Document 11129560
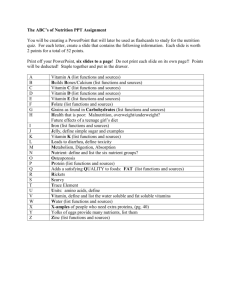
advertisement

Hypovitaminosis D, Bone Health Implications and Related Co-Morbidities Andrew Shajari, MS1; Tan Duong, MS1; Kevin Russo, MS1; Domingo Hallare, MD2; Dahlia Lee, MD2; Lindsay Russell, DPM, FACFAS2; Daniel K Lee, DPM, PhD, FACFAS2 Masters in Medical Science Program, Drexel University Sacramento, CA 2 Kaiser Permanente South Sacramento Medical Center, Sacramento, CA 1 INTRODUCTION Serum Calcidiol (D2) Concentra4ons and Health Status ng/mL Health Status <12 Associated with vitamin D deficiency, leading to rickets in infants and children and osteomalacia in adults 12-­‐20 Generally considered inadequate for bone and overall health in healthy individuals >20 Generally considered adequate for bone and overall health in healthy individuals >60 Emerging evidence links poten8al adverse effects to such high levels, par8cularly (>60 ng/mL) Current studies have shown that estrogen can play a role in maintaining bone density.10,11,14 As a result, post-­‐menopausal women are at a higher risk of developing bone abnormali8es, due to a reduc8on of estrogen synthesis. The results in figure 4 show that 70% of encountered pa8ents were female, and table 2 shows that more than 52% of the pa8ents were above the age of 55. Therefore, our collected data can ajest to other literature findings regarding the importance of estrogen and its poten8al impact on bone health, and further support that post-­‐menopausal women are more prone to abnormali8es of the bone. Current recommenda8ons also considers a serum vitamin D level of 20-­‐30 ng/ mL to be within a normal range and sufficient for bone health.9 Looking at our collected data in table 3, it is clear that the majority (70%) of our pa8ents examined had serum vitamin D levels above 20 ng/mL. As a result, it would seem that the general vitamin D recommenda8ons, specifically for our older pa8ent popula8ons, are insufficient in maintaining bone density and overall bone health. Furthermore, many of the examined pa8ents ooen presented with a variety of co-­‐morbidi8es, which are shown in figure 5. The top 3 commonly encountered co-­‐morbidi8es were Diabetes, Obesity and Cigareje Smoking. Obesity seems to be the most linearly correlated co-­‐morbidity to bone abnormali8es that pa8ents ooen present with. Firstly, obese pa8ents place a greater amount of strain on their bones due to the excess weight. Secondly, the increased fajy 8ssue that obese pa8ents possess reduces the available circula8ng vitamin D levels, and as a result further predisposes obese pa8ents to bone abnormali8es. Thirdly, fajy acid molecules tend to compete with vitamin D molecules for the binding to the Vitamin D Binding Protein (VDBP).15 As a result, obese pa8ents with increased fajy acid concentra8ons have another method of reducing the effec8veness of vitamin D and increase their disposal to bone abnormali8es. Addi8onally, most of the encountered co-­‐morbidi8es produce a pro-­‐inflammatory environment, which supports the recently proposed mechanism behind the role of estrogen in inhibi8ng the pro-­‐inflammatory cytokines and reducing their detrimental effects on bone health.10,11 Table 1: Serum Calcidiol (D2) Concentra4ons and Health Status (Ins4tute of Medicine 201113) Figure 3: Dietary Vitamin D References for Different Age Groups and Genders (Ins4tute of Medicine 20119) MATERIALS AND METHODS Pa8ents seeking treatment and/or undergoing surgery for foot, ankle and other lower extremity bone abnormali8es have their blood drawn at the 8me of their ini8al checkup, along with other subsequent visits. This is done in order to measure pa8ents’ serum Calcidiol, or more commonly referred to as simply vitamin D, levels. Pa8ent data is collected and sorted by sex, age, vitamin D levels, diagnosis, along with any associated co-­‐morbidi8es (obesity, diabetes, smoking, etc…) that many pa8ents frequently present with. CONCLUSION The growing aging popula8on, along with a growing endemic of diabetes and obesity that may further exacerbate and nega8vely impact bone health, is an area of concern and much needed research. Furthermore, the increased dermatological precau8on of the current genera8on has caused a mass avoidance of UV rays through the use of sunscreens, which have shown to reduce vitamin D synthesis by up to 98%. Unfortunately, there is no consensus on dis8nct vitamin D recommenda8ons pertaining to the older pa8ent popula8on and therefore it is impera8ve to gain further insight into producing more individualized recommenda8ons for this specific pa8ent popula8on that is at the greatest risk of developing bone abnormali8es. RESULTS 30% 34% Fracture 66% Pa8ents 0-­‐20 years of age 11 Male 70% Osteoarthritis Figure 4 – Primary Diagnosis of Pa4ent Popula4on Female REFERENCES Figure 5 -­‐ Pa4ent Popula4on Gender Ra4o (N=209) Pa8ents with 0-­‐10 ng/mL Calcidiol 8 Pa8ents with10-­‐20 ng/mL Calcidiol 54 Pa8ents with 20-­‐30 ng/mL Calcidiol 58 Pa8ents 21-­‐30 years of age 8 Pa8ents 31-­‐54 years of age 81 Pa8ents with >30 ng/mL Calcidiol 89 Pa8ents ≥ 55 years of age 109 Pa4ents with >20 ng/mL Calcidiol 147 Table 2 -­‐ Pa4ent Age Ranges (N=209) 60 Number of Patients Vitamin D is a group of fat-­‐soluble secosteroids, commonly called a vitamin while in actuality not an essen8al dietary need. Its role has long been implicated in calcium and phosphorous regula8on, along with mineraliza8on of bone. Vitamin D can be consumed through diet and/or synthesized from cholesterol through exposure of skin melanocytes to UV rays. While vitamin D from our diets can come from a plethora of sources, UV skin exposure produces up to 90% of our total needed vitamin D levels.1-­‐4 Within the skin, Cholesterol is converted to 7-­‐dehydrocholesterol and then subsequently converted to Cholecalciferol, a precursor of vitamin D. Cholecalciferol is then bound to the Vitamin D B inding P rotein ( VDBP) a nd t ransported t o t he l iver. I n t he l iver, c holecalciferol i s hydroxylated to Calcidiol (D2), which is the major storage form of vitamin D in fajy 8ssue and t he m ain s erum m arker u sed c linically. C alcidiol i s t hen t ransported t o t he k idney t o b e further h ydroxylated t o i ts a c8ve f orm, C alcitriol ( D3), w hich a cts a s a t ranscrip8on f actor i n 5-­‐7 inters88al c ells o f t he s mall i ntes8nes. Within intes8nal mucosal cells of the small intes8nes, calcitriol induces the produc8on of a calcium transport protein and a calcium binding protein, TRPV5 and Calbindin respec8vely. The overall goal at this point is to increase the absorp8on of calcium from both the intes8nes and kidneys, while increasing the excre8on of phosphorous from both sources. Within the bone, calcitriol and parathyroid hormone promote bone resorp8on through an 5-­‐7 Figure 1 provides a summary of the above men8oned increased ac8vity of Osteoclasts. steps and processes.8 Hypovitaminosis D is widely encountered throughout the orthopedic pa8ent popula8on. Research and recommenda8ons regarding vitamin D deficiency have been controversial, generalized and understudied. Figure 1 -­‐ Vitamin D Sources, Synthesis, Metabolism and Impact8 Currently the general recommenda8ons from the Ins8tute of Medicine, regarding vitamin D levels, are generalized for different pa8ent popula8ons. Table 1 and figure 3 outline the general recommenda8ons from the Ins8tute of Medicine regarding vitamin D levels and overall bone health status for different pa8ent Figure 2 -­‐ Microscopic role of Estrogen on Bone Metabolism10-­‐11 popula8ons. 9,13 Current literature suggests that not only are higher levels of vitamin D needed for ideal bone health for different pa8ent popula8ons than previously recommended, but that the vitamin may also play a role in a number of disease states, such as heart disease, diabetes 12 Furthermore, the leading cause of osteoporosis in women is due to a and c ertain c ancers. 20 The role of estrogen regarding bone metabolism reduc8on in estrogen post-­‐menopause. and homeostasis is correlated with the ac8vity of osteoclasts. Current studies hypothesize that a reduc8on in estrogen availability is responsible for an increase in pro-­‐inflammatory 10 Another current cytokines ac8vity, which in turn increase the ac8vity of osteoclasts. proposed mechanism regarding the role of estrogen in maintaining bone density is based on the inhibi8on of C-­‐C chemokine receptor 2 (CCR2). If uninhibited, these 11receptors respond to available chemokines and further increase the ac8vity of osteoclasts. Figure 2 portrays both current mechanisms regarding the role of Estrogen on bone metabolism. With the increasing na8onal prevalence of obesity and diabetes, two of the most commonly associated co-­‐morbidi8es regarding hypovitaminosis D, among children and adults, the urgency for further research in Vitamin D deficiency cannot be understated. This research inves8gates serum levels of Vitamin D in pa8ents with fractures, in rela8on to age, gender and associated co-­‐morbidi8es. DISCUSSION 50 55 54 Table 3 -­‐ Measured Pa4ent Calcidiol Ranges (ng/mL) (N=209) 50 40 30 20 10 25 17 17 11 11 5 0 Figure 5 -­‐ Common Co-­‐Morbidi4es Encountered in Pa4ent Popula4on 5 1. Holick MF (March 2006). High prevalence of vitamin D inadequacy and implica7ons for health. Mayo Clin. Proc. 81 (3): 353– 73. 2. Norman AW (August 2008). From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essen7al for good health. Am. J. Clin. Nutr. 88(2): 491S–499S. 3. Holick MF (July 2007). Vitamin D deficiency. N. Engl. J. Med. 357 (3): 266–81. 4. Brown JE (2008). Nutri7on through the life cycle. Belmont, CA: Thomson/Wadsworth. Crissey SD, Ange KD, Jacobsen KL, Sliga KA, Bowen PE, Stacewicz-­‐Sapuntzakis M, Langman CB, Sadler W, Kahn S. Serum concentra7ons of lipids, vitamin D metabolites, re7nol, re7nyl esters, tocopherols and selected carotenoids in twelve cap7ve wild felid species at four zoos. The Journal of nutri8on 133 (1): 160–6. (2003). 5. Adams JS, Hewison M. Update in Vitamin D.Journal of Clinical Endocrinology & Metabolism 95 (2): 471–8. (2010). 6. Cheng JB, Levine MA, Bell NH, Mangelsdorf DJ, Russell DW Gene7c evidence that the human CYP2R1 enzyme is a key vitamin D 25-­‐hydroxylase. Proc Natl Acad Sci U S A 101 (20): 7711–7715. May 2004. 7. Laing CJ, Cooke NE. Sec7on I: Ch. 8: Vitamin D Binding Protein. Academic Press. pp. 117–134. (2 ed.)2004. 8. Kris8n K. Vitamin D signaling pathways in cancer: poten7al for an7cancer therapeu7cs. Nature Reviews Cancer 7, 684-­‐700 (September 2007) 9. Ross AC. Ins8tute of Medicine (US) Commijee to Review Dietary Reference Intakes for Vitamin D and Calcium; Washington (DC): Na8onal Academies Press (US); 2011. 10. Riggs, B.L. et al. (2002) Endocr. Rev. 23:279. 11. Binder, N.B. et al. (2009) Nat. Med. 15:417. 12. Holick MF. Sunlight and vitamin D for bone health and preven7on of autoimmune diseases, cancers, and cardiovascular disease. Am J Clin Nutr 2004, Dec;80(6 Suppl):1678S-­‐88S. 13. Ross AC, Taylor CL, Yak8ne AL, Del Valle HB, editors. Ins8tute of Medicine (US) Commijee to Review Dietary Reference Intakes for Vitamin D and Calcium; Dietary Reference Intakes for Calcium and Vitamin D. Washington (DC): Na8onal Academies Press (US); 2011. 14. Norman AW (August 2008). From vitamin D to hormone D: fundamentals of the vitamin D endocrine system essen7al for good health. Am. J. Clin. Nutr. 88(2): 491S–499S. 15. Narasimha Swamy.Fajy acid-­‐binding site environments of serum vitamin D-­‐binding protein and albumin are different Fajy acid-­‐binding site environments of serum vitamin D-­‐binding protein and albumin are different Fajy acid-­‐binding site environments of serum vitamin D-­‐binding protein and albumin are different FaUy acid-­‐binding site environments of serum vitamin D-­‐binding protein and albumin are different. Bioorg Chem. Author manuscript; available in PMC 2009 June Published in final edited form as Bioorg Chem. 2008 June; 36(3): 165–168a