Current Issues in the Diagnosis of Developmental Language Disorders
advertisement

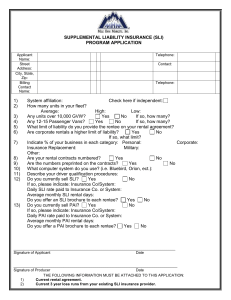
4/4/2016 Current Issues in the Diagnosis of Developmental Language Disorders Sean Redmond, PhD, CCC-SLP sean.redmond@health.utah.edu Shifting Terms and Taxonomies Diagnosis of Language Impairment Agenda Advances in Differential Diagnosis Break Comorbidities Advances in Assessment of LI in Bilingual Students Working Conclusions/Questions ? What should this profile be Research Participant (Blinded Examiner) called? 5;9 female Nonverbal Standard Score (NNAT): 92 Phonological Screening: Pass CELF-4 Standard Score: 56 Reading Standard Score (TOWRE-2): 100 TEGI elicited grammar composite [52%]: Standard Score: 25 CBCL ADHD: T Score 54 (within normal limits) 1 4/4/2016 Internet Resources https://www.youtube.com/user/RALLIcampaign http://www.asha.org/public/speech/disorders/LBLD/ https://www.nidcd.nih.gov/health/specific-language-impairment Shifting Terms and Taxonomies Initial recommendations for the new DSM 5 Communication Disorders section and ASHA’s response Special issue in International Journal of Language and Communication Disorders, July-August 2014 “Criteria and Terminology Applied to Language Impairments: Synthesizing the Evidence”: CATALISE consortium project DSM 5 Proposal “Communication Disorders - Restructured to now include Social Communication Disorder plus two diagnostic categories: Language Disorders and Speech Disorders. These categories each contain appropriate subtypes to cover all seven of the disorders previously proposed for this diagnostic category (Late Language Emergence; Specific Language Impairment; Social Communication Disorder; Voice Disorder; Speech-Sound Disorder; Motor Speech Disorder; Child Onset Fluency Disorder)”. Proposed Revisions for DSM-5, June 15, 2012 2 4/4/2016 ….However, we question the inclusion of SLI as a specifier. SLI is a controversial diagnosis that is not available in the vast majority of clinical settings. It is widely used in research, but consensus among language scientists on the robustness and validity of the category has not been reached. Nonverbal IQ is required to make the diagnosis of SLI, and this information is not available in many or most clinical settings. It is not best practice to rely on formal testing to make a diagnosis. The problems with formal tests are well-known and pervasive. For example, culturally and linguistic appropriate measures are not available for many children who are L2 English learners and speakers of nonstandard dialects. Therefore the diagnosis will not apply to many groups of children. In addition, a relatively small number of papers representing a relatively narrow view have been cited to support the proposed categories. The science is not sufficiently advanced and the controversies surrounding this label have not been laid to rest. Issues include the fact that nonverbal IQ declines with age (L. Leonard, 1998, Specific Language Impairment, Cambridge, MA: MIT Press), thus rendering the concept of the relation between IQ and language more difficult to understand, and the concern with the use of 85 as a cut-off IQ for normal functioning, which is higher than that used for determination of intellectual impairment. Recommendation ASHA recommends omitting Specific Language Impairment as a specifier of a language disorder. ASHA’s Recommended Revisions to the DSM-5, June 2012 (p. 15) BUT: S(P)CD is really SS(P)CD or “Specific Social (Pragmatic) Communication Disorder” because….. “..cases of intellectual disability and global developmental delay are excluded…. unless the communication deficits are clearly in excess of the intellectual limitations” (p. 49). BUT: This would require assessment of individual’s nonverbal IQ BUT: Notice also, the same IQ discrepancy criteria are still involved with DSM 5’s Language Disorder (p. 43). S(P)CD also excludes social/pragmatic problems which are the result of semantic or syntactic deficits (p. 48) – i.e. SLI. How common are language impairments? Tomblin, Smith, & Zhang (1997). Epidemiology of specific language impairment: Prenatal and perinatal risk factors. Journal of Communication Disorders, 30, 325-344. Nonverbal IQ + Language _ + _ Typical & Above “Spared Language” Low Cognition w/ TL 75% 11.9% “Specific Language Impairment” “Concomitant LI” Low Cognition w/ LI 8.1% 5.0% 3 4/4/2016 Speech delays? How common are language impairments? Tomblin, Smith, & Zhang (1997). Epidemiology of specific language impairment: Prenatal and perinatal risk factors. Journal of Communication Disorders, 30, 325-344. Shriberg,Tomblin, & McSweeny(1999). Prevalence of speech delay in 6-year-old children and comorbidity with language impairment. Journal of speech, Language, and Hearing Research, 42, 1451-1481. SLI: 8% CLI: 5% + Language _ Nonverbal IQ + _ Typical & Above “Spared Language” Low Cognition w/ TL 75% 11.9% “Specific Language Impairment” “Concomitant LI” Low Cognition w/ LI 8.1% 5.0% Classroom A Classroom D Classroom B Classroom E 2.3% 1.25% Classroom C SLI-CLI: 13.8% CLI-SLI: 10.5% Tomblin & Nippold (2014). Understanding Individual Differences in Language Development Across the School Years. pg. 124). Classroom A Classroom D Classroom B Classroom E Classroom C 4 4/4/2016 How big is the gap between SLI and CLI? Who receives SLP services? Zhang & Tomblin (2000). The association of intervention receipt with speechlanguage profiles and social-demographic variables. American Journal of SpeechLanguage Pathology, 11 (9), 345-357. 17% of LI cases were receiving services in kindergarten Who receives SLP services? Zhang & Tomblin (2000).The association of intervention receipt with speech-language profiles and social-demographic variables. American Journal of Speech-Language Pathology, 11 (9), 345-357. Morgan et al. (2016). Who receives speech/language services by 5 years of age in the United States? American Journal of Speech-Language Pathology, 25 (2), 1-17. Morgan et al. (2015). Minorities are disproportionately underrepresented in special education: Longitudinal evidence across five disability conditions. Educational Researcher, 44 (5), 278-292. SLI > (CLI+ Autism + Down Syndrome + Stuttering + Traumatic Brain Injury) Why haven’t we heard more about SLI? Bishop, D.V.M. (2010). Which neurodevelopmental disorders get researched and why? PLoS ONE, 5 (11), 1-9. Classroom A Classroom D Classroom B Classroom E Classroom C Classroom A Classroom D Classroom B Classroom E Classroom C LI + Speech White Have health insurance > Middle SES 5 4/4/2016 So if most children with SLI and CLI are not receiving SLP services then who are? One possibility is that within the clinical context, services are reserved for the most severe cases of LI….. ….. Or maybe not. Schmitt, et al. (2014) examined the correspondence between students’ symptoms of language disorder as measured by standardized assessment (grammar, vocabulary, listening comp, literacy) against goals on their IEPs. Schmitt, M.B., Justice, L.M., Logan, J.A., Schatschneider, C., & Bartlett C.W. (2014). Do the symptoms of language disorder align with treatment goals? An exploratory study of primary-grade students’ IEPs. Journal of Communication Disorders, 52, 99-110. There was no correspondence between students’ goals and their test profiles. For example, students with significant vocabulary deficits were as likely to have vocabulary goals as students whose vocabulary skills were within normal limits. Adjusting for different severity levels had no impact on the observed lack of correspondence. Another possibility is that our caseloads are overly burdened with students who do not have speech or language impairments but who have other problems that trigger referrals (e.g. Reading, Behavior Problems). Data from the Utah Verbal Screening Study 181 participants from the grades 1, 2, and 3 groups (mean age 8;1) LI defined as “CELF-4 core language < 85” during blinded assessment Combined parent report of services received with school records Ash, A., Pfaff, T., & Redmond, S. (2015). When language impairment isn’t enough: Factors that influence service status for school-age children. Poster presentation at the Symposium on Research in Child Language Disorders, University of Wisconsin, Madison SLP services +/ Other Conditions +/- “Typical Language” (n = 136) typically developing and “spared language” with other conditions “Language Impairment” (n = 45) SLI and concomitant LI with other conditions Mother’s NNAT Table 1. ParticipantEducation information: TL groups TL:SLP(n = 102) 56.9% male 86.3% Caucasian, non-Hispanic TL:SLP+ (n = 34) 70.6% male 85.3% Caucasian, non-Hispanic t-test (2, 134) CELF4 TEGI AWMA Reading Composite CCC-2 Pragmatic Composite CBCL ADHD 3.77 (.90) 2-5 110.20 (12.55) 82-145 104.79 (9.94) 87-123 98.32 (2.41) 89-100 101.61 (10.86) 78-124 106.30 (11.40) 80-132 42.60 (8.08) 11-57 53.22 (5.57) 50-75 3.62 (.82) 2-5 112.00 (16.60) 81-161 99.71 (8.89) 87-117 93.85 (16.32) 10-100 99.30 (11.27) 83-124 94.15 (13.77) 64-119 35.35 (9.99) 12-55 59.76 (8.64) 50-77 t = .900, p = .370 t = -.667 p = .506 t = 2.651 p = .009 t = 1.59 p = .121 t = 1.062 p = .290 t = 5.103 p = <.001 t = 4.260 p <.001 t = -4.142 p <.001 Mother’s Ed: 5-point scale of 1 = some high school; 3 = some college; 5 = advanced degree NNAT, CELF4 Core Language Score, AWMA, Reading Composite standard scores (M = 100; SD = 15) TEGI Early Grammatical Composite based upon percentage correct finiteness production CCC-2 Pragmatic Composite sum of pragmatic subscales (initiation, nonverbal communication, social relations, interests) CBCL ADHD T score (M = 50, SD = 10) 6 4/4/2016 Mother’s Education NNAT CELF4 TEGI AWMA Reading Composite LI:SLP(n = 14) 3.07 (.73) 2-4 96.64 (13.25) 83-125 75.93 (6.94) 62-85 90.71 (7.93) 71-100 88.75 (8.91) 74-102 90.46 (11.24) 71-108 LI:SLP+ (n = 31) 3.06 (.93) 1-5 92.19 (13.79) 73-125 67.19 (14.55) 42-85 77.16 (24.76) 4-100 85.22 (9.57) 71-105 79.21 (13.64) 54-102 42.9% male 71.4% Caucasian, nonHispanic 61.3% male 71% Caucasian, nonHispanic t-test (2, 43) t = .025, p = .981 t = 1.01, p = .316 t = 2.76, p = .009 t = 2.75, p = .009 t = 1.17, p = .248 t = 2.698, p = .010 CCC-2 Pragmatic Composite CBCL ADHD 38.29 (10.14) 16-49 59.64 (10.40) 50-75 35.94 (9.44) 17-54 57.68 (7.65) 50-75 t = .756, p = .454 t = .712, p = .481 Mother’s Ed: 5-point scale of 1 = some high school; 3 = some college; 5 = advanced degree NNAT, CELF4 Core Language Score, AWMA, Reading Composite standard scores (M = 100; SD = 15) TEGI Early Grammatical Composite based upon percentage correct finiteness production CCC-2 Pragmatic Composite sum of pragmatic subscales (initiation, nonverbal communication, social relations, interests) CBCL ADHD T score (M = 50, SD = 10) Demographic factors Chi Square Analysis: SLP+ in TL Sex: ns., Race and Ethnicity: n.s. Hx of Other Conditions (13% vs. 66.7%) [χ2 = 34.05, p <.001] Chi Square Analysis: SLP+ in LI Sex: n.s., Race and Ethnicity: n.s., Hx of Other Conditions, n.s. Backwards Stepwise Regression: SLP+ in TL Initial Analysis: Hx for Other Conditions, CELF-4, Reading, CCC-2 Pragmatics and CBCL ADHD Developmental factors Final Solution: HX for Other Conditions and Reading accounted for 39.2% of the variance [χ2 = 41.807, df = 2, N = 136, p <.001] Backward Stepwise Regression: SLP+ in LI Initial Analysis: CELF-4, TEGI, Reading Final Solution: Reading accounted for 20.6% of the variance [χ2 = 7.117, df = 1, N = 45, p = .008] In other words, on their own, the severity of children’s primary language symptoms did not affect their likelihood of receiving SLP services. Rather, the presence of reading difficulties and other clinical conditions predicted receipt of sLP services. 7 4/4/2016 LI TD Number of children How should we diagnose Language Disorders? Performance level Number of children Clinical marker distribution LI TD Performance level Brown’s 14 Morphemes Finite Verbal Forms Present progressive –ing Finite = TNS, AGR “tense marking” In Also includes: modal On auxiliaries, auxiliary DO Plural “s” and HAVE Irregular past tense Possessive “s” Uncontractible copula Articles We have known for at least 20 years that children with language impairments have difficulty with only a subset of Brown’s grammatical morphemes.. Regular past tense 3rd person regular present 3rd person irregular Uncontractible auxiliary Contractible copula Kamhi, A.G. (2014). Improving clinical practices for children with language and learning disorders. Language, Speech, and Hearing Services in Schools, 45, 92-103 Contractible auxiliary 8 4/4/2016 Ash, A.C., & Redmond, S.M.(2014). Using finiteness as a clinical marker to identify language impairment. Perspectives on Language Learning and Education, 21, 148-158. Pawlowska, M. (2014). Evaluation of three proposed markers for language impairment in English: A meta-analysis of diagnostic accuracy studies. Journal of Speech, Language, and Hearing Research, 57, 2261–2273. Adapting clinical markers into screeners for LI Redmond, S.M. (2005). Differentiating SLI from ADHD using children’s sentence recall and past tense morphology. Clinical Linguistics and Phonetics, 19, 109-127. Proposed clinical markers of language impairment: Grammar (tense-marking) Verbal Memory (nonword repetition, sentence recall) Ongoing Limitations: more unselected samples needed, independent blinded assessments needed Utah Verbal Screening Study (n = 1060) Ethnicity: 88.5% non-Hispanic, 10.7% Hispanic Race: 88.6% White; 4.1% Asian; 3.9% Black; Native American 1.4%; 0.8% Pacific Islander Gender: 52% Male; 48% Female Screening Measures Sentence Recall (Redmond, 2005) Past Tense Marking (PT probe from Test of Early Grammatical Impairment) TEGI Protocol: https://cldp.ku.edu/ricewexler-tegi 9 4/4/2016 Not Screened 124 Not Returned 1399 Flyers Sent 2907 Parental Permission 1184 41% Absenteeism, Moved out of district, Student declined = 9 89.5% Screened 1060 Declined 313 Unmarked 11 Excluded 207 Bilingual, gifted/ELP, siblings, missing service information 80% Screened 1060 75.8% Passed 647 Included 853 Regular Ed. = 844 LD, CD, EBD, RD, Resource = 77 Pass/fail criteria for each age based on regular ed means (SDs) Failed 206 Cutoffs: “10%ile on one screener or 15%ile on both [PT, SR]” Supplemental Cases: Jordan District: 48 U of U Clinic: 3 Referred: 7 Passed 647 22% Failed 206 25% Confirmatory Testing (SLC) 144 PASSED: Confirmatory Testing 165 Confirmatory Testing (SLC) 52 FAILED: Confirmatory Testing 89 10 4/4/2016 I. Inter-rater Consistency (n = 50): #agreement/(#agreements/#disagreements) * 100 Sentence Recall: 98.8% [r = .990, p <.001] Reliability of Screeners Past Tense: 93.5% [r = .921, p <.001] II. Test-retest Reliability (n =37): < 4 weeks [M = 1.03, SD = 1.0] Sentence Recall: r = .946, p < .001 Past Tense: r = .905, p <.001 III. Screening-to-Confirmatory Testing Stability (n = 96): < 20 weeks [M = 14.72, SD = 4.31] Sentence Recall: r = .906, p < .001 Past Tense: r = .883, p <.001 Zero-order correlations among screeners and confirmatory measures (N = 254) Validity of Screeners SR PT CELF-4 TEGI SR -- PT .606*** -- CELF-4 .804*** .614*** -- TEGI .695*** .905*** .694*** -- *p <.05, **p <.01, ***p < .001 Zero-order correlations among screeners and confirmatory measures (N = 254) Validity of Screeners SR PT CELF-4 TEGI SR -- PT .606*** -- CELF-4 .804*** .614*** -- TEGI .695*** .905*** .694*** -- *p <.05, **p <.01, ***p < .001 11 4/4/2016 Zero-order correlations among screeners and demographic variables from those who participated in confirmatory testing (N = 254) SR SR PT -- Gender PT Gender Ethnicity Race -- .016 -.070 .091 -- .082 .606*** -.006 -- Ethnicity Race Age -.052 -.032 .065 .122 Age .274*** .220*** -- -.029 .108 -.007 -- *p <.05, **p <.01, ***p < .001 PASSED: Confirmatory Testing 165 FAILED: Confirmatory Testing 89 PASSED: Confirmatory Testing 165 FAILED: Confirmatory Testing 89 CORRECT REJECTION: 156 *LI/NON-LI status determined by CELF-4 core language score <85* MISS: 9 HIT: 59 FALSE ALARM: 30 CORRECT REJECTION: 156 Sensitivity = 87.87% Specificity = 83.51% PPV = 65.17% NPV = 95.15% *LI/NON-LI status determined by CELF-4 core language score <85* MISS: 9 HIT: 59 FALSE ALARM: 30 Atypical (LD, ADHD, EBD, Autism, head trauma/seizur es) 40% Typical Developing 60% 12 4/4/2016 A. CELF 4 < 85 Screening for Different definitions of LI (TL = 188, LI = 66) Sensitivity = 87.87% Specificity = 83.51% PPV = 65.17%, NPV = 95.15% C. “Receiving SLP services” (TL = 165, LI = 89) Sensitivity = 60.67% Specificity = 78.78% PPV = 60.67%, NPV= 78.78 % B. CELF 4 < 80 (TL = 203, LI = 51) Sensitivity = 92.15% Specificity = 79.31% PPV = 52.18%, NPV = 97.58% D. “2 of the following: CELF4 < 85, TEGI below criteria, CCC-2 < 85, SLP services” (TL = 185, LI = 69) Sensitivity = 82.61% Specificity = 82.70% PPV = 60.04%, NPV = 92.72% Clinical markers of S(P)CD have yet to be proposed. How should we diagnose S(P)CD? Rather there is a collection of pragmatic symptoms that are homologous to symptoms historically associated with autism. The S(P)CD designation is reserved for individuals who have these symptoms but do not meet the full criteria for autism. Suggested protocol (after ADOS and ADI-R ruled out autism): Children’s Communication Checklist-2 (use SDI) Test of Narrative Language (esp. story grammar items) Figurative language subtests Observational protocol (e.g. Prutting & Kirchner, 1983) Is it possible to have a “social skills” deficit that isn’t language based (e.g. impulsivity from ADHD, social anxiety/withdrawal)? What language measures would differentiate these from S(P)CD? “The identification of a specific disorder when several diagnoses are possible because of shared symptoms and signs” (McCauley, 2001). Differential Diagnosis Needed to address the threats of missed diagnosis, misdiagnosis, diagnostic overshadowing as well as offset potential educational and health disparities Needed for the clinical management of true comorbidity Needs clearly articulated diagnostic constructs Needs clinical markers and protocols that are capable of differentiating pediatric language disorders from other conditions 13 4/4/2016 SLP Textbooks [14]: Angell (2009); Bernstein & Tigerman-Farber (2009); Farber & Radziekicz (2008); Hedge (2006); Kaderavek (2011), Lahey (1988); McCauley (2001); Nelson (2010); Owens (2014); Paul & Norbury (2012); Pence & Justice (2008); Tomblin et al (2002); Yoder (1988) 8 A Neglected Topic in SLP pre-professional training… 7 Differential diagnosis is not covered on ASHA’s online portal/practice issues 6 5 4 3 2 1 0 Not Mentioned Less than a Paragraph 1-2 Paragraphs > 2 Paragraphs ADHD Differentiating Language Disorder from ADHD “Developmentally inappropriate levels of inattention, hyperactivity, and impulsivity” DSM5: symptoms must be present in non-academic contexts. ADHD Parent-rated behavior, Visuospatial Memory, Speaking rate, Vocal abuse, Mazes SLI “Diminished language proficiencies in the absence of significant limitations in hearing acuity, cognitive development, or social development” SLI Reading, Academics, Teacher-rated behavior, Peer Difficulties, Pragmatics, CPT, EF Tense-Marking, Nonword Rep., Sentence Recall, Verbal Memory, Narratives 14 4/4/2016 References* Diagnostically Neutral Symptoms and Signs: Barkley (2006); Brock & Knapp, (1996); Camarata & Gibson (1999); Cardy et al., (2010); Catts et al., (2002); Charach et al., (2009); Conti-Ramsden & Botting (2004); Finneran, Francis, & Leonard (2009); Henry, Messer, & Nash (2012); Humphrey, Storch, & Gefken, 2007; Johnson et al., (2002); Knox & Conti-Ramsden (2007); Milberger et al., (1995); Nigg et al., (2005); Parriger (2012); Rabiner & Cole, 2000; Redmond (2011); Redmond & Rice (1998); Redmond & Rice (2001); Riccio & Jemison (1998); Riccio, Reynolds, & Lowe (2001); Reilly et al (1999); Spaulding, Plante, & Farinella (2006); Wiener & Mak, 2009; Willcutt et al., (2005); Willoughby & Blair (2011); Zelnik et al. (2012) Clinical Markers SLI: Archibald & Joanisse,(2009); Bishop, North, & Donlan, (1996); Conti-Ramsden, (2003); Conti-Ramsden, Botting, & Faragher (2001); Dollaghan & Campbell, (1998); Leonard (2014); Oram et al., (1999); Palowska (2014); Parriger (2012); Rice, Wexler, & Cleave, (1995); Rice, Wexler, & Hershberger (1998); Redmond, Thompson, & Goldstein (2011);SLI Consortium (2002); Spaulding et al., 2006; TagerFlusberg & Cooper (1999) Clinical Markers ADHD: Barkley (2006); Biederman, Keenan, & Farone (1990); Garcia-Real et al., (2013); Hamdan et al., (2009); Martinussen et al., (2005); Merwood et al., (2013); Nigg (2006); Redmond (2004); Redmond & Ash (2014); Rooderyns (2006) *Redmond, S.M. (2016). “Language impairment in the Attention-Deficit/Hyperactivity Disorder context.” Journal of Speech Language Hearing Research, 59, 133-142. X (Other Conditions) Disassociation Table Rice, M.L. (2016). Specific language impairment, nonverbal IQ, attentiondeficit/hyperactivity disorder, autism spectrum disorder, cochlear implants, bilingualism and dialectical variants: Defining the boundaries, clarifying conditions, and sorting out causes. Journal of Speech, Language, and Hearing Research, 59 (1), 122-132 + + _ Typical & Above “Spared Language” TL w/ X “Specific Language Impairment” “Concomitant X+LI” Language _ Sometimes referred to in the literature as “non-specific language impairment (NLI)” Language Impairment + Low Nonverbal IQ Standardized tests, narratives: NLI lower than SLI (Wetherell, Botting, & Conti-Ramsden, 2007; Tomblin & Nippold, 2014) Tense marking: NLI lower and slower than SLI (Rice, Tomblin, Hoffman, Richman, & Marquis, 2004). Expository samples: NLI = SLI (Nippold, Mansfield, Billow, & Tomblin, 2008). NLI increased risk for socioemotional behavioral problems (e.g. ADHD): (Elbro et al., 2009; Snowling et al, 2006) NLI increased risk for reading problems: (Bishop & Adams, 1990; Catts, Fey, Tomblin, & Zhang, 2002). Children with NLI less responsive to reading interventions: (Bowyer-Crane et al., 2011) Children with NLI and SLI may respond differently to language intervention strategies… (Goorhuis-Brouwer & Knijff, 2002) ….or maybe not (Bowyer-Crane et al., 2011; Cole, Dale, & Mills, 1990; Fey, Long, & Cleave, 1994). BUT: small study samples and moderate treatment effects limit synthesis. NLI = SLI + “spared language” with low cognition i.e. low nonverbal IQ and LI are additive comorbid disorders 15 4/4/2016 Language Impairment + Reading Disability Tense marking, nonword repetition, standardized language tests: SLI+RD = SLI (Bishop et al., 2009; Catts et al., 2005). Standardized reading tests: SLI+ RD = RD (Bishop et al., 2009; Catts et al., 2005). SLI+ RD increased risk for teacher (not parent) reported behavior problems (Tomblin, Zhang, Buckwalter, & Catts, 2000). SLI+RD = SLI. i.e. LI and RD are non-additive, non-interactive comorbid disorders Language Impairment + ADHD Standardized tests, tense marking, nonword repetition, sentence recall: ADHD+LI = SLI (Redmond, Ash, & Hogan, 2015). Modest (but significant) positive correlations (were found between ADHD symptoms and some of the language measures. ADHD is protective?? Narratives: ADHD+LI = SLI (standardized scores on TNL)…..but children with ADHD+LI may have fewer story grammar elements than SLI (Hamilton, Ruetschle, Mong, Timler, & Redmond, 2015). Peer victimization: Elevated ADHD symptoms in SLI study samples associated with higher rates of peer victimization (i.e. being bullied) (Redmond, 2011) Impact on Intervention: ADHD+LI more likely to receive SLP services than SLI (Sciberras et al., 2014) Paradis, Emmerzael, & Sorensen. (2010). Assessment of English Language Learners: Using Parent Report on First Language Development. Journal of Communication Disorders, 43, 474497. Alberta Language and Development Questionnaire (ALDeQ) Parents compare their child to other ELL children they know Early language milestones and family history items in particular differentiated Bi-SLI from Bi-TD http://www.linguistics.ualberta.ca/en/CHESL_Centre/~/media/ling uistics/Media/CHESL/Documents/Paradis_ALDeQ_15Apr11.pdf 16 4/4/2016 The common reality of mixed dominance in bilinguals linguistic abilities challenges the traditional logic of “testing in the student’s dominant language”. BESA The Bilingual English-Spanish Assessment (BESA) protocol accommodates for mixed dominance. Age range: 4:0 to 6;11 Phonology, Morphosyntax (cloze, sentence recall) and Semantics (receptive, expressive) Subtests in both English and Spanish Morphosyntax subtests are designed around each language’s common LI symptoms Subtests standard scores based on child’s best performance (English or Spanish) Parent/Teacher questionnaires of language input/output used to determine if testing should be in Spanish, English, or both Administered by a bilingual examiner over 2-days (1 day for each language – Spanish first) Accuracy against reference standard [language samples measures + parent and teacher report + clinical observation] (Se = 92-96%, Sp = 85-92%). European COST Action IS0804 Measures of bilingual-SLI need to be able to accommodate a wide variety of language combinations Comprehension: Exhaustive Wh-Questions: “who (all) is holding a soccer ball; “who is giving what to whom” Elicitation: subject-verb agreement, case marking, object clitics Sentence repetition: negation, biclausal sentences, wh-questions, relative clauses Nonword repetition: a common “quasi-universal” list of words (2-5 syllables in length) built from CV syllables from a limited range of common phonemes (e.g. zibalita). Native informants select 16 from the set that are not a real word in their language. Carrizo & Redmond (under review) Could performance on the COST Action quasi-universal NWR predict children’s performance on the BESA subtests as well as their English, Spanish or Best NWR? What are the trade-offs involved in using percent whole word correct (PWWC) rather than percent phonemes correct (PCC)? 26 Spanish-English speaking bilingual children (5:0-6:11) (3 were receiving SLP services). 17 4/4/2016 Results: All of the NWR tasks were significantly and moderately-highly correlated with BESA subtests and Language Index Score Carrizo & Redmond (under review) cont’d PPC r range: 0.66 to 0.87 (higher values with Morphosyntax) PWWC r range: 0.5 to .76 (higher values with morphosyntax) Linear regression PPC: Quasi-universal NWR accounted for 85% of the variance on BESA Language Index Score Linear regression PWWC: Quasi-universal NWR and Best NWR accounted for 83% of the variance on BESA Language Index Score i.e. PPC with one NWR task was as good as PWWC with three (BEST NWR requires both Spanish and English to determine). This could be used by monolingual SPLS to screen for Bi-LI Our evidence base on the diagnosis of LI remains modest relative to what’s available for other neurodevelopmental disorders. Working Conclusions For now, grammatical and verbal memory measures represent our strongest choices for the diagnosis of LI and its differential diagnosis (other clinical conditions, bilingualism). More work is needed to complete the picture across the life-span There are ongoing disconnects between cases of LI identified by standardized, research-based protocols and cases identified in the field by SLPs. S(P)CD is currently a “safety net” designation for cases which don’t meet enough autism criteria but would benefit from services. Evidence that S(P)CD can be reliably differentiated from SLI, ADHD, Selective Mutism, neglect, PTSD, and other clinical conditions is needed. Concomitant impairments impact LI in different ways: Working Conclusions cont’d Low Nonverbal IQ and LI are additive disorders: lower language levels and slower growth than SLI; may be less-responsive to some kinds of therapy (mixed evidence) Reading Disorder and LI are non-additive, non-interactive disorders: same levels and growth as SLI; increased risk for teacher reported behavioral problems ADHD and LI are non-additive, non-interactive disorders: same levels as SLI; impact on growth unknown; may benefit from preferential access to SLP services; may be at increased risk for peer difficulties 18 4/4/2016 Working Conclusions cont’d The largest obstacle to advancing the diagnostic integrity of LI maybe ourselves. We (ASHA) need to do a better job of raising the public visibility of “language impairments”. Terminological disputes (SLI vs. LI vs. LLD vs. LBLD vs. CD) compromise the message and confuse parents. Educational/health disparities in receipt of LI services exist and will likely persist. Individuals with LI and their families need to have a stronger voice in the policies that affect them. We (ASHA) need to install mechanisms to keep track of rates of LI over time and across different regions. Aggregates of students “receiving SL/CD services” (cf. ASHA and USOE) can’t be used to advance these agendas. Updated, multi-site, epidemiological studies of LI are long overdue. 19