Providers’ Perceptions of Mental Healthcare Needs in Primary Care Patients
advertisement
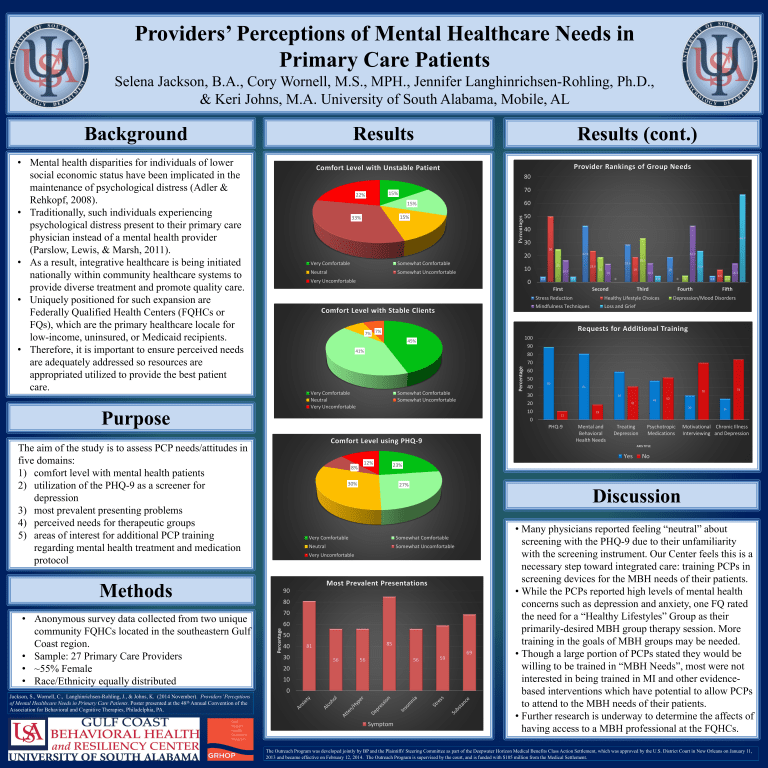
Providers’ Perceptions of Mental Healthcare Needs in Primary Care Patients Selena Jackson, B.A., Cory Wornell, M.S., MPH., Jennifer Langhinrichsen-Rohling, Ph.D., & Keri Johns, M.A. University of South Alabama, Mobile, AL Background Results • Mental health disparities for individuals of lower social economic status have been implicated in the maintenance of psychological distress (Adler & Rehkopf, 2008). • Traditionally, such individuals experiencing psychological distress present to their primary care physician instead of a mental health provider (Parslow, Lewis, & Marsh, 2011). • As a result, integrative healthcare is being initiated nationally within community healthcare systems to provide diverse treatment and promote quality care. • Uniquely positioned for such expansion are Federally Qualified Health Centers (FQHCs or FQs), which are the primary healthcare locale for low-income, uninsured, or Medicaid recipients. • Therefore, it is important to ensure perceived needs are adequately addressed so resources are appropriated utilized to provide the best patient care. Results (cont.) Provider Rankings of Group Needs Comfort Level with Unstable Patient 80 70 15% 22% 60 15% Percentages 15% 33% Very Comfortable Somewhat Comfortable Neutral 66.7 30 50 Somewhat Uncomfortable 0 Comfort Level with Stable Clients 25 23.8 16.7 19 19 14 4.2 4.2 33.3 28.6 14.3 0 First 23.8 19 4.8 Second 0 Third 5 4.8 Fourth Stress Reduction Healthy Lifestyle Choices Mindfulness Techniques Loss and Grief 9.5 14.3 4.8 Fifth Depression/Mood Disorders Requests for Additional Training 7% 7% 45% Very Comfortable Neutral Very Uncomfortable Percentage 41% Somewhat Comfortable Somewhat Uncomfortable K Comfort Level using PHQ-9 8% 42.9 42.9 10 Very Uncomfortable The aim of the study is to assess PCP needs/attitudes in five domains: 1) comfort level with mental health patients 2) utilization of the PHQ-9 as a screener for depression 3) most prevalent presenting problems 4) perceived needs for therapeutic groups 5) areas of interest for additional PCP training regarding mental health treatment and medication protocol 100 90 80 70 60 50 40 30 20 10 0 89 81 12% 74 70 59 48 41 52 30 11 PHQ-9 19 Mental and Behavioral Health Needs Treating Depression Psychotropic Medications 26 Motivational Chronic Illness Interviewing and Depression AXIS TITLE Yes No 23% 30% 27% Discussion Very Comfortable Somewhat Comfortable Neutral Somewhat Uncomfortable Very Uncomfortable Methods Jackson, S., Wornell, C., Langhinrichsen-Rohling, J., & Johns, K.. (2014 November). Providers’ Perceptions of Mental Healthcare Needs in Primary Care Patients. Poster presented at the 48th Annual Convention of the Association for Behavioral and Cognitive Therapies, Philadelphia, PA. 40 20 Purpose Most Prevalent Presentations 90 80 70 60 Percentage • Anonymous survey data collected from two unique community FQHCs located in the southeastern Gulf Coast region. • Sample: 27 Primary Care Providers • ~55% Female • Race/Ethnicity equally distributed 50 50 40 30 85 81 56 56 56 20 10 0 Symptom 59 69 • Many physicians reported feeling “neutral” about screening with the PHQ-9 due to their unfamiliarity with the screening instrument. Our Center feels this is a necessary step toward integrated care: training PCPs in screening devices for the MBH needs of their patients. • While the PCPs reported high levels of mental health concerns such as depression and anxiety, one FQ rated the need for a “Healthy Lifestyles” Group as their primarily-desired MBH group therapy session. More training in the goals of MBH groups may be needed. • Though a large portion of PCPs stated they would be willing to be trained in “MBH Needs”, most were not interested in being trained in MI and other evidencebased interventions which have potential to allow PCPs to attend to the MBH needs of their patients. • Further research is underway to determine the affects of having access to a MBH professional at the FQHCs. The Outreach Program was developed jointly by BP and the Plaintiffs' Steering Committee as part of the Deepwater Horizon Medical Benefits Class Action Settlement, which was approved by the U.S. District Court in New Orleans on January 11, 2013 and became effective on February 12, 2014. The Outreach Program is supervised by the court, and is funded with $105 million from the Medical Settlement.