Tumor cell extravasation in an in vitro microvascular network platform 2014 LIBRARIES
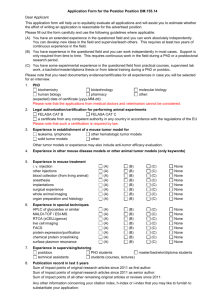
advertisement

Tumor cell extravasation in an in vitro microvascular network platform by MASSACHUSETTS INSTIUTE OF TECHNOLOGY Michelle B. Chen OCT 16 2014 B.S., Mechanical Engineering University of Toronto, 2012 LIBRARIES Submitted to the Department of Mechanical Engineering in Partial Fulfillment of the Requirements for the Degree of Master of Science in Mechanical Engineering at the Massachusetts Institute of Technology September 2014 2014 MIT. All rights reserved. The author hereby grants MIT permission to reproduce and to distribute publicly paper and electronic copies of this thesis document in whole or in any part medium now known or hereafter created. Signaure Of .Author: Certified by: Signature redacted Department of Mechanical Engineering August 8, 2014 Signature redacted Roger D. Kamm ],fessor of Mechanical and Biological Engineering -. 00 Accepted by: Signature redacted Thesis Supervisor David E. Hardt Professor of Mechanical Engineering Chairman, Committee for Graduate Students Tumor cell extravasation in an in vitro microvascular network platform Michelle B. Chen Submitted to the Department of Mechanical Engineering on August 8dI, 2014 in Partial Fulfillment of the Requirements for the Degree of Master of Science in Mechanical Engineering Abstract A deeper understanding of the mechanisms of tumor cell extravasation is essential in creating therapies that target this crucial step in cancer metastasis. Extravasation assays exist, but with limitations; data from in vivo models are frequently inferred from low-resolution end-point assays while most in vitro platforms are limited in their physiological relevance of the tumor microenvironment. To address this need, we developed a microfluidic platform to study tumor cell extravasation from in vitro microvascular networks formed via vasculogenesis. Various techniques to yield optimal networks were assessed in order to achieve an appropriate balance between vascular growth, remodeling and stabilization. These include the application of various soluble biochemical factors and both paracrine and juxtacrine co-culture with stromal cells. We demonstrate that out of all methods attempted, paracrine non-contact co-culture with human lung fibroblasts yield the most interconnected and stable networks. Vasculatures developed exhibit tight endothelial cell-cell junctions, basement membrane deposition and physiological values of vessel permeability. Employing our assay, we demonstrate impaired endothelial barrier function and increased extravasation efficiency with inflammatory cytokine stimulation, as well as positive correlations between the metastatic potentials of tumor cells lines and their extravasation capabilities. High-resolution time-lapse microscopy reveals the highly dynamic nature of extravasation events, beginning with thin tumor cell protrusions across the endothelium followed by extrusion of the remainder of the cell body through the formation of sub nuclear sized openings in the endothelial barrier. No disruption to endothelial cell-cell junctions is discernible at 60X, or by changes in local barrier function after completion of transmigration. Using our platform, we also elucidate the extravasation patterns of different tumor cell subpopulations, including mechanically lodged cells, single arrested non-trapped cells, and tumor cell clusters. Our platform offers key advantages over existing in vitro extravasation models by enabling all of the following: (1} high temporal and spatial resolution of extravasation events, (2) the ability to perform parametric studies in a tightly controlled and high throughput microenvironment and (3) increased physiological relevance compared to 2D and 3D planar monolayer models. Findings from our platform result in a deeper understanding of tumor cell extravasation mechanisms and demonstrate our assay's potential to be employed for the discovery of factors that could inhibit this crucial step in metastasis. Thesis supervisor. Roger D. Kamm Title: Professor of Mechanical and Biological Engineering Acknowledgements I would like to thank my advisor, Prof. Roger Kamm for his valuable guidance and insight throughout the course of my work. He has taught me what it means to be a good scientist and I am grateful that he has allowed me the opportunity to explore his lab and make a contribution to the scientific community. I would also like to thank the graduate students and post-docs who helped me along the way. In particular, I would like to thank Ran Li for countless insights on the biological side of things. Sebastien Uzel for his valuable expertise on microfluidics, troubleshooting, and for efforts in keeping the lab running smoothly each day. Jordan Whisler for teaching me everything there is to know about microvascular networks. Bill Polacheck for his wisdom on experiment and device design, and cell culture techniques. Lastly, I like to thank my family, as they continue to support me daily from 2000 miles away over the last 6 years of being away from home. My sister and mother have always encouraged me in their quirky yet heartfelt ways. My dad has taught me what it means to be an excellent and upright scientist and scholar, and that as long as I follow my passion even the hardest times will pass. Our countless discussions about my research, my trials and tribulations, and my direction in life have been my most valuable source of guidance. This work is supported by a National Science Foundation Graduate Research Fellowship. 3 List of Figures Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure Figure 1. The metastatic cascade ........................................................................................................ 2. Current extravasation assays................................................................................................10 3. Formation of microvasculature in vitro ............................................................................. 4. Device schematic ....................................................................................................................... 5. Vessel network quantification metrics ................................................................................ 6. Microvascular networks formed via HUVEC monoculture ........................................... 7. Vessel stability from HUVEC monoculture ...................................................................... 8. Increase in vessel diameter with application of various cytokines .................................. 9. Juxtacrine co-culture of HUVECs with HLFs .................................................................. 10. Microvascular network formation via non-contact HUVEC-HLF co-culture ........ 11. Formation of microvascular networks in microfluidic devices .................................... 12. Characterization of microfluidic microvascular network platform ............................. 13. Extravasation in jtVNs ...................................................................................................... 14. Visualization of MDA-MB-231 extravasation events ...................................................... 15. The effect of TNF-a on barrier function and TEM capabilities .................. 16. Correlation of metastatic potential and TEM capabilities ................................................. 17. Visualization of extravasation dynamics ........................................................................ 18. Dynamics of nuclear TEM ................................................................................................. 19. VE cadherin staining at extravasation sites ................................................................... 20. TEM efficiencies of different tumor cell subpopulations .................................................... 6 17 20 22 23 24 25 27 29 40 41 42 43 45 46 48 49 49 50 4 Table of Contents CHAPTER 1: INTRODUCTION ................................................................................................................. 1.1 The m etastatic cascade and extravasation .................................................................................. 1.2 Com parisons of existing extravasation m odels ......................................................................... 1.3 Objective and thesis overview .................................................................................................... Chapter 1 References ........................................................................................................................... 6 6 8 11 12 CHAPTER 2: IN VITRO MICROVASCULAR NETWORK FORMATION AND STABILIZATION 15 STRATEGIES ............................................................................................................................................. 2.1 Introduction......................................................................................................................................15 2.1.1 In vitro vascular network models - a potential tool for recapitulating the tumor cell extravasation m icroenvironment ..................................................................................................... 2.1.2 Vascular stabilization and regulation in vivo and in vitro ..................................................... 2.2 M ethods ............................................................................................................................................ 2.2.1 Assay design .............................................................................................................................. 2.2.2 Cells and device preparation .................................................................................................. 2.2.3 Fluorescent imaging and analysis.......................................................................................... 2.3 Results .............................................................................................................................................. 2.3.1 Vessel form ation and stability via HUVEC m onoculture ..................................................... 2.3.2 Cytokine cocktails ...................................................................................................................... 2.3.3 Co-culture with stromal cells (human lung fibroblasts) ....................................................... 2.3 Discussion ......................................................................................................................................... Chapter 2 references ............................................................................................................................. 15 17 19 19 21 22 23 23 24 26 29 30 CHAPTER 3: TUMOR-ENDOTHELIAL INTERACTIONS DURING EXTRAVASATION FROM IN 34 VITRO M ICROVASCULAR NETW ORKS ........................................................................................ 3.1 Introduction......................................................................................................................................34 36 3.2 M ethods ............................................................................................................................................ 36 3.2.1 M icrovascular network formation and maintenance ........................................................... 36 3.2.2 Tum or cell seeding in uVN s .................................................................................................. 37 ........................................................... 3.2.3 Tum or cell extravasation quantification and m etrics 38 3.2.4 TNF-a stim ulation of HUVECs .......................................................................................... 38 3.2.5 Calculation of vessel perm eability ........................................................................................ 39 3.2.6 Im m unofluorescent staining, imaging and imaging processing ............................................ 3.3 Results...............................................................................................................................................40 3.3.1 Formation, characterization and validation of microvascular networks via vasculogenesis .... 40 42 3.3.2 Tum or cell seeding and extravasation in m icrovascular networks......................................... 3.3.3 Effect of TNF-a on endothelial barrier function and transendothelial migration .................. 44 45 3.3.4 Correlation of tum or cell m etastatic potential with extravasation ability ............................ 46 3.3.5 Visualization of dynam ics of extravasation events .............................................................. 50 3.3.6 Transm igration of different tumor cell subpopulations.......................................................... 51 3.4 Discussion ......................................................................................................................................... Chapter 3 references..............................................................................................................................55 CHAPTER 4: CONCLUSIONS ................................................................................................................. Appendix 1: Vasculogenesis seeding protocol .................................................................................... 58 59 5 Chapter 1: Introduction and background 1.1 The metastatic cascade and extravasation In the early phases of tumor progression, cancer cells multiply near the site where they first began uncontrolled proliferation, and as a result, a primary tumor mass is formed. However, as insidious as these primary tumors are, they are ultimately responsible for only about 10% of the deaths from cancer [1]. The remaining 90% percent of patients are struck by metastasis, which is the growth of secondary tumors far from the primary origin. Cancer cells disseminate in the body by undergoing several steps, including the invasion of surrounding tissues of the primary tumor, intravasation into the blood vessel, transport in the circulation, extravasation from the vasculature and proliferation at a secondary site. Primary tumor 1. Invasion 2. Intravasation 3. Systemic dissemination Secondary tumor T 4E raasation 6. Colonization 5. Dormancy Weinberg, Seminars in Cancer Biology, 2012] Figure 1. The metastatic cascade. Tumor cells first detach from the primary tumor and invade into the surrounding tissue. Cells intravasate into a nearby blood vessel, circulate throughout the body and eventually arrests and extravasates at a distant organ where they proliferate and colonize, forming a secondary tumor. 6 At the primary tumor site, the initial phase of metastasis includes the loss of cellular contacts and acquisition of enhanced invasiveness and motility due to genetic and epigenetic alterations. Secretion of pro-angiogenic factors from the primary tumor results in the induction of tumor angiogenesis, allowing an entry point for tumor cells into the circulation - a process known as intravasation [1,2]. The few cells that successfully intravasate (also known as circulating tumor cells (CTCs)) must survive in the circulation before extravasating at a secondary site. Factors such as clearance by natural killer (NK) cells or other immune cells, as well as mechanical stresses such as shear due to blood flow may inhibit CTC survival in the circulation prior to extravasation [3]. Extravasation involves a cascade of events consisting of (1) tumor cell arrest on the endothelium resulting in the formation of dynamic contacts that give rise to significant cytoskeletal changes, and (2) tumor cell transendothelial migration (TEM) and subsequent invasion. There have been two general hypotheses regarding the mode of arrest of CTCs in a blood vessel: (1) mechanical trapping of cells and/or (2) active preferential adhesion of the tumor cell onto the endothelium at a distant organ. James Ewing proposed that metastasis at distant organs is dictated by the anatomy of the blood and lymphatic vessels and blood circulatory oaths between primary and secondary tumor sites [4]. CTCs are relatively large (-20 um) in diameter may become physically trapped in small vessel of the microcirculation, become activated, and eventually transmigrate [5]. However, Steven Paget's "seed and soil" hypothesis suggests that there exist interactions between different tumor cell types and specific organ microenvironments that guide their metastatic spread [6]. The vasculature of such organs may be primed with surface receptors/molecules or secrete chemokines that cause specific tumor cell types to preferentially "home and seed" at that particular tissue environment. For instance, breast cancer cells frequently metastasize to the bone [7,8]. Although two distinct phenomena have been described, is it clear now that the two theories may not be mutually exclusive; in fact, it has been suggested that tissue/organ tropism can be influenced both by physical trapping and interactions between "seed cells" and "receptive soils" [2,9]. Although the mechanisms of intravasation have been widely studied, the precise cellular interactions and molecular alterations associated with extravasation are poorly understood. In fact, most data are gathered from low-resolution in vivo studies and endpoint assays that 7 indirectly observe tumor cells via quantification of secondary tumor formation in existing animal models [10-14]. As such, direct observation of tumor cell arrest on and subsequent migration across an endothelium in a precisely controlled and physiologically relevant microenvironment would provide important insight into extravasation mechanisms and further enable the discovery of new anti-cancer agents to inhibit adhesion and/or transmigration of metastatic tumor cells, and break the metastatic cascade. 1.2 Comparisons of existing extravasation models Conventional studies of extravasation have been mostly limited to in vivo mouse models. Such platforms have allowed the investigation of genes involved in the metastatic cascade and proteins that mediate cancer invasion [15-17]. Mostly commonly used mouse models of metastasis include rat-tail vein, orthotopic, intracardial and subcutaneous injections. For instance, tumor cells can be injected intravenously and intravital microscopy can be employed to visualize the circulation of tumor cells in the vasculature and interactions with the metastatic organ [18,19]. Although these models allow for a high degree of physiological relevance, there remain a number of challenges associated with studying the underlying mechanisms of tumor cell extravasation. For example, probing the molecular mechanisms and cellular interactions is further complicated due to the adaptive response of the tumor microenvironment, such as the recruitment of immune cells. Real-time intravital imaging requires custom setups, which may perturb tumor pathophysiology [20]. Many in vivo assays are limited to end-point data collection and does allow for real-time high-resolution dynamic visualization of extravasation events. More recently, intravital microscopy performed on optically transparent transgenic zebra fish has enabled high spatial and temporal resolution imaging [13] (Fig 2A); however, as with most in vivo platforms, the ability to perform parametric high throughput studies in a tightly regulated microenvironment is restricted. The most commonly used and accepted in vitro model is the Boyden chamber/Transwell assay, which provide a relatively simple and high throughput method for parametric cell migration studies [21,22], and overcomes some limitations of in vivo experiments by increasing 8 throughput, ease of quantification of transmigration events and the ability to employ human cell culture (Fig 2B). However, these assays do not allow real time and high resolution monitoring of the entire process of extravasation due to its layered configuration. Moreover, the assay does not allow a high degree of control over the local environment and the 2D planar configuration is limited in its physiological relevance. Recently, the a new generation of in vitro extravasation platforms has emerged, in order to address the need for greater resolution, throughput, control of the cellular microenvironment and physiological relevance compared to traditional culture methods. Microfluidic technologies have revolutionized the field of cell biology by allowing 2 and 3D cell culture in highly controlled microenvironments coupled with benefits such as tunable spatio-temporal chemical gradients, relevant mechanical stress applications, complex interactions between different cell types and small reagent volumes [23-25]. Microfluidic devices have recently been employed enable high resolution and dynamic study of both tumor cell intravasation and extravasation [26-30]. For instance, the Takayama group described a microfluidic chip consisting of two chambers separated by a thin membrane onto which an endothelial monolayer is cultured [27] (Fig 2C). Tumor cell adhesion and arrest on the endothelium can be observed dynamically and in high resolution. It was demonstrated that breast cancer cell receptors CXCR4 and CXCR7 are involved in the adhesion of tumor cells to the endothelium [27]. Similarly, Shin et al developed a microfluidic platform to recapitulate the metastatic cascade on a single chip, beginning with intravasation followed by arrest and adhesion on an endothelial monolayer. It was demonstrated that E-selectin expression and shear stress values dictated the adhesion of colon cancer cells onto the endothelium [26]. Our group has previously described microfluidic devices consisting of microchannels connected by 3D ECM hydrogels, where tumor cells are seeded in one channel, arrest onto and extravasate across an endothelial cell (EC) monolayer and into a collagen gel. Tumor cell transmigration events were shown to occur in the first 24 hours and were accompanied with an increase in endothelial monolayer permeability [29] (Fig 2D). While this assay allows for high resolution and dynamic monitoring of extravasation events, the use of polydimethylsiloxane (PDMS) posts to contain the gel often prevents the formation of a continuous, low-permeable EC mono- layer. It is also difficult to predict how changes in stiffness 9 between the PDMS and gel affect extravasation mechanisms. Lastly, it is important to note that most studies of transendothelial migration across planar EC monolayers are limited in their physiological relevance. For instance, the barrier permeability values achieved are usually 1 to 2 orders of magnitude higher than those found in vivo, and the planar geometry does not allow recapitulation of physiological phenomena such as tumor cell trapping in the circulation [28,29,32]. Thus, there is a need for the development of in vitro tumor cell extravasation assays that encapsulates the capabilities delivered by microfluidic technologies, while delivering a higher degree of physiological relevance. EC MDAwt<FP MDAtwistaP b C d Figure 2. Current extravasation assays. (A) Transgenic zebrafish model enables high resolution in vivo observation of tumor cell arrest and extravasation, via perivascular tumor cell injection. (B) Schematic of Boyden Chamber assay: tumor cells are seeded on top of a membrane (or endothelial monolayer) and are allowed to migrate to the underside of the insert. (C) A microfluidic membrane device that allows flowing tumor cells to adhere and arrest on an endothelial monolayer. (D) An endothelial lined micro channel next to a collagen gel allows enables high resolution observation of tumor cell arrest and subsequent transendothelial migration. 10 1.3 Objective and thesis overview The objective of this project encompasses engineering design and scientific discovery. Current in vivo extravasation assays are restricted in their ability to perform tightly regulated parametric studies in a high throughput and high-resolution manner. On the other hand, planar endothelial monolayer models are limited in its physiological relevance. As such, the current lack of tumor cells extravasation models that combine high-resolution, high throughput and a good degree of physiological relevance may be limiting our understanding of the mechanisms involved in this crucial step of metastasis. Our goal is to build an in vitro extravasation assay that allows for all of the following: high spatio-temporal resolution of extravasation events in a high throughput manner with increased physiological relevance in terms of vascular network geometry and barrier function, compared to planar monolayer models. The first aim of this project (Chapter 2) is to establish an in vitro perfusable vascular model in which tumor cells can be seeded and extravasation events from within the vasculature can be observed. This is done by creating microvascular networks within microfluidic devices via vasculogenesis. Specifically the assay requirements include: a. 3D microvascular networks ([tVNs) composed of human endothelial cells that are stable and exhibit a physiologically relevant barrier function and vascular geometry b. t VNs that are perfusable to tumor cells and allow observation of tumor arrest, transendothelial migration and invasion into a surrounding 3D ECM c. Ability to apply physiologically relevant levels of shear flow throughout RVNs d. Ability to perform dynamic live cell imaging at a single cell resolution to investigate underlying molecular mechanisms of extravasation from within pVNs e. Moderate level of throughput (ability to produce >12 devices per experiment) to readily allow for parametric studies Different methods to achieve an optimal balance of vascular network growth and stabilization are explored, including the application of various soluble biochemical factors and co-culture with stromal cells with both paracrine and juxtacrine manners. 11 In Chapter 3, the final tumor cell extravasation platform developed is described, which consists of HUVEC paracrine co-culture with normal human lung fibroblasts. The platform is validated prior to the introduction of tumor cells by tracking vessel stability over time as well as EC tight junction formation, vessel barrier function, and the ability to recapitulate known EC responses to specific inflammatory cytokines. Using this assay, we will begin to probe different questions regarding the mechanisms of tumor cell extravasation, including the dynamics of the single and collective tumor cell transmigration, interactions between endothelial and tumor cells during extravasation, the correlation between extravasation capabilities and metastatic potential, and the extravasation patterns of trapped or adhered tumor cells. Through these studies, we aim to demonstrate the assay's ability to facilitate a better understanding of the mechanisms of extravasation and potentially identify factors that can inhibit extravasation and thus, break the metastatic cascade. Chapter 1 References 1. Chaffer, C.L. and R.A. Weinberg, A perspective on cancer cell metastasis. Science, 2011. 331(6024): p. 1559-64. 2. Fidler, 1.J., The pathogenesis of cancer metastasis: the 'seed and soil' hypothesis revisited. Nat Rev Cancer, 2003. 3(6): p. 453-8. 3. Gupta, G.P. and J. Massague, Cancer metastasis: building a framework. Cell, 2006. 127(4): p. 679-95. 4. Psaila, B. and D. Lyden, The metastatic niche: adapting the foreign soil. Nat Rev Cancer, 2009. 9(4): p. 285-93. 5. Crissman, J.D., et al., Morphological study of the interaction of intravascular tumor cells with endothelial cells and subendothelial matrix. Cancer Res, 1988. 48(14): p. 4065-72. 6. Paget, S., The distribution of secondary growths in cancer ofthe breast. 1889. Cancer Metastasis Rev, 1989. 8(2): p. 98-101. 7. Bussard, K.M., C.V. Gay, and A.M. Mastro, The bone microenvironment in metastasis: what is special about bone? Cancer Metastasis Rev, 2008. 27(1): p. 41-55. 8. Coleman, R.E., Skeletal complications of malignancy. Cancer, 1997. 80(8 Suppl): p. 1588-94. 12 9. Chambers, A.F., A.C. Groom, and I.C. MacDonald, Dissemination and growth of cancer cells in metastatic sites. Nat Rev Cancer, 2002. 2(8): p. 563-72. 10. K. J. Luzzi, I. C. MacDonald, E. E. Schmidt, N. Kerkvliet, V. L. Morris, A. F. Chambers and A. C. Groom, Am. J Pathol, 1998, 153, 865-873 11. Sahai, Nat. Rev. Cancer, 2007, 7, 737-749. 12. K. Podsypanina, Y. C. Du, M. Jechlinger, L. J. Beverly, D. Hambardzumyan and H. Varmus, Science, 2008, 321, 1841-1844. 13. K. Stoletov, H. Kato, E. Zardouzian, J. Kelber, J. Yang, S. Shattil and R. Klemke, J. Cell Sci., 2010, 123, 2332-2341. 14. J. L. Townson and A. F. Chambers, Cell cycle, 2006, 5, 1744-1750. 15. Bos, P.D., et al., Genes that mediate breast cancer metastasis to the brain. Nature, 2009. 459(7249): p. 1005-9. 16. Minn, A.J., et al., Genes that mediate breast cancer metastasis to lung. Nature, 2005. 436(7050): p. 518-24. 17. Kang, Y., et al., A multigenic program mediating breast cancer metastasis to bone. Cancer Cell, 2003. 3(6): p. 537-49. 18. Saiki, I., et al., Functional role of sialyl Lewis X and fibronectin-derived RGDS peptide analogue on tumor-cell arrest in lung s followed by extravasation. Int J Cancer, 1996. 65(6): p. 833-9. 19. Hamalukic, M., et al., Rac 1-regulated endothelial radiation response stimulates extravasation and metastasis that can be blocked by HMG-CoA reductase inhibitors. PLoS One, 2011. 6(10): p. e26413. 20. Brown E, Munn LL, Fukumura D, & Jain RK (2010) In vivo imaging of tumors. Cold Spring Harb Protoc 2010(7):pdb prot5452. 21. 7. M. J. Hendrix, E. A. Seftor, R. E. Seftor and I. J. Fidler, Cancer Lett., 1987, 38, 137-147. 22. Q. J. Dimilla PA, Albelda SM, Lauffenburger DA AIChE J., 1992, 38, 1092-1104. 23. Chung, S., et al., Microfluidic platforms for studies of angiogenesis, cell migration, and cellcell interactions. Sixth International Bio-Fluid Mechanics Symposium and Workshop March 28-30, 2008 Pasadena, California. Ann Biomed Eng, 2010. 38(3): p. 1164-77. 24. Lii, J., et al., Real-time microfluidic system for studying mammalian cells in 3D 13 microenvironments. Anal Chem, 2008. 80(10): p. 3640-7. 25. Huang, Y., et al., Microfluidics-based devices: New tools for studying cancer and cancer stem cell migration. Biomicrofluidics, 2011. 5(1): p. 13412. 26. Y. Shin, S. Han, J. S. Jeon, K. Yamamoto, I. K. Zervantonakis, R. Sudo, R. D. Kamm and S. Chung, Nat. Protoc., 2012, 7, 1247-1259. 27. J. W. Song, S. P. Cavnar, A. C. Walker, K. E. Luker, M. Gupta, Y. C. Tung, G. D. Luker and S. Takayama, PLoS One, 2009, 4, e5756. 28. Q. Zhang, T. Liu and J. Qin, Lab on a chip, 2012, 12, 283 7-2842. 29. J. S. Jeon, I. K. Zervantonakis, S. Chung, R. D. Kamm and J. L. Charest, PLoS One, 2013, 8, e56910. 30. I. K. Zervantonakis, S. K. Hughes-Alford, J. L. Charest, J. S. Condeelis, F. B. Gertler and R. D. Kamm, Proc. Natl. Acad. Sci. U. S. A., 2012, 109, 13515-13520. 31. K. C. Chaw, M. Manimaran, E. H. Tay and S. Swaminathan, Lab on a chip, 2007, 7, 104 11047. 32. C. Heyder, E. Gloria-Maercker, F. Entschladen, W. Hatzmann, B. Niggemann, K. S. Zanker and T. Dittmar, J. Cancer Res. Clin. Oncol., 2002, 128, 533-538. 14 Chapter 2: In vitro microvascular network formation and stabilization strategies 2.1 Introduction 2.1.1 In vitro vascular network models - a potential tool for recapitulating the tumor cell extravasation microenvironment One of the pressing challenges in the fields of tissue engineering is understanding and control of vascularization. In vivo, capillary networks deliver oxygen and nutrients to thick (> 1-2 mm) tissues which cannot be supported by passive diffusion [1,2]. There currently exists an enormous clinical demand for engineered vascular networks, both for the vascularization of tissue engineered organs, as well as allow fundamental studies of blood vessel formation in vitro. Recently, microfluidic platforms have been developed for the purpose of studying the fundamental aspects of angiogenesis, with the advantages such as such as real-time high resolution imaging of anastomoses [3], precise control of the microenvironment and the ability to apply spatial and temporal chemical and mechanical cues, such as the contribution of interstitial pressure to angiogenic sprouting [4]. Vascular "networks" can be formed via templated lumens embedded in hydrogels, such as those developed by Zheng and Jeon group [5,6]. While these systems are highly informative experimentally, the capillary channels designed in these studies are two-dimensional (2D) vessels that lie at 90-degree angles to each other or in parallel, and do not closely model physiologic capillaries. In vivo, both networks respond to angiogenic signals and sprout to organize themselves into complex, three-dimensional (3D) capillary beds that undergo repeated branching, and sprout along random paths [7,8]. Alternatively, networks can be formed without templates for ECs to grow on, arising from a self-organized, physiologically relevant vascularization processes. This can be achieved via two different mechanisms - in one, dispersed ECs organize into a vessel network (vasculogenesis), and in the other, existing vessels sprout or split into new ones (angiogenesis) 15 [9]. Angiogenic sprouting has been achieved by seeding endothelial cells on the surfaces of gels and incorporating angiogenic stimuli including vascular endothelial growth factor (VEGF) to promote vascular growth [4,10,11]. Similarly, vasculogenesis has been explored by seeding ECs directly into gel matrices (i.e. collagen or fibrin) and applying similar angiogenic factors to induce network formation [12, 13]. Vasculogenesis is typical during the initial development stages of an organism where individual endothelial cells extend protrusions to connect to neighboring cells. Cells form into interconnected networks and mature into tubular structure with patent lumens [14]. While the delivery of angiogenic factors has been successful in promoting new capillary formation, the structure of the newly formed vessels is often non-ideal. The vessels can be immature and unstable and may result in poor perfusion and possibly vessel regression upon a decrease in the vascular stimulus [12,15]. This may be due to the fact that most platforms do not capture the complexity of the vascular microenvironment, including the important paracrine and juxtacrine roles played by perivascular cells during vessel stabilization [16,17]. Despite these challenges, it is thought that these platforms may be the beginning of new set of tools to study the basic biology of angiogenesis and can be utilized to create different disease models relating to vasculature such as cancer. While no in vitro system can fully recapitulate the complexity of an in vivo situation, such vasculature platforms have the potential to more closely model the tumor cell extravasation environment compared to conventional Boyden chamber and Transwell assays, while potentially alleviating challenges associated with in vivo platforms. 16 3D Self-organized networks (a) Template vasculature (b) (c) Sprouting angiogenesis (e) (d) Vasculogenesis (f) Figure 3. Formation of microvasculature in vitro. Various assays have been developed to recapitulate vascular networks in vitro. (A-B) Endothelial cells can be seeded into hollow channels in hydrogels and allowed to take the shape of the template [4,5]. Vascular networks can also form via self-assembly, including sprouting angiogenesis (C-D) [13] and vasculogenesis (E-F) [12,13]. 2.1.2 Vascular stabilization and regulation in vivo and in vitro It is well established that vascular endothelial growth factor (VEGF) is the master regulator of angiogenesis [18,19]. However, angiogenesis is a complex multi-step process that requires the temporal and spatial co-ordination of different factors and cell types. Endothelial cells proliferate and migrate in response to VEGF gradients to form new tubular structures. Vascular maturation and stabilization is defined as the induction of endothelial quiescence and protection against VEGF withdrawal. In vivo, this involves a series of events requiring the coordination of endothelial cells (ECs), smooth muscle cells (SMCs)/pericytes, and myeloid cells. Association of ECs and pericytes renders new vessels independent of continued VEGF expression. Mural cells are then recruited and coat vascular tubes while ECs deposit new basement membrane (i.e. collagen IV, laminin and other BM proteins). Such perivascular cells play an important role in the stability of functional networks and their proper spatial organization relative to endothelial cells and delivery of secreted factors may be paramount [16,17]. 17 Subsequently, tight and adherens junctions begin to form between ECs, providing endothelial integrity, mechanical strength and a barrier to molecular transport. On the contrary, during sprouting angiogenesis, junctions partially disorganize, increase vessel permeability and allow for cell migration and proliferation. Thus, characteristics of quiescent vessels include: reduction in vessel coalescing (decreased number of branches), maintenance of vessel diameter, prevention of vessel dilation, remodeling and cell proliferation, localization of tight junctions and basement membrane deposition. As such, stable, operational vascular networks results from a balance between signals that favor angiogenesis and vascular stabilization [14]. Vessel stabilization in vitro has been approached in several ways. For instance, the application cocktails of pro- or anti-angiogenic factors have been shown to promote initial angiogenesis and later stabilization. Important growth factors include VEGF, angiopoietins, fibroblasts growth factors (FGF), transforming growth factors (TGF), platelet-derived growth factors (PDGF), tumor necrosis factors (TNF) and interleukins [20-22]. For instance, Angl (angiopoietin 1) is expressed by pericytes has been shown to inhibit vascular permeability in the skin, in tumors and in an in vitro model of the blood-brain barrier by acting as an agonist for the Tie2 receptor [23]. Ang 1 has been shown to promote interactions between ECs and mural cells to decrease vessel permeability and remodeling. Stimulation with Angl prevents the internalization of VE cadherin into internal compartment caused by VEGF leading to the tight junction localization [18]. SIP, another soluble factor, has been shown to inhibit angiogenesis through Sl P-induced release of a soluble mediator from smooth muscle cells, which then recruits MCs to associate with vessels [24]. SIP has also been shown in an ex vivo human arterial model of angiogenesis to induce a localization of VE-cadherin to endothelial junctions, leading to decreased tubulogenesis [25]. Cyclic AMP (cAMP) is also a well-known intracellular signaling molecule that acts to improve barrier function in vascular endothelial cells. Barrier permeability is decreased and VE-cadherin dependent cell adhesion is enhanced, incidicating that cAMP may be a potent player in vascular stabilization [26]. In vivo co culture of endothelial and supporting stromal cells has also been shown to facilitate stable vasculature formation [27-29]. For instance, Jain et al demonstrated the ability to form a network of lasting and functional blood vessels (>1 year) in mice by co-implantation of 18 vascular endothelial cells and mesenchymal precursor cells [27]. The importance of these accessory cells may be both paracrine and juxtacrine: secreted factors from stromal cells may enhance vessel stabilization and stromal-endothelial cell contacts may also be necessary to provide physical support and/or initiate signaling pathways leading to factor(s) secretion. Mechanical factors such as shear stress, interstitial fluid flow and extracellular matrix stiffness can also play a role in vasculature development. For instance, application of shear stress on the endothelial wall in vitro to recapitulate blood flow has been shown to regulate the angiogenic process. In particular, it has been demonstrated that shear stress not only initiates endothelial cell migration and proliferation in the early stages of angiogenesis via an up regulation of VEGF expression [30,31], but also promotes the development of EC tight junctions and overall vessel stabilization [9,32]. Other growth factors related to shear stress stimulation include TGF-P1, TNF-a, MCP-l and PIGF [22,33,34]. In fact, vessel regression has been observed in vitro when shear is decreased for ceased, indicating its importance in vessel stabilization and maintenance. 2.2 Methods 2.2.1 Assay design Microfluidics has emerged as a powerful means for cell culture and recapitulating cellular microenvironments [34-36]. Soft lithography is a low cost, high throughput and robust technique for producing microfluidic devices compatible with cell culture. In order to meet the requirements of an in vitro tumor cell extravasation assay as listed in Chapter 1, we employ a microfluidic device in order to generate perfusable 3D human endothelial microvascular networks assembled via vasculogenesis. The procedure for vascular network formation via vasculogenesis has been documented previously in various platforms, particularly by Jeon et al and George et al. In this study, we employ a vasculogenesis device based on earlier designs from our lab [37]. The general design of the polydimethysiloxane (PDMS) microfluidic device design consists of gel regions for cell culture, flanked by media channels which can all be independently filled via inlet and outlet ports at the ends of the channel. Small micro posts allow for surface 19 tension assisted filing of hydrogels and media. Cells residing in the gel regions can communicate via diffusion and paracrine signaling with other cells and soluble factors present in other channels through the gaps between micro posts. A schematic of the device is presented in Fig 4. Channels are 750 urn wide and 300 um high and the length varies between 2 cm to 4 cm depending on the device being used in this study. The gaps between micro posts are 150 urn. To generate microvascular networks via vasculogenesis, human umbilical cord vein cells (HUVECs) are seeded as a suspension into one gel region. Via application of appropriate biochemical stimuli, HUVECs spontaneously form into 3D interconnected perfusable lumens. Tumor cells, beads and other particulates (<30 um in diameter) can be perfused into the network as the lumens open up at the inter-post regions, allowing communication between the media channel and lumens. More details of the device design are discussed below. 500 ur width Fibri gel HUVEC Vessels (EC) Figure 4. Device Schematic. Microfluidic devices consist of a central gel region that allows surface tension assisted filling via spaced micro-posts. The gel region is seeded with endothelial cells to form a microvascular network. Flanking media regions provide access to an access for nutrients and perfusion of cells into the network. 20 2.2.2 Cells and device preparation Microfluidic device fabrication Microfluidic devices were fabricated using soft lithography via a protocol described previously [39]. Polydimethylsiloxane (PDMS, Ellsworth Adhesives, MA) was mixed at a 10:1 ratio of base: curing agent and poured over a silicon master. The PDMS slabs were incubated overnight at 80C and subsequently, cut from the master, trimmed, punched and autoclaved in water. Devices were then dry autoclaved and dried overnight at 80C. PDMS slabs and No. I glass coverslips were then plasma treated for 3 minutes and 20 seconds (Harrick Plasma, Ithaca, NY), bonded and left at 80C for 24 hours before sterile use. Cell culture Human umbilical vein endothelial cells (HUVECs) were cultured on collagen 1 coated flasks (50 ptg/ml collagen in ascetic acid for 30 min) in EGM-2MV (Lonza) growth media and used at passage 5. Gel fabrication and cell seeding Fibrinogen solution was prepared by reconstituting 5 mg/mL of bovine fibrinogen (Sigma, MO) in PBS and dissolving the mixture in a 37*C water bath for 2 h. The solution was then filtered using a 0.2 prm filter and stored at 4*C. HUVECs (Lonza, MA) were cultured in supplemented endothelial growth medium (EGM-2, Lonza) and grown to passage 5 before they were trypsinized and resuspended at a concentration of 8 million cells per mL in a solution of EGM with thrombin (0.5 U/mL, Sigma). The cell suspension was then mixed in a 1:1 ratio with 20 ptL of 5 mg/mL fibrinogen to achieve a final concentration of 4 million cells per mL and immediately injected into the HUVEC gel channel. Devices were placed in a humidity chamber for 30 minutes at room temperature to allow gel curing, and were subsequently filled with EGM2 and placed in the incubator (37*C, 5% CO2 )- 21 2.2.3 Fluorescent imaging and analysis To visualize microvascular network formation, live devices were imaged via phase contrast microscopy (Nikon, Japan). End point visualization of the vasculature was done via confocal microscopy (Olympus, Japan). Cells in the devices were fixed with 4% PFA for 15 minutes and permeabilized with 0.01% Triton X for 10 minutes. Devices were then stained with rhodamine phalloidin (Alexa Fluor 568, Invitrogen) (1:100) for actin at the final time point to visualize the HUVEC network. In co-culture experiments, HUVECs were differentiated from fibroblasts via immunostaining with anti-CD-31 (Sigma, MO). Samples were blocked with 5% BSA (Sigma) and 2% goat serum (Sigma) for 2 h at room temperature followed by primary antibody incubation (1:100) then a secondary antibody (Alexa Fluor 488, Invitrogen) (1 : 200) at room temperature for 3 h. Devices were then counterstained with rhodamine phalloidin for actin and DAPI for nuclei (1 : 1000, Invitrogen). All images were obtained via confocal microscopy and processed using the IMARIS imaging software. Metrics used to quantify and assess degree of vascular network formation and stabilization include: average vessel (branch) diameter, number of skeletons/device, number of branches per skeleton, and number of perfusable interpost regions. To calculate average diameters, the diameter at three cross-sections per branch is averaged. The average value of 30 branches per device is then calculated. A skeleton is defined as one interconnected network (Figure 5 depicts 4 separate skeletons). Branches per skeleton are defined as a section of a vessel between two intersecting points (Figure 5C depicts 5 branches). Finally, the number of perfusable interpost regions is defined as a region where the lumen is open and accessible to the media channel. 2 Figure 5. Vessel network quantification metrics. A, B, C and D depict separate skeletons. 22 2.3 Results 2.3.1 Vessel formation via HUVEC monoculture and stability Via HUVEC monoculture, microvascular networks could be formed in 5-6 days. No exogenous growth factors were applied during this time frame. Networks were fixed and stained on day 5, permeabilized and stained with phalloidin for actin. Image analysis reveals networks spanning along the entire gel region with some vessels opening up to the media channels at the inter-post regions, as confirmed via confocal imaging (Fig. 6) (opening at ~60% of inter-post regions, n=5). Figure 6. Microvascular networksformed via HUVEC monoculture. (A) HUVEC monoculture after 4 days results in a perfusable vascular network, as depicted by actin staining (red). (B) Some vessels open up to the media channel at the interpost regions, allowing for perfusion. Live, daily tracking of the same devices reveals that average vessel diameters increased steadily from 30 um on day 2 to ~110 um on day 6. At the same time, the number of vessel branches declines rapidly from -0. 14 (normalized to total number of cells in the device) on day 2 23 to ~0.04 on day 6. As time progresses individual vessel branches merge with adjacent branches suggesting that endothelial cells are not quiescent as they continue to remodel (Fig. 7). Vessel Diameter 140 120 100 60 - - -- 40 - 8B0 - -- 20 __ 0 1 2 3 4 5 6 7 Day Number of Branches 0.2 0.18 0.16 - 0.14 3 0.12 0.1 0.08 0.06 U 004 0.02 0 2 3 4 Day 6 5 33 Figure 7. Vessel stability from HUVEC monoculture. (A) Phase contrast images of the same region of interest from Days 2 to 4 show an increase in vessel diameter and a gradual decrease in the branch number. (B) Vessels coalesce resulting in less branches with larger diameters. (C) Quantification of average vessel diameter and branch number from Days 2 to 6. 2.3.2 Cytokine cocktails In an effort to enhance vessel stability and perfusability, we applied mixtures of pro and stabilizing angiogenic factors to the culture media throughout the culture duration. In particular, we hoped to improve parameters including (1) average vessel diameter, (2) skeleton number/device and (3) number of perfusable vessel openings at interpost regions. Cytokines used include: VEGF, S 1 P, cAMP, Ang 1, TGF-s3 1, and GM600 1. These particular cytokines and their respective working concentrations were chosen based on prior literature indicating their relevance to vessel formation and stabilization in either in vivo or in vitro assays. 24 140 120 - 25ng VEGF -0-10ng VEGF E 100 .0.50ng VEGF +s1P 80 - cAMP - TGB-B1 -GM6001 60 Angl f, - Basal >40 '-50ng VEGF 20 0 1 2 3 4 Day 5 6 7 36 Figure 8. Increase in vessel diameter with application of various cytokines. Application of Ang- 1 results in the least amount of change in vessel diameter over time without vessel regression, compared to other conditions. Addition of TGF- 1, cAMP, VEGF (25 ng/mL and 50 ng/mL), 50 ng/mL VEGF+SIP (20 ng/mL), GM6001 (10 ng/mL), Ang 1 (10 ng/mL) and SIP (20 ng/mL) alone all caused continued vessel dilation past day 5. Note that application of basal media (EGM fully supplemented with Lonza bullet kit, except for VEGF) or only 10 ng/mL VEGF caused a decrease in vessel diameter, suggesting that the level of VEGF applied to the system was insufficient for vessel maintenance. Further analysis reveals that in these conditions, vessel branches begin to detach from one another, forming island-like structures instead of interconnected networks. Compared to the control conditions (fully supplemented EGM-MV2) treatments of 50 ng VEGF+S 1 P, 25 ng/mL VEGF, Si P alone or Ang- 1 resulted in smaller vessel diameters past day 5, while cAMP or TGF-P1 alone resulted in the opposite. Out of all the cytokines tested at these concentrations, application of Ang-1 appears to be the most effective in stabilizing the vascular network, with the vessel diameter increasing only slightly from -70 pim to -80 pm between days 5-7. Application of Ang-1 also yields the smallest vessel diameter at day 5, but does not regress compared to the basal and 10 ng/mL VEGF treatments (Fig. 8). 25 2.3.3 Co-culture with stromal cells (human lung fibroblasts) Juxtacrine and paracrine culture It is important to consider that in vivo, endothelial cells do not form vascular networks in isolation. In addition to he mechanical cues provided by the extracellular matrix, communication with supporting cell types is critical. Our microfluidic platform is very amenable to co-culture with multiple cell types, with the option to control their spatial segregation. For non-contact, paracrine-only co-culture, another gel region can be designed and placed next to the existing HUVEC channel, while being separated by a media channel. In this manner, cells within both gel regions can communicate via diffusion of secreted soluble factors. Here, we investigated the effect of co-culture with stromal support cells, namely human lung fibroblasts (HLFs) and their role in secreting pro-angiogenic and stabilizing factors when co-cultured with HUVECs during vasculogenesis. We first co-cultured HLFs and HUVECs in the same gel region, allowing both juxtacrine and paracrine communication to occur. A variety of HUVEC: HLF ratios were used, while constantly maintaining HUVEC densities at 4e6 cells/mL. Data collected at an end point of 5 days include average vessel diameter, number of skeletons/device and number of branches normalized to the skeleton number. We found that while a ratio of 2:1 (EC: HLF) gave the largest diameters at day 5 (-60 um), the value was nearly half of that obtained from HUVEC monoculture alone (Fig. 9). Moreover the 2:1 ratio also yielded the smallest number of skeletons/device (-5) and the most normalized number of branches (-24) at ay 5, compared to all other ratios attempted. Higher HLF densities (namely 1:1 and 2:3) resulted in much smaller vessel diameters however, skeleton numbers were increased and branch number were decreased. It is likely that the presence of more HLFs decreases the free ECM space for lumens to dilate, resulting in smaller diameters. At the same time, the decrease in free ECM space may also prevent individual ECs from contacting each other and anastomosing, which may explain the increase in decrease in skeleton and branch number, respectively. Furthermore, the absolute increase in the number of cells upon the addition of HLFs may compromise the health of the HUVECs as the amount of nutrients supplied to the device remains constant. Lastly, it is important to note that although there is a reduction in vessel 26 diameter at day 5 compared to HUVEC monoculture in the 2:1 culture, the percentage of perfusable vessel openings at the inter-post regions exhibited only a slight increase (~65% compared to -60%). D 20 70 30 25 60 15 E 50 40 10 30 20 A 2 1 10 B 2 2 5 C 2 3 D 2 0 15 5 10 0 B A *p<0. C D 05 A B C D A B C D 41 Figure 9. Juxtacrine co-culture of HUVECs with HLFs. (A-C) Fixing and fluorescent staining with actin and CD31 at Day 5 reveals a interconnected network of HUVECs with HLFs in close association in the ECM, at different EC:HLF ratios. (D) A 2:1 EC:HLF ratio results in the largest vessel diameters but the least number of skeletons and greatest number of branches/skeleton. Paracrine only culture Next, we investigated the effect of HUVEC-HLF co culture via a non-contact method. In this configuration, communication between the two cell types occurs only via diffusion, as the cells are confined within their respective gel regions and are separated by a media channel. Several HLF : HUVEC ratios were explored, including 1:2, 1:1 and 2:1 while keeping final HUVEC cell densities at 4M cells/mL. Live, daily tracking of average vessel diameter was performed (Fig. 10). Cultures at a 2:1 ratio yielded the smallest vessel diameters over a 7-day period while 1:2 cultures yielded the largest, past day 4. 1:1 ratio cultures exhibited an 27 intermediate value of average diameter past day 4. Although more HLFs than HUVECs (2:1 cultures) showed the smallest diameters and most branch numbers/skeleton, the differences between the 2:1 and 1:1 cultures were only slight. Moreover, 2:1 cultures showed increased invasion of fibroblasts into the media channel and flanking HUVEC regions, indicating that the HLF density may be too high. This phenomenon may pose problems, as HLFs begin to degrade the fibrin gel at the interpost regions in the HUVEC channel, which may ultimately affect tumor cell seeding. Thus, despite the slight increase in average diameters in the 1:1 compared to the 2:1 culture, it is still the optimal culture condition out of the three attempted. With these findings 1:1 non-contact cultures were further explored and characterized. Single HUVECs begin to spread and organize into tubule-like structures within the gel by day 2, and by day 4, [tVNs with lumens ranging from 8 to 96 pm in diameter are formed. Lumens communicate with the two flanking media channels, allowing vessel perfusion. Vessels are relatively quiescent, with individual vessel diameters increasing by 5.1 + 4.7% from days 4 to 5, and 5.7 + 5.4% from days 5 to 6. 28 B Average vessel diameter A 140 120 100 80 WMO1:1 60 O1:2 40 2:1 20 0 5 4 3 2 7 6 Day c D 6 120 C 100 0 80 Go 4 S60 U c 5 2 0 40 4A 20 0 0 1:1 1:2 2:1 1:2 juxtracrine 1:1 1:2 2:1 1:2 ju xtracrine Figure 10. Microvascular network formation with non-contact HUVEC-HLF co-culture. (A-B) 1:1 HUVEC:HLF non contact culture reveals an intermediate level of vessel dilation compared to other ratios, while exhibiting a large number of branches (C) and small number of skeletons/device (D). 2.3 Discussion Compared to the optimal contact HLF-HUVEC culture method attempted previously (1:2, HLF: HUVEC), the average diameter of the 1:1 non-contact culture is still higher on day 5 (-80 rn vs -65 tm). However, the skeleton number/device and branches/skeleton of the non- contact culture is more ideal. The average skeleton number is -1.2 per device compared to 5 in the 1:1 contact culture. This suggests that the networks formed via the 1:1 non-contact culture are much more interconnected than any of the contact cultures. Likewise, the average number of branches/skeleton is much lower in the 1:1 non-contact culture compared to the 1:2 contact 29 culture (-70 compared to -20), indicating that the decrease in number of skeletons does not correlate to a decrease in overall branch number, and in fact are quite similar (both in the range of -100 branches per device). Compared to HUVEC monoculture with Ang-1 application, 1:1 non-contact cultures also yield slightly larger diameters at later days of culture (days 4-7); however, the branch number/skeleton and skeletons/device showed no significant differences between the two culture conditions. Moreover, despite the larger average vessel diameters yielded by 1:1 non-contact culture, the number of perfusable open interpost regions is significantly higher compared to both contact and monoculture conditions (-84% compared to 60% of total interpost regions on both sides of the HUVEC gel region). Thus, taken together, the 1:1 non-contact culture condition yields more ideal vessels than the 1:2 contact culture and even monoculture with Ang-1, since average vessel diameters are only modestly (-15 pm) wider while providing a -35% increase in perfusable interpost regions. In summary, results obtained from the previously described culture conditions suggests that (1) co-culture with supporting stromal cells yields enhanced stabilization and perfusability effects than monoculture with application of selected cytokines, and (2) non-contact cultures in general yields much more interconnected vascular networks than contact cultures, yet with similar average vessel diameters. Increased fibroblast numbers seem to yield more ideal networks with smaller diameters and more interconnected branches. The fact that this effect of fibroblasts seem to be cell concentration dependent and that the effects on network formation is seem even in non-contact culture indicates that paracrine signaling between HLFs and HUVECs play a strong role. Chapter 2 References 1. Johnson PC, Mikos AG, Ph D, Fisher JP, Jansen JA (2007) Strategic Directions in Tissue Engineering. Tissue Engineering 13: 2827-37. 2. Griffith CK, Miller C, Sainson RC, Calvert JW, Jeon NL, et al. (2005) Diffusion limits of an in vitro thick prevascularized tissue. Tissue engineering 11: 257-266. 30 3. Yeon JH, Ryu HR, Chung M, Hu QP, Jeon NL (2012) In vitro formation and characterization of a perfusable three-dimensional tubular capillary network in microfluidic devices. Lab on a Chip 12: 2815-2822. 4. Song JW, Munn LL (2011) Fluid forces control endothelial sprouting. Proceedings of the National Academy of Sciences of the United States of America 108: 15342-15347. 5. Zheng Y, Chen J, Craven M, Choi NW, Totorica S, et al. (2012) In vitro microvessels for the study of angiogenesis and thrombosis. Proceedings of the National Academy of Sciences of the United States of America 109: 9342-9347. 6. Yeon JH, Ryu HR, Chung M, Hu QP, Jeon NL (2012) In vitro formation and characterization of a perfusable three-dimensional tubular capillary network in microfluidic devices. Lab on a Chip 12: 2815-2822. 7. Folkman J (2007) Angiogenesis: an organizing principle for drug discovery? Nature reviews Drug discovery 6: 273-286. 8. Folkman J, Haudenschild C (1980) Angiogenesis in vitro. Nature 288: 551-556. 9. Risau W (1997). Mechanisms of angiogenesis. Nature 386: 671-674. 10. Chung S, Sudo R, Vickerman V, Zervantonakis IK, Kamm RD (2010) Microfluidic Platforms for Studies of Angiogenesis, Cell Migration, and Cell-Cell Interactions. Annals of Biomedical Engineering 38: 1164-1177. 11. Duc-Huy T. Nguyen et al (2013) Biomimetic model to reconstitute angiogenic sprouting morphogenesis in vitro. PNAS 6712-6717. 12. Moya ML, Hsiu YH, Lee AP, Hughes CC, George SC (2013). In vitro perfused human capillary networks. Tissue Eng Part C Methods. Sep;19 (9):730-7. 13. Kim S, Lee H, Chung M, Jeon NL. (2013). Engineering of functional, perfusable 3D microvascular networks on a chip. Lab Chip. Apr 21;13(8):1489-500. 14. Carmeliet P (2000). Mechanisms of angiogenesis and arteriogenesis. Nat Med 6: 389395. 15. Bruno Vailhe, Daniel Vittet, Jean-Jacques Feige (2001). In vitro models of vasculogenesis and angiogenesis. Lab Invest 2001, 81:439-452 16. Gerhardt, H. and C. Betsholtz, Endothelial-pericyte interactions in angiogenesis. Cell and Tissue Research, 2003. 314(1): p. 15-23. 17. Hirschi, K.K. and P.A. DAmore, Pericytes in the microvasculature. Cardiovascular 31 Research, 1996. 32(4): p. 687-698. 18. Shin, Y., et al., In vitro 3D collective sprouting angiogenesis under orchestrated ANG-] and VEGF gradients. Lab on a Chip, 2011. 11(13): p. 2175-2181. 19. Folkman, J. and M. Klagsbrun, A Family of Angiogenic Peptides. Nature, 1987. 329(6141): p. 671-672. 20. Giraudo, E., et al., Tumor necrosis factor-alpha regulates expression of vascular endothelial growth factorreceptor-2andofits co-receptor neuropilin-I in human vascular endothelialcells. Journal of Biological Chemistry, 1998. 273(34): p. 22128-22135. 21. Au, P., et al., Paradoxical Effects of PDGF-BB Overexpression in Endothelial Cells on Engineered Blood Vessels In Vivo. American Journal of Pathology, 2009. 175(1): p. 294-302. 22. Cao, R.H., et al., Angiogenic synergism, vascular stability and improvement of hind-limb ischemia by a combination ofPDGF-BBandFGF-2. Nature Medicine, 2003. 9(5): p. 604613. 23. Fukuhara S, Sako K, Noda K, Zhang J, Minami M, Mochizuki N, (2010). Angiopoietin1/Tie2 receptor signaling in vascular quiescence and angiogenesis. Histol Histopathol. 2010 Mar;25(3):387-96. 24. Yoh Takuwa, Wa Du, Xun Qi, Yasuo Okamoto, Noriko Takuwa, and Kazuaki Yoshioka. (2010) Roles of sphingosine- 1-phosphate signaling in angiogenesis. World J Biol Chem. 1(10): 298-306. 25. Mascall KS', Small GR, Gibson G, Nixon GF. (2012). Sphingosine-1-phosphate-induced release of TIMP-2 from vascular smooth muscle cells inhibits angiogenesis. J Cell Sci. 125(Pt 9):2267-75 26. Fukuhara S', Sakurai A, Sano H, Yamagishi A, Somekawa S, Takakura N, Saito Y, Kangawa K, Mochizuki N. (2005). Cyclic AMP potentiates vascular endothelial cadherin-mediated cell-cell contact to enhance endothelial barrier function through an Epac-RapI signaling pathway. Mol Cell Biol. ;25(1):136-46. 27. Koike, N., et al., Creation of long-lasting blood vessels. Nature, 2004. 428(6979): p. 138139. 28. Au, P., et al., Differential in vivo potential of endothelial progenitor cells from human 32 umbilical cord blood and adult peripheral blood to form functional long-lasting vessels. Blood, 2008. 111(3): p. 1302-1305. 29. Jain, R.K., et al., Engineering vascularized tissue. Nature Biotechnology, 2005. 23(7): p. 821- 823. 30. Resnick, N., et al., Fluid shear stress and the vascular endothelium: for better and for worse. Progress in Biophysics & Molecular Biology, 2003. 81(3): p. 177-199. 31. Milkiewicz, M., et al., Association between shear stress, angiogenesis, and VEGF in skeletal muscles in vivo. Microcirculation, 2001. 8(4): p. 229-241. 32. Resnick, N. and M.A. Gimbrone, Hemodynamic Forces Are Complex Regulators of Endothelial Gene-Expression. Faseb Journal, 1995. 9(10): p. 874-882. 33. Pipp, F., et al., VEGFR- I-selective VEGF homologue PIGF is arteriogenic - Evidence for a monocyte-mediated mechanism. Circulation Research, 2003. 92(4): p. 378-385. 34. Luttun, A., et al., Revascularization of ischemic tissues by PIGF treatment, and inhibition of tumor angiogenesis, arthritis and atherosclerosis by anti-Fltl. Nature Medicine, 2002. 8(8): p. 831-840. 35. Griffith, LG, and Swartz, MA. 2006. Capturing complex 3D tissue physiology in vitro. Nat. Rev. MCB. 7:211-24. 36. Park, T.H. and Shuler, M.L. 2003 Integration of cell culture and microfabrication technology. Biotechnol. Prog. 19:243-253. 37. Meyvantsson, 1. and Beebe, D.J. 2008. Cell culture models in microfluidic systems. Ann. Rev. of Analytical Chem. 1:423-449. 38. Chung, S. et al. Cell migration into scaffolds under co-culture conditions in a microfluidic platform. Lab. Chip 9, 269-275 (2009). 39. Y. Shin, S. Han, J. S. Jeon, K. Yamamoto, 1. K. Zervantonakis, R. Sudo, R. D. Kamm and S. Chung, Nat. Protoc., 2012, 7, 1247-1259. 33 Chapter 3: Tumor-endothelial interactions during extravasation from in vitro microvascular networks 1 [1] This chapter is modifiedfrom Ref 56 with the publisher'spermission 3.1 Introduction Cancer cells disseminate in the body by undergoing several steps, including the invasion of surrounding tissues, intravasation into the blood vessel, transport in the circulation, extravasation from the vasculature and proliferation at a secondary site. During extravasation, tumor cells (TCs) form dynamic contacts with the endothelium that give rise to significant cytoskeletal changes required for transendothelial migration (TEM) (1). Although the mechanisms of intravasation have been widely studied, the precise cellular interactions and molecular alterations associated with extravasation are poorly understood. In fact, most data are gathered from low-resolution in vivo studies and endpoint assays that indirectly observe tumor cells via quantification of secondary tumor formation in existing animal models (2-6). As such, direct observation of tumor cell arrest on and subsequent migration across an endothelium in a precisely controlled and physiologically relevant microenvironment would provide important insight into extravasation mechanisms. Current in vivo models of extravasation include rat tail vein injection of tumor cells (7), which, although the most physiologically relevant, does not allow for high resolution visualization of extravasation events. More recently, intravital microscopy performed on optically transparent transgenic zebrafish has enabled high spatial and temporal resolution imaging (5); however, as with most in vivo platforms, the ability to perform parametric studies is restricted. In vitro models such as the Boyden chamber-Transwell assays provide a relatively simple and high throughput method for parametric cell migration studies (8, 9), yet do not allow monitoring of the entire process of extravasation. Recently, microfluidic technologies have been developed to study TEM (10-12), including those enabling high resolution and dynamic study of both tumor cell intravasation and extravasation (13, 14). In the latter, devices consist of microchannels connected by 3D ECM hydrogels, where tumor cells are seeded in one channel, 34 arrest onto and extravasate across an endothelial cell (EC) monolayer and into a hydrogel. Although these devices allow extravasation events to be readily imaged, the EC monolayer is sometimes discontinuous with a high permeability. Furthermore, most studies of TEM across planar EC monolayers (12, 13, 15, 16) are limited in their physiological relevance. 3D microvascular networks ([iVNs) have been widely explored in vitro and are particularly amenable to the study of vascular biology and modeling of disease in a more physiologically relevant configuration than endothelial lined tubes or monolayers. ptVNs can be formed from self-organized, physiologically relevant vascularization processes, including sprouting angiogenesis and vasculogenesis. Recently, several groups have developed microfluidic platforms capable of generating perfusable 3D p.VNs (17-19). While no in vitro system can fully recapitulate the complexity of an in vivo situation, such vasculature have the potential to more closely model the in vivo tumor cell extravasation environment. In this chapter, we present a microfluidic platform for the modeling of the entire process of extravasation from within in vitro IiVNs assembled via vasculogenesis. Our platform offers key advantages over existing in vitro TEM models by enabling all of the following: (1) high temporal and spatial resolution of extravasation events, (2) the ability to perform parametric studies in a tightly controlled and high throughput microenvironment and (3) increased physiological relevance compared to 2D and 3D planar monolayer models. We employ our model to demonstrate the effect of inflammatory cytokine stimulation on endothelial barrier function and extravasation efficiency, and the positive correlation between metastatic potentials of different tumor cell lines and their extravasation capabilities. We demonstrate high spatiotemporal visualization of the sequential steps of extravasation from in vitro pVNs, and observe the extravasation patterns of different tumor cell subpopulations including mechanically entrapped cells, single arrested tumor cells and cell clusters. Findings from our platform results in a deeper understanding of tumor cell extravasation mechanisms and demonstrates our assay's potential to be employed for the discovery of factors that could inhibit this crucial step in metastasis. 35 3.2 Methods 3.2.1 Microvascular network formation and maintenance HUVECs were suspended in a fibrin gel, seeded and cured in the gel region. Fibrinogen solution was prepared by reconstituting 5 mg/mL of bovine fibrinogen (Sigma, MO) in PBS and dissolving the mixture in a 37 C water bath for 2 h. The solution was then filtered using a 0.2 um filter and stored at 4 C. HUVECs (Lonza, MA) were cultured in supplemented endothelial growth medium (EGM-2, Lonza) and grown to passage 5 before they were trypsinized and resuspended at a concentration of 8 million cells per mL in a solution of EGM with thrombin (0.5 U/mL, Sigma). The cell suspension was then mixed in a 1:1 ratio with 20 uL of 5 mg/mL fibrinogen to achieve a final concentration of 4 million cells per mL and immediately injected into the HUVEC gel channel. In experiments where normal lung fibroblasts (NHLFs) (Lonza, MA) was used, cells were cultured in supplemented FGM (Sigma, MO) until passage 5 were similarly dissociated and suspended with the 10 mg mL fibrinogen solution to reach a final cell density of 4 million cells per mL, and was injected into the NHLF channel. Devices were placed in a humidity box at room temperature and gels were allowed to cure for 20 minutes before filling the media channels with supplemented EGM. Media was replenished every 24 h for the . duration of the culture. All cells were maintained in a humidified incubator at 37 C and 5%CO 2 3.2.2 Tumor cell seeding in WVNs MDA-MB-231, HT-1080 (from Dr Frank Gertler, MIT) cultured in DMEM (Sigma, MO) supplemented with 10% FBS and 1% Pen-Strep (Invitrogen, CA), and MCF-10A cells (from the Brugge Lab, cultured as described previously 20 ) were trypsinized and resuspended at a final concentration of 0.4 M cells per mL in EGM. Media from the reservoirs of the two channels flanking the HUVEC channel were aspirated and 40 mL of the tumor cell suspension was introduced into one of the reservoirs of the central media channel. This creates a pressure drop of 5.2 mmH20 across the vascular network, drawing the tumor cells into the vasculature. Devices were placed in an incubator immediately after seeding and left to equilibrate for 30 min, after which devices were washed by applying fresh media via a pressure drop in the same direction as 36 the tumor cell seeding to remove any non-adherent cells. 3.2.3 Tumor cell extravasation quantification and metrics Using the IMARIS imaging software, the nucleus of each tumor cell in an ROI was identified and marked using the IMARIS Spot tracker function. Only cells with nuclei found on the basal side of the endothelial barrier (either directly adjacent to or migrated away from the barrier) were counted as an extravasation event. ROIs were selected such that the edge effects at the boundary between the gel and media channel were avoided, as such areas may contain cells that have migrated into the gel from the outside media channel. As a further precaution, time- lapse confocal microscopy was performed for each device for the entire duration of the culture period, to ensure that cells migrated from media channel were not considered in the final calculation. We calculated the extravasation efficiency as the ratio of extravasated cells to the total number of cells found inside the microvasculature by analyzing a minimum of 6 ROI per device, which were selected randomly out of 30 total ROI per device. The dimensions of each ROI were 750 um by 750 ptm by 300 pm (height). For the quantification of TEM efficiency of different sub-populations, tumor cells whose diameter was larger than the segment of vessel immediately downstream was categorized as entrapped, while all other cells that remained after washing with medium were considered to be part of the adhered non- trapped population. The TEM efficiency of each subpopulation was defined as the ratio of the number of extravasated cells to the total number of cells classified in the subpopulation. Like-wise, clusters were defined as a group of 2 or more tumor cells in direct contact with one another, while single cells were those not in contact with any other tumor cell. In these experiments, extravasation events were analyzed via live fluorescent-bright field overlay images. The location of the vessel wall was determined by live images taken at 0 h. Extravasated cells were identified as those with a spread morphology and protrusions past the vessel wall into the matrix, and non extravasated cells were identified as generally rounded cells within the vessel. 37 3.2.4 TNF-a stimulation of HUVECs For cytokine stimulation experiments, HUVECs were stimulated with 2, 5 or 10 ng/mL of TNF-a (R&D systems, MI), at 96 h after endothelial seeding, for 12 h. To ensure that the results observed were not due to the direct modulation of TNF-a on tumor cell migration, devices were washed and incubated in normal media for 30 min prior to tumor cell seeding. 3.2.5 Calculation of vessel permeability The method used to quantify vessel permeability was based on that described previously.5 5 Briefly, background fluorescence images of the vascular network were obtained (Ib). The media in all reservoirs were aspirated and the three reservoirs on one side were injected with 45 mL of 10 mM 70 kDa MW Texas red dextran solution (Invitrogen, CA) simultaneously. Devices were placed in an incubator for 20 min, and then transferred to the microscope environmental chamber for another 10 min, to account for time required for dextran diffusion into the vessels and recovery from agitation during transfer. Once equilibrium was established (i.e. intensity inside the vessels remained constant), fluorescent images were captured every 5 min for 60 min. The permeability coefficient was calculated by obtaining the average intensity in a measuring window containing both the vessel segment and surrounding gel at the initial and final time points. Individual sections of the vessel network of length B80 mm each (2 sections/ROI, 4 ROI/device, n = 3) were selected for analysis. The length of each section varied slightly, in order to capture a segment that was relatively uniform in diameter. Care was taken to select vessel segments in the central region of the channel, which was far enough from the media-gel boundary. Permeability coefficients were computed as: i - Ib A 4 where Ii, If and lb are the initial, final and background average intensities, dt is the time between the two captured images, and d is the average diameter of the vessel segment.55 All imaging was 38 performed using a confocal microscope (Olympus, Japan). 3.2.6 Immunofluorescent staining, imaging and imaging processing To quantify extravasation events, HUVECs were fixed and stained with rhodamine phalloidin (Alexa Fluor 568, Invitrogen) at the final time point to visualize the position of the tumor cell relative to the endothelial barrier. For live tracking of extravasation events, a plasma membrane cell tracker was used (Cell Mask Deep Red Stain, Invitrogen) on HUVECs via incubation at 5 mg/mL for 30 min. Cell viability assays were performed using a Live/dead cytotoxicity kit (Invitrogen) containing SYTO 10 (2 ptM) and ethidium homodimer (4 piM), and following the manufacturer's instructions. To verify the presence of tight cell-cell junctions, rabbit monoclonal primary antibody for human VE cadherin (Abcam, MA) and secondary antibodies (Alexa Fluor 568, Invitrogen) were used. To verify the presence of basement membrane deposition, mouse monoclonal antibody for human collagen IV (Abcam) was used, followed by a secondary antibody (Alexa Fluor, 488, Invitrogen). Devices were washed once with PBS, fixed with 4% (w/v) paraformaldehyde in PBS for 20 min and permeabilized with 0.1% Triton X-100 (Sigma) for 10 min. Samples were blocked with 5% BSA (Sigma) and 2% goat serum (Sigma) for 2 h at room temperature, and incubated with primary antibodies for 24 h at 4 IC (VE-cadherin, 1 : 100; collagen IV, 1 : 100). This was followed by washing and incubation with secondary antibodies (1 : 200) at room temperature for 3 h. Devices were then counterstained with rhodamine phalloidin for actin (1 : 200) and DAPI for nuclei (1 : 1000, Invitrogen). All images were obtained via confocal microscopy and processed using the IMARIS imaging software. 39 3.3 Results 3.3.1 Formation, characterization and validation of microvascular networks via vasculogenesis In order to model a physiologically relevant tumor cell extravasation microenvironment, we employ a microfluidic plat- form' 3 " to develop stable, functional and perfusable in vitro tVNs via vasculogenesis. We use a two gel-channel device to allow the co-culture of HUVECs and NHLFs in a 3D ECM hydrogel (Fig. 12A and B). This spatial patterning of both HUVECs and stromal cells allows diffusion-dependent, non-juxtacrine, and paracrine cell-cell interactions that give rise to more natural blood vessels, compared with HUVEC monoculture.1 7 ,1 Single HUVECs begin to spread and organize into tubule-like structures within the gel by day 2, and by day 4, pVNs with lumens ranging from 8 to 96 mm in diameter are formed. Lumens communicate with the two flanking media channels, allowing vessel perfusion. Vessels are relatively quiescent, with individual vessel diameters increasing by 5.1 + 4.7% from days 4 to 5, and 5.7 + 5.4% from days 5 to 6 (Fig. I1). A B 0.2 - T .5 - E 0.1- - 0.1 - FA 0.12 0.080 0.06 0.04 0I -. 01 . 08T -0 days 5-6 days 4-5 Time after HUVEC seeding 2 3 5 4 6 7 Day Figure 11. Formation of microvascilar networks in nicrofluidic devices. (A) Change in individual vessel diameters (n=40 vessels) during time frame of extravasation experiments (days 4 to 6). (B) Changes in total vessel branches normalized by the total number of cells over time (6 ROI/device, 3 devices). Data are presented as mean +SD, with *p<0.05. 40 Figure 12. Characterization of microfluidic microvascular network platform. (A) A schematic of the microfluidic device and cell-seeding configuration. Suspended HUVECs form microvascular networks in a gel matrix communicating with NHLFs in a paracrine fashion across the central media channel through the inter-post regions. Micro-posts (black) allow for surface tension-assisted gel filling via ports at the ends of each gel region. Medium is replenished every 24 hours via hydrostatic pressure applied between the media reservoirs on each end of the media channels. (B) Photograph of 2-gel region microfluidic device. (C) Visualization of VE-cadherin (red) at 60X reveals continuous cell-cell junctions. (D) Collagen IV basement membrane deposition (green) around the lumen (red) and in the perivascular space suggests vessel maturation. (E) Perfusion of vessels with 70 kDa dextran reveals patent lumens void of local leaks. Scale bars are 20 ptm. To confirm the integrity of the endothelial barrier, staining of the networks at 96 h with anti-VE-cadherin showed the presence of continuous cell-cell junctions spanning the entire circumference of the lumen (Fig. 12C). We further detected the presence of collagen IV in the perivascular extracellular matrix, a sign of vessel maturation and stabilization (Fig. 12D). Perfusion of the vasculature with 70 kDa dextran revealed patent lumens that were void of local leaks (Fig. 12E) and exhibited a diffusive permeability of (8.92 1.47) X 10-7 cm s- (n = 24 vessel segments over 3 devices) at 96 h after HUVEC seeding. 41 3.3.2 Tumor cell seeding and extravasation in microvascular networks Cells were seeded at a density low enough to prevent clogging of the lumen openings and be reflective of the low cell density in vivo,2 yet high enough to observe at least one extravasation event per region of interest (ROI). After varying tumor seeding densities (Fig. + 13A), we selected 0.4 million MDA-MB-231 cells per mL, which produced an average of 21.2 8.7 tumor cells per ROI (24 ROIs over 3 devices) (Figure 13B, 14A). This corresponds to an estimated 0.63 million cells per mL of vascular volume. A B B 35 30 25 25 CL S20 15 0 10 5 0 50 45 40 35 30 0 25 E 20 z 15 10 5 0 20 000 100000 400000 Tumor cell seeding density (cells/mL) * Total cells in 30 C vessels at time 0 of seeding E ' Extravasated cells 0 .0 C I 25 20 15 U 10 5 <t 0 1 2 3 4 5 Region of Interest 6 0 24 Hours after tumor cell seeding . Figure 13. Extravasation in pVNs. (A) Tumor cell seeding density versus the number of tumor cells found per ROI (n=18 ROI over 3 devices). (B) Example of the distribution of the number of extravasated cells in different ROls in a single device. (C) No significant increase in the number of tumor cells from 0 to 24 h is found. Data are presented as mean SD, with *p<0. 0 5 42 C35 -* * 30 j25 20 15 10 5 0 6 24 48 Hours after tumor cell seeding B9 (iii)(A + Figure 14. Visualization of MDA-MB-231 extravasation events. (A) A region of interest 30 minutes after seeding MDA-MB-231 (green) at 0.4 M cells/mL in live RFP-labeled [VN (red). Scale bar is 200 pm. (B) The various positions of tumor cells (green) relative to the endothelial barrier (red) that can be found during a 24-hour culture period, imaged in fixed samples. These include cells that are (i) spread but contained within the lumen, (ii) transmigrated and spread on the outside of the lumen, (iii) circular with protrusions penetrating the HUVEC barrier and contacting the matrix, (iv) transmigrated away from the lumen, (v) circular and adhered within the lumen, and (vi) circular and trapped in vessels with diameters smaller than that of the cell. (C) Extravasation rates of MDA-231 in HUVEC vessels over 48 hours (9 total devices over 3 independent experiments). Data is represented as mean SD. Statistical significance was tested with one-way ANOVA (*p<0.05). Scale bars are 20 pm. 43 Tumor cells were seeded into the vascular network via the application of a 5.2 mmH 20 pressure drop across the HUVEC channel, 96 h after HUVEC seeding. This corresponds to estimated shear stress values in the range of 0.012 to 0.48 Pa during cell seeding, comparable to the range of wall shear stresses found in venular microvessels, (- Pa).2 2 Fixed sample images of seeded MDA-MB-231 revealed their possible locations and morphologies throughout a 4 hour observation period (Fig. 14B). These include cells that are (i) spread but contained within the lumen, (ii) transmigrated and spread on the outside of the lumen, (iii) circular with protrusions penetrating the HUVEC barrier and contacting the matrix, (iv) transmigrated away from the lumen, (v) circular and adhered within the lumen, and (vi) circular and trapped in vessels with diameters smaller than that of the cell. In untreated HUVECS, we quantified an MDA-MB-231 extravasation efficiency of 12.3 + 3.4% after 6 h and 23.6 + 4.5% after 24 h (Fig. 14B). Extravasation could be observed as early as 30 min after tumor cell introduction into the vasculature, while the number of extravasated cells plateaued at around 24 h, with no significant difference in the number of extravasated cells at 48 h (p = 0.298). The average number of tumor cells found in each ROI exhibited a slight yet insignificant (p = 0.37) increase between 0 h and 24 h (Fig. 13C). These results suggest that most extravasation events occur in the first 24 h, which is similar to the time scales witnessed in vivo 9, 3 and in other in vitro platforms." Cell viability was 95.2 + 3.7% at 24 h, suggesting that the adhered yet non-migratory and/or circular cells were likely not due to tumor cell apoptosis. Lastly, 10 tm fluorescent beads introduced into the vasculature were lodged but never extravasated, confirming that extravasation from within the vessels is not a passive process inherent to the platform. 3.3.3 Effect of TNF-a on endothelial barrierfunction and transendothelial migration Inflammation can play a mediating role in cancer progression and metastasis.2426 For instance, elevated levels of pro-inflammatory cytokines including IL- 1s, TNF-a and IL-6 have been found in the circulation of cancer patients, and may upregulate the expression of adhesion molecules on the endothelium or in target organs.2 5 Here, we investigated the response endothelial barrier function and tumor cell TEM rates to TNF-a. Treatment of p.VNs with 2 ng/mL TNF-a for 12 h resulted in a 2.1-fold increase in HUVEC permeability ((18.4 1.1) X 44 10-7 cm/s compared to (8.68 + 0.6) X 10-7 cm/s) to 70 kDa dextran, with no significant difference in cell viability (Fig. 15A). Stimulation with 10 ng/ mL TNF-a led to a 4.6-fold increase in permeability ((41.5 + 7.21) X 10-7 cm/s). The high standard deviation in the 10 ng/mL treatment was investigated; upon closer inspection, we observed what appeared to be focal leaks, and cell viability was found to be significantly lower compared to the control, indicating that such a high concentration of TNF-a led to endothelial cell-death induced ruptures in the lumen (Fig. 15B). Consistent with this, in TNF-a stimulated (2 ng/mL) HUVECs, tumor cell TEM rates increased 2.3-fold (32.3 5.1% compared to 13.1 + 2.12%) (Fig. 15C). These increases in both TEM rate and endothelial permeability to TNF-a stimulation suggest that impaired endothelial function may regulate trans- endothelial migration. 0 * C B . A 30 ~25 ~4O 40 20 .30 J2 20I E lo 10 0 _ 0 ~ _ _ 2 5 0 _ 0 10 2 Concentration of TNF-a (ng/mL) Concentration of TNF-a (ng/mL) Figure 15. The effect of TNF-a on barrier function and TEM efficiency. (A) Graded response of vessel permeability to TNF-a perturbation. (B) High concentrations of TNF-a (10 ng/mL) results in cell-death induced ruptures and focal leaks (red arrow) seen by 70 kDa dextran (white). (C) Effect of TNF-a stimulation on TEM efficiency of MDA-MB-321. Data is represented as mean SD, with 9 total devices over 3 experiments for each condition. Statistical significance was tested with one-way ANOVA and Tukey's Test (*p<0.05). Scale bars are 20 [rM. 3.3.4 Correlation of tumor cell metastatic potential with extravasation ability We investigated the dependency of tumor cell extravasation efficiency on their corresponding metastatic potential. In untreated HUVECs, highly invasive HT-1080 fibrosarcoma cells were found to exhibit a 27.34 + 4.9% extravasation efficiency, which was significantly different from the 13.23 + 3.2% extravasation rate for MDA-MB-231, 4 h after tumor cell seeding (Fig. 16). Furthermore, the non-metastatic normal epithelial cell line MCF- 45 IOA exhibited a 5.31 + 2.3% extravasation rate. These results indicate that human tumor cells exhibiting different metastatic potentials exit the vascular system with different efficiencies and 3s* * that our platform possesses the sensitivity to detect such variations. 30 ' 25 C 20 0 M 15 U1 10 LU Figure 16. Correlation of metastatic potential and TEM efficiency. Extravasation rates of cell lines with different metastatic potentials (MDA-MB-231. HT-1080 and MCF-10A). Statistical significance was tested with one-way ANOVA and Tukey's Test (*p<0.05). Scale bars are 20 prn 3.3.5 Visualization of dynamics of extravasation events Time-lapse confocal microscopy of TC-EC interactions can offer important insights into the temporal and spatial mechanisms of tumor cell extravasation. Analysis of a sequence of images of a transmigrating MDA-MB-231 cell (Fig. 17A) revealed that (1) trans- migrating tumor cells first penetrate the EC barrier by extending thin fillipodial protrusions (-1 pm in width) into the subendothelial matrix, (2) protrusions continue to increase and branch out while the remaining body on the apical side of the lumen maintains its sphericity (3), the spherical body decreases in diameter as more of the cell and the nucleus clears the barrier (4), the tumor cell undergoes significant shape changes as it adopts a final spread morphology upon exiting the lumen. Live time-lapse microscopy at 40X did not reveal a discernable gap in the endothelial plasma membrane at the site of transmigration, suggesting that the area through which tumor cell protrusions penetrate is relatively small, and likely paracellular rather than transcellular. A 46 definitive opening in the barrier was only observed near the end of the extravasation event (i.e. at 3:30 h, Fig. 17A), which was presumably larger to allow the transmigration of the nucleus. This was confirmed via higher resolution imaging at 60X, which revealed small gaps (~1-2 prm) in the endothelial barrier during the initial stages of transmigration (Fig. 17B). Gaps then gradually increased in size to form holes -8-10 pm in diameter upon the transmigration of the tumor cell nuclei (Fig. 17C and D). The remaining portion of the cell body on the apical side remains spherical, even after transmigration of the nucleus, suggesting that the sphericity is not due to that of the nucleus. Furthermore, live nuclear staining at 40X reveals that transmigration of the nucleus occurs within a relatively short time frame (~15 min) com- pared to the total time required for complete tumor cell TEM (Fig. 18). Microscopy at 90X revealed a thin segment of the tumor cell joining the two parts of the cell body on each side of the lumen, suggesting that TEM of most of the cell body occurs via extrusion through a gap of sub nuclear dimensions (Fig. 17J). After transmigration of the tumor cell nucleus, gaps in the EC barrier decreases in size and eventually becomes indiscernible after complete TEM (Fig. 17E and F). Interestingly, staining of VE-cadherin in samples fixed at different time points throughout extravasation events revealed largely intact cell-cell junctions as discerned by confocal microscopy at 60X. Images of MDA-MB-23 I sending out protrusions through the EC barrier before the transmigration of the nucleus revealed localization of the tumor cell protrusions at EC cell-cell junctions (Fig. 19A, B). Notably, ECs adjacent to tumor cells that had undergone nuclear (Fig. 19B) and complete (Fig. 17G-I) transmigration also showed no discernable signs of junction disruption. Importantly, perfusion of the live vessels with 70 kDa dextran revealed no apparent leaks at the sites of complete TEM (Fig. 19C). 47 Figure 17. Visualization of extravasation dynamics. (A) High resolution time-lapse confocal microscopy (40X) of an extravasating entrapped MDA-MB-231 (green). Lumens were labeled with a far-red plasma membrane stain (purple). Tumor cells transmigrate through the endothelium and into the 3D matrix over a period of 4 h. The white arrow at 3:30 h indicates the location of a vessel opening at the site of tumor cell TEM. (B) Confocal images taken at a single slice shows a small gap -1-2 pm forming in the EC barrier at the initial stages of TEM. (C) Gaps in the EC plasma membrane grow in size (-8-10 pm) to allow TEM of the nucleus. (D) A circular is hole is seen in the vessel lumen at the location and instant of tumor cell nuclear TEM. (E) EC membrane gaps diminish in size and (F) eventually become indiscernible after complete TEM. (G) Staining of VE-cadherin (red) after tumor cell (green) extravasation in fixed samples. Images of VE-cadherin and two tumor cells (H) merged and (I) unmerged reveal no apparent disruptions in EC junctional staining after complete TEM. (J) MDA-MB-231 extravasates through a small gap in the EC barrier, as seen by a thin segment of the cell joining the apical/basal portions of the tumor cell (red arrow). All scales bars are 10 pm. 48 - 15 min Figure 18. Dynamics of nuclear TEM. Time-lapse confocal microscopy at 40X reveals the dynamic nature of the transmigration of the tumor cell nucleus (blue). Transmigration of the nucleus occurs within a relatively short time frame (-15 min) compared the total time required for complete cell TEM (-4 h). Figure 19. VE-cadherin staining at extravasation sites. (A) An MDA-MB-231 cell that has extended protrusions into the subendothelial matrix, before transmigration of the nucleus. Tumor cell (green) protrusions appear localized at EC cell-cell junctions (red). (B) Tumor cell in mid-TEM, after transmigration of the nucleus. Unmerged and merged images of VE-cadherin and tumor cells in all images show indiscernible delocalization in junctional staining. Scale bars are 10 pm. (C) Perfusion with 70-kDa dextran revealed no leaks at the sites of extravasation (red: dextran, green: MDA-MB-23 1). Scale bar is 20 pm. 49 3.3.6 Transmigration of different tumor cell subpopulations We are able to observe arrested cells on the endothelium that are either mechanically trapped, or adhered and non-trapped. Non-trapped cells remained adhered onto the luminal side of the endothelium in vessels with diameters larger than that of the tumor cell, even after vessel perfusion (Fig. 20A). This suggests the presence of purely adhesive interactions with the endothelium in contrast to cells lodged mechanically in narrow constrictions (Fig. 20B), which composed an average of 16.2 + 12.3% of the total number of tumor cells found in each ROT. Analysis of each subpopulation revealed that trapped cells exhibited a significantly higher rate of 4.67%) compared to arrested non-trapped cells (9.8 + 3.3%) (Fig. 20D). A - D 60 50 * TEM (47.8 *40 V 30 20 B0 E 80 trapped * adhered 70 -60 S50 &40 230 20 10 0 single cells clusters Figure 20. TEM efficiencies of different tumor cell subpopulations. (A) Non-trapped adhered tumor cell at 30 min and 4 h after seeding. (B) Entrapped tumor cell at 30 min and 4 h after seeding. (C) Tumor cell cluster (>2 adjacent cells) at 30 min and 4 h after seeding. (D) TEM efficiency of adhered non-trapped and trapped subpopulations. (E) SD, with 9 total devices over 3 TEM efficiency of single cell and collective cells. Data are represented as mean independent experiments for each condition. Statistical significance was tested with one-way ANOVA and Tukey's Test (*p<0.00 1). All scale bars are 20 pm. 50 Furthermore, we visualized TEM events of both single adhered tumor cells and tumor cell clusters, which is defined as a group of more than 2 contacting cells (Fig. 20C). Cells classified in the cluster population exhibited a TEM rate of 67.8 + 7.2% while single cells exhibited a significantly lower rate of 8.3 + 2.6% (Fig. 20E). 3.4 Discussion Our extravasation platform features the advantages of microfluidic technology, including tight control of tumor microenvironment factors and high spatiotemporal resolution, combined with the increased physiological relevance of self-organized 3D pVNs. Vessel permeability values found were comparable to that of in vivo venules 27 and similar to existing in vitro ptVN platforms produced via angiogenic sprouting' 8 suggesting a strong and more physiologically relevant barrier compared to those reported in in vitro EC monolayers.13 ,4 2 8 2 9 Moreover, the relative quiescence of these microvessels allows us to justify the decoupling of vessel remodeling and extravasation occurring within the time frame in which the events are studied. Together, these results confirm that TEM in our platform is an active process of endothelial barrier penetration by the invading tumor cell. Although progress has been made in identifying critical regulators of endothelial-tumor interactions in the context of intravasation,30- 32 it remains unclear whether impaired barrier function is a necessary precursor to TEM in extravasation. Here, the increased TEM efficiency and endothelial permeability observed in response to TNF-a stimulation corroborates the findings of our previous work involving increased intravasation rates of HT-1080 cells across TNF- a activated HUVEC mono- layers.' 4 The positive correlations observed between extravasation rates and vessel permeability have also been observed in in vivo rat tail-vein 9 and transparent zebrafish 5 models subject to VEGF overexpressing tumor cells, which induced endothelial barrier disruption. Although not explored in this study, in addition to promoting vascular leak, TNF-a is known to upregulate cell surface adhesion molecule expression on endothelial monolayers3 3 and promotes tumor cell adhesion to endothelial cells.3 3 ,3 4 It is well 51 accepted that leukocyte adhesion, and more recently, tumor cell adhesion to the endothelium is a precursor to TEM.16,35,36 Although the metastatic potentials of different tumor cell lines are well characterized in various in vivo models, 3 7- 3 9 the dependence of extravasation efficiency on metastatic abilities remains unclear. Koop et al. demonstrated similar extravasation kinetics of highly metastatic PAP2, non-metastatic NIH3T3 and primary fibroblast cells from mouse embryos, suggesting that extravasation is independent of metastatic potential in chick CAM models.40 Contrarily, Stoletov et al. showed a clear positive correlation between the metastatic potentials of different tumor cell lines and their extravasation abilities (HT1080 > MDA-MB-231 > MDA-MB-435) in an in vivo zebrafish model.5 Interestingly, the results obtained from our platform corroborate those observed in the zebrafish model, with HT1080 exhibiting a higher extravasation rate than MDAMB-231. MCF-10A is a non-tumorigenic cell line often used as a control condition in TEM assays. Here, they exhibit a significantly decreased tendency to extravasate compared to metastatic cells lines. The basal level of extravasation present (~5%) is likely dependent on the level of robustness of the endothelial barrier in the in vitro platform, and is consistent with the basal levels of MCF-1OA extravasation observed in in vitro 2D transwell assays. 41 These results indicate tumor cell extravasation correlates with metastatic potential, and that our platform possesses the sensitivity to detect such differences in invasiveness. Visualization of the cellular mechanisms of extravasation in mouse and chick chorioallantoic membrane assays have established the existence of complex tumor-endothelial inter- actions that may involve passive or active tumor cell movement, adhesion and transmigration; characterized. however, the precise mechanisms 4 4 at the single cell level are poorly Understanding these mechanisms are important because metastasis is inherently a mechanical transport phenomenon characterized by the release of single cells from a primary tumor, which invade through small pores of the tissue matrix, extravasate across EC barriers, and circulate in the vasculature. The effects of tumor cell extravasation on the structure and viability of the endothelium have also been studied, although the precise nature of these 52 events remains unclear.16 32 Using our assay, we demonstrate, for the first time, the dynamic ECTC interactions during TEM in high spatio-temporal resolution from within in vitro microfluidic iVNs. The portion of the tumor cell body on the apical side of the lumen was found to retain its sphericity, while extending fillipodial protrusions into the matrix through a small gap in the endothelial barrier through which the rest of the cell body extrudes. This gap gradually increases in size from ~1 pm to 8 pm as the tumor cell nucleus transmigrates. Cells then finally achieve spread morphology upon transit of the entire cell body through the vascular wall and gaps in the EC barrier are repaired. Furthermore, via immunofluorescent visualization of VE-cadherin, we hypothesize that any disruption to endothelial junctions associated with TEM may be (1) only transient, (2) indiscernible by high magnification confocal imaging at 60X, (3) small enough to allow continued local barrier function against 70 kDa dextran, or (4) non-existent due to transcellular instead of paracellular TEM. The ability of tumor cells to migrate past narrow constrictions was recently demonstrated via the transit of MDA-MB-231 through mechanical confinements of sub nuclear dimensions by undergoing significant cell elongation and nuclear deformations.45 Furthermore, the observed TEM mechanism resembles paracellular leukocyte diapedisis, where cells penetrate the endothelial junction by insertion of microvilli-like projections and migrate between ECs by squeezing through a narrow channel of sub nuclear dimensions while maintaining extensive membrane contact, and imposing only a small transient disruption to the endothelial junction. 4 - 8 Lastly, comparison with intravasation events in a planar EC monolayer platform' 4 leads to a hypothesis regarding the mechanistic differences between two processes. In the intravasation assay, traction forces are likely only generated at the leading edge of the migrating cell and may be limited to the 2D apical and basal surfaces of the contacting endothelium. In contrast, extravasating cells are likely to adhere to the 3D subendothelial matrix by extending extensive protrusions and generate traction forces via the matrix, possibly allowing them to pull their body past the endothelial barrier. Currently, two theories exist regarding the mechanisms of cell arrest on the vessel wall. Paget's "seed and soil" hypothesis describes the selective adherence of tumor cells to the endothelium prior to TEM. In another mode, tumor cells can become physically trapped in small vessels due to their size and eventually become activated and transmigrate.- 5 However, current experimental data using various types of assays reveal contradictory results regarding the 53 specificity of the initial interactions between the endothelium and circulating tumor cells. Using our platform, we observe a subpopulation of physically occluded tumor cells within the iiVNs, which exhibited a markedly higher TEM rate than adhered non- trapped cells. This may be attributed to the fact that lodged cells have access to more adhesion sites on the endothelium, as the area of TC-EC contact is greater. In future studies, the perfusability of our ptVNs will enable us to elucidate the mechanisms of tumor cell extravasation under dynamic conditions including the mechanisms of cell rolling and adhesion under continuous flow. Similarly, our platform enables the observation of tumor clusters, which exhibited a significantly higher TEM efficiency compared to single adhered cells. The increased TEM rate of clusters may be attributed to several mechanisms including (1) an increase in the local concentration of tumor-secreted biochemical factors that regulate endothelial permeability, (2) access to the subendothelial matrix provided by a previously transmigrated cell, and (3) the inability to repair the endothelial damage before the transmigration of another tumor cell in the cluster. In particular, tumor paracrine factors can contribute to increased TEM efficiency via the modulation of endothelial permeability, such as impairment of the endothelial barrier function by tumor secreted VEGF.' As such, tumor cell clusters may induce a higher localized concentration of permeability enhancing paracrine factors. Furthermore, studies have revealed the irreversibility of endothelial barrier damage after transmigration of tumor spheroids1 6 compared to the reversibility after single cell transmigration,5 indicating that there may exist differences in single and collective cell behavior. As such, the increased TEM efficiency of cell clusters may be attributed to an irreversibly damaged endothelium, induced by the loss of ECM contacts, endothelial retraction and apoptosis. 54 Chapter 3 References 1. G. L. Nicolson, Curr. Opin. Cell Biol., 1989, 1, 1009-1019. 2. K. J. Luzzi, I. C. MacDonald, E. E. Schmidt, N. Kerkvliet, V. L. Morris, A. F. Chambers and A. C. Groom, Am. J. Pathol., 1998, 153, 865-873. 3. K. Podsypanina, Y. C. Du, M. Jechlinger, L. J. Beverly, D. Hambardzumyan and H. Varmus, Science, 2008, 321, 1841-1844. 4. E. Sahai, Nat. Rev. Cancer, 2007, 7, 737-749. 5. K. Stoletov, H. Kato, E. Zardouzian, J. Kelber, J. Yang, S. Shattil and R. Klemke, J Cell Sci., 2010, 123, 2332-2341. 6. J. L. Townson and A. F. Chambers, Cell cycle, 2006, 5, 1744-1750. 7. M. J. Hendrix, E. A. Seftor, R. E. Sefior and I. J. Fidler, CancerLett., 1987, 38, 137-147. 8. Q. J. Dimilla PA, Albelda SM, Lauffenburger DA AIChE J., 1992, 38, 1092-1104. 9. A. B. Al-Mehdi, K. Tozawa, A. B. Fisher, L. Shientag, A. Lee and R. J. Muschel, Nat. Med., 2000, 6, 100-102. 10. Y. Shin, S. Han, J. S. Jeon, K. Yamamoto, I. K. Zervantonakis, R. Sudo, R. D. Kamm and S. Chung, Nat. Protoc., 2012, 7, 1247-1259. 11. J. W. Song, S. P. Cavnar, A. C. Walker, K. E. Luker, M. Gupta, Y. C. Tung, G. D. Luker and S. Takayama, PLoS One, 2009, 4, e5756. 12. Q. Zhang, T. Liu and J. Qin, Lab on a chip, 2012, 12, 2837-2842. 13. J. S. Jeon, I. K. Zervantonakis, S. Chung, R. D. Kamm and J. L. Charest, PLoS One, 2013, 8, e56910. 14. 1. K. Zervantonakis, S. K. Hughes-Alford, J. L. Charest, J. S. Condeelis, F. B. Gertler and R. D. Kamm, Proc. Natl..Acad. Sci. U. S. A., 2012, 109, 13515-13520. 15. K. C. Chaw, M. Manimaran, E. H. Tay and S. Swaminathan, Lab on a chip, 2007, 7, 1041- 1047. 16. C. Heyder, E. Gloria-Maercker, F. Entschladen, W. Hatzmann, B. Niggemann, K. S. Zanker and T. Dittmar, J. CancerRes. Clin. Oncol., 2002, 128, 533-538. 17. Y. H. Hsu, M. L. Moya, P. Abiri, C. C. Hughes, S. C. George and A. P. Lee, Lab on a chip, 2013, 13, 81-89. 18. S. Kim, H. Lee, M. Chung and N. L. Jeon, Lab on a chip, 2013, 13, 1489-1500. 55 19. J. W. Song and L. L. Munn, Proc. Natl. Acad. Sci. U. S. A., 2011, 108, 15342-15347. 20. S. K. Muthuswamy, D. Li, S. Lelievre, M. J. Bissell and J. S. Brugge, Nat. Cell Biol., 2001, 3, 785-792. 21. S. Nagrath, L. V. Sequist, S. Maheswaran, D. W. Bell, D. Irimia, L. Ulkus, M. R. Smith, E. L. Kwak, S. Digumarthy, A. Muzikansky, P. Ryan, U. J. Balis, R. G. Tompkins, D. A. Haber and M. Toner, Nature, 2007, 450, 1235-1239. 22. S. Sheikh, G. E. Rainger, Z. Gale, M. Rahman and G. B. Nash, Blood, 2003, 102, 2828-2834. 23. D. Y. Qian B, Im JH, Muschel RJ, Zou Y, et al. , PLoS One, 2009, 4. 24. B. McDonald, J. Spicer, B. Giannais, L. Fallavollita, P. Brodt and L. E. Ferri, Int. J. Cancer, 2009, 125, 1298-1305. 25. A. Mantovani, P. Allavena, A. Sica and F. Balkwill, Nature, 2008, 454, 436-444. 26. P. L. Tremblay, J. Huot and F. A. Auger, Cancer Res., 2008, 68, 5167-5176. 27. W. Yuan, Y. Lv, M. Zeng and B. M. Fu, Microvasc. Res., 2009, 77, 166-173. 28. K. M. Chrobak, D. R. Potter and J. Tien, Microvasc. Res., 2006, 71, 185-196. 29. Y. Zheng, J. Chen, M. Craven, N. W. Choi, S. Totorica, A. Diaz-Santana, P. Kermani, B. Hempstead, C. Fischbach-Teschl, J. A. Lopez and A. D. Stroock, Proc. Natl. Acad Sci. U. S. A., 2012, 109, 9342-9347. 30. C. T. Mierke, J. Biol. Chem., 2011, 286, 40025-40037. 31. H. H. Peng and C. Dong, Cellular and molecular bioengineering, 2009, 2, 375-3 85. 32. S. Weis, J. Cui, L. Barnes and D. Cheresh, J. Cell Biol., 2004, 167, 223-229. 33. G. S. Teo, J. A. Ankrum, R. Martinelli, S. E. Boetto, K. Simms, T. E. Sciuto, A. M. Dvorak, J. M. Karp and C. V. Carman, Stem Cells, 2012, 30, 2472-2486. 34. G. Haraldsen, D. Kvale, B. Lien, I. N. Farstad and P. Brandtzaeg, J. Immunol., 1996, 156, 2558-2565. 35. F. L. Miles, F. L. Pruitt, K. L. van Golen and C. R. Cooper, Clin. Exp. Metastasis, 2008, 25, 305-324. 36. K. Zen, Liu, D.-Q., Guo, Y.-L., Wang, C., Shan, J., Fang, M., Zhang, C.-Y., et al., PloS one, 2008, 3. 37. R. E. Hewitt, A. McMarlin, D. Kleiner, R. Wersto, P. Martin, M. Tsokos, G. W. Stamp and W. G. Stetler-Stevenson, J. Pathol., 2000, 192, 446-454. 56 38. K. Stoletov, V. Montel, R. D. Lester, S. L. Gonias and R. Klemke, Proc. Natl. Acad Sci. U. S. A., 2007, 104, 17406-17411. 39. A. Zijlstra, R. Mellor, G. Panzarella, R. T. Aimes, J. D. Hooper, N. D. Marchenko and J. P. Quigley, CancerRes., 2002, 62, 7083-7092. 40. S. Koop, E. E. Schmidt, I. C. MacDonald, V. L. Morris, R. Khokha, M. Grattan, J. Leone, A. F. Chambers and A. C. Groom, Proc. Natl. Acad. Sci. U. S. A., 1996, 93, 11080-11084. 41. A. Sahni, M. T. Arevalo, S. K. Sahni and P. J. Simpson-Haidaris, Int. J. Cancer, 2009, 125, 577-584. 42. A. Colmone, M. Amorim, A. L. Pontier, S. Wang, E. Jablonski and D. A. Sipkins, Science, 2008, 322, 1861-1865. 43. Y. Kienast, L. von Baumgarten, M. Fuhrmann, W. E. Klinkert, R. Goldbrunner, J. Herms and F. Winkler, Nat. Med., 2010, 16, 116-122. 44. D. A. Sipkins, X. Wei, J. W. Wu, J. M. Runnels, D. Cote, T. K. Means, A. D. Luster, D. T. Scadden and C. P. Lin, Nature, 2005, 435, 969-973. 45. M. Mak, C. A. Reinhart-King and D. Erickson, Lab on a chip, 2013, 13, 340-348. 46. M. Vicente-Manzanares and F. Sanchez-Madrid, Nat. Rev. Immunol., 2004, 4, 110-122. 47. B. Petri and M. G. Bixel, The FEBSjournal,2006, 273, 43 99-4407. 48. S. Nourshargh, P. L. Hordijk and M. Sixt, Nat. Rev. Mol. Cell Biol., 2010, 11, 366-378. 49. I. J. Fidler, Nat. Rev. Cancer, 2003, 3, 453-458. 50. J. D. Crissman, J. S. Hatfield, D. G. Menter, B. Sloane and K. V. Honn, Cancer Res., 1988, 48, 4065-4072. 51. S. Koop, R. Khokha, E. E. Schmidt, I. C. MacDonald, V. L. Morris, A. F. Chambers and A. C. Groom, Cancer Res., 1994, 54, 4791-4797. 52. E. J, Philadelphia:W. B. Saunders., 1928. 53. L. Hu, N. Ferrara and R. B. Jaffe, Exp. Biol. Med. (Maywood), 2006, 231, 1646-1652. 54. N. Utoguchi, H. Mizuguchi, K. Saeki, K. Ikeda, Y. Tsutsumi, S. Nakagawa and T. Mayumi, CancerLett., 1995, 89, 7-14. 55. F. E. Curry, V. H. Huxley and R. H. Adamson, Am. J. Physiol., 1983, 245, H495-505. 57 Chapter 4: Conclusions We have presented a microfluidic extravasation assay consisting of self-organized perfusable 3D vasculature that allows for the study of tumor extravasation from within in vitro p.VNs. We demonstrate the effect of inflammatory cytokine stimulation on endothelial barrier function and TEM efficiency, and the positive correlation between metastatic potentials of different cell lines and their extravasation capabilities. We characterize, for the first time, the mechanisms of tumor cell extravasation dynamics in high spatiotemporal resolution from within in vitro pVNs and observe the TEM patterns of different tumor cell subpopulations, including mechanically trapped tumor cells, single adhered cells and tumor clusters. Our ability to enable high-throughput parametric studies in a tightly con- trolled environment coupled with increased physiological relevance compared to 2D and 3D planar monolayer models will give rise to new insights regarding the complex endothelial- tumor cell interactions in extravasation and facilitate the identification of factors to target this crucial step in cancer metastasis. 58 Appendix 1: Vasculogenesis Seeding Protocol Michelle Chen 05/24/2014 1. Aliquot 15 ul of fibrin gel into 0.5mL eppendorf tubes. Mix well before aliquoting. 2. Get HUVEC and FB (T 25 flasks) from incubator. Aspirate media. Wash each once with warm PBS. Aspirate. 3. Add 1 mL trypsin to each flask. Swirl to make sure it covers entire bottom. 4. At 3 minutes, remove from incubator, tap the flask gently on the side to loosen cells. Check under microscope that they are indeed detached and floating. 5. Add I mL of warm EGM to each flask and mix gently a few times with P1000. 6. Transfer the 2mL to corresponding 15 mL tubes. 7. Count cells using Trypan blue using hemocytometer 8. Place tubes in centrifuge 9. 6 million/mL (HUVEC) and 10 million/mL (FB). 10. While centrifuge is still running, make suspension media -4 Aliquot 920 ul of the EGM into eppendorf tube. Add the thrombin aliquot (around 40 ul, the whole tube). 11. Get collagen I from fridge (hold by stopper) 12. Put collagen on ice and add 80 ul of it to suspension media. Now we have total 1000 ul of suspension media. Put collagen back in fridge immediately. 13. Take vials from centrifuge and aspirate supernatant. 14. Resuspend cells 15. Get humidity box from incubator. 16. Put one device into a 10cm2 dish (NOT cell star!) 17. Do ECs first. Take 15 ul of EC suspension and mix with 15ul of fibrin aliquot 18. Immediately fill middle channel, from both sides. 19. Cap dish and check under scope to see if density is good. Adjust density using leftover suspension media if necessary. 20. Do the same for the 2 FB channels. Use one vial for for both channels 21. Put into humidity box, start timer after 1s device 22. After 25 minutes, start media filling. 23. Make a humidity dish using PBS and put next to device. 24. Incubate and repeat with other devices. 59