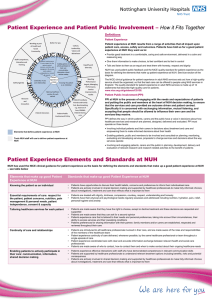
thoughtful caring safe Quality Account
advertisement

thoughtful caring safe Quality Account 2013/14 CONTENTS 01 Introduction from the Chairman and Chief Executive01 Declaration of Accuracy 03 02 Quality review of 2013/14 04 03 Quality priorities for 2014/15 12 04 Assurance of service quality in 2013/14 17 05 Quality management34 06 Workforce and quality49 07 Research & Innovation51 08Appendices 52 Appendix 1 – Statements of assurance 52 Appendix 2 – Statements of Directors’ responsibilities in respect of the Quality Account 55 Appendix 3 – NHS Outcomes Framework 56 Appendix 4 – Auditors’ Report 59 Appendix 5 – Peer hospitals 61 Appendix 6 – Glossary of terms 62 01 INTRODUCTION 01 INTRODUCTION Welcome to our 2013/14 Quality Account, which describes how well we did against our quality and safety standards. For the first time we publish this Report in the same month as our Annual Report, which provides information about how we are doing in all areas of performance, including finance. We have made strong progress against many of the quality and safety priorities we developed after listening to what our patients, carers, members and staff told us was most important to them. The views of our local health and social care partners and national requirements also influenced our priorities. We want this document to be easy to follow. Wherever possible we show (1) our performance over a number of years and (2) how we compare to other similar hospitals. We can confidently say that patients are safer in our care this year than last and that most have a good experience in our care. Our infection rates are lower than ever, we had 11.5% fewer falls, fewer deaths from severe sepsis, and significantly improved safety in our theatres. We have expanded the use of the ‘friends and family’ test to our Emergency and Maternity Departments. We have consistently been in the top quarter of trusts for response rates and scores: most of our patients would recommend our hospitals. This ward-level, near real-time patient feedback is helping us to respond quickly when there are problems. In late 2013 a 60-strong Care Quality Commission (CQC) team inspected each of the care pathways across Queen’s Medical Centre and Nottingham City Hospital over a fourday period. In February 2014 the CQC published its Report and concluded we are a ‘good trust’: safe, caring, effective, responsive and well-led. The CQC commended our hard working, compassionate and dedicated staff, and observed many examples of good and excellent practice. The CQC described two areas where we were non-compliant with the mandatory standards and need to make quicker improvement: attendance by staff at mandatory training and maintenance of medical equipment. They acknowledged we were working to improve in these areas before their inspection, but requested our improvement plans were strengthened. More detailed information about our inspection is on page 17. We recognise the importance of improving patient communication and listening to and responding to feedback. This includes involving patients and carers better in decisions about their care: improvements include the roll-out of a new nurse handover project across every inpatient ward. Cancelled operations are lower than ever, although we appreciate that one cancellation is one too many. ‘Better for You,’ our established whole-hospital transformation programme, continues to deliver exceptional results, driven by the feedback we receive from our patients, their loved ones, carers and staff. Over the last year we have brought together our programme for system and process redesign (‘Better for You’) and our Learning and Organisational Development. This is enabling us to better support all of our improvement work across safety, experience and effectiveness. We have continued to renew and update our plans to support key national developments in the last year. Our priorities have been influenced by publications including the Francis, Keogh and Berwick Reviews, and more recently by our CQC Inspection Report. For the second year running, staff voted NUH one of the best trusts in which to work. Our staff survey results put NUH in the top 25% for: job satisfaction, motivation at work, feeling able to contribute to improvements and feeling satisfied with the quality of patient care. These features were recognised by the CQC during their inspection. NUH | 2013/14 Quality Account 01 For the second year running, staff voted NUH one of the best trusts in which to work. 02 NUH | 2013/14 Quality Account INTRODUCTION 01 While we are proud of our improvements, there are some areas in which we have not made sufficient progress. We cover these areas in this Report, and describe our improvement plans. Notably, we did not achieve the four hour access target (95%) for emergency patients, despite much hard work from teams across NUH and investment in extra beds and staffing. The cumulative effect of more older and sicker patients being admitted to our hospital and unpredictable surges in demand on our emergency services put our services under extreme pressure in our busiest months of the year. We are giving very close attention to improving our internal processes to improve the timeliness and safety of emergency care. We are also working closely with our health and social care partners in the wider system to improve the timeliness of emergency care for patients. We have introduced a new rapid response team to improve cleanliness inside and outside our hospitals. However, patients, visitors and self-inspections tell us we have more work to do, including tackling smoking and consistently keeping our hospitals clean and tidy, all the time. Our priorities in the coming year will be: •Attitudes: embedding our values and behaviours, particularly in the recruitment and appraisal processes, and better involving patients in their care •Behaviour: better communication between staff and patients •Combat harms: giving increased attention to (1) harms from medicines and equipment, (2) mandatory training and (3) involving trainee staff in this programme •Doing more to improve the experience of vulnerable patients and their carers, notably those with dementia and extreme frailty •Environmental improvements •Fewer waits: in the emergency pathway at admission, at discharge (medication and transport), for communication (letters) DECLARATION OF ACCURACY I confirm, on behalf of all Executive Directors at NUH, that to the best of my knowledge the information presented in our Quality Account is accurate. Peter Homa Louise Scull Chief ExecutiveChair NUH | 2013/14 Quality Account 03 02 QUALITY REVIEW OF 2013/14 Our quality ‘6 pack’ Last year we launched our quality ‘6 pack,’ our authentic way of describing our quality priorities to our patients and staff. This is how we did in 2013/14. A: ATTITUDE & BEHAVIOUR Attitude + behaviour Be: • On guard • On stage • On duty for your patients’ experience We aimed for all staff to have attended values and behaviours training by the end of March 2013: we managed 13,200 of our 14,000 staff. We have embedded our values into our appraisal and recruitment processes by introducing behavioural-based questions and involving more patient representatives on interview panels. We evaluated the effectiveness of ‘nurse rounding’ (‘Caring around the Clock’) on patient experience following its introduction on our inpatient wards in 2012/13. Over 1,000 clinical staff contributed their views on its impact of ward-level safety and patient experience. We are working to improve consistency of practice and to build trust and confidence in our patients through regular contact and conversations with patients and relatives. 04 NUH | 2013/14 Quality Account QUALITY REVIEW OF 2013/14 02 “Throughout any treatment, referral, tests, and information-giving appointments, I have been treated with the utmost respect and spoken to as an individual.” Patient “I couldn’t imagine having a tube down my throat and every waking moment worrying about it. But when I met the nurse who was with me throughout the procedure, she guided me through everything, reassured me and stayed with me all the time.” Patient NUH | 2013/14 Quality Account 05 B: BETTER COMMUNICATION AND LISTENING C: COMBAT INFECTION, FALLS AND OTHER HARMS Better communication + listening Combat infection + falls (and other harms) Involve patients in: •Risk assess, then act on results •Use the available toolkits • Decisions about their care • Planning our services Working in collaboration with our community partners, we undertake comprehensive geriatric assessments on all of our frail older patients who are admitted as emergencies. Patients are screened and assessed to ensure they are cared for in the most appropriate place and have appropriate ongoing management plans and case managers. We have achieved high feedback rates in the ‘friends and family’ test. The information helps make rapid improvements at ward level. These have included: •A dedicated room on our Major Trauma Unit for clinicians to have confidential discussions with patients and relatives •The development of a new leaflet ‘Welcome to C31’ (an emergency admission unit) •Our short-stay emergency admissions unit at QMC now offer every patient earplugs on the evening drug round and waste-bins are now ‘quiet-closing’ •Refurbishment of a bathroom in Maternity Services Our national target was fewer than 74 cases of Clostridium difficile (C diff). We had 90 cases, which is our lowest number on record. We have had no cases of cross-infection, no outbreaks since April 2013 and no C diff-related deaths in 2013/14. No C diff cases this year have been caused by deficiencies in our care. The national target for all acute hospitals was zero MRSA bacteraemias. We had two cases. This compares favourably with many similar hospitals and has been our best performance to date. We continue work to prevent bacteraemia (blood stream infection) including by MRSA. We have an extensive programme of screening and decolonisation. The Infection Prevention and Control Team visit every newly-diagnosed MRSA positive patient, and those readmitted with MRSA, to ensure patients are offered support and correct information regarding their diagnosis, and that we do all we can to prevent serious infection. Trust estimated C diff & MRSA rates April-March 2014 Estimated MRSA rate per 100,000 bed days This year we rolled-out our new nurse handover project to all wards. This improves patient safety with fewer drugs not given and better completion of fluid balance and observation charts. The next phase of this work will see the development of an electronic handover system. 3.0 2.5 2.0 Peer trust 2013/14 1.5 NUH 2013/14 1.0 National average 2012/13 0.5 NUH 2012/13 0.0 0.0 0.5 1.0 1.5 2.0 2.5 Estimated C diff rate per 10,000 bed days My consultant @nottmhospitals was amazing yesterday. He listened and treated me as an individual.” Patient 06 NUH | 2013/14 Quality Account 3.0 QUALITY REVIEW OF 2013/14 02 CASE STUDY HOW WARD C53 AT QMC REDUCED FALLS BY 40% IN 2013/14 In 2013/14 C53 (an acute medical ward) reduced falls by 40% (from 139 to 84). The staff focused on consistent assessment for falls risk and actions prompted by the assessment. We check things that make falls more likely (eg poor sight, delirium, drugs or inappropriate footwear) and remove or reduce as many hazards as we can. Debbi Hughes, Falls Champion for the ward, said “a number of other measures have also helped, including minimising clutter in the ward, installing lamps for use at night, increased dementia training for staff, and introducing falls and dementia icons on the patient board so that staff could easily see who might be at risk”. We risk assessed 94.98% of patients for venous thrombo-embolism (blood clots) in line with the national (96%) and peer hospitals performance. We have established robust identification of all cases of hospital-acquired thrombosis. In 2013/14 there were 97 hospital-acquired thrombosis events. Themes from root cause analyses (RCAs) are shown in the chart on page 8 and inform our improvement actions. Falls We set ourselves a target of 5% fewer falls than in 2012/13. We achieved a 14.6 % reduction. We had 11.5% fewer harmful falls (vs our 10% target reduction). We had 9.3% fewer repeat fallers (short of our 15% target). Key actions to reduce falls (notably harmful falls) included: •Our Falls Prevention Team, who provide extra support to our acute medical wards. Since the team has been in place we have seen 16% fewer falls. In 2014/15 we will expand the team into other clinical areas •Nursing high-falls-risk patients in the same bay to facilitate their continuous observation •Learning from previous falls by root cause analysis, notably focusing our attention on supervising patients during toileting (while respecting privacy and dignity) NUH | 2013/14 Quality Account 07 VTE hospital-acquired thrombosis themes (April 2013 to March 2014) from RCAs We launched our ‘React to red’ campaign, which is encouraging staff to identify early skin damage and to ensure the right plan of care is in place. We have rolled-out new patient bedside chairs and pressure-relieving boots to protect patients from pressure damage. Patient lower limb fracture Extended prophylaxis prescribed % VTE not prevented This campaign and the new SSKIN bundle helped us achieve a 17% reduction in stage three and four avoidable pressure ulcers (68 compared to 82 in 2012/13). Extensive patient co-morbidities Delay to initiation of prophylaxis Stage four are the most serious ulcers with extreme skin damage. It is now 12 months since we reported a Stage four pressure ulcer. TED stockings not applied/prescribed correctly Doses of LMWH not reviewed following change in patients condition Missed prophylaxis doses/not administered Recognise and Rescue Prophylaxis prescribed & VTE not prevented 0 1 2 3 4 5 6 7 We have a Trust-wide programme to recognise patient deterioration and to reduce delays to intervention. We call this ‘Recognise and Rescue.’ Following this year’s introduction of a ‘Recognise and Rescue’ dashboard we have seen: 8 No. of Pressure ulcers •Nursing escalation of Early Warning Score increase by 46% Our target was to reduce avoidable stage two pressure ulcers by 40% in 2013/14. Following the launch of the new SSKIN bundle (and increased awareness and reporting) we have seen an increase in the number of reported stage one and two pressure ulcers. (SSKIN: Support surface, skin evaluation, keeping moving, incontinence and nutrition). •Compliance with sepsis bundle increase to 86% •Administration of antibiotics in less than an hour in severe sepsis increase to 90% •No unexpected cardiac arrests in the Nottingham Children’s Hospital since April 2013 •Failure to rescue incident reporting (i.e. identification of a learning opportunity) increased three-fold R – Remove the source of pressure E – Ensure you protect the skin A – Assess an evalutate the impact your action has had C – Communicate with your team T – Talk to your patient 08 NUH | 2013/14 Quality Account QUALITY REVIEW OF 2013/14 02 CASE STUDY SEPSIS Severe sepsis affects patients of all ages, in all specialties. It is a medical emergency: prompt treatment makes the difference between survival and death (mortality is 30-40%). Our nationally-renowned Sepsis Action Group have used a range of innovative methods to raise the profile and urgency of severe sepsis treatment, resulting in demonstrable improvements in how effectively and quickly we treat patients at high risk of death. We have seen a significant fall in critical care mortality. Compliance with antibiotics in <1hr 90 80 Percent The table right shows our improvement in giving antibiotics within the first hour of diagnosis. 100 70 60 50 40 30 Mar-14 Feb-14 Jan-14 Dec-13 Nov-13 Oct-13 Sep-13 Aug-13 Jul-13 Jun-13 May-13 Apr-13 Mar-13 Feb-13 Jan-13 Dec-12 Nov-12 Oct-12 Sep-12 Aug-12 Jul-12 Jun-12 May-12 Apr-12 Mar-12 Feb-12 Jan-12 Dec-11 Nov-11 2010 2006 20 D: DEMENTIA CARE Dementia care •Look beyond the diagnosis to the experience of your patient and their carers We have developed a three-year dementia strategy which sets out how we will further improve care for patients with dementia and their carers. The strategy focuses on five key areas: 1Personalised assessment and care plans 2Education and training of our staff 3Dementia friendly-environments 4Active research 5Involving and supporting carers of patients with dementia In 2013/14 we: •Implemented an electronic screening tool to identify potential undiagnosed dementia in emergency patients aged over 75. Patients are then referred to appropriate specialist services. By year-end, over 90% of eligible patients were being screened on the admission wards, with 100% onward referral. We are embedding this tool across all our adult wards during 2014/15. •Rolled-out learning from our specialist dementia ward (Ward B47 at QMC) to other healthcare of elderly people wards NUH | 2013/14 Quality Account 09 •Trained over 360 frontline nursing staff in advanced dementia care. A further 600 healthcare assistants attended a theatre production and participated in workshops which explored the complexities of caring for patients with dementia •Were one of just nine trusts who gained a place on the Royal College of Nursing Transforming Dementia Care programme. This year-long programme (to March 2014) explored how we can better support and develop staff to improve our care of patients with dementia. •Were shortlisted in the ‘dementia friendly hospital’ category in the national dementia care awards •Surveyed carers of patients with dementia. 71% felt involved in the care and 65% would recommend the support given by the hospital to their family/ friends Safeguarding vulnerable patients We participated in a benchmarking exercise to assess staff awareness of indicators of abuse, and ability to assess mental capacity. Wards and clinics were awarded gold, green, amber or red status. Year-on-year there was significant improvement. Over 90% of wards achieved gold or green status in 2013. There was a correlation between scores and training attendance. CQC inspectors were content that our staff had an understanding of how to protect patients from abuse. E: ENVIRONMENT IMPROVED Environment improved •Know who cleans what •Keep your area clutter-free NUH was assessed between April and June 2013 as part of the new patient-led inspections of hospital environments. NHS England introduced the new Patient-Led Assessments of the Care Environment (PLACE) to replace Patient Environment Action Teams (PEAT) inspections. Teams comprising at least 50% patients scored wards against 150 standards taking into account the cleanliness, condition, appearance and maintenance of patient areas, as well as food and hydration for patients and their privacy and dignity. Our scores (and the national average): MEASURE Cleanliness 94% 86% 96% Food 91% 86% 85% Privacy, dignity and wellbeing 85% 87% 89% Condition, appearance and maintenance 85% 76% 89% Our second PLACE audit was in March 2014. The results are expected later this year. In October 2013, in response to feedback from patients and staff, we invested in a six-strong rapid response cleaning team to help improve the overall appearance of our hospitals – inside and out. The teams take rapid action to remove clutter from main entrance areas, corridors and lift lobbies. They challenge smokers (and offer advice on how to give it up). We improved a number of our wards by creating new shower/wet room facilities. My only gripe with @nottmhospitals is that they don’t enforce no smoking – hate taking our son out the main door after clinic.” Patient 10 NUH | 2013/14 Quality Account CITY QMC NATIONAL AVERAGE QUALITY REVIEW OF 2013/14 F: FEWER CANCELLED OPERATIONS Fewer cancelled operations •Help avoid unnecessary delays, waits and interruptions by better organising your work 02 Directorate performance management Each month our directorates are held to account for their performance against the Trust’s agreed quality and performance targets and compliance with expected standards for each of their clinical services. Co-producing our quality priorities with our patients and local community Our quality improvement priorities are based on feedback from our patients, carers and staff, and on national standards. We have engaged and worked with our patients, public and carers from the communities we serve through a range of meetings and events, including: Our 2013/14 rate of on-the-day cancelled operations is our lowest ever: less than 0.8%. Our total cancelled operation rate was also lower than previous years. We remain the only Trust in the country to publish total (‘on the day’ and ‘prior to the day) cancellation rates. We committed to zero tolerance of repeat cancellations and have significantly reduced them to a total of eight in the year. We will continue with our zero tolerance approach in 2014/15. PRIORITIES FOR IMPROVEMENT & BOARD STATEMENTS OF ASSURANCE Review of services in 2013/14 •NUH Children and Young People Group •NUH Equality and Diversity Steering Group •NUH Sensory Impaired •NUH Patient Partnership Group •NUH Directorate patient (and carer) groups •Healthwatch (Nottingham City and Nottinghamshire County) •QMC Residents’ Forum •Caribbean Carnival •PRIDE •Learning Disability Big Health Days During 2013/14 NUH provided 130 NHS services as identified in Schedule two, part four of the contract between the trust and our principal commissioners NHS Nottingham West Clinical Commissioning Group. The income generated represented more than 90% of the total income generated from the provision of NHS services by NUH for 2013/14. Review of clinical strategies Over the past 24 months, NUH has reviewed all the data available to us on the quality of care in 43 clinical service strategies which covers over 90% of the 130 commissioned services at NUH. Our review included how each met current and future care quality standards. In refreshing their clinical service strategies, services were analysed against national benchmarks (on mortality, length of stay, readmission rates, waiting times, patient and staff experience scores, staff vacancy and sickness rates). We have carefully analysed the patient feedback we collect throughout the year – including from surveys, ‘friends and family’ test, complaints, social media and online feedback – to identify areas where patients say they wish to see the biggest improvements. A questionnaire tested this analysis. We surveyed our public members in summer 2013 and held a focus group. We surveyed our patients monthly to find out if they felt safe in our care. We held 857 patient involvement events across NUH with 15,890 participants during 2013/14. 43 public members contributed to our online survey on our 2014/15 priorities and objectives. 20 members attended our focus group to develop these priorities further. 60 patients, staff and members responded to our online survey which asked patients and carers for their views on what our quality and safety priorities should be in 2014/15. The result is in our updated quality ‘6 pack’ (priorities) for 2014/15. There are three key priorities – involving patients and carers in care, reducing noise at night and improving discharge. NUH | 2013/14 Quality Account 11 03 QUALITY PRIORITIES FOR 2014/15 A C E 12 NUH | 2013/14 Quality Account ATTITUDE • I am always aware of the impression I give • We only recruit colleagues whio share our values COMBAT HARMS • I attend mandatory training • We protect patients from harm from medications, infections, falls, pressure ulcers, blood clots and poor hydration and nutrition ENVIRONMENT • I do my best to keep wards quiet at night • We do our best to keep our workplaces clean and tidy QUALITY PRIORITIES FOR 2014/15 B D F 03 BEHAVIOUR • I communicate promptly and clearly to keep patients safe and well-informed • We support patients, relatives, carers and each other DECREASE DISTRESS • I use ‘About Me’ to know my patients • We adapt our practices to meet the needs of distressed, vunerable or frail patients of all ages FEWER WAITS • I prioritise ‘live a day’ actions for flow • We act quickly to avoid delays to patient’s drugs, tests, treatment and transport NUH | 2013/14 Quality Account 13 Behaviour: better communication by staff and patients (recognise & rescue and handover projects). We will: PRIORITY 1 A ATTITUDE • I am always aware of the impression I give • We only recruit colleagues whio share our values Attitudes: embedding our values and behaviours, particularly in the recruitment and appraisal processes, and in better involving patients in their care. •Our new appraisal system has as a mandatory objective for staff to demonstrate achievement of all NUH values and behaviours In 2014/15 we will •(1) Complete a values-based audit (seeking the views of patients, staff and external stakeholders) to inform the next stage of the development of our ‘culture’ •Ward teams will implement three key actions for carers (1) record their details in patient records, (2) ‘About me’ documentation will be completed with patients and carers on admission and includes information about family life, history, likes and dislikes, current routine, and usual response to stress or pain, and (3) all carers will receive trust information on ‘Caring for Carers’ •We will ensure staff are supported to better recognise patients whose condition deteriorates and escalate and handover to more senior staff compared to 2012/13 (notably in our admission areas) •Roll-out an electronic nursing handover which also captures patient acuity daily PRIORITY 3 C •(2) We will roll-out a staff-version of the ‘friends and family’ test COMBAT HARMS • I attend mandatory training • We protect patients from harm from medications, infections, falls, pressure ulcers, blood clots and poor hydration and nutrition PRIORITY 2 B BEHAVIOUR • I communicate promptly and clearly to keep patients safe and well-informed • We support patients, relatives, carers and each other 14 NUH | 2013/14 Quality Account Combat harms: (1) prevent harms from medicines, (2) improve uptake of mandatory training and (3) involve trainee staff in our safety programme. We will: •Implement a new approach to mandatory training from May 2014, which will incorporate a new all staff video for core training and local training for high risk topic areas (e.g. including fire and resuscitation training) •Develop a tool to track harm in medicines and the impact of safety actions (especially in high risk medicines e.g. insulin) QUALITY PRIORITIES FOR 2014/15 PRIORITY 4 D PRIORITY 6 DECREASE DISTRESS • I use ‘About Me’ to know my patients • We adapt our practices to meet the needs of distressed, vunerable or frail patients of all ages F FEWER WAITS • I prioritise ‘live a day’ actions for flow • We act quickly to avoid delays to patient’s drugs, tests, treatment and transport Improve the experience of vulnerable patients and their carers, notably those with dementia and extreme frailty by: Fewer waits: in the emergency pathway at admission, at discharge (medication and transport), for communication (letters) and for parking. We will •Transferring learning from our nationally-recognised ‘dementia ward’ to all healthcare of the elderly wards •(1) Reduce delays to discharges due to medication and transport delays •Ensure we screen all emergency inpatients over the age of 75 for dementia and referring to the most appropriate services as promptly as possible •(2) Reduce wait time for patient letters PRIORITY 5 E 03 ENVIRONMENT We will monitor and report progress against each of these priorities to Trust Board and in performance meetings with our commissioners. Our ‘Better for You’ programme will also focus on •Re-designing outpatient services •Reducing readmissions • I do my best to keep wards quiet at night • We do our best to keep our workplaces clean and tidy Environmental improvements, including: •(1) Ward focus on reducing noise at night from both staff and other patients by delivering on individual ward pledges and updating patient information about the use of mobile phones •(2) Working with our staff, partners, local residents and Carillion, our new provider of Estates and Facilities services, we will (1) reduce smoking outside our hospitals, (2) improve responsiveness when areas are not clean and uncluttered •(3) Implement the improvements recommended in the 2014 PLACE audit I waited a long time for an appointment which was booked over the telephone. I telephoned to confirm the details two days prior to the appointment as I had not received a letter only to be told that my appointment had been changed and I had missed it. At no point have I received any correspondence via mail from the hospital regarding the appointment, I now have to wait another two months which is unacceptable. Surely the booking department could have contacted me by phone as they did in the first instance.” Patient NUH | 2013/14 Quality Account 15 COMMISSIONING FOR QUALITY AND INNOVATION (CQUIN) GOALS AGREED WITH COMMISSIONERS FOR 2014/15 Delivery: Assurance There are regular CQUIN performance meetings with commissioners to assess progress and from 2014/15 is included within our ‘Better for You’ whole hospital programme management governance framework. The Trust Board receives quarterly reports. CQUIN goals agreed with commissioners for 2014/15 Nationally-determined 1‘Friends and family test’ (FFT): to include staff FFT, and roll-out to outpatient settings by October 2014 2Safety Thermometer: focus on further reducing pressure ulcers 3Dementia screening, clinical leadership and supporting carers: for 90% of patients aged 75 years and over admitted as an emergency Locally-agreed 1Scope the number of patients attending outpatients and who are admitted to hospital who have fallen within the last 12 months 2Improve patient experience by improved complaints management 3Reduce delays in the management of high risk patients undergoing emergency surgery 4Improve the care of patients who deteriorate whilst in hospital 5Improve patient safety in transfers of care from and to hospital 6Information sharing: cross-organisational shared protocols and information sharing agreements 16 NUH | 2013/14 Quality Account Specialised CQUINS 1Specialised services quality dashboards. To ensure providers embed and routinely use the clinical dashboards developed in 2013/14 2Highly-specialised services to hold a clinical outcome collaborative audit workshop 3HIV: GP registration and communication. The proportion of patients diagnosed with HIV registered with and disclosed to their GP with at least annual communication 4To achieve an increase in percentage of pre-term babies who receive some of their mother’s milk at final discharge from neonatal care 5Specialised orthopaedics (Adults) Network Development. To ensure that complex cases (mainly revisions) are discussed at network 6Access to prosthetics mutli-disciplinary team (MDT) assessment. All new referrals to be triaged within four weeks and offered a MDT within six weeks 7Increase effectiveness of rehabilitation after critical illness. Implementation of rehab prescription for all patients on discharge from critical care Further information on last year’s and this year’s CQUINs can be found at www.nuh.nhs.uk. 04 ASSURANCE OF SERVICE QUALITY IN 2013/14 04 ASSURANCE OF SERVICE QUALITY IN 2013/14 NUH was registered with the QCQ in 2010, and we have continued to maintain our registration without conditions or enforcement action during 2013/14. CQC INSPECTION IN 2013 The Trust was inspected three times by the CQC during 2013. A responsive review at QMC campus in July 2013, considered outcome two (consent to care and treatment), and 13 (staffing), CQC concluded that the Trust had met outcome two, but had not met standard 13, but that the impact on patients of this non-compliance was minor. The CQC undertook a follow-up review of compliance with outcome 13 in October 2013 and judged that the Trust was now meeting this standard. NUH underwent a wave one acute hospital inspection in November 2013. This was one of the new style Chief Inspector of Hospitals inspections. The CQC concluded that our services are safe, caring, effective, responsive and well-led. A team of over 60 inspectors, including doctors, nurses and patients visited our hospitals (planned and unannounced) in November/December 2013. They examined most of our services in detail. This included our Emergency Department, medical, surgical and maternity care, and outpatients. They inspected our care of children, frail older people and at the end of life. They assessed our complaints process. CQC spoke to patients, carers, visitors and staff and to other organisations, including local commissioners. NUH | 2013/14 Quality Account 17 As a Trust committed to making continuous quality improvements, we work hard to learn from feedback we receive from patients and partner organisations. We appreciate we can always do better. The inspection identified two areas which need quicker improvement – we were improving before the inspection, but need to move faster and more effectively.” Peter Homa, Chief Executive The CQC Report said inspectors saw examples of compassionate care. We found staff to be hard working, caring and committed. We noted many staff spoke with passion about their work and were proud of what they did.” The report describes we have an open culture – staff feel able to report issues and raise concerns, and we learn from patient safety incidents. Many examples of good patient care and excellent work were identified, including: •The commitment shown by staff to provide the best possible patient care •Our regional trauma centre and critical care units providing effective care and very good outcomes for patients •Delivering person-centred care on our dementia wards •The hand-written letters sent to relatives of deceased patients by our bereavement nurse on the Lyn Jarrett Unit (observation and treatment unit) at QMC •The quality of bereavement care offered by our multifaith centre and compassion shown by staff working in the mortuary towards relatives and friends of deceased patients •Our comprehensive geriatric assessment for frail older people, which is improving the experience for older patients in our care ACTION WE ARE TAKING TO IMPROVE: 1. Attendance at mandatory training Mandatory training is how staff keep up-to-date in crucial skills. Despite considerable efforts, fewer than 50% of staff were up-to-date midway through 2013. Although the CQC were satisfied there had been no adverse impact on patient care, the Trust Board had earlier instructed that exceptional measures be taken to substantially increase training attendance. There has been considerable improvement since October 2013, when a new training video was introduced for all staff (now watched by 11,796 staff). Our target is that all staff will have watched the film by the end of March 2014. Some staff require additional specialised training. We aim to have delivered this training in the highest risk topics by April 2015. A new approach to mandatory training is being adopted from May 2014. 2. Medical equipment maintenance We use several thousand types of medical equipment. We have struggled to undertake manufacturers’ recommended maintenance schedules on all items. We have undertaken a thorough risk assessment to identify priorities for maintenance, even as we expand the number of machines and equipment. CQC identified that we had to accelerate this programme. Other areas CQC suggest we could make improvements include: •Recording use of controlled drugs •Adopting recognised tool to calculate necessary staff levels in children’s wards and departments •Our outpatient service to ensure consistently good practices •Visitors’ access to hot meals after 2pm •Privacy and dignity in the Emergency Department when the department is busy and under pressure •The care and range of services at Hayward House at City Hospital •Hand gel dispensers should not be empty •Medical staffing levels and the support given to doctors in training by senior medical staff •More patient information in different languages and formats •Board governance and leadership •Ensuring children are given opportunities to give feedback on their experiences in our care The Chief Inspector of Hospitals for CQC, Professor Sir Mike Richards, said: •Reviewing the time patients wait for outpatient appointments and ensure people are given information about waiting times “Staff we spoke to were positive and engaged and patients we spoke to were generally positive about the care that they had received at the hospital. There are improvements that could be made at the trust to improve the care delivered to local people, but overall we judge this to be a good trust.” 18 NUH | 2013/14 Quality Account •Improving outpatient follow-up appointments in ophthalmology ASSURANCE OF SERVICE QUALITY IN 2013/14 Our Inspection Report is available to read here on our website: www.nuh.nhs.uk. Executive Directors undertake monthly unannounced ward visits, using the CQC’s framework and standards, to monitor progress against the essential standards. PARTICIPATION IN NATIONAL CLINICAL AUDITS 2013/14 04 which trusts should consider in their 2013/14 Quality Account. During that period, NUH participated in 92% (47) of the national clinical audits (NUH is not eligible for four) and 100% of national confidential enquiries. The national clinical audits and national confidential enquiries that NUH was eligible to participate in are listed in the table below. During 2013/14 the Department of Health described 51 national clinical audits and six national confidential enquiries NATIONAL AUDIT 2013/14 Moderate or severe asthma in children (care provided in Emergency Departments: College of Emergency Medicine) Dementia PARTICIPATION NUMBER OF CASES ELIGIBLE/ REQUESTED FOR SUBMISSION % OF CASES SUBMITTED (OR NO CASES) Yes 50 100% No data required N/A N/A Emergency use of oxygen (STEAT) No 0 Lung cancer (subscription funded from April 2012) Yes 450 National Review of Asthma Deaths No 2 0 Paracetamol overdose (care provided in Emergency Departments: College of Emergency Medicine) Yes 50 100% No data required N/A N/A Yes 50 100% Pulmonary hypertension (Pulmonary Hypertension Audit) Severe sepsis and septic shock (College of Emergency Medicine) National COPD Audit Inpatient Falls Audit (part of overall FFFAP) Rheumatoid and early inflammatory arthritis (new NCAPOP topic under development) Data collection ongoing 14 No data required N/A N/A Data collection not commenced yet N/A N/A Prostate Cancer (new NCAPOP topic under development) Yes 1 survey 100% National comparative audit for use of Anti-D Yes 131 100% National Emergency Laparotomy Audit 2013 Yes approx 96 35% Inflammatory bowel disease Includes: Paediatric Inflammatory Bowel Disease Services Yes Biologocal Therapies Ulcerative Colitis 50 100% Oesophago-gastric cancer (NAOGC) (subscription funded from April 2012) Yes >150 100% Bowel cancer (NBOCAP) (subscription funded from April 2012) Yes 432 90% NUH | 2013/14 Quality Account 19 NATIONAL AUDIT 2013/14 Sentinel Stroke: National Audit Programme (SSNAP) – programme combines the following audits, which were previously listed separately in the Quality Account: a) Sentinel stroke audit (2010/11, 2012/13) b) Stroke improvement national audit project (2011/12, 2012/13) PARTICIPATION Yes NUMBER OF CASES ELIGIBLE/ REQUESTED FOR SUBMISSION % OF CASES SUBMITTED (OR NO CASES) a ) 298 a) 87% b ) 298 b) 76% Adult cardiac surgery audit Yes Myocardial Ischaemia National Audit Project (MINAP): formerly Acute coronary syndrome or Acute myocardial infarction (MINAP) (subscription funded from April 2012) Yes 1597 89% Cardiac arrhythmia: now known as Cardiac Rhythm Management Yes 1073 100% Heart failure (subscription funded from April 2012) Yes 406 39% Congenital heart disease (Paediatric cardiac surgery) Yes 33 100% Coronary angioplasty (subscription funded from April 2012) Yes 1321 100% Diabetes (Adult) ND(A) Yes Unknown 4013 National Diabetes Inpatient Audit Yes 171 96% National Vascular Registry (elements will include CIA, National Vascular Database, AAA, peripheral vascular surgery/VSGBI Vascular Surgery Database) Yes Renal replacement therapy (Renal Registry) Yes 1217 100% Renal transplantation (NHSBT UK Transplant Registry) Yes 95 100% No data required N/A N/A Data collection ongoing N/A N/A Chronic kidney disease in primary care (new NCAPOP topic under development) Epilepsy 12 audit (Childhood Epilepsy) Maternal, infant and newborn programme (MBRRACE-UK)* *This programme was previously also listed as Perinatal Mortality Data collection ongoing Yes Diabetes (Paediatric) (NPDA) Yes Neonatal intensive and special care No Paediactric bronchiectasis (British Thoracic Society) Paediatric asthma (British Thoracic Society) 20 NUH | 2013/14 Quality Account 62% 100% 340 85% Yes 6 100% Yes 21 80% ASSURANCE OF SERVICE QUALITY IN 2013/14 NATIONAL AUDIT 2013/14 PARTICIPATION Paediatric intensive care (PICANet) Yes Child health programme (CHR-UK) (also known as the Child Health Clinical Outcome Review Programme) No National Audit of Pregnancy (Diabetes) Head and neck oncology (subscription funded from April 2012) Ophthalmology (new NCAPOP topic under development) NUMBER OF CASES ELIGIBLE/ REQUESTED FOR SUBMISSION % OF CASES SUBMITTED (OR NO CASES) 343 92% Yes Unknown 49 Yes 174 100% Data collection not commenced yet N/A N/A National Joint Registry DATE (NJR) Yes 1731 100% National hip fracture database Yes 794 100% Fracture liaison service Yes Unknown 658 Elective surgery (national PROMs programme) Yes 1489 97% National audit of seizure management (NASH) No 30 0 Adult critical care (case mix programme – ICNARC CMP) Yes 2501 100% Severe trauma (Trauma Audit and Research Network, TARN): TARN is a Research Database that is utilised in reporting the Major Trauma performance and best practice tariff Yes 1079 100% National Cardiac Arrest Audit (NCAA) Yes 134 100% Data collection has not commenced N/A N/A Specialist rehabilitation for patients with highly-complex needs (new NCAPOP topic under development) 04 *IT data collection issues. Therefore October-December data only available NUH | 2013/14 Quality Account 21 PARTICIPATION IN NATIONAL CONFIDENTIAL ENQUIRIES/INQUIRIES 2013/14 During 2013/14 we participated in all relevant enquiries undertaken by the National Confidential Enquiry into Patient Outcome and Death (NCEPOD) and by the Maternal Infant and Newborn Programme (MBRRACE-UK). NCEPOD helps improve standards by identifying common poor practice. For the relevant published reports, NUH has identified a consultant who leads our consideration of the report and makes recommendations to the Trust’s Clinical Effectiveness Committee. TITLE OF STUDY RETURN RATE* (% OF ELIGIBLE CASES SUBMITTED BY NUH) Alcohol related liver diseases 100 Subarachnoid haemorrhage 100 Tracheostomy care 100 Maternal and perinatal mortality surveillance 100 Lower limb amputation 100 – still ongoing Sepsis study Study ongoing *Relates to case notes requested and returned. In 2013/14, no NUH patients were eligible for the National Confidential Enquiries (NCI) into Suicide and Homicide by People with Mental Illnesses (NCI/NCISH). RESPONSE TO NATIONAL CONFIDENTIAL ENQUIRIES 2013/14 •Audit of colorectal Enhanced Recovery After Surgery (ERAS). ERAS success is dependent on both patients and staff compliance with the multi-faceted ERAS protocol. The number of patients being discharged by the target day has more than doubled and the number of patients succeeding on the colorectal ERAS programme rose from 13.8% in 2012 to 39.3% in 2013 In 2013/14 two National Confidential Enquiries were published relevant to the services provided by NUH: Alcohol-related liver diseases – measuring the units (June 2013) and subarachnoid haemorrhage – managing the flow (November 2013). •Radiology reduced the shock frequency in Lithotripsy (used to shatter kidney stones). The treatment success rate was improved: total clearance rate (no stone fragments left after treatment) 53% vs 44%, additional procedures (21% vs 36%), complication rate (2% vs 10%) Consultants have been involved in reviewing each Report and identifying what actions are required to implement the recommendations at NUH. Both Reports have been discussed in detail at our Clinical Effectiveness Committee, a sub-committee of the Quality Assurance Committee. The Quality Assurance Committee received the following internal reports (and where necessary action plans) prompted by external alerts during 2013/14: LEARNING FROM CLINICAL AUDITS 2013/14 The Clinical Effectiveness Committee receives Reports and updates from departments across the Trust against relevant national and local audits. •Report on coronary atherosclerosis and other heart disease following CQC alert •Report on deaths amenable to healthcare prompted by a Dr Foster alert •Case note review on deaths coded as dementia/senility prompted by a Dr Foster alert During 2013/14 the Clinical Audit Plan consisted 348 audits, (47 were national audits). •Retrospective audit following a Dr Foster mortality alert for diagnosis group pneumonia Some examples of improvements as a result of audits are: In each case, NUH analysis and investigation offered assurance for each alert with no indication of poor standards of care. 22 NUH | 2013/14 Quality Account ASSURANCE OF SERVICE QUALITY IN 2013/14 PERFORMANCE AGAINST 2013/14 CQUIN GOALS AGREED WITH COMMISSIONERS CQUIN framework 2013/14 04 of NHS services. These goals are known as CQUIN’s (Commissioning for Quality Improvement and Innovation payment framework). We had three national, six local, eight specialised and two community CQUINs in 2013/14, with a total value of £16,041,737. 2.5% of the NUH’s contract income 2013/14 was conditional on achieving quality improvement and innovation goals we agreed with persons and bodies with whom we entered a contract, agreement or arrangement for the provision DESCRIPTION OF EACH GENERAL CQUIN PROGRESS ACHIEVEMENT/ NON-ACHIEVEMENT Expansion of ‘friends and family’ test to Emergency Department (ED) and Maternity Services Implemented in both the Emergency Department and Maternity Services Achieved NHS Safety Thermometer: harm-free care. Collection of Data collection process in data on pressure ulcers, falls, catheter-associated urinary place tract infections, VTE reported monthly Achieved Dementia screening for emergency admissions aged 75 years and over to include case finding risk assessment, investigation and referral to specialist services System developed and screening in place Achieved Named clinical leadership and appropriate training for staff In place Achieved Undertake a monthly audit of carers of people with dementia to test whether they feel supported Monthly audit in place. Scores improved Achieved Theatre safety: pre-list briefings to 90% compliance, cultural survey, action plan and implementation 90% compliance Achieved Patients perception of safety: monthly survey In place and results show improvement in perceptions Achieved Diabetes: reducing the length of stay for patients with diabetes by one day Data analysis and review of national data identified this was not achievable Commissioners agreed to suspend this element Reduction in insulin medication errors: 80% error-free 84% error-free Achieved Deteriorating patient: increase in proportion of patients to 60% who receive all elements of the surviving sepsis resuscitation bundle admitted to intensive care 86% exceeded our target Achieved Timely x-ray results to GP: number reported on within three days 90% by the end of March 2014, and number reported on within five days 95% by end March 2014 Both targets met Achieved Reducing harm by correct use of the early warning score on patients admitted to acute admission wards for adults and children Achieved 4/5 targets Partially achieved NUH | 2013/14 Quality Account 23 Specialised and Community CQUINS for 2013/14 DESCRIPTION OF EACH GENERAL CQUIN PROGRESS ACHIEVEMENT Q3 Dashboard: to implement the routine use of specialised services clinical dashboards in the following areas: radiotherapy, cystic fibrosis and paediatric neurosurgery Data submitted Achieved Adult neurosurgery: to ensure patients receive optimal outcomes from neurosurgical shunt surgery Performance report submitted meeting compliance against key indicators Achieved Cardiac Surgery: reduce inpatient waits: 71.6% to be treated within seven days 92.7% Achieved Bone Marrow Transplant (BMT): Donor acquisition measures. This is aimed at gaining a better understanding and improvement of a number of processes used to identify unrelated donors. All four elements are equally weighted at 25% of the CQUIN value Process in place to submit information on number of UK donors, tests, Achieved searches and turnaround times To reduce the cold ischaemic time for all kidney transplants. This is a two part CQUIN looking at donations after brainstem death (DBD) and donations after circulatory death (DCD). The target is 90% transplants to take place with less than 18/12 hours of cold ischaemic time for DBD/DCD transplants Data presented, including exceptions. Working group established to Achieved review practice to achieve target Neonatal Intensive Care: CONS infections – to achieve a reduction in the rate of central venous catheter-related coagulase negative staphylococcus (CONS) bloodstream infections Rate-reduction to 11.7% Achieved Paediatric Intensive Care: monitoring and minimising the number of children transferred out of region to a PICU Data submitted – NUH service transfers in patients rather than transfers to other centres Achieved Fetal medicine: 90% of tertiary referrals to be seen within three days 100% Achieved Community CQUINS percentage of 15-25 year olds taking up offer of Chlamydia screening. A strategic priority is to ensure Chlamydia screening is promoted to the target age group and is available in a choice of venues. Uptake needs to increase in line with the national target together with appropriate targeting to increase diagnosis of the positive cases. This scheme is managed jointly by Nottingham City (target 25%) and County (target 44%) Public Health Community CQUINS percentage of CASH core service contacts who are prescribed a Long Acting Reversible Contraception (LARC) as a % of core service contacts – a strategic priority is to ensure access to the full range of contraception is available to all. LARC methods are highly effective and cost effective. As uptake is lower than required within NHS CASH core services, an increase in the provision of LARC is a proxy measure for wider access to the range of contraceptive methods and should also lead to a reduction in rates of unintended pregnancy. This scheme is managed jointly by Nottingham City and County Public Health with a target of 33% 24 NUH | 2013/14 Quality Account 44% city patients 43% county patients Achieved 34.7% for city patients 33.9% for county patients Achieved ASSURANCE OF SERVICE QUALITY IN 2013/14 WHAT OTHERS SAY ABOUT NUH Dr Foster Hospital Guide The Dr Foster Hospital Guide – available at www.drfosterhealth.co.uk – was published in November 2013. It is an independent assessment of standards of care and clinical outcomes. This year the guide returned to the subject of hospital care at weekends and looked at a wide range of measures – mortality rates, readmission rates, access to diagnostic tests and the length of time that urgent patients wait for surgery. NUH performed as expected for Hospital Standardised Mortality Ratio (HSMR) and deaths after surgery and better than expected on Summary Hospital level Mortality Indicator (SHMI) (see section on Outcomes Framework). Our weekend mortality rates for emergency admissions were identified by Dr Foster as being higher than expected in 2011/12 in three specialties; trauma and orthopaedics, cardiology and general surgery. 04 NHS Litigation Authority (NHSLA) risk management assessment Previously, organisations were required to be assessed against a set of risk management standards that had been developed from key issues identified through claims and incidents. NHSLA have decided that no further assessments will be undertaken after March 2014. They are moving the focus to improving outcomes, learning lessons from claims and improving patient and staff safety. This new approach is also designed to reduce duplication of activity carried out by other external agencies. NUH has achieved compliance at level one of the Trustwide standards and in March 2014 reached level two of the maternity standards. We will continue to monitor our performance against Trust policies which reflect NHSLA standards through our NHSLA working group. 4Cs We have worked with Dr. Foster to better understand this data. The risk of dying is greater for emergency patients admitted at weekends (compared to weekdays) but when adjustment is made for the higher age and more severe illness of weekend admissions (Dr. Foster does not do this), this mortality is not significantly higher than expected. 2013/14 is the fifth year we have been using the 4C (complaints, concerns, comments and compliments) approach to capture feedback from patients, carers and families. Quarterly reports demonstrating themes from complaints and examples of learning are received by the Quality Assurance Committee. Even with Dr Foster unadjusted data our mortality rates have reduced from significantly higher than expected to within the expected range for emergency admissions at weekends in the most recently available data (April-February 2014). It is our ambition to roll-out innovation which further improves outcomes both in week and at weekends. The charts on page 26 describe the number of complaints received and the number referred to the Parliamentary Health Service Ombudsman (PHSO), and the five most common complaint themes for years 2010/11–2013/14. There are examples of learning from complaints on pages 27-28. Since NUH became the region’s major trauma centre in April 2012, we have had 24-hour consultant cover in our Emergency Department, increased our emergency theatre capacity in and out of hours, and doubled the number of consultant anesthetists present on site during weekdays, out of hours and over weekends. We also provide a tertiary specialist cardiology service, admitting the most severely-ill heart patients. NUH | 2013/14 Quality Account 25 Number of local complaints and Ombudsman referrals 2010/11 2011/12 2012/13 2013/14 Complaints 737 876 819 693 Ombudsman contacts 67 51 78 *awaiting response from PHSO Ombudsman referrals upheld against the Trust 2 fully (both investigations from 2009/10) 2 fully (both investigations from 2009/10) 1 fully 1 fully Most frequent complaint themes 2010/11 2011/12 2012/13 2013/14 Standards of care (medical) Standards of care (medical) Standards of care (medical) Standards of care (medical) Standards of care (nursing and midwifery) Standards of care (nursing and midwifery) Manner and attitude Complications Manner and attitude Manner and attitude Complications Manner and attitude Complications Complications Communication Standards of care (nursing and midwifery) Communication Communication (patient safety) Discharge Delays * Final figures from PHSO not available until June/July 2014 26 NUH | 2013/14 Quality Account ASSURANCE OF SERVICE QUALITY IN 2013/14 04 Examples of learning and actions from complaints (including case study) QUALITY OBJECTIVE AREAS OF CONCERN ACTION TAKEN Better communication and listening • Plans for care and clinical intervention not being fully explained • ‘Caring around the Clock’ (hourly rounding) enables patients and relatives to ask questions about their care and treatment in a timely way • Lack of communication leading to increased concerns of relatives • Vascular services have developed information for patients and relatives giving information regarding when ward rounds occur, and how to access consultants to ask questions and receive explanations • Concerns regarding lack of information regarding diagnosis of condition • Reviews of clinic slots to accommodate additional follow up slots for patients requiring explanations and further information • The outcome and learning from complaints being shared in multi-disciplinary team meetings • The introduction of ‘Accountability around the Clock’ ensures that information relating to care and treatment is passed on between staff members at shift changes Combat falls • Relatives unhappy that their father fell whilst in hospital • Poor communication relating to relative’s fall during hospital stay • Ward teams have adopted ‘safety briefings’ where patients who are at risk of harm, e.g. falls are discussed and actions planned to prevent • NUH campaign: ‘Act Now….Stop Falls’ adopted in all areas – the focus of our campaign in 2013/14 was on preventing falls when toileting and by cohort nursing • Use of the ‘Falls Toolkit’ – this ensures risk assessment is completed on patients and the appropriate plan of care is implemented • Falls booklet available in all wards explaining ways to help prevent falls in hospital Attitude and behaviour • Patient expressed concern that the pain he was experiencing after surgery was not taken seriously • ‘’Nurse rounding’ enables the patient to have regular assessment of pain, and pain killers as required • Through ‘nurse rounding,’ Ward Sisters undertake leadership rounding where they speak to patients, and also observe how their team are interacting with patients and relatives so issues with poor behaviour can be addressed at the time NUH | 2013/14 Quality Account 27 CASE STUDY UNSATISFACTORY END OF LIFE CARE Background: The daughter of a lady who was terminally ill was unhappy with the care her mum received and felt we had let her mum down. She was transferred from QMC to City Hospital in her nightclothes in a cold ambulance. Her mum was then transferred to two wards which she believed were unsuitable for her mum as she was terminally ill. Her ultimate transfer to the palliative care ward did not meet her expectations: it was noisy and there was no single room. She felt that her mum’s final hours were undignified. Areas of concern: Actions taken •Ward staff lacking in the skills to care for the dying •NUH End of Life Steering Group established in July 2013 to develop the end of life care plan for use in all areas of the Trust •Inappropriate transferring of the patient •Lack of privacy and dignity at end of life •The Development of the ‘End of Life’ Benchmark has been developed so that end of life care is now formally monitored against a set of ‘best practice’ standards in all in patient areas •All ward areas have End of Life champions who lead on the training and development of wards staff in relation to End of Life care •A targeted educational initiative has been developed to support rapid discharge home process for patients who express a wish to return home for End of Life care IMPROVING COMPLAINT HANDLING PATIENT SURVEYS •2013/14 was the first full year in which we have used the Patients’ Association Peer Review process. Six complaint responses a month are scored (poor to excellent) by a panel of professionals and patient representatives. After early analysis we are currently piloting a new investigation and response methodology We monitor and measure patient experience and satisfaction in a range of ways, including complaints, national surveys, local surveys, the friends and family test, social media and online patient feedback. •In the Complaint Benchmarking Survey complainants are surveyed after their complaint is closed. Feedback to date suggests we often do not fully address complainants’ concerns in our responses. We are now more frequently offering complainants a meeting (rather than only a letter) to more fully understand and resolve their concerns The 2013 inpatient survey results were published in April 2014. Patients were asked 85 questions. This year we scored significantly better than last year for 12 questions (see chart opposite): Learning from complaints is presented via patient stories by clinical colleagues every month at our Public Board meeting. These stories are published on our website. 28 NUH | 2013/14 Quality Account INPATIENT SURVEY (GENERAL) The survey was carried out on a random sample of patients who stayed at City Hospital or QMC in July 2013. Of 817 patients asked 392 responded. ASSURANCE OF SERVICE QUALITY IN 2013/14 04 OUR PATIENT SURVEY RESULTS 2013 OUR I SURV NPATIEN T E WAY Y IS ON E S PATIE WE MEA OF THE N S AND T EXPER URE SATI I SFAC ENCE TION Resu . lts We did significantly better in 12 key areas are u from th s is sur feed ed, alon vey g b sour ack from with ces, in othe Frien r cludin d comp s and Fa g the m laint feed s and ily test, b unde ack, to b online e r patie stand wh tter nts t hink at abou t us.. . Feedback we receive from patients throughout the year – including these survey results – have been used to inform our 2014/15 quality priorities (our quality ‘6 pack’). Information given about your condition/treatment in the Emergency Department 7.9 8.7 Information received about danger signals to watch out for on discharge 4.9 5.8 Privacy when being examined/treated in the Emergency Department 8.4 9.0 Discussions on equipment or home adaptations needed on discharge 7.4 8.5 Waiting time for a bed or ward 7.4 8.3 Accessibility and usefulness of appointment letters 8.5 9.0 Cleanliness of room or ward 8.5 8.8 Whether patients were treated with respect and dignity overall 8.7 9.1 Cleanliness of toilets and bathrooms 8.0 8.4 Overall experience 7.8 8.1 Emotional support from staff 6.7 7.4 If patients were asked to give their views on the quality of their care 1.5 2.4 We didn’t score significantly worse in any area in 2013 Vs 2012 Scores are on a scale of 1-10 (10 = best) MATERNITY SURVEY Approximately 10,000 babies are born each year in our two maternity units. The national maternity survey (December 2013) gave us a greater insight into women’s experiences of these units. 150 women responded (response rate 45%, similar to the national average). Our scores were in the ‘expected range’ for a trust of our size and for the types of patients we care for during labour and birth. We can do better in after-birth care and advice to women about feeding. We have an action plan to address this. The full reports are available on our website at: www.nuh.nhs.uk. ‘FRIENDS AND FAMILY’ TEST Since April 2012, patients leaving our hospitals (on the day of discharge or within 24 hours) have been invited to give feedback on their care and experience by answering one simple question: “how likely is it that you would recommend this service to a friend or your family?” In April 2013, along with other NHS trusts across England, we extended this question to our Emergency Department patients. We welcomed the introduction of the ‘friends and family’ test in Maternity in October 2013. Our inpatient, Emergency Department and maternity results are continuously improving. We publish our results and how we compare to our peers every month on our website at www.nuh.nhs.uk. ELECTRONIC LOCAL INPATIENT SURVEYS 10,165 inpatients, 5,437 outpatients and 800 carers completed an electronic survey, providing important information about their experience in our care and allowing us to track month-on-month changes. Between April 2013 and March 2014, 76.1% of inpatients and 87% of outpatients surveyed felt they were involved as much as they wanted to be in decisions about their care and treatment. 65% of carers (non-dementia) and 71% of carers (dementia) surveyed felt that they had been involved and we had worked with them as carers. NUH | 2013/14 Quality Account 29 SOCIAL MEDIA SUPPORTING CARERS The Trust receives increasing feedback via social media and other online feedback forums, including Twitter, Facebook, Patient Opinion and NHS Choices websites. We have a system in place to monitor and respond to such feedback 24/7. This feedback is fed into the 4Cs process to give a rounded picture of patient experience, and is shared with the relevant ward/clinical area for information and action. In 2013/14 we: In 2013/14 NUH had 500 mentions on Twitter, of which approximately 100 were complaints. Most of these complaints were about smoking, car parking and waits (on the phone and waits for appointments). In the same period NUH received 214 comments from patients via Patient Opinion and NHS Choices, of which 126 were positive and 73 were negative/complaints. Themes from this feedback included waiting times and appointments, and attitude and behaviour. 15 STEPS CHALLENGE Our ’15 steps’ challenge ward visits are carried out twiceyearly by patients, Board members and clinical colleagues. In 2013we did walkabouts in April and October. They look at care and the environment through the eyes of patients and help us to focus on first impressions of our wards (we know this impacts on patients’ confidence in our care and services). In 2013/14 the ’15 steps’ visits prompted several changes. We worked with our patients to standardise ward performance boards, (including only information that is relevant to patients and their carers in a format they can easily understand). 30 NUH | 2013/14 Quality Account •Developed support and information for carers through activities and events during carers week •Reviewed our ‘Caring for Carers’ cards at ‘About Me’ document •Introduced carers surveys Over the coming year we will: •Implement our updated Carers Policy (includes carers toolkit) •Continue with monthly carers surveys ASSURANCE OF SERVICE QUALITY IN 2013/14 04 DATA QUALITY MANAGEMENT AND ASSURANCE NHS NUMBER AND GENERAL PRACTICE CODE VALIDITY Improving data quality The Trust submits records to the Secondary Uses Services (SUS) for inclusion in the Hospital Episodes Statistics. Between April 2013 and January 2014 the NHS number was included in 99.7% (99.1% previous year) of admissions and 99.4% (99.3% previous year) outpatients. Data has not been included for Emergency Department as difficulties have been experienced with our local EDIS system and figures are artificially low. A valid General Medical Practice Code was included in 100% submissions (as in 2012/13). Our Data Quality Team has a proactive approach to the accuracy and completeness of data. The keystone of data is the patient’s NHS Number. Once this is obtained, the patient’s identity is verified and all other demographic data items can be searched in national databases. Our team work with frontline staff fixing issues where they arise. Extensive work has been done to enable Emergency Department Assistants to capture the patient’s NHS Number when they first present to the department. This has resulted in improvement in the timeliness and accuracy of our data capture. CLINICAL CODING AND ERROR RATE Clinical coding translates medical terminology written by clinicians to describe a patient’s diagnosis and treatment into standard codes. Our data is normally taken from external audits commissioned by the Audit Commission. This year, only trusts with the poorest coding rates were audited. NUH was not subject to the Payment by Results clinical coding audit during 2013/14 and is one of the strongest performing trusts (we are in the best 25% of trusts for error rates). The Data Quality team had an extensive work programme including cleansing four years of historic data prior to successfully migrating our huge data store and multiple systems to a new data collection and storage system (PAS). Over the next year, our Data Quality team will be taking the following actions to improve data quality: INFORMATION GOVERNANCE •Investigate and, where possible, enable improvement in the accuracy of other demographic data items (such as the identity of patients) •Work with wards and other colleagues to establish procedures and standards for timeliness in updating patients’ whereabouts Information governance guides organisations in handling all information, in particular the personal and sensitive information of patients and employees, legally, securely, and confidentially. The Information Governance Toolkit allows NHS organisations to self-assess their compliance with current legislation and national guidance. The Trust’s overall Toolkit score for 2013/14 was again 80% and graded as ‘not satisfactory’ (red). The Trust achieved a satisfactory standard for 44 out of 45 Toolkit requirements. The one deficiency was a requirement for all staff to complete information governance training annually. For 2014/15 the Trust has commissioned a mandatory training film that incorporates information governance, and has in place a robust plan for all staff to attend. Information Governance toolkit self-assessment 2011/12, 2012/13, 2013/14 INFORMATION GOVERNANCE TOOLKIT PERFORMANCE 2011/12 2012/13 2013/14 Information governance management 66% 73% 80% Confidentiality and data protection assurance 66% 74% 74% Information security assurance 80% 84% 84% Clinical information assurance 80% 86% 80% Secondary use assurance 79% 83% 83% Corporate information assurance 66% 66% 66% Overall percentage 74% 80% 80% Overall assessment Not satisfactory Not satisfactory Not satisfactory NUH | 2013/14 Quality Account 31 PERFORMANCE AGAINST NATIONAL QUALITY STANDARDS AND TARGETS IN 2013/14 The table below sets out our performance against a range of quality measures, and provides a comparison with peer hospitals. QUALITY MEASURE (%UNLESS SHOWN) Patients waiting less than 62 days from urgent referral to treatment for all cancers NUH PEERS 2010/11 2011/12 2012/13 2013/14 AVERAGE 13/14 TARGET 14/15 86.8 84.9 82.4 84.9 84.9 84.9 Patients waiting < 31 days from diagnosis to first treatment for all cancers 97 96.5 96.3 96.4 97.5 96 Patients waiting < 31 days for subsequent treatments for all cancers – surgery 95 94.9 94.5 96.5 96.5 94 Patients waiting < 31 days for subsequent treatments for all cancers – drug treatment (%) 99 99.7 99.4 99.8 99.8 98 Patients waiting < 2 months from referral to treatment for all cancers – referrals from national screening programmes 91 91.5 94.2 99 95.8 94 Patients waiting < 2 weeks from urgent GP referral to date first seen for all urgent suspected cancer referrals 94 94.8 93.6 94.7 95.4 93 Patients waiting < 18 weeks from referral to admitted treatment 93 91 90.5 94.2 89.3 90 Patients waiting < 18 weeks from referral to non-admitted treatment 98 98.7 98.5 97.5 95.4 95 Patients waiting longer than 4 hours from arrival to admission, transfer, discharge 97 93.9 93.9 93.3 94.3 95 7.92 10.15 13.31 3.2 5.3 0 86 83.4 85.1 84.6 86.4 Breaches of the 28 day readmission guarantee as % of cancelled operations Midnight bed occupancy 32 NUH | 2013/14 Quality Account ASSURANCE OF SERVICE QUALITY IN 2013/14 04 NUH has implemented many of the recommendations of the Emergency Care Intensive Support Team (ECIST) who visited in 2012/13. Other significant improvements include: •12 additional respiratory beds on the Specialist Receiving Unit and the conversion of an elective orthopaedic ward to respiratory medicine at City Hospital •The development of a new and improved emergency respiratory pathway so that more than 70% of patients with a respiratory diagnosis are brought straight to the Respiratory Assessment Unit at City Hospital rather than transferred from the Emergency Department at QMC •The embedding of ‘5-a-day’, our five daily actions that have seen 50% healthcare for older people patients being discharged before noon and 50% via the Discharge Lounge. This has aided flow at the start of each day to be improved, particularly for our most elderly and frail patients •Significant progress in closing the Acute Medicine Receiving Unit (AMRU) overnight. This is a unit which receives patients referred by GP’s for tests and Consultant Physician review on whether admission to hospital in-patients beds is required. In 12/13 this unit frequently stayed open overnight as bed capacity in the hospital was limited EMERGENCY ACCESS STANDARD We did not achieve the 2013/14 national standard for emergency care of 95% of patients waiting less than four hours in our Emergency Department (we achieved 93.3%). In quarters three and four the severity of illness in admitted patients increased, and there was significant increase in the number of patients aged over 80 years. This group of patients usually stay in hospital longer than average and often require health and social care services on discharge. The inflow of such patients was quicker than the outflow – this meant that we could not move patients as quickly through our hospitals (including through our Emergency Department. We had a further ECIST visit in March 2014 to inform our focus for 2014/15. Our priority is to improve our internal processes and thereby build greater resilience. Work will continue into 2014/15 and beyond to embed improved working practices with provider organisations, GPs and commissioners to ensure that patients are in hospital only for as long as required. We will continue to work as a fully engaged member of the Urgent Care Board to understand the demands on (and the capacity of) our local health and social care system. We are determined to achieve this important safety standard in 2014/15. NUH | 2013/14 Quality Account 33 05 QUALITY MANAGEMENT Our aim is to deliver excellent, caring, safe and thoughtful healthcare for patients in Nottinghamshire and the East Midlands. Our ambition is to be the best acute teaching trust in England by 2016 by when each of our services will be in the top three of our 12 peer hospitals. Our patients will have healthcare outcomes which achieve or exceed those described in the NHS Outcomes Framework and NICE quality standards. We want to achieve this in a way which is recognisable, measurable and meaningful to everybody in our community. We are committed to delivering a compassionate, caring, communicative and collaborative experience for our patients and their carers. Two committees meet regularly to ensure we deliver this strategy. The Quality Assurance Committee (of the Trust Board) monitors the quality of services we provide and the quality of our risk management and assurance processes. 34 NUH | 2013/14 Quality Account The Directors’ Group (Quality) meets monthly. Members are the executive directors, corporate advisors to the Board, and our senior clinical leadership team (nurses and doctors). The group is responsible for leading and delivering the required quality standards or for driving continuous and sustainable improvement in the quality of services we provide. Members are responsible for adopting and sharing local best practice to enable Trust-wide sharing and learning. In order to ensure that improving our efficiency and reducing our overall costs is not to the detriment of the quality of our services. All cost improvement programmes are risk assessed using a quality impact assessment (QIA). Each QIA is reviewed and signed off by the Director of Nursing and Medical Director and shared with Commissioners who are able to check and challenge the impact of any proposed changes before they take place. The Trust’s Quality Assurance Committee also reviews these on an annual basis. QUALITY MANAGEMENT 05 Trust Quality Management Structure TRUST BOARD BOARD COMMITTEES Chief Executive Officer Chief Executive’s Team Quality Assurance Committee eight other Committees Directors’ Group Four meetings a month, one with a focus on Quality Investment Governance Committee Operational Performance Group Patient and Public Involvement Steering Committee Theatres Strategy Group Procurement Steering Group Equality and Diversity Steering Group Learning and Education Committee Sustainable Development group Clinical Risk Committee Clinical Effectiveness Committee Trust Health and Safety committee Organisational Risk Committee Pressure Ulcers Operational Group Infection Control Operational Group Falls Operational Group Venous Thromboembolic (VTE) Operational Group NUH | 2013/14 Quality Account 35 PERFORMANCE AGAINST NHS OUTCOMES FRAMEWORK We report our performance against the five domains/areas of the NHS National Outcomes Framework. We can compare our performance year-on-year and with other hospitals. We benchmark ourselves against a group of 12 similar acute teaching hospitals. The five domains are: Domains 1 and 2: Preventing people from dying prematurely Hospital Summary Hospital level Mortality Indicator (SHMI) compares its death rate with the rate in the ‘average’ hospital (100). SHMI’s much higher than 100 suggest poor care and those much lower than 100 good care. See table below. Our latest SHMI is 91. This is within normal range for all hospitals and for our peer trusts (see table below). 1Preventing people from dying prematurely 2Enhancing quality of life for people with long-term conditions 3Helping people to recover from episodes of ill health or following injury 4Ensuring that people have a positive experience of care 5Treating and caring for people in a safe environment and protecting them from harm INDICATOR SHMI NUH NATIONAL AVERAGE October 2012 – October 2012 – September 2013 September 2013 The value and banding of the summary hospital level mortality indicator 91 (as expected) (SHMI) for the Trust reporting period 100 LOWEST AND HIGHEST REPORTED TRUST October 2012 – September 2013 63-118.59 The table below shows how we compare with our peer trusts (data taken from Dr Foster). Peer group SHMI for all admissions: October 2012-September 2013 (with 95% confidence intervals) 140 Relative risk 120 100 80 60 40 20 Provider 36 NUH | 2013/14 Quality Account Li ve En rp gl oo an l d av En er ag gl an e d hi gh En es gl t an d lo w es t Br ist ol Ro ya l Sh ef fie ld O xf or So d ut ha m pt on N ew ca st le Ca m Bi br rm id ge in gh am (U H B) L an Ce ca nt sh ra ire lM ac nh es te r Le ed s Le ice st er N ot tin gh am 0 QUALITY MANAGEMENT The Trust Board and Clinical Effectiveness Committee regularly monitor the SHMI, which provides an important independent confirmation for our patients and community that the care provided by our many thousands of staff is safe and of a high standard. NUH considers this data is an authentic description of our mortality rate. NUH has a programme of safety improvements to reduce complication and mortality rates which includes improved recognition of deteriorating patient, falls reduction, and improved sepsis care (as described above). The SHMI makes no direct adjustment for the proportion of patients who are admitted for end of life (palliative) care. If this proportion is inappropriately high, the SHMI will be inappropriately low (because more patient deaths will be counted as expected). For October 2012-September 2013, 16.8% of NUH deaths included palliative care code(s) – see table below for comparison with other hospitals. INDICATOR – PALLIATIVE CARE CODING (DOMAIN 1 AND 2) NUH PEERS NATIONAL AVERAGE LOWEST TO HIGHEST The percentage of patient deaths with palliative care coded at either diagnosis or speciality level 16.8 22.5 21.2 0 - 44.9 Domain 3: Helping people to recover from episodes of ill health or following injury Indicator 1. Patient Reported Outcome Measures (PROMS) PROMs describe the health gains after four operations using pre and post-operative surveys. NUH participation rates for hip and knee replacements are good. We undertake relatively few groin hernia repairs and therefore not included in 2013/14 case mix adjusted data and no varicose vein operations. INDICATOR PROMS NUH 2013/14 PEER MEAN 2013/14 NATIONAL AVERAGE 2013/14 LOWEST AND HIGHEST REPORTED TRUSTS 2013/14 Hip replacement surgery 0.447 0.412 0.439 0.301 – 0.527 Knee replacement surgery 0.344 0.321 0.33 0.193 – 0.416 NUH compared to peer trusts (below) PROMS 0.6 Average health gain NUH believes that this data is an accurate reflection of outcomes based on the detailed work undertaken within the speciality based on previous year’s results. NUH PROMs for both hip and knee replacement surgery have improved each year over the last three years (as illustrated below). The reported patient benefits are slightly higher than large peer trusts. Compared to the national average the outcomes are in line with expected. Considering the complex nature of the work undertaken at NUH these results are encouraging. The data is kept under review by the Orthopaedic Board and presented annually at the Trust’s Clinical Effectiveness Committee. 05 0.5 0.4 0.3 0.2 0.1 0 -0.1 FY FY FY FY FY FY FY FY FY 2011/12 2012/13 2013/14 2011/12 2012/13 2013/14 2011/12 2012/13 2013/14 PROMS groin hernia Min Max PROMS hip replacement National mean Peer mean PROMS knee replacement NUH NUH | 2013/14 Quality Account 37 Indicator 2. Readmission within 28 days Our readmission rate for patients 15 years and over is higher than the national average (below). INDICATOR EMERGENCY READMISSIONS TO HOSPITAL 2012/13 NUH PEER MEAN NHS ENGLAND AVERAGE LOWEST REPORTED TRUST HIGHEST REPORTED TRUST The percentage of patients aged 0 to 14 readmitted to a hospital which forms part of the Trust within 28 days of being discharged during the reporting period 8.1 9.03 10.01 3.75 14.94 The percentage of patients aged 15 or over readmitted to a hospital which forms part of the Trust within 28 days of being discharged during the reporting period 12.54 11.79 11.45 3.35 41.65 The proportion of readmissions is not fully understood. Whilst readmissions have been subject to audit previously, we will now undertake clinical reviews during a patient’s readmitted hospital stay to understand in a patient-centred way the underlying reasons for the readmission. These clinical reviews will be undertaken by staff from across the local health and social care system. A better understanding of the contributory factors to a patient returning unnecessarily to hospital will enable us to work with our community-based partners to design effective interventions and pathway changes to reduce the number of avoidable emergency readmissions. This will enable improvement work across NUH and the wider health and social care system to: In 2013/14, the new patient administration system enabled the development of live and accurate readmissions data. Patients can be identified during their current hospital stay (previously patients could only be identified reliably retrospectively). Where data and clinical experience show opportunities for readmission reduction, we will develop and implement short and medium term programmes of work. •Live view of current readmissions available to clinicians •Data can be very rapidly analysed for trends and patterns 38 NUH | 2013/14 Quality Account 1Reduce differences in how readmissions are defined and measured by different stakeholders 2Help understand why readmissions occur (clinical and nonclinical reasons) 3Help describe the changes needed to improve patient care and subsequently reduce avoidable readmissions 4Provide best practice in monitoring, reporting and reducing readmissions. QUALITY MANAGEMENT 05 Domain 4: Ensuring people have a positive experience of care Indicator 1: The Trust’s responsiveness to the personal needs of its patients during the reporting period. NUH 2013/14 compared to the lowest average and highest scores DOMAIN LOWEST HIGHEST AVERAGE NUH NUH IN TOP 20% Access and waiting 73 96 84.6 88.1 Yes Safe, high quality co-ordinated care 53 81 66.1 67.9 No Better information, more choice 57 82 68.8 68.6 No Building closer relationships 75 93 84.7 85.3 No Clean, comfortable, friendly place to be 72 91 80.1 80.3 No Overall 67 87 76.9 78.0 No The scores for each question are out of 100. They are the age-gender standardised average score given by patients. A higher score indicates a better performance, for example a score of 80 reflects an overall result of ‘very good’ and a score of 60 reflect an overall result of ‘good.’ The domain score is the average of the trust scores within that domain. The overall score is the average of the domain scores. The Trust believes that this is a true reflection of NUH data. The Trust has taken a range of improvement actions which we have identified in the patient feedback section above. Indicator 2: the percentage of staff employed by, or under contract to, the trust during the reporting period who would recommend the trust as a provider of care to their family or friends. % staff who would recommend the Trust to a friend or relative 100 % 80 60 40 20 Sh ef fie ld O xf or So d ut ha m pt on N ew ca st le Ca m Bi br rm id ge in gh am (U H B) La Ce n ca nt sh ra ire lM ac nh Ro es te ya r lL iv er po ol En Br ist gl an ol d av En er ag gl an e d hi gh En es gl t an d lo w es t Le ed s Le ice st er N ot tin gh am 0 Trust 72% of our staff would be happy with the standard of our care if a friend or relative needed treatment. We are in the top 20% of trusts for this indicator NUH | 2013/14 Quality Account 39 Indicator 3 Le ed s Le ice st er Sh ef fie ld O xf or So d ut ha m pt on N ew ca st le Ca m Bi br rm id ge in gh am (U H B) L an Ce ca nt sh ra ire lM ac nh Ro es te ya r lL iv er po ol En Br ist gl an ol d av En er ag gl an e d hi gh En es gl t an d lo w es t 100 90 80 70 60 50 40 30 20 10 0 N ot tin gh am Score Inpatient (Net Promoter Score) Trust Le ed s Le ice st er Sh ef fie ld O xf or So d ut ha m pt on N ew ca st le Ca m Bi br rm id ge in gh am (U H B) L an Ce ca nt sh ra ire lM ac nh Ro es te ya r lL iv er po ol En Br ist gl an ol d av En er ag gl an e d hi gh En es gl t an d lo w es t 100 90 80 70 60 50 40 30 20 10 0 N ot tin gh am Score Emergency Department (Net Promoter Score) Trust The Trust considers both inpatient and Emergency Net Promoter Scores are an authentic representation of our performance during 2013/14. These scores, including analysis and actions to improve, are regularly discussed at our Patient and Public Involvement Steering Group. We have seen an increase in both response rate and score across the year. 40 NUH | 2013/14 Quality Account QUALITY MANAGEMENT 05 Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm Indicator 1: The percentage of patients admitted to hospital and who were risk assessed for VTE during the reporting period. NUH averaged 94.78% for VTE assessment. The Trust considers that this data is an authentic representation of our performance during 13/14. The table below shows our performance against peers and the national average for England. VTE Assessment as % of Total Admissions 100% % Assessed 95% 90% 85% 80% 75% Sh ef fie ld O xf or So d ut ha m pt on N ew ca st le Ca m Bi br rm id ge in gh am (U H B) L an Ce ca nt sh ra ire lM ac nh Ro es te ya r lL iv er po ol En Br ist gl an ol d av En er ag gl an e d hi gh En es gl t an d lo w es t Le ed s Le ice st er N ot tin gh am 70% Trust The Trust has (1) ensured the data is available at speciality and consultant level and (2) included this as one of a number of metrics used to review the quality of care provided by our specialties. Indicator 2: Rate per 100,000 bed days of cases of C diff infection reported within the trust amongst patients aged two or over during the reporting period. Rate of Clostridium difficile infections per 100,000 bed days 2013/14 43 23 20 Le ed s Le ice st er Sh ef fie ld O xf or So d ut ha m pt on N ew ca st le Ca m Bi br rm id ge in gh am (U H B) L an Ce ca nt sh ra ire lM ac nh Ro es te ya r lL iv er po ol En Br ist gl an ol d av En er ag gl an e d hi gh En es gl t an d lo w es t 0 N ot tin gh am 50 45 40 35 30 25 20 15 10 5 0 Trust NUH | 2013/14 Quality Account 41 We have seen a substantial reduction in C diff over the past five years, we have demonstrated that we now have a healthcare environment which is near-free from C diff contamination, and that cross-infection with C diff has been virtually eliminated. We have wiped out completely the most common hospital outbreaks strains (ribotypes 027, 001 and 106), and the pattern of C diff infection we now see is virtually identical to that seen in community onset cases. Our antibiotic stewardship is of a high standard and continuing to improve, and we design our antibiotic guidelines around antibiotics that minimise C diff risks. In 2013, NHS England started the staged publication of clinical outcome data for 10 specialties at trust and consultant level. The specialties are: Cardiac surgery •Vascular •Bariatric •Interventional cardiology •Orthopaedics We aim to reduce C diff infection to an absolute minimum and we have a highly-active C diff programme at NUH , including 2 separate weekly meetings looking in detail at each case in terms of epidemiology, risk factors, clustering, antibiotic use, treatment, and overall management. This is backed up by a comprehensive C Diff action plan. •Endocrine and thyroid •Urology •Head and neck •Bowel cancer We have agreed an approach with commissioner colleagues to measure our performance by focusing on the drivers for improvement – namely an enhanced root cause analysis process, a rigorous approach to hand hygiene compliance and a limit to the number of cases caused by cross infection. •Upper gastrointestinal (mouth and stomach) We have included outcomes framework indicator data for the most recent reporting periods for comparison in Appendix 3. This programme is central to our ambition to deliver care which is free of avoidable harm. PUBLICATION OF OUTCOME DATA NUH supports the publication of outcomes of operations by our surgeons. This information enables patients to make decisions and helps us provide better services. 42 NUH | 2013/14 Quality Account This information is published on our website. TRUST-WIDE PATIENT SAFETY PROGRAMME SAFER SURGERY Following a series of serious incidents in theatres in 2010 and 2011 (including 11 never events), we looked hard at our processes to see how we could improve safety in our theatres. We developed a three-year strategy with three inter-related streams: (1) building a safety culture, (2) understanding and learning, (3) and education and training. We have not had a theatres-related never event since 2012. QUALITY MANAGEMENT 05 BUILDING A SAFETY CULTURE We needed to create an open, responsive culture. We encouraged ideas and engagement from ‘front-line’ staff. We created a trust-wide Safe Surgery Group to oversee our programme of safety work. All incidents with actual or potential significant harm are reviewed and safety concerns are raised and challenged. We have worked hard to understand what our staff think about safety at NUH. Formal safety climate studies were completed by over 800 staff in 2012/13 and 2013/14. 80% of our staff believe safety issues are assigned a high priority, and that they can influence patient safety. UNDERSTANDING AND LEARNING FROM INCIDENTS We have focused on three areas: improving the process; individual feedback; and sharing the learning. A cross-directorate, multi-professional incident subgroup designed a ‘learning from incidents’ staff feedback tool. There is a cascade of learning using a variety of methodologies. We have striven to ensure processes and practices are consistent in every theatre. Our safety dashboards provide individual theatre teams with visible, peer-reviewed data on how they’re doing against local metrics of excellent care. EDUCATION AND TRAINING MEDICINES SAFETY Our medicines optimisation work examines and improves the way we manage medicines. Focused on patients and their experiences, the aim is to improve patient outcomes and prevent avoidable harm. This includes all aspects of choosing, prescribing, supplying, administering and using medicines. The Medicines Management Committee (MMC) is a multi-disciplinary group which works collaboratively using a patient-centred approach to promote and deliver safety, effectiveness and value-for-money in medicines use. We held our third annual Safe Surgery conference: ‘Five Steps One Shared Goal.’ This year we welcomed 400 delegates from NUH and our regional partner hospitals. The MMC regularly reviews relevant policies on how the Trust procures, handles, stores, prescribes, dispenses, administers and monitors medication to ensure that this is done as safely as possible. There is an emphasis on achieving safe prescribing and improving information flows and patients’ understanding of their medicines, particularly as they transfer between hospital and community. Our safety leads developed a training package around the Five Steps to Safer Surgery that is provided face-to-face and online. Over 700 staff were trained in 2013. Interaction with staff in these sessions is crucial to our continual improvement. The Drugs and Therapeutics Committee (DTC) ensures that drugs available for prescription at NUH are appropriately safe, efficacious and cost-effective. The DTC works closely with the Area Prescribing Committee when making decisions about drugs which are also prescribed from primary care. Each theatre team has a ‘safety champion.’ They attend a programme around theatre safety, successfully reinforce key messages (e.g. safety message of the month), and bring team concerns to wider attention. Alongside the MMC the Medicines Safety Group (MSG) works to raise awareness around medicine safety, identifies medicines hazards, and implements actions to reduce the likelihood and severity of medicine-related harm. Trust-wide medication incident data are reviewed quarterly to look for trends and develop actions. We have prioritised work on omitted doses by raising awareness of the effect of omitted or delayed doses and implementing a suite of actions to ensure our patients receive their medication on time. We have invested in staff education: theory and practice of human factors, importance of excellent communication, learning from ourselves and how good teams work. NUH | 2013/14 Quality Account 43 The MSG works closely with the Directorates, which regularly review their medicine-related incidents and analyse them for patterns and trends according to a structured algorithm. Twenty reports were received during 2013. The number of incidents reported and investigated, and the detail of the reports demonstrate an improving safety culture with respect to medication safety within the Trust. They have also informed the work plan for 2014/15 when NUH will focus on: •Improving medicines safety culture, especially among doctors, when we will focus on improving the visibility of medicines safety to increase awareness and support ongoing learning •Improve the safety of our patients who require insulin •Procure an electronic prescribing and administration system HEALTH FOUNDATION SAFER CLINICAL SYSTEMS PROJECT The Health Foundation chose NUH as one of eight sites nationally to pilot a novel approach to improve patient safety. At the end of a two year project on the Trust’s busiest admission ward the project’s successes include a significantly improved safety culture on the ward and better communication between members of the multidisciplinary teams to ensure safe medicines management for our patients. The work has also supported a successful bid for additional pharmacy staff in admission areas to improve safety. Primary care colleagues have supported the initiative by further encouraging patients to bring their medication to hospital to ensure that the information we hold about their usual treatment is accurate and there are no delays in receiving it. WORKING WITH OTHER ORGANISATIONS ON MEDICINES SAFETY NUH has shaped proposed national medicines safety initiatives including: a tool for assessing the risk of introduction of new medicines into an organisation and draft NHS England patient safety alerts on ‘Patient safety alert on non-luer spinal (intrathecal) devices for chemotherapy’ and ‘improving medication error incident reporting and learning’ the National Medicines Safety Thermometer. DEPARTMENT OF HEALTH NEVER EVENTS – MEDICATION RELATED Ten of the Department of Health’s ‘Never Events’ concern medication. NUH has developed an assurance framework which is updated every quarter to allow regular review of the risks around medication Never Events. This framework has been adopted by other Trusts in our region to allow benchmarking of medication Never Events, and shared 44 NUH | 2013/14 Quality Account learning. In 2013/14, NUH has declared one medication Never Event. A patient was administered a drug called methotrexate on two consecutive days rather than weekly. The patient was not harmed. There has been a full investigation and an action plan is being implemented. KNOWING HOW WE ARE DOING To ensure that medicines management practices are safe and that changes are indeed improvements, medicationrelated audits are included in the Trust audit plan. Towards the end of 2012 a Trust-wide audit of omitted doses was completed and a number of actions have been implemented during 2013. CONTINUED LEARNING AND USEFUL INFORMATION The Medicines Education Group (MEG) is developing online learning and assessment modules, has produced a series of medicines safety podcasts, which have been delivered at foundation doctor (F1/F2) teaching sessions, has introduced a new induction programme for trainee doctors and a face-toface “Safe Prescribing” talk (mandatory for all doctors), and produces a regular newsletter. HIGH RISK EMERGENCY SURGERY The Recognise and Rescue programme at NUH aims to improve our response to the deteriorating patient. Patients who require emergency surgery are some of the most vulnerable patients in our hospital. Over the past year, a huge amount of work has been done by a variety of clinical teams and individuals from anaesthesia, critical care, radiology and surgery to improve our emergency surgery service. ‘High risk’ emergency surgery patients account for 20% of the surgical workload but up to 80% of the mortality and morbidity. Ensuring these patients get care in a timely and effective manner is crucial to their experience and outcome. Building on the success of the Emergency Theatre Case Review Group, a focussed audit of emergency laparotomies has delivered great insight into how we can improve. Over the next two years, we have committed to improve our management of emergency surgical patients with the adoption of a High Risk Emergency Surgery CQUIN from April 2014. The Emergency Laparotomy Group at NUH have developed a program of care that includes early identification of high risk patients on admission, fast-track CT scans, and triggered senior clinical input with rapid admission to theatre if required. Intra-operative surgical and anaesthetic guidelines aim to standardise care and ensure patients receive the best evidence-based care. We hope this high quality care program will not only improve patient experience and outcome but also reduce hospital and critical care length of stay and complication rates. QUALITY MANAGEMENT SUPPORTING THE SPEAK OUT SAFELY CAMPAIGN TRAINEE DOCTORS (STAFF IMPROVING PATIENT SAFETY – SIPS) In 2013, we signed up to the Nursing Times’ ‘speak out safely’ campaign, demonstrating our commitment to a culture of openness which includes staff feeling comfortable to raise concerns about patient safety and quality of care. SIPS are a new group, formed in 2013, made up of wardbased staff (medical and nursing colleagues) to co-ordinate patient safety improvement projects across NUH. We already have an active programme to encourage our staff to raise concerns. From the Trust Board to each ward and department, we are committed to ensuring the fundamentals of patient care are consistently delivered to patients. At our regular patient safety walkabouts Trust Board member talk with front line staff who can share concerns directly with senior colleagues. Our whistleblowing policy protects colleagues who feel the need for anonymity. At NUH, our staff can ‘speak out safely.’ Through this campaign we have sought to reassure our patients, staff and volunteers that we are building a culture of openness in which staff can raise concerns about care quality and standards. They can be confident their concerns will be listened to, taken seriously and acted upon. Following its inspection of our hospitals at the end of 2013, the CQC Report described we have an open culture, that staff feel able to report issues and raise concerns, and that we learn from patient safety incidents. 05 SIPS is a front-line initiative by all staff and trainees to help implement our patient safety programme and co-ordinate projects, communicate with the Trust patient safety leads, deliver human factors education, and provide a voice for trainee clinical staff. PATIENT SAFETY CONVERSATIONS In 2009, we launched Patient Safety Conversations to enable front-line staff to talk directly to members of the Trust Board about their safety concerns. These conversations take place in the staff workplace and support board members in their understanding of patient safety issues across the Trust, and allow triangulation against the level of assurance offered by other systems and reports. NUH | 2013/14 Quality Account 45 RESULTS/ACHIEVEMENTS Incidents reported by degree of harm for acute teaching organisations (1 April 2013-30 September 2013) 43 patient safety conversations were planned for 2013/14. 41 were completed with 19 at QMC and 22 at City Hospital. 80% 70% The six most common patient safety issues described by staff were: •Patient discharge delays including ‘take-out’ medicines and ambulance transfers •Staffing establishment/vacancies and skill-mix % of incidents occurring •Estate issues 61.2 60% 50% 40% 30% •Patient falls 20% •Equipment availability 10% •Medication-related incidents SERIOUS INCIDENTS Incident reporting is a key element of our patient safety programme. Our staff appreciate that when we learn from errors or mishaps we can prevent future harm to our patients. Recognising and reporting an incident (or near miss) is the first step to that learning. Our rate of incident reporting is 10.17 per 100 admissions (NHS England September 2013). NUH is in the best 25% of acute teaching hospitals for rate of incident reporting. Incidents are classified by degree of harm. Those resulting in severe harm or death undergo serious incident or high level investigation. Some incidents that have resulted in low or no harm may still undergo robust investigation due to the potential for harm. During the first six months of 2013/14, NUH reported to NHS England via the National Reporting and Learning System (NRLS) 6,197 no harm incidents, 3,118 low harm, 792 moderate harm, 15 severe harm and 11 deaths in patients affected by an incident. This distribution of harms is similar to that reported in peer hospitals, although NHS England identifies that organisations apply degree of harm inconsistently, making comparison difficult (see chart above). NUH has a robust process in place to review degree of harm assigned at the time of reporting. This may result in re-grading the incident to a higher or lower level following clinical review. 46 NUH | 2013/14 Quality Account 0% None Low Moderate Severe Death Degree of harm NUH All acute teaching organisations There are categories of serious incidents: 1) Never Events Never Events are a sub-set of serious incidents and are defined as ‘serious largely preventable patient safety incidents.’ 2) Specific class The department of health has also classified certain incidents in specific categories as serious incidents: •Patient fall resulting in fracture or significant head injury •Pressure ulcers (stages three and four) •Specific infection prevention and control incidents •Maternity related matters for example admission of the baby or mother to intensive care 3) Unclassified Such incidents might include medication error or serious infection causing severe patient harm. QUALITY MANAGEMENT 05 In 2013/14, we reported 10 unclassified Serious Incidents including two Never Events, as described below: April 2013 to March 2014 NEVER EVENT SERIOUS INCIDENTS (SI) UNCLASSIFIED 2013/14 Transiently retained foreign object following procedure Wrong site insertion of chest drain SI TOTAL 1 1 1 1 Incorrect approach used to insert device prior to surgery 1 1 Wrong level spinal injections 1 1 1 2 Failure to follow-up test results 1 1 Maternity service ICT error 1 1 Patient misidentification 1 1 Tissue process error 1 1 8 10 Medication 1 Total 2 Serious incidents in specific categories – 2013 to 2014 CLASSIFICATION 2012/13 2013/14 Patient falls resulting in a fracture or a significant head injury 49 51 Maternity-related matters 32 39 Infection Prevention and Control 41 28 Pressure Ulcers (stages three & four) 107 104 81 70 - avoidable 26 34 - unavoidable All our serious incidents are subject to robust investigation, and the resulting action plan is scrutinised and tracked to completion by the Clinical Risk Committee. We have developed bespoke root cause analysis tools for each of the specific four classes of incident. These ask precise questions relevant to the type of event. All our investigation reports are shared with our commissioners who also apply their level of external scrutiny. They visit a selection of our clinical areas where serious incidents have occurred to see first-hand the improvements made and to gain assurance around our systems and processes. NUH | 2013/14 Quality Account 47 COMMUNICATING PATIENT SAFETY INCIDENTS WITH PATIENTS, THEIR FAMILIES AND CARERS The harmful impact of an incident on a patient can be multifactorial , including emotional and physical consequences. We take our responsibility to be honest and transparent with our patients (duty of candour) very seriously. We are committed to acknowledging, apologising and explaining when things go wrong. When a patient has suffered severe harm or death, the patient (and/or family/carer) will be given an explanation of the sequence of events and an apology. They will be invited to contribute to the investigation and receive a copy of the investigation report together with an explanation of how the incident happened and the action being taken as a result. We share Trust-wide our learning from incidents with all staff via a safety newsletter to prevent a recurrence. 48 NUH | 2013/14 Quality Account EXAMPLES OF LEARNING FROM OUR INCIDENTS •Improved recognition when a patient’s condition is deteriorating and clearer defined processes to escalate concerns to senior staff •Wider implementation of the World Health Organisation’s (WHO) surgical safety checklist resulting in bespoke checklists for areas outside of theatres (e.g: cardiac catheter labs and radiology) supporting clinicians preparation for invasive procedures •Improvements in continuity of senior medical staff cover on our acute medical admissions wards •Greater emphasis on ‘safety culture’ including strengthening of team working and supporting and encouraging staff to speak up A copy of our full 2013/14 Annual Patient Safety Report is available on our website. 06 WORKFORCE & QUALITY 06 WORKFORCE & QUALITY STAFF ENGAGEMENT In the 2013 staff survey, NUH was in the best 20% of trusts in the country for overall staff engagement. This is an important indicator of a safe and effective organisation. The chart below shows how we did in 2013 compared to 2012. WHAT YOU THINK OF WORKING AT NUH 272 staff responded in the 2013 national staff survey mORe sTAFF RecOmmeNded NUH As A plAce TO WORK IN 2013 veRsUs pRevIOUs YeAR We’ve ONce AGAIN beeN vOTed bY YOU As ONe OF THe besT plAces TO WORK IN THe UK! OUR sTAFF eNGAGemeNT scORe WAs AmONG THe besT IN THe cOUNTRY WeshowcasedtheworkofNUH inthenationalaward-winning InsideYourHospitalsseries withtheNottinghamPost ebest inth We’re 3 85% 81% HQUA 73% 77% s WARd UTe TO NTRIb TO cO ORK W G Able FeelIN emeNTs AT v ImpRO 3.95 K R AT WO ATION mOTIv 3.82 3.98 3.71 ter) risbet he o5(hig le1scaf sona TheCQCjudged NUH to be a‘good’organisation WeheldtwoJustDoitaward eventsandanewJustDoItfund tocelebratestaffideas * Weheldthefirstpeople’sNurse andMidwifeoftheYearAwards WeintroducednewTwitter accountstokeepstaff-up-to-date: @nuhstaffand@betterforyou * CTION TISFA JOBSA GOOd HundredsofNUHstaffpledged toimprovepatientcareand experienceaspartofNHS ChangeDay ORK FW LITYO IT SFIEDW GSATI FEELIN TIeNT cARe ANd pA *Figure Over2mTVviewerswatchedour teamsinactionin24HoursLive inA&EatQMConSkyNews IN 201 2 IN 201 13,200staffattendedvalues andbehaviourstrainingsince itslaunchin2009 2m tsfor: tetrus facu 20%o 13,200 We need to do better when it comes to... • • • • • Equality&diversitytraining Health&safetytraining Reportingerrors,nearmisses or incidents we witness Tacklingdiscriminationatwork Staffexperiencingphysicalviolence NUH | 2013/14 Quality Account 49 From May 2014, we will introduce a quarterly ‘friends and family’ test for staff, covering two questions: •How likely are you to recommend this organisation to friends and family if they needed care or treatment? On a quarterly basis our Director of Nursing and Midwifery updates the Board on our nurse staffing levels. These reports are published on our website along with staffing levels by shift and actual versus planned hours of care on each ward by month at www.nuh.nhs.uk. •How likely are you to recommend this organisation to friends and family as a place to work?” LEADER AND MANAGER DEVELOPMENT We will report on these results in next year’s Quality Account. NUH supports its staff to undertake leadership development. This year 236 staff attendrd either an Introduction to Leadership, Building Essential Leadership, RCN Clinical Leadership programme or Franklin Covey Performance Improvement course. We have provided over 20 ‘bespoke’ events. NURSING SKILL-MIX Our nursing skill mix remains (March 2014) 70% registered to 30% unregistered nurses. In summer 2013, we began displaying nurse staffing levels on every inpatient ward (including establishment against expected staffing levels and recruitment underway). This information is updated by ward managers daily. From early 2014 we have published daily staffing levels for all wards (per shift) on our public website. 50 NUH | 2013/14 Quality Account 07 RESEARCH & INNOVATION AT NUH 07 RESEARCH & INNOVATION AT NUH Hospitals which engage in research generally provide higher standards of treatment and better outcomes for patients. During 2013/14, NUH received £13million of research income from various National Institute of Health Research (NIHR) and Research Council funding streams and collaborations with the Life Sciences Industry. This is a 13% decrease in income compared to the previous year (£15million 2012/13) and is mainly attributable to changes in the calculation of the annual allocations to Trusts by the Treasury and to a reduction in our patient recruitment to clinical trials rates (and associated funding). The number of patients receiving NHS services provided or subcontracted by NUH in 2013/14 that were recruited during that period to participate in research approved by a research ethics committee was as follows: 6,223 patients were recruited to 406 NIHR adopted studies in 2013/14 (66% of our target). We are implementing strategic and structural changes to expand our portfolio of studies, improve recruitment (and hence increased income). The Nottingham Health Sciences Biobank (NHSB) collected more than 18,000 biosamples (a >20% increase in 2013/14). NUH has become one of the most efficient Trusts in setting up complex clinical trials. The Trust’s average set-up time is 57 days (against a national benchmark of 70 days). This will lead to more patients being offered the opportunity to access innovative healthcare in NUH. 15 new NIHR research grants were awarded to NUH (total value £7million). An innovative Research Business Unit has been developed to provide research management services across NUH. Our nursing and midwifery research infrastructure leads on pioneering research into improving compassionate care. This programme of work will accelerate the implementation of research findings into service improvements and staff support. NUH is proud to host the East Midlands Academic Health Science Network (AHSN) which provides a unique platform for the alignment of education, clinical research, informatics, innovation, training and education and healthcare delivery. The AHSN goal is to improve patient and population health outcomes by translating research into practice, and developing and implementing integrated health care services. The AHSN will support knowledge exchange networks to actively share best practice, and provide for rapid evaluation and early adoption of new innovations. NUH | 2013/14 Quality Account 51 08 APPENDICES: APPENDIX 1 – STATEMENTS OF ASSURANCE STATEMENT FROM NHS NOTTINGHAM WEST CLINICAL COMMISSIONING GROUP (CCG) Clinical Commissioning Groups have in place a collaborative commissioning arrangement for which Nottingham West CCG is the co-ordinating commissioner for NUH on behalf of a number of clinical commissioning groups. We have shared the Quality Account with a number of the CCGs and this narrative is a collective response. The commissioners have in place a number of measures for monitoring the quality of services we commission. This includes a schedule of regular visits to all areas of the hospital. These visits in conjunction with our regular contract reviews provide commissioners with real time data from which we can form a judgement about the quality of services NUH offer. We are pleased to see the CQC inspection found NUH to be a safe, effective, responsive, caring and a well lead organisation in November 2013. NUH have a number of quality initiatives in place to safeguard the quality of services delivered to patients and their families. These include a suite of quality improvement measures (CQUIN) which have been co-produced with commissioners and bring real added value. In addition the Trust has a well embedded service improvement programme; the ‘Better for You’ programme and good staff engagement. 52 NUH | 2013/14 Quality Account Commissioners have seen progress in a number of areas such as; the reduction of never events through the trust wide safety programme, continued improvement in patient experience seen through the ‘Friends and Family’ Test and the Patient Association Peer Review of complaints programme among others. NUH do have challenges and therefore risks to quality. These include financial risks and recruitment of staff. NUH have a robust assessment of nurse staffing and are compliant with the Francis recommendations and staffing guidance, however recruitment of both medical and nursing staff remains a significant challenge. In addition the four hour target has remained a significant challenge for the Trust. It is acknowledged that this is a system-wide and multi-factorial issue and NUH are engaged with the healthcare economy to find solutions in order to improve and meet the target. Commissioners note the increased number of emergency readmissions and are working with the trust to reduce these. Dr Guy Mansford, Accountable Officer NHS Nottingham West Clinical Commissioning Group APPENDICES 08 STATEMENT FROM THE JOINT NOTTINGHAM AND NOTTINGHAMSHIRE HEALTH SCRUTINY COMMITTEE The Joint Health Scrutiny Committee welcomes the opportunity to comment on the Nottingham University Hospitals NHS Trust Quality Account 2013/14. Our comment focuses on the areas in which we have engaged with the Trust during 2013/14. The Committee has found Nottingham University Hospitals willing to engage, listen and respond positively to recommendations from scrutiny during the year. The Committee is pleased to see the sustained improvement in performance relating to cancelled operations and supports the Trust’s decision not to continue with this as a specific priority and instead focus attention on other areas of wait that are important to patients. The Committee has heard about work to minimise waits for medication in the discharge process and feels that there could be scope for better communicating the discharge process and timescales to patients so that they have a greater understanding of what to expect. The Committee has highlighted concerns about the pharmacy service for outpatients and is pleased that the Trust has taken this issue on board to explore further. During the year the Committee reviewed the Trust’s approach to complaints management and was satisfied that the organisation has a robust complaints handling process in place and takes complaints seriously at both an individual complainant and Trust level. Over the past few years the Committee has monitored the ongoing work of Nottingham University Hospitals to improve care for those with dementia and has welcomed the improvements that have been made. Committee members are pleased to hear that the use of ‘About Me’ documentation is being expanded to support other patients with vulnerabilities and that learning from specialist dementia care practitioners is being shared with other areas of the organisation. During the year the Committee met with clinicians and ‘walked the frail, elderly pathway’ at the Queens Medical Centre. This visit did not highlight any significant issues of concern and Committee members felt that patients seen during the visit were being treated with dignity. The Committee welcomed the largely positive report arising from the recent Care Quality Commission inspection of the Trust and is reassured about the Trust’s governance arrangements that it was already aware of the issues before the inspection took place. The Committee has been assured that recommendations from the inspection are being implemented, and supports the Trust’s approach of incorporating this, and work arising from other reviews such as Francis and Berwick, into ongoing improvement works. The Committee has heard some concerns about environmental issues on the Queen’s Medical Centre and City Hospital sites, which are acknowledged by the Trust in its Quality Account and it has listened to specific issues that councillors have raised. The Committee understands the challenges faced in improving the environment, particularly at the Queen’s Medical Centre site, and welcomes that this remains a focus for the Trust going forward. The Committee will be interested in reviewing progress in environmental improvements during the forthcoming year. STATEMENT FROM HEALTHWATCH NOTTINGHAMSHIRE Healthwatch Nottinghamshire is pleased to have the opportunity to read and respond to the Quality Account at an early stage, although we have not been able to comment fully, due to the lack of complete data. We note the openness of the document, which contains comprehensive data in excess of the requirements. A huge amount of work is reflected in the document, demonstrating a range of approaches to improvement. Some improvements are very clear and are welcomed – for example the reduction in C diff cases. We particularly like sections of the document where case studies were used, such as in the section on complaints. We also welcome the work with Patient Association, introducing new methods and sharing stories with the Board and on the website. We are pleased to see the work which has gone on to improve dealing with and learning from complaints and will continue to monitor this. NUH | 2013/14 Quality Account 53 However, an overall picture of how programmes, priorities, CQUIN goals, external assessments, national outcomes framework domains, and various other indicators fit together is needed. For example – how do these programmes of action relate to improved outcomes, how are they integrated at ward level and who is responsible, e.g. at director level for ensuring goals are met? Perhaps a clear illustration such as how a patient’s pathway for a specific condition is impacted on by all the relevant quality initiatives would be useful. This would help to provide assurance that actions are leading to improved outcomes and patient experience. Topics specifically raised with Healthwatch in 2013/14 include: complaints system, discharge, ophthalmology, hearing services. We have been very pleased with the response we have received from NUH. For example following comments received on Ophthalmology Outpatients, we had an open exchange of information and as a result Healthwatch are going to be taking part in the SIPPI (patient) group for Head and Neck Directorate. We will continue to work with NUH as one of the key provider Trusts used by the population we represent and look forward to an increasingly productive partnership in the future. STATEMENT FROM HEALTHWATCH NOTTINGHAM The organisation’s quality ‘six pack’ is a simple and effective way of packaging a range of measures being taken in relation to key priority areas and making them clear for the benefit of both patients and staff. We are pleased to see the continuation of this approach into 2014/15. In relation to these priority areas, of particular note is the Trust’s work around: Attitude and behaviour – its programme of ‘rounding’ staff, embedding core values and behaviours. It is noted that the staff survey undertaken this year, whilst reflecting the views of a relatively small proportion of staff, reflects a broadly positive view of the organisation from amongst its staff and places it as one of the best NHS organisations to work for. Better communication – NUH has undertaken some notable work in this area, particularly in relation to dementia, and is continuing this work into 2014/15 as it rightly remains a priority for the organisation. In its first year of operation, Healthwatch Nottingham has benefited from NUH’s positive approach to developing its relationship with the Healthwatch Nottingham Board and staff. Fewer cancelled operations – the Trust has made significant improvements in this area and is now shifting its focus to delays in emergency care and delayed transfers of care due to internal waits, both of which remain a challenge and impact on the patient experience of care. It is hoped that the dialogue between the organisations will remain one of openness, with the Trust being proactive in its engagement with ourselves and neighbouring Healthwatch, establishing regular meetings to discuss issues of concern and to update on plans, as well as dealing swiftly and fully with requests for information. NUH continues to build the patient experience into its work. The ‘15 steps challenge’ is a positive element of this. Other elements of this work are evidenced throughout the Quality Account and demonstrate a commitment to valuing the patient and using their views and experiences to improve the quality of its provision. NUH has benefited, this year, from an assessment of ‘good’ from the CQC. This very much reflects the majority of opinion gathered about the Trust through Healthwatch Nottingham. This is not to say that there have not been concerns raised by individuals, but these have always been taken seriously and plans to address specific matters have been provided as appropriate. It should be noted that the Trust was commended on its approach to risk management in its CQC inspection. We are pleased, on the basis of our experience to date, to be able to support the finding that the Trust has good systems in place for identifying and addressing areas requiring improvement. 54 NUH | 2013/14 Quality Account APPENDICES 08 APPENDIX 2 – STATEMENTS OF DIRECTORS’ RESPONSIBILITIES IN RESPECT OF THE QUALITY ACCOUNT The directors are required under the Health Act 2009, National Health Service (Quality Accounts) Regulations 2010 and National Health Service (Quality Account) Amendment Regulation 2011 to prepare Quality Accounts for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporate the above legal requirements). In preparing the Quality Account, directors are required to take steps to satisfy themselves that: •the Quality Accounts presents a balanced picture of the Trust’s performance over the period covered; •the performance information reported in the Quality Account is reliable and accurate; •there are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; •the data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, is subject to appropriate scrutiny and review; and the Quality Account has been prepared in accordance with Department of Health guidance The directors confirm to the best of their knowledge and belief that they have complied with the above requirements in preparing the Quality Account. By order of the Board Chair 6 June 2014 Chief Executive 6 June 2014 NUH | 2013/14 Quality Account 55 APPENDIX 3 – NHS OUTCOMES FRAMEWORK PERFORMANCE AGAINST NHS OUTCOMES FRAMEWORK We report our performance against the five domains/areas of the NHS National Outcomes Framework. We can compare our performance year-on-year and with other hospitals. The five domains are: 1Preventing people from dying prematurely 2Enhancing quality of life for people with long-term conditions 3Helping people to recover from episodes of ill health or following injury 4Ensuring that people have a positive experience of care 5Treating and caring for people in a safe environment and protecting them from Harm We have provided information on a number of indicators and shown how outcomes at Nottingham University Hospital compare to the national average and the best and worst outcomes in the most recent reporting periods for each indicator in the tables below. Domain 1 and 2: Preventing people from dying prematurely NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) INDICATOR TIME PERIOD NUH NATIONAL AVERAGE The value and banding of SHMI July 2012-June 2013 91.4 100 115.6 62.6 October 2012-September 2013 90.8 100 118.6 63 INDICATOR TIME PERIOD NUH NATIONAL AVERAGE NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) % of patient deaths with Palliative Care coded at either diagnosis or speciality level July 2012-June 2013 15.53 20.6 44.1 0 October 2012-September 2013 16.8 21.2 44.9 0 56 NUH | 2013/14 Quality Account APPENDICES 08 Domain 3: Helping people to recover from episodes of ill health or following injury NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) INDICATOR TIME PERIOD NUH NATIONAL AVERAGE PROMs – hip replacement April 2012-March 2013 0.413 0.438 0.539 0.319 April 2013-March 2014 0.447 0.439 0.527 0.301 PROMs – knee surgery treatment (primary) April 2012-March 2013 0.307 0.318 0.416 0.209 April 2013-December 2013 0.343 0.330 0.416 0.193 NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) INDICATOR TIME PERIOD NUH NATIONAL AVERAGE % of patients aged 0-15 readmitted to hospital within 28 days of discharge 2010/11 8.19 4.21 0 16.05 2011/12 8.1 4.19 0 14.94 12.36 6.03 0 22.76 12.54 6.16 % of patients aged 16+ 2010/11 readmitted to hospital within 28 days of 2011/12 discharge 41.65 Domain 4: Ensuring people have a positive experience of care INDICATOR TIME PERIOD NUH NATIONAL AVERAGE NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) Responsiveness to personal needs of patients 2011/12 66.4 67.4 85 56.5 2012/13 67.4 68.1 84.4 57.4 NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) 95 25 INDICATOR TIME PERIOD NUH NATIONAL AVERAGE Patient Friends and Family Test score June 2013 77.8 63 NUH | 2013/14 Quality Account 57 Domain 5: Treating and caring for people in a safe environment and protecting them from avoidable harm INDICATOR TIME PERIOD NUH NATIONAL AVERAGE NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) % of patients who were risk assessed for VTE Q3 2013/14 94.6 95.8 100 74.1 February 2014 95.6 96 100 77 NATIONAL HIGHEST (WORST) NATIONAL LOWEST (BEST) INDICATOR TIME PERIOD NUH NATIONAL AVERAGE Rate per 100,000 bed days of cases of Clostridium difficile infection reported 2011/12 23.5 22 0 58.2 2012/13 22.7 17.3 0 30.8 Incidents reported by degree of harm INCIDENT DEGREE OF HARM NONE LOW MODERATE SEVERE DEATH Oct 2012 to 31 March 2013 6144 2283 716 29 22 1 April to 31 September 2013 6197 3118 792 15 11 58 NUH | 2013/14 Quality Account APPENDICES 08 APPENDIX 3 – AUDITORS’ REPORT INDEPENDENT AUDITORS’ LIMITED ASSURANCE REPORT TO THE DIRECTORS OF NOTTINGHAM UNIVERSITY HOSPITALS NHS TRUST ON THE ANNUAL QUALITY ACCOUNT In preparing the Quality Account, the Directors are required to take steps to satisfy themselves that: We are required by the Audit Commission to perform an independent assurance engagement in respect of Nottingham University Hospitals NHS Trust’s Quality Account for the year ended 31 March 2014 (“the Quality Account”) and certain performance indicators contained therein as part of our work under section five (1) (e) of the Audit Commission Act 1998 (“the Act.”) NHS trusts are required by section eight of the Health Act 2009 to publish a quality account which must include prescribed information set out in The National Health Service (Quality Account) Regulations 2010, the National Health Service (Quality Account) Amendment Regulations 2011 and the National Health Service (Quality Account) Amendment Regulations 2012 (“the Regulations”). •The performance information reported in the Quality Account is reliable and accurate; Scope and subject matter The indicators for the year ended 31 March 2014 subject to limited assurance consist of the following indicators: •Percentage of patients risk-assessed for venous thromboembolism (VTE); and •The Quality Account presents a balanced picture of the Trust’s performance over the period covered; •There are proper internal controls over the collection and reporting of the measures of performance included in the Quality Account, and these controls are subject to review to confirm that they are working effectively in practice; •The data underpinning the measures of performance reported in the Quality Account is robust and reliable, conforms to specified data quality standards and prescribed definitions, and is subject to appropriate scrutiny and review; and •The Quality Account has been prepared in accordance with Department of Health guidance The Directors are required to confirm compliance with these requirements in a statement of directors’ responsibilities within the Quality Account. Our responsibility is to form a conclusion, based on limited assurance procedures, on whether anything has come to our attention that causes us to believe that: •‘Friends and family’ test – patient element We refer to these two indicators collectively as “the indicators.” Respective responsibilities of Directors and auditors The directors are required under the Health Act 2009 to prepare a Quality Account for each financial year. The Department of Health has issued guidance on the form and content of annual Quality Accounts (which incorporates the legal requirements in the Health Act 2009 and the Regulations). •The Quality Account is not prepared in all material respects in line with the criteria set out in the regulations; •The Quality Account is not consistent in all material respects with the sources specified in the NHS Quality Accounts Auditor Guidance 2013/14 issued by the Audit Commission on 17 February 2014 (“the Guidance”); and •The indicators in the Quality Account identified as having been the subject of limited assurance in the Quality Account are not reasonably stated in all material respects in accordance with the Regulations and the six dimensions of data quality set out in the guidance NUH | 2013/14 Quality Account 59 We read the Quality Account and conclude whether it is consistent with the requirements of the Regulations and to consider the implications for our report if we become aware of any material omissions. We read the other information contained in the Quality Account and consider whether it is materially inconsistent with: •Board minutes for the period April 2013 to June 2014; •Papers relating to the Quality Account reported to the Board over the period April 2013 to June 2014; •Feedback from the Commissioners; •Feedback from Local Healthwatch; •The Trust’s complaints report published under regulation 18 of the Local Authority, Social Services and NHS Complaints (England) Regulations 2009; •Feedback from other named stakeholder(s) involved in the sign off of the Quality Account; •The latest national patient survey for 2013; •The latest national staff survey for 2013; •The Head of Internal Audit’s annual opinion over the Trust’s control environment for 2013/14; •The annual governance statement dated 06/06/204; and •Care Quality Commission quality and risk profiles/intelligent monitoring dated February 2014 and March 2014 We consider the implications for our report if we become aware of any apparent misstatements or material inconsistencies with these documents (collectively the “documents”). Our responsibilities do not extend to any other information. This report, including the conclusion, is made solely to the Board of Directors of Nottingham University Hospitals NHS Trust in accordance with Part II of the Audit Commission Act 1998 and for no other purpose, as set out in paragraph 45 of the Statement of Responsibilities of Auditors and Audited Bodies published by the Audit Commission in March 2010. We permit the disclosure of this report to enable the Board of Directors to demonstrate that they have discharged their governance responsibilities by commissioning an independent assurance report in connection with the indicators. To the fullest extent permissible by law, we do not accept or assume responsibility to anyone other than the Board of Directors as a body and Sandwell and West Birmingham Hospitals NHS Trust for our work or this report save where terms are expressly agreed and with out prior consent in writing. 60 NUH | 2013/14 Quality Account Assurance work performed We conducted this limited assurance engagement under the terms of our appointment under the Audit Commission Act 1998 and in accordance with the Commission’s Guidance. Our limited assurance procedures included: •Evaluating the design and implementation of the key processes and controls for managing and reporting the indicators; •Making enquiries of management; •Testing key management controls; •Limited testing, on a selective basis, of the data used to calculate the indicator back to supporting documentation; •Comparing the content of the Quality Account to the requirements of the Regulations; and •Reading the documents A limited assurance engagement is narrower in scope than a responsible assurance engagement. The nature, timing and extent of procedures for gathering sufficient appropriate evidence are deliberately limited relative to a reasonable assurance engagement. Limitations Non-financial performance information is subject to more inherent limitations than financial information, given the characteristics of the subject matter and the methods used for determining such information. The absence of a significant body of established practice on which to draw allows for the selection of different but acceptable measurement techniques which can result in materially different measures and can impact comparability. The prescription of different measurement techniques may also vary. Furthermore, the nature and methods used to determine such information, as well as the measurement criteria and the precisions thereof, may change over time. It is important to read the Quality Account in the context of the criteria set out in the Regulations. The nature, form and content required of Quality Accounts are determined by the Department of Health. This may result in the omission of information relevant to other users, for example for the purpose of comparing the results of different NHS organisations. APPENDICES 08 In addition, the scope of our assurance work has not included governance over quality or non-mandated indicators which have been determined locally by Nottingham University Hospitals NHS Trust. Conclusion Based on the results of our procedures, nothing has come to our attention that causes us to believe that, for the year ended 31 March 2014: •The Quality Account is not prepared in all material respects in line with the criteria set out in the regulations; •The Quality Account is not consistent in all material respects with the sources specified in the Guidance; and •The indicators in the Quality Account subject to limited assurance have not been reasonably stated in all material respects in accordance with the Regulations and the six dimensions of data quality set out in the guidance KPMG LLP, Statutory Auditor Chartered Accountants St Nicholas House 31 Park Row Nottingham NG1 6FQ 26 June 2014 NUH | 2013/14 Quality Account 61 APPENDIX 5 – PEER HOSPITALS PEER HOSPITALS Cambridge University Hospitals NHS Foundation Trust Central Manchester University Hospitals NHS Foundation Trust Lancashire Teaching Hospitals NHS Foundation Trust Leeds Teaching Hospitals NHS Trust Oxford Radcliffe Hospitals NHS Trust Royal Liverpool and Broadgreen University Hospitals NHS Trust Sheffield Teaching Hospitals NHS Foundation Trust Southampton University Hospitals NHS Trust The Newcastle Upon Tyne Hospitals NHS Foundation Trust University Hospitals Birmingham NHS Foundation Trust University Hospitals Bristol NHS Foundation Trust University Hospitals of Leicester NHS Trust 62 NUH | 2013/14 Quality Account APPENDICES 08 APPENDIX 6 – GLOSSARY OF TERMS ‘15 steps challenge’ – a series of toolkits to help staff, patients, service users and others to improve patient care. The improvements should be clear within 15 steps of entering the area. Care Quality Commission (CQC) – the independent regulator of health and social care in England. The CQC regulates care provided by the NHS, local authorities, private companies and voluntary organisations. 4Cs – refers to complaints, concerns, comments and compliments received by NUH. Carers Policy – NUH’s formal approach to supporting unpaid carers. Acute – describes a disease of rapid onset, severe symptoms and brief duration. The majority of hospital services provided by QMC and Nottingham City Hospital are for acute illnesses. Caring around the Clock – the Trust’s version of hourly rounding day to ensure patients are checked regularly, day and night. Area Prescribing Committee – advises CCGs on drug use, including effectiveness, prescribing, and value. Case managers – single point of contact, co-ordinating a case load of patients through treatment (EG in the Regional Trauma Centre). Audit Commission – an independent watchdog, driving economy, efficiency and effectiveness in public services, including the NHS. Berwick Report – commissioned in August 2013 to recommend NHS improvements after the Francis Report on high mortality rates in Mid Staffordshire. Better for You – NUH’s continuous improvement programme acting on ideas from staff and patients. Biomedical Research Units (BRUs) – partnerships between NHS Trusts and universities translating basic science research into practical applications. Board (of the Trust) – the Trust Board is accountable for setting the strategic direction of the Trust, monitoring performance against objectives, ensuring high standards of corporate governance and helping to promote links between the Trust and the community. CABG – Coronary Artery Bypass Graft surgery. An operation in which a section of vein or artery is used to bypass a blockage in a coronary artery, to prevent heart attacks and to relieve chest pain. Care pathways – the sequence of health and social care services a patient in the UK receives after entering the system during a particular episode of care. Centre for Maternal and Child Enquiries (CMACE) – independent charity dedicated to improving the health of mothers, babies and children through audits and research. Champions – colleagues who support, lead, and promote particular causes within the Trust, for instance Falls Champions. Chronic Obstructive Pulmonary Disease (COPD) – a number of lung conditions; including chronic bronchitis and emphysema. Clinical audit – measuring the quality of care and services against agreed standards to indicate areas for improvement. Clinical coding – clinical coding officers are responsible for assigning a code for every inpatient stay and day case visit (or ‘episode’). The coding process enables patient information to be easily sorted for statistical analysis. Clinical Commissioning Group (CCGs) – replaced PrimaryCare Trusts with effect from April 1 2013. These groups will comprise of GPs and other clinicians who will have a greater influence on how the NHS budget is spent. There will also be a new national NHS Commissioning Board to oversee the process. Clinical dashboard – a clinical dashboard is a toolset of visual displays developed to provide clinicians with the relevant and timely information they need to inform daily decisions that improve quality of patient care. NUH | 2013/14 Quality Account 63 Clinical Effectiveness Committee – provides assurance that all NUH clinical services and treatment programmes meet best-practice standards for assessing and maintaining their clinical effectiveness. Clinical variation – the difference between how each patient responds to the same care. College of Emergency Medicine – responsible for setting standards of training and administering examinations in emergency medicine. Clostridium difficile (C difficile or C diff) – a healthcare associated intestinal infection that mostly affects elderly patients with other underlying diseases. Commissioners of services – these are organisations that buy services on behalf of people living in a defined geographical area. They may purchase services for the population as a whole, or for individuals who need specific care, treatment and support. Healthcare services are commissioned by the local authorities. Elective – elective care is planned. A patient will be aware of the required treatment and has been given a date to be admitted to hospital. Non-elective care is provided in critical or emergency situations when a medical professional deems specific treatments or hospital admission cannot be delayed for more than 24 hours. Emergency Department (formerly A&E) – specialising in acute care of patients who present without prior appointment, either by their own means or by ambulance. Essence of Care – aims to support localised quality improvement on wards, by providing a set of established and refreshed benchmarks supporting front line care across care settings at a local level. It aims to improve the quality of fundamental aspects of nursing care. Early Warning Score – a quick assessment of a patient’s condition based on blood pressure, heart rate, respiratory rate, body temperature and level of consciousness. EDIS – Emergency Department Information System – ICT system which tracks emergency patients’ status. Complaint – this is an expression of dissatisfaction that can relate to any aspect of a person’s care, treatment or support. It can be expressed orally, through gestures or in writing. Emergency Theatre Case Review Group – surgeons’ group to review and improve emergency care. CQUIN – Commissioning for Quality and Innovation – a process where local NHS commissioners pay trusts for meeting targets to reward excellence in care. Equality and Diversity Steering Group – monitors bullying and harassment cases and their associated outcomes to advise on improvement. Cross-infection – cross-infection is the transfer of harmful microorganisms between people, pieces of equipment, or within the body, which can cause many complications. Four hour standard – relates to the emergency access standard set by the Department of Health. The target states that at least 95% of patients attending Emergency Departments must be seen, treated, admitted or discharged within four hours. Day surgery – surgery which can be performed in a single day, without the need to admit the patient for an overnight stay in hospital. Department of Health – the Department of Health is the department of the UK government responsible for policies on health, social care and the NHS (in England only). Discharge – the point at which a patient leaves hospital to return home; or is transferred to another service; or the provision of a service is formally concluded. Dr Foster Good Hospital Guide – Dr Foster is an independent organisation dedicated to making information about the performance of hospitals and medical staff as accessible as possible. East Midlands Academic Health Science Network – a network of NHS, higher education and industry to identify, adopt and spread innovative health care across the region. 64 NUH | 2013/14 Quality Account Francis Inquiry – public inquiry in 2010 into high mortality rates at Stafford Hospital. Health Foundation – a charitable health think tank. Healthcare associated infection – an avoidable infection that occurs as a result of the healthcare that a person receives. Healthwatch – independent patient campaigning and lobbying group. Hospital Episode Statistics (HES) – is the national data for England of the care provided by NHS hospitals and for the NHS hospital patients treated elsewhere. HES is the data source for a wide range of healthcare analysis for the NHS, government and many other individuals and organisations. APPENDICES Hospital Standardised Mortality Ratio (HSMR) – is an indicator of healthcare quality that measures if the death rate at a hospital is higher or lower than you would expect. The HSMR compares the expected rate of death in a hospital with the actual rate of death. Factors such as age and severity of illness are taken into account. Medicines optimisation – the safe and effective use of medicines to enable the best possible outcomes. Hourly rounding – nurses proactively visiting patients on an hourly basis, on top of their usual duties. This is the basis of NUH’s ‘Caring around the Clock’ programme. MRSA – methicillin-resistant Staphylococcus aureus – bacteria that can cause infection in a range of tissues such as wounds, ulcers, abscesses or bloodstream. Infection Prevention and Control Team – senior multi disciplinary, cross site infection control specialists. NCEPOD – National Confidential Enquiry into Patient Outcome and Death – a charity which uses surveys to review medical and surgical clinical practice and makes recommendations. Information Governance – how organisations handle information, particularly personal data. In the NHS, personal information is dealt with legally, securely, efficiently and effectively in order to deliver the best possible care. Myocardial Ischaemia National Audit Project (MINAP) – examines the quality of management of heart attacks (myocardial infarction) in hospitals in England and Wales. NCI/NCISH – National Confidential Inquiry into Suicide and Homicide by People with Mental Illnesses – Manchester University’s leading research programme into the subject. Intensive Care National Audit & Research Centre (ICNARC) – a centre to foster improvements in the organisation and practice of critical care (intensive and high dependency care) in the UK. National Emergency Laparotomy Audit – audit to improve care for emergency laparotomy patients, following evidence of high mortality rates. Intrapartum care – management and delivery of care to women in labour. National patient surveys – legally required Trust surveys of patients, to help set future priorities. Joint Health Scrutiny Committee (known as Overview and Scrutiny Committees (OSCs)) – local authority health service scrutiny committees. National Institute for Clinical Excellence (NICE) – an independent organisation responsible for providing national guidance on promoting good health and treating ill health. Keogh Review – a review ordered by the prime minister to review the quality of care and treatment at hospitals with persistent high mortality indicators, following the Francis Inquiry. National Institute for Health Research (NIHR) – is the body responsible for creating a health research system in which the NHS supports outstanding individuals, working in world class facilities, conducting leading edge research focused on the needs of patients and the public. Liverpool Care Pathway – an integrated care pathway that is used at the bedside to drive up sustained quality of the dying in the last hours and days of life. Local Involvement Networks (LINks) – individuals and community groups, such as faith groups and residents’ associations, working together to improve health and social care services. In Nottingham there are two LINks groups – one for Nottingham city and another for Nottinghamshire. MBRRACE-UK – Maternal Infant and Newborn Programme – online reporting system for stillbirths, perinatal deaths, and infant deaths. 08 National Patient Safety Agency (NPSA) – an arms-length body of the Department of Health that leads and contribute to improved, safe patient care by informing, supporting and influencing organisations and people working in the health sector. National Reporting and Learning System (NRLS) – a central database of patient safety incident reports to identify hazards, risks and opportunities. Never Events – a sub-set of Serious Incidents and are defined as ‘serious largely preventable patient safety incidents’. MDT (multi-disciplinary team) – a team of representatives from several different professional backgrounds who all have different areas of expertise. NUH | 2013/14 Quality Account 65 NHS Blood and Transplant (NHSBT) – provides a reliable, efficient supply of blood, organs and associated services to the NHS. NHS Choices – NHS-run health information website. NHS East Midlands – is the strategic health authority for the region providing leadership of the NHS across Derbyshire, Leicestershire and Rutland, Lincolnshire, Northamptonshire and Nottinghamshire. The role of NHS East Midlands is to relay and explain national policy, set direction and support and develop all NHS Trust bodies (Primary Care Trusts and NHS Trusts providing acute, mental health and ambulance services). NHS Foundation Trust – NHS foundation trusts are a type of NHS trust in England and have been created to devolve decision-making from central Government control to local organisations and communities so they are more responsive to the needs and wishes of their local people. Ombudsman – government body which investigates complaints of unfairness or poor service about the NHS. Overview and Scrutiny Committees (OSCs) – see Joint Health Scrutiny Committee. Paediatric – medical care of children. Patient – this is a person who receives health or social care through a regulated activity. Patients are defined as ‘service users’ in the Health and Social Care Act 2008. Patient Environmental Action Team (PEAT) – an annual assessment of inpatient healthcare sites in England that have more than 10 beds. It is a benchmarking tool to ensure improvements are made in the non-clinical aspects of patient care including environment, food, privacy and dignity. The assessment results help to highlight areas for improvement and share best practice across healthcare organisations in England. NHS Litigation Authority (NHSLA) – the NHSLA is a special health authority responsible for handling negligence claims made against NHS bodies. It also aims to raise safety standards and reduce the number of negligent or preventable incidents through its risk management programme. This incorporates organisational, clinical and health and safety risks. Most healthcare providers, including NUH, are assessed against their standards. Patient and Public Involvement Steering Group – a directors’ committee overseeing the patient and public involvement. NHS Outcomes Framework – sets out the outcomes and corresponding indicators used to hold NHS England to account for improvements in health outcomes. Patient Partnership Group – works with the Patient and Public Involvement Steering Group to communicate and engage with patients and public. NHS Number – is the only National Unique Patient Identifier, used to help healthcare staff and service providers match you to your health records. Patients’ Association Peer Review process – a new approach to complaints handling which includes establishing panels to assess the quality of complaints investigations through regular sampling and peer review, run by the Patients Association. NICE – National Institute for Health and Care Excellence – official body giving independent, authoritative and evidence-based guidance on the most effective ways to prevent, diagnose and treat disease and ill health, reducing inequalities and variation. All NHS treatments must be approved by NICE. Nottingham West Clinical Commissioning Group – 12 local GP practices in Eastwood, Kimberley, Stapleford, Beeston, Bramcote and Chilwell who plan and pay for local health services. Nurse handover – information passed from nurses at the end of one shift to nurses starting the next shift. 66 NUH | 2013/14 Quality Account Patient Opinion – a website (www.patientopinion.org. uk) that allows patients and carers to find out what other people think of local hospitals, hospices and mental health services. Perinatal – the period shortly before or after birth. Peri-operative – the care that is given before, during and after surgery. Picker Institute – this is a not-for-profit organisation that works with patients, professionals and policy makers to promote a patient-centred approach to care. The Institute uses surveys, focus groups and other methods to gain a greater understanding of patients’ needs. APPENDICES PROMS – Patient Reported Outcome Measures – PROMs measures health gain in patients undergoing hip replacement, knee replacement, varicose vein and groin hernia surgery in England, based on responses to questionnaires before and after surgery. Primary care – first contact and principal point of continuing care, such as GP or community service. Providers – organisations that provide NHS services, such as hospitals and clinics. They may be NHS, private, or voluntary-run. Rapid Response Team – a team of Estates and Facilities staff focussing on swiftly cleaning and tidying areas of NUH. Research Council – funding and training body for researchers. Root Cause Analysis – a method of problem solving that tries to identify the root causes of faults or problems and remove them. Quality ‘6 pack’ – six priorities underlying the Trust’s quality strategy. Quality Assurance Committee – a sub-committee of the Trust Board, which oversees the delivery of the Trust’s quality and patient safety strategies and monitors improvement. Quality, Innovation, Productivity and Prevention (QIPP) programme – Government strategy for saving £20billion in the NHS budget by 2015 while improving care. Quality Impact Assessment (QIA) – a structured analysis of the impact a particular project or action may have on the Trust’s Quality Strategy. Patient-Led Assessments of the Care Environment (PLACE) – a programme of volunteer community teams assessing patients’ privacy and dignity, food, and cleanliness, focussing entirely on the care environment rather than clinical issues. Patient Led Action Teams (PEAT) inspections – the predecessor of PLACE. Person-centred care – care in which patients are supported to make informed decisions about their own health and care. 08 Pulmonary hypertension – is a condition in which high blood pressure in the arteries of the lungs (the pulmonary arteries) is abnormally high. Regional Trauma Centre – NUH hosts the East Midlands regional trauma centre, with leading experts in trauma and orthopaedic surgery, neurosurgery and intensive care. It is the hub of a network which has been set up across the region. Research – clinical research and clinical trials are an everyday part of the NHS, and often conducted by medical professionals who also see patients. A clinical trial is a particular type of research that tests one treatment against another. It may involve either patients, or people in good health, or both. Transforming Dementia Care programme – a major year-long RCN programme in which nine NHS trusts developed innovative ways to improve dementia care in hospitals. Safeguarding – safeguarding means putting measures in place to enable people to live free from harm, abuse and neglect. The measures protect their health, wellbeing and human rights. Children, and adults in vulnerable situations, need to be safeguarded. Safer Surgery Checklist – a tool for the relevant clinical teams to improve the safety of surgery by reducing deaths and complications. In June 2008, World Health Organisation (see WHO) launched a second Global Patient Safety Challenge, ‘Safe Surgery Saves Lives’, to reduce the number of surgical deaths across the world. The checklist is part of this initiative. Safety culture – staff’s constant and active awareness of the potential for things to go wrong. Both the staff and the organisation are able to acknowledge mistakes, learn from them, and take action to put things right. Safety dashboard – a single page summary of key safety statistics, such as infections, pressure ulcers and falls. Safety Leads – member of staff with particular responsibility for safe practice. Safety Thermometer – the NHS’s IT system for its Safety Dashboard. Secondary User Services (SUS) – single source of comprehensive data to enable a range of reporting and analysis. NUH | 2013/14 Quality Account 67 Sepsis Action Group – consultant led project to raise awareness of sepsis as a medical emergency and cut the number of deaths it causes. ‘We are here for you’ – our values, known as ‘we are here for you’, developed after consultation with patients and staff, describe the NUH way of doing things. Skill-mix – making sure the duty staff collectively bring the right combination of skills for the work that needs to be done. World Health Organisation (WHO) – is the directing and coordinating authority for health within the United Nations system. It is responsible for providing leadership on global health matters, shaping the health research agenda, setting norms and standards, articulating evidence-based policy options, providing technical support to countries and monitoring and assessing health trends. SSKIN – a five step model for pressure ulcer prevention. The acronym stands for Support surface, skin evaluation, keeping moving, incontinence and nutrition bundle. Stroke Improvement National Audit Programme (SINAP) – a national audit to assess and improve stroke care, run by the Stroke Programme at the Royal College of Physicians (RCP). Smoking cessation – is the process of discontinuing the practice of inhaling a smoked substance. Staff survey – the official annual national survey of NHS staff by the Care Quality Commission. Strategic Health Authority – see NHS East Midlands. Summary Hospital level Mortality Indicator (SHMI) – the ratio between the actual number of patients who die following hospitalisation at the trust and the number that would be expected to die on the basis of average England figures, given the characteristics of the patients treated there. Think Glucose campaign – is a major programme from the NHS Institute, designed to improve the management of people with diabetes when they are admitted to hospital. Transfer of Care – the process of discharging a patient from NUH care to home, a community health service, or social services Urgent Care Board – committee of NHS organisations focussing on improving emergency care provision. Venous thromboembolism (VTE) – a condition in which a blood clot (thrombus) forms in the vein. Vascular Society of Great Britain and Ireland (VSGBI) – a registered charity founded to relieve sickness and to preserve, promote & protect the health of the public by advancing excellence & innovation in vascular health, through education, audit & research. Wave one acute hospital inspections – CQC’s inspection of 18 NHS Trusts in 2013, using a more intensive, data-analysis driven methodology. 68 NUH | 2013/14 Quality Account Designed by NUH Communications Team and Mono Design Ltd. Photographs by Nottingham University Hospitals NHS Trust. ©2014 Nottingham University Hospitals NHS Trust. All rights reserved.