compliance certificate, in respect of Paragraph 2 of the Trust’s enforcement undertakings accepted by Monitor on 20 December 2013 stating: 18 “…inspection of the Licensee [Calderstones Partnership NHS FT] by the Care Quality Commission in July 2014 found that some of the Licensee’s Governance systems were not effective. This was demonstrated by the quality concerns highlighted, including: failure to maintain clean ward environments and to fully implement infection control procedures; non enforcement of medicines management procedures; a lack of awareness of and failure to follow; trust policies relating to seclusion, segregation and restraint; and a failure to adequately monitor the Mental Health Act at Board level” The CQC has not taken enforcement action against the Trust during 2014 – 2015. However, following the CQC special review based upon the draft of the Mental Health Pilot Standards during July 2014 Calderstones Partnership has made the following progress by 31st March 2015 in taking such action: • • • • • • • • Introduced systems to improve practice and adherence to cleanliness and infection control. These include: • Credits for Cleaning (C4C) electronic cleanliness audit tool • Introducing ‘PLACE Lite’ Improved practices and adherence to food labelling, fridge temperature monitoring (including medicine fridges) and the maintenance of equipment, and introduced daily monitoring at ward level to ensure compliance Reviewed the policy for restraint, and taken account of the DH guidance ‘Positive Proactive Care: reducing the need for restrictive interventions’. Introduced a central register for all people requiring ‘mechanical restraint’ Developed a Mental Health Act Administrator work programme and a quarterly assurance report to the Trust Board Introduced systems to ensure emergency equipment on the wards is checked to confirm it is current, working and correctly labelled so all staff can access it quickly in an emergency. Introduced a monthly Safe Staffing Report to the Trust Board to provide assurance that appropriate resource requirements are allocated to meet the assessed clinical, relational and activity needs of service users in each area. This includes use of Agency and Bank Nurse staffing over the 24 hour period Reviewed communication treatment and care plans and for all service users, and the communication passports for those service users where needed 19 2.3.6 Data Quality NHS Number and General Medical Practice Code Validity Calderstones Partnership did not submit records during 2014-2015 to the Secondary Uses service for inclusion in the Hospital Episode Statistics which are included in the latest published data. 2.3.7 Information Governance Toolkit attainment levels The Trust score for 2014-2015 for Information Quality and Records Management assessed using the Information Governance Toolkit was 71% based upon the score of level 2 for 41 applicable items and level 3 for 3 applicable items (total 44 applicable items) and was graded satisfactory. The key features in developing the action plan for 2015-2016 include: • • • • • • • Standardising clinicians approach to coding for consistent use of primary/secondary diagnosis codes Review of systems/data to ensure appropriate recording and reporting in line with NHS Data Dictionary Review processes for clinical staff validating care records following recent changes to allow support worker involvement in confirming notes Monthly MHLDDS being provided by Information Manager to HSCIC and Information Governance Steering Group Further development of Informatics intranet page as a means to enable staff awareness Routine spot check reports to be provided to Information Governance Steering Group Review related procedures to incorporate any additions or amendments supporting the above work 2.3.8 Clinical coding error rate The Trust was not subject to the Payment by Results clinical coding audit during 2014-2015 by the Audit Commission. 20 PART 3: 3.1 Review of Quality Performance: Priorities for Improvement 2014-2015 In June 2014 the Trust produced its fifth Quality Account aligned to the Trust’s quality commitments as outlined in the Clinical Quality Strategy 2013-2018 and the quality framework of patient safety, patient experience and clinical effectiveness. The following section outlines what we have achieved over the past year both against our quality improvement priorities and our quality dashboard. Testing the Vision and Values of the Organisation In 2013-2014 a the Trust vision, values and strategic aspirations were revised (see figure 2) to ensure the Trust’s workforce has a common purpose of providing high quality services. During 2014-2015 we have been integrating the values to develop an organisational culture that fits the Trust’s vision. Implicit to the achievement of the Trust’s strategy is the core values and associated behaviours, which respond to the current and changing needs of our service users. Figure 2 Director Walkabouts One of the means of testing the values of an organisation is through ward based director visits. Board members undertake both Director Walkabouts and ‘Patient Safety Visits’ for the purpose of visiting service users, staff and clinical areas to 21 ensure: • • • • Through visibility and familiarisation directors, staff and service users establish ‘trust’ and ‘communication’ channels. Board members become an integral part of developing and recognising ‘excellence’ By taking ‘ownership’ of ward based quality issues Board members can work in ‘partnership’ with clinical teams Providing service users and staff with an informal opportunity to give the Board a window of insight as to what it is like to live and work in Calderstones shows ‘respect’ and ‘compassion’ During 2014-2015 the following themes and issues have emerged as part of the Director visits schedule: Medicine Management Staff talked frankly about their concerns about medication safety and the number of initiatives to support improvement. There were risk factors identified as part of the visits, which include location of medication cupboards in older ward; this currently part of a programme of review, and general distractions in the ward environment. The Directors were also able to discuss the staffs’ protective plans to try and prevent medication errors, such as; stable staff teams; service users not moving wards without good clinical reason; briefing of registered nurses on a daily basis regarding medication changes; and lessons learned from medication errors being briefed to staff. Physical Healthcare Staff reported to Directors that they received good support from the Trust Health Centre. Additional support was identified from Specialty Doctors especially those who have primary healthcare experience. However, Directors noted differences in health provision for service users living away from the Calderstones site. These service users were registered with local GPs and the Directors were seeking assurance that these service users were receiving an equitable service. As a result, any gap in local provision will be filled via access to all the health services on the Calderstones site. Clinical Audit The Trust’s annual clinical audit programme is aligned to the Trust quality commitments with the principle emphasis upon delivering ‘excellence’ through ‘ownership’, ‘partnership’ and ‘communication’. 22 The effectiveness of clinical audit is underpinned by ensuring audit projects are relevant. Concerns regarding clinical care are often identified through clinical governance structures. Within the Trust, it is these concerns alongside national guidance that inform our annual programme. 1. Service user views or complaints. 2. Adverse incident/near miss reporting 3. Identified local priorities or concerns Within the 2014-2015 Clinical Audit Programme we have aimed to increase the number of NICE audits to 10 completed audits, Appendix C outlines the Trust’s achievements to completing this objective. However, it is locally driven audits that are driving improvement most notably with Medicine Management, linking to Director Walkabouts and adverse events and ensuring improvement in standards of record keeping. With the emphasis on restrictive practices, the clinical audit programme has audited seclusion practices, rapid tranquillisation and positive behaviour support plans. There has been significant improvement work in terms of redefining standards and improving record keeping compliance. These audits also triangulate with surveys undertaken with both service users and carers, ensuring ‘compassion’ and ‘respect’ are at the heart of clinical practices. Physical Health Monitoring In 2014-2015, we extended our commitment to improve the physical health monitoring of service users, both in relation to their general physical health and increased monitoring around those people who take antipsychotic medicines. People with learning disabilities are known to have increased risks of health problems compared to the rest of the population. They are also less likely to have good access to healthcare services. Therefore, we committed to provide an annual physical health check for all service users but also complex case management support from a dedicated advanced nurse practitioner for service users with a long term health condition. We have implemented a standardised ‘annual physical health check’. Monitoring of annual health check is completed every month as part of the Quality Dashboard, average compliance score is 98.66%, not quite meeting 100% target. Nevertheless there have been significant improvements both in relation to engagement and completion of checks. The Advanced Nurse Practitioner role is using the ‘complex 23 case management’ model and has made good progress in helping service users who usually find the health check too distressing to have active monitoring of their health. In support of the annual health check the Trust has also started using the Health Equalities Framework (HEF) (iHAL, 2013) as part of the CQUIN programme. The HEF is a tool that provides overarching health-focused outcomes framework which informs and supports both commissioning and service provision and across health and social care settings. We have compiled a database of all current service users’ physical health conditions. Analysis is underway of the data compiled in order to write a profile of physical health needs for the Trust population, completed at the end of March 2015 and will be used to inform the development of a health inequalities strategy during 2015/16. This will support the Trust physical health steering group to target resources to the areas of most need for the health of the service user population. In addition to the annual health check we have ensured that all service users prescribed antipsychotic medication receive comprehensive physical health screening. Antipsychotic medicine can help people as part of the recovery process but there are also risks to health with long-term use that can be addressed if regular health checks are completed. To achieve this we have developed a set of standards and a reporting process in the healthcare record aligned to the standards. This is administered via a centralised clinic at the Health Centre, which also incorporates a recall process. This is audited twice a year and the audit results continue to show better systems for monitoring and following up people who have not attended via a dedicated clinic. Figure 3 gives an overview of the results from audits in 2013 and 2014. There still needs to be improvement in record keeping for ward-based health monitoring in particular BP and BMI. 24 Figure 3 2013 and 2014 Comparison 100% 89% 87% 88% 69% 58% 56% 60% 43% 40% 84% 80% 80% 29% 30% 32% 98% 92% 69% 60% 2013 43% 2014 27% 20% 0% BMI BP Blood Liver Glucose Function Lipid Profile U&E FBC Prolactin ECG In addition to physical health monitoring associated with antipsychotics we also continue to embed the use of the Liverpool University Neuroleptic Side Effects rating Scale: (LUNSERS) as an outcome measure from the service users’ perspective in relation to the monitoring and management of the side effects of antipsychotics. LUNSERS is a widely used self-assessment tool for measuring the side effects of antipsychotic medications. Regular reviews and discussions about tolerability are an important factor in helping people to adhere to treatment. Side–effects should be assessed in the early stages of starting any new treatment and at regular intervals throughout treatment. Side effects should also be assessed after any dose changes and at treatment review meetings. The original LUNSERS was hard for people with learning disabilities to understand so in 2012-2013 there was a Trust wide project to support people using services to develop a version of LUNSERS that was easier to understand. This included adding pictures and additional text. In 2014-2015 we developed LUNSERS as part of the care record with an inbuilt prompt response (Carenotes Assist) to notify clinicians when the person needs to review their experience of side-effects of antipsychotic medication. Development within the electronic care records will improve the regularity of review both in line with the quarterly requirement and in response to a change in clinical presentation At the point of reporting, no service users are self-reporting high levels of side effects, which is an indication of the effectiveness of monitoring and intervention by 25 the care team. This is especially important when trying to establish good medicine adherence with service users and is integral to discharge planning. Whilst there is evidence that care teams take the issue of medication side effects seriously and demonstrate strong commitment to address these for the benefit of service users, in the past 12 months the wards have not achieved the target of ensuring all service users were assessed every 12 weeks. Standards for Wards Transfers An initiative introduced by the Trust last year was driven through consultation with service user Governors, and was to improve the experience for people in our service when they are transferring wards. Based upon feedback from service users their families, and from complaints information we need to improve the experience of people in our services when they are moving wards within the care pathways This was done by developing standards in partnership with the service users and support staff. A number of consultation events were held through our ‘Speak Up’ network. There were a number of key themes that emerged through the consultation process: • • • • • Orientation to the ward Having access to current and updated information Care of personal belongings Continuity of Activity Schedule Handover as part of the Care programme Approach A set of standards has been drafted to address these themes, and we were hoping to audit the implementation and compliance during 2014-2015, however, this has not been possible so this has been added to the audit programme for 2015-2016. We will also continue to monitor feedback on ward transfers through our complaint data. MaPSAF Analysis Report 2014 Background and Introduction The Manchester Patient Safety Framework (MaPSAF) was originally developed for use in primary care services by Manchester University. The framework is based on Ron Westrum’s (1993) theory of organisational safety – “organisational personality”, used within the oil industry but developed for further use in acute, mental health, ambulance settings 26 MaPSAF covers nine dimensions of safety: 1. 2. 3. 4. 5. 6. 7. 8. 9. Overall commitment to quality Priority given to patient safety Perceptions of the causes of patient safety incidents and their identification Investigating patient safety incidents Organizational learning following PSIs Communication about safety issues Personnel management and safety issues Staff education and training about safety Team working around safety issues Patient safety is a complex multidimensional concept; using the tool enables the Trust to self-reflect on our maturity as a learning organisation, and how we continue to develop and embed patient safety across the Trust. It also supports and stimulates discussion about the strengths, weaknesses and differences of the patient safety culture within teams across the Trust. MaPSAF also helps us evaluate any specific intervention to change the safety culture In 2011, Calderstones developed MaPSAF Mental Health (NPSA, 2006) into an online survey tool, and have been collecting data between 2011 and 2014. In 2014, this was part of the local CQUIN Programme. The principle behind interpreting the result is that the more scores obtained at the lower end of the scale the less safe an organisation is and the more score at the upper end of the scale the organisation is deemed safer. The respective dimensions are measured against the following criteria: • • • • • A – Pathological - Why do we need to waste our time on patient safety issues? B – Reactive - We take patient safety seriously and do something when we have an incident C – Bureaucratic - We have systems in place to manage patient safety. D – Proactive - We are always on the alert/thinking about patien that might emerge. E – Generative - Managing patient safety is an integral part of everything we do. We hope to be able to demonstrate that our feedback results are predominantly in the ‘D and E’ dimensions and that year on year comparison show improved ‘patient safety culture’. 27 2014 MaPSAF Results Figure 4 Profile of results across all MaPSAF dimensions An initial glance of the profile of results; the Trust has achieved the objective of ensuring the results of the survey are predominantly weighted towards ‘D – proactive’ and ‘E – generative’ results, for all dimensions these responses sets are the highest, with the exception of ‘7 – Personal management and safety issues’. This is clearly the area that suggests a need for improvement. The chart below (figure 5) gives an overview of the average results across all dimensions for the five response sets and that gives a good indication that the Trust is receiving positive feedback with regards to ‘safety culture’. 28 Figure 5 Average scores across all dimensions 2014 When reviewing the results for the three data collection periods of 2011, 2013 and 2014 (table 2) there is no evidence that the Trust has achieved its objective of year on year improvement, however, neither is there a concerning picture of declining results. There is good evidence of variation of responses across all domains and reporting periods, which gives an indication that staff have made considered responses to each question. The survey was completed anonymously and no demo graphic information has been collected. For 2015 the Trust intends to develop the survey to identify clinical groups or care pathways so we can focus our efforts with regards to patient safety. Table 2 Comparison of Results for 2011, 2013 and 2014 APathological 'Why do we need to waste our time on patient safety issues?' B - Reactive 'We take patient safety seriously and do something when we have an incident.' CBureaucratic 'We have systems in place to manage patient safety.' D - Proactive 'We are always on the alert/thinking about patient safety issues that might emerge.' E - Generative 'Managing patient safety is an integral part of everything we do.' 1. Overall commitment to quality 2011 2% 9% 8% 59% 22% 2013 2% 14% 7% 53% 25% 29 APathological 'Why do we need to waste our time on patient safety issues?' 2014 B - Reactive 'We take patient safety seriously and do something when we have an incident.' 1% CBureaucratic 'We have systems in place to manage patient safety.' D - Proactive 'We are always on the alert/thinking about patient safety issues that might emerge.' E - Generative 'Managing patient safety is an integral part of everything we do.' 13% 10% 57% 18% 2. Priority given to patient safety 2011 1% 17% 30% 24% 29% 2013 1% 12% 17% 34% 36% 2014 0% 15% 20% 28% 36% 3. Perceptions of the causes of patient safety incidents and their identification 2011 4% 1% 13% 36% 46% 2013 5% 1% 15% 32% 47% 2014 4% 1% 17% 36% 42% 4. Investigating patient safety incidents 2011 0% 2% 32% 24% 42% 2013 3% 7% 20% 27% 43% 2014 1% 7% 19% 24% 49% 5. Organisational learning following PSIs 2011 0% 6% 21% 43% 30% 2013 3% 4% 26% 40% 27% 2014 2% 5% 23% 39% 31% 6. Communication about safety issues 2011 3% 6% 39% 26% 26% 2013 6% 9% 34% 25% 25% 2014 5% 7% 32% 23% 32% 7. Personnel management and safety issues 2011 4% 7% 38% 28% 23% 2013 4% 15% 23% 36% 21% 2014 9% 12% 29% 31% 20% 8. Staff education and training about safety 2011 2% 2% 19% 42% 34% 2013 4% 3% 18% 41% 34% 2014 1% 5% 21% 36% 37% 9. Team working around safety issues 2011 1% 7% 15% 43% 34% 2013 5% 5% 21% 35% 34% 2014 2% 10% 22% 32% 34% 30 We have responded to this years survey results by ensuring there is an action plan in place to ensure that ‘patient safety’ continues to be embedded and at the fore across all Trust service delivery lines. Patient Safety Improvement Plan Information from the Patient Safety metrics will continue to be used to raise the quality of interventions with the Service Users; this will be shared alongside monthly incident data reports per area with the local team meetings and the Patient Safety Champions based within the Wards so that local ownership exists of the information outputs and responses required. The new risk management system (Ulysses) will be more efficient in its outputs particularly in relation to Patient Safety Incidents – this information will enable teams to respond to information trends within their own areas of responsibility. Incident Managers in closing Ulysses incidents will require a greater analysis of report content which will then be scrutinised as part of output reports for learning that has taken place. Incident requiring RCA investigation will continue to be completed using experienced investigators with less experienced investigators. Support will be delivered for the Organisational learning sessions being organised and also in the delivery of lessons learned to the NHS England Quality and Safety Network meetings. Patient Safety Walkabouts will continue with Directors of the Trust feeding back into the Board Meeting and Clinical Management Teams. Patient Safety will be delivered as a key message for all new employees as they start at the Trust via the induction programme content per topic area. Improvements to Team and Partnership working is the desire for the next MaPSAF survey in 2015. Escalation and Assurance In 2013-2014, the Trust commissioned an independent review of quality governance. This review highlighted concerns regarding how the Trust’s quality systems and organisational learning were monitored. Calderstones Partnership NHS FT Trust has developed a range of policies, systems and processes, which together comprise an integrated assurance and escalation framework. The Trust uses Monitor’s definition of quality governance as being the combination of structures and processes at and below board level to lead on trust-wide quality performance. We have introduced a number of systems and processes that support delivery of high quality care and ensure good governance. These processes enable those 31 responsible for delivering, monitoring and receiving care to provide assurance to the Trust Board and also identify and raise concerns. Staff Involvement We have a number of policies and systems, which encourage staff at all levels to be involved in monitoring quality and performance and to raise concerns about any issues. To improve this process we have introduced further engagement initiatives, all hosted by the Chief Executive, both routinely and in response to changing circumstances: • • ‘The Big Breakfast’ is a monthly engagement event, which invites all staff with a birthday in the month to meet with the Chief Executive. ‘The Big Conversation’ was our initial consultation event followed by the ‘The Big Picture’ as the Trust strategic direction continues to develop. Service User and Carer Involvement The Trust positively engages with service users, carers and the public and welcomes their involvement and feedback on how they can become more involved in decision making processes. There are a number of established mechanisms. • • • • • PALS (Patient Advice and Liaison Service) Complaints Experience surveys Involvement Forums HealthWatch Over the past year, we have developed our structures to engage with carers both via a regular six-weekly support group with a growing membership, and holding two halfday events at the weekend hosted by the Chief Executive. The feedback has been very positive and there is a commitment from the Trust to continue with these events. Reportable Issues Log A weekly Trust wide Reportable Issues Log has been introduced. The log provides comprehensive information for Board members on new significant issues that have occurred each week. The log also tracks progress on action against previously reported issues. The Quality and Risk Committee monitor the log. Reportable Issues relate to information, which has identified potential issues with quality, safety or organisation reputation. 32 Committee Structure To support the Trust Board in carrying out its duties effectively, the subcommittees reporting to the Board were reviewed. The remit and terms of reference of these subcommittees were reviewed to ensure robust governance and assurance arrangements are now in place. Each subcommittee receives a set of regular assurance reports from other committees and group, as outlined within their terms of reference and provides summary reports to Trust Board after each meeting. Risk Monitoring Escalation and Assurance Framework The Trust introduced a new risk management system, replacing PRISM with Ulysses, which enabled us to develop to improve our systems for escalating risk and refining the ‘Significant Risk Register’. Further work continues into 2015-2016 with the development of ‘Balanced Scorecards’ and a defined set of key performance indicators as ‘Early Warning System Scorecards’. Organisational Learning Calderstones Partnership NHS FT aspires to continually expand our capacity to improve through shared learning. The primary objective for our service delivery is getting it right the first time, however, if this is not achieved than we need feedback and evaluation to learn and implement changes to practice. When things go wrong in services it is important that all staff have the opportunity to hear what happened and what has been done to address the issues. We have systems in place to get feedback about the services we provide, and use this feedback to improve. We review all adverse events as an opportunity to learn, and as a prospect for improvement, and ensure these are communicated to staff. In 2014-2015 we introduced a mechanism in which staff listened first hand to feedback about organisational learning from serious incidents, safeguarding, and serious complaints. This reinforced the principle of that all staff are part of the organisational learning process. We have organised themed two events during the year, aligned to key strategic goals: ‘The Carer Experience’ This was a half-day event, which involved a session co presented by a carer and ward manager both sharing their distinct perspective of the same adverse event. This session involved both presenters telling their personal story including the personal impact mistakes have both on service users and carers, but also staff 33 members. Whilst, it was a challenging session to deliver the evaluations from both internal and external stakeholders were extremely positive. ‘Positive and Safe – Service User Perspective’ This half-day event aligns to the Positive and Safe Programme and links to the feeding back the survey results from regarding the use of restrictive practices, and also the opportunity for one of our service users and staff to recount their unique experiences of restrictive practices whilst at living at Calderstones. The Service User’s Perspective on the Impact and Outcomes from Crisis Management The aim of the initiative was to obtain the service user’s perspective on the impact and outcomes from crisis management using high risk practices, which include physical intervention, seclusion and rapid tranquillisation; using this information to inform and improve the service user’s outcomes and experience. We hope to measure those critical aspects of service delivery that provide insight from the service users’ perspective around the use of restrictive practices, and maximise the service user opportunity to articulate the impact, effectiveness and experience of restrictive practices. There has been extensive consultation with service users about their experiences of the use of restrictive practices. It was evident from the feedback that a number of care and management interventions, which are high risk and intensive, do not always deliver a good outcome for the service user. In addition, the Trust’s CQC inspection in 2014 highlighted concerns regarding the amount of restraint used with service users. The importance of soliciting and responding to feedback from people experiencing restrictive practices is highlighted through the ‘Positive and Safe Programme’ and is an essential element of the 2015-2016 work plan. Work has taken place to address these issues through awareness raising and procedural guidance, to ensure privacy and dignity is given an equal priority to clinical risk. The implementation of these interventions are described primarily though Positive Behaviour Support Plans (PBSP) both in proactive and reactive terms, which in best practice are co-created with the service user and describe a good outcome for the service user as a result of the care and support interventions. This is the second year of data collection. In 2013-2014 data collection was monthly and as near as possible to the time of an incident. For 2014-2015 due to the increased volume of consultation exercises during the year the interview schedule was changed to four data collection exercises in May, August, October and January. Consequently, the numbers of people interviewed are significantly different, 170 in 2013-2014 and 86 in 2014-2015. The service users were interviewed post crisis by 34 an interviewer independent of the ward usually within 14 days of the incident. Service users were only interviewed once every 3 months regardless of the number of incidents involving restrictive practices. This was to avoid survey fatigue amongst the service users. On occasions, service users may have had multiple incidents before the interview was actually completed. However, the focus of the questions is not situation specific and is about their level of support in general post incident. There are no discussions in relation to the events leading up to, during or after the incident. The questions are based upon themes aligned to a Human Rights Based Approach to Healthcare: • • • • • • Involvement Safety Dignity Support Communication Relationships Analysis of results is based upon three distinct categories: • • • All service users Service users fully aware of the ‘positive behaviour support plan’ Service users unaware of their ‘positive behaviour support plan’ Involvement Compared to last years results (44%) there has been a minor improvement (50% in 2014-2015) in the level of involvement of service users reporting that they are fully aware of their ‘positive behaviour support plan’. However there has been no change in relation to the percentage of service users reporting co-creation of their plan (63%). This features significantly within the ‘Positive and Safe Programme’ for 20152016, with emphasis upon co-creation both with service users and families and carers wherever possible. Safety We ask service users about their perception of personal safety during the use of restrictive practices (see figure 6). For 2014-2015, there has been a reduction in the top response ‘all of the time’ for ‘feeling safe’. With the Positive and Safe Programme highlighting both the physical and psychological risks from restrictive practices service users may understandably be expressing greater concern. When reviewing those service users who report not being aware of their ‘positive behaviour support plan’. This adds greater emphasis upon the need for co-creation of ‘positive 35 behaviour support plans’ so that if restrictive practices are used the service user is familiar with the techniques. Figure 6 Dignity One of the key objectives of this survey is to evaluate whether we are achieving our aim of ensuring that privacy and dignity are given equal consideration to risk management issues. The feedback regarding the sense of ‘being watched’ during restraint has risen this year (figure 7) and is not what we would have hoped for as a Trust. This question is regarding the service user’s perceptions as it may be hard to discriminate if people are actually watching. However, it is important that service users have a sense of privacy when they are experiencing the use of restrictive practices. When we review figure 8 we get a sense of the negative impact this has on service users, and when we review by groups of perceived watchers then it is other service users watching that appears to cause the most distress. This information is critical as part of the Prevention and Management of Aggression Training as the need to offer reassurance around privacy and dignity issues is critical. This principle also extends to the need to make sure people are covered up and their clothing adjusted. 36 Figure 7 Figure 8 Support There is a marked difference between perceived levels of support during restrictive practices and afterwards with very little variation between the different reporting groups (see figure 9). It is likely that this correlates with the privacy and dignity issues and the focus upon reassurance during any restrictive practices. The feedback for support afterwards is very positive and it is good evidence that the staff quickly begin to re-engage with the service user and build therapeutic relationship. 37 There is also a marked difference in how much mutual peer support there is for service users. Peer support is beneficial and service users have an important role to play in their own and in their peers' recovery. This feedback requires us to look towards collaborative working partnerships with service users, and reviewing the Positive and Safe Programme exploring the potential for peer support as part of the debrief process. Figure 9 Communication Again we see a marked difference in the feedback(see figure 10) during the restrictive practice and afterwards. Service users are reporting lower levels of satisfaction with the communication than we would anticipate during the restrictive practice, but generally report that communication afterwards is very helpful. As in the ‘support’ section, this needs to be a key feature of training, particularly around the level of engagement with service users whilst they are in crisis and distress. This will be a key factor in the Trusts revised training for Prevention and Management of Violence and Aggression, as part of the Positive and Safe Programme. 38 Figure 10 Relationships These results are quite unusual (see figure 11). Both questions use a four point likert scale and the results are for the ‘very good’ response. There is a widely held belief that restraint and restrictive practices can damage the staff and service user therapeutic relationship, whereas these results suggest something very different. This is a good indication that staff recognise the negative of experience of service user after restrictive practices and endeavour to rebuild relationships. This correlates with the communication findings. Figure 11 39 Overall, the results from 2014-2015 have not demonstrated the improvements we had anticipated. However, there has been significant investment in the Positive and Safe Programme and as service users become more engaged with the debate around restrictive practices they can actually become more discerning in their judgements of their experiences. For 2015-2016 the service user experience will inform the underpinning knowledge delivery of the Prevention and Management of Aggression training. Customer Care During the financial year 2014-2015 the Trust’s Membership and Involvement Office has been restructured so that the Patient and Public Involvement element of the work has now been incorporated into the Trust Governance Department. This move has enabled the development of a Customer Care Service which incorporates Trust Patient Advice and Liaison (PALS) with the aim of improving customer focused approach to responding to concerns in a timely and effective manner. The steps taken to improve the effectiveness of how concerns and requests for help information and advice are received and dealt with, have been implemented in an incremental way to ensure that this new service is embedded in each aspect of service delivery. The elements introduced as part of this phrased implementation are as follows: • • • • • • • The development of a Trust Customer Care Strategy and Customer Care Action Plan Establishing a bespoke Customer Care Service confidential telephone line; voicemail and email account Re-launching the Patient and Advice and Liaison Service supported by posters and leaflets which include the new telephone numbers and email address of Customer Care Services The introduction of a 24 hour voicemail and email contact which goes to a Customer Care Service confidential inbox which is can be picked up by the Customer Care Service Manager, Complaints Lead or Head of Governance so that contacts can be responded to within 2 working days Inclusion of PALs Information into the newly designed Trust Website Revision of the PALS Procedure 17.6 and Involvement Group Procedure 17.5 Delivery of Customer Care Training as part of the Trust Induction Programme and further Customer Care training is provided to Trust staff on an ongoing basis as a one day training course delivered by the Trust Learning and Development Department. Family and Carer Involvement has been improved through the development of the Trust Carer Strategy and supporting action plan. This has been developed in 40 partnership with the Trust Social Worker/Carer Lead. The strategy includes the setting up of a Family and Carer Group and the group has been in operation since January 2014. The group meets on a six weekly basis and the numbers of families that attend is growing steadily. The group have guest speakers to provide opportunities families to find out about the services that the Trust provides. The Trust has also signed up to the Triangle of Care which is an accredited family and carer framework/assessment scheme designed by Family and Carer Organisations. As an integral part of this framework an annual survey has been completed by families and a self-assessment audit have been completed during the year. The Triangle of Care have been a platform on which to improve our partnership working with families and carers. A Family and Carer Event took place on Saturday 29th November 2014 with the aim of reaching more family contacts. The theme of the day was support for Families and Carers. The results of the work completed at the event have informed the Triangle of Care/Family and Carer Work plan. A further event was held 27th March 2015, a large number of family members attended to hear about future strategy and to discuss all aspects of care with directors, senior staff and experts. Carers voiced their views and agreed to move forward with their involvement in our services and learning disability provision. We also announced that the Carers' Trust have awarded Calderstones their Gold Star; a powerful recognition of our partnership with family members. We were proud to share that with carers and recognise the work we do together. Speak Up Groups provide opportunities in another format for service users to have their say. The discussions topics groups from these groups inform the Governance and Quality agenda. The discussion topics this year have been Food and Staff to Support Me. The information collated from this work have been fed back to the Speak Up Groups and reported through Clinical Management Team, Quality Committee and Contract Monitoring structures. Recording and monitoring feedback is currently captured through reports presented at Clinical Management Team in a bi-monthly report and to the Quality and Risk Committee annually. The implementation of the Trust’s new Risk Management System which will be available in April 2015 will record both the PALS and Complaints information which will further enhance the Customer Care reporting. The Friends and family test is not a statistical robust league table measure however the free text will hopefully provide another valuable patient experience measure that will inform the Trust Governance programme and service delivery. The uptake of contacting Customer Care Services using the Customer Care Line does remain small. It would appear at present that the preferred method of contact for service users, staff, families, advocates and outside agencies is by contacting the Customer Care Manager direct and in person. This might be due the fact that they 41 want to speak to someone in person rather than leave a message. Further work will be completed during 2015-2016 to publicise the 24 hour Customer Care Line. The re-launch of the PALS has seen an increased amount of PALS requests during the last six months of the year (September to February 2015). There has been large increase in families getting in touch with the service. This is probably due to the increased opportunities for family and carer support and involvement. The Customer Care Service Manager has presented at the organisational learning event in October 2014 providing information about involvement initiatives and patient experience with the emphasis on Family and Carer Involvement, and also in March 2015 looking at Restraint. The Customer Service Manager will support service users to present their patient experience stories, which will inform this staff learning forum. In January 2015 the Friends and Family Test was introduced to Mental Health and Community Services by NHS England. The Test asks the question “Would you recommend this service to your Friends and Family?” it also enables participants to enter free text to support the answer option they choose. Prior to implementation discussion has taken place with Commissioners to agree the best way of incorporating the Friends and Family Test Question into the Trust survey/audit programme. It has been agreed that the question should be included as the first question in the Service User Satisfaction Survey. The benefits of which is to ensure that all service users have the opportunity to be asked this question on a quarterly basis and avoid the potential for survey fatigue within our small and long stay client group. The Friends and family test is not a statistical robust league table measure however the free text will hopefully provide another valuable patient experience measure that will inform the Trust Governance programme and service delivery. The Friends and Family Test (FFT) requires all patients to be asked: “How likely are you to recommend our Trust to friends and family if they needed similar care or treatment?” The answers given are used to give a score which is the percentage of patients who responded that they would recommend our service to their friends and family. The Trust had a score of 74% recommended for the Friends and Family Test 42 Multi-Focused Training Package for Individualised Support Packages Individual packages of care (IPCs) are bespoke services for individuals whose behaviour presents significant challenges to services. Such packages of care are person centred; involve extensive specialist multi-disciplinary support and high staffing levels; and are facilitated within single person living environments with specific consideration of the broad range of resources required to meet the individual’s needs. It is recognised that both the working conditions and the training requirements of staff teams supporting individuals within IPC’s and with those displaying challenging rather than offending behaviour, mean that an additional specialist approach to training is warranted. The development of a multi-focused training package, facilitated by individuals from a range of professional backgrounds and with specialist expertise was proposed. This proposal reflects the importance of training in enhancing skills, capabilities and knowledge in order to enable staff teams to support the development of multi-disciplinary interventions and appropriate treatment and care. It was recognised that training should address the key training needs of teams supporting individuals with complex needs and challenging behaviour. A substantial proportion of the individuals supported within this context have a diagnosis of autism, and therefore there is a requirement for all attendees to have attended prior level 1 autism awareness training and to have completed the British Psychological Society online autism training modules level 1 and level 2. A two day multi-focused training package was developed with the following content: • • • • • • • Discussion regarding the differences associated with working into IPC’s Shared framework of care Positive behavioural support Recording of Challenging behaviour Communication Sensory Difficulties Activity Planning Working in IPC teams The training has been facilitated by the following professionals: Clinical psychologists, Lecture in Positive behavioural Support, Behaviour Nurse Therapists, Speech and Language Therapists, Occupational Therapists and qualified nursing staff. All professionals involved are experienced at working in to IPC’s. Service user input has to date been limited to a video provided by the parents of one individual supported within an IPC, discussing their experiences of collaborating in developing 43 and providing ongoing support to the team providing an individual package of care to their son. The first cycle of training was facilitated in June 2014. Since that date a further six sessions (two days duration) have been facilitated with a total of 46 staff having attended. Attendees have been both qualified nursing staff and support workers. Four sessions have been cancelled due to difficulties with staffing and a lack of attendance. Feedback from staff attending the training has on the whole been extremely positive. ‘Fantastic training really emphasises core values which underpin new care pathway. Positive and highly motivating.’ ‘Very helpful to working life, more training of this nature (specific to IPCs) would be good.’ 44 CQUIN 2014-2015 A range of CQUIN targets were agreed for both the Forensic and High Support Services. The end of year outcomes is shown in fig 2. (CQUIN Targets, 2014-2015). Table 3: CQUIN for 2014-2015 CQUIN Target Outcome Rationale Forensic Services 1. Family and Friends Achieved 2. Improving Physical Health Achieved 3. Collaborative Risk Assessment Not achieved The 90% target of training packages delivered was not achieved by Q4 due to competing work pressures and reduced staffing resources Action has been undertaken to address the underlying workforce issues to reduce working pressures which will facilitate staff to attend training programmes. 4. Supporting Carers Involvement Achieved 5. Needs Formulation at Transition Achieved High Support 1. Friends and Family Achieved 2. Improving Physical Health Achieved 3. Care Planning with Supported Achieved Discharge 4. Communication with GP Achieved 5. Developing a Safety Culture Achieved 45 3.2 Review of Quality Performance: Quality Indicators 2014-2015 3.2.1 Department of Health Quality Indicators The Trust will report on the following indicators as required by Monitor’s Compliance Framework/Risk Assessment Framework: Indicator Rate of patient safety incidents reported within the trust during the reporting period, and the number and percentage of such patient safety incidents that resulted in severe harm or death. The data made available to the trust by the Information Centre with regard to the percentage of patients aged— (i) 0 to 15; and (ii) 16 or over, readmitted to a hospital which forms part of the trust within 28 days of being discharged from a hospital which forms part of the trust during the reporting period. • Score National Average Highest Scoring Trust Lowest Scoring Trust 0% (0/1159) Not Applicable Not Applicable Not Applicable Not Applicable Not Applicable Not Applicable 0% The Trust does not routinely report this information to the Health and Social Care Information Centre because as a specialist learning disability service we are not included in the Mental Health Minimum Dataset, therefore there is no comparative data for either indicator. However, there are plans to introduce a Learning Disability Minimum Dataset. 3.2.2 Development of a Quality Dashboard The Quality Dashboard has been designed with clinical teams to help improve performance by providing regular, timely feedback against locally predetermined measures to assist successful intervention and improvement. They are an active performance-monitoring tool for safety, effectiveness, clinical outcomes and service user experience. They also provide opportunities to detect emerging quality and safety issues and permit timely mitigating actions to be taken - improving the overall level of high quality, person-centred care. The Trust recognises that good quality information is a driver of performance amongst clinical teams, and helps to ensure the right services and best possible care is provided to service users. A key element of providing good quality information is ensuring that clinicians delivering the service receive regular and timely feedback on their performance 46 The Trust has continued to develop the Quality Dashboard in collaboration with the clinicians, which provides them with the information they need to inform daily decisions that improve quality of care for people using services. There are three different versions of the dashboard, one for the ward teams, one for directorate leads and one for the board. The individual dashboard functionality means clinicians as well as managers can view their compliance and performance against the measures for service users’ care planning, risk assessments, outcomes and experience. With the clinical dashboard you have a visual display, which enables clinicians and managers to look at differences between wards. Having the same information, which goes from ‘ward to board’, is key. The Quality Dashboard largely reflects effectiveness, safety and experience of service users on their care pathway. Our metrics are aimed at improving the efficiency and effectiveness of the care pathway for people using services. For 2015-2016 we are introducing additional metrics associated with the NHS England initiative ‘Open and Honest Care’: • Number of omitted medicines (all medicines) The following information is an overview of the performance of the metrics that inform the Trust’s Quality Dashboard. The information is structured around national priorities and the three domains of High Quality Care for All (DH, 2008): • • • Patient Safety Clinical Effectiveness Patient Experience The following key is used to explain Trust performance and trend in relation to the metrics: NB All the data is sourced via the Trust’s Business Intelligence System or Risk Management System • The direction of the arrow means: • The colour of the arrow means: Improving No change Worsening Achieving target Just below target Not achieving target 47 National Priorities Delayed transfers of care are below the national target, but have increased from previous two years. This is possibly due to the effects of the national programme ‘Improving Lives’ reviews as part of the Winterbourne Joint Improvement Plan. All people with learning disabilities within inpatient services have been reviewed, therefore it is expected that more people have been identified as ready for discharge. This impetus now for the Trust and community services is effective discharge planning and good partnership working with receiving services. All Annual Health Checks are undertaken in the Trust’s Primary Care Service based within the Calderstones site, and physical healthcare of service users is seen as an integral part of the care pathway. Advanced Nurse Practitioners continue to play a lead role in delivering annual physical, and have implemented systems to ensure all reporting is standardised through the EMIS system (electronic record of primary care). Every service user is provided with an appointment and the recall system for the service users who do not attend has improved. However, we are still not engaging all service users in the Annual Health Check, either due to their level of understanding or unwillingness to engage; there still needs to be further work with this small group to find creative ways of involving them in the process and realising the benefits. The Advanced Practitioner addresses this through caseload management of people with complex needs. Data quality on ethnic groups has achieved target this year. Table 4 National Priorities Metric 12-13 13-14 14-15 Target Trend Delayed transfers of care 1.25% 0.76% 2.69% <= 7% Annual health check <100% 96% 98.23% 100% Data quality in ethnic group <100% <100% 100% 100% Patient Safety One of the key aims of the Trust is to ensure everyone plays a part in helping to reduce harm and improve the safety of services. The vulnerable nature of many service users means staff play a particularly active and important role in safeguarding and improving safety. The Trust is dedicated to building a service where every member of staff has the commitment, confidence and skills to eliminate 48 harm to service users, and by doing so builds the capacity and capability for improving the quality and safety of services. The Trust’s profile of metrics outlines the Trust’s priority concern for the safety and to provide a safer environment for service users. The Trust is committed to ensuring there is a strong safety culture. The metrics focus on the systems for assessing and managing the highest risks to service users, at specific junctures in the care pathway and across clinical teams. Safe and Effective Physical Intervention The Trust continues to try and deal with the challenges of service users and staff becoming injured during physical intervention. There have been a number of initiatives attempting to address the significant differential between service user and staff injuries. There is standardised training for all staff using both the non-aversive British Institute of Learning Disabilities approved training, and the more commonly used care and responsibility methods with much more secure holds for people. During 2014-2015 aligned to the Positive and Safe Programme the Trust has introduced alternative training methods, which do not require the use of prone (facedown) restraint. There has been an improvement from the previous year’s results; analysis of the injuries has revealed that they are minor harm incidents usually soft tissue or abrasions, and that the majority of injuries to staff are caused by a very few service users. The majority of injuries are still cause by service users cared for in personalised packages of care with enduring and complex needs that continue to present challenges to services. Table 5 Injuries during physical intervention Metric 12-13 13-14 14-15 Target Trend Reduction of injuries sustained by service users as a result of physical intervention 2.5% 1.5% 0.8% <= 2% Reduction of injuries sustained by staff as a result of physical intervention 11% 11% 7.94% <= 5% Care Planning In relation to ‘Advanced Support Plans’, it is disappointing that we have not achieved our target. The transition work positive behaviour support plans will address this issue, as advanced planning will be integrated into this part of the ‘Integrated Treatment and Care Plan’. This new systems still ensures that service users are 49 supported to help develop their own plans for any aspect of crisis or period of distress. With regards to the ‘Suicide Risk Screening Assessment’, the results of 85% (n17/20) are still not meeting the 100% target, however this is an improvement on previous years. The failure to meet the target is again associated with the 24-hour timeframe from admission. All service users are assessed within 48 hours. However, the target remains unchanged as it is important that we seek assurance that the wards recognise the increased risk of attempted suicide in the crucial first 24 hours of admission to hospital and ensure the safety of service users. Table 6 Care Planning Measures Metric 12-13 13-14 14-15 Target Trend All service users who self injure (clinically assessed as high risk) will have an advanced support plan 99% 78% 91.75% >= 95% All new admissions to the Trust will have a ‘Suicide Risk Screening Assessment’ completed within 24 hours of admission 100% 67% 85% >= 95% Medicine Management The purpose of the Trust’s Medicines Management Strategy is to proactively support staff and service users in achieving safe and effective medicines management. Medicine management for the Trust means service users getting the maximum benefit from their medicines whilst at the same time minimising potential harm. All healthcare practitioners have a duty to competently perform safe medicines management. Table 6 outlines the measures for missed medications and high risk errors based upon the number of people affected. The Trust also revised the target to 0% for critical medicine omissions and high-risk medication errors. There has been increased monitoring of safe and effective medicines management, with an emphasis on missed dose incidents. There has been significant improvement on the number of incidents of ‘critical medicine omissions’. The incidents that have occurred have been ‘near-misses’ so no actual harm occurred to the service users affected. However, the Trust recognises that there is potential for serious harm from omitted critical medicines. Where the main reasons for missed doses related to physical unavailability of medicines, effective interventions to improve this situation included: increasing the 50 range of stock held in the emergency cupboard and the availability of a 24 hour taxi service to collect urgent medicines from pharmacy. For high-risk errors the emphasis is upon continuing professional development. These include errors like wrong dose or wrong frequency. There is a programme in place for both registered nurses and medical staff that focuses upon safety and accountability in practice. Medicine safety was a key theme for Director walkabout visits and has led to changes in practice associated with changes in the environment and how registered nurses administer medicines. With all errors the priority is to ensure that the service user does not come to harm and we can report than no service users suffered harm as a result of medication errors. Table 7 High Risk Medication Errors Metric Apr 14 May 14 Jun 14 Jul 14 Aug 14 Sep 14 Oct 14 Nov 14 Dec 14 Jan 15 Feb 15 Mar 15 Critical Medicine Omissions High Risk Medication Errors 0.5% (n1) 0% 1% (n2) 0% 0% 0.5% (n1) 0% 0% 0% 0.5% (n1) 0% 0% 2.25% (n5) 0.5% (n1) 1% (n2) 2% (n4) 0% 1.5% (n3) 2% (n4) 1% (n2) 1.5% (n3) 1% (n2) 1% (n2) 1.5% (n3) Clinical Effectiveness Clinical effectiveness is about whether or not a service users treatment, care and support was successful and whether it has the impact that it is supposed to have, is it achieving the best possible result or outcome for the service user? Providing effective treatment, care and support is at the heart of our vision to make a meaningful impact and change to our service users’ lives. We aim to make sure that the care we provide to our service users and their families achieves the best possible impact on their health, wellbeing and quality of life. We continue to work with our clinical team to develop a set of clinical effectiveness metrics because we believe they act as an incentive to improve quality. Clinical effectiveness metrics also inform our service users and others to see how we are doing in relation to the effectiveness of the care pathway, and enable the Trust board, through its Quality and Risk committee, to monitor performance. 51 Safe and Effective Identification of Risk of Choking The metrics in relation to risk of choking indications of the Trust focusing on an evidenced based approach to mitigating against one of the highest risk of injury to our service users. The Trust has been at the forefront of developing a riskscreening tool for dysphagia, and has previously been nominated for a national ‘Patient Safety Award’. There has been a focused effort on ensuring that all service users are risk assessed routinely and in response to a change in clinical presentation. It is disappointing that for the screening upon admission, it has not made the target. However, we are assured that all service users had a risk screen on admission but not within the first 2 weeks. The annual review of risk of choking has significantly improved. Ward managers have worked with case managers to ensure that they recognise it as a priority to maintain the safety of service users and encourage them to maintain compliance with routine annual screening. Table 8 Risk of Choking Assessments Metric 12-13 13-14 14-15 Target Trend All new admissions to the Trust have received a risk of choking screening assessment by week 2 of the care pathway 92% 79% 78% 100% All service users receive an annual risk of choking screening assessment 99.5% 97% 99% 100% The Care Pathway The purpose of the Trust’s care pathways is to show a clear journey of care for service users, which set out what they can expect from their treatment, how long it may take and who will provide their care. Table 9 gives an overview of the metrics that identify key processes in the care pathway, and give an indication of the effectiveness of the Trust’s care pathways. The clinical teams have made continued and sustained improvement over the past three years, to ensure there is a comprehensive treatment and care plan in place by week 12 of the care pathway. Historically, the target was 70% but given previous year’s improvements this has been reviewed and increased to 95%. The clinical teams have missed the target in 2014-2015 achieving 88% (22 out of 25). We are assured that all service users have a treatment and care plan, although completion within 12 weeks of the care pathway has not always been achieved. We will continue to try and achieve this target to ensure that all our service users have a 52 treatment and care plan in place at the earliest opportunity to ensure that their stay is no longer than it needs to be. There is almost full compliance with six-monthly review of the risk assessment, the areas of non-compliance are related to the risk assessment being fully authorised by the consultant psychiatrist, although the multi disciplinary team had fully reviewed the risk assessments. In September 2014 we introduced a new metric in response to concerns raised as part of the ‘Improving Lives’ reviews. The review team stated it was difficult to find evidence of service users having an MDT review other than during formal ward round. This measure has been introduced alongside the relocation of all clinical staff (not direct care) in to clinical areas. As previously reported we have not had any reported cases of service users experiencing side-effects resulting in a ‘high’ score. However, we continue to monitor that service e users are reviewed routinely every 12 weeks. Table 9 Care Pathway Measures Metric 12-13 13-14 14-15 Target Trend All service users will have a comprehensive multi disciplinary treatment and care plan by week 12 of the care pathway All service users will have a review of their current risk profile by the MDT at least every six months 93% 83% 88% >= 95% <100% 99% 99.% >= 95% Service users have had a review in between their ward round review (new September 2014) NA NA 51% 100% 3 monthly monitoring of side effects of antipsychotics using Liverpool University Neuroleptic Side Effect rating Scale (LUNSERS) NA NA 35% >= 95% Patient Experience Listening to service users' views is essential to provide person-centred services. The experience metrics systematically gather the views of service users about the care they have recently received. 53 The metrics outlined in tables 10 to 15 focus upon the experience of service users, and endeavour to address the importance of the service user experience within the Trust, and ensure that service users are treated with compassion, dignity and respect within a clean, safe and well-managed environment (High Quality Care for All, 2008). The Trust has a revised set of experience metrics aligned to the NICE Clinical Guidelines 136 (2011) “Service User Experience in Adult Mental Health”, and the Department of Health’s Final review of Winterbourne View (DH, 2012), the CNO’s 6Cs, and the values and principles underpinning the preferred ‘model of care’. Therefore it is not possible to publish comparative results for previous years so the three data collection points for the 2013-2014 reporting period are reported to provide an overview of consistency of performance. Partnership and Involvement The Trust is committed to ensuring that service users are at the centre of their own care. Our priority is to ensure that personalisation and person-centred planning, are embedded in all of our services. Involvement is the central tenet for ensuring that person-centred planning is key to ensuring that every service user is being supported and cared for appropriately. The Trust’s vision of ‘changing lives through excellence’ is underpinned by the values that people have learning disabilities are capable of being involved in the decisions that affect their lives, through the value of ‘partnership’ , putting service users at the heart of their own care planning leads to better outcomes. Whilst this year there has been a drop in the results they remain consistently high performing with all the measures for partnership and involvement with particular reference to the support that our service users receive from their case managers ensure they are fully engaged in the CPA process. Table 10 Partnership and Involvement Metrics Partnership and Involvement Metrics Target 13-14 14-15 Trend I am involved in my treatment and care 80% 90% 86% I am listened to when talking about my treatment and care 80% 86% 83% I am confident that my treatment and care at Calderstones will help me move on I know what I need to do to move on from Calderstones 80% 89% 86% 80% 87% 90% I understand my treatment and care plan 80% 87% 85% I am supported by my case manager with ward rounds 80% 90% 85% I am supported by my case manager with my CPA/117 meeting 80% 93% 92% 54 Trust and Support A service users’ ‘trust’ in their care teams is recognised as vital as it underpins a positive therapeutic relationship. We understand the concept of ‘trust’ to mean ‘we keep our promises’ to our service users. The notion of ‘trust’ is not only relevant to individual clinicians but is also relevant to how our service users feel towards Calderstones as an organisation. We endeavour to build ‘trust’ through good support throughout their care pathway. Service users are much more likely to establish ‘trust’ if they receive good support and have a voice in the planning and delivery of their care. These metrics are a means of assessing service user satisfaction with the level of support they receive. All of the measures are meeting the 80% threshold, and in the case of supporting contact with significant others the feedback is excellent. This is important when considering future planning for service users and supporting the relationship between service users, family/friends and the care team. Table 11 Trust and Support Metrics Trust and Support Metrics Target 13-14 14-15 Trend I can get the help that I need when I'm having problems 80% 85% 86% I am supported to maintain contact with the people who are important to me I am supported to make choices in my daily life 80% 94% 93% 80% 88% 89% I know the staff are supporting me 80% 89% 87% I trust the staff who are supporting me 80% 85% 81% I feel safe 80% 82% 81% Communication and Support Communication is vital in ensuring that people with learning disabilities can express themselves and make sense of what is happening within their treatment and care pathway. With the right support, people with a learning disability can achieve their full potential, as long as support is communicated in an understanding way. Communication as a Trust value means ‘we are open and honest in our communication’. The metrics in table xx outlined in our experience metrics are a way of enabling us to evaluate how well we communicate with service users. 55 There is variation in feedback from service users to this set of measures, which is good indication that they are making considered responses. Although the service users appear to have confidence in talking to the staff, again this year there is disparity in the responses to questions related to ‘time with staff’ and ‘perceived understanding’. The Trust has a current standard that all service users will have the opportunity of one-to-one time with a member of staff daily, a weekly meeting with their case manager and monthly with their consultant psychiatrist to discuss their care pathway. There has been an increased emphasis up on multidisciplinary team members having more time in the clinical area. This is to ensure that service users have access to this group of people not just within appointment time. It was hoped that tis would improve feedback from service users. In this financial year, there has continued to be high bank and agency staff use compounded by vacancies and sickness absence. There is an exercise underway to review and rationalise staff resources across Forensic and High Support Services. Table 12 Communication and Support Metrics Communication and Support Metrics Target 13-14 14-15 Trend I can talk to the staff who are supporting me 80% 87% 84% I get one to one time every day with a member of staff that I know I get enough information to help me make important decisions 80% 74% 74% 80% 81% 82% Staff understand me and my problems 80% 79% 78% My legal rights are explained to me in a way that I understand 80% 91% 91% Ownership and Empowerment People with learning disabilities when viewed as service users are not seen as equal partners in designing and implanting solutions to a wide range of issues and problems. These metrics are designed to get feedback from our service users on how empowered they feel about taking control and making decisions about personal care and service delivery at Calderstones. The feedback relation to their personal treatment and care is very positive, and correlates with previous measures about involvement with treatment and care, which scored 86%. 56 However, in relation to wider Calderstones issues the feedback is not as positive as we would have hoped given the increase in Customer Care Services and the coordination of consultation and involvement. This will be considered as part of the ‘Speak Up’ groups core topics to try and get a better understanding of what would change service users expect to see. Table 13 Ownership and Empowerment Metrics Ownership and Empowerment Metrics Target 13-14 14-15 Trend I have the chance to make decisions with my team that are right for me 80% 85% 85% I think what I say matters to make Calderstones better 80% 76% 77% Compassion and Respect For the Trust values ‘compassion’ and ‘respect’ we endeavour to show empathy and sympathy to the needs of others, as well as engage, listen to and value the contribution of others. As a Trust, we believe that 'kindness' is central core value to ensure service users recovery. It is reassuring that our service users have given such positive feedback regarding the level of kindness they receive from staff, however, whilst the score for politeness is above the target there is a 5% reduction from previous years. Interestingly there is a renewed emphasis upon customer care within the Trust with training being available to all staff. This feedback will be reviewed in detail with increased granularity to see if there are any target areas for improvement. Table 14 Compassion and Respect Metrics Compassion and Respect Metrics Target 13-14 Mid 14-15 Trend Staff are kind to me 80% 88% 87% Staff are polite to me 80% 88% 83% 57 Excellence and the Meaningful Day NICE Quality Standard 14 Service User Experience in Adult Mental Health states people in hospital for mental health care will access meaningful and culturally appropriate activities seven days a week and not restricted to 9am to 5pm. This should be tested through experience surveys and feedback that service users in hospital. These metrics have been developed to test our compliance with the NICE standard, and how well we align to our Trust value of ‘excellence’. We have been able to meet the targets in relation to meaningful activities across seven days a week. This metric is based upon service user feedback. Occupation and leisure services have been redesigned around the Integrated Therapy Model. The aim is to ensure that service users will have improved access to therapeutic, occupation and leisure services, which are aligned to their personal goals and treatment outcomes. This is of high importance to services and service users, and there is ongoing consultation with service users to ensure responsiveness to service users’ issues. Table 15 Excellence and Meaningful Day Metrics Excellence and Meaningful Day Metrics Target 13-14 Mid 14-15 Trend I have a shared activity planner 80% 94% 92% My shared activity planner has activities I like to do on it 80% 84% 89% If I don't like my activities I can change them with my OT or case manager 80% 82% 86% I get 25 hours of activity every week e.g. trips out, social/leisure time, domestic skills, meetings and individual/group therapy 80% 79% 82% There is a timetable of evening and weekend activity in my ward/house 80% 68% 81% I am satisfied with how I spend my time in the evenings 80% 81% 82% I am satisfied with how I spend my time at the weekends 80% 80% 80% 58 Appendix A: Statements from Local Involvement Networks, Service Users Forum, Overview and Scrutiny Committee, Primary Care Trust and Specialist Commissioning Healthwatch Lancashire’s Response to Calderstones Partnership NHS Foundation Trust’s Quality Account 2014/15 Thank you for giving Healthwatch Lancashire the opportunity to feedback on Calderstones Partnership NHS Foundation Trust 2014/15 Quality Account. The report contextualises services provided at a challenging time for the NHS and indicates the Trust's commitment to improve the quality of medium secure, low secure and specialist NHS services which it delivers to adult men and women with learning disabilities or other developmental disorders, mental health problems or extremes of serious offending behaviour. It's pleasing to see the Trust is making good progress with its clinical quality strategy and its commitment to engagement, not only with service users but also with their families /carers and staff too. Achievements with 'The Avenue' and 'The Media Crew' are to be particularly commended. Projects to improve the Trust's accommodation and facilities is encouraging to see as the Trust provides a home for its service users, sometimes for a number of years. In this respect its also good to see the Trust focusing on improving standards of cleanliness. The Trust is also to be commended for reviewing the workforce's capacity and capability to deliver safe and effective care and in reducing restrictive practices. The positive outcome from the annual staff survey in respect of effective engagement and initiatives such as the Staff Charter, the Chief Executive's Big Conversation, Big Breakfast Meetings and Director Walkabouts are an indication of an engaged workforce which is critical to achieve the Trust's quality priorities. Such outcomes also evidence the Trust's focus, commitment and aspirations as a good employer, which again is pleasing to note. However high bank and agency use, compounded by vacancies and sickness absence indicates the Trust has had a very challenging year. The Trust's quality improvement priorities selected for 2015-16 will help to underpin and progress the Trust's clinical quality strategy and are therefore are to be applauded, as is the Trust's commitment to clinical research and audit programmes. Review of the Trust's 2014-15 priorities for improvement shows a number of areas where progress has been made eg Physical Health Monitoring. However, areas which the Trust recognises where further improvement is required are also noted eg Use of restrictive practices and care planning, but it is reassuring to note that work has taken place to improve these particular programmes including the aforementioned review of the workforce's capacity and capability to deliver safe and effective care. 59 Overall, the Quality Account provides the reader with an honest and comprehensive account of the Trust's commitment to improving the quality of healthcare service delivery for a particularly vulnerable group of adults at a very challenging time for health and social care. Service Users Forum Response to Calderstones Partnership NHS Foundation Trust’s Quality Account 2014/15 Thank you for coming to talk to us about the Trust’s Quality Accounts at our meeting on Monday 5th January. We thought that you did really well explaining the accounts to us as there was a lot of information to tell us. We were very interested to hear about the work that is being done to keep everyone as safe as possible, have good treatment and care and that there have been lots of ways that service users and their families have been able to be involved.. We were also pleased that the Trust wants to know about our experience of the care we have at Calderstones. We went through the Quality Accounts again at our meeting on Monday 11th May and were very pleased to see all the work that had been done. If you need any help this year with the Quality Accounts the members of the Calderstones Involvement Group would be happy to involve. Lancashire Overview and Scrutiny Committee Response to Calderstones Partnership NHS Foundation Trust’s Quality Account 2014 - 2015 The role of the Lancashire Health Scrutiny Committee is to review and scrutinise any matter relating to the planning, provision and operation of the health service in the area and make reports and recommendations to NHS bodies as appropriate. The Committee undertake this responsibility through engagement and discussions with the Trust, addressing any areas of concern as they arise. It is the intention of the Committee that this methodology of ensuring that the Trust improve patient safety and deliver the highest quality care to the residents of Lancashire will continue by having an oversight of how the Trust evidence the provision of quality and safe services. In addition the Health Scrutiny Committee will seek reassurance that every effort is being made to ensure financial stability and the safeguarding of the most vulnerable. 60 Specialised Commissioning, Cheshire West and Wirral Local Area Team, NHS England have reviewed the Trusts Quality Account 2014-2015, and appreciate the opportunity to comment on this document. It must be noted there is room for significant improvement as highlighted by the CQC and Specialised Commissioning’s quality review process. This is primarily around staffing levels, use of bank and agency staff, sick leave, supervision and appraisals, and environmental issues including cleanliness of wards some of which are no longer up to national secure standards. However the Trust continues to work with commissioners to strive to improve quality, patient pathways and the overall patient experience and consistently demonstrate extensive patient involvement. Relevant action and improvement plans are in place which are regularly monitored and reviewed, and the Trust actively participate in local and regional meetings to positively impact on organisational change. East Lancashire Clinical Commissioning Group Response to Calderstones Partnership NHS Foundation Trust’s Quality Account 2013/14 East Lancashire Clinical Commissioning Group (EL CCG) welcomes the opportunity to comment on the 2014/15 Quality Account for Calderstones Partnership NHS Foundation Trust (CPFT). The CCG acknowledges that CPFT has been through a challenging year prior to and following the Care Quality Commission (CQC) inspection during July 2014. Considerable work has been undertaken both within CPFT and across the health and care economy to address the concerns raised to ensure a safe, effective and patient focused service. The CQC inspection highlighted a number of areas where improvements ‘must and should’ be made and the CCG have been committed to working with CPFT and other relevant stakeholders to ensure all fundamental standards of quality and safety are delivered so that the Trust can become highly regarded and trusted by the people of East Lancashire and beyond. In light of this the CCG believes that the draft Quality Account does not fully demonstrate the context of the current position and challenges faced by CPFT during 2014/15 as a result of this and the ongoing challenges through 2015/16. The Quality Account lacks detail of the resulting Quality & Risk Summits and engagement with the National Team and the ongoing Quality Improvement Board process. 61 Priorities 2015/16 EL CCG support the priorities put forward for 2015/16 and have worked with the Trust to agree Quality and CQUIN measures for the coming year which will compliment these priorities, including the development of the Care and Treatment Reviews (CTR) task and finish group CQUIN. It is positive to see the development of key actions highlighted in the CQC review, such as Credits for Cleaning (C4C), in the CPFT priorities for 2015/16. The CCG will continue to work closely with the Trust throughout 2015/16 on the Quality agenda, including meeting regularly with the Trust and engaging in a series of announced and unannounced safe, personal and effective care walk-rounds. Quality Indicators and CQUIN 14/15 To date there are a number of outstanding issues, including data time lags, on requirements of the National and Local quality indicators included in the CPFT contract. EL CCG continues to work with CPFT to work through these issues. Four out of the six Commissioning for Quality and Innovation (CQUIN) schemes have been achieved, while further information is due to be submitted for the remaining two. EL CCG notes that CPFT has seen an improvement in harm free care from previous years. Priorities 2014/15 Progress has been made against some of the priorities set out in last year’s account although clear evidence is not consistently demonstrated to show achievement in all priority areas. EL CCG will continue to support CPFT in their commitment to ensuring outstanding actions are addressed. EL CCG commends CPFT on the Director Visits which have been implemented during 2014/15 and would like to highlight the visibility of senior staff and the familiarity between those staff and service users which is clearly evident during CCG visits to the Trust. Although work around restraint is still ongoing, the CCG is particularly pleased to see the improvements made regarding the amount of restraint used and the importance of feedback from service users experiencing restrictive practice to ensure privacy and dignity is maintained in these instances. Concerns around the amount of restraint used at the Trust were also highlighted during the CQC inspection in 2014 62 and CPFT presented at the EL CCG Quality and Safety Committee to provide assurance to commissioners around some of these concerns. EL CCG notes a number of clinical audits have taken place during 2014/15 with changes being implemented to improve outcomes. There is some concern around a number of projects previously audited which have seen little or no improvement despite having action plans implemented previously. EL CCG looks forward to working with CPFT to ensure robust action plans are now in place to address these concerns. Annual physical health checks for all inpatients has seen significant improvement in both engagement and completion of checks and has narrowly missed out on achieving the desired target of 100% with an average compliance score of 98.66%. The CCG is pleased to see a dedicated Advanced Nurse Practitioner using the complex case management model, making good progress in supporting service users who usually find the health checks too distressing. CPFT have ensured all service users prescribed antipsychotic medication receive comprehensive physical health checks and a set of standards have been developed to guide the reporting process. A number of initiatives have been implemented to collect and share feedback from service users and staff around serious incidents, safeguarding and complaints. One specific programme of work is the use of the Manchester Patient Safety Framework (MaPSAF) which was also part of the 14/15 CQUIN scheme. This tool is used to collect staff feedback on patient safety incidents and CPFT will ensure that action plans are in place to embed patient safety across all Trust service delivery lines. The Information Governance Toolkit attainment was 71% based upon the score of level 2 for 41 applicable items, and level 3 for 3 applicable items. This was graded as satisfactory and is an improvement on the 2013/14 position of 68%. EL CCG look forward to working with CPFT over the next year to ensure that services commissioned are of a high quality standard and provide safe, personal and effective care. 63 Annex 2: Statement of directors’ responsibilities for the quality report The directors are required under the Health Act 2009 and the National Health Service (Quality Accounts) Regulations to prepare Quality Accounts for each financial year. Monitor has issued guidance to NHS foundation trust boards on the form and content of annual quality reports (which incorporate the above legal requirements) and on the arrangements that NHS foundation trust boards should put in place to support the data quality for the preparation of the quality report. In preparing the Quality Report, directors are required to take steps to satisfy themselves that: • the content of the Quality Report meets the requirements set out in the NHS Foundation Trust Annual Reporting Manual 2014/15 and supporting guidance • the content of the Quality Report is not inconsistent with internal and external sources of information including: o board minutes and papers for the period April 2014 to 28 May 2015 o papers relating to Quality reported to the board over the period April 2014 to 28 May 2015 o feedback from commissioners dated 13/05/2015 o feedback from governors dated 12/02/2015 & 16/04/2015 o feedback from local Healthwatch organisations dated 01/05/2015 o feedback from Overview and Scrutiny Committee dated 29/04/2015 o the trust’s complaints report published under regulation 18 of the Local Authority Social Services and NHS Complaints Regulations 2009, dated 28/05/2015 o the 2014 national staff survey 24/02/2015 64 o the Head of Internal Audit’s annual opinion over the trust’s control environment dated 29/04/2015 • the Quality Report presents a balanced picture of the NHS foundation trust’s performance over the period covered • the performance information reported in the Quality Report is reliable and accurate • there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Report, and these controls are subject to review to confirm that they are working effectively in practice • the data underpinning the measures of performance reported in the Quality Report is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review and • the Quality Report has been prepared in accordance with Monitor’s annual reporting guidance (which incorporates the Quality Accounts regulations) (published at www.monitor.gov.uk/annualreportingmanual) as well as the standards to support data quality for the preparation of the Quality Report (available at www.monitor.gov.uk/annualreportingmanual). The directors confirm to the best of their knowledge and belief they have complied with the above requirements in preparing the Quality Report. By order of the board .28 May 2015 ......Date.. ..Chairman .28 May 2015 ...... Date... Chief Executive 65 Appendix C Clinical Audit Projects 2014-2015 1. Project Title Synopsis of Findings and Actions National Learning Disability Census The Department of Health published Transforming Care: A national response to Winterbourne View Hospital and the Concordat: Programme of Action in December 2012. The review of services received indicated that failings were widespread within the operating organisation but importantly also evident across the wiser care system. The concordat and sixty three actions detailed within the review seek to address poor and inappropriate care and achieve the best outcomes for people with a learning disability, or autism, who may also have mental health needs or behaviour that challenges. The Learning Disability Census will be the mechanism employed by the Department of Health, Care Quality Commission, Public Health England and Health and Social Care Information Centre to deliver action (17), which says that, “The Department of Health will commission an audit of current services for people with challenging behaviour to take a snapshot of provision, numbers of out of area placements and lengths of stay.” All requested data was collected and submitted. 2. 3. 4. Compliance with National Standards for Annual Health Check The use of Physical Restraint Completed as part of the Physical Healthcare Schizophrenia Audit. See project number 13. Positive Behavioural Support Plans This was a new audit within secure services. 13 service users were included in the audit as they each received high numbers of interventions, to see if the Positive Behaviour Support Plans were compliant with the Positive and Proactive Care standards. This is completed via a monthly restraint report which is presented to the Operational Governance Committee. It is instrumental in the Trusts overall Restraint Reduction Strategy and supports delivery of the Positive and Safe Programme. The audit found all service users had a Positive Behaviour Support Plan but identified the following concerns: • Most service users did not have a functional analysis. • Most service users did not have a post crisis support plan • All service users had elements missing within their primary, secondary and tertiary strategies. • In the event of an incident 50% did not detail evidence that the positive behaviour support plan was followed. • On looking at the treatment & care plans these were far more detailed than the positive behaviour support plans. The positive behaviour support plans are currently being replaced with an integrated Treatment & Care Plan. 66 Project Title Synopsis of Findings and Actions A re-audit on these new integrated treatment and care plans is scheduled for 2015/2016. 5. NHS Benchmarking: Learning Disability Provider Benchmarking Calderstones Partnership NHS FT was one of 33 provider organisations who submitted data to this pilot project for learning disabilities. Four key domains were used in this benchmarking work; activity, workforce, finance and quality measures. A project report was written by the NHS Benchmark Network in December 2014 on the results. The next cycle of benchmarking will take place in 2016. 6. NHS Benchmarking: Restraint This data was requested on behalf of Norman Lamb, Minister of State for Care and Support. The first phase of data collection was in August 2014 and the second phase of data collection was January 2015. All required data was collected and submitted. 7. NHS Benchmarking: Out of Area Treatments In November 2014 the NHS Benchmark Network asked organisations to answer the following questions relating to patients who were occupying their beds on the census date of 30/09/2014: • Number of beds (by bed type) across MH, CAMHS and LD • Number of beds occupied by people from the local area • Number of beds occupied by people from outside the local CCG area i.e. Out of Area Of these ‘Out of Area’ beds: • Number occupied by people still within their host Trust area • Number occupied by people from a different area than their host Trust. All required data was collected and submitted. 8. Critical Medicines This was a re-audit within secure services reviewing whether the use of critical medicines is compliant with Patient Safety Alert NPSA RRR009. This includes identifying a list of critical medicines and identifying any medication errors involving a critical medicine. Comparing with last year’s audit there has been an increase in the number of reported incidents involving critical medicines. This could be due to the critical medicines list having been updated and improved quality of documentation. Critical medicines is now included as a metric each month on the Quality Dashboard and is reported on quarterly in the Medicine Error Report. 9. Medical Appraisals There were two audits completed involving Medical Appraisals. An ‘Exception’ Audit for all missed/ incomplete appraisals and an Audit of the 67 Project Title Synopsis of Findings and Actions Medical Appraisal Systems. The ‘Exception’ Audit for all missed/ incomplete appraisals is a mandatory audit. Audit standards are contained within ‘Appraisal and Revalidation Procedure’ (Trust procedure 9.37). This audit is required by NHS North via requirements of the ‘Annual Organisational Audit (AOA). 94% of doctors had a completed appraisal. An action plan was developed and communicated through the doctors CPD meeting to ensure: • Doctors avoid leaving their appraisals until March 2015. • An active prompts/reminder system for doctors will continue to be used. • Collection of information throughout the appraisal year. Audit of Medical Appraisal Systems was a re-audit and is now a mandatory audit. It is a structured review or audit of the designated body’s appraisal system against the standards described in GMC guidance and AOA (Annual Organisational Audit) Issued by NHS England in March 2014. Comparing with the previous audit there were very significant improvements (compared with 2012) in all areas of the Doctor’s portfolios of evidence including all portfolios being well organised, complete and detailed. An action plan was developed from the audit and the procedure was updated to recommend that doctors change their appraiser every three years and will be re-audited in 2015/2016. 68 10. Project Title Synopsis of Findings and Actions Controlled Drugs This audit was a re-audit completed within secure services to establish compliance with Controlled Drugs Trust Procedure M9.0 written in accordance with (Safer Management of Controlled Drugs: A guide to good practice in secondary care (England) – Oct 2007). This included: • • • • • Requisitioning Storage Key holding Record keeping Destruction and disposal of controlled drugs in clinical areas. The audit discovered issues with: • • Completing and respecting record books and controlled drugs stationary. Controlled Drugs cabinets did not comply with standards and in most cases needed properly securing to the wall. From the audit an action plan was developed and is currently ongoing. The Trust also completes a report on controlled drug activity across the Forensic and High Support Services three times a year. As part of the report all incidents involving controlled drugs are audited to ensure all the statutory reporting requirements have been met. The Trust was fully compliant. This will be re-audited in 2015/2016. 11. Compliance with prescribing practice for ADHD in adults This audit was completed to check compliance against the recommendations in the NICE CG72 (2008) in patients with a diagnosis of ADHD. The audit found that physical health monitoring achieved 100%, no patients were prescribed antipsychotic medication for the treatment of ADHD and that referral’s to PTS are considered in the MDT Meetings. Areas for improvement were around the processes before starting treatment and the availability of easy read documents regarding medication. An action plan was developed which included an action to re-audit in 6 months’ time on patients newly starting on ADHD medication, however no new patients were identified. 12. Obesity This audit was completed due to a systematic rise in obesity in the hospitals patient population over the past four years and to see whether this relates to background trends in the population or to clinical practices. The audit found issues with the following: • • • Unhealthy eating habits Poor physical activity No consistent approach to recording both weight and BMI 69 Project Title Synopsis of Findings and Actions An action plan was developed and the issues raised are currently being looked at by the Trusts Physical Health Steering Group. 13. 14. Physical Healthcare Schizophrenia Clozapine Audit completed. Awaiting the National audit results. This was a retrospective audit of service users who started treatment on Clozapine medication between January 2014 and October 2014 and was a re-audit of the audit completed in 13-14. The audit found reasonable levels of good practice and recommended a review of the procedure with some minor amendments to improve practice further. There is no requirement for this to be re-audited. 15. Rapid Tranquilisation Non Oral This was a re-audit to review current practice in accordance with the Trust (M9.1) and NICE guidelines. The audit focussed on patients at medium secure wards of Calderstones hospital who received non oral rapid tranquillisation (IM and Buccal Midazolam) during April 2014. During the audit no evidence could be found in PRISM or Care notes regarding the requirement of regular observations being recorded following administration of rapid tranquillisation. Although a PRISM incident record had been completed for each occasion rapid tranquillisation had been administered the record was missing the required information on physical/visual observations by staff. An action plan was developed and the audit was re-audited again between August and September 2014. The re-audit found the same failings resulting in a new action plan being implemented along with a rapid improvement notice. The audit will be re-audited in 2015/2016. 16. Hypertension This was a re-audit to identify whether NICE CG 34 Hypertension is followed for the diagnosis and treatment of hypertension involving Forensic and High Support Services. The findings show some slight improvements but there are still issues and room for improvement in the following areas: • • • • 24hr Ambulatory Blood pressure monitoring Immediate start on hypertensive drugs where client was diagnosed with severe hypertension Investigations and formal assessments while awaiting confirmation of diagnoses of hypertension Treatment guidelines. The trust has implemented an action plan to address the audit results and 70 Project Title Synopsis of Findings and Actions to support compliance with the guidance and this will be re-audited in 2015/2016. 17. Health Monitoring of people taking antipsychotic medicines This was a re-audit against Trust Policy and Procedure M2.2 to determine whether recommended tests are being carried out within specified time periods. Patients from Forensic and High Support Services were included in the audit. Those patients on Clozapine and High Dose Antipsychotics were excluded from the audit as there are specified protocols in Calderstones for the regular monitoring of these drugs. The audit found an increase from the previous year with all tests apart from BMI and blood pressure scoring between 90-100% compliance. An Action plan was implemented and a decision was made to re-audit within the year just the two areas of concern. This took place in February/March 2015 with little improvement A further action plan is currently being discussed by senior managers to find a way forward and once agreed will be implemented. These two components will be re-audited in 2015/2016. 18. Sharps This is an annual audit to establish whether sharps are being disposed of in a safe manner. The audit was carried out by Daniels Healthcare. 12 wards/departments were visited and 27 sharps containers were sighted. The audit showed an improvement in practice from the previous audit but still found issues with the following: • • • Sharps containers were unlabelled during use. Sharps containers containing a significant amount of inappropriate non-sharp contents. Sharp containers did not have temporary closure lids in place when left unattended or during movement. The trust has developed an action plan which is currently being implemented. Daniels will re-audit in 2015-2016. 19. Follow up on actions from CPA Meetings This audit was completed to see if actions and service tasks identified and set at CPA/117 meetings, have documented evidence at subsequent CPA/117 meetings to say if they have been completed or not or are no longer applicable. Nearly two thirds 63% of the Service Tasks/Action generated from CPA/117 meetings were found to be Completed and a nearly a quarter 23% were found to be Incomplete. During the course of the audit it was found that there was a number of Service Tasks/Action documented as Complete in the Meetings minutes but there was no evidence found in the 71 Project Title Synopsis of Findings and Actions CPA Care notes to confirm this. An action plan was devised in which the results were broken down and disseminated to each individual ward. 20. Medication errors reported and investigated by the Clinical Director This audit was conducted to identify the different types of medication errors from the investigations which have been conducted by the Clinical Director. Every medication error attributable wholly or in part to a doctor is referred to the Clinical Director for investigation and thereafter reporting to Clinical Governance. There were 39 incidents of medication errors that had been investigated and recorded between January 2013 and May 2014. The reasons stated for the medication errors included: • • • • • • • Too many medication cards were written on the same occasion hence increasing the risk of errors being made. Locum GP conducting clinics without having been inducted on the trust medication practice. Writing cards away from the ward. Cards not vetted for accuracy by a nursing staff after they have been written up. Patients having multiple medicine cards. Not triangulating prescription with medications tab in Care notes. Medication tabs in Care notes not adequately completed to include all prescribed medications. All the issues that arose from the audit were dealt with through the Trusts Medicine Management Committee. 21. Consultants Work Plans This audit was completed to ensure that consultants work plans set out their duties, responsibilities and objectives for the coming year is accordance to the publication by the British Medical Association (BMA). The job plan should outline the consultant’s commitments to the NHS, specifically to the Trust that has employed them. The audit found that although there were areas of full compliance there was need for improvement in the following areas: • • • 22. Capacity to Consent to Personal objectives need to be well developed so it can be embedded into future Job planning meeting, as these are meant to be distinct from the personal Development plan in appraisal. The needs of the Trust, including organisational objectives should be aligned with the Consultants job plans. There is a need to recognise areas of increase workload, including incidental demands from commissioners, Care Quality Commission (CQC) visits and CQUIN. This audit was completed to ensure that Section 58 (Consent to 72 Project Title Synopsis of Findings and Actions Medication Treatment) of the Mental Health Act is being adhered to. A list of 137 service users from across the Trust, who had a T2/T3/T6 or section 61 in place and which had recently been revised or renewed, was produced. and care notes was examined to answer 5 questions: • • • • • Is the capacity to consent documented in the clinical notes at the time of the T2/T3/T6/Section 61? Is consent /refusal/no capacity documented in the clinical notes? If yes to Q (2) did the client refuse/consent or lack capacity to consent? If the service user has capacity to consent is there evidence in the clinical notes of a discussion with the service user with regard to this? If the service user has capacity to consent is there evidence of a discussion with the service user about the treatment, side effects and alternatives? The audit showed areas of good practice but notes of concern were: • • 23. Seclusion Clinical notes in different areas of the electronic system do not correlate with one another. Less than half of service users who had the capacity to consent had a fully completed clinical note evidencing a discussion with them, with regard to their capacity to consent, when a change of T2/T3/T6/section was documented. This audit was completed to measure compliance with the aspects of the Trusts Seclusion Policy 20.2 issued 25th April 2014, with regard to the Duty Doctor attending incidents of seclusion and ensuring the correct recording of their assessment of the service user in seclusion. There were 44 incidents requiring seclusion during July 2014 which were included in the audit and the following issues were found: • • • • • 2 of the incidents were not attended by the Duty Dr. On 2 occasions there was no record of the Duty Doctor assessing the service user in seclusion. For 13 of the assessments, it was unclear from the records where the assessment took place. 11 did not have a record of the Duty Doctor authorising the continued use of seclusion. Of the duty Doctor’s assessment records audited only 10 were recorded in Care Notes and on the Seclusion Observation Chart. Following the audit the results were broken down by individual ward areas and disseminated via the ward managers and a re-audit is scheduled for 2015/2016. 24. Medicine This audit was conducted in order to establish the quality of information 73 Project Title Synopsis of Findings and Actions Management recorded on medication cards, in relation to prescribing, dispensing, checking and administration of medicines. It forms part of the Trust’s Quality Account – Metrics in relation to measures identifying the potential for errors due to the quality of record keeping. This is a Trust wide audit. The audit discovered issues with: • • Omitted medicines for short term prescriptions. Nurse’s witness signing (initialling) medicine cards after medication is administered. However, overall there has been a sustained improvement from both the medical and nursing staff. There is an action plan in place to address areas of poor compliance and a re-audit is scheduled for 2015/2016. 25. T2 This audit was conducted in order to check compliance of T2 forms against prescribed medications. All patients across the Trust with a T2 form in place were included in the audit. The T2 form was checked against medications prescribed for the treatment of “Mental Disorder” listed on the MAR Medicines Administration Sheet. The audit found the majority of T2 forms were fully compliant with requirements with only the following issues: • • There was one instance of a drug not being authorised on the T2 form. There were two instances of the maximum dose not being clearly specified on the relevant T2 form. An action plan was implemented and a re-audit is scheduled for 2015/2016. 26. Staff First Aid Kits This audit was a re-audit of that completed in March 2014 and was undertaken to ascertain whether the Trust’s First Aid at Work policy (H & S 4) was being implemented with regards to there being: • • • • • Suitable first aid boxes and kit that were accessible for staff A conspicuously positioned notice locating the box and kit and detailing staff first aiders in that area, which had been updated in the past six months Daily briefing of staff by the person in charge regarding their nearest first aider Appropriate content in the first aid box Appropriate numbers of personnel trained and holding a current First Aid at Work certificate. The audit found an improvement in the levels of compliance but there were still concerns in regards to the following: 74 Project Title Synopsis of Findings and Actions • • • Some areas had no conspicuous notices displayed. Appropriate content in the first aid box Appropriate numbers of personnel trained and holding a current First Aid at Work certificate. An action plan has been implemented and a re-audit has been scheduled for 2015/2016. 27. Rapid Tranquilisation This audit was a re-audit to establish if all instances involving the use of rapid tranquillisation have been documented in PRISM by the appropriate person(s). Also to establish if recommendations from previous audits have been achieved. The audit was carried out in both May and October 2014 due to poor levels of compliance. All service users residing at Calderstones hospital who received non oral rapid tranquillisation (IM /buccal) were included in the audit. During the audit it was found that - one incident recorded on care notes was fully compliant with regards to recording the refusal of the patient to have any physical observation carried out for the 12 hours following the administration on Rapid tranquillisation (non – oral). The audit, highlighted another incident that went someway to complying to the requirements of the procedure by recording Physical Observations being taken for up to 2 hours following rapid tranquillisation (non-oral) On one occasion the relevant person did not enter the PRISM following an incident requiring rapid tranquillisation (non oral). One service users had been administered rapid tranquillisation but the medication had not been recorded in PRISM or Carenotes. An action plan was implemented and a re-audit has been scheduled for 2015/2016. 28. Clinical Risk Management This was a re-audit of that completed in 2013-2014 and whose strategic drivers were the CQC outcomes framework. The audit’s objectives were to establish the Trust compliance with its clinical risk management procedures, to provider reasonable assurance that the Trust is complying with CQC Outcome Frame Work 4 and to determine the involvement of clients in their risk assessment. Data was obtained on all incidents reported to StEIS for Quarter 1 20132014 Apr-Jun, Quarter 2 2013-2014 Jul-Sept and Quarter 3 2013-2014 Oct – Dec. Three abscond incidents were audited to determine whether their risk assessment was reviewed or reassessed and whether the incident was recorded in the ward round following the incident and documented in care notes. The audit results showed the following: 75 Project Title Synopsis of Findings and Actions • • • • Good compliance with reporting and Service Users being seen post incident by Case Managers Client involvement with the risk assessment review poor although risks were reviewed Risks sometimes not reviewed until sometime after the incident Ward rounds cover the incidents but you have to wait for the next one. These only take place monthly. An action plan is currently in development. 29. Security of Contractors Tools entering Woodview This was a re-audit and the aim of the audit was to establish the compliance with the Trusts Security and Control of Tools, Equipment and Materials policy S1.21, with regard to contractors and their tools entering and leaving the Woodview MSU environment and contractor’s tools being appropriately identifiable. The previous audits showed no evidence that the action recommendations were implemented. Approved lists were not signed off, tools were not permanently marked, no spot checks were carried out. This audit showed some evidence that remedial works from the last audit have been implemented, however there were still significant concerns raised about the safety and effective functioning in the management of tools prior to entering a medium secure unit. An action plan has been developed and the practice and procedural elements of this activity require a complete multi-disciplinary review as a matter of urgency. 30. Handcuffs This was a new audit completed to establish the compliance with the Trusts Handcuffs Policy (S1.34). The primary aim of the activity is to assist in the management of patients, outside a clearly defined secure perimeter, whereby the significant risk factors of absconding and serious violence and aggression can be assisted by the use of a handcuffing device. The audit results highlighted significant concerns about the safety and effective functioning in the management of handcuff activity. An action plan was devised and practice and procedural elements of this activity are undergoing a complete multi-disciplinary review. A re-audit has been scheduled for 2015/2016 31. Shared Pathway Goal Setting This was a new audit completed to test how well embedded goal planning is into the ‘shared pathway’. A total of 30 service users were included looking at the following: • • Whether goals were SMART (Using clinical judgement) Reviewing ward round notes and CPA minutes for ongoing evidence of review, monitoring and achievement. 76 Project Title Synopsis of Findings and Actions • Looking for key words associated with personal goals. The audit results found several concerns including: • • • A lack of understanding of what constitutes a change, behaviour or goal. Goal setting only by nurses so no MDT ownership. Extensive evidence of staff writing literally what the service user says e.g. ‘behave’ ‘get out’ ‘get married’ An action plan was implemented and the shared pathway goal setting was integrated into the Model of Care Framework. 32. Management of choking incidents This was a re-audit to ensure that all service users who have had a choking incident have been screened to assess the risk of choking in accordance with Trust Procedure 4.15: Dysphagia dated 1st December 2013. All choking incidents that had occurred between the 1st April 2014 and 31st October 2014 were included and the following areas looked at: • • • • • • Screen reviews Severity of incident Referrals Discussions with service users Risk Training Significant failings were found in the audit. This is currently being looked at in depth by the Trusts senior managers following which an action plan will be implemented. A re-audit has been scheduled for 2015/2016. 77