Health Law and the Relationship Between Prayer and Health Outcomes
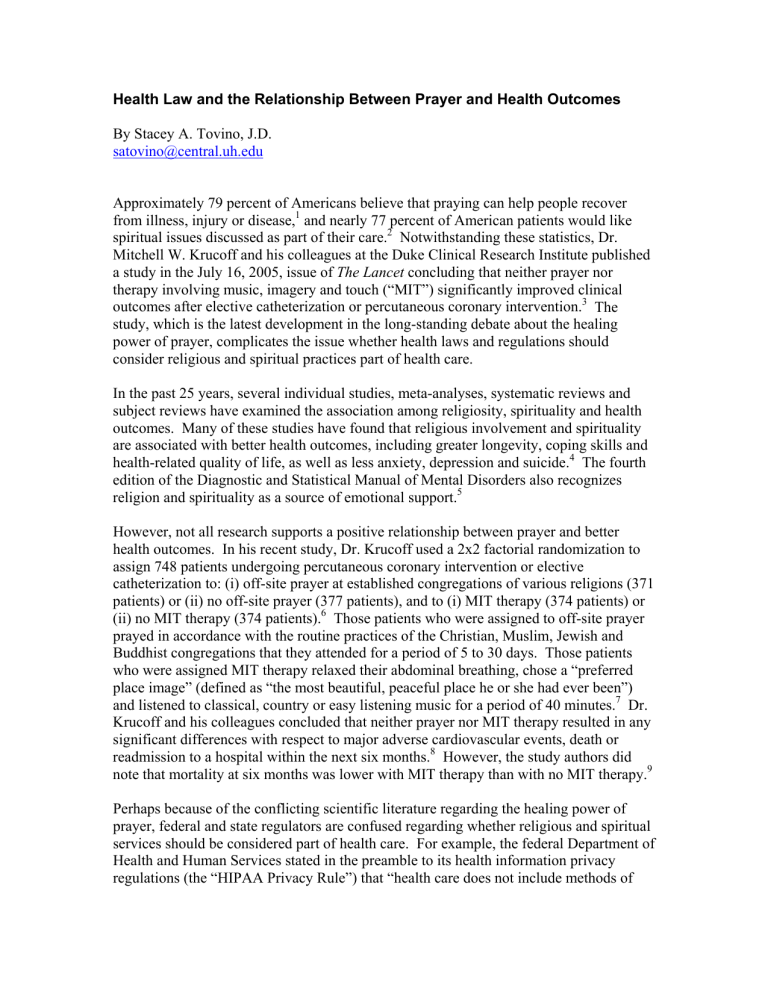
Health Law and the Relationship Between Prayer and Health Outcomes
By Stacey A. Tovino, J.D. satovino@central.uh.edu
Approximately 79 percent of Americans believe that praying can help people recover from illness, injury or disease,
and nearly 77 percent of American patients would like
spiritual issues discussed as part of their care.
Notwithstanding these statistics, Dr.
Mitchell W. Krucoff and his colleagues at the Duke Clinical Research Institute published a study in the July 16, 2005, issue of The Lancet concluding that neither prayer nor therapy involving music, imagery and touch (“MIT”) significantly improved clinical outcomes after elective catheterization or percutaneous coronary intervention.
study, which is the latest development in the long-standing debate about the healing power of prayer, complicates the issue whether health laws and regulations should consider religious and spiritual practices part of health care.
In the past 25 years, several individual studies, meta-analyses, systematic reviews and subject reviews have examined the association among religiosity, spirituality and health outcomes. Many of these studies have found that religious involvement and spirituality are associated with better health outcomes, including greater longevity, coping skills and health-related quality of life, as well as less anxiety, depression and suicide.
edition of the Diagnostic and Statistical Manual of Mental Disorders also recognizes religion and spirituality as a source of emotional support.
However, not all research supports a positive relationship between prayer and better health outcomes. In his recent study, Dr. Krucoff used a 2x2 factorial randomization to assign 748 patients undergoing percutaneous coronary intervention or elective catheterization to: (i) off-site prayer at established congregations of various religions (371 patients) or (ii) no off-site prayer (377 patients), and to (i) MIT therapy (374 patients) or
(ii) no MIT therapy (374 patients).
Those patients who were assigned to off-site prayer
prayed in accordance with the routine practices of the Christian, Muslim, Jewish and
Buddhist congregations that they attended for a period of 5 to 30 days. Those patients who were assigned MIT therapy relaxed their abdominal breathing, chose a “preferred place image” (defined as “the most beautiful, peaceful place he or she had ever been”) and listened to classical, country or easy listening music for a period of 40 minutes.
Krucoff and his colleagues concluded that neither prayer nor MIT therapy resulted in any significant differences with respect to major adverse cardiovascular events, death or readmission to a hospital within the next six months.
However, the study authors did
note that mortality at six months was lower with MIT therapy than with no MIT therapy.
Perhaps because of the conflicting scientific literature regarding the healing power of prayer, federal and state regulators are confused regarding whether religious and spiritual services should be considered part of health care. For example, the federal Department of
Health and Human Services stated in the preamble to its health information privacy regulations (the “HIPAA Privacy Rule”) that “health care does not include methods of
healing that are solely spiritual”
and that “clergy or other religious practitioners that
provide solely religious healing services are not health care providers within the meaning of th[e HIPAA Privacy Rule] . . . .”
On the other hand, the Centers for Medicare & Medicaid Services stated in the preamble to its January 12, 2001, final regulations addressing Medicare payment for nursing and allied health education that, “[a]s early as the mid-1970s, Medicare recognized pastoral care as having a beneficial and therapeutic effect on the medical condition of a patient, and, therefore, the costs a provider incurs to furnish such care to its patients are considered patient care related costs.”
In addition, regulations implementing the Texas
Hospital Licensing Law explain that “the care of the patient includes consideration of the
. . . spiritual . . . variables that influence the perceptions of illness.”
Scientists have yet to reach a consensus regarding the relationship between prayer and health outcomes. Until they do, federal and state regulators may continue to debate the appropriateness of including religious and spiritual services within legal definitions of health care.
1
See Laurel Arthur Burton & Marcia Sue DeWolf Bosek, When Religion May Be an Ethical Issue , 39 J.
R ELIGION & H EALTH 97, 97 (2000) (citing a poll Gallup conducted for CNN/USA Today); P ROFESSIONAL
C HAPLAINCY : I TS R OLE AND I MPORTANCE IN H EALTHCARE 2 (Larry VandeCreek & Laurel Burton eds.,
2001) [hereinafter P ROFESSIONAL C HAPLAINCY ] (citing Marty Kaplan, Ambushed by Spirituality , T IME ,
June 24, 1996, at 62) (citing similar statistics).
2
Burton & Bosek, supra note 1, at 97. For additional statistics describing Americans’ beliefs relating to religion, spirituality, and health care, see H AROLD G. K OENIG ET AL ., H ANDBOOK OF R ELIGION AND
3
H EALTH 4 (2001).
Mitchell W. Krucoff, Music, Imagery, Touch, and Prayer as Adjuncts to Interventional Cardiac Care:
The Monitoring and Actualisation of Noetic Trainings (MANTRA) II Randomised Study , 366 L ANCET 211,
4
211 (July 16, 2005), available at http://home.infostations.net/srm/3204A.pdf
.
See, e.g.
, P ROFESSIONAL C HAPLAINCY , supra note 1, at 11 (discussing a recent meta-analysis of data from
42 published mortality studies, involving approximately 126,000 participants, that demonstrated that persons who reported frequent religious involvement were significantly more likely to live longer than persons who were involved infrequently); Paul S. Mueller et al., Religious Involvement, Spirituality, and
Medicine: Implications for Clinical Practice , 76 M AYO C LINIC . P ROC . 1225, 1226 (2001) (“[A] majority of the nearly 350 studies of physical health and 850 studies of mental health that have used religious and spiritual values have found that religious involvement and spirituality are associated with better health outcomes.”). S ee generally L ARRY D OSSEY , H EALING W ORDS : T HE P OWER OF P RAYER AND THE P RACTICE
OF M EDICINE 161-230 (1993); P ASTOR AND P ATIENT : A H ANDBOOK FOR C LERGY W HO V ISIT THE S ICK
(Richard Dayringer ed., 1982); T
HE
S
PIRITUAL
C
HALLENGE OF
H
EALTH
C
ARE
(Mark Cobb & Vanessa
Robshaw eds., 1998); Martha Ellen F. Highfield, Providing Spiritual Care to Patients with Cancer , 4
C LINICAL J. O NCOLOGY N URSING 115 (2000); Jeffrey S. Levin & Linda M. Chatters, Research on Religion and Mental Health: An Overview of Empirical Findings, in H ANDBOOK OF R ELIGION AND M ENTAL H EALTH
33, 33-50 (Harold G. Koenig ed., 1998); Jacqueline R. Mickley et al., Spiritual Well-Being, Religiousness and Hope Among Women with Breast Cancer, 24 I MAGE J. N URSING S CHOLARSHIP . 267 (1992); William R.
Miller & Carl E. Thoresen, Spirituality, Religion, and Health: An Emerging Research Field , 58 A M .
P SYCHOLOGIST 24 (2003); William R. Miller & Carl E. Thoreson, Spirituality and Health , in I NTEGRATING
S
PIRITUALITY INTO
T
REATMENT
3-18 (William R. Miller ed., 1999); Johanna J. Mytko & Sara J. Knight,
Body, Mind and Spirit: Towards the Integration of Religiosity and Spirituality in Cancer Quality of Life
Research , 8 P SYCHO ONCOLOGY 439 (1999).
5
A MERICAN P SYCHIATRIC A SSOCIATION , D IAGNOSTIC AND S TATISTICAL M ANUAL OF M ENTAL D ISORDERS
685 (4 th
ed., 1994).
6
Krucoff, supra note 3, at 211.
7
Id . at 212.
8
Id . at 211.
9
Id .
10
Standards for Privacy of Individually Identifiable Health Information, 65 Fed. Reg. 82462, 82568 (Dec.
28, 2000), as amended by 67 Fed. Reg. 53138 (Aug. 14, 2002) [hereinafter “HIPAA Privacy Rule”].
11
Id . See generally Stacey A. Tovino, Hospital Chaplaincy: Health Care or “Just Visiting the Sick?” 2
I
NDIANA
H
EALTH
L. R
EV
. (forthcoming 2005) (discussing the implications of hospital chaplaincy under the
HIPAA Privacy Rule).
12
Medicare Program; Payment for Nursing and Allied Health Education, 66 Fed. Reg. 3358, 3366 (Jan. 12,
2001). The Medicare Program allows hospitals to include costs relating to most first year clinical pastoral education residencies in their administrative and general cost centers. Medicare Program; Changes to the
Hospital Inpatient Prospective Payment Systems and Fiscal Year 2004 Rates, 68 Fed. Reg. 45346, 45426-
27 (Aug. 1, 2003).
13
25 T EX . A DMIN . C ODE § 133.42(a)(1)(B)(i) (2005).