Pericardial Disease
advertisement
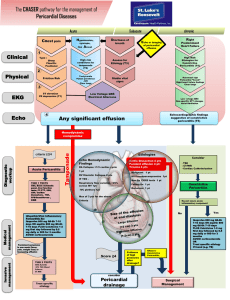
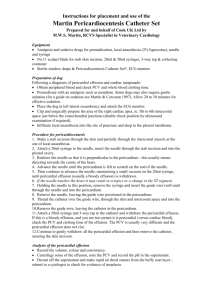
Pericardial Disease Susan A. Raaymakers, MPAS, PA-C, RDCS (AE)(PE) Radiologic and Imaging Sciences - Echocardiography Grand Valley State University, Grand Rapids, Michigan raaymasu@gvsu.edu Normal Pericardium For ARDMS Exam Three layers: Fibrous pericardium – thick outer sack Serous parietal – bound to fibrous pericardium smooth, ‘the wall of a cavity’ Serous visceral – bound to epicardium smooth, ‘toward the organ’ 5 to 10 ml pericardial fluid found in between the two serous layers Normal Pericardium Pericardial fluid is often appreciated as a very small echofree space in the posterior atrioventricular groove. Echo-free space between visceral and parietal pericardium (epicardium and fibrous pericardium) Visualized as a small anechoic space in the posterior AV groove that may be visible only in systole 09-001a-1b Feigenbaum Pericardial Diseases Can present as several different clinical scenarios Pericardial effusions can accumulate in any infectious or inflammatory process involving the pericardium Most infectious and inflammatory process involve both layers of the pericardium (visceral and parietal) Pericardial Diseases Pericardial space is limited Accumulation of significant pericardial fluid reduces the space that the heart may occupy Non-dynamic Pericardial Diseases Hemodynamic compromise is related to intrapericardial pressure Intrapericardial pressure is related to the volume of pericardial fluid and the COMPLIANCE OR DISTENSIBILITY of the pericardium Pericardial Diseases Slowly developing large effusions are better tolerated than a smaller but more rapidly developing effusion More rapidly developing effusion does not allow the heart to compromise 09-004a Feigenbaum Difference in pericardial pressures Rapid vs slow accumulation ACUTE PRESSURE VOLUME CHRONIC Detection and Quantification of Pericardial Fluid Detection and Quantification of Pericardial Fluid M-Mode Appears as anechoic space both anterior and posterior to the heart. Note: An isolated anterior free space is not specific for pericardial fluid. Isolated anterior anechoic space may be due to mediastinal fat Detection and Quantification of Pericardial Fluid M-Mode Size of anechoic space is directly proportional to the amount of fluid No accurate M-mode techniques for quantifying absolute volume of pericardial fluid Detection and Quantification of Pericardial Fluid 2D Most often used for screening Seen between Descending Ao and CS Most echocardiographic labs visually quantify pericardial effusion as: Minimal Small Moderate Large Further characterize: Either free or loculated Presence or absence of hemodynamic compromise Detection and Quantification of Pericardial Fluid Small Pericardial Effusion- 1 cm of posterior anechoic space with or w/out fluid accumulation elsewhere 09-003 Feigenbaum Minimal Pericardial Fluid - Normal 09-001a-1b Feigenbaum Detection and Quantification of Pericardial Fluid Large Pericardial Effusion – more than 2 cm of maximal separation 09-004b Feigenbaum Moderate Pericardial Effusion – 1 to 2 cm of anechoic space 09-004a Feigenbaum Minimal Pericardial Fluid Moderate Pericardial Effusion Small Pericardial Effusion Large Pericardial Effusion Large pericardial effusion: signs Soft heart sounds Reduced intensity of friction rub Ewart’s sign: Dullness and decreased breath sounds, over posterior L lung due to compression by large pericardial sac Electrical alternans on ECG Large pericardial effusion: signs Electrical alternans on ECG Large Pericardial Effusion and a Swinging Heart Large pericardial effusion In this image also a large pleural effusion 09-010a-10b Feigenbaum Detection and Quantification of Pericardial Fluid On 2D echo: pericardial effusion typically appears maximal in the posterior atrioventricular groove 09-004a Feigenbaum Use multiple views to reliably assess fluid including PSAX, Apicals, and Subcostals Detection and Quantification of Pericardial Fluid Small Pericardial Effusion – PSAX PM Large Pericardial Effusion – PSAX PM 09-007 Feigenbaum 09-006 Feigenbaum Detection and Quantification of Pericardial Fluid Moderate, predominately lateral pericardial effusion (PEF) Note PEF behind RA Mod to Large PEF w/greatest dimension lateral to LV free wall 09-009 Feigenbaum 09-008 Feigenbaum Detection and Quantification of Pericardial Fluid PEF may be localized or loculated rather than circumferential May occur after cardiac surgery or cardiac trauma Non-dynamic Loculated effusion at apex Non-dynamic Stranding and Fluid Accumulation Presence of fluid accumulation, masses and stranding Occur either on the visceral pericardium or the interior aspect of the parietal pericardium Fibrin strands are commonly seen in longstanding effusions or effusions from metastatic diseases 09-016 Feigenbaum Direct Visualization of the Pericardium 09-017 Feigenbaum Detection and Quantification of Pericardial Fluid Several schemes have been used for actual quantification of pericardial volume None have had universal clinical acceptance 3D echo may provide the most accurate technique for quantification and assessment 3D volume of entire pericardial space is calculated Overall total volume of the entire heart is calculated Pericardial fluid is calculated as the difference between entire pericardial space and overall total volume Little significance due to lack of 3D availability and lack of clinical need to determining precise pericardial volume Detection and Quantification of Pericardial Fluid 3D Pericardial Effusion 09-013b Feigenbaum Direct Visualization of the Pericardium Direct Visualization of the Pericardium Pleural effusion creates a fluid layer on either side of the pericardium In absence of pleural effusion exterior potion of parietal pericardium abuts the normal intrathoracic structures Therefore, thickness and character of the pericardium cannot be separated from the surrounding tissues When both pericardial and pleural effusions are present, thickness of pericardium in hat area can be assessed Direct Visualization of the Pericardium 09-010a-10b Feigenbaum Direct Visualization of the Pericardium Presence of calcific pericarditis may be marked shadowing seen posterior to pericardium Normal pericardium is highly reflective Hyperechoic pericardium alone should not be used to diagnose constrictive pericarditis 09-015 Feigenbaum Differentiation of Pericardial from Pleural Effusion Differentiation of Pericardial from Pleural Effusion Pleural effusion can be mistaken for pericardial effusion Fluid appearing exclusively behind the LA is more likely to represent pleural than pericardial effusion Pericardial reflections surround the pulmonary veins and tend to limit the potential space behind the LA Differentiation of Pericardial from Pleural Effusion Location of fluid-space with respect to descending thoracic aorta Pericardial reflection is typically anterior to the descending aorta Fluid appearing posterior to descending aorta more likely pleural Non-dynamic Hierarchy of Significant Pericardial Effusions Hierarchy of Hemodynamically Significant Pericardial Effusions 1. Exaggerated respiratory variation of tricuspid inflow 2. Exaggeration in mitral inflow 3. Right atrial collapse occurs at lower levels of intrapericardial pressure elevations than RVOT collapse 4. Right ventricular free wall collapse (may be seen in expiration but not inspiration with RV filling is increased) 5. When intrapericardial pressure is elevated and consistently exceeds intravascular pressures the above findings will be present simultaneously Hierarchy of Hemodynamically Significant Pericardial Effusions Instances with changes may not be seen: Significant RVH usually d/t pulmonary hypertension Thick, noncompliant RV wall is not compressed by modest elevation in pericardial pressure Thickening of the ventricular wall d/t malignancy, an overlying inflammatory respoinse or an overlying thrombus in a hemhorrhagic pericarditis Hypovolumia causing a low pressure tamponade Cardiac Tamponade Cardiac Tamponade Clinical diagnosis made at the bedside; Echo helps determine the amount and location of fluid Occurs mostly with moderate-to-large effusions although small, rapidly accumulated effusions may also cause tamponade Cardiac Tamponade Clinical Features Symptoms dyspnea, fatigue, cough, agitation and restlessness, syncope, and shock Physical examination pulsus paradoxus (may also be present in COPD patients or patients on ventilators) ECG may shows electrical alternans increased jugular venous pressure Beck’s triad Elevated venous pressure Hypotension Quiet heart Respiration Variation Review Respiration Variation Review: Inspiration: intrathoracic and intrapericardial pressures ↓ ↑flow into right heart ↑right ventricular filling and stroke volume ↓ flow to pulmonary veins Compensatory decrease in left ventricular stroke volume in early inspiration Respiration Variation Review: Expiration: Intrathoracic pressure and intrapericardial pressure ↑ Mild ↓ in RV diastolic filling ↑ in LV filling Respiration Variation Cyclic variation of LV and RV filling is sufficient to create mild changes in stroke volume (SV) and blood pressure Normal respiratory variation of SV results in ≤ 10 mmHg ↓ in systolic arterial systolic pressure with inspiration Processes that alter the respiratory cycle (i.e. COPD) ↑ work of breathing ↑intrathoracic pressure swings Alter variation of SV and arterial pulse pressure Cardiac Tamponade ↑ accumulation of pericardial fluid ↑ intrapericardial pressure and affects RV filling Overall effect of ↑volume of pericardial fluid limits total blood volume within four cardiac chambers Exaggerate the respiration-dependent ventricular volume If intrapericardial pressure >normal filling pressure, filling is determined by intrapericardial pressure Cardiac Tamponade LV has stiffer wall and diastolic filling is determined largely by active relaxation LV filling is relatively unaffected compared to RV filling In large pericardial effusions, elevation of interpericardial pressure inspiration results in disproportionately greater filling of RV than normal and leads to greater compromise of LV filling Pericardial Tamponade: Pathophysiology Increased intra-pericardial pressure Causing impaired diastolic filling Elevated venous pressure Exceeds ventricular diastolic pressure JVP, hepatomegaly, edema Dyspnea Decreased filling decreased stroke volume Reflex tachycardia, hypotension Cardiac Tamponade Marked exaggeration in phasic changes with respiration Greater decrease in systolic arterial blood pressure with inspiration Variation of BP with respiration called pulses paradoxus Cardiac Tamponade- Doppler Findings Under normal circumstances, peak velocity of mitral inflow varies by 15% with respiration and tricuspid by 25% Variation of aortic and pulmonary flow velocities vary less than 10% Cardiac Tamponade- Doppler Findings In presence of hemodynamically significant pericardial effusion: Respiratory variation is exaggerated above normal variation and therefore velocities are exaggerated Inspiration: ↑right↓left Expiration: ↓right ↑left Tricuspid Mitral Respiratory variation of tricuspid inflow > 50% Respiratory variation of mitral inflow > 30% Cardiac Tamponade- Doppler Findings Reciprocal and phasic variation respiration: physiologic evidence of exaggerated intraventricular interdependence Pulmonic Aortic Results: pulsus paradoxus Pulsus paradoxus Exaggerated (>10mmHg) cyclic decrease in systolic BP during normal inspiration Inspiration: increased venous return increased RV volume. Interventricular septum shifts left, decreased LV volume decreased stroke volume systolic pressure falls. Pulsus Paradoxus an exaggerated drop in SBP with inspiration (>10mmHg) Berliner Klinische Wochenschrift 1878; 10:461 Cardiac Tamponade- Doppler Findings Hepatic vein flow pattern may reflect exaggerated respiratory phase dependence of RV filling Note loss of forward flow in hepatic veins during expiratory phase (E) of respiratory cycle Flow is confined exclusively to early inspiratory (I) phase Cardiac Tamponade – Echocardiographic Findings Cardiac Tamponade- Echocardiographic Findings Signs of elevated intrapericardial pressure Diastolic right ventricular collapse Exaggerated right atrial collapse during atrial systole (ventricular diastole) ES: End-systole DC: Diastolic collapse RV Diastolic Collapse Cardiac Tamponade- Echocardiographic Findings Moderate Pericardial Effusion with hemodynamic compromise and diastolic RV collapse 9-22a & b Feigenbaum RV Compression With Large Pericardial Effusion Non-dynamic image Cardiac Tamponade- Echocardiographic Findings Hemodynamic significant pericardial effusion and right ventricular outflow tract collapse 9-23a & b Feigenbaum Cardiac Tamponade- Echocardiographic Findings Large pericardial effusion and evidence of right atrial collapse occurring immediately after normal atrial systolic contraction In the presence of marked elevation of intrapericardial pressure, right atrial wall will remain collapsed throughout atrial diastole 9-24 Feigenbaum IVC collapse IVC diameter decreases by > 50% if RA pressure normal Lack of IVC collapse indicates RA pressure > 20 mm Hg and restriction to diastolic filling No change in IVC diameter with inspiration Non-dynamic Evaluation of the inferior vena cava Other causes of IVC dilatation and failure to collapse Positive pressure ventilation Right heart failure Constrictive pericarditis Cardiac Tamponade Early stage mild to moderate elevation of central venous pressure Advanced stage intrapericardial pressure ventricular filling, stroke volume hypotension impaired organ perfusion Acute Tamponade Blood in pericardial space Complication of catheter or pacemaker procedures Post-surgical or traumatic Rupture heart or aorta into pericardial space Acute chest pain and dyspnea Volume of pericardial fluid may be low Life threatening Postoperative Effusions May occur post cardiac surgery, not uncommon Can range from small and self-limited to larger effusions Most often localized to the posterior and lateral aspects of the heart and may be loculated Complication of assessment: postoperative status of patient, pericardial fluid most likely is hemorrhagic and intrapericardial hematoma may be present 9-41 Feigenbaum Subacute Tamponade Neoplasm, uremia, infection Gradual onset chest pain, SOB, cough Effort intolerance due to limited cardiac output Can progress to cardiac arrest When to Treat Pericardial Effusion When to treat pericardial effusion? Tamponade is not an all-or-none-phenomena Echo more sensitive than clinical criteria Limited data exist with respect to the optimal timing of intervention for pericardial effusion Cardiogenic shock must be aggressively addressed Infusion of large volume of IV fluids may temporarily stabilize the patient Echo-guided Pericardiocentesis SAFE and EFFECTIVE Locating the optimal site of puncture Determining the depth of the pericardial effusion and the distance form the puncture site to the effusion Monitoring the results of the pericardiocentesis Treatment Options Nonsurgical pericardiocentesis Surgical subxiphoid blind video-assisted ECG guided thoracoscopy Echo guided pericardial-peritoneal CT guided pericardial window balloon pericardiotomy pericardiectomy Pericardiocentesis Diagnostic tap not always indicated Pericardial biopsy may be more definitive Therapeutic drainage indicated for tamponade Is this tamponade http://www.echojournal.org/video/64/Tampo nade Pericardiocentesis Non-dynamic Note approximately 1.5cm distance between the pericardium and RV free wall implying a significant distance between the pericardium and heart A significant distance may indicate a decreased risk of pericardiocentesis if approached from the subcostal position http://www.youtube.com/watch?v=koD2mEDoXSY Pericardiocentesis Nn-dynamic Many labs use echo guided pericardiocentesis and attempt to visualize needle as it enters the pericardial cavity Helpful to avoid cardiac damage in a relatively small effusion but may not play a big role in larger effusions Pericardiocentesis Contrast injection Non-dynamic images Contrast Pericardial effusion L Pre and post-pericardiocentesis Focal Tamponade Most often occurs after cardiac surgery May be difficult to diagnose on TTE Respiratory variation may also be focal TEE often necessary to make the diagnosis Constrictive Pericarditis Pericarditis Acute Pericarditis Infectious viral tuberculosis pyogenic bacterial (AKA bacterial pericarditis) Several different bacteria can cause this disease. Examples include staphylococci, group A streptococci (strept throat, scarlet fever), and the bacteria that cause Lime disease (tick) Acute Pericarditis Non-infectious Post-myocardial infarction Uremia Condition resulting from advanced stages of kidney failure in which urea and other nitrogen-containing wastes are found in the blood. Uremia can be caused by NSAIDs (nonsteroid antiinflammatory drugs), especially in older patients treated primarily with ibuprofen for arthritis. Treatment of uremia, which is directed at the underlying kidney disease, is usually with dialysis and renal transplantation. Neoplastic disease Acute Pericarditis Non-infectious – Continued… Radiation induced Connective tissue diseases Rheumatoid arthritis, Systemic Lupis Erythematous, Sclerodoma etc. Drug induced procainamide, hydralazine, isoniazid, methysergide, phenytoin, or anticoagulants Acute pericarditis: clinical findings Chest pain Pleuritic, positional, may mimic MI Fever, tachycardia, dyspnea Pericardial friction rub 3 component “scratchy” sound Abnormal ECG Diffuse ST elevation PR depression * Acute Pericarditis: Electrocardiogram Diffuse ST elevation PR depression Viral Pericarditis Coxsackievirus and Echovirus Enterovirus: found in alimentary canal (the intestines) of infected people Often diagnosed as idiopathic Seasonal variation Can occur with AIDS as a result of Cytomegalovirus (CMV) CMV: Common virus in the herpes virus family that affects 5085% of adults in the US by age 40. Found in saliva, urine, and other body fluids and can be spread through sexual contact or other more casual forms of physical contact such as kissing. Usually self-limited Complications: myocarditis, recurrence, tamponade, constriction Treat underlying disorder Viral Pericarditis The echo is usually normal especially during the first presentation Pericardial thickening, effusions and constriction are UNCOMMON TB Pericarditis Uncommon in US, except AIDS population Often bloody effusion Infection usually spread from chest lymph nodes Often progresses to constriction, calcification Bacterial Pericarditis Multiple Gram+ and Grambacteria can cause Previously complication from pneumonia, now more commonly seen post-op, with endocarditis, remote GI abscess or bacteremia Treatment is antibiotics tailored to organism Survival is only 30% Early surgical drainage is essential Uremic Pericarditis Uremia is a buildup of urea and other waste material in the blood due to kidney failure. Usually responds to aggressive hemodialysis Occasionally causes tamponade Usually accumulates slowly allowing pericardium to accommodate volume Large effusion not always be present on echo Malignant Pericarditis - Neoplastic Tumor or fluid may cause tamponade Lung, breast, lymphoma most common Overall mean survival 4 months Percutaneous drainage vs surgical window Large tumor fills pericardial space PL - pleural effusion T - tumor Non-dynamic Radiation Pericarditis Usually after treatment for Hodgkin’s, NHL and Breast CA Acutely sub-clinical Chronic - pain Constriction Restriction Drainage of fluid may not relieve symptoms Subcostal view - severely thickened pericardium A- ascites Non-dynamic Post-MI Pericarditis Dressler’s syndrome Acute illness occurring weeks to months after an MI Not Dressler’s if occurs early after MI Difficult to distinguish from recurrent MI in either case Cause unknown ?autoimmune Can be recurrent Can cause constriction Recurrent Pericarditis Incidence ~25% Treatment NSAID’s (non-steroidal anti-inflammatory) initially Steroids Rarely Colchicine Used to prevent or treat attacks of gout (also called gouty arthritis). People with gout have too much uric acid in their blood and joints. An attack of gout occurs when uric acid causes inflammation (pain, redness, swelling, and heat) in a joint. It prevents or relieves gout attacks by reducing inflammation Well Tolerated 60% effective long-term, more effective if taken chronically Fewer side effects than long-term steroids Constrictive pericarditis Fibrous thickening, adhesion, calcification of the pericardium Most common etiologies: TB Idiopathic Radiation therapy Long-term steroid use Chronic pericarditis (see etiologies for effusion) Constriction Fibrosis and/or calcification of pericarium results in restriction of diastole Equalization of RV and LV diastolic pressures by catheterization Treatment involves pericardiectomy Constrictive pericarditis: clinical findings Dyspnea Kussmaul’s sign (inspiration rise in venous pressure) Pericardial “knock” Abrupt cessation of early diastolic inflow (classic in constrictive pericarditis) Ascites Edema Constrictive pericarditis: Diagnosis Calcified pericardium on Xray Image thickened pericardium: CT scan, MRI Cardiac cath: Elevated, equalized diastolic pressures Restricted filling pattern in RV (“dip and plateau”) Calcified pericardium ANT MRI- Constriction RV LV Restriction of diastolic filling Brief rapid, fall of ventricular pressure in early diasotle, followed by •High early diastolic pressure plateau •Rapid descent of right atrial pressure with the onset of ventricular filling •Only modest elevation of RV and PA systolic pressures •RV diastolic plateau that is a third or more of systolic pressure •Equalizaiton of diastolic pressures in the RV and LV even after volume loading Echocardiographic signs of constriction Normal systolic function Thickened pericardium Flat LV posterior wall motion in diastole Early diastolic “notching” of the IVS Right and left atrial enlargement Dilated IVC – no inspiratory collapse Premature opening of the PV Constrictive pericarditis Posterior pericardium is adherent to posterior wall Diastolic septal bounce with inspiration • • • Non-dynamic Venous return increases leading to increased RV volume Total cardiac volume constrained by pericardium Interventricular dependence leads to septal shift Constrictive Pericarditis - Doppler Mitral and tricuspid regurgitation is usually present Mitral inflow has prominent E velocity, rapid deceleration and a small A wave Respiratory variation >25% in RV/LV diastolic filling Respiration and Constrictive Pericarditis Inspiration LVIT decreased >25% RVIT increased LVIT Expiration RVIT decreased >25% LVIT increased RVIT Constriction Treatment Medical management-palliative Diuretics to minimize edema Anti TB drugs x 4 weeks before surgery Surgical management-Pericardiectomy Mortality ~10% Symptomatic improvement 90% Poor Prognostic Indicators: NYHA class III or IV Incomplete resection Radiation induced Quiz 8 Questions All of the following may result in jugular venous distension EXCEPT: 1. 2. 3. 4. 5. Cardiac tamponade Pulmonary hypertension Tricuspid stenosis Hypovolemia Constrictive pericarditis All of the following may result in jugular venous distension EXCEPT: 1. 2. 3. 4. 5. Cardiac tamponade Pulmonary hypertension Tricuspid stenosis Hypovolemia Constrictive pericarditis An enlarged heart on chest x-ray could be all of the following EXCEPT: 1. 2. 3. 4. Pericardial effusion Pleural effusion Aortic stenosis Hypertrophic cardiomyopathy An enlarged heart on chest x-ray could be all of the following EXCEPT: 1. 2. 3. 4. Pericardial effusion Pleural effusion Aortic stenosis Hypertrophic cardiomyopathy What do you do if tamponade is suspected? What do you do if tamponade is suspected? Immediate interpretation. Do not let the patient leave the hospital/doctor’s office What causes a pericardial knock? What causes a pericardial knock? Abrupt cessation of early diastolic inflow (classic in constrictive pericarditis) Other than tamponade, what pericardial abnormality causes impaired ventricular filling? Other than tamponade, what pericardial abnormality causes impaired ventricular filling? Constrictive pericarditis A pericardial effusion can often be seen in patients with: 1. 2. 3. 4. Aortic stenosis Atrial flutter Myocardial infarction Renal failure A pericardial effusion can often be seen in patients with: 1. 2. 3. 4. Aortic stenosis Atrial flutter Myocardial infarction Renal failure Challenging Case Studies What would the cardiologist do? Susan A. Raaymakers, BS, RDCS (AE)(PE) Coordinator of Radiologic and Imaging Sciences - Echocardiography Grand Valley State University, Grand Rapids, Michigan raaymasu@gvsu.edu Echo-free Space 75 year old man with previous history of coronary artery disease and bypass surgery complained of dyspnea. Workup reviewed severe mitral regurgitation, and the patient underwent mitral valve replacement with a tissue prosthesis. There was no immediate postoperative problems. On the seventh post-operative day he developed dyspnea at rest and weakness. Physical examination was unremarkable. Echo-free Space A transthoracic echocardiogram was obtained. Based on these findings, you should order: 1. Follow-up echo in one week; drain if effusion increases or if more symptoms appear 2. Urgent needle pericardiocentesis (apical approach) 3. Urgent needle pericardiocentesis (parasternal approach) 4. Contrast echo 5. Anticoagulation with heparin, followed by warfarin (international normalized ratio = 2 to 3) Echo-free Space A transthoracic echocardiogram was obtained. Based on these findings, you should order: 1. Follow-up echo in one week; drain if effusion increases or if more symptoms appear 2. Urgent needle pericardiocentesis (apical approach) 3. Urgent needle pericardiocentesis (parasternal approach) 4. Contrast echo 5. Anticoagulation with heparin, followed by warfarin (international normalized ratio = 2 to 3) If you chose answers 1,2,3 or 5, you are in big trouble because the echo-free space between the left ventricle apex and the chest wall is a pseudoaneurysm of the LV.