An Abstract of the Thesis of
advertisement

An Abstract of the Thesis of
A.B. Moos for the degree of Doctor of Philosophy in Comparative Veterinary Medicine
presented on December 12, 1996, Title: The Role of Proinflammatory Mediators Effects
of 2.3.7.8-tetrachlorodibenzo-p-dioxin Induced Immunotoxicities.
Redacted for Privacy
Abstract Approved
Nancy I. Kerkvliet
Exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) results in both an
enhanced inflammatory response and a suppressed antibody response following
administration of intraperitoneal (ip) sheep red blood cells (SRBC). The objectives of
these studies were to evaluate the role of inflammatory mediators in these immunotoxic
responses to TCDD and to determine whether these responses are linked mechanistically
through an alteration in levels of specific inflammatory mediators.
The role of interleukin-1 (IL-1), tumor necrosis factor (TNF) and nitric oxide
(NO) in the TCDD-induced enhanced peritoneal inflammatory response and suppressed
antibody response to SRBC was evaluated in C57B1/6 mice. The inflammatory cell
influx and the number of plaque forming cells (PFC) generated in response to ip SRBC
were measured following exposure to TCDD and the administration of exogenous
cytokines or specific cytokine inhibitors. The effects of exposure to TCDD on the
production of inflammatory mediators by peritoneal cells were also measured. Finally,
the effects of TCDD exposure on the intracellular processing and secretion of TNF was
evaluated in cultured murine macrophages using immunohistochemistry and flow
cytometry.
TCDD exposure resulted in an increase in the production and secretion of TNF by
peritoneal cells. Circulating levels of TNF also increased in mice exposed to TCDD and
injected with SRBC. Studies using specific cytokine inhibitors demonstrated that the
TCDD-induced increase in TNF activity is critical in mediating the enhanced
inflammatory response to SRBC. Interestingly, although exogenous TNF was shown to
suppress antibody production, increased TNF activity did not affect the TCDD-induced
antibody suppression. TCDD exposure also resulted in an increase in NO produced by
activated peritoneal cells, and inhibition of NO production partially restored the TCDDinduced suppression in the antibody response to SRBC.
These studies indicate that TCDD exposure alters the profile of inflammatory
mediators produced by peritoneal cells, and that an alteration in levels of specific
inflammatory mediators contributes to the TCDD-induced effects of hyperinflammation
and antibody suppression. Results suggest, however, that enhancement of the
inflammatory response by TCDD is not linked mechanistically to suppression of the
antibody response through an alteration in levels of the inflammatory mediators tested.
The Role of Proinflammatory Mediators in
2,3,7,8-Tetrachlorodibenzo-p-dioxin Induced
Immunotoxicities
by
A.B. Moos
A Thesis
submitted to
Oregon State University
In partial fulfillment of the requirements
for the degree of
Doctor of Philosophy
Completed December 12, 1996
Commencement June 1997
Doctor of Philosophy thesis of A. B. Moos presented on December 12, 1996
APPROVED:
Redacted for Privacy
Major Professor, representing Comparative Veterinary Medicine
Redacted for Privacy
Dean, College of Veterinary Medicine
Redacted for Privacy
Dean of Graduate Sc
I understand that my thesis will become part of the permanent collections of Oregon State
University libraries. My signature below authorizes release of my thesis to any reader
upon request.
Redacted for Privacy
A.B. Moos, Author
Contribution of Authors
The coauthors of the chapters are listed below.
L. Baecher-Steppan
Technical support
N.I. Kerkvliet
Technical support
Critical review of data, experimental design and
manuscripts
J.A. Oughton
Technical support
Table of Contents
Chapter One:
Introduction
1
Chapter Two:
Acute Inflammatory Response to Sheep Red Blood Cells
in Mice Treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD):
The Role of Proinflammatory Cytokines, IL-1 and TNF
17
Chapter Three:
The Effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) on
Tumor Necrosis Factor (TNF) Production by Peritoneal Cells
30
Chapter Four:
Inhibition of Tumor Necrosis Factor Activity Fails to Restore 2,3,7,8­
tetrachlorodibenzo-p-dioxin (TCDD)-induced Suppression of the Antibody
Response to Sheep Red Blood Cells
50
Chapter Five:
The Involvement of Nitric Oxide in TCDD-induced Hyperinflammation
and Antibody Suppression
65
Chapter Six:
Conclusions
83
References
86
List of Figures
Figure
Page
1.1
Structure of 2,3,7,8-tetrachlordibenzo-p-dioxin (TCDD)
1
1.2
The Ah Receptor Model
5
1.3
Acute Inflammatory Response: Endothelial Cell Activation
9
2.1
The Effect of TCDD on Peritoneal Exudate Cells
22
2.2
The Effects of IL-lra and rhuTNFR:Fc on Peritoneal Exudate Cells
25
3.1
Intra-cellular TNF Staining Evaluated by Immunofluorescence
and Flow Cytometric Analysis
38
3.2
TNF Fluorescence of LPS Stimulated IC-21 Cells
40
4.1
The Effects of rhuTNFR:Fc on Plaque-forming Cells
57
5.1
The Effects of Aminoquanidine on Spleen Cell Recovery
and Plaque-forming Cells
74
List of Tables
Table
2.1
Page
Comparison Between the Effects of TCDD and Exogenous Cytokines
on Peritoneal Exudate Cells
23
The Effects of TCDD on Plasma TNFa Following Sheep Red Blood
Cell Injection
26
The Effects of TCDD Exposure on TNF Secretion by
LPS Stimulated IC-21 Cells
36
The Effects of TCDD Exposure on TNF Secretion by
LPS Stimulated Peritoneal Cells
37
3.3
TNF Mean Channel Fluorescence in IC-21 Exposed to TCDD
42
4.1
The Effects of Exogenous of TNF on Anti-SRBC Plaque-forming Cells
56
5.1
The Effects of TCDD Thioglycollate-elicited Peritoneal Exudate Cells
70
5.2
The Effects of In Vivo Exposure to TCDD on Ex Vivo Production of NO
by Peritoneal Exudate Cells
71
The Effects of Aminoquanidine on SRBC-induced Peritoneal Exudate Cells
72
2.2
3.1
3.2
5.3
The Role of Proinflammatory Mediators in
2,3,7,8-Tetrachlorodibenzo-p-dioxin Induce Immunotoxicities
Chapter One
Introduction
TCDD:
2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) is the prototype for a large group of
structurally related halogenated aromatic hydrocarbons (HAH) (fig. 1). These compounds
are lipophilic and extremely resistant to environmental and biological degradation. As a
consequence they tend to persist in the environment for long periods of time and
concentrate in the food chain (Poland and Knutson, 1982). HAHs induce a similar battery
of biochemical and toxic responses in animals which vary primarily in potency.
Figure 1.1. Structure of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD)
TCDD, the most extensively studied HAH, is highly toxic (Poland and Knutson,
1982) and its persistence in the environment renders this compound a potential health
hazard. Except for its use as a prototypic ligand in scientific studies, TCDD has no known
industrial or commercial use and is not intentionally manufactured by any industry. It is
inadvertently produced in the industrial manufacturing of certain pesticides the most
renowned being trichlorophenoxy acetic acid (2,4,5 TCP) or Agent Orange, the defoliant
used in Vietnam. It is also generated in low levels during the incineration of industrial
and municipal wastes and as a byproduct of the chlorine bleaching process. At this time,
there is some controversy over health risks associated with human exposure (Birnbaum
1994; Johnson 1993; Vanden Heuvel and Lucier, 1993). The best documented adverse
2
1994; Johnson 1993; Vanden Heuvel and Lucier, 1993). The best documented adverse
response to high dose exposure to TCDD is chloracne, a disfiguring skin condition
characterized by alterations in epithelial cell growth and differentiation (Gaido, et al.,
1991). A variety of different cancers including soft-tissue sarcoma (Fingerhut et al.,
1991) and an increase in the overall cancer death rate (Manz, 1991) have been reported in
chemical workers exposed to TCDD. Studies of U.S. veterans exposed to TCDDcontaminated Agent Orange found that these men also faced an increased risk of
developing a variety of different cancers and of fathering a child with birth defects (Houk,
1991). In studies evaluating the immunotoxic effects of TCDD on humans, there is a lack
of consistent, significant exposure-related effects (Kerkvliet and Burlson, 1994). This is
likely due to a number of factors including difficulties in assessing subclinical immune
modulation in an outbred (human) population, the lack of studies on individuals with
known documented exposure and an inappropriateness of the assays used to assess
immune function (Kerkvliet and Burlson, 1994). The ubiquitous occurrence of TCDD in
the environment also complicates the comparison between exposed and supposedly
unexposed populations (Vanden Heuvel and Lucier, 1993). Consequently, the subtle
effects of chronic, low dose exposure that might result from ingestion of contaminated
fish or vegetables or in nursing infants (Schecter et al., 1994) are difficult to detect and
have not been well documented. This is in contrast to the well characterized toxic effects
that are observed in laboratory animals following exposure to TCDD under controlled,
experimental conditions.
General Toxicity:
In laboratory animals, the toxic responses to TCDD exposure vary greatly. For
example, there is a marked difference in the LD50 among species. While guinea pigs are
extremely sensitive with an LD50 of 1 ug/kg body weight, hamsters are relatively resistant
with an LDS() five thousand times greater (Poland and Knutson, 1982). In addition to
variation in susceptibility among species, lethality due to TCDD exposure is intriguing
for two reasons. First, the time from exposure to death is quite long; (2-3 weeks in mice
3
and up to six weeks in monkeys (Theobald et al 1983)), and independent of dose
(Birnbaum, 1994). Second, the cause of death is enigmatic. Except in the rabbit where
extensive liver necrosis develops and in monkeys that succumb to profound
pancytopenia, it is difficult to identify what organ system failure is responsible for death
(Poland and Knutson, 1982). In response to TCDD exposure, animals become cachetic,
lipid and carbohydrate metabolism are altered (Lentnek, et al., 1991)(Sparrow et al.,
1994), and a profound wasting disease develops, often involving the loss of as much as
one third to one half of the total body weight (Birnbaum, 1994). Clinically, multisystem
effects are seen that resemble the effects of starvation, although cachexia and starvation
alone cannot account for the lethal effects of TCDD exposure. (Theobald, 1983)
Pathologic responses to TCDD can be grouped into three general classes:
1) altered metabolism resulting from changes in enzyme levels; 2) altered homeostasis
resulting from changes in hormones and their receptors; and 3) altered growth and
differentiation resulting from changes in growth factors and their receptors (Birnbaum,
1994) and include tissue specific hyper- and hypo-plasia, teratogenicity, hepatotoxicity,
skin lesions, altered carbohydrate metabolism, altered hormone and hormone receptor
levels and carcinogenesis (James et al., 1993; Lucier et al., 1993; Dickson and Buzik,
1993; and Safe 1990). Not all effects occur in all species and many are tissue- and
developmental-stage specific. Within a species, adverse effects vary with the strain, sex
and age of the animal. The large quantitative differences in species sensitivity and the
large qualitative differences in tissue specificity cannot be explained by a difference in
metabolism or clearance of the TCDD (Poland and Knutson, 1982; Hankinson, 1995).
However, but variation in the degree of susceptibility and response to TCDD may result
in part from differences in distribution and/or affinity of the aryl hydrocarbon receptor
complex (AhRC) discussed below.
Mechanism of Action:
The biochemical and toxic effects of TCDD appear to be mediated via binding to
an intracellular receptor, the aryl hydrocarbon or Ah receptor (Whitlock, 1993, Van den
4
Heuvel; Lucier 1993, Kerkvliet, N.I. and Burlson, G.R. 1994.) This ligand/receptor
interaction is analogous to the mechanism of action of steroid hormones although the
receptor protein itself differs in structure and is not a member of the steroid-thyroid­
retinoic acid receptor superfamily of proteins (Hankinson, 1995). (Figure 2) In its
unbound form, the cytoplasmic receptor is complexed to at least two heat shock proteins
(HSP) and possibly another 46 kDa protein (Hankinson, 1995). TCDD, lipophilic in
nature, readily passes through the cellular membrane and binds with high affinity to the
cytoplasmic Ah receptor (Kd=10-12M) (Lai et al., 1996). Once the ligand binds, the heat
shock proteins dissociate and the ligand-receptor complex binds to another protein called
ART, an acronym for Ah receptor translocating protein. ART was originally thought to
be cytoplasmic but more recent studies leave the cellular location of ART unresolved
(Hankinson, 1995). The exact function of this protein is also in question. In spite of its
name, ART does not appear to be directly involved in translocating the AhRC to the
nucleus, as ART-deficient mutants are proficient in this translocation process (Pollenz, et
al 1994). The ART protein does function to stabilize the receptor complex and facilitates
the binding of this complex to discrete DNA sequences, so called dioxin response
elements (DREs) in the promoter regions of specific genes (Lai, et al., 1996). The
activated AhRC acts as a ligand-activated transcription factor inducing transcription of
specific genes and an increase in the synthesis of the corresponding mRNA. It is
hypothesized that alterations in the expression of specific gene products mediates the
biochemical and toxic effects of TCDD exposure.
TCDD has been shown to modulate the expression of a large array of genes in
different tissues and cells lines. The best characterized among these is the induction of the
CYP1A 1 family of mixed function oxidases (Nebert et al., 1993; Hankinson, 1995).
Other gene products regulated by transcriptional activation by the AhRC include other
enzymes of xenobiotic metabolism (Phase 1; CYP1A2 and CYP1B1, and Phase 11;
NADP(H):oxidoreductase, aldehyde dehydrogenase (ALDH) (Nebert et al., 1993),
proteins involved in the processes of cell growth and activation (plasminogen activator
inhibitor (PAI-2), transforming growth factors a and 132 (TGFa, TG932) (Gaido and
5
Maness, 1994; Gaido et al., 1992), c-fos, Jun-B, c-jun and Jun-D (Puga, et al., 1992)),
and aminolevulinic acid synthase (ALAS) (involved in porphyrin biosynthesis and
essential for oxygen and electron carrying proteins) (Hankinson, 1995).
A number of other proteins or mRNAs have been shown to be modulated by
TCDD exposure in particular tissues or cells although it has not yet been confirmed that
these alterations are direct effects of TCDD or that they are AhR dependent (Hankinson,
1995; Lai et al., 1996). TCDD-dependent alterations in mRNA and/or proteins involved
in inflammatory processes are of particular interest in these studies and include
interleukin-1 p (IL-113), (Sutter, et al., 1991; Yin, et al., 1994; Vogel and Abel 1995; Lai
et al., 1996) tumor necrosis factor a (TNFa) (Vogel and Abel, 1995; Lai et al., 1996) and
prostaglandin G/H synthase (responsible for the synthesis of prostaglandin from
arachidonic acid) (Olnes et al, 1994).
Figure 1.2. The Ah Receptor Model
6
Immunotoxicity of TCDD:
The immune system appears to be one of the most sensitive targets for the toxicity
of TCDD. Although best characterized in the mouse, the immunosuppressive effects of
HAH have been described in numerous species including rodents, guinea pigs, rabbits,
monkeys, marmosets, cattle and chickens (Kerkvliet and Burleson, 1994; Poland and
Knutson, 1982). The profile of immunotoxicity is complex and suggests that a number of
different cell types and immunologic processes may be targeted by TCDD and contribute
to the observed immunosuppression following exposure (Vos and Luster, 1989;
Holsapple, 1991; Holsapple et al., 1991; Kerkvliet and Burleson, 1994; Kerkvliet, 1995).
Involution of the thymus gland in response to TCDD exposure is considered a
hallmark of TCDD toxicity in many animal species (Poland and Knutson, 1982;
Holsapple, 1991). Exposure to relatively low doses results in a dramatic reduction in
size and weight of the thymus characterized histologically by a loss of cortical
lymphocytes (Poland and Knutson, 1982). Because the thymus is a central organ for T
cell maturation, initial immunotoxic studies focused on the effects of TCDD on T cell-
mediated immunity. In vivo exposure to TCDD results in suppression of delayed type
hypersensitivity (DTH) responses, graft-vs-host responses, allospecific cytotoxic T
lymphocyte (CTL) activity, and host defense responses to viral challenge (Reviewed by
Vos and Luster, 1989;Vos et al., 1991; Hindsill et al., 1980; Holsapple et al., 1991).
Exposure to TCDD also produces a profound suppression of humoral immune
responses in different species (Vos and Luster, 1989; Holsapple, 1991; Kerkvliet and
Burleson, 1994). One of the most sensitive indicators of TCDD immunotoxicity in the
mouse is suppression of the macrophage and T cell-dependent antibody response to sheep
red blood cells (SRBC) with an acute single dose ED50 of approximately 0.7 ug/kg
(Vecchi et al., 1980; Davis and Safe, 1988; Kerkvliet and Brauner, 1990). The targeted
cell(s) and the specific mechanisms underlying TCDD-induced suppression of the
antibody response are poorly understood. The anti-SRBC response depends on the
concerted interactions of antigen presenting cells (APC), regulatory T cells and B cells. In
vivo studies designed to evaluate target cell sensitivity to TCDD demonstrated an
7
increased sensitivity of antibody responses to T cell-dependent compared to T cellindependent antigens suggesting that TCDD may target regulatory T cells and/or APC
(Kerkvliet et al., 1990). In contrast, ex vivo studies suggest that B cells from TCDD-
exposed mice are functionally compromised in in vitro antibody production while T cells
and APC are not (Dooley and Holsapple, 1988; Dooley et al., 1990). The basis for the
different responses to TCDD in vivo versus ex vivo and in vitro has not been established.
A number of studies have examined the effects of TCDD exposure on innate
immunity. Characterized by non-antigen-specific responses to immune challenge, innate
immunity involves the interaction of a number of different effector cells including
neutrophils, macrophages, eosinophils and natural killer cells as well as proteins of the
complement system. Although TCDD exposure can decrease complement activity and
serum C3 levels (White et al., 1986; Lin et al., 1991) and cause an inhibition of phorbol
ester-activated tumor cell lysis by neutrophils (Ackerman et al., 1989), the innate immune
responses appear overall to be relatively resistant to the suppressive effects of TCDD
(Kerkvliet, 1995). Natural killer cell activity, macrophage-mediated phagocytosis and
tumor cell lysis, (House et al., 1990; Mantovani et al., 1980), and the oxidative reactions
and degranulation capabilities of neutrophils (Ackerman et al., 1989) are not altered by
TCDD. TCDD exposure may activate innate immune responses as pathologies associated
with TCDD exposure often involve an inflammatory reaction characterized by an
accumulation of neutrophils and activated macrophages (Puhvel and Sakamoto, 1988).
There is increasing experimental evidence to suggest that TCDD exposure may actually
enhance inflammatory responses (Kerkvliet and Oughton, 1993; Theobald et al., 1983).
The Acute Inflammatory Process:
Pathophysiology: The acute inflammatory process involves a well orchestrated
series of responses initiated by an irritation or injury and resulting in a local increase in
blood flow and permeability of the vasculature. Plasma and inflammatory cells travel
across the vascular wall and accumulate in the perivascular space. The end result of this
process is production of the classical signs rubor (redness), tumor (swelling), dolor
8
(pain), and calor (heat), and functio laesa (loss of function) that characterize acute
inflammation.
The events of acute inflammation are initiated and maintained by a variety of
chemical mediators. Potent proinflammatory cytokines, IL-1 and TNF produced locally
in response to an inflammatory insult stimulate endothelial cells to produce a cascade of
soluble mediators including platelet activating factor (PAF), arachidonic acid (AA)
metabolites, nitric oxide (NO) and interleukin-8 (IL-8), and to upregulate the expression
of adhesion molecules on the endothelial cell surface (Fig. 3) (Dinarello et al., 1993).
Arterioles, capillaries and venules dilate in response to histamine produced from mast
cells, PAF, AA and NO and an increase in blood flow and permeability result in the
exudation of fluids and plasma proteins into the perivascular space. IL-8, a potent
neutrophil chemotractant recruits circulating neutrophils and stimulates adherence of
these cells to the endothelial cell surface (Dinarello, 1993; Van Zee et al., 1991; Rot,
1992). By a process of diapedesis, neutrophils migrate into the perivascular space where
they phagocytize and digest microbial agents and necrotic tissue. Monocytes are
subsequently recruited by a similar process from the circulation to the site of
inflammation (Stein and Keshav, 1992) and upon entering the tissues, are transformed
into macrophages. Initially the macrophages participate jointly with neutrophils to rid the
body of the injurious substance. If the inflammatory stimulus persists, macrophages will
become the dominant inflammatory cell, lymphocytes will be recruited to the site of
injury, and the character of the response will shift from an acute to a chronic
inflammatory response.
IL-
IL-1
TF
TNF
PAF
PGE
NO
1L-8
olimaikAwlim-...4alkiammoilidti rr 41110 411110
Vascular Smooth Muscle
Extravpscular
Space
CD Endothelial Cell
Endothelial Cell
PAF
platelet activating factor
expressing Adhesion
Molecules
0 Neutrophil
POE
prostaglandin E
NO
nitric oxide
Figure 1.3. Acute Inflammatory Response: Endothelial Cell Activation (from Dinarello,
1993).
Proinflammatory Mediators:
Cytokines are potent polypeptides that act in an autocrine, paracrine or
occasionally in an endocrine fashion, via specific cell surface receptors to regulate cell
function. Cytokines participate in the regulation of the immune response, in the
processes of inflammation and wound healing, and are involved in normal homeostatic
processes. Produced by a wide variety of cell types in response to infection, injury or
inflammation, cytokines are highly conserved across species boundaries (Stein and
Keshav, 1992). They are extremely potent, often active at femtomolar concentrations
(Dinarello, 1993) and they are pleiotropic in nature a single cytokine may have multiple
tissue targets and result in a broad array of physiologic effects. A further feature that
characterizes cytokines is their redundancy, that is different cytokines often share the
same broad spectrum of activities. Redundancy is particularly characteristic of the
proinflammatory cytokines IL-1 and TNF. These inflammatory mediators are critical
9
10
components of normal host defenses and serve as major host-derived inducers of
important inflammatory and immunoregulatory processes. While cytokine activity is
generally considered beneficial to the host, dysregulation of these potent mediators can
lead to deleterious effects (Dinarello, 1991). The predominant manifestations of certain
disease states including cachexia and endotoxic shock, for example, are directly
attributable to a deranged cascade of cytokine effects (Tracey and Cerami, 1993).
IL-1: The IL-1 family consists of three structurally related peptides, IL -la, IL-113,
and IL-lra. IL-1 a and IL-1I3 are separate gene products produced by the same cells in
response to identical stimuli. Evidence suggests that IL-la remains membrane associated
while IL-1 p is secreted into the extracellular fluid (Dinarello, 1988). Membrane bound
IL-la facilitates the ability of IL-1 to participate in autocrine and paracrine events
without inducing the systemic effects that occur when IL-1 gains access to the circulation.
Although IL-la and IL-1f3 share only 25% homology at the amino acid level, they share
the same receptors and mediate the same spectrum of biological activities (Dinarello,
1992) including inflammatory, metabolic, immunologic and hematopoietic processes
(Fenton, 1992).
The biological effects of IL-1 can be divided into local (paracrine or autocrine)
and systemic (endocrine) effects. First identified in the 1940's as an "endogenous
pyrogen", systemic IL-1 includes fever, neutrophilia, anorexia, hypotension and shock
(Dinarello, 1992). The local effects of IL-1 include neutrophil migration, an increase in
production of prostaglandin, activation of B and T lymphocytes, induction of acute phase
proteins from hepatocytes, fibroblast proliferation, and differentiation and proliferation of
bone marrow cells (Dinarello and Wolff, 1993).
The third member of the IL-1 family, IL-1 receptor antagonist (IL -IRA) is a
specific inhibitor of IL-1 activity that acts by blocking the binding of IL-1 to its cell-
surface receptors. Structurally related to IL-la and IL-1I3, IL -IRA binds both type 1 and
type 11 IL-1 receptors with high affinity and exhibits no agonist activity. Initially purified
from the urine of patients with fever or monocytic leukemia (Arend, 1991), IL-1RA can
11
be measured in the circulation following experimental inflammation and clinical disease
(Fisher et al., 1992). The synthesis of IL -IRA is a natural part of the resolution or
containment of the inflammatory process and inhibition of IL-1 activity helps to maintain
a balance between the beneficial and deleterious effects of this potent cytokine. A large
number of studies have demonstrated the ability of recombinant IL-1RA to block IL-1
activity both in vitro and in vivo (Dinarello and Thompson, 1991), and IL -IRA is
currently in clinical trials for treatment of IL-1 mediated diseases.
TNF: Initially characterized by its ability to promote tumor cell lysis, TNF is a
multifunctional cytokine capable of influencing the growth, differentiation and function
of a broad range of cells (Sherry and Cerami, 1988, Vassalli, 1992). TNFa is produced by
macrophages (MAC) (Beutler et al., 1985) as well as by other activated cells including T
cells, B cells, NK cells, mast cells (which are unique in that they contain TNF in stored
granules), PMN, keratinocytes, astrocytes and microglial cells (Vasselli, 1992). Like IL­
1, TNF mediates a broad range of biological responses, exerts both systemic and local
effects and, although an essential element of normal host defense, excessive or
overproduction of TNF can be detrimental to the host. (Van Zee et al., 1992).
Systemically, TNF is a critical mediator of endotoxic shock, induces fever mediated
through an increase in prostaglandin biosynthesis in the hypothalamus, and causes the
cachexia of chronic disease characterized by protein catabolism, organ failure and
suppressed immunologic function (Tracey and Cerami, 1993). On a local level, TNF
plays an integral role in immune and inflammatory responses, and affects multiple
different cells. Endothelial cells, considered a primary target of TNF, respond to
exposure with an increased production of inflammatory mediators, upregulation of
adhesion molecules, and promotion of procoagulant activity. Monocytes and
macrophages are both a main source and a primary target of TNF, exposure results in
activation and differentiation and potentiates further TNF release. TNF enhances
degranulation, phagocytosis and the generation of superoxide radicals in neutrophils and
promotes neutrophil adhesion to endothelial cells. TNF promotes the growth and
12
differentiation of activated T and B cells, stimulates production of numerous cytokines
and inhibits collagen synthesis in fibroblasts and increases differentiation and cytokine
production in keratinocytes (reviewed by Vassealli, 1992; Tracey and Cerami, 1993;
Beuler and Cerami, 1989).
Naturally occurring inhibitors of TNF activity have been identified in human
urine and serum and in cell-culture systems (Van Zee et al., 1992). The inhibitors are the
extracellular domains of the TNF receptors proteolytically cleaved from the cell surface
in response to many of the same inflammatory stimuli that induce TNF production. It is
unclear at this time whether circulating soluble receptors function to inhibit TNF activity
by binding TNF and making it unavailable for receptor binding and signal transduction or
if they function to increase the halflife of circulating TNF by acting as a slow release
reservoir (Mohler et al., 1993). In either case, the appearance of extracellular soluble
receptors provides a regulatory mechanism to modulate the potentially harmful effects of
excessive TNF activity that might arise in response to severe injury or infection (Van
Zee, et al.; 1992, Lantz). Recombinant TNF soluble receptors dimerized and fused to the
Fc portion of IgG immunoglobulin have been used effectively to inhibit TNF activity in
many model systems (Lesslauer, 1991;Wooley, et al., 1993; Mohler, et al., 1993).
NO: Nitric Oxide (NO), biologically active compound involved in acute and
chronic inflammatory process plays a critical role in cell signaling and has been
implicated in the pathophysiology of a number of diseases (Moncada and Higgs, 1993).
NO is synthesized from L-arginine by a family of enzymes, the nitric oxide synthases.
The constitutive isoform of NO synthase (NOS) is Ca' dependent and produces small
amounts of NO which mediate endothelium-dependent relaxation and neural transmission
(Corbett et al., 1992; Moncada and Higgs, 1993). Larger amounts of NO are produced by
the cytokine-inducible form of NO synthase which is Ca' -independent (Corbett et al.,
1992; Moncada and Higgs, 1993). The NO produced by the inducible enzyme plays a
key role in nonspecific defense mechanisms against pathogens (Salvemini et al., 1996)
13
and in the vascular dilitation characteristic ct acute inflammation (Moncada and Higgs,
1993).
The Effects of TCDD on Acute Inflammation:
Many of the toxic syndromes associated with TCDD exposure involve a local
accumulation of inflammatory cells (Chapman, 1985; Puhvel and Sakamoto, 1988).
Theobold et al. (1983) were the first to identify and characterize a TCDD-induced
proinflammatory response. These investigators observed enhanced paw edema formation
in response to subplantar injections of carrageenan or dextran in rats exposed to TCDD.
In these studies, the TCDD effect was limited to the acute phase of the inflammatory
response and was not due to an increase in the vasoactive amines, histamine or serotonin..
The results led these investigators to speculate that TCDD targets the vascular
endothelium by altering production, release or degradation of other proinflammatory
mediator(s) involved in edema formation, or by increasing the responsiveness of the
vascular endothelium to those mediators.
Kerkvliet and Oughton (1993) observed that C57B1/6 mice exposed to TCDD
generated an enhanced inflammatory response following an intraperitoneal (ip) injection
of SRBC. This response was characterized by an increase in neutrophils (PMN) and
MAC harvested from the peritoneum at various times following antigen exposure. Since
TCDD administered orally did not by itself initiate an inflammatory reaction, exposure to
TCDD appears to exert some effect that results in an enhancement of the response to an
inflammatory stimulus. One mechanism by which TCDD could augment the peritoneal
inflammatory response is through enhanced production of inflammatory mediators.
Because of the similarities between the pathophysiologic effects of the
inflammatory mediators and the adverse effects of TCDD exposure, the role of these
mediators in TCDD toxicities has been investigated. A relationship between IL-1 and
TCDD was first identified by Sutter et al (1991). In the skin, epidermal keratinocytes are
the primary producer of IL-1. Normally produced in low levels, IL-1 production can
increase dramatically in response to stimulation or injury and recent studies have
14
identified a role for IL-1 in skin injury and disease processes involving altered regulation
and differentiation of epithelial cells (Yin et al., 1994). Increased levels of IL-1 p mRNA
were identified in a human keratinocyte cell line exposed to TCDD, suggesting that IL-1I3
may be transcriptionally regulated by TCDD (Yin et al., 1994).
Reports from several different laboratories suggest that an increase in TNF
activity may be associated with the toxic effects of TCDD. Clark et al. (1991)
demonstrated a hypersensitivity to endotoxin in mice exposed to TCDD and a
corresponding dose-dependent increase in serum TNF levels. Studies by Taylor et al.
(1992) also suggest that TNF is a mediator of TCDD toxicity. Administration of antiTNF antibodies inhibited the weight loss, elevations in serum chemistry values and
mortality associated with acute TCDD toxicity. Alsharif et al. (1994) identified TNF as
playing a critical role in amplifying the oxidative stress-induced tissue injury observed in
TCDD-exposed mice. Increased levels of TNF were measured in LPS-stimulated PEC
harvested from mice exposed to ip doses of TCDD (Massa, 1992) and from HIV infected
promonocytic Ul cells (Gollapudi et al., 1996).
At this time there have been no reports describing an effect of TCDD on NO
production. A single reference to the production of reactive nitrogen intermediates
formed in response to TCDD was cited by Alsharif (1994). Several lines of evidence,
however, suggest that NO may contribute to toxicities induced by TCDD. For example,
NO plays a critical role in the acute inflammatory response (Moncada and Higgs, 1993;
Dinarello et al., 1993; Salvemini et al., 1996), and has been shown to mediate suppression
of the primary antibody response to SRBC in mice (Al-Ramadi et al., 1992; Eisenstein et
al., 1994).
Objectives
The overall objectives of the following studies were twofold; first, to better
understand the pathophysiologic mechanisms involved in the TCDD-induced
hyperinflammatory response to SRBC, and second, to address the question of whether the
15
TCDD-induced hyperinflammatory response to SRBC is linked mechanistically to the
TCDD-induced suppression of the anti-SRBC antibody response.
Chapter Two describes studies designed to test the hypothesis that TCDD
exposure increases activity of the proinflammatory cytokines, IL-1 and/or TNF resulting
in an enhanced inflammatory response to ip SRBC. To test this hypothesis, we first
examined the ability of exogenous IL-1 and TNF to mimic the effects of TCDD on
peritoneal inflammation. Second, to determine the contribution of these cytokines to the
TCDD-induced enhanced inflammatory response, we specifically blocked IL-1 and TNF
activity using an IL-1 receptor antagonist and a TNF soluble binding protein and
evaluated the peritoneal inflammatory response in TCDD-exposed and control mice. In
addition, plasma TNF levels were measured to determine whether TCDD exposure can
increase production of this cytokine in response to ip SRBC.
Studies in Chapter Three were designed to test the hypothesis that TCDD targets
the peritoneal exudate cell and increases production of TNF in response to an appropriate
inflammatory stimulus. The effects of TCDD on TNF production by both an LPSstimulated macrophage cell line and ex vivo peritoneal exudate cells were evaluated. In
addition, immunocytochemistry and flow cytometric analysis were used to characterize
intracellular production and cellular processing of TNF in these cells.
In Chapter Four we tested the hypothesis that the TCDD-induced
hyperinflammatory response to SRBC and the TCDD-induced suppression in the antiSRBC primary antibody response are linked mechanistically through an increase in TNF
activity. To determine whether altered levels of TNF are capable of affecting the primary
antibody response, we evaluated the effects of TNF on the splenic plaque-forming cell
response to SRBC. To determine the contribution of elevated TNF levels to TCDDinduced antibody suppression, we blocked TNF activity using a soluble TNF binding
protein during the course of antibody production. The effect of TNF inhibition on the
antibody response to SRBC was measured in control and TCDD-exposed mice.
The involvement of NO in TCDD-induced immunotoxicities was evaluated in
Chapter Five. These studies were designed to test the hypothesis that in response to
16
TCDD exposure and an appropriate inflammatory stimulus, more NO is produced locally
contributing to both an enhanced inflammatory response to SRBC and a downstream
suppression in the primary antibody response. To test this hypothesis, we first examined
the effects of TCDD exposure on NO production by activated peritoneal cells. The
involvement of NO in TCDD-induced hyperinflammation and TCDD-induced antibody
suppression was then evaluated by measuring the SRBC-induced peritoneal inflammatory
response and SRBC antibody production in mice following treatment with
aminoguanidine, an inhibitor of NO production.
17
Chapter Two
Acute Inflammatory Response to Sheep Red Blood Cells in Mice
Treated with 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD):
The Role of Proinflammatory Cytokines, IL-1 and TNF
AUTHORS:
A. B. Moos
L. Baecher-Steppan
N. I. Kerkvliet
Reprinted from Toxicology and Applied Pharmacology Vol. 127
18
Abstract
Recent studies have demonstrated that TCDD exposure of C57BI/6 mice results in
an enhanced inflammatory response to intraperitoneal injection of sheep red blood cells
(SRBC). This response is characterized by an increase in total peritoneal cells (PEC) as
well as an increase in relative and absolute numbers of neutrophils (PMN) harvested 16 to
40 hours following injection of SRBC. The mechanisms whereby TCDD increases
cellular influx are unknown. In the present studies, the role of the proinflammatory
cytokines interleukin 1 (IL-1) and tumor necrosis factor (TNF) in TCDD-induced
hyperinflammation was examined. Intraperitoneal administration of recombinant IL -1(3
(0.4 U) or TNFa (10 ng) resulted in an enhanced peritoneal inflammatory response
compared to PBS injected control animals measured 20 hours following injection of
SRBC. The effect of exogenous cytokines mimicked the effects of exposure to 5 ug/kg
TCDD. When endogenous IL-1 activity was blocked using an IL-1 receptor antagonist
(IL-lra, 1 mg every 3 hrs.), the PMN influx was significantly decreased in control
animals but not in animals exposed to 20 ug/kg TCDD. When endogenous TNF activity
was blocked using a TNF soluble receptor (rhuTNFR:Fc 100 ug) the numbers of total
PEC and macrophages (MAC) harvested from control mice was reduced while in mice
exposed to 20 ug/kg TCDD, inhibition of TNF activity dramatically reduced the numbers
of PEC, MAC, and PMN. Following rhTNFR:Fc treatment, there was no difference
between TCDD treated and control mice in inflammatory cell influx. These results
demonstrate that TNF plays a major role in mediating TCDD induced
hyperinflammation. In support of this conclusion, a dose dependent increase in plasma
TNFa was measured by ELISA in TCDD treated mice following SRBC injection.
Introduction
2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) represents the prototype of a large
group of toxic halogenated aromatic hydrocarbons that are widespread environmental
contaminants. The immunotoxic properties of TCDD are well documented in several
animal species (Holsapple et al., 1991). One of the most sensitive indicators of TCDD
19
immunotoxicity is a suppression of the macrophage and T-cell dependent antibody
response to sheep red blood cells (SRBC) (Vecchi et al., 1980; Davis and Safe, 1988;
Kerkvliet and Brauner, 1990).
We recently reported that TCDD exposure in mice results in an enhanced
inflammatory response to intraperitoneal (ip) injection of SRBC (Kerkvliet and Oughton,
1993). This effect was characterized by increases in total peritoneal cell (PEC) numbers
as well as absolute and relative numbers of neutrophils (PMN) harvested from the
peritoneal cavity 16 to 40 hours following injection of SRBC. The mechanisms whereby
TCDD increases cellular influx following SRBC injection are not known.
IL-1 and TNF represent integral components of normal host defense and serve as
major host derived inducers of important immunoregulatory factors. Both recombinant
IL-1 and TNF induce neutrophil infiltration into the peritoneal cavity in mice (Sayers et
al., 1988). Dysregulation or enhancement in activity of these cytokines may lead to a
proinflammatory condition and disruption in normal immune function. Recent reports
have demonstrated that both of these inflammatory mediators may be involved in
responses to TCDD exposure. Sutter et al. (1991) reported increased levels of IL -1(3
mRNA in keratinocytes exposed in vitro to TCDD, suggesting that the IL-lp gene may
be transcriptionally regulated by TCDD. Significantly elevated levels of TNF have been
measured in the serum of TCDD exposed mice following endotoxin treatment (Clark et
al., 1991b). Pretreatment with TNF antibodies reduced TCDD-induced endotoxin
hypersensitivity (Clark et al., 1991a) and acute toxicity resulting from TCDD exposure
(Taylor et al., 1992).
To examine the role that IL-1 and TNF play in TCDD-induced hyperinflammation, we first examined the ability of exogenous cytokines to mimic the effects
of TCDD on peritoneal inflammation. Secondly, we used an IL-1 receptor antagonist
(IL-lra) and a TNF soluble binding protein (rhuTNFR:Fc) to specifically block IL-1 and
TNF activity during the inflammatory response (Dinarello et al., 1993). In addition,
plasma TNFoc levels were measured to determine whether TCDD exposure increases
circulating levels of this cytokine following antigen sensitization.
20
Methods and Materials
Female C57BI/6 mice (Jackson Laboratories, Bar Harbor ME) were maintained in
a specific virus free colony, housed 4-6 per cage in front of a laminar flow unit and
provided with food (Wayne Rodent Blox) and water ad libitum. Mice were acclimated
for a minimum of 10 days and were used at 7-8 weeks of age.
TCDD obtained from Cambridge Isotope Laboratories, Inc. (Woburn, MA) as a
certified reference standard of >98% purity was dissolved in anisole and diluted in peanut
oil. A vehicle solution of anisole in peanut oil was prepared similarly. Mice were given
a single dose (0.2 ml) of TCDD or vehicle by gavage 2 days prior to SRBC
sensitization.
A single lot of SRBC was purchased from Colorado Serum Co. (Denver, CO).
Mice were sensitized with a single intraperitoneal injection of 2.5 X 108 SRBC 2 days
after TCDD exposure.
Animals were killed by CO2 asphyxiation 18-20 hours following injection with
SRBC. Peritoneal cells were harvested by lavage with 6 mls of RPMI-1640
supplemented with 1% FCS, 50 ug/ml Gentamicin, 20mM Hepes and 5 U/ml Sodium
heparin. The abdomen was massaged and 4 mis were withdrawn as described by Coligan
et al. (1992). Total peritoneal cells were enumerated on a Coulter Counter and
differential cell counts were determined following cytocentrifugation and staining with
Gugol blue. Total numbers of macrophages (MAC) and PMN were calculated by
multiplying the total PEC by the percent MAC or PMN determined from differential cell
counts.
To test the effects of exogenous IL-1 and TNF on the peritoneal inflammatory
response to SRBC, 0.4U of murine recombinant IL-113 (Genzyme, Cambridge, MA) or
10 ng of murine recombinant TNFa (Genzyme, Cambridge, MA) were administered ip
30 minutes before and 6 hours following SRBC injection.
In separate studies, specific cytokine inhibitors were used to block the activity of
IL-1 or TNF. To inhibit IL-1 activity 1 mg of a recombinant human IL-1 receptor
antagonist (I L-lra, generously provided by Dr. James L. Vannice, Synergen, Boulder,
21
CO) was injected sc 30 minutes before and at 3 hour intervals following SRBC injection.
Due to the spare receptor phenomenon whereby only a small percent of IL-1 receptors
need to be occupied to trigger a biological response, a high dose of IL-lra is required to
inhibit IL-1 activity (Dinarello and Thompson, 1991; McIntyre et al., 1991). Frequent
injections are necessary because the half life of this reagent is very short in mice
(personal communication, Dr. James L. Vannice). To inhibit TNF activity, 100 ug of a
recombinant human soluble TNF receptor: Fc fusion protein (rhuTNFR:Fc) was injected
iv 30 minutes before SRBC injection (the fusion protein and dosing regime was
generously provided by Dr. M. B. Widmer, Immunex, Seattle, WA)
.
To measure TNFcc levels in plasma, mice exposed to increasing doses of TCDD
were killed by CO, asphyxiation 90 minutes following ip injection of SRBC. Blood was
collected by cardiac puncture and kept at 4 degrees until the plasma was harvested. In all
cases, plasma was separated from cells within 40 minutes (Exley and Cohen, 1990).
Plasma was kept at -70 degrees until assayed. All samples were collected on the same day
and assayed together. TNFa levels in plasma harvested from vehicle and TCDD exposed
mice were measured and compared using a murine TNFa Elisa kit (Genzyme, Cambridge
MA)
The Student's t test was used to analyze data for statistical significance. In all
analyses, p<0.05 was considered statistically significant. The results in this paper are
representative of data that were validated in at least two independent studies.
Results and Discussion
As shown in Fig. 2.1, TCDD enhanced the peritoneal inflammatory response to ip
injection of SRBC in a dose dependent manner. In agreement with previous studies
(Kerkvliet and Oughton, 1993), this effect was characterized by an increase in total
peritoneal exudate cells (panel A) as well as an increase in the relative (panel B) and
absolute (panel A) numbers of neutrophils harvested 18-20 hours following antigen
challenge.
22
SHORT COMMUNICATION
90
B
80
D
70
X
60
**
50
40
30
20
10
VEHICLE
5 UG/KG
20 UG/KG
0
VEHICLE
5 UG/KG
20 uc/KG
Fig. 2.1. The effect of increasing doses of TCDD on the total number of peritoneal
exudate cells (PEC) and the number (Panel A) and percent of macrophages (MAC) and
neutrophils (PMN) (Panel B) harvested from the peritoneal cavity of mice following
injection of SRBC. Data are presented as means ± SE of 6-8 mice per group.
* p<0.05 5 ug TCDD/kg versus Vehicle
** p<0.05 20 ug TCDD/kg versus 5 ug TCDD/kg
To determine if IL-1 or TNF were capable of promoting neutrophil influx in
response to ip injection of SRBC, animals were treated with recombinant murine IL-113 or
TNFa. Exogenous cytokines were administered ip 30 minutes before SRBC injection to
mimic the hypothesized increase in proinflammatory cytokine activity resulting from
TCDD exposure and 6 hours following SRBC injection to prolong cytokine activity
throughout the experimental period (Sayers et al., 1988). Peritoneal cells were harvested
18-20 hours later, counted and characterized (Table 2.1). Results indicate that both
exogenous I
p and TNFa enhanced the inflammatory response to SRBC in a manner
analogous to TCDD exposure.
23
Table 2.1: Comparison between the effect of TCDD and exogenous cytokines on total
peritoneal cell (PEC) and neutrophil (PMN) accumulation following sheep red blood cell
inj ectiona
Treatment
PEC
PMN
X 10`
Vehicle
& PBS
33.0 ± 4.2
X106
22.2 ± 1.6
7.3 + 1.1
5ug/kg TCDD
& PBS
47.5 + 8.4
36.4 + 3.3*
16.4 ± 2.2*
Vehicle
& IL-1p
45.7 ± 9.5
26.9 + 2.1
11.6± 1.6*
Vehicle
& TNFa
55.4 ± 9.7*
29.5 ± 2.1*
16.3 + 2.9*
a C57B1/6 mice were injected with SRBC 2 days following oral exposure to 5ug/kg TCDD or vehicle.
Recombinant IL-113 (0.4U), TNFa (l Ong) or PBS was injected intraperitoneally 30 minutes before and 6
hours following antigen stimulation. Data are presented as means + SE of six mice per group.
*p<0.05 compared to vehicle & PBS
Having demonstrated that increased levels of IL-1 and TNF could mimic TCDD
effects on inflammation, we asked whether increased cytokine activity was responsible
for the observed TCDD effects. To address this question, specific cytokine inhibitors
were used, and their effect on peritoneal inflammation following injection of SRBC was
measured. We first tested specific blockade of cytokine activity rather than measuring
cytokine protein levels for two reasons. First, the presence of naturally occurring
inhibitors receptor antagonists for IL-1 and soluble receptors for TNF makes
interpretation of cytokine levels difficult (Dinarello, 1993). Second, TCDD induced
changes in cytokine half-life, cytokine receptor number or affinity, or cytokine
endogenous inhibitors would be reflected in alterations in cytokine activity but not
necessarily in altered protein levels. As shown in Fig. 2.2 (panel A), IL-lra significantly
inhibited neutrophil influx in vehicle treated animals without affecting the total cell
24
number harvested from the peritoneal cavity. No significant alteration in cellular
infiltration was observed in the TCDD exposed mice following treatment with IL- lra. A
similar pattern of response was observed whether the antagonist was administered sc or ip
(data not shown). Comparable results were obtained in a single study using an anti IL-lp
neutralizing antibody (R&D, Minneapolis MN) to inhibit IL -1(3 activity (data not shown).
These results suggest that IL-1 may play a role in neutrophil recruitment in control mice,
however, an increase in IL-1 activity does not appear to account for the observed TCDD
induced hyperinflammation.
As shown in Fig. 2.2 (panel B), inhibition of TNF activity with rhuTNFR:Fc in
vehicle treated mice significantly reduced the total number of PEC and the number of
macrophages harvested from the peritoneum. The number of neutrophils was not
affected. In TCDD exposed animals, rhuTNFR:Fc dramatically reduced the
inflammatory response. Numbers of PEC, macrophages and neutrophils were decreased
resulting in a pattern of response nearly identical to that of control animals treated with
rhuTNFR:Fc. Repeated experiments produced comparable results only if the reagent was
administered iv. Intraperitoneal injections had no effect on cellular influx in this model
(data not shown). These results suggest that TNF plays a major role in mediating TCDD
induced hyperinflammation.
An increase in TNF activity could result from an alteration in production, release,
and/or degradation of the protein, a decrease in endogenous inhibitors, and/or an increase
in responsiveness to this inflammatory mediator. To evaluate alterations in production
and or release of TNF, we measured plasma TNFa levels by ELISA 90 minutes following
SRBC injection. Repeated studies demonstrated a dose dependent increase in circulating
levels of TNFa in TCDD treated mice (Table 2.2).
25
70
so
50
40
30
20
10
0
VEHICLE
& PBS
VEHICLE
TCDD
& TNFR:Fc
& PBS
TCDD
& TNFR:Fc
Fig. 2.2. The effects of IL-Ira (Panel A) and rhuTNFR:Fc (Panel B) on total numbers of PEC, MAC and
PMN harvested from the peritoneal cavity of vehicle and TCDD (20 ug/kg) exposed mice 18-20 hours
following ip injection of SRBC. 1 mg of IL-lra was given sc 30 minutes before and at 3 hour intervals
following SRBC injection. 100 ug of rhuTNFR:Fc was injected iv 30 minutes before injection of SRBC.
Data are presented as means ± SE of 6-8 mice per group.
* p<0.05 TCDD & PBS versus vehicle & PBS
** p<0.05 treatment with cytokine inhibitor versus respective PBS treatment
26
Table 2.2: The effect of TCDD on plasma TNFa levels 90 minutes following sheep red
blood cell injection
TCDD
(ug/kg)
0
5
20
TNFa
(pg/ml)
501 ± 122
910 ± 348
1213 ± 295*
a Mice were killed by CO, asphyxiation 90 minutes following ip injection of SRBC. Blood was collected
by cardiac puncture, plasma was harvested and stored at -70 degrees until TNF ELISA assay was
performed. All samples were collected on the same day and assayed together. Data are presented as means
± SE of 6 mice per treatment.
*p<0.05 2Oug TCDD/kg versus Oug TCDD/kg
These findings indicate that TCDD exposure increases circulating levels of TNF
in response to antigenic stimulation, but does not address whether other alterations in
TNF activity occur. Interestingly, when the identical plasma samples were measured by
bioassay (cytotoxicity toward murine WEHI-164 cell line, described by Eskendari et al.,
1990), a similar pattern of response was observed but the measured concentrations of
TNF were much lower (data not shown). The presence of immunologically detectable
TNF with low levels of biologically active TNF is likely explained by the presence of
circulating binding proteins that inhibit TNF activity without compromising its
immunologic properties (Bemelmans et al., 1993). Inhibition of biologically active TNF
by endogenous soluble binding proteins may be an important protective mechanism to
down regulate the inflammatory process and protect the animal from the adverse
consequences of excessive TNF activity (Van Zee et al., 1992).
27
The data presented here strongly suggest that increased TNF activity plays a
critical role in TCDD induced hyperinflammation. Whether increased TNF activity
contributes to the downstream suppression of antibody response to SRBC is currently
under investigation.
The mechanisms whereby TCDD exposure increases TNF activity are not known.
No effect of TCDD on TNF mRNA levels have been reported to date (Steppan and
Kerkvliet, 1991). Studies to examine the effect of TCDD on translation and secretion of
TNF from a macrophage cell line are in progress.
28
References
Bemelmans, M.H.A., Gouma, D.J., and Buurman, W.A. (1993). Influence of
nephrectomy on tumor necrosis factor clearance in a murine model. J. Immunol.
150, 2007-2017.
Clark, G.C., Lucier, G., Luster, M., Thompson, M., Mahler, J., and Taylor, M. (1991a).
Tumor necrosis factor (TNF) antibodies and dexamethasone (DEX) treatment
reverse the acute toxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD).
Toxicologist 11, 37. [Abstract 53]
Clark, G.C., Taylor, M.J. Tritscher, A.M. and Lucier, G.W. (1991b). Tumor necrosis
factor involvement in 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated endotoxin
hypersensitivity in C57B1/6 mice congenic at the Ah locus. Toxicol. Appl.
Pharmacol. 111, 422-431.
Coligan, J.E., Kruisbeck, A.M., Margulies, D.H., Shevach, E.M. and Strober, W. (eds.)
(1992) Current Protocols in Immunology, pp. 3.15.4-3.15.5. John Wiley & Sons,
New York.
Davis, D. and Safe, S. (1988). Immunosuppressive activities of polychlorinated
dibenzofuran congeners: quantitative structure-activity relationships and
interactive effects. Toxicol. Appl. Pharmacol. 94, 141-149.
Dinarello, C.A., Gelfand, J.A. and Wolff, S.M. (1993). Anticytokine strategies in the
treatment of the systemic inflammatory response syndrome. JAMA 269, 1829­
1835.
Dinarello, C.A. and Thompson, R.C. (1991). Blocking IL-1: interleukin 1 receptor
antagonist in vivo and in vitro. Immunol. Today 12, 404-410.
Eskendari, (1990). WEHI 164 subclone 13 assay for TNF: sensitivity, specificity, and
reliability. Immunol. Investigation, 19, 69-79.
Exley, A.R. and Cohen, J. (1990). Optimal collection of blood samples for the
measurement of tumor necrosis factor a. Cytokine 2, 353-356.
Holsapple, M.P., Morris, D.L., Wood, S.C. and Snyder, N.K. (1991). 2,3,7,8­
tetrachlorodibenzo-p-dioxin-induced changes in immunocompetence: possible
mechanisms. Annu. Rev. Pharmacol. Toxicol. 31, 73-100.
29
Kerkvliet, N.I. and Brauner, J.A. (1990). Flow cytometric analysis of lymphocyte
subpopulations in the spleen and thymus of mice exposed to an acute immunosup­
pressive dose of 2,3,7,8-tetrachlorodibenzo-p-dioxin. Environ. Research 52, 146­
164
.
Kerkvliet, N.I. and Oughton, J.A. (1992). Acute inflammatory response to sheep red
blood cell challenge in mice treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin
(TCDD): phenotypic and functional analysis of peritoneal exudate cells. Toxicol.
Appl. Pharmacol. 119,248-257.
McIntyre, K.W., Stepan, G.J., Kolinsky, K.D., Benjamin, W.R., Plocinski, J.M., Kaffka,
K.L., Campen, C.A., Chizzonite, R.A. and Kilian, P.L. (1991). Inhibition of
interleukin 1 (IL-1) binding and bioactivity in vitro and modulation of acute
inflammation in vivo by IL-1 receptor antagonist and anti-IL-1 receptor
monoclonal antibody. J. Exp. Med. 173, 931-939.
Sayers, T.J., Wiltrout, T.A., Bull, C.A., Denn, A.C., Pilaro, A.M., and Lokesh, B. (1988).
Effect of cytokines on polymorphonuclear neutrophil infiltration in the mouse. J.
Immunol. 141, 1670-1677.
Steppan, L.B. and Kerkvliet, N.I. (1991). Influence of 2,3,7,8-tetrachloro dibenzo-p­
dioxin (TCDD) on the production of inflammatory cytokine mRNA by C57B1/6
macrophages. Toxicologist 11, 35. [Abstract 45]
Sutter, T.R., Guzman, K., Dold, K.M., and Greenlee, W.F. (1991). Targets for dioxin:
genes for plasminogen activator inhibitor-2 and interleukin-1(3. Science, 254, 415­
418.
Taylor, M.J.. Lucier, G.W., Mahler, J.F., Thompson, M., Lockhart, A.C., and Clark, G.C.
(1992). Inhibition of acute TCDD toxicity by treatment with anti-tumor necrosis
factor antibody or dexamethasone. Toxicol. Appl. Pharmacol. 117, 126-132.
Van Zee, K. J., Kohno, T., Fischer, E. Rock, C.S., Moldawer, L.L., and Lowry, S.F.
(1992). Tumor necrosis factor soluble receptors circulate during experimental and
clinical inflammation and can protect against excessive tumor necrosis factor a in
vitro and in vivo. Proc. Natl. Acad. Sci. 89, 4845-4849.
Vecchi,A., Mantovani, A., Sironi, M., Luini, M., Cairo, M., and Garattini, S. (1980)
Effect of acute exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin on humoral
antibody production in mice. Chem. Biol. Interact. 30, 337-341.
30
Chapter Three
The Effects of 2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) on Tumor Necrosis Factor
(TNF) Production by Peritoneal Cells
AUTHORS:
A. B. Moos
J.A. Oughton
N.I. Kerkvliet
Accepted for publication in Toxicology Letters
31
Abstract
Recent studies in mice have demonstrated that TNF plays a critical role in
mediating the TCDD-induced enhanced inflammatory response to intraperitoneal (ip)
sheep red blood cells (SRBC). The current studies were designed to evaluate the effects
of TCDD on TNF production by ex-vivo peritoneal cells and a peritoneal macrophage cell
line (IC-21) stimulated with LPS. In support of the hypothesis that TCDD can act
directly on the peritoneal macrophage to increase TNF production, following
pretreatment with TCDD, both ex-vivo peritoneal cells and IC-21 cells produced
increased levels of bioactive TNF when stimulated with LPS. Flow cytometric analyses
of IC-21 cells indicate that TCDD exposure increases intracellular production and
secretion of TNF but does not alter levels of membrane associated TNF.
Introduction
2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) represents the prototype of a large
group of toxic halogenated aromatic hydrocarbons that are widespread environmental
contaminants. TCDD exposure in mice elicits a broad spectrum of biochemical and
pathophysiologic effects, including hepatotoxicity, induction of drug metabolizing
enzymes (Poland and Knutson, 1982), cachexia (Gasiewicz and Neal, 1979; Brewster and
Matsumura, 1989) and immunosuppression (Holsapple, et al., 1991; Kerkvliet and
Burleson, 1994). The mechanisms of TCDD immunotoxicity have been extensively
investigated and are known to involve both Ah receptor-mediated and Ah receptorindependent events (Kerkvliet et al., 1990; Davis and Safe, 1991; Whitlock, 1990).
However, the cell type(s) targeted by TCDD and the biochemical mechanism(s) of
immunotoxicity remain elusive (Holsapple, et al., 1991). Tumor necrosis factor a (TNF),
also known as cachectin, is best characterized as a primary mediator of the acute
inflammatory response and septic shock (Vassalli, 1992; Sherry and Cerami, 1988). TNF
alone or in concert with interleukin 1 (IL-1) induces the expression of other
proinflammatory cytokines, and initiates a cascade of events involved in endothelial cell
activation (Dinarello, et al., 1993). TNF also inhibits lipoprotein lipase, leading to
32
cachexia and the wasting syndrome observed during chronic infection (Kerkvliet and
Burleson, 1994; Vassal li, 1992; Tracey and Cerami, 1993).
Because of the similarities between the toxic effects of TCDD and the
pathophysiologic effects of TNF, recent attention has been focused on the role of TNF in
TCDD-induced toxicities. In studies by Taylor, et al. (Taylor, et al., 1992), anti-TNF
antibodies inhibited the loss of body weight, elevations in serum chemistry values, and
mortality associated with acute TCDD toxicity. Clark et al. (1991) demonstrated a
hypersensitivity to endotoxin in mice exposed to TCDD and a corresponding dose-
dependent increase in serum TNF. Alsharif et al. (1994) identified TNF as playing a
critical role in sensitizing and activating phagocytic cells and in amplifying the oxidative
stress-induced tissue injury observed in TCDD-exposed mice. Recently, we have
demonstrated that TNF activity plays a role in mediating the TCDD-induced
hyperinflammatory response to intraperitoneal (ip) sheep red blood cells (SRBC)(Moos,
et al., 1994). In several in vivo (Clark, et al., 1991; Moos, et al., 1994) and ex vivo (Jung,
et al., 1993) model systems, increased levels of circulating TNF have been measured
following TCDD exposure.
Based on these prior reports and, in particular, the observation that TNF is a
mediator of the TCDD-induced enhanced peritoneal inflammatory response (Moos, et al.,
1994) we hypothesized that TCDD targets the peritoneal cells (PEC) and that, in response
to TCDD exposure, stimulated PEC produce more TNF. In this study, we measured TNF
production by an LPS-stimulated murine peritoneal macrophage cell line (IC-21) cultured
with TCDD and by LPS-stimulated PEC harvested from mice exposed to TCDD in vivo.
In addition, immunocytochemistry and flow cytometric analysis were used to characterize
intracellular production and cellular processing of TNF in LPS-stimulated IC-21 cells.
Results from these studies indicate that in response to pretreatment with TCDD
stimulated ex-vivo PEC and IC-21 cells secrete increased levels of bioactive TNF
supporting the hypothesis that TCDD can act directly on the peritoneal macrophage to
increase TNF secretion.
33
Methods and Materials
Animals:
Female C57B1/6 mice (The Jackson Laboratory, Bar Harbor, ME), 8-10 weeks of age
were used in this study. Mice were maintained according to NIH guidelines and
acclimated for a minimum of 2 weeks prior to treatment.
Cells:
IC-21 murine macrophage cells (ATCC TIB 186) were maintained in continuous culture
using RPMI-1640 supplemented with 10% FBS and 501,1g/m1 gentamicin sulfate
(BioWhittaker). Murine L929 fibroblast cells (generously provided by Dr. Mark Blazha,
National Institute of Environmental Health Sciences, NC) were maintained similarly.
Chemicals:
TCDD was obtained from Cambridge Isotope Laboratories, Inc. (Woburn, MA) as a
certified reference standard of >98% purity. For in vivo use, TCDD was dissolved in
anisole and diluted in peanut oil. A vehicle solution of anisole in peanut oil was prepared
similarly. For in vitro use, TCDD was dissolved in DMSO, and DMSO (<0.02% final
concentration) was used as a vehicle control.
Antibodies:
Biotinylated anti-mouse TNF and phycoerythrin (PE) labeled strepavidin (Pharmingen,
San Diego, CA) were used to detect intracellular and membrane associated TNF.
Biotinylated normal rat IgG (Pharmingen) was used as an isotypic control. Antibodies
were pretreated for optimal fluorescence and biotinylated antibodies were centrifuged at
10,000 g for 20 minutes prior to use.
Induction of TNF:
IC-21 cells were stimulated with increasing doses of LPS (E.Coli serotype 026:B6,
Sigma, St. Louis, MO) following 24 hours of incubation with TCDD (10-9 M) or DMSO.
34
In some studies, monensin (31.1M, Sigma) was added 30 minutes prior to LPS stimulation
to inhibit protein secretion from the cells (Jung, et al., 1993). At various times following
LPS stimulation, culture supernatants were collected and stored at -70°C until assayed for
TNF activity. Resident peritoneal cells from mice treated with 20 pg TCDD/kg or
vehicle were harvested. Total peritoneal cells were enumerated on a Coulter counter and
differential cell counts were determined following cytocentrifugation and staining with
Gugol blue (Moos, et al., 1994). Cells were pooled and lx106 cells were incubated in
DMEM supplemented with 5% FBS at 37°C with 5% CO2 for 2 hours before being
stimulated with 1 µg /m1 LPS for 90 minutes. Culture supernatants were collected and
stored at -70 °C until assayed for TNF activity.
Cell Fixation and Immunocytochemical Staining:
Fixation and staining procedures were performed as described by deCaestecker et al.
(1992) with minor modifications. Prior to staining, cells were fixed in 2%
paraformaldehyde for 20 minutes. Cells that were permeabilized were incubated with 1%
saponin (Sigma) for 30 minutes and maintained in 0.1% saponin throughout the staining
procedure (Sander, et al., 1991). Nonspecific binding was blocked by the addition of rat
anti-mouse Fcg receptor mAb (Pharmingen San Diego, CA) and rat IgG (Cappel). Cells
were stained with biotinylated anti-TNF mAb for 30 minutes, followed by several washes
and 20 minutes of incubation with PE-labeled strepavidin. Following several final
washes, cells were stored at 4°C for 24 hours before being analyzed by flow cytometry.
Flow cytometric data were collected on 20,000 cells by listmode acquisition using an
EPICS V flow cytometer (Coulter Electronics, Hiahleah, FL) and analyzed using Cyclops
software (Cytomation, Inc. Fort Collins, CO). Cells were also examined by fluorescent
microscopy using a Zeiss Axiovert 35 microscope.
TNF Bioassay:
L929 cells (2.5 x 104) were incubated in 96 well plates at 37°C in a humidified
atmosphere with 5% CO, until confluent. Mono layers were incubated with actinomycin
35
D (6 µg /ml, Calbiochem, La Jolla, CA) for 30 minutes before adding dilutions of cell
culture supernatants or murine recombinant INFa, standard (Genzyme, Cambridge, MA).
Cells were incubated overnight and monolayers were stained with 0.2% crystal violet,
rinsed and air dried. Well contents were solubilized with 1% SDS for 2 hours and the
plates were read at 595 nm using a BIO-TEK plate reader. Samples and standards for the
bioassay were run in triplicate and the criteria for acceptable variation were that the
standard deviation had to fall within 15% of the mean for each set of samples.
Statistics:
The paired Student 's t test was used to evaluate data for statistical significance. A p value
<0.05 was considered significant.
Results
The effect of TCDD on TNF secretion by LPS-stimulated IC-21 cells:
TNF bioactivity was measured in supernatants collected from LPS-stimulated IC-21 cell
cultures pretreated with TCDD (10-9 M) or DMSO. Viability and cell growth was
unaffected by in vitro exposure to this concentration of TCDD (data not shown). As
shown in Table 3.1A, TNF bioactivity increased over time in response to stimulation with
1 lig LPs/ml. At all times measured, there was an increase in TNF secreted from cells
cultured with TCDD compared to those cultured with DMSO. Although differences in
TNF levels were small, they were consistently observed in multiple experiments. The
results of a single representative experiment are reported here. TNF bioactivity also
increased in response to stimulation with increasing doses of LPS for 120 minutes (Table
3.1B). More TNF was secreted from cells cultured with TCDD compared to cells
cultured with DMSO.
36
Table 3.1. TCDD Pretreatment Increases TNF Secretion by LPS-stimulated 1C-21 Cells*
DMSO
TNF (pg/106 cells)
TCDD
A. 1 lag LPS/ml
10 min.
30 min.
60 min.
90 min.
120 min.
53
57
155
70
97
191
416
613
484
0.1 !_tg LPs /ml
1.0 _tg, LPs/m1
496
856
10.0 µg LPs/m1
1000
516
1026
1520
661
B. 120 min.
* IC-21 cells (1x10') were incubated with DMSO or TCDD (10' M) for 24 hours prior to
stimulation with LPS. At various times following the addition of LPS, culture
supernatants were harvested and assayed for TNF activity using the L929 cytotoxicity
assay. Data presented represent a single experiment, although various doses of LPS and
incubation times were repeated up to 4 times and in every case comparable data were
generated.
The Effect of in vivo exposure to TCDD on ex vivo production of TNF by LPS-stimulated
peritoneal cells:
Mice were exposed to 20 ug TCDD/kg or vehicle and resident PEC were harvested 2
days later. In agreement with a previous report by Kerkvliet and Oughton (Kerkvliet and
Oughton, 1993), TCDD exposure (20 µg /kg) alone did not affect the total number or
differential distribution of resident peritoneal cells harvested. TNF activity was measured
in cell culture supernatants following LPS stimulation (Table 3.2). This experiment was
repeated 5 times, and, in each case, PEC from mice exposed to TCDD in vivo produced
more TNF following LPS stimulation than cells harvested from mice exposed to peanut
oil. No TNF was measured in supernatants of unstimulated PEC harvested from TCDD
or vehicle-exposed mice (data not shown).
37
Table 3.2. In vivo TCDD Exposure Increases TNF Secretion by LPS-stimulated
Peritoneal Cells*
TNF (pg/106 cells)
Expt.
Vehicle
TCDD
1
93
142
2
200
328
3
459
588
4
404
517
5
151
276
*Peritoneal cells were harvested from mice 2 days following exposure to TCDD (20
µg /kg) or vehicle. Peritoneal cells were incubated for 2 hours and then stimulated with 1
pg/m1LPS for 90 minutes.
Data represent the results of five separate experiments.
p = .0001, paired Student's t-test.
Immunocytochemical detection of TNF in IC-21 cells:
Fluorescent micrographs of IC-21 cells stimulated with LPS for 3 hours are shown in
Figure 3.1. Cells were permeabilized with saponin and stained with isotypic control
antibody (Fig 3.1A) or biotinylated anti-TNF (Fig 3.1B). In those cells stained with antiTNF antibody, small focal regions of membrane associated TNF fluorescence are
discernible
38
0
TNF Fluorescence
Figure 3.1. Intracellular TNF staining evaluated by immunofluorescence (A,B,C) and
flow cytometric analysis (D). LPS-stimulated IC-21 cells were permeabilized with
saponin and stained with isotypic control antibody (A), biotinylated anti-TNF antibody
(B) or biotinylated anti-TNF following pretreatment with monensin (C). A representative
histogram generated by flow cytometric analysis is shown in panel D to compare the
fluorescent intensities of TNF staining of cells from panels A, B and C.
as is a distinct intracellular Golgi staining pattern. Pretreatment of the cells with the
carboxylic ionophore monensin interrupts intracellular transport processes leading to an
accumulation of cytokine in the Golgi complex. This is apparent in Fig. 3.1C where
monensin-treated cells showed increased intracellular staining. Cells from the same
sample were examined by flow cytometry, and the pattern of TNF fluorescence is
39
illustrated in the representative histogram shown in Fig. 3.1D. Cells stained with
biotinylated anti-TNF have a strong fluorescent signal relative to cells stained with the
isotypic control antibody. Pretreatment with monensin enhanced the intensity of TNFpositive staining but did not affect the percent of TNF positive cells.
Flow Cytometric Analysis of IC-21 Cells Stimulated over Time with LPS:
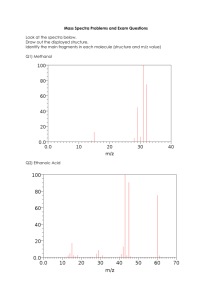
Histograms in Figure 3.2 represent the fluorescent staining pattern of TNF positive IC-21
cells stimulated with 1 ug/m1LPS for 0, 10, 30, 60, 90 and 120 minutes. The fluorescent
intensities of permeabilized and nonpermeabilized cells were compared at each time
point. Increased fluorescent staining of permeabilized cells observed at time zero was
attributed to increased nonspecific binding. This increase in nonspecific binding was
consistently observed in permeabilized cells due to the difficulty in effectively blocking
all intracellular binding sites (See also Table 3, compare 0 minutes stimulation,
permeabilized versus nonpermeabilized). Both intracellular and membrane-associated
fluorescence increased over time in response to LPS. Intracellular TNF staining was first
evident at 10 minutes and was maximal following 90 minutes of stimulation with LPS.
Membrane-associated TNF became apparent between 10 and 30 minutes and continued to
increase throughout the 120 minute period of stimulation.
40
Non-permeabilized
Permeabilized
0 min
10 min
LA
30 min
60 min
90 min
120 min
TNF Fluorescence
Fig. 3.2. Representative histograms generated by flow cytometric analysis illustrate TNF
fluorescence of IC-21 cells at various times following stimulation with 11.1g/m1 LPS. Non­
permeabilized cells and cells permeabilized with saponin are compared at each time
point. Cell staining and analysis by flow cytometry were performed as described in
Materials and Methods. Data were collected on 20,000 cells by listmode acquisition using
an EPICS V flow cytometer.
The effect of TCDD exposure on TNF fluorescence intensity:
Exposure to 10-' M TCDD for 24 hours prior to LPS-stimulation resulted in an increase in
TNF production by IC-21 cells as measured by an increase in mean channel fluorescence
(MCF) of TNF staining (Table 3.3). TCDD exposure did not alter the time course of
41
TNF production or membrane levels of TNF (Table 3.3), but increased intracellular TNF
production. Somewhat unexpectedly, we were unable to detect any difference between
TCDD and DMSO exposure in TNF production in LPS-stimulated IC-21 cells pretreated
with monensin (data not shown).
Table 3.3. TNF Mean Channel Fluorescence (MCF) in 1C-21 Cells Exposed to TCDD or DMSO and Stimulated with
LPS*
Permeabilized
Expt
Time
DMSO
Non-Permeabilized
TCDD
DMSO
TCDD
(min)
Control
TNF
Control
TNF
Control
TNF
Control
TNF
0
ND
ND
12
15
ND
ND
4
5
10
13
20
12
34
4
5
4
5
60
17
88
17
101
4
18
4
14
90
15
128
13
141
5
25
4
25
120
15
109
14
144
4
25
4
29
2
120
4
58
4
75
3
3
3
16
3
120
7
54
7
78
3
11
4
10
1
ND = not done
* TNF MCF of permeabilized and nonpermeabilized IC-21 cells are compared following incubation with 1 µg /m1 LPS over
time. Cells were exposed to TCDD (10-9 M) or DMSO for 24 hours prior to stimulation with LPS. MCF was determined from
single-parameter histograms of TNF fluorescence (using a log scale).
43
Discussion
TNF has been implicated as a mediator of TCDD toxicity in several animal model
systems (Kerkvliet and Burleson, 1994; Taylor, et al., 1992; Clark, et al., 1991; Alsharif,
et al., 1994). and increased TNF activity following exposure to TCDD has been measured
(Clark, et al.. 1991; Moos, et al., 1994; Jung, et al., 1993). Studies in our laboratory have
demonstrated that exposure to TCDD results in an enhanced peritoneal inflammatory
response when C57B1/6 mice are injected ip with SRBC (Kerkvliet and Oughton, 1993)
and that this response is mediated by increased TNF activity (Moos, et al., 1994). We
hypothesized that PEC were the source of increased TNF in this model. To evaluate the
effects of TCDD exposure on TNF production by PEC cells, we measured TNF
production by a peritoneal macrophage cell line (IC-21) derived from C57B1/6 mice.
TCDD exposure (10 -9 M) resulted in a small but consistently measured increase in
bioactive TNF secreted from IC-21 cells, both in response to stimulation with LPS over
time and in response to stimulation with increasing doses of LPS. These results indicate
that LPS stimulated IC-21 cells are capable of increasing secretion of TNF in response to
TCDD exposure.
To take into account the diverse host derived signals that may modulate secretory
responses, we also tested the ability of ex vivo PEC from mice exposed to TCDD or
vehicle to produce TNF in response to LPS stimulation in culture. The results from 5
separate experiments demonstrated that PEC harvested from mice exposed to TCDD
produced a modest but statistically significant increase in TNF compared to cells
harvested from control mice. We conclude from these data that TCDD targets the
peritoneal cell to produce more TNF upon LPS stimulation. The cell type targeted by
TCDD is not clear from these studies, but the peritoneal macrophage is a likely candidate.
Not only is the LPS-stimulated macrophage the largest source of TNF (Vassalli, 1992;
Tracey and Cerami, 1993) but macrophages comprise the majority of the resident
peritoneal cells (Kerkvliet and Oughton, 1993). A TCDD effect on TNF production by
peritoneal macrophages has previously been reported by Massa et al. (1992). These
investigators measured more TNF produced by adherent peritoneal cells harvested from
44
NMRI mice injected with TCDD than by cells from control mice following stimulation
with LPS. The amount of TNF produced correlated with the degree of cachexia and
weight loss resulting from TCDD exposure in these mice.
The mechanism whereby TCDD exposure increases TNF secretion is unclear.
Because TCDD binds to the Ah receptor which acts as a ligand-activated transcription
factor (Gaido and Maness, 1994), we initially hypothesized that TCDD acts directly on
the peritoneal macrophage to increase transcription of TNF in response to an
inflammatory stimulus. Small increases in TNFa transcripts have been measured by
reverse transcription polymerase chain reaction (RT-PCR) in a human breast cancer cell
line following incubation with TCDD (Vogel and Abel, 1995). Results in our laboratory
using RT- PCR to evaluate the effects of TCDD on TNFa mRNA in IC-21 cells or
peritoneal cells, however, have been inconclusive. No differences in TNF specific
mRNA were identified by Northern blotting following TCDD exposure in either IC-21 or
ex vivo peritoneal cells (Steppan and Kerkvliet, 1991). Murine TNF is initially
synthesized as a pro-protein with an extra N-terminal peptide of 79 amino acids (Kim, et
al., 1993). This presequence is not cleaved in the rough endoplasmic reticulum like a
typical signal sequence but rather functions to anchor the TNF precursor polypeptide in
the plasma membrane (Pradines-Figueres and Raetz, 1992). Membrane associated proTNF is then proteolytically cleaved into two biologically active compounds. Soluble
mature TNF is released into the medium while the membrane portion of the protein
remains cell-associated. It has been suggested that the two forms of TNF function in
different pathophysiologic processes. For example, the membrane bound form may
mediate direct effector-target cell interactions (Kim, et al., 1993) while the soluble form
may act in a paracrine manner to activate other immunoreactive or inflammatory cells, or
in an endocrine manner as a mediator of septic shock and cachexia associated with
chronic disease states (Kinkhabwala, et al., 1990). We postulated that TCDD exposure
may affect either the translation or processing of TNF, and we used immunocytochemical
methods to evaluate the effects of TCDD on intracellular production and membrane
association of TNF.
45
Intracellular TNF was easily detected by immunocytochemical evaluation of LPS-
stimulated IC-21 cells permeabilized with saponin. The bright positive TNF staining
pattern which represents both membrane and cytoplasmic protein was enhanced by
pretreating the cells with monensin, a carboxylic ionophore that interrupts intracellular
transport processes leading to an accumulation of cytokine in the Golgi complex (Jung, et
al., 1993). Evaluation of the same cells by flow cytometry revealed a comparable pattern
of staining, a bright positive TNF signal enhanced by pretreatment with monensin. Based
on the good correlation between immunocytochemical and flow cytometric analyses, we
felt confident that flow cytometry is a suitable technique to evaluate TNF production in
these cells.
When permeabilized and nonpermeabilized cells were compared by flow
cytometry, the pattern of intracellular production and membrane associated TNF in IC-21
cells was evaluated independently. Over time, LPS stimulation increased both
intracellular and membrane associated TNF, and the pattern of fluorescent staining
reflected what is known about the synthesis, processing and secretion of TNF in
macrophages. Intracellular TNF was detected after only 10 minutes of stimulation with
LPS, and there was a short lag before membrane associated TNF could first be identified.
Secreted TNF could be reliably measured between 30 and 60 minutes of stimulation with
LPS.
Exposure of IC-21 cells to TCDD increased intracellular production and secretion
of TNF but did not influence the association of TNF with the cellular membrane. The
mechanism(s) whereby TCDD exposure results in an increase in intracellular and secreted
TNF without altering membrane levels of TNF is unknown at this time. It is possible that
there is some inherent property of the membrane that limits either the expression or the
stability of these molecules on the cell surface. Alternatively, only a limited number of
TNF molecules may be available for antibody detection due to alteration or stearic
inaccessibility. Additionally, it is also possible that TCDD-exposure decreases the
stability of the membrane-bound portion of the TNF molecule. In any case, an increase
in secreted bioactive TNF without an alteration in the membrane levels may explain how
46
TCDD exposure enhances the inflammatory (paracrine) and systemic (endocrine)
manifestations of TNF but has little effect on TNF's tumoricidal properties (attributable to
membrane associated TNF). Monensin arrests the process of protein secretion and
initially we expected that monensin treatment would enhance differences observed
between TCDD and DMSO exposed cells. Our failure to measure differences following
monensin treatment is possibly explained by the inability of the flow cytometer to discern
differences in fluorescence intensity when the signal is extremely bright and compact
relative to the cell as a whole.
Exposure to TCDD resulted in an increase in bioactive TNF secreted by IC-21
cells and ex vivo peritoneal cells in response to LPS. TCDD did not appear to alter
transcription (evaluated by Northern blot), but, in IC-21 cells where production and
intracellular processing can be evaluated by flow cytometric analysis, TCDD exposure
enhanced intracellular production. The mechanism whereby TCDD exposure increases
TNF production is not identified, but may involve stabilization of TNF mRNA, or an
increase in rate of translation (Tracey and Cerami, 1993).
47
References
Alsharif, N.Z., Hassoun, E., Bagchi, M., Lawson, T., Stohs, S.J. (1994) The effects of
anti-TNF-alpha antibody and dexamethasone on TCDD-induced oxidative stress
in mice. Pharmacology 48, 127-136.
Brewster, D.W. and Matsumura, F. (1989) Differential effect of 2,3,7,8­
tetrachlorodibenzo-p-dioxin on adipose tissue lipoprotein lipase activity in the
guinea pig, rat, hamster, rabbit and mink. Comp Biochem Physiol 93, 49-53.
Clark, G.C., Taylor, M.J., Tritscher, A.M. and Lucier, G.W. (1991) Tumor necrosis factor
involvement in 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated endotoxin
hypersensitivity in C57B1/6J mice congenic at the Ah locus. Toxicol. Appl.
Pharmacol. 111, 422-431.
Davis, D. and Safe, S. (1991) Halogenated aryl hydrocarbon-induced suppression of the
in vitro plaque-forming cell response to sheep red blood cells is not dependent on
the Ah receptor. Immunopharm. 21, 183-190.
de Caestecker, M.P., Telfer, B.A., Hutchinson, I.V. and Ballardie, F.W. (1992) The
detection of intracytoplasmic interleukin-la, interleukin-13 and tumour necrosis
factor a expression in human monocytes using two color immunofluorescence
flow cytometry. J. Immunol. Methods 154, 11-20.
Dinarello, C.A., Gelfand, J.A. and Wolff, S.M. (1993) Anticytokine strategies in the
treatment of the systemic inflammatory response syndrome. JAMA 269, 1829­
1835.
Gaido, K.W. and Maness, S.C. (1994) Regulation of gene expression and acceleration of
differentiation in human keratinocytes by 2,3,7,8-tetrachlorodibenzo-p-dioxin.
Toxicol. Appl. Pharmacol. 127, 199-208.
Gasiewicz, T.A., Neal, R.A. (1979) 2,3,7,8-Tetrachlorodibenzo-p-dioxin tissue
distribution, excretion and effects on clinical chemical parameters in guinea pigs.
Toxicol Appl Pharmacol. 51, 329-339.
Holsapple, M.P., Morris, D.L., Wood, S.C. and Snyder, N.K. (1991) 2,3,7,8­
Tetrachlorodibenzo-p-dioxin-induced changes in immunocompetence: possible
mechanisms. Annu. Rev. Pharmacol. Toxicol. 31, 73-100.
Jung, T., Schauer, U., Huesser, C. Neumann, C. and Rieger, C. (1993) Detection of
intracellular cytokines by flow cytometry. J. Immunol. Methods 159, 197-207.
48
Kerkvliet,
Steppan, L.B., Brauner, J.A., Deyo, J.A., Henderson, M.C.. Tomar, R.S.
and Buhler, D.R. (1990) Influence of the Ah locus on the humoral
immunotoxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin: evidence for Ah-receptor­
dependent and Ah-receptor-independent mechanisms of immunosuppression.
Toxicol. Appl. Pharmacol. 105, 26-36.
Kerkvliet, N.I. and Oughton, J.A. (1993) Acute inflammatory response to sheep red blood
cell challenge in mice treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD):
phenotypic and functional analysis of peritoneal exudate cells. Toxicol. Appl.
Pharmacol. 119, 248-257.
Kerkvliet, N.I. and Burleson, G.R. (1994) Immunotoxicity of TCDD and related
halogenated aromatic hydrocarbons.In: J.H. Dean, M.I. Luster. A.E. Munson and
I. Kimber (Eds.), Immunotoxicity and Immunopharmacology, Raven Press, Ltd.
New York, pp.97-121.
Kim, K.U., Kwon, O.J. and Jue, D.M. (1993) Pro-tumor necrosis factor cleavage enzyme
in macrophage membrane/particulate. Immunology 80, 134-139.
Kinkhabwala, M., Sehajpal, P., Skolnik, E. Smith, D., Sharma, V.K., Vlassara, H.,
Cerami, A. and Suthanthiran, M. (1990) A novel addition to
the T cell
repertory: cell surface expression of tumor necrosis factor/cachetin by activated
normal human T cells. J. Exp. Med.171, 941-946.
Massa, T., Esmaeili, A., Fortmeyer, H., Schlatterer, B., Hagenmaier, H.and Chandra, P.
(1992) Cell transforming and oncogenic activity of 2,3,7,8-tetrachloro-and
2,3,7,8-tetrabromodibenzo-p-dioxin. Anticancer Research 12, 2053-2060.
Moos, A.B., Baecher-Steppan, L. and Kerkvliet, N.I. (1994) Acute inflammatory
responses to sheep red blood cells in mice treated with 2,3,7,8­
tetrachlorordibenzo-p-dioxin: the role of proinflammatory cytokines, IL-1 and
TNF. Toxicol. Appl. Pharmacol. 127, 331-335.
Poland, A. and Knutson, J.C. (1982) 2,3,7,8-Tetrachlorodibenzo-p-dioxin and related
halogenated aromatic hydrocarbons: examination of the mechanism of toxicity.
Annu. Rev. Pharmacol. Toxicol. 22, 517-554.
Pradines- Figueres, A. and Raetz, C.R.H. (1992) Processing and secretion of tumor
necrosis factor a in endotoxin-treated mono mac 6 cells are dependent on phorbol
myristate. J. Biol. Chem. 267, 23261-23268.
49
Sander, B., Andersson, J. and Andersson, U. (1991) Assessment of cytokines by
immunofluorescence and the paraformaldehyde-saponin procedure. Immunol.
Reviews 119, 65-93.
Sherry, B. and Cerami, A. (1988) Cachectin/tumor necrosis factor exerts endocrine,
paracrine and autocrine control of inflammatory responses. J. Cell Bio. 107, 1269­
1 277.
Steppan, L.B. and Kerkvliet, N.I. (1991) Influence of 2,3,7,8-tetrachlorodibenzo-p-dioxin
(TCDD) on the production of inflammatory cytokine mRNA by C57B1/6
macrophages. Toxicologist 11, 35 (abst.).
Taylor, M.J., Lucier, G.W., Mahler, J.F., Thompson, M., Lockhart, A.C. and Clark, G.C.
(1992) Inhibition of acute TCDD toxicity by treatment with anti-tumor necrosis
factor antibody or dexamethasone. Toxicol. Appl. Pharmacol. 117, 126-132.
Tracey, K.J., and Cerami, A. (1993) Tumor necrosis factor, other cytokines and disease.
Annu. Rev. Cell Bio. 9, 317-343.
Vassal li, P. The pathophysiology of tumor necrosis factors. (1992) Annu. Rev. Immunol.
10, 411-452.
Vogel, C. and Abel, J. (1995) Effect of 2,3,7,8-tetrachlorodibenzo-p-dioxin on growth
factor expression in the human breast cancer cell line MCF-7. Arch Toxicol. 69,
259-265.
Whitlock, J.P. (1990) Genetic and molecular aspects of 2,3,7,8-tetrachlorodibenzo-p­
dioxin action. Annu. Rev. Pharmacol. Toxicol. 30, 251-277.
50
Chapter Four
Inhibition of Tumor Necrosis Factor Activity Fails to Restore
2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD)-induced Suppression of the Antibody
Response to Sheep Red Blood Cells
AUTHORS:
A. B. Moos
N. I. Kerkvliet
Reprinted from Toxicology Letters Vol. 81
51
Abstract
2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) immunotoxicity is characterized in
part by a profound suppression in T cell-dependent antibody production to sheep red
blood cells (SRBC); however the mechanisms involved in antibody suppression are not
fully understood. Recent studies from several different laboratories have suggested that
increased tumor necrosis factor (TNF) activity may mediate some of the toxicity
associated with TCDD exposure. The current studies were designed to evaluate the role
TNF play in TCDD-induced suppression of the antibody response. We examined the
effects of exogenous TNFa and the effects of blocking TNF activity with a soluble TNF
receptor (rhuTNFR:Fc) on antibody production in control and TCDD exposed C57B1/6
mice. Results indicate that under certain conditions, increased TNF can suppress
antibody production to SRBC, but TNF does not appear to mediate TCDD-induced
antibody suppression.
Introduction
2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD) represents the prototype of a large
group of toxic halogenated aromatic hydrocarbons that are widespread environmental
contaminants. The immunotoxic properties of TCDD are well documented in several
animal species (Holsapple, 1991). One of the most sensitive indicators of TCDD
immunotoxicity is a suppression of the macrophage and T cell dependent antibody
response to sheep red blood cells (SRBC) in 'responsive' mouse strains (Vecchi, et al.,
1980; Davis and Safe, 1988; Kerkvliet and Brauner, 1990).
We have recently reported that C57B1/6 mice exposed to 5-20 ,ug TCDD/kg body
weight develop an enhanced inflammatory response to SRBC injected intraperitoneally
(I.P.)(Kerkvliet and Oughton, 1992; Moos, et al., 1994). This hyperinflammatory
response was characterized by an increase in the total number of peritoneal cells (PEC)
and an increase in relative and absolute numbers of neutrophils (PMN) harvested from
the peritoneum 18-40 h following injection of SRBC antigen.
52
To better understand the mechanism underlying the hyperinflammatory response
in TCDD-exposed mice, a series of studies using specific inhibitors of the proinflammatory cytokines TNF and interleukin-1 (IL-1) was carried out (Moos, et al.,
1994). When TNF activity was inhibited using a TNF soluble receptor (rhuTNFR:fc), the
TCDD-induced hyperinflammatory response was normalized. In contrast, when IL-1
activity was blocked using an IL-1 receptor antagonist (IL- lra), the peritoneal
inflammatory response was not altered in TCDD-exposed mice (Moos, et al., 1994).
These studies suggest that TNF but not IL-1 plays a critical role in mediating the
observed TCDD-induced hyperinflammatory response to ip SRBC.
Based on these observations we hypothesized that the increased inflammatory
response and suppressed antibody response to SRBC observed in TCDD-exposed mice
are linked mechanistically through an increase in TNF. The current studies were
designed to test this hypothesis by examining whether increased TNF levels influence
antibody production to SRBC, and whether neutralization of TNF activity normalizes
TCDD-induced suppression of the humoral immune response. To evaluate the role TNF
plays in antibody production, we first examined the effects of increasing doses of
exogenous TNF on the splenic plaque-forming cell response to SRBC. Secondly we
blocked TNF activity both at the time of antigen exposure and throughout the course of
antibody production with intravenous (i.v.) administration of rhuTNFR:Fc, a potent
antagonist of TNF activity (Wooley, et al., 1993; Moher, et al., 1993). The effect of
inhibition of TNF activity on antibody production in vehicle control and TCDD-exposed
mice was evaluated by comparing the number of splenic plaque-forming cells from mice
in each treatment group.
Materials and Methods
Animals:
Female C57B1/6 mice (Jackson Laboratories, Bar Harbor, ME), 8-10 weeks of age,
weighing 18-20 g were used in this study. They were maintained in a specific virus-free
colony with a 12 h light/dark cycle, at 22 + 2°C and 40-60% humidity. Mice were
53
housed 4-6 per cage in front of a laminar flow unit on Bed-o-Cob bedding (The
Andersons, Maumee, OH). Food (Wayne Rodent Blox, Harlan Sprague Dawley Co.,
Bartonville, IL) and tap water were provided ad libitum. All mice were acclimated for a
minimum of two weeks prior to treatment.
Chemicals:
TCDD, obtained from Cambridge Isotope Laboratories, Inc. (Woburn, MA) as a certified
reference standard of >98% purity, was dissolved in anisole and diluted in peanut oil. A
vehicle solution of anisole in peanut oil was prepared similarly. Murine recombinant
TNFa was purchased from Genzyme (Cambridge, MA) and diluted in Dulbecco's
phosphate buffered saline (DPBS, Bio Whittaker, Inc., Walkersville, MD).
The TNF soluble receptor (rhuTNFR:Fc), generously provided by Dr. M. B. Widmer
(Immunex, Seattle, WA) is a dimeric form of the extra-cellular portion of the p80 cell
surface TNF receptor (TNFR) linked to the Fc portion of human IgG1 and expressed in
mammalian cells (Wooley, et al., 1993; Moher, et al., 1993). This chimeric fusion
protein binds TNF with high affinity and inhibits activity by preventing the ligand from
binding to cellular receptors and initiating signal transduction. The ability of this reagent
to block TNF activity has been demonstrated in many model systems (Wooley, et al.,
1993; Moher, et al, 1993; Ashkenazi, et al., 1991; Lesslauer, et al., 1991; Peppel, et al.,
1991; Loetscher, et al.)
Antigen Sensitization:
Sheep red blood cells (SRBC) collected each month from a single sheep (Colorado Serum
Co., Denver, CO) were washed three times in 10 x volume and diluted to 5 x 108
SRBC/ml in DPBS. Mice were sensitized by ip injection of 2.5 x 108 SRBC in 0.5 ml
DPBS 2 days after TCDD exposure.
54
Plaque-forming Cell Assay:
Splenic plaque-forming cells (PFC) were enumerated 5 days following SRBC injection.
The PFC assay was a modification of the assay described by Cunningham and Szenberg
(1968). Briefly, single cell spleen suspensions were prepared in Hank's balanced salt
solution supplemented with 2.5% fetal bovine serum (2.5% HBSS) by gently teasing the
spleen with forceps. Spleen cells were washed two times and diluted in 2.5% HBSS to
2.28 x 106 cells/ml. A 175 41 aliqout of this dilution (4 x 105 cells) was placed in a 12 x
75 mm glass culture tube. SRBC (50 4L OF 2 x 109 SRBC/ml) and 25 ,u1 of SRBC-
absorbed guinea pig complement (Colorado Serum Co., Denver, CO) diluted 1:2 in 2.5%
HBSS were added. A 55 41 aliquot of this mixture was placed in a microscope slide
chamber, sealed with a warm wax and Vaseline' mixture and incubated at 37°C for 45
min. Placques were enumerated using a Bellco plaque viewer (Bellco Glass Co.,
Vineland, NJ). The number of PFC/106 spleen cells and the number of PFC/spleen were
compared among groups.
Experimental Design:
Effect of exogenous TNF on the anti-SRBC response: Four groups of 6 mice were
treated i.p. with 0,1,10, or 100 ng of recombinant TNFa in 0.2 ml. A dose of 10 ng of
TNFa was selected based on studies from our laboratory demonstrating that this dose
mimics the hyperinflammatory effects of TCDD exposure to SRBC (Moos, et al., 1994).
Ten-fold higher and ten-fold lower dilution were also tested. Mice were injected 30 min
prior to antigen exposure and every 24 h for the next 4 days. On day 5, mice were killed
by CO2 asphyxiation, spleens were removed and processed, and PFC were enumerated.
Effect of inhibition of TNF activity on the anti-SRBC response:
In each of three separate experiments, mice were divided into four groups with 6-10
animals per group. Mice received either 5 jig TCDD/kg body weight or peanut oil
vehicle by gavage in a volume of 0.1 m1/10 g body weight. Mice were injected with
SRBC 2 days later. In two separate experiments, 100 ,ug or 350 ,ug of rhuTNFR:Fc in 0.2
55
ml or 0.2 ml DPBS dilutent was injected into a lateral tail vein 30 min prior to antigen
exposure. In a third experiment, 100 ug of rhuTNFR:Fc or 0.2 ml dilutent was injected
30 min before SRBC injections and every morning for the next 4 days. The 100 ,ug dose
of rhuTNFR:Fc was previously shown to normalize the TCDD-induced
hyperinflammatory response to SRBC (Moos, et al., 1994). Five days following antigen
sensitization, mice were killed by CO, asphyxiation, spleens were removed, and PFC
were enumerated.
Statistical Analysis:
Exogenous TNF data were analyzed by one way analysis of variance (ANOVA)
modeling using SAS statistical software (Version 6.03, SAS Institute Inc., Cary, NC) at a
significance level of a = 0.05. LSD t-test was used for multiple comparisons. TNF
inhibition studies were evaluated for significance using Student's t-test. In all analyses, a
probability level of 0.05 was considered significant.
Results
Effects of Exogenous TNFa on Antibody Production:
To determine whether elevated levels of TNF were capable of altering the antibody
response to SRBC, three doses of recombinant TNFa were administered i.p. 30 min prior
to SRBC injection and daily for the next 4 days. As shown in Table 4.1, there was a
statistically significant suppression in the number of PFC/106 spleen cells in mice that
received injections of 10 or 100 ng TNFa, although there was no statistical difference
between these two doses. The PFC response in mice receiving the lower (1 ng) dose of
TNFa was not statistically different from control mice. Spleen cell recovery was not
affected by treatment with exogenous TNF, thus similar results were seen when data were
expressed on a whole spleen basis (Table 4.1). Based on daily evaluations and body
weights, repeated injections of TNF did not elicit any clinical manifestations of cachexia
or wasting during the experimental period.
56
Table 4.1 Effect of exogenous TNF on number of anti-SRBC PFC in control mice*
ng TNF
PFC/106 spleen cells
PFC/spleen x 104
0
4117a(120)
66.4c(0.2)
1
407 P(255)
65.8c(0.5)
10
2386b(390)
48.1 d(0.4)
100
2970b(480)
46.2d(0.3)
*Murine recombinant TNF was administered IP 30 min prior to SRBC antigen and
every 24 h for the next 4 days. Spleens were removed and PFC were enumerated on Day
5. Date are presented as means (SE) of six mice per treatment group.
a'b'"Different letters indicate statistical significance between treatment groups
(P < 0.05).
Effects of rhuTNFR:Fc on Antibody Production in Control Mice:
To evaluate the role of endogenous TNF in antibody production, TNF activity was
inhibited with rhuTNFR:Fc administered at the time of antigen exposure or throughout
the period of antibody production. Two doses of rhuTNFR:Fc administered 30 min
before antigen exposure were tested in separate studies. There was no statistically
significant alteration in the frequency of PFC/106 spleen cells in animals treated with a
single low dose (100 ,ug/mouse) or single high does (350 gg/mouse) of rhuTNFR:Fc
compared to DPBS treated control mice (Fig. 4.1A). In contrast, when TNF activity was
blocked by the administration of daily i.v. injections of 100 4g rhuTNFR:Fc, a
statistically significant suppression of the PFC response was observed (Fig. 4.1A).
Effects of rhuTNFR:Fc on TCDD-Induced Antibody Suppression:
As expected, in all experiments, exposure to 5,ug TCDD/kg body weight suppressed the
number of PFC /106 spleen cells (compare Fig 4.1A and 4.1B). Unexpectedly, PFC
production was further suppressed in TCDD-exposed mice that were given a single dose
57
of 350,ug rhuTNFR:Fc or five daily injections of 100 ,ug rhuTNFR:Fc (Fig. 4.1B). A
single dose of 100,ug rhuTNFR:Fc did not affect PFC production (Fig 4.1B).
2500
B: TCDDTREATED
k VEHIpLETREATED
J
2000
1500
*
1000
500
DPBS
100
350
100 X 5
DPBS
100
350
100 X 5
rhuirNFR:Fc TREATMENT (ug)
Figure 4.1: The effects of rhuTNFR:Fc on the number of PCF/106 spleen cells generated
in response to i.p. SRBC in vehicle control (A) and TCDD (5 ,ug/kg) exposed (B) mice.
Thirty min prior to antigen exposure, a single dose of 100 pig or 350 jig rhuTNFR:Fc was
administered i.v. In one study, 100 ktg of rhuTNFR:Fc was administered i.v. every 24 h
for a total of 5 doses. PFC were enumerated 5 days following antigen exposure. Data are
presented as means + SE of 6-10 mice per treatment group. Data from vehicle control or
TCDD exposed mice injected with DPBS from 3 separate experiments were not different
and were pooled (N= 24). *P < 0.05 treatment with rhuTNFR:Fc versus DPBS control.
Discussion
TCDD exposure in adult animals produces a profound suppression of the
macrophage- and T cell-dependent antibody response to SRBC (Vecchi, et al., 1980;
Davis and Safe, 1988; Kerkvliet and Brauner, 1990). Although this phenomenon has
been described by many investigators, the cell type(s) targeted by TCDD and the
underlying mechanisms of TCDD-induced antibody suppression remain elusive
(Kerkvliet and Burleson, 1994). The anti-SRBC response depends on the concerted
interactions of antigen-presenting cells (APC), regulatory T cells and B cells. In vivo
58
studies designed to evaluate target cell sensitivity to TCDD have demonstrated an
increased sensitivity of antibody responses to T cell-dependent compared to T cellindependent antigens (Kerkvliet, et al., 1990) suggesting that TCDD may target
regulatory T cells and/or APC. In contrast, ex vivo studies demonstrate that B cells from
TCDD-exposed mice are functionally compromised in in vivo antibody production while
T cells and APC are not (Dooley and Holsapple, 1988; Dooley, et al., 1990). In vitro
studies suggest that TCDD may inhibit the terminal differentiation of B cells via an early
activational event (Luster, et al., 1988; Morris and Holsapple, 1991) possibly increased
tyrosine kinase activity and phosphorylation (Luster, et al., 1988; Morris and Holsapple,
1991; Clark, et al., 1991). The basis for the different responses to TCDD in vivo versus ex
vivo or in vitro has not been established.
Reports from several different laboratories suggest that TCDD toxicity may be
associated with an increase in production or activity of TNF, a potent pro-inflammatory
cytokine produced by many different cell types (Beutler and Cerami, 1989; Vassal li,
1992). Clark et al. (1991) demonstrated a hypersensitivity to endotoxin in C57B1/6 mice
exposed to TCDD, and a corresponding dose-dependent increase in serum TNF levels.
Studies by Taylor et al. (1992) suggest that TNF is a mediator of TCDD toxicity in that
anti-TNF antibodies inhibit the loss of body weight, elevations in serum chemistry values
and mortality associated with acute TCDD toxicity. Alsharif et al. (1994) identified TNF
as playing a critical role in amplifying the oxidative stress-induced tissue injury observed
in TCDD-exposed mice. Masssa et al. (1992) reported that PEC harvested from mice
exposed to increasing i.p. doses of TCDD produce more TNF in culture when stimulated
with LPS than PEC harvested from vehicle control mice. Most recently, we have
demonstrated that TNF activity is involved in mediating the TCDD-induced
hyperinflammatory response to SRBC (Moos, et al., 1994)
.
Based on these observations, we hypothesized that an increase in TNF activity
contributes to TCDD-induced suppression in antibody production in vivo. A TCDDinduced increase in TNF activity could alter the inflammatory cytokine signaling
pathways and subsequently disrupt the immunostimulatory signals required to generate a
59
normal antibody response. To test this hypothesis, we examined the effects of exogenous
TNF and the effects of blocking endogenous TNF on humoral immunity in control and
TCDD-exposed mice. The data presented here suggest that either an increase or a
decrease in TNF activity can alter the number of PFC generated in response to SRBC
antigen.
When mice were given exogenous TNF on a daily basis at a level of 10 or 100 ng,
a statistically significant suppression in the number of PFC was observed. Although
bolus administration of a single cytokine may not reliably mimic a physiologic response,
these results are the first to suggest that increased levels of TNF can suppress antibody
production.
On the other hand, studies using rhuTNFR:Fc indicate that some level of TNF is
required for antibody production. When rhuTNFR:Fc was administered daily to inhibit
TNF activity throughout the course of antibody production, there was a statistically
significant suppression in the number of PFC generated. A similar inhibitory effect on
antibody production was observed in a model of collagen-induced arthritis in mice when
TNF activity was blocked by daily ip administrations of 50,ug rhuTNFR:Fc (Wooley, et
al.,
1993).
TNF has also been shown to be required for IgG secretion by human tonsil B
cells (Rodriquez, et al.,
1993).
Spontaneous IgG secretion by these cells was dependent
on endogenous TNFa and not affected by other cytokines (IL, I a,
IL-1/3, IL-2, IL-3, IL-4,
IFN, TGF-(3 and IL-6). Although the mechanisms whereby TNF supports antibody
production are not clear at this time TNF appears to be critical for tonsil B cell
differentiation (Rodriquez, et al., 1993).
As expected, in this study TCDD exposure had a pronounced suppressive effect
on antibody production. Unexpectedly, coincident treatment with a single high dose or
daily low doses of rhuTNFR:Fc further suppressed rather than normalized the total
number of PFC harvested from the spleens of TCDD-exposed mice. The data suggest
that although the antibody response to SRBC can be influenced by alterations in TNF
activity, TNF does not appear to mediate TCDD-induced suppression of this response.
Apparently, TCDD-induced hyperinflammation and TCDD-induced antibody suppression
60
are not linked mechanistically through an increase in TNF activity as initially
hypothesized. It is unlikely that the lack of anticipated effect of rhuTNFR:Fc in the
present study was due to lack of efficacy of the reagent. This reagent has been shown to
inhibit TNF activity in numerous model systems. In addition, this same reagent
normalizes the TCDD-induced increase in peritoneal cell influx mediated by an increase
in TNF activity (Moos, et al., 1994).
It is possible that TCDD-induced antibody suppression results from increased
expression of an inflammatory mediator(s) other than TNF. Nitric oxide (NO), for
example, has been reported to enhance the inflammatory response and mediate
suppression of the antibody response to SRBC in mice immunized with attenuated
Salmonella typhimurium (Al-Ramadi, et al., 1992; Eisenstein, et al., 1994). However,
when we administered aminoguanidine daily through the 5 day course of antibody
production to inhibit inducible NO synthase (Corbett, et al., 1992; Beckerman, et al.,
1993), there was no effect on the anti-SRBC response in TCDD exposed mice (data not
shown). These findings suggest that NO does not play a role in mediating the TCDD
effects on antibody production in this model.
It is unclear at this time whether the hyperinflammation and the antibody
suppression seen in TCDD-treated mice are independent phenomena or are linked
through some as yet unidentified mechanism. Studies are currently underway in our
laboratory to examine other immunomodulating inflammatory mediators such as
arachidonic acid metabolites (Rifkind, et al., 1990) and IL-1 (Sutter, et al., 1991) that may
be influenced by TCDD exposure and contribute to suppression of the SRBC antibody
response.
61
References
Al-Ramadi, B.K., Meisser, J.J., Huang, D.and Eisenstein, T.K. (1992).
Immunosuppression induced by nitric oxide and its inhibition by interleukin-4.
Eur. J. Immunol. 22, 2249-2254.
Alsharif, N.Z., Hassoun, E., Bagchi, M., Lawson, T. and Stohs, S.J. (1994). The effects of
anti-alpha antibody and dexamethasone on TCDD-induced oxidative stress in
mice. Pharmacology 48, 127-136.
Beckerman, K.P., Rogers, H.W., Corbett, J.A., Schreiber, R.D.,McDaniel, M.L. and
Unanue, E.R. (1993). Release of nitric oxide during the T cell-independent
pathway of macrophage activation: its role in resistance to Listeria
monocytogenes. J. Immunol. 150, 888-895.
Beutler, B. and Cerami, A. (1989) The biology of cachetin/TNF- a primary mediator of
the host response. Annu. Rev. Immunol. 7, 625-655.
Clark, G.C., Taylor, M.J., Tritscher, A.M. and Lucier, G.W. (1991) Tumor necrosis factor
involvement in 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated endotoxin
hypersensitivity in C57B1/6J mice congenic at the Ah locus. Tox. Appl.
Pharmacol. 111, 422-431.
Corbett, J.A., Tilton, R.G., Chang, K., Hasan, K.S., Ido, Y., Wang, J.L., Sweetland, M.A.,
Lancaster, J.R. Williamson, J.R. and Mcdaniel, M.L. (1992). Aminoguanidine, a
novel inhibitor of nitric oxide formation, prevents diabetic vascular dysfunction.
Diabetes 41, 552-556.
Cunningham, A.J. and Szenberg, A. (1968) Further improvements in the plaque technique
for detecting single antibody forming cells. Immunology 14, 599-600.
Davis, D., and Safe, S. (1988). Immunosuppressive activities of polychlorinated
dibenzofuran congeners: Quantitative structure-activity relationships and
interactive effects. Toxicol. Appl. Pharmacol. 94, 141-149.
Dinarello, C.A., Gelfand, J.A. and Wolff, S.M. (1993). Anticytokine strategies in the
treatment of the systemic inflammatory response syndrome. JAMA 269, 1829­
1835.
Eisenstein, T.K., Huang, D., Meissler, J.J. and Al-Ramadi, B. (1994). Macrophage nitric
oxide mediates immunosuppression in infectious inflammation. Immunobiol. 191,
495-502.
62
Gibaldi, M. (1993). What is nitric oxide and why are so many people studying it? J. Clin.
Pharmacol. 33, 488-496.
Green, L.C., Wagner, D.A., Glogowski, J., Skepper, P.L., Wishnok, J.S. and
Tannenbaum, S.R. (1982) Analysis of nitrate, nitrite and [15N]nitrite in biological
fluids. Anal. Biochem. 124, 131.
Holsapple, M.P., Morris, D.L., Wood, S.C. and Snyder, N.K. (1991) 2,3,7,8­
Tetrachlorodibenzo-p-dioxin-induced changes in immunocompetence: possible
mechanisms. Annu. Rev. Pharmacol. Toxicol. 31, 73-100.
House, R.V., Lauer, L.D. and Muarry, M.J. (1990). Examination of immune parameters
and host resistance mechanisms in B6C3F1 mice following adult exposure to
2,3,7,8-tetrachlorodibenzo-p-dioxin. J. Toxicol.Environ. Health 31, 203-215.
lalenti, A., lanaro, A., Moncada, S. and DiRosa, M. (1992) Modulation of acute
inflammation by endogenous nitric oxide. Eur. J. Pharmacol. 211, 177-182.
Kaplan, S.S., Billiar, T.R., Curran, R.D., Zdziarski, U.E., Simmons, R.L. and Basford,
R.E. (1990) Inhibition of chemotaxis with N °- monomethyl- L- arginine: a role for
cyclic GMP. In: Moncada, S., Higgs, A. eds. Nitric oxide from L-arginine: a
bioregulatory system: proceedings of the Symposium on Biological Importance of
Nitric Oxide, London, 1989. Elsevier, Amsterdam 499-500.
Kerkvliet, N.I. (1995) Immunological effects of chlorinated dibenzo-p-dioxins. Environ
Health Perspect 103 (Suppl 9), 47-53.
Kerkvliet, N.I. and Burleson, G.R. (1994) Immunotoxicity of TCDD and related
halogenated aromatic hydrocarbons. In: J.H. Dean, M.I. Luster, A.E. Munson and
I. Kimber (Eds.), Immunotoxicity and Immunopharmacology, Raven Press, Ltd.
New York, pp.97-121.
Kerkvliet, N.I., Steppan, L.B., Brauner, J.A., Deyo, J.A., Henderson, M.C., Tomar, R.S.
and Buhler, D.R. (1990) Influence of the Ah locus on the humoral
immunotoxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin: Evidence for Ah­
receptor-dependent and Ah-receptor-independent mechanisms of
immunosuppression. Toxicol. Appl. Pharmacol. 105, 26-36.
Kerkvliet, N.I. and Brauner, J.A. (1990) Flow cytometric analysis of lymphocyte
subpopulations in the spleen and thymus of mice exposed to an acute
immunosuppressive dose of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD).
Environ. Research 52, 146-154.
63
Kerkvliet, N.I. and Oughton, J.A. (1993) Acute inflammatory response to sheep red blood
cell challenge in mice treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD):
Phenotypic and functional analysis of peritoneal exudate cells. Toxicol. Appl.
Pharmacol. 119, 248-257.
Kubes, P., Suzuki, M. and Granger, D.N. (1991) Nitric oxide: An endogenous modulator
of leukocyte adhesion. Proc. Natl. Acad. Sci. USA 88, 4651-4655.
Lejeune, P., Lagadec, P., Onier, N., Pinard, D., Ohshima, H. and Jeannin, J.F. (1994)
Nitric oxide involvement in tumor-induced immunosuppression. J. Immunol. 152,
5077-5083.
Liew, F.Y. (1994) Regulation of nitric oxide synthesis in infectious and autoimmune
diseases. Immunol. Letters 43, 1-2.
Manthey, C.L., Perera, P., Salkowski, C.A.,and Vogel, S.N. (1993) Taxol provides a
second signal for murine macrophage tumoricidal activity. J. Immunol. 152, 825­
831.
Massa, T., Esmaeili, A., Fortmeyer, H., Schlatterer, B., Hagenmaier, H. and Chandra, P.
(1992) Cell transforming and oncogenic activity of 2,3,7,8-tetrachloro- and 2,3,7,8
tetrabromodibenzo-p- dioxin. Cancer Research 12, 2053-2060.
Miller, M.J.S., Sadowska-Krowicka, H., Chotinaruemol, S., Kakkis, J.L. and Clark, D.A.
(1993) Amelioration of chronic ilieitis by nitric oxide synthase inhibition. J.
Pharmacol. Exper. Therap. 264, 11-16.
Misko, T.P., Moore, W.M., Kasten, T.P., Nickols, G.A., Corbett, J.A., Tilton, R.G.,
McDaniel, M.L., Williamson, J.R. and Currie, M.G. (1993) Selective inhibition of
the inducible nitric oxide synthase by aminoguanidine. J. Pharmacol. 233, 119­
125.
Moncada, S., and Higgs, A. (1993) The L-arginine- nitric oxide pathway. N. Engl. J.
Med. 329, 2002-2012.
Moncada, S., Palmer, R.M.J. and Higgs, E.A. (1991) Nitric oxide: Physiology,
pathophysiology, and pharmacology. Pharmacol. Reviews 43, 109-142.
Moos, A.B., Baecher-Steppan, L. and Kerkvliet, N.I. (1994) Acute inflammatory
response to sheep red blood cells in mice treated with 2,3,7,8-tetrachlorodibenzo­
p-dioxin: The role of the inflammatory cytokines, IL-1 and TNF. Toxicol. Appl.
Pharmacol. 127, 331-335.
64
Moos, A.B., Baecher-Steppan, L. and Kerkvliet, N.I. (1994) Acute inflammatory
response to sheep red blood cells in mice treated with 2,3,7,8-tetrachlorodibenzo­
p-dioxin: The role of proinflammatory cytokines, IL-1 and TNF. Toxicol. Appl.
Pharmacol. 127, 331-335
Peppel, K., Crawford, D. and Beutler, B. (1991) A tumor necrosis factor (TNF) receptorIgG heavy chain chimeric protein as a bivalent antagonist of TNF activity. J. Exp.
Med. 174, 1483-1489.
Rifkind, A.B., Gannon, M., and Gross, S.S. (1990) Arachodonic acid metabolism by
dioxin-induced cytochrome P-450: a new hypothesis on the role of P-450 in
dioxin toxicity. Biochem. Biophys. Res. Comm. 172, 1180-1188.
Rodriquez, C., Roldan, E., Navas, G. and Brieva, J.A. (1993) Essential role of tumor
necrosis factor-a in the differentiation of human tonsil in vivo induced B cells
capable of spontaneous and high-rate immunoglobulin secretion. Eur. J. Immunol.
23, 1160-1164.
Sutter, T.R., Guzman, K., Dold, K.M. and Greenlee, W.F. (1991) Targets for dioxin:
genes for plasminogen activator inhibitor-2 and interleukin-lp. Science 254, 415­
418.
Taylor, M.J., Lucier, G.W., Mahler, J.F., Thompson, M., Lockhart, A.C. and Clark, G.C.
(1992) Inhibition of acute TCDD toxicity by treatment with anti-tumor necrosis
factor antibody or dexamethasone. Toxicol. Appl. Pharmacol. 117, 126-132.
Vassalli, P. (1992) The pathophysiology of tumor necrosis factors. Annu. Rev. Immunol.
10, 411-452.
Vecchi, A., Mantovani, A., Sironi, M., Luini, M., Cairo, M. and Garattini, S. (1980)
Effect of acute exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin on humoral
antibody production in mice. Chem. Biol. Interact. 30, 337-341.
Wooley, P.H., Dutcher, J., Widmer, M.B. and Gillis, S. (1993) Influence of a
recombinant human soluble tumor necrosis factor receptor FC fusion protein on
type II collagen-induced arthritis in mice. J. Immunol. 151, 6602-6607.
65
Chapter Five
The Involvement of Nitric Oxide in TCDD-Induced
Hyperinflammation and Antibody Suppression
AUTHORS:
A.B.Moos
N.I.Kerkvliet
Submitted to Fundamentals and Applied Toxicology
66
Abstract
The current studies were designed to evaluate the role of nitric oxide (NO) in
TCDD-induced alterations in immune function. The effect of TCDD on NO production
(as measured by nitrite formation) was evaluated in stimulated peritoneal exudate cells
(PEC) elicited by thioglycollate (TG) or primed by sheep red blood cells (SRBC). More
NO was produced by both TG-elicited and SRBC-primed PEC harvested from TCDD-
exposed mice compared to PEC harvested from control animals. The role of NO in
TCDD-induced hyperinflammation and antibody suppression was evaluated by inhibiting
cytokine-inducible NO with aminoguanidine (AG). Inhibition of NO by AG did not
appear to alter TCDD-induced hyperinflammation, although the results were complicated
by an apparent proinflammatory effect of AG treatment alone. However, when AG was
used to inhibit NO production during the antibody response, the TCDD-induced
suppression of the anti-SRBC response was partially ameliorated. These results
demonstrate that, following TCDD exposure, PEC are capable of producing more NO
during a peritoneal inflammatory response, and that increased production of NO may
contribute to TCDD-induced suppression in antibody production to SRBC.
Introduction
2,3,7,8-Tetrachlorodibenzo-p-dioxin (TCDD) represents the prototype of a large
group of toxic halogenated aromatic hydrocarbons that are widespread environmental
contaminants. The immunotoxic properties of TCDD are well documented in several
animal species (Holsapple et al., 1991; Kerkvliet and Burleson, 1994, Kerkvliet, 1995).
One of the most sensitive indicators of TCDD immunotoxicity in laboratory animals is a
suppression of the macrophage and T-cell-dependent antibody response to sheep red
blood cells (SRBC) (Vecchi et al., 1980; Davis and Safe, 1988; Kerkvliet and Brauner,
1990). TCDD exposure also results in an enhanced acute inflammatory response
measured by an increase in SRBC-induced peritoneal inflammation (Kerkvliet and
Oughton, 1993; Moos et al., 1994) or an increase in carageenan or dextran-induced paw
edema (Theobald et al., 1983). It is not clear at this time whether the enhanced
67
inflammatory responses and the suppressed antibody responses are linked mechanistically
or whether they are independent immunotoxic events.
The inflammatory process is initiated by endothelial cell activation and involves
the release of a cascade of soluble mediators including tumor necrosis factor (TNF),
interleukin 1 (IL-1), interleukin 8 (IL-8), arachidonic acid (AA) metabolites, platelet
activating factor (PAF) and nitric oxide (NO) (Dinarello et al., 1993). A TCDD-induced
increase in the concentration of, or sensitivity to, one or more of these proinflammatory
mediators could result in an enhancement of the acute inflammatory response. Alteration
in the inflammatory cytokine signaling pathways could disrupt the normal
immunostimulatory signals required to generate an optimal anti-SRBC response leading
to a down-stream suppression of antibody production.
NO is a biologically active compound involved in acute and chronic inflammatory
reactions as well as specific immune responses (Moncada and Higgs, 1993). Produced by
activated macrophages, PMN and endothelial cells, NO plays a critical role in endothelial
cell activation by promoting cytokine-induced vasodilation (Dinarello et al., 1993).
Excessive NO production has been shown to alter T-cell responses (Rowland et al., 1994;
Lejeune et al., 1994) and induce immunosuppression (Liew, 1994). We hypothesized that
in response to TCDD exposure and an appropriate inflammatory stimulus (SRBC), more
NO is produced locally resulting in an enhancement of the inflammatory response and a
subsequent suppression of the splenic antibody response to SRBC. To test this
hypothesis, we examined the effects of TCDD on NO production by peritoneal cells. We
also evaluated the contribution of NO to TCDD-induced hyperinflammation and TCDDinduced antibody suppression by measuring the inflammatory response and antibody
production following treatment with aminoguanidine (AG), an inhibitor of cytokine­
induced NO production (Misko et al., 1993; Corbett et al., 1992).
68
Methods and Materials
Animals:
Female C57B1/6 mice (The Jackson Laboratories, Bar Harbor, ME), 8-10 weeks of age
were used in this study. They were maintained according to NIH guidelines.
TCDD Exposure:
TCDD, obtained from Cambridge Isotope Laboratories, Inc. (Woburn, MA) as a certified
reference standard of >98% purity, was dissolved in anisole and diluted in peanut oil. A
vehicle solution of anisole in peanut oil was prepared similarly (vehicle control). Mice
were given a single dose of TCDD (5 or 20 µg /kg) or vehicle by gavage.
Ex Vivo NO Production in Peritoneal Exudate Cell (PEC) Culture:
NO production was evaluated in PEC elicited by TG or primed by SRBC. Two days
following exposure to 20 µg /kg TCDD, mice were injected ip with 1.5 ml sterile 3% TG
broth or 2.5x108 SRBC. TG-elicited PEC were harvested from the peritoneum 3 days
following injection; SRBC-primed cells were harvested 90 minutes following injection.
Total peritoneal cells and differential cell counts were determined as described (Moos et
al., 1994). PEC (1x106 cells /ml) were maintained at 37°C and 5% CO2 in DMEM with
5% FBS for 2 hours before being stimulated with 50 U IFNy (Pharmingen, San Diego,
CA) or LPS (E. Coli serotype 026:B6, Sigma, St. Louis, MO) for 48 hours. Supernatants
were collected 48 hours following stimulation and stored at -70°C until evaluated for NO
production.
The colorimetric Greiss reaction (Green et al., 1982) was used to assay culture
supernatants for nitrite (NO2), a stable oxidative metabolite of NO (Rowland et al.,1994;
Al-Ramadi et al., 1992; Beckerman et al., 1993). Briefly, 50 41 aliquots of supernatant
were mixed with an equal volume of Griess reagent (1.32% sulfanilamide in 60% acetic
acid, 0.1% N-1-naphthyl-ethylenediamine-HC1), (Sigma, St. Louis, MO) and incubated at
room temperature for 10 minutes. The absorbance at 562nm was measured in an
automated microtiter plate reader. NO2- was quantitated using NaNO2 as a standard.
69
Inhibition of NO Activity during SRBC-induced Inflammation:
The peritoneal inflammatory response to SRBC was measured in TCDD or vehicle
exposed mice treated with AG or DPBS. Fifty-six hours following exposure to 20 ,ug
TCDD/kg or vehicle mice were sensitized with ip SRBC (2.5x108). PEC were harvested
18 hours following SRBC injection. Either 501.tg AG/kg or an equal volume of DPBS
was injected ip every 12 hours throughout this period beginning 24 hours after exposure
to TCDD or vehicle. A total of 5 injections of AG were given.
Inhibition of NO Activity during the Anti-SRBC Antibody Response:
The splenic plaque forming cell (PFC) response was measured in TCDD-treated and
vehicle control mice sensitized with SRBC and treated with AG or DPBS. SRBC
(2.5x108) were injected ip 48 hours following exposure to 51.1g TCDD/kg or vehicle.
Beginning 24 hours after exposure to TCDD, mice were dosed with 50 1,1g AG/ kg or an
equal volume of DPBS every 12 hours for a total of 6 doses. This was followed by 2
doses of 3 mg AG/mouse or DPBS given once every 24 hours (Beckerman et al., 1993;
personal communication Howard W. Rogers). Five days following antigen sensitization,
PFC were enumerated (Cunningham and Szenberg, 1968; Moos and Kerkvliet, 1995) and
treatment groups were compared.
Statistical Analysis:
The Student's t test was used to analyze data for statistical significance. In all analyses,
p<0.05 was considered statistically significant.
Results
The Effect of TCDD on TG-elicited PEC:
As shown in Table 5.1, TCDD exposure resulted in a statistically significant increase in
the total numbers of TG-elicited cells and in the relative and absolute numbers of PMN
harvested from the peritoneum.
70
Table 5.1. Effect of TCDD on Thioglycollate-elicited PECa
PEC x 106
PMN x 106
% PMN
Control
21.4 (2.2)
1.6 (0.9)
7 (3.5)
TCDD
31.5 (4.2)*
7.1 (0.7)*
22.6 (2.5)*
Treatment'
a) Data are presented as means (SE) of 3 mice per treatment group.
b) Mice were injected with 1.5 ml sterile TG broth 2 days following exposure to 2Oug/kg
TCDD or vehicle. TG-elicited PEC were harvested from the peritoneum 3 days following
TG injection. Total peritoneal cells were enumerated on a Coulter counter and differential
cell counts were determined following cytocentrifugation and staining with Gugol blue.
*p <0.05
NO Production by PEC:
Table 5.2 summarizes the effects of TCDD exposure on NO production by PEC. TGelicited PEC demonstrated an LPS-dose responsive increase in NO production following
stimulation. When stimulated with the higher doses of LPS (0.10 lag and 1.0 lig), PEC
harvested from mice exposed to TCDD produced significantly more NO than cells
harvested from control animals. Very low levels of NO were measured in cultures of
SRBC-primed PEC in response to stimulation with LPS or IFNy (Table 5.2). In spite of
these low levels, SRBC-primed PEC from mice exposed to TCDD produced significantly
more NO than cells from control mice in response to LPS or IFNy.
71
Table 5.2. Effect of in vivo Exposure to TCDD on ex vivo Production of NO by PECa
Vehicle
TCDD
NO2-(nM)
TG-elicited PECK
0 ng LPS
10 ng LPS
100 ng LPS
1000 ng LPS
0.19 (0.01)
3.53 (0.6)
3.70 (0.5)
4.59 (0.6)
0.19 (0.02)
5.10 (0.9)
6.20 (1.1)*
7.40 (0.7)*
0.011 (0.002)
0.205 (0.11)
0.088 (0.002)*
1.69 (0.15)*
SRBC-primed PE('
1000 ng LPS
50 U IFNy
a) Data are presented as means (SE) of 3 mice per treatment group.
b) Mice were injected i.p. with 1.5 ml sterile TG broth 2 days following exposure by
gavage to 20 ug/kg TCDD or vehicle. PEC were harvested 3 days following TG injection.
TG-elicited PEC (1x106 cells /ml) were maintained at 37°C and 5% CO2 in DMEM with
5% FBS for 2 hours before being stimulated with LPS. Supernatants were collected after
48 hours and stored at -70 C until evaluated for NO production.
c) Mice were injected i.p. with 2.5x108 SRBC 2 days following exposure to 20 ug/kg
TCDD or vehicle. SRBC-primed PEC were harvested 90 minutes following injection, and
maintained (1x106 cells/m1) at 37°C and 5% CO2 in DMEM with 5% FBS for 2 hours
before being stimulated with IFNy or LPS. Supernatants were collected 48 hours later
and stored at -70°C until evaluated for NO production.
* p <0.05 TCDD treatment versus vehicle.
Influence of AG on TCDD-induced Enhancement of the Anti-SRBC Inflammatory
Response:
Consistent with earlier reports (Kerkvliet and Oughton, 1992; Moos et al., 1994),
exposure to TCDD resulted in an increase in total cell number as well as an increase in
the relative and absolute numbers of PMN harvested from the peritoneum following
SRBC-induced inflammation (Table 5.3). In order to examine the role of NO in this
process, AG was administrated to inhibit cytokine-inducible NO synthase (iNOS)
72
throughout the inflammatory response. This resulted in an unexpected increase in the
relative number of PMN harvested from control mice and a further increase in the
absolute and relative numbers of PMN harvested from TCDD-exposed mice (Table 5.3).
Table 5.3 Effect of AG on SRBC-induced PEC in Vehicle and TCDD-exposed Micea
Treatment'
PEC x 106
PMN x 106
% PMN
Vehicle + DPBS
6.36 (1.3)
1.55 (0.4)
22.2 (3.3)
Vehicle + AG
5.65 (0.6)
1.95 (0.4)
33.3 (4.4)**
TCDD + DPBS
8.44 (1.3)
3.57 (0.7)*
41.2 (2.6)*
TCDD + AG
10.64 (0.9)
5.53 (0.9)**
52.0 (3.3)**
a) Data are presented as the mean (SE) of 8 mice per treatment group.
b) Mice were sensitized with ip SRBC (2.5x108) two days following exposure by gavage
to 20 ug/kg TCDD or vehicle and SRBC-elicited PEC were harvested 18 hours after
injection. Either 50 ug AG/kg or an equal volume of DPBS was injected ip every 12
hours throughout this period beginning 24 hours after exposure to TCDD (24 hours prior
to exposure to SRBC). A total of 5 injections of AG or DPBS were administered. SRBCelicited PEC were enumerated using a coulter counter and differential cells counts were
determined following cytocentrifugation and staining with Gugol blue.
* p<0.05 TCDD versus vehicle.
* * p<0.05 AG treatment versus respective DPBS treatment.
Influence of AG on TCDD-induced Suppression of the Anti-SRBC Antibody Response:
Similar to previous studies, (Kerkvliet et al., 1990; Moos and Kerkvliet, 1995) exposure
to TCDD suppressed the anti-SRBC antibody response (Fig. 5.1B and 5.1C), but did not
alter spleen cell number (Kerkvliet et al., 1990) (Fig. 5.1A). In TCDD-exposed animals,
administration of AG resulted in a trend towards an increase in spleen cellularity (Fig.
73
5.1A) and a statistically significant increase in the total number of PFC generated/spleen
(Fig. 5.1C). These parameters were not affected by AG treatment in control mice. AG
treatment did not alter the concentration of PFC in spleens (PFC/106 spleen cells) in
either TCDD-exposed or control mice (Fig. 5.1B).
74
I
O
100
X
80
C
1500
CD
(1)
T)
-CT)
0
,
CD
60
-6­
U)
40
a)
1000
0
500
20
LL
CL
I
12000
1
Vehicle + DPBS
Vehicle + AG
® TCDD + DPBS
10000
8000
TCDD+ AG
**
6000
4000
2000
Figure 5.1. The effects of AG on spleen cell recovery (A), number of PFC/10° spleen
cells (B) and the number of PFC/spleen © generated in response to ip SRBC in TCDD (5
µg /kg) and vehicle exposed mice. AG (50 pg/kg) was administered ip every 12 hours
starting 1 day before antigen exposure for a total of 6 doses followed by 2 daily doses of
3 [tg AG/mouse. Spleen cells were harvested and PFC were enumerated 5 days following
antigen exposure. Data are presented as means (SE) of 8 mice per treatment group.
*p<0.05 TCDD versus control. **p<0.05 AG treatment versus respective DPBS control.
(Statistical comparisons were not made between TCDD-exposed mice treated with AG
and vehicle control mice treated with AG).
75
Discussion
Several reports (Clark et al., 1991; Taylor et al., 1992; Massa et al., 1992; Alsharif
et al., 1994), have suggested that TCDD toxicities may be associated with an increase in
production or activity of TNF a potent proinflammatory cytokine produced by many
different cell types (Beutler and Cerami, 1989; Vassalli, 1992; Tracey and Cerami, 1993).
Studies in our laboratory have shown that TNF is a critical mediator in the TCDDinduced hyperinflammatory response to SRBC (Moos et al., 1995) but TNF does not
appear to be involved in TCDD-induced suppression of the anti-SRBC response (Moos
and Kerkvliet, 1995). It is possible that the TCDD-induced hyperinflammation and
antibody suppression are linked mechanistically through increased expression of other
inflammatory mediators involved in the process of endothelial cell activation. We
considered NO to be a likely candidate for mediating these responses for the following
reasons. NO is produced by macrophages (MAC) as well as PMN and endothelial cells
in response to TNF during the acute inflammatory reaction (Moncada and Higgs, 1993)
and plays a critical role in vascular dilatation during endothelial cell activation (Dinarello
et al., 1993). In addition. NO has been shown to mediate the suppression of the splenic
antibody response to SRBC in mice immunized with attenuated aro A- mutants of
Salmonella typhimurium (Al-Ramadi et al., 1992; Eisenstein et al., 1994).
NO is synthesized from L-arginine by a family of enzymes, the nitric oxide
synthases. The constitutive isoform of NO synthase (NOS) is Ca' dependent and
produces small amounts of NO which mediate endothelium-dependent relaxation and
neural transmission (Corbett et al., 1992;Moncada and Higgs, 1993). Larger amounts of
NO are produced by the cytokine-inducible form of NO synthase which is Ca'­
independent (Corbett et al., 1992; Moncada and Higgs, 1993). The NO produced by the
inducible enzyme mediates the cytotoxic activity of MAC on target cells and the vascular
dilatation characteristic of acute inflammation (Moncada and Higgs, 1993).
To evaluate the effects of TCDD on NO production, we compared nitrite
production in cultures of TG-activated and SRBC-primed PEC harvested from TCDD-
exposed and control mice. Following TCDD exposure, there was an increase in the
76
magnitude of the cellular inflammatory response to TG as measured by an increase in the
total number of PEC as well as an increase in the absolute and relative numbers of PMN
harvested from the peritoneum. Consistent with an earlier report by House et al., (1990)
there was no difference between groups in the absolute or relative numbers peritoneal
MAC elicited by TG. A TCDD-induced neutrophilic response has also been observed
following SRBC-induced peritoneal inflammation (Kerkvliet and Oughton, 1993; Moos
et al., 1994) and suggests that TCDD exposure may increase neutrophil chemotaxic
signals or PMN endothelial cell interactions.
The ability of PEC to produce NO in response to an inflammatory stimulus
depends in part on the degree of priming or stage of activation (Rutherford et al., 1993;
Manthey et al., 1993). In this study, for example, TG-elicited PEC produced significant
quantities of NO, while NO was not detected in cultures of resident peritoneal cells
stimulated with LPS or SRBC (data not shown) and only very low levels of NO were
produced by SRBC-primed PEC stimulated with LPS or IFNy. The low levels of NO
measured in cultures of SRBC-primed cells may be due in part to a buffering action of the
SRBC. Oxyhemoglobin binds NO with high affinity (Moncada et al., 1991) and
detectable levels of NO are decreased by adding increasing concentrations of SRBC to
spleen cell cultures (Al-Ramadi et al., 1992). Regardless of the magnitude of the
response, PEC harvested from mice exposed to TCDD produced significantly more NO
than cells harvested from control mice. The mechanisms involved in the TCDD-induced
increase in NO production are not yet identified. Regulation of NO secretion appears to
be primarily at the level of transcription of the iNOS gene (Xie et al., 1992) but at this
time, it is not yet known if TCDD exposure directly affects this transcriptional process.
The capability of PEC from TCDD-exposed mice to produce more NO in
response to an inflammatory stimulus led us to hypothesize that an increase in NO
contributes to the enhanced inflammatory response observed following ip sensitization
with SRBC. NO has been shown to play a critical role in both acute and chronic
inflammatory processes (Moncada and Higgs, 1993) and in vivo treatment with inhibitors
of NO have been shown to reduce the inflammatory response in several animal models,
77
(Ialenti et al., 1992; Mulligan et al., 1991; and Miller et al., 1993). The direct effects of
NO on neutrophil chemotaxis and recruitment, however, are debated, and both
enhancement (Kaplan et al., 1990) and inhibition (Kubes et al., 1991) of neutrophil
migration by NO have been reported. To evaluate the role of NO in TCDD-induced
hyperinflammation, we measured the peritoneal inflammatory response to SRBC
following inhibition of iNOS with AG, a compound structurally related to L-arginine.
Based on cellular responses, organ culture studies and enzyme-based measurements, AG
has been shown to be equipotent to other inhibitors of iNOs but 10 to 100-fold less potent
an inhibitor of the constitutive isoform of NOS (Misko et al., 1992). In vivo treatment
with AG selectively inhibits iNOS and results in minimal alterations in the homeostatic
mechanisms attributed to constituitively produced NO (Corbet et al., 1992; Misko et al.,
1993; Gibaldi, 1993).
Based on our hypothesis that the increase in NO produced in TCDD-exposed mice
contributes to the enhanced inflammatory response observed following injection with
SRBC, we anticipated that inhibition of iNOS would decrease or normalize the degree of
inflammation measured in these mice. Treatment with AG throughout the inflammatory
response to SRBC, however, had the unexpected effect of increasing, rather than
reducing, the number of PMNs harvested from the peritoneum in both control and TCDD
exposed animals. AG itself appears to have proinflammatory properties resulting in an
enhancement of the neutrophilic response to SRBC.
The role of NO in TCDD-induced antibody suppression was also evaluated using
AG. Daily administration of AG throughout the course of the primary antibody response
to SRBC resulted in a trend towards an increase in spleen cellularity in TCDD-exposed
mice, although the numbers among treatment groups were not statistically different. In
addition, AG treatment did not significantly alter the concentration of PFC in the spleen.
However, the total number of PFC per spleen was significantly increased in TCDDexposed mice treated with AG suggesting that inhibition of iNOS can reverse the
antibody suppression observed in these animals. In non- AG treated animals, TCDDexposure suppressed the antibody response by 65% whereas in AG treated mice, TCDD
78
suppressed the response by only 23%. The potential for excess NO to suppress the antiSRBC response has previously been demonstrated by Al-Ramadi et al. (1992). These
investigators observed that mice immunized with attenuated Salmonella mutants were
protected against virulent Salmonella challenge but were unable to mount antibody
responses to non-Salmonella antigens including SRBC. Suppressed antibody production
in these mice correlated with high levels of NO and was reversed when NO production
was inhibited.
Although increased NO activity appears to contribute to the suppression of the
anti-SRBC response by TCDD, the mechanism whereby excess NO suppresses antibody
production is not known. One hypothesis that has been proposed is that increased
amounts of NO produced by macrophages in response to an inflammatory stimulus
`poison' lymphocytes in the vicinity of the activated macrophages. The resulting
cytostasis of the proximal lymphocytes renders them ineffective in participating in the
antibody response (Eisenstein et al., 1994). The lack of total restoration of the antibody
response by AG in TCDD-exposed mice may indicate that not all inducible NO was
inhibited or that more than one mechanism contributes to antibody suppression in this
model.
To the best of our knowledge, this is the first reported examination of the effects
of TCDD on NO production and evaluation of the role of NO in TCDD-induced
immunotoxicities. It remains to be determined if TCDD directly alters NO production by
enhancing expression of iNOS or if TCDD affects NO production by some other, indirect
mechanism.
79
References
Al-Ramadi, B.K., Meisser, II, Huang, D.and Eisenstein, T.K. (1992).
Immunosuppression induced by nitric oxide and its inhibition by interleukin-4.
Eur. .1. Immunol. 22, 2249-2254.
Alsharif, N.Z., Hassoun, E., Bagchi, M., Lawson, T. and Stohs, S.J. (1994). The effects of
anti-alpha antibody and dexamethasone on TCDD-induced oxidative stress in
mice. Pharmacology 48, 127-136.
Beckerman, K.P., Rogers, H.W., Corbett, J.A., Schreiber, R.D.,McDaniel, M.L. and
Unanue, E.R. (1993). Release of nitric oxide during the T cell-independent
pathway of macrophage activation: its role in resistance to Listeria
monocytogenes. J. Immunol. 150, 888-895.
Beutler, B. and Cerami, A. (1989) The biology of cachetin/TNF- a primary mediator of
the host response. Annu. Rev. Immunol. 7, 625-655.
Clark, G.C., Taylor, M.J., Tritscher, A.M. and Lucier, G.W. (1991) Tumor necrosis factor
involvement in 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated endotoxin
hypersensitivity in C57B1/6J mice congenic at the Ah locus. Tox. Appl.
Pharmacol. 111, 422-431.
Corbett, J.A., Tilton, R.G., Chang, K., Hasan, K.S., Ido, Y., Wang, J.L., Sweetland, M.A.,
Lancaster, J.R. Williamson, J.R. and Mcdaniel, M.L. (1992). Aminoguanidine, a
novel inhibitor of nitric oxide formation, prevents diabetic vascular dysfunction.
Diabetes 41, 552-556.
Cunningham, A.J. and Szenberg, A. (1968) Further improvements in the plaque
technique for detecting single antibody forming cells. Immunology 14, 599-600.
Davis, D., and Safe, S. (1988). Immunosuppressive activities of polychlorinated
dibenzofuran congeners: Quantitative structure-activity relationships and
interactive effects. Toxicol. Appl. Pharmacol. 94, 141-149.
Dinarello, C.A., Gelfand, J.A. and Wolff, S.M. (1993). Anticytokine strategies in the
treatment of the systemic inflammatory response syndrome. JAMA 269, 1829­
1835.
Eisenstein, T.K., Huang, D., Meissler, J.J. and Al-Ramadi, B. (1994). Macrophage nitric
oxide mediates immunosuppression in infectious inflammation. Immunobiol. 191,
495-502.
80
Gibaldi, M. (1993). What is nitric oxide and why are so many people studying it? J. Clin.
Pharmacol. 33, 488-496.
Green, L.C., Wagner, D.A., Glogowski, J., Skepper, P.L., Wishnok, J.S. and
Tannenbaum, S.R. (1982) Analysis of nitrate, nitrite and rNinitrite in biological
fluids. Anal. Biochem. 124, 131.
Holsapple, M.P., Morris, D.L., Wood, S.C. and Snyder, N.K. (1991) 2,3,7,8­
Tetrachlorodibenzo-p-dioxin-induced changes in immunocompetence: possible
mechanisms. Annu. Rev. Pharmacol. Toxicol. 31, 73-100.
House, R.V., Lauer, L.D. and Muarry, M.J. (1990). Examination of immune parameters
and host resistance mechanisms in B6C3F1 mice following adult exposure to
2,3,7,8-tetrachlorodibenzo-p-dioxin. J. Toxicol.Environ. Health 31, 203-215.
Ialenti, A., Ianaro, A., Moncada, S. and Di Rosa, M. (1992) Modulation of acute
inflammation by endogenous nitric oxide. Eur. J. Pharmacol. 211, 177-182.
Kaplan, S.S., Billiar, T.R., Curran, R.D., Zdziarski, U.E., Simmons, R.L. and Basford,
R.E. (1990) Inhibition of chemotaxis with NG-monomethyl-L-arginine: a role for
cyclic GMP. In: Moncada, S., Higgs, A. eds. Nitric oxide from L-arginine: a
bioregulatory system: proceedings of the Symposium on Biological Importance of
Nitric Oxide, London, 1989. Elsevier, Amsterdam 499-500.
Kerkvliet, N.I. (1995) Immunological effects of chlorinated dibenzo-p-dioxins. Environ
Health Perspect 103 (Suppl 9), 47-53.
Kerkvliet, N.I. and Burleson, G.R. (1994) Immunotoxicity of TCDD and related
halogenated aromatic hydrocarbons. In: J.H. Dean, M.I. Luster, A.E. Munson and
I. Kimber (Eds.), Immunotoxicity and Immunopharmacology, Raven Press, Ltd.
New York, pp.97-121.
Kerkvliet, N.I., Steppan, L.B., Brauner, J.A., Deyo, J.A., Henderson, M.C., Tomar, R.S.
and Buhler, D.R. (1990) Influence of the Ah locus on the humoral
immunotoxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin: Evidence for Ah­
receptor-dependent and Ah-receptor-independent mechanisms of
immunosuppression. Toxicol. Appl. Pharmacol. 105, 26-36.
Kerkvliet, N.I. and Brauner, J.A. (1990) Flow cytometric analysis of lymphocyte
subpopulations in the spleen and thymus of mice exposed to an acute
immunosuppressive dose of 2,3,7,8- tetrachlorodibenzo-p-dioxin (TCDD).
Environ. Research 52, 146-154.
81
Kerkvliet, N.I. and Oughton, J.A. (1993) Acute inflammatory response to sheep red blood
cell challenge in mice treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD):
Phenotypic and functional analysis of peritoneal exudate cells. Toxicol. Appl.
Pharmacol. 119, 248-257.
Kubes, P., Suzuki, M. and Granger, D.N. (1991) Nitric oxide: An endogenous modulator
of leukocyte adhesion. Proc. Natl. Acad. Sci. USA 88, 4651-4655.
Lejeune, P., Lagadec, P., Onier, N., Pinard, D., Ohshima, H. and Jeannin, J.F. (1994)
Nitric oxide involvement in tumor-induced immunosuppression. J. Immunol. 152,
5077-5083.
Liew, F.Y. (1994) Regulation of nitric oxide synthesis in infectious and autoimmune
diseases. Immunol. Letters 43, 1-2.
Manthey, C.L., Perera, P., Salkowski, C.A.,and Vogel, S.N. (1993) Taxol provides a
second signal for murine macrophage tumoricidal activity. J. Immunol. 152, 825­
831.
Massa, T., Esmaeili, A., Fortmeyer, H., Schlatterer, B., Hagenmaier, H. and Chandra, P.
(1992) Cell transforming and oncogenic activity of 2,3,7,8-tetrachloro- and
2,3,7,8 tetrabromodibenzo-p- dioxin. Cancer Research 12, 2053-2060.
Miller, M.J.S., Sadowska-Krowicka, H., Chotinaruemol, S., Kakkis, J.L. and Clark, D.A.
(1993) Amelioration of chronic ilieitis by nitric oxide synthase inhibition. J.
Pharmacol. Exper. Therap. 264, 11-16.
Misko, T.P., Moore, W.M., Kasten, T.P., Nickols, G.A., Corbett, J.A., Tilton, R.G.,
McDaniel, M.L., Williamson, J.R. and Currie, M.G. (1993) Selective inhibition of
the inducible nitric oxide synthase by aminoguanidine. J. Pharmacol. 233, 119­
125.
Moncada, S., and Higgs, A. (1993) The L-arginine- nitric oxide pathway. N. Engl. J.
Med. 329,2002-2012.
Moncada, S., Palmer, R.M.J. and Higgs, E.A. (1991) Nitric oxide: Physiology,
pathophysiology, and pharmacology. Pharmacol. Reviews 43, 109-142.
Moos, A.B., Baecher-Steppan, L. and Kerkvliet, N.I. (1994) Acute inflammatory
response to sheep red blood cells in mice treated with 2,3,7,8-tetrachlorodibenzo­
p-dioxin: The role of the inflammatory cytokines, IL-1 and TNF. Toxicol. Appl.
Pharmacol. 127, 331-335.
82
Moos, A.B. and Kerkvliet, N.I. (1995) Inhibition of tumor necrosis factor activity fails to
restore 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD)- induced suppression of the
antibody response to sheep red blood cells. Tox. Letters 81, 175-181.
Mulligan, M.S., Hevel, J.M., Marletta, M.A., and Ward, P.A.(1991) Tissue injury caused
by deposition of immune complexes is L-arginine dependent. Proc. Natl. Acad.
Sci. USA 88, 6338-6342.
Rowland, R.R.R., Butz, E.A., and Plagemann, P.G.W. (1994) Nitric oxide production by
splenic macrophages is not responsible for T cell suppression during acute
infection with lactate dehydrogenase-elevating virus. J. Immunol. 152, 5785­
5795.
Rutherford, M.S., Witsell, A. and Schook, L.B. (1993) Mechanisms generating
functionally heterogenous macrophages: chaos revisited. J. Leukoc.Biol. 53, 602­
618.
Taylor, M.J., Lucier, G.W., Mahler, J.F., Thompson, M., Lockhart, A.C. and Clark, G.C.
(1992) Inhibition of acute TCDD toxicity by treatment with anti-tumor necrosis
factor antibody or dexamethasone. Tox. Appl. Pharmacol. 117, 126-132.
Theobald, H.M., Moore, R.W., Katz, L.B., Pieper, R.O. and Peterson, R.E. (1983)
Enhancement of carrageenan and dextran-induced edemas by 2,3,7,8­
tetrachlorodibenzo-p-dioxin and related compounds. J. Pharmacol. Exp.Therap.
225, 576-583.
Tracey, K.J. and Cerami, A. (1993) Tumor necrosis factor, other cytokines and disease.
Annu. Rev. Cell Biol. 9, 317-343.
Vassalli, P. (1992) The pathophysiology of tumor necrosis factors. Annu. Rev. Immunol.
10, 411-452.
Vecchi, A., Mantovani, A., Sironi, M., Luini, M., Cairo, M.and Garattini, S. (1980) Effect
of acute exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin on humoral antibody
production in mice. Chem. Biol. Interact. 30, 337-341.
Xie Q., Cho, H.J. Calaycay, J. Mumford, R.A., Swiderek, K.M., Lee, T.D., Ding, A.,
Troso, T. and Nathan, C. (1992) Cloning and characterization of inducible nitric
oxide synthase from mouse macrophages. Science 256, 225-228.
83
Chapter Six
Conclusions
Exposure to TCDD has been shown to enhance the peritoneal inflammatory
response to intraperitoneal SRBC. An increase in both the relative and absolute numbers
of neutrophils harvested from the peritoneum has been reported following ip SRBC in
mice pretreated with TCDD. The studies described here focus in general on the effects of
TCDD exposure on the acute inflammatory response and address the question of whether
TCDD-induced hyperinflammation is linked mechanistically to TCDD-induced antibody
suppression. More specifically, the role of specific inflammatory mediators in TCDDinduced hyperinflammation and the effects of cytokine dysregulation on downstream
antibody production were evaluated.
We hypothesized that TCDD exposure increases the activity of one or more
proinflammatory mediators resulting in an enhanced inflammatory response to SRBC.
Results from these studies demonstrate that TCDD exposure can alter levels of
proinflammatory mediators. Pre-exposure to TCDD resulted in an increase in circulating
levels of TNF in mice as well as an increase in TNF secretion from ex vivo peritoneal
cells and a peritoneal macrophage cell line stimulated in culture. Studies using specific
TNF inhibitors demonstrated that TNF activity is important in supporting the TCDD-
induced hyperinflammatory response. Inhibition of TNF activity in TCDD treated mice
reduced the inflammatory response to control levels but had little effect on the
inflammatory response in vehicle mice. A TCDD effect on TNF activity and production
has been described in multiple studies in different model systems, (Clark et al., 1991;
Taylor et al., 1992; Massa et al., 1992; Alsharif et al., 1994; Olnes et al., 1994; Vogel and
Abel, 1995; Gollapudi et al., 1996), although a recent report targeting TCDD specific
DRE sequences in human and murine genes failed to identify a DRE in the TNF specific
DNA (Lai et al., 1996; Chemico-Biolical Interactions 100:97-112). These findings
suggest that TCDD may have a post-transcriptional effect on TNF production, possibly
influencing the rate of translation or stability of TNF mRNA (Tracey and Cerami, 1993).
84
TCDD exposure also resulted in an increase in NO production by activated
peritoneal cells measured ex vivo or in vitro. Inhibition of NO activity in vivo, however,
did not appear to affect the TCDD-induced hyperinflammatory response. Although these
results suggest that NO does not play an active role in this process, these studies were
complicated by an apparent proinflammatory effect of aminoguanidine, the reagent used
to inhibit NO production. The effects of TCDD exposure on NO synthase, which
regulates NO production have not been clearly identified, but studies are currently
underway in our laboratory to examine the effects of TCDD-exposure on NO synthase
expression. To the best of our knowledge, no DRE has yet been identified in the NOS or
iNOS gene.
We hypothesized that TCDD-induced hyperinflammation and TCDD-induced
antibody suppression are linked mechanistically through an increase in level and/or
activity of one or more proinflammatory mediators. To test this hypothesis, specific
inhibitors of TNF and NO were used and the effects of these inhibitors on TCDD-induced
antibody suppression were evaluated. Results from Rodriquez et al. (1993) suggest that
TNF is critical for IgG secretion and that alterations in TNF activity can influence
antibody production (Wooley et al., 1993), but studies here demonstrate that an increase
in TNF production does not contribute to the TCDD-induced antibody suppression to
SRBC. Increased levels of NO, however, do appear to play a role in TCDD-induced
antibody suppression. When NO production was inhibited in TCDD-exposed mice, the
anti-SRBC response as measured by the total number of PFC generated per spleen, was
partially restored to control values. Inhibition of NO production had no effect on the antiSRBC response in vehicle-treated mice.
We conclude from these studies that the enhancement of the inflammatory
response by TCDD is not linked mechanistically to the suppression of the antibody
response through either an increase in TNF activity or an increase in NO production.
Either these two immunomodulating effects of TCDD exposure are mechanistically
independent events, or there is an as yet unidentified upstream mediator altered by
TCDD-exposure that affects both the inflammatory response and the SRBC antibody
85
response. A potential candidate for such an upstream event is a TCDD-induced increase
in production of AA metabolites. These oxygenated eicosanoids, enzymatically derived
from membrane AA by cyclooxygenase, lipoxygenase, or P450 activity, are critical
mediators in endothelial cell activation and acute inflammation. Certain eicosanoids have
been shown to increase in response to TCDD exposure and increased activity of HETEs
and EETs has been linked to TCDD toxicities in the chick embryo model (Rifkind et al.,
1990). Studies in our laboratory have demonstrated that AA metabolites do not play an
active role in TCDD-induced suppression of the CTL response, but the role of these
compounds in TCDD-induced hyperinflammation and antibody suppression has not yet
been addressed.
86
References
Ackerman, M.F., Gasiewicz, T.A., Lamm, K.R., Germolec, D.R., Luster, M.I. (1989)
Selective inhibition of polymorphonuclear neutrophil activity by 2,3,7,8­
tetrachlorodibenzo-p-dioxin. Toxicol. Appl. Pharmacol. 101: 470-480.
Al-Ramadi, B.K., Meisser, J.J., Huang, D.and Eisenstein, T.K. (1992)
Immunosuppression induced by nitric oxide and its inhibition by interleukin-4.
Eur. J. Immunol. 22: 2249-2254.
Alsharif, N.Z., Hassoun, E., Bagchi, M., Lawson, T. and Stohs, S.J. (1994) The effects of
anti-alpha antibody and dexamethasone on TCDD-induced oxidative stress in
mice. Pharmacology 48: 127-136.
Arend, W.P. (1991) Interleukin 1 Receptor Antagonist - A new member of the Interleukin
1 family. J. Clin. Invest. 88: 1445-1451
Ashkenazi, A., Marsters, S.A., Capon, D.J., Chamow, S.M., Figari, I.S., Pennica, D.,
Goeddel, D.V., Palladino, M.A., Smith, D.H. (1991) Protection against endotoxic
shock by a tumor necrosis factor receptor immunoadhesion. Proc. Natl. Acad.
Sci. USA 99: 10535-10539
Barnes, P.J. and Liew, F.Y. (1995) Nitric Oxide and asthmatic inflammation.
Immunology Today
Beckerman, K.P., Rogers, H.W., Corbett, J.A., Schreiber, R.D.,McDaniel, M.L. and
Unanue, E.R. (1993) Release of nitric oxide during the T cell-independent
pathway of macrophage activation: its role in resistance to Listeria
monocytogenes. J. Immunol. 150: 888-895.
Bemelmans, M.H.A., Gouma, D.J., and Buurman, W.A. (1993) Influence of nephrectomy
on tumor necrosis factor clearance in a murine model. J. Immunol. 150: 2007­
2017.
Beutler, B. and Cerami, A. (1989) The biology of cachetin/TNF- a primary mediator of
the host response. Annu. Rev. Immunol. 7: 625-655.
Birnbaum, L.S. (1994) The Mechanism of dioxin toxicity: relationship to risk assessment.
Environ. Health Perspect 102 (Suppl 9): 157-167
Brewster, D.W. and Matsumura, F. (1989) Differential effect of 2,3,7,8­
tetrachlorodibenzo-p-dioxin on adipose tissue lipoprotein lipase activity in the
guinea pig, rat, hamster, rabbit and mink. Comp Biochem Physiol 93: 49-53.
87
Clark, G.C., Bland, J.A., Germolec, D.R., Luster, M.I. (1991) 2,3,7,8­
Tetrachlorodibenzo-p-dioxin stimulation of tyrosine phosphorylationin B
lymphocytes: potential role in immunosuppression. Mol. Pharmacol 39: 495-501.
Clark, G.C., Taylor, M.J., Tritscher, A.M. and Lucier, G.W. (1991) Tumor necrosis factor
involvement in 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated endotoxin
hypersensitivity in C57B1/6J mice congenic at the Ah locus. Tox. Appl.
Pharmacol. 111: 422-431.
Clark, G.C., Lucier, G., Luster, M., Thompson, M., Mahler, J., and Taylor, M. (1991a)
Tumor necrosis factor (TNF) antibodies and dexamethasone (DEX) treatment
reverse the acute toxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD).
Toxicologist 11: 37. [Abstract 53]
Coligan, J.E., Kruisbeck, A.M., Margulies, D.H., Shevach, E.M. and Strober, W. (eds.)
(1992) Current Protocols in Immunology, pp. 3.15.4-3.15.5. John Wiley & Sons,
New York.
Corbett, J.A., Tilton, R.G., Chang, K., Hasan, K.S., Ido, Y., Wang, J.L., Sweetland, M.A.,
Lancaster, J.R. Williamson, J.R. and Mcdaniel, M.L. (1992) Aminoguanidine, a
novel inhibitor of nitric oxide formation, prevents diabetic vascular dysfunction.
Diabetes 41: 552-556.
Cunningham, A.J. and Szenberg, A. (1968) Further improvements in the plaque
technique for detecting single antibody forming cells. Immunology 14: 599-600.
Davis, D. and Safe, S. (1988) Immunosuppressive activities of polychlorinated
dibenzofuran congeners: quantitative structure-activity relationships and
interactive effects. Toxicol. Appl. Pharmacol. 94: 141-149.
Davis, D. and Safe, S. (1991) Halogenated aryl hydrocarbon-induced suppression of the
in vitro plaque-forming cell response to sheep red blood cells is not dependent on
the Ah receptor. Immunopharm. 21: 183-190.
de Caestecker, M.P., Telfer, B.A., Hutchinson, I.V. and Ballardie, F.W. (1992) The
detection of intracytoplasmic interleukin-la, interleukin-113 and tumour necrosis
factor a expression in human monocytes using two color immunofluorescence
flow cytometry. J. Immunol. Methods 154: 11-20.
Dickson, L.C., Buzik, S.C. (1993) Health risks of "dioxins": a review of environmental
and toxicological considerations. Vet. Hum. Toxicol. 35: 68-77.
Dinarello, C.A. (1988) Biology of Interleukin 1. FASEB J. 2: 108-115
88
Dinarello, C.A., Gelfand, J.A. and Wolff, S.M. (1993) Anticytokine strategies in the
treatment of the systemic inflammatory response syndrome. JAMA 269: 1829­
1835.
Dinarello, C.A. and Thompson, R.C. (1991) Blocking IL-1: interleukin 1 receptor
antagonist in vivo and in vitro. Immunol. Today 12: 404-410.
Dinarello, C.A. and Wolff, S.M. (1993) The role of interleukin-1 in disease. The New
England Journal of Medicine 2;328: 106-113
Dooley, R.K. and Holsapple, M.P. (1988) 1. Elucidation of cellular targets responsible for
tetrachlorodibenzo-p-dioxin (TCDD)-induced suppression of antibody response:
The role of the B lymphocyte Immunopharmacology 16: 167-180. 2. Elucidation
of cellular targets responsible for tetrachlorodibenzo-p-dioxin (TCDD)-induced
suppression of antibody response. 2. Role of the t lymphocyte.
Immunopharmacology 19: 47-58
Fenton, M.J. (1992) Review: Transcriptional and post-transcriptional regulation of
interleukin 1 gene expression. Int. J. Immunopharmac. Vol 14: 3: 401-411
Fingerhut, M.A., Halperin, W.E., Marlow, D.A., Piacitelli, L.A., Honchar, P.A.,
Sweeney, M.H., Greife A.L., Dill, P.A., Steenland, K., Suruda, A.J. (1991) Cancer
Mortality in workers exposed to 2,3,7,8-tetrachlorodibenzo-p-dioxin. N. Engl. J.
Med. 324: 212-218
Fisher, E., Van Zee, K.J., Marano, M.A., Rock, C.S., Kenney, J.S., Poutsiaka, D.D.,
Dinarello, C.A., Lowry, S.F., Moldawer, L.L. (1992) Interleukin-1 receptor
antagonist circulates in experimental inflammation and in human disease. Blood
Vol. 79;9: 2196-2200
Eisenstein, T.K., Huang, D., Meissler, J.J. and Al-Ramadi, B. (1994) Macrophage nitric
oxide mediates immunosuppression in infectious inflammation. Immunobiol. 191:
495-502.
Eskendari, (1990) WEHI 164 subclone 13 assay for TNF: sensitivity, specificity, and
reliability. Immunol. Investigation 19: 69-79.
Exley, A.R. and Cohen, J. (1990) Optimal collection of blood samples for the
measurement of tumor necrosis factor a. Cytokine 2: 353-356.
Gaido, K.W., Leonard, L.S., Maness, S.C., Andersen, M.E. (1991) TCDD-dependent
regulation of gene expression in human keratinocytes. Activities 11; 12:1-8
89
Gaido, K.W. and Maness, S.C. (1994) Regulation of gene expression and acceleration of
differentiation in human keratinocytes by 2,3,7,8-tetrachlorodibenzo-p-dioxin.
Toxicol. Appl. Pharmacol. 127: 199-208.
Gasiewicz, T.A., Neal, R.A. (1979) 2,3,7,8-Tetrachlorodibenzo-p-dioxin tissue
distribution, excretion and effects on clinical chemical parameters in guinea pigs.
Toxicol Appl Pharmacol. 51: 329-339.
Gibaldi, M. (1993) What is nitric oxide and why are so many people studying it? J. Clin.
Pharmacol. 33: 488-496.
Gollapudi, S., Kim, C.H., Patel, A., Sindhu, R., Gupta, S. (1996) Dioxin activates human
immunodeficienty virus-1 expression in chronically infected promonocytic U1
cells by enhancing NF-Kb activity and production of tumor necrosis factor-a.
Biochemical and Biophysical Research Communications 226: 889-894.
Green, L.C., Wagner, D.A., Glogowski, J., Skepper, P.L., Wishnok, J.S. and
Tannenbaum, S.R. (1982) Analysis of nitrate, nitrite and [15N]nitrite in biological
fluids. Anal. Biochem. 124: 131.
Hankinson, Oliver (1995) The aryl hydrocarbon receptor complex. Ann. Rev. Pharmacol.
Toxicol. 35: 307-340.
Hinsdill, R.D., Couch, D.L., Speirs, R.S. (1980) Immunosuppression in mice induced by
dioxin (TCDD) in feed. J Environ Pathol Toxicol 4(2-3): 401-425.
Holsapple, M.P. (1991) A review of 2,3,7,8-tetrachlorodibenzo-p-dioxin-induced change
in innumocompetence: 1991 update. Toxicology 69: 219-255.
Holsapple, M.P., Morris, D.L., Wood, S.C. and Snyder, N.K. (1991) 2,3,7,8­
tetrachlorodibenzo-p-dioxin-induced changes in immunocompetence: possible
mechanisms. Annu. Rev. Pharmacol. Toxicol. 31: 73-100.
Houk, V.N. (1991) Discussion of Vietnam veteran and Agent Orange issues. Bandury
Report 35: 259-276.
House, R.V., Lauer, L.D. and Muarry, M.J. (1990) Examination of immune parameters
and host resistance mechanisms in B6C3F1 mice following adult exposure to
2,3,7,8-tetrachlorodibenzo-p-dioxin. J. Toxicol. Environ. Health 31: 203-215.
Ialenti, A., Ianaro, A., Moncada, S. and Di Rosa, M. (1992) Modulation of acute
inflammation by endogenous nitric oxide. Eur. J. Pharmacol. 211: 177-182.
90
James, R.C., Busch, H., Tamburro, C.H., Roberts, S.M., Schell, J.D., Harbison, R.D.
(1993) Polychlorinated biphenyl exposure and human disease. J. Occup. Med. 35:
136-148.
Johnson, A.U. (1993) Important aspect of the evidence for TCDD carcinogenicity in man.
Environ. Health Perspec. Mar 99: 383-390.
Jung, T., Schauer, U., Huesser, C. Neumann, C. and Rieger, C. (1993) Detection of
intracellular cytokines by flow cytometry. J. Immunol. Methods 159: 197-207.
Kaplan, S.S., Billiar, T.R., Curran, R.D., Zdziarski, U.E., Simmons, R.L. and Basford,
R.E. (1990) Inhibition of chemotaxis with NG-monomethyl-L-arginine: a role for
cyclic GMP. In: Moncada, S., Higgs, A. eds. Nitric oxide from L-arginine: a
bioregulatory system: proceedings of the Symposium on Biological Importance of
Nitric Oxide, London, 1989. Elsevier, Amsterdam 499-500.
Kerkvliet, N.I. (1995) Immunological effects of chlorinated dibenzo-p-dioxins. Environ
Health Perspect 103 (Suppl 9): 47-53.
Kerkvliet, N.I. and Brauner, J.A. (1990) Flow cytometric analysis of lymphocyte
subpopulations in the spleen and thymus of mice exposed to an acute
immunosuppressive dose of 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD).
Environ. Research 52: 146-154.
Kerkvliet, N.I. and Burleson, G.R. (1994) Immunotoxicity of TCDD and related
halogenated aromatic hydrocarbons. In: J.H. Dean, M.I. Luster, A.E. Munson and
I. Kimber (Eds.), Immunotoxicity and Immunopharmacology, Raven Press, Ltd.
New York, pp. 97-121.
Kerkvliet, N.I. and Oughton, J.A. (1993) Acute inflammatory response to sheep red blood
cell challenge in mice treated with 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD):
Phenotypic and functional analysis of peritoneal exudate cells. Toxicol. Appl.
Pharmacol. 119h: 248-257.
Kerkvliet, N.I., Steppan, L.B., Brauner, J.A., Deyo, J.A., Henderson, M.C., Tomar, R.S.
and Buhler, D.R. (1990) Influence of the Ah locus on the humoral
immunotoxicity of 2,3,7,8-tetrachlorodibenzo-p-dioxin: Evidence for Ah­
receptor-dependent and Ah-receptor-independent mechanisms of
immunosuppression. Toxicol. Appl. Pharmacol. 105: 26-36.
Kim, K.U., Kwon, O.J. and Jue, D.M. (1993) Pro-tumor necrosis factor cleavage enzyme
in macrophage membrane/particulate. Immunology 80: 134-139.
91
Kinkhabwala, M., Sehajpal, P., Skolnik, E. Smith, D., Sharma, V.K., Vlassara, H.,
Cerami, A. and Suthanthiran, M. (1990) A novel addition to the T cell repertory:
cell surface expression of tumor necrosis factor/cachetin by activated normal
human T cells. J. Exp. Med. 171: 941-946.
Kubes, P., Suzuki, M. and Granger, D.N. (1991) Nitric oxide: An endogenous modulator
of leukocyte adhesion. Proc. Natl. Acad. Sci. USA 88: 4651-4655.
Lai, Z.W., Pineau, T., Esser, C. (1996) Identification of dioxin-responsive elements
(DREs) in the 5' regions of putative dioxin-inducible genes. Chemico-Biological
Interactions 100: 97-112
Lantz, M., Bjornberg, F., Olsson, I., Richter, J. (1994) Adherence of neutrophils induces
release of soluble tumor necrosis factor receptor forms. J. Immunol. 152: 1362
Lejeune, P., Lagadec, P., Onier, N., Pinard, D., Ohshima, H. and Jeannin, J.F. (1994)
Nitric oxide involvement in tumor-induced immunosuppression. J. Immunol. 152:
5077-5083.
Lentnek, M., Griffith, 0.W., Rifkind, A.B. (1991) Tetrachlorodibenzo-p-dioxin increases
reliance on fats as a fuel souce independently of diet: evidence that diminished
carbohydrate supply contributes to dioxin lethality. Biochemical and Biophysical
Research Communication 174;3: 1267-1271
Liew, F.Y. (1994) Regulation of nitric oxide synthesis in infectious and autoimmune
diseases. Immunol. Letters 43: 1-2.
Lin, W.Q. and White, K.L. (Jr.) (1991) Suppression of serum C3 production by TCDD is
not due to a direct effect on hepatocytes. A paper: TCDD Abstracts Eastern
Regional Symposium on Mechanisms of Immunotoxicity.
Lucier, G.W., Portier, C.J., Gallo, M.A. (1993) Receptor mechanisms and dose-response
models for the effects of dioxins. Environ. Health Perspect. 101:34-44
Luster, M.I., Germolec, D.R., Clark, G., Wiegand, G., Rosenthal, G.J. (1988) Selective
effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin and corticostroid on in vitro
lymphocyte maturation. J. Immunol. 140: 928-935
Manthey, C.L., Perera, P., Salkowski, C.A.,and Vogel, S.N. (1993) Taxol provides a
second signal for murine macrophage tumoricidal activity. J. Immunol. 152: 825­
831.
92
Mantovani, A., Vecchi, A., Luini, W., Sironi, M., Candiani, G.P., Speafico, F., Garattini,
S. (1980) Effect of 2,3,7,8-tetrachlorodibenzo-p-dioxin on macrophage and
natural killer cell mediated cytoxicity in mice. Biomedicine 32: 200-204
Massa, T., Esmaeili, A., Fortmeyer, H., Schlatterer, B., Hagenmaier, H. and Chandra, P.
(1992) Cell transforming and oncogenic activity of 2,3,7,8-tetrachloro- and
2,3,7,8- tetrabromodibenzo-p-dioxin. Cancer Research 12: 2053-2060.
McIntyre, K.W., Stepan, G.J., Kolinsky, K.D., Benjamin, W.R., Plocinski, J.M., Kaffka,
K.L., Campen, C.A., Chizzonite, R.A. and Kilian, P.L. (1991) Inhibition of
interleukin 1 (IL-1) binding and bioactivity in vitro and modulation of acute
inflammation in vivo by IL-1 receptor antagonist and anti-IL-1 receptor
monoclonal antibody. J. Exp. Med. 173: 931-939.
Miller, M.J.S., Sadowska-Krowicka, H., Chotinaruemol, S., Kakkis, J.L. and Clark, D.A.
(1993) Amelioration of chronic ilieitis by nitric oxide synthase inhibition. J.
Pharmacol. Exper. Therap. 264: 11-16.
Misko, T.P., Moore, W.M., Kasten, T.P., Nickols, G.A., Corbett, J.A., Tilton, R.G.,
McDaniel, M.L., Williamson, J.R. and Currie, M.G. (1993) Selective inhibition of
the inducible nitric oxide synthase by aminoguanidine. J. Pharmacol. 233: 119­
125.
Mohler, K.M., Torrance, D.S., Smith, C.A., Goodwin, R.G., Stremler, K.E., Fung, V.P.,
Madani, H., Widmer, M.B. (1993) Soluble tumor necrosis factor (TNF) receptors
are effective therapeutic agents in lethal endotoxemia and function simultaneously
as both TNF carriers and TNF antagonists. J. Immunol. 151: 1548-1561 No. 3.
Moncada, S., and Higgs, A. (1993) The L-arginine- nitric oxide pathway. N. Engl. J.
Med. 329: 2002-2012.
Moncada, S., Palmer, R.M.J. and Higgs, E.A. (1991) Nitric oxide: Physiology,
pathophysiology, and pharmacology. Pharmacol. Reviews 43: 109-142.
Moos, A.B., Baecher-Steppan, L. and Kerkvliet, N.I. (1994) Acute inflammatory
response to sheep red blood cells in mice treated with 2,3,7,8-tetrachlorodibenzo­
p-dioxin: The role of the inflammatory cytokines, IL-1 and TNF. Toxicol. Appl.
Pharmacol. 127: 331-335.
Moos, A.B. and Kerkvliet, N.I. (1995) Inhibition of tumor necrosis factor activity fails to
restore 2,3,7,8-tetrachlorodibenzo-p-dioxin (TCDD)-induced suppression of the
antibody response to sheep red blood cells. Tox. Letters 81: 175-181.
93
Morris, D.L. and Holsapple, M.P. (1991) Effects of 2,3,7,8-tetrachlorodibenzo-p-dioxin
(TCDD) on humoral immunity: II b cell activation. Immunopharmacology 21:
171-182.
Mulligan, M.S., et al. (1991) Tissue injury caused by deposition of immune complexes is
L-arginine dependent. Proc. Natl. Acad. Sci. USA 88: 6338-6342.
Nebert, D.W., Jenson, N.M., Perry, J.W., Oka, T (1990) Association between ornithine
decarboxylase induction and the Ah locus in mice treated with polycyclic
aromatic hyrdocarbons. J. Biol. Chem. 255: 6836-6842.
Nebert, D.W., Puga, A. Vasiliou, V. (1993) Role of the Ah receptor and the Dioxininducible (Ah) gene battery in toxicity, cancer, and signal transduction. Annals
New York Acad. Sciences 685: 624-640.
Olnes, M.J., Verma, M., Kurl, R.N. (1994) 2,3,7,8-tetrachlorodibenzo-p-dioxin-mediated
gene expression in the immature rat thymus. Exp. Clin. Innunogenet 11: 102-109.
Peppel, K., Crawford, D. and Beutler, B. (1991) A tumor necrosis factor (TNF) receptorIgG heavy chain chimeric protein as a bivalent antagonist of TNF activity. J. Exp.
Med. 174: 1483-1489.
Pollenz, R.S., Sattler, C.A., Poland, A. (1994) The aryl hydrocarbon receptro and aryl
hyrdocarbon receptor nuclear translocator protein show distinct subcellular
localizations in Hepa lcic7 cells by immunofluorescence microscopy. Mol.
Pharmacol 45: 428-438.
Poland, A. and Knutson, J.C. (1982) 2,3,7,8-Tetrachlorodibenzo-p-dioxin and related
halogenated aromatic hydrocarbons: examination of the mechanism of toxicity.
Annu. Rev. Pharmacol. Toxicol. 22: 517-554.
Puhvel, S.M., Sakamoto, M. (1988) Effect of 2,3,7,8-tetrachlorodibenzo-p-dioxin on
murine skin. J. Invest. Dermatol. 90: 354-358.
Puga, A.N., Nebert, D.W., Carrier, F. (1992) Dioxin induces expression of c-fos and c­
jun proto-oncogenes and a large increase in transcription factor. AP-1 DNA Cell.
Biol. 11: 269-283.
Pradines-Figueres, A. and Raetz, C.R.H. (1992) Processing and secretion of tumor
necrosis factor a in endotoxin-treated mono mac 6 cells are dependent on phorbol
myristate. J. Biol. Chem. 267: 23261-23268.
94
Rifkind, A.B., Gannon, M., and Gross, S.S. (1990) Arachodonic acid metabolism by
dioxin-induced cytochrome P-450: a new hypothesis on the role of P-450 in
dioxin toxicity. Biochem. Biophys. Res. Comm. 172: 1180-1188.
Rodriquez, C., Roldan, E., Navas, G. and Brieva, J.A. (1993) Essential role of tumor
necrosis factor-a in the differentiation of human tonsil in vivo induced B cells
capable of spontaneous and high-rate immunoglobulin secretion. Eur. J. Immunol.
23: 1160-1164.
Rot, Antal (1992) Endothelial cell binding of NAP-1/IL-8: role in neutrophil emigration.
Immunology Today 13;8: 291-294.
Rowland, R.R., Butz, E.A., Plagemann, P.G.W. (1994) Nitric oxide production by splenic
macrophages is not responsible for T cell suppression during acute infection with
lactate dehydrogenase-elevating virus. J. Immunol. 152: 5785-5795.
Rutherford, M.S., Witsell, A., Schook, L.B. (1993) Mechanisms generating functionally
hetergenous macrophages: chaos revisited. J. Leukoc. Biol. 53: 602-818.
Safe, S. (1990) Polychlorinated biphenyls (PCBSs), dibenzo-p-dioxins (PCDDs),
dibenzofurans PCDFs), and related compounds: environmental and mechanistic
considerations which support the development of toxic equivalency factors. Crit.
Rev. Toxicol. 21: 51-88.
Salvemini, D., Wang, Z.Q., Wyatt, P.S., Bourdon, D.M., Marino, M.H., Manning, P.T.,
Currie, M.G. (1996) Nitric oxide: a key mediator in the early and late phase of
carrageenan-induced rat paw inflammation. British Journal of Pharmacology 118:
829-838.
Sander, B., Andersson, J. and Andersson, U. (1991) Assessment of cytokines by
immunofluorescence and the paraformaldehyde-saponin procedure. Immunol.
Reviews 119: 65-93.
Sayers, T.J., Wiltrout, T.A., Bull, C.A., Denn, A.C., Pilaro, A.M., and Lokesh, B. (1988)
Effect of cytokines on polymorphonuclear neutrophil infiltration in the mouse. J.
Immunol. 141: 1670-1677.
Schecter, A., Startin, J., Wright, C., Kelly, M., Papke, 0., Lis, A., Ball, M. Olson, J.R.,
(1994) Congener-specific levels of dioxin and dibenzofurans in US food and
estimated daily dioxin toxic equivalent intake. Environ. Health Perspec. 102;11:
962-966
95
Sherry, B. and Cerami, A. (1988) Cachectin/tumor necrosis factor exerts endocrine,
paracrine and autocrine control of inflammatory responses. J. Cell Bio. 107: 1269­
1277.
Sparrow, B.R., Thompson, C.S., Ryu, B.W., Selevonchick, D.P., Schaup, H.W. (1994)
2,3,7,8-tetrachlorodibenzo-p-dioxin induced alterations of pyruvate carboxlyase
levels and lactate dehydrogenase isozyme shifts in C57BL/6J male mice. J.
Biochem. Tox. 9;6: 329-335.
Stein, M., and Keshave, S. (1992) The versatility of macrophages. Clinical and
Experimental Allergy 22: 19-27.
Steppan, L.B. and Kerkvliet, N.I. (1991) Influence of 2,3,7,8-tetrachlorodibenzo-p-dioxin
(TCDD) on the production of inflammatory cytokine mRNA by C57B1/6
macrophages. Toxicologist 11: 35 (abst.).
Sutter, T.R., Guzman, K., Dold, K.M. and Greenlee, W.F. (1991) Targets for dioxin:
genes for plasminogen activator inhibitor-2 and interleukin-lp. Science 254: 415­
418.
Taylor, M.J., Lucier, G.W., Mahler, J.F., Thompson, M., Lockhart, A.C. and Clark, G.C.
(1992) Inhibition of acute TCDD toxicity by treatment with anti-tumor necrosis
factor antibody or dexamethasone. Toxicol. Appl. Pharmacol. 117: 126-132.
Theobold, H.M., Moore, R.W., Katz, L.B., Pieper, R.O., and Peterson, R.E. (1983)
Enhancement of carrageenan and dextran-induced edemas by 2,3,7,8­
tetrachlorodibenzo-p-dioxin and related compounds. J. Pharmacol. Exp. Therap.
225: 576-583.
Tracey, K.J., and Cerami, A. (1993) Tumor necrosis factor, other cytokines and disease.
Annu. Rev. Cell Bio. 9: 317-343.
Vanden Heuvel, J.P. and Lucier, George (1993) Environmental toxicology for
polychlorinated dibenzo-p-dioxins and polychlorinated dibenzofurans.
Environmental Health Perspectives 100: 189-200.
Van Zee, K.J., Deforge, L.E., Fischer, E., Marano, M.A., Kenney, J.S., Remick, D.G.,
Lowry, S.F., Moldawer, L.L. (1991) IL-8 in septic shock, endotoxemia, and after
IL-1 administration. J. Immunol. 146: 3478-3482.
96
Van Zee, K. J., Kohno, T., Fischer, E. Rock, C.S., Moldawer, L.L., and Lowry, S.F.
(1992) Tumor necrosis factor soluble receptors circulate during experimental and
clinical inflammation and can protect against excessive tumor necrosis factor a in
vitro and in vivo. Proc. Natl. Acad. Sci. 89: 4845-4849.
Vassal li, P. (1992) The pathophysiology of tumor necrosis factors. Annu. Rev. Immunol.
10: 411-452.
Vecchi, A., Mantovani, A., Sironi, M., Luini, M., Cairo, M. and Garattini, S. (1980)
Effect of acute exposure to 2,3,7,8-tetrachlorodibenzo-p-dioxin on humoral
antibody production in mice. Chem. Biol. Interact. 30: 337-341.
Vogel, C. and Abel, J. (1995) Effect of 2,3,7,8-tetrachlorodibenzo-p-dioxin on growth
factor expression in the human breast cancer cell line MCF-7. Arch Toxicol. 69:
259-265.
Vos, J.G., Luster, M.I. (1989) Immune alterations. In: Halogenated Biphenyls,
Terphenyls, Napthalenes, Dibenzodioxins and Related Products. R.D. Kimbrough
and A.A. Jensen, Ed. Elsevier Science Publishers B.V., Amsterdam, pp. 295-322.
Vos, J.G., van Loveren, H., Shuurman, H.J. (1991) Immunotoxicity of dioxin: immune
function and host resistance in laboratory animals and humans. In: Banbury
report 35: biological basis for risk assessment of dioxins and related compounds.
Gallo, M.A., Scheuplein, R.J., van der Heijden, K.A., Eds. Cold Spring Harbor
Press, New York, pp. 79-93.
White, K.L., Lysy, H.H., McCay, J.A., Anderson, A.C. (1986) Modulation of serum
complement levels following exposure to polychlorinated dibenzo-p-dioxins.
Toxicol Applied Pharmacol. 84: 209-219.
Whitlock, J.P. (1990) Genetic and molecular aspects of 2,3,7,8-tetrachlorodibenzo-p­
dioxin action. Annu. Rev. Pharmacol. Toxicol. 30: 251-277.
Whitlock, J.P. (JR)(1993) Mechanistic aspects of dioxin action. Chem. Res. Toxicol.
6;6:758.
Wooley, P.H., Dutcher, J., Widmer, M.B. and Gillis, S. (1993) Influence of a
recombinant human soluble tumor necrosis factor receptor FC fusion protein on
type II collagen-induced arthritis in mice. J. Immunol. 151: 6602-6607.
Xie, Q., Cho, H.J., Calaycay, J., Mumford, R.A., Swiderek, K.M., Lee, T.D., Ding, A.,
Troso, T., Nathan, C. (1992) Cloning and characterization of inducible nitric
oxide synthase from mouse macrophages. Science 256: 225-228.
97
Yin, H., Li, Y., Sutter, T.R. (1994) Dioxin-enhanced expression for interleukin-1P in
human epidermal keratinocytes: potential role in the modulation of immune and
inflammatory responses. Exp. Clin. Ummunogenet 11: 63-64.