SEP 17 2009 LIBRARIES Factors in Myocardial Tissue
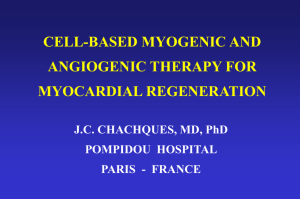
advertisement

Local Pharmacokinetics and Pharmacodynamics of Angiogenic Growth
Factors in Myocardial Tissue
by
MASSACHUSETTS INSTlJTE
Kha N. Le
SEP 17 2009
OF TECHNOLOGY
B.S., Bioengineering, University of California, San Diego
MIT
S.M., Electrical Engineering and Computer Science,
__.
LIBRARIES
SUBMITTED TO THE HARVARD-MIT DIVISION OF HEALTH SCIENCES AND
TECHNOLOGY IN PARTIAL FULFILLMENT OF THE REQUIREMENTS FOR THE
DEGREE OF
DOCTOR OF PHILOSOPHY IN ELECTRICAL AND MEDICAL ENGINEERING
AT THE
MASSACHUSETTS INSTITUTE OF TECHNOLOGY
FEBRUARY 2009
© 2009 Kha N. Le. All rights reserved.
ARCHIVES
The author hereby grants to MIT permission to reproduce
and to distribute publicly paper and electronic
copies of this thesis document in whole or in part
in any medium now known or hereafter created
Signature of Author:
Division of Health Sciences and Technology
February 09, 2009
Certified by:
Elazer R. Edelman, M.D., Ph.D.
(I
Thomas D. and Virginia W. Cabot Professor of Health Sciences and Technology
Thesis Supervisor
4ZZZ_7___
Accepted by:
Ram Sasisekharan, Ph.D.
Director, Harvard-MIT Division of Health Sciences and Technology
of Health Sciences & Technology and Biological Engineering
Professor
Edward Hood Taplin
Local Pharmacokinetics and Pharmacodynamics of Angiogenic Growth
Factors in Myocardial Tissue
By
Kha N. Le
Submitted to the Harvard-MIT Division of Health Sciences and Technology on
February 10, 2009 in Partial Fulfillment of the Requirements for the Degree of Doctor of
Philosophy In Electrical and Medical Engineering
Abstract
Early enthusiasm over angiogenic therapy, a method to induce vascular regeneration to
treat ischemic tissue with growth factors, has been tempered by a series of unsuccessful clinical
trials with limited late efficacy and a wide range of mixed results. This thesis was designed to
examine critically whether the lack of late efficacy of local delivery of angiogenic factors could
be explained by a comprehensive understanding of local pharmacokinetics (PK) and
pharmacodynamics (PD) in the myocardial tissue. Our central hypothesis is that early success at
inducing vessel growth powerfully self-regulates angiogenic therapies by dynamically altering
local tissue pharmacokinetic properties and hinders long-term efficacy. We used a multipronged approach to investigate this hypothesis. We characterized the baseline local myocardial
PK through a series of ex-vivo isolated heart studies and mathematical analysis, examined the
local coupling of PK and PD with an in-vivo ischemic heart model, created a computational
model of myocardial PK and PD to predict distribution of growth factors and their biologic
effects, discussed implications and future studies. Our findings suggest that microvascular
washout impedes myocardial drug transport, early angiogenic response further exacerbates drug
washout and is likely responsible for late vessel regression, modulating drug PK properties to
mitigate drug clearance through washout can enhance late tissue response. These results imply
that local PK-PD interdependence should be carefully examined to improve clinical efficacy of
angiogenic therapy with local angiogenic growth factor delivery.
Thesis Committee:
Prof. Elazer R. Edelman (Thesis Supervisor)
Prof. Matthew Nugent
Prof. Collin Stultz (Committee Chair)
Prof. K. Dane Wittrup
Table of Contents
A bstract ...................................................
...................................................................
2
T able of C ontents ............................................................................................................................ 3
6
List of Figures ...................................................
8
Acknowledgements..................................
9
Chapter 1: Background and Significance .............................................................................
Overview of Thesis ..............................................................................................................
9
1.1 Clinical M otivation ................................................ ....................................................... 10
.......... 10
Clinical Problem and Angiogenic Therapy..................................
1.1.1
1.1.2 Local M yocardial D elivery................................................................................ . 13
1.2 Technical Background ............................................ ...................................................... 14
14
1.2.1 Local Pharmacokinetics and Pharmacodynamics .....................................................
1.2.2 Pharmacokinetics/Pharmacodynamics Modeling .....................................
...... 15
1.3 Thesis Theme .................................................
17
1.4 Thesis Organization ............................................................................................................ 18
1.5 Referen ces ......................................................
............................................................... 19
Chapter 2: Baseline Local Pharmacokinetics of FGF in Myocardium ......................................... 23
A b stract ...................................................................................................................... ..... . .... 2 3
2.1 Introduction......................................
24
2.2 M aterials and Methods........................................................................................................ 26
2.2.1 Recombinant FGF2 Production .........................................................................
26
2.2.2 Fluorescence Labeling of FGF2.........................................................................
27
2.2.3 Size Exclusion Column Chromatography........................................
28
2.2.4 Measurements of Diffusivity ....................................................... 29
2.2.5 Ex-vivo Myocardial Drug Delivery with and without Perfusion......................... . 30
.............. 33
2.2.6 Fluorescence imaging and processing .........................................
2.2.7 Measurement of FGF in Outflow.................................................
33
2.2.8 Continuum Pharmacokinetic Model of Myocardial Drug Transport With and Without
Perfusion ...................................................
34
2.2.9 Analytical Model Calculation of Cumulative FGF Clearance...........................
. 37
2.2.10 Statistical analysis ........................................... ..................................................... 38
2 .3 Results ........................................................................................
................................... 39
2.3.1 FGF Diffusivity in the Absence of Myocardial Perfusion.......................... ....
. 39
2.3.2 FGF Distribution is Limited by Myocardial Perfusion.............................
...... 40
2.3.3 FGF is Washed-out Through Microvascular Clearance Followed Ex-vivo Myocardial
D elivery...........................................
41
2.3.4 SOS limits the effects of capillary washout on FGF2.............................................. 42
2.3.5 Effects of Molecular Weight on Myocardial Transport Under Perfusion ................ 44
2.3.6 Drug Diffusivity, Trans-endothelial Permeability and Vessel Density Influence Local
Drug Distribution and Deposition......................................................46
2.4 Discussion .................................................................................................................... ...... 50
2.4.1 Capillaries limit drug penetration in a manner dependent on molecular weight ......... 50
2.4.2 Ischemic and non-ischemic tissues present different barriers to transport .............. 51
2.4.3 Angiogenesis limits its own success ....................................................
.................. 52
2.5 Summ ary ...........................................
............ .............................................................
53
2.6 References........................................
54
Chapter 3: Interdependence of Local Pharmacokinetics and Pharmacodynamics ...........
57
Abstract .................................................................
..........................................
57
3.1 Introduction......................................
58
3.2 M aterials and Methods........................................................................................................ 60
3.2.1 Recombinant S35-FGF1 Production..............................................
60
3.2.2 Fabrication and Kinetics of Controlled Release Device .....................................
. 62
3.2.3 In-vivo Myocardial Drug Delivery ....................................................................
63
3.2.4 Quantification of in-vivo FGF1 and Blood Vessels Distribution ............................. 64
3.2.5 Statistical analysis ............................................ ...................................................... 65
3.3 Results
............................................
66
3.3.1 Polymeric Devices Sustain Release FGF1 over 30 days in-vivo.............................. 66
3.3.2 In-vivo Angiogenic Response Limits Drug Distribution.......................... ...... 67
3.4 D iscussion ........................................................................................................................... 72
3.5 References ........................................................................................
......... 75
7............
Chapter 4: Computational Modeling of Local Pharmacokinetics and Pharmacodynamics of FGF
in Myocardium.........................................
78
A bstract .................................................................................................................................. 78
4.1 Introduction......................................
79
4.2 M ethods
.............................................
80
4.2.1 Local Pharmacokinetic Model ......................................
82
4.2.1.1 Mass Transport Equations.......................................
82
4.2.2 Local Pharmacodynamic Model ...............................................................................
84
4.2.2.1 C apillary sprouting......................................... ................................................. 84
4.2.2.2 Capillary m aturation ............................................................. .......................... 85
4.2.2.3 C apillary regression ............................................................. ........................... 86
4.2.3 M odel Param eters ............................................. ..................................................... 88
4.2.4 N umerical M ethods........................................... ..................................................... 89
4.3 Results ............................................................................................
90
4.3.1 Local Pharmacokinetic (PK) Model Results: Effects Diffusivity, Trans-endothelial
Permeability and Vascularity on Drug Transport. ........................................
......... 90
4.3.2 Local Pharmacokinetic-Pharmacodynamic (PK-PD) Model Results ....................... 92
4.3.2.1 PK-PD Interdependence: ....................................................... 92
4.3.2.2 Model Sensitivity Analysis: .......................................................
........... 94
4.3.2.2.1 Timings of Capillary Maturation and Regression Have Little Effect on Steady
State C apillary G ain ..................................................................
.............................. 94
4.3.2.2.2 Trans-endothelial Permeability, Diffusivity, Biologic Threshold, Initial
capillary density and Release Kinetics Have Significant Effect on Steady State Drug
Distribution and Capillary gain.................................................................................. 98
4.4 Discussion: .................................................
103
4.4.1 Traditional Continuum PK vs. Continuum PK-PD Analysis.............................
103
4.4.2 Minimizing Microvascular Clearance as an Approach to Optimize Angiogenic Effect
.......................................................................
10 4
4.4.3 Release Rate and Diffusivity Modification to Optimize Angiogenic Effect.......... 105
4.4.4 Minimizing Late Loss as an Effective Approach to Improve Angiogenic Therapy.. 106
4.5 Summ ary .................................................
108
4.6 References
........................................
109
4
Chapter 5: Effects of Tissue Binding on Local Pharmacokinetics of FGF in Myocardium.......
A b stract ...................................................................................................................................
.......................................
5.1 Introduction
5.2 Methods.............................................
5.2.1 Effect of Binding on Myocardial Transport ............................
5.2.2 Long-time point uptake studies.................................
5.3 Results .........................................................................................................................
5.3.1 Tissue Binding Impedes FGF Transport in Myocardial Tissue ..............................
5.3.2 Modulating tissue binding alters myocardial FGF2 transport ................................
5.4 D iscu ssion .........................................................................................................................
5.4.1 Binding reduces effective diffusivity, but can be modulated by protective groups...
5.4.2 Implications for Angiogenic Growth Factor Delivery .....................................
5.5 Summary .................................................
5.6 References........................................
Chapter 6: Future Studies and Conclusions .....................................
6.1 Future Studies ...................................................................................................................
6. 1.1 Characterization of Trans-endothelial Permeability in Myocardium. .....................
6.1.2 Computational Models of Angiogenesis ......................................
6.1.3 Characterization of Effect of Binding.....................................................................
6.2 Thesis Sum mary................................................................................................................
6.3 References ......................................................................... ......................... ....................
APPENDIX:
.........................................
MATLAB code: PK-PD Model ........................................
111
111
112
114
114
115
116
116
117
12 1
121
123
125
126
128
128
128
130
130
132
133
134
134
List of Figures
Chapter 2: Baseline Pharmacokinetics of FGF in Myocardium
Fig. 2-1
Elution profile of FGF2
27
Fig. 2-2
Isolated perfused heart apparatus
30
Table 1-1
Continuum pharmacokinetic model equations
37
Fig. 2-3
FGF2 diffusivity measurements
39
Fig. 2-4
Myocardial capillary perfusion impedes drug penetration
40
Fig. 2-5
FGF is washed-out through microvascular clearance
41
Fig. 2-6
Size exclusion chromatography of FGF2, and its complexes
42
Fig. 2-7
Distribution of TR-(FGF2)2-SOS
43
Fig. 2-8
Deposition with and without flow of EBD, Dextrans, FGF, FGF-SOS, BSA
45
Fig. 2-9
Continuum pharmacokinetic model
46
Fig. 2-10
FGF distribution is sensitive to alteration in drug clearance
47
Chapter 3: Interdependence of Local Pharmacokinetics and Pharmacodynamics
35
Fig. 3-1
Recombinant
S-FGF1 production and purification
60
Fig.3-2
In-vivo ischemic heart model of local myocardial delivery of FGF
64
Fig. 3-3
Polymeric devices sustain release FGF1 over 30 days
66
Fig 3-4
Spatial-temporal profiles of 35S-FGF1 in-vivo
69
Fig 3-5
Representative fluorescent images of stained blood vessels
70
Fig 3-6
Vascular to tissue surface fraction at different times
71
Chapter 4: Computational Modeling of Local Pharmacokinetics and Pharmacodynamics
Fig. 4-1
Schematics of computational model
83
Table 4-1
Summary of model equations
84
Table 4-2
Summary of angiogenic model algorithm.
87
Table 4-3
Baseline parameter values
88
Fig. 4-2
PK model results
91
Fig. 4-3
PK/PD model results: drug and capillary distributions as a function of time
93
Fig. 4-4
Effects of tfinctional
96
Fig. 4-5
Effects of t regression
97
Fig. 4-6
Effect of initial vascularity
98
Fig. 4-7
Effects of diffusivity, permeability, C,, and release rate
101
Fig. 4-8
Steady state percentage capillary gain as function of model parameters
102
Fig. 4-9
Approaches to improve pro-angiogenic therapy
107
Chapter 5: Effect of Binding on Local PK of FGF in Myocardium
Table 5-1
Summary of derivation of effect of tissue binding on effective diffusivity
114
Fig. 5-1
Concentration dependent transport of FGF2
119
Fig. 5-2
Modulation of binding alters myocardial FGF2 transport
120
Acknowledgements
I would like to express my gratitude to many people without whom this work would not
be possible.
First I am especially proud to have worked with my advisor, Prof. Elazer Edelman, a
great teacher and scientist. I'm indebted to Prof. Edelman for his mentorship and guidance
throughout my academic career, and for allowing me the unique independence and
responsibilities. I have learned much from many experiences working with him in the lab and the
HST.090 course. Prof. Edelman has been my role model as a critical thinker, problem solver,
scientist, and teacher.
I would like to thank my Thesis Committee members, Dr. Matthew Nugent, Dr. Collin
Stultz, and Dr. K. Dane Wittrup, for agreeing to serve on the committee, asking tough questions
to make me think harder about the project, and for their time reading the thesis.
I would like to thank all the people in the Edelman lab for their help, encouragement and
support. In particular, Rami Tzafriri for many helps in mathematical analysis and publishing
process, and for many interesting scientific discussions and friendship, Chao-Wei Hwang for his
help in getting my project started and solving many technical problems and friendship, Mark
Lovich for advising many experimental aspects of the project and agreeing to be my HST.203
preceptor, Peter Wu for friendship, and help with labeling FGF and many interesting scientific
discussions, David Ettenson for answering many questions from biology to job hunting,
Abraham Wei, for technical help with FGF, Laurie May for helping with many of the logistics of
thesis meetings and defense, and Michele Miele for making sure my radioactive experiments are
safe. I would like to also thank Dr. Alison Hayward and Dr. Robert Marini in MIT DCM for
their help creating the rabbit ischemic heart model, and helping with the surgeries.
I would like to express my gratitude to my family. First and foremost my wife, Thoa, for
her love, patience and support throughout my academic years and my sons, Khoi and Ben for
making my everyday life meaningful and enjoyable, and my parents without whom none of the
work in this thesis would have been possible in the first place.
Kha Le
2/2009
Chapter 1: Background and Significance
Overview of Thesis
The paradox of angiogenesis science is that stable sustained vascular regeneration in humans
has not been realized despite promising preclinical findings. The driving hypothesis for this
Thesis is that early success at inducing vessel growth powerfully self-regulates angiogenic
therapies by dynamically alteringlocal tissuepharmacokineticproperties.This thesis was
designed to critically examine this hypothesis and to examine whether it could in part explain the
limited late efficacy of local delivery of angiogenic factors.
Specifically, this thesis consists of a series of studies designed to examine the
interdependence of local pharmacokinetics and pharmacodynamics of local angiogenic growth
factor delivery. The aims include:
Chapter 2: Defines myocardial PK at a multi-cellular level with ex-vivo experimental
studies and quantitative analysis of steady state drug distributions.
Chapter 3: Examines the PK-PD interdependence with in-vivo animal model of drug
transport and angiogenesis.
Chapter 4: Derives a mechanistically based computational model of the local PK-PD of
angiogenic growth factors in myocardial tissue to predict distribution of drugs and
biologic effects.
Chapter 5: Examines the effect of tissue binding on transport and discusses implications
and future studies.
The quantitative framework presented here may help guide rational selection of specific
angiogenic compounds based on a favorable physicochemical profile, and drug delivery
strategies that take advantage of the tight regulation between growth factor pharmacokinetics and
angiogenic pharmacodynamics.
1.1 Clinical Motivation
1.1.1
Clinical Problem and Angiogenic Therapy
Cardiovascular diseases affect more than 70 million Americans and account for 1 out of 2.7
deaths in the United States 1. The most common cause leading to these cardiovascular diseases
is coronary artery disease (CAD) causing by blockage of one or more coronary arteries supplying
blood to the heart tissue as a result of loss of endothelial integrity, infiltration of monocytes,
macrophages and vascular smooth muscle cells, and/or aberrant vasospasm. These partial or
complete stenoses of coronary arteries can threaten cardiac tissue integrity. The severity of the
consequences of myocardial ischemia as a result of inadequate oxygenation and accumulation of
metabolic waste products depends on the magnitude and duration of the reduction in myocardial
supply. These range from rapid and full recovery of myocyte function, prolonged contractile
dysfunction without myocyte necrosis, to irreversible myocardial necrosis. Rescuing the
ischemic myocardium prior to necrosis can restore its function. The few available therapeutic
interventions including angioplasty, atherectomy, stenting, and vascular bypass surgery center on
mechanical revascularization to increase lumen diameter of the occluded arteries. These
interventional procedures are effective for well-defined lesions in large coronary arteries.
However, a substantial number of patients with diffuse and small-vessel coronary artery disease
whose lesions are not readily accessible by these treatments and those who lack of conduits for
bypass surgery cannot be benefited. Almost 1.5 million cardiac catheterization procedures and
0.5 million coronary artery bypass surgeries are performed yearly for attempted relief of the
complications of these illnesses
'.
It has been estimated that up to a third of patients presenting
with advanced coronary disease receive incomplete revascularization with conventional
percutaneous and surgical techniques due to the presence of diffuse disease and unsuitable
coronary anatomy 2
Collateral coronary vessel formation stimulation using angiogenic growth factors has the
potential to reduce myocardial infarct size and improve cardiac function 4. Induced angiogenesis
may prove to be the optimal therapy for coronary arteries that are not suited for traditional
intervention and may also be of benefit when given as an adjunct to mechanical
revascularization. While the biological time scale for angiogenesis exceeds the time required for
salvaging infracting myocardium for acute myocardial infarction patients, this approach holds
promise for those with chronic myocardial ischemia, and may be the only hope for those patients
with small-vessel disease and are ill-suited for transplantation. Furthermore, just as coronary
artery obstruction induces myocardial ischemia, peripheral artery obstruction can induce skeletal
muscle ischemia, causing debilitating symptoms in patients with peripheral artery disease (PAD)
intermittent claudication and critical limb ischemia 5. Biological revascularization with
angiogenic therapy remains an equally promising therapeutic approach for PAD as well as CAD
patients.
Fibroblast growth factors 1 and 2 (FGF1 and FGF2) are the most studied growth factors
for the induction of myocardial angiogenesis
6. They
belong to a large family of polypeptide
growth factors that are found in many organisms ranging from worms to humans, and are highly
conserved in both gene structure and amino acid sequence 6. In addition to binding to its cognate
surface receptors, FGFR, FGFs also exhibit a high affinity for heparan sulfate proteoglycans.
These interactions have been shown to stabilize FGFs from thermal denaturation and proteolysis
and can result in the formation of dimers or higher order oligomers -10. It has also been
suggested that these interactions with heparin/heparan sulfate are required for effective signaling
downstream of FGFR activation 11-13. FGFs are known to have diverse roles in regulating cell
proliferation, migration and differentiation during embryonic development and in tissue repair in
adult life. Upon FGFR activation and FGF endocytosis, FGFs are known to promote
angiogenesis not only by stimulating the growth of new blood vessels
their apoptotic potential
15.
14,
but also by abrogating
FGF1 and 2 can promote all of the requisite events for angiogenesis,
including endothelial activation, proliferation, increased survival, migration, and differentiation
.
Yanagisawa-Miwa et. al. 4 was one of the first study to show that intracoronary injection
of FGF to ischemic myocardium can stimulate neovascularization, reduce myocardial infarct size
studies
and improve cardiac function. Despite many subsequent impressive animal
14,16-19
clinical trials of myocardial angiogenesis employing intracoronary infusion have been
disappointing
20,21.
Local intra-myocardial and pericardial sustained delivery can elevate
myocardial drug concentration and lower systemic exposure in animal models 22 but such
techniques have not proven uniformly effective in humans. Of the 8 clinical investigations to
date
20,' 21, 23-25,
Laham et.al. 2 1 is the only one to show any effectiveness of angiogenic therapy
using sustained local perivascular delivery of bFGF. The reasons accounting for these mixed
results remained unanswered.
1.1.2 Local Myocardial Delivery
Angiogenic growth factors are highly potent and short in half-life, but require long
retention time to establish chemotactic and survival signals. These properties and requirements
pose a challenge to systemic administration and underscore the need for local myocardial
delivery 30. Several strategies have been developed to allow local growth factor delivery to the
myocardial tissue. Bolus delivery that preferentially deposits drug to myocardium includes intracoronary and intra-myocardial injection 3 1. Controlled-release delivery involves using pumpbased or chemical-based devices, such as polymers, that hold and apply drugs to myocardial
tissue through pericardial or intra-myocardial routes
release of drugs for months
34-36
17, 32, 33.
Polymeric based devices can sustain
and can offer better pharmacokinetic advantage than local bolus
administration and systemic delivery. Despite advanced local delivery technologies, angiogenic
therapy has not endured clinical success. It is unclear whether these mixed successes are related
to basic growth factor biology or drug transport issues. With tremendous resources being poured
into therapeutic angiogenesis research at both preclinical and clinical stages, a detailed
systematic characterization of local myocardial pharmacokinetics therefore is imperative to help
answer this question.
1.2 Technical Background
1.2.1 Local Pharmacokinetics and Pharmacodynamics
Pharmacokinetics (PK), the science of the kinetics of drug absorption, distribution, and
elimination, and pharmacodynamics (PD), the study of relationship between drug concentration
and pharmacologic response, are established fields of study in biopharmaceutics 37. These
conventional PK and PD analyses although well suited to study drugs targeting the central
plasma compartment but in general do not consider spatial aspect of the problem and are not
suitable for local drug delivery studies. The large and dynamic concentration gradients imparted
by the delivery devices across target tissues have proven difficult to identify, characterize and
control. Cells near the source of drug release are likely surrounded by a vastly different
concentration than cells far away. Drug levels are not static in time, and indeed can depend on
local tissue structures and local transport parameters
36, 38, 39.
It is, therefore, anticipated that local
tissue response to angiogenic growth factors will track the latter's spatio-temporal distribution
27.
Thus, failure to sustain the requisite myocardial growth factor distribution may underlie much
of the variability in the results of local approaches in angiogenic therapy. Yet, local
pharmacokinetics in the myocardium has not been well characterized. For instance, little is
known about the mechanism growth factor transport following local delivery.
Studies in arteries suggested that tissue ultrastructure and local physiologic forces
influence drug distribution 26-29. The mechanisms of soluble drug transport and elimination are,
therefore, most likely responsible for myocardial distribution and deposition of growth factors.
For highly vascularized tissues such as the myocardium, in addition to diffusion and tissue
binding, these also include the mechanism of drug clearance through microvascular washout.
Reversible binding to fixed tissue components that are required for endocytotic internalization
and biologic activity is expected to have a significant impact on drug transport. Furthermore, as
current drug release technologies allow more growth factors to be released in a controlled
manner over a long period of time, the tissue response and remodeling process become
increasingly important in altering the local pharmacokinetics by modifying the factors mentioned
above, for instance changes in vascular density, trans-endothelial permeability as a result of
therapeutic success. A quantitative appreciation and systematic characterization of these local
pharmacokinetics and pharmacodynamics factors influencing drug distribution will thus be
conducive to a more rational approach to delivery strategy, dosage and drug design.
1.2.2 Pharmacokinetics/Pharmacodynamics Modeling
Drugs are in a dynamic state within the body as they move within tissues and between
tissues and blood, bind with different cellular and extracellular components, or are cleared and
metabolized. The distribution of drugs and their biologic effects is complex since it can be
influenced by any of these drug events. Yet detailed understanding of such events is crucial to
characterize drug PK and PD. Such complexity requires the use of mathematical models to
predict the time course of drug distribution and effects to guide drug and delivery strategy
designs. Mathematical modeling of PK is traditionally divided into three categories: empirically,
compartmentally, and physiologically or mechanistically based. Empirical models are useful in
obtaining specific parameters by curve fitting well controlled experimental data. Compartmental
models, lumping various tissues into instantaneously well mixed compartments, are simple and
useful for systemic PK studies but not suited for local PK analysis. Mechanistic models based on
known physiologic processes are useful for regional analysis, such as local pharmacokinetic
models used in arterial drug delivery
26, 28, 29, 40, 41.
These mechanistically based models are
crucial for predicting drug distribution and optimization studies with local delivery, but require
accurate and difficult to obtain model parameters.
1.3 Thesis Theme
The paradox of angiogenesis science is that stable sustained vascular regeneration in
humans has not been realized despite promising preclinical findings. Our hypothesis is that the
limited late efficacy of local delivery of angiogenicfactors stems partlyfrom the very early
success at inducing vessel growth because angiogenic therapiespowerfully self-regulate by
dynamically alteringlocal tissuepharmacokineticproperties.These local changes can affect
global outcome of therapy and require in depth studies of local PK and PD of angiogenic growth
factor within myocardial tissues. This interdependence of pharmacokinetics and
pharmacodynamics may explain the difficulty of realizing sustained clinical angiogenesis with
local release. The quantitative framework presented here may help guide rational selection of
specific angiogenic compounds based on a favorable physicochemical profile, and drug delivery
strategies that take advantage of the tight regulation between growth factor pharmacokinetics and
angiogenic pharmacodynamics.
1.4 Thesis Organization
This thesis consists of a series of studies designed to examine the interdependence of
local pharmacokinetics and pharmacodynamics of local angiogenic growth factor delivery. The
specific aims include:
Chapter 2: Defines myocardial PK at a multi-cellular level with ex-vivo experimental
studies and quantitative analysis of steady state drug distributions.
Chapter 3: Examines the PK-PD interdependence with in-vivo animal model of drug
transport and angiogenesis.
Chapter 4: Derives a mechanistically based computational model of the local PK-PD of
angiogenic growth factors in myocardial tissue to predict distribution of drugs and
biologic effects.
Chapter 5: Examines the effect of tissue binding on transport and discusses implications
and future studies.
1.5 References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Thom T, Haase N, Rosamond W, Howard VJ, Rumsfeld J, Manolio T, Zheng ZJ, Flegal
K, O'Donnell C, Kittner S, Lloyd-Jones D, Goff DC, Jr., Hong Y, Adams R, Friday G,
Furie K, Gorelick P, Kissela B, Marler J, Meigs J, Roger V, Sidney S, Sorlie P,
Steinberger J, Wasserthiel-Smoller S, Wilson M, Wolf P. Heart disease and stroke
statistics--2006 update: a report from the American Heart Association Statistics
Committee and Stroke Statistics Subcommittee. Circulation. 2006; 113:e85-151.
Kleisli T, Cheng W, Jacobs MJ, Mirocha J, Derobertis MA, Kass RM, Blanche C,
Fontana GP, Raissi SS, Magliato KE, Trento A. In the current era, complete
revascularization improves survival after coronary artery bypass surgery. J Thorac
Cardiovasc Surg. 2005; 129:1283-1291.
Rivard A, Isner JM. Angiogenesis and vasculogenesis in treatment of cardiovascular
disease. Mol Med. 1998; 4:429-440.
Yanagisawa-Miwa A, Uchida Y, Nakamura F, Tomaru T, Kido H, Kamijo T, Sugimoto
T, Kaji K, Utsuyama M, Kurashima C. Salvage of infarcted myocardium by angiogenic
action of basic fibroblast growth factor. Science. 1992; 257:1401-1403.
Aviles RJ, Annex BH, Lederman RJ. Testing clinical therapeutic angiogenesis using
basic fibroblast growth factor (FGF-2). Br J Pharmacol. 2003; 140:637-646.
Ornitz DM, Itoh N. Fibroblast growth factors. Genome Biol. 2001; 2:REVIEWS3005.
Moscatelli D. High and low affinity binding sites for basic fibroblast growth factor on
cultured cells: absence of a role for low affinity binding in the stimulation of plasminogen
activator production by bovine capillary endothelial cells. J Cell Physiol. 1987; 131:123130.
Herr AB, Ornitz DM, Sasisekharan R, Venkataraman G, Waksman G. Heparin-induced
self-association of fibroblast growth factor-2. Evidence for two oligomerization
processes. J Biol Chem. 1997; 272:16382-16389.
Mach H, Volkin DB, Burke CJ, Middaugh CR, Linhardt RJ, Fromm JR, Loganathan D,
Mattsson L. Nature of the interaction of heparin with acidic fibroblast growth factor.
Biochemistry. 1993; 32:5480-5489.
Moy FJ, Safran M, Seddon AP, Kitchen D, Bohlen P, Aviezer D, Yayon A, Powers R.
Properly oriented heparin-decasaccharide-induced dimers are the biologically active form
of basic fibroblast growth factor. Biochemistry. 1997; 36:4782-4791.
Ornitz DM, Yayon A, Flanagan JG, Svahn CM, Levi E, Leder P. Heparin is required for
cell-free binding of basic fibroblast growth factor to a soluble receptor and for
mitogenesis in whole cells. Mol Cell Biol. 1992; 12:240-247.
Rapraeger AC, Krufka A, Olwin BB. Requirement of heparan sulfate for bFGF-mediated
fibroblast growth and myoblast differentiation. Science. 1991; 252:1705-1708.
Yayon A, Klagsbrun M, Esko JD, Leder P, Ornitz DM. Cell surface, heparin-like
molecules are required for binding of basic fibroblast growth factor to its high affinity
receptor. Cell. 1991; 64:841-848.
Montesano R, Vassalli JD, Baird A, Guillemin R, Orci L. Basic fibroblast growth factor
induces angiogenesis in vitro. Proc Natl Acad Sci U S A. 1986; 83:7297-7301.
Dimmeler S, Zeiher AM. Endothelial cell apoptosis in angiogenesis and vessel
regression. Circ Res. 2000; 87:434-439.
16.
17.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
Unger EF, Banai S, Shou M, Lazarous DF, Jaklitsch MT, Scheinowitz M, Correa R,
Klingbeil C, Epstein SE. Basic fibroblast growth factor enhances myocardial collateral
flow in a canine model. Am J Physiol. 1994; 266:H1588-1595.
Lopez JJ, Edelman ER, Stamler A, Hibberd MG, Prasad P, Thomas KA, DiSalvo J,
Caputo RP, Carrozza JP, Douglas PS, Sellke FW, Simons M. Angiogenic potential of
perivascularly delivered aFGF in a porcine model of chronic myocardial ischemia. Am J
Physiol. 1998; 274:H930-936.
Watanabe E, Smith DM, Sun J, Smart FW, Delcarpio JB, Roberts TB, Van Meter CH, Jr.,
Claycomb WC. Effect of basic fibroblast growth factor on angiogenesis in the infarcted
porcine heart. Basic Res Cardiol. 1998; 93:30-37.
Harada K, Friedman M, Lopez JJ, Wang SY, Li J, Prasad PV, Pearlman JD, Edelman ER,
Sellke FW, Simons M. Vascular endothelial growth factor administration in chronic
myocardial ischemia. Am J Physiol. 1996; 270:H1791-1802.
Henry TD, Annex BH, McKendall GR, Azrin MA, Lopez JJ, Giordano FJ, Shah PK,
Willerson JT, Benza RL, Berman DS, Gibson CM, Bajamonde A, Rundle AC, Fine J,
McCluskey ER. The VIVA trial: Vascular endothelial growth factor in Ischemia for
Vascular Angiogenesis. Circulation. 2003; 107:1359-1365.
Simons M, Annex BH, Laham RJ, Kleiman N, Henry T, Dauerman H, Udelson JE,
Gervino EV, Pike M, Whitehouse MJ, Moon T, Chronos NA. Pharmacological treatment
of coronary artery disease with recombinant fibroblast growth factor-2: double-blind,
randomized, controlled clinical trial. Circulation. 2002; 105:788-793.
Lazarous DF, Shou M, Stiber JA, Dadhania DM, Thirumurti V, Hodge E, Unger EF.
Pharmacodynamics of basic fibroblast growth factor: route of administration determines
myocardial and systemic distribution. Cardiovasc Res. 1997; 36:78-85.
Henry TD, Rocha-Singh K, Isner JM, Kereiakes DJ, Giordano FJ, Simons M, Losordo
DW, Hendel RC, Bonow RO, Eppler SM, Zioncheck TF, Holmgren EB, McCluskey ER.
Intracoronary administration of recombinant human vascular endothelial growth factor to
patients with coronary artery disease. Am Heart J. 2001; 142:872-880.
Pecher P, Schumacher BA. Angiogenesis in ischemic human myocardium: clinical results
after 3 years. Ann Thorac Surg. 2000; 69:1414-1419.
Unger EF, Goncalves L, Epstein SE, Chew EY, Trapnell CB, Cannon RO, 3rd, Quyyumi
AA. Effects of a single intracoronary injection of basic fibroblast growth factor in stable
angina pectoris. Am J Cardiol. 2000; 85:1414-1419.
Lovich MA, Philbrook M, Sawyer S, Weselcouch E, Edelman ER. Arterial heparin
deposition: role of diffusion, convection, and extravascular space. Am J Physiol. 1998;
275:H2236-2242.
Lovich MA, Edelman ER. Tissue concentration of heparin, not administered dose,
correlates with the biological response of injured arteries in vivo. Proc Natl Acad Sci U S
A. 1999; 96:11111-11116.
Hwang CW, Wu D, Edelman ER. Physiological transport forces govern drug distribution
for stent-based delivery. Circulation. 2001; 104:600-605.
Hwang CW, Edelman ER. Arterial ultrastructure influences transport of locally delivered
drugs. Circ Res. 2002; 90:826-832.
Epstein SE, Fuchs S, Zhou YF, Baffour R, Kornowski R. Therapeutic interventions for
enhancing collateral development by administration of growth factors: basic principles,
early results and potential hazards. Cardiovasc Res. 2001; 49:532-542.
31.
32.
33.
34.
35.
36.
37.
38.
39.
40.
41.
42.
43.
44.
45.
46.
Biswas SS, Hughes GC, Scarborough JE, Domkowski PW, Diodato L, Smith ML,
Landolfo C, Lowe JE, Annex BH, Landolfo KP. Intramyocardial and intracoronary basic
fibroblast growth factor in porcine hibernating myocardium: a comparative study. J
Thorac Cardiovasc Surg. 2004; 127:34-43.
Lopez JJ, Edelman ER, Stamler A, Hibberd MG, Prasad P, Caputo RP, Carrozza JP,
Douglas PS, Sellke FW, Simons M. Basic fibroblast growth factor in a porcine model of
chronic myocardial ischemia: a comparison of angiographic, echocardiographic and
coronary flow parameters. J Pharmacol Exp Ther. 1997; 282:385-390.
Sakakibara Y, Tambara K, Sakaguchi G, Lu F, Yamamoto M, Nishimura K, Tabata Y,
Komeda M. Toward surgical angiogenesis using slow-released basic fibroblast growth
factor. Eur J Cardiothorac Surg. 2003; 24:105-111; discussion 112.
Edelman ER, Brown L, Langer R. Quantification of insulin release from implantable
polymer-based delivery systems and augmentation of therapeutic effect with
simultaneous release of somatostatin. J Pharm Sci. 1996; 85:1271-1275.
Edelman ER, Mathiowitz E, Langer R, Klagsbrun M. Controlled and modulated release
of basic fibroblast growth factor. Biomaterials. 1991; 12:619-626.
Raman VK, Edelman ER. Coated stents: local pharmacology. Semin Interv Cardiol.
1998; 3:133-137.
Shargel L, Wu-Pong S, Yu ABC. Applied biopharmaceutics& pharmacokinetics.5th ed.
New York: Appleton & Lange Reviews/McGraw-Hill, Medical Pub. Division; 2005.
Rippley RK, Stokes CL. Effects of cellular pharmacology on drug distribution in tissues.
Biophys J. 1995; 69:825-839.
Baumbach A, Herdeg C, Kluge M, Oberhoff M, Lerch M, Haase KK, Wolter C, Schroder
S, Karsch KR. Local drug delivery: impact of pressure, substance characteristics, and
stenting on drug transfer into the arterial wall [see comments]. Catheter Cardiovasc
Interv. 1999; 47:102-106.
Hwang CW, Wu D, Edelman ER. Impact of transport and drug properties on the local
pharmacology of drug-eluting stents. Int J Cardiovasc Intervent. 2003; 5:7-12.
Lovich MA, Edelman ER. Mechanisms of transmural heparin transport in the rat
abdominal aorta after local vascular delivery. Circ Res. 1995; 77:1143-1150.
Mahoney MJ, Saltzman WM. Millimeter-scale positioning of a nerve-growth-factor
source and biological activity in the brain. Proc Natl Acad Sci U S A. 1999; 96:45364539.
Dowd CJ, Cooney CL, Nugent MA. Heparan sulfate mediates bFGF transport through
basement membrane by diffusion with rapid reversible binding. J Biol Chem. 1999;
274:5236-5244.
Natke B, Venkataraman G, Nugent MA, Sasisekharan R. Heparinase treatment of bovine
smooth muscle cells inhibits fibroblast growth factor-2 binding to fibroblast growth
factor receptor but not FGF-2 mediated cellular proliferation. Angiogenesis. 1999; 3:249257.
Fannon M, Forsten KE, Nugent MA. Potentiation and inhibition of bFGF binding by
heparin: a model for regulation of cellular response. Biochemistry. 2000; 39:1434-1445.
Richardson TP, Trinkaus-Randall V, Nugent MA. Regulation of basic fibroblast growth
factor binding and activity by cell density and heparan sulfate. J Biol Chem. 1999;
274:13534-13540.
47.
Flaumenhaft R, Moscatelli D, Rifkin DB. Heparin and heparan sulfate increase the radius
of diffusion and action of basic fibroblast growth factor. J Cell Biol. 1990; 111:1651 1659.
Chapter 2: Baseline Local Pharmacokinetics of FGF in Myocardium
Abstract
While mechanistically attractive, local delivery of angiogenic growth factors has a
disappointing record at inducing sustained therapeutic myocardial angiogenesis in human clinical
trials. We hypothesized that these results partly stem from the inherent local pharmacokinetics
of drugs in myocardium. Transport forces in myocardium include diffusion and microvascular
clearance. For some drugs especially growth factors such as FGFs, binding to fixed tissue sites
can further complicate drug transport. In non-perfused rat myocardium, drug transport is mainly
governed by diffusion and binding processes. Without coronary perfusion, FGF2 distributions
followed linear diffusion with low diffusivity (0.024m 2/s) and low tissue penetration (65pm).
Restoration of coronary flow enhanced clearance, limiting penetration even further. FGF2
penetration depth contracted by 46% to 35 tm. FGF clearance through washout was confirmed
by the presence of FGF in coronary outflow. These findings were well explained by a diffusionclearance analytical model, with a clearance rate constant determined to be K = 1.15x 10-4 se-1
for FGF2 and 4.37x 10- 5 sec l for FGF2 dimer. Penetration of high molecular weight and low
capillary permeability (FGF2) 2-sodium octa-sulfate dimer was unaffected by coronary perfusion.
Furthermore, studies with additional molecules revealed the relationship between capillary drug
washout and drug molecular weight is sigmoidal, with an inflection point at 20 kDa. Our results
suggest that capillary networks present physical obstacles to drug uptake following local
myocardial delivery, and given the gradations in capillary density and trans-endothelial
permeability with angiogenic therapy, uptake and deposition of angiogenic growth factors will
vary tremendously across the heart.
2.1 Introduction
Different approaches of localizing drugs to myocardial tissue have been studied
extensively including Swanz Ganz catheter, left atrial, intracoronary, intramyocardial, and
pericardial routes. Intrapericardial delivery have been shown to have a significant
pharmacokinetic advantage over the cathether based intravascular local delivery routes 1, 2, and to
be a consistent way to deliver drug to the heart tissue 3. As a small fluid filled closed
compartment surrounding the heart, pericardial space provides an ideal drug reservoir for local
myocardial delivery 4. Intrapericardial application of nitric oxide donors 5,6 and antiarrthymic
agents 7have been shown to elicit expected biologic effects on heart functions.
Chemotherapeutic drug 8 and glucocorticoids 9 have also been delivered to pericardial space to
treat pericardial effusions. These pharmacodynamic studies suggest that pericardial delivery is a
promising strategy for local myocardial delivery. Nevertheless, many fundamental
pharmacokinetic questions regarding this route of local delivery have not been satisfactorily
answered. For instance, it is not clear how the extensive vascular networks within the
myocardium affect solute transport within the tissue, and whether this effect can be characterized
in a quantitative manner to allow for comparative studies and facilitate predictive computational
modeling.
Local physiological forces have been shown to significantly influence drug deposition in
arterial tissues 1 -' 5 . Unlike arterial wall, cardiac myocytes are perfused by a dense capillary
network
16, 17.
Theoretically, if downstream convection dominates, capillaries can act as sinks
and decrease drug uptake 18. If lumen-tissue interfacial diffusion is rapid, then capillaries act as
conduits to other parts of tissue and increase drug penetration. Drug transport within the
myocardial tissue therefore is dictated by a balance between downstream convection and lumentissue interfacial diffusion. In this chapter, we sought to understand how physiological factors in
myocardium affect delivery of angiogenic growth factors. First, we show that in the absence of
coronary perfusion, diffusion and binding are the dominant transport hindrance factors. We
attempt to characterize the myocardial effective diffusivity of many drug compounds in this
chapter and defer the studies of effects of tissue binding to Chapter 5. Using an ex vivo perfused
rat heart model, we also show that myocardial capillaries act primarily as sinks rather than
conduits for drugs with physicochemical parameters similar to angiogenic growth factors. Next,
we show that the substantial capillary washout of FGF2 can be modulated by physical alteration
of the growth factor. This can be accomplished by creating complexes of FGF2 and sugar
groups such as sucrose octasulfate (SOS) and inducing FGF2 dimerization. We designed these
pharmacokinetic experiments to look at the effect of transport factors in isolation. Our analysis
represents a systematic approach to local myocardial pharmacokinetics that may eventually
allow the selection of angiogenic compounds based on favorable physicochemical properties,
potentially leading to the design of controlled-release strategies that take advantage of local
pharmacokinetics to maximize pharmacologic revascularization.
2.2 Materials and Methods
2.2.1 Recombinant FGF2 Production
Recombinant FGF2 was expressed in Escherichiacoli strain FICE-127 transformed by
plasmid vector pFC80 that confers resistance to ampicillin and encodes FGF2 under the control
of the tryptophan promoter (the transformed FICE-127 strain was a gift from John Heath,
University of Birmingham, and was originally constructed by Antonella Isacchi, Amersham
Pharmacia Biotech and Upjohn). FICE-127 cells containing pFC80 were inoculated into LB
Medium (MP Biomedicals) containing 0.29 mmol/L (10 mg/dL) of ampicillin (Invitrogen) and
grown overnight at 37C in a shaker at 250 RPM. The inoculums were diluted 1:100 in M9
Minimal Medium (Fisher Scientific) containing 1 g/L amino acids (Becton Dickinson) without
tryptophan to induce protein production. Cells were grown for 6 h at 370 C in a shaker at 250
RPM. Cells were collected by centrifugation at 8000 RPM for 10 m and kept frozen at -800 C.
Frozen cell pellets were resuspended in 6.94x 10-2 mmol/L (100 mg/dL) lysozyme in GET buffer
(100 mmol/L Glucose, 10 mmol/L EDTA, and 50 mmol/L Tris, pH 8.0), vigorously agitated for
5 m and homogenized (Polytron; Kinematica) 5 times for 30 s each with break periods of 60-90 s
at 4°C to prevent overheating and denaturation of proteins.
Bacterial lysate was collected by centrifugation at 9,000 RPM for 10 m at 40 C. FGF2 was
then purified using affinity chromatography with FPLC (Pharmacia Biotech). Lysate was loaded
into 5 mL heparin Sepharose column (HiTrap, GE Healthcare) and allowed to bind for 2 h at
4°C. The FPLC system was programmed to wash the column with phosphate buffered saline
(PBS) containing incrementally concentrated NaCl with a linear gradient (150 mmol/L to 2000
mmol/L). Elutions were collected in sequential 1 mL fractions, with FGF2 eluting at 1400
mmol/L to 1600 mmol/L NaC1. The FGF2 solution was desalted by centrifugation using
centrifugal filters with 10 kDa molecular weight cut-off (Centricon, Millipore). After each
purification, the presence of FGF2 was confirmed at a 18kDa band using SDS-PAGE, and
protein concentration was quantified with a BCA assay (Pierce). Bioactivity of FGF2 was
confirmed by in vitro proliferation assays using bovine aortic endothelial cells.
2.2.2 Fluorescence Labeling of FGF2
A heparin Sepharose
-[NaCI]
column (HiTrap, GE Healthcare)
FGF2
* Fluorescence
was loaded with 1 mL of 0.12
mmol/L (200 mg/dL) FGF2 in
.
PBS and allowed to bind for 1 h
0.5
0
z
at room temperature. The FGF2loaded column was washed with
5 mL of 100 mmol/L NaHCO3 to
increase the pH to 8.3 and loaded
(100
with 1 mL of 1.60 mmol/L
0
5
10
15
Fraction number
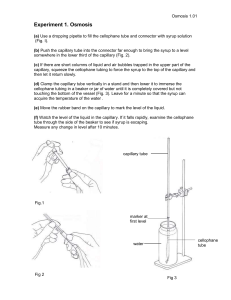
FIGURE 1: Elution profiles of FGF2 (blue), TR (red),
and NaC1 (black).
mg/dL) Texas Red succinimidyl ester (Invitrogen). Texas Red succinimidyl ester was allowed to
react with FGF2 for 10 m at room temperature. The column was then placed in-line on the FPLC
system, and FGF2 was eluted as described above. Elutions of 1 mL were collected and assayed
for protein content (absorbance at 280 nm, FPLC System) and Texas Red fluorescence intensity
(595 nm/615 nm excitation/emission wavelengths, Fluoroskan II, Lab Systems Oy). Texas Red
was appropriately conjugated to FGF2 as indicated by the concurrence of the elution peaks of
fluorescence intensity and protein concentration. Both came off the column between 1400 to
1600 mmol/L NaCi (Fig. 1), similar to the elution range of unlabeled FGF2, suggesting that
Texas Red conjugation did not change the heparin binding properties of FGF2. Buffer exchange
was performed on the Texas Red labeled-FGF2 (TR-FGF2) solution by centrifugation as above.
SDS-PAGE indicated that the molecular weight of TR-FGF2 is not significantly different from
that of FGF2. Fluorescence intensity was calibrated to protein concentration prior to delivery
using microplate fluorometry (Fluoroskan).
2.2.3 Size Exclusion Column Chromatography
Size exclusion analysis of FGF2 alone, FGF2 complexed with sucrose octasulfate (FGF2SOS), unfractionated heparin (FGF2-UFH, Sigma-Aldrich) or low molecular weight heparin
(FGF2-LMWH, Sigma-Aldrich) was performed by injecting 1 mg of the complexes in PBS into
a Superose 12 10/300GL column (GE Healthcare) on a FLPC system (Pharmacia Biotech). The
molar ratios of FGF2 to SOS, UFH and LMWH were each 1:100 to ensure all FGF2 molecules
are complexed before loading on to the column.
Soybean trypsin inhibitor (20.1 kDa),
ovalbumin (42.7 kDa), f3-galactosidase (112 kDa) and bovine serum albumin (65 kDa) (SigmaAldrich) were used as gel filtration molecular weight standards. 5 mg of the standards were
injected into the column for the chromatographic analysis.
2.2.4 Measurements of Diffusivity
In the absence of blood flow, drug transport in the myocardium is dominated by
diffusion. The effective diffusivity can be estimated by curve fitting drug spatial concentration
profile to the solution of the diffusion equation derived at similar conditions. The most
straightforward approach is to employ the solution of the diffusion equation for semi-infinite
boundary conditions C(x=O) = Csource and C(x=oo)=0
C/C =erfe
[Eq. El]
Experimentally, drugs were delivered to myocardium according to the methods described in "Exvivo Myocardial Drug Delivery without Perfusion", imaged and processed according to
"Fluorescence imaging and processing" section. Concentration profiles were obtained by
averaging multiple drug profiles using an automatic Matlab code (Appendix). Curve fitting was
then done on the mean concentration profile with GraphPad Prizm software.
2.2.5 Ex-vivo Myocardial Drug Delivery with and without Perfusion
N* Diffusion and permeation
-- Convection
Perfusate
(95%02 / 5%CO 2, T=37 0C)
FIGURE 2: Isolated perfused heart apparatus. Rat coronary arteries were perfused
antegrade through an aortic canula at constant physiologic mean pressure while a
constant, well mixed drug source was applied to the epicardial surface. Spatial
drug distribution was quantified in myocardial tissue regions exposed to drug.
High magnification schematic illustrates the examined physiologic forces: drug
diffusion within tissue and clearance through convection by intravascular flow
after permeation across capillary wall.
Sprague Dawley rats (0.5-0.6 kg) were anesthetized with 35 mg/kg ketamine and 5 mg/kg
xylazine, and anticoagulated with 1000 U subcutaneous heparin prior to CO 2 euthanasia. The
aorta was cannulated and heart retrograde perfused with cardioplegia (Osmolality = 289
mOsm/kgH 20 + 5%) composed of Krebs-Henseleit buffer (Sigma-Aldrich) with high potassium
(30 mmol/L KC1) and 4 % BSA (Sigma-Aldrich) to establish diastolic arrest. The heart was
excised and perfused at 95 mmHg. Coronary flow was monitored periodically and ranged 8-10
ml/minutes throughout experiment. The perfusate was oxygenated by a foam bubble oxygenator
with 95 % 02 / 5 % CO 2 at 37oC (Fig. 2). Samples were also examined in the absence of
coronary perfusion to eliminate other effects. Here the aorta was cannulated and flushed with
perfusate. As blood cleared from the circulation, coronary outflow from coronary sinus was
stopped by clamping the right atrium and pulmonary artery ensuring myocardial capillaries
patency and that the only difference between the control and perfused cases was coronary
perfusion. The entire configuration resided within an enclosed box with 100 % humidity. We
ascertained myocardial viability at 6 h by quantitatively documenting no additional tissue edema
on H&E stained sections. Experimental protocols were in accordance with NIH guidelines for
the humane care and use of laboratory animals and MIT committee on animal care.
Texas Red-FGF2 (TR-FGF2, 17 kDa, 5.88x 10-2 mmol/L) and Texas Red labeled FGF2
conjugated to SOS complex (TR-(FGF2) 2-SOS complex, -35 kDa, 2.86x 102 mmol/L) were
delivered to the rat myocardium from a drug-releasing chamber affixed to the anterior epicardial
surface by a cyanoacrylate based surgical adhesive (Glustitch). The heart was placed on a shaker
at 100 RPM to ensure a well mixed epicardial drug source. A core of myocardial tissue in contact
with and immediately adjacent to the drug source was harvested 6 h later using an 8 mmdiameter biopsy punch (Miltex). Tissue cores were cryo-sectioned (Leica CM1850)
perpendicular to the epicardium for quantitative epifluorescence imaging (Leica DMRA2
microscope, Hamamatsu C4742-95 camera, MetaMorph software, Texas Red filter set). Since
the fluorescent intensity of TR-FGF2 is linearly proportional to fluorophore 19, total drug
deposition in the absence (Mdg. ) or the presence (Mdfclear) of coronary perfusion were
calculated by summing fluorescence intensities in the spatial distributions. Percent clearance of
drug from coronary perfusion is
%clearance = 100 x (1 - M dff-clear / Mdff).
[Eq. E2]
2.2.6 Fluorescence imaging and processing
Tissue samples were snap-frozen with liquid nitrogen, mounted onto a cryotome and
sectioned into 10 um slides (Leica CM1850). Drug distribution was imaged with a fluorescence
microscope (Leica DMRA2, Metamorph software). The images were analyzed with MATLAB
(Mathworks) to quantify spatial drug concentration profiles. Tissue autofluorescence at the
excitation and emission wavelengths of TR-FGF2 (560nm excitation / 645nm emission) is
minimal and readily compensated for by subtracting background fluorescence obtained by
imaging myocardium incubated in PBS from the sample fluorescence signal.
2.2.7 Measurement of FGF in Outflow
We verified that capillary washout of FGF through microvascular clearance was indeed
35
responsible for the reduction in FGF penetration in the presence of perfusion with S-FGF1. Rat
hearts were isolated and perfused using identical procedures and experimental parameters
described in the "Ex-vivo Myocardial Drug Delivery" methods section for perfused hearts. 35SFGF1 (4.2 mg/ml) was applied to the epicardial surface (n=3) for 3 hours. The perfusate in these
experiments was not re-circulated, hence presence of 35 S-FGF1 in the outflow results from direct
washout of exogenous growth fact in tissue. Outflow perfusate was collected in 6-30m fractions.
At the end of perfusion experiments, 3ml samples of the outflow fractions were decolorized with
0.5ml hydrogen peroxide at 60 0 C for 1 hour (30%, Sigma-Aldrich), and assayed for 35S
radioactivity using liquid scintillation counter (Packard).
2.2.8 Continuum Pharmacokinetic Model of Myocardial Drug Transport With and
Without Perfusion
Following Tzafriri et. al.20 we model interstitial drug transport in a perfused tissue using
the classical diffusion equation with a linear sink term
aC
D
8 2C
= -kC
(M1)
ax 2
at
where the apparent clearance rate constant k is proportional to trans-endothelial permeability as
k-
MvSmv
(1- Omy)
(M2)
Here Smv is the surface fraction of capillaries and m,,is the capillary volume fraction. Since the
surface fraction of a cylinder of radius Rmv is related to the volume fraction as S,, = 2 mv / R.,
we can rewrite the proportionality between the apparent clearance rate constant and transendothelial permeability as
k =R 2
Rmv
Pmvm
1- mv
(M3)
A rich literature exists on the analysis of Eq. Ml. For our purposes, it suffices to note that
localization of the experimental growth factor profiles close to the drug source justifies the
analysis of distribution profiles in terms of penetration into a semi-infinite domain
21. Namely,
we assume that the concentration of growth factor at the far end of the tissue is negligible
C=O, x=L.
(M4)
With this in mind, under the conditions of a constant surface concentration
C=CO,
x=O
(M5)
the concentration profile takes the form 21
C/Co=-e-x erfc
x
-
e r-x x/+
.
(M6)
where
£=
(M7)
k
Thus, clearance gives rise to a length scale £ that is independent of the dimensions of the
tissue and is inversely related to the clearance rate constant. Correspondingly, using Danckwert's
method 21 it is possible to show that net tissue deposition M depends on time as
M = C0 erf(i-t) .
(M8)
Thus, k-' operates as the time scale for the tissue to approach its steady state deposition
(M9)
M = Cog
and distribution
C = Coe -x /i.
(M10)
Hence, increasing the clearance rate constant results in less drug penetration and more significant
localization near the drug source. On the contrary, as the clearance rate constant tends to zero,
the limitation on drug penetration is lifted (£ >> L ) such that drug penetration and deposition
reduce to the classical linear diffusion limits
C/Co
erfcx
2, D-
(Ml1)
and
M - 2Co -Dt/.
(M12)
The preceding analysis wherein the surface concentration was held constant provides
insights on drug transport during the initial burst release phase. Subsequently drug release from
the polymer device occurs at an essentially constant rate. Consider next the extreme limit
wherein the flux Fo rather than the concentration is held constant at the surface
-D
aC= F o
ax
,
x=O
(M13)
The steady state distribution of drug implied by Eq. Ml is then
C = (Fo / D)e - x"~.
(M14)
Thus , in the face of first order clearance, steady state drug distribution is always
exponential with a length scale £; device release kinetics is seen to only impact the steady state
concentration of drug at the device:tissue interface (x=0). Integrating the steady state distribution
profile Eq. M14 over the entire tissue we find that steady state tissue deposition M scales linearly
with flux and inversely with the apparent clearance rate constant
M=
k
(M15)
Using the Danckwert's method 21, it is possible to derive the time dependent counterpart of Eq
M15, as
M = F (1 - e-k'),
K
(M16)
thus confirming that k-1 also operates as the time scale for the attainment of steady state tissue
deposition when drug is released at a constant flux from the polymeric device. The main model
equations are summarized in Table 1 below.
D
Eq. 1
k-
Eq. 2
2P
". I)1-I .
Eq. 3
er
C iCo %fc,
Eq. 4
C=
Eq. 5
= -kC
- =.
DCe
%clearance =100 x 1- (erf(k)]
TABLE 1: Continuum Pharmacokinetic Model Equations for Epicardial Drug Delivery.
Detailed derivations are included in Supplemental Methods. Eq. 1 describes the transport of
drug in the presence of capillary clearance. C represents drug concentration in the tissue as a
function of time t, distance from the epicardium x, diffusivity D and apparent clearance
constant k. Eq. 2 relates the apparent clearance constant k to capillary permeability Pmv,
capillary volume fraction qmy and capillary diameter Rmv. Eq. 3 describes tissue concentration
profile normalized to source concentration Co in the absence of capillary perfusion as a
function of time and effective diffusivity. Eq. 4 shows the steady state tissue concentration in
the presence of capillary perfusion, where -(is drug penetration depth. Eq. 5 shows the
percent drug clearance by capillary perfusion as a function of k and D.
2.2.9 Analytical Model Calculation of Cumulative FGF Clearance
Cumulative FGF washout through microvascular clearance, between times tl and t2 can
be calculated from the experimental value of clearance constant k and the total deposition M
(Eqn. M8) by the following relationship:
CL = kMdt = JkColerf(k/t
tl
(M17)
tl
2.2.10 Statistical analysis
All data were presented as means ± s.e.m., except values for the clearance rate constants
k which were reported as means ± propagated standard errors. Propagated errors sk were
calculated using the formula( -)2
k
= (sD)2
D
+ 2(sx9 ) 2 , where s D and sx9 are standard errors for
X90
effective diffusivity D and penetration depth x 90 , respectively. Statistical analyses were
performed with the Student's t test where appropriate. P<0.05 (two-tailed) was considered
statistically significant. Non-linear regression was performed using GraphPad software (Prism 5)
to fit steady state spatial drug distributions to Eqs. M6 and M11 in obtaining values for clearance
rate constant k and effective diffusivity D, respectively.
2.3 Results
2.3.1 FGF Diffusivity in the Absence of Myocardial Perfusion
In the absence of coronary perfusion,
2500
SDATA
-Cxerfc(x/sqrt(4xDeffxt))
concentration profiles of FGF2 fit well to the2000
-
solution of the diffusion equation for semi-
Coxerfc(xlsqrt(4x10xDeffxt))
Coxerfc(x/sqrt(4x0.1xDeffxt))
1500
2 1000
infinite boundary conditions (Fig.3). To
U-
validate the consistency of our experimental
500
0
method, the experiments were carried out at
50
0
100
150
200
Distance from epicardium
two different time points 4hr (Fig.3A) and
96hr (Fig.3B). Effective diffusivity of FGF2
FIGURE 3: FGF2 Diffusivity in excised
myocardial tissue performed at 4hr
2 S-1
smfor
in myocardium was 0.021 + 0.001
2
TR-FGF2 when measured at 4hr, agrees with the value of 0.018 + 0.001 gm S-' when measured
at 96hr, suggesting that the transport of FGF2 in myocardium within these time points is
primarily diffusion mediated transport, and that the tissue transport properties were not
significantly altered up to 96 hr at 40 C. We further quantified effective diffusivity of similar
molecular weight dextrans and dextrans sulfate using the same method. Effective diffusivities of
2 -1
2
10kD, 20kD dextrans and 8kD dextran sulfate were 10.24 + 2.72 pm s', 1.35 ± 0.063 gm S ,
and 7.88 ± 1.37
[m2s
- 1,
respectively. Larger molecular weight accounts for slower transport of
20kD dextrans when compared to 10kD dextrans, and negative charge accounts for slower
transport of dextran sulfate, consistent with transport studies in arterial tissuelo. The further drop
in effective diffusivity of FGF2 is likely due to the effect of tissue binding. Using 10kD dextrans
as a reference, the impedance a =
Bm
Kd
+ 1 was 512, or
B
mx
Kd
=
511.
2.3.2 FGF Distribution is Limited by Myocardial Perfusion
Drug transport through and deposition within tissues are governed by molecular weightdependent processes such as diffusion and convection, and physicochemical attributes such as
binding, partitioning, and
metabolism
2' 22' 23. We
2500
examined the effects of
capillary perfusion on
myocardial growth factor
2000
a
1500
21000
0 0
500
transport in rat hearts
incubated at constant
0
30
90
60
Distance from Epicardium (im)
120
epicardial source
concentrations (Fig. 2) with
and without controlled
coronary flow. When
delivered to the ex-vivo
FIGURE 4: Myocardial Capillary perfusion Impedes
Drug Penetration. Distribution and representative
fluorescence microscopy images of TR-FGF2 in rat
myocardium with (magenta) and without coronary
perfusion (blue). Data represent mean ± s.e.m. (n=3).
Penetration depth (x90) is estimated as the location of the
90 % drop-off from the threshold (vertical dashed lines).
Error bars were only shown at regular intervals.
myocardium in the absence of
flow, TR-FGF2 distributed via diffusion to a penetration depth of 66 tm in 6 h (Fig. 4).
Restoration of coronary perfusion reduced TR-FGF2 penetration depth more than 2-fold to 28
tm, localizing growth factor closer to the epicardial drug source (Fig. 4).
2.3.3 FGF is Washed-out Through Microvascular Clearance Followed Ex-vivo Myocardial
Delivery
We further used a highly
10000
sensitive radioactive FGF (35S-FGFl)
S 1000
to verify that capillary washout of
C
0
FGF through microvascular clearance
was indeed responsible for the
100
n
10
reduction in FGF penetration in the
1
0
presence of perfusion.
3 5S-FGF1
was
observed in the perfusate at the
outflow soon after 35S-FGF1 was
delivered at epicardial surface (Fig. 5),
suggesting that capillary washout was
0.5
1
1.5
2
2.5
3
3.5
Time (hr)
FIGURE 5: FGF is Washed-out Through
Microvascular Clearance Followed Ex-vivo
Myocardial Delivery. 35 S-FGF1 in the outflow
perfusate was measured as a function of time after
local epicardial 35 S-FGF1 delivery (n=3).
Experimental washout of 35S-FGF-1 (in blue) is
well explained by Eq. S 17 (magenta line) using
the parameter values of TR-FGF2.
indeed responsible for the limited
penetration of this growth factor in the presence of perfusion (Fig. 4). These results were further
compared to analytical model results of cumulative drug clearance (Eqn M17) calculated using
pharmacokinetic parameters of FGF-2 (k = 1.15 + 0.06x 10-4 s-land D=0.02 jm 2/s) derived from
experiments. The experimental results fit the model well within one order of magnitude,
suggesting that the pharmacokinetics of 35 S-FGF 1 are well explained by our diffusion with
clearance model and moreover that the clearance constants and diffusivities of 35S-FGF1 and
TR-FGF2 are similar.
2.3.4 SOS limits the effects of capillary washout on FGF2
FGF2 is customarily delivered in association with unfractionated heparin (UFH) to
24 26
protect the growth factor from premature proteolysis - . Given the importance of molecular
weight in determining capillary washout and tissue penetration, we characterized the relative
effective molecular size of FGF2 when delivered alone and in association with UFH, low
molecular weight heparin (LMWH), or SOS. The average molecular size of FGF2 is largest
when complexed with UFH and LMWH (Fig. 6). Both FGF2-UFH and FGF2-LMWH span a
large range of molecular size, reflecting different degrees of FGF2 multimerization and the
intrinsic distribution of
0.04
113kD
molecular weights of
FGF+UFH
0.03
65kD
42.7kD
heparin. Interestingly,
> 002
FGF2+SOS
FGF2
I
FGF2-SOS exhibits an
apparent molecular size
ooo
7
larger than would be
expected from a simple
addition of the respective
H
FGF+L
0.01o
8
9
10
11
12
13
14
15
16
17
Fraction number
FIGURE 6: Size exclusion chromatography of FGF2 alone,
FGF2 complexed with SOS, FGF2 complexed with low
molecular weight heparin (LMWH) and FGF2 complexed
with unfractionated heparin (UFH). Molecular weight
markers where indicated.
molecular weights of the
component molecules. This observation is supported by the work of Herr et al. in which they
proposed that SOS induced reversible FGF2 dimerization27
We delivered TR-FGF2-SOS via a pericardial reservoir to perfused and non-perfused rat
myocardial tissue similarly to the delivery of TR-FGF2 and determined the fluorescence
distribution of the drug in tissue. Unlike TR-FGF2, TR-FGF2-SOS appeared to be significantly
less sensitive to capillary washout, so that the distributions of TR-FGF2-SOS both with and
without coronary flow are nearly
Texas red-FGF2-SOS dimer
identical (Fig. 7). Therefore, while the
2500
( 2000
larger size of TR-FGF2-SOS results in
lower bulk diffusivity, decreased
8 1500
8 1000
i 500
M
sensitivity to capillary washout as a
0
0
30
60
90
120
Distance from epicardium (( m)
result of lower trans-endothelial
permeability may actually lead to a net
tissue drug
increased tissue
drug uptake
uptake and
and
penetration in a system with capillary
perfusion.
FIGURE 7: Distribution and representative
fluorescence microscopy images of TR-(FGF2) 2 SOS in rat myocardium with coronary perfusion
(magenta) and without coronary perfusion (blue).
Data represent mean + s.e.m. (n=3).
2.3.5 Effects of Molecular Weight on Myocardial Transport Under Perfusion
We further examined the effects of capillary perfusion on myocardial drug transport of
model drug compounds of a range of molecular weights (1 kDa Evans Blue Dye, 10 kDa
Dextran, 8 kDa
14
14C-
C-Dextran sulfate, 17 kDa FGF2, 35 kDa FGF2-SOS, and 65 kDa 125I1
Albumin). For all these drugs, there was less myocardial deposition after 6 hours in the presence
of coronary flow compared to no coronary flow (Figs. 8A-F). The reduction in deposited drug
with coronary perfusion, computed by normalizing perfused to non-perfused drug deposition,
was inversely proportional to molecular weight: 96.3% for Evans Blue Dye (EBD), 91.8% for
14 C-Dextran
(14C-Dx), 84.5% for 14 C-Dextran sulfate (14C-DxS) and 53.2% for FGF2. Coronary
perfusion did not reduce deposition of FGF2-SOS or
125I-Albumin
to a statistically significant
degree. The sigmoidal relationship between perfusion-related drug reduction and drug molecular
weight appears to have an inflection point at a molecular weight of about 20 kDa (Fig. 8G).
1.5
-
A
D
1.5
1.0
1.0
0.5
0.5
0.0
0o.o
Flow
No Flow
o
1.5
B
0
1.5
0.5
0.5
a)
N
0.0
No FLow
Flow
No Flow
Flow
-E
0.0
Flow
No Flow
1.5
1.5
0 1.0
1.0
0.5
0.5
0.0
0.0
1000. EBD
8W% -
Flow
No Flow
Flow
No Flow
1kD
* Dextran 10OkD
extran Sulfate 8kD
FGF2 7kD
FGF2-SOS 35kD
20%
G
0
10
20
Albumin 65kD
30
40
50
60
70
Molecular Wght (kD)
FIGURE 8: Total drug deposition in rat myocardium following pericardial delivery
over 6 hours with and without coronary perfusion, normalized to the no-perfusion
case. (A) Evan's Blue Dye in PBS, (B) 8 kDa Dextran sulfate, (C) 10 kDa
Dextran, (D) FGF2, (E) FGF2-SOS, and (F) Albumin. (G) Percentage of deposited
drug cleared by capillary flow as a function of drug molecular weight displays a
sigmoidal pattern. * denotes statistical significance (p < 0.05).
2.3.6 Drug Diffusivity, Trans-endothelial Permeability and Vessel Density Influence Local
Drug Distribution and Deposition
We examined the impact of coronary
1000
100
flow on drug penetration within the context
0
of a continuum pharmacokinetics model of
.
1
10
drug diffusion in the face of microvascular
,
,
,
Diffusivity (mlis
2
)
S1000
clearance (Eq. 1, Table 1). In the absence of
100
V
perfusion the growth factor distribution
0
curve mimics the analytical solution of the
1.E-05 1.E-04
1.E-03
1.E-02
1.E-01
Permeability (Tlmls)
diffusion equation (Eq. 3, Table 1) with an
- 1000
0
apparent diffusivity of 0.021 ± 0.001 [im 2s-1
=
for TR-FGF2. This value is four orders of
0.
100
10
0.01%
magnitude smaller than the reported
diffusivity of FGF in free aqueous solution 28,
reflecting the impact of steric hindrance and
binding within tissues. TR is small (600 Da)
and hydrophilic. Its diffusion is significantly
higher than FGF in HSPG-rich myocardium
and detected fluorescence is likely specific
for TR-FGF-2. In the presence of coronary
perfusion, the capacity of capillaries to clear
drugs is restored and the distribution of TR-
0.10%
1.00%
10.00%
volume fraction
Capillary
FIGURE 9: Continuum Pbarmacokinetic
Model. Penetration depth x9o,defined as
distance from source to 90 % drop-off
threshold,x9o = x ln(O), where f is
calculated based on Eq. 4 (Table 1), is
expressed as a function of drug diffusivity
(A),trans-endothelial permeability (B),and
capillary volume fraction (C). Parameter
values cover a range of two orders of
magnitude below to above those ofFGF2 in
the heart. FGF2 diffusivity = 0.02 gm2s1 and
clearance constants k were empirically
verified, and trans-endothelial permeability
derived from Eq. 2 (Table 1). Capillary
volume fraction (,,,,) was varied over 3 log
orders between the extremes of ischemic and
normal tissue vascularity. These
relationships are linear in log-log scale axes,
demonstrating adherence to power law
functions.
FGF2 at 6 h approaches an
exponential steady state profile
100%
.~
75%
consistent with an apparent
50%
clearance rate constant k = 1.15
25%
*
TR-FGF2
" TR-FGF2-SOS
- 4 -1
± 0.06x10 S
(Eq. 4, Table 1).
Given that normal myocardial
capillary density is- 12.9 % 29
and FGF2 aqueous diffusivity
(2.2x 102 m2S-1) 28, our estimate
of the clearance rate constant of
FGF2 implies that trans-
0%
1.E-08 1.E-07
.
1.E-06
1.E-05 1.E-04 1.E-03
1.E-02 1.E-01 1.E+00
k (s "')
FIGURE 10: FGF Distribution is Sensitive to
Alteration in Drug Clearance. Percent drug cleared
by capillaries calculated using the analytical model
(Eq. 5, Table 1) as a function of clearance rate
constant k (black line). Experimental data points for
TR-FGF2 and TR-(FGF2) 2 -SOS analyzed by Eq. Ml
(Methods) are superimposed (magenta squares) on
model predictions providing perspective on the
sensitivity of FGF to manipulation of its clearance
constant.
endothelial permeability and the
3
permeability-to-diffusivity ratio are approximately 1.9x 10- pms-', and 8.8x 10-6 tm-'. This
estimate is in line with the trans-endothelial permeability of a molecule with a molecular size of
FGF2 30
Analytic models of drug transport and loss to capillary flow were evaluated across a
range of diffusivities, trans-endothelial permeabilities, and microvascular volume fractions.
Steady state results (Eq. M7) were used as equilibrium is rapidly achieved. Penetration depth at
steady state increases as the square root of the diffusion coefficient (Fig. 9A), and decreases as
the square root of the trans-endothelial permeability constant (Fig. 9B). It is worth contrasting
our results with those from systemic drug delivery through an intravascular route, where a
diametrically opposite relationship exists between tissue penetration and trans-endothelial
permeability. Intravascular drugs can only access target tissues by crossing the trans-endothelial
barrier. Increasing transvascular penetration in systemic delivery requires drugs that permeate
across the endothelium and interventions that increase, rather than decrease, vascular
permeability 31 33. Tissues with higher degrees of vascularization, as embodied by the vascular
volume fraction, clear drugs faster and have lower steady state drug penetration (Fig. 9C). Thus,
steady state drug penetration and distribution are highly dependent on drug diffusivity through
tissue and net microvascular clearance, the compounded effect of trans-endothelial permeability
and microvascular volume fraction (Eq. 2, Table 1).
The theoretical reduction in total deposition due to capillary clearance was calculated
(Eq. 5, Table 1) and expressed as a function of the clearance rate constant k (Eqs. M8 and M12).
Percent clearance of drug with coronary perfusion is most sensitive for clearance rate constants
1x 10-5 to 1x 10-2 S-1 (Fig. 10). Notably, our measurement of the clearance rate constant of TRFGF2 falls within this range, suggesting that FGF clearance is highly sensitive to transendothelial permeability and microvascular volume fraction.
To examine whether the clearance rate constant of FGF might be modulated by altering
its physicochemical properties, we used quantitative fluorescence imaging and mathematical
modeling to further contrast the distribution of TR-FGF2 alone or in association with sucroseoctasulfate (SOS). SOS induces FGF dimerization and increases the effective molecular weight
of TR-FGF2
27.
The increase in size was confirmed by size-exclusion chromatography (Fig. 6),
and should reduce trans-endothelial permeability, capillary washout, and effective diffusivity.
Indeed, in the absence of coronary perfusion, TR-(FGF2) 2 -SOS penetrated 40 % less than TR-
FGF2 into the myocardium (40 um,with an effective diffusivity of 0.013 ± 0.001 ~m2S-1)
reflecting its increased size (Deff TR-FGF = 0.021 ± 0.001
, Fig. 4 vs. Fig.7). But the larger
m2 S-1
compound was also less affected by coronary perfusion, with penetration depth falling only 26 %
to 30 um and total deposition falling by only 12 % (Fig. 7). The muted sensitivity of TR(FGF2) 2-SOS to flow (Fig. 10) is consistent with the estimated clearance rate constant (k-4.37
0.33x10-5 s-1), model predictions, and our hypothesis that larger molecules enter capillaries less
readily and are less prone to clearance by coronary perfusion.
2.4 Discussion
The potential of angiogenic promoters of endothelial cell growth and neocapillary
formation is well established in cell and tissue culture models 34 ,35. Unfortunately, when
delivered to ischemic myocardium in human clinical trials, angiogenic growth factors have yet to
produce stable, sustained angiogenesis36' 37 . While there are undoubtedly biological factors
involved38 , our study suggests that fundamental physical barriers can also impair the realization
of sustained angiogenesis. Chief among these is capillary washout increasing clearance and
restricting penetration of angiogenic growth factors into myocardial tissue.
2.4.1 Capillaries limit drug penetration in a manner dependent on molecular weight
For all but the largest molecules, myocardial capillary networks promote drug washout.
Having entered the capillary lumen, drugs become subject to downstream convective forces far
in excess of trans-endothelial diffusive forces, so that rather than acting as conduits and fostering
deposition deeper in the myocardium, capillary flow actually limits drug penetration. Our data
show that the degree to which drug penetration is affected depends on the size of the compound.
1 kDa Evans Blue Dye, 8 kDa Dextran Sulfate, 10 kDa Dextran are all essentially entirely
washed out in the presence of coronary flow, whereas albumin and FGF2-SOS are relatively
unaffected. The relationship between capillary washout and molecular weight is sigmoidal,
suggesting an "on-off' mechanism, wherein molecules below a threshold (- 20 kDa) permeate
through pores within the endothelium (3.5 to 7 nm diameter
39, 40),
and molecules above the
threshold do not. The splay in the sigmoidal curve about the inflection point likely reflects the
range of sizes of trans-endothelial pores. Vasoactive drugs which affect capillary permeability
may affect both the actual threshold and the slope of the splay.
2.4.2 Ischemic and non-ischemic tissues present different barriers to transport
In normally vascularized myocardium, cardiac myocytes are arranged in a complicated
three-dimensional configuration, with more than 2000 capillaries per square mm
between two capillaries is only three times their diameter
17.
41.
The distance
As myocardium progresses to
ischemia and infarction, this density of vascularity declines markedly. Because capillaries act as
spatially distributed barriers to the transport of drug molecules, regions with denser functional
vascularity will clear drug more efficiently and rapidly create low drug zones.
Gradations in vascularity across the myocardium as a result of ischemic events therefore
have important consequences for angiogenic drug delivery. Since capillary flows in ischemic
and infarcted regions are substantially less than in normal tissue, our data predict that drug
penetration would be greater in ischemic and infarcted areas. Therefore, placing delivery
devices directly in the ischemic region should confer pharmacokinetic advantages of decreased
capillary washout. If placed in well-perfused regions, drug molecules may never reach ischemic
areas at sufficient levels. For instance, pericardial delivery of angiogenic growth factors to target
endocardial ischemic regions may prove to be futile since drugs will not easily cross the wellperfused epicardial region. Appropriate positioning of the drug source is therefore critical to
achieve adequate drug concentrations in target tissues.
2.4.3 Angiogenesis limits its own success
An intriguing implication of our data is that drug delivery for therapeutic angiogenesis
may ultimately be self-defeating. Since the ultimate purpose of angiogenic therapy is to induce
growth of collateral blood vessels, over time capillary density would increase at a rate of growth
dependent on the spatial angiogenic factor distribution. As angiogenic treatment proceeds,
neocapillaries would begin to increase drug washout, ultimately limiting the very angiogenic
process the treatment is trying to promote. This negative feedback could account for why
therapeutic angiogenesis has not been sustained in clinical trials. The full implications of a
treatment modality can ultimately be limited by its own effect merit detailed investigation, and is
the subject of studies in the subsequent chapters.
2.5 Summary
Complex pharmacokinetics drives the transport of angiogenic growth factors through
myocardium. Capillary networks impede drug uptake and penetration by increasing drug
elimination through washout. Trans-endothelial permeability and vessel density increase drug
washout in a similar manner. Drug transport in perfused myocardium can be adequately
explained by a diffusion-elimination model, and an empirically derived clearance rate constant
can be obtained and used to predict the drug's pharmacokinetic advantage. Careful drug selection
and device placement are critical to achieve adequate drug concentration in target tissue.
Protective groups, if carefully selected, act to curtail the effects of capillary washout. These
results further imply that even when angiogenic therapy achieves some degree of neocapillary
formation, they may in turn act as sinks for drug washout, ultimately reducing the effectiveness
of the growth factors.
2.6 References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
Lazarous DF, Shou M, Stiber JA, Dadhania DM, Thirumurti V, Hodge E, Unger EF.
Pharmacodynamics of basic fibroblast growth factor: route of administration determines
myocardial and systemic distribution. Cardiovasc Res. 1997; 36:78-85.
Hermans JJ, van Essen H, Struijker-Boudier HA, Johnson RM, Theeuwes F, Smits JF.
Pharmacokinetic advantage of intrapericardially applied substances in the rat. J
Pharmacol Exp Ther. 2002; 301:672-678.
Stoll HP, Carlson K, Keefer LK, Hrabie JA, March KL. Pharmacokinetics and
consistency of pericardial delivery directed to coronary arteries: direct comparison with
endoluminal delivery. Clin Cardiol. 1999; 22:110-16.
Daemen MJ, Smits JF, Thij ssen HH, Struyker-Boudier HA. Pharmacokinetic
considerations in target-organ directed drug delivery. Trends Pharmacol Sci. 1988; 9:138141.
Willerson JT, Igo SR, Yao SK, Ober JC, Macris MP, Ferguson JJ. Localized
administration of sodium nitroprusside enhances its protection against platelet
aggregation in stenosed and injured coronary arteries. Tex Heart Inst J. 1996; 23:1-8.
Waxman S, Moreno R, Rowe KA, Verrier RL. Persistent primary coronary dilation
induced by transatrial delivery of nitroglycerin into the pericardial space: a novel
approach for local cardiac drug delivery. J Am Coll Cardiol. 1999; 33:2073-2077.
Ayers GM, Rho TH, Ben-David J, Besch HR, Jr., Zipes DP. Amiodarone instilled into
the canine pericardial sac migrates transmurally to produce electrophysiologic effects and
suppress atrial fibrillation. J Cardiovasc Electrophysiol. 1996; 7:713-721.
Kohnoe S, Maehara Y, Takahashi I, Saito A, Okada Y, Sugimachi K. Intrapericardial
mitomycin C for the management of malignant pericardial effusion secondary to gastric
cancer: case report and review. Chemotherapy. 1994; 40:57-60.
Buselmeier TJ, Davin TD, Simmons RL, Najarian JS, Kjellstrand CM. Treatment of
intractable uremic pericardial effusion. Avoidance of pericardiectomy with local steroid
instillation. Jama. 1978; 240:1358-1359.
Elmalak O, Lovich MA, Edelman E. Correlation of transarterial transport of various
dextrans with their physicochemical properties. Biomaterials. 2000; 21:2263-2272.
Hwang CW, Edelman ER. Arterial ultrastructure influences transport of locally delivered
drugs. Circ Res. 2002; 90:826-832.
Hwang CW, Wu D, Edelman ER. Physiological transport forces govern drug distribution
for stent-based delivery. Circulation. 2001; 104:600-605.
Hwang CW, Wu D, Edelman ER. Impact of transport and drug properties on the local
pharmacology of drug-eluting stents. Int J Cardiovasc Intervent. 2003; 5:7-12.
Lovich MA, Edelman ER. Mechanisms of transmural heparin transport in the rat
abdominal aorta after local vascular delivery. Circ Res. 1995; 77:1143-1150.
Lovich MA, Philbrook M, Sawyer S, Weselcouch E, Edelman ER. Arterial heparin
deposition: role of diffusion, convection, and extravascular space. Am J Physiol. 1998;
275:H2236-2242.
Kassab GS, Fung YC. Topology and dimensions of pig coronary capillary network. Am J
Physiol. 1994; 267:H319-325.
Poole DC, Mathieu-Costello O. Analysis of capillary geometry in rat subepicardium and
subendocardium. Am J Physiol. 1990; 259:H204-210.
18.
19.
20.
21.
22.
23.
24.
25.
26.
27.
28.
29.
30.
31.
32.
33.
34.
Le KN, Massachusetts Institute of Technology. Dept. of Electrical Engineering and
Computer Science. Pharmacokineticsof local growth factor delivery in myocardial tissue
[Thesis S.M. --Massachusetts Institute of Technology Dept. of Electrical Engineering and
Computer Science 2002.]; 2002.
Lakowicz JR. Principlesoffluorescence spectroscopy. 3rd ed. New York: Springer;
2006.
Tzafriri AR, Lemer EI, Flashner-Barak M, Hinchcliffe M, Ratner E, Parnas H.
Mathematical modeling and optimization of drug delivery from intratumorally injected
microspheres. Clin Cancer Res. 2005; 11:826-834.
Crank J. The mathematics of diffusion. 2d ed. Oxford, [Eng]: Clarendon Press; 1979.
Edelman ER, Lovich M. Drug delivery models transported to a new level. Nat
Biotechnol. 1998; 16:136-137.
Baxter LT, Zhu H, Mackensen DG, Jain RK. Physiologically based pharmacokinetic
model for specific and nonspecific monoclonal antibodies and fragments in normal
tissues and human tumor xenografts in nude mice. Cancer Res. 1994; 54:1517-1528.
Hershey JC, Corcoran HA, Baskin EP, Gilberto DB, Mao X, Thomas KA, Cook JJ.
Enhanced hindlimb collateralization induced by acidic fibroblast growth factor is
dependent upon femoral artery extraction. Cardiovasc Res. 2003; 59:997-1005.
Laham RJ, Rezaee M, Post M, Novicki D, Sellke FW, Pearlman JD, Simons M, Hung D.
Intrapericardial delivery of fibroblast growth factor-2 induces neovascularization in a
porcine model of chronic myocardial ischemia. J Pharmacol Exp Ther. 2000; 292:795802.
von Degenfeld G, Raake P, Kupatt C, Lebherz C, Hinkel R, Gildehaus FJ, Munzing W,
Kranz A, Waltenberger J, Simoes M, Schwaiger M, Thein E, Boekstegers P. Selective
pressure-regulated retroinfusion of fibroblast growth factor-2 into the coronary vein
enhances regional myocardial blood flow and function in pigs with chronic myocardial
ischemia. J Am Coll Cardiol. 2003; 42:1120-1128.
Herr AB, Omitz DM, Sasisekharan R, Venkataraman G, Waksman G. Heparin-induced
self-association of fibroblast growth factor-2. Evidence for two oligomerization
processes. J Biol Chem. 1997; 272:16382-16389.
Filion RJ, Popel AS. A reaction-diffusion model of basic fibroblast growth factor
interactions with cell surface receptors. Ann Biomed Eng. 2004; 32:645-663.
Wacker CM, Bauer WR. Myocardial microcirculation in humans--new approaches using
MRI. Herz. 2003; 28:74-81.
Michel CC, Curry FE. Microvascular permeability. Physiol Rev. 1999; 79:703-761.
Dreher MR, Liu W, Michelich CR, Dewhirst MW, Yuan F, Chilkoti A. Tumor vascular
permeability, accumulation, and penetration of macromolecular drug carriers. J Natl
Cancer Inst. 2006; 98:335-344.
Lejeune FJ. Clinical use of TNF revisited: improving penetration of anti-cancer agents by
increasing vascular permeability. J Clin Invest. 2002; 110:433-435.
Siegal T, Zylber-Katz E. Strategies for increasing drug delivery to the brain: focus on
brain lymphoma. Clin Pharmacokinet. 2002; 41:171-186.
Dinbergs ID, Brown L, Edelman ER. Cellular response to transforming growth factorbetal and basic fibroblast growth factor depends on release kinetics and extracellular
matrix interactions. J Biol Chem. 1996; 271:29822-29829.
35.
36.
37.
38.
39.
40.
41.
42.
Nabel EG, Yang ZY, Plautz G, Forough R, Zhan X, Haudenschild CC, Maciag T, Nabel
GJ. Recombinant fibroblast growth factor-i promotes intimal hyperplasia and
angiogenesis in arteries in vivo. Nature. 1993; 362:844-846.
Henry TD, Annex BH, McKendall GR, Azrin MA, Lopez JJ, Giordano FJ, Shah PK,
Willerson JT, Benza RL, Berman DS, Gibson CM, Bajamonde A, Rundle AC, Fine J,
McCluskey ER. The VIVA trial: Vascular endothelial growth factor in Ischemia for
Vascular Angiogenesis. Circulation. 2003; 107:1359-1365.
Simons M, Annex BH, Laham RJ, Kleiman N, Henry T, Dauerman H, Udelson JE,
Gervino EV, Pike M, Whitehouse MJ, Moon T, Chronos NA. Pharmacological treatment
of coronary artery disease with recombinant fibroblast growth factor-2: double-blind,
randomized, controlled clinical trial. Circulation. 2002; 105:788-793.
Cao R, Brakenhielm E, Pawliuk R, Wariaro D, Post MJ, Wahlberg E, Leboulch P, Cao Y.
Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a
combination of PDGF-BB and FGF-2. Nat Med. 2003; 9:604-613.
Kellen MR, Bassingthwaighte JB. Transient transcapillary exchange of water driven by
osmotic forces in the heart. Am J Physiol Heart Circ Physiol. 2003; 285:H1317-1331.
Marcus ML, Chilian WM, Kanatsuka H, Dellsperger KC, Eastham CL, Lamping KG.
Understanding the coronary circulation through studies at the microvascular level.
Circulation. 1990; 82:1-7.
Stoker ME, Gerdes AM, May JF. Regional differences in capillary density and myocyte
size in the normal human heart. Anat Rec. 1982; 202:187-191.
Finsen AV, Woldbaek PR, Li J, Wu J, Lyberg T, Tonnessen T, Christensen G. Increased
syndecan expression following myocardial infarction indicates a role in cardiac
remodeling. Physiol Genomics. 2004; 16:301-308.
Chapter 3: Interdependence of Local Pharmacokinetics and
Pharmacodynamics
Abstract
The challenge of angiogenesis science is that stable, sustained vascular regeneration in
humans has not been realized despite promising preclinical findings. We hypothesized that the
challenges faced by angiogenic therapies reflect powerful self-regulation by dynamic alteration
of tissue characteristics. In Chapter 2, through ex-vivo and mathematicalmodels we showed that
FGF spatial loading was significantly reduced with intact coronary perfusion, and that
penetration and loading decreased with trans-endothelial permeability and higher vascularity.
Induction of neocapillaries as the goal of angiogenic therapy adds pharmacokinetic complexity
because it induces changes in both permeability and vascularity. In this chapter, through an invivo model of local growth factor delivery to ischemic rabbit heart, we showed that sustained
local FGF delivery in vivo produced a burst of neovascularization in ischemic myocardium but
was followed by drug washout and a five-fold decrease in FGF penetration depth. The very
efficacy of pro-angiogenic compounds enhances their clearance and abrogates their
pharmacologic benefit. This self-limiting property of angiogenesis may explain the failures of
promising pro-angiogenic therapies.
3.1 Introduction
Stimulation of neovascularization using angiogenic growth factors might reduce
myocardial infarct size and improve cardiac function', and peripheral tissue 2 perfusion. Yet,
impressive results in tissue culture and animal studies 3-7 have not been sustained in clinical
trials8
11 .
Intravascular delivery of angiogenic factors is convenient but challenged by the
requirements for high doses and long residence times 8 ' 10. Cell and gene injections might provide
a continuous source of growth factor, and intramyocardial or pericardial delivery have elevated
local tissue drug concentrations with lower systemic exposure in animal modelsl2. However, the
promise of symptomatic improvement and increased capillary density seen in early clinical trials
with intramyocardial injections of FGF2 after coronary artery bypass graftingl 3 has not endured
in larger clinical trials, and clinical outcomes in general with local growth factor delivery have
been mixed9' 14-18
Some have postulated that myocardial growth factor concentrations and/or drug residence
time were inadequate for sustained angiogenesis despite controlled release delivery 19 , and yet,
the local pharmacokinetic processes governing uptake and distribution of growth factors in
highly vascularized tissues such as myocardium remain undefined. It is possible that the reverse
is true and concentrations may be more than sufficient. In Chapter 2, we showed that coronary
perfusion impedes drug penetration by increasing drug clearance through microvascular
washout. In this Chapter, we hypothesized that local delivery can induce neocapillary growth but
in doing so changes the balance between drug delivery and microvascular drug clearance
favoring the latter, such that the very pharmacologic efficacy of these compounds limits their
biological effect. To test this hypothesis, we used sustain growth factor release technology and in
vivo ischemic heart model to quantify how drugs move within vascularized tissue, and how
neovascularization following delivery of angiogenic growth factors affects their
pharmacokinetics and efficacy. These studies are the first to track both drug distribution and
angiogenic response simultaneously upon local growth factor delivery, and strongly suggest that
angiogenesis is powerfully self-regulating as the capillaries induced by angiogenic drug therapy
may increase clearance rates limiting tissue levels of growth factor and subsequent angiogenesis
even with sustained delivery.
3.2 Materials and Methods
3.2.1 Recombinant S35-FGF1 Production
35S-FGF1
was chosen as a model
SELECTED FRACTIONS
S35-FGF1
/
for FGF in the in-vivo setting because
S- -
its high detection sensitivity allows for
0.75
NaCI]
Radioactivity
S0.75-
the possibility of tracking spatial drug
distribution in the setting of controlled
delivery of therapeutic doses. It also
UV Absorbance
o.s5
'
,
0.25-
0
.
10
30
.
50
.70
70
Elution Volume (mL)
presents a safer alternative to using 25I
labeled FGF2 in-vivo. Recombinant
human FGF1 was expressed in
Escherichiacoli strain BL21-pLysS
FIGURE 1: Recombinant S35-FGF1
production and purification. Elution
profiles of protein and radioactivity
following binding to heparin sepharose
column and application of NaCl gradient.
Eluted fractions selected for experiments are
shown in highlighted area.
transformed by plasmid, pET3c that
confers resistance to ampicillin and encodes FGF1 (obtained as a gift from the late Dr. Thomas
Maciag, Maine Medical Center, Portland, ME). Transfected bacteria stocks were added to LB
medium (MP Biomedicals) containing 100 tg/mL Carbenicillin and 35 pg/mL Chloramphenicol
(Sigma-Aldrich) and incubated with vigorous shaking at 250 RPM at 370 C overnight. Bacteria
culture was then diluted in antibiotics-free LB medium (1:40 v/v of bacteria/medium) and
incubated with vigorous shaking at 250 RPM and the optical density of the solution was
measured at 600 nm. When cell culture reached an optical density of 0.6-0.8 bacteria were
centrifuged and resuspended in DMEM medium deficient in L-cysteine and L-methionine
(Invitrogen) supplemented with 1 % L- glutamine and 7.15 mCi of 35S (Promix L-
[35S]Methionine and Cysteine, GE Healthcare Life Sciences) and buffered with 25 mM HEPES
(Invitrogen) and then induced with 0.4 mM IPTG for 3 h with shaking at 250 RPM at 370 C.
Cells were then collected by centrifugation at 8000 RPM for 10 m and kept frozen at -800 C.
Frozen cell pellets were resuspended in lmg/ml lysozyme in GET buffer (50 mM Tris, 10
mM EDTA, 100 mM glucose, pH 8.0), mixed well for 5 m and then homogenized (Polytron;
Kinematica) 5 times for 30 s each with break periods of 60-90 s at 40 C to prevent overheating
and denaturation of proteins. Cell lysate was collected by centrifugation at 9,000 RPM for 10 m
at 4°C.
35S-FGF1
was then purified using affinity chromatography with FPLC. Bacterial lysates
were loaded into 5 ml heparin sepharose column (HiTrap Heparin HP column, GE Healthcare
Life Sciences) and allowed to bind for 1 h at room temperature. The FPLC system was
programmed to wash the column with PBS and gradually increase NaCl concentration with a
linear gradient (0.15-2 M). Elutions of 1 mL were collected and assayed for protein
concentration (absorbance at 280 nm, FPLC System) and radioactivity (2500TR Liquid
Scintillation Analyzer, Packard). Elution peaks of protein concentration and radioactivity
coincided (Fig. 1). The 35S protein product came out of the heparin sepharose column at 1.4 M to
1.6 M NaC1, similar to FGFI, and indicating 35S was incorporated in FGF 1. These elution
fractions were collected and further purified for use in experiments.
35S-FGF1
solution was
desalted by centrifugation using centrifugal filter devices with a 10 kDa molecular weight cut-off
(Centricon, Millipore). The presence of FGF1 was confirmed at a 18 kDa band using SDS-PAGE
and protein quantification was carried out using BCA assay (Pierce). Bioactivity of FGF 1 was
confirmed in proliferation assays of bovine aortic endothelial cells. FGF1 was further purified
from any endotoxin contamination using endotoxin removing columns (Detoxi-Gel AffinitiPak
columns, Pierce), and the FGF1 purity was confirmed with limulus amebocyte lysate assay
(Pyrotell-T, Associates of Cape Cod Inc., MA). Purification was continued (typically 2-3 times)
until endotoxin concentration is below 0.01 EU/[tg FGF1.
3.2.2 Fabrication and Kinetics of Controlled Release Device
A slurry mixture of heparin-Sepharose beads/alginate solution was prepared by mixing
sterilized heparin-Sepharose microbeads (GE Healthcare) with filter-sterilized sodium alginate
(Sigma-Aldrich, 5 %), placed in a customized 20mm x 20mm x Imm glass mold, and incubated
overnight in filter-sterilized 10 % CaCl 2 . The heparin-Sepharose embedded sodium alginate
material is exposed to CaCl 2 through two open surfaces of the mold. The gel was further
incubated in the 10 % CaCl 2 for 24 h to allow thorough cross-linking of the polymer after being
taken out of the mold under UV light for sterilization. The hardened polymeric gel device was
then incubated in
35S-FGF
solution for 48 h prior to experiment to allow complete and uniform
loading of drug.
To characterize
35S-FGF 1 release
kinetics from the device, 8 mm diameter circular shape
devices were made from the 20 x 20 x 1 mm 3 polymeric slab using 8 mm biopsy punch (Miltex).
These circular devices were incubated in 1 ml PBS and gently agitated throughout the
experiment with a shaker. At various time points the elution mixture was collected and assayed
for 35S activity using liquid scintillation counter (Packard). Fresh PBS was used to renew the
elution buffer.
3.2.3 In-vivo Myocardial Drug Delivery
Rabbits (New Zealand White, 3-3.5 kg) received an intramuscular injection of 35 mg kg'
ketamine and 5 mg kg' of xylazine, and inhaled isoflurane anesthesia (1-3%) and positive
pressure ventilation via a 3.0 mm endotracheal tube. The chest was shaved and sterilely prepared
with Betadine and alcohol. A left thoracotomy was performed after local lidocaine injection. A
clamp kept the chest open and a small opening in the pericardium was created with care to
minimize pericardial damage. The left anterior descending coronary artery was ligated. Ischemia
was confirmed by ST segment elevation on simultaneous continuous electrocardiography (Fig.
2A). Sodium alginate polymeric devices sustain-releasing
35S-FGF1
from encapsulated heparin
Sepharose beads (Fig. 2B) were placed in the pericardial space (Fig. 2C) and the pericardiotomy
suture-repaired to prevent leakage. The thoracotomy and skin incision were closed. Positive endexpiratory pressure ventilation and a negative pressure chest tube prevented pneumothorax.
Analgesia was with 0.03 mg kg'-buprenorphine subcutaneous injections every 8 h for the first 72
h. Control animals received alginate encapsulated heparin Sepharose beads without FGF. Hearts
were harvested 2, 8, 16 and 31 days after surgery, the aorta cannulated, flushed retrogradely with
PBS, and snap-frozen in liquid nitrogen. Drug release devices were confirmed to be physically
intact and adhered to epicardium at up to 1 month (Fig. 2 D&E).
B
After LAD Coronar Li ation
D
MYO
FIGURE 2: In-vivo ischemic heart model of local myocardial delivery of FGF.
Ischemic heart model was induced by ligation of left anterior descending coronary arteries.
Evidence of ischemia was checked with EKG (A). Heparin sepharose microbeads
35
embedded in sodium alginate device was used to sustain release S -FGF1 (B). Pericardial
cradle was created to allow LAD ligation and placement of controlled release drug devices
(C). Devices were physically intact up to 1 month in-vivo (D). Cross section of rabbit heart
with zoomed in H&E stained micrograph showing the proximity of drug release device to
epicardium.
3.2.4 Quantification of in-vivo FGF1 and Blood Vessels Distribution
Two frozen myocardial cores were excised adjacent to the polymeric devices using an 8
mm diameter biopsy punch (Miltex). One core was mounted and cryosectioned (Leica CM1850)
into 100 gm sections parallel to the epicardium. Sections were digested in 1 ml of Solvable tissue
solubilizer (PerkinElmer) at 60 0 C overnight prior to radioactivity quantification (2500TR Liquid
Scintillation Analyzer, Packard). The discrete spatial FGF1 concentration data were fit to the
exponential profile implied by Eq. 4 (Table 1) using GraphPad software (Prism 5). The fit was
used to estimate the penetration depth x90 , defined as distance from source to 90 % drop-off
threshold, as x90 = g x ln(10). The other tissue core was cryo-sectioned into 10 ptm thick sections
in transmural direction. Sections were fixed for 5 m with 4 % paraformaldehyde (Electron
Microscopy Sciences), washed for 30 s with cold acetone (Sigma-Aldrich), incubated in blocking
serum (200ptl of 1 % chicken serum, 1 h, 37°C), then in goat anti-PECAM-1 IgG (Santa Cruz
Biotechnology, 200pl of 1:50 dilution, 2 h, 370 C), washed three times in 0.1 % Tween 20 in
PBS, incubated further with Alexa Fluor 488 chicken anti-goat IgG (Invitrogen, 200tl 1:200
dilution, 2 h, 370C), washed three times in Tween 20/PBS, cover-slip mounted, and imaged
immediately with a fluorescence microscope (Leica DMRA2, FITC filter set). The images were
thresholded to maximize the signal to noise ratio with Matlab (Mathworks, MA), yielding binary
images of vessel distribution. Neovascular formation of tissue regions within 500 itm from
epicardial source was quantified by computing the tissue area fraction stained by PECAM-1
(total number of pixels with PECAM-1 stain / total number of pixels of tissue area).
3.2.5 Statistical analysis
All data were presented as means + s.e.m., except values for the clearance rate constants
k which were reported as means + propagated standard errors. Statistical analyses were
performed with the Student's t test where appropriate. P<0.05 (two-tailed) was considered
statistically significant.
3.3 Results
3.3.1 Polymeric Devices Sustain Release FGF1 over 30 days in-vivo
S35-FGF1 can be released with heparin sepharose beads / sodium alginate devices over 30
days in-vitro (Fig. 3, dashed line), with the shape consistent with previous study
20.
The release
kinetics in-vivo was indirectly obtained from the amount of initial drug and drug remained in
release devices after each treatment period with the assumption that the burst release phase
similar to those in-vitro. This result also suggested that S35 -FGF1 was released at a steady rate
125
o In-vitro
-
* In-vivo
100 -
S.......................
00
*
Burst Release
0
0
5
10
15
20
25
30
Time (days)
FIGURE 3: Polymeric Devices Sustain Release FGF1 over 30
days. Percentage of cumulative 35S-FGF1 released into PBS buffer
in-vitro (white diamonds, data represent mean + s.e.m. (n= 10),
100% corresponds to approximately 90tg 35S-FGF1 per circular
disk of 8mm diameter and 1 mm thickness), and throughout in-vivo
experiment (black circles, data represent mean ± s.e.m. (n=3),
100% corresponds to approximately 450 gpg 35 S-FGF1 per device
(20mm x 20mm x Imm) for in-vivo experiments), calculated by %
drug released = (total drug within source - total drug remaining)/
total drug within source x 100 %.
in-vivo after the burst phase (Fig. 3, solid line).
3.3.2 In-vivo Angiogenic Response Limits Drug Distribution
Conventional pharmacokinetic models for drug distribution do not take into account the
potential that drugs can alter capillary density, trans-endothelial permeability or drug clearance.
Yet, angiogenic growth factors such as FGF1 and FGF2 are specifically administered to induce
capillary growth, and it would be unreasonable to assume that trans-endothelial permeability and
drug clearance are not similarly modified. Induced neovascularization implies an increase in the
density of blood capillaries that could provide negative feedback limiting growth factor tissue
penetration (Fig. 16C, Chapter 2). Our analysis of myocardial drug transport suggested that FGF
would be particularly sensitive to induced capillary washout (Figs. 9 and 17, Chapter 2). We
tested this hypothesis in vivo using radiolabeled FGF1 (35S-FGF1). TR-FGF2 could not be used
in vivo as its labeling intensity is much lower than that of 35S-FGF 1, rendering it virtually
transparent at the doses delivered.
Following the sustain-release of biologically active 35S-FGF1 fractions with heparin
Sepharose-alginate wafers, FGF1 successfully penetrated 442 + 91 pm into the myocardium over
the first two days after release initiation. Yet, despite sustained delivery, penetration regressed
over time falling 5-fold by day 8 (81 + 30 tm), and remained low through day 31 (Fig. 4B).
Enhanced growth factor clearance was associated with the induction of neovasculature (Fig 5A),
after controlled for any angiogenesis with devices without FGF1 (Fig. 5B). Two days after
device implantation the fraction of PECAM-1 stained tissue was 56 % greater in animals
receiving FGF1 (4.4 %) compared to baseline density (2.8 %) in control animals with identical
devices devoid of growth factor (P < 0.05, Fig. 6). Neovascularization peaked at day 8 (8.7 %)
doubled that from day 2 (P < 0.01, Fig. 6), coinciding with the drop in drug distribution.
Similarly, the fraction of PECAM- I1stained tissue decreased significantly from day 8 to day 31 (62 % P < 0.01, Fig. 6), most likely from regression of neocapillaries as the concentration of
FGF1 becomes sub-therapeutic. Drug delivery devices were examined for remaining drug
content after each treatment period to verify that the decreasing myocardial concentrations arose
from increasing capillary clearance rather than decreasing drug delivery. None of the delivery
devices were depleted of drug, and all continued to release drug with constant flux (Fig. 3)
following the expected burst release of-37.5 % during the first 6 h.
1.5x10
05
B
0o
E
Day 2
Day8
Penetration depth
C
1.0x10
05
S
C..
5.0x10
06
*
Day 31
0.0x10 -00
0
200
400
600
Distance from epicardium (
800
1000
pm)
FIGURE 4: FGF1 penetrates myocardium at day 2 but regressedat later time points.
Spatial profile of S3 -FGF 1 from epicardium was obtained by serial sectioning of
myocardial plug (A). S35 -FGF1 spatial concentration distribution at days 2, 8, and 31
following coronary ligation and implantation of sustained release source was quantified
using liquid scintillation counting of sectioned tissues. Data represent mean ± s.e.m. (n=3)
HS / Alginate with FGF-1
Day 2
Source
B
Day 8
Day 31
Pene ration depth
Control: HS /Alginate without FGF-1
Day 31
Day 8
Day 2
FIGURE 5: Representative fluorescent images of
PECAM-1 labeled blood vessels in tissue regions
adjacent to drug source for experimental animals
receiving heparin-Sepharose beads / alginate source
with S35-FGF1 and control animals receiving devices
without FGF1. Dashed red line on the right edge
denotes interface between source and epicardium.
Magenta, blue and green dashed lines represent the
penetration depth at 90 % drop-off threshold from
tissue/source interface calculated from spatial S35FGF1 distributions. Scale bars represent 100 pm.
0.10-
NS
<
L 0.08-**
0.06
-*- Control
FGF1
.
0.04-
2 0.02-
0
7
14
21
Time (d)
28
35
FIGURE 6: Vascular to tissue surface
fraction (calculated by normalizing total
number of pixels stained by PECAM-1 to
total tissue area within 500 im depth from
source) is expressed as a function of time.
Data points represent PECAM-1 stained
surface fraction of individual hearts (n=3),
and connecting lines denote trend of mean
value. * denotes P < 0.05. ** denotes P <
0.01 (P = 0.007 between days 2 and 8, and
P = 0.003 between days 8 and 31).
3.4 Discussion
While biological factors 2 1 might be responsible for unsuccessful realization of angiogenic
growth factors potential to induce stable sustained collaterals in clinical trials'
10
, our study
suggests a fundamental barrier in local drug delivery, in particular the self-limiting
pharmacokinetics of angiogenic therapy to impair the induction and maintenance of sustained
neovascularization.
The previous chapter revealed that drug trans-endothelial permeability plays a vital role
in governing drug distribution. Lower trans-endothelial permeability ensures greater myocardial
drug penetration following local application (Fig. 16B). The dependence of drug distribution on
trans-endothelial permeability and capillary density takes on further complexity for angiogenic
compounds that can remodel the tissue into which they are being delivered. Over the course of
treatment, vessel density in ischemic tissues increases in FGF -laden tissue regions (within 500600 p.m depth from epicardium, Fig 5A). Indeed, abundant neovascularization occurs from day 2
to 8, but drug washout rises as well precipitously dropping the local tissue concentration and
penetration depth of FGF 1 (Fig 4B), despite no quantifiable change in growth factor delivery.
FGF- 's instability in the absence of heparin 22 cannot account for the observed effects, as the
factor was released directly from the heparin Sepharose devices to the epicardial tissue (Fig. 2E).
Released FGF-1 likely binds reversibly to myocardial HSPGs, prolonging tissue half-life.
Indeed, angiogenic activity was observed 8 days after delivery (Fig 5A). Moreover, changes in
angiogenic action correlated with regression of FGF distribution, not a decrease in activity or
stability. Continuum pharmacokinetic model (Eq. M15, Chapter 2) suggest a 5-fold increase in
capillary washout between days 2-8. Such an increase in the FGF1 clearance could arise from an
increase in microvascular density and/or trans-endothelial permeability (Eq. 2, Table 1). The
observed 65 % rise in capillary density between days 2 and 8 (Fig. 6) indicates that the latter
plays a dominant role and suggests that the induced vasculature is immature and highly
permeable to FGF1.
Our findings in this chapter and in chapter 2, therefore, offer possibilities for engineering
drugs to penetrate tissue better by reducing their trans-endothelial permeability. FGF2 lies within
the region where drug penetration depth is highly sensitive to the clearance rate constant k (Fig.
17, Chapter 2) which is directly proportional to trans-endothelial permeability (Eq. 2, Table 2,
Chapter 2), whereas (FGF2) 2 -SOS with its 2.6 times lower clearance is less affected by flow.
More than 50 % of FGF2 is cleared by coronary perfusion, but only 12 % for (FGF2) 2-SOS (Fig.
9 vs. Fig. 14, Chapter 2). Therefore, one way to decrease permeability is to consider drugs of
higher molecular weight. While higher molecular weight implies lower myocardial drug
diffusivity, the ratio of permeability to diffusivity can drop two orders of magnitude as molecular
radius increases from 2.4 to 36 A
23.
A different method for modulating trans-endothelial
permeability can be modification of drug charge. Indeed, it has been shown that negatively
charged dextrans exhibit 10 times lower trans-endothelial permeability than neutral analogs 24.
This approach may present a method for lowering trans-endothelial permeability of a drug to
increase penetration depth and deposition.
These integrated studies (Chapter 2 and 3) suggested that angiogenesis is powerfully selfregulating as the very capillaries induced by angiogenic drug therapy may increase clearance as
well. The pharmacodynamic changes during the early angiogenic therapy can tip the
pharmacokinetics to conditions that are unfavorable for growth factor penetration, which in turn
affects long term therapeutic goals. This mechanism implies a natural upper limit effect for
pharmacologic revascularization which restricts angiogenic drug penetration and spatially
confines the sprouting of new vessels near the drug source. At day 31, the FGF 1 level in the 100500 jtm tissue region falls to undetectable levels, and significant regression of neovascularization
consequently occurs in the absence of local growth factor (Fig. 6, day 31). One might well
imagine that such forces are essential to endogenous regulation of tissue morphogenesis and
repair, and that loss of such regulation may help explain the growth of vascular tumors, and other
arterial-venous malformations and anomalies.
The interdependence of the pharmacokinetics and pharmacodynamics elucidated in this
study may explain the difficulty of realizing the clinical potential of angiogenic compounds and
suggests that efficacy becomes critically dependent on device placement and drug's transendothelial permeability. The quantitative framework presented here and in Chapter 2 may help
guide rational selection of angiogenic compounds based on a favorable physicochemical profile,
and drug delivery strategies that take advantage of the regulation between growth factor
pharmacokinetics and angiogenic pharmacodynamics. In Chapter 4, we will attempt to achieve
this goal through computational modeling building on the experimental results presented in
Chapter 2 and 3.
3.5 References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
Yanagisawa-Miwa A, Uchida Y, Nakamura F, Tomaru T, Kido H, Kamijo T, Sugimoto
T, Kaji K, Utsuyama M, Kurashima C. Salvage of infarcted myocardium by angiogenic
action of basic fibroblast growth factor. Science. 1992; 257:1401-1403.
Takeshita S, Pu LQ, Stein LA, Sniderman AD, Bunting S, Ferrara N, Isner JM, Symes
JF. Intramuscular administration of vascular endothelial growth factor induces dosedependent collateral artery augmentation in a rabbit model of chronic limb ischemia.
Circulation. 1994; 90:11228-234.
Harada K, Friedman M, Lopez JJ, Wang SY, Li J, Prasad PV, Pearlman JD, Edelman ER,
Sellke FW, Simons M. Vascular endothelial growth factor administration in chronic
myocardial ischemia. Am J Physiol. 1996; 270:H1791-1802.
Lopez JJ, Edelman ER, Stamler A, Hibberd MG, Prasad P, Thomas KA, DiSalvo J,
Caputo RP, Carrozza JP, Douglas PS, Sellke FW, Simons M. Angiogenic potential of
perivascularly delivered aFGF in a porcine model of chronic myocardial ischemia. Am J
Physiol. 1998; 274:H930-936.
Montesano R, Vassalli JD, Baird A, Guillemin R, Orci L. Basic fibroblast growth factor
induces angiogenesis in vitro. Proc Natl Acad Sci U S A. 1986; 83:7297-7301.
Unger EF, Banai S, Shou M, Lazarous DF, Jaklitsch MT, Scheinowitz M, Correa R,
Klingbeil C, Epstein SE. Basic fibroblast growth factor enhances myocardial collateral
flow in a canine model. Am J Physiol. 1994; 266:H1588-1595.
Watanabe E, Smith DM, Sun J, Smart FW, Delcarpio JB, Roberts TB, Van Meter CH, Jr.,
Claycomb WC. Effect of basic fibroblast growth factor on angiogenesis in the infarcted
porcine heart. Basic Res Cardiol. 1998; 93:30-37.
Simons M, Annex BH, Laham RJ, Kleiman N, Henry T, Dauerman H, Udelson JE,
Gervino EV, Pike M, Whitehouse MJ, Moon T, Chronos NA. Pharmacological treatment
of coronary artery disease with recombinant fibroblast growth factor-2: double-blind,
randomized, controlled clinical trial. Circulation. 2002; 105:788-793.
Rajagopalan S, Mohler ER, 3rd, Lederman RJ, Mendelsohn FO, Saucedo JF, Goldman
CK, Blebea J, Macko J, Kessler PD, Rasmussen HS, Annex BH. Regional angiogenesis
with vascular endothelial growth factor in peripheral arterial disease: a phase II
randomized, double-blind, controlled study of adenoviral delivery of vascular endothelial
growth factor 121 in patients with disabling intermittent claudication. Circulation. 2003;
108:1933-1938.
Henry TD, Annex BH, McKendall GR, Azrin MA, Lopez JJ, Giordano FJ, Shah PK,
Willerson JT, Benza RL, Berman DS, Gibson CM, Bajamonde A, Rundle AC, Fine J,
McCluskey ER. The VIVA trial: Vascular endothelial growth factor in Ischemia for
Vascular Angiogenesis. Circulation. 2003; 107:1359-1365.
Gyongyosi M, Khorsand A, Zamini S, Sperker W, Strehblow C, Kastrup J, Jorgensen E,
Hesse B, Tagil K, Botker HE, Ruzyllo W, Teresinska A, Dudek D, Hubalewska A, Ruck
A, Nielsen SS, Graf S, Mundigler G, Novak J, Sochor H, Maurer G, Glogar D, Sylven C.
NOGA-guided analysis of regional myocardial perfusion abnormalities treated with
intramyocardial injections of plasmid encoding vascular endothelial growth factor A-165
in patients with chronic myocardial ischemia: subanalysis of the EUROINJECT-ONE
multicenter double-blind randomized study. Circulation. 2005; 112:I157-165.
12.
13.
14.
15.
16.
17.
18.
19.
20.
21.
22.
23.
Lazarous DF, Shou M, Stiber JA, Dadhania DM, Thirumurti V, Hodge E, Unger EF.
Pharmacodynamics of basic fibroblast growth factor: route of administration determines
myocardial and systemic distribution. Cardiovasc Res. 1997; 36:78-85.
Laham RJ, Chronos NA, Pike M, Leimbach ME, Udelson JE, Pearlman JD, Pettigrew RI,
Whitehouse MJ, Yoshizawa C, Simons M. Intracoronary basic fibroblast growth factor
(FGF-2) in patients with severe ischemic heart disease: results of a phase I open-label
dose escalation study. J Am Coll Cardiol. 2000; 36:2132-2139.
Hedman M, Hartikainen J, Syvanne M, Stjernvall J, Hedman A, Kivela A, Vanninen E,
Mussalo H, Kauppila E, Simula S, Narvanen O, Rantala A, Peuhkurinen K, Nieminen
MS, Laakso M, Yla-Herttuala S. Safety and feasibility of catheter-based local
intracoronary vascular endothelial growth factor gene transfer in the prevention of
postangioplasty and in-stent restenosis and in the treatment of chronic myocardial
ischemia: phase II results of the Kuopio Angiogenesis Trial (KAT). Circulation. 2003;
107:2677-2683.
Lederman RJ, Mendelsohn FO, Anderson RD, Saucedo JF, Tenaglia AN, Hermiller JB,
Hillegass WB, Rocha-Singh K, Moon TE, Whitehouse MJ, Annex BH. Therapeutic
angiogenesis with recombinant fibroblast growth factor-2 for intermittent claudication
(the TRAFFIC study): a randomised trial. Lancet. 2002; 359:2053-2058.
Makinen K, Manninen H, Hedman M, Matsi P, Mussalo H, Alhava E, Yla-Herttuala S.
Increased vascularity detected by digital subtraction angiography after VEGF gene
transfer to human lower limb artery: a randomized, placebo-controlled, double-blinded
phase II study. Mol Ther. 2002; 6:127-133.
Stewart DJ, Hilton JD, Arnold JM, Gregoire J, Rivard A, Archer SL, Charbonneau F,
Cohen E, Curtis M, Buller CE, Mendelsohn FO, Dib N, Page P, Ducas J, Plante S,
Sullivan J, Macko J, Rasmussen C, Kessler PD, Rasmussen HS. Angiogenic gene therapy
in patients with nonrevascularizable ischemic heart disease: a phase 2 randomized,
controlled trial of AdVEGF(121) (AdVEGF121) versus maximum medical treatment.
Gene Ther. 2006; 13:1503-1511.
van Royen N, Schirmer SH, Atasever B, Behrens CY, Ubbink D, Buschmann EE,
Voskuil M, Bot P, Hoefer I, Schlingemann RO, Biemond BJ, Tijssen JG, Bode C,
Schaper W, Oskam J, Legemate DA, Piek JJ, Buschmann I. START Trial: a pilot study
on STimulation of ARTeriogenesis using subcutaneous application of granulocytemacrophage colony-stimulating factor as a new treatment for peripheral vascular disease.
Circulation. 2005; 112:1040-1046.
Gounis MJ, Spiga MG, Graham RM, Wilson A, Haliko S, Lieber BB, Wakhloo AK,
Webster KA. Angiogenesis is confined to the transient period of VEGF expression that
follows adenoviral gene delivery to ischemic muscle. Gene Ther. 2005; 12:762-771.
Edelman ER, Mathiowitz E, Langer R, Klagsbrun M. Controlled and modulated release
of basic fibroblast growth factor. Biomaterials. 1991; 12:619-626.
Cao R, Brakenhielm E, Pawliuk R, Wariaro D, Post MJ, Wahlberg E, Leboulch P, Cao Y.
Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a
combination of PDGF-BB and FGF-2. Nat Med. 2003; 9:604-613.
Rosengart TK, Kuperschmid JP, Maciag T, Clark RE. Pharmacokinetics and distribution
of heparin-binding growth factor I (endothelial cell growth factor) in the rat. Circ Res.
1989; 64:227-234.
Michel CC, Curry FE. Microvascular permeability. Physiol Rev. 1999; 79:703-761.
24.
25.
26.
27.
28.
29.
Elmalak O, Lovich MA, Edelman E. Correlation of transarterial transport of various
dextrans with their physicochemical properties. Biomaterials. 2000; 21:2263-2272.
Martini J, Honig CR. Direct measurement of intercapillary distance in beating rat heart in
situ under various conditions of O 2 supply. Microvasc Res. 1969; 1:244-256.
Rubio-Gayosso I, Platts SH, Duling BR. Reactive oxygen species mediate modification
of glycocalyx during ischemia-reperfusion injury. Am J Physiol Heart Circ Physiol.
2006; 290:H2247-2256.
McDonagh PF, Cohen DM, Suaudeau J, Laks H. The effects of myocardial ischemia
followed by reperfusion on perfused coronary capillarity. Microcirc Endothelium
Lymphatics. 1985; 2:67-84.
Van Kerckhoven R, van Veghel R, Saxena PR, Schoemaker RG. Pharmacological
therapy can increase capillary density in post-infarction remodeled rat hearts. Cardiovasc
Res. 2004; 61:620-629.
Xie Z, Gao M, Batra S, Koyama T. The capillarity of left ventricular tissue of rats
subjected to coronary artery occlusion. Cardiovasc Res. 1997; 33:671-676.
Chapter 4: Computational Modeling of Local Pharmacokinetics and
Pharmacodynamics of FGF in Myocardium
Abstract
Local delivery of angiogenic factors to ischemic tissues for vascular regenerative therapy
is a promising treatment for patients with small vessel disease and diffuse atherosclerotic lesions,
but this approach has not endured in long term clinical trials. Our experimental studies have
shown that capillaries act as sinks to clear drugs and that there is an inherent coupling of local
pharmacokinetics and pharmacodynamics in pro-angiogenic therapy. To derive a quantitative
framework to examine further the implications of these results, facilitate sensitivity analysis and
suggest ways to optimize angiogenic therapy, we have constructed a computational model that
couples the continuum pharmacokinetics of angiogenic growth factors with their induced
biological effects using experimentally derived parameters. The model accounts for FGF release
kinetics from controlled released source, diffusion within myocardial tissue, elimination of FGF
through permeation across capillaries, and angiogenic processes: sprouting, maturation and
regression. The model predicts that FGF transport in cardiac muscle can be significantly impeded
by capillary clearance, despite uniform FGF release. FGF distributions were dependent on FGF
diffusivity, trans-endothelial permeability, capillary density, and FGF release rate. FGF-induced
capillary sprouting further reduces penetration depth of FGF, increases FGF gradient, and elicits
regression of its super-therapeutic threshold wave front through microvascular washout. The
trans-endothelial permeability, drug diffusivity, baseline tissue vascularity, drug release rate and
biological potency determined the growth factor gradients and steady state distribution of
sprouted capillary distribution. Decreasing drug trans-endothelial permeability can potentially
result in a significant increase in sustained angiogenic response. This simplified mechanistic
model of angiogenic pharmacodynamics combined with local FGF tissue transport support
experimental results that angiogenic therapy is self-limited, provides a framework for the study
of local growth factor transport in dynamic tissue states, and offers insights into the design and
evaluation of therapeutic compounds and delivery approaches.
4.1 Introduction
Pharmacokinetic (PK) studies in local drug delivery typically assume that drug transport
occurs in a static tissue environment where the tissue is stable and unchanged, and do not
account for drug effects in transforming the tissue; in essence the pharmacodynamics (PD).
While this conventional approach might be valid for many drugs, it is questionable with regard to
angiogenic growth factors that specifically alter tissue ultra-structure drastically and can change
the way tissue handles drugs. Such action could have an indirect effect on the drug efficacy that
can be difficult to predict, and yet could have tremendous implications for local drug delivery.
Indeed, our in-vivo experiments (Chapter 3) showed that FGF1, an angiogenic growth factor,
when locally delivered to rabbit epicardial tissue increases the local drug clearance rates
significantly above baseline, and as a result limits the drug's spatial penetration and angiogenic
effect. Early drug action limits its long term effectiveness. These findings have important
implications for optimizing drug delivery not only because they suggested that one should look
at both PK and PD in evaluating drug studies but also pointed out limiting factors for drug
transport and offered possibility for optimization of system parameters. To effectively carry out
optimization studies, it is necessary to have a quantitative understanding of the system. In this
chapter, we sought to quantitatively characterize the angiogenic growth factor / myocardial tissue
PK-PD system using computational modeling. This approach provides a framework for
examining the isolated effects of many tissue and drug parameters that is impossible to study in
an in-vivo animal model in this time.
Angiogenesis is tremendously complicated process '. It involves interactions between
growth factors, inhibitors, and their regulators at molecular, cellular and tissue levels. These
interactions are multidimensional, evolving in time and varying throughout the tissue space, and
can be highly nonlinear. Previous studies have described and characterized the key angiogenic
processes: growth, maturation, and regression. Generation of new blood vessels is initiated with
growth factor stimulation and new sprouts can be from preexisting mature or new blood vessels
2. Morbidelli
et. al. showed that angiogenesis will not occur if growth factor concentration is
below a threshold 3, and others that angiogenesis will reach a plateau if growth factor
concentration exceeds a saturation level 4. Stokes and Lauffenburger
5,6 estimated
the rate of
sprout formation in the rat cornea based on experimental data 7. These newly formed vessels
must anastomose or form a closed circuit to preexisting vessels to allow blood flow and become
functional. Vessel maturation is an active area of research 8. Maturation requires well
orchestrated interactions of many molecular players; disregulation of this cascade of events can
lead to leaky vessels with impaired perfusion function 8. Furthermore, regression of blood
vessels can take place when immature vessels are not exposed to an adequate dose of survival
angiogenic growth factors
7',9
The goal of this Chapter is to create an integrated computational model of angiogenic
growth factor effect and transport in myocardial tissue using a continuum approach. The model
combines many experimentally derived parameters with known pharmacokinetic and
pharmacodynamics processes of FGF in myocardial tissue to provide prediction tool for
optimization studies, explain experimental observations and guide future studies.
4.2 Methods
To understand the forces that govern the unique interdependence of the pharmacokinetics
and pharmacodynamics of angiogenic compounds, we created a computational framework that
allows investigation of subtle mechanisms that cannot be elucidated with animal investigations.
The pharmacokinetic component of our model accounts for molecular transport through
vascularized tissues and allows for an examination of the effects of capillary uptake and clearance
on tissue distribution. This allows us to study the impact of capillary density and drug
physicochemical properties on myocardial transport. When coupled to the pharmacodynamic
model the integrated model describes the response of capillary beds to super-threshold
concentrations of angiogenic compounds.
The model describes (1) release of growth factor from source (2) diffusion of growth
factors within extravascular tissue (3) microvessel uptake and clearance (4) capillary sprouting
(5) capillary maturation, and (6) capillary regression.
The computational tissue area consists of 200 x 200 nodes with grid size dx = 5 jtm,
resulting in a 1000 pm 2 tissue space. The initial capillary distribution is generated randomly and
uniformly distributed in both x and y directions. Capillaries are assumed to have an average
diameter of 5 pm o
4.2.1 Local Pharmacokinetic Model
4.2.1.1 Mass Transport Equations
The myocardium is divided into extravascular and intravascular regions with distinct
mass transport properties (Fig. lA). Molecular transport within the extravascular region is
governed by:
ct = D Ac,
(Eq. 1)
where ct is the molecular concentration within extravascular space, Deff is effective drug
diffusivity in extravascular space, and t is time. Binding of growth factor to tissue components is
not explicitly considered, but is included implicitly in the experimentally derived value of the
effective diffusion coefficient Deffas measured for FGF-2 in myocardial tissue (Chapter 2). The
trans-endothelial flux from tissue to blood is
J
(Eq. 2)
= P(c' (-Ccap)
where Pm, is trans-endothelial permeability, and K , the partition coefficient of drug from the
intra-vascular space into extra-vascular tissue space. We assumed that convective washout within
the intravascular region is significantly faster than the permeation rate into intravascular space,
or capillaries act as sinks to molecular transport (Chapter 2), hence set the boundary condition of
intravascular concentration
ccap=
0 (Fig. 1B). Drug release kinetics is incorporated into the
boundary conditions at the tissue-polymer interface, either as constant flux (Fo) or constant
concentration (co) boundary conditions, respectively
c,
or:
source
= Co
(Eq. 3)
-D
(Eq. 4)
c t =FO
ax
.0
C
Permanent
Vessel
Functional
Vessel
Nascent
Vessel
O
Nascent
Vessel
N
0
Regression
Maturation
Sprouting
Functional
Vessel
Intertitium
:%
Nascent Vessel
1
a
n
Permanent
Vessel
Functional
Vessel
s
c
e
n
t
V
Regressed
Vessel
Nascent
Vessel
0
FIGURE 1: Schematics of FGF transport and angiogenic response in myocardium
A. Cross sectional view of myocardial tissue: background represents a H&E stained
image of cardiac tissue cross section with pink regions denoting intracellular space,
brown circles denoting permanent vessels including initial vessels prior to therapy,
yellow circles denoting nascent vessels, red circles represent functional vessels,
black circles with cross represent regressed vessels, dotted green line shows isoconcentration line at biologic effectiveness concentration threshold.
B. A two-region continuum pharmacokinetic model for FGF transport includes
intravascular and interstitial space. Capillary flow clears drug instantaneously. FGF
transport within the interstitium is described by effective diffusivity and passive
permeation between capillary and interstitial space.
C. Three-step angiogenic model includes sprouting, maturation and regression.
4.2.2 Local Pharmacodynamic Model
The angiogenic response to growth factor is modeled by three fundamental events: (1)
capillary sprouting, (2) capillary maturation, and (3) capillary regression (Fig. 1C). These events
are implemented according the algorithm summarized in Table 2.
Source:-D Tissue:
aC
- =D
at
+
(a2C
x
=
a2
+2
ay2
Trans-endothelial Flux: J = P
Capillary Sprouting:
Capillary Maturation:
1. Functional:
2. Stabilized:
Capillary Regression:
C
- Ccap )
Psprouting = Pmax f(C)At
(tsup-tsprout) > tfunctional
t
IH(C, - C)dt <
H(C,
-
C)dt >
t
regression
regression
TABLE 1: Summary of models: (A) PK model equations, (B) PK-PD model equations.
4.2.2.1 Capillary sprouting
We assume that induced capillaries form only from pre-existing capillaries and model
this as a stochastic process with a formation probability that is an increasing function of
angiogenic growth factor concentration
3. Following
Tong et.al.' l , we calculated the probability
of vessel formation Pspro,,,,ting for each segment length of capillary dx, and each time interval dt :
Pprout,,,g = Pmax f (c)dxdt.
Here P,,ax is a rate constant that determines the maximum probability of sprout formation per
unit time and vessel length, andf(c) is a threshold function defined as
f 0()
e-a(c
f(c =
<c,,
0
-c
)
<C
where ct is threshold concentration, and a is a constant that controls the rate of transition of the
threshold function ". This concentration dependence accounts for the observation that
angiogenesis only occurs above some threshold growth factor concentration 3, and that the
response is maximal above this threshold 4. A tissue node can become a capillary node only if it
is adjacent to any existing capillary node and if its probability of sprouting from Psprouting is
greater than a random probability sampled from a uniform distribution using Matlab.
4.2.2.2 Capillary maturation
The model draws a distinction between nascent, functional and permanent capillaries
(Fig. IC). Nascent capillaries are those of early sprouts, and require anastomosis to support
blood flow and become functional capillaries. Maturation progresses from nascent to functional
to permanent capillaries, with the exception that initial capillaries have permanent status. We
model the maturation process of nascent capillaries to become functional capillaries by tracking
the time nascent capillaries are exposed to super-threshold growth factor concentration. This
super-threshold duration needs to be above a test condition tfunctional, which is a surrogate for the
time taken to make an anastomosis to an existing capillary to establish blood flow. In this
context, tfunctional is approximately
c
where dc is intercapillary distance and vsprouting is
Vsprouting
sprouting velocity. Stokes et.al. demonstrated that endothelial cells migrate at speed of 20tm/h
and can increase to 40[tm/h with FGF stimulation 6. Others have demonstrated that the front edge
of vascular networks in cornea pocket assay moves with a speed of 15gtm/h with FGF
stimulation
12.
We chose the range of tfunctional from 6m to 3h to reflect the heterogeneity of
vascular density and to agree with the experimentally determined mean intercapillary distance of
20um/h
13.
Functional capillaries further require exposure to growth factors to become
permanent. Both functional and permanent capillaries contribute to intra-vascular space and can
clear drug, whereas nascent capillaries cannot.
4.2.2.3 Capillary regression
Survival of neo-capillaries is dependent on the local presence of angiogenic growth
factors 7. In the corneal pocket assay FGF and VEGF induced vessels would regress soon after
removal of growth factor sources 9. To account for this property, the model assumed that nascent
vessels are regressed when the average growth factor concentration in adjacent tissue is below
the sprouting threshold concentration for a period of time tregression. To account for tissue
variability we varied tregression over a uniform distribution bounded by tregressionl and tregression2
between 5m and 5d and performed sensitivity analysis on this variation. If satisfying this
requirement, functional capillaries will become permanent capillaries and are assumed to be
stable and do not regress.
Non-vascular
Sprouting:
and
NO ---
Non-vascular
YES
Nascent vessel
Maturation:
t sup
> tfunctional
NO --
Nascent vessel
NO --
Regression
YES
Functional vessel
Regression:
YES
Permanent vessel
TABLE 2: Summary of angiogenic model. Non-vascular tissue nodes are subjected to
several different conditions of sprouting, maturation and avoiding regression to progress to a
permanent vessel.
4.2.3 Model Parameters
Initial capillary volume fraction is assumed to range from 1%-100% of the normal range
of 2000-3000 capillaries per mm
2
14.
Baseline trans-endothelial permeability and diffusivity
values are assumed to be similar to those observed in arterial tissue for hydrophillic drugs
15.
For
the constant flux release mode, drug was initiated and maintained with zero-th order kinetics,
with a baseline rate of lx10
1 1 ng/s,
similar to a published estimate for VEGF release from fibrin
glue release device' 6 . The baseline model parameters are summarized in Table 3.
Parameter Description
Deff
PmV
Kc
Fo
Ct
a
Pmax
tfunctional
tregression
N
Effective diffusivity
Microvascular
permeability
Partition coefficient
Release rate
Biologic threshold
Threshold function
constant
Maximum probabililty
of sprout formation
Functional delay time
Regression half life
Initial capillary density
Baseline value
1 am 2/s
10 gm/s
1
1x10-T ng/s
0.1 ng/ml
1
5 x 10-4 um'hrVaried
Varied
Varied
TABLE 3: Baseline parameter values
4.2.4 Numerical Methods
Numerical simulation of the model was accomplished by dividing the myocardium into
computational elements each with a specific drug concentration. A forward difference numerical
procedure was applied on the computational grid to solve the transport equations (See Appendix
for MATLAB code).
4.3 Results
4.3.1 Local Pharmacokinetic (PK) Model Results: Effects Diffusivity, Trans-endothelial
Permeability and Vascularity on Drug Transport.
We simulated the PK-only module of the model to examine the isolated effects of
diffusivity, and capillary clearance on drug deposition and penetration depth to account for our
ex-vivo experimental observations (Chapter 2). This model demonstrated that drug diffusivity,
trans-endothelial permeability, and capillary volume fraction have significant impact on drug
transport following locally applied drug source of constant concentration. As drug diffusion
coefficient increases, it can penetrate tissue easily, however interestingly those with higher
diffusion coefficient have lower total deposition at steady state (Fig 2A). Such trend is
counterintuitive, and is opposite from those expected in diffusion through solid media where
distributed sinks are absent. Drugs with higher diffusivity can transport further into tissue and
effectively see more capillaries and are cleared at higher rate hence have lower total deposition.
Our analysis also highlights the impact of capillary trans-endothelial permeability and tissue
vascularity on drug distribution and elimination (Fig 2B-C). Both drug trans-endothelial
permeability and tissue vascularity contribute similarly to drug clearance, and limit tissue
penetration and deposition of drug. The sensitivity to permeability and vascularity is highest
when permeability and vascularity is lower than 0.5 um/s and 500 capilllaries/mm 2 , respectively.
600
7.50E-07
400
5.OOE-07
.
a
o
2.50E-07
200
0
0.OOE+00
-
0
100
50
Diffusivity (um2/sec)
250 -
-
200 E
4.00E-06
me
-3.00E-06
0
150
2.00E-06
.t
il
100
- 1.00E-06
50
00
'-
a
0.OOE+00
0 0
0
0.5
1
Permeability (um/s)
250
-5.00E-06
._
200
4.00E-06
o
150
3.00E-06
a
100
2.00E-06
P
50
1.00E-06
0
0.OOE+O0
a0
0
500
1000
1500
Capillary density (#/mm2)
FIGURE 2: Continuum Pharmacokinetics Model:
Effects of diffusivity, permeability, and initial vessel
volume fraction. Black curves and y-axes represent
penetration depth, defined as distance from source to
spatial locations with 90% drop-off threshold
concentration from source. Blue curves and y-axes
represent total drug deposition.
4.3.2 Local Pharmacokinetic-Pharmacodynamic (PK-PD) Model Results
4.3.2.1 PK-PD Interdependence:
To provide a conceptual model of how the dynamics of induced angiogenesis affect drug
distribution, we coupled an angiogenic pharmacodynamics (PD) model of capillary sprouting
and maturation (without regression) to the pharmacokinetic (PK) model. Simulated drug release
kinetics recapitulated in vitro release kinetics (Chapter 3). Angiogenesis affects drug distribution
significantly (Fig 3A-B). The pure PK model (Fig. 3A) shows drug reaching super-threshold
concentration throughout the Imm2 tissue region at up to 48 hours and remaining high over the
tissue region at day 10. The PK/PD model predicts that the super-threshold drug concentration
front initially penetrates deeper into the tissue with time, similar to the predictions of the PK only
model. However, at later times the threshold front slows down and eventually regresses between
72-96 hour as the formation of new capillaries increases drug clearance. Notably, the steady state
depth of the threshold front (Fig. 3B) is significantly lower than PK only model (Fig. 3A).
Such negative pharmacodynamic feedback on drug transport observed in Fig 3B can have
indirect effects on drug action. We studied this possibility by examining the relationship of rate
of angiogenesis as a function of tissue angiogenic state measured by vascularity (Fig 3C). The
ascending limb of the curve is a manifestation of the fact that new capillaries can only sprout
from existing capillaries. The descending limb of the curve represents a negative feedback where
the generation of neo-capillaries has an inhibitory effect on drug transport. Capillary growth
1hr
10min
24hr
6hr
2hr
240hr
A
400
C
"
00
oo
S300
o0 OO
o0
0
000OM
0140 o0
ooo
OO
00
O
0
o
OO
0
00
D
D
o
oooo 5
oo
a o~o0
0
140
280
0
0
0o00oo
O
0
0
00
0
0CD 0
000
0O 00000
0
oo
o
oo
oo
00000
o
ooc
o a
0
ooo
S o(Do
o
Sooo
o
oooo
7o
o
aD oGWoD
420
560
700
Number of Capillaries
FIGURE 3: Pharmacokinetic/Pharmacodynamic Model. Drug and capillary distribution as
a function of time of (A) PK model, (B) PK/PD model. Orange color regions denote superthreshold drug distribution, and white dots represent functional capillaries. (C) Rate of
angiogenesis (#capillary/hr), defined as first time derivative of capillary number, as a function
of capillary number.
increases drug clearance through washout and impedes drug penetration, reducing the areas of
super-threshold concentration and angiogenic response. Thus, there is an interdependence of
pharmacokinetics and pharmacodynamics. As the pro-angiogenic therapy starts to become
effective, this unique PK-PD coupling inhibits the distribution of the therapeutic drug and limits
the intended effect of the therapy. It should be noted that these results also support our
experimental observations in-vivo (Fig. 4-5, Chapter 3), and offer a possible explanation for the
regression of neo-vascularization observed in early time points: lack of growth factor due to
clearance through microvascular washout.
4.3.2.2 Model Sensitivity Analysis:
Since capillary washout has significant impact on drug transport and angiogenic
response, we performed the sensitivity analysis on model parameters whose baseline values are
either not available experimentally or can potentially be altered to optimize the angiogenic effect.
4.3.2.2.1 Timings of CapillaryMaturationand Regression Have Little Effect on Steady State
CapillaryGain
We modeled the maturation process of new blood vessels by drawing a distinction
between nascent, functional and permanent capillaries. Nascent capillaries can become
functional capillaries (capable of carrying blood flow and clear drugs) when exposed to growth
factor for a period of time above tfunctional. However, our model also allow for regression to occur
if vessels are subjected to long period of sub-therapeutic concentration. To implement this
requirement, the model imposed a regression condition that if capillaries are exposed to subthreshold growth factor concentration for more than a period of time tregression, which varied over a
uniform distribution bounded by tregressionl and tregression2 between 5m and 5d. In principle, because
functional capillaries can clear drug, the timings of their occurrence and disappearance are
expected to have an impact on the permanent capillary number. However, interestingly although
there were differences in transient dynamics, the steady state angiogenesis was not significantly
affected by parameters controlling the timings of biologic activities (functional and tregression).
Drugs initially distributed within tissue, but as total capillary number increased drug
distribution quickly regressed. Greater values of tfunctional correspond to longer delay to gaining of
functional vessels (Fig. 4B) and allow for higher drug penetration into tissue (Fig. 4A). The
higher drug penetration (higher peak for longer tfunctional in Fig. 4A) in turns leads to higher
maximum total capillary number (Fig. 4B). However, greater angiogenic response only occurred
transiently. This is because higher functional capillary number attained during the early phase
also led to a higher clearance rate of drug washout, resulting in greater regression of penetration
depth of super-threshold growth factor concentrations (Fig. 4A). The greater drops in penetration
depth, in turns, led to more regression (Fig. 4B), and cancelled out the higher early gains.
The sensitivity of late angiogenic gain to regression timings was further examined by
changing parameters (tregression and tregression2) controlling the distribution of required maximal
duration of sub-threshold exposure before undergoing regression. Peak angiogenic response and
drug penetration depth were not sensitive to altering regression conditions as expected since they
do not alter the sprouting and maturation properties (Fig 5). These parameters, however,
influenced the start time of when functional vessels regress. The regression timings interestingly
also did not influence the steady state functional capillary number (in both cases of varying
tregressionl (Figs. 5A&C) and tregression2 (Figs.5B&D)), but only the time taken to reach this steady
of
state (tregression). Therefore, the pharmacodynamic timings only impact the transient response
angiogenesis and not steady state angiogenesis (number of permanent capillaries).
180E
0.
a
I
120-
-. t functional = 6min
*-t functional = lhr
-- tfunctional = 2hr
t_functional = 3hr
0
" 60a)
4)
0-
.4
Time (hrs)
B
500 -L
a.
400
0
0
I--
= 1 hr
t functional = 2hr
E
z 300
.7
t functional = 6min
-tfunctional
t_functional = 3hr
200
100
0
.1
0.1
1
10
Time (hrs)
100
10 00
FIGURE 4: Effects of tfunctional on penetration depth
(A) and total capillary number (B) as a function of
time.
120
2hr-4hr (3hr +- lhr)
1205m - 48hr (24.5hr +- 23.4hr
--
2hr - 48hr (25hr +- 23hr)
E 90 -
-
-*-2hr-5d (61hr +- 59hr)
E 90
12hr - 48hr (30hr +- 18hr)
2hr-48hr (25hr +- 23hr)
-
aL
r 60
0
a,
C
(U
. 30
6 30
0 i
i
T
Timdb rs)
1
aH
,i
0
1000
1
0.1
10
Time (hrs)
10,
100
400
400-
300
300
-
200
o 200 I-
100-
100
5min-48hr (24.5hr +- 23.4hr)
2hr-48hr (25hr +- 23hr)
12hr-48hr (30hr +- 18hr)
0.
1
Time hrs)
1000
i
0.1
m
2hr-4hr (3hr +- 1hr)
-- 2hr-48hr (25hr +- 23hr)
S2hr-5d (61hr +- 59hr)
10
Time (hrs)
FIGURE 5: Effects of tregression range on penetration depth (A&C) and total capillary number (C&D) as
a function of time. Legends denote tregressionl-tregression2 (tregression +- 0.5 range of tregression).
1000
4.3.2.2.2 Trans-endothelialPermeability,Diffusivity, Biologic Threshold,Initial capillary
density and Release Kinetics Have Significant Effect on Steady State Drug Distributionand
Capillarygain.
Our results also revealed the factors that have significant impact on steady state
angiogenesis. These include ones involved in drug clearance (initial tissue vascularity and transendothelial permeability), bulk transport (diffusivity), drug input (release rate), and biologic
threshold.
3000
A
2500
N=2400
Initial tissue vascularity:
.
2000
Tissues with higher baseline
1500
vascularity are expected to have
1000
N=8
500
N=400
higher drug clearance to begin with
0.1
and thus would create a local tissue
environment with higher impedance
10
Time (hrs)
100
1000
100
1000
600.00%
B
for drug transport. Indeed, total
capillary number sprouted over time
1
t-
400.00%
i
is inversely proportional to the initial
N=10
S200.00%
vascularity (Fig 6A), and the trend
_
N200
N=400
can be better revealed when looking
0o.oo00%
-.
0.1
at the percentage capillary gain over
of 50
capillary density of 50
2-0-
1
10
Time (hrs)
starting 6: Effect of initial vascularity (N=50,
time (Fig 6B). With aFIGURE
100, 200, 400, 800 and 2400 denote the initial
number of capillaries per mm 2) on absolute
capillary number (A) and percentage capillary
gain (B) as a function of time.
capillaries/mm 2, the peak percent capillary gain can be as much as 600%. This percent gain
decreased with higher baseline vascularities and was as little as 2% for baseline vascularity of
2400 capillaries/mm 2 (Fig 6B). Unlike the effect of tfunctional (Fig. 4), higher peak angiogenic
response in this experiment translated to higher steady state percentage capillary gain. Higher
initial capillary density led to higher baseline clearance, making it more difficult for drug to
penetrate into tissue to achieve super-therapeutic threshold for angiogenesis.
Diffusivity: Drugs with higher diffusivity can stimulate higher peak percentage capillary
gain (2100%, 570%, and 244% for rD (=D/DFGF) = 10, 1 and 0.1 respectively). Capillary
regression reduces the magnitude of the gain, but does not alter the dependence on diffusivity
(260%, 71%, and 28% for rD = 10, 1 and 0.1, respectively) (Fig 7A). More readily diffusive
drugs can move faster into tissue and effectively increase the penetration depth of supertherapeutic drug front, increasing both peak and steady state angiogenic response.
Trans-endothelial permeability: Drugs with lower trans-endothelial permeability can
stimulate higher peak percentage capillary gain (2100%, 510%, and 280% for r_P (=P/PFGF)
0.1, 1, 10 respectively), and retain larger gain in permanent capillaries (404%, 71%, and 20% for
rP = 0.1, 1, 10 respectively) (Fig 7B). Lower trans-endothelial permeability improved
penetration and at the same time also minimized drug loss to microvascular washout, leading to
both gain in peak and steady state angiogenesis.
Growth factor therapeutic threshold concentration: Potent growth factors elicit effects at
lower threshold concentrations, stimulating higher peak percentage capillary gain (1400%,
970%, 570% and 240% for r_Ct (=Ct/Ct
FGF)
= 0.1, 1, 10, 100 respectively), and higher steady
state gain (140%, 108%, 71% and 50% for r_Ct = 0.1, 1, 10, 100 respectively) (Fig 7C).
Lowering therapeutic threshold is equivalent to increasing drug penetration depth since it is
easier for tissue to achieve therapeutic threshold concentration with the same drug PK properties.
Therefore, drugs with higher potency had higher peak and steady state angiogenic gain.
Release rate: Releasing drug at a higher rate can stimulate higher peak percentage
capillary gain (890%, 570%, and 320% for r RR (=RR/RRbaseline)
=
10, 1, 0.1 respectively), and
steady state gain (101%, 71%, and 44% for r_RR = 10, 1, 0.1 respectively) (Fig 7D). The
response to increasing drug release rate was similar to that of lowering therapeutic threshold in
that both act to increase the early capillary gain (elicit higher peak angiogenic response) by
increasing the penetration depth of the drug's super-therapeutic wave front, and as a result
increased the number of capillaries with permanent status.
Comparing the effects of different model parameters on steady state percentage capillary
gain (Fig. 8) revealed that capillary permeability is the most sensitive parameter at producing
permanent capillaries with local myocardial growth factor delivery. The green line in the curve
denotes the sensitivity of the model to changing the drug's biologic threshold but keeping its PK
properties unchanged. While modulating release rate (blue line) can achieve a similar response to
effect of changing drug potency (green line), altering trans-endothelial permeability of the
growth factor (magenta line) can produce a significantly greater return in permanent
angiogenesis.
100
2500%
L
0 2000%
-
r D=0.1
-
r D=1
-
r D=10
a1500%
c
2500%
20
(
2000%
. 1500%
01000%
C
500%/o
S 500%
0%
100
1000
a)
Time (hrs)
1000.00%
1500%
1000
100
10
Time (hrs)
1
-rRR=
-rRR=1
.a
0
750.00%
0.1
rRR=10
CO
c1000%
o 500.00%
a)
(D
a
C)
O
C
500%
250.00%
a
0.00%
1
1
100
10
1000
100
10
1000
Time (hrs)
Time (hrs)
FIGURE 7: Effects of diffusivity, trans-endothelial permeability, biologic threshold,
and release rate on percent capillary gain over time. r D, rP, and rCt are defined as
ratio of diffusivity (A), trans-endothelial permeability (B), and biologic threshold (C),
respectively, over the respective baseline values of FGF. rRR is defined as ratio of
release rate to baseline release rate (D).
101
500.00%
* Release Rate
M Permeability
400.00%.831
= 0.8319X
yS=
"
A Bioloqic Threshold
6527
-0.6527
2
R = 0.9921
, 300.00%
2y
=
-0.1277Ln(x) +y
= 0.1249Ln(x) + 0.7225
2
R = 0.9991
R = 0.9925
100.00%
0.00%
0.01
0.1
1
10
100
Folds changed compared to baseline value
FIGURE 8: Steady state percentage capillary gain as a function folds change
in biologic threshold, drug release rate, and permeability
102
4.4 Discussion:
4.4.1 Traditional Continuum PK vs. Continuum PK-PD Analysis
Continuum pharmacokinetic analyses have been successful in providing insights into
local drug transport mechanisms
17, 18.
This continuum approach adapts traditional
compartmental pharmacokinetic analysis to the local environment by supplanting discrete global
parameters with continuous local values of concentration, transport and binding. These
parameters and local boundary conditions define local drug distribution in space and time. These
continuum PK models explain experimental results well and give tremendous insights into
optimizing local perivascular 18, and stent based
17
arterial drug delivery for heparin and
paclitaxel that have minimal effect on tissue transport properties. Our results suggest that drugs
such as angiogenic growth factors significantly modulate the local drug clearance properties of
tissue over the course of local sustained delivery, thereby powerfully regulating their biological
effects. Therefore, studies of angiogenic growth factor delivery should augment the continuum
PK approach with a PD processes in analyzing local drug delivery.
As the pro-angiogenic therapy starts to become effective, the balance of transport forces
is shifted to clearance dominant regime. In our model, this effect arises primarily as a result of
increasing capillary density. We did not specifically examine the changes in trans-endothelial
permeability when the tissue is in angiogenic state. It is very likely that trans-endothelial
permeability can be significantly higher as angiogenesis occurs
19, 20.
Such changes in
permeability would further increase drug clearance through washout and tips the balance point
even more to the clearance dominant regime, potentially resulting in more powerful negative
103
pharmacodynamics feedback. This further raised the need to consider pharmacodynamic effects
of drug on tissue transport properties when studying local drug delivery.
4.4.2 Minimizing Microvascular Clearance as an Approach to Optimize Angiogenic Effect
The negative feedback of PD on PK in local growth factor delivery for angiogenic
therapy suggests an optimal approach to improve drug penetration and angiogenesis through
minimizing microvascular clearance. Indeed, our results revealed that lowering trans-endothelial
permeability provide significant improvement in inducing permanent vessel formation by
increasing drug retention to prevent vessel regression after they were induced. The effect of
lowering trans-endothelial permeability interestingly can be significantly greater than changing
the biologic threshold of the growth factor at inducing permanent vessel formation. Since the
clinical goal of angiogenic therapy is to maintain permanent collateral vessels, growth factors
might be designed through chemical modification or genetic engineering to optimize the balance
of opposing forces of drug distribution and drug clearance. For instance, it might be possible to
add negative charge chemical groups to drugs to lower trans-endothelial permeability
21 to
improve penetration depth and retention to achieve a more uniform and longer lasting angiogenic
response. These results suggest that computational modeling of local continuum PK-PD can be
used to guide engineering of drug properties to achieve desire biologic response. We used a
simple, mechanistic, 2D model in this chapter to focus our studies on the effects drug clearance
through microvascular washout in governing drug transport, it can be improved further to
consider more realistic three dimensional vascular networks and flow patterns when
computational power can be improved.
104
4.4.3 Release Rate and Diffusivity Modification to Optimize Angiogenic Effect
Our sensitivity analyses also suggest that the model response is sensitive to changes in
diffusivity and drug release rate. The parameter that can perhaps be modulated most easily is the
rate of drug release. For example, FGF release rate from heparin alginate device changes as a
function of heparin concentration 22 . Increasing the rate of angiogenic drug input achieves a
steady angiogenic effect equivalent to lowering the biologic threshold of the drug which might
not be so easily to alter. This approach might be advantageous for drugs with large therapeutic
window when high tissue concentration does not present toxicity to the myocardial tissue.
Different ways of modulating effective diffusivity of growth factor may include altering
size, charge, and binding domains. The effect of size and charge on effective diffusivity of
macromolecules in tissue has been experimentally determined
21.
Our results in Chapter 5
suggest that penetration depth of FGF can be improved by minimizing its interaction with tissue
HSPGs through the use of sucrose octasulfate (SOS). This binding interaction may be
accountable for an approximately 500 times slower in effective diffusivity and therefore presents
a potential optimizing target for enhancing diffusivity. Although, this modification with SOS can
be achieved at the expense of increasing steric hindrance, it is perhaps possible some day to
engineer binding domains of growth factors to achieve the optimal balance of binding property,
molecular size changes, and retention of the drug's biologic effect to improve effective
diffusivity.
105
4.4.4 Minimizing Late Loss as an Effective Approach to Improve Angiogenic Therapy
One of the most significant implications from our computational model results was that it
identified distinct temporal tissue responses following angiogenic therapy (representative
response is shown in Fig. 9), and showed the differential response of each phase to changing
various drug and tissue properties. "Early gain" phase consists of sprouting of nascent blood
vessels and their maturation to functional vessels capable of perfusing ischemic tissue. These
new vessels though functional require super-therapeutic growth factor levels to survive,
otherwise undergoing regression. The regression process is the main feature of the "late loss"
phase. Because functional vessels clear drugs through microvascular washout (Chapter 2), the
increase of these vessels in the "early gain" phase act as a powerful negative feedback
mechanism to cause vessel regression, accounting for the magnitude of the "late loss" of
functional vessels (Fig. 9). Most PK and PD properties of drugs and drug release device, such as
effective diffusivity, potency, and release kinetics, can be modulated to directly maximize the
response in the "early gain" phase. However, lowering trans-endothelial permeability can both
increase "early gain" and minimize "late loss". Therefore, modulation of trans-endothelial
permeability contributes most significantly to the permanent angiogenic response (Fig. 8).
Furthermore, these results also suggested that minimizing "late loss" phase by any
therapeutic means can potentially increase "permanent gain" and unlock the vast angiogenic
potential of the "early gain" phase. One way of doing this may be by releasing many drugs with
different biologic actions at different times during the therapeutic treatment. An early drug can
be FGF or VEGF that act to maximize the "early gain" phase, while a late drug can be
106
angiopoietin-1
23,
which act to minimize vessel leakiness to reduce "late loss" and maximizing
"permanent gain". With current advances in drug release device technology
24,
it may be possible
to precisely control the release time of these different drugs to modulate both early and late
phases of angiogenesis for optimal effect in long term.
D, Pmv, Cth, RR
Pmv
600.00%
400.00%
0Early
G in
Late Loss
CU
S200.00%
Permanent Gain
- -
0.00%
0.1
1
100
10
1000
Time (hrs)
FIGURE 9: Approaches to improve pro-angiogenic therapy. Typical angiogenic
response is represented in brown curve. An early angiogenic gain is followed by a
late loss in functional vessels as a result of regression. The difference between the
response from these two phases is permanent angiogenic gain. Maximizing this
permanent gain is the goal of angiogenic therapy. While many factors can affect the
early angiogenic gain, the drug's trans-endothelial permeability is most effective at
minimizing late loss, and as a result has a significant effect on permanent gain.
107
4.5 Summary
The unique problem faced by angiogenic therapy is that its very success in stimulating
blood vessel growth limits further angiogenic activity. Our computational models confirm our
experimental results in previous chapters and suggest strategies for drug design and drug
delivery systems to enhance drug penetration and subsequent induction of permanent collateral
vessels. Engineering angiogenic myocardial drugs and drug delivery systems thus required
understanding of PK-PD interdependence and careful calibration of factors involved in local
tissue PK and PD.
108
4.6 References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
16.
17.
18.
Folkman J. Angiogenesis and angiogenesis inhibition: an overview. Exs. 1997; 79:1-8.
Jain RK, Schlenger K, Hockel M, Yuan F. Quantitative angiogenesis assays: progress and
problems. Nat Med. 1997; 3:1203-1208.
Morbidelli L, Parenti A, Giovannelli L, Granger HJ, Ledda F, Ziche M. B 1 receptor
involvement in the effect of bradykinin on venular endothelial cell proliferation and
potentiation of FGF-2 effects. Br J Pharmacol. 1998; 124:1286-1292.
Dellian M, Witwer BP, Salehi HA, Yuan F, Jain RK. Quantitation and physiological
characterization of angiogenic vessels in mice: effect of basic fibroblast growth factor,
vascular endothelial growth factor/vascular permeability factor, and host
microenvironment. Am J Pathol. 1996; 149:59-71.
Stokes CL, Lauffenburger DA. Analysis of the roles of microvessel endothelial cell
random motility and chemotaxis in angiogenesis. J Theor Biol. 1991; 152:377-403.
Stokes CL, Lauffenburger DA, Williams SK. Migration of individual microvessel
endothelial cells: stochastic model and parameter measurement. J Cell Sci. 1991; 99 ( Pt
2):419-430.
Sholley MM, Ferguson GP, Seibel HR, Montour JL, Wilson JD. Mechanisms of
neovascularization. Vascular sprouting can occur without proliferation of endothelial
cells. Lab Invest. 1984; 51:624-634.
Jain RK. Molecular regulation of vessel maturation. Nat Med. 2003; 9:685-693.
Cao R, Brakenhielm E, Pawliuk R, Wariaro D, Post MJ, Wahlberg E, Leboulch P, Cao Y.
Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a
combination of PDGF-BB and FGF-2. Nat Med. 2003; 9:604-613.
Kassab GS, Fung YC. Topology and dimensions of pig coronary capillary network. Am J
Physiol. 1994; 267:H319-325.
Tong S, Yuan F. Numerical simulations of angiogenesis in the cornea. Microvasc Res.
2001; 61:14-27.
Kenyon BM, Voest EE, Chen CC, Flynn E, Folkman J, D'Amato RJ. A model of
angiogenesis in the mouse cornea. Invest Ophthalmol Vis Sci. 1996; 37:1625-1632.
Feldstein ML, Henquell L, Honig CR. Frequency analysis of coronary intercapillary
distances: site of capillary control. Am J Physiol. 1978; 235:H321-325.
Rakusan K, Flanagan MF, Geva T, Southern J, Van Praagh R. Morphometry of human
coronary capillaries during normal growth and the effect of age in left ventricular
pressure-overload hypertrophy. Circulation. 1992; 86:38-46.
Creel CJ, Lovich MA, Edelman ER. Arterial paclitaxel distribution and deposition. Circ
Res. 2000; 86:879-884.
Ehrbar M, Djonov VG, Schnell C, Tschanz SA, Martiny-Baron G, Schenk U, Wood J,
Burri PH, Hubbell JA, Zisch AH. Cell-demanded liberation of VEGF121 from fibrin
implants induces local and controlled blood vessel growth. Circ Res. 2004; 94:11241132.
Hwang CW, Wu D, Edelman ER. Physiological transport forces govern drug distribution
for stent-based delivery. Circulation. 2001; 104:600-605.
Lovich MA, Edelman ER. Computational simulations of local vascular heparin
deposition and distribution. Am J Physiol. 1996; 271:H2014-2024.
109
19.
20.
21.
22.
23.
24.
Lin CY, Chang C, Cheung WM, Lin MH, Chen JJ, Hsu CY, Chen JH, Lin TN. Dynamic
changes in vascular permeability, cerebral blood volume, vascular density, and size after
transient focal cerebral ischemia in rats: evaluation with contrast-enhanced magnetic
resonance imaging. J Cereb Blood Flow Metab. 2008; 28:1491-1501.
Wang L, Dudek SM. Regulation of vascular permeability by sphingosine 1-phosphate.
Microvasc Res. 2008.
Elmalak O, Lovich MA, Edelman E. Correlation of transarterial transport of various
dextrans with their physicochemical properties. Biomaterials. 2000; 21:2263-2272.
Edelman ER, Mathiowitz E, Langer R, Klagsbrun M. Controlled and modulated release
of basic fibroblast growth factor. Biomaterials. 1991; 12:619-626.
London NR, Whitehead KJ, Li DY. Endogenous endothelial cell signaling systems
maintain vascular stability. Angiogenesis. 2009.
Richardson TP, Peters MC, Ennett AB, Mooney DJ. Polymeric system for dual growth
factor delivery. Nat Biotechnol. 2001; 19:1029-1034.
110
Chapter 5: Effects of Tissue Binding on Local Pharmacokinetics of
FGF in Myocardium
Abstract
In previous chapters we focused on the effects of microvascular clearance on local
myocardial distribution of FGF. In non-perfused rat myocardium, drug transport is mainly
governed by diffusion and binding processes. FGF binding to its specific receptor and the more
abundant heparan sulfate glycosaminoglycans (HSPGs) binding sites was accounted for in a
simplified manner that presumes receptor excess. In this chapter we examined in more detail the
effects of myocardial binding on FGF transport. Effective diffusivity of FGF2 in myocardium is
-500 times lower than that of similar size Dextrans. Even at 96 hours, myocardial FGF2
accumulated only superficially, and penetration remained below 50 um unless the concentration
was increased to 8.82 ptM (150 jtg/ml), presumably due to the saturation of tissue binding sites.
Sucrose octasulfate (SOS) partially dampened the effects of binding-related transport hindrance.
Conjugation of FGF-2 to SOS decreased general binding, while not significantly affecting
superficial drug uptake, thereby increasing the rate of deep tissue drug uptake by 132.8%.
As the densities of vascularity and tissue binding sites are both expected to vary with the
level of ischemia, our results suggest that uptake and deposition of angiogenic growth factors
will vary intricately across the heart. This calls for careful attention in the choice of drug, and
formulation and placement of the delivery device.
111
5.1 Introduction
The "binding site barrier" hypothesis, the concept that molecular transport is impeded by
specific binding to fixed tissue sites has been introduced and experimentally verified in the
analysis of antibody distribution in microscopic tumor nodules
1-5.
When monoclonal antibodies
were administered intravenously, specific binding to tumor tissue antigens retarded their deeper
penetration into tumor tissue. Higher binding affinity, antigen density or lower antibody dose
can exacerbate the problem. This phenomenon may well be relevant for fibroblast growth factor
(FGF) transport since this growth factor binds avidly to its cognate cell receptor (FGFR)6' 7, and
less avidly to abundant fixed tissue binding sites including heparin sulfate proteoglycans
(HSPGs) 8, 9 . In fact, it has been shown that FGF2 when applied to monolayer of bovine aortic
endothelial cells in the presence of heparin stimulate morphological changes at a 10-fold greater
radius than bFGF alone as a result of partitioning preferentially in the soluble phase rather than
binding to fixed glycosaminoglycans in the extracellular matrix 10. Furthermore, native FGF
transport across Descemet's membrane (DM) is 20-fold slower than non-heparin binding form of
FGF 9. In this Chapter we examined the degree to which myocardial FGF transport is hindered
by binding and whether such hindrance can be controllably modulated.
The two classes of receptors for FGF are high affinity, low capacity FGFR, a tyrosine
kinase receptor family on cell surfaces, and low affinity, high capacity HSPGs 11, found on cell
surfaces as well as in extracellular matrix and basement membrane. FGFR family is composed of
four members: FGFR-1, -2, -3 and -4, but only FGFR-1 is found in the heart
12-14.
In myocardial
tissue, syndecan-3 and glypican are the most abundant types of HSPGs 15. In addition to the
abundant presence of HSPG in extracellular matrix and basement membrane, HSPG cell surface
112
density is also approximately 100-fold higher than FGFR density
16.
HSPG binding sites are at
much higher concentration in basement membranes than extracellular matrix
8,9. Although
basement membrane and extracellular matrix concentrations of HSPG in the myocardium have
not been reported, Descemet's membrane (DM) has been used as a model basement membrane
and the value of HSPG binding site concentration in DM 9 and in extracellular matrix of
endothelial cell culture have been quantified 8. As the myocardium is highly vascularized, and
that both myocardial capillaries and cardiac myocytes are lined with basement membranes of
high HSPG concentration, it is reasonable to expect that the "binding site barrier" limitation to
FGF transport in myocardium is significant.
In this Chapter, we show that tissue binding is the dominant transport hindrance on FGF
transport in a non-perfused myocardium and that while binding enhances local growth factor
uptake significantly, it also limits penetration and late uptake. Moreover, we illustrate that this
effect that is dampened when general binding is reduced with protective sugar groups.
113
5.2 Methods
5.2.1 Effect of Binding on Myocardial Transport
The degree to which reversible FGF
binding affects its myocardial transport can be
ko
B
F +R
(RI1)
quantified following the analysis of effect of
koff
immobilizing adsorption on gas diffusion in
polymers
17.
(1)
In this analysis, the diffusion
equation can be modified to allow for molecules
F
ax 2
B
(2)
being trapped in non-diffusing holes according
2
(F + B)
t
O0
-
ct
B
or
B F
"ax
Kd + F
to a simple Langmuir-type isotherm 18. The
(3)
diffusion in the presence of binding to
x ))2 d
B.maF/Kd
1+
(1+
=
a 22
O 2t
immobilizing sites is described by (1) where F
D
OF
B
denotes the concentration of FGF, B is the
2
F
Kd
K+maxOx2
concentration of FGF-receptor bound complex
created from the reaction (RI) between FGF and
(4)
Dqf=D
1+ Bmax /Kd)2
its receptors, assuming to consist of mostly
HSPGs. With the quasi-steady state assumption
of enzyme kinetics 19, i.e. the change of
TABLE 1: Summary of derivation of
effect of tissue binding on effective
diffusivity.
intermediate binding complexes FGF-HSPGs is
assumed to be minimal, B can be approximated by (2), where Kd is the dissociation constant
defined as the ratio of rate of dissociation to association of FGF-HSPG complex, and Bmax is the
maximum tissue binding sites. B can be substituted to equation (1) to arrive at the modified
114
D
diffusion equation (3), which defines the ratio
S
Bmax
as effective diffusivity Df.
Kd
(1+ F/K )2
Therefore, the effect of FGF-HSPG binding on FGF transport can be quantified by the
impedance factor a-
+ 1, which is non-linear and dependent of boundary
(1+F/Kd ) 2
concentration F. The larger a is the slower FGF transport would be. We can approximate the
value of a by comparing Dff of FGF to comparable molecular weight inert compounds.
5.2.2 Long-time point uptake studies
Rat myocardial tissue blocks of 8-10 mm3 in size were obtained from the left ventricular
free wall of harvested PBS-flushed hearts following euthanasia. Myocardial tissue sections were
incubated in serially diluted concentrations of drug solutions (TR-FGF2 and TR-FGF2-SOS at 0,
19, 38, 75, 150, 300 pg/ml of FGF2 in PBS) for 96 hours at 40 C. Following incubation, tissue
sections were processed for quantitative fluorescence imaging.
115
5.3 Results
5.3.1 Tissue Binding Impedes FGF Transport in Myocardial Tissue
Our experimental measurement of effective diffusivity of FGF (0.02 Im2/s) is
significantly lower than the diffusivity of Dextran 10OkD (10.24 [tm 2/s) in myocardial tissue. With
the assumption that steric hindrance of 10OkD Dextran and 17 kD FGF are similar, we can
approximate impedance factor a =
max
+1 to be 512. This number is within 0.25-1-
d
(1+F/Kd)2
folds values obtained for FGF in Descemet's membrane ( -500-2184 calculated in Tzafriri et.al
20
from data by Dowd. et.al.
9).
These results suggested that tissue binding hindrance is
significant for FGF transport in myocardium, within one order of magnitude of binding
hindrance in DM, which is known to contain high concentrations of heparan sulfate. Because
FGF is known to bind to FGFR and HSPG and that HSPG is more abundant than the specific
receptor FGFR, this binding hindrance is most likely a result of the reversible HSPG binding.
116
5.3.2 Modulating tissue binding alters myocardial FGF2 transport
To further examine the effect of HSPG binding on FGF transport, we incubated explanted
plugs of rat myocardium (8-10 mm 3) in varying concentrations of Texas Red FGF2 (TR-FGF2)
for 96 hours at 40 C and examined myocardial drug distribution (Fig. 1A). Penetration of TRFGF2 (at 25% source) was extremely limited, with drug mostly residing within the first -50 iim
of the surface even at 96 hrs. Increasing the applied concentration raised overall myocardial TRFGF2 uptake in a concentration-dependent manner. The depth of penetration remained
unchanged at low concentrations. Only when 8.82 tM (150 pg/mL) or greater of TR-FGF2 was
delivered did faster effective diffusion and deeper penetration occur (Fig. 1B). In pure diffusion
process, penetration depth at a fraction of source concentration would be independent of source
concentration as predicted by solution to diffusion equation c/Csource = erfc(x/2 Dt). A
concentration dependent process such as that observed by Fig. IB likely suggests a diffusive
transport mechanism that is modulated by saturable binding. Diffusive hindrance by abundant
local HSPG binding sites, which only begin to saturate at high drug concentrations, likely
accounts for such ineffective tissue penetration. Indeed, tissue equilibration for dextrans, a
compound much less encumbered by general binding, is known to occur in similarly sized plugs
within 48 hours 21, 22
We further compared the distributions of TR-FGF2 with Texas Red FGF2-SOS (TR-FGF2SOS) to examine the possibility of improving drug penetration depth with altering tissue binding.
At a concentration of 4.41 ptM (75 gig/ml), the penetration of TR-FGF2-SOS exceeded that of
TR-FGF2 (Fig. 2B). Interestingly, at a concentration of 1.76 ptM (300 gg/mL), the penetration
117
depths were reversed, with TR-FGF2 penetrating deeper than TR-FGF2-SOS (Fig. 2A).
Surprisingly, raising the applied drug concentration by over one order of magnitude only
increased the penetration depth of TR-FGF2, and not that of TR-FGF2-SOS. A concentrationdependent balance between susceptibility to repeated on/off non-specific binding and sizemediated diffusivity likely accounts for this observation. For TR-FGF2-SOS, the SOS
component decreases susceptibility to general binding, accounting for deeper penetration at
lower concentration and decreased sensitivity to changes in applied drug concentration. On the
other hand, at overwhelmingly high concentrations, TR-FGF2 itself can saturate general binding.
As a result, the lower diffusivity of TR-FGF2-SOS conferred by its significantly higher
molecular weight likely limits its penetration depth compared to that of TR-FGF2.
118
-19
ug/ml
-38
ug/ml
3000
-
75 ug/ml
--
150 ug/ml
2000
-300
1000
ug/ml
0
0
50
200
150
100
Distance from Source (um)
-- 300-
E
CLr
G 200-
0C
0
1001
(L
Expt Data
-4
I
100
200
300
400
Source Concentration (uglml)
FIGURE 1: FGF2 concentration profile (A) and penetration depth defined as 25%
of source concentration (B) as a function of source concentration. Error bars were
only shown at regular intervals.
119
3000
A
3000
-300ug/ml
-300
FGF-SOS
ug/ml FGF Alone
S2000
o0
o
I.
10
1000
750
50
0
1000
every
50
u,
500
-75ug/ml
FGF-SOS
-75ug/ml
FGF Alone
150
100
Penetration Distance (urn)
200
(A)Band
75ug/ml (B).
Error bars
-75ug/m300ug/ml
were only shown
atOS at
FGF2-SOS
and
-transport.
FGF2
ofFGF2
distribution
every 50pgm.
120
5.4 Discussion
5.4.1 Binding reduces effective diffusivity, but can be modulated by protective groups
Drugs diffusing through myocardium can bind to both their specific receptors and to
general fixed tissue binding sites
8.
The equilibrium between on-off binding reactions translates
into a concentration dependent partition coefficient and a concentration dependent hindrance of
myocardial transport. Our data show that the density of binding sites for FGF2 in myocardial
tissue is so overwhelming that equilibrium distribution in a 8-10 mm 3 plug of tissue is not
reached even after several days. As source concentration was raised, more and more tissue
binding sites were saturated and only then was FGF able to penetrate deeper part of tissue (Fig.
IB). This implies that binding hindrance accounts for a significantly lower effective diffusivity,
several orders of magnitude lower than would be expected for a molecule the size of FGF2 in the
myocardium. Our data also suggest that it is possible to circumvent poor FGF penetration by
increasing the delivery dose (Fig. 1A), similar to the case of targeting tumor micrometastases
with monoclonal antibodies 4
Our studies are the first to report the "binding site barrier" effect of FGF transport in
myocardium. This effect is between 1-4 fold lower than that reported for FGF in heparin sulfate
rich Descemet's membrane 9 as analyzed by Tzafriri et.al
20.
These results are reasonable for
extracellular-space-confined FGF as Descemet's membrane is likely to be richer in heparan
sulfate content than myocardial extracellular matrix. Nevertheless, the effect of binding on FGF
transport in myocardium is highly significant and likely accounts for 500 folds lower in
diffusivity of non-binding FGF. FGF binding to the myocardium is then a double edged sword,
121
enhancing uptake in the superficial regions of the tissue, but markedly reducing effective
diffusivity and severely limiting tissue penetration. Thus, modulation of FGF binding to the
myocardium may improve the efficacy of pro-angiogenic therapy with FGF.
It is therefore significant that we have shown that the adverse effects of binding on
myocardial transport can be dampened by flooding the tissue with high concentrations of drug or
by using protective groups such as SOS or various types of heparins. While delivering high FGF
concentrations might give rise to toxicity, the use of protective groups can be promising if done
with care. Foremost, protective groups must not adversely affect biological activity. The
specific binding activity of the drug to its receptor (e.g., FGF2 to FGFR) should not be perturbed.
In general, conjugation of FGF to another molecule can alter its general as well as specific
binding. In this case, the reduction in binding is likely limited to general tissue binding (eg., to
HSPGs). Since SOS does not reduce FGF2 biological effect in vitro 23,24, our data suggest that
SOS primarily blocks general binding only. Indeed, some studies suggest that SOS actually
enhances FGF2 activity 23, 24, through imitating heparin role, promoting FGFR dimerization and
increasing FGF-FGFR affinity, hence potentiates FGF intracellular signaling. Second, protective
groups must not be so large as to increase the steric hindrance experienced by the drug. For
example, using unfractionated heparins (UFH) as a protective group for FGF2, while protecting
against capillary washout and proteolysis, may actually slow drug penetration due to the large
size of the FGF2-UFH complex (well above 100 kDa, Fig. 6, Chapter 2). SOS conjugation
presents an attractive approach to improve pro-angiogenic therapy with FGF by enhancing not
only cellular PK
23, 24,
but also tissue PK by minimizing general tissue binding and maximizing
tissue penetration and late uptake.
122
5.4.2 Implications for Angiogenic Growth Factor Delivery
We used the non-perfused myocardium model for the studies in this Chapter to highlight
the effects of tissue binding. However, in the in-vivo heart, binding and capillary washout act
simultaneously on FGF transport. Any gain in penetration depth as a result of binding
modulation to increase the free to bound fraction of FGF by increasing source concentration
would be dampened by the effect of microvascular flow (previous 3 chapters). Even higher
doses of drug must be delivered to overcome both binding and clearance impedance. The
myocardial and other vascularized tissue environment, therefore, present a remarkable challenge
for growth factor transport, and a possible reason for mixed success in pro-angiogenic therapy.
Conjugation of FGF to SOS is an attractive approach for minimizing the effects of
binding and of microvascular washout. SOS conjugation reduces general tissue binding by
neutralizing HSPG-FGF interactions and also induces dimerization of FGF and effectively
minimizes microvascular washout as shown in Chapter 2. This approach, however, can come at
a cost of doubling the molecular weight as FGF-SOS complex is twice the size of FGF, but this
2-fold increase in size is still significantly better than the >10-fold increase with the common use
of UFH as protective groups for FGFs. The slow transport as a result of increasing in steric
hindrance, however, may be overcome with using controlled release sources that can sustain
release for longer time. As shown in previous chapters, molecular washout hence transendothelial permeability is more dominant determinant of myocardial transport in-vivo and in the
presence of angiogenic response, SOS conjugation provides a possible modulation of transendothelial permeability of FGF while also overcoming transport impedance due to general
123
tissue binding.
Furthermore, our results in this Chapter also raise an important implication specific to
pro-angiogenic therapy. As capillaries sprout and grow in response to angiogenic therapy, they
can retard drug penetration not only by clearing drugs, as highlighted in the previous chapters,
but also further by increasing specific and non-specific binding sites to drugs. This is because
blood vessels are lined with HSPG rich basement membranes. The increase in vascularity as a
result of successful therapy potentially results in a stronger negative feedback response than
predicted in Chapter 4, ultimately limiting the very angiogenic process the treatment is trying to
promote. This negative feedback could additionally account for the challenge of achieving
sustained therapeutic angiogenesis in clinical trials. The increase in binding site density may not
be a simple linear function of vascularity and may also drastically over time, which can introduce
additional complexity to the system. The full implications of this effect, therefore, merit detailed
investigation.
124
5.5 Summary
Tissue binding further complicates the complex local myocardial pharmacokinetics of
angiogenic growth factors described in previous chapters. Specific and general binding act as
double-edged swords, increasing local tissue uptake while drastically restricting tissue
penetration. Protective groups, if carefully selected, act to curtail the "binding site barrier"
problem. Growth factor formulation and engineering myocardial drug delivery systems based on
careful analysis of local myocardial pharmacokinetics and pharmacodynamics can improve drug
penetration and potentially angiogenic therapy outcome.
125
5.6 References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Baxter LT, Zhu H, Mackensen DG, Jain RK. Physiologically based pharmacokinetic
model for specific and nonspecific monoclonal antibodies and fragments in normal
tissues and human tumor xenografts in nude mice. Cancer Res. 1994; 54:1517-1528.
Juweid M, Neumann R, Paik C, Perez-Bacete MJ, Sato J, van Osdol W, Weinstein JN.
Micropharmacology of monoclonal antibodies in solid tumors: direct experimental
evidence for a binding site barrier. Cancer Res. 1992; 52:5144-5153.
Netti PA, Berk DA, Swartz MA, Grodzinsky AJ, Jain RK. Role of extracellular matrix
assembly in interstitial transport in solid tumors. Cancer Res. 2000; 60:2497-2503.
Saga T, Neumann RD, Heya T, Sato J, Kinuya S, Le N, Paik CH, Weinstein JN.
Targeting cancer micrometastases with monoclonal antibodies: a binding-site barrier.
Proc Natl Acad Sci U S A. 1995; 92:8999-9003.
van Osdol W, Fujimori K, Weinstein JN. An analysis of monoclonal antibody
distribution in microscopic tumor nodules: consequences of a "binding site barrier".
Cancer Res. 1991; 51:4776-4784.
Rosengart TK, Johnson WV, Friesel R, Clark R, Maciag T. Heparin protects heparinbinding growth factor-I from proteolytic inactivation in vitro. Biochem Biophys Res
Commun. 1988; 152:432-440.
Filion RJ, Popel AS. Intracoronary administration of FGF-2: a computational model of
myocardial deposition and retention. Am J Physiol Heart Circ Physiol. 2005; 288:H263279.
Bashkin P, Doctrow S, Klagsbrun M, Svahn CM, Folkman J, Vlodavsky I. Basic
fibroblast growth factor binds to subendothelial extracellular matrix and is released by
heparitinase and heparin-like molecules. Biochemistry. 1989; 28:1737-1743.
Dowd CJ, Cooney CL, Nugent MA. Heparan sulfate mediates bFGF transport through
basement membrane by diffusion with rapid reversible binding. J Biol Chem. 1999;
274:5236-5244.
Flaumenhaft R, Moscatelli D, Rifkin DB. Heparin and heparan sulfate increase the radius
of diffusion and action of basic fibroblast growth factor. J Cell Biol. 1990; 111:1651 1659.
Jaye M, Schlessinger J, Dionne CA. Fibroblast growth factor receptor tyrosine kinases:
molecular analysis and signal transduction. Biochim Biophys Acta. 1992; 1135:185-199.
Kardami E, Liu L, Pasumarthi SK, Doble BW, Cattini PA. Regulation of basic fibroblast
growth factor (bFGF) and FGF receptors in the heart. Ann N Y Acad Sci. 1995; 752:353369.
Liu L, Pasumarthi KB, Padua RR, Massaeli H, Fandrich RR, Pierce GN, Cattini PA,
Kardami E. Adult cardiomyocytes express functional high-affinity receptors for basic
fibroblast growth factor. Am J Physiol. 1995; 268:H1927-1938.
Sheikh F, Sontag DP, Fandrich RR, Kardami E, Cattini PA. Overexpression of FGF-2
increases cardiac myocyte viability after injury in isolated mouse hearts. Am J Physiol
Heart Circ Physiol. 2001; 280:H1039-1050.
Asundi VK, Keister BF, Stahl RC, Carey DJ. Developmental and cell-type-specific
expression of cell surface heparan sulfate proteoglycans in the rat heart. Exp Cell Res.
1997; 230:145-153.
126
16.
17.
18.
19.
20.
21.
22.
23.
24.
Li J, Shworak NW, Simons M. Increased responsiveness of hypoxic endothelial cells to
FGF2 is mediated by HIF-1 alpha-dependent regulation of enzymes involved in synthesis
of heparan sulfate FGF2-binding sites. J Cell Sci. 2002; 115:1951-1959.
Paul D. Effect of immobilizing adsorption on the diffusion time lag. Journal of Polymer
Science A-2. 1969; 7:1811-1818.
Crank J. The mathematics of diffusion. 2d ed. Oxford, [Eng]: Clarendon Press; 1979.
Briggs GE, Haldane JB. A Note on the Kinetics of Enzyme Action. Biochem J. 1925;
19:338-339.
Tzafriri A, Levin A, Edelman E. Diffusion-Limited Binding Explains Binary Dose
Response for Local Arterial and Tumor Drug Delivery. Cell Proliferation. 2008.
Elmalak O, Lovich MA, Edelman E. Correlation of transarterial transport of various
dextrans with their physicochemical properties. Biomaterials. 2000; 21:2263-2272.
Hwang CW, Edelman ER. Arterial ultrastructure influences transport of locally delivered
drugs. Circ Res. 2002; 90:826-832.
Yeh BK, Eliseenkova AV, Plotnikov AN, Green D, Pinnell J, Polat T, Gritli-Linde A,
Linhardt RJ, Mohammadi M. Structural basis for activation of fibroblast growth factor
signaling by sucrose octasulfate. Mol Cell Biol. 2002; 22:7184-7192.
Omitz DM, Herr AB, Nilsson M, Westman J, Svahn CM, Waksman G. FGF binding and
FGF receptor activation by synthetic heparan-derived di- and trisaccharides. Science.
1995; 268:432-436.
127
Chapter 6: Future Studies and Conclusions
6.1 Future Studies
This thesis attempted to identify and characterize the key determinants of local
pharmacokinetics and effects of angiogenic growth factors in myocardial tissue. In doing so, we
reported an important finding that growth factor deposition and tissue penetration are tightly
coupled to the growth factor pharmacodynamics through microvascular clearance. A
computational model of myocardial drug delivery and effect incorporating experimental
parameters and boundary conditions was constructed to predict tissue distribution of growth
factor concentration and biologic effect. This model predicts that steady state angiogenic effect
can be significantly affected by altering drug's trans-endothelial permeability and can be for used
as a basis for optimization studies.
As in any study of complex issues, the work in this thesis also raised several questions
that need to be addressed to further our understanding of local myocardial drug transport.
6.1.1 Characterization of Trans-endothelial Permeability in Myocardium.
The most important implication from our studies is that microvascular clearance acts as a
link between local myocardial pharmacokinetics and angiogenic pharmacodynamics.
Microvascular clearance is in turn affected by the vascular density and trans-endothelial
permeability. Since the goal of pro-angiogenic therapy is to maximize tissue vascularity,
controlling trans-endothelial permeability offers the most effective handle on the negative
pharmacodynamic feedback. Many experimental models have offered ways to quantify trans-
128
endothelial permeability. Permeability values of a-lactalbumin, a globular protein of comparable
size to FGF, were reported for frog mesenteric capillaries
1, 2 and
rat mesenteric capillaries 3
FGF's trans-endothelial permeability, however, has not been reported. Although it remains a
technical challenge to experimentally quantify myocardial capillary permeability of molecules, it
is important to be able to have an accurate assay for in-vivo permeability. This assay can provide
screening tool for evaluating drugs with favorable pharmacokinetic properties prior to
pharmacodynamics testing in costly animal experiments.
Furthermore, angiogenesis is a highly dynamic process in that vascular properties
including trans-endothelial permeability can change drastically. Such dynamic changes have not
been explored but its characterization would provide a better understanding of the temporal PKPD changes and suggest ways to design drug delivery strategy. For example, one can design a
drug controlled release profile to take advantage of the PK-PD changes and give appropriate
maintenance dose of growth factors to sustain long term chemotactic and survival signals for the
neo-vascularization.
129
6.1.2 Computational Models of Angiogenesis.
The angiogenic model created in this thesis is a simple mechanistic model in twodimensional space to provide both a proof of concept and a first order estimate of the angiogenic
response. There exist many models of angiogenesis of varying complexity in the literature
4-9.
A
unifying model remains to be explored. Since the biology of angiogenesis is an active area of
research and many the details of this process have not been fully defined. This is especially true
in the context of myocardial tissue. It is envisioned that a more detailed model of angiogenesis in
three dimensions can be coupled with local continuum pharmacokinetic model to provide a good
tool for predicting biologic response from any drug compound with any delivery modality.
6.1.3 Characterization of Effect of Binding
We attempted to characterize the effect of binding on growth factor transport in
myocardium using FGF as a model molecule. Although tissue binding was shown to have a
significant impact on FGF effective diffusivity, several questions remained unanswered. Since
the effect of binding on transport and deposition can be highly non-linear, tissue studies require
sensitive and high resolution assay of spatio-temporal distribution of FGF, its intermediate
binding complexes, tissue binding sites and biological response. Better knowledge of the effect
of binding on growth factor tissue transport can be included in our PK-PD to provide a more
comprehensive model to predict tissue response following local drug delivery.
130
Similar to trans-endothelial permeability, tissue binding sites may be altered drastically
during the angiogenic process and can further contribute to the negative pharmacodynamic
feedback. A high resolution characterization of binding site dynamics as a response to growth
factor delivery would be an important contribution in building a better PK-PD model of
angiogenic response following therapy.
131
6.2 Thesis Summary
Early enthusiasm over angiogenic therapy has been tempered by a series of failed clinical
trials with a wide range of mixed results. This thesis was designed to critically examine whether
the limited late efficacy of local delivery of angiogenic factors could be explained by a detailed
understanding of local pharmacokinetics and pharmacodynamics in the myocardial tissue. Our
combination of ex-vivo, in-vivo and computational modeling has provided novel insights into
local therapeutic angiogenesis and suggests that early success at inducing vessel growth
powerfully self-regulates angiogenic therapies by
dynamically altering local tissue
pharmacokinetic properties and imply that it may be possible to modulate the local
pharmacokinetics by better drug, drug formulation and drug delivery device designs.
132
6.3 References
1.
2.
3.
4.
5.
6.
7.
8.
9.
10.
11.
12.
13.
14.
15.
Fu BM, Shen S. Structural mechanisms of acute VEGF effect on microvessel
permeability. Am J Physiol Heart Circ Physiol. 2003; 284:H2124-2135.
Huxley VH, Curry FE, Adamson RH. Quantitative fluorescence microscopy on single
capillaries: alpha-lactalbumin transport. Am J Physiol. 1987; 252:H188-197.
Zeng M, Zhang H, Lowell C, He P. Tumor necrosis factor-alpha-induced leukocyte
adhesion and microvessel permeability. Am J Physiol Heart Circ Physiol. 2002;
283:H2420-2430.
Balding D, McElwain DL. A mathematical model of tumour-induced capillary growth. J
Theor Biol. 1985; 114:53-73.
Bauer AL, Jackson TL, Jiang Y. A cell-based model exhibiting branching and
anastomosis during tumor-induced angiogenesis. Biophys J. 2007; 92:3105-3121.
Byrne HM, Chaplain MA. Mathematical models for tumour angiogenesis: numerical
simulations and nonlinear wave solutions. Bull Math Biol. 1995; 57:461-486.
Levine HA, Sleeman BD, Nilsen-Hamilton M. A mathematical model for the roles of
pericytes and macrophages in the initiation of angiogenesis. I. The role of protease
inhibitors in preventing angiogenesis. Math Biosci. 2000; 168:77-115.
McDougall SR, Anderson AR, Chaplain MA. Mathematical modelling of dynamic
adaptive tumour-induced angiogenesis: clinical implications and therapeutic targeting
strategies. J Theor Biol. 2006; 241:564-589.
Milde F, Bergdorf M, Koumoutsakos P. A hybrid model for three-dimensional
simulations of sprouting angiogenesis. Biophys J. 2008; 95:3146-3160.
Fannon M, Forsten KE, Nugent MA. Potentiation and inhibition of bFGF binding by
heparin: a model for regulation of cellular response. Biochemistry. 2000; 39:1434-1445.
Forsten KE, Fannon M, Nugent MA. Potential mechanisms for the regulation of growth
factor binding by heparin. J Theor Biol. 2000; 205:215-230.
Forsten-Williams K, Chua CC, Nugent MA. The kinetics of FGF-2 binding to heparan
sulfate proteoglycans and MAP kinase signaling. J Theor Biol. 2005; 233:483-499.
Richardson TP, Trinkaus-Randall V, Nugent MA. Regulation of basic fibroblast growth
factor binding and activity by cell density and heparan sulfate. J Biol Chem. 1999;
274:13534-13540.
Sperinde GV, Nugent MA. Heparan sulfate proteoglycans control intracellular processing
of bFGF in vascular smooth muscle cells. Biochemistry. 1998; 37:13153-13164.
Sperinde GV, Nugent MA. Mechanisms of fibroblast growth factor 2 intracellular
processing: a kinetic analysis of the role of heparan sulfate proteoglycans. Biochemistry.
2000; 39:3788-3796.
133
APPENDIX:
MATLAB code: PK-PD Model
%This program calls gencap.m and transport2d.m.
%Objective: to analyze sensitivity of Drug Distribution (or Deposition) vs.
%number of capillaries started with.
%Source location and flux are specified in transport2d.m
%Independent variables: D, R, numcap
%Variables to try: Flux, maxgrid
clear all;
warning('off');
rand('state',sum(100*clock));
%maximum computational grid dimension
maxgrid=200;
%um
gridsize=5;
%seconds
tscale=l;
% um^2/sec diffusivity
D run um = [0.1 1 10 100];
% sec/um % resistance 1/permeability
R run um = [1 10 100];
% initial cap density
numcap run = [50 100 200 400 800 2400];
functional delay run = [6/(60*24) 1/24 3/24]; % MEAN functional delay (time to become sink)
UNIT:DAYS
% threshold of sprouting unit: ng/ml
sprouting_threshold_run = [1 .1 .01 .001];
release rate run = [le-5 le-6 le-7 le-8 le-9 le-10 le-ll]; % Release rate unit: ngps
MONTECARLONUMBER = 10;
endtime = 3600*24*10*tscale;
YES = 1;
NO = 0;
Check for presence of old simulation files
% -------
paramfile = 'D_paramfile.mat';
fid = fopen(paramfile);
fclose('all');
foundparamfile = 0;
if (fid == -1) % NO Paramfiie, start new simulation
disp(['--> Starting new simulation.']);
disp([' ']);
old D loop=l;
old R loop=l;
old numcap loop=l;
oldfunctional delay loop=l;
old_sprouting threshold_loop=l;
old releaserateloop=l;
old N=l;
old 1=0;
else
%
Paramfile found,
load(paramfile);
disp(['--> Continuing simulation.']);
disp(['--> Paramfile located, re-starting from last saved file
disp([' ']);
load(filename);
old D loop=Dloop;
old R loop=R loop;
old numcap_loop=numcap_loop;
old_functional delay_loop=functional_delay_loop;
old_sprouting_threshold loop=sprouting_thresholdloop;
old releaserateloop=release rate loop;
old N=N;
old l=l+tscale;
foundparamfile = 1;
134
' filename
'.']);
% -----------------
end;
for numcap_loop = old_numcaploop:length(numcap_run)
numcap=numcap_run(numcap_loop);
for N = old N:MONTECARLONUMBER
for D_loop = old D_loop:length(Drun um)
% um^2/sec
DTissum = Drunum(D loop);
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%% CHANGE
for R loop = old R loop:length(R_run_um)
% sec/um
R um = Rrunum(R loop);
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
%%%%%%%%%%%55555%%%%%%%%%%%%%%%%%%%%% CHANGE
for functional delay loop = oldfunctional_delay_loop:length(functional_delayrun)
mean fdelay = 3600*24*functional_delay_run(fun
seconds
stdfdelay =
ctional_delay_loop); % MEAN func delay unit:
meanfdelay + 6*3600; % STDEV of func delay:
seconds
for sprouting_threshold_loop = old_sprouting_thresholdloop:length(sprouting thresholdrun)
sprouting_threshold = sprouting_threshold_run(sprouting_thresholdloop);% unit: ng/ml
for release_rate loop = oldrelease_rate_loop:length(release_rate_run)
release rate = release rate run(releaserate loop);
% unit: ngps
fileroot = ['KL D' num2str(DTissum) ' R' num2str(R_um) 'Cp' num2str(numcap) '_Fd'
num2str(meanfdelay) '_Ct' num2str(sprouting_threshold) '_RR' num2str(release_rate) '_N' ];
disp(['D ',
num2str(Drun_um(D_loop))]);
disp(['R ',
num2str(R_run_um(R_loop))]);
%disp(['capillary density ', num2str(numcaprun(numcap_loop))]);
%disp(['Functional Delay ', num2str(functionaldelay_run(functional_delay_loop))]);
%disp(['Sprouting Threshold ', num2str(sprouting_threshold_run(sprouting threshold_loop))]);
%disp(['Release Rate ', num2str(release_rate_run(releaserateloop))]);
%disp(['Montecarlo number ', num2str(N)]);
%disp(['P_age ', num2str(sum(sum(p_age)))]);
if
(foundparamfile == 1)
p=p;
foundparamfile == 2;
else
cummulative dcl = 0;
cummulative dcl2 = 0;
cummulative dr = 0;
cummulative cons =0;
135
cummulativedep =0;
cummulative P=0;
cummulative dr save =[];
cummulative dcl save =[1;
cummulative dcl save2 =[];
cummulative cons save =[];
cummulative dep save =[];
cummulative P save=[];
1 save =[];
c=zeros(maxgrid+2,maxgrid+2);
pl = gencap(maxgrid+2,maxgrid+2,numcap);
pl = l.-pl;
p = pl;
pnonsink = zeros(maxgrid+2);
page = (p>O) .* (2);
p resorp = zeros(maxgrid+2,maxgrid+2);
t sub = zeros(maxgrid+2,maxgrid+2);
t sub half = 3600*2 + rand(maxgrid+2)*3600*2*24;
fdelay = rand(maxgrid+2)*std_fdelay + mean fdelay;
end;
RUNTRANSPORT = YES;
DIFFERENTCAPILLARIES = YES;
for l=old l:endtime,
p(1:5,1:5) =0;
% TRANSPORT
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
if (DIFFERENTCAPILLARIES == YES)
RUNTRANSPORT = YES;
end;
if (RUNTRANSPORT == YES)
m ,
[c,percentchange,DCL_sum,DCL_sum2,DR]=transport2d(c,p,maxgrid,gridsize,tscale,DTissum,R_u
se rate);
end;
if
relea
(percentchange == 0)
RUNTRANSPORT = NO;
end;
% Tracking drug over time
cummulative dr = (cummulative dr + DR)
cummulative dcl = (cummulative dcl+ DCL sum)
cummulative dcl2 = (cummulative dcl2+ DCL_sum2)
cummulative dep = (sum(sum(c(2:maxgrid+1,2:maxgrid+l)*gridsize^3)));
cummulative cons = cummulative dr - (cummulative dep + cummulative_dcl2);
cummulative-P = sum(sum(p(2:maxgrid+1,2:maxgrid+l)));
if
mod(1,600)==0
1 save = [1 save 1];
cummulative
cummulative
cummulative
cummulative
cummulative
cummulative
end;
dr save = (cummulative dr save cummulative_dr]
dcl save = [cummulative dcl save cummulative dcl];
dcl save2 = [cummulative dcl save2 cummulativedcl2];
dep save = [cummulative_dep_save cummulative_dep];
cons save = [cummulativecons save cummulative_cons];
P save = [cummulative P save cummulative P];
if mod(l,3600)==0
%
%plot(1_save,cummulative dr save/max(cummulative dr save),'rx',l save,cummulative depsave/max(cu
mmulative dr save),'go',1_save,cummulative dcl save2/max(cummulative dr save),'mo',l_save,cummula
136
P save),'k
tive cons save/max(cummulative dr save),'ko',l_save,cummulative P save/max(cummulative
+');drawnow;
end
%
if mod(1,3600)==0
disp(['Time completed ', num2str(round(1/3600)),
end;
'hours']);
% ANGIOGENESIS %%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
DIFFERENTCAPILLARIES = NO;
rand mat0 l=get randmat2d(maxgrid);
[pr,fc] = pr2d(c,maxgrid,gridsize,tscale,sprouting threshold); %Calculate probability of
sprouting
p_new = pr>=randmat0 _1;
p nonsink = p_nonsink I (p new==l); %pnonsink: new but non-functional capillaries
%Calculating local concentration around p_nonsink
[avgC] = localconc(c,p_nonsink,maxgrid);
% Tracking age of new capillaries
p_age = page + ((avgC*lel2>sprouting_threshold).*(p_nonsink*tscale));
p_age = p age .* (1-presorp);
p_before = p;
% Determine if capillaries are functional
p(3:maxgrid,3:maxgrid) = (p(3:maxgrid,3:maxgrid)==l) I
((page(3:maxgrid,3:maxgrid) > fdelay(3:maxgrid,3:maxgrid)
(p(1:maxgrid-2,3:maxgrid)~=1)
&
(p(2:maxgrid-1,3:maxgrid)~=l)
&
(p(4:maxgrid+1,3:maxgrid)~-=l)
&
(p(5:maxgrid+2,3:maxgrid)~=1)
&
(p(3:maxgrid,l:maxgrid-2) =1)
&
(p(3:maxgrid,2:maxgrid-l)=l)
&
(p(3:maxgrid,4:maxgrid+l) =l)
&
(p(3:maxgrid,5:maxgrid+2)~=1)
&
...
..
..
...
...
...
...
p(1:5,1:5) = 0;
p_after = p;
p_diff = p_after - pbefore;
% Conserve drugs at new nodes where tissue --> capillary
if sum(sum(pdiff)) > 0
, 2:maxgrid+l) +
= c(l:maxgrid
, 2:maxgrid+l)
c(l:maxgrid
(p_diff(2:maxgrid+1,2:maxgrid+l)==l).*(c(2:maxgrid+1,2:maxgrid+l)/4);
= c(3:maxgrid+2 , 2:maxgrid+l) +
c(3:maxgrid+2 , 2:maxgrid+l)
(pdiff(2:maxgrid+l,2:maxgrid+l)==l).*(c(2:maxgrid+l,2:maxgrid+1)/4);
= c(2:maxgrid+l , l:maxgrid) +
c(2:maxgrid+l , 1:maxgrid)
(p_diff(2:maxgrid+l,2:maxgrid+l)==l).*(c(2:maxgrid+l,2:maxgrid+l)/4);
= c(2:maxgrid+l , 3:maxgrid+2) +
c(2:maxgrid+1 , 3:maxgrid+2)
(p diff(2:maxgrid+1,2:maxgrid+l)==l).*(c(2:maxgrid+l,2:maxgrid+l)/4);
c=c.*(l-p);
DIFFERENTCAPILLARIES = YES;
end;
%REGRESSION%%%%%%%%%%%%%%%%%%%%%%%%%%% %%%
[avgC] = localconc(c,p,maxgrid);
137
%unit conversion
ctngum3 = sprouting_threshold * le-12;
t sub = (avgC < ctngum3) .* (t_sub + tscale);
p before = p;
resorptioncondition = (t sub > t sub half);
(p - resorption_condition)
p = pl
p after = p;
p resorp = p before - p_after;
clear pt sub
p_rand ;
%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%%
if (1 <= 3600) & mod(1,600)==0 & (1-~=0)
filename = [fileroot wwnum2ipstr(N) '_tmin' num2str(round(1/60))
disp(['Completed ' filename]);
save(filename);save(paramfile,'filename');
disp(['Capillaries ', num2str(sum(sum(p)))]);
%
disp(['P_age ', num2str(sum(sum(p_age)))]);
%
end
if mod(1,7200)==0 & (l~=0)
filename = [fileroot wwnum2ipstr(N) ' thr' num2str(round(1/3600))
disp(['Completed ' filename]);
%
save(filename);save(paramfile,'filename');
disp(['Capillaries ', num2str(sum(sum(p)))]);
%
disp(['P age ', num2str(sum(sum(p_age)))]);
%
disp(['RR' num2str(releaserate) ' ' num2str(1/60)]);
%
'.mat'];
'.mat'];
end
if l==endtime
1 = 1;
old 1 = 1;
numcap loop=min(numcap_loop+l,length(numcap_run));
N=min(N+1,MONTECARLONUMBER);
Dloop=min(D_loop+l,length(D_run_um));
R loop=min(Rloop+l,length(R_run_um));
functional delay loop=min(functional delay_loop+l,length(functional_delay_run));
sproutingthreshold_loop=min(sprouting thresholdloop+l,length(sprouting_threshold_run));
releaserateloop=min(release_rateloop+l,length(release_rate_run));
filename = [fileroot wwnum2ipstr(N) '_thr' num2str(round(1/3600))
disp(['Completed ' filename]);
save(filename);save(paramfile,'filename');
disp(['Capillaries ', num2str(sum(sum(p)))]);
%
disp(['P_age ', num2str(sum(sum(p_age)))]);
%
disp(['RR' num2str(releaserate) ' ' num2str(1/60)]);
%
end;
end; % 1 loop ie time
cummulative
cummulative
cummulative
cummulative
cummulative
cummulative
dcl = 0;
dcl2 = 0;
dr = 0;
cons =0;
dep =0;
P=0;
cummulativedr save =[];
cummulative dcl save =[];
cummulative dcl save2 =[];
cummulative cons save =[];
cummulative dep save =[];
138
'.mat'];
end;
cummulative P save=[];
1 save =[];
c=zeros(maxgrid+2,maxgrid+2);
pl = gencap(maxgrid+2,maxgrid+2,numcap);
pl = l.-pl;
p = pl;
p nonsink = zeros(maxgrid+2);
page =
(p>O) .* (2);
p_resorp = zeros(maxgrid+2,maxgrid+2);
t sub = zeros(maxgrid+2,maxgrid+2);
t sub half = 3600*2 + rand(maxgrid+2)*3600*2*24;
fdelay = rand(maxgrid+2)*std_fdelay + mean_fdelay;
')
disp('
end; %release rateloop
%sprouting thresholdloop
end;
%functional_delay loop
end;
end; %R loop
end; %D loop
end; %MONTECARLONUMBER
end; %numcap loop
% Function Gencap
% capmatrix = gencap (totX,totY,numcap);
% totX is dimension in X direction, totY is dimension in Y direction,
% numcap is number of capillaries desired
% Generates 2D cross section of random capillaries, no two adjacent.
% Border of matrix has no capillaries (border is all l's)
% 1 = tissue, 0 = capillary
% IMPORTANT: BECAUSE OF NO TWO ADJACENT CONDITION, numcap should be
% much less than 1/3*(totX-2)*(totY-2), OR ELSE WILL NOT BE ABLE TO
% FIT IN ALL THE CAPILLARIES
function capmatrix = gencap (totX,totY,numcap);
if (numcap > 0.32*(totX-2)*(totY-2))
disp('WARNING: MAY NOT BE ABLE TO FIND SPOTS FOR ALL YOUR CAPILLARIES!');
end;
TRUE = 1;
FALSE = 0;
capmatrix = ones(totX,totY);
% Positions of spots that are caps
used X =
[0];
used Y =
[0];
% Resets random seed generator to clock
rand('state',sum(100*clock))
for count = l:numcap
approvedposition = FALSE;
spots tried = 0;
while ((approved_position == FALSE) & (spots_tried <= 2*totX*totY))
% Pick numbers between 2 to totX-1 or totY-1 inclusive
try X = round(rand*(totX-3))+2;
139
try Y = round(rand*(totY-3))+2;
spots_tried = spots_tried + 1;
% Find the relative displacement of the trial point from all of
% the other "good points" selected thus far
displace_X = abs(tryX - used_X);
displace_Y = abs(try_Y - used_Y);
tot displace = displace_X+displace_Y;
% If total displacement is greater than 1, accept
if min(tot displace > 1)
approved position = TRUE;
end;
end;
if (spots tried > 2*totX*totY)
disp(['Placed ' num2str(count) ' points.
break;
else
% Found a spot -> place it in capmatrix
capmatrix(try_X,try_Y) = 0;
used _X = [used X try X];
usedY = [used Y try Y];
end;
Cannot find more spots.']);
end;
function
[C,percentchange,DCLsum,DCL-sum2,DR]=transport2d(C,P,maxgrid,gridsize,tscale,DTiss-um,R-um,relea
se rate);
YES = 1;
NO = 0;
CAPILLARY IS SINK = YES;
dx = 1; % dx = 1 = gridsize microns
dy = 1; % dy = 1 = gridsize microns
% Size of simulation space: Each pixel = gridsize microns
x = maxgrid+2;
y = maxgrid+2;
% Scaling of Tissue Diffusion Constants
DTiss = DTiss um/(gridsize^2)*tscale; % Convert units into gridsizes and tscales
% Scaling of Endothelial Resistances
R = R um/tscale*gridsize; % Convert units into gridsizes and tscales
if (R um == 0)
DEnd = DTiss;
else
DEnd = dx/R; % Effective Endothelial Diffusion Constant
end;
% Scaling of Time Constants
dt raw = min([l dx^2/(4*max([DEnd DTiss]))]);
dt = 1/(ceil(l/dt raw));
% Scaling of Capillary constants
K = 0; % Inactivation constant
U = 0; % Uptake constant
DX = DTiss*ones(x-l,y-2); % Diffusivities in X
DY = DTiss*ones(x-2,y-l); % Diffusivities in Y
% Change Diffusion Matrices
DX(l:x-2,:) = DX(l:x-2,:) DX(2:x-l,:) = DX(2:x-l,:) DY(:,l:y-2) = DY(:,l:y-2) -
Based on Capillary Positions
P(2:x-1,2:y-1).*DX(l:x-2,:) + P(2:x-1,2:y-l)*DEnd;
P(2:x-1,2:y-1).*DX(2:x-l,:) + P(2:x-1,2:y-l)*DEnd;
P(2:x-1,2:y-1).*DY(:,l:y-2) + P(2:x-1,2:y-l)*DEnd;
140
DY(:,2:y-1) = DY(:,2:y-1) - P(2:x-1,2:y-1).*DY(:,2:y-1) + P(2:x-1,2:y-l)*DEnd;
%DTiss
%DEnd
%'dt/dx^2*DTiss'
%dt/dx^2*DTiss
%'dt/dx^2*DEnd'
%dt/dx^2*DEnd
%'dt*dx*DTiss'
%dt*dx*DTiss
%'dt*dx*DEnd'
%dt*dx*DEnd
% Find drug amount
olddrug = sum(sum(C(2:x-1,2:y-1)));
DCL sum = 0; DCL sum2=0;
DR = 0;
for fraction of tscale = 1: round(l/dt)
%Constant flux BC conditions
RR ngps = release_rate; %in ngps
%delta V = gridsize^3;
C(2,2)= C(2,2) + (RR ngps*tscale*dt)/gridsize^3; %C changes by delta_C due to released
substance
DR = DR + (RR ngps*tscale*dt);
% Impose Symmetry Boundary Conditions
C(1,:)
= C(2,:);
C(x,:)
= C(x-l,:);
C(:,l) = C(:,2);
C(:,y) = C(:,y-l);
% Impose Zero Boundary Conditions
%C(1,:)
%C(x,:)
%C(:,l)
%C(:,y)
= 0;
= 0;
= 0;
= 0;
% Calculate Drug Loss through Permeation into Capillary
DCL =
sum(sum((P(2:x-1,2:y-l)==l).*((dt*dx)*(DX(l:x-2,:).*C(:x-2,2:y
-1)
+ DX(2:x-
1,:).*C(3:x,2:y-1)) + (dt*dy)*(DY(:,l:y-2).*C(2:x-l,l:y-2) + DY(:,2:y-1).*C(2:x-1,3:y)))));
DCL sum = DCL sum + DCL;
% Diffuse
%C(2:x-1,2:y-1)
%'sum C*vol BEFORE Diffuse'
%sum(sum(C(2:x-1,2:y-l)*gridsize^3))
C(2:x-1,2:y-1) = C(2:x-1,2:y-1) + ...
(dt/dx^2)*(DX(1:x-2,:).*C(1:x-2,2:y-)-(DX(1:x-2,:)+DX(2:x-1,:)).*C(2:x-1,2:y-1)+DX(2:x1,:).*C(3:x,2:y-1)) + ...
(dt/dy^2)*(DY(:,1:y-2).*C(2:x-1,1:y-2)-(DY(:,l:y-2)+DY(:,2:y-1)).*C(2:x-1,2:y1)+DY(:,2:y-1).*C(2:x-1,3:y));
%C(2:x-1,2:y-1)
%'sum C*vol AFTER Diffuse'
%sum(sum(C(2:x-1,2:y-l)*gridsize^3))
DCL2 = sum(sum((C(2:x-1,2:y-1).*P(2:x-1,2:y-1))*gridsize^3));
DCL sum2 = DCL sum2 + DCL2;
% Impose Capillary Conditions;
(CAPILLARY IS SINK == YES)
C(2:x-1,2:y-1) = C(2:x-1,2:y-1) .* (1-P(2:x-1,2:y-1))
else
C(2:x-1,2:y-1) = C(2:x-1,2:y-1) - (dt*(K+U))*P(2:x-1,2:y-1).*C(2:x-1,2:y-1);
if
141
end;
%C(2:x-1,2:y-1)
%'sum C*vol AFTER Diffuse and SINK'
%sum(sum(C(2:x-1,2:y-l)*gridsize^3))
%
'sum C*vol + DCL'
%sum(sum(C(2:x-1,2:y-l)*gridsize^3)) + DCL_sum2
%'Permeability Matrix'
%P
end;
newdrug = sum(sum(C(2:x-1,2:y-1)));
% Check if steady state has been reached
if (olddrug > 0)
percentchange = 100*(newdrug-olddrug)/olddrug;
else
percentchange = 1;
end;
% in: c (concentration matrix)
% out: pr (probability matrix: probability of capillary formation at each position)
function [pr,fc] = pr2d(c,maxgrid,gridsize,tscale,sprouting threshold);
% Converting ng/um3 to ng/ml: ng/um3*(10^4um/lcm)^3
c-ngml=c*lel2;
% [ng/ml] threshold concentration 2 orders of mag below
ct=sprouting_threshold;
c saturation: 30-3000ng/ml vessel density increases significantly, 3000-30,000 does not produce
more vessels: Dellian M et.al.Am.J.Pathol 1996; Yuan & Tong's paper uses 5ng/ml
% constant control shape of fc curve
alpha=10;
fc=(c ngml>=ct).*(l-exp((-alpha)*(c_ngml-ct)));
Smax= 5e-4/3600; % (um.sec)^(-l);
pr=Smax*fc*tscale*gridsize^3;
% function newstr=wwnum2ipstr(num);
% Forms a string with leading zeros as in IPLab save format.
Output String
Input Number
% Examples:
0010
10
%
%
165
0165
function newstr=wwnum2ipstr(num);
if (num==0)
newstr='0000';
elseif (num<10)
newstr=['000' num2str(num)];
elseif (num<100)
newstr=['00' num2str(num)];
elseif (num<1000)
newstr=['0' num2str(num)];
else
newstr=num2str(num);
end
142