Successful Chloroquine Treatment of Porphyria Cutanea Tarda in
advertisement

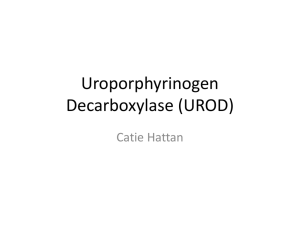
Successful Chloroquine Treatment of Porphyria Cutanea Tarda in HIV Patient on Hemodialysis Joanna Yun, Steven Zivich, Geoff Lim, RoseMary Harris Department of Family Medicine, Drexel University College of Medicine, Philadelphia, PA . Case Report Background References A 52 year old Caucasian male with HIV/AIDS recently restarted on antiretroviral therapy, Hepatitis C with cirrhosis of the liver resistant to Pegasus/ribavirin therapy, and end-stage renal disease on hemodialysis for past 18 months; presents to his primary care doctor with complaints of new hand lesions that developed over the last 2 months. The patient is heterosexual male, 40 pack year tobacco smoking history, alcohol abuse and has a history of heroin dependence. Porphyria cutanea tarda (PCT) is a metabolic disease characterized by a decrease in the enzyme activity of uroporphyrinogen decarboxylase (UROD), the 5th enzyme in the heme biosynthesis pathway.(1,2) Reduction of UROD activity results in accumulation of uroporphyrin and other highly carboxylated porphyrins in the skin and liver, resulting in delayed phototoxic skin reactions and asymptomatic chronic hepatopathy.(3) The accumulated byproducts are photosensitive, which results in much of the clinical presentation.(4) 1. Singal AK, Kormos-Hallberg C, Lee C, et al. Lowdose hydroxychloroquine is as effective as phlebotomy in treatment of patients with porphyria cutanea tarda. Clin Gastroenterol Hepatol. 2012;10(12):1402-9. doi:10.1016/j.cgh.2012.08.038. 2. Munoz-Santos C, Guilabert A, Moreno N, ToFigueras J, Badenas C, Darwich E, Herrero C. Familial and sporadic porphyria cutanea tarda: clinical and biochemical features and risk factors in 152 patients. Medicine. 2010;89: 69-74. 3. Balwani M, Desnick RJ. The porphyrias; advances in diagnosis and treatment. Blood. 2012;120(23): 4496-504. 4. Huang Y-C, Wang C-C, Sue Y-M. Porphyria cutanea tarda in a hemodialysis patient. QJM. 2013;106(6):591-2. doi:10.1093/qjmed/hcs115. 5. Quansah R, Cooper CJ, Said S, Bizet J, Paez D, Hernandez GT. Hepatitis C- and HIV-induced porphyria cutanea tarda. Am J Case Rep. 2014;15:35-40. doi:10.12659/AJCR.889955. 6. Markova A, Lester J, Wang J, Robinson-Bostom L. Diagnosis of common dermopathies in dialysis patients: a review and update. Semin Dial. 2012;25(4): 408-18. 7. Mansourati F, Stone V, Mayer K. Porphyria cutanea tarda and HIV/AIDS: a review of pathogenesis, clinical manifestations and management. Int J STD AIDS. 1999;10:51-56. 8. Poh-Fitzpatrick MB. Porphyria cutanea tarda: treatment options revisited. Clin Gastroenterol Hepatol. 2012;10(12):1410-1. doi:10.1016/j.cgh.2012.09.005. 9. Shieh S, Cohen JL, Lim HW. Management of porphyria cutanea tarda in the setting of chronic renal failure: A case report and review. J Am Acad Dermatol. 2000;42(4):645-652. doi:10.1067/mjd.2000.105504. 10. Tarwater K, Misra S, Misra M. Type I (sporadic) porphyria cutanea tarda in a hemodialysis patient: a case report. Hemodial Int. 2008;12 Suppl 2(Figure 3):S38-42. doi:10.1111/j.1542-4758.2008.00323.x. Lesions were excoriated with multiple blisters and crusting, localized only to the hands. The patient had no other complaints. Lesions were cultured for HSV, which later resulted negative. Patient was discharged on Triamcinolone 0.1% cream, Acyclovir 400mg and Silvadene cream daily. Patient returns 3 months later, hands lesions remained unchanged from antivirals and topical therapy. At this time patient’s CD4 171 and HIV VL 70. Patient was evaluated by dermatology, underwent skin biopsy and was diagnosed with porphyria cutanea tarda (PCT). Patient did not tolerate the initial therapy of prednisone 20mg due to psychiatric side effects. Phlebotomy therapy was initiated, however after 2 months of intermittent compliance of phlebotomy there was no affect on the hand lesions. Due to poor response to previous therapies and lack of alternative options, He was placed on Chloroquine Phosphate despite literature stating poor efficacy in patients on hemodialysis. After 8 weeks of Chloroquine therapy, the patient had almost completely resolution of rash. PCT is often divided into two types. Type I is acquired deficiency in UROD with common inciting factors of type I are: Hepatitis C infection, alcohol abuse, hemochromatosis, HIV, smoking, estrogen use, hemodialysis (HD) and chlorinated polycyclic aromatic hydrocarbons; which our patient had 5 risk factors.(5, 6, 7) Type 2 results from an autosomal dominant genetic mutation of UROD. Treatments include photoprotection and avoidance of triggers, serial phlebotomies and antimalarials chloroquine phosphate and hydroxychloroquine sulfate.(8) Antimalarials such as chloroquine form a watersoluble complex with the porphyrins and are excreted by the kidneys.(9) HD patients do not benefit from this treatment as chloroquine-porphyrin complexes are not efficiently cleared during dialysis.(9) The first reported case of antimalarial therapy effectively treating a patient was PCT in 2008 with serial phlebotomies and low-dose hydrochloroquine.(10) This is the first case of a HD patient effectively being treated with chloroquine therapy without phlebotomy. Before After